Abstract
Prior studies have demonstrated the effects of the COVID-19 pandemic on weight management and lifestyle behaviors, though identification of who may be at greatest risk for negative consequences has not been fully explored. Addictive-like eating behavior, or food addiction, has been associated with an array of problematic eating behaviors, which may suggest heightened susceptibility to poorer outcomes. In this online, cross-sectional study, adults (ages 18–78; M = 42.36, SD = 13.08) living in the United States (n = 288) completed questionnaires assessing food addiction and reported changes to their weight, eating, and physical activity before and during the COVID-19 pandemic. Individuals with food addiction gained an average of 12.42 lb (5.63 kg) since March 2020, compared to an average weight gain of 2.14 lb (0.97 kg) for those without food addiction (p < .001). Linear regression analyses controlling for age and body mass index (BMI) showed that food addiction was independently associated with higher weight gain (B = 9.28, t = 4.97, p < .001), greater intake of ultra-processed foods before and during COVID-19 (B = 1.08, t = 5.71, p < .001; B = 1.18, t = 6.42, p < .001, respectively), greater attribution of their overall current eating behaviors to COVID-19 circumstances (B = 23.19, t = 4.62, p < .001), and higher distress about their overall current eating behaviors (B = −22.12, t = −2.50, p = .01). Interaction effects demonstrated that individuals with food addiction who are older may be at particularly high risk for weight gain and distress. The present research suggests that food addiction is a uniquely meaningful phenotype, beyond the effects of BMI, to identify risk for the negative consequences of COVID-19. Individuals with food addiction, particularly those who are older, may benefit from support with weight management and addictive-like eating as the COVID-19 pandemic persists and resolves.
Keywords: Food addiction, Obesity, COVID-19 pandemic
1. Introduction
The COVID-19 pandemic has resulted in numerous and extensive changes to everyday life due to stay-at-home orders introduced in many locations across the United States in March 2020. From March 1, 2020 to May 31, 2020, 42 states had mandatory stay-at-home orders, which included work-from-home for most people except essential workers and the shutdown of public facilities (e.g., gyms, schools, daycare facilities) and leisure activities (e.g., in-person dining, movie theaters) (Moreland et al., 2020). While some of these restrictions were modified beginning in June 2020 (e.g., increases in outdoor dining), the majority of individuals continue to experience alterations to their typical schedules (e.g., working from home, childcare). These interruptions have had differential effects, and individuals with obesity seem to have been particularly significantly impacted by the negative physical and psychological consequences of COVID-19 (Fernandez-Rio, Cecchini, Mendez-Gimenez, & Carriedo, 2020; Kwok et al., 2020; Poly et al., 2021). Thus, understanding how the circumstances of COVID-19 may influence weight, eating, and activity behavior for specific presentations of problematic eating behavior in a manner that may exacerbate obesity and increase risk for negative outcomes remains important.
1.1. The influence of COVID-19 on weight, eating, and physical activity
1.1.1. Weight change
Prospective studies conducted early in the pandemic (April–May 2020) did not show significant weight changes among adults (Keel et al., 2020; Lamarche et al., 2021), while one conducted in May–July 2020 among adolescents did show significant excess gains, with participants gaining an average of 3.47 lb (1.57 kg) compared to baseline data collected between October 2018 and October 2019 (Mason, Barrington-Trimis, & Leventhal, 2021). In cross-sectional studies conducted during April and May 2020 among adults from the United States (Zachary et al., 2020), Italy (Marchitelli et al., 2020; Pellegrini et al., 2020; Scarmozzino & Visioli, 2020), India (Chopra et al., 2020), and Lithuania (Kriaucioniene, Bagdonaviciene, Rodriguez-Perez, & Petkeviciene, 2020), between 19.5 and 66% of individuals endorsed gaining weight compared to before March 2020, though the degree of weight change was not reported. Only one study reported the average amount of weight gain at 3.3 lb (1.5 kg) (Pellegrini et al., 2020). Individuals with higher body weights, problematic eating behaviors, and psychological symptoms have exhibited elevated risk for weight gain during this time (Kriaucioniene et al., 2020; Marchitelli et al., 2020; Pellegrini et al., 2020).
1.1.2. Eating behaviors and physical activity
Cross-sectional online studies reporting on physical activity levels have fairly consistently reported decreases for children, adolescents, and adults in North America, Europe, and Asia in April and May 2020 compared to before March 2020 (Carroll et al., 2020; Chopra et al., 2020; López-Bueno et al., 2020; Maugeri et al., 2020; Pietrobelli et al., 2020; Robinson et al., 2020; Robinson, Gillespie, & Jones, 2020; Zachary et al., 2020). In contrast, significant variability has been reported with changes to eating behaviors since the start of COVID-19 stay-at-home orders were introduced in March 2020. For example, in a large, retrospective, online study of Italian adults, 52.9% of participants self-reported eating more when surveyed in April 2020, compared to their typical consumption before March 2020, particularly increasing intake of “comfort foods” like sweets and salty snacks (Scarmozzino & Visioli, 2020). Retrospective studies conducted in April and May 2020 have suggested that individuals with obesity seem to have exhibited greater increases in calorie intake, especially for high-fat, high-sugar foods (Almandoz et al., 2020; Chopra et al., 2020; Kriaucioniene et al., 2020; Pellegrini et al., 2020; Robinson et al., 2020). However, the only prospective study of changes in eating behaviors found that Canadian adults reported improvements in diet quality in April–May 2020, compared to before March 2020, with greater improvements observed for persons with obesity (Lamarche et al., 2021).
1.1.3. Gaps in the literature
While obesity has been associated with increased negative changes in eating and activity behavior since the start of COVID-19, inconsistent findings have been observed between retrospective studies and the one prospective approach in Canadian adults. This may be because obesity is a heterogeneous condition that can be related to factors besides energy balance (e.g., medication side effects). As such, obesity is an oversimplified proxy for identifying who may be at greatest risk for problematic eating and activity behaviors related to the circumstances of COVID-19. Profiles of eating behaviors that overlap with, but are not synonymous with, obesity may better highlight specific intervention targets (e.g., binge eating, addictive-like eating) and public policy initiatives.
1.2. Food addiction
Food addiction has been proposed as a distinct profile of eating behaviors that reflects a substance-based addiction to ultra-processed foods (Gearhardt, Corbin, & Brownell, 2009a; Gearhardt, Davis, Kuschner, & Brownell, 2011; Schulte, Avena, & Gearhardt, 2015). Ultra-processed foods (e.g., pizza, pastries, potato chips, soda) are recognized as class 4 foods by the NOVA classification system (Monteiro et al., 2019). Ultra-processed foods are not in a natural state and are created to contain added amounts of fat, refined carbohydrates, and/or salt, compared to naturally occurring, minimally processed foods like fruits, vegetables, and animal protein (NOVA class 1 foods) (Monteiro et al., 2019). Food addiction is most commonly operationalized by the Yale Food Addiction Scale (YFAS), which adapts the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) (American Psychiatric Association, 2013) criteria for substance-use disorders to addictive-like consumption of ultra-processed foods (e.g., use despite negative consequences, repeated unsuccessful attempts to cut down) (Gearhardt, Corbin, & Brownell, 2009b, 2016). While problematic eating behavior may occur with an array of foods, the theoretical perspective of food addiction aligns with substance-use disorders to posit the direct, specific addictive potential of ultra-processed foods. In support of this theoretical perspective, prior studies have found that individuals with food addiction, as assessed by the YFAS, have exhibited self-reported and behavioral features of addiction with ultra-processed foods, whereas minimally processed foods (fruits, vegetables, animal protein) have had little association with problematic eating in this population (Curtis & Davis, 2014; Pursey, Collins, Stanwell, & Burrows, 2015; Schulte et al., 2015, 2017, 2018). Thus, though additional research is needed to determine which ingredient(s) in ultra-processed foods may be the addictive agent, akin to nicotine in cigarettes, the literature presently provides strong support that the category of ultra-processed foods are uniquely associated with behavioral indicators of food addiction.
Using the YFAS, approximately 13–15% of individuals in general population samples meet criteria for food addiction, with rates estimated higher (25%) for persons with obesity (Schulte & Gearhardt, 2017, 2018). Numerous biological and behavioral parallels have been observed between food addiction and substance-use disorders (Davis et al., 2013; Hardee et al., 2020; Murphy, Stojek, & MacKillop, 2014; Pivarunas & Conner, 2015; Ravichandran et al., 2021; Schulte, Grilo, & Gearhardt, 2016; Schulte et al., 2019, Schulte et al., 2019; VanderBroek-Stice, Stojek, Beach, vanDellen, & MacKillop, 2017), including the use of rewarding substances (e.g., ultra-processed foods) to cope with stress (Hardy, Fani, Jovanovic, & Michopoulos, 2018; Joyner, Schulte, Wilt, & Gearhardt, 2015; Pivarunas & Conner, 2015). Given that overeating, often with comfort foods, to cope with the COVID-19 pandemic was associated with elevated weight gain (Mason et al., 2021), individuals with food addiction who exhibit compulsive consumption of high-calorie, ultra-processed foods, may be at particularly high risk for negative changes in weight, eating, and physical activity due to COVID-19. Notably, Panno, Carbone, Massullo, Farina, and Imperatori (2020) found that YFAS symptoms were associated with greater psychological distress during the COVID-19 pandemic, though it is unknown how this may translate to reported behaviors. Further, one study found no difference in food addiction symptoms reported in a general population sample of United States adults in February 2019 to a second, similar sample recruited just after the start of COVID-19 on March 31, 2020 (Cummings, Ackerman, Wolfson, & Gearhardt, 2021). While this provides preliminary insight that the prevalence of food addiction indicators did not increase among United States adults within the first two weeks of COVID-19, this study was conducted very early in the pandemic and did not assess the consequences of COVID-19 among persons who screen positive for food addiction.
1.3. The current study
The present research is among the first, to our knowledge, to examine changes in weight, eating behavior, and physical activity due to the COVID-19 pandemic among individuals who screen positive for food addiction. Changes to eating behavior were examined for both ultra-processed (NOVA class 4) and minimally processed, naturally occurring (NOVA class 1; e.g., fruits, vegetables, lean proteins) food consumption. The primary aim of this research was to assess whether food addiction was associated with changes in weight, eating behavior, and physical activity related to the circumstances of COVID-19, above and beyond the effect of body mass index (BMI). It was hypothesized a priori that individuals with food addiction would exhibit greater weight gain, higher consumption of ultra-processed foods, and greater psychological distress associated with the COVID-19 pandemic. Notably, the present approach allowed for the assessment of whether food addiction was associated with these negative behavioral and weight change consequences of COVID-19 above and beyond the effects of BMI. Understanding how the clinical relevance of food addiction extends beyond overweight and obesity has the potential to translate meaningfully into public policy initiatives and clinical interventions by targeting addictive-like responses to ultra-processed foods.
2. Methods
2.1. Ethics
This research was performed in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board at the University of Pennsylvania (protocol #844818). All individuals provided written informed consent for their participation electronically.
2.2. Participants
Participants (N = 306) over the age of 18 years living in the United States were recruited in February 2021 through Amazon Mechanical Turk (MTurk), an online service that recruits samples with similar demographic characteristics as convenience samples (Paolacci & Chandler, 2014). All individuals resided in the United States and were pre-registered MTurk users who found the study information within the MTurk platform. Participants were excluded from analyses if they reported height and weight measurements considered biologically implausible values [height <44 inches (112 cm) or >90 inches (229 cm); weight <55 lb (24.95 kg) or >1000 lb (453.59 kg)] (Littman, Boyko, McDonell, & Fihn, 2012) (n = 3) or for incorrectly answering “catch questions,” which have commonly-known answers (e.g. 2 + 2) designed to “catch” participants who respond without reading the questions carefully (n = 15). After these exclusions, 288 participants were included in the analyses.
2.3. Measures
2.3.1. Modified Yale Food Addiction Scale 2.0 (mYFAS 2.0)
The mYFAS 2.0 is a validated, brief assessment of food addiction (Schulte & Gearhardt, 2017) that adapts the 11 DSM-5 diagnostic criteria for substance-use disorders (American Psychiatric Association, 2013) to addictive-like consumption of certain foods individuals may experience problems with, including references to numerous ultra-processed foods (e.g., pizza, chocolate, potato chips) that have been most closely associated with indicators of food addiction in prior research (Curtis & Davis, 2014; Pursey et al., 2015; Schulte et al., 2015). Thus, while individuals could respond by thinking of any foods they exhibited problems with in the past year, they are primed to think of ultra-processed foods. In addition, the mYFAS 2.0 asks respondents to think about their eating behavior since the start of COVID-19 stay-at-home orders (from March 2020 until the time of survey in February 2021). The mYFAS 2.0 can be scored continuously to reflect how many of the 11 DSM-5 criteria are met, or the measure can be scored as a dichotomous “diagnostic” threshold met by endorsing two or more criteria and a question about either functional impairment or distress. The mYFAS 2.0 had excellent internal consistency in this sample (α = 0.96). In the current study, the dichotomous “diagnostic” threshold was used to compare individuals who did versus did not meet the mYFAS 2.0 criteria for clinically significant food addiction.
2.3.2. COVID-19 eating and activity questionnaire
The research team developed questions to assess the impact of the COVID-19 pandemic on eating and activity behaviors of interest. Participants were asked to report whether they gained or lost weight and then to specify the number of pounds gained/lost and the factors to which they attributed their weight change, if applicable.
Participants were then asked to think about their typical eating and activity behaviors in the 6 months before the COVID-19 pandemic began (September 2019 to February 2020) and answered nine questions indicating how frequently they consumed fast food, junk food snacks, sweets, sugar-sweetened beverages, take-out, and fruits/vegetables, and how often they cooked healthy meals, exercised, or were physically active in their daily routine. All items were rated on a 7-point Likert scale: 1 = “Less than once per month; ” 2 = “1–3 times per month; ” 3 = “1–3 times per week; ” 4 = “4–6 times per week; ” 5 = “Once per day; ” 6 = “2–3 times per day; ” and 7 = “4 or more times per day.”
Participants were then asked to think about the time period they struggled most with healthy eating and physical activity since the COVID-19 pandemic began in March 2020, and they then answered the same nine questions for this time period. Change scores were calculated for each of the nine questions (frequency of most difficult time – frequency before the start of COVID-19; positive values mean an increase during the most difficult period). At both time periods and for the calculated change scores, the questions related to ultraprocessed food consumption (fast food, junk food snacks, sweets, sugar-sweetened beverages, take-out) were highly correlated (rs = 0.24-0.72; ps < .001), as were the questions assessing minimally processed food consumption (fruits/vegetables, healthy cooking at home) (rs = 0.19-0.75; ps < .001) and physical activity (exercise, daily activity) (rs = 0.22-0.62; ps < .001). In addition, principal components analysis revealed a two-factor solution (evidenced by a scree plot and eigenvalues >1) grouping the five questions asking about ultra-processed food consumption in one factor (eigenvalue = 3.21, 35.62% of variance explained) and the two questions about minimally processed food consumption and two questions about physical activity into a second factor (eigenvalue = 2.46, 27.27% of variance explained). However, given the theoretical differences between assessing changes in minimally processed food intake and physical activity, we retained the three categories for analyses. Average scores were created for these three categories for both time points and for the calculated change scores.
Visual analog scales ranging from −100 to 100 were created to assess whether participants felt the COVID-19 pandemic made it more difficult (−100) or easier (100) to engage in healthy eating and physical activity, as well as how they currently felt about the way they were eating (−100 = extremely upset; 0 = not at all upset; 100 = extremely pleased). Finally, participants answered on a visual analog scale how much they believed the circumstances of the COVID-19 pandemic contributed to their current eating habits (0 = not at all; 100 = extremely significantly).
2.3.3. Demographics and BMI
Demographics and height and current weight (used to calculate BMI) were self-reported. Participants were asked about their current weight and how recently they weighed themselves; 15.3% had taken their weight on the day of completing the survey, 44.4% within the last week, 22.6% within the last month, 8.3% in last 1–3 months, and only 9.4% had not taken their weight in >3 months. This was compared to participants’ retrospectively reported change in their weight since the start of the COVID-19 stay-at-home orders in March 2020, and 83.5% of individuals reported that they had confirmed this weight change using a scale.
2.4. Data analytic plan
The data analytic plan was pre-specified based on the aforementioned a priori hypotheses. All variables were checked to meet the assumptions of normality and linearity, and no outliers were found or excluded from the analyses. The first aim of the study was to provide descriptive information related to changes in eating behavior and physical activity attributed to the COVID-19 pandemic and compare these outcomes among individuals with versus without “food addiction” (using the “diagnostic” scoring method on the mYFAS 2.0). Frequencies and descriptive statistics were explored for the variables on the COVID-19 eating and activity questionnaire, and one-way analysis of variance (ANOVA) or chi-squared tests were conducted to investigate significant differences in group means for participants with versus without food addiction.
The second aim of the study was to assess whether mYFAS 2.0 food addiction was associated with weight change since the beginning of the COVID-19 pandemic in March 2020 (about one year prior to the time of this survey), changes in eating behavior and physical activity patterns since the COVID-19 pandemic began, and attributions of eating and activity behavior to the circumstances of COVID-19. Stepwise linear regression models were employed to examine these associations. One-way ANOVA and chi-square analyses were first conducted to assess whether covariates needed to be controlled for in the linear regression models. Food addiction was found to be significantly associated with BMI (F(1, 286) = 20.87, p < .001) and age (F(1, 286) = 7.22, p < .01) but not with other demographic variables (race, gender, education, income; geographic region; ps > .27). Thus, BMI and age were entered as control variables in each linear regression model, and mYFAS 2.0 food addiction and its interactions with BMI and age were entered as independent variables in each model. Significant interactions were followed up by examining correlations for individuals with versus without food addiction.
Given the differences related to restrictions of work and public places due to the COVID-19 pandemic by geographic region in the United States, one-way ANOVA was used to examine significant associations between geographic region with all of the dependent variables of interest. The only significant relationship with geographic region was with the degree to which participants attributed their current eating behavior to the COVID-19 pandemic (F(3,284) = 2.70; p < .05), with individuals in the Southern region reporting a significantly lower attribution compared to those in the Northeast region (M = 50.35, SD = 31.06; M = 61.76; SD = 23.33, respectively); all other associations between geographic region and the dependent variables were insignificant (ps > .14). For sensitivity, the linear regression model specifying the attribution of current eating behavior to the circumstances of COVID-19 was tested with geographical region specified as a control variable in the model. The findings with the independent variables of interest did not change and thus the original model with only BMI and age specified as control demographic variables was reported. Correction for multiple comparisons were not used given the exploratory nature of the survey.
3. Results
3.1. Participant characteristics
For the 288 participants included in the analyses, 54.5% identified as female (n = 157), 44.1% as male (n = 127), and 1.4% preferred not to identify their gender (n = 4). Participants varied in age from 18 to 78 years old (M = 42.36, SD = 13.08). Self-reported racial identification was: 80.9% white or Caucasian (n = 233), 6.9% black or African American (n = 20), 6.6% East Asian or Asian American (n = 19), 3.1% multiracial (n = 9), and 2.4% South Asian or Indian American (n = 7). Education level ranged from “less than high school” to “doctorate degree or equivalent,” with the median education level falling withing “bachelor's degree,” and annual household income ranged from “less than $10,000” to “$500,000+,” with the median annual household income falling within “$50,001–75,000.” Participants geographic distribution in the United States was: 38.9% lived in the Southern region (n = 112), 23.6% lived in the Northeast region (n = 68), 22.2% lived in the Midwest region (n = 64), and 15.3% lived in the Western region (n = 44).
Participants’ BMI ranged from 16.04 to 56.24 kg/m2 (M = 26.61, SD = 6.74), and weight class distribution was as follows: 2.4% had underweight (BMI<18.5 kg/m2), 46.2% had normal weight (BMI = 18.5–24.9 kg/m2), 29.2% had overweight (BMI = 25.0–29.9 kg/m2), and 22.2% had obesity (BMI>30.0 kg/m2). The number of mYFAS 2.0 symptoms endorsed ranged from 0 to 11 (M = 1.77, SD = 3.10), and the “diagnostic” threshold for food addiction was met by 15.6% of participants (n = 45), similar to prior research in online community samples (Schulte & Gearhardt, 2017, 2018). Among these individuals, “diagnostic” severity criteria were: 15.5% mild (2–3 symptoms plus impairment/distress), 6.7% moderate (4–5 symptoms plus impairment/distress), 77.8% severe (6–11 symptoms plus impairment/distress), paralleling prior rates for overall prevalence and severity criteria (Gearhardt, Corbin, & Brownell, 2016; Schulte & Gearhardt, 2017, 2018).
3.2. Descriptive overview of weight change since the start of the COVID-19 pandemic
Across all participants, 59.0% (n = 170) reported that their weight changed since the beginning of the COVID-19 pandemic in March 2020, 35.8% (n = 103) reported no weight change, and 5.2% (n = 15) did not know if their weight had changed. Of the 170 individuals reporting weight change, 75.9% reported gaining weight (n = 129) and 24.1% reported losing weight (n = 41). Further, including both individuals reporting weight change and those reporting no weight change (coded as 0) (n = 273), weight change ranged from −60 lb to +50 lb (M = 3.84, SD = 12.72) (−27.22 kg to +22.68 kg; M = 1.74, SD = 5.77). Including only those who gained weight (n = 129), weight gain ranged from 2 to 50 lb (M = 12.53 lb, SD = 9.58) (0.91–22.68 kg; M = 5.86 kg, SD = 4.35). Table 1 details the reported differences in frequencies of weight change and the factors to which participants attributed weight change by food addiction status.
Table 1.
Weight and lifestyle changes since the start of the COVID-19 pandemic by food addiction status.
| Participants w/Food Addiction (n = 45) % (n) or M (SD) |
Participants w/o Food Addiction (n = 243) % (n) or M (SD) |
Sig. (p) | |
|---|---|---|---|
| Age | 37.60 (11.42) | 43.24 (13.19) | .008** |
| BMI (at time of survey; kg/m2) | 30.69 (8.25) | 25.85 (6.16) | <.001** |
| Weight Change Since COVID-19 Began? | Yes: 91.1 (41) No: 8.9 (4) |
Yes: 53.1 (129) No: 40.7 (99) Don't Know: 6.2 (15) |
<.001** |
| Weight Gain or Loss? | Gain: 80.0 (36) | Gain: 38.3 (93) | .04* |
| Lost: 11.1 (5) | Lost: 14.8 (36) | ||
| No change: 8.9 (4) | No change: 46.9 (114) | ||
| Weight Change in Kg | 5.63 (7.15), ranging from −11.34 to 22.68 | .97 (5.13), ranging from −27.22 to 18.14 | <.001** |
| Median (Interquartile Range) | Median (Interquartile Range) | ||
| 4.54 (6.80) | 0.0 (3.63) | ||
| Variables Attributed to Weight Change (reporting %(n) who endorsed): | |||
| Changes in amount of junk food Eaten |
68.9 (31) | 35.4 (86) | <.001** |
| Changes in amount of fruits and vegetables eaten | 24.4 (11) | 12.8 (31) | .04* |
| Illness or hospitalizations | 11.1 (5) | 3.3 (8) | .02* |
| Changes in the smell or taste of Food | 15.6 (7) | 2.5 (6) | <.001** |
| Changes in level of physical Activity |
62.2 (28) | 37.0 (90) | .002** |
| Joined a weight control program | 6.7 (3) | 0.8 (2) | .01* |
| Changes in number of meals eaten each day | 22.2 (10) | 14.4 (35) | .19 |
| Changes in ability to get groceries | 22.2 (10) | 4.5 (11) | <.001** |
| Changes in frequency of eating Alone |
15.6 (7) | 4.5 (11) | .01* |
| Changes in amount of money to buy food | 13.3 (6) | 4.1 (10) | .01* |
Note: *p < .05; **p < .01.
3.3. Associations of food addiction symptoms with outcomes since the start of COVID-19
3.3.1. Weight change
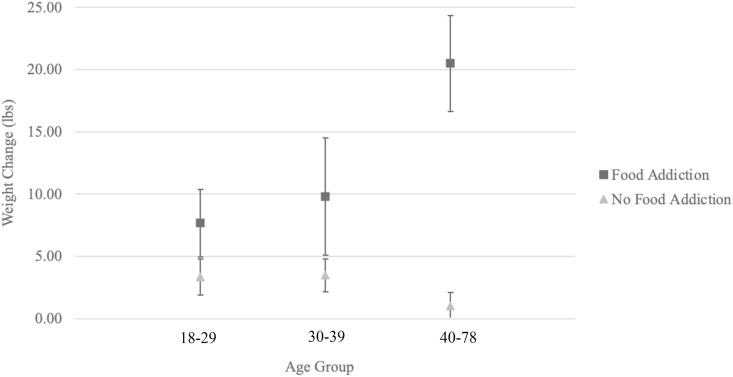
mYFAS 2.0 food addiction (B = 9.28, t = 4.97, p < .001), higher BMI (B = 0.48, t = 3.85, p < .001), and the interaction between mYFAS 2.0 food addiction and age (B = 0.51, t = 3.13, p = .001) were significantly associated with the reported weight gained or lost since the beginning of the COVID-19 pandemic in March 2020. Among individuals with mYFAS 2.0 food addiction, age was positively associated with greater weight gain (r = 0.30, p = .04), whereas no significant association was observed for those without food addiction (r = −0.08, p = .24) (see Fig. 1 ).
Fig. 1.
Interaction of food addiction and age on weight change. Note: Age was analyzed as a continuous variable in the dataset but divided into categories to illustrate the interaction. Categories were created to have roughly equal sample size based on the 45 individuals with food addiction, given the overall more conservative sample size for this group (ages 18–29: n = 15; ages 30–39: n = 16; ages 40–78: n = 14).
3.3.2. Eating and activity behaviors before COVID-19
mYFAS 2.0 food addiction (B = 1.08, t = 5.71, p < .001), higher BMI (B = 0.03, t = 3.03, p = .003), younger age (B = −0.01, t = −2.38, p = .02), and the interaction between mYFAS 2.0 food addiction and BMI (B = −0.06, t = −2.81, p = .005) were significantly associated with higher consumption of ultra-processed foods before the COVID-19 pandemic began. For individuals with mYFAS 2.0 food addiction, higher BMI and greater intake of ultra-processed foods was not significantly correlated (r = −0.16, p = .29), though a significant positive correlation was observed among those without food addiction (r = 0.20, p = .002). Lower BMI (B = −0.05, t = −3.67, p < .001) and older age (B = 0.01, t = 2.05, p = .04) were significantly associated with higher minimally processed food consumption. Only lower BMI was significantly related to higher physical activity (B = −0.04, t = −2.91, p = .004).
3.3.3. Eating and activity behaviors during most difficult period since the start of COVID-19
mYFAS food addiction (B = 1.18, t = 6.42, p < .001), elevated BMI (B = 0.06, t = 5.69, p < .001), younger age (B = −0.02, t = −3.33, p = .001), and the interaction between mYFAS 2.0 food addiction and BMI (B = −0.06, t = −2.78, p = .01) were significantly associated with higher ultra-processed food consumption during the time period since the start of the COVID-19 pandemic that participants identified as being the most difficult to maintain healthy eating and physical activity. For individuals with mYFAS 2.0 food addiction, BMI and intake of ultra-processed foods were not correlated (r = 0.01, p = .96), though a positive correlation was observed among those without food addiction (r = 0.34, p < .001). Lower BMI (B = −0.05, t = −3.43, p = .001) and older age (B = 0.02, t = 3.46, p = .001) were significantly related to higher minimally processed food consumption. Lower BMI (B = −0.04, t = −2.53, p = .01) and the interaction between mYFAS 2.0 food addiction and BMI (B = −0.08, t = −2.69, p = .01) were significantly associated with physical activity. For individuals with mYFAS 2.0 food addiction, BMI and physical activity were negatively correlated (r = −0.52, p < .001), and this association was also observed to a lesser degree for those without food addiction (r = −0.16, p = .01).
3.3.4. Changes from most difficult period compared to before COVID-19
Elevated BMI (B = 0.03, t = 2.85, p = .01) was significantly associated with an increase in ultra-processed food consumption from the most difficult period compared to before the COVID-19 pandemic began. Older age (B = 0.01, t = 2.07, p = .04) and the interaction between mYFAS 2.0 food addiction and BMI (B = −0.05, t = −2.30, p = .02) was related to an increase in minimally processed food consumption. Among those with mYFAS 2.0 food addiction, a trend-level negative association was observed between BMI and changes in minimally processed food consumption (r = −0.28, p = .06) and no association was observed for those without food addiction (r = 0.01, p = .84). Only the interaction between mYFAS 2.0 food addiction symptoms and BMI was associated with physical activity (B = −0.06, t = −2.43, p = .02). However, for individuals with and without mYFAS 2.0 food addiction, age and change in physical activity were not significantly correlated (r = 0.01, p = .96 and r = 0.05, p = .48, respectively).
3.4. Attributions of COVID-19 circumstances to eating and activity behavior
mYFAS 2.0 food addiction was the only variable associated with the extent to which participants attributed their current eating behavior to the circumstances of the COVID-19 pandemic (B = 23.19, t = 4.62, p < .001). BMI (B = −1.43, t = −2.79, p = .01) and the interaction between mYFAS 2.0 food addiction and age (B = −0.2.27, t = −3.29, p = .001) was significantly related to whether participants endorsed that the COVID-19 pandemic made it more difficult to eat healthy (negative values correspond to greater difficulty). For individuals with mYFAS 2.0 food addiction, older age was correlated with greater endorsement that COVID-19 negatively impacted their ability to eat healthy (r = −0.39, p = .01), and no association was observed for those without food addiction (r = 0.04, p = .52). Higher BMI (B = −1.63, t = −2.87, p = .004) and the interaction between mYFAS 2.0 food addiction and age (B = −2.02, t = −2.64, p = .01) were also significantly associated with whether participants reported that the circumstances of the COVID-19 pandemic made it more difficult to be physically active (negative values correspond to greater difficulty). For individuals with mYFAS 2.0 food addiction, older age was correlated with greater endorsement that the COVID-19 circumstances negatively impacted their ability to be physically active (r = −0.35, p = .02), and no association was observed for those without food addiction (r = −0.01. p = .93). Lastly, mYFAS 2.0 food addiction (B = −22.12, t = −2.50, p = .01), higher BMI (B = −2.53, t = −5.16, p < .001), and the interaction between mYFAS 2.0 food addiction and age (B = −0.2.13, t = −3.23, p = .001) were significantly related to whether an individual reported greater distress about their current eating behavior (negative values correspond to greater distress). Among individuals with mYFAS 2.0 food addiction, older age was correlated with greater distress about eating behavior (r = −0.32, p = .03), and no association was observed for those without food addiction (r = 0.06, p = .33).
4. Discussion
4.1. Weight change since the onset of COVID-19
Fifty-nine percent of all participants endorsed weight change since the beginning of the COVID-19 pandemic in March 2020, and, of these individuals, 75.9% reported weight gain. While this parallels the variability in weight change observed by prior studies conducted during COVID-19 (Chopra et al., 2020; Keel et al., 2020; Kriaucioniene et al., 2020; Lamarche et al., 2021; Marchitelli et al., 2020; Mason et al., 2021; Pellegrini et al., 2020; Scarmozzino & Visioli, 2020; Zachary et al., 2020), the incidences of reported weight change and weight gain are higher. Given that the majority of these prior studies were conducted between April and July 2020, the higher rates of reported weight gain in the present sample may be attributed to the data collection occurring 6–9 months later. Thus, it may be that the risk and extent of weight gain during the COVID-19 pandemic has increased over time.
4.1.1. Associations with food addiction
A clearer picture of elevated risk for weight gain emerged for individuals with food addiction, who were not only significantly more likely to report weight gain since the start of the COVID-19 pandemic but strikingly endorsed gaining approximately six times more weight than participants without food addiction (an average of 12.42 lb/5.63 kg versus 2.14 lb/.97 kg, respectively). Individuals with food addiction were also significantly more likely to attribute weight gain to greater consumption of ultra-processed foods and decreased intake of minimally processed foods, which parallels prior findings demonstrating that ultra-processed foods are most implicated in addictive-like eating behavior (Curtis & Davis, 2014; Pursey et al., 2015; Schulte et al., 2015). Further, individuals with food addiction were significantly more likely to attribute changes in weight to changes in physical activity, ability to get groceries, frequency of eating alone, financial resources to buy food, changes in the smell or taste or food, joining a weight control program, and illness or hospitalization. Broadly, this suggest that persons with food addiction exhibited a greater disruption to many factors associated with healthy eating and physical activity that related to weight change. Notably, food addiction was associated with greater weight gain beyond the significant effect of BMI, which underscores the unique clinical utility of the food addiction phenotype for delineating groups at elevated risk for weight management difficulties.
Among persons with food addiction, a positive relationship was observed between age and weight gain. Interestingly, while participants with food addiction had a significantly younger age compared to those without food addiction, consistent with prior research (Schulte & Gearhardt, 2017, 2018), those with food addiction who were older (>sample mean of 37.60) reported greater weight gain. Researchers have suggested that older individuals may have experienced greater disruption related to COVID-19 due to having a wider array of responsibilities that could have been impacted, such as potential for changes in professional obligations, employment status, financial strain, social isolation, managing children or grandchildren at home, intimate relationships, and many more (Brooke & Jackson, 2020). Thus, among older participants with food addiction, the circumstantial changes and stress of COVID-19 may have exacerbated ultra-processed food consumption in a manner that contributed to elevated weight gain. Given that prior research assessing trends in mental health outcomes since the beginning of COVID-19 by age group have been mixed (Bruine de Bruin, 2021; Krendl & Perry, 2021; Pieh, Budimir, & Probst, 2020; van Tilburg, Steinmetz, Stolte, van der Roest, & de Vries, 2020), replication of the present findings is needed. However, these preliminary data suggest that screening adults for food addiction may be beneficial for identifying those who may need additional support with weight management and intervention for clinically significant problematic eating behavior as the COVID-19 pandemic persists.
4.2. Individual differences in eating and activity behaviors before and during COVID-19
4.2.1. Before COVID-19
Considering participants’ typical eating and activity patterns in the 6 months before the beginning of the COVID-19 pandemic in March 2020 (September 2019 to February 2020), food addiction was associated with higher consumption of ultra-processed foods while controlling for the effect of BMI. A significant interaction emerged between food addiction and BMI, with higher ultra-processed food intake only being positively related to elevated BMI for individuals without food addiction. In other words, persons with food addiction reported consuming elevated quantities of ultra-processed foods regardless of their current BMI, suggesting that food addiction may be more associated with ultra-processed food intake beyond the effects of current weight status (which, for many individuals with food addiction, was reflective of recent weight gain). These data also expand upon prior findings to once again posit that ultra-processed foods seem to be more associated with behavioral indicators of addictive-like eating behavior measured by the mYFAS 2.0, whereas minimally processed foods have demonstrated little association (Curtis & Davis, 2014; Pursey et al., 2015; Schulte et al., 2015).
Higher BMI and younger age were both also independently associated with higher ultra-processed and lower minimally processed food consumption during as compared to before the pandemic, and higher BMI was related to less engagement in physical activity, suggesting that these demographic variables may be related to a broader array of potentially obesogenic lifestyle behaviors generally, but additionally, these individuals with higher BMI at the time of the survey may have had greater fears about going out to shop or exercise given the increased risk of severe disease with higher BMI (Gallo Marin et al., 2021; Zhang et al., 2021). Mechanisms that may be shared among individuals with obesity and youths (e.g., impulsivity (Pivarunas & Conner, 2015; Steinberg et al., 2008) may similarly contribute to this reported reduced engagement in healthy lifestyle behaviors.
4.2.2. During COVID-19
When participants were asked to think about their eating and activity habits during a time period they identified as the most difficult for maintain a healthy lifestyle since COVID-19 began (from March 2020 to the time of data collection in February 2021), nearly identical patterns were observed as the models assessing typical behaviors before COVID-19. The only discrepancy was the significant interaction between food addiction and BMI with physical activity. Among participants with food addiction, higher BMI at the time of the survey was strongly associated with less physical activity during the time period each participant identified as most difficult for adhering to a healthy lifestyle since the start of COVID-19. No prior studies have yet investigated factors that positively or negatively influence physical activity engagement among individuals with food addiction, and the present findings highlight the need for future empirical investigation.
One possible explanation for the observed interaction between food addiction and BMI on physical activity may be that the increased stress associated with COVID-19 reduced self-efficacy particularly among individuals with food addiction and a higher body weight. Self-efficacy, defined as the belief that one can successfully complete an intended behavior, has been identified as a key psychosocial determinant for whether an individual exercises (Bauman et al., 2012). Prior studies have demonstrated reduced self-efficacy for health behaviors among persons with obesity and binge eating disorders (Cargill, Clark, Pera, Niaura, & Abrams, 1999; Richman, Loughnan, Droulers, Steinbeck, & Caterson, 2001), which has been attributed to a diminished belief that one's efforts would translate to meaningful weight or lifestyle changes. Individuals with food addiction and a higher BMI at the time of the survey may have particularly elevated susceptibility for experiencing decreases in self-efficacy during COVID-19, as the associated stress and/or circumstantial changes may have reduced confidence in their ability to regularly engage in physical activity. Given that the higher BMI at the time of the survey was reflective of weight gain for many individuals with food addiction, the potential relationship between BMI and diminished self-efficacy may have intensified over time to contribute to decreased engagement in physical activity. Thus, evidence-based interventions enhancing self-efficacy towards exercise among those with obesity [e.g., (Buckley, 2016; Middelkamp, van Rooijen, Wolfhagen, & Steenbergen, 2017)] may warrant consideration for those with a higher body weight and food addiction.
4.2.3. Changes since the start of COVID-19
Interestingly, food addiction was not associated with significant changes in eating or activity when comparing typical patterns before the beginning of COVID-19 to the period of time each participant identified as most difficult to stick to a healthy lifestyle during COVID-19. This is likely because of the significantly higher reported pre-morbid frequency of ultra-processed food consumption among these individuals or a reporting bias where higher pre-morbid reports were influenced by experiencing greater distress associated with ultra-processed food consumption, which is characteristic of persons with food addiction. Thus, the potential for assessing changes among participants with food addiction may have been diminished. In contrast, elevated BMI was related to greater ultra-processed food consumption. Taken together, this may suggest that individuals with higher BMIs at the time of the survey may have experienced a worsening in their dietary habits since the start of COVID-19, whereas individuals with food addiction may have been exhibiting greater rates of problematic eating behaviors all along or were less able to differentiate between their behavior typically versus the most difficult time period since the beginning of COVID-19.
4.3. Attributions of eating and activity behaviors to COVID-19
Despite no reported increases to ultra-processed food consumption when comparing typical eating patterns before COVID-19 to the most difficult time period since COVID-19 began in March 2020, food addiction (but not BMI) was uniquely associated with greater endorsement that one's current eating behaviors could be attributed to the circumstances of COVID-19. This attribution may also allude to reduced self-efficacy among these participants due to COVID-19, as the perceived barriers caused by the circumstances may have been intensely overwhelming and reduced individuals' confidence in their ability to manage their weight and addictive-like eating behavior during this time, which in turn translated to diminished engagement in healthy lifestyle behaviors.
Persons with food addiction, especially those who were older, also reported greater emotional distress about their current eating behavior, which extends findings from a prior study of Italian adults that observed an association between food addiction symptoms and general levels of psychological distress (Panno et al., 2020). Individuals with food addiction who were older also had higher endorsements that COVID-19 directly and negatively impacted their ability to eat healthy and be physically active. Thus, persons with food addiction, especially those who were older, appear to emerge as a risk group for greater distress and perceived attributions of COVID-19 negatively impacting their lifestyle, which is particularly concerning when coupled with the elevated weight gain reported by this group. The present findings again suggest that these individuals may warrant clinical attention during the remainder and aftermath of the pandemic.
Finally, BMI at the time of the survey was also independently related to elevated distress and greater endorsements that COVID-19 made it more difficult to adhere to healthy eating and activity behaviors. While food addiction appears to represent a unique clinical risk group, individuals with a higher body weight, which likely reflects, in part, those who gained weight since the start of COVID-19, also reported greater perceived psychological distress and difficulty engaging in healthy eating and activity behaviors due to COVID-19. Thus, these persons also deserve attention when assessing and treating the physical and mental health consequences of COVID-19.
4.4. Limitations
This research had several limitations that should be considered in future research. Most notably, the present approach was cross-sectional and all data were collected based on retrospective reports. This likely resulted in the diminished accuracy of participants’ reported weight changes and reflections on eating and activity behaviors for the two time periods (before and during COVID-19). In addition, a differential reporting bias may have existed for individuals with versus without food addiction. In order to screen positive for food addiction on the mYFAS 2.0, an individual must have reported having clinically significant impairment or distress related to his or her eating behavior. Thus, this elevated impairment/distress may have created a more salient bias in reporting negative changes to weight, eating, and physical activity. Another way that the retrospective nature of this approach may have influenced the findings is that the mYFAS 2.0 asks participants to report on their addictive-like eating behavior since the start of COVID-19 stay-at-home orders (from March 2020 until the time of survey in February 2021). While the YFAS has been found to be a stable tool to assess the trait of food addiction over time (Pursey, Collins, Stanwell, & Burrows, 2016), but it is plausible that some of the participants may have developed food addiction between March 2020 to February 2021, perhaps related to the stressful circumstances of the COVID-19 pandemic. Ongoing longitudinal studies with measurements of weight, eating behavior, and food addiction collected before the onset of the COVID-19 pandemic in March 2020 would be equipped to assess more rigorous prospective associations.
While one strength of the current study was the inclusion of adults across the United States, it is acknowledged that another limitation is that individual states adhered to different timelines and restrictions associated with COVID-19 stay-at-home orders. Though statistically controlling for geographic region did not impact the observed associations, the variation in circumstances by state does not permit generalized conclusions about which facets of the COVID-19 pandemic influenced the findings (e.g., social isolation, spending more time at home, restaurant closures). Future studies may consider using qualitative approaches to better understand each participant's unique experience in a manner that may better account for state-by-state variability. Further, there may have been individual variability in the duration of the time period that participants reported they struggled most with healthy eating and physical activity since March 2020, which may be helpful to assess in future studies, and subjectivity in how this phrase was interpreted. Relatedly, the present approach assessed changes from typical behavior compared to the most difficult period, which may limit conclusions related to positive changes in healthy eating and activity observed in prior studies of general population samples (e.g., Deschasaux-Tanguy et al., 2021). Another limitation was that the BMI covariate used in the analyses was calculated based on the participants' height and weight at the time of the survey, and thus was expected to be associated with weight gain. The findings are interpreted with nuance of this methodological approach, but future work may consider including variables for BMI both before and during the time periods of interest. Lastly, the category of “takeout” was highly correlated with the other categories of ultra-processed foods (p < .001), but may have incidentally captured some forms of takeout that may not have been considered ultra-processed (e.g., takeout from a salad restaurant). Future studies should define takeout for specifically to ensure that participants only report on ultra-processed foods.
4.5. Conclusions
Individuals who met the mYFAS 2.0 “diagnostic” threshold score for food addiction, versus those who did not, had significantly higher weight gain, greater reported consumption of ultra-processed foods both before and during the COVID-19 pandemic, greater endorsement of attributing their eating behavior to the circumstances of COVID-19, and higher distress about their current eating behaviors. Further, those with food addiction who were older appeared to be at particularly elevated risk for weight gain and psychological distress. While BMI was associated with poorer engagement in several healthy eating and activity behaviors, food addiction emerged a construct with unique utility for identifying individuals who may benefit from clinical support in managing the physical and psychological consequences of the COVID-19 pandemic.
Author contributions
All authors contributed to study development and writing the manuscript. E.S. collected and analyzed the data. All authors have reviewed and approved the final article.
Ethical statement
This research was performed in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board at the University of Pennsylvania (protocol #844818). All individuals provided written informed consent for their participation electronically.
References
- Almandoz J.P., Xie L., Schellinger J.N., Mathew M.S., Gazda C., Ofori A., et al. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin. Obes. 2020;10(5) doi: 10.1111/cob.12386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . American Psychiatric Publishing; Arlington: 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- Bauman A.E., Reis R.S., Sallis J.F., Wells J.C., Loos R.J., Martin B.W., Lancet Physical Activity Series Working, Group Correlates of physical activity: Why are some people physically active and others not? Lancet. 2012;380(9838):258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- Brooke J., Jackson D. Older people and COVID-19: Isolation, risk and ageism. Journal of Clinical Nursing. 2020;29(13–14):2044–2046. doi: 10.1111/jocn.15274. [DOI] [PubMed] [Google Scholar]
- Bruine de Bruin W. Age differences in COVID-19 risk perceptions and mental health: Evidence from a national U.S. survey conducted in March 2020. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2021;76(2):e24–e29. doi: 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley J. Exercise self-efficacy intervention in overweight and obese women. Journal of Health Psychology. 2016;21(6):1074–1084. doi: 10.1177/1359105314545096. [DOI] [PubMed] [Google Scholar]
- Cargill B.R., Clark M.M., Pera V., Niaura R.S., Abrams D.B. Binge eating, body image, depression, and self-efficacy in an obese clinical population. Obesity Research. 1999;7(4):379–386. doi: 10.1002/j.1550-8528.1999.tb00421.x. [DOI] [PubMed] [Google Scholar]
- Carroll N., Sadowski A., Laila A., Hruska V., Nixon M., Ma D.W.L., et al. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020;12(8):2352. doi: 10.3390/nu12082352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopra S., Ranjan P., Singh V., Kumar S., Arora M., Hasan M.S., et al. Impact of COVID-19 on lifestyle-related behaviours- A cross-sectional audit of responses from nine hundred and ninety-five participants from India. Diabetes and Metabolic Syndrome. 2020;14(6):2021–2030. doi: 10.1016/j.dsx.2020.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings J.R., Ackerman J.M., Wolfson J.A., Gearhardt A.N. COVID-19 stress and eating and drinking behaviors in the United States during the early stages of the pandemic. Appetite. 2021;162:105163. doi: 10.1016/j.appet.2021.105163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis C., Davis C. A qualitative study of binge eating and obesity from an addiction perspective. Eating Disorders. 2014;22(1):19–32. doi: 10.1080/10640266.2014.857515. [DOI] [PubMed] [Google Scholar]
- Davis C., Loxton N.J., Levitan R.D., Kaplan A.S., Carter J.C., Kennedy J.L. Food addiction' and its association with a dopaminergic multilocus genetic profile. Physiology & Behavior. 2013;118:63–69. doi: 10.1016/j.physbeh.2013.05.014. [DOI] [PubMed] [Google Scholar]
- Deschasaux-Tanguy M., Druesne-Pecollo N., Esseddik Y., de Edelenyi F.S., Allès B., Andreeva V.A., et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March–May 2020): Results from the French NutriNet-Santé cohort study. American Journal of Clinical Nutrition. 2021;113(4):924–938. doi: 10.1093/ajcn/nqaa336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Rio J., Cecchini J.A., Mendez-Gimenez A., Carriedo A. Weight changes during the COVID-19 home confinement. Effects on psychosocial variables. Obesity Research & Clinical Practice. 2020;14(4):383–385. doi: 10.1016/j.orcp.2020.07.006. [DOI] [PubMed] [Google Scholar]
- Gallo Marin B., Aghagoli G., Lavine K., Yang L., Siff E.J., Chiang S.S., et al. Predictors of COVID-19 severity: A literature review. Reviews in Medical Virology. 2021;31(1):1–10. doi: 10.1002/rmv.2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gearhardt A.N., Corbin W.R., Brownell K.D. Food addiction: An examination of the diagnostic criteria for dependence. Journal of Addiction Medicine. 2009;3(1):1–7. doi: 10.1097/ADM.0b013e318193c993. [DOI] [PubMed] [Google Scholar]
- Gearhardt A.N., Corbin W.R., Brownell K.D. Preliminary validation of the Yale food addiction scale. Appetite. 2009;52(2):430–436. doi: 10.1016/j.appet.2008.12.003. [DOI] [PubMed] [Google Scholar]
- Gearhardt A.N., Corbin W.R., Brownell K.D. Development of the Yale food addiction scale version 2.0. Psychology of Addictive Behaviors. 2016;30(1):113–121. doi: 10.1037/adb0000136. [DOI] [PubMed] [Google Scholar]
- Gearhardt A.N., Davis C., Kuschner R., Brownell K.D. The addiction potential of hyperpalatable foods. Current Drug Abuse Reviews. 2011;4(3):140–145. doi: 10.2174/1874473711104030140. [DOI] [PubMed] [Google Scholar]
- Hardee J.E., Phaneuf C., Cope L., Zucker R., Gearhardt A., Heitzeg M. Neural correlates of inhibitory control in youth with symptoms of food addiction. Appetite. 2020;148:104578. doi: 10.1016/j.appet.2019.104578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy R., Fani N., Jovanovic T., Michopoulos V. Food addiction and substance addiction in women: Common clinical characteristics. Appetite. 2018;120:367–373. doi: 10.1016/j.appet.2017.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyner M.A., Schulte E.M., Wilt A.R., Gearhardt A.N. Addictive-like eating mediates the association between eating motivations and elevated body mass index. Translational Issues in Psychological Science. 2015;1(3):217. [Google Scholar]
- Keel P.K., Gomez M.M., Harris L., Kennedy G.A., Ribeiro J., Joiner T.E. Gaining “The Quarantine 15:” Perceived versus observed weight changes in college students in the wake of COVID‐19. International Journal of Eating Disorders. 2020:1–8. doi: 10.1002/eat.23375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krendl A.C., Perry B.L. The impact of sheltering in place during the COVID-19 Pandemic on older adults' social and mental well-being. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2021;76(2):e53–e58. doi: 10.1093/geronb/gbaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriaucioniene V., Bagdonaviciene L., Rodriguez-Perez C., Petkeviciene J. Associations between changes in health behaviours and body weight during the COVID-19 quarantine in Lithuania: The Lithuanian COVIDiet Study. Nutrients. 2020;12(10) doi: 10.3390/nu12103119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok S., Adam S., Ho J.H., Iqbal Z., Turkington P., Razvi S., et al. Obesity: A critical risk factor in the COVID-19 pandemic. Clinical Obesity. 2020;10(6) doi: 10.1111/cob.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamarche B., Brassard D., Lapointe A., Laramée C., Kearney M., Côté M., et al. Changes in diet quality and food security among adults during the COVID-19–related early lockdown: Results from NutriQuébec. American Journal of Clinical Nutrition. 2021;113(4):984–992. doi: 10.1093/ajcn/nqaa363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littman A.J., Boyko E.J., McDonell M.B., Fihn S.D. Evaluation of a weight management program for veterans. Preventing Chronic Disease. 2012;9:E99. doi: 10.5888/pcd9.110267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Bueno R., López-Sánchez G.F., Casajús J.A., Calatayud J., Gil-Salmerón A., Grabovac I.…Smith L. Health-related behaviors among school-aged children and adolescents during the Spanish COVID-19 confinement. Frontiers in Pediatrics. 2020;8:573. doi: 10.3389/fped.2020.00573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchitelli S., Mazza C., Lenzi A., Ricci E., Gnessi L., Roma P. Weight gain in a sample of patients affected by overweight/obesity with and without a psychiatric diagnosis during the COVID-19 lockdown. Nutrients. 2020;12(11) doi: 10.3390/nu12113525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason T.B., Barrington-Trimis J., Leventhal A.M. Eating to cope with the COVID-19 pandemic and body weight change in young adults. Journal of Adolescent Health. 2021;68(2):277–283. doi: 10.1016/j.jadohealth.2020.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maugeri G., Castrogiovanni P., Battaglia G., Pippi R., D'Agata V., Palma A., et al. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon. 2020;6(6) doi: 10.1016/j.heliyon.2020.e04315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middelkamp J., van Rooijen M., Wolfhagen P., Steenbergen B. The effects of a self-efficacy intervention on exercise behavior of fitness club members in 52 weeks and long-term relationships of transtheoretical model constructs. Journal of Sports Science and Medicine. 2017;16(2):163–171. [PMC free article] [PubMed] [Google Scholar]
- Monteiro C.A., Cannon G., Levy R.B., Moubarac J., Louzada M.L.C., Rauber F., et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutrition. 2019;22(5):936–941. doi: 10.1017/S1368980018003762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreland A., Herlihy C., Tynan M.A., Sunshine G., McCord R.F., Hilton C., et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement—United States, March 1–May 31, 2020. Morbidity and Mortality Weekly Report. 2020;69(35):1198. doi: 10.15585/mmwr.mm6935a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy C.M., Stojek M.K., MacKillop J. Interrelationships among impulsive personality traits, food addiction, and body mass index. Appetite. 2014;73:45–50. doi: 10.1016/j.appet.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panno A., Carbone G.A., Massullo C., Farina B., Imperatori C. COVID-19 related distress is associated with alcohol problems, social media and food addiction symptoms: Insights from the Italian experience during the lockdown. Frontiers in Psychiatry. 2020;11:577135. doi: 10.3389/fpsyt.2020.577135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paolacci G., Chandler J. Inside the turk: Understanding mechanical turk as a participant pool. Current Directions in Psychological Science. 2014;23(3):184–188. [Google Scholar]
- Pellegrini M., Ponzo V., Rosato R., Scumaci E., Goitre I., Benso A., et al. Changes in weight and nutritional habits in adults with obesity during the “lockdown” period caused by the COVID-19 virus emergency. Nutrients. 2020;12(7):2016. doi: 10.3390/nu12072016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. Journal of Psychosomatic Research. 2020;136:110186. doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrobelli A., Pecoraro L., Ferruzzi A., Heo M., Faith M., Zoller T., et al. Effects of COVID‐19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study. Obesity. 2020;28(8):1382–1385. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pivarunas B., Conner B.T. Impulsivity and emotion dysregulation as predictors of food addiction. Eating Behaviors. 2015;19:9–14. doi: 10.1016/j.eatbeh.2015.06.007. [DOI] [PubMed] [Google Scholar]
- Poly T.N., Islam M.M., Yang H.C., Lin M.C., Jian W.S., Hsu M.H., et al. Obesity and mortality among patients diagnosed with COVID-19: A systematic review and meta-analysis. Frontiers of Medicine. 2021;8:620044. doi: 10.3389/fmed.2021.620044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pursey K.M., Collins C.E., Stanwell P., Burrows T.L. Foods and dietary profiles associated with 'food addiction' in young adults. Addictive Behavior Reports. 2015;2:41–48. doi: 10.1016/j.abrep.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pursey K.M., Collins C.E., Stanwell P., Burrows T.L. The stability of ‘food addiction’as assessed by the Yale Food Addiction Scale in a non-clinical population over 18-months. Appetite. 2016;96:533–538. doi: 10.1016/j.appet.2015.10.015. [DOI] [PubMed] [Google Scholar]
- Ravichandran S., Bhatt R.R., Pandit B., Osadchiy V., Alaverdyan A., Vora P., et al. Alterations in reward network functional connectivity are associated with increased food addiction in obese individuals. Scientific Reports. 2021;11(1):3386. doi: 10.1038/s41598-021-83116-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richman R.M., Loughnan G.T., Droulers A.M., Steinbeck K.S., Caterson I.D. Self-efficacy in relation to eating behaviour among obese and non-obese women. International Journal of Obesity and Related Metabolic Disorders. 2001;25(6):907–913. doi: 10.1038/sj.ijo.0801606. [DOI] [PubMed] [Google Scholar]
- Robinson E., Boyland E., Chisholm A., Harrold J., Maloney N.G., Marty L., et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite. 2020 doi: 10.1016/j.appet.2020.104853. 104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Gillespie S., Jones A. Weight-related lifestyle behaviours and the COVID-19 crisis: An online survey study of UK adults during social lockdown. Obesity Science & Practice. 2020;6(6):735–740. doi: 10.1002/osp4.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarmozzino F., Visioli F. COVID-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample. Foods. 2020;9(5) doi: 10.3390/foods9050675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte E.M., Avena N.M., Gearhardt A.N. Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS One. 2015;10(2) doi: 10.1371/journal.pone.0117959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte E.M., Gearhardt A.N. Development of the modified Yale food addiction scale version 2.0. European Eating Disorders Review. 2017;25(4):302–308. doi: 10.1002/erv.2515. [DOI] [PubMed] [Google Scholar]
- Schulte E.M., Gearhardt A.N. Associations of food addiction in a sample recruited to be nationally representative of the United States. European Eating Disorders Review. 2018;26(2):112–119. doi: 10.1002/erv.2575. [DOI] [PubMed] [Google Scholar]
- Schulte E.M., Grilo C.M., Gearhardt A.N. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clinical Psychology Review. 2016;44:125–139. doi: 10.1016/j.cpr.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte E.M., Smeal J.K., Gearhardt A.N. Foods are differentially associated with subjective effect report questions of abuse liability. PLoS One. 2017;12(8) doi: 10.1371/journal.pone.0184220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte E.M., Sonneville K.R., Gearhardt A.N. Subjective experiences of highly processed food consumption in individuals with food addiction. Psychology of Addictive Behaviors. 2019;33(2):144–153. doi: 10.1037/adb0000441. [DOI] [PubMed] [Google Scholar]
- Schulte E.M., Yokum S., Jahn A., Gearhardt A.N. Food cue reactivity in food addiction: A functional magnetic resonance imaging study. Physiology & Behavior. 2019;208:112574. doi: 10.1016/j.physbeh.2019.112574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L., Albert D., Cauffman E., Banich M., Graham S., Woolard J. Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: Evidence for a dual systems model. Developmental Psychology. 2008;44(6):1764–1778. doi: 10.1037/a0012955. [DOI] [PubMed] [Google Scholar]
- van Tilburg T.G., Steinmetz S., Stolte E., van der Roest H., de Vries D.H. Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2020 doi: 10.1093/geronb/gbaa111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderBroek-Stice L., Stojek M.K., Beach S.R.H., vanDellen M.R., MacKillop J. Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite. 2017;112:59–68. doi: 10.1016/j.appet.2017.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachary Z., Brianna F., Brianna L., Garrett P., Jade W., Alyssa D., et al. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obesity Research & Clinical Practice. 2020;14(3):210–216. doi: 10.1016/j.orcp.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Lewis A.M., Moley J.R., Brestoff J.R. A systematic review and meta-analysis of obesity and COVID-19 outcomes. Scientific Reports. 2021;11(1):7193. doi: 10.1038/s41598-021-86694-1. [DOI] [PMC free article] [PubMed] [Google Scholar]