Abstract
Geographic disparities in adult mortality within the US have grown over the past several decades, but the reasons for these trends remain unclear. In this article, we examine trends in adult mortality (ages 55+) across US states from 1977-2017, paying close attention to the shifting geographic pattern of high- and low-mortality states. We find that states in the South tended to fall behind the rest of the country in the 1970s and 1980s, while states in the Great Plains and Mountain West tended to fall behind in the 1990s, 2000s, and 2010s. In contrast, states on the East and West Coasts have tended to see considerable improvement in mortality. We consider the role of state-level per-capita spending on public welfare programs in the mortality experience of states between 1977 and 2017. We use fixed effects models to show that greater state welfare generosity predicts greater yearly reductions in mortality. State shifts toward more generous welfare spending regimes may contribute to significant geographic divergences in adult mortality in the United States.
Introduction
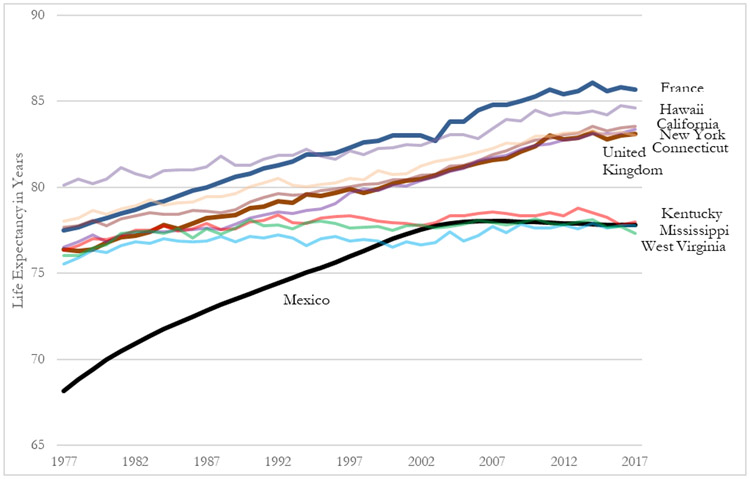
The growing crisis of American life expectancy—exemplified by the recent multi-year decline and the growing gap between the United States and other high-income countries—has recently been contextualized within the unique geographic pattern of health and morality in the US (Woolf and Schoomaker, 2019). Life expectancy gains in the United States have been sluggish relative to other high-income countries for at least the last four decades, but the gap has accelerated in recent years following the life expectancy decline in the US (Case and Deaton, 2015; Division, 2017; Mehta et al., 2020). In addition, since the 1960s and 1970s, mortality declines in many southern US states have not kept pace with those in the Northeast and West, giving rise to the well-documented “southern disadvantage” in adult mortality (Author, 2013; Montez et al., 2016). Since the 1980s, the geographic divergence in US mortality has been two-sided, combining sluggish or non-existent mortality improvement among southern states with rapid improvements in mortality in states on the East and West Coasts (Elo et al., 2019; Author et al., 2019; Vierboom et al., 2019). As a result, some American states (for example, California and New York) have life expectancies that resemble those in Western Europe, while other states (for example, West Virginia and Mississippi) have life expectancies similar to that of Mexico (Figure 1).
Figure 1:
Selected State Trends in Life Expectancy Compared to France, the United Kingdom, and Mexico: 1977-2017
Notes: US state life expectancy figures come from the United States Mortality Database (2020). Life expectancy figures for France, the United Kingdom, and Mexico come from the World Bank (https://data.worldbank.org/indicator/SP.DYN.LE00.FE.IN)
Understanding the causes of these changing fortunes is critically important. We argue that state government liberalism, and particularly the different social welfare policies that liberal and conservative state governments pursue, is likely to explain some of this variation in state mortality outcomes. State government liberalism reflects whether government policy preferences are left-leaning or right-leaning, with more left-leaning governments being more liberal. State government liberalism or leftism is likely important for mortality outcomes because systematic review of cross-national research shows that left-leaning parties and the policies that they champion are associated with lower mortality rates across high-income countries (Barnish et al., 2018). Navarro et al. (2006, 2003) find that governments controlled by left parties are associated with greater health expenditures and that support for left-leaning parties in the electorate is positively associated with life expectancy. Beckfield and Bambra (2016) find that the U.S. mortality disadvantage compared to other high-income countries can be attributed to the less generous American welfare state. Similarly, Montez et al. (2020) find that states that adopt liberal policies tend to have higher life expectancies than states with more conservative policies.
One way, but certainly not the only way, that more liberal governments can improve population health is through increased spending on social welfare programs (Avendano and Kawachi, 2014; Beckfield and Bambra, 2016). This is especially relevant to the mortality experience of US states because, since the late 1970s, evidence suggests that states have taken on an increasing role in policy innovation and in addressing U.S. social problems (Author et al., 2018; Grumbach 2018; Hertel-Fernandez 2019). States have substantial authority over the form and generosity of welfare programs (Michener, 2018), and currently exhibit significant variation in per-capita expenditures on major welfare programs that provide cash assistance, food support, and health care to low-income families. For each of these programs the states play an important role in determining program eligibility, identifying and enrolling eligible people, and determining benefit generosity. Each role presents opportunities for states to expand or reduce program utilization, and thus benefits, among potential recipients (Herd and Moynihan, 2019).
The largest public welfare programs with significant state discretion are Medicaid (health insurance for low-income people), the Children’s Health Insurance Program (CHIP, which provides health insurance for lower-income children whose family income falls just above the threshold for Medicaid), and Temporary Assistance to Needy Families (TANF, which provides cash assistance to the poor).1 Research shows that left-leaning state governments are more generous with these programs and pursue a more equitable distribution of economic and social goods (Author et al., 2018; Author et al., 2018). In the case of Medicaid and CHIP, more liberal states have long opted to cover larger populations through Medicaid waivers (Center on Budget and Policy Priorities, 2020; Grogan, 1994), and states with Democratic governors have more generous state CHIP programs (Brooks, 2018; Grogan and Rigby, 2009). Furthermore, liberal state governments were more likely to opt in to expansion as part of the Affordable Care Act (ACA) (Hertel-Fernandez, 2019; Hertel-Fernandez et al., 2016). As a result, liberal states tend to have greater “welfare generosity” as it is usually called in the cross-national policy literature. That is, liberal states spend more per capita on welfare than conservative states (Beckfield and Bambra, 2016; Author et al., 2018; Author et al., 2010).
Despite the fact that public welfare programs often provide assistance to individuals and families across the life course, many studies have focused on their effects on health and mortality outcomes in particular age groups. During the introduction and initial expansion of Medicaid in the 1960s, those that became eligible early experienced reduced infant mortality, better health and mortality in later life, reduced rates of disability, and improved labor market outcomes in adulthood (Boudreaux et al., 2016; Boudreaux and Lipton, 2021; Goodman-Bacon, 2018; Sohn, 2017). Furthermore, ACA Medicaid expansion led to reductions in mortality and improvements in health and health care access in expanding states (Borgschulte and Vogler, 2020; Sommers, 2017; Wherry and Miller, 2016). Findings are similar for other programs although there has been less research. Leonard and Mas (2008) find that the introduction of time limits for TANF led to an increase in infant mortality. Additionally, individuals who grew up in states that adopted the food stamp program earlier experienced better health and labor market outcomes in adulthood (Hoynes et al., 2016). At the state level, increases in state SNAP generosity are associated with reduced male suicide rates (Rambotti, 2020). Bradley and colleagues (2016) found that states that spent more on nutrition and income support, conditional on health care spending, had lower prevalence of chronic conditions (2016). Beyond state welfare programs, more progressive state programs such as more generous Earned Income Tax Credit (EITC) and paid family leave are associated with improved health outcomes (Hamad and Niedzwiecki, 2019; Herd, 2016; Lee et al., 2020). More liberal policy orientations at the state level across a large number of policy domains are associated with increased life expectancy (Montez et al., 2020), but it remains unclear whether social spending itself is an important factor.
In this study we examine state-level trends in adult mortality from 1977-2017, focusing specifically on the role of per capita public welfare spending. Combining data on US vital statistics, state government liberalism, state spending data and US census characteristics, we confirm that more liberal governments spend more per-capita on welfare or social programs and, in turn, find that these expenditures are also associated with better mortality outcomes for adults aged 55 and above. These findings have important implications for understanding diverging mortality fortunes and potential solutions for states that are doing poorly. Our findings also show the potential dangers of a fragmented and unequal welfare state in the context of U.S. federalism.
Data and Methods
As noted, to investigate the relationship between welfare generosity and state trends in morality we combine data on state mortality, state government liberalism, state government expenditures, and state economic and demographic characteristics. All state-level variables are measured annually from 1977 to 2017. A description of sources for individual state-level variables is shown in Table B1.
Outcome Variable: State Adult Mortality
Our mortality data come from United States vital statistics provided by CDC Wonder (Centers for Disease Control and Prevention, 2018). These data provide all-cause age-adjusted death rates by state of residence for men and women at adult ages (55+) in each year from 1977-2017. These death rates are standardized to the 2000 US standard population in order to account for changes in population age structure across states and over time. We examine all-cause mortality to avoid issues with state differences in cause of death coding (Maresh et al., 2012; Patnaik et al., 2011), and because welfare spending may have effects on a wide variety of causes of death. We focus on adult mortality since the majority of deaths occur after age 55 (Crimmins et al., 2011) and the causes of mortality are more likely to reflect chronic disease patterns, senescent mortality, and healthy aging, which is an important target of public policy. This goal is also distinct from recent research focused on the concerning rise in mortality among non-Hispanic white adults ages 45-54 (Case and Deaton, 2015). To the extent that welfare spending improves healthcare access and utilization, deaths at older ages are also more likely to be responsive to changes in welfare generosity (Sommers et al., 2014). In sensitivity analyses (Table C4), we consider death rates for different age categories, including all ages, where we find generally consistent results.
Explanatory Variable: State Government Liberalism
We use a measure of government ideology from Berry et al. (1998). This index ranges from 0-100 indicating the level of policy liberalism views of the state government (governor and legislature). This measure combines information about both the partisan control of state institutions of government as well as the left-right ideological position of the two major parties using information about the ideology of the state’s party representatives in the U.S. Congress so that the parties can be placed on a single ideological dimension. In prior work, the liberalism index has been shown to be a robust predictor of numerous policy outcomes we would expect of more liberal governments, such as more stringent campaign finance laws and more expansive welfare policies (Berry et al., 2010; Fellowes and Rowe, 2004; Author, 2007).2
Explanatory Variable: State Welfare Generosity
We incorporate information on state-level welfare expenditures from the Government Finance Database (Pierson et al., 2015), which uses US Census Bureau Government Finance and Employment codes to categorize state spending categories in each year. Expenditure data are provided annually 1977-2017; annual state expenditure data are not available prior to 1977. We measure welfare generosity using total per-capita expenditures on programs that provide cash assistance, health insurance and care, or in-kind benefits to the poor. The largest such programs are Medicaid, CHIP, TANF (previously AFDC), and SNAP (discussed above). For each of these programs federal aid is given to the states by formula, and then states must also spend a portion of their funds. Because state policies and administrative decisions affect not only generosity of programs, but also the number of enrollees, states have considerable discretion over the amount of money that they spend from their own treasuries, and to a substantial extent, the aid that they receive from the federal government, because by expanding the number of program enrollees states receive more money from the federal government. We adjust per-capita expenditures for inflation and report values in thousands of 2017 dollars.
State Controls
We also include characteristics of the economic and demographic circumstances of states from the US Census and Bureau of Labor Statistics that might be associated with changes in welfare generosity and mortality. We include the poverty rate, median wage income, percent married, median age, population size, unemployment rate, and percent black or African-American. We do not control for state health insurance coverage or total program enrollment, because these are likely to be mechanisms through which welfare generosity affects mortality (Boudreaux and Lipton, 2021). Descriptive characteristics of state-level variables are shown in Appendix Table B2.
Analytical Strategy
Our analytical strategy involves three steps. First, we examine state-level mortality trends and the realignment of the geographic pattern of adult mortality since 1977. Second, we assess the relationship between state government liberalism and mortality. Finally, we examine the relationship between state welfare generosity and adult mortality over time. Because welfare generosity is a policy choice that has been found to shape mortality and it is something that varies across the states based on state liberalism, we consider it as a mechanism translating government liberalism into divergent mortality outcomes across the states.
We use fixed-effects panel regression to predict all-cause mortality as a function of state-level spending on public welfare programs (Rambotti, 2020). These models examine whether spending is associated with mortality, within states and adjusting for year-specific effects. Fixed-effects models effectively control for unobserved time-invariant characteristics of states, such as culture, climate etc., that may affect mortality in each year. State fixed-effects cannot address changes over time, and year fixed-effects cannot fully account for state-specific trends in predictors and outcomes. But such models have become an important part of the toolkit for examining the macro impacts of state-level policies.
Because the key outcome and predictor variables demonstrated the presence of a unit root, we use a single equation error-correction model, in which each predictor is represented in the regression model with both the lagged level and first-differenced term.3 These models are commonly used with dynamic data that is integrated or near-integrated (Enns et al., 2016), and also frequently used in panel data applications (e.g. Author et al., 2018). We also examined the data to determine that there is at least weak exogeneity of welfare spending and government liberalism with respect to mortality (i.e. short-term lags of welfare spending and liberalism predict mortality, but mortality does not predict spending or liberalism, net of controls), which is required for unbiased coefficients, using the approach recommended by Charemza and Deadman (1992).4 Our models predict adult death rates (ages 55+) by state and year
Where Dit is the first-difference of the all-cause age-adjusted death rate at ages 55+ in state i and year t, Wit is the state welfare generosity (public welfare expenditures per capita in $1,000s of 2017 dollars), Xit is a vector of state economic and demographic controls, i is a state fixed effect, t a year fixed effect, and ϵit is a normally-distributed error term. We include the lagged death rate (t − 1 ) and the first difference (Δ) and lagged values of our primary independent variables in the model. We run this model separately for men and women. Although these models lag welfare generosity by one year, it is possible that the effects of spending may take slightly longer to emerge. We experiment with different lag lengths in Appendix Table C7.
Results
U.S. State Mortality and Patterns of Divergence 1977-2017
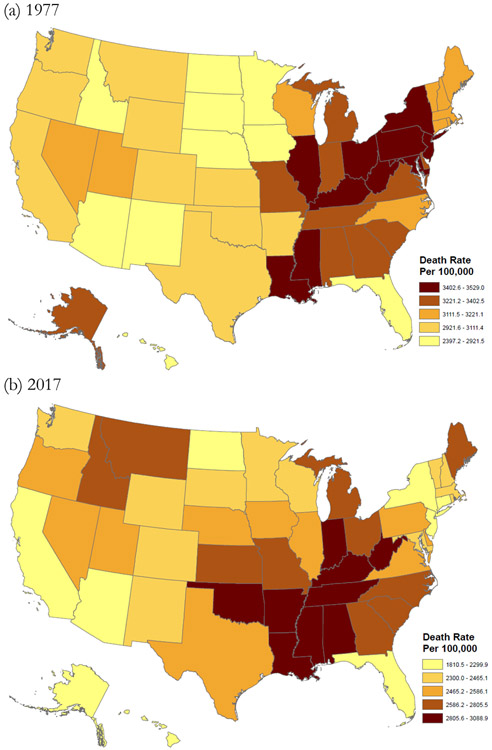
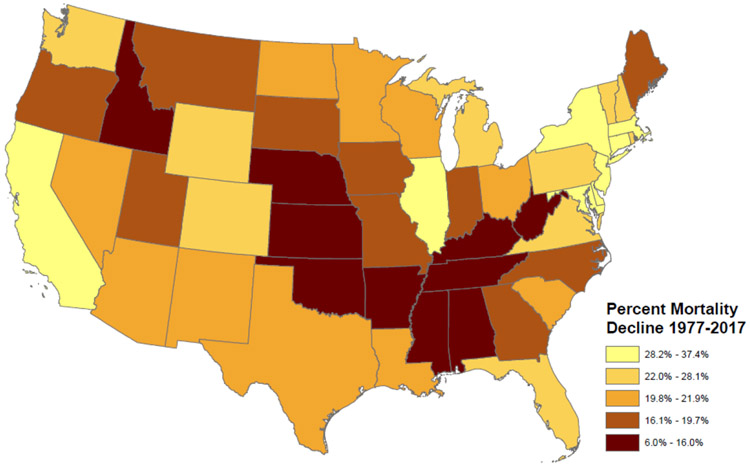
Since 1977, there has been a significant realignment of the geographic pattern of adult mortality in the United States (Figure 2). The current geographic pattern of US adult mortality—rather than being a persistent pattern of regional inequality—reflects trends of the past 40 years. Although much of the focus in the literature has been on the relatively poor performance of southern states, it is notable that states on the East and West Coasts have experienced significant progress in reducing adult mortality (Population Reference Bureau, 2018). The top performers are increasingly concentrated on the coasts while the South, Great Lakes, and Great Plains have begun to fall behind.
Figure 2:
Female Age-Adjusted Death Rate Ages 55+ 1977 and 2017
Source: CDC Wonder
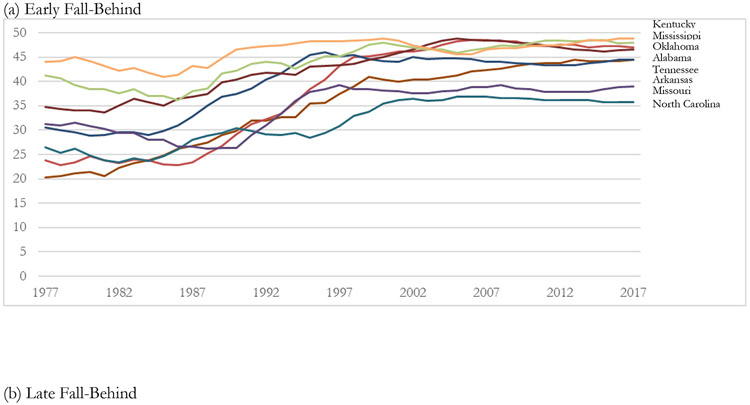
Figure 3 presents changes in the mortality ranking (1=lowest mortality, 50=highest mortality) of selected states from 1977-2017 among women ages 55+ (similar patterns for men).5 In Figure 3 panel a, states in the South—termed Early Fall-Behind—have seen sluggish mortality improvement and have sunk to the bottom of the rankings during the 1970s and 1980s. As a result, the cluster of mortality disadvantage in the US South has become increasingly concentrated. States in the Great Plains and Mountain West (Figure 3 panel b, Late Fall-Behind) have experienced slow mortality decline since the 1990s and have fallen in the rankings. Idaho, Iowa, Kansas, Montana, and Nebraska were in the top 10 in the rankings in the early 1990s but have since fallen. In contrast, states on the East and West Coasts (Figure 3 panel c) have seen tremendous mortality reductions and have risen in the rankings (Coastal Improvement). New York, New Jersey, Maryland, Pennsylvania, Delaware, Connecticut, California and Massachusetts each rose more than 14 spots in the rankings between 1977 and 2017.
Figure 3:
Trends in Female Mortality Ranks Among Selected States 1977-2017
Notes: Mortality ranks run from 1=lowest mortality to 50=highest mortality. Graphs show 3-year moving averages of ranks 1977-2017.
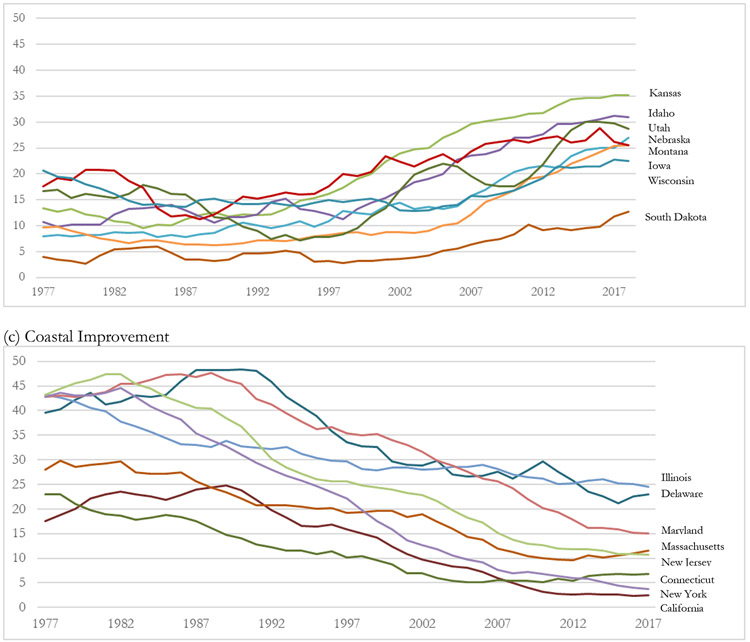
The rankings in Figure 3 somewhat mask absolute and relative differences in death rates between states during the 1977-2017 period. Over this period, the gap between the top-performing states and lowest-performing states has grown. The largest mortality declines occurred in liberal, coastal states—adult mortality fell by more than 30% among women and more than 40% among men in New York, New Jersey, California, Maryland, and Connecticut (Figure 4). In Oklahoma, Arkansas, Tennessee, Alabama, and Kentucky, mortality declined by less than 12% among women and less than 30% among men.
Figure 4:
Percent Decline in Female Age-Adjusted Death Rate Ages 55+ 1977-2017
Source: Authors’ Calculations from CDC Wonder.
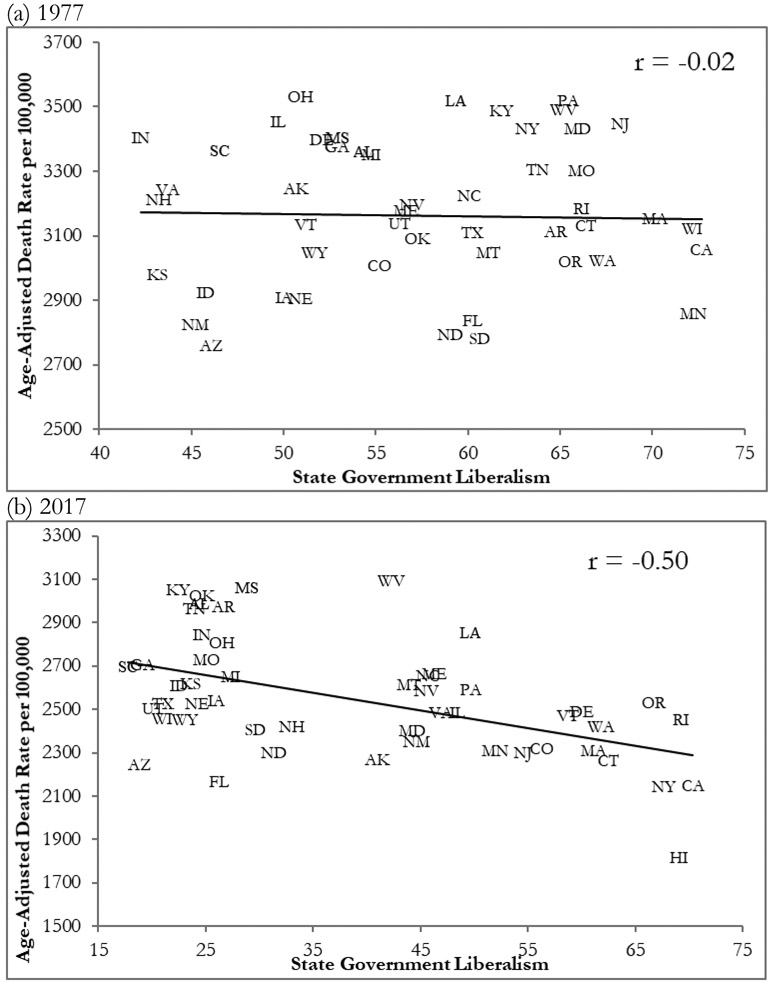
State Political Divergences and Growing Political Divides
The outcome of 40 years of mortality shifts is that the contemporary pattern of US adult mortality is strongly patterned both by geography and by state politics. Conservative states are heavily represented among the highest-mortality states. Particularly since the mid-1990s, liberal states are increasingly represented among the top mortality performers. Figure 5 Shows the relationship between state government liberalism and female adult mortality in 1977 and 2017. In 1977, there was no relationship between state government liberalism and mortality. By 2017, this had transformed into a strong negative relationship (r = −0.5). Fixed-effects models in Appendix Table C2 show that state government liberalism is a robust predictor of adult mortality over this period.
Figure 5:
Relationship between State Government Liberalism and Adult Mortality 1977 and 2017
Notes: State government liberalism index from Berry et al. (1998) and incorporates state legislature and governor ideology. Death rate data from CDC Wonder.
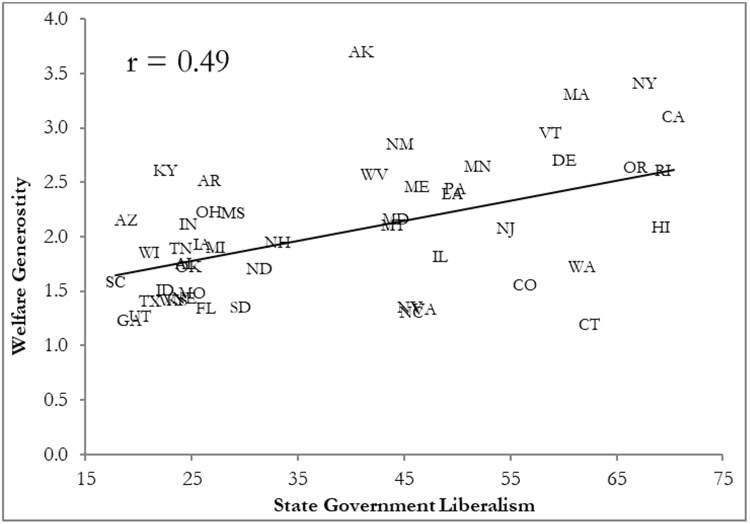
State-Level Welfare Generosity and Mortality
Welfare generosity varies substantially across states and offers a potential mechanism linking state government liberalism to the divergence in US mortality. Although welfare generosity is not strongly related to the poverty rate or median income (Appendix D), more liberal states tend to have greater welfare generosity (Figure 6), which may help to explain the emerging political divide in mortality. Fixed-effects models in Appendix Table C3 demonstrate that state government liberalism is a consistent predictor of welfare spending (including Medicaid), but not spending on other health programs or hospital spending.
Figure 6:
State Government Liberalism and Welfare Generosity 2017
Notes: State government liberalism index from Berry et al. (1998) and incorporates state legislature and governor ideology. Welfare generosity is total state public welfare expenditures per-capita in thousands of 2017 dollars.
Compare the experiences of New York and Nebraska. Although most states have seen increases in welfare generosity since the late 1970s, New York has consistently had relatively generous welfare spending, including $3,400 per capita in 2017. New York also saw significant improvements in its mortality rank over this period. New York women rose from being ranked 43rd in 1977 to ranked 2nd in 2017 in terms of adult mortality. A similar pattern of increased welfare generosity and improved mortality rank can be seen in other coastal states including Massachusetts, California, Delaware, and Maryland.
In contrast, Nebraska spent only $1,434 per capita in 2017, and has shown no real change in per capita welfare spending since 2004. At the same time, Nebraska has gradually fallen in the mortality rankings; Nebraska women consistently ranked in the top 10 in the 1970s and 1980s, but since declined to number 26. Similar spending and mortality trends are found in Kansas, Alabama, Missouri, North Carolina, and Utah, among other states.
In Table 1, we present the results of fixed-effects panel regression models predicting annual changes in the age-adjusted death rate (ages 55+ per 100,000) as a function of welfare generosity (results in Appendix Table C4 show similar results for other age groups). The coefficients denote the effect of $1,000 increase in per-capita spending on the additional annual change in the death rate. An increase in welfare generosity is associated with large declines in the death rate for both women and men (p<0.05 for both). Although the coefficient magnitude is larger for men, reflecting greater declines in mortality for men during this period, the standardized beta coefficients are very similar. Both indicate that a standard deviation increase in welfare generosity is associated with around one-sixth to one-fifth of a standard deviation change in the annual mortality decline. The magnitude of the coefficients also reflects the fact that while year-to-year changes in mortality are relatively modest, overall declines between 1977 and 2017 are substantial, as shown in Figure 4.6
Table 1:
Fixed Effects Panel Regression Models Predicting Adult Death Rate as a function of Welfare Generosity 1977-2017
| First Difference Female Death Rate Ages 55+ |
First Difference Male Death Rate Ages 55+ |
|
|---|---|---|
| Lagged Welfare Generosity ($1,000s) | −23.31* (10.83) beta=−0.1670 |
−41.08* (17.01) beta=−0.2032 |
| State & Year Fixed Effects | Yes | Yes |
| State Controls | Yes | Yes |
| Lagged Mortality | Yes | Yes |
| N | 2,000 | 2,000 |
Notes: All models include lagged and first-difference values of the independent variables. Robust standard errors in parentheses. Beta coefficients are standardized to standard deviation increase. Models include state and year fixed effects and one-year lagged mortality. Models adjust for state characteristics: Percent non-Hispanic white, percent married, poverty rate, median age, unemployment rate, population size, and median wage income. Full regression results in Appendix Table C1.
p<0.10
p<0.05
p<0.01
Because greater welfare generosity is associated with larger annual mortality declines, the benefits of increased spending in generous states compound over time. The graphs in Figure 7 present counterfactual mortality trends for Minnesota and Wisconsin—states with similar geographic and demographic characteristics and histories. Since 1977, welfare generosity has increased significantly more in Minnesota than in Wisconsin, with Minnesota spending 43% more per-capita than Wisconsin in 2017. The counterfactuals show predicted mortality trends had Minnesota adopted the welfare spending increases in Wisconsin, and vice-versa. The mortality improvement in Wisconsin was dampened relative to the counterfactual of larger increases in welfare generosity. In contrast, Minnesota experienced significant reductions in mortality, which could in part be attributed to rising welfare generosity.
Figure 7:
Counterfactual Mortality Scenarios in Minnesota and Wisconsin: Women 1977-2017
Notes: Counterfactual mortality scenarios assume that annual increases in welfare generosity followed the trend in the counterpart state. Both graphs show death rates per 100,000 standardized to the 2000 U.S. standard population. Results for men shown in Appendix Figure A5.
Discussion
In the past 40-50 years, there has been a significant divergence in a number of aspects of social and political life across U.S. states; now more than ever in the recent past, one’s state of residence is a powerful determinant of quality of life (Montez et al., 2020). Particularly significant is the growing variation in adult mortality and life expectancy (Elo et al., 2019; Author, 2013; Population Reference Bureau, 2018). Joining recent work that identifies an important role for state policy in these patterns (Bradley et al., 2016; Montez et al., 2020), our results suggest that success among states on the East and West Coasts in reducing adult mortality is not an isolated trend but instead most likely part of a broader process of political divergence that has come to shape U.S. welfare state policies. Although comparisons between US life expectancy and that of other high-income countries have become increasingly salient, media depictions often suggest that European social democracies offer a picture of what U.S. mortality experience could be with better policy. Instead, our results indicate that states within the U.S. exhibit large differences both in welfare generosity and mortality, with some states having outcomes similar to Western Europe and others more similar to middle-income countries.
Our study contributes to a growing literature on mortality gaps between US divisions, states, counties, rural and urban areas, metropolitan and non-metropolitan areas, and major cities (Chetty et al., 2016; Dwyer-Lindgren et al., 2017; Elo et al., 2019; Author et al., 2019; Montez et al., 2019; Woolf and Schoomaker, 2019). Since the late 1970s, states in the Northeast and on the West Coast have increasingly risen in the mortality rankings, while states in the South, Great Plains, and Mountain West have fallen in the rankings. The overall magnitude of the mortality gap between the lowest-mortality and highest-mortality states has increased, potentially reflecting widening gaps in state policy. We suggest that per-capita public welfare program spending is likely to be an important mechanism driving divergences in mortality outcomes. We use 41 years of state spending and mortality data and fixed effects regression techniques to demonstrate that greater state welfare generosity predicts larger annual declines in adult mortality. As states have taken on an increasing role in policy development and the administration of federal programs (Author et al., 2018; Grumbach, 2018), they have also taken on a more important role in improving population health (Montez et al., 2020). Indeed, as wages have stagnated for low-income workers and fewer workers receive benefits like good health insurance and pensions from employers, the role of social policy at the federal and state level becomes ever more important for mortality outcomes.7
State welfare generosity has increased over time in every state, largely reflecting increased expenditures on medical care. Overall, payments to vendors (largely through Medicaid) make up about 80% of all public welfare spending in US states (Pierson et al., 2015). However, since 1977 states have diverged in their strategies, with some focusing on increasing Medicaid enrollment and benefits and other states using policy and administrative burdens to reduce Medicaid rolls (Herd et al., 2013). Differences in Medicaid benefits and enrollment may play a significant part in state mortality trends, especially given consistent evidence of the mortality benefits of increased healthcare access (Myerson et al., 2020). Indeed, quasi-experimental research demonstrates that Medicaid expansion through the ACA was responsible for a 3.6% mortality reduction in expanding states (Borgschulte and Vogler, 2020). The effects of increased Medicaid generosity would be expected to be largest for adults 55-64—since adults qualify for Medicare at age 65—but may also have significant benefits for Medicare beneficiaries who also receive Medicaid, a group whose size varies substantially across states (Kaiser Family Foundation, 2019).
Other factors undoubtedly contribute to geographic trends in mortality since the 1970s. In particular, growing geographic disparities in cigarette smoking, obesity, and drug overdoses almost certainly explain part of the trends documented here (Woolf and Schoomaker, 2019). For instance, smoking explained around 50% of state mortality divergences between 1965 and 2004 (Author, 2013) and lung cancer is a major contributor to widening disparities at the regional and metropolitan area level since 2000 (Vierboom et al., 2019). Similarly, state differences in obesity prevalence and obesity-related mortality follow similar patterns to that shown in the maps in Figure 2 and Figure 4—high mortality and sluggish improvement in the south, low mortality and rapid improvement in the Northeast (Roth et al., 2017; Ward et al., 2016). At the same time, health-related behaviors may partly result from welfare generosity (Beckfield, 2018). For instance, the welfare safety net may increase the chances of success at quitting smoking; uninsured adults who gained access to Medicaid were more likely to quit smoking and more likely to draw on resources to maintain smoking cessation after quitting (Bailey et al., 2016; Koma et al., 2017).
Interstate migration and other economic and demographic characteristics not included in the models may still contribute to both geographic patterns of adult mortality and the relationship between welfare generosity and adult mortality. To the extent that healthier individuals are more likely to migrate across state lines or that migrant origin and destination states are related to state politics, welfare spending policies, or death rates, the results may be biased. This would be particularly concerning if healthier individuals migrate more often to states experiencing rising welfare generosity. Indeed, state politics and policies do attract different types of migrants (Liu et al., 2019; Author et al., 2020) and generous welfare state policies could attract high-education or high-earning migrants, who may be both healthier and more supportive of stronger welfare state policies. As a result, political pressure may induce some states to spend more per-capita on welfare programs and some states may be able to spend more due to greater per-capita tax revenues. At the same time, if welfare generosity attracts healthy migrants or increases tax revenues, migration could be one indirect pathway through which more generous welfare spending affects state mortality trends. Since our data come from vital statistics and are based on state of residence at the time of death, we do not observe how long an individual has lived in their state of residence. Past work in this area has concluded that while health selective migration does occur, the magnitude of migration (and health selection) is not large enough to explain state differences in mortality or mortality trends (Author, 2013; Montez et al., 2019). Further, a relatively small number of people migrate from state-to-state, meaning that any effects are likely to be fairly modest. However, migration remains an issue that our data cannot effectively address, and future work should combine information on migration and mortality to assess its contribution to observed geographic patterns.
Limitations
Our analysis has limitations that reflect our reliance on vital statistics and our focus on subnational geographies. State expenditure data are available beginning in 1977, which may miss trends from the 1950s and 1960s that contribute to mortality experience during the study period, but reflects the beginning of the continuous panel of state spending data and the period of greater state policy burden (Grumbach, 2018; Pierson et al., 2015).
Second, we do not explicitly consider causal channels through which welfare generosity affects mortality, such as increased healthcare utilization or welfare program enrollment. Although more liberal states may seek to increase program participation among low-income individuals, thereby spending more on public welfare programs, a detailed analysis of these mechanisms is beyond the scope of the current study. Future work should quantify the contribution of increasing health insurance coverage to the relationship between welfare spending and adult mortality.
Third, our panel regression procedure may be susceptible to unobserved state-specific trends that are correlated with both changes in welfare generosity and changes in mortality. Our cointegration tests demonstrate that while the welfare generosity and mortality panels are cointegrated, there is at least weak exogeneity in the effect of welfare generosity on mortality. This provides some assurance that our coefficients are not biased by unobserved selection.
Fourth, we examine total state welfare spending including federal aid. If additional welfare spending at the state level is valuable, then in theory the source of the funds should not matter. However, models in Appendix Table C5 indicate that subtracting federal aid from total spending produces similar results, while federal aid alone does not significantly predict mortality. Additionally, we limit our analysis to public welfare programs, and do not specifically consider the role of other state-level poverty reduction programs such as EITC or paid leave programs. Future work should consider whether spending on these programs occurs alongside or in competition with spending on Medicaid, TANF, and CHIP.
Finally, we consider all-cause mortality and do not distinguish effects of welfare generosity by cause of death. This is partially to avoid potential state differences in cause of death coding practices (Stevens and Landes, 2021), which may produce a spurious effect on cause specific mortality. But previous research has also provided little guidance about which causes of death and conditions should be most responsive to changes in welfare generosity. The mortality effects of welfare spending might be quite broad, particularly if increased spending reduces poverty or increases access to preventive health care, but research should examine this.
Conclusion
The favorable adult mortality trends among coastal states to some extent contradict the broader underperformance of US mortality; while American mortality has fallen in the rankings, states on the East Coast and West Coast have increasingly demonstrated improvements comparable to other high-income countries. Our results suggest that this shift followed a similar trend toward increased per-capita spending on social programs that support the poor. Scholars and advocates often point to the experience of Canada and Europe as examples of the successful deployment of welfare state programs to reduce mortality and increase life expectancy (Author et al., 2016; Kindig et al., 2018; Reynolds and Avendano, 2018). Yet we demonstrate that examples of this approach need not focus abroad—several states have seen successful approaches to social welfare and population health and have seen mortality improvements as a result. In addition, the relationship between social spending and mortality highlights both the potential and limits of the U.S.’ fragmented welfare state. Individuals living in high-spending states experience mortality on par with more generous European welfare states, while individuals in states with lower per-capita expenditures exemplify the stereotypically shorter American lives. These divergent outcomes based solely on the state where one resides underscore some of the problematic consequences of the current federalized U.S. welfare state arrangements.
Supplementary Material
Highlights.
Since 1977, adult death rates in East and West Coast states have improved significantly, while states in the South and Great Plains have fallen behind
States with more rapid improvement are characterized by liberal state governments
State welfare generosity—public welfare spending per capita—is a robust predictor of adult mortality improvements of US states from 1977-2017
Welfare spending may help to explain the political divergence in mortality experience among US states
Acknowledgments
The authors acknowledge institutional support from the Population Research Institute at Penn State (P2C-HD041025). The authors are grateful to the Population Health Working Group at Penn State and the Network on Life Course Health Dynamics and Disparities supported by the National Institute on Aging.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest
The authors declare no conflict of interest.
States also share administrative costs and have some discretion over the level of benefits for the Supplemental Nutrition Assistance Program (SNAP) and can increase Supplemental Security Income (SSI) payments even though Social Security is entirely managed by the federal government.
We use the DW-Nominate variant of the Berry et al. measure here. Models examining the effect of State Government Liberalism—separate from and in concert with welfare generosity are shown in Appendix Table C2.
We examined a number of unit root tests using the xtunitroot routine in Stata 16.
Specifically, we model government liberalism and welfare generosity as a function of mortality, a series of controls and state and time fixed-effects. In these models, mortality is not a significant predictor of liberalism and social spending once we control for these variables’ own past lags.
The groups of states in each group are selected to illustrate regional trends, but do not satisfy objective criteria or statistical clusters, and are not intended to reflect the experience of entire regions.
Models in Appendix Table C7 examine different lag lengths for the relationship between welfare generosity and mortality. These models show similar coefficients for lags up to 4 years, but lags 5 years or above show no relationship between welfare generosity and mortality.
Although spending on other public programs is also associated with adult mortality, results in Appendix Table C6 show that welfare generosity is the most consistent predictor of reduced death rates.
Contributor Information
Andrew Fenelon, School of Public Policy and Department of Sociology and Criminology, Penn State University 331 Pond Laboratory, University Park, PA 16802.
Christopher Witko, School of Public Policy and Department of Political Science, Penn State University.
References
- Avendano M, Kawachi I, 2014. Why do Americans have shorter life expectancy and worse health than do people in other high-income countries? Annu. Rev. Publ. Health 35, 307–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey SR, Hoopes MJ, Marino M, Heintzman J, O’Malley JP, Hatch B, Angier H, Fortmann SP, DeVoe JE, 2016. Effect of gaining insurance coverage on smoking cessation in community health centers: a cohort study. J. Gen. Intern. Med 31, 1198–1205. 10.1007/s11606-016-3781-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnish M, Tørnes M, Nelson-Horne B, 2018. How much evidence is there that political factors are related to population health outcomes? An internationally comparative systematic review. BMJ Open 8, e020886. 10.1136/bmjopen-2017-020886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckfield J, 2018. Political Sociology and the People’s Health, Political Sociology and the People’s Health. Oxford University Press, Oxford. [Google Scholar]
- Beckfield J, Bambra C, 2016. Shorter lives in stingier states: social policy shortcomings help explain the US mortality disadvantage. Soc. Sci. Med 171, 30–38. 10.1016/j.socscimed.2016.10.017. [DOI] [PubMed] [Google Scholar]
- Berry WD, Fording RC, Ringquist EJ, Hanson RL, Klarner CE, 2010. Measuring citizen and government ideology in the U.S. States: a Re-appraisal. State Polit. Policy Q 10, 117–135. 10.1177/153244001001000201. [DOI] [Google Scholar]
- Berry WD, Ringquist EJ, Fording RC, Hanson RL, 1998. Measuring citizen and government ideology in the American states, 1960-93. Am. J. Pol. Sci 42 (327) 10.2307/2991759. [DOI] [Google Scholar]
- Borgschulte M, Vogler J, 2020. Did the ACA medicaid expansion save lives? J. Health Econ 102333 10.1016/j.jhealeco.2020.102333. [DOI] [PubMed] [Google Scholar]
- Boudreaux MH, Golberstein E, McAlpine DD, 2016. The long-term impacts of Medicaid exposure in early childhood: evidence from the program’s origin. J. Health Econ 45, 161–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudreaux MH, Lipton BJ, 2021. Medicaid benefit generosity and labor market outcomes: evidence from medicaid adult vision benefits. J. Hum. Resour 56, 536–569. 10.3368/jhr.56.2.1117-9193r2. [DOI] [Google Scholar]
- Bradley EH, Canavan M, Rogan E, Talbert-Slagle K, Ndumele C, Taylor L, Curry LA, 2016. Variation in health outcomes: the role of spending on social services, public health, and health care, 2000-09. Health Aff. 35, 760–768. 10.1377/hlthaff.2015.0814. [DOI] [PubMed] [Google Scholar]
- Brooks T, 2018. CHIP funding has been extended, what’s next for children’s health coverage? [WWW Document]. Health Aff. URL https://www.healthaffairs.org/do/10.1377/hblog20180130.116879/full/. [Google Scholar]
- Case A, Deaton A, 2015. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. Unit. States Am 112, 15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center on Budget and Policy Priorities, 2020. Policy basics: introduction to medicaid.
- Centers for Disease Control and Prevention, 2018. CDC wonder [WWW document]. URL http://wonder.cdc.gov. .
- Charemza WW, Deadman DF, 1992. In: Cointegrat (Ed.), New directions in econometric practice: general to specific modelling. Edward Elgar Publishing, England. [Google Scholar]
- Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, Bergeron A, Cutler D, 2016. The association between income and life expectancy in the United States, 2001-2014. Jama 315, 1750–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Preston SH, Cohen B, 2011. Explaining divergent levels of longevity in high-income countries. [PubMed] [Google Scholar]
- Division, U.N.P., 2017. World Population Prospects. United Nations Population Division, New York, 2017 Revision. [Google Scholar]
- Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, Morozoff C, Mackenbach JP, van Lenthe FJ, Mokdad AH, Murray CJL, 2017. Inequalities in life expectancy among US counties, 1980 to 2014: temporal trends and key drivers. JAMA intern. Med [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo IT, Hendi AS, Ho JY, Vierboom YC, Preston SH, 2019. Trends in non-Hispanic white mortality in the United States by metropolitan-nonmetropolitan status and region, 1990–2016. Popul. Dev. Rev 45, 549–583. 10.1111/padr.12249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enns PK, Kelly NJ, Masaki T, Wohlfarth PC, 2016. Don’t jettison the general error correction model just yet: a practical guide to avoiding spurious regression with the GECM. Res. Pol 3 (205316801664334) 10.1177/2053168016643345. [DOI] [Google Scholar]
- Fellowes MC, Rowe G, 2004. Politics and the New American Welfare States. Am. J. Pol. Sci 48, 362–373. 10.1111/j.0092-5853.2004.00075.x. [DOI] [Google Scholar]
- Fenelon Andrew, 2013. Geographic divergence in mortality in the United States. Popul. Dev. Rev 39 (4), 611–634. 10.1111/j.1728-4457.2013.00630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon Andrew, Boudreaux Michel, 2019. Life and death in the American City: men’s life expectancy in 25 major American cities from 1990 to 2015. Demography 56 (6), 2349–2375. 10.1007/s13524-019-00821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon Andrew, Chen Li-Hui, Baker Susan P., 2016. Major causes of injury death and the life expectancy gap between the United States and other high-income countries. JAMA 315 (6), 609–611. 10.1001/jama.2015.15564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franko WW, Witko C, 2018. The New Economic Populism: How States Respond to Economic Inequality. Oxford University Press, Oxford. [Google Scholar]
- Goodman-Bacon A, 2018. Public insurance and mortality: evidence from medicaid implementation. J. Polit. Econ 126, 216–262. 10.1086/695528. [DOI] [Google Scholar]
- Grogan CM, 1994. Political-economic factors influencing state medicaid policy. Polit. Res. Q 47, 589–622. 10.1177/106591299404700303. [DOI] [Google Scholar]
- Grogan CM, Rigby E, 2009. Federalism, partisan politics, and shifting support for state flexibility: the case of the U.S. State children’s health insurance program. Publius J. Fed 39, 47–69. 10.1093/publius/pjn031. [DOI] [Google Scholar]
- Grumbach JM, 2018. From backwaters to major policymakers: policy polarization in the states, 1970-2014. Perspect. Polit 10.1017/S153759271700425X. [DOI] [Google Scholar]
- Hamad R, Niedzwiecki MJ, 2019. The short-term effects of the earned income tax credit on health care expenditures among US adults. Health Serv. Res 54, 1295–1304. 10.1111/1475-6773.13204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herd P, 2016. The Influence of Social Welfare Policies on Health Disparities across the Life Course. In: Shanahan M, Mortimer J, Kirkpatrick Johnson M (Eds.), Handbook of the Life Course. Handbooks of Sociology and Social Research. Springer, pp. 661–675. 10.1007/978-3-319-20880-0_29. [DOI] [Google Scholar]
- Herd P, DeLeire T, Harvey H, Moynihan DP, 2013. Shifting administrative burden to the state: the case of medicaid take-up. Public Adm. Rev 73, S69–S81. 10.1111/puar.12114. [DOI] [Google Scholar]
- Herd P, Moynihan DP, 2019. Administrative burden: policymaking by other means. Russell Sage Foundation, New York. [Google Scholar]
- Hertel-Fernandez A, 2019. State capture ;: How Conservative Activists, Big Businesses, and Wealthy Donors Reshaped the American States–And the Nation. Oxford University Press, New York. [Google Scholar]
- Hertel-Fernandez A, Skocpol T, Lynch D, 2016. Business associations, conservative networks, and the ongoing Republican war over Medicaid expansion. J. Health Polit. Pol. Law 41, 239–286. 10.1215/03616878-3476141. [DOI] [PubMed] [Google Scholar]
- Hoynes H, Schanzenbach DW, Almond D, 2016. Long-run impacts of childhood access to the safety net. Am. Econ. Rev 106, 903–934. [Google Scholar]
- Kaiser Family Foundation, 2019. In: Henry J (Ed.), Dual eligibles as a percent of total Medicare beneficiaries. Kaiser fam. Found. [Google Scholar]
- Kindig D, Nobles J, Zidan M, 2018. Meeting the institute of medicine’s 2030 US life expectancy target. Am. J. Public Health 108, 87–92. 10.2105/AJPH.2017.304099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koma JW, Donohue JM, Barry CL, Huskamp HA, Jarlenski M, 2017. Medicaid coverage expansions and cigarette smoking cessation among low-income adults. Med. Care 55, 1023–1029. 10.1097/MLR.0000000000000821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee BC, Modrek S, White JS, Batra A, Collin DF, Hamad R, 2020. The effect of California’s paid family leave policy on parent health: a quasi-experimental study. Soc. Sci. Med 251 (112915) 10.1016/j.socscimed.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard J, Mas A, 2008. Welfare reform, time limits, and infant health. J. Health Econ 27, 1551–1566. 10.1016/j.jhealeco.2008.05.013. [DOI] [PubMed] [Google Scholar]
- Liu X, Andris C, Desmarais BA, 2019. Migration and political polarization in the U.S.: an analysis of the county-level migration network. PLoS One 14, e0225405. 10.1371/journal.pone.0225405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maresh J, Guse C, Layde P, 2012. National trends and coding patterns in fall-related mortality among the elderly in the United States. J. Publ. Health Pol 33, 202–214. 10.1057/jphp.2012.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta NK, Abrams LR, Myrskylä M, 2020. US life expectancy stalls due to cardiovascular disease, not drug deaths. Proc. Natl. Acad. Sci. U. S. A 117, 6998–7000. 10.1073/pnas.1920391117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michener J, 2018. Fragmented democracy, fragmented democracy: medicaid, federalism, and unequal politics. Cambridge University Press, Cambridge. 10.1017/9781108224987. [DOI] [Google Scholar]
- Moldogaziev TT, Monogan JE, Witko C, 2018. Income inequality and the growth of redistributive spending in the United States (US) states: Is there a link? J. Publ. Pol 38, 141–163. 10.1017/S0143814X17000125. [DOI] [Google Scholar]
- Montez JK, Beckfield J, Cooney J, Hayward MD, Grumbach JM, Koytak HZ, Woolf S, Zajacova A, 2020. US state policies, politics, and life expectancy. Milbank Q. 10.1111/1468-0009.12469, 1468-0009.12469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez JK, Zajacova A, Hayward MD, 2016. Explaining inequalities in women’s mortality between US States. SSM Popul. Health 2, 561–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez JK, Zajacova A, Hayward MD, Woolf SH, Chapman D, Beckfield J, 2019. Educational disparities in adult mortality across US states: how do they differ, and have they changed since the mid-1980s? Demography 1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myerson RM, Tucker-Seeley RD, Goldman DP, Lakdawalla DN, 2020. Does Medicare coverage improve cancer detection and mortality outcomes? J. Policy anal. Manag 10.1002/pam.22199pam.22199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navarro V, Borrell C, Benach J, Muntaner C, Quiroga A, Rodríguez-Sanz M, Vergés N, Gumá J, Pasarín MI, 2003. The importance of the political and the social in explaining mortality differentials among the countries of the OECD, 1950–1998. Int. J. Heal. Serv 33, 419–494. 10.2190/R7GE-8DWK-YY6C-183U. [DOI] [PubMed] [Google Scholar]
- Navarro V, Muntaner C, Borrell C, Benach J, Quiroga Á, Rodríguez-Sanz M, Vergés N, Pasarín MI, 2006. Politics and health outcomes. Lancet 368, 1033–1037. 10.1016/S0140-6736(06)69341-0. [DOI] [PubMed] [Google Scholar]
- Nelson MJ, Witko C, 2020. Government reputational effects of COVID-19 public health actions: A job opportunity evaluation conjoint experiment. J. Behav. Public Adm 3 (1) 10.30636/jbpa.31.174. [DOI] [Google Scholar]
- Patnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD, Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: A retrospective cohort study. Breast Cancer Res. 13, R64, 2011. 10.1186/bcr2901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierson K, Hand ML, Thompson F, 2015. The government finance database: a common resource for quantitative research in public financial analysis. PLoS One 10. 10.1371/journal.pone.0130119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington, DC: Population Reference Bureau,. Declines in adult death rates lag in the U. S. South, Available from. http://www.prb.org/prb17/mortality/index.html. . [Google Scholar]
- Rambotti S, 2020. Is there a relationship between welfare-state policies and suicide rates? Evidence from the U.S. states, 2000–2015. Soc. Sci. Med 246 (112778) 10.1016/j.socscimed.2019.112778. [DOI] [PubMed] [Google Scholar]
- Reynolds MM, Avendano M, 2018. Social policy expenditures and life expectancy in high-income countries. Am. J. Prev. Med 54, 72–79. 10.1016/j.amepre.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth GA, Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, Morozoff C, Naghavi M, Mokdad AH, Murray CJL, 2017. Trends and patterns of geographic variation in cardiovascular mortality among US counties, 1980-2014. JAMA - J. Am. Med. Assoc 317, 1976–1992. 10.1001/jama.2017.4150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohn H, 2017. Medicaid’s lasting impressions: population health and insurance at birth. Soc. Sci. Med 177, 205–212. 10.1016/j.socscimed.2017.01.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommers BD, 2017. State medicaid expansions and mortality, revisited: a cost-benefit analysis. Am. J. Health Econ 3, 392–421. 10.1162/ajhe_a_00080. [DOI] [Google Scholar]
- Sommers BD, Long SK, Baicker K, 2014. Changes in mortality after Massachusetts health care reform : a quasi-experimental study. Ann. Intern. Med 160, 585–593. 10.7326/M13-2275. [DOI] [PubMed] [Google Scholar]
- Stevens JD, Landes SD, 2021. Assessing state level variation in signature authority and cause of death accuracy, 2005–2017. Prev. Med. Rep 21 (101309) 10.1016/j.pmedr.2020.101309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vierboom YC, Preston SH, Hendi AS, 2019. Rising geographic inequality in mortality in the United States. SSM - Popul. Health 9 (100478). 10.1016/j.ssmph.2019.100478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward ZJ, Long MW, Resch SC, Gortmaker SL, Cradock AL, Giles C, Hsiao A, Wang YC, 2016. Redrawing the US obesity landscape: bias-corrected estimates of state-specific adult obesity prevalence. PLoS One 11, e0150735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wherry LR, Miller S, 2016. Early coverage, access, utilization, and health effects of the affordable care act medicaid expansions: a quasi-experimental study. Ann. Intern. Med 164, 795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witko C, 2007. Explaining increases in the stringency of state campaign finance regulation, 1993–2002. State Polit. Pol. Q 7, 369–393. 10.1177/153244000700700402. [DOI] [Google Scholar]
- Witko C, Newmark AJ, 2010. The strange disappearance of investment in human and physical capital in the United States. J. Publ. Adm. Res. Theor 20, 215–232. [Google Scholar]
- Woolf SH, Schoomaker H, 2019. Life expectancy and mortality rates in the United States, 1959–2017. JAMA - J. Am. Med. Assoc 10.1001/jama.2019.16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.