Abstract
Background/Objectives:
Older adults are at high risk for adverse outcomes as they transition from hospital to home. Transitional care interventions primarily focus on care coordination and medication management and may miss key components. The objective of this study is to examine the current scope of hospital to home transitional care interventions that impact health-related outcomes and to examine other key components including engagement by older adults and their caregivers.
Design:
Scoping Review.
Methods:
Eligible articles focused on hospital transition to home intervention, measured primary outcomes post-hospitalization, used randomized controlled trial designs, and included primarily adults aged 60 and older. Articles included in this review were reviewed in full and all data were extracted that related to study objective, setting, population, sample, intervention, primary and secondary outcomes, and main results.
Results:
Five hundred sixty-seven records were identified by title. Forty-four articles were deemed eligible and included. Most common transitional care intervention components were care continuity and coordination, medication management, symptom recognition, and self-management. Few studies reported a focus on caregiver needs or goals. Common modes of intervention delivery included by phone, in person while the patient was hospitalized, and in person in the community following hospital discharge. The most common outcomes were readmission and mortality.
Conclusion:
To improve outcomes beyond healthcare utilization, a paradigm shift is required in the design and study of care transition interventions. Future interventions should explore methods or novel interventions for caregiver engagement; leverage an interdisciplinary team or care coordination hub with engagement from underrepresented specialties such as social work and occupational therapy; and examine opportunities for interventions designed specifically to address older adult and caregiver-reported needs and their well-being.
Keywords: transitional care, patient discharge, caregivers, patient readmission, continuity of patient care
Older adults are at high risk for adverse outcomes as they transition from hospital to home, including rehospitalization,1 loss of function,2–4 and death.4 As a result, numerous transitional care interventions have targeted this group. Many of these transitional care interventions contain similar components, primarily focusing on care coordination/continuity and medication management.5–8 These components have documented efficacy in reducing healthcare utilization, such as readmissions or hospitalizations.5–11 Although these are important aspects of improving older adults’ care transitions, they do not comprehensively address all suboptimal outcomes related to older adult transitions.
To address the range of suboptimal outcomes associated with older adults’ care transitions, we must address additional aspects documented as issues for older adults and their caregivers (unpaid, family members, or friends) during the transition. Additional aspects documented as challenges in prior research include function (e.g., older adults ability to complete self-care, social, and household activities), engagement (e.g., active participation in care and interventions), health and well-being, care planning, and education.2–4,11–14 Naylor et al. provide a framework for examining important components of transitional care (such as older adult and caregiver education, engagement, and well-being and continuity of care), but does not examine how existing interventions address these components.15 Another review summarizes certain aspects of the interventions, such as pre versus post-discharge contact, but focuses primarily on outcomes11 and examines only a few prominent transitional care interventions in-depth.16 Given the complex care needs of transitioning older adults, it is also important to examine the providers used as interventionists and use of interdisciplinary care teams.17
The purpose of this scoping review is to examine the current scope of hospital to home transitional care interventions, including their mechanisms and ability to mitigate a broad range of suboptimal outcomes. Information gleaned from this review can help guide future intervention work to improve outcomes for older adults transitioning from hospital to home.
Method
In this scoping review, we synthesized transitional care interventions for older adults transitioning from hospital to home. We selected a scoping review over other types of reviews because it best aligns with the objective of summarizing the quantity and characteristics of the literature by design and other key features,18 and we followed guidelines set forth for conducting systematic scoping reviews.19 Specially, we focused on peer-reviewed, randomized controlled trials (RCTs) to examine the current scope of hospital to home transitional care interventions that impact health-related outcomes and other key components including engagement by older adults and their caregivers.
Search strategy
We conducted the review from electronic literature searches of CINAHL, PubMed, and Scopus to identify peer-reviewed English (because the authors are English literate) original research studies published between January 2000 and February 2021. These dates were chosen to focus on most recent transitional care interventions, while including most prominent models developed in the early 2000s. We chose these databases to achieve a good representation of medical, health sciences, and social sciences literature. We used the following search terms: ((“Coordinated-Transitional Care” OR “continuity of care” OR “care transition” OR “care transitions” OR “hospital to home” OR “transitional care” OR “discharge plan” OR “discharge planning” OR “Patient Discharge” ) AND ( (“high risk” OR high-risk OR at-risk OR “chronically ill” OR “medically complex” OR “complex medical” OR comorbid* OR multimorbid* OR “multiple conditions” ) AND ( outcome or intervention OR rehospitaliz* ) AND ( geriatric OR senior OR aged OR older OR elder OR “80 and older” OR gerontolog*) NOT ( (surgical OR surgery OR “skilled nursing” OR “long-term care” OR “day surgery”).
Inclusion criteria
We included articles that met the following criteria: focused on hospital (non-ICU) transition to home or discharge planning intervention for hospitalized individuals going home, measured primary outcomes post-hospitalization, used randomized controlled trial (RCT) designs, and included primarily adults aged 60 and older.
We excluded articles that met the following criteria: were a narrative review, meta-analysis, commentary, secondary analysis, protocol, or pilot or feasibility study, did not report data on primary/main outcome, and did not include any direct contact with the older adult and/or caregiver. We also excluded programs designed specifically for individuals recovering from stroke or hip fracture, as these programs focused on recovery from acute events with specific treatment programs not applicable for a more general medical population of older adults. We did not exclude studies focused on prevalent comorbidities in the older adult population, such as heart failure or chronic obstructive pulmonary disease (COPD), as many transitional care interventions for older adults have been designed to consider management of these comorbidities. Care transition interventions for older adults with heart failure and COPD have similar characteristics to those focusing on a general medical population, which makes them relevant to the present research questions.
Data extraction and synthesis
We reviewed eligible articles in full and extracted data related to study objective, setting, population, sample, intervention component, primary and secondary outcomes, and main results. Given the focus of the review on intervention components, we extracted information on type or mode of intervention delivery, purpose of each contact, the focus of the content delivered during intervention contacts, frequency and duration of contact, who delivers the intervention, who receives the intervention, and level of caregiver involvement.
In order to synthesize study characteristics, we summarized the study setting, target age group, population health conditions, and sample characteristics (age, race, sex). We synthesized content delivered in each intervention into components of transitional care, using prior research as a guide for organizing the data.15 We categorized level of caregiver involvement by 1) had no described involvement in the intervention, 2) were involved in older adult components of the intervention, and/or 3) received specific attention to their own needs or goals. We summarized intervention follow-up with older adults and caregivers by frequency and mode (e.g., phone, home visit). We also summarized types of healthcare professional or other professional/volunteer involved in the intervention, as well as primary and secondary outcomes associated with each intervention.
Risk of bias
We used the ROBIS tool to identify concerns in the review process and judge risk of bias in this review.20 We categorized concerns in the review process into: article eligibility criteria, identification and selection of articles, data collection and study appraisal, and synthesis and findings.20 In summary, we defined the objectives of the review and eligibility criteria prior to review. Therefore, concern regarding specification of eligibility criteria was low.20 Two authors (DL and NW) were involved in article identification and selection. We used several databases, a variety of search terms, and additional methods (e.g., bibliography review) to identify articles for potential inclusion. Therefore, concern regarding identification and selection was low.20 We determined relevant article characteristics for data extraction and synthesis prior to conducting the review. We also assessed risk of bias formally. Therefore, concerns regarding data collection and appraisal were low.20 Last, the synthesis included all articles that were determined eligible by authors (DL and NW) using pre-determined criteria. The pre-determined plan for synthesis of results adequately addressed the research questions of the review. Therefore, the concerns regarding synthesis and findings were low.20 Given that concerns in conducting a review, outlined above, were addressed and selected publications were relevant to the authors’ research questions, overall risk of bias in this review was considered low.20
Results
Search results
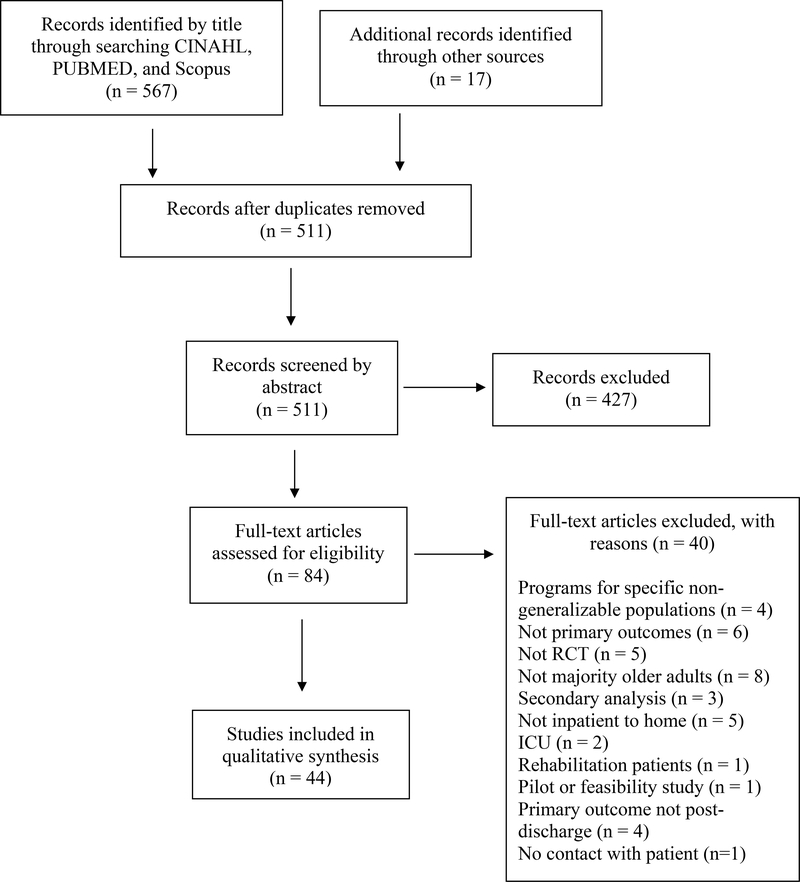
We identified 567 records by title through searching CINAHL, PubMed, and Scopus (Figure 1). We identified 17 additional articles through other sources (e.g., bibliography review). After removing duplicates, DL and NW screened 511 articles by abstract. Four hundred twenty-seven were deemed ineligible per inclusion and exclusion criteria, and we reviewed the remaining 84 articles in full. We excluded 40 articles after full-text review, most commonly due to not being an RCT, not reporting primary outcomes in the article, not focusing on inpatient to home transition, and the majority of the sample not being older adults. Forty-four articles were deemed eligible and included in this review (Figure 1).
Figure 1.
PRISMA Flow Diagram of Search Strategy and Study Selection.
Setting and Sample characteristics
The majority of the studies were conducted in the USA, Australia, Denmark, and China (supplemental Table S1). Studies commonly focused on individuals with heart failure, multiple chronic illnesses, and/or other readmission risk factors. Sample sizes, mean age, race/ethnicity, and sex are summarized for each study in supplemental Table S1.
Transitional care intervention components
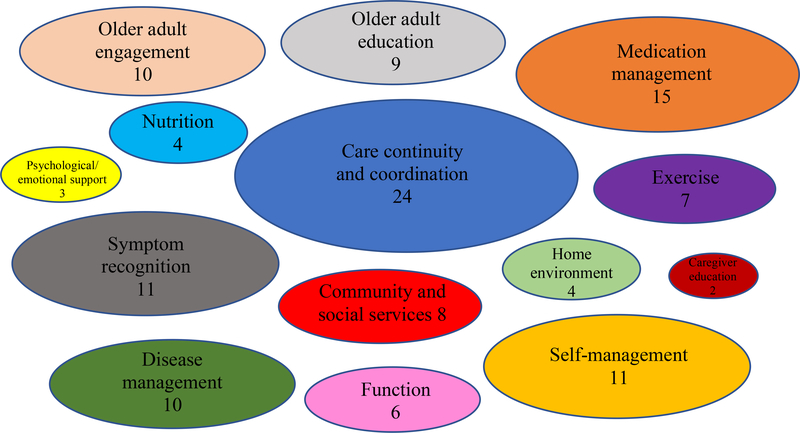
Components included in each intervention are mapped in Figure 2 by number of studies in this review. We used the studies included in this review as a guide for defining each component (Supplemental Table S2), while using prior research on transitional care components as a supporting framework.15 As shown in Figure 2, the majority of the studies included aspects of care continuity and coordination as a part of their intervention (24/44).21–44 Several studies included aspects of medication management (15/44),21–25,27,29–31,34–36,44–46 symptom recognition and care seeking (11/44),21,22,25,26,30,32,34,37,38,47,48 self-management (11/44),22,25,32,34,38,43,45,47–50 older adult engagement (10/44),22,25,29,33,34,41–43,51 disease management (10/44),26,31–33,39,42,43,46,48,52 and/or older adult education (9/44)26,28,30,31,33,37,39,43,47,48 in their interventions. A few studies also included aspects of community and social services (8/44),22,24,31,35,42,44,51,53 function (6/44),24,31,36,50,53,54 exercise (7/44),55–61 nutrition (4/44),24,62–64 home environment and accessibility (4/44),24,28,31,53 psychological and emotional support (3/44),30,38,49 and/or caregiver education (2/44).31,33
Figure 2.
Map of Transitional Care Components by Number of Studies in Review.
Caregiver involvement
The majority of studies did not describe caregiver involvement in the intervention (29/44).22–24,26,27,30,32,35,36,38–45,47,50,52,53,55–61,64 Other studies (14/44) reported involving caregivers in older adult components of the intervention (i.e., components that were designed for the older adult, but the caregiver was invited or encouraged to join).21,28,29,33,34,37,46,48,49,51,54,62,63 Only a few studies reported a focus on caregiver needs in the interventions, described as either assessing caregiver goals or values (3/44)29,33,51 and/or assessing caregiver competency and providing training to caregivers (2/44).31,33
Modes and frequency of intervention contacts
The modes and frequency of intervention contacts are represented in Table 1. Modes of intervention delivery included by phone (24/44),21,22,25,28,30–34,37,38,40–44,48–50,54,56–58 in person while the older adult was hospitalized (27/44),22,23,26,27,29–33,37,40–51,54,55,57,58,62,64 in person in the community (29/44),23–25,31–37,39–44,46,50,52–54,56,57,59–64 and in person in the outpatient setting (2/44).26,35 A majority of the studies reported using a combination of delivery modes (27/44),22,23,25,26,30–35,37,38,40–44,46,48–50,54,56–58,62–64 with 15 studies reporting using two modes22,23,25,26,30,34,35,46,48,49,56,58,62–64 and 12 reporting using three modes.31–33,37,40–44,50,54,57 Several studies reported using only one mode of intervention delivery (17/44).21,24,27–29,36,38,39,45,47,51–53,55,59–61 Those studies that reported using only one mode of intervention delivery used either the phone (3/17),21,28,38 in person while the older adult was hospitalized (6/17),27,29,45,47,51,55 or in person in the community (8/17).24,36,39,52,53,59–61 An additional finding of this review was that no studies reported using information technologies such as electronic health records, patient portals, or mobile health applications as intervention modes. Two studies had older adults maintain a personal health record, which was a physical document they could use to track their own care and preferences.25,34
Table 1.
Duration and frequency of intervention contact.
Note.  =Hospital or clinic visit,
=Hospital or clinic visit,  =Home visit,
=Home visit,  =Phone,
=Phone,  =Video call, “,”=And, “/”=Or
=Video call, “,”=And, “/”=Or
Intervention contact post discharge ranged from only once21,28,30,52 to 32 contacts.61 The majority of studies (25/44)22–25,28,30–34,37,39–44,46,48,49,54,56–58,62 included both pre- and post-discharge contact. Seven of the studies included in this review had only pre- or at-discharge intervention contact,27,29,45,47,51,53,55 and twelve of the studies had only post-discharge intervention contact.21,26,35,36,38,50,52,59–61,63,64 Post discharge contact duration ranged from one week to two years post-discharge. A large majority of the studies included intervention contact within 1 month of hospital discharge (37/44).21–26,28,30–44,46,48–50,52,54,56–64 Twenty studies included intervention contact in months 2 and 3.24,26,31–33,35–38,42,46,48,49,56–61,64 Nine studies included intervention contact in months 4–6.23,26,32,42,46,56,57,61,62 Only two studies included intervention contact between 7–24 months.26,32
Roles
The majority of care transition interventions used nurses as interventionists (28/44),24–26,28,30–44,46–48,50–52,56–58 with 17 of those studies using nurses with additional training, such as specific transitional care training and specialty training (e.g., community care, cardiology).25,26,28,30,31,33,34,37,39–42,44,46,48,50,58 Of the seven studies that included physicians in the intervention, three included the primary care physician,31,35,36 three included a specialist such as a cardiologist,27,29,53 and one included both.26 Other roles included in the interventions were Dieticians (5/44),24,48,62–64 Physical/Physio Therapists (6/44),24,55,57,59–61 Social Workers (4/44),21,31,40,53 Pharmacists (3/44),23,31,45 Occupational Therapists (3/44),24,53,54 a Community Health Worker (1/44).22 One study reported using community volunteers.40 Only nine studies reported including interdisciplinary teams (including more than one discipline) to implement the intervention.24,26,31,35,36,40,48,53,57
Outcomes
Readmission or hospitalization was the most common outcome assessed in studies included in this review (33/44)21–44,46–48,50,53,54,56,57,64 (Table 2). Many studies reported efficacy in reducing incidence of readmission or hospitalization (17/44).23–26,28,29,31,33–35,38,40,41,47,48,56,57 Other common outcomes included mortality (23/44),21,23,24,26–33,35,37,38,42,44,46–48,50,53,62,64 quality of life (24/44),23,24,26–28,32,33,37–42,44,45,47,50,51,55,56,58,60,61,63 and functional status (14/44).24,26,27,32,33,35,39,46,53,54,60,62–64 Several reported significant improvements in mortality (7/44).26,31,33,46–48,62 and quality of life (8/44),26,33,37,41,42,51,56,58 while only one study was efficacious in improving functional status.26
Table 2.
Primary and Secondary Outcomes by Outcome Domains.
| Outcome domain | Subdomain | Outcome details | Outcomes, No. | Positive, No. (%) |
|---|---|---|---|---|
| Total | 208 | 83 (40) | ||
| Healthcare utilization | 77 | 37 (48) | ||
| Readmission or hospitalization | All-cause, disease-specific, and/or nonelective readmission. Some included planned readmissions. | 45 | 24 (53) | |
| Length of stay | Including time to discharge home | 5 | 3 (60) | |
| Physician follow-up | Contact with a physician (e.g., PCP, GP), GP satisfaction with transition/ communication processes | 5 | 4 (80) | |
| Outpatient visit | Occurrence of outpatient visits | 6 | 4 (67) | |
| Emergency service utilization | Emergency department or urgent care | 11 | 0 (0) | |
| Institutionalization | Long-term care admission | 2 | 0 (0) | |
| Use of social services | Meals-on-wheels, home nursing care, private care | 3 | 2 (67) | |
| Health and well-being | 116 | 36 (31) | ||
| Mortality | Death and time to death | 26 | 8 (31) | |
| Quality of life | Assessment of Quality of LIfe (AQoL), EQ-5D-3L, Minnesota Living with Heart Failure Questionnaire (MLHF), St. George's Respiratory Questionnaire (SGRQ), Euroqol Scale (EQ-5D), life satisfaction | 25 | 8 (33) | |
| Nutritional status | Body weight, BMI, energy, dietary intake, Mini Nutritional Assessment (MNA) | 5 | 3 (60) | |
| Physical function | Muscle/hand-grip strength, Six Minute Walk Test6MWD, Timed up and go (TUG), 30-s chair-to-stand, stability and balance, Cumulated Ambulation Score (CAS) | 13 | 6 (46) | |
| Functional status | Activities of daily living (ADL), Instrumental activities of daily living (IADL), mobility, Barthel Index | 14 | 1 (7) | |
| Physical activity | Physical Activity Scale for the Elderly (PASE) questionnaire | 1 | 1 (100) | |
| Cognitive function | Mini-Mental State Examination (MMSE) | 3 | 0 (0) | |
| Self-rated health | Also perceived health | 5 | 3 (60) | |
| Falls | Includes self-reported falls, fall risk, fall efficacy | 4 | 1 (25) | |
| Psychological well-being | Depression, anxiety, psychosocial adjustment to illness, stress, self-efficacy, social support | 12 | 2 (17) | |
| Blood tests | Serum albumin, cholesterol, hemoglobin, lymphocyte count | 2 | 0 (0) | |
| Heart failure self-care | Maintenance, management, confidence, and knowledge | 2 | 2 (100) | |
| Constipation | As measured by tools like the Constipation Assessment Scale (CAS) | 1 | 0 (0) | |
| Heart functioning | Resting heart rate, left ventricular ejection fraction, blood pressure | 2 | 0 (0) | |
| Health-related lifestyle | Understanding of and adherence to diet, medications, exercise | 1 | 1 (100) | |
| Quality of Care | 15 | 10 (67) | ||
| Prescribing appropriateness | Criteria were developed according to the most frequent medications prescribed to older adults and the most frequent medical conditions for which older adults consulted their general practitioners | 1 | 0 (0) | |
| Quality of care | Includes quality of care transition | 2 | 2 (100) | |
| Cost of care | 3 | 2 (67) | ||
| Satisfaction with care | Includes satisfaction with discharge, care, education, medications, referral | 8 | 5 (63) | |
| Discharge preparedness | 1 | 1 (100) |
Discussion
The results of this scoping review support that, while many interventions designed for older adults transitioning from hospital to home share common components, transitional care interventions remain heterogenous. There are a few key components that are commonly targeted, including care continuity and coordination, medication management, and symptom recognition and care seeking. As a result, these components often emerge as focal areas for transitional care interventions.5,7 However, newer evidence reveals additional important components, including older adult and caregiver engagement, education, and well-being.2,15,65,66 Future research should explore mechanisms of incorporating these components into interventions for older adults transitioning from hospital to home and how to leverage related outcomes.
The lack of involvement of caregivers in care transition interventions reveals an important challenge in addressing older adult and caregiver needs. For instance, there is a high prevalence of older adults requiring help from caregivers with self-care, complex medical tasks, and medication management, and caregivers themselves often experience poor health, economic, and well-being outcomes.67 When caregivers are involved in care transition interventions, it is rarely for the purpose of assessing and addressing their caregiving needs, more often it is focused on the older adult’s needs. This is problematic as increasing evidence highlights the important role caregivers play in helping older adults transition from hospital to home.13,65,66 Indeed, many states have recognized the importance of involving caregivers in care transitions by passing the Caregiver Advise, Record, and Enable (CARE) Act. This Act mandates hospitals to 1) ask patients if they want to identify a caregiver, 2) notify that identified caregiver of the patient’s discharge, and 3) provide instruction to the caregiver on tasks to be performed in the home post discharge.68 Future research should explore methods to increase caregiver engagement and their potential influence on health and functional outcomes for the older adult. This work could provide a foundation to help hospitals meet the CARE act mandates and ultimately, better support older adults’ transition from hospital to home.
The modes of intervention contact also vary across interventions. Most common modes identified in this review were by phone, in home, or in hospital/clinic. Some have suggested that in home contact is an important aspect,10 while others used telephone only contact and had success.21,28,38 However, there is evidence supporting the importance of both pre and post hospital contact.16 If not carefully considered in terms of other aspects of the system (e.g., other tools, people involved, environments, etc.) mode of delivery can have unanticipated consequences for transitional care outcomes, as well as intermediary outcomes such as communication and team dynamics.69 It is important to further examine potential consequences of different modes of delivery in future work. An additional finding of this review is that information technologies such as electronic health records, patient portals, or mobile health applications appear to be underutilized as modes of intervention contact for care transition interventions. Therefore, further reviews should focus on use of technologies in interventions for older adults transitioning from hospital to home to inform future intervention research. There may be opportunities to expand the use of information technologies, especially with the increased use of telehealth since COVID-1970 and funding initiatives focused on improving healthcare quality through health information technology.71
This review also reveals that the duration and frequency of the interventions contact vary, with some trends, such as most common contact occurring from 1–3 months post-discharge, after which contact becomes uncommon. The focus on shorter duration could be potentially problematic for older adults that experience transitions as occurring over a longer period of time as they attempt to integrate new functional limitations and self-management routines into their daily lives.2,65,66 There may be opportunities for bridging short-term interventions from one set of providers to those delivering more long-term interventions. These may require bridging multiple providers along the continuum of care including the hospital, primary care, and community pharmacy. Further research is necessary to examine most appropriate duration and frequency of intervention contact for these groups and which providers would be best positioned to affect important short versus long-term outcomes.11 Further, it is important to examine how interventions could be stratified or tailored to match specific needs of certain groups of older adults and caregivers, such as by intensity, duration, or modality.
Interdisciplinary teams are relatively uncommon in delivery of the care transition interventions. Use of team-based care appears more common during pre-discharge contact, with post-discharge contact commonly conducted by a single profession or other trained individual or volunteer. Some studies suggest that intentional transitional care delivered by a multidisciplinary team leads to a reduction in healthcare costs and an improvement in patient outcomes (e.g., length of stay),72 and this could be especially important for older adults with complex care needs. Teams in healthcare have also been shown to improve patient satisfaction73 and provider outcomes such as increased job satisfaction.74 Further exploration of how teams can be effectively leveraged throughout the care transition process will be important to achieving optimal quality and safety outcomes. It will also be important to further explore the most prominent roles in post-discharge care, as there was significant variability in our review. Nurses with and without additional training are commonly utilized and cited as having knowledge and capabilities in many of the important transition care components. However, it is important to consider why some roles are less represented and explore potential contributions of additional disciplines, such as social work or occupational therapy.
Last, we found that the majority of RCTs for older adults transitioning from hospital to home focus on a similar limited set of outcomes, readmission or rehospitalization, mortality, and quality of life. The most common outcomes are related to utilization and mortality, which has been triggered by financial penalties for hospital readmissions.75 This finding is consistent with the need to select outcomes that show impact of an intervention to important stakeholders and healthcare systems to enable widespread adoption and sustainability. However, in some cases, readmission may not be a negative outcome, but instead a rational choice to prevent other adverse outcomes including death as exemplified by research in heart failure patients.75,76 Some studies have examined other important metrics for older adults, such as function, quality of life, and psychological well-being, 2–4,11–14 but it is important to further prioritize these metrics in intervention and study designs, such as by including them as a primary outcome and considering how the intervention should be designed to impact these metrics. Given the critical role of caregivers in care transition quality and safety,13,65,66 future research on transitional care interventions should employ methods for caregiver engagement, examine caregiver outcomes, and investigate whether caregiver and older adult outcomes are related. There is also an opportunity to examine newer payment models that could include caregiver engagement, older adult function, and safety issues as important outcomes of care transitions.77 For instance, shared savings programs and Medicare advantage plans promote time spent on improving care quality and coordination to help address the broad range of suboptimal outcomes.78
Limitations
First, only RCTs that were published in English were included. Second, our review was limited to databases of peer-reviewed journals, and thus, did not include ‘grey’ literature. Third, choice of inclusion and exclusion criteria could be considered a limitation, such as excluding transitional care interventions for hip fracture and stroke patients. These populations may be important subjects for further review. Lastly, a formal quality appraisal was not conducted, as scoping reviews aim to provide an overview of a topic and identify gaps in knowledge and implications for future research agendas.
Conclusions
Current care transition interventions share some key limitations in addressing important care transition outcomes, such as function and engagement among older adults and their caregivers. To improve outcomes beyond healthcare utilization, a paradigm shift is required in the design and study of care transition interventions. Future interventions should explore methods or novel interventions for caregiver engagement; leverage an interdisciplinary team or care coordination hub with involvement from underrepresented specialties such as social work and occupational therapy; and examine opportunities for interventions designed specifically to address older adult and caregiver-reported needs and their well-being. This review also reveals important considerations for providers and organizations as to whether existing measures to improve older adult transitions are optimally positioned to address their target healthcare utilization and patient outcomes.
Supplementary Material
Supplemental Table S1. Characteristics of each Study Included in the Review.
Supplemental Table S2. Definitions of each Transitional Care Component.
Key points
Older adult care transition interventions have limitations.
Interventions should consider caregivers, interdisciplinary teams, and older adult and caregiver-reported needs and well-being.
Why does this matter?
A care transition intervention paradigm shift is needed to comprehensively improve older adults’ care.
Acknowledgements:
Funding. The project described was supported by an OAA Advanced Fellowship in Geriatrics (William S. Middleton Memorial Veterans Hospital, Madison, WI). This work was also supported by the University of Wisconsin-Madison Clinical and Translational Science Award (CTSA) program through the National Institutes of Health National Center for Advancing Translational Sciences (NCATS), grant 1UL1TR002373, KL2 grant KL2TR002374, and the National Institute on Aging, grant R03 AG062848. The content is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Department of Veterans Affairs, the United States Government, or the National Institutes of Health.
Sponsor’s role. N/A
Footnotes
Conflicts of interest. None
References
- 1.Hoyer EH, Needham DM, Atanelov L, Knox B, Friedman M, Brotman DJ. Association of impaired functional status at hospital discharge and subsequent rehospitalization. J Hosp Med. 2014;9(5):277–282. doi: 10.1002/jhm.2152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liebzeit D, Bratzke L, Boltz M, Purvis S, King B. Getting Back to Normal: A Grounded Theory Study of Function in Post-hospitalized Older Adults. The Gerontologist. 2020;60(4):704–714. doi: 10.1093/geront/gnz057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang H-T, Chang C-M, Liu L-F, Lin H-S, Chen C-H. Trajectories and predictors of functional decline of hospitalised older patients. J Clin Nurs. 2013;22(9/10):1322–1331. doi: 10.1111/jocn.12055 [DOI] [PubMed] [Google Scholar]
- 4.Buurman BM, Hoogerduijn JG, de Haan RJ, et al. Geriatric conditions in acutely hospitalized older patients: prevalence and one-year survival and functional decline. PLoS One. 2011;6(11):e26951. doi: 10.1371/journal.pone.0026951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tomlinson J, Cheong V-L, Fylan B, et al. Successful care transitions for older people: a systematic review and meta-analysis of the effects of interventions that support medication continuity. Age Ageing. 2020;afaa002.49(4):558–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Le Berre M, Maimon G, Sourial N, Guériton M, Vedel I. Impact of transitional care services for chronically Ill older patients: a systematic evidence review. J Am Geriatr Soc. 2017;65(7):1597–1608. [DOI] [PubMed] [Google Scholar]
- 7.Facchinetti G, D’Angelo D, Piredda M, et al. Continuity of care interventions for preventing hospital readmission of older people with chronic diseases: A meta-analysis. Int J Nurs Stud. 2020;101:103396. doi: 10.1016/j.ijnurstu.2019.103396 [DOI] [PubMed] [Google Scholar]
- 8.Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The importance of transitional care in achieving health reform. Health Aff (Millwood). 2011;30(4):746–754. [DOI] [PubMed] [Google Scholar]
- 9.Allen J, Hutchinson AM, Brown R, Livingston PM. Quality care outcomes following transitional care interventions for older people from hospital to home: a systematic review. BMC Health Serv Res. 2014;14:346. doi: 10.1186/1472-6963-14-346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Linertová R, García-Pérez L, Vázquez-Díaz JR, Lorenzo-Riera A, Sarría-Santamera A. Interventions to reduce hospital readmissions in the elderly: in-hospital or home care. A systematic review. J Eval Clin Pract. 2011;17(6):1167–1175. doi: 10.1111/j.1365-2753.2010.01493.x [DOI] [PubMed] [Google Scholar]
- 11.Rennke S, Nguyen OK, Shoeb MH, Magan Y, Wachter RM, Ranji SR. Hospital-Initiated Transitional Care Interventions as a Patient Safety Strategy. Ann Intern Med. 2013;158(5_Part_2):433–440. doi: 10.7326/0003-4819-158-5-201303051-00011 [DOI] [PubMed] [Google Scholar]
- 12.Greysen SR, Hoi-Cheung D, Garcia V, et al. ‘Missing Pieces’-Functional, Social, and Environmental Barriers to Recovery for Vulnerable Older Adults Transitioning from Hospital to Home. J Am Geriatr Soc. 2014;62(8):1556–1561. doi: 10.1111/jgs.12928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hestevik CH, Molin M, Debesay J, Bergland A, Bye A. Older persons’ experiences of adapting to daily life at home after hospital discharge: a qualitative metasummary. BMC Health Serv Res. 2019;19(1):224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walker R, Johns J, Halliday D. How older people cope with frailty within the context of transition care in Australia: implications for improving service delivery. Health Soc Care Community. 2015;23(2):216–224. doi: 10.1111/hsc.12142 [DOI] [PubMed] [Google Scholar]
- 15.Naylor MD, Shaid EC, Carpenter D, et al. Components of Comprehensive and Effective Transitional Care. J Am Geriatr Soc. 2017;65(6):1119–1125. doi: 10.1111/jgs.14782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rennke S, Ranji SR. Transitional care strategies from hospital to home: a review for the neurohospitalist. The Neurohospitalist. 2015;5(1):35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Interdisciplinary Care for Older Adults with Complex Needs: American Geriatrics Society Position Statement. J Am Geriatr Soc. 2006;54(5):849–852. doi: 10.1111/j.1532-5415.2006.00707.x [DOI] [PubMed] [Google Scholar]
- 18.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J. 2009;26(2):91–108. [DOI] [PubMed] [Google Scholar]
- 19.Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evid Implement. 2015;13(3):141–146. doi: 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- 20.Whiting P, Savović J, Higgins JP, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Altfeld SJ, Shier GE, Rooney M, et al. Effects of an enhanced discharge planning intervention for hospitalized older adults: a randomized trial. The Gerontologist. 2013;53(3):430–440. [DOI] [PubMed] [Google Scholar]
- 22.Balaban RB, Galbraith AA, Burns ME, Vialle-Valentin CE, Larochelle MR, Ross-Degnan D. A patient navigator intervention to reduce hospital readmissions among high-risk safety-net patients: a randomized controlled trial. J Gen Intern Med. 2015;30(7):907–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barker A, Barlis P, Berlowitz D, Page K, Jackson B, Lim WK. Pharmacist directed home medication reviews in patients with chronic heart failure: a randomised clinical trial. Int J Cardiol. 2012;159(2):139–143. [DOI] [PubMed] [Google Scholar]
- 24.Beck A, Andersen U, Leedo E, et al. Does adding a dietician to the liaison team after discharge of geriatric patients improve nutritional outcome: a randomised controlled trial. Clin Rehabil. 2015;29(11):1117–1128. [DOI] [PubMed] [Google Scholar]
- 25.Coleman EA, Parry C, Chalmers S, Min S. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–1828. [DOI] [PubMed] [Google Scholar]
- 26.Del Sindaco D, Pulignano G, Minardi G, et al. Two-year outcome of a prospective, controlled study of a disease management programme for elderly patients with heart failure. J Cardiovasc Med. 2007;8(5):324–329. [DOI] [PubMed] [Google Scholar]
- 27.Edmans J, Bradshaw L, Franklin M, Gladman J, Conroy S. Specialist geriatric medical assessment for patients discharged from hospital acute assessment units: randomised controlled trial. Bmj. 2013;347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lainscak M, Kadivec S, Kosnik M, et al. Discharge coordinator intervention prevents hospitalizations in patients with COPD: a randomized controlled trial. J Am Med Dir Assoc. 2013;14(6):450–e1. [DOI] [PubMed] [Google Scholar]
- 29.Legrain S, Tubach F, Bonnet-Zamponi D, et al. A New Multimodal Geriatric Discharge-Planning Intervention to Prevent Emergency Visits and Rehospitalizations of Older Adults: The Optimization of Medication in AGE d Multicenter Randomized Controlled Trial. J Am Geriatr Soc. 2011;59(11):2017–2028. [DOI] [PubMed] [Google Scholar]
- 30.Linden A, Butterworth SW. A comprehensive hospital-based intervention to reduce readmissions for chronically ill patients: a randomized controlled trial. Am J Manag Care. 2014;20(10):783–792. [PubMed] [Google Scholar]
- 31.Low LL, Tan SY, Ng MJM, et al. Applying the integrated practice unit concept to a modified virtual ward model of care for patients at highest risk of readmission: a randomized controlled trial. PLoS One. 2017;12(1):e0168757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meisinger C, Stollenwerk B, Kirchberger I, et al. Effects of a nurse-based case management compared to usual care among aged patients with myocardial infarction: results from the randomized controlled KORINNA study. BMC Geriatr. 2013;13(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675–684. [DOI] [PubMed] [Google Scholar]
- 34.Parry C, Min S-J, Chugh A, Chalmers S, Coleman EA. Further application of the care transitions intervention: results of a randomized controlled trial conducted in a fee-for-service setting. Home Health Care Serv Q. 2009;28(2–3):84–99. [DOI] [PubMed] [Google Scholar]
- 35.Rytter L, Jakobsen HN, Rønholt F, et al. Comprehensive discharge follow-up in patients’ homes by GPs and district nurses of elderly patients: A randomized controlled trial. Scand J Prim Health Care. 2010;28(3):146–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thygesen LC, Fokdal S, Gjørup T, Taylor RS, Zwisler A-D, Prevention of Early Readmission Research Group. Can municipality-based post-discharge follow-up visits including a general practitioner reduce early readmission among the fragile elderly (65+ years old)? A randomized controlled trial. Scand J Prim Health Care. 2015;33(2):65–73. doi: 10.3109/02813432.2015.1041831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Van Spall HGC, Lee SF, Xie F, et al. Effect of Patient-Centered Transitional Care Services on Clinical Outcomes in Patients Hospitalized for Heart Failure: The PACT-HF Randomized Clinical Trial. JAMA. 2019;321(8):753–761. doi: 10.1001/jama.2019.0710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wakefield BJ, Ward MM, Holman JE, et al. Evaluation of home telehealth following hospitalization for heart failure: a randomized trial. Telemed J E-Health Off J Am Telemed Assoc. 2008;14(8):753–761. doi: 10.1089/tmj.2007.0131 [DOI] [PubMed] [Google Scholar]
- 39.Wong FKY, Chow S, Chung L, et al. Can home visits help reduce hospital readmissions? Randomized controlled trial. J Adv Nurs. 2008;62(5):585–595. [DOI] [PubMed] [Google Scholar]
- 40.Wong FK, Ho MM, Yeung S, Tam SK, Chow SK. Effects of a health-social partnership transitional program on hospital readmission: a randomized controlled trial. Soc Sci Med. 2011;73(7):960–969. [DOI] [PubMed] [Google Scholar]
- 41.Wong FKY, Chow SKY, Chan TMF, Tam SKF. Comparison of effects between home visits with telephone calls and telephone calls only for transitional discharge support: a randomised controlled trial. Age Ageing. 2014;43(1):91–97. doi: 10.1093/ageing/aft123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yu DSF, Lee DTF, Stewart S, Thompson DR, Choi K-C, Yu C-M. Effect of Nurse-Implemented Transitional Care for Chinese Individuals with Chronic Heart Failure in Hong Kong: A Randomized Controlled Trial. J Am Geriatr Soc. 2015;63(8):1583–1593. doi: 10.1111/jgs.13533 [DOI] [PubMed] [Google Scholar]
- 43.Zhao Y, Wong FKY. Effects of a postdischarge transitional care programme for patients with coronary heart disease in China: a randomised controlled trial. J Clin Nurs. 2009;18(17):2444–2455. doi: 10.1111/j.1365-2702.2009.02835.x [DOI] [PubMed] [Google Scholar]
- 44.Gilbert T, Occelli P, Rabilloud M, et al. A Nurse-Led Bridging Program to Reduce 30-Day Readmissions of Older Patients Discharged From Acute Care Units. J Am Med Dir Assoc. Published online November 20, 2020. doi: 10.1016/j.jamda.2020.09.015 [DOI] [PubMed] [Google Scholar]
- 45.Basger BJ, Moles RJ, Chen TF. Impact of an enhanced pharmacy discharge service on prescribing appropriateness criteria: a randomised controlled trial. Int J Clin Pharm. 2015;37(6):1194–1205. [DOI] [PubMed] [Google Scholar]
- 46.Buurman BM, Parlevliet JL, Allore HG, et al. Comprehensive Geriatric Assessment and Transitional Care in Acutely Hospitalized Patients: The Transitional Care Bridge Randomized Clinical Trial. JAMA Intern Med. 2016;176(3):302–309. [DOI] [PubMed] [Google Scholar]
- 47.Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111(2):179–185. [DOI] [PubMed] [Google Scholar]
- 48.McDonald K, Ledwidge M, Cahill J, et al. Heart failure management: multidisciplinary care has intrinsic benefit above the optimization of medical care. J Card Fail. 2002;8(3):142–148. [DOI] [PubMed] [Google Scholar]
- 49.Gallagher R, McKinley S, Dracup K. Effects of a telephone counseling intervention on psychosocial adjustment in women following a cardiac event. Heart Lung. 2003;32(2):79–87. [DOI] [PubMed] [Google Scholar]
- 50.Lindhardt T, Loevgreen SM, Bang B, Bigum C, Klausen TW. A targeted assessment and intervention at the time of discharge reduced the risk of readmissions for short-term hospitalized older patients: a randomized controlled study. Clin Rehabil. 2019;33(9):1431–1444. [DOI] [PubMed] [Google Scholar]
- 51.Preen DB, Bailey BE, Wright A, et al. Effects of a multidisciplinary, post-discharge continuance of care intervention on quality of life, discharge satisfaction, and hospital length of stay: a randomized controlled trial. Int J Qual Health Care. 2005;17(1):43–51. [DOI] [PubMed] [Google Scholar]
- 52.Konradsen H, Rasmussen MLT, Noiesen E, Trosborg I. Effect of home care nursing on patients discharged from hospital with self-reported signs of constipation. Gastroenterol Nurs. 2017;40(6):463–468. [DOI] [PubMed] [Google Scholar]
- 53.Pardessus V, Puisieux F, Di Pompeo C, Gaudefroy C, Thevenon A, Dewailly P. Benefits of home visits for falls and autonomy in the elderly: a randomized trial study. Am J Phys Med Rehabil. 2002;81(4):247–252. [DOI] [PubMed] [Google Scholar]
- 54.Clemson L, Lannin NA, Wales K, et al. Occupational therapy predischarge home visits in acute hospital care: a randomized trial. J Am Geriatr Soc. 2016;64(10):2019–2026. [DOI] [PubMed] [Google Scholar]
- 55.Brovold T, Skelton DA, Bergland A. Older adults recently discharged from the hospital: effect of aerobic interval exercise on health-related quality of life, physical fitness, and physical activity. J Am Geriatr Soc. 2013;61(9):1580–1585. [DOI] [PubMed] [Google Scholar]
- 56.Courtney M, Edwards H, Chang A, Parker A, Finlayson K, Hamilton K. Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled trial to determine the effectiveness of a 24-week exercise and telephone follow-up program. J Am Geriatr Soc. 2009;57(3):395–402. [DOI] [PubMed] [Google Scholar]
- 57.Finlayson K, Chang AM, Courtney MD, et al. Transitional care interventions reduce unplanned hospital readmissions in high-risk older adults. BMC Health Serv Res. 2018;18(1):956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xueyu L, Hao Y, Shunlin X, Rongbin L, Yuan G. Effects of low-intensity exercise in older adults with chronic heart failure during the transitional period from hospital to home in china: a randomized controlled trial. Res Gerontol Nurs. 2017;10(3):121–128. [DOI] [PubMed] [Google Scholar]
- 59.Timonen L, Rantanen T, Ryynänen O-P, Taimela S, Timonen TE, Sulkava R. A randomized controlled trial of rehabilitation after hospitalization in frail older women: effects on strength, balance and mobility. Scand J Med Sci Sports. 2002;12(3):186–192. doi: 10.1034/j.1600-0838.2002.120310.x [DOI] [PubMed] [Google Scholar]
- 60.Vogler CM, Sherrington C, Ogle SJ, Lord SR. Reducing risk of falling in older people discharged from hospital: a randomized controlled trial comparing seated exercises, weight-bearing exercises, and social visits. Arch Phys Med Rehabil. 2009;90(8):1317–1324. doi: 10.1016/j.apmr.2009.01.030 [DOI] [PubMed] [Google Scholar]
- 61.Sunde S, Hesseberg K, Skelton DA, et al. Effects of a multicomponent high intensity exercise program on physical function and health-related quality of life in older adults with or at risk of mobility disability after discharge from hospital: a randomised controlled trial. BMC Geriatr. 2020;20(1):464. doi: 10.1186/s12877-020-01829-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Feldblum I, German L, Castel H, Harman-Boehm I, Shahar DR. Individualized nutritional intervention during and after hospitalization: the nutrition intervention study clinical trial. J Am Geriatr Soc. 2011;59(1):10–17. [DOI] [PubMed] [Google Scholar]
- 63.Pedersen JL, Pedersen PU, Damsgaard E. Early nutritional follow-up after discharge prevents deterioration of ADL functions in malnourished, independent, geriatric patients who live alone–A randomized clinical trial. J Nutr Health Aging. 2016;20(8):845–853. [DOI] [PubMed] [Google Scholar]
- 64.Terp R, Jacobsen KO, Kannegaard P, Larsen A-M, Madsen OR, Noiesen E. A nutritional intervention program improves the nutritional status of geriatric patients at nutritional risk-a randomized controlled trial. Clin Rehabil. 2018;32(7):930–941. doi: 10.1177/0269215518765912 [DOI] [PubMed] [Google Scholar]
- 65.Liebzeit D, Bratzke L, King B. Strategies older adults use in their work to get back to normal following hospitalization. Geriatr Nurs N Y N. 2020;41(2):132–138. doi: 10.1016/j.gerinurse.2019.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Werner NE, Tong M, Borkenhagen A, Holden RJ. Performance-shaping factors affecting older adults’ hospital-to-home transition success: a systems approach. The Gerontologist. 2019;59(2):303–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Families Caring for an Aging America. National Academy of Medicine. Accessed January 28, 2021. https://nam.edu/families-caring-for-an-aging-america/
- 68.CARE Act assists family caregivers | JustCare. Accessed January 28, 2021. https://justcareusa.org/care-act-assists-family-caregivers/
- 69.Carayon P, Hundt AS, Karsh B, et al. Work system design for patient safety: the SEIPS model. BMJ Qual Saf. 2006;15(suppl 1):i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Koonin LM. Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic — United States, January–March 2020. MMWR Morb Mortal Wkly Rep. 2020;69. doi: 10.15585/mmwr.mm6943a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.NIH Guide: All Active Funding Opportunities (RFAs & PAs). Accessed May 4, 2021. https://grants.nih.gov/grants/guide/search_results.htm?scope=pa&year=active
- 72.Blewett LA, Johnson K, McCarthy T, Lackner T, Brandt B. Improving geriatric transitional care through inter-professional care teams. J Eval Clin Pract. 2010;16(1):57–63. [DOI] [PubMed] [Google Scholar]
- 73.Deeter-Schmelz DR, Kennedy KN. Patient care teams and customer satisfaction: the role of team cohesion. J Serv Mark. 2003.17(7):666–684. [Google Scholar]
- 74.Lemieux-Charles L, McGuire WL. What do we know about health care team effectiveness? A review of the literature. Med Care Res Rev. 2006;63(3):263–300. [DOI] [PubMed] [Google Scholar]
- 75.Gupta A, Allen LA, Bhatt DL, et al. Association of the Hospital Readmissions Reduction Program Implementation With Readmission and Mortality Outcomes in Heart Failure. JAMA Cardiol. 2018;3(1):44–53. doi: 10.1001/jamacardio.2017.4265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sevilla-Cazes J, Ahmad FS, Bowles KH, et al. Heart Failure Home Management Challenges and Reasons for Readmission: a Qualitative Study to Understand the Patient’s Perspective. J Gen Intern Med. 2018;33(10):1700–1707. doi: 10.1007/s11606-018-4542-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hospital Value-Based Purchasing Program | CMS. Accessed May 4, 2021. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Hospital-Value-Based-Purchasing-
- 78.About the Program | CMS. Accessed April 6, 2021. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/about
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table S1. Characteristics of each Study Included in the Review.
Supplemental Table S2. Definitions of each Transitional Care Component.