Abstract
Aims
The novel coronavirus pandemic (COVID-19) has impacted the lives of people worldwide since March 2020. Social restrictions aimed at flattening the curve may be associated with an increase in mental health problems and have raised concerns regarding their effect on alcohol consumption. The objective of this study was to characterize changes in alcohol use during lockdown in Ireland and associations with drinking motives and psychopathological symptoms.
Methods
We collected data from 713 adults (aged 18–60) during the second lockdown period (October/December 2020). By means of an online survey, participants self-reported their alcohol use before COVID and during lockdown. Motives to drink and psychopathological symptoms were also recorded.
Results
Our findings showed that 66% decreased their alcohol consumption, while 15% increased their alcohol consumption. An older age and coping motives were the strongest predictors of increased alcohol use during lockdown. Depression and hostility were the specific psychopathological dimensions associated with drinking to cope.
Conclusions
Older adults who drink to cope—mainly with depression symptomatology—are an important at-risk population, in line with predictions from alcohol self-medication frameworks. Future research is needed to incorporate strategies into the public mental health ecosystem.
INTRODUCTION
On 11 March 2020, the World Health Organization declared the COVID-19 outbreak a global pandemic, which has massively impacted the lives of people worldwide (WHO, 2020a). Unprecedented measures were adopted to contain the spread of virus, focusing on social distancing and lockdown measures, such as stay-at-home orders, the closure of non-essential businesses and schools, etc. The unprecedented contextual factors surrounding COVID-19, including widespread lost income, health-related concerns or social isolation, are likely risk factors for increases in mental health problems and substance abuse among the general population around the world (González-Sanguino et al., 2020; Rehm et al., 2020; Avery et al., 2020a; Wang et al., 2021). The use of alcohol as a coping mechanism in response to stressful life events and societal crises (Rehm et al., 2020) is well stablish and underscores that individuals who drink for coping reasons are those at heightened risk to develop alcohol problems (Skrzynski and Creswell, 2020). Furthermore, alcohol misuse is of important concern in the context of the current crisis as it exacerbates psychopathological symptoms in a vicious circle (Anker et al., 2017), increases the risk of domestic violence (White and Chen, 2002; Kaysen et al., 2007) and weakens the immune system (Molina et al., 2010; Testino, 2020), reducing immunity to viral infections.
It is therefore important to determine the unique psychopathological symptoms associated with drinking motives and changes in alcohol consumption linked to COVID lockdown restrictions to provide the basis for targeted interventions. In comparison with other crisis (e.g., natural disaster, economic crisis), the particularizes of the COVID pandemic lies in radical changes to our social lives resulting in reduced environmental/social rewards, which—as behavioral theories of depression posit—is likely to increase frustration and depression levels (Lewinsohn, 1974; McPhee et al., 2020). Such drastic changes affect also the context in which drinking episodes occur and—likely—the motives to drink. Motivational models of alcohol use (Cooper, 1994) define motives to drink by two dimensions: type of reinforcement (positive/negative) and the source of the effects (internal/external) (e.g., external-positive characterize social motives and internal-negative characterize coping motives).
Earlier studies from March/April have shown changes in alcohol consumption in the initial phase of the pandemic (i.e., one month into the first lockdown). Overall, the majority of people reported a decrease in alcohol consumption during lockdown, while a minority reported an increase. Increases appear more evident among older adults than younger adults (Boschuetz et al., 2020; Callinan et al., 2020) and stress and depression were consistently reported as predictor of such increase (David, 2013; Dumas et al., 2020; Grossman et al., 2020; McPhee et al., 2020; Avery et al., 2020a). Only a few studies have investigated the role of motives to drink during the early stage of the pandemic (in university students (Bollen et al., 2021); adults (Wardell et al., 2020)), highlighting the role of coping motives in increased alcohol use. To our knowledge, only one (McPhee et al., 2020) has focused on investigated the links between motivational and psychopathological factors, showing depression symptoms and coping motives as crucial determinants for severity of alcohol use during the early weeks of the COVID-19 pandemic.
Despite the importance of investigating these relationships during the first weeks of lockdown, maladaptive emotional regulations strategies such as drinking to cope are more likely to manifest at later stages in those individuals who lack adaptive methods to effectively cope with accumulated frustration, isolation and negative affect derived from maintained social restrictions and other COVID distress factors (Brooks et al., 2020; Rogers et al., 2020). The unparalleled circumstances of Ireland, which has endured one of the longest lockdowns in Europe and was the first European country placed in a second full lockdown the 21st October 2020, offered a unique context in which to study the consequences of such restrictions in relation to alcohol consumption, motives to drink and underlying psychopathological symptoms. Therefore, by taking advantage of the second full lockdown, we sought examine which motivations to drink are linked to changes in alcohol consumption in a later stage of the pandemic when the maintenance of social (e.g., reduced interpersonal contact) and environmental restrictions (e.g., closure of public drinking venues) are more likely to impact the reasons to drink and people’s mental health, in comparison with earlier studies focused on the initial months of the pandemic.
We conducted a cross-sectional study characterizing changes in alcohol use during lockdown and the associations between drinking motives and psychopathological symptoms among adults living in Ireland. Thus, in an effort to capture the specific factors underlying drinking escalation, we identify both motivational and psychopathological risk factors controlling for other COVID contextual factors as potential sources of distress, often overlooked in previous studies. Based on traditional views on negative reinforcement (e.g., self-medication hypothesis), we hypothesized that strong coping motives will be associated with an increase of consumption during the second lockdown associated with greater psychopathological symptoms, especially depression and anxiety.
METHODS
Study design
On the 21st of October, Ireland was placed on the highest level of restrictions (Level 5) for a period of 6 weeks (stay-at-home orders, pubs and restaurants closure, non-essential moves ban, etc.) After 4 weeks of restrictions, we recruited participants via an online survey during the last two weeks of this second lockdown, that is, from the 19th of October until the 3rd of December 2020. The survey was advertised principally on social media (e.g., Twitter and Facebook) but also via email to staff and students at UCC, with the support of Communications Management team at APC Microbiome Ireland. We recruited adults from 18 to 60 years old that have lived in Ireland (at least) over the past year and reported having consumed alcohol at least once in their lifetime. The study was reviewed by the Clinical Research Ethics Committee of the Cork Teaching Hospitals and no ethical concerns were raised. This survey employed Google Forms and was completely anonymous (no personal identifiers were collected) and data were analysed and stored at UCC (Network File Store [NAS]), following UCC Data Protection Policy and no third parties were involved. The study complied with General Data Protection Regulations as well as UCC regulations for IT protection.
Participants
A total of 784 adults participated. Among them, 60 participants reported being lifetime alcohol abstainers which lead to no further data collection and finalization of the survey. We excluded 6 participants due to incomplete data and 5 participants due to anomalous data. Thus, the final dataset included 713 participants.
Measures
Alcohol consumption
In order to capture normal drinking patterns before COVID-19 started (March 2020), we used the Alcohol Use Disorder Identification Test (AUDIT) (Babor et al., 2001). As a clarification, before each of the AUDIT questions, the following specifications were included: ‘The following section refers to your alcohol consumption the year before COVID-19 restrictions started (March 2020)’. At the beginning of that section, each question was followed by a reminder of the time period referred, e.g., ‘How often did you have a drink containing alcohol? (Before March 2020)’. The AUDIT has 10 items with a score range from 0 to 40. We used the AUDIT Total and AUDIT-C (first 3 items of the AUDIT which are a validated screening instrument for problem drinking (Bush et al., 1998; Bradley et al., 2007; de Meneses-Gaya et al., 2009)). Question 1 (Q1) refers to ‘How often do you have a drink containing alcohol?’, Question 2 (Q2) refers to ‘How many drinks containing alcohol do you have on a typical day when you are drinking?’ and Question 3 (Q3) refers to binge drinking defined as ‘How often do you have six or more drinks on one occasion?’. Additionally, one more question regarding number of standard drinks (SDs) in 2 h of maximum consumption on a typical occasion was included. In Ireland, an SD unit contains 10 g of pure alcohol. All questions that referred to SD displayed a table with drinks and SD equivalences in the online survey. In order to measure alcohol consumption during lockdown, AUDIT-C together with number of drinks in the 2 h of maximum consumption and total maximum drinks in the last month (i.e., ‘In the last month, how many standard drinks did you drink in total the day you drank the most?’) were recorded. A difference score (during-lockdown score minus pre-COVID) was calculated for AUDIT-C, as well as each of its items individually Q1, Q2, Q3 and number of drinks in the 2 h of maximum consumption. A negative score indicated a reduction and a positive score indicated an increase, while zero indicated no changes. AUDIT showed good reliability in our sample (Cronbach’s alpha = 0.79).
Drinking motives
The Drinking Motive Questionnaire-Revised (DMQ–R) (Cooper, 1994) is a 20-item self-report questionnaire that assesses the relative frequency of alcohol use (on a 5-point scale, from ‘almost never’ to ‘almost always’) for reasons that relate to four different factors: enhancement (to improve positive mood state), coping (to relieve negative mood state), social facilitation (to obtain social benefits) and conformity motives (external social pressures that push an individual to conform and engage in alcohol use). People were asked to report their drinking motives with reference to the current consumption during lockdown. The Drinking Motives Questionnaire showed a very good level of reliability (Cronbach’s alpha = 0.91).
Psychopathological symptoms
Participants reported their psychopathological symptoms during lockdown (i.e., last week before filling out the survey) using the Brief Symptom Inventory (BSI) (Derogatis, 1993). This questionnaire is a short version of the SCL-R-90 with 53 items that informs of the following nine dimensions: Somatization, Obsession-Compulsion, Interpersonal Sensitivity, Depression, Anxiety, Hostility (e.g., anger, irritation), Phobic anxiety, Paranoid ideation and Psychoticism; four additional symptoms (i.e., poor appetite, sleep problems, guilt and thoughts of death) and a global index of distress, the Global Severity Index (GSI). GSI is the most sensitive indicator of the respondent’s distress level and combines information about the number of symptoms and the intensity of distress. In addition, participants reported on their levels (liker scale 0–5) of anxiety, depression and loneliness due to the current COVID situation (e.g., ‘How much do you feel the current pandemic (COVID-19, since March 2020) has increased your feelings of depression?’). In this sample, the BIS questionnaire showed an excellent level of reliability (Cronbach’s alpha = 0.97).
COVID-related distress
Participants reported on the negative impact of the COVID-19 pandemic on their life at an economical, educational, professional, social (social ties with family and friends) and health-related level (worries about own health and somebody else’s health including friends or relatives). Participants reported the negative impact of COVID-related distress in a Likert scale from 0 to 5 and the items were created based on the Report of Social Implications of COVID-19 in Ireland.
Statistical analysis
Statistical analyses were carried out in SPSS Statistics Software (version 27, Chicago, IL, USA). Descriptive statistics were explored by Pearson’s two-tailed correlations independent t-tests and chi-square tests for differences in proportions. To assess the relation between drinking motives and changes in consumption during lockdown (difference scores), we used Stepwise Multiple Regression. The models meet the assumptions of multiple regression and multicollinearity was assessed using variance inflation factor (VIF) and following a conservative criterion (VIF < 3) (Hocking, 2013). The same analytical strategy was used for the association between psychopathological symptoms and coping motives. Graphs were carried out in GraphPad Prism (version 9, La Jolla, CA, USA).
RESULTS
Sample characteristics
Descriptive statistics are depicted in Table 1 (sociodemographic variables). A detailed description of the sample by age decades can be found in supplementary material Table S1. Table 2 depicts drinking variables, motives and psychopathological symptoms. Mean age of participants was 35.77 (12.84) and 68% of respondents were females. Before COVID (March 2020), participants reported a mean AUDIT Total of 7.28 (SD = 4.43) and an AUDIT-C score of 5.05 (SD = 2.50), while during lockdown, AUDIT-C mean score was 3.37 (SD = 2.76). Males showed a more hazardous or risky alcohol consumption than females as evidenced by the AUDIT-C both before COVID ([t(707) = 5.63, P < 0.001] and during lockdown ([t(707) = 4.43, P < 0.001]. Interestingly, partial correlations (controlling for gender) showed that age negatively correlated with AUDIT-C scores before COVID (r = −0.199, P < 0.001), and conversely, age showed a positive correlation with AUDIT-C scores during lockdown (r = 0.150, P < 0.001). Before COVID, age negatively correlated with higher alcohol consumption regarding number of drinks in the 2 h of maximum consumption (r = −0.291, P < 0.001), units on a typical day (Q2) (r = −0.373, P < 0.001) and frequency of binge drinking (Q3) (r = −0.214, P < 0.001); no significant correlations were found during lockdown in the same variables, with the exception of frequency of alcohol drinking (Q1), which showed a positive correlation with age before (r = 0.230, P < 0.001) and—even stronger—during lockdown (r = 0.310, P < 0.001).
Table 1.
Sociodemographic characteristics
| Characteristics | N of respondents (%) or mean (SD) |
|---|---|
| Female/Malea | 488 (68.4%)/221 (31%) |
| Age | 35.77 (12.84) |
| County b | |
| Cork | 527 (73.9%) |
| Dublin | 40 (5.6%) |
| Kerry | 23 (3.2%) |
| Education level | |
| Third level | 642 (90.0%) |
| Secondary level | 71 (10%) |
| Housing | |
| Family unit | 496 (69.5%) |
| Sharing | 152 (21.3%) |
| Alone | 65 (9.6%) |
| Occupation | |
| Student | 219 (30.7%) |
| Workingc | 469 (65.8%) |
| Unemployed | 29 (4.1%) |
aA total of 4 people (0.6%) reported ‘Other’ as gender.
bPercentage of people living in each county (only the top three counties in the current sample were depicted in this table).
cAmong those working, 296 (41%) were working from home and 173 (24.3%) were working outside the home.
Table 2.
Drinking variables, drinking motives and psychopathology
| Characteristics | N of respondents (%) or mean (SD) | Min/Max values |
|---|---|---|
| Drinking variables | ||
| Pre-COVID | ||
| AUDIT total | 7.28 (4.43) | (0/25) |
| AUDIT-C | 5.05 (2.50) | (0/12) |
| Q1a | 2.19 (0.88) | (0/4) |
| Q2b | 1.43 (1.29) | (0/4) |
| Q3c | 1.42 (1.02) | (0/4) |
| Maximum drinks in 2 h | 3.56 (1.96) | (1/15) |
| During lockdown | ||
| AUDIT-C | 3.37 (2.76) | (0/12) |
| Q1a | 1.95 (1.21) | (0/4) |
| Q2b | 0.76 (1.06) | (0/4) |
| Q3 c | 0.66 (1.05) | (0/4) |
| Maximum drinks in 2 h | 2.72 (1.90) | (1/10) |
| Total maximum drinks | 4.49 (3.36) | (1/15) |
| Drinking motives | ||
| Enhancing | 5.73 (4.73) | |
| Coping | 3.25 (3.77) | |
| Social | 5.87 (5.17) | |
| Conformity | 1.00 (2.04) | |
| Psychopathology | ||
| GSI | 32.93 (32.94) | |
| Somatization | 3.01 (4.58) | |
| Obsession-compulsion | 5.81 (5.63) | |
| Interpersonal sensitivity | 3.48 (4.08) | |
| Depression | 5.74 (5.78) | |
| Anxiety | 4.13 (5.11) | |
| Hostility | 2.62 (3.12) | |
| Phobic anxiety | 2.55 (3.64) | |
| Paranoid ideation | 2.80 (3.80) | |
| Psychoticism | 2.74 (3.64) | |
| Additional symptoms | 3.14 (3.39) | |
| Psychiatric diagnosis | 61 (8.6%) |
a‘How often do you have a drink containing alcohol?’
b‘How many drinks containing alcohol do you have on a typical day when you are drinking?’
c‘How often do you have six or more drinks on one occasion?’
Lockdown-related changes in consumption
The percentages for different changes in drinking patterns are depicted in Table 3. Using the difference score of AUDIT-C, we observed that the majority (65.8%) of the people have decreased their consumption. Among them, only 31% decreased their risky alcohol consumption (having less than ≥4 in AUDIT-C during lockdown in comparison with pre-lockdown) (Bush et al., 1998; Bradley et al., 2007; de Meneses-Gaya et al., 2009). A total of 19.6% of participants did not change their drinking patterns and 14.6% increased their consumption. A total of 20% reported drinking more often, only 6% reported an increase in binge drinking frequency (Q3) and 10 and 12% reported an increase in units on a typical day and units during the peak of consumption (Q2 and maximum number of drinks in 2 h). No gender differences were found in the proportion of people who increased, maintained or decreased (χ2(2, N = 709) = 3.9, P = 0.140) their alcohol consumption as measured by AUDIT-C. Figure 1 represents changes in alcohol consumption during lockdown by age and age-related changes by decades can be found in supplementary material Fig. S1.
Table 3.
Changes in alcohol consumption during lockdown
| Alcohol variables | Decreased | Maintained | Increased |
|---|---|---|---|
| AUDIT-C | 469 (65.8%) | 140 (19.6%) | 104 (14.6%) |
| Q1a | 255 (35.8%) | 314 (44.0%) | 144 (20.2%) |
| Q2b | 313 (43.9%) | 328 (46.0%) | 72 (10.1%) |
| Q3c | 421 (59.0%) | 249 (34.9%) | 43 (6.0%) |
| Maximum Drinks in 2 h | 328 (46.0%) | 299 (41.9%) | 86 (12.1%) |
N of respondents (%) are reported.
a‘How often do you have a drink containing alcohol?’
b‘How many drinks containing alcohol do you have on a typical day when you are drinking?’
c‘How often do you have six or more drinks on one occasion?’
Fig. 1.
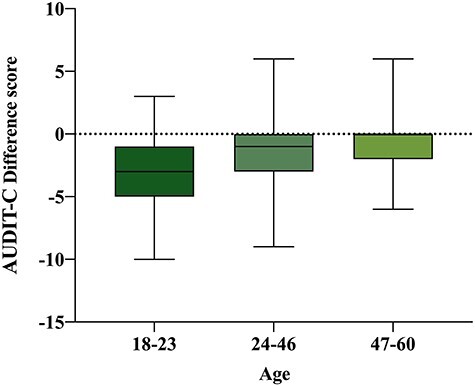
Changes in alcohol consumption during lockdown by age group; age was divided in three groups (first group represents 25th percentile and third group 75th percentile): early adulthood (18–23 years old), middle adulthood (24–46 years old) and late adulthood (47–60 years old); regarding AUDIT-C, a difference score was calculated (during-lockdown score minus pre-COVID score); a negative score indicates a reduction in alcohol use, a positive score indicates an increase and zero indicates no changes; mean values together with maximum and minimum values are represented; the older group has more positive scores representing an increase in alcohol consumption during lockdown, while the younger group has more negative scores representing an overall reduction of consumption during lockdown.
Drinking motives as predictors of consumption during lockdown
Age, coping and social motives during lockdown were predictive of AUDIT-C (difference score), the model accounted for 21% of the variance (F(3, 709) = 60.87, P < 0.001, R2Adjusted = 0.21). Age showed the strongest effect, (β = 0.368, P < 0.001), followed by coping (β = 0.296, P < 0.001) and social (β = −0.098, P = 0.010) motives. While an older age and greater coping motives significantly predicted an increase in consumption, the relationship for social motives was negative (i.e., the higher the social motives the lower the consumption during lockdown). Models accounted for gender as a covariable. When accounting for the variable housing, the same results were obtained. Coefficients for regression models can be found in Table 4. Coping motives, age and social motives accounted for 13% of the variance in drinking frequency (Q1), (F(3, 709) = 37.84, P < 0.001). Coping showed the strongest effect (β = 0.353, P < 0.001) followed by age (β = 0.191, P < 0.001) and social (β = −0.105, P < 0.001). Age and coping motives were also the best predictors for units on a typical day (Q2) (16% R2 Adjusted) and frequency of binge drinking (Q3) (9% R2 Adjusted). Regarding number of drinks in the 2 h of maximum consumption, age, coping and conformity motives significantly (β = 0.272, β = 0.225, β = −0.089) accounted for 11% of the variance (F(3, 709) = 30.81, P < 0.001), with age and coping motives again showing the strongest (positive) association with increase in consumption. Figure 2 represents drinking motives and changes in alcohol consumption during lockdown.
Table 4.
Regression coefficients for alcohol consumption, drinking motives and psychopathology during lockdown
| Model | Unstandardized coefficients | Standardized coefficients | t | P | ||
|---|---|---|---|---|---|---|
| B | SE | Beta (β) | ||||
| Model 1 | Age | 0.070 | 0.007 | 0.368 | 10.429 | 0.000 |
| Coping motives | 0.193 | 0.024 | 0.296 | 8.117 | 0.000 | |
| Social motives | -0.047 | 0.018 | -0.098 | -2.580 | 0.010 | |
| Model 2 | Depression | 0.151 | 0.036 | 0.232 | 4.173 | 0.000 |
| Hostility | 0.215 | 0.052 | 0.178 | 4.108 | 0.000 | |
| Additional symptoms | 0.184 | 0.057 | 0.166 | 3.210 | 0.001 | |
Model 1: Age, coping and social motives were the significant predictors associated with alcohol consumption measured as AUDIT-C difference score.
Model 2: Depression, hostility and additional symptoms were the significant predictors associated with coping motives for drinking.
Fig. 2.
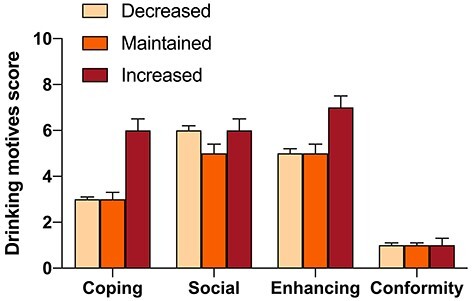
Drinking motives and changes in alcohol use during lockdown; changes in alcohol consumption during lockdown are divided in three groups: decreased, maintained and increased; a difference score was calculated using AUDIT-C (during-lockdown score minus pre-COVID score); mean values and standard error of the mean are represented.
Psychopathological symptoms associated with drinking to cope
Depression, hostility (e.g., anger, frustration) and additional symptoms (e.g., sleep problems, guilt) during lockdown accounted for 26% of the variance explaining coping motives during lockdown (F(3, 709) = 83.13, P < 0.001). Depression showed the strongest effect (β = 0.232, P < 0.001), followed by hostility (β = 0.178, P < 0.001) and additional symptoms (β = 0.166, P = 0.001). Models accounted for gender as a covariable. When accounting in the regression model for COVID-related Distress (economic impact, professional, educational, health worries and negative impact on social ties), the same psychopathological symptoms were found to be the best predictors of coping motives and no distress variables entered the model. Higher psychopathological symptoms (measured by the Global Severity Index [GSI]) during lockdown showed a positive correlation with increased levels of depression, loneliness and anxiety (r = 0.598, P < 0.001; r = 0.497, P < 0.001; r = 0.486, P < 0.001, respectively) that participants specifically attributed to the start of the COVID pandemic. Figure 3 depicts psychopathological symptoms and changes in alcohol consumption.
Fig. 3.
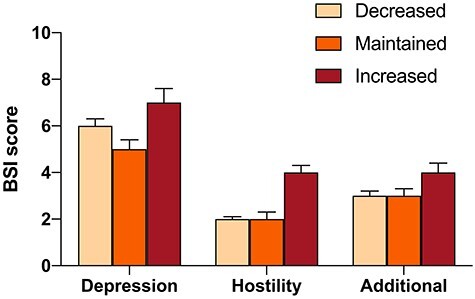
Psychopathology and changes in alcohol consumption; the three psychopathological dimensions of the BSI predictive of drinking to cope are represented (mean values and standard error of the mean) in those who decreased, maintained and increased their alcohol consumption during lockdown; additional symptoms include poor appetite, sleep problems, guilt and thoughts of death.
DISCUSSION
The goal of this study was to characterize changes in alcohol consumption during COVID lockdown restrictions and to examine motivational factors and psychopathological symptoms associated with such changes in order to help inform targeted interventions. Ireland not only has experienced one of the longest full lockdowns in Europe but also has been one of the first countries to impose a second full lockdown. This unfortunate situation provided a unique context to examine alcohol use and mental health linked to maintained environmental restrictions during a later stage of the pandemic, when more likely these changes are to manifest. We found that the majority (66%) of adults in Ireland reduced their alcohol consumption during the second lockdown, while 15% reported a significant increase in their alcohol consumption. Our results add to previous studies conducted in the first stages of the pandemic (March/April) and showing similar percentages of changes, with the majority of individuals decreasing and a worrying minority (around 14% in most studies, e.g., (Chodkiewicz et al., 2020; Avery et al., 2020b; Bollen et al., 2021)) showing increased alcohol consumption during lockdown.
An older age was the strongest predictor for increased drinking. This is of special concern in the current situation given that an older age is both a vulnerability factor for COVID and chronic heavy alcohol consumption weakens the immune system (Carbia et al., 2020) and reduces immunity to viral and bacterial infections (Molina et al., 2010; Szabo and Saha, 2015; Testino, 2020). In fact, the World Health Organization (WHO, 2020b) manifested its concern by strongly advising to reduce alcohol consumption among older adults during this unprecedented time. Regarding drinking motives, high coping motives and low social drinking motives were associated with increased consumption. These findings are in line with predictions from alcohol self-medication models (Khantzian, 1997). Environmental contingencies associated with COVID might increase the opportunities for internal negative reinforcement (e.g., ‘coping’, i.e., drinking to alleviate negative affect) and reduce the opportunities for external positive reinforcement motives to drink (e.g., ‘social’, i.e., social celebrations/parties). Previous studies have also supported the co-existence of these two motivational scenarios (Rehm et al., 2020). Interestingly, the first scenario (overall drinking reductions) seems particularly associated with young adults (Chodkiewicz et al., 2020; Bollen et al., 2021), while the second one (drinking increase) appears more evident in older adults (Callinan et al., 2020; Chodkiewicz et al., 2020; Panagiotidis et al., 2020; Oksanen et al., 2021), which highlights the especial vulnerability of this subgroup in which to focus clinical interventions. Drinking to cope in response to stressful life events or crisis (Leonard and Rothbard, 1999; Margerison-Zilko et al., 2016) has been consistently associated with the development of alcohol-related problems (Wu et al., 2008; Grant et al., 2009), a risk that seems to increase over time (Kanehara et al., 2016; Lechner et al., 2020). Coping motives were associated with higher psychopathological symptoms accounting for the effects of other COVID-related stressors such as economic impact or health worries. Those who presented higher psychopathological symptoms during the second lockdown also reported increases in depression, loneliness and anxiety specifically associated with the start of COVID pandemic. In particular, depression scores and hostility were the strongest predictors of drinking to cope. Several studies have shown that the current crisis is having a massive impact in people’s mental health, with depression and anxiety being the most common symptomatology (González-Sanguino et al., 2020; Torales et al., 2020; Vindegaard and Benros, 2020; Wang et al., 2021), and—in the context of COVID—depression seems to show strong links with increased drinking (Dumas et al., 2020; Lechner et al., 2020). Interestingly, a global study (Veer et al., 2021) has highlighted the role of internal emotional regulation strategies (i.e., a positive reappraisal or reframing of one’s thoughts) as one of the strongest protective factors against mental health problems during COVID. To our knowledge, only one study to date have jointly investigated motivational and psychopathological dimensions of drinking escalation during COVID. It has been shown that depression severity, coping motives and increased drinking (including solitary drinking) were significantly greater post-social-distancing relative to pre-social-distancing in the early stage of the pandemic (McPhee et al., 2020). Behavioral theories of depression (Lewinsohn, 1974) posit that reductions in access to environmental/social rewards (e.g., those derived from social distancing or stay-at-home orders) predict risk for depression, which might result in drinking to cope and a problematic escalation in alcohol use, especially when opportunities for healthier external emotion regulation strategies, including social interaction or physical activity, are limited. In addition, alcohol has potent anxiolytic effects (Morales-Mulia et al., 2012) which are part of the reinforcing properties of this drug, but also depressogenic effects (Hauser et al., 2011) that, in turn, are likely to exacerbate psychopathological symptoms creating a vicious circle.
Online surveys may be less accessible for some groups of people such as older adults. Future studies should extend our findings by investigating such relationships on the elderly (60 and above). Findings should be also replicated in larger samples with a more equal ratio of males/females and more diverse samples, including a better representation of low-income/education individuals. Our measures focused on self-reported and retrospective measures, which might have induced biases. Additionally, the cross-sectional nature of the current study limits causative interpretations. Even when participants reported pre-pandemic consumption, the lack of a pre-COVID-19 measure is of notable relevance when interpreting the associations observed in the current study. Longitudinal studies with pre- and post-measures are important to identify cause-effects relationships regarding the risk of increased drinking to cope and underlying psychopathological problems over time. In conclusion, the present findings highlight older adults as an especially vulnerable group for the vicious circle of drinking to cope with negative affect, conforming a target group in which to focus clinical coping skills interventions.
Authors’ contributions
C.C. and T.G.D. designed the study. C.C. and R.G.C. performed data analysis. C.C. wrote the paper and R.G.C., T.G.D. and J.F.C. contributed to the final manuscript.
Data availability statement
Data available on request. The data underlying this article will be shared on reasonable request to the corresponding author.
Supplementary Material
ACKNOWLEDGEMENTS
C.C. and R.G.-C. received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement No. 754535. APC Microbiome Ireland is a research centre funded by Science Foundation Ireland (SFI), through the Irish Government’s National Development Plan [grant no. SFI/12/RC/2273_P2].
Contributor Information
Carina Carbia, APC Microbiome Ireland, University College Cork, Cork T12 YN60, Ireland.
Rubén García-Cabrerizo, APC Microbiome Ireland, University College Cork, Cork T12 YN60, Ireland.
John F Cryan, APC Microbiome Ireland, University College Cork, Cork T12 YN60, Ireland; Department of Anatomy and Neuroscience, University College Cork, Cork T12 YN60, Ireland.
Timothy G Dinan, APC Microbiome Ireland, University College Cork, Cork T12 YN60, Ireland; Department of Psychiatry and Neurobehavioural Science, University College Cork, Cork T12 YN60, Ireland.
Conflict of interest statement
The authors declare no conflicts of interest.
References
- Anker JJ, Forbes MK, Almquist ZW et al. (2017) A network approach to modeling comorbid internalizing and alcohol use disorders. J Abnorm Psychol 126:325–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avery AR, Tsang S, Seto EYW et al. (2020a) Stress, anxiety, and change in alcohol use during the COVID-19 pandemic: findings among adult twin pairs. Front Psychiatry 11:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avery AR, Tsang S, Seto EYW et al. (2020b) Stress, anxiety, and change in alcohol use during the COVID-19 pandemic: findings among adult twin pairs. Front Psychiatry 11:1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor T, De la Fuente R, Saunders J et al. (2001) AUDIT: the Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care, 2nd edn. Geneva: WHO division of mental health. [Google Scholar]
- Bollen Z, Pabst A, Creupelandt C et al. (2021) Prior drinking motives predict alcohol consumption during the COVID-19 lockdown: a cross-sectional online survey among Belgian college students. Addict Behav 115:106772 England. [DOI] [PubMed] [Google Scholar]
- Boschuetz N, Cheng S, Mei L et al. (2020) Changes in alcohol use patterns in the United States during COVID-19 pandemic. WMJ 119:171–6 United States. [PubMed] [Google Scholar]
- Bradley KA, DeBenedetti AF, Volk RJ et al. (2007) AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res 31:1208–17 England. [DOI] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE et al. (2020) The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395:912–20 Elsevier Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB et al. (1998) The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory care quality improvement project (ACQUIP). Alcohol use disorders identification test. Arch Intern Med 158:1789–95 United States. [DOI] [PubMed] [Google Scholar]
- Callinan S, Smit K, Mojica-Perez Y et al. (2020) Shifts in alcohol consumption during the COVID-19 pandemic: early indications from Australia. Addiction 116(6):1381–88 add.15275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbia C, Lannoy S, Maurage P et al. (2020) A biological framework for emotional dysregulation in alcohol misuse: from gut to brain. Mol Psychiatry 26(4):1098–1118. [DOI] [PubMed] [Google Scholar]
- Chodkiewicz J, Talarowska M, Miniszewska J et al. (2020) Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int J Environ Res Public Health 17:4677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML. (1994) Motivations for alcohol use among adolescents: development and validation of a four-factor model. Psychol Assess 6:117–28 US: American Psychological Association. [Google Scholar]
- David DJ. (2013) Adult hippocampal neurogenesis: an actor in the antidepressant-like action. Ann Pharm Fr 71:143–9 Elsevier Masson SAS. [DOI] [PubMed] [Google Scholar]
- de Meneses-Gaya C, Zuardi AW, Loureiro SR et al. (2009) Alcohol use disorders identification test (AUDIT): an updated systematic review of psychometric properties. Psychol Neurosci 2:83–97. [Google Scholar]
- Derogatis LR. (1993) BSI Brief Symptom Inventory. Administration, Scoring, and Procedures Manual, 4th edn. Minneapolis, MN: National Computer Systems. [Google Scholar]
- Dumas TM, Ellis W, Litt DM. (2020) What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health 67:354–61 Elsevier Inc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C, Ausín B, Castellanos MÁ et al. (2020) Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 87:172–6 Elsevier Inc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant VV, Stewart SH, Mohr CD. (2009) Coping-anxiety and coping-depression motives predict different daily mood-drinking relationships. Psychol Addict Behav 23:226–37 United States. [DOI] [PubMed] [Google Scholar]
- Grossman ER, Benjamin-Neelon SE, Sonnenschein S. (2020) Alcohol consumption during the COVID-19 pandemic: a cross-sectional survey of US adults. Int J Environ Res Public Health 17:9189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser SR, Getachew B, Taylor RE et al. (2011) Alcohol induced depressive-like behavior is associated with a reduction in hippocampal BDNF. Pharmacol Biochem Behav 100:253–8 Elsevier Inc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hocking RR. (2013) Methods and Applications of Linear Models: Regression and the Analysis of Variance, 3rd edn. Hoboken, NJ: JohnWiley & Sons. [Google Scholar]
- Kanehara A, Ando S, Araki T et al. (2016) Trends in psychological distress and alcoholism after the great East Japan earthquake of 2011. SSM - Popul Heal 2:807–12 United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Dillworth TM, Simpson T et al. (2007) Domestic violence and alcohol use: trauma-related symptoms and motives for drinking. Addict Behav 32:1272–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ. (1997) The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry 4:231–44 United States. [DOI] [PubMed] [Google Scholar]
- Lechner WV, Laurene KR, Patel S et al. (2020) Changes in alcohol use as a function of psychological distress and social support following COVID-19 related university closings. Addict Behav 110:106527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard KE, Rothbard JC. (1999) Alcohol and the marriage effect. J Stud Alcohol 13:139–46 United States. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM. (1974) A behavioral approach to depression. In The Psychology of Depression: Contemporary Theory and Research. Oxford, England: John Wiley & Sons, 150–80. [Google Scholar]
- Margerison-Zilko C, Goldman-Mellor S, Falconi A et al. (2016) Health impacts of the great recession: a critical review. Curr Epidemiol Reports 3:81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPhee MD, Keough MT, Rundle S et al. (2020) Depression, environmental reward, coping motives and alcohol consumption during the COVID-19 pandemic. Front Psychiatry 11:1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina PE, Happel KI, Zhang P et al. (2010) Focus on: alcohol and the immune system. Alcohol Res Health 33:97–108. [PMC free article] [PubMed] [Google Scholar]
- Morales-Mulia M, Estrada-Camarena E, Amaya MI et al. (2012) Anxiolytic effects of ethanol are partially related to a reduced expression of adenylyl cyclase 5 but not to μ-opioid receptor activation in rat nucleus accumbens. Behav Brain Res 235:189–94 Elsevier B.V. [DOI] [PubMed] [Google Scholar]
- Oksanen A, Savolainen I, Savela N et al. (2021) Psychological stressors predicting increased drinking during the COVID-19 crisis: a longitudinal National Survey Study of Workers in Finland. Alcohol Alcohol 56:299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panagiotidis P, Rantis K, Holeva V et al. (2020) Changes in alcohol use habits in the general population, during the COVID-19 lockdown in Greece. Alcohol Alcohol 55:702–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Kilian C, Ferreira-Borges C et al. (2020) Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug Alcohol Rev 39:301–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers AH, Shepherd JM, Garey L et al. (2020) Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Res 293:113407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skrzynski CJ, Creswell KG. (2020) Associations between solitary drinking and increased alcohol consumption, alcohol problems, and drinking to cope motives in adolescents and young adults: a systematic review and meta-analysis. Addiction 115:1989–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabo G, Saha B. (2015) Alcohol’s effect on host defense. Alcohol Res 37:159–70. [PMC free article] [PubMed] [Google Scholar]
- Testino G. (2020) Are patients with alcohol use disorders at increased risk for Covid-19 infection? Alcohol Alcohol 55:344–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torales J, O’Higgins M, Castaldelli-Maia JM. et al. (2020) The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry 66:317–20. England. [DOI] [PubMed] [Google Scholar]
- Veer IM, Riepenhausen A, Zerban M et al. (2021) Psycho-social factors associated with mental resilience in the corona lockdown. Transl Psychiatry 11:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N, Benros ME. (2020) COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun 89:531–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang QQ, Kaelber DC, Xu R. et al. (2021) COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry 26:30–9. Springer US. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell JD, Kempe T, Rapinda KK et al. (2020) Drinking to cope during COVID-19 pandemic: the role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcohol Clin Exp Res 44:2073–83. [DOI] [PubMed] [Google Scholar]
- White HR, Chen P-H. (2002) Problem drinking and intimate partner violence. J Stud Alcohol 63:205–14. [DOI] [PubMed] [Google Scholar]
- WHO . (2020a) Director-General’s opening remarks at the media briefing on COVID-19. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarksat-the-media-briefing-on-covid-19—29-june-2020.
- WHO . (2020b) Alcohol and COVID-19: What You Need to Know, Vol. 19. World Heal Organ, 1–6. [Google Scholar]
- Wu P, Liu X, Fang Y et al. (2008) Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak: Table 1. Alcohol Alcohol 43:706–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available on request. The data underlying this article will be shared on reasonable request to the corresponding author.


