Abstract
Background
The incidence of nosocomial infections including ventilator-associated pneumonia and bacteraemia has been described during the COVID-19 pandemic. However, information regarding the impact of COVID-19 on the incidence of catheter-related bloodstream infections (CR-BSIs) is very limited.
Aim
To evaluate the impact of the COVID-19 pandemic in the evolution of CR-BSIs in a large hospital.
Methods
This was a retrospective study comparing the incidence, aetiology and outcome of CR-BSIs during the months of March to May 2019 (pre-pandemic) and 2020 (during the pandemic).
Findings
The number of patients with one or more CR-BSIs in 2019 and 2020 were 23 and 58, respectively (1.89 vs 5.53/1000 admissions); P<0.001. Median time from catheter implantation to demonstration of CR-BSI was 27.5 days (range 11.75–126.00 days) in the 2019 cases and 16.0 days (range 11.00–23.50 days) in the 2020 population (P=0.032).
Conclusions
A dramatic increase of CR-BSIs was found during the COVID-19 pandemic. Reinforcement of classic and new preventive measures is necessary.
Keywords: COVID-19, Catheter-related bloodstream infections, Infection control, Nosocomial infections, COVID-19 secondary infections
Introduction
Catheter-related infection is one of the leading causes of bacteraemia and sepsis in developed countries and its adequate control by multi-disciplinary teams represents one of the best-quality indicators of an institution. The incidence can range from 0.8 to 18 episodes/1000 days of catheter exposure, depending on the type of patient, the type of catheter and the care provided during implantation and follow-up [[1], [2], [3], [4], [5]].
The COVID-19 pandemic has led to a huge increase in the workload of hospitals around the world and many patients have required long hospital stays including extended admissions to intensive care units (ICUs) [[6], [7], [8]].
Care for these patients has been provided under strenuous circumstances, not only because of the increased workload but also because sometimes there was a need to implicate staff with a sub-optimal degree of training with ICU patients [[9], [10], [11]].
Under these conditions, it is not surprising that an increased incidence of nosocomially acquired infections, including ventilator-associated pneumonia and bacteraemia, has been described in some centres [[12], [13], [14]]. Surprisingly, information regarding the impact of COVID-19 on the incidence of catheter-related bloodstream infections (CR-BSIs) is thus far limited.
Our aim was to evaluate the impact of the COVID-19 pandemic in the evolution of CR-BSIs in a large hospital, including incidence, aetiology and outcome.
Material and methods
Setting
Our institution is a general reference hospital, located in Madrid, Spain, with 1350 beds and approximately 55,000 admissions/year. The number of ICU beds is normally 70, but was expanded to 140 during the study period.
Study design
We performed a retrospective study in which we compared the incidence, aetiology, and outcome of CR-BSIs during the months of March to May in 2019 and 2020 (before and during the COVID-19 pandemic).
Ethics approval and consent to participate
The Ethics of Hospital General Universitario Gregorio Marañon approved the study. The need for informed consent for this study was waived by Ethics Committee MICRO.HGUGM.2020-030 of Hospital General Universitario Gregorio Marañon. All procedures were carried out in accordance with relevant guidelines and regulations.
Endpoints
The primary endpoint was the incidence of CR-BSI episodes before and during the pandemic. The secondary endpoints were the aetiology and consequences of CR-BSI during the first wave of the pandemic.
Definitions
CR-BSI
Presence of bacteraemia or fungaemia in a patient with clinical manifestations of infection and no other apparent source of bloodstream infection (with the exception of the catheter). A catheter-tip culture, quantitative or semiquantitative, positive for the same micro-organism was also required [5,15].
Non–CR-BSI
In the present study, episodes of bacteraemia with a non-documented catheter origin.
Attributable mortality
In the present study, death occurring within 7 days after confirmation of CR-BSI in the absence of an alternative evident cause was considered as attributable.
Statistical analysis
Qualitative variables are expressed as a frequency distribution. Quantitative variables are expressed as the mean and standard deviation (SD) and as the median and interquartile range (IQR) if their distribution was skewed. Normally distributed continuous variables were compared using the t-test; non-normally distributed continuous variables were compared using the Mann–Whitney test. The chi-squared or Fisher exact test was used to compare categorical variables. Statistical significance was set at P≤0.05.
We compared the incidence rate of catheter-related bacteraemia per 1000 admissions between the two periods using Epidat version 3.1.
Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp, Armonk, NY, USA) and Epidat 3.1.
Results
Hospital admissions during the study periods (1st March to 31st May 2019 and 2020) were, respectively, 12,111 and 10,479 patients. Similarly, the number of blood cultures processed by the microbiology department was, respectively, 9520 (786.06/1000 admissions) and 8802 (839.96/1000 admissions) (P<0.001), and the number of episodes of significant bloodstream infections was 358 (29.55/1000 admissions) and 379 (36.16/1000 admissions) in each three-month period in 2019 and 2020, respectively (P=0.007). The rate of contaminated blood cultures was 2.8% and 3.8% (P<0.001), before and during the pandemic.
The number of withdrawn catheters processed for culture in our laboratory was 302 (24.93/1,000 admissions) in 2019 and 617 (58.87/1000 admissions) in 2020 (P<0.001), and the number of positive catheter tips was 59 (4.87/1,000 admissions) and 161 (15.36/1,000 admissions) (P=0.066), respectively, in 2019 and 2020 study periods.
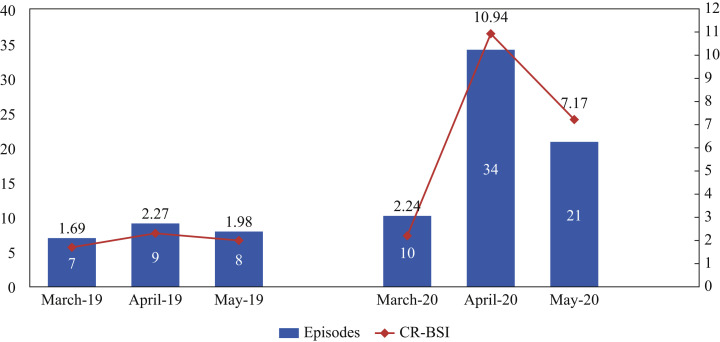
The number of patients with one or more CR-BSIs increased significantly in 2020 (Figure 1 ) (23 and 58 (1.89 vs 5.53/1000 admissions); P<0.001). The number of CR-BSI episodes in the study periods 2019 and 2020 was, respectively, 24 and 65 (1.98 vs 6.20/1000 admissions) (P<0.001). The proportion of CR-BSIs from all significant episodes of bloodstream infections was 6.7% in 2019 and 17.1% in 2020 (P<0.001).
Figure 1.
Incidence rate of catheter-related bloodstream infections (CR-BSIs)/1000 admissions during the study periods.
The underlying conditions and characteristics of both populations are compared in Table I . A high proportion of the cases of CR-BSI in 2020 occurred in COVID-19 patients (77.58%), and the vast majority of episodes occurred during their ICU stay (91.37%). The median ICU stay in patients with CR-BSIs was much longer in 2020 than in 2019 (35.0 (17.0–59.7)) vs 17.0 (0.0–52.0); P=0.042).
Table I.
Comparison of patients with catheter-related bloodstream infections (CR-BSIs) in 2019 and 2020
| Patients | Total N = 81 |
2019 N = 23 |
2020 N = 58 |
P |
|---|---|---|---|---|
| Median age in years, adults (IQR) | 65.0 (57.50–70.50) | 69.00 (58.00–73.00) | 64.50 (56.00–68.25) | 0.168 |
| Median age in years, children (IQR) | 0.0 (0.0–27.50) | 0.0 (0.0–99.00) | 0.5 (0.0–27.50) | 0.629 |
| ICU (%) | 68 (83.95) | 15 (65.21) | 53 (91.37) | 0.007 |
| Sex (%) | 0.010 | |||
| Male | 60 (74.07) | 12 (52.17) | 48 (82.75) | |
| Female | 21 (25.92) | 11 (47.82) | 10 (17.24) | |
| Underlying conditions (%) | ||||
| COVID-19 | 45 (55.55) | 0 (0.0) | 45 (77.58) | <0.001 |
| Myocardial infarction | 2 (2.46) | 0 (0.0) | 2 (3.44) | 1.000 |
| Congestive heart failure | 1 (1.23) | 0 (0.0) | 1 (1.72) | 1.000 |
| Central nervous system disease | 3 (3.70) | 2 (8.69) | 1 (1.72) | 0.193 |
| Chronic obstructive pulmonary disease | 12 (14.81) | 1 (4.34) | 11 (18.96) | 0.164 |
| Renal dysfunction | 7 (8.64) | 2 (8.69) | 5 (8.62) | 1.000 |
| Diabetes mellitus | 18 (22.22) | 5 (21.73) | 13 (22.41) | 1.000 |
| Peptic ulcer disease | 10 (12.34) | 6 (26.08) | 4 (6.89) | 0.027 |
| Peripheral vascular disease | 2 (2.46) | 1 (4.34) | 1 (1.72) | 0.490 |
| Tumour | 16 (19.75) | 11 (47.82) | 5 (8.62) | 0.001 |
| Median length of hospital stay in days (IQR) | 47.00 (29.00–83.50) | 35.00 (19.00–83.00) | 53.00 (34.75–91.75) | 0.059 |
| Median length of ICU stay in days (IQR) | 36.50 (21.25–65.75) | 17.00 (0.00–52.00) | 35.00 (17.00–59.70) | 0.042 |
| Other infections (%) | 57 (70.37) | 10 (43.47) | 47 (81.03) | 0.002 |
| Mortality (%) | 32 (39.50) | 7 (30.43) | 25 (43.10) | 0.325 |
| Mortality attributable to CR-BSI (N = 32) (%) | 12 (37.5) | 2 (28.57) | 10 (40.00) | 0.465 |
ICU, intensive care medicine; IQR, interquartile range.
In 2019, 10 patients developed nosocomial infection (five of them had two or more infections): six urinary tract infections, eight respiratory infections, one surgical wound infection and one cytomegalovirus disease. Of these 10 patients, nine (90%) were in the ICU. In 2020, 47 patients developed nosocomial infection (22 had two or more infections): 15 urinary tract infection, 23 respiratory infections, one surgical wound infection, 13 cytomegalovirus disease, one Clostridioides difficile infection and six bloodstream infections. Forty-six patients (97.8%) were in the ICU.
The characteristics of the catheters in both populations are summarized in Table II . A large proportion of catheters in the 2020 patients were non-tunneled central lines (64.6%), and, of these, 78.6% were inserted into the jugular vein partially due to the prone position.
Table II.
Characteristics of the catheters
| Catheters | Total N = 89 |
2019 N = 24 |
2020 N = 65 |
P |
|---|---|---|---|---|
| Type of catheter, adults, N (%) | ||||
| Non-tunneled central venous | 49 (55.05) | 7 (29.16) | 42 (64.61) | 0.004 |
| Tunneled central venous | 12 (13.48) | 8 (33.33) | 4 (6.15) | 0.204 |
| Peripheral venous catheter | 3 (3.37) | 0 (0.0) | 3 (4.61) | 1.000 |
| Peripherally inserted central catheter | 15 (16.85) | 1 (4.16) | 14 (21.53) | 0.277 |
| Arterial | 10 (11.23) | 8 (33.33) | 2 (3.07) | 1.000 |
| Location of non-tunneled central venous, N=49 (%) | ||||
| Jugular | 35 (71.42) | 2 (28.57) | 33 (78.57) | 0.015 |
| Subclavian | 8 (16.32) | 4 (57.14) | 4 (9.52) | 0.009 |
| Femoral | 6 (12.24) | 1 (14.28) | 5 (11.90) | 1.00 |
| Catheter days, median (IQR) | 17.00 (11.00–28.50) | 27.50 (11.75–126.00) | 16.00 (11.00–23.50) | 0.032 |
| Catheter days, total | 5222 | 3637 | 1585 | NA |
IQR, interquartile range.
Median time from insertion to demonstration of CR-BSIs was 27.5 days (range, 11.75 to 126.00 days) in the 2019 cases and 16.0 days (range, 11.00–23.50 days) in 2020 (P=0.032).
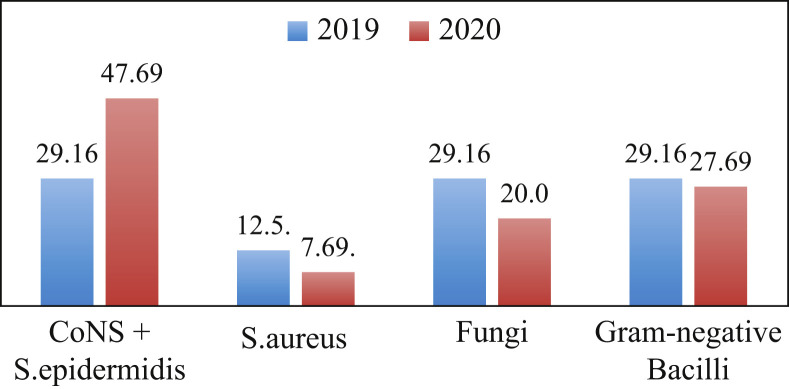
The comparative aetiologies of the CR-BSI episodes in 2019 and 2020 are shown in Figure 2 . We were unable to detect significant differences in the proportion of causative micro-organisms of CR-BSIs between the 2019 cases and the 2020 cases.
Figure 2.
Aetiology of episodes of catheter-related bloodstream infection (CR-BSI). Percentages of micro-organisms causing CR-BSI in 2019 and 2020.
The attributable mortality of CR-BSIs, in 2019 and 2020 was 28.6% and 40.0%, respectively (P=0.465).
Discussion
Our results demonstrate the substantial quantitative and qualitative impact of the COVID-19 pandemic in CR-BSI. The incidence of CR-BSI increased at least three-fold during the first 3 months of the COVID-19 pandemic in our institution.
The damage caused by the COVID-19 pandemic in different aspects of healthcare and infection control has been devastating, although not yet sufficiently analysed [[16], [17], [18], [19], [20]]. At the beginning of the pandemic, it was already anticipated that patients with severe COVID-19 would develop superinfections, most commonly pneumonia due to nosocomial bacteria and invasive aspergillosis [21,22]. This was confirmed, and, nosocomial secondary infections have been estimated to have occurred in between 7% and 14.3% of hospitalized COVID-19 patients (95% confidence interval, 9.6–18.9%) [23,24]; these infections are more frequent in ICU patients [25,26].
Most common secondary infections in this population are nosocomial pneumonia, mainly associated with mechanical ventilation [27], and bloodstream infections. The most frequent micro-organisms, as expected, were Staphylococcus aureus, Enterococcus spp., Escherichia coli, and Pseudomonas aeruginosa [24]. The infections frequently involved multi-drug-resistant micro-organisms [[25], [26], [27], [28], [29]]. Surprisingly, and despite overuse of antibiotics during the pandemic, preliminary data suggest that the incidence of C. difficile infection decreased in COVID-19 cases [[30], [31], [32], [33]].
Fungal superinfections are also a considerable problem [33,34] and include invasive candidiasis and candidaemia [35], coronavirus-associated pulmonary aspergillosis [[36], [37], [38], [39]], and even Saccharomyces fungaemia [40].
Interestingly, data on episodes of bacteraemia were contradictory in the initial reports of the pandemic period and usually do not specify the policy of blood cultures drawing in different institutions [41,42]. However, it seems clear that prolonged hospital stay, in ICUs, has led most authors to report an increase in episodes of bacteraemia [43].
Our series includes 81 patients with proven CR-BSIs and compared a similar time period in 2019 and 2020; we found that the frequency of CR-BSIs increased three-fold during the COVID-19 period. Very recently, Le Rose et al. [30] reported an increase in the incidence of vascular catheter-related infections during the pandemic. The authors analysed a series of bloodstream infections, with no clear portal of entry, that they related with central-line-associated bloodstream infection (CLABSI). Of the 36 patients who developed CLABSI, six (17%) were in a pre-COVID-19 cohort, while 30 (83%) were in the COVID-19 cohort. The average monthly CLABSI rate increased from 0.40 to 1.7 during COVID-19 (P<0.01). Data from an Italian institution showed that 30% of all BSI episodes during the COVID-19 pandemic originated in endovascular catheters [44]. In our study, this proportion is lower because we included only microbiologically confirmed episodes (CR-BSIs).
In our study 93.7% of the patients with CR-BSI during the pandemic period were in the ICU, in addition these patients received high doses of steroids and most of them were in the prone position, all risk factors for developing more nosocomial infections as described in other studies [43,44]. The use of the prone position to improve ventilation is used in many ICUs, and poses difficulties for both insertion and care of endovascular catheters and has been related to higher risk of CVC infectious complications [45,46].
Patients who developed CLABSI in the pre–COVID-19 cohort had a median length of stay of 19 days compared with patients in the COVID-19 cohort, who had a median length of stay of 27 days (P=0.12) [30]. However, in our study, despite a longer ICU stay, episodes of CR-BSI occurred earlier after catheter insertion than in 2019. If we combine these findings with an increased rate of contaminated blood cultures and a higher proportion of CR-BSI caused by coagulase-negative staphylococci, we can conclude that catheter insertion and care worsened.
Other risk factors reported in the literature include the use of corticosteroids and tocilizumab, although we have little insight into the role that other risk factors may have in these patients [44].
In our study, the micro-organisms causing CR-BSI were mainly Gram-positive. Other authors, analysing the aetiologies of CLABSI in a COVID-19 cohort, reported that 53.3% were caused by Gram-positive bacteria, followed by 26.7% fungal and 20% Gram-negative bacteria [30].
The main limitation of our study is that it was performed in a single hospital and further studies with multi-centre data would be welcome. While our study reflects findings from a single hospital, we believe that it appropriately quantifies a problem that may well have affected many centres throughout the world.
We hope that our findings will contribute to urge health professionals to immediately reinforce nosocomial infection control measures. These figures should and can be lowered [5,47].
Acknowledgements
We thank Thomas O'Boyle for his help in the preparation of the manuscript.
Author contributions
E.B. and M.J.P.G. participated in the conception and design of the study, carried out the analysis, interpreted the data and drafted the manuscript. C.S., P.M.R., M.V., M.O. and PM collected the samples and data and participated in drafting the manuscript. All of the authors read and approved the final version of the manuscript.
Conflict of interest statement
The authors declare no conflicts of interest.
Funding sources
This study was supported in part by CIBER Enfermedades Respiratorias-CIBERES (CB06/06/0058), Madrid, Spain; by grants from the ISCIII (PI20/00575) II-PI-ENF-1-2019 and the European Regional Development Fund (FEDER) “A way of making Europe”. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Stevens V., Geiger K., Concannon C., Nelson R.E., Brown J., Dumyati G. Inpatient costs, mortality and 30-day re-admission in patients with central-line-associated bloodstream infections. Clin Microbiol Infect. 2014;20:O318–O324. doi: 10.1111/1469-0691.12407. [DOI] [PubMed] [Google Scholar]
- 2.Ferrer C., Almirante B. Venous catheter-related infections. Enferm Infecc Microbiol Clin. 2014;32:115–124. doi: 10.1016/j.eimc.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Rosenthal V.D., Bat-Erdene I., Gupta D., Belkebir S., Rajhans P., Zand F., et al. International Nosocomial Infection Control Consortium (INICC) report, data summary of 45 countries for 2012-2017: Device-associated module. Am J Infect Control. 2020;48:423–432. doi: 10.1016/j.ajic.2019.08.023. [DOI] [PubMed] [Google Scholar]
- 4.Pittiruti M., Pinelli F. Recommendations for the use of vascular access in the COVID-19 patients: an Italian perspective. Crit Care. 2020;24:269. doi: 10.1186/s13054-020-02997-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Timsit J.F., Baleine J., Bernard L., Calvino-Gunther S., Darmon M., Dellamonica J., et al. Expert consensus-based clinical practice guidelines management of intravascular catheters in the intensive care unit. Ann Intensive Care. 2020;10:118. doi: 10.1186/s13613-020-00713-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ceylan Z. Estimation of COVID-19 prevalence in Italy, Spain, and France. Sci Total Environ. 2020;729:138817. doi: 10.1016/j.scitotenv.2020.138817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kazemi-Karyani A., Safari-Faramani R., Amini S., Ramezani-Doroh V., Berenjian F., Dizaj M.Y., et al. World one-hundred days after COVID-19 outbreak: incidence, case fatality rate, and trend. J Educ Health Promot. 2020;9:199. doi: 10.4103/jehp.jehp_483_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang L., Wang Y., Liu J., Ye P, Chen X, Xu H, et al. Factors influencing anxiety of health care workers in the radiology department with high exposure risk to COVID-19. Med Sci Monit. 2020;26 doi: 10.12659/MSM.926008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sorbello M., El-Boghdadly K., Di Giacinto I., Cataldo R., Esposito C., Falcetta S., et al. The Italian coronavirus disease 2019 outbreak: recommendations from clinical practice. Anaesthesia. 2020;75:724–732. doi: 10.1111/anae.15049. [DOI] [PubMed] [Google Scholar]
- 11.Scoppettuolo G., Biasucci D.G., Pittiruti M. Vascular access in COVID-19 patients: smart decisions for maximal safety. J Vasc Access. 2020;21:408–410. doi: 10.1177/1129729820923935. [DOI] [PubMed] [Google Scholar]
- 12.Cataldo M.A., Tetaj N., Selleri M., Marchioni L., Capone A., Caraffa E., et al. Incidence of bacterial and fungal bloodstream infections in COVID-19 patients in intensive care: An alarming "collateral effect. J Glob Antimicrob Resist. 2020;23:290–291. doi: 10.1016/j.jgar.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonazzetti C., Morena V., Giacomelli A., Oreni L., Casalini G., Galimberti L.R., et al. Unexpectedly high frequency of enterococcal bloodstream infections in coronavirus disease 2019 patients admitted to an Italian ICU: an observational study. Crit Care Med. 2021;49:e31–40. doi: 10.1097/CCM.0000000000004748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guan W.J., Liang W.H., Zhao Y., Liang H.R., Chen Z.S., Li Y.M., et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55:2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Grady N.P., Alexander M., Burns L.A., Dellinger E.P., Garland J., Heard S.O., et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52:e162–e193. doi: 10.1093/cid/cir257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ball S., Banerjee A., Berry C., Boyle J.R., Bray B., Bradlow W., et al. Monitoring indirect impact of COVID-19 pandemic on services for cardiovascular diseases in the UK. Heart. 2020;106:1890–1897. doi: 10.1136/heartjnl-2020-317870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shapiro L.I., Kajita G.R., Arnsten J.H., Tomer Y. Toward better preparedness for the next pandemic. J Clin Invest. 2020;130:4543–4545. doi: 10.1172/JCI140296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen A., Selles R.W., De Ridder W.A., Ter Stege M.H.P., Souer J.S., Wouters R.M. What is the impact of the COVID-19 pandemic on quality of life and other patient-reported outcomes? An analysis of the hand-wrist study cohort. Clin Orthop Relat Res. 2021;479:335–345. doi: 10.1097/CORR.0000000000001514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tan E., Song J., Deane A.M., Plummer M.P. Global impact of coronavirus disease 2019 infection requiring admission to the ICU: a systematic review and meta-analysis. Chest. 2021;159:524–536. doi: 10.1016/j.chest.2020.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harrison D., Muradali K., El Sahly H., Bozkurt B., Jneid H. Impact of the SARS-CoV-2 pandemic on health-care workers. Hosp Pract. 2020;48:161–164. doi: 10.1080/21548331.2020.1771010. [DOI] [PubMed] [Google Scholar]
- 21.Dupont D., Menotti J., Turc J., Miossec C., Wallet F., Richard J.C., et al. Pulmonary aspergillosis in critically ill patients with Coronavirus Disease 2019 (COVID-19) Med Mycol. 2021;59:110–114. doi: 10.1093/mmy/myaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clancy C.J., Nguyen M.H. COVID-19, superinfections and antimicrobial development: what can we expect? Clin Infect Dis. 2020;71:2736–2743. doi: 10.1093/cid/ciaa524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Langford B.J., So M., Raybardhan S., Leung V., Westwood D., MacFadden D.R., et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26:1622–1629. doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garcia-Vidal C., Sanjuan G., Moreno-García E., Puerta-Alcalde P., Garcia-Pouton N., Chumbita M., et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect. 2021;27:83–88. doi: 10.1016/j.cmi.2020.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang H., Zhang Y., Wu J., Li Y., Zhou X., Li X., et al. Risks and features of secondary infections in severe and critical ill COVID-19 patients. Emerg Microbes Infect. 2020;9:1958–1964. doi: 10.1080/22221751.2020.1812437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barrasa H., Rello J., Tejada S., Martín A., Balziskueta G., Vinuesa C., et al. SARS-CoV-2 in Spanish Intensive Care Units: Early experience with 15-day survival in Vitoria. Anaesth Crit Care Pain Med. 2020;39:553–561. doi: 10.1016/j.accpm.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ceccarelli G., Alessandri F., Oliva A., Dell'Isola S., Rocco M., Ruberto F., et al. Superinfections in patients treated with Teicoplanin as anti-SARSCoV2 agent. Eur J Clin Invest. 2021;51 doi: 10.1111/eci.13418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nori P., Cowman K., Chen V., Bartash R., Szymczak W., Madaline T., et al. Bacterial and fungal coinfections in COVID-19 patients hospitalized during the New York City pandemic surge. Infect Control Hosp Epidemiol. 2021;42:84–88. doi: 10.1017/ice.2020.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu C.P., Adhi F., Highland K. Recognition and management of respiratory co-infection and secondary bacterial pneumonia in patients with COVID-19. Cleve Clin J Med. 2020;87:659–663. doi: 10.3949/ccjm.87a.ccc015. [DOI] [PubMed] [Google Scholar]
- 30.LeRose J., Sandhu A., Polistico J., Ellsworth J., Cranis M., Jabbo L., et al. The impact of COVID-19 response on central line associated bloodstream infections and blood culture contamination rates at a tertiary care center in the Greater Detroit area. Infect Control Hosp. 2021;42:997–1000. doi: 10.1017/ice.2020.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ponce-Alonso M., Sáez de la Fuente J., Rincón-Carlavilla A., Moreno-Nunez P., Martínez-García L., Escudero-Sánchez R., et al. Impact of the coronavirus disease 2019 (COVID-19) pandemic on nosocomial Clostridioides difficile infection. Infect Control Hosp Epidemiol. 2021;42:406–410. doi: 10.1017/ice.2020.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bentivegna E., Alessio G., Spuntarelli V., Luciani M., Santino I., Simmaco M., et al. Impact of COVID-19 prevention measures on risk of health care-associated Clostridium difficile infection. Am J Infect Control. 2021;49:640–642. doi: 10.1016/j.ajic.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heard K.L., Hughes S., Mughal N., Moore L.S.P. COVID-19 and fungal superinfection. Lancet Microbe. 2020;1:e107. doi: 10.1016/S2666-5247(20)30065-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nestler M., Godbout E., Lee K., Kim J., Noda A.J., Taylor P., et al. Fungal superinfection in patients with COVID-19: role of antifungal stewardship? Am J Infect Control. 2021;49:279–280. doi: 10.1016/j.ajic.2020.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arastehfar A., Carvalho A., Nguyen M.H., Hedayati M.T., Netea M.G., Perlin D.S., et al. COVID-19-associated Candidiasis (CAC): an underestimated complication in the absence of immunological predispositions? J Fungi (Basel) 2020;6:211. doi: 10.3390/jof6040211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bassetti M., Giacobbe D.R., Grecchi C., Rebuffi C., Zuccaro V., Scudeller L. Performance of existing definitions and tests for the diagnosis of invasive aspergillosis in critically ill, adult patients: a systematic review with qualitative evidence synthesis. J Infect. 2020;81:131–146. doi: 10.1016/j.jinf.2020.03.065. [DOI] [PubMed] [Google Scholar]
- 37.Blaize M., Mayaux J., Nabet C., Lampros A., Marcelin A.G., Thellier M., et al. Fatal invasive Aspergillosis and coronavirus disease in an immunocompetent patient. Emerg Infect Dis. 2020;26:1636–1637. doi: 10.3201/eid2607.201603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arastehfar A., Carvalho A., van de Veerdonk F.L., Jenks J.D., Koehler P., Krause R., et al. COVID-19 Associated pulmonary aspergillosis (CAPA) – from immunology to treatment. J Fungi (Basel) 2020;6:91. doi: 10.3390/jof6020091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Machado M., Valerio M., Álvarez-Uría A., Olmedo M., Veintimilla C., Padilla B., et al. Invasive pulmonary aspergillosis in the COVID-19 era: an expected new entity. Mycoses. 2021;64:132–143. doi: 10.1111/myc.13213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ventoulis I., Sarmourli T., Amoiridou P., Mantzana P., Exindari M., Gioula G., et al. Bloodstream infection by Saccharomyces cerevisiae in two COVID-19 patients after receiving supplementation of Saccharomyces in the ICU. J Fungi (Basel) 2020;6:98. doi: 10.3390/jof6030098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sepulveda J., Westblade L.F., Whittier S., Satlin M.J., Greendyke W.G., Aaron J.G., et al. Bacteremia and blood culture utilization during COVID-19 surge in New York City. J Clin Microbiol. 2020;58 doi: 10.1128/JCM.00875-20. e00875-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yu D., Ininbergs K., Hedman K., Giske C.G., Strålin K., Özenci V. Low prevalence of bloodstream infection and high blood culture contamination rates in patients with COVID-19. PLos One. 2020;15 doi: 10.1371/journal.pone.0242533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Engsbro A.L., Israelsen S.B., Pedersen M., Tingsgaard S., Lisby G., Andersen C., et al. Predominance of hospital-acquired bloodstream infection in patients with Covid-19 pneumonia. Infect Dis (Lond) 2020;52:919–922. doi: 10.1080/23744235.2020.1802062. [DOI] [PubMed] [Google Scholar]
- 44.Giacobbe D.R., Battaglini D., Ball L., Brunetti I., Bruzzone B., Codda G., et al. Bloodstream infections in critically ill patients with COVID-19. Eur J Clin Invest. Oct 2020;50 doi: 10.1111/eci.13319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Louis G., Belveyre T., Jacquot A., Hochard H., Aissa N., Kimmoun A., et al. Infection related catheter complications in patients undergoing prone positioning for acute respiratory distress syndrome: an exposed/unexposed study. BMC Infect Dis. 2021;21:534. doi: 10.1186/s12879-021-06197-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chun T.T., Judelson D.R., Rigberg D., Lawrence P.F., Cuff R., Shalhub S., et al. Managing central venous access during a health care crisis. J Vasc Surg. 2020;72:1184–1195. doi: 10.1016/j.jvs.2020.06.112. [DOI] [PMC free article] [PubMed] [Google Scholar]