Abstract
Rationale for the review
Air travel may be associated with viruses spread via infected passengers and potentially through in-flight transmission. Given the novelty of the Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, transmission associated with air travel is based on transmission dynamics of other respiratory viruses. Our objective was to provide a rapid summary and evaluation of relevant data on SARS-CoV-2 transmission aboard aircraft, report policy implications and to highlight research gaps requiring urgent attention.
Methods
We searched four electronic databases (1 February 2020–27 January 2021) and included studies on SARS-CoV-2 transmission aboard aircraft. We assessed study quality based on five criteria and reported important findings.
Key findings
We included 18 studies on in-flight SARS-CoV-2 transmission (130 unique flights) and 2 studies on wastewater from aircraft. The quality of evidence from most published studies was low. Two wastewater studies reported PCR-positive samples with high cycle threshold values (33–39). Index case definition was heterogeneous across studies. The proportion of contacts traced ranged from 0.68 to 100%. Authors traced 2800/19 729 passengers, 140/180 crew members and 8/8 medical staff. Altogether, 273 index cases were reported, with 64 secondary cases. Three studies, each investigating one flight, reported no secondary cases. Secondary attack rate among studies following up >80% of passengers and crew (including data on 10 flights) varied between 0 and 8.2%. The studies reported on the possibility of SARS-CoV-2 transmission from asymptomatic, pre-symptomatic and symptomatic individuals. Two studies performed viral cultures with 10 positive results. Genomic sequencing and phylogenetic analysis were performed in individuals from four flights.
Conclusion
Current evidence suggests SARS-CoV-2 can be transmitted during aircraft travel, but published data do not permit any conclusive assessment of likelihood and extent. The variation in design and methodology restricts the comparison of findings across studies. Standardized guidelines for conducting and reporting future studies of transmission on aircraft should be developed.
Keywords: COVID-19, SARS-CoV-2, transmission, aircraft
Introduction
SARS-CoV-2 is a new coronavirus strain that spreads rapidly. The World Health Organization (WHO), national governments and public health officials have been working to coordinate the response and rapid development of prevention, control and management measures on several fronts. The overarching aim is to control COVID-19 by suppressing the transmission of the virus and to prevent associated illness and death.1 However, the transmission of the SARS-CoV-2 virus and the many facets of the illness it causes are incompletely understood, and public health measures for restricting transmission are based on best available information.2
Air travel may be associated with the spread of viruses via infected passengers and potentially through in-flight transmission. The high number of passengers, frequently in close proximity to each other, increases the likelihood of transmitting infectious diseases via micro-organisms which may be spread through multiple routes of transmission. As in other closed/semi-closed settings, the on-board transmission of viruses can be facilitated by direct person-to-person contact, contact with contaminated surfaces3–5 and droplet transmission. The risk of transmission of infections depends on contact among passengers at the departure gate, proximity to an index case, passengers, crew movement and fomites.6,7
The WHO and the European Centre for Disease Prevention and Control (ECDC) have elaborated specific guidance recommendations for case management in air transport for several pathogens.3,8
Given the novelty of SARS-CoV-2, air travel transmission models of spread are based on what is known of the dynamics of other respiratory infections, especially those due to other coronaviruses and influenza. One of the most important aspects of models of spread is the uncertainty regarding the modes and circumstances of transmission of newly identified agents. Consequently, research is ongoing to understand SARS-CoV-2 modes of transmission, with a continuous array of new publications. As a result, there is a need to continuously and systematically conduct reviews of available studies with the latest knowledge to inform recommendations using the most up-to-date information.
Objectives
Our objectives were to provide a rapid summary and evaluation of relevant data on the transmission of SARS-CoV-2 aboard aircraft, report important policy implications and highlight research areas urgently needed. This transmission area includes airborne, contact and droplet, fomite and orofecal.
Methods
The present work is an open evidence review on the transmission of SARS-CoV-2 in aircraft. The protocol (Supplementary Material S1 available as Supplementary data at JTM online) was developed based on a previous protocol for a series of systematic reviews on the evidence on transmission dynamics of COVID-19 (Supplementary Material S2 available as Supplementary data at JTM online) (see https://www.cebm.net/evidence-synthesis/transmission-dynamics-of-covid-19/ for the original protocol).
For this review, we conducted searches in the following electronic databases: LitCovid, medRxiv, Google Scholar and the WHO Covid-19 database up to 27 January 2021. Search terms were Covid-19, SARS-CoV-2, transmission and airplane appropriate synonyms (Supplementary Material S3 available as Supplementary data at JTM online). In addition, we screened for additional studies the reference lists of relevant articles, including reviews and the systematic review on close contact transmission of SARS-CoV-2.9 We did not impose any language restrictions.
We included studies reporting on the on-board transmission of SARS-CoV-2 from passengers and crew to passengers or crew. We considered any potential transmission mode, including droplet, airborne, fomite, fecal-oral or other. We included studies of any design, except predictive or modelling studies.
From the included studies, we extracted the following information: publication details (authors, year and country); study type; flight characteristics (origin and destination of the aircraft, flight duration, technical specifications of the airplane, ground delays and information on ventilation systems); data on the index cases (number, age, gender, country of residence or nationality, seating, whether they wore masks, symptoms during the flight and laboratory confirmation of diagnosis); details on contact-tracing (definition of contact, secondary cases demographic data, symptoms, laboratory confirmation, contact-tracing strategy, methods used to identify contacts, methods used for contacting contacts, total number of contacts identified, the total number of successfully traced contacts, the seating of contacts in relation to the index case, immunological status and if they wore or not masks); exposure of primary and secondary cases (before, during and after the flight); conclusion on disease transmission (the number of cases/number of contacted passengers and crew excluding index cases); interventions used; and source of funding for the study. One reviewer (E.C.R.) extracted data from the included studies, and these were independently checked by a second reviewer (C.H.).
We assessed the quality of included human studies on a modified QUADAS-2 tool using five criteria: (i) a clearly defined setting (aircraft details, location of index cases and secondary cases); (ii) demographic characteristics (age and gender), sampling procedures adequately described with the day of the sampling procedure and data on symptoms (with onset day); (iii) follow-up duration sufficient for the outcomes; (iv) the transmission outcomes assessed adequately (including demographic, clinical and paraclinical data); (v) main biases that are threats to validity taken into consideration (follow up >80% of individuals, alternative exposures excluded) (Supplementary Material S1 available as Supplementary data at JTM online). For non-human studies, we used the modified QUADAS-2 tool to assess the following aspects: (i) description of methods with sufficient detail to replicate, (ii) sample sources clear, (iii) analysis and reporting appropriate, (iv) bias assessment and (v) applicability (Supplementary Material S1 available as Supplementary data at JTM online).
The QUADAS-2 tool was adapted because the included studies were not primarily designed as diagnostic accuracy studies. One reviewer (E.C.R.) assessed the reporting quality of included studies and these were independently checked by a second reviewer (E.A.S.). Disagreements were resolved by consensus.
For studies that generated hypothesis testing of on-board COVID-19 transmission, we also assessed the strength of evidence of each study depending on the methods used to investigate the SARS-CoV-2 transmission.10 We presented the results in tabular format. We reported results of specific subgroups of studies where relevant. The included studies showed substantial heterogeneity; therefore, we considered meta-analyses inappropriate.
Results
Our searches identified 753 studies out of which 20 were considered eligible (Supplementary Material S4 available as Supplementary data at JTM online). We assessed in full text 25 studies. We excluded five studies: two narrative reviews, two modeling studies and one preprint version of an included study (Supplementary Material S5 available as Supplementary data at JTM online). In total, we included 20 studies: two studies on the wastewater from aircrafts11,12 and 18 studies considering in-flight transmission of SARS-CoV-213–30 (Supplementary Material S6 available as Supplementary data at JTM online). The main characteristics of the included studies are presented in Tables 1 and 2.
Table 1.
In-flight transmission studies
| Study | Year | Country | Number of passengers and crew | Number of index cases | Number of passengers and crew traced (%) | Number of secondary cases identified (%) | Attack rate (%) | Number of secondary cases within two rows (%) | Number of secondary cases outside the area of two rows (%) | Strength of evidence |
|---|---|---|---|---|---|---|---|---|---|---|
| Bae | 2020 | South Korea | 299 px; 10 crew; 8 medical staff | 6 px | 299 px; 10 crew; 8 medical staff (100%) | 1 px | 1/311 (0.32%) | 0 | 1 | RT-PCR, no data on Ct |
| Chen | 2020 | China | 335 px; 11 crew | 15 px | 335 px; 11 crew (100%) | 1 px | 1/331 (0.30%) | 1 | 0 | RT-PCR, no data on Ct |
| Choi | 2020 | China | 294 px; unknown no of crew members | 2 px | 2 crew (only symptomatic COVID-19 cases and known contacts of those and other cases were identified and traced) (1.36%) | 2 crew | N/A | N/A | N/A | RT-PCR, no data on Ct, GS |
| Eldin | 2020 | France | Not specified | 1 px | 3 px | 1 px | N/A | Not specified | Not specified | RT-PCR, no data on Ct |
| Hoehl | 2020 | Germany | 102 px | 7 px | 71 px (69.60%) | 2 px | 2/71. | 2 px | 0 | RT-PCR, no data on Ct; SARS-CoV-2 IgG |
| Khanh | 2020 | Vietnam | 201 px; 16 crew | 1 px | 168 px; 16 crew (83.40%) | 14px; 1 crew | 15/184 (8.15%) | 11 px | 1 px; 1 crew | RT-PCR, no data on Ct |
| Kong—flight 1 | 2021 | China | 59 px | 1 px | 58 px (98.3%) | 3 px (unclear) | N/A | 0 | 3 px | RT-PCR, no data on Ct |
| Kong—flight 2 | 2021 | China | 232 px | Unspecified | 232 px (100%) | 2 px | N/A | Not specified | Not specified | Symptomatic, exposure to COVID-19; RT-PCR negative, no data on Ct |
| Murphy | 2020 | Ireland | 49 px; 12 crew | Unknown (1 to 7) | 37 px (60.65%) | 4 to 12 | 4/41 (9.8%) to 12/48 (25%) | Not specified | Not specified | GS 5/13 px |
| Ng | 2020 | Singapore | 94 px | 2 px | 92 px (96.66%) | 1 (1.08%) | 1/92 (1.08%) | Not specified | Not specified | RT-PCR, no data on Ct |
| Nir-Paz | 2020 | Israel | 11 px | 2 px | 11 px | 0 | 0 | 0 | 0 | Index cases—RT-PCR positive (Ct 34 and Ct 24), positive viral cultures |
| Park | 2020 | Korea | Not specified | 30 px | Not specified | 1 crew | N/A | N/A | N/A | RT-PCR positive, Ct < 40 |
| Pavli—flight 1 | 2020 | Greece | 164px; 6 crew | 2 px | 163 px, 6 crew (99.41%) | 4 px, 1 crew | 5/167 (2.99%) | 4 px, 1 crew | 0 | RT-PCR, no data on Ct |
| Pavli—flights 2 | 2020 | Greece | 2203px, 110 crew | 21 px | 870px, 90 crew (41.50%) | 4 px, 1 crew | 5/960 | 4 px, 1 crew | 0 | RT-PCR, no data on Ct |
| Schwartz | 2020 | Canada | approx. 350 px, unspecified number of crew | 1 | Unclear | 0 | N/A | 0 | 0 | RT-PCR, no data on Ct |
| Speake | 2020 | Australia | 241 px | 18 px | 46 px (19.8%) | 8 px | 8/223 | 5 px | 3 px | RT-PCR; no data on Ct. GS; viral cultures |
| Swadi | 2021 | New Zealand | 86 px | 2 px | 86 px (100%) | 4 px | 4/84 (4.76%) | 4 | 0 | RT-PCR, with Ct data; GS |
| Yang | 2020 | China | 325 px | 1 px | 9 px, 9 crew (5.53%) | 9 px | N/A | Not specified | Not specified | RT-PCR, no data on Ct |
| Zhang XA—flight 1 | 2020 | China | Unspecified | 2 px | 8 px, 1 crew | 0 px | N/A | 0 | 0 | Epidemiologic data; RT-PCR negative in 1 px; RT-PCR not done in asymptomatic cases (5px, 1 crew); no data on Ct |
| Zhang XA—flight 2 | 2020 | China | 343 px, 21 crew | Unclear; minimum 3 px | 325 px, 11 crew (92.3%) | Unclear, max 7 px | N/A | Not specified | Not specified | RT-PCR, no data on Ct |
| Zhang J | 2020 | China | 14 505 | 159 px | 161 px (1.10%) | 2 px | 0.14 ‰ | Not specified | Not specified | RT-PCR, no data on Ct |
Abbreviations: px, passengers.
Table 2.
Non-human studies (wastewater studies)
| Study | Setting | Methods | Sample source | Sample n/d | Live cultures | Notes |
|---|---|---|---|---|---|---|
| Ahmed 2020 | Commercial passenger aircrafts; (i) Los Angeles–Brisbane (arrival on 26 April 2020; 117 px plus crew; duration 13 h and 52 min); (ii) Hong Kong–Brisbane (arrival on 07 May 2020; 19 px plus crew; duration 8 h and 10 min; (iii) New Delhi–Sydney (arrival on 10 May 2020; 185 passengers plus crew; duration 11 h and 23 min | Observational; seven samples were concentrated using the adsorption—extraction method and three samples were concentrated using Amicon® Ultra-15 centrifugal filter (Merck Millipore Ltd). RNA was directly extracted from the electronegative membrane using a combination of two kits (RNeasy PowerWater Kit and RNeasy PowerMicrobiome Kit; Qiagen, Hilden, Germany). The authors used five different RT qPCR assays (targeting different regions of RNA from SARS-CoV-2 genome) | Wastewater; 3 wastewater samples (1 l each) were collected from a valve at the bottom of the vacuum-truck that collects the wastewater tanks of the aircraft immediately after landing. The tanks of the aircraft and the vacuum trucks were emptied but not cleaned between flights | The results showed positive SARS-CoV-2 signals though concentrations were close to the limit of detection | N/A | Cq values of SARS-CoV-2 in RT-qPCR positive samples were near the assay limit of detection ALOD (i.e. amplified between 37 and 40 cycles). The RT-qPCR amplifications were not consistent for all RT-qPCR replicates; Cq values of the positive samples ranged from 36.3 to 39. 0 It is possible that the SARS-CoV-2 RNA detected could be carried over from other flights or residuals left in the vacuum truck |
| Albastaki 2020 | 198 commercial aircrafts from 59 airport destinations from all six continents | Observational; viral RNA was concentrated following a modified method, with an initial step of pipetting 10 ml of the wastewater sample through 11-μm pore size, 125-mm diameter cellulose filter (Z240095; Whatman®), followed by centrifuging 1.5 ml of the filtered sample at 4750 g for 30 min. Without disturbing the pellet, 400 μl of the supernatant was later centrifuged at 3500 g for 15 min through MB Spin Column from the DNeasy PowerSoil Kit® (12888-100; Qiagen, Germany), the eluted sample was collected for extraction. Viral RNA was extracted using MagMax Viral/Pathogen Kit (A42352; ThermoFisher Scientific™, MA, US) following the manufacturer manual using KingFisher™ Flex Purification System (5 400 610, ThermoFisher Scientific™, Massachusetts, US). The presence of SARS-CoV-2 RNA was tested using RT-PCR by the detection of three different genes specific to this virus; ORF1ab, N gene and S gene. The adopted qPCR methodology followed TaqPath™ Covid-19 RT-PCR Kit (A48067; ThermoFisher Scientific™, Massachusetts, US), using the manufacturer’s protocol. MS2 is used as an internal standard, and nuclease free water as a negative control. Samples were prepared and set accordingly with the total volume of 25 μl. The reactions were carried out using QuantStudio™ 5 Real-Time PCR System (A34322; ThermoFisher Scientific™, Massachusetts, US). The results were analyzed as instructed in the manual | Wastewater. A dedicated team from Dubai Airports collected samples from arriving aircrafts directly from the excretory valve beneath the airplane, using a big bucket. The wastewater was then transferred into1000-ml LDPE bottles (BNH1000BULK; Azlon®, Staffordshire, UK) and stored at room temperature waiting for processing | Percentage of positive signals showed to be 13.6%; Ct values that ranged from 33 to 36 | N/A | Ct = 33–36. 10/16 flights coming from Pakistan were found to be positive for SARS-CoV-2 RNA |
Table 3.
Quality assessment of included studies: in-flight transmission studies
| Study | Study type | Clearly defined setting | Demographic characteristics/sampling procedures adequately described | Follow-up strategy and duration sufficient for the outcomes | The transmission outcomes assessed adequately | Main threats to validity taken into consideration? | Notes |
|---|---|---|---|---|---|---|---|
| Bae 2020 | Cohort, prospective | Yes | Unclear | Yes | Unclear | Yes | No data on Ct |
| Chen 2020 | Cohort, prospective | Yes | Unclear | Yes | Unclear | Unclear | No data on Ct; case ascertainment, alternative exposures, recall bias |
| Choi 2020 | Retrospective, case series | Yes | Unclear | No | Unclear | No | No data on Ct; alternative exposures; asymptomatic px may be missed; use of GISAID |
| Eldin 2020 | Retrospective, case study | No | Unclear | No | Unclear | No | No data on Ct; no comprehensive contact-tracing (<20%); use of a database (which may be incomplete); alternative exposures |
| Hoehl 2020 | Cohort, retrospective | Yes | Unclear | No | Unclear | No | No data on Ct; use of other laboratory measures (IgG); tested only symptomatic px; >20% of px were not tested |
| Khanh 2020 | Cohort, retrospective | Yes | Unclear | Yes | Unclear | Yes | No data on Ct |
| Kong 2021—flight 1 | Cohort, retrospective | Yes | Unclear | No | Unclear | No | No data on Ct; asymptomatic cases may be missed; recall bias; alternative exposures; unclear number of secondary cases |
| Kong 2021—flight 2 | Cohort, retrospective | Yes | Unclear | No | Unclear | No | No data on Ct; asymptomatic cases may be missed; recall bias; alternative exposures |
| Murphy 2020 | Cohort, retrospective | Yes | No | No | Unclear | No | Unclear number/data of index cases and secondary cases; no data on Ct; tracing −60.65%; alternative exposures; GS in 5/13 |
| Ng 2020 | Cohort | No | Unclear | Yes | Unclear | No | No data on Ct; alternative exposure |
| Nir-Paz 2020 | Cohort | Yes | No | Yes | Unclear | Unclear | Ct—34 (1 px, with no viral vultures); no data on crew |
| Park 2020 | Cohort, retrospective | No | No | No | Unclear | No | Index cases: upper respiratory tract (n = 23) Ct = 27.0 (22.1–32.0); Lower respiratory tract (n = 27) Ct = 26.4 (22.7–28.8); secondary case: Ct < 40. no comprehensive tracing strategy; alternative exposures |
| Pavly 2020—flight 1 | Cohort, retrospective | No | Unclear | No | Unclear | No | No data on Ct; tracing strategy—within two seats; recall bias, alternative exposures |
| Pavli 2020—all flights | Cohort, retrospective | No | Unclear | No | Unclear | No | No data on Ct; tracing strategy—within two seats, recall bias |
| Schwartz 2020 | Cohort, retrospective | No | Unclear | No | Unclear | No | No data on Ct; asymptomatic cases could be missed; alternative exposures; no date of symptoms onset or RT-PCR |
| Speake 2020 | Cohort | Yes | Unclear | No | Unclear | No | No data on Ct; alternative exposures; asymptomatic cases could be missed; recall bias; use of GISAID |
| Swadi 2021 | Cohort, retrospective | Yes | Yes | Yes | Yes | No | Use of GISAID; some Ct > 25; alternative exposures |
| Yang 2020 | Case series, retrospective | No | Unclear | No | Unclear | No | No data on Ct; follow-up < 20%; alternative exposure, case ascertainment |
| Zhang XA 2020—flight 1 | Case series, retrospective | No | Unclear | No | Unclear | No | No data on Ct; follow-up – within 2 rows; asymptomatic cases were not tested; alternative exposure |
| Zhang XA 2020—flight 2 | Cohort, retrospective | Yes | Unclear | No | Unclear | No | No data on Ct; follow-up -asymptomatic cases were not tested; alternative exposure |
| Zhang J 2020 | Cohort, retrospective | No | Unclear | No | Unclear | No | No data on Ct; follow-up < 20%; no data on RT-PCR date; no data on the date of the symptom’s onset, asymptomatic cases were not tested, selection bias |
In the present review, we included two studies that were very likely based on the same flight and published independently of each other.14,28 Despite our efforts to clarify this issue (e.g. contacting the authors and the editors of the journals), we could not ascertain with certainty whether both studies report the same flight. Although there are many similarities between the results of the studies, there are also some minor discrepancies, including the number of passengers (335 vs. 325), the number of index cases (15 vs.1) and the arrival time (9:40 p.m. vs. 10:00 p.m.). We considered it to be highly unusual to have two flights arriving within 20 min of each other with full passenger loads with the same departure and arrival sites. What is most important is one investigation reported 15 cases and suggested in-flight transmission and the other suggested that the cases were incubating SARS-CoV-2 from community acquisition. Given it is likely the same flight, our findings illustrate how dramatically different conclusions were reached between the two investigations. A detailed comparison of the data extracted from the studies is presented in Supplementary Material S7 available as Supplementary data at JTM online.
Quality of included studies
None of the included studies reported a published protocol. The risk of bias assessment of the included studies is presented in Tables 3 and 4.
For the two studies on wastewater,11,12 the description of methods with sufficient detail to replicate the findings was considered adequate. The sample sources were clear, the analysis and reporting were considered appropriate and there were no concerns about their applicability. However, we considered no studies adequately addressed the potential biases (Table 4).
Regarding the in-flight transmission studies, 12/130 flights (9.2%) presented a clearly defined setting, and 1/130 flights (0.77%) adequately described demographic characteristics and sampling procedures. In 6/130 (4.6%) flights, the strategy and duration of follow-up were found sufficient for the outcome assessments. The transmission outcomes were considered to be adequately assessed for only 1/130 (0.77%) flights, and data validity concerns were taken into consideration for 2/130 (1.54%) flights (Table 3). The overall quality of the latter category of studies was considered to be low (Figure 1).
Figure 1.
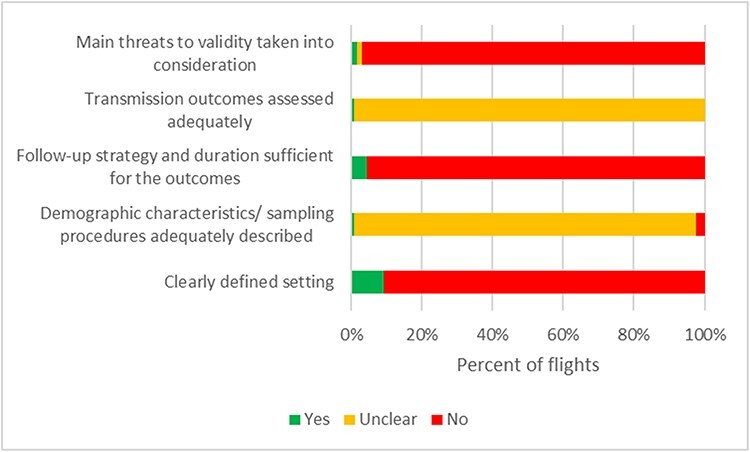
Risk of bias graph in studies on in-flight transmission of SARS-CoV-2.
Table 4.
Quality assessment of included studies: wastewater studies
| Study | Study type | Description of methods with sufficient detail to replicate | Sample sources clear | Analysis and reporting appropriate | Is bias dealt with? | Applicability | Notes |
|---|---|---|---|---|---|---|---|
| Ahmed 2020 | Observational | Yes | Yes | Yes | No | Yes | Cq values of the positive samples ranged from 36.3 to 39.0. |
| Albastaki 2020 | Observational | Yes | Yes | Yes | No | Yes | Ct of the positive samples = 33–36 |
Wastewater studies
One study investigated the wastewater from three commercial passenger aircrafts.11 The results showed positive SARS-CoV-2 RNA in the samples processed though concentrations were close to the limit of detection [quantification cycle (Cq) values ranged from 36 to 39] (Table 2). The second study12 investigated the wastewater of 198 commercial aircrafts from 59 airport destinations from all six continents. The percentage of positive SARS-CoV-2 RNA was 13.6%, with cycle threshold (Ct) values ranging from 33 to 36 (Table 2).
Studies on the in-flight transmission of SARS-CoV-2
Flight details
The total number of flights (n = 130) exceeded the number of the included studies (n = 18). Four studies reported multiple flights (see Supplementary Material S8 available as Supplementary data at JTM online): 2 flights,19,30 18 flights24 and 94 flights.29 The aircraft type was reported for 11 flights,14,15,17,22,26,27,29 and the flight numbers were provided for 6 flights.18,19,23,30 No technical specifications data on the airplanes were mentioned for 113 flights. The flight duration was reported in 15 studies, ranging from ~2 to 18 h. Nine flights were long duration, lasting >7 h; one flight was short-haul, lasting ~2 h, and five flights had a medium duration, between 3 and 5 h. Flight time was not specified in 115 flights. Ground delays were not reported by any study except for one where the aircraft had a refueling stop of 2 h, and the auxiliary power unit was inoperative for ~30 min, with inoperative ventilation.27 Data on the ventilation system were provided for only three flights. Two studies reported on the airflow in the cabin,17,29 and one study described the ventilation system.22
Case definitions: index cases, contacts and secondary cases
The definition of index case varied across the studies (see Supplementary Material S8 available as Supplementary data at JTM online) and included asymptomatic, pre-symptomatic and symptomatic individuals. A clear definition of the index cases was not provided for 103 flights, and the contact definitions differed between studies. Two studies, including 95 flights, did not provide any information on contacts. The case definitions for secondary infections were also variable, including asymptomatic and symptomatic passengers or crew.
Study types and contact-tracing strategies
The majority of included studies presented retrospective follow-up of passengers and crew after identifying one or more index cases (Table 1, Supplementary Material S8 available as Supplementary data at JTM online). Some authors also used travel and airline information data, medical records from hospitals, telephone interviews or a notifiable disease database. A prospective study with the immediate quarantine of all the passengers was done for two flights.13,21 Active daily contact monitoring was done in one study,25 and active surveillance with quarantine of >80% of the passengers and crew was reported for one flight.30 The time span for initiating follow-up ranged between the day of arrival and several months. The follow-up strategies focused on passengers seated within two rows or 2 m of the index case, passengers in the same section or class or used a comprehensive approach. In addition, crew members of 25 flights were followed up for possible transmission of SARS-CoV-2. The proportion of contacts that were identified and traced ranged from 0.6815 to 100%.13,14
In total, the authors identified 19 729 passengers, 180 crew members and 8 medical staff. Among them, they successfully traced 2.800 passengers, 140 crew members and 8 medical staff. Three studies did not report the number of passengers or crew members on the aircraft board.16,23,30
On-board transmission
Overall, 273 index cases were reported across 18 studies. However, three studies did not clearly report the number of index cases, and therefore, we considered the minimum number of index cases in each report.16,20,30
In the index cases, laboratory diagnosis was based on real-time reverse transcription–polymerase chain reaction (RT-PCR) in all 18 studies (Supplementary Material S8 available as Supplementary data at JTM online). The RT-PCR timing varied from the day of arrival to Day 11 after the flight, and passengers were reported as pre-symptomatic, symptomatic or asymptomatic. Fifteen studies report a binary result (positive/negative) for passengers or crew from 127 flights, including 239 cases.13–21,24–26,28–30 The RT-PCR Ct was reported for 34 index cases from three flights.22,23,27
Only three index cases reported in two studies had a positive RT-PCR test at a Ct value <25.22,27 One study reported that among the 30 index cases, 23 upper respiratory samples were positive at a median Ct of 27 (interquartile range: 22.1–32.0), and 27 lower respiratory tract samples were positive at a median Ct of 26.4 (interquartile range: 22.7–28.8).23
In total, 64 secondary cases were reported (59 passengers and 5 crew members). The number of secondary cases was not clear in 3 reports.19,20,30 Three studies, each investigating one flight, reported no secondary cases.22,25,30 The secondary attack rate (number of secondary cases/all successfully traced persons) among the studies that followed-up >80% of the passengers and crew,13,14,18,19,21,22,24,27,30 varied between 022 and 8.2%.18 However, genome sequencing (GS) was performed only in one study that reported a secondary attack rate of 4.76%.27
The secondary cases were asymptomatic or symptomatic individuals. The symptom onset day ranged from the 1st day after arrival to the 24th day after arrival. They presented an RT-PCR test positive for SARS-CoV-2. The sample collection timing ranged from the 2nd to the 16th day after arrival. In one study,17 the diagnosis of secondary infection was based on SARS-CoV-2 IgG antibodies, performed on Week 7 or Week 9 after the flight.
The seating position of secondary cases in relation to the index cases was specified for 24 flights across eight studies,13,14,17–19,24,26,27 with 27 passengers seated within 2 rows or 2 m14,17,18,24,26,27 and with one crew member who served the index cases,24 and four studies reported eight passengers seated outside of two rows (or presumed 2 m) from the index cases and one crew.13,18,19,26 The seating position of the secondary cases was not specified in eight studies for 102 flights.15,16,20,21,23,28–30 The location of the passengers in the aircraft, as presented by the study authors, is displayed in the Supplementary Material S9 available as Supplementary data at JTM online. Nonetheless, the images should be interpreted with caution, considering the potential risk of bias of each study. In addition, the seating plans do not account for passenger or crew movements and activities such as visiting the toilet that occur during the flight.
Regarding the use of masks, one study reported the use of N95 masks,13 one study reported the use of FFP2 masks,22 while seven studies did not report on masking of passengers or crew.15,16,18,19,23,24,30
Alternative exposures were not fully assessed in 13 studies including for 32 flights.14–16,19–21,23–28,30 Furthermore, in three studies including 21 flights, some secondary cases were family members.21,24,30
In eleven studies, asymptomatic passengers or crew members from 106 flights were not tested for SARS-CoV-2 infection.15–17,19,21,23,25,26,28–30
GS and phylogenetic analysis
GS and phylogenic analysis were performed in individuals from four flights.15,20,26,27 The methods used for performing these investigations were essentially similar across the studies (see Supplementary Material S10 available as Supplementary data at JTM online). The completeness of coverage of the positive samples ranged from 81 to 100% across the studies. The phylogenetic analysis showed >99% similarity across the entire viral genomes.
One study investigating the near full-length genomes from two index cases and two secondary cases found that they were 100% identical and phylogenetically grouped to the same clade; all deduced sequences had a minimum coverage of 100.15
In another study, the authors performed GS in 5 of the 13 flight-associated cases of SARS-CoV-2 infection. They found 99% homology across the entire virus genome in all 5 cases.20
A third study26 reported that sufficient viral RNA was available to generate an adequate sequence for 25 of the 29 samples that were RT-PCR-positive. The authors obtained 100% coverage for 21 and partial coverage (81–99%) for 4 samples. The phylogenetic tree for the 21 complete genomes revealed that they belonged to either the A.2 (n = 17) or B.1 (n = 4) sublineages of SARS-CoV-2. All of the complete A.2 sequences belonged to a distinct genomic cluster separated by < 2 single-nucleotide polymorphisms. The 4 B.1 viruses comprised 3 B.1.31 and 1 phylogenetically more distant B.1 strain. Of the four partial sequences, three clustered with the A2 strains, and the other was designated as B.1.1 and was phylogenetically close to the B.1.31 sequences.26
On another flight, the authors demonstrated that the viral sequences of the index cases and the secondary cases were assigned to lineage B.1 and were genetically identical apart from one mutation from the sample from one secondary case.27 Three studies used databases [e.g. Global Initiative on Sharing All Influenza Data (GISAID)] to identify the country of the source of infection.15,26,27
Viral cultures
Two studies22,26 performed viral culture (Table 1, Supplementary Materials S8 and S11 available as Supplementary data at JTM online). One study22 reported that one asymptomatic index case presented positive viral cultures 4 days after arrival. No data was provided on the methods used for the cultures. The Ct value of RT-PCR, performed on the first day after arrival was 24. The authors report that the passenger presented a RT-PCR positive for 26 days, but the latter Ct values are not specified.22
In another study,26 viral cultures were performed using Vero E6 cells. Specimens were inspected for cytopathic effects daily for up to 10 days. The authors attempted to culture 17 PCR-positive specimens, 9 (53%) of which grew SARS-CoV-2. Of note, 4/11 persons who were infectious on the flight had culture-positive specimens collected the next day.
Discussion
Summary of main findings
We identified 18 studies assessing the in-flight transmission of SARS-CoV-2 and 2 studies investigating the presence of the virus in the wastewater of aircrafts. The evidence from the studies reporting on the on-board transmission suggests that the risk of infection could be higher in individuals seated within two rows of the index cases. Nonetheless, identifying secondary cases seated within a greater distance limits the evidence for restricting the contact-tracing to this area.
Regarding the duration of the flight, there were short, medium and long flights with a low or a high number of secondary cases. For example, in one short flight, of ~2 h, the authors reported two index cases and five secondary cases.24 Another study investigating a flight that lasted 18 h reported two index cases and four secondary cases.27 The hypothesis on the assumption that the risk of transmission increases with the length of flight due to higher exposure postulated in other airborne diseases31 needs further investigation.
It is not clear whether the use of masks can prevent transmission of SARS-CoV-2 in flights. The flights where some of the passengers and crew used FFP2 masks22 or N95 masks13 presented an attack rate of 0 and 0.32%, respectively. However, the authors did not specify if a ‘fit test’ was performed to assess if the mask fits and seals properly so that potentially contaminated air cannot leak into the respirator. Furthermore, most of the studies did not provide clear data on the masking of passengers and crew.
The included studies reported on the possibility of SARS-CoV-2 transmission from asymptomatic, pre-symptomatic or symptomatic individuals. However, a major limitation of most studies consisted of the possibility of asymptomatic index cases transmitting the infection and of asymptomatic secondary cases not being investigated due to lack of any symptoms, lowering the quality of case ascertainment.
In addition, the number of studies that reported on Ct of RT-PCR is limited; therefore, case ascertainments are likely to be biased.10 The timeline of the sample collections also is suggestive of bias in some studies.
The four studies that performed GS and phylogenetic analysis15,20,26,27 report higher quality reliable evidence, indicating that aircraft may be a setting associated with SARS-CoV-2 transmission. The GS alone cannot prove the presence of infectious materials, as the amplicon-based methods now often used to assemble SARS-CoV-2 genome sequences require only viral RNA. Nor can amplification-based SARS-CoV-2 sequencing exclude infections caused by other agents, such as rhinoviruses and OC43. However, such methods do provide secure phylogenetic insights into the relationship between the putative index and secondary cases. Nonetheless, the use of databases like GISAID to ascertain transmission may induce bias. A recent review32 found that even though many developing countries have high numbers of SARS-CoV-2 infected cases, they have few published sequences. Such missing data could create bias in a phylogeographic analysis to elucidate the global transmission dynamics of SARS-CoV-2. Substantial gaps in global sequencing data may impede the accurate identification of a source of infection.
The positive results of viral cultures observed in two studies22,26 bring further evidence on aircraft transmission of SARS-CoV-2. The positive viral cultures of index cases indicate that infectious virus was present with potential for transmission to the secondary cases. The transmission of the virus to the secondary cases is documented by the evidence that the index case was contaminated (i.e. Ct values < 25) with infectious virus (i.e. cultivatable virus); the spread is confirmed by genetic sequencing, associated with the proof that they were clearly exposed to the virus in the environment (i.e. the route of transmission). It is noteworthy that samples from the environment were not performed in any of the studies.
Nonetheless, the authors of one study22 did not report on the methods used for viral cultures, and they did not perform GS. They report non-transmission of SARS-CoV-2 to the other passengers of the flight, based on RT-PCR results, but the Ct values of the other individuals are not provided.
The second study26 had an elegant design with GS and viral cultures. They did not provide Cts which would have provided additional insights into the relative abundance of infectious materials in the environment.
Similar to previous studies on aircraft transmission of pathogens,5 the validity of many studies is limited by the possibility of alternative exposures. Some common sites of alternative exposures include sites before the flight (i.e. waiting spaces), during flight (i.e. at the lavatory and movement of passengers during flight) and after landing (i.e. lining up to exit the aircraft, security checkpoints and documents check).
The included studies in our review focused mainly on the gate-to-gate transmission of SARS-CoV-2, relating to the aircraft portion of the trip. Nonetheless, the curb-to-curb portion of travel in the airport is also of significant importance for transmission of SARS-CoV-2 as well. The curb-to-curb passenger activities from the point at which a person arrives at the airport terminal, curbside or entrance includes the check-in, baggage drop-off, security screening, concessions, support facilities (e.g. restaurants, shopping and restrooms) and departure holding rooms at the gate area before entering the jetway to board the aircraft. After landing, the curb-to-curb passenger’s travel continues from disembarking and entering the terminal building to passing through customs checkpoints, the baggage claim area and leaving the terminal. Also, the use of buses, trams or trains is included as part of the intra-airport (between terminals and gates) activities; travel to and from the airport is excluded.
The variations observed in the contact-tracing strategies, the timeliness of contact-tracing, the proportion of passengers and crew successfully traced, the use of different case definitions, the testing strategy and case ascertainment also give rise to further doubts about the validity of the overall findings.
Our review results are consistent with the suggestion that transmission of SARS-CoV-2 can occur in aircrafts but is a relatively rare event. Similar to the close contact transmission,9 the research shows evidence of positive virus cultures as well as genomic evidence of on-board transmission in one study.26 However, definitive route(s) of transmission needs further investigation. For example, recent systematic reviews reported a lack of positive viral cultures in studies on airborne33 and fomite transmission.34 Nonetheless, a recent study has reported on the presence of significant amounts of infectious SARS-CoV-2 in the environment by focusing on cultures in the early stages of illness.35 Previous to this latter report, positive viral cultures were demonstrated mainly in studies on orofecal transmission.36
This review did not address a comparison of risk between aircraft and non-aircraft settings. Furthermore, there is currently little evidence on the risk for transmission within comparable, non-aircraft settings (i.e. enclosed spaces like theaters or subways) with air exchange filtration system, mask wearing and minimal movement once in place and with variable screening strategies before entry.
To our knowledge, no other systematic review of the literature has been undertaken to assess the evidence for transmission of SARS-CoV-2 aboard aircraft. We performed an extensive search of the literature for eligible studies, accounted for the quality of included studies and have reported outcomes (GS and viral cultures). We included results from one non-peer-reviewed study, which may affect the reliability of the review results. However, due to the ongoing pandemic, such studies could potentially be of research benefit.
The limitations in this review are mainly related to the quality of the included studies and the fact that we could not ascertain with certainty if two papers were reporting on the same flight.14,28 In addition, the data extraction was challenging due to missing, incomplete or unclear descriptions of the investigations.
Several reasons may explain the low quality of the published literature found to date. First, the current lack of standardized methodology and clear reporting criteria contribute to substantial methodological variation in SARS-CoV-2 transmission studies.37 Other factors include several variables that should be taken into account, like the technical specifications of the aircraft, flight duration, the infectivity of the index case, passenger spacing, movement and activities (i.e. eating or drinking, contact with contaminated surfaces and use of lavatory), masking practices on-board and pre-flight screening strategies.38,39 All these factors have been previously presented in earlier narrative reviews.38,39 Nonetheless, in times of a pandemic, the opportunities for rigorous studies have been challenging and are often lacking.38
In addition, we may not have identified all relevant studies examining the SARS-CoV-2 transmission of aircraft-associated transmission events. We did not include in our review lists of public health authorities from different countries. Public lists contain over 1000 flights with documentation of retrospectively known cases of SARS-COV-2 infection on-board, like the Hong Kong database (described in a previous narrative review).38 Still, analyses of these databases have not been published.38
Our findings emphasize the need for a standardized approach to investigation and reporting on the transmission of SARS-CoV-2 aboard aircraft. Future studies should aim for comprehensive assessment of passengers and crew, with a complete follow-up strategy. Factors that may influence transmission, such as infectivity of the index case (asymptomatic, pre-symptomatic or symptomatic, with or without mask), the susceptibility of passengers (previous COVID-19 infection or vaccination and wearing or not of masks) and effectiveness of exposure (proximity to the index case, duration of exposure, technical specifications of the airplane and quality of cabin air) should be consistently assessed across studies.
Research should include Ct values when reporting RT-PCR results and should describe the timing and sample collection methods. In addition, further studies, including virus isolation, GS and phylogenetic analysis, should be conducted to strengthen the current evidence. Therefore, standardization of research reporting should be a priority. Furthermore, new studies should take into account other factors that might impact transmission patterns, including natural immunity and vaccination coverage.
Conclusion
Current evidence indicates that the risk of transmission of SARS-CoV-2 aboard aircraft is low, but the published data do not permit any conclusive assessment of the likelihood and extent of the transmission. Furthermore, the quality of evidence from most published studies is low. The variation in study design and methodology restricts the analysis of findings across studies. Standardized guidelines for the reporting of future research should be developed.
Authors’ contributions
All authors contributed in equal part to the conceptualization and development of the content. J.B. conducted the searches. E.C.R. and C.H. extracted data. E.C.R. and E.A.S. completed the risk of bias assessments. E.C.R. and C.H. wrote the first draft. All authors contributed to the subsequent drafts, provided input on the study analysis and results and approved the final version.
Funding
C.H., A.P. and E.A.S also receive funding support from the National Institute of Health Research School of Primary Care Research Evidence Synthesis Working Group project 390 (https://www.spcr.nihr.ac.uk/eswg).
Conflict of interest: T.J. was in receipt of a Cochrane Methods Innovations Fund grant to develop guidance on the use of regulatory data in Cochrane reviews (2015-018). In 2014–16, he was a member of three advisory boards for Boehringer Ingelheim. T.J. was a member of an independent data monitoring committee for a Sanofi Pasteur clinical trial on an influenza vaccine. T.J. is occasionally interviewed by market research companies about Phase I or II pharmaceutical products for which he receives fees (current). T.J. was a member of three advisory boards for Boehringer Ingelheim (2014–16). T.J. was a member of an independent data monitoring committee for a Sanofi Pasteur clinical trial on an influenza vaccine (2015–17). T.J. is a relator in a False Claims Act lawsuit on behalf of the USA, which involves sales of Tamiflu for pandemic stockpiling. If resolved in the US favor, he would be entitled to a percentage of the recovery. T.J. is coholder of a Laura and John Arnold Foundation grant for development of a RIAT support center (2017–20) and Jean Monnet Network Grant, 2017–20, for The Jean Monnet Health Law and Policy Network. T.J. is an unpaid collaborator to the project Beyond Transparency in Pharmaceutical Research and Regulation led by Dalhousie University and funded by the Canadian Institutes of Health Research (2018–22). T.J. consulted for Illumina LLC on next generation gene sequencing (2019–20). T.J. was the consultant scientific coordinator for the HTA Medical Technology programme of the Agenzia per i Servizi Sanitari Nazionali of the Italian MoH (2007–19). T.J. is Director Medical Affairs for BC Solutions, a market access company for medical devices in Europe. T.J. was funded by NIHR UK and the WHO to update Cochrane review A122, physical interventions to interrupt the spread of respiratory viruses. T.J. is funded by Oxford University to carry out a living review on the transmission epidemiology of COVID-19. Since 2020, T.J. receives fees for articles published by The Spectator and other media outlets. T.J. is part of a review group carrying out Living rapid literature review on the modes of transmission of SARS-CoV-2 (WHO Registration 2020/1077093-0). He is a member of the WHO COVID-19 Infection Prevention and Control Research Working Group for which he receives no funds. T.J. is funded to co-author rapid reviews on the impact of Covid restrictions by the Collateral Global Organisation. He is also an editor of the Cochrane Acute Respiratory Infections Group. T.J.’s competing interests are also online at https://restoringtrials.org/competing-interests-tom-jefferson.
C.H. holds grant funding from the NIHR, the NIHR School of Primary Care Research, the NIHR BRC Oxford and the WHO for a series of living rapid review on the modes of transmission of SARs-CoV-2 reference WHO registration No 2020/1077093. He has received financial remuneration from an asbestos case and has given legal advice on mesh and hormone pregnancy tests cases. He has received expenses and fees for his media work, including occasional payments from BBC Radio 4 Inside Health and The Spectator. He receives expenses for teaching EBM and is also paid for his GP work in NHS out of hours (contract Oxford Health NHS Foundation Trust). He has also received income from the publication of a series of toolkit books and for appraising treatment recommendations in non-NHS settings. He is a director of CEBM, an NIHR senior investigator and an advisor to Collateral Global. He is also an editor of the Cochrane Acute Respiratory Infections Group.
D.H.E. holds grant funding from the Canadian Institutes for Health Research and Li Ka Shing Institute of Virology relating to the development of Covid-19 vaccines as well as the Canadian Natural Science and Engineering Research Council concerning Covid-19 aerosol transmission. He is a recipient of WHO and Province of Alberta funding which supports the provision of BSL3-based SARS-CoV-2 culture services to regional investigators. He also holds public and private sector contract funding relating to the development of poxvirus-based Covid-19 vaccines, SARS-CoV-2-inactivation technologies and serum neutralization testing.
J.M.C. holds grants from the Canadian Institutes for Health Research on acute and primary care preparedness for COVID 19 in Alberta, Canada, and was the primary local investigator for a Staphylococcus aureus vaccine study funded by Pfizer for which all funding was provided only to the University of Calgary. He is a co-investigator on a WHO-funded study using integrated human factors and ethnography approaches to identify and scale innovative IPC guidance implementation supports in primary care with a focus on low-resource settings and using drone aerial systems to deliver medical supplies and PPE to remote First Nations communities during the COVID 19 pandemic. He also received support from the Centers for Disease Control and Prevention (CDC) to attend an Infection Control Think Tank Meeting. He is a member and chair of the WHO Infection Prevention and Control Research and Development Expert Group for COVID 19 and a member of the WHO Health Emergencies Programme Ad hoc COVID 19 IPC Guidance Development Group, both of which provide multidisciplinary advice to the WHO, for which no funding is received and from which no funding recommendations are made for any WHO contracts or grants. He is also a member of the Cochrane Acute Respiratory Infections Group.
J.B. is a major shareholder in the Trip Database search engine (www.tripdatabase.com) as well as being an employee. In relation to this work, Trip has worked with a large number of organizations over the years, and none have any links with this work. The main current projects are with AXA and Collateral Global.
A.P. is a senior research fellow at the Centre for Evidence-Based Medicine and reports grant funding from NIHR School of Primary Care Research (NIHR SPCR ESWG project 390 and project 461) during the conduct of the study and occasionally receives expenses for teaching evidence-based medicine.
E.C.R. was a member of the European Federation of Neurological Societies/European Academy of Neurology Scientist Panel—Subcommittee of Infectious Diseases (2013–17). Since 2021, she is a member of the International Parkinson and Movement Disorder Society Multiple System Atrophy Study Group, the Mild Cognitive Impairment in Parkinson Disease Study Group and the Infection Related Movement Disorders Study Group. She was an external expert and sometimes rapporteur for COST proposals (2013, 2016, 2017, 2018 and 2019) for Neurology projects.
I.J.O. and E.A.S. have no interests to disclose.
Data availability
All data included in the review are provided in the tables or in the supplemental files.
Supplementary Material
Contributor Information
Elena C Rosca, Department of Neurology, Victor Babes University of Medicine and Pharmacy, Piata Eftimie Murgu 2, Timisoara 300041, Romania.
Carl Heneghan, Centre for Evidence Based Medicine, Nuffield Department of Primary Care Health Sciences, University of Oxford, Radcliffe Observatory Quarter, Oxford OX2 6GG, UK.
Elizabeth A Spencer, Centre for Evidence Based Medicine, Nuffield Department of Primary Care Health Sciences, University of Oxford, Radcliffe Observatory Quarter, Oxford OX2 6GG, UK.
Jon Brassey, Trip Database Ltd, Glasllwch Lane, Newport NP20 3PS, UK.
Annette Plüddemann, Centre for Evidence Based Medicine, Nuffield Department of Primary Care Health Sciences, University of Oxford, Radcliffe Observatory Quarter, Oxford OX2 6GG, UK.
Igho J Onakpoya, Department of Continuing Education, University of Oxford, Rewley House, 1 Wellington Square, Oxford OX1 2JA, UK.
David H Evans, Li Ka Shing Institute of Virology, Edmonton Alberta T6G 2E1, Canada; Department of Medical Microbiology & Immunology, University of Alberta, Edmonton, Alberta T6G 2E1, Canada.
John M Conly, Departments of Medicine, Microbiology, Immunology & Infectious Diseases, and Pathology & Laboratory Medicine, Synder Institute for Chronic Diseases and O’Brien Institute for Public Health, Cumming School of Medicine, University of Calgary and Alberta Health Services, Calgary T2N 2T9, Canada.
Tom Jefferson, Department of Continuing Education, University of Oxford, Rewley House, 1 Wellington Square, Oxford OX1 2JA, UK.
References
- 1. WHO . Operational Planning Guidance to Support Country Preparedness and Response. 2020. https://www.who.int/publications/i/item/draft-operational-planning-guidance-for-un-country-teams (23 March 2021, date last accessed).
- 2. EASA . COVID-19 Aviation Health Safety Protocol. Operational Guidelines for the Management of Air Passengers and Aviation Personnel in Relation to the COVID-19 Pandemic. 2020. https://www.ecdc.europa.eu/sites/default/files/documents/EASA-ECDC_COVID-19_Operational-guidelines-for-management-of-passengers-issue-2.pdf (29 June 2021, date last accessed).
- 3. ECDC . Risk Assessment Guidelines for Infectious Diseases Transmitted on Aircraft (RAGIDA) - Influenza. 2014. https://www.ecdc.europa.eu/en/publications-data/risk-assessment-guidelines-infectious-diseases-transmitted-aircraft-ragida#no-link.(23 March 2021, date last accessed).
- 4. Leitmeyer K. European risk assessment guidance for infectious diseases transmitted on aircraft--the RAGIDA project. Euro Surveill Apr 21 2011; 16:19845. [PubMed] [Google Scholar]
- 5. Leitmeyer K, Adlhoch C. Review article: influenza transmission on aircraft: a systematic literature review. Epidemiology Sep 2016; 27:743–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. ECDC . European Centre for Disease Prevention and Control. Infectious Diseases on Aircraft. 2017. https://www.ecdc.europa.eu/en/all-topics-z/travellers-health/infectious-diseases-aircraft (30 March 2021, date last accessed).
- 7. Hertzberg VS, Weiss H. On the 2-row rule for infectious disease transmission on aircraft. Ann Glob Health Sep-Oct 2016; 82:819–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. WHO . WHO Technical Advice for Case Management of Influenza A(H1N1) in Air Transport. 2009. https://www.who.int/ihr/travel/A(H1N1)_air_transport_guidance.pdf (14 August 2021, date last accessed).
- 9. Onakpoya IJ, Heneghan CJ, Spencer EA et al. SARS-CoV-2 and the role of close contact in transmission: a systematic review [version 1; peer review: awaiting peer review]. F1000Research 2021; 10:280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jefferson T, Heneghan C, Spencer E et al. A hierarchical framework for assessing transmission causality of respiratory viruses. Preprints. 2021, 2021040633. doi: 10.20944/preprints202104.0633.v1. [DOI] [PMC free article] [PubMed]
- 11. Ahmed W, Bertsch PM, Angel N et al. Detection of SARS-CoV-2 RNA in commercial passenger aircraft and cruise ship wastewater: a surveillance tool for assessing the presence of COVID-19 infected travellers. J Travel Med 2020; 27:taaa116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Albastaki A, Naji M, Lootah R et al. First confirmed detection of SARS-COV-2 in untreated municipal and aircraft wastewater in Dubai, UAE: the use of wastewater based epidemiology as an early warning tool to monitor the prevalence of COVID-19. Sci Total Environ Mar 15 2021; 760:143350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bae SH, Shin H, Koo HY, Lee SW, Yang JM, Yon DK. Asymptomatic transmission of SARS-CoV-2 on evacuation flight. Emerg Infect Dis Nov 2020; 26:2705–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chen J, He H, Cheng W et al. Potential transmission of SARS-CoV-2 on a flight from Singapore to Hangzhou, China: an epidemiological investigation. Travel Med Infect Dis 2020; 36:101816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Choi EM, Chu DKW, Cheng PKC et al. In-flight transmission of SARS-CoV-2. Emerg Infect Dis Nov 2020; 26:2713–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Eldin C, Lagier J-C, Mailhe M, Gautret P. Probable aircraft transmission of Covid-19 in-flight from the Central African Republic to France. Travel Med Infect Dis 2020; 35:101643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hoehl S, Karaca O, Kohmer N et al. Assessment of SARS-CoV-2 transmission on an international flight and among a tourist group. JAMA Netw Open Aug 3 2020; 3:e2018044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Khanh NC, Thai PQ, Quach HL et al. Transmission of SARS-CoV 2 during long-haul flight. Emerg Infect Dis Nov 2020; 26:2617–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kong D, Wang Y, Lu L et al. Clusters of 2019 coronavirus disease (COVID-19) cases in Chinese tour groups. Transbound Emerg Dis 2021; 68:684–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Murphy N, Boland M, Bambury N et al. A large national outbreak of COVID-19 linked to air travel, Ireland, summer 2020. Euro Surveill Oct 2020; 25:2001624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ng OT, Marimuthu K, Chia PY et al. SARS-CoV-2 infection among travelers returning from Wuhan, China. N Engl J Med Apr 9 2020; 382:1476–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nir-Paz R, Grotto I, Strolov I et al. Absence of in-flight transmission of SARS-CoV-2 likely due to use of face masks on board. J Travel Med 2020; 27:taaa117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Park JH, Jang JH, Lee K, Yoo SJ, Shin H. COVID-19 outbreak and presymptomatic transmission in pilgrim travelers who returned to Korea from Israel. J Korean Med Sci Dec 14 2020; 35:e424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pavli A, Smeti P, Hadjianastasiou S et al. In-flight transmission of COVID-19 on flights to Greece: an epidemiological analysis. Travel Med Infect Dis Nov-Dec 2020; 38:101882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schwartz KL, Murti M, Finkelstein M et al. Lack of COVID-19 transmission on an international flight. Can Med Assoc J 2020; 192:E410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Speake H, Phillips A, Chong T et al. Flight-associated transmission of severe acute respiratory syndrome coronavirus 2 corroborated by whole-genome sequencing. Emerg Infect Dis Dec 2020; 26:2872–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Swadi T, Geoghegan JL, Devine T et al. Genomic evidence of in-flight transmission of SARS-CoV-2 despite predeparture testing. Emerg Infect Dis Mar 2021; 27:687–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yang N, Shen Y, Shi C et al. In-flight transmission cluster of COVID-19: a retrospective case series. Infect Dis (Lond) Nov-Dec 2020; 52:891–901. [DOI] [PubMed] [Google Scholar]
- 29. Zhang J, Li J, Wang T et al. Transmission of SARS-CoV-2 on Aircraft. 2020. Available at SSRN: https://ssrn.com/abstract=3586695 or 10.2139/ssrn.3586695. [DOI]
- 30. Zhang XA, Fan H, Qi RZ et al. Importing coronavirus disease 2019 (COVID-19) into China after international air travel. Travel Med Infect Dis May-Jun 2020; 35:101620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dowdall NP, Evans AD, Thibeault C. Air travel and TB: an airline perspective. Travel Med Infect Dis Mar 2010; 8:96–103. [DOI] [PubMed] [Google Scholar]
- 32. Furuse Y. Genomic sequencing effort for SARS-CoV-2 by country during the pandemic. Int J Infect Dis Feb 2021; 103:305–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Heneghan CJ, Spencer EA, Brassey J et al. SARS-CoV-2 and the role of airborne transmission: a systematic review [version 1; peer review: 1 approved with reservations, 2 not approved]. F1000Research 2021; 10:232. [Google Scholar]
- 34. Onakpoya IJ, Heneghan CJ, Spencer EA et al. SARS-CoV-2 and the role of fomite transmission: a systematic review [version 3; peer review: 2 approved]. F1000Research 2021; 10:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lin Y-C, Malott RJ, Ward L et al. Detection and quantification of infectious severe acute respiratory coronavirus-2 in diverse clinical and environmental samples from infected patients: evidence to support respiratory droplet, and direct and indirect contact as significant modes of transmission. medRxiv 2021.07.08.21259744. 10.1101/2021.07.08.21259744. [DOI]
- 36. Heneghan CJ, Spencer EA, Brassey J et al. SARS-CoV-2 and the role of orofecal transmission: a systematic review [version 1; peer review: 1 approved with reservations]. F1000Research 2021; 10:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jefferson T, Spencer EA, Brassey J et al. Transmission of SARS-CoV-2 from pre and asymptomatic infected individuals. A systematic review. medRxiv 2021.07.28.21261254. 10.1101/2021.07.28.21261254. [DOI] [PMC free article] [PubMed]
- 38. Freedman DO, Wilder-Smith A. In-flight transmission of SARS-CoV-2: a review of the attack rates and available data on the efficacy of face masks. J Travel Med 2020; 27:taaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Khatib AN, Carvalho A-M, Primavesi R, To K, Poirier V. Navigating the risks of flying during COVID-19: a review for safe air travel. J Travel Med 2020; 27:taaa212. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data included in the review are provided in the tables or in the supplemental files.


