Abstract
The effectiveness of Promoting First Relationships® (PFR), a 10-week home visiting program with video feedback, was tested in a randomized controlled trial involving 252 mothers and their 8- to 12-week-old infants. Mothers were eligible if they initiated treatment after mental health screening (depression, anxiety, post-traumatic stress disorder/PTSD) at a community or public health primary care center in pregnancy. At baseline, 51% had mild to severe depression symptoms, 54% had mild to severe anxiety, and 35% had PTSD. Their ages ranged from 18 to 42 years. Mothers were 66% White, 18% Black, and 16% other races. Forty-seven percent identified as Hispanic, and 33% preferred to read and speak in Spanish. The median family annual income was less than $20,000. The PFR program or receipt of a resource packet (control condition) followed the baseline assessment and randomization; we assessed outcomes when infants were age 6 and 12 months. Compared to mothers in the control condition, mothers in the PFR condition had significantly (ps < .05) higher observed sensitivity scores at both follow-up time points (d = .25, d = .26), improved understanding of infant-toddler social-emotional needs at both time points (d = .21, d = .45), and reported less infant externalizing behavior at age 12 months (d = .28). This study is the fourth completed RCT of the PFR program, all involving populations experiencing adversity.
Keywords: home visiting, antenatal distress, depression, anxiety, PTSD, parenting sensitivity
Pregnancy is a time of heightened risk for depression and anxiety (Biaggi et al., 2016), conditions that are frequently comorbid (Falah-Hassani et al., 2017; Kessler et al., 2003). Anxiety and depression in pregnancy predict postnatal depression and anxiety (Beck, 1996; Leigh & Milgrom, 2008), which are consistently associated with less sensitive caregiving (Binda et al., 2019; Ierardi et al., 2019; Parfitt et al., 2013; Stein et al., 2014; Warnock et al., 2016 ) and more impaired infant regulatory capacity, negative affectivity, and later child psychopathology (Glover, 2014; Goodman, 2020; Goodman & Halperin, 2020; Goodman et al., 2018; Hayes et al., 2013; O’Donnell et al., 2014, Rogers et al., 2020; Prenoveau et al., 2017; Stein et al., 2014). Maternal antenatal depression, anxiety, and stress influence infant neurodevelopment in ways that may make offspring especially susceptible to ongoing postnatal influences such as caregiving quality (O’Donnell & Meaney, 2017), reflecting the bidirectional or cyclic nature of maternal behavior and offspring well-being. Infants of mothers with former depression/anxiety may be challenging to care for because they exhibit higher levels of difficulty, including negative emotional expressiveness, few positive facial expressions, poor self-soothing, and sustained social withdrawal (Cohn, et al., 1986; Field, et al., 2009; Mantymaa, et al., 2008; Thomas et al., 2017; van der Wal, et al., 2007; Warnock et al., 2016). A recent meta-analysis reported that parenting quality is a mediator of associations between mothers’ depression and child outcomes (Goodman et al., 2020).
Antenatal depression is prevalent, affecting about 21% of pregnant women worldwide. Prevalence has increased in the past decade and is even more common in low- and lower-middle income countries (Yin et al., 2021). Poverty, young maternal age, lack of social support, low education (Goyal, et al., 2010; Wang, et al., 2011), lack of partner support, history of abuse or domestic violence, adverse life events, high perceived stress (Biaggi et al., 2016), unplanned pregnancy, experience with violence (Yin et al., 2021), and childhood emotional trauma (Ammerman et al., 2011) are all risk factors for depression and anxiety in pregnancy. Post-traumatic stress symptoms are frequently comorbid with perinatal depression and anxiety (Beck, 1996; Beck, et al., 2011; Geller & Stasko, 2017; Yildiz et al., 2017). Women who experienced trauma in childhood are particularly vulnerable to this comorbidity (Kaplan & Klinetob, 2000; Muzik et al., 2013; Widom, et al., 2007), which is difficult to treat (Grote & Frank, 2003; Kaplan & Klinetob, 2000), associated with more severe and enduring symptoms (Lippard & Nemeroff, 2020), and especially detrimental to parenting (Seng et al., 2013).
The American College of Obstetricians and Gynecologists recommends that medical providers conduct a depression and anxiety screening at least once during the perinatal period. Providers should offer medical therapy and/or refer patients to behavioral health resources when indicated (ACOG, 2018). However, OB/Gyn settings do not systematically provide interventions to promote mental health (Bayrampour et al., 2018; Bhat et al., 2017; Tourtelot et al., 2020). Psychosocial, psychological, and antidepressant medications effectively treat perinatal depression (Dennis & Dowswell, 2013; Stuart-Parrigon & Stuart, 2014; Yasuma et al., 2020). However, the type of treatment women with perinatal depression receive, particularly those with low income, varies greatly, and disparities exist in access to care (Geier et al., 2015; Kozhimannil et al., 2011). In a review of interventions in outpatient perinatal care settings (Byatt et al., 2015), 70.5% of included studies reported that their approach to positive perinatal depression screens was referral out to mental health services. However, referral alone is usually insufficient for pregnant and postpartum women to receive mental health services. Smith et al. (2009) prospectively studied a cohort of pregnant and postpartum women screened for psychiatric distress in a publicly funded clinic and referred for mental health treatment. Only 38.1% of referred women had at least one mental health appointment, and only 6% received sustained treatment. However, if mental health and obstetric care were co-located onsite, the odds of receiving treatment were four times higher.
The current study sought to leverage co-located obstetric and mental health services to support parenting in new mothers with low income. Publicly funded healthcare for pregnant and postpartum women in the greater Seattle, Washington area, where we conducted the study, is primarily offered through community health centers and the public health system. Pregnant women who are positive on mental health screening may receive pharmacotherapy through their health care provider, referral to mental health providers, case management and support through Maternity Support Services (MSS), and/or collaborative care through the Mental Health Integration Program (MHIP). MSS providers are public health social workers, nurses, and nutritionists who offer health education and counseling to promote healthy pregnancies and positive birth and parenting outcomes. MHIP uses a collaborative care approach for mental health within the health care clinics. The co-located care team includes the primary care provider, mental health coordinator, and caseload manager. Psychiatric case review and consultation are also available.
Treating Maternal Mood or Parenting Alone does not Prevent Adverse Infant Outcomes
The necessity of parenting support as an adjuvant to treatment for perinatal depression and anxiety is based on findings that show mothers continue to exhibit a reduced capacity to acknowledge and sensitively respond to child cues even after depression improves (Forman et al., 2007; Seifer, et al., 2001); treating mothers’ mood alone is not sufficient to override the mechanisms of parenting risk involving early emotional trauma (Lyons-Ruth, et al., 2002; Seng et al., 2013). However, interventions designed to improve mothers’ antenatal mood do show small, significant positive effects on offspring functioning, with stronger effects for younger children (Goodman et al., 2018). These results suggest that treating mood in pregnancy may interrupt some of the in-utero transmission that contributes to the impact of mothers’ negative mood on offspring. For women dealing with current adversities and past trauma, treatment of negative mood in pregnancy followed by the provision of parenting support after birth might further promote positive development in their offspring by improving maternal sensitivity and the mother-infant relationship. However, as babies do not (yet) exhibit problem behavior, many clinicians who work with adults do not see the need to refer new mothers with depression, anxiety, and PTSD to a home visiting or group-based mother-baby program (van Doesum, et al., 2008).
Innovative Strategies to Address Both Perinatal Mental Health and Parenting
Researchers have concluded, and policymakers agree, that healthy development in offspring of new mothers with depression and anxiety requires both mental health treatment and parenting support (Forman et al., 2007; Goodman & Garber, 2017; National Research Council and Institute of Medicine, 2009; O’Connor et al., 2019; van Doesum, et al., 2008). Although technology has allowed for a variety of non-contact approaches for parent training (Feil et al., 2008), our focus is on home visiting, a common source of public health funding for families in the perinatal period and first years of life (HomVEE, 2020).
Few home visiting models address both perinatal mental health and parenting beyond referring out for mental health treatment. Still, barriers often result in women receiving little or no mental health care (Smith et al., 2009). More women might be helped by incorporating an evidence-based mental health treatment into existing home visiting approaches. For example, Ammerman et al. (2010) conducted a randomized controlled trial of participants experiencing depression of a home visiting model (Nurse Family Partnership or Healthy Families America) and randomized to also receive cognitive behavior therapy (CBT) in a 16 session In-Home CBT module, delivered by a master’s level social worker. The home visiting component was provided as usual by a nurse or paraprofessional, depending on the model. In-Home CBT did not result in changes to parenting stress, nurturing parenting, or child adjustment (Ammerman et al., 2015), but did show improvement in depressive symptoms and functioning (Ammerman et al., 2013).
In another example, Beeber et al. (2013) conducted an RCT among mothers with low income enrolled in Early Head Start (EHS) who screened for clinical levels of depressive symptoms. The intervention group received 10 weekly modules of Interpersonal Psychotherapy (IPT) plus individualized parenting enhancement modules that helped mothers apply IPT strategies to override depressive symptoms that interfered with sensitive parenting, delivered by advanced psychiatric nurse practitioners. The comparison group received 10 weekly modules of attention control provided by a registered nurse. Both groups continued to receive EHS programming. One month after the intervention, both groups showed reductions in depression, with no mean treatment group differences. Only the IPT group, however, showed improvements in parenting rated from videotaped observations. The converse of the models above, which added a mental health component to a home visiting model, is to augment antenatal mental health treatment with a home visiting program. The current RCT leveraged existing infrastructure in mental health treatment to support a specific population of mothers at risk for negative parenting outcomes.
Home visiting programs are diverse. A broad array of program elements is possible. Gubbels et al. (2021) conducted a meta-analysis on 35 individual home visiting components’ effectiveness to prevent child maltreatment. Programs using video feedback, in which the provider filmed a short parent-child interaction and then watched it with the parent to promote understanding of the child’s cues and needs, versus those programs that did not, yielded larger effect sizes d = .39 vs. d =.12. However, video feedback was uncommon in these home visiting programs. Of the 65 study samples (N = 48,761) in the meta-analysis, only five used video feedback. O’Hara et al., 2019, conducted a meta-analysis of 20 home visiting RCTs or quasi-RCTs that compared video-feedback versus no treatment, an inactive treatment, or treatment as usual, on parenting sensitivity (1757 dyads). Video-feedback had a moderate effect on parental sensitivity, with a standardized mean difference of .35. These results are congruent with earlier meta-analyses. Bakermans-Kranenburg et al. (2003) found that interventions with video feedback were more effective in promoting sensitivity than interventions without the method, Cohen’s d = .44 vs. d = .31. Fukkink (2008) found similar positive results on parenting sensitivity, Hedge’s g = .47. Both meta-analyses also found that programs that were shorter in duration (< 3 months) or had fewer sessions (< 16) overall were more effective in improving parenting sensitivity than more intensive programs.
The effectiveness of video feedback in brief home visiting programs underlies the current study’s design, which examined the additive benefit of Promoting First Relationships® (PFR; Kelly et al., 2008) for postpartum women who began mental health treatment in the clinic where they received prenatal care. PFR is a brief home visiting model that uses video feedback, a relatively underutilized home visiting program component (Gubbels et al., 2021).
Promoting First Relationships® Home Visiting Intervention
Promoting First Relationships (PFR) Home Visiting is a brief 10- week model previously tested in two RCTs in child welfare. PFR was evaluated with 1-to-2-year-old children in foster care (Spieker et al., 2012) and families under investigation for maltreatment by Child Protective Services (Oxford, Spieker, et al., 2016). In both trials, PFR increased caregiver sensitivity and understanding of infant and toddler socioemotional development and meaning of child distress, reduced child problem behavior, and improved caregiver-child relationships. It also increased parenting quality in a subsample of reunified birth families (Oxford, Marcenko et al., 2016). PFR was related to the normalization of stress response systems (e.g., stimulated cortisol, vagal regulation) (Hastings et al., 2019; Nelson & Spieker, 2013) as well as to parent-reported reductions in child sleep problems, partially mediated by reductions in observed child separation distress (Oxford et al., 2013) or by buffering the effects of adversity (Hash et al., 2019). In both RCTs, the PFR group had real-world improvements in child welfare outcomes—including fewer foster care placement changes (Spieker et al., 2014) and fewer foster care placements (6% vs. 13%) (Oxford, Spieker et al., 2016). A benefit-cost analysis of this reduction found that PFR had a benefit from $1 to $32,072 per dollar spent on the intervention, depending on assumptions about the extent of benefit to the child and society of preventing an out-of-home placement (Kuklinski et al., 2020).
PFR has been culturally adapted and tested in a small sample (N = 34) within an American Indian community (Booth-LaForce et al., 2020). PFR significantly improved caregivers’ sensitivity and responsiveness, and caregivers’ reports of their knowledge of child development. Child outcomes, while strong, were not statistically significant (reduction of externalizing behavior, Cohen’s d = 1.18; internalizing behavior Cohen’s d = .29; and improvement in child competence Cohen’s d = .29).
The present study is the first to deliver PFR in a language other than English, provide PFR to a sample of women with low income who received an antenatal mental health referral, and initiate PFR with mothers of 2-to-3-month-old infants.
Purpose of the Present Study
The present study uniquely addressed the needs of women with perinatal mood distress and its pervasive effects on child development, recognizing that only treating negative mood or only focusing on parenting will be ineffective in improving child outcomes. The literature points to combining mental health and parenting interventions to meet both the caregiver and child’s needs (Goodman & Garber, 2017). This randomized controlled trial leveraged existing county-wide public health initiatives providing mental health treatment to pregnant women with low income at the community health centers where they received prenatal care. The purpose was to test Promoting First Relationships® (PFR), implemented between infant age 3 and 6 months, as an adjuvant to mental health services begun during pregnancy for a sample of Spanish- and English-speaking mothers with low income. The primary aim was to improve parenting sensitivity, maternal confidence, and knowledge of infant and toddler development relative to the control group that only received a resource packet and usual care. Both groups received MHIP or MSS mental health services during pregnancy. The secondary aim was to decrease observed infant difficult behaviors at 6 and 12 months and mothers’ reports of externalizing and internalizing behaviors and dysregulation at 12 months, relative to the control group.
Method
Participants
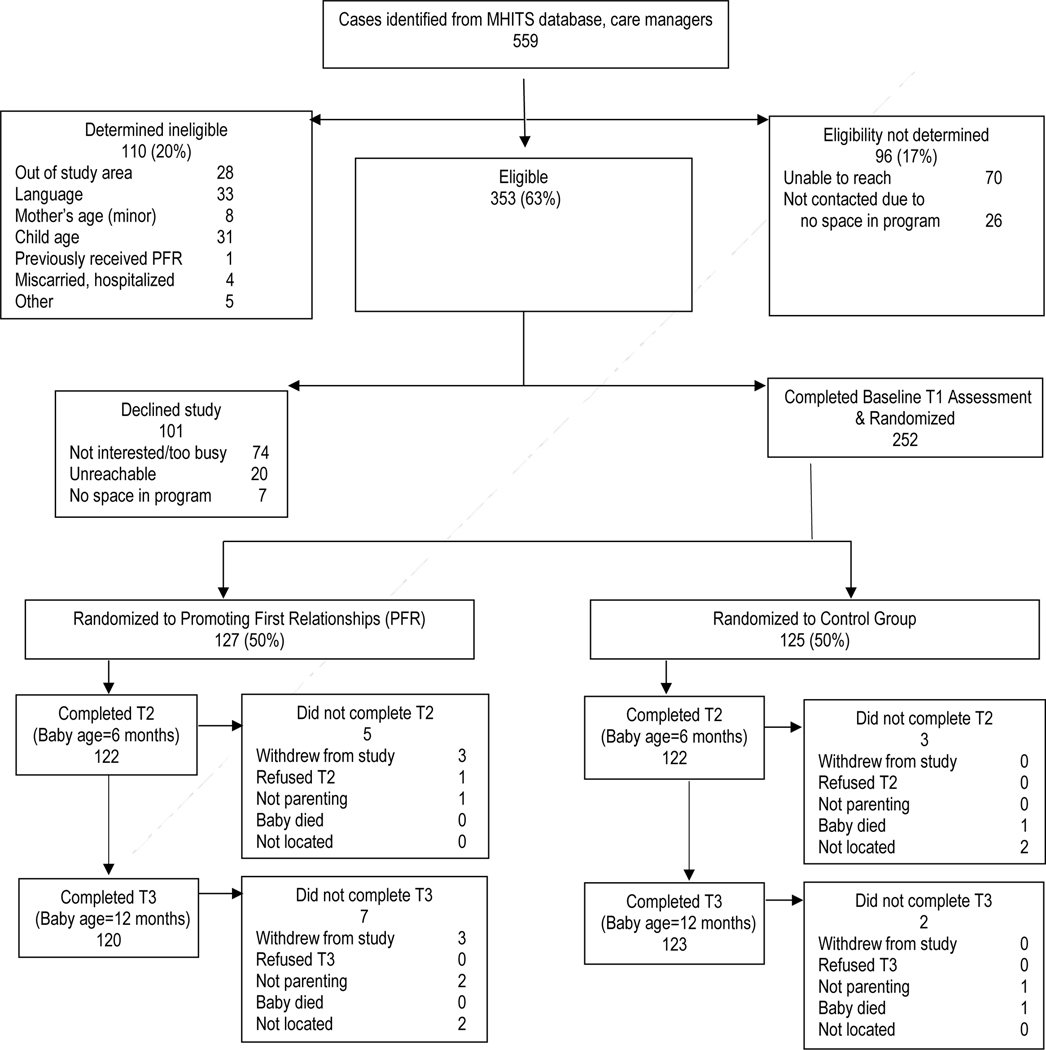
The Moms and Babies Program/Programa para Mamás y Bebés (MBP) research procedures were reviewed and approved by the University of Washington Institutional Review Board (study ID 00010114). Between November 2015 and June 2019, 252 mothers with their infants living in King County, Washington were enrolled in the study. The flow of participant recruitment, assignment, and completion of assessments is shown in Figure 1. Information on demographic and other baseline characteristics, including mental health concerns (PHQ-9 depression and GAD-7 anxiety, Spitzer et al., 1999; PCL-C-SF post-traumatic stress disorder, Lang & Stein, 2005) is shown by condition in Table 1.
Figure 1.
Moms and Babies Program/Programa para Mamás y Bebés Study Flowchart
Table 1.
Baseline Demographics by Treatment Assignment
| PFR n = 127 | Control n = 125 | |
|---|---|---|
|
|
||
| n (%) | n (%) | |
|
| ||
| Child gender | ||
| Female | 56 (44.1) | 64 (51.2) |
| Male | 71 (55.9) | 61 (48.8) |
| Child race | ||
| African American | 20 (15.7) | 17 (13.6) |
| Caucasian | 79 (62.2) | 68 (54.4) |
| Multiracial | 25 (19.7) | 33 (26.4) |
| Other | 3 (2.4) | 7 (5.6) |
| Child ethnicity, Hispanic | 68 (53.5) | 66 (52.8) |
| Preferred language | ||
| English | 87 (68.5) | 82 (65.6) |
| Spanish | 40 (31.5) | 43 (34.4) |
| Mother race | ||
| African American | 21 (16.5) | 23 (18.4) |
| Caucasian | 84 (66.1) | 81 (64.8) |
| Multiracial | 16 (12.6) | 10 (8.0) |
| Other | 6 (4.8) | 11 (8.8) |
| Mother ethnicity, Hispanic | 62 (48.8) | 57 (45.6) |
| Mother education | ||
| High school graduate | 85 (66.9) | 75 (60.0) |
| GED | 15 (11.8) | 15 (12.0) |
| Neither high school graduate nor GED | 27 (21.3) | 35 (28.0) |
| Marital status | ||
| Never married | 65 (51.2) | 71 (56.8) |
| Married | 46 (36.2) | 41 (32.8) |
| Divorced, separated, widowed | 16 (12.6) | 13 (10.4) |
| Living with a spouse/partner | 86 (67.7) | 88 (70.4) |
| Household income | ||
| $ 10,000 or less | 31 (24.4) | 42 (33.6) |
| $ 10,001 to $ 20,000 | 27 (21.3) | 26 (20.8) |
| $ 20,001 to $ 30,000 | 30 (23.6) | 18 (14.4) |
| $ 30,001 to $ 40,000 | 18 (14.2) | 15 (12.0) |
| $ 40,001 or more | 13 (10.2) | 14 (11.2) |
| No response | 8 (6.3) | 10 (8.0) |
| Number of children | ||
| 1 | 50 (39.4) | 60 (48.0) |
| 2 | 43 (33.9) | 33 (26.4) |
| 3 | 22 (17.3) | 19 (15.2) |
| 4 or more | 12 (9.4) | 13 (10.4) |
| Receive WIC program | 117 (92.1) | 116 (92.8) |
| PHQ-9 Depression | ||
| No depression (score of 0–4) | 64 (50.4) | 60 (48.0) |
| Mild depression (score of 5–9) | 38 (29.9) | 41 (32.8) |
| Moderate depression (score of 10–14) | 16 (12.6) | 16 (12.8) |
| Moderately severe depression (score 15–19) | 8 ( 6.3) | 7 ( 5.6) |
| Severe depression (score 20–27) | 1 ( 0.8) | 1 ( 0.8) |
| GAD-7 anxiety | ||
| No anxiety (score 0–4) | 60 (47.2) | 57 (45.6) |
| Mild anxiety (score 5–9) | 39 (30.7) | 32 (25.6) |
| Moderate anxiety (score 10–14) | 16 (12.6) | 22 (17.6) |
| Severe anxiety (score 15–21) | 12 ( 9.4) | 14 (11.2) |
| PCL-C-SF post-traumatic stress disorder | ||
| No PTSD (score 6–13) | 85 (66.9) | 80 (64.0) |
| Yes PTSD (score 14–30) | 42 (33.1) | 45 (36.0) |
| M (SD) | M (SD) | |
|
|
||
| Child age in months | 1.8 (0.5) | 1.9 (0.5) |
| Mother age in years | 28.8 (5.8) | 27.4 (5.6) |
Note. PFR = Promoting First Relationships; WIC = Women, Infants, and Children nutrition program for low income families; Household income had 18 missing cases (n = 8 for PFR group, n = 10 for control group)
Eligibility and recruitment.
Participants were eligible if they had received mental health treatment during pregnancy at one of the participating health centers, were conversant in English or Spanish, had an infant under three months of age, had access to a telephone, were planning to remain in the study area until the child’s first birthday, and had not already received PFR. All aspects of the study, including the intervention and research visits, were offered in English and Spanish.
Study recruitment was conducted in collaboration with the Mental Health Integration Program (MHIP) and Maternity Support Services (MSS) of Public Health Seattle and King County, Washington. MHIP is based on a public health approach that uses a collaborative care model to treat behavioral health problems like depression, anxiety, and trauma symptoms through primary care clinics in low-resourced settings (Huang et al., 2012; Unützer & Park, 2012). Public Health in Seattle/King County (PHSKC) targets pregnant and parenting women for collaborative care through the MHIP Moms program. Five community health clinics offering MHIP agreed to assist in study recruitment. In addition to MHIP Moms, PHSKC offers MSS, provided by public health social workers, nurses, and nutritionists who deliver case management plus referral to community mental health services from pregnancy through two months postpartum. Mothers were recruited for the study through both mechanisms.
Usual care services for parenting support and mental health being received at the time of enrollment and throughout participation in the study consisted primarily of home visiting, mental health counseling, and medication for mental health needs (see supplemental materials Table S1).
Eligible mothers were identified via the Mental Health Integrated Tracking System (MHITS), the database for MHIP managed by PHSKC, or the PHSKC MSS database. Each MHIP community health center ‘owned’ the list of its patients and agreed for the county public health department to generate a monthly list of potentially eligible pregnant women receiving mental health services. The monthly list contained their patients who were pregnant or had an infant less than three months of age. MHIP care managers and MSS social workers talked with women on the list by phone or at a clinic visit, briefly outlining the study. If the mother was interested in learning more about the study, the care manager or social worker connected her to the study recruitment coordinator either immediately or through a follow-up phone call. The study recruitment coordinator conducted additional screening and answered any questions the mother had. If the mother was eligible and interested, the study research visitor scheduled and completed the first research visit when the baby was between 6 and 12 weeks old. Written informed consent was obtained in the mothers’ homes at the first research visit.
The project director initiated the randomization after the first research visit. Mother-infant dyads were stratified into two groups based on mother’s preferred language, and then dyads were randomized within strata into the PFR intervention or control condition. Randomization was computer-generated, using an algorithm based on the minimization method described by Pocock (1983). The algorithm conditioned probability for assignment on prior allocations to generate roughly balanced numbers in the intervention and control condition while avoiding entirely predetermined assignments anticipated by research staff. Sample attrition was very low. Staff conducted follow-up research visits when infants were 6 and 12 months old. At both follow-up time points, over 94% of families in both conditions completed the assessments. Overall, 95.2% completed all three research visits, 2.0% completed only the first visit, 1.6% completed the first and second visits, and 1.2% completed the first and third visits. Comparing the 240 cases with complete data with the 12 cases that missed one or both follow-up time points, attrition did not differ significantly by condition, nor did tests of condition-by-baseline characteristics reveal any evidence of differential attrition by condition with respect to language, race/ethnicity, age of mother, baseline mental health measures, or any of the primary outcome measures. Mothers with incomplete data were more likely to be separated, divorced or widowed, had lower incomes, and had more children at baseline.
Promoting First Relationship® (PFR) Intervention
The manualized PFR intervention was delivered by seven female master’s-prepared mental health professionals. Six were employees of a community agency, and one was employed by the University of Washington. Four primary providers, who were all employed by the community agency, worked with 93% of the study families, and three fill-in providers administered the intervention to the remaining 7%. Three providers were fluent in Spanish, and all were fluent in English. The providers completed PFR training and were certified before meeting with study families. Throughout the study, fidelity was monitored by a PFR master trainer. The providers were required to submit videotapes of themselves working with the families during the sixth session for each family on their caseload, which the master trainer reviewed to rate the quality of delivery. If a provider did not meet fidelity (i.e., received a rating of less than 4 on a 5-point scale), she received additional one-on-one mentoring from the master trainer until her fidelity to PFR was reestablished. Providers were not assigned additional families to work with until they reestablished fidelity. Of 98 fidelity videotapes that were coded, 6% did not meet fidelity. Fidelity videotapes were not received for 29 families, either because they did not have six sessions of PFR (n = 16) or because the baby was asleep or there were technical issues or other circumstances preventing videotaping (n = 13). The PFR training model includes weekly reflective practice group sessions, facilitated by a PFR consultant, to support providers in their work with vulnerable families.
The majority of the 127 mothers randomized to PFR received a full dose of the intervention: 82% received 9–10 weekly sessions, 9% had 5–8 sessions, 8% had 1–4 sessions, and 2% did not start the intervention. The sessions typically ranged from 60 to 75 minutes and took place in the families’ homes. The providers delivered activities and instructional content as prescribed in the PFR manual; however, the pace of delivery of these components was tailored to individual mothers, and some sessions were adapted for very young infants. A key component of PFR is videotaped caregiver-child interaction, completed during five sessions and serving as the focus of reflective video feedback during alternating weeks. The tapes were viewed together by the mother and intervention provider, who guided discussion focusing on parenting strengths and interpretation of her baby’s cues.
Control Condition
The 125 mothers randomized to the control condition were mailed a resource packet containing a listing of a variety of local resources, child development handouts, and parenting handouts. Packets were provided in the mother’s desired language. The materials did not overlap with the content of PFR. To help minimize attrition, mothers in the control condition also received two check-in phone calls before the second research visit to see if their contact information had changed and to answer any questions about the study.
Measures and Procedures
Infants and their mothers were assessed at home in three 90-minute research visits: at baseline (infant age 6–12 weeks), and when the babies were 6 months and 12 months old. The intervention was completed between the baseline and 6-month research visits. Assessments were conducted by three bilingual study research visitors who had bachelor’s or master’s degrees, who were blinded to intervention assignment, and whose offices were not near the intervention staff. One primary research visitor completed 96% of the research visits. The time from baseline to the 6-month research visit averaged 4.4 months, and the time from the 6-month to 12-month research visit averaged 6.0 months. Time between visits did not differ by intervention group. The research visits included standardized interview questions and videotaped mother-infant activities. The consent form and all study measures were read to the participants to ensure understanding and minimize missing data. All measures have been used with mothers from different cultural backgrounds, including Latina mothers, in other studies. Research visits were conducted by telephone if the family moved outside of the study area after the first research visit (15 research visits), and also for the final five families completing the 12-month research visit due to stay-at-home requirements caused by the COVID-19 pandemic in 2020. Research visits were conducted in-person and in-home for 98% of the assessments. Study participants received $50 in cash or gift card after each research visit to compensate for their time.
The study’s protocol is registered at ClinicalTrials.gov Protocol Registration and Results System (NCT02724774).
Primary Caregiver Outcomes
Parenting sensitivity was an observational measure collected at each research visit using the Nursing Child Assessment Teaching Scale (NCATS; Barnard, 1994). Mothers were presented with a list of activities and instructed to select the first activity that their infant could not yet do (e.g., hold onto a rattle, transfer an object from one hand to another, play pat-a-cake), to attempt to teach their infant. A standard set of manipulatives were provided for the activities. Teaching interactions were videotaped. A single bilingual and bicultural coder, blind to intervention condition, was trained to reliability by a certified NCATS instructor and passed biannual reliability checks with a minimum of 85% inter-rater agreement with a master trainer. Videotaped interactions were scored on 50 caregiver items measuring sensitivity to cues, response to distress, and fostering of social, emotional, cognitive growth, and continency between mother and infant. The NCATS manual reports, in a sample of 2,100 mothers, the average mean for parenting sensitivity was 41.73 (standard deviation of 6.45), Cronbach’s α =.87 (Barnard, 1994). Items were scored yes (1) or no (0) and summed for a total sensitivity score. Sensitivity scores can range from 0 to 50, with higher scores indicating greater sensitivity. Cronbach’s α in the study sample ranged from .66 to .72 across the three time points.
The Infant CARE-Index (ICI, Crittenden,1979–2010) assesses parent-infant interaction during play, and was included at each research visit. The ICI yields scores for a parent-infant scale (dyadic synchrony), three parent scales (, sensitivity, control, unresponsiveness) and four infant scales (cooperation, compulsivity, difficultness, passivity). The mother was asked to play with her child as she usually would, and the interaction was filmed for 3–5 minutes. If mothers wanted to use toys, they were offered toys that they could use, or they could choose their own toys. The videos were scored by 16 coders from 12 different countries who spoke English as well as other languages, and had been previously certified to code the ICI for research purposes. To be certified for research, coders rated videos from a collection of videos gathered in multiple countries and that represented the full range of potential scores on the ICI constructs. Coders had to meet a standard for inter-rater reliability of r = .80 on the measure of dyadic synchrony and an average of r = .70 across all scales. The coders’ work was overseen by the author of the coding scheme (Crittenden). To address the study’s primary hypotheses regarding caregiver outcomes, the rating for dyadic synchrony in play was used in the current study. Dyadic synchrony is any mutual pattern of behavior that enables the infant to explore the activity with interest and spontaneity and without inhibiting or exaggerating negative affect. Dyadic synchrony scores of 11–14 are sensitive, with mutual delight or a smooth, pleasing interaction. Scores between 7 and 10 are adequate, with satisfactory play but noticeable periods of desynchrony. Scores between 5 and 6 reflect clear, unresolved problems and limited playfulness, but no evidence of hostility or unresponsiveness. Scores between 0 and 4 reflect high risk, with a clear lack of empathy, insufficient or unsuccessful attempt to respond to the infant, or total failure to perceive or attempt to soothe the infant, and no play. As a further check of reliability, over the course of coding approximately 20% of the videos were randomly selected to be coded by a reliability coder. Inter-rater correlations for dyadic synchrony between pairs of coders averaged r = .67.
Understanding of infant and toddler behavior was measured by the Raising a Baby Scale (RAB; Kelly, Korfmacher, & Buehlman, 2008). The RAB is a measure of caregiver knowledge of infant and toddler social-emotional needs and developmentally appropriate expectations. Evidence of construct validity has been demonstrated in other studies of PFR, and has shown treatment effects among parents with an open child protective services investigation of child maltreatment (Oxford, Spieker et al., 2016), and with caregivers of toddlers who had recently had a court ordered placement change (Spieker et al., 2012). At each research visit, mothers rated the 16 RAB items on a 4-point scale (strongly agree to strongly disagree). Cronbach’s αs ranged from .68 to .71 across the three time points. The scale was summed, and scores could range from 16 to 64 with higher scores indicating greater parental knowledge.
Maternal confidence, the perceptions mothers have of their ability to care for and understand their infants, was measured at each research visit using the Maternal Confidence Questionnaire (MCQ; Zahr, 1991). Mothers rated 14 items on a 5-point scale (never to always; Cronbach’s αs ranged from .66 to .76 across the three time points). Maternal confidence is reflected by the mean of the scale, with higher scores indicating greater confidence. A review of research with the MCQ supports the reliability and validity of the scale (Badr, 2005). The MCQ has been used in over 20 studies and translated into nine languages, including Spanish. It has shown acceptable internal consistency and reliability; and convergent, predictive, and discriminant validity (Badr, 2005; Crncec et al., 2010). In a dyadic intervention with depressed mothers, only improvements in maternal confidence were associated with improvements in observed mother-infant interaction (Paris et al., 2011). For those samples with many risk factors, higher confidence/self-efficacy is associated with observed parenting competence (Jones & Prinz, 2005).
Secondary Infant Outcomes
The Infant CARE-Index (ICI, described above) also yields scores for the infant’s contribution to the interaction. We included infant difficultness in our analysis. Scores could range from 0 to 14. Higher scores reflect more infant difficult behaviors, such as crying and fussing, turning away, negative facial expressions, avoidance of eye contact, high arousal, and lack of engagement in a developmentally satisfying shared activity. Inter-rater correlations for difficultness on the 20% of videos selected for coding by an additional coder averaged r = .49.
At the final research visit, when infants were 12 months old, infant externalizing behavior, internalizing behavior, and dysregulation were measured with mother’s report on the Infant Toddler Social Emotional Assessment (ITSEA; Carter & Briggs-Gowan, 2006). The ITSEA was not included at the baseline or 6-month research visits because it is not valid for children younger than 12 months. Research has supported the reliability and validity of the measure, and high correlations with other measures of child behavior problems have been reported (Carter & Biggs-Gowan, 2006). The ITSEA has been standardized and normed on a nationally representative sample that was stratified to match the 2002 United States Census. Mothers rated their infant on an extensive list of behaviors from 0 (not true/rarely) to 2 (very true/often). T-scores were calculated for externalizing, internalizing, and dysregulation domains. In the study sample, alpha reliabilities for the domains were α = .81 for externalizing, α = .68 for internalizing, and α =.80 for dysregulation.
Analysis
All analyses were conducted as intention-to-treat, analyzing all 252 cases as randomly assigned to the PFR and control group (CG). Multiple linear regression was used to examine the treatment effect of PFR (0 = CG, 1 = PFR) on study outcomes including the primary caregiver outcomes (parenting sensitivity, dyadic synchrony, understanding of infant and toddler behavior, and maternal confidence) and the secondary infant outcomes (infant difficultness, internalizing behavior, externalizing behavior, and dysregulation). Covariates included preferred language (0 = English, 1 = Spanish) and the baseline measure (unavailable for the ITSEA scales). Covariates were decided upon prior to analyzing outcome data in order to align with stratification in the randomization design (Moher et al., 2021) and obtain precise and unbiased estimates of the intervention effect (Van Breukelen, 2006). Adjusting for the baseline measure, which was expected to be the strongest correlate of outcomes, increases the precisions of intervention effect estimates. Standardized effect sizes (d) were calculated based on the unstandardized effect coefficient for PFR divided by the pooled standard deviation of the measure at baseline (if available) or at the follow-up time point (when the baseline measure was not available). The sign of the standardized effect was coded so that a positive d would reflect a desired positive effect of PFR on the given outcome (e.g., a positive d would reflect higher parent sensitivity or reduced externalizing behavior associated with PFR). We interpret ds as small (0.20), medium (0.50), and large (0.80; Cohen, 1988).
Regression analyses were conducted in Mplus Version 7.31 (Muthén & Muthén, 1998–2015). Covariate missingness was modeled to allow for inclusion of all 252 cases in all regression models, including cases with partially missing data (Muthén, et al., 2016; Muthén & Muthén, 1998–2015). Maximum likelihood parameter estimates with conventional standard errors were obtained using the default maximum likelihood estimator (Muthén & Muthén, 1998–2015), which provides unbiased estimates assuming data are missing at random after adjusting for model covariates (Graham, 2012). There was a small amount of missing data at baseline (< 2% on any given measure). Missing data were also minimal among dyads completing the follow-up assessments (< 8% on any given measure at any given time point). Descriptive statistics were examined in IBM SPSS Version 19 (IBM Corp., 2010).
Results
At baseline (see Table 1), mothers averaged 28.8 (PFR) and 27.4 (CG) years of age, and their child averaged 1.8 (PFR) and 1.9 (CG) months old. Slightly more than half of the participants reported they were never married, 51% (PFR), and 57% (CG), and the majority of participants identified as White, 66% (PFR) and 65% (CG); 49% of mothers in the PFR group and 46% of mothers in the CG reported Hispanic/Latinx ethnicity. Approximately half of the participants in both groups reported no current depressive symptoms, 50% (PFR) and 48% (CG), nor anxiety symptoms 47% (PFR) and 46% (CG). A larger proportion of participants reported no significant level of PTSD symptoms, 67% (PFR) and 64% (CG). Table 2 shows means and standard deviations of caregiver and infant outcomes across each time point by treatment condition.
Table 2.
Means and standard deviations for caregiver and infant outcomes by treatment assignment at the three assessment time points
| Baseline | Infant age 6 months | Infant age 12 months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Control n = 125 | PFR n = 127 | Control n = 122 | PFR n = 122 | Control n = 123 | PFR n = 120 | |||||||
|
|
|
|
|
|
|
|||||||
| M | (SD) | M | (SD) | M | (SD) | M | (SD) | M | (SD) | M | (SD) | |
|
| ||||||||||||
| Primary caregiver outcomes | ||||||||||||
| Parenting sensitivity | 34.16 | (5.07) | 35.10 | (4.84) | 32.38 | (4.74) | 33.86 | (5.22) | 35.32 | (4.52) | 36.73 | (4.30) |
| Dyadic synchrony | 3.85 | (2.09) | 4.66 | (2.46) | 5.31 | (2.57) | 5.43 | (195) | 5.98 | (2.35) | 6.45 | (2.12) |
| Understanding of toddlers | 49.97 | (5.08) | 51.33 | (5.21) | 50.17 | (4.96) | 52.07 | (5.06) | 48.67 | (5.06) | 51.84 | (4.88) |
| Maternal confidence | 4.19 | (0.48) | 4.23 | (0.44) | 4.36 | (0.36) | 4.44 | (0.32) | 4.36 | (0.37) | 4.40 | (0.33) |
| Secondary infant outcomes | ||||||||||||
| Difficultness | 4.26 | (3.02) | 3.77 | (3.22) | 2.13 | (2.05) | 2.24 | (189) | 2.71 | (2.37) | 2.23 | (2.02) |
| Externalizing behavior | 62.54 | (12.37) | 59.24 | (11.06) | ||||||||
| Internalizing behavior | 54.93 | (11.48) | 53.64 | (10.82) | ||||||||
| Dysregulation | 55.33 | (13.66) | 54.82 | (13.62) | ||||||||
Note. PFR = Promoting First Relationships. n = maximum sample size at each time point. Parent sensitivity was measured by the Nursing Child Assessment Teaching Scale observational tool. Dyadic synchrony and infant difficultness were measured by the Infant CARE-Index observational tool. Understanding of toddlers was measured by the Raising a Baby parent-report tool. Maternal confidence was measured by the Maternal Confidence Questionnaire parent-report tool. Infant externalizing behavior, internalizing behavior, and dysregulation were measured by the Infant Toddler Social Emotional Assessment parent-report tool.
Table 3 shows the multiple linear regression models’ results examining the treatment effects of PFR, controlling for preferred language, and baseline measure (when available). There was a positive and significant effect of PFR on observed parenting sensitivity. The effect sizes were small at both time points (ds = 0.25 and 0.26 at age 6 and 12 months, respectively). There was also a positive and significant effect of PFR on maternal understanding of infant and toddler behavior. The effect size was small at age 6 months (d = 0.21) and small-to-medium at age 12 months (d = 0.45). Infants in the PFR group also scored lower on mother-reported externalizing behavior at age 12 months, with a small effect size (d = 0.28). The PFR and control groups did not significantly differ on follow-up measures of dyadic synchrony, maternal confidence, infant difficultness, infant internalizing behavior, or infant dysregulation. However, the direction of the beta coefficients favored the PFR group for all but one outcome (infant difficultness at age 6 months).
Table 3.
Estimates of effects of PFR on outcomes at infant age 6 and 12 months
| Infant age 6 months | Infant; age 12 months | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| b | (SE) | 95% CI | p | d | b | (SE) | 95% CI | p | d | |
|
| ||||||||||
| Primary caregiver outcomes | ||||||||||
| Parent sensitivity | 1.24 | (0.63) | [0.01, 2.48] | .048 | 0.25 | 1.28 | (0.58) | [0.15, 2.41] | .026 | 0.26 |
| Dyadic synchrony | 0.01 | (0.29) | [−0.57, 0.58] | .981 | 0.00 | 0.43 | (0.30) | [−0.16, 1.01] | .154 | 0.19 |
| Understanding of toddlers | 1.06 | (0.49) | [0.10, 2.01] | .030 | 0.21 | 2.32 | (0.50) | [1.35, 3.30] | <.001 | 0.45 |
| Maternal confidence | 0.05 | (0.03) | [−0.01, 0.12] | .101 | 0.12 | 0.02 | (0.04) | [−0.05, 0.09] | .516 | 0.05 |
| Secondary infant outcomes | ||||||||||
| Difficultness | 0.10 | (0.25) | [−0.40, 0.60] | .693 | −0.03 | −0.49 | (0.29) | [−1.06, 0.08] | .094 | 0.16 |
| Externalizing behavior | −3.27 | (150) | [−6.21, −0.34] | .029 | 0.28 | |||||
| Internalizing behavior | −1.22 | (142) | [−4.00, 1.56] | .389 | 0.11 | |||||
| Dysregulation | −0.56 | (1.74) | [−3.97, 2.85] | .747 | 0.04 | |||||
Note. N = 252. PFR = Promoting First Relationships. b = unstandardized coefficient for PFR effect. Multiple regression models included covariates for preferred language (English v. Spanish) and the baseline measure when available. d = effect size calculated as the b divided by the pooled standard deviation of the measure at baseline (when available) or at follow-up (when baseline not available); the sign of d indicates whether the estimate of the PFR effect is in the desired direction (e.g., a positive sign indicates a desired effect of increasing parent sensitivity or reducing infant externalizing behavior). Parent sensitivity was measured by the Nursing Child Assessment Teaching Scale observational tool. Dyadic synchrony and infant difficultness were measured by the Infant CARE-Index observational tool. Understanding of toddlers was measured by the Raising a Baby parent-report tool. Maternal confidence was measured by the Maternal Confidence Questionnaire parent-report tool. Infant externalizing behavior, internalizing behavior, and dysregulation were measured by the Infant Toddler Social Emotional Assessment parent-report tool.
Discussion
PFR is a brief home visiting program that uses video feedback of parent-child interactions to help parents read their infant’s cues for more effective and sensitive responding. This RCT shows that PFR improved mothers’ observed sensitive caregiving and knowledge of infant and toddler development, as well as reduced mothers’ reports of infants’ externalizing behavior at 12 months of age. Caregivers were mothers with low-income who initiated treatment for an antenatal mental health concern, primarily depression, anxiety, and/or PTSD.
Although the mental health treatment they received in MHIP or MSS ameliorated symptoms for some women, many of these new mothers were still experiencing high rates of psychological distress. In the postpartum period, 52% of the mothers in the sample had a PHQ-9 score indicating mild to severe depression (scores of 5 to 27), compared to 27% in a representative sample of US women (Shim et al., 2011). Similarly, 54% of the mothers in this sample experienced mild-to-severe anxiety, as determined by a GAD score between 5 and 21, compared to a recent report from the National Center for Health Statistics in which 19% of women experienced mild-to-severe anxiety symptoms in the past two weeks (Terlizzi & Villarroel, 2020). Finally, 36% of the mothers in this sample likely had PTSD, compared to 8% reported in a prospective study of 2,654 pregnant women (Yonkers et al., 2014). Our sample is unique in that all mothers had received at least a minimal level of support services for stress and mental health during pregnancy, which makes it difficult to compare with other studies of national samples, or even low-income samples not receiving services. One large multi-state study of 75,234 postpartum women, using the common depression cut point score of 10 on the PHQ-9, found a depression prevalence rate of 19.8% among women receiving WIC services (Pooler et al., 2013). In our sample, similar in that 93% of the mothers were receiving WIC, the depression prevalence rate (PHQ-9 score ≥ 10) was comparable at 19.5%. A clinical trial for perinatal depression treatment with a sample of women who were clinically depressed and receiving public health services reported post-birth rate of anxiety of 20% (Grote et al., 2015), which compares closely with our sample at 25.4%. These types of psychological distress can impair a mother’s ability to care for her infant without additional support.
This study’s findings are important because treating maternal mood disorders alone does not necessarily translate to improved child outcomes (Forman et al., 2007). Instead, parenting quality mediates maternal depression on child developmental outcomes (Goodman et al., 2020). Thus, it is critical to identify intervention practices that enhance maternal caregiving in the context of mental health challenges. PFR is a brief home visiting program that can be delivered in the context of ongoing community mental health treatment for new mothers, yielding positive outcomes on parenting and child behavior. PFR has improved parenting in various contexts and samples (Spieker et al., 2012; Oxford, Spieker, et al., 2016; Booth-LaForce et al., 2020). The current work is the first study to show PFR’s effectiveness for Spanish- or English-speaking women with low income and their newborn infants.
It is worth noting that the intervention effect on both parent and child outcomes was significant at 6-months post-intervention, with effect sizes ranging from .26 to .45. Considering these results from a relationship-based attachment perspective, increasing caregiver sensitivity and reducing child externalizing behavior may have long-term reciprocal effects, promoting relationship satisfaction between mother and child and promoting a positive developmental cascade. A developmental cascade is a process by which cumulative interactions/transactions of one type or another (positive or negative) will “flow” across other domains, levels of functioning, or systems/generations (Masten & Cicchetti, 2010). In this case, reduced externalizing behavior and increased parenting sensitivity could foreshadow a more positive, rewarding relationship that could impact the child’s relationship with other caregivers or in different contexts, such as childcare. Our earlier work suggests a positive developmental cascade for child welfare and other child outcomes that reached beyond the six-month follow-up (Oxford, Spieker et al., 2016; Pasalich et al., 2016; Spieker et al., 2014) rather than the effects fading out over time which is common among interventions in early childhood (Bailey et al., 2017).
While the primary findings from this study were as predicted, some hypotheses were not supported. Mother-reported infant internalizing behavior and dysregulation on the ITSEA, and observed dyadic synchrony and infant difficultness in the ICI were nonsignificant. Differences in dyadic synchrony and infant difficultness, though nonsignificant, were generally in the expected direction with small effect sizes at child age 12 months (.19 and .16, respectively). PFR is a strengths- and relationship-based program that seeks explicitly to increase caregiver confidence by using positive and instructive feedback given during video feedback observation sessions. Thus, it was unexpected that PFR did not increase mothers’ reports of caregiving confidence. The maternal confidence scores were very high for both groups (averaging over 4 on the 5-point scale). Possibly the scale was subject to social desirability; mothers may not want to admit that they do not understand or know how to take care of their baby, or do not feel satisfied being a parent. The other maternal report measures of their infants’ behaviors and knowledge of infant/toddler development may be less likely to be influenced by social desirability.
PFR is not a mental health treatment, and we had no hypothesis that PFR would improve mothers’ negative mood. However, we explored this possibility with post hoc analyses of mothers’ 6- and 12-month PHQ-9 and GAD-7 severity scores, entering baseline scores and preferred language as covariates and including all 252 cases in analyses (as done above for the hypothesized outcome variables). Mothers in the PFR group had lower severity scores on both measures at both time points. Differences trended toward significance at 6 months for the GAD-7, d = 0.19, p = .054, and at 12 months for the PHQ-9, d = 0.18, p = .089. These unanticipated findings warrant further exploration of ways to leverage ongoing mental health treatment in combination with a relationship program like PFR, to improve outcomes for distressed mothers and their infants.
Strengths, Limitations, and Future Directions
The strengths of this study were its successful enrollment of a diverse sample of new mothers with low income through community health centers and public health clinics, a high rate of retention (96.4%) in the research, excellent fidelity to PFR by the community mental health providers who delivered the program, and a high rate of completion of the PFR program (82% receiving 9–10 sessions and only 2% receiving no session) by mothers assigned to the PFR condition. The high completion rate suggests the intent-to-treat estimate for the effect of being offered the intervention is close to an estimate of the effect of the intervention on those treated (Yau & Little, 2001). The study design for research and service delivery enabled both Spanish- and English-speaking mothers to participate. There were very few exclusion/inclusion criteria such that the sample reflected the community. Participants were eligible if they received mental health treatment during pregnancy, spoke Spanish or English, and had access to a phone with no immediate plans to move out of the area. We also recruited out of five area clinics that offered MHIP or MSS rather than relying on one or two clinics for recruitment; this allowed a much broader regional recruitment strategy.
Despite these strengths, a critical limitation of the study was the poor inter-rater agreement of the ICI coders, which may have compromised the ability to detect intervention effects. Unlike the NCATS, for which one coder coded all observations and with a single reliability partner, 16 workers from 12 countries, all certified to code for research, coded the ICIs. All ICI coders spoke English, but also German, Italian, Greek, or Spanish. They each coded roughly 50 ICIs over a few years, which may have adversely affected agreement. Coders also coded the baseline, 6-, and 12-month ICIs in random order. In hindsight, we think completing one age group before moving on to the next might have enhanced inter-rater agreement by focusing the coders within each developmental epoch. Another intervening factor out of our control led to a smaller Spanish-speaking subsample than intended. We aimed to have 50% Spanish-speaking participants. We were on track to achieve this goal until the 2016 United States presidential election, after which there was a sharp decline in enrollment of Spanish-speaking mothers. Anecdotal evidence suggests that many Latina women were anxious about their immigration status or the potential deportation of loved ones due to anti-immigrant policies and rhetoric.
Future analyses will examine the role of language group, the severity of maternal distress, early childhood trauma, and maternal reflective functioning concerning parent and child behavioral outcomes. These analyses will include exploring both the direct effects of these variables and whether they moderate the PFR intervention’s effectiveness. We plan to conduct a follow-up study of the sample to examine whether the benefits of PFR extend to the child’s cardiometabolic health in early childhood.
Conclusion
In conclusion, this RCT showed that PFR is effective for infant-mother dyads in which the infant is very young, and mothers were experiencing perinatal distress. In this context, PFR showed improvement in maternal sensitive caregiving and knowledge of child development, with excellent program completion, suggesting that distressed mothers with very young infants are open to receiving these services if offered. It is feasible to provide this brief intervention as part of integrated care through community-based clinics.
Supplementary Material
ACKNOWLEDGMENTS:
This paper was supported by a grant from the National Institute of Health Eunice Kennedy Shriver National Institute of Child Health and Human Development, R01 HD052809, awarded to Dr. Susan Spieker. The study’s protocol is registered at ClinicalTrials.gov Protocol Registration and Results System (NCT02724774). We thank our research team (Solange Mecham, Ivonne Poveda, Anthippy Petras, and Boeun Kim) and our collaborative partners at Wellspring Family Services for the work and support of this project. Special thanks are given to the participating families.
Contributor Information
Monica L. Oxford, Child, Family, and Population Health Nursing, University of Washington
Jonika B. Hash, Child, Family, and Population Health Nursing, University of Washington
Mary J. Lohr, Child, Family, and Population Health Nursing, University of Washington
Maria E. Bleil, Child, Family, and Population Health Nursing, University of Washington
Charlie B. Fleming, Department of Psychiatry and Behavioral Sciences, University of Washington
Jurgen Unützer, Psychiatry & Behavioral Sciences, University of Washington.
Susan J. Spieker, Child, Family, and Population Health Nursing, University of Washington
References
- ACOG Committee Opinion No. 757 Summary: Screening for Perinatal Depression. (2018). Obstetrics & Gynecology, 132(5), 1314–1316. 10.1097/AOG.0000000000002928 [DOI] [PubMed] [Google Scholar]
- Ammerman RT, Altaye M, Putnam FW, Teeters AR, Zou Y, & Van Ginkel JB (2015). Depression improvement and parenting in low-income mothers in home visiting. Archives of Women’s Mental Health, 18(3), 555–563. 10.1007/s00737-014-0479-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Altaye M, Stevens J, Teeters AR, & Van Ginkel JB (2013). A clinical trial of in-home CBT for depressed mothers in home visitation. Behavior Therapy, 44(3), 359–372. 10.1016/j.beth.2013.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Bosse NR, Teeters AR, & Van Ginkel JB (2010). Maternal depression in home visitation: A systematic review. Aggression and Violent Behavior, 15(3), 191–200. PMCID: 2855144. 10.1016/j.avb.2009.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Shenk CE, Teeters AR, Noll RB, Putnam FW, & Van Ginkel JB (2011). Impact of depression and childhood trauma in mothers receiving home visitation. Journal of Family Studies, 21, 612–625. 10.1007/s10826-011-9513-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badr LK (2005). Further psychometric testing and use of the Maternal Confidence Questionnaire. Issues in Comprehensive Pediatric Nursing, 28, 163–174. doi: 10.1080/01460860500227572. PMID: 16251162. [DOI] [PubMed] [Google Scholar]
- Bailey D, Duncan GJ, Odgers CL, & Yu W. (2017). Persistence and fadeout in the impacts of child and adolescent interventions. Journal of Research on Educational Effectiveness, 10(1), 7–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, van Ijzendoorn MH, & Juffer F. (2003). Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychological Bulletin, 129(2), 195–215. 10.1037/0033-2909.129.2.195 [DOI] [PubMed] [Google Scholar]
- Barnard KE (1994). What the Teaching Scale measures. In Sumner GS & Spietz A. (Eds.), NCAST: Caregiver/parent-child interaction teaching manual. University of Washington NCAST Publications. [Google Scholar]
- Bayrampour H, Hapsari AP, & Pavlovic J. (2018). Barriers to addressing perinatal mental health issues in midwifery settings. Midwifery, 59, 47–58. 10.1016/j.midw.2017.12.020 [DOI] [PubMed] [Google Scholar]
- Beck CT (1996). A meta-analysis of predictors of postpartum depression. Nursing Research, 45(5), 297–303. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=8831657 [DOI] [PubMed] [Google Scholar]
- Beck CT, Gable RK, Sakala C, & Declercq ER (2011). Posttraumatic stress disorder in new mothers: results from a two-stage U.S. national survey. Birth, 38(3), 216–227. 10.1111/j.1523-536X.2011.00475.x [DOI] [PubMed] [Google Scholar]
- Beeber LS, Schwartz TA, Holditch-Davis D, Canuso R, Lewis V, & Hall HW (2013). Parenting enhancement, interpersonal psychotherapy to reduce depression in low-income mothers of infants and toddlers: a randomized trial. Nursing Research, 62(2), 82–90. 10.1097/NNR.0b013e31828324c2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat A, Reed SD, & Unützer J. (2017). The obstetrician-gynecologist’s role in detecting, preventing, and treating depression. Obstetrics & Gynecology, 129(1), 157–163. 10.1097/AOG.0000000000001809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biaggi A, Conroy S, Pawlby S, & Pariante CM (2016). Identifying the women at risk of antenatal anxiety and depression: A systematic review. Journal of Affective Disorders, 191, 62–77. 10.1016/j.jad.2015.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binda V, Figueroa-Leigh F, & Olhaberry M. (2019). Antenatal and postnatal depressive symptoms: Association with quality of mother-infant interaction. Infant Behavior and Development, 57, 101386. 10.1016/j.infbeh.2019.101386 [DOI] [PubMed] [Google Scholar]
- Booth-LaForce C, Oxford ML, Barbosa-Leiker C, Burduli E, & Buchwald DS (2020). Randomized controlled trial of the Promoting First Relationships® preventive intervention for primary caregivers and toddlers in an American Indian community. Prevention Science, 21(1), 98–108. 10.1007/s11121-019-01053-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byatt N, Levin LL, Ziedonis D, Moore Simas TA, & Allison J. (2015). Enhancing participation in depression care in outpatient perinatal care settings: A systematic review. Obstetrics & Gynecology, 126(5), 1048–1058. 10.1097/AOG.0000000000001067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter AS & Briggs-Gowan M. (2006). Infant - Toddler Social and Emotional Assessment (ITSEA): Examiner’s manual. Pearson. [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Cohn JF, Matias R, Tronick EZ, Connell D, & Lyons-Ruth K. (1986). Face-to-face interactions of depressed mothers and their infants. New Directions in Child Development (34), 31–45. 10.1002/cd.23219863405 [DOI] [PubMed] [Google Scholar]
- Crittenden PM (1979–2010). CARE-Index: Infant coding manual. Family Relations Institute. [Google Scholar]
- Crncec R, Barnett B, & Matthey S. (2010). Review of scales of parenting confidence. Journal of Nursing Measurement, 18(3), 210–240. 10.1891/1061-3749.18.3.210 [DOI] [PubMed] [Google Scholar]
- Dennis CL, & Dowswell T. (2013). Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Systematic Review (2), CD001134. 10.1002/14651858.CD001134.pub3 [DOI] [PubMed] [Google Scholar]
- Falah-Hassani K, Shiri R, & Dennis CL (2017). The prevalence of antenatal and postnatal co-morbid anxiety and depression: a meta-analysis. Psychological Medicine, 47(12), 2041–2053. 10.1017/S0033291717000617 [DOI] [PubMed] [Google Scholar]
- Feil EG, Baggett KM, Davis B, Sheeber L, Landry S, Carta JJ, & Buzhardt J. (2008). Expanding the reach of preventive interventions: development of an Internet-based training for parents of infants. Child Maltreatment, 13(4), 334–346. 10.1177/1077559508322446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Diego M, Hernandez-Reif M, Figueiredo B, Deeds O, Ascencio A, Schanberg S, & Kuhn C. (2009). Comorbid depression and anxiety effects on pregnancy and neonatal outcome. Infant Behavior and Development, 33(1), 23–29. 10.1016/j.infbeh.2009.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman DR, O’Hara MW, Stuart S, Gorman LL, Larsen KE, & Coy KC (2007). Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Development & Psychopathology, 19(2), 585–602. 10.1017/S0954579407070289 [DOI] [PubMed] [Google Scholar]
- Fukkink RG (2008). Video feedback in widescreen: a meta-analysis of family programs. Clinical Psychology Review, 28(6), 904–916. 10.1016/j.cpr.2008.01.003 [DOI] [PubMed] [Google Scholar]
- Geier M, Hills N, Gonzales M, Tum K, & Finley P. (2015). Detection and treatment rates for perinatal depression in a state Medicaid population. CNS Spectrums, 20(1), 11–19. doi: 10.1017/S1092852914000510 [DOI] [PubMed] [Google Scholar]
- Geller PA, & Stasko EC (2017). Effect of previous posttraumatic stress in the perinatal period. Journal of Obstetric, Gynecological, and Neonatal Nursing, 46(6), 912–922. 10.1016/j.jogn.2017.04.136 [DOI] [PubMed] [Google Scholar]
- Glover V. (2014). Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Practice & Research Clinical Obstetrics & Gynaecology, 28(1), 25–35. 10.1016/j.bpobgyn.2013.08.017 [DOI] [PubMed] [Google Scholar]
- Goodman SH (2020). Intergenerational transmission of depression. Annual Review of Clinical Psychology, 16, 213–238. 10.1146/annurev-clinpsy-071519-113915 [DOI] [PubMed] [Google Scholar]
- Goodman SH, Cullum KA, Dimidjian S, River LM, & Kim CY (2018). Opening windows of opportunities: Evidence for interventions to prevent or treat depression in pregnant women being associated with changes in offspring’s developmental trajectories of psychopathology risk. Development & Psychopathology, 30(3), 1179–1196. 10.1017/S0954579418000536 [DOI] [PubMed] [Google Scholar]
- Goodman SH, & Garber J. (2017). Evidence-based interventions for depressed mothers and their young children. Child Development, 88(2), 368–377. 10.1111/cdev.12732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, & Halperin MS (2020). Perinatal depression as an early stress: Risk for the development of psychopathology in children. In Harkness KL & Hayden EP (Eds.), The Oxford handbook of stress and mental health. Oxford University Press. 10.1093/oxfordhb/9780190681777.013.13 [DOI] [Google Scholar]
- Goodman SH, Simon HFM, Shamblaw AL, & Kim CY (2020). Parenting as a mediator of associations between depression in mothers and children’s functioning: A systematic review and meta-analysis. Clinical Child Family Psychological Review. 10.1007/s10567-020-00322-4 [DOI] [PubMed] [Google Scholar]
- Goyal D, Gay C, & Lee KA (2010). How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first-time mothers? Women’s Health Issues, 20(2), 96–104. 10.1016/j.whi.2009.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham J. (2012). Missing data: Analysis and design (Vol. Springer; ). [Google Scholar]
- Grote NK, & Frank E. (2003). Difficult-to-treat depression: the role of contexts and comorbidities. Biological Psychiatry, 53(8), 660–670. 10.1016/s0006-3223(03)00006-4 [DOI] [PubMed] [Google Scholar]
- Grote NK, Katon WJ, Russo JE, Lohr MJ, Curran M, Galvin E, & Carson K. (2015). Collaborative care for perinatal depression in socioeconomically disadvantaged women: a randomized trial. Depression and Anxiety, 32, 821–834. 10.1002/da.22405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubbels J, van der Put CE, Stams GJM, Prinzie PJ, & Assink M. (2021). Components associated with the effect of home visiting programs on child maltreatment: A meta-analytic review. Child Abuse & Neglect, 114, 104981. 10.1016/j.chiabu.2021.104981 [DOI] [PubMed] [Google Scholar]
- Hash JB, Oxford ML, Fleming CB, Ward TM, Spieker SJ, & Lohr MJ (2019). Impact of a home visiting program on sleep problems among young children experiencing adversity. Child abuse & neglect, 89, 143–154. 10.1016/j.chiabu.2018.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastings PD, Kahle S, Fleming C, Lohr MJ, Katz LF, & Oxford ML (2019). An intervention that increases parental sensitivity in families referred to Child Protective Services also changes toddlers’ parasympathetic regulation. Developmental Science, 22(1), e12725. 10.1111/desc.12725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes LJ, Goodman SH, & Carlson E. (2013). Maternal antenatal depression and infant disorganized attachment at 12 months. Attachment & Human Development, 15(2), 133–153. 10.1080/14616734.2013.743256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- HomVEE. (2020). Early Childhood Home Visiting Models: Reviewing Evidence of Effectiveness (OPRE Report #2020–126). https://homvee.acf.hhs.gov/sites/default/files/2020-12/HomVEE_Summary_Brief.pdf
- Huang H, Chan YF, Katon W, Tabb K, Sieu N, Bauer AM, Wasse JK, & Unützer J. (2012). Variations in depression care and outcomes among high-risk mothers from different racial/ethnic groups. Family Practice, 29(4), 394–400. 10.1093/fampra/cmr108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp. (2010). IBM SPSS Statistics for Windows, Version 19.0. [Google Scholar]
- Ierardi E, Ferro V, Trovato A, Tambelli R, & Riva Crugnola C. (2019). Maternal and paternal depression and anxiety: their relationship with mother-infant interactions at 3 months. Archive of Women’s Mental Health, 22(4), 527–533. 10.1007/s00737-018-0919-x [DOI] [PubMed] [Google Scholar]
- Jones TL, & Prinz RJ (2005). Potential roles of parental self-efficacy in parent and child adjustment: A review. Clinical Psychology Review, 25, 341–363. [DOI] [PubMed] [Google Scholar]
- Kaplan MJ, & Klinetob NA (2000). Childhood emotional trauma and chronic posttraumatic stress disorder in adult outpatients with treatment-resistant depression. Journal of Nervous Mental Diseases, 188(9), 596–601. http://www.ncbi.nlm.nih.gov/pubmed/11009333 [DOI] [PubMed] [Google Scholar]
- Kelly J, Korfmacher J, & Buehlman K. (2008). Raising a Baby. University of Washington. [Google Scholar]
- Kelly J, Sandoval D, Zuckerman TG, & Buehlman K. (2008). Promoting First Relationships: A program for service providers to help parents and other caregivers nurture young children’s social and emotional development (2 ed.). NCAST Programs. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS, & National Comorbidity Survey R. (2003). The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA, 289(23), 3095–3105. 10.1001/jama.289.23.3095 [DOI] [PubMed] [Google Scholar]
- Kozhimannil KB, Trinacty CM, Busch AB, Huskamp HA, & Adams AS (2011). Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatric Services, 62(6), 619–625. 10.1176/ps.62.6.pss6206_0619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuklinski MR, Oxford ML, Spieker SJ, Lohr MJ, & Fleming CB (2020). Benefit-cost analysis of Promoting First Relationships®: Implications of victim benefits assumptions for return on investment. Child Abuse & Neglect, 106, 104515. 10.1016/j.chiabu.2020.104515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang AJ, & Stein MB (2005). An abbreviated PTSD checklist for use as a screening instrument in primary care. Behavior Research Therapy, 43(5), 585–594. 10.1016/j.brat.2004.04.005 [DOI] [PubMed] [Google Scholar]
- Leigh B, & Milgrom J. (2008). Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry, 8, 24. 10.1186/1471-244X-8-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippard ETC, & Nemeroff CB (2020). The devastating clinical consequences of child abuse and neglect: Increased disease vulnerability and poor treatment response in mood disorders. American Journal of Psychiatry, 177(1), 20–36. 10.1176/appi.ajp.2019.19010020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons-Ruth K, Wolfe R, Lyubchik A, & Steingard R. (2002). Depressive symptoms in parents of children under age 3: Sociodemographic predictors, current correlates, and associated parenting behaviors. In Halfon N, Taafe TM, & Schuster MA (Eds.), Child rearing in America: Challenges facing parents with young children (pp. 217–262). Cambridge University Press. [Google Scholar]
- Mantymaa M, Puura K, Luoma I, Kaukonen P, Salmelin RK, & Tamminen T. (2008). Infants’ social withdrawal and parents’ mental health. Infant Behavior and Development, 31(4), 606–613. https://doi.org/S0163-6383(08)00070-2 [pii] 10.1016/j.infbeh.2008.07.005 [DOI] [PubMed] [Google Scholar]
- Masten AS, & Cicchetti D. (2010). Developmental cascades. Development and Psychopathology, 22(3), 491–495. [DOI] [PubMed] [Google Scholar]
- Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG, & Consort. (2012). CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomized trials. International Journal of Surgery, 10(1), 28–55. 10.1016/j.ijsu.2011.10.001 [DOI] [PubMed] [Google Scholar]
- Muthén BO, & Muthén LK (1998–2015). Mplus user’s guide (7th ed.). Muthén & Muthén. [Google Scholar]
- Muthén BO, Muthén LK, & Asparouhov T. (2016). Regression and mediation analysis using Mplus. Muthén & Muthén. [Google Scholar]
- Muzik M, Bocknek EL, Broderick A, Richardson P, Rosenblum KL, Thelen K, & Seng JS (2013). Mother-infant bonding impairment across the first 6 months postpartum: the primacy of psychopathology in women with childhood abuse and neglect histories. Archives of Women’s Mental Health, 16(1), 29–38. 10.1007/s00737-012-0312-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council and Institute of Medicine (2009). Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. The National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK215117/ [PubMed] [Google Scholar]
- Nelson EM, & Spieker SJ (2013). Intervention effects on morning and stimulated cortisol responses among toddlers in foster care. Infant Mental Health Journal, 34(3). 10.1002/imhj.21382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor E, Senger CA, Henninger M, Gaynes BN, Coppola E, & Soulsby Weyrich M. (2019). In Interventions to Prevent Perinatal Depression: A Systematic Evidence Review for the U.S. Preventive Services Task Force. https://www.ncbi.nlm.nih.gov/pubmed/30807060 [PubMed]
- O’Donnell KJ, Glover V, Barker ED, and O’Connor TG (2014). The persisting effect of maternal mood in pregnancy on childhood psychopathology. Development & Psychopathology, 1–11. 10.1017/S0954579414000029 [DOI] [PubMed] [Google Scholar]
- O’Donnell KJ, & Meaney MJ (2017). Fetal origins of mental health: The developmental origins of health and disease hypothesis. American Journal of Psychiatry, 174(4), 319–328. 10.1176/appi.ajp.2016.16020138 [DOI] [PubMed] [Google Scholar]
- O’Hara L, Smith ER, Barlow J, Livingstone N, Herath NI, Wei Y, Spreckelsen TF, & Macdonald G. (2019). Video feedback for parental sensitivity and attachment security in children under five years. Cochrane Database Systematic Review, 11(7), CD012348. 10.1002/14651858.CD012348.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford M, Fleming C, Nelson E, Kelly J, & Spieker S. (2013). Randomized trial of Promoting First Relationships: Effects on maltreated toddlers’ separation distress and sleep regulation after reunification. Children and Youth Services Review, 35(12), 1988–1992. doi: 10.1016/j.childyouth.2013.09.021. PMCID: PMC386474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford M, Marcenko M, Fleming C, Spieker S. (2016). Promoting birth parents’ relationships with their toddlers upon reunification: Results from Promoting First Relationships® home visiting program. Child and Youth Service Review, 61, 109–116. 10.1016/j.childyouth.2015.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford ML, Spieker SJ, Lohr MJ, & Fleming CB (2016). Promoting First Relationships® : Randomized trial of a 10-week home visiting program with families referred to child protective services. Child Maltreatment, 21(4) 267–277. 10.1177/1077559516668274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parfitt Y, Pike A, & Ayers S. (2013). The impact of parents’ mental health on parent-baby interaction: a prospective study. Infant Behavior and Development, 36(4), 599–608. 10.1016/j.infbeh.2013.06.003 [DOI] [PubMed] [Google Scholar]
- Paris R, Bolton RE, & Spielman E. (2011). Evaluating a home-based dyadic intervention: Changes in postpartum depression, maternal perceptions, and mother-infant interactions. Infant Mental Health Journal, 32(3), 319–338. Doi 10.1002/Imhj.20299 [DOI] [PubMed] [Google Scholar]
- Pasalich DS, Fleming CB, Oxford ML, Zheng Y, & Spieker SJ (2016). Can parenting intervention prevent cascading effects from placement instability to insecure attachment to externalizing problems in maltreated toddlers? Child Maltreatment, 21(3), 175–185. 10.1177/1077559516656398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pocock SJ (1983). Clinical trials: a practical approach. John Wiley and Sons. [Google Scholar]
- Pooler J, Perry DF, & Ghandour RM (2013). Prevalence and risk factors for postpartum depressive symptoms among women enrolled in WIC. Maternal and Child Health Journal, 17, 1969–1980. 10.1007/s10995-013-1224-y [DOI] [PubMed] [Google Scholar]
- Prenoveau JM, Craske MG, West V, Giannakakis A, Zioga M, Lehtonen A, Davies B, Netsi E, Cardy J, Cooper P, Murray L, & Stein A. (2017). Maternal postnatal depression and anxiety and their association with child emotional negativity and behavior problems at two years. Developmental Psychology, 53(1), 50–62. 10.1037/dev0000221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers A, Obst S, Teague SJ, Spry EA, Macdonald JA, Sunderland M, Olsson CA, & Youssef G, Hutchinson D. (2020). Association between maternal perinatal depression and anxiety and child and adolescent development: A meta-analysis. JAMA Pediatrics. 10.1001/jamapediatrics.2020.2910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifer R, Dickstein S, Sameroff AJ, Magee KD, & Hayden LC (2001). Infant mental health and variability of parental depression symptoms. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1375–1382. 10.1097/00004583-200112000-00007 [DOI] [PubMed] [Google Scholar]
- Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, & Liberzon I. (2013). Childhood abuse history, posttraumatic stress disorder, postpartum mental health, and bonding: a prospective cohort study. Journal of Midwifery and Women’s Health, 58(1), 57–68. 10.1111/j.1542-2011.2012.00237.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim RS, Baltrus P, Ye J, & Rust G. (2011). Prevalence, treatment, and control of depressive symptoms in the United States: results from the National Health and Nutrition Examination Survey (NHANES), 2005–2008. Journal of the American Board of Family Medicine, 24(1), 33–38. 10.3122/jabfm.2011.01.100121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MV, Shao L, Howell H, Wang H, Poschman K, & Yonkers KA (2009). Success of mental health referral among pregnant and postpartum women with psychiatric distress. General Hospital Psychiatry, 31(2), 155–162. 10.1016/j.genhosppsych.2008.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spieker SJ, Oxford ML, & Fleming CB (2014). Permanency outcomes for toddlers in child welfare two years after a randomized trial of a parenting intervention. Child and Youth Service Review, 44, 201–206. 10.1016/j.childyouth.2014.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spieker SJ, Oxford ML, Kelly JF, Nelson EM, & Fleming CB (2012). Promoting first relationships: randomized trial of a relationship-based intervention for toddlers in child welfare. Child Maltreatment, 17(4), 271–286. 10.1177/1077559512458176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, & Williams JB (1999). Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA, 282(18), 1737–1744. https://doi.org/joc90770 [pii] [DOI] [PubMed] [Google Scholar]
- Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, & Pariante CM (2014). Effects of perinatal mental disorders on the fetus and child. Lancet, 384(9956), 1800–1819. 10.1016/S0140-6736(14)61277-0 [DOI] [PubMed] [Google Scholar]
- Stuart-Parrigon K, & Stuart S. (2014). Perinatal depression: An update and overview. Current psychiatry reports, 16(9), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terlizzi EP, & Villarroel MA (2020). Symptoms of generalized anxiety disorder among adults: United States, 2019. NCHS Data Brief, no. 378. https://www.cdc.gov/nchs/products/databriefs/db378.htm [PubMed] [Google Scholar]
- Thomas JC, Letourneau N, Campbell TS, Tomfohr-Madsen L, Giesbrecht GF, & Team APS (2017). Developmental origins of infant emotion regulation: Mediation by temperamental negativity and moderation by maternal sensitivity. Developmental Psychology, 53(4), 611–628. 10.1037/dev0000279 [DOI] [PubMed] [Google Scholar]
- Tourtelot EJ, Davis JR, Trabold N, Shah DK, & Poleshuck E. (2020). She screened positive for depression at the first prenatal visit, what really happens next? Journal of Clinical Psychology in Medical Settings. 10.1007/s10880-020-09734-4 [DOI] [PubMed] [Google Scholar]
- Unützer J, & Park M. (2012). Strategies to improve the management of depression in primary care. Primary Care, 39(2), 415–431. https://doi.org/S0095-4543(12)00024-3 [pii] 10.1016/j.pop.2012.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Breukelen GJ (2006). ANCOVA versus change from baseline: more power in randomized studies, more bias in nonrandomized studies [corrected]. Journal of Clinical Epidemiology, 59(9), 920–925. 10.1016/j.jclinepi.2006.02.007 [DOI] [PubMed] [Google Scholar]
- van der Wal MF, van Eijsden M, & Bonsel GJ (2007). Stress and emotional problems during pregnancy and excessive infant crying. Journal of Developmental and Behavioral Pediatrics, 28(6), 431–437. 10.1097/DBP.0b013e31811ff8f4 [DOI] [PubMed] [Google Scholar]
- van Doesum KTM, Riksen-Walraven JM, Hosman CMH, & Hoefnagels C. (2008). A randomized controlled trial of a home-visiting intervention aimed at preventing relationship problems in depressed mothers and their infants. Child Development, 79(3), 547–561. https://doi.org/DOI 10.1111/j.1467-8624.2008.01142.x [DOI] [PubMed] [Google Scholar]
- Wang L, Wu T, Anderson JL, & Florence JE (2011). Prevalence and risk factors of maternal depression during the first three years of child rearing. Journal of Women’s Health (Larchmt), 20(5), 711–718. 10.1089/jwh.2010.2232 [DOI] [PubMed] [Google Scholar]
- Warnock FF, Craig KD, Bakeman R, Castral T, & Mirlashari J. (2016). The relationship of prenatal maternal depression or anxiety to maternal caregiving behavior and infant behavior self-regulation during infant heel lance: an ethological time-based study of behavior. BMC Pregnancy Childbirth, 16, 264. 10.1186/s12884-016-1050-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom CS, DuMont K, & Czaja SJ (2007). A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry, 64(1), 49–56. 10.1001/archpsyc.64.1.49 [DOI] [PubMed] [Google Scholar]
- Yasuma N, Narita Z, Sasaki N, Obikane E, Sekiya J, Inagawa T, Nakajima A, Yamada Y, Yamazaki R, Matsunaga A, Saito T, Watanabe K, Imamura K, Kawakami N, & Nishi D. (2020). Antenatal psychological intervention for universal prevention of antenatal and postnatal depression: A systematic review and meta-analysis. Journal of Affective Disorders, 273, 231–239. 10.1016/j.jad.2020.04.063 [DOI] [PubMed] [Google Scholar]
- Yau LH, & Little RJ (2001). Inference for the complier-average causal effect from longitudinal data subject to noncompliance and missing data, with application to a job training assessment for the unemployed. Journal of the American Statistical Association, 96(456), 1232–1244. [Google Scholar]
- Yildiz PD, Ayers S, & Phillips L. (2017). The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. Journal of Affective Disorders 208, 634–645. 10.1016/j.jad.2016.10.009 [DOI] [PubMed] [Google Scholar]
- Yin X, Sun N, Jiang N, Xu X, Gan Y, Zhang J, Qiu L, Yang C, Shi X, Chang J, & Gong Y. (2021). Prevalence and associated factors of antenatal depression: Systematic reviews and meta-analyses. Clinical Psychology Review, 83, 101932. 10.1016/j.cpr.2020.101932 [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin H, & Belanger K. (2014). Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry, 71(8), 897–904. 10.1001/jamapsychiatry.2014.558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahr LK (1991). The relationship between maternal confidence and mother–infant behaviors in premature infants. Research in Nursing & Health, 14, 279–286. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.