Abstract
Objective:
Veterans with posttraumatic stress disorder (PTSD) often experience difficulties with social reintegration after deployment. Experiential avoidance, the tendency to avoid unwanted thoughts, feelings, and bodily sensations (including in response to interactions with others) may be a key factor that explains the association between PTSD symptoms and postdeployment social support. The present study evaluated whether experiential avoidance mediates the association between PTSD symptoms and perceptions of postdeployment social support.
Method:
Veterans (n = 145) who served in support of the conflicts in Iraq and Afghanistan were enrolled in a study evaluating returning veterans’ experiences. Participants were evaluated at an initial baseline assessment and 8-months later. Participants completed the lifetime Clinician Administered PTSD Scale and the Acceptance and Action Questionnaire—II at baseline, as well as the Deployment Risk and Resilience Inventory—Post Deployment Social Support Questionnaire at the 8-month assessment.
Results:
Baseline experiential avoidance mediated the association between lifetime PTSD symptoms and 8-month social support.
Conclusions:
Experiential avoidance may be an important target for treatment to improve long-term functional recovery and reintegration.
Keywords: posttraumatic stress disorder, trauma, social support, experiential avoidance, veterans
A considerable number of the veterans returning from the conflicts in Iraq and Afghanistan develop posttraumatic stress disorder (PTSD; Dursa, Reinhard, Barth, & Schneiderman, 2014; Fulton et al., 2015) with prevalence rates ranging from 17 to 23% (Fulton et al., 2015; Hoge et al., 2004; Seal et al., 2009). Veterans diagnosed with PTSD often have substantial interpersonal problems and low perceived social support from family, partners, and peers. These difficulties result in poor social reintegration, in turn permeating all aspects of their functioning (Price, Gros, Strachan, Ruggiero, & Acierno, 2013) including being associated with greater suicidal ideation (DeBeer, Kimbrel, Meyer, Gulliver, & Morissette, 2014). Such problems appear to emerge rapidly, with one study indicating that veterans demonstrate a fourfold increase in rates of self-reported interpersonal conflict within 6 months of returning from deployment (Milliken, Auchterlonie, & Hoge, 2007). Extensive evidence documents that military veterans with PTSD demonstrate higher levels of marital stress, relationship abuse, difficulties with intimacy, and more parenting problems (Beckham, Feldman, Kirby, Hertzberg, & Moore, 1997; Cohen, Zerach, & Solomon, 2011; MacDonald, Chamberlain, Long, & Flett, 1999; Solomon, Dekel, & Zerach, 2008). Thus, identifying mechanisms that influence the link between PTSD symptoms and perceived social support is important for promoting meaningful recovery.
Low social support is a key factor related to poor physical health, emotional functioning, clinical outcomes, and increased mortality risk across a broad range of mental and physical health problems (Holt-Lunstad, Smith, & Layton, 2010; Karelina, & DeVries, 2011; Prins et al., 2011). Low social support is an important risk factor for PTSD in veterans and civilians (Brewin, Andrews, & Valentine, 2000; Ozer, Best, Lipsey, & Weiss, 2003; Xue et al., 2015), with a weighted effect size of r = .28 in one meta-analysis (Ozer et al., 2003) and an odds ratio (OR) of 2.70 (OR = 0.37 if reversed and social support was seen as a protective factor) in another meta-analysis (Xue et al., 2015). According to the erosion model of social support in PTSD postulated by King and colleagues (2006), PTSD symptoms lead to a reduction in social support because of interpersonal difficulties, irritability, feelings of detachment from others, and avoidance of social situations (King et al., 2006). In veterans, PTSD symptoms are also associated with erosion of perceived interpersonal resources from social supports, particularly nonveterans (Laffaye, Cavella, Drescher, & Rosen, 2008). However, there may be potential mediating factors that account for why some people with PTSD develop more interpersonal difficulties than others. One such mechanism may be experiential avoidance.
Avoidance of social contact among people experiencing symptoms of PTSD may be conceptualized as experiential avoidance within psychological flexibility theory (Bond et al., 2011; Gerhart, Baker, Hoerger, & Ronan, 2014). Experiential avoidance is the tendency to avoid unwanted thoughts, feelings, and bodily sensations, including those experienced in response to interacting with others (Bond et al., 2011; Hayes, Strosahl, & Wilson, 2012). Psychological flexibility theory maintains that experiential avoidance interferes with living a life consistent with one’s values (Hayes et al., 2012), which, for many people, includes maintaining relationships with family, partners, friends, peers, and others (Gerhart et al., 2014). Thus, within the erosion model of social support in PTSD (King et al., 2006; Shallcross, Arbisi, Polusny, Kramer, & Erbes, 2016), experiential avoidance may play a key role in mediating the association between PTSD symptoms and social support after deployment. For instance, veterans with PTSD who perceive others as threatening may withdraw to avoid the anxiety they experience when interacting with others, including others who may be sources of social support (Gerhart et al., 2014). Veterans with PTSD who experience anger and irritability in social situations, perhaps triggered by perceptions of others or of social environments as threatening, frequently act aggressively to control or avoid the perceived threat (i.e., another form of experiential avoidance; Gardner & Moore, 2008), leading to further decline in support over time. Relatedly, many veterans who have made angry outbursts toward others report that they fear having future outbursts and avoid social situations to reduce their likelihood.
The few published data available from cross-sectional studies provide support for the role of experiential avoidance in the association between PTSD and social support. Experiential avoidance is associated with both PTSD symptom severity and social support in a prior cross-sectional analysis using the same sample of Iraq and Afghanistan veterans as the current study (Meyer, Morissette, Kimbrel, Kruse, & Gulliver, 2013). Further, Iraq and Afghanistan veterans who screened positive for PTSD were significantly more likely to report emotional hiding, defined as efforts to avoid talking about their problems and emotions with social supports, compared with veterans who did not screen positive for PTSD (Duax, Bohnert, Rauch, & Defever, 2014). Finally, social avoidance mediated the association between PTSD and partner satisfaction in Iraq and Afghanistan war veterans (Tsai, Harpaz-Rotem, Pietrzak, & Southwick, 2012). However, to our knowledge, no published study has evaluated whether experiential avoidance mediates the association between PTSD symptom severity and level of perceived social support within the context of a longitudinal design.
The present study evaluated whether experiential avoidance mediated the association between PTSD symptom severity and social support in veterans who served in support of the conflicts in Iraq and Afghanistan and postdeployment social support. It was hypothesized that baseline experiential avoidance would mediate the association between lifetime PTSD symptom severity (i.e., during the worst month identified by veterans related to their most traumatic event) and perceived social support 8 months after the baseline assessment.
Method
Participants
Veterans who served in support of the conflicts in Iraq and Afghanistan (N = 145) were recruited to participate in a longitudinal study that examined postdeployment readjustment. Participants were recruited via a variety of channels including in-service presentations to veterans administration (VA) staff (e.g., primary care, mental health, and Operation Enduring Freedom/Operation Iraqi Freedom [OEF/OIF] program), advertisements at recruitment sites and veterans’ service organizations, and letters mailed to potentially eligible veterans residing in the local area. Participants were eligible for the study if they were: (a) enrolled in the local VA health care system (though not necessarily receiving treatment); (b) able to provide informed consent; and (c) able to complete the full assessment battery. Participants were excluded from the study if they: (a) had a diagnosis of bipolar or psychotic disorder; (b) recently began (i.e., had not reached stabilization) psychiatric medications or psychotherapy; (c) were in suicidal or homicidal crisis; or (d) planning to move out of the area within 4 months of the start of the study. As functioning was the primary outcome, veterans who had recently started medication or therapy were excluded because medications may influence functional outcomes over time. A phone screen assessed initial study eligibility. In addition, our recruitment strategy involved oversampling for veterans experiencing PTSD and other trauma-related mental health challenges. Veteran names were pulled from the medical record if they (a) had a prior mental health appointment; (b) had a previous diagnosis of PTSD; (c) had a previous diagnosis of depression; and (d) had a mental health disorder in their medical record other than schizophrenia or bipolar disorder. Targeted mailings that provided information about the study were sent to random samplings of individuals from this list. Of the 145 participants enrolled, 15 were ruled ineligible resulting in a final sample of 130 eligible participants. Although suicidal or homicidal crisis was an exclusion criterion for ethical reasons, none of the participants were excluded based for this reason.
The majority of the sample was male (85.4%), with a mean age of 37.8 years (SD = 10.6). Of the total sample, 26.6% identified as of Hispanic ethnicity. In terms of race, 64.6% identified as White, 18.9%, as African American, 2.4% as American Indian/Alaska Native, 3.9% as Asian American, .8% as Hawaiian/Pacific Islander, and 9.4% as “Other” (categories were not mutually exclusive). On average, participants reported an average education level of 14.1 years (SD = 2.5 years). Most had served in the Army (82.0%), while 4.7% served in the Air Force, 8.6% in the Marine Corps, and 6.3% in the Navy (categories were not mutually exclusive). Participants deployed an average of 2.17 times (SD = 1.26, range 1–7), and had returned from their most recent deployment an average of 3.46 years (SD = 2.12) before the baseline assessment.
Measures
Diagnostic interview.
The Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1998) is a diagnostic assessment for Axis I disorders that is administered by a clinician. The bipolar and psychosis portions of the MINI were used to screen for exclusionary criteria.
Demographic information.
A demographic form created for the study assessed relevant participant characteristics, including age, gender, race and ethnicity, relationship status, education, and military service characteristics.
PTSD symptoms.
The Clinician Administered PTSD Scale for Diagnostic and Statistical Manual for Mental Disorders (CAPS; Blake et al., 1995) is a clinician administered, semistructured diagnostic interview that assesses PTSD symptoms. Within the present research, the CAPS interview assessed responses to traumatic events related to a warzone deployment. Participants were administered a checklist of traumatic events commonly experienced in a warzone followed by clinician-guided discussion of the three worst events the participant experienced during their deployment. Then, the clinician and participant discussed which of these events was their worst traumatic event and the CAPS was administered using this event. PTSD symptoms were assessed for the past 30 days and during the month when participants identified symptoms as being most severe (i.e., lifetime worst month). Life-time worst symptom level was used in the hypothesized mediational model to reflect the chronology among PTSD symptoms, the mediator, and the outcome. The CAPS produces both a continuous symptom severity score and a categorical PTSD diagnosis. Internal consistency in the current study was .96 for lifetime worst month symptoms and .96 for the baseline symptoms.
Experiential avoidance.
The Acceptance and Action Questionnaire-II (AAQ-II; Bond et al., 2011) was used to assess experiential avoidance and psychological inflexibility. The AAQ-II is a self-report measure consisting of 7-items and uses a 7-point Likert scale from 1 (never true) to 7 (always true). Examples of items from this scale include “My painful experiences and memories make it difficult for me to live a life that I would value,” and “I’m afraid of my feelings.” Higher scores on the AAQ-II indicate higher levels of experiential avoidance. Internal consistency in the current study was .94.
Social support.
The Deployment Risk and Resilience Inventory (DRRI) is a collection of scales that assess deployment risk and resilience factors. The scales are also designed to be used individually (King et al., 2006; Vogt, Proctor, King, King, & Vasterling, 2008). The postdeployment social support (PDSS) subscale of the DRRI was used to assess perceived social support. The PDSS includes 15 items rated on a scale from 1 (strongly disagree) to 5 (strongly agree). Item examples include “Among my friends or relatives there is someone who makes me feel better when I am feeling down” and “there are people to whom I can talk about my deployment experiences” Internal consistency for the PDSS was 0.84.
Procedures
The local Institutional Review Board reviewed and approved all study procedures before the start of the research. After the initial telephone screening, veterans deemed initially eligible were scheduled for an in-person assessment. Written informed consent was obtained at the baseline assessment and final eligibility confirmed. During the appointment, veterans completed a clinical interview to assess PTSD symptoms and filled out self-report measures assessing basic demographic information, experiential avoidance, and social support.
Masters and doctoral-level interviewers underwent a series of stepped training procedures before conducting interviews independently. Procedures were as follows: (a) Observe one interview with a trained interviewer and attempt to match on diagnoses; (b) Listen to audio recordings of previous baseline interviews and match on diagnoses and ±5 points on the CAPS total severity score for a minimum of three interviews; (c) Conduct a joint interview with a trained interviewer and match on diagnoses for at least one interview; (d) Conduct at least two interviews independently while being observed by a trained interviewer and match on diagnoses and CAPS total severity score within ±5 points. We added this information to the Measures section of the article discussing the CAPS.
As part of determining whether individuals met diagnostic criteria for PTSD, individual symptoms from the CAPS were reviewed by a doctoral level clinician to reach consensus on symptom ratings. Both individual symptoms and symptom clusters that were barely missed or barely met threshold were reviewed, along with additional symptoms as needed based upon the judgment of the interviewer or head of the review team.
Following the baseline interview, participants were mailed self-report questionnaires 8 months later and returned them using a self-addressed stamped envelope. Of the total sample, 90.8% of participants were retained at the 8-month follow-up. Participants who did not complete the 8-month did not differ significantly from those who did complete 8-month on any of the following variables at baseline: gender, F(2, 127) = .67, p = .51; age, F(2, 127) = 1.15, p = .32; education level: 2.49, p = .09; current PTSD symptoms (CAPS), F(2, 127) = .46, p = .63; postdeployment social support, F(2, 127) = .57, p = .57; experiential avoidance, F(2, 127) = .14, p = .87.
Data Analytic Plan
The Preacher and Hayes (2008) method of mediation with bootstrapping was used to test the mediational model using 1,000 bootstrapped samples. This type of mediational analysis relies on nonparametric bootstrapping, which produces an approximate sampling distribution. This analysis provides point estimates and also 95% confidence intervals (CIs) for the indirect effects. The model is considered significant if 0 does not fall in the 95% bias corrected and accelerated CIs for the indirect effect (Hayes, 2013; Preacher & Hayes, 2004; Preacher, Rucker, & Hayes, 2007). Several covariates were selected to be included in the model: gender, age, education, and time between last deployment. We controlled for gender, age and education, as there are differences in these demographic factors in those diagnosed with PTSD (Dirkzwager, Bramsen, & van der Ploeg, 2005; Ditlevsen & Elklit, 2010; Meyer et al., in press).
Results
Descriptive Statistics and Bivariate Correlations
Means and SDs for study measures are included in Table 1. A significant portion (n = 50) of the 130 veterans met criteria for PTSD in the past 30 days and over half (72/130) met criteria for PTSD during their lifetime worst month. On average, lifetime worst month was 4.75 years before the baseline assessment interview (SD = 2.55). All measures, including baseline and lifetime PTSD severity, experiential avoidance, and perceived postdeployment social support were significantly correlated (all ps < .01; see Table 1).
Table 1.
Means and SDs of Measures of PTSD, Social Support, and Experiential Avoidance
| Measure | M (SD) | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| 1. CAPS total score past month | 45.20 (30.19) | — | — | — | — |
| 2. CAPS total score lifetime | 65.60 (34.88) | .797** | — | — | — |
| 3. AAQ-II | 23.29 (11.40) | .685** | .542** | — | — |
| 4. DRRI postdeployment social support | 32.80 (6.76) | −.472** | −.331** | −.510** | — |
Note. PTSD = posttraumatic stress disorder; CAPS = Clinician-Administered PTSD Scale; AAQ-II = Acceptance and Action Questionnaire–II; DRRI = Deployment Risk and Resilience Inventory.
Significant at the p < .01 level.
Mediation Analyses
Nonparametric bootstrapping was used to test the mediation model (see Figure 1). Baseline experiential avoidance was examined as a mediator in the association between lifetime worst PTSD symptoms and 8-month social support. Covariates included demographic variables of gender, age, and education. Education was a significant predictor in the model, point estimate (PE) = .0558, SE = .0244, p = .03, as was time since last deployment PE = .0057, SE = .0024, p = .02; however, other demographic factors were not significant (gender: PE = ‒.0912, SE = .1602, p = .57, age: PE = ‒.0065, SE = .0059, p = .27). The direct effect of lifetime worst month PTSD symptoms on baseline experiential avoidance was PE = .0258, SE = .0038, p < .001, and the direct effect of baseline experiential avoidance on 8-month social support was PE = ‒.2091, SE = .0445, p < .001. Baseline experiential avoidance mediated the association between lifetime worst month PTSD symptoms and 8-month social support (indirect effect = ‒.0054, SE = .0013, 95% CI [‒.0082, ‒.0030]), such that increased PTSD symptoms predicted increased experiential avoidance, which, in turn predicted lower perceived social support. The indirect effect is significantly different from 0 at p < .05, as the 95% CI did not contain 0.
Figure 1.
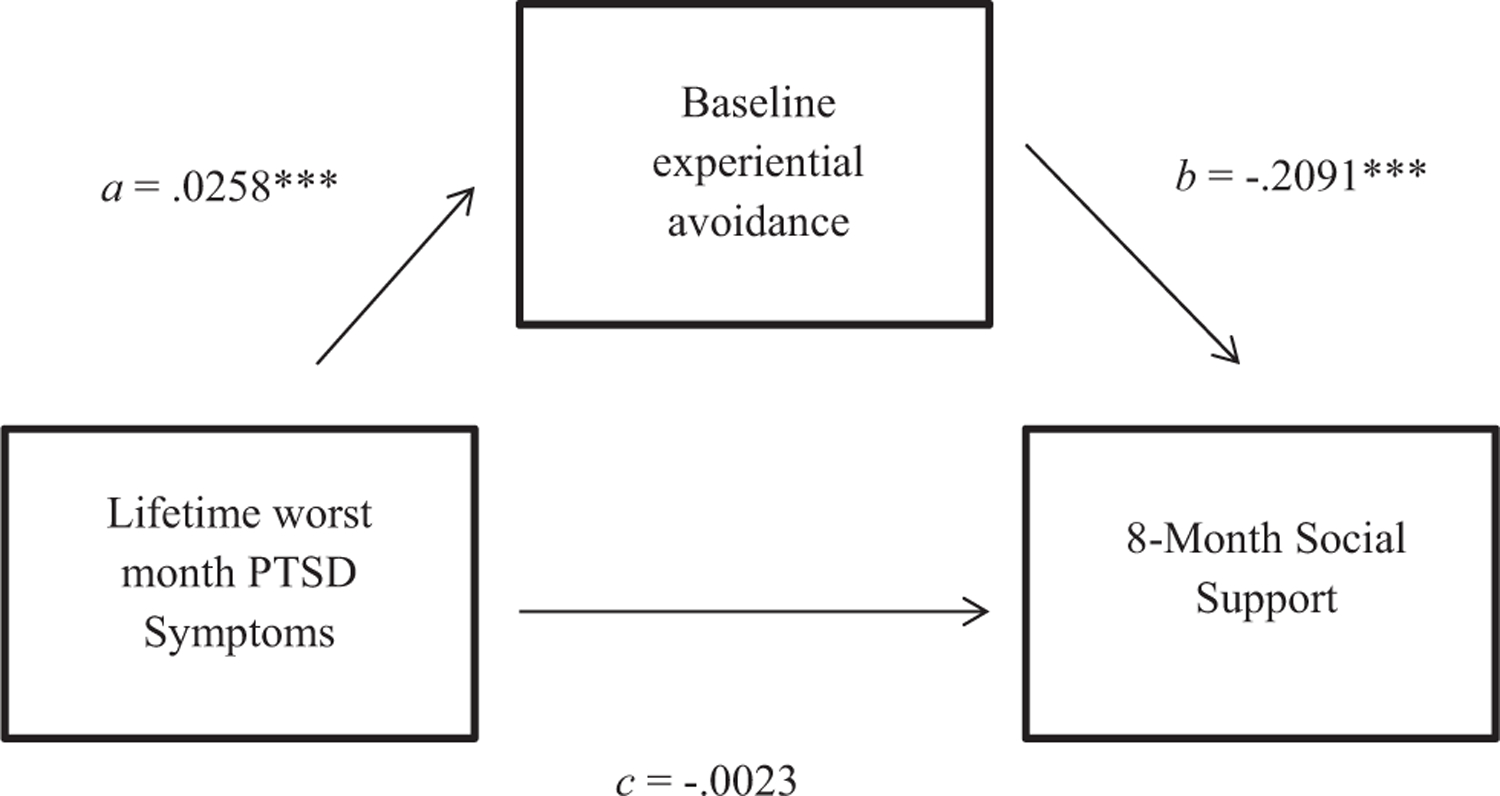
Mediational model of baseline experiential avoidance as a mediator of the association between lifetime worst month PTSD symptoms and 8-month social support. ***p < .001.
Discussion
Results indicated that experiential avoidance is a significant mediator between PTSD symptoms and perceived postdeployment social support. These results support the erosion model of social support demonstrating that loss of social support could be a consequence of PTSD (King et al., 2006; Shallcross et al., 2016). In addition, psychological flexibility theory adds to our understanding of these relations based on the erosion model by suggesting that experiential avoidance may be a key mechanism that links PTSD symptoms and social support (Gerhart et al., 2014). These findings also further support literature linking experiential avoidance to interpersonal difficulties for veterans who served in support of the conflicts in Iraq and Afghanistan. For instance, Reddy and colleagues (2011) showed that for both male and female veterans, higher levels of experiential avoidance are associated with decreases in relationship adjustment. In addition, for male veterans, higher levels of experiential avoidance were also associated with increases in physical aggression perpetration and victimization. However, the present study was the first to demonstrate the mediational links between PTSD symptoms, experiential avoidance, and levels of postdeployment social support.
The research literature also shows that social support may have a buffering effect for veterans who have been deployed (Cohen & Wills, 1985). Higher levels of social support (i.e., partner, military leadership, neighbor; not specific to any time period) are associated with better postdeployment adjustment, regardless of the degree or amount of negative deployment experiences (Welsh, Olson, Perkins, Travis, & Ormsby, 2015). Social support of this type has also been shown to moderate the impact of negative deployment experiences on depressive symptoms, with low levels of support (i.e., partner, neighbor) associated with more postdeployment depressive symptoms compared with those with higher levels of social support (Welsh et al., 2015). Underscoring the importance of this buffering effect, social support moderates the association between PTSD and depressive symptoms and suicidal ideation (DeBeer et al., 2014). Lower experiential avoidance likely facilitates the ability to maintain social support while managing negative deployment experiences and may protect veterans from developing more severe symptoms and other negative outcomes. Future research should evaluate the role of experiential avoidance within such a buffering context. There is also some evidence suggesting that the link between mental health symptoms and social support may be bidirectional (Gerhart et al., 2014). The current findings suggest that experiential avoidance may influence such a relationship, and additional research examining these relations is warranted.
The results of the present study suggest that experiential avoidance could be an important treatment target for returning veterans experiencing PTSD symptoms, particularly in terms of improving social outcomes. In a prior study (Meyer et al., 2013), we found that the association between experiential avoidance and PTSD symptom severity was broader than that accounted for by avoidance of internal and external reminders of the trauma. This association between experiential avoidance and PTSD symptoms likely includes avoidance of a broad range of unwanted cognitions and emotions in social contexts leading to deterioration of relationships. While targeting avoidance of trauma cues is a core facet of many approaches to treating PTSD, it is possible that targeting experiential avoidance more broadly may yield additional benefits. Contemporary contextual behavioral treatments such as Acceptance and Commitment Therapy (ACT; Hayes et al., 2012) directly target experiential avoidance. There is empirical support for such interventions in treating a number of mental and physical health problems with which PTSD frequently co-occurs (Arch, Eifert, Davies, Vilardaga, Rose, & Craske, 2012; Forman, Herbert, Moitra, Yeomans, & Geller, 2007; Gratz & Gunderson, 2006; Vowles & McCracken, 2008; Walser, Garvert, Karlin, Trockel, Ryu, & Taylor, 2015), but research is ongoing to determine its efficacy for the treatment of PTSD (e.g., Hermann, Meyer, Schnurr, Batten, & Walser, in press). Interventions that incorporate approaches within the contextual behavioral framework could help veterans with PTSD to accept negative thoughts and emotions associated with interpersonal interactions, pursue life goals consistent with their values (e.g., intimacy, love, and friendship), and become more psychologically flexible overall. Future research should evaluate whether treatment for veterans with PTSD focusing on reducing experiential avoidance in social contexts may result in improved social support and social functioning for these veterans.
Several limitations should be considered when interpreting the current findings. First, returning veterans included in this sample were mostly male, White, and enrolled in VA health care. Therefore, the current findings may not apply to other populations. Second, although the CAPS is often considered a gold standard PTSD assessment, ratings of lifetime PTSD symptom severity were based on retrospective self-report. Our measure of experiential avoidance, the AAQ-II measures the general tendency to engage in experiential avoidance. Therefore, we are not aware of the specific tendency for individuals in the present study to avoid interpersonal or trauma-related experiences. In addition, we do not have information specifically on participants’ predeployment experiential avoidance or predeployment social support, and whether their experience of trauma changed their tendency to avoid trauma-related or interpersonal experiences. Individuals high in experiential avoidance may also be more likely to develop PTSD and poor social support. Future longitudinal studies that have the opportunity to include measures before deployment may be able to provide more important information about these associations. The study also had several notable strengths, including its longitudinal design, its inclusion of well-validated measures, and its use of bootstrapping to test the hypothesized mediational model.
In conclusion, experiential avoidance appears to be an important mediator between PTSD symptoms and levels of perceived social support after deployment for Iraq and Afghanistan war veterans. Further research on interventions that target experiential avoidance in veterans may help improve levels of social support and the overall social reintegration of veterans with PTSD.
Clinical Impact Statement.
Veterans with posttraumatic stress disorder (PTSD) often have low levels of social support. Experiential avoidance appears to be an important mediator that accounts for why some people with PTSD have lower levels of social support than others. Interventions that target experiential avoidance in veterans with PTSD may help to improve their social support and overall social reintegration, but more research in this area is necessary.
Acknowledgments
This material is based upon work supported by the VISN 17 Center of Excellence for Research on Returning War Veterans, the VISN 1 Mental Illness Research, Education, and Clinical Center, the Social and Community Reintegration Research Program, a VA Merit Award I01RX000304–01 to SBM and I01RX000304–04 to ECM and SBM from the Rehabilitation Research and Development Service of the VA Office of Research and Development (ORD), a Career Development Award (IK2 CX000525) to NAK from Clinical Sciences Research and Development Service of VA ORD, the Department of Veterans Affairs VISN 17 Center of Excellence for Research on Returning War Veterans, and the Central Texas Veterans Health Care System. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. We thank and Julie A. Kittel for help with formatting the manuscript.
Contributor Information
Megan M. Kelly, Edith Nourse Rogers Memorial Veterans Hospital, Bedford, Massachusetts and University of Massachusetts Medical School
Bryann B. DeBeer, VISN 17 Center of Excellence for Research on Returning War Veterans, Waco, Texas and Texas A&M University Health Science Center College of Medicine
Eric C. Meyer, VISN 17 Center of Excellence for Research on Returning War Veterans, Waco, Texas and Texas A&M University Health Science Center College of Medicine
Nathan A. Kimbrel, VA Mid-Atlantic Mental Illness Research, Education, and Clinical Center, Baltimore, Maryland and Duke University Medical Center
Suzy B. Gulliver, Baylor, Scott & White Healthcare System, Dallas, Texas and Texas A&M University Health Science Center College of Medicine
Sandra B. Morissette, The University of Texas at San Antonio
References
- Arch JJ, Eifert GH, Davies C, Vilardaga JCP, Rose RD, & Craske MG (2012). Randomized clinical trial of cognitive behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for mixed anxiety disorders. Journal of Consulting and Clinical Psychology, 80, 750–765. 10.1037/a0028310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckham JC, Feldman ME, Kirby AC, Hertzberg MA, & Moore SD (1997). Interpersonal violence and its correlates in Vietnam veterans with chronic posttraumatic stress disorder. Journal of Clinical Psychology, 53, 859–869. 10.1002/(SICI)10974679(199712)53:8859:AID-JCLP113.0.CO;2-J [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). Development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8, 75–90. 10.1002/jts.2490080106 [DOI] [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, … Zettle RD(2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42, 676–688. 10.1016/j.beth.2011.03.007 [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, & Valentine JD (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–766. 10.1037/0022-006X.68.5.748 [DOI] [PubMed] [Google Scholar]
- Cohen E, Zerach G, & Solomon Z (2011). The implication of combat-induced stress reaction, PTSD, and attachment in parenting among war veterans. Journal of Family Psychology, 25, 688–698. 10.1037/a0024065 [DOI] [PubMed] [Google Scholar]
- Cohen S, & Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98, 310–357. 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- DeBeer B, Kimbrel NA, Meyer EC, Gulliver SB, & Morissette SB (2014). Combined PTSD and depressive symptoms interact with post-deployment social support to predict suicidal ideation in Operation Enduring Freedom and Operation Iraqi Freedom veterans. Psychiatry Research, 216, 357–362. 10.1016/j.psychres.2014.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirkzwager AJE, Bramsen I, & van der Ploeg HM (2005). Factors associated with posttraumatic stress among peacekeeping soldiers. Anxiety, Stress, & Coping, 18, 37–51. 10.1080/10615800412336418 [DOI] [Google Scholar]
- Ditlevsen DN, & Elklit A (2010). The combined effect of gender and age on post traumatic stress disorder: Do men and women show differences in the lifespan distribution of the disorder? Annals of General Psychiatry, 9, 32. 10.1186/1744-859X-9-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duax JM, Bohnert KM, Rauch SAM, & Defever AM (2014). Posttraumatic stress disorder symptoms, levels of social support, and emotional hiding in returning veterans. Journal of Rehabilitation Research and Development, 51, 571–578. 10.1682/JRRD.2012.12.0234 [DOI] [PubMed] [Google Scholar]
- Dursa EK, Reinhard MJ, Barth SK, & Schneiderman AI (2014). Prevalence of a positive screen for PTSD among OEF/OIF and OEF/OIF-era veterans in a large population-based cohort. Journal of Traumatic Stress, 27, 542–549. 10.1002/jts.21956 [DOI] [PubMed] [Google Scholar]
- Forman EM, Herbert JD, Moitra E, Yeomans PD, & Geller PA (2007). A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior Modification, 31, 772–799. 10.1177/0145445507302202 [DOI] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, … Beckham JC (2015). The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans: A meta-analysis. Journal of Anxiety Disorders, 31, 98–107. 10.1016/j.janxdis.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Gardner FL, & Moore ZE (2008). Understanding clinical anger and violence: The anger avoidance model. Behavior Modification, 32, 897–912. 10.1177/0145445508319282 [DOI] [PubMed] [Google Scholar]
- Gerhart JI, Baker CN, Hoerger M, & Ronan GF (2014). Experiential avoidance and interpersonal problems: A moderated mediation model. Journal of Contextual Behavioral Science, 3, 291–298. 10.1016/j.jcbs.2014.08.003 [DOI] [Google Scholar]
- Gratz KL, & Gunderson JG (2006). Preliminary data on an acceptance-based emotion regulation group intervention for deliberate self-harm among women with borderline personality disorder. Behavior Therapy, 37, 25–35. 10.1016/j.beth.2005.03.002 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression based approach. New York, NY: Guilford Press. [Google Scholar]
- Hayes SC, Strosahl KD, & Wilson KG (2012). Acceptance and commitment therapy: The process and practice of mindful change (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Hermann BA, Meyer EC, Schnurr PP, Batten SV, & Walser RD (in press). Acceptance and Commitment Therapy for co-occurring PTSD and substance use: A manual development study. Journal of Contextual Behavioral Science.
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, & Koffman RL (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine, 351, 13–22. 10.1056/NEJMoa040603 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, & Layton JB (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine, 7, e1000316. 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karelina K, & DeVries AC (2011). Modeling social influences on human health. Psychosomatic Medicine, 73, 67–74. 10.1097/PSY.0b013e3182002116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King D, Taft C, King LA, Hammond C, & Stone ER (2006). Directionality of the association between social support and posttraumatic stress disorder: A longitudinal investigation. Journal of Applied Social Psychology, 36, 2980–2992. 10.1111/j.0021-9029.2006.00138.x [DOI] [Google Scholar]
- Laffaye C, Cavella S, Drescher K, & Rosen C (2008). Relationships among PTSD symptoms, social support, and support source in veterans with chronic PTSD. Journal of Traumatic Stress, 21, 394–401. 10.1002/jts.20348 [DOI] [PubMed] [Google Scholar]
- MacDonald C, Chamberlain K, Long N, & Flett R (1999). Posttraumatic stress disorder and interpersonal functioning in Vietnam War veterans: A mediational model. Journal of Traumatic Stress, 12, 701–707. 10.1023/A:1024729520686 [DOI] [PubMed] [Google Scholar]
- Meyer EC, Konecky B, Kimbrel NA, DeBeer BB, Marx B, Schumm J, … Morissette SB (in press). Gender differences in associations between DSM–5 posttraumatic stress disorder symptom clusters and functional impairment in war veterans. Psychological Services. [DOI] [PubMed]
- Meyer EC, Morissette SB, Kimbrel NA, Kruse MI, & Gulliver SB (2013). Acceptance and Action Questionnaire-II scores as a predictor of posttraumatic stress disorder symptoms among war veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 5, 521–528. 10.1037/a0030178 [DOI] [Google Scholar]
- Milliken CS, Auchterlonie JL, & Hoge CW (2007). Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. Journal of the American Medical Association, 298, 2141–2148. 10.1001/jama.298.18.2141 [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, & Weiss DS (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52–73. 10.1037/0033-2909.129.1.52 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments & Computers, 36, 717–731. 10.3758/BF03206553 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, & Hayes AF (2007). Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research, 42, 185–227. 10.1080/00273170701341316 [DOI] [PubMed] [Google Scholar]
- Price M, Gros DF, Strachan M, Ruggiero KJ, & Acierno R (2013). The role of social support in exposure therapy for Operation Iraqi Freedom/Operation Enduring Freedom Veterans: A preliminary investigation. Psychological Trauma: Theory, Research, Practice, and Policy, 5, 93–100. 10.1037/a0026244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins MA, Verhaak PF, Hilbink-Smolders M, Spreeuwenberg P, Laurant MG, van der Meer K, … Bensing JM (2011). Outcomes for depression and anxiety in primary care and details of treatment: A naturalistic longitudinal study. BMC Psychiatry, 11, 180. 10.1186/1471-244X-11-180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy MK, Meis LA, Erbes CR, Polusny MA, & Compton JS (2011). Associations among experiential avoidance, couple adjustment, and interpersonal aggression in returning Iraqi war veterans and their partners. Journal of Consulting and Clinical Psychology, 79, 515–520. 10.1037/a0023929 [DOI] [PubMed] [Google Scholar]
- Seal K, Metzler TJ, Gima KS, Bertenthal D, Maguen S, & Marmar CR (2009). Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care. American Journal of Public Health, 99, 1651–1658. 10.2105/AJPH.2008.150284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shallcross SL, Arbisi PA, Polusny MA, Kramer MD, & Erbes CR (2016). Social causation versus social erosion: Comparisons of causal models for relations between support and PTSD symptoms. Journal of Traumatic Stress, 29, 167–175. 10.1002/jts.22086 [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Janavs J, Baker R, Harnett-Sheehan K, Knapp E, Sheehan M, … Bonora LI (1998). MINI-Mini International Neuropsychiatric Interview-English Version 5.0. 0-DSM–IV. The Journal of Clinical Psychiatry, 59, 34–40. [PubMed] [Google Scholar]
- Solomon Z, Dekel R, & Zerach G (2008). The relationships between posttraumatic stress symptom clusters and marital intimacy among war veterans. Journal of Family Psychology, 22, 659–666. 10.1037/a0013596 [DOI] [PubMed] [Google Scholar]
- Tsai J, Harpaz-Rotem I, Pietrzak RH, & Southwick SM (2012). The role of coping, resilience, and social support in mediating the relation between PTSD and social functioning in veterans returning from Iraq and Afghanistan. Psychiatry, 75, 135–149. 10.1521/psyc.2012.75.2.135 [DOI] [PubMed] [Google Scholar]
- Vogt DS, Proctor SP, King DW, King LA, & Vasterling JJ (2008). Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment, 15, 391–403. 10.1177/1073191108316030 [DOI] [PubMed] [Google Scholar]
- Vowles KE, & McCracken LM (2008). Acceptance and values-based action in chronic pain: A study of treatment effectiveness and process. Journal of Consulting and Clinical Psychology, 76, 397–407. 10.1037/0022-006X.76.3.397 [DOI] [PubMed] [Google Scholar]
- Walser RD, Garvert DW, Karlin BE, Trockel M, Ryu DM, & Taylor CB (2015). Effectiveness of Acceptance and Commitment Therapy in treating depression and suicidal ideation in Veterans. Behaviour Research and Therapy, 74, 25–31. 10.1016/j.brat.2015.08.012 [DOI] [PubMed] [Google Scholar]
- Welsh JA, Olson J, Perkins DF, Travis WJ, & Ormsby L (2015). The role of natural support systems in the post-deployment adjustment of active duty military personnel. American Journal of Community Psychology, 56, 69–78. 10.1007/s10464-015-9726-y [DOI] [PubMed] [Google Scholar]
- Xue C, Ge Y, Tang B, Liu Y, Kang P, Wang M, & Zhang L (2015). A meta-analysis of risk factors for combat-related PTSD among military personnel and veterans. PLoS ONE, 10, e0120270. 10.1371/journal.pone.0120270 [DOI] [PMC free article] [PubMed] [Google Scholar]


