Key Points
Question
Do secular trends in cardiovascular risk factors differ by race and ethnicity and by socioeconomic status in the US?
Findings
In this US serial cross-sectional survey study conducted from 1999 through 2018 that included 50 571 participants, there were significant increases in body mass index and hemoglobin A1c and significant decreases in serum total cholesterol and cigarette smoking from 1999 to 2018. Mean age- and sex-adjusted estimated 10-year risk of atherosclerotic cardiovascular disease was constantly higher in non-Hispanic Black participants compared with non-Hispanic White participants, but this difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
Meaning
In a national US survey study from 1999 to 2018, differences in cardiovascular risk factors persisted between Black and White participants; the difference may be moderated by social determinants of health.
Abstract
Importance
After decades of decline, the US cardiovascular disease mortality rate flattened after 2010, and racial and ethnic differences in cardiovascular disease mortality persisted.
Objective
To examine 20-year trends in cardiovascular risk factors in the US population by race and ethnicity and by socioeconomic status.
Design, Setting, and Participants
A total of 50 571 participants aged 20 years or older from the 1999-2018 National Health and Nutrition Examination Surveys, a series of cross-sectional surveys in nationally representative samples of the US population, were included.
Exposures
Calendar year, race and ethnicity, education, and family income.
Main Outcomes and Measures
Age- and sex-adjusted means or proportions of cardiovascular risk factors and estimated 10-year risk of atherosclerotic cardiovascular disease were calculated for each of 10 two-year cycles.
Results
The mean age of participants ranged from 49.0 to 51.8 years and the proportion of women from 48.2% to 51.3% in the surveys. From 1999-2000 to 2017-2018, age- and sex-adjusted mean body mass index increased from 28.0 (95% CI, 27.5-28.5) to 29.8 (95% CI, 29.2-30.4); mean hemoglobin A1c increased from 5.4% (95% CI, 5.3%-5.5%) to 5.7% (95% CI, 5.6%-5.7%) (both P < .001 for linear trends). Mean serum total cholesterol decreased from 203.3 mg/dL (95% CI, 200.9-205.8 mg/dL) to 188.5 mg/dL (95% CI, 185.2-191.9 mg/dL); prevalence of smoking decreased from 24.8% (95% CI, 21.8%-27.7%) to 18.1% (95% CI, 15.4%-20.8%) (both P < .001 for linear trends). Mean systolic blood pressure decreased from 123.5 mm Hg (95% CI, 122.2-124.8 mm Hg) in 1999-2000 to 120.5 mm Hg (95% CI, 119.6-121.3 mm Hg) in 2009-2010, then increased to 122.8 mm Hg (95% CI, 121.7-123.8 mm Hg) in 2017-2018 (P < .001 for nonlinear trend). Age- and sex-adjusted 10-year atherosclerotic cardiovascular disease risk decreased from 7.6% (95% CI, 6.9%-8.2%) in 1999-2000 to 6.5% (95% CI, 6.1%-6.8%) in 2011-2012, then did not significantly change. Age- and sex-adjusted body mass index, systolic blood pressure, and hemoglobin A1c were consistently higher, while total cholesterol was lower in non-Hispanic Black participants compared with non-Hispanic White participants (all P < .001 for group differences). Individuals with college or higher education or high family income had consistently lower levels of cardiovascular risk factors. The mean age- and sex-adjusted 10-year risk of atherosclerotic cardiovascular disease was significantly higher in non-Hispanic Black participants compared with non-Hispanic White participants (difference, 1.4% [95% CI, 1.0%-1.7%] in 1999-2008 and 2.0% [95% CI, 1.7%-2.4%] in 2009-2018]). This difference was attenuated (–0.3% [95% CI, –0.6% to 0.1%] in 1999-2008 and 0.7% [95% CI, 0.3%-1.0%] in 2009-2018) after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
Conclusions and Relevance
In this serial cross-sectional survey study that estimated US trends in cardiovascular risk factors from 1999 through 2018, differences in cardiovascular risk factors persisted between Black and White participants; the difference may have been moderated by social determinants of health.
This National Health and Nutrition Examination Survey study assesses US trends in cardiovascular risk factors by race and ethnicity and by socioeconomic status from 1999 to 2018.
Introduction
Despite substantial declines in cardiovascular disease mortality since 1950, it remains the leading cause of death in the US general population.1 In addition, recent data show that the cardiovascular disease mortality rate flattened while the total number of cardiovascular deaths increased in the US general population from 2010 to 2018.1,2,3 The reasons for this deceleration in the decline of cardiovascular disease mortality are not entirely understood. Several recent studies have reported that the prevalences of obesity and diabetes have increased4,5 and the proportion of patients with controlled hypertension has decreased in the US general population.6
Racial and ethnic differences in cardiovascular disease mortality persist despite a significant reduction in the cardiovascular disease burden in the US general population.1,7 In the US, Black persons are at an increased risk of obesity, diabetes, and hypertension compared with White persons.4,5,8,9,10 Social determinants of health, including socioeconomic status, neighborhood and physical environment, social support networks, and access to health care, may help explain persistent racial and ethnic differences in cardiovascular disease and risk factors.11,12 Understanding the secular trends of cardiovascular risk factors among US subpopulations with various racial and ethnic backgrounds and socioeconomic status may be helpful to guide the development of national public health policies for targeted interventions aimed at eliminating health disparities.
The current study aimed to estimate 20-year trends in multiple cardiovascular risk factors in the US population and to compare these trends according to race and ethnicity and socioeconomic status using data from the National Health and Nutrition Examination Surveys (NHANES) from 1999 to 2018.
Methods
Study Participants
NHANES was designed to assess the health and nutritional status of the US general population. A stratified, multistage probability sampling method was used to select a series of cross-sectional, nationally representative samples.13 Since 1999-2000, the survey has been conducted in 2-year cycles. For the current analysis, 10 cycles conducted from 1999-2000 through 2017-2018 were used. The study protocols were approved by the institutional review board of the National Center for Health Statistics, and written informed consent was obtained from each participant.
Data Collection
In each 2-year survey, participants completed in-home interviews and visited a mobile examination center, where they responded to additional questionnaires and underwent a physical examination and blood sample collection. A standardized questionnaire was used to collect information on age, race and ethnicity, sex, education, income, and medical history.14 Self-reported race data including 6 categories (American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Pacific Islander, White, or other) in addition to Hispanic origin were collected. Non-Hispanic Asian was not listed as a separate race and ethnicity until 2011-2012. Data on education, income, employment, housing, health insurance, and access to health care were collected. The income-to-poverty ratio (annual family income divided by the poverty threshold adjusted for family size and inflation) was used as a measure of income. Cigarette smoking status was based on responses to questionnaires regarding whether a participant was currently smoking or had formerly smoked cigarettes. Personal medical history and medication use for hypertension, diabetes, and hypercholesterolemia were assessed during the in-home interview. Self-reported history of cardiovascular disease was defined as having ever been diagnosed as having coronary heart disease, stroke, or congestive heart failure.
During the physical examination, weight and height were measured and body mass index was calculated as weight in kilograms divided by height in meters squared. Blood pressure was measured by trained staff using a mercury sphygmomanometer after the participant rested quietly in a seated position for at least 5 minutes.15 Three blood pressure measurements were obtained and the mean of all measurements was used in analyses. Blood samples were collected at the mobile examination center, stored at −20 °C, and sent to central laboratories for the determination of total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein (LDL) cholesterol, triglycerides, plasma glucose, and hemoglobin A1c using standard methods. Eight-hour fasting blood samples were only available in a subsample of survey participants for measuring LDL cholesterol, triglycerides, and glucose.
The 10-year risk of atherosclerotic cardiovascular disease was calculated using the Pooled Cohort Equations among individuals without a self-reported history of cardiovascular disease.16 Obesity was defined as body mass index of 30 or higher; hypertension as systolic blood pressure of 130 mm Hg or higher, diastolic blood pressure of 80 mm Hg or higher, or use of antihypertensive medications; diabetes as fasting plasma glucose of 126 mg/dL or higher, hemoglobin A1c of 6.5% or higher, or use of antidiabetic medications; and hypercholesterolemia as total cholesterol of 240 mg/dL (6.2 mmol/L) or higher or use of lipid-lowering medications.1,17,18 The same cut point of body mass index for obesity was used for Asian participants because the same pattern of body mass index and mortality associations was observed in large prospective cohort studies in Asian populations and non-Asian populations.19,20
Statistical Analysis
The age- and sex-adjusted means or proportions of cardiovascular risk factors were calculated separately using data from each of the 10 two-year cycles from 1999-2000 through 2017-2018.21 Age and sex adjustment was performed using the direct standardization method to the 2000 US Census population using the following 6 age and sex categories: men aged 20 to 39, 40 to 59, and 60 or more years, and women aged 20 to 39, 40 to 59, and 60 or more years.13 For sex-specific estimates, 3 age categories were used for adjustment. Subgroup analyses by race and ethnicity (non-Hispanic Asian, non-Hispanic Black, Hispanic, and non-Hispanic White), education levels (less than high school, high school graduate, some college, and college graduate or higher), and family income-to-poverty ratios (≤100%, >100%-299%, 300%-499%, and ≥500%) were conducted.
Linear regression was used for age- and sex-adjusted means and logistic regression for proportions to test the statistical significance of linear or nonlinear trends as well as group differences. Nonlinearity of secular trend was tested by adding a quadratic term into the regression models. In addition, Joinpoint trend analysis was applied to assess the statistical significance of changes in regression slopes between 2 or more time periods.22 Age- and sex-adjusted means or proportions over time with zero joinpoints (linear trend) were first fit and a Monte Carlo permutation method was then used to test whether more joinpoints were statistically significant.23 Statistically significant changes in trends by time periods were reported. The homogeneity of secular trends among subgroups was tested using an interaction term of time by subgroup in the regression models. A linear or quadratic term of time was used for testing the homogeneity of linear or nonlinear trends. To examine whether observed racial and ethnic differences in cardiovascular disease and risk factors were moderated by social determinants of health, racial and ethnic differences were compared after adjusting for education, income, home ownership, employment, health insurance, and access to health care. Data from 1999-2008 and 2009-2018 were pooled to increase sample size, and analyses were limited to White, Black, and Hispanic participants due to lack of data from Asian participants in most years.
All analyses were conducted using SAS statistical software, version 9.4 (SAS Institute Inc) with survey analysis procedures to account for the complex sampling design. The survey examination weights were used for analysis as appropriate to obtain nationally representative estimates. These original weights were recalibrated based on the proportion of participants with missing data by age, sex, and race and ethnicity categories within each cycle.13 All statistical tests were 2-sided, and P < .05 was considered statistically significant. Because of the potential for type I error due to the absence of adjustment for multiple comparisons, the analysis results should be interpreted as exploratory.
Results
The current analyses were limited to participants aged 20 years or older (n = 55 081). In addition, those who did not participate in physical examinations (n = 2683) or were pregnant or lactating at the time of examination (n = 1827) were excluded. After exclusion, a total of 50 571 participants were included in the final analysis sample (Table 1). The mean age of study participants ranged from 49.0 to 51.8 years and the proportion of women from 48.2% to 51.3% in the surveys (Table 1). Participants in Asian, Black, and Hispanic subpopulations were oversampled in all surveys. Proportions of persons with less than high school education decreased from 39.7% in 1999-2000 to 20.0% in 2017-2018, while those who were college graduates or higher increased from 15.4% to 24.0% during the same period. Proportions of persons who lived in poverty varied from 16.9% to 25.7%, those who did not own a home from 32.0% to 43.7%, those who were unemployed from 19.6% to 25.2%, those who did not have health insurance from 13.7% to 25.5%, and those who did not have regular health care access from 13.9% to 18.3%.
Table 1. Characteristics of Study Participants in the National Health and Nutrition Examination Surveys (NHANES), 1999-2018.
| Characteristics | 1999-2000 | 2001-2002 | 2003-2004 | 2005-2006 | 2007-2008 | 2009-2010 | 2011-2012 | 2013-2014 | 2015-2016 | 2017-2018 |
|---|---|---|---|---|---|---|---|---|---|---|
| Total No. of participants | 4158 | 4685 | 4486 | 4410 | 5619 | 5960 | 5239 | 5484 | 5360 | 5170 |
| Age, mean (SD), y | 51.4 (18.5) | 50.6 (18.7) | 51.7 (19.3) | 49.9 (18.7) | 50.9 (17.8) | 49.8 (17.8) | 49.0 (17.7) | 49.5 (17.4) | 49.9 (17.6) | 51.8 (17.6) |
| Women, No. (%) | 2084 (50.1) | 2299 (49.1) | 2211 (49.3) | 2126 (48.2) | 2822 (50.2) | 3031 (50.9) | 2619 (50.0) | 2815 (51.3) | 2736 (51.0) | 2629 (50.9) |
| Men, No. (%) | 2074 (49.9) | 2386 (50.9) | 2275 (50.7) | 2284 (51.8) | 2797 (49.8) | 2929 (49.1) | 2620 (50.0) | 2669 (48.7) | 2624 (49.0) | 2541 (49.1) |
| Race and ethnicity, No. (%)a | n = 4031 | n = 4540 | n = 4295 | n = 4238 | n = 5391 | n = 5631 | n = 5091 | n = 5325 | n = 5167 | n = 4907 |
| Non-Hispanic Asian | 743 (14.6) | 621 (11.7) | 633 (12.3) | 746 (15.2) | ||||||
| Non-Hispanic Black | 815 (20.2) | 924 (20.4) | 896 (20.9) | 1039 (24.5) | 1169 (21.7) | 1074 (19.1) | 1383 (27.2) | 1125 (21.1) | 1140 (22.1) | 1215 (24.8) |
| Hispanic | 1368 (33.9) | 1173 (25.8) | 1014 (23.6) | 975 (23.0) | 1574 (29.2) | 1682 (29.9) | 1046 (20.5) | 1224 (23.0) | 1631 (31.6) | 1166 (23.8) |
| Non-Hispanic White | 1848 (45.8) | 2443 (53.8) | 2385 (55.5) | 2224 (52.5) | 2648 (49.1) | 2875 (51.1) | 1919 (37.7) | 2355 (44.2) | 1763 (34.1) | 1780 (36.3) |
| Education, No. (%) | n = 4144 | n = 4677 | n = 4477 | n = 4403 | n = 5613 | n = 5946 | n = 5235 | n = 5479 | n = 5357 | n = 5158 |
| Less than high school | 1645 (39.7) | 1444 (30.9) | 1338 (29.9) | 1224 (27.8) | 1743 (31.1) | 1704 (28.7) | 1253 (23.9) | 1186 (21.6) | 1278 (23.9) | 1033 (20.0) |
| High school graduate | 939 (22.7) | 1102 (23.6) | 1145 (25.6) | 1063 (24.1) | 1392 (24.8) | 1370 (23.0) | 1104 (21.1) | 1240 (22.6) | 1168 (21.8) | 1233 (23.9) |
| Some college | 921 (22.2) | 1215 (26.0) | 1207 (27.0) | 1254 (28.5) | 1432 (25.5) | 1665 (28.0) | 1568 (30.0) | 1690 (30.8) | 1584 (29.6) | 1653 (32.0) |
| College graduate or higher | 639 (15.4) | 916 (19.6) | 787 (17.6) | 862 (19.6) | 1046 (18.6) | 1207 (20.3) | 1310 (25.0) | 1363 (24.9) | 1327 (24.8) | 1239 (24.0) |
| Family income-to-poverty ratio, No. (%) | n = 3562 | n = 4347 | n = 4222 | n = 4200 | n = 5097 | n = 5382 | n = 4791 | n = 5061 | n = 4803 | n = 4485 |
| ≤100% | 734 (20.6) | 753 (17.3) | 781 (18.5) | 710 (16.9) | 1056 (20.7) | 1214 (22.6) | 1233 (25.7) | 1146 (22.6) | 1092 (22.7) | 843 (18.8) |
| >100%-299% | 1521 (42.7) | 1795 (41.3) | 1869 (44.3) | 1721 (41.0) | 2245 (44.0) | 2261 (42.0) | 1879 (39.2) | 1977 (39.1) | 2118 (44.1) | 1991 (44.4) |
| 300%-499% | 714 (20.0) | 926 (21.3) | 888 (21.0) | 959 (22.8) | 909 (17.8) | 1017 (18.9) | 865 (18.1) | 996 (19.7) | 813 (16.9) | 858 (19.1) |
| ≥500% | 593 (16.6) | 873 (20.1) | 684 (16.2) | 810 (19.3) | 887 (17.4) | 890 (16.5) | 814 (17.0) | 942 (18.6) | 780 (16.2) | 793 (17.7) |
| Home ownership, No. (%) | n = 4098 | n = 4617 | n = 4446 | n = 4376 | n = 5569 | n = 5926 | n = 5214 | n = 5415 | n = 5188 | n = 4918 |
| Owned homeb | 2637 (64.3) | 3141 (68.0) | 2906 (65.4) | 2952 (67.5) | 3640 (65.4) | 3654 (61.7) | 2937 (56.3) | 3274 (60.5) | 3076 (59.3) | 2951 (60.0) |
| Rented home or other arrangement | 1461 (35.7) | 1476 (32.0) | 1540 (34.6) | 1424 (32.5) | 1929 (34.6) | 2272 (38.3) | 2277 (43.7) | 2141 (39.5) | 2112 (40.7) | 1967 (40.0) |
| Employment status, No. (%) | n = 4155 | n = 4683 | n = 4483 | n = 4407 | n = 5617 | n = 5956 | n = 5238 | n = 5479 | n = 5348 | n = 5167 |
| Employed, student, or retired | 3265 (78.6) | 3765 (80.4) | 3538 (78.9) | 3542 (80.4) | 4374 (77.9) | 4459 (74.9) | 3919 (74.8) | 4230 (77.2) | 4119 (77.0) | 4012 (77.6) |
| Unemployed | 890 (21.4) | 918 (19.6) | 945 (21.1) | 865 (19.6) | 1243 (22.1) | 1497 (25.1) | 1319 (25.2) | 1249 (22.8) | 1229 (23.0) | 1155 (22.4) |
| Type of health insurance, No. (%) | n = 4062 | n = 4580 | n = 4425 | n = 4392 | n = 5602 | n = 5940 | n = 5207 | n = 5452 | n = 5284 | n = 5096 |
| Private | 2403 (59.2) | 2760 (60.3) | 2372 (53.6) | 2453 (55.9) | 2991 (53.4) | 3039 (51.2) | 2594 (49.8) | 2853 (52.3) | 2645 (50.1) | 2540 (49.8) |
| Governmentc | 805 (19.8) | 957 (20.9) | 1180 (26.7) | 960 (21.9) | 1284 (22.9) | 1386 (23.3) | 1363 (26.2) | 1438 (26.4) | 1713 (32.4) | 1782 (35.0) |
| None | 854 (21.0) | 863 (18.8) | 873 (19.7) | 979 (22.3) | 1327 (23.7) | 1515 (25.5) | 1250 (24.0) | 1161 (21.3) | 926 (17.5) | 774 (15.2) |
| Regular health care access, No. (%) | n = 4155 | n = 4685 | n = 4486 | n = 4410 | n = 5619 | n = 5960 | n = 5239 | n = 5484 | n = 5360 | n = 5168 |
| ≥1 Health care facilityd | 3457 (83.2) | 3971 (84.8) | 3870 (86.3) | 3723 (84.4) | 4786 (85.2) | 5019 (84.2) | 4428 (84.5) | 4599 (83.9) | 4426 (82.6) | 4222 (81.7) |
| None | 698 (16.8) | 714 (15.2) | 616 (13.7) | 687 (15.6) | 833 (14.8) | 941 (15.8) | 811 (15.5) | 885 (16.1) | 934 (17.4) | 946 (18.3) |
NHANES collected self-reported race data in 6 categories (American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Pacific Islander, White, or other) and data on Hispanic origin. Non-Hispanic Asian was listed as a race and ethnicity group starting in NHANES 2011-2012. American Indian or Alaska Native and Native Hawaiian or Pacific Islander were not listed as separate race and ethnicity groups in the data sets.
Answered “owned or being bought” to “Is this home owned, being bought, rented, or occupied by some other arrangement by you or someone else in your family?” A person owned a home if paying a mortgage.
Medicare, Medicaid, and other government insurance.
Answered “yes” or “There is more than one place” to “Is there a place that you usually go when you are sick or you need advice about your health?”
Cardiovascular Risk Factors From 1999-2000 to 2017-2018
Age- and sex-adjusted mean body mass index increased from 28.0 (95% CI, 27.5-28.5) in 1999-2000 to 29.8 (95% CI, 29.2-30.4) in 2017-2018 (P < .001 for linear trend) in the study population (Figure 1; eTable 1 in the Supplement). Mean systolic blood pressure decreased from 123.5 mm Hg (95% CI, 122.2-124.8 mm Hg) in 1999-2000 to 120.5 mm Hg (95% CI, 119.6-121.3 mm Hg) in 2009-2010, then increased to 122.8 mm Hg (95% CI, 121.7-123.8 mm Hg) in 2017-2018 (P < .001 for nonlinear trend). The joinpoint trend was significant (P = .006) for differences in slopes between the 2 time periods. The similar nonlinear trend was observed in age groups of 40 to 59 years and 60 years or older (eTable 2 in the Supplement). Mean hemoglobin A1c increased from 5.4% (95% CI, 5.3%-5.5%) in 1999-2000 to 5.7% (95% CI, 5.6%-5.7%) in 2017-2018 (P < .001 for linear trend). Mean serum total cholesterol decreased from 203.3 mg/dL (95% CI, 200.9-205.8 mg/dL) in 1999-2000 to 188.5 mg/dL (95% CI, 185.2-191.9 mg/dL) in 2017-2018 (P < .001 for linear trend). Age- and sex-adjusted prevalence of current smoking decreased from 24.8% (95% CI, 21.8%-27.7%) in 1999-2000 to 18.1% (95% CI, 15.4%-20.8%) in 2017-2018 (P < .001 for linear trend).
Figure 1. Trends in Cardiovascular Risk Factors in US Adults.
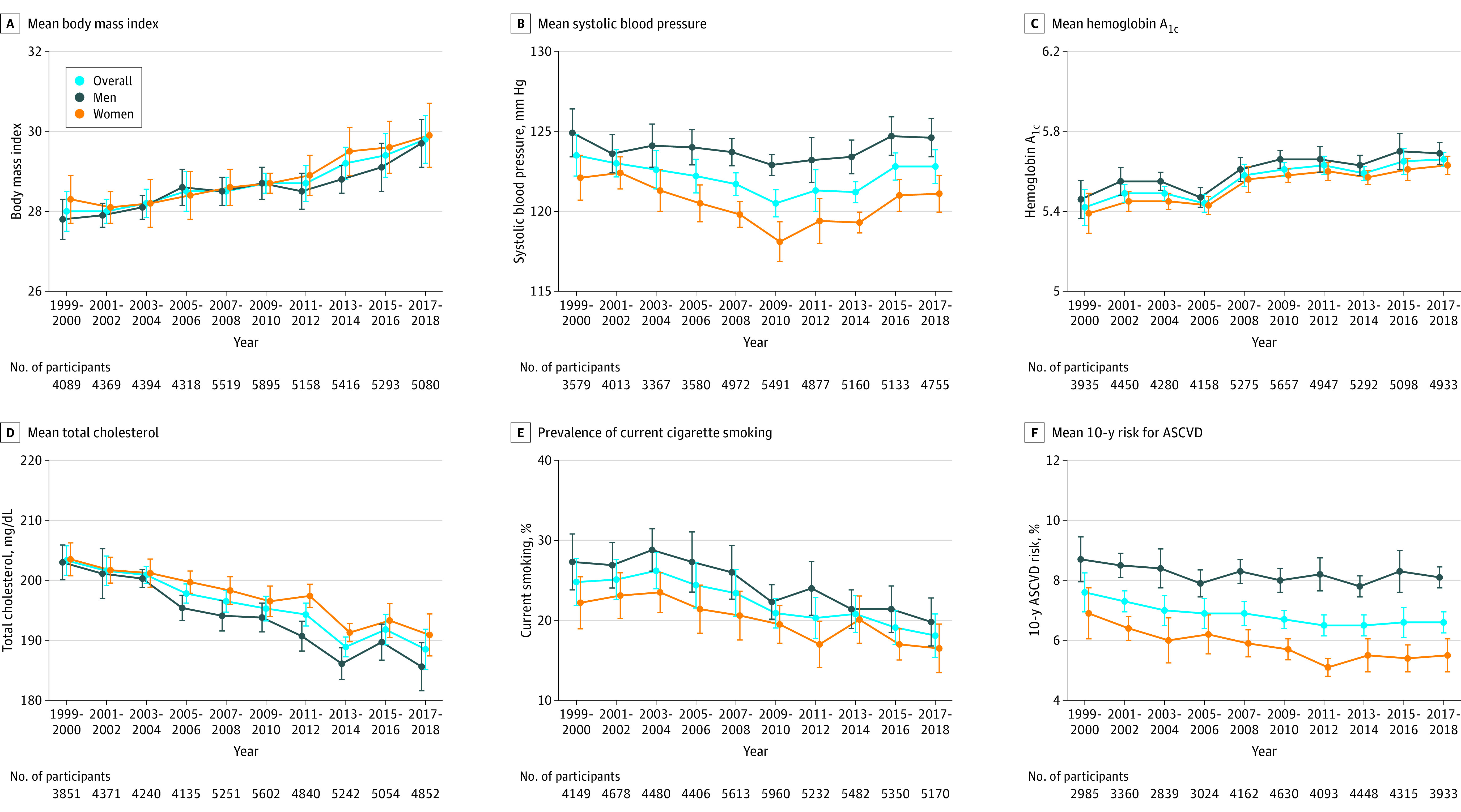
Trends in (A) mean body mass index (calculated as weight in kilograms divided by height in meters squared) (all P < .001 for linear trend); (B) mean systolic blood pressure (P < .001 overall, P = .01 for men, and P < .001 women for nonlinear trend); (C) mean hemoglobin A1c (all P < .001 for linear trend); (D) mean serum total cholesterol (to convert to millimoles per liter, multiply by 0.0259) (all P < .001 for linear trend); (E) prevalence of current cigarette smoking (all P < .001 for linear trend); and (F) mean estimated 10-year risk of atherosclerotic cardiovascular disease (ASCVD) (P < .001 overall, P = .10 for men, and P < .001 for women for linear trend). The 10-year risk of ASCVD was calculated using the Pooled Cohort Equations among individuals without a self-reported history of cardiovascular disease. The probability of developing ASCVD over 10 years ranged from 0% to 100%. All estimates were standardized to the 2000 US Census population using 6 age and sex categories: men aged 20-39, 40-59, and ≥60 years and women aged 20-39, 40-59, and ≥60 years. Linear and polynomial models were used to test linear and nonlinear trends. Error bars indicate 95% CIs.
Age- and sex-adjusted prevalence of obesity increased from 30.2% (95% CI, 26.9%-33.4%) in 1999-2000 to 42.4% (95% CI, 38.6%-46.3%) in 2017-2018 and diabetes from 8.2% (95% CI, 6.8%-9.6%) to 12.7% (95% CI, 11.5%-14.0%) in the same period (both P < .001 for linear trend) (eTable 3 in the Supplement). Prevalence of hypertension decreased from 47.3% (95% CI, 44.1%-50.5%) in 1999-2000 to 42.9% (95% CI, 40.5%-45.4%) in 2009-2010, then increased to 46.5% (95% CI, 43.5%-49.5%) in 2017-2018 (P = .007 for nonlinear trend). Prevalence of hypercholesterolemia increased from 25.7% (95% CI, 22.7%-28.7%) in 1999-2000 to 30.4% (95% CI, 27.9%-32.9%) in 2009-2010, then decreased to 24.8% (95% CI, 23.2%-26.5%) in 2017-2018 (P < .001 for nonlinear trend). The joinpoint trend was significant (P = .003) for differences in slopes between the 2 time periods.
The age- and sex-adjusted proportions of antihypertensive medication and statin use increased from 17.2% (95% CI, 15.1%-19.3%) and 10.3% (95% CI, 9.1%-11.4%) in 1999-2000 to 22.3% (95% CI, 20.5%-24.1%) and 18.0% (95% CI, 16.9%-19.1%) in 2009-2010, then decreased to 21.1% (95% CI, 19.0%-23.3%) and 15.5% (95% CI, 14.0%-17.0%) in 2017-2018, respectively (both P < .001 for nonlinear trend (eTable 4 in the Supplement). The proportion of antidiabetic medication use increased from 5.3% (95% CI, 4.1%-6.5%) in 1999-2000 to 8.6% (95% CI, 7.5%-9.6%) in 2017-2018 (P < .001 for linear trend).
Age- and sex-adjusted estimated 10-year risk of atherosclerotic cardiovascular disease decreased from 7.6% (95% CI, 6.9%-8.2%) in 1999-2000 to 6.5% (95% CI, 6.1%-6.8%) in 2011-2012, then became flat among individuals without a self-reported history of cardiovascular disease (Figure 1; eTable 1 in the Supplement). The joinpoint trend was significant (P = .02) for difference in slopes between 1999-2010 and 2011-2018. The estimated 10-year risk decreased from 1.8% (95% CI, 1.3%-2.4%) in 1999-2000 to 1.1% (95% CI, 0.9%-1.3%) in 2017-2018 among those aged 20 to 39 years (P < .001 for linear trend); did not significantly change among those aged 40 to 59 years (P = .35 for linear trend); and decreased from 22.9% (95% CI, 20.8%-25.0%) in 1999-2000 to 19.3% (95% CI, 18.2%-20.4%) in 2011-2012 and increased to 20.0% (95% CI, 18.6%-21.4%) in 2017-2018 among those aged 60 years or older (P = .04 for nonlinear trend) (eTable 2 in the Supplement). Age- and sex-adjusted prevalence of self-reported cardiovascular disease was stable, at 7.2% (95% CI, 5.9%-8.6%) in 1999-2000 and 7.3% (95% CI, 6.2%-8.5%) in 2017-2018 (P = .16 for linear trend) (eTable 4 in the Supplement).
Secular Trends by Race and Ethnicity
Age- and sex-adjusted cardiovascular risk factors by race and ethnicity followed the same pattern, although with different magnitudes, as those in the overall population for mean body mass index, hemoglobin A1c, total cholesterol, and prevalence of cigarette smoking (all P < .05 for subgroup homogeneity) (Figure 2; eTable 5 in the Supplement). Moreover, age- and sex-adjusted mean body mass index, systolic blood pressure, and hemoglobin A1c were significantly higher while total cholesterol levels were lower in Black participants compared with White participants in all time periods. White participants had the lowest mean hemoglobin A1c while Asian participants had the lowest mean body mass index and prevalence of current smoking.
Figure 2. Trends in Cardiovascular Risk Factors by Race and Ethnicity in US Adults.
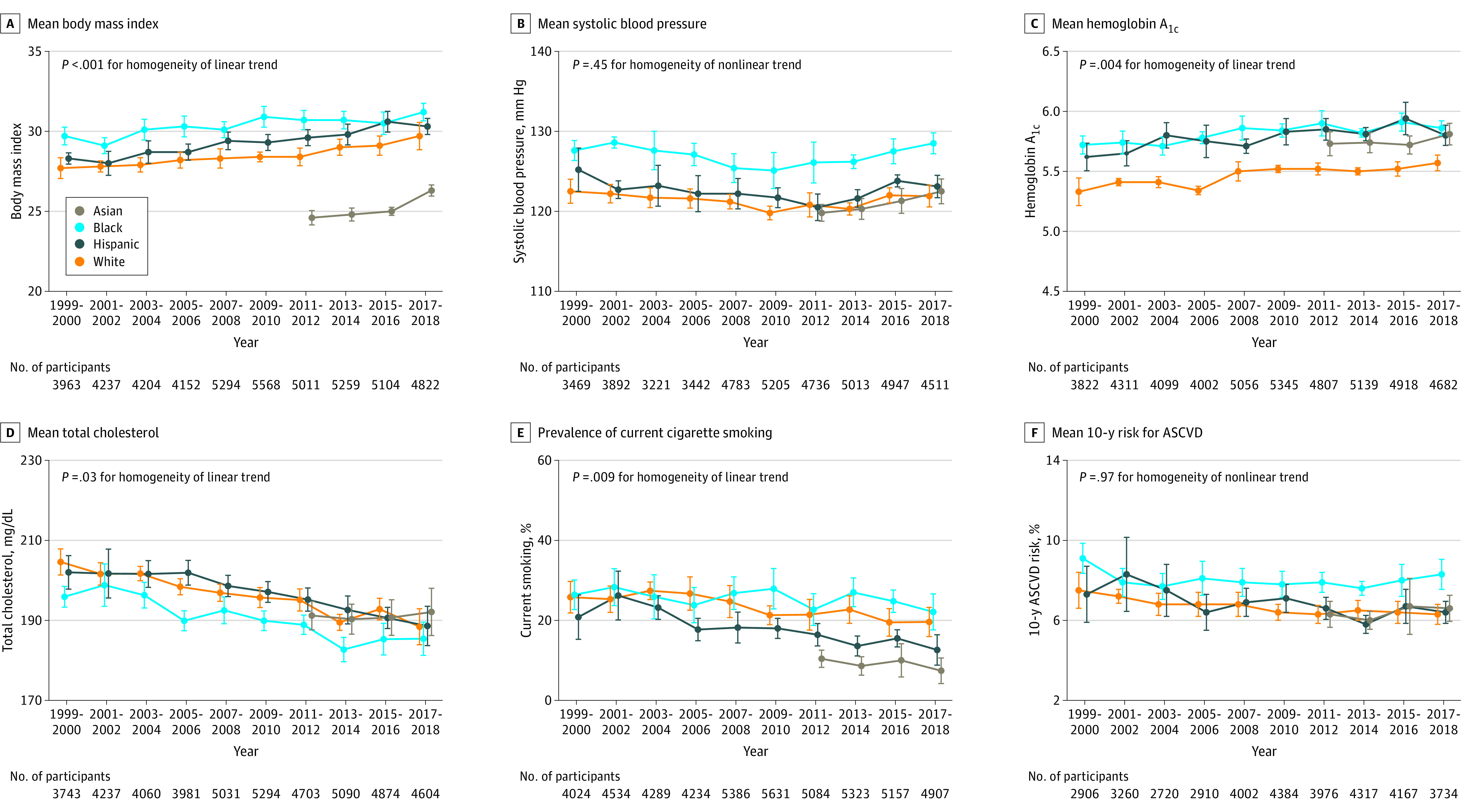
Trends in (A) mean body mass index (calculated as weight in kilograms divided by height in meters squared) (all P < .001 for linear trend); (B) mean systolic blood pressure (P = .001 for linear trend, P < .001 for nonlinear trend, P = .003 for nonlinear trend, and P = .002 for nonlinear trend in Asian, Black, Hispanic, and White individuals, respectively); (C) mean hemoglobin A1c (P = .26 for trend in Asian individuals; for all others, P < .001 for linear trend); (D) mean serum total cholesterol (to convert to millimoles per liter, multiply by 0.0259) (P = .76 for linear trend in Asian individuals; for all others, P < .001 for linear trend); (E) prevalence of current cigarette smoking (P > .05 for trend in Asian and Black individuals; P < .001 for linear trend in Hispanic and White individuals); and (F) mean estimated 10-year risk of atherosclerotic cardiovascular disease (ASCVD) (P = .26 for trend, P = .03 for nonlinear trend, P = .02 for linear trend, and P < .001 for linear trend in Asian, Black, Hispanic, and White individuals, respectively). The 10-year risk of ASCVD was calculated using the Pooled Cohort Equations among individuals without a self-reported history of cardiovascular disease. The probability of developing ASCVD over 10 years ranged from 0% to 100%. All estimates were standardized to the 2000 US Census population using 6 age and sex categories: men aged 20-39, 40-59, and ≥60 years and women aged 20-39, 40-59, and ≥60 years. Linear and polynomial models were used to test linear and nonlinear trends. The homogeneity of trends among racial and ethnic subgroups was tested using an interaction term of time × race and ethnicity in the regression models. Error bars indicate 95% CIs.
Racial and ethnic differences in the age- and sex-adjusted prevalences of obesity, hypertension, and diabetes were significant in all time periods from 1999 to 2018 (all P < .001 for group differences) (eTable 6 in the Supplement). For example, the age- and sex-adjusted prevalences of obesity, hypertension, and diabetes were consistently and significantly higher in Black participants compared with other racial and ethnic groups. The age- and sex-adjusted prevalence of high total cholesterol was not significantly different by racial and ethnic groups.
The age- and sex-adjusted estimated 10-year risk of atherosclerotic cardiovascular disease decreased from 7.5% (95% CI, 6.6%-8.4%) to 6.3% (95% CI, 5.8%-6.8%) in White individuals (P < .001 for linear trend) and from 7.3% (95% CI, 5.9%-8.7%) to 6.4% (95% CI, 5.8%-6.9%) in Hispanic individuals (P = .02 for linear trend) among participants without a self-reported history of cardiovascular disease from 1999-2000 to 2017-2018 (Figure 2; eTable 5 in the Supplement). The estimated 10-year risk decreased from 9.1% (95% CI, 8.3%-9.8%) in 1999-2000 to 7.6% (95% CI, 7.3%-8.0%) in 2013-2014 but increased to 8.3% (95% CI, 7.5%-9.0%) in 2017-2018 in Black participants (P = .03 for nonlinear trend). The estimated 10-year risk was consistently higher in Black participants in all time periods (all P < .05 for group difference).
Secular Trends by Education Levels
Secular trends in age- and sex-adjusted mean cardiovascular risk factors between 1999 and 2018 by education levels were similar with those in the overall population except that those with high school education had a greater reduction in mean total cholesterol (Figure 3; eTable 5 in the Supplement). Individuals with college or higher education had significantly lower age- and sex-adjusted mean body mass index, systolic blood pressure, hemoglobin A1c, and 10-year risk of atherosclerotic cardiovascular disease, as well as a lower prevalence of current smoking, in all time periods. Individuals with less than high school education had significantly higher mean hemoglobin A1c and 10-year risk of atherosclerotic cardiovascular disease during all time periods (all P < .001 for group difference). The prevalences of obesity, hypertension, and diabetes were significantly lower among individuals with college or higher education (eTable 6 in the Supplement).
Figure 3. Trends in Cardiovascular Risk Factors by Education Level in US Adults.
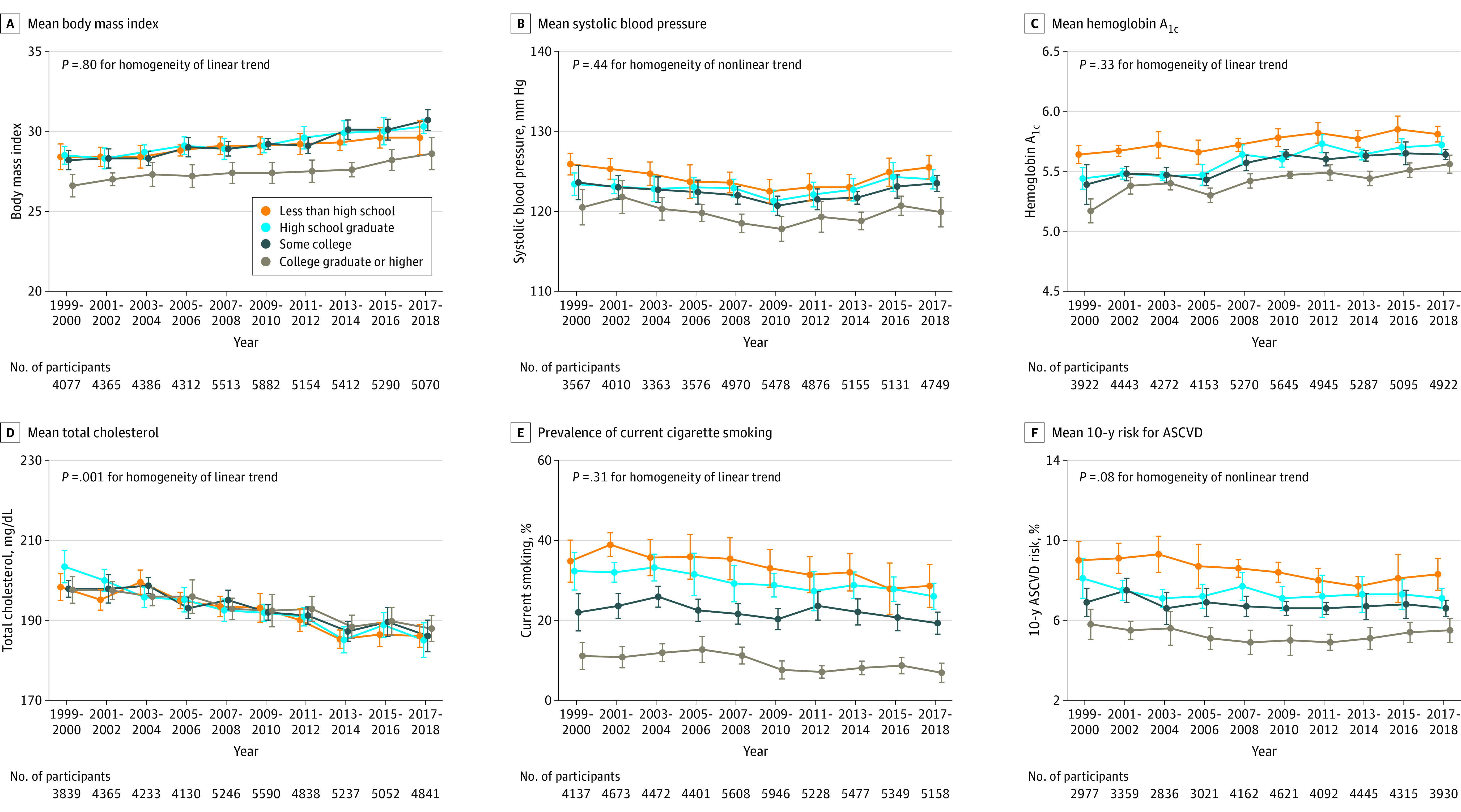
Trends in (A) mean body mass index (calculated as weight in kilograms divided by height in meters squared) (all P < .001 for linear trend); (B) mean systolic blood pressure (all P ≤ .02 for nonlinear trend); (C) mean hemoglobin A1c (all P < .001 for linear trend); (D) mean serum total cholesterol (to convert to millimoles per liter, multiply by 0.0259) (all P < .001 for linear trend); (E) prevalence of current cigarette smoking (P = .03 for linear trend in individuals with some college; P < .001 for linear trend in all others); and (F) mean estimated 10-year risk of atherosclerotic cardiovascular disease (ASCVD) (P = .004 for linear trend in individuals with less than high school; P > .05 for trend in high school graduates and those with some college; and P = .01 for nonlinear trend in college graduates or higher). The 10-year risk of ASCVD was calculated using the Pooled Cohort Equations among individuals without a self-reported history of cardiovascular disease. The probability of developing ASCVD over 10 years ranged from 0% to 100%. All estimates were standardized to the 2000 US Census population using 6 age and sex categories: men aged 20-39, 40-59, and ≥60 years and women aged 20-39, 40-59, and ≥60 years. Linear and polynomial models were used to test linear and nonlinear trends. The homogeneity of trends among education subgroups was tested using an interaction term of time × education in the regression models. Error bars indicate 95% CIs.
Secular Trends by Family Income
Secular trends in age- and sex-adjusted mean cardiovascular risk factors by family income were similar to those in the overall population, although significant variations existed for mean total cholesterol (P = .006 for homogeneity) and prevalence of cigarette smoking (P = .003 for homogeneity) (Figure 4; eTable 5 in the Supplement). Individuals with higher income (≥500% of family income-to-poverty ratios) had consistently lower body mass index, hemoglobin A1c, prevalence of current smoking, and 10-year risk of atherosclerotic cardiovascular disease. Individuals in poverty (family income-to-poverty ratio ≤100%) had significantly higher hemoglobin A1c, cigarette smoking, and 10-year risk of atherosclerotic cardiovascular disease.
Figure 4. Trends in Cardiovascular Risk Factors by Family Income-to-Poverty Ratio in US Adults.
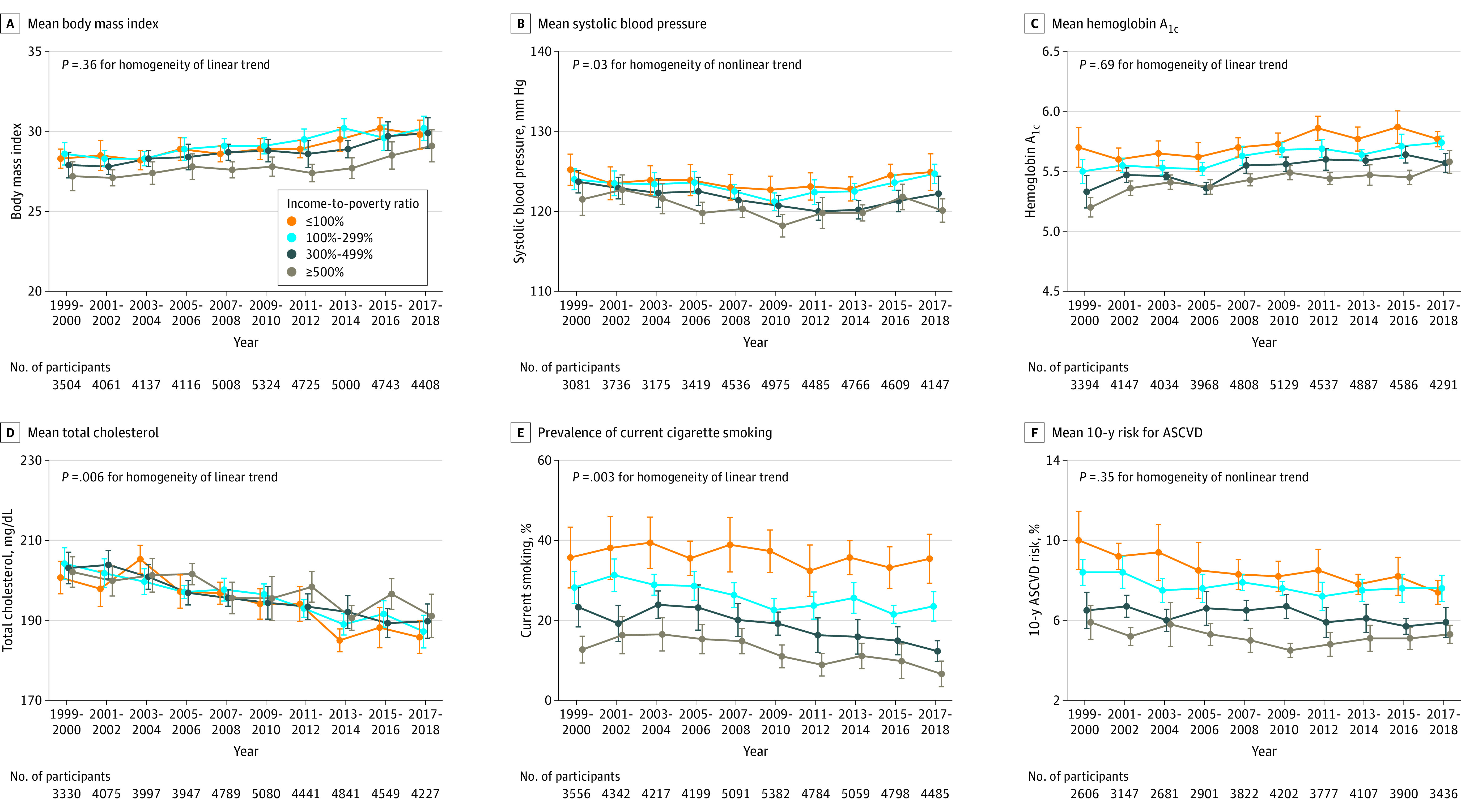
Trends in (A) mean body mass index (calculated as weight in kilograms divided by height in meters squared) (all P < .001 for linear trend); (B) mean systolic blood pressure (all P ≤ .03 for nonlinear trend); (C) mean hemoglobin A1c (all P < .001 for linear trend); (D) mean serum total cholesterol (to convert to millimoles per liter, multiply by 0.0259) (all P < .001 for linear trend); (E) prevalence of current cigarette smoking (P = .15 for linear trend in individuals with an income-to-poverty ratio ≤100%; P < .001 for linear trend for all others); and (F) mean estimated 10-year risk of atherosclerotic cardiovascular disease (ASCVD) (P < .001, P = .02, and P = .06 for linear trend in individuals with income-to-poverty ratios ≤100%, >100-299%, and 300-499%, respectively; P = .009 for nonlinear trend in individuals with an income-to-poverty ratio ≥500%). The 10-year risk of ASCVD was calculated using the Pooled Cohort Equations among individuals without a self-reported history of cardiovascular disease. The probability of developing ASCVD over 10 years ranged from 0% to 100%. All estimates were standardized to the 2000 US Census population using 6 age and sex categories: men aged 20-39, 40-59, and ≥60 years and women aged 20-39, 40-59, and ≥60 years. The poverty threshold for a 4-person family was $17 029 in 1999 ($25 743 in 2018 dollar value) and $25 701 in 2018. Linear and polynomial models were used to test linear and nonlinear trends. The homogeneity of trends among family income subgroups was tested using an interaction term of time × family income subgroup in the regression models. Error bars indicate 95% CIs.
Adjustment for Social Determinants of Health
After further adjusting for education, income, home ownership, employment, health insurance, and access to health care, the cardiovascular risk factors of mean body mass index, systolic blood pressure, and hemoglobin A1c remained significantly higher, but mean total cholesterol and prevalence of cigarette smoking remained lower, in Black participants compared with White participants in both periods, 1999-2008 and 2009-2018 (Table 2). Mean age- and sex-adjusted 10-year risk of atherosclerotic cardiovascular disease was higher in Black participants compared with White participants (difference, 1.4% [95% CI, 1.0%-1.7%] in 1999-2008 and 2.0% [95% CI, 1.7%-2.4%] in 2009-2018). This difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care (−0.3% [95% CI, –0.6% to 0.1%] in 1999-2008 and 0.7% [95% CI, 0.3%-1.0%] in 2009-2018). The prevalences of obesity, hypertension, and diabetes were higher while prevalence of hypercholesterolemia was lower in Black participants compared with White participants (eTable 7 in the Supplement). The prevalence of self-reported cardiovascular disease was higher in Black participants compared with White participants. However, this difference was no longer statistically significant after adjusting for education, income, home ownership, employment, health insurance, and access to health care.
Table 2. Differences in Cardiovascular Risk Factors by Race and Ethnicity, Adjusting for Social Determinants of Health, During 1999-2008 and 2009-2018a.
| Cardiovascular risk factors | NHANES 1999-2008 | NHANES 2009-2018 | ||||
|---|---|---|---|---|---|---|
| No. of participants | Age- and sex-adjusted difference | Age-, sex-, and SDOH-adjusted differenceb | No. of participants | Age- and sex-adjusted difference | Age-, sex-, and SDOH-adjusted differenceb | |
| Mean body mass indexc | ||||||
| Black − White | 4253/10 407 | 2.1 (1.8 to 2.4) | 2.0 (1.7 to 2.4) | 5124/9826 | 2.0 (1.7 to 2.4) | 1.8 (1.5 to 2.1) |
| Hispanic − White | 5280/10 407 | 0.7 (0.3 to 1.1) | 0.9 (0.5 to 1.2) | 5677/9826 | 1.2 (0.9 to 1.5) | 1.2 (0.8 to 1.5) |
| Mean systolic blood pressure, mm Hg | ||||||
| Black − White | 3516/9100 | 5.5 (4.7 to 6.4) | 4.6 (3.8 to 5.5) | 4831/9409 | 6.4 (5.6 to 7.2) | 5.3 (4.5 to 6.1) |
| Hispanic − White | 4585/9100 | 1.7 (0.7 to 2.7) | 0.2 (–0.8 to 1.2) | 5375/9409 | 1.7 (1.0 to 2.4) | 0.2 (–0.5 to 0.9) |
| Mean hemoglobin A1c, % | ||||||
| Black − White | 3991/10 295 | 0.4 (0.3 to 0.4) | 0.3 (0.3 to 0.4) | 4801/9663 | 0.4 (0.3 to 0.4) | 0.3 (0.3 to 0.4) |
| Hispanic − White | 5207/10 295 | 0.3 (0.2 to 0.3) | 0.2 (0.2 to 0.3) | 5535/9663 | 0.3 (0.3 to 0.4) | 0.3 (0.2 to 0.3) |
| Mean total cholesterol, mg/dL | ||||||
| Black − White | 3933/10 194 | –5.6 (–7.3 to –3.9) | –4.4 (–6.3 to –2.5) | 4694/9571 | –5.9 (–7.8 to –4.1) | –4.3 (–6.0 to –2.5) |
| Hispanic − White | 5167/10 194 | 0.1 (–1.7 to 1.9) | 0.4 (–1.5 to 2.3) | 5493/9571 | 0.5 (–1.8 to 2.8) | 1.3 (–1.1 to 3.6) |
| Prevalence of current cigarette smoking, % | ||||||
| Black − White | 4388/10 697 | –0.5 (–2.9 to 1.8) | –8.0 (–10.0 to –5.9) | 5183/9973 | 3.8 (1.7 to 6.0) | –4.0 (–5.9 to –2.1) |
| Hispanic − White | 5412/10 697 | –6.1 (–9.1 to –3.1) | –17.5 (–20.6 to –14.4) | 5740/9973 | –6.1 (–8.3 to –3.9) | –16.6 (–18.9 to –14.3) |
| Mean 10-y risk of atherosclerotic cardiovascular disease, %d | ||||||
| Black − White | 2855/7633 | 1.4 (1.0 to 1.7) | –0.3 (–0.6 to 0.1) | 3905/7828 | 2.0 (1.7 to 2.4) | 0.7 (0.3 to 1.0) |
| Hispanic − White | 4054/7633 | 0.8 (0.3 to 1.3) | –1.3 (–1.9 to –0.7) | 4752/7828 | 0.7 (0.3 to 1.0) | –0.7 (–1.1 to –0.4) |
Abbreviation: NHANES, National Health and Nutrition Examination Survey.
SI conversion factor: To convert total cholesterol to millimoles per liter, multiply by 0.0259.
Racial and ethnic differences in cardiovascular risk factors were defined as mean values in Black participants minus mean values in White participants or mean values in Hispanic participants minus mean values in White participants. NHANES participants with complete data for cardiovascular risk factors were included in the analysis. Absolute values on which this table is based can be found in eTable 5 in the Supplement. Additional data on obesity, hypertension, diabetes, high total cholesterol, and self-reported history of cardiovascular disease can be found in eTable 6 and eTable 7 in the Supplement.
Social determinants of health (SDOH) included education (less than high school, high school graduate, some college, or college graduate or higher), family income-to-poverty ratio, home ownership, employment (employed, student, retired, or unemployed), health insurance (private, government, or none), and regular access to health care facility.
Calculated as weight in kilograms divided by height in meters squared.
The 10-year risk of atherosclerotic cardiovascular disease was calculated using the Pooled Cohort Equations among individuals without a self-reported history of cardiovascular disease. The probability of developing atherosclerotic cardiovascular disease over 10 years ranged from 0% to 100%.
Compared with White participants, Hispanic participants had higher mean body mass index and hemoglobin A1c but lower prevalence of cigarette smoking (Table 2). Adjusted 10-year risk of atherosclerotic cardiovascular disease and prevalence of self-reported cardiovascular disease were significantly lower in Hispanic participants compared with White participants (Table 2; eTable 7 in the Supplement).
Discussion
In this serial cross-sectional survey study that estimated US trends in cardiovascular risk factors from 1999 through 2018, differences in cardiovascular risk factors persisted between Black participants and White participants; the difference may have been moderated by social determinants of health.
Several studies have examined the secular trends of individual cardiovascular risk factors using data from NHANES.4,5,6,9 A study by Ogden et al4 reported increases in obesity and severe obesity in both men and women in the US from 1999-2000 to 2017-2018. A study by Dorans et al9 reported that age-standardized prevalence of hypertension in the US decreased from 48.4% in 1999-2000 to 45.4% in 2015-2016. A study by Wang et al5 reported that the estimated age-standardized prevalence of diabetes among US adults increased significantly from 9.8% in 1999-2000 to 14.3% in 2017-2018 (P < .001 for trend). The current analysis comprehensively examined multiple major cardiovascular risk factors using the most recent national survey data available.
The trends in this analysis reflected both primary prevention (ie, lifestyle intervention) and secondary prevention (ie, pharmaceutical treatment) efforts. Muntner et al6 reported that the age-adjusted estimated proportion of US adults with controlled blood pressure among patients with hypertension increased from 31.8% in 1999-2000 to 48.5% in 2007-2008 (P < .001 for trend), did not significantly change from 2007-2008 through 2013-2014 (P = .14 for trend), and then declined to 43.7% in 2017-2018 (P = .003 for trend).6 Yang et al24 reported that in the US, the proportion of adults with diabetes that is controlled (hemoglobin A1c <7%) increased from 44.0% in 1999-2002 to 57.4% in 2007-2010 but then declined to 50.5% in 2015-2018. Therefore, declines in hypertension and diabetes control might have partially contributed to increases in mean blood pressure and hemoglobin A1c levels in the US population. In addition, changes in statin use may explain the discrepancy between secular trends of mean serum total cholesterol and the prevalence of hypercholesterolemia observed in this study.
Systolic blood pressure and diabetes are 2 major predictors in the Pooled Cohort Equations,16 and recent increases in these risk factors may contribute to the deceleration of cardiovascular disease risk decline. Several previous studies assessed the secular trends of overall cardiovascular disease risk using combinations of various cardiovascular disease risk factors.24,25 The current analysis additionally studied the estimated 10-year risk of atherosclerotic cardiovascular disease, which provides a quantitative risk measurement that is widely used in clinical practice and public health.16,26,27
Racial and ethnic differences in cardiovascular disease mortality and risk factors have been well documented.28,29,30 Although cardiovascular disease mortality and risk factors have decreased significantly since 1950, Black persons still have higher risk compared with individuals in other racial and ethnic groups.3,28,29,30 To our knowledge, this is the first study to report that body mass index, systolic blood pressure, and hemoglobin A1c were persistently higher in the Black population compared with the White population after adjustment for important social determinants of health, such as education, income, housing, employment, health insurance, and access to health care. Other unmeasured social determinants, such as neighborhood and physical environment, access to healthy foods, and social integration, were not included in this analysis but seem likely to play an important role in racial and ethnic differences.11,12,31
Socioeconomic factors, such as educational attainment and family income level, are important social determinants of cardiovascular disease.27,31 Low socioeconomic status, based on household income, education, and employment status, was associated with multivariable-adjusted hazard ratios of 2.3 for cardiovascular disease mortality and 1.7 for cardiovascular disease incidence in the UK Biobank cohort.32
Limitations
This study has several limitations. First, NHANES comprises a series of cross-sectional surveys, so longitudinal changes in cardiovascular risk factors at an individual level could not be evaluated. Second, fasting plasma glucose, serum LDL cholesterol, and triglycerides were available for only a subsample of participants. Third, the physical activity questionnaire and dietary intake assessment methods were changed between 1999 and 2018. Therefore, direct comparisons in physical activity and dietary intake among survey cycles were not feasible. Fourth, the Pooled Cohort Equations were not validated in Hispanic or Asian populations. In addition, Hispanic and Asian participants were aggregated into single categories although there were heterogeneities within these racial and ethnic groups. Fifth, due to small sample size, other races were not included in this analysis. Sixth, many important social determinants of health were not measured and could not be included in this analysis.
Conclusions
In this serial cross-sectional survey study that estimated US trends in cardiovascular risk factors from 1999 through 2018, differences in cardiovascular risk factors persisted between Black and White participants; the difference may have been moderated by social determinants of health.
eTable 1. Age-Sex-Adjusted and Age-Adjusted Means or Percentage (95% Confidence Intervals) of Cardiovascular Risk Factors in US Adults Aged ≥20 Years, NHANES 1999-2018
eTable 2. Sex-Adjusted Mean and Prevalence (95% Confidence Intervals) of Cardiovascular Risk Factors by Age Groups, NHANES 1999-2018
eTable 3. Age-Sex-Adjusted or Age-Adjusted Prevalences (95% Confidence Intervals) of Elevated Cardiovascular Risk Factors in US Adults Aged ≥20 Years, NHANES 1999-2018
eTable 4. Age-Sex-Adjusted and Age-Adjusted Prevalences (95% Confidence Intervals) of Self-Reported History of Cardiovascular Disease and Use of Medications in US Adults Aged ≥20 Years, NHANES 1999-2018
eTable 5. Age-Sex-Adjusted Mean (95% Confidence Intervals) Cardiovascular Risk Factors Overall and by Race and Socioeconomic Status, NHANES 1999-2018
eTable 6. Age-Sex-Adjusted Prevalences (95% Confidence Intervals) of Elevated Cardiovascular Risk Factors Overall and by Race and Socioeconomic Status, NHANES 1999-2018
eTable 7. Racial and Ethnic Differences in Proportion of Elevated Cardiovascular Risk Factors Adjusting for Social Determinants of Health During 1999-2008 and 2009-2018
References
- 1.Virani SS, Alonso A, Aparicio HJ, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254-e743. doi: 10.1161/CIR.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 2.Shah NS, Lloyd-Jones DM, O’Flaherty M, et al. Trends in cardiometabolic mortality in the United States, 1999-2017. JAMA. 2019;322(8):780-782. doi: 10.1001/jama.2019.9161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murphy SL, Xu J, Kochanek KD, Arias E, Tejada-Vera B. Deaths: final data for 2018. Natl Vital Stat Rep. 2021;69(13):1-83. [PubMed] [Google Scholar]
- 4.Ogden CL, Fryar CD, Martin CB, et al. Trends in obesity prevalence by race and Hispanic origin—1999-2000 to 2017-2018. JAMA. 2020;324(12):1208-1210. doi: 10.1001/jama.2020.14590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang L, Li X, Wang Z, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999-2018. JAMA. 2021. doi: 10.1001/jama.2021.9883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muntner P, Hardy ST, Fine LJ, et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324(12):1190-1200. doi: 10.1001/jama.2020.14545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mokdad AH, Ballestros K, Echko M, et al. ; US Burden of Disease Collaborators . The state of US health, 1990-2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444-1472. doi: 10.1001/jama.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015;314(10):1021-1029. doi: 10.1001/jama.2015.10029 [DOI] [PubMed] [Google Scholar]
- 9.Dorans KS, Mills KT, Liu Y, He J. Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guideline. J Am Heart Assoc. 2018;7(11):e008888. doi: 10.1161/JAHA.118.008888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bundy JD, Mills KT, Chen J, Li C, Greenland P, He J. Estimating the association of the 2017 and 2014 hypertension guidelines with cardiovascular events and deaths in US adults: an analysis of national data. JAMA Cardiol. 2018;3(7):572-581. doi: 10.1001/jamacardio.2018.1240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Havranek EP, Mujahid MS, Barr DA, et al. ; American Heart Association Council on Quality of Care and Outcomes Research, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, and Stroke Council . Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(9):873-898. doi: 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 12.Carnethon MR, Pu J, Howard G, et al. ; American Heart Association Council on Epidemiology and Prevention, Council on Cardiovascular Disease in the Young, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, Council on Functional Genomics and Translational Biology, and Stroke Council . Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21):e393-e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention . National Health and Nutrition Examination Survey. Accessed July 15, 2021. https://www.cdc.gov/nchs/nhanes/index.htm
- 14.Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National Health and Nutrition Examination Survey: plan and operations, 1999-2010. Vital Health Stat 1. 2013;(56):1-37. [PubMed] [Google Scholar]
- 15.Pickering TG, Hall JE, Appel LJ, et al. ; Council on High Blood Pressure Research Professional and Public Education Subcommittee, American Heart Association . Recommendations for blood pressure measurement in humans: an AHA scientific statement from the Council on High Blood Pressure Research Professional and Public Education Subcommittee. J Clin Hypertens (Greenwich). 2005;7(2):102-109. doi: 10.1111/j.1524-6175.2005.04377.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25)(suppl 2):S49-S73. doi: 10.1161/01.cir.0000437741.48606.98 [DOI] [PubMed] [Google Scholar]
- 17.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):2199-2269. doi: 10.1016/j.jacc.2017.11.005 [DOI] [PubMed] [Google Scholar]
- 18.American Diabetes Association . Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(suppl 1):S11-S61. doi: 10.2337/dc10-S011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Global BMI Mortality Collaboration . Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776-786. doi: 10.1016/S0140-6736(16)30175-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng W, McLerran DF, Rolland B, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364(8):719-729. doi: 10.1056/NEJMoa1010679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ingram DD, Malec DJ, Makuc DM, et al. National Center for Health Statistics guidelines for analysis of trends. Vital Health Stat 2. 2018;(179):1-71. [PubMed] [Google Scholar]
- 22.National Cancer Institute Surveillance Research Program . Joinpoint Trend Analysis Software. Version 4.8.0.1. Published April 22, 2020. Accessed February 2021. https://surveillance.cancer.gov/joinpoint/
- 23.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-351. doi: [DOI] [PubMed] [Google Scholar]
- 24.Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307(12):1273-1283. doi: 10.1001/jama.2012.339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim JK, Ailshire JA, Crimmins EM. Twenty-year trends in cardiovascular risk among men and women in the United States. Aging Clin Exp Res. 2019;31(1):135-143. doi: 10.1007/s40520-018-0932-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):3168-3209. doi: 10.1016/j.jacc.2018.11.002 [DOI] [PubMed] [Google Scholar]
- 27.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. doi: 10.1161/CIR.0000000000000678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mitchell UA, Ailshire JA, Kim JK, Crimmins EM. Black-White differences in 20-year trends in cardiovascular risk in the United States, 1990-2010. Ethn Dis. 2019;29(4):587-598. doi: 10.18865/ed.29.4.587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown AF, Liang LJ, Vassar SD, et al. Trends in racial/ethnic and nativity disparities in cardiovascular health among adults without prevalent cardiovascular disease in the United States, 1988 to 2014. Ann Intern Med. 2018;168(8):541-549. doi: 10.7326/M17-0996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tajeu GS, Safford MM, Howard G, et al. Black-White differences in cardiovascular disease mortality: a prospective US study, 2003-2017. Am J Public Health. 2020;110(5):696-703. doi: 10.2105/AJPH.2019.305543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018;137(20):2166-2178. doi: 10.1161/CIRCULATIONAHA.117.029652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang YB, Chen C, Pan XF, et al. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. 2021;373(n604):n604. doi: 10.1136/bmj.n604 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Age-Sex-Adjusted and Age-Adjusted Means or Percentage (95% Confidence Intervals) of Cardiovascular Risk Factors in US Adults Aged ≥20 Years, NHANES 1999-2018
eTable 2. Sex-Adjusted Mean and Prevalence (95% Confidence Intervals) of Cardiovascular Risk Factors by Age Groups, NHANES 1999-2018
eTable 3. Age-Sex-Adjusted or Age-Adjusted Prevalences (95% Confidence Intervals) of Elevated Cardiovascular Risk Factors in US Adults Aged ≥20 Years, NHANES 1999-2018
eTable 4. Age-Sex-Adjusted and Age-Adjusted Prevalences (95% Confidence Intervals) of Self-Reported History of Cardiovascular Disease and Use of Medications in US Adults Aged ≥20 Years, NHANES 1999-2018
eTable 5. Age-Sex-Adjusted Mean (95% Confidence Intervals) Cardiovascular Risk Factors Overall and by Race and Socioeconomic Status, NHANES 1999-2018
eTable 6. Age-Sex-Adjusted Prevalences (95% Confidence Intervals) of Elevated Cardiovascular Risk Factors Overall and by Race and Socioeconomic Status, NHANES 1999-2018
eTable 7. Racial and Ethnic Differences in Proportion of Elevated Cardiovascular Risk Factors Adjusting for Social Determinants of Health During 1999-2008 and 2009-2018


