Purpose of review
To review the recent literature on the epidemiology of anorexia nervosa and bulimia nervosa in terms of incidence, prevalence and mortality.
Recent findings
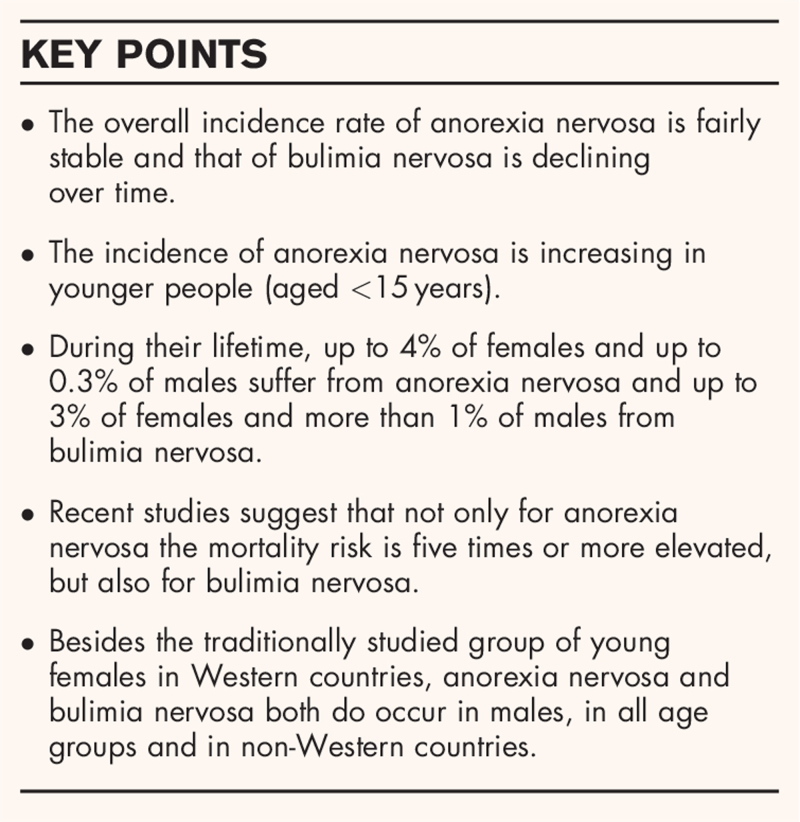
Although the overall incidence rate of anorexia nervosa is considerably stable over the past decades, the incidence among younger persons (aged <15 years) has increased. It is unclear whether this reflects earlier detection or earlier age of onset. Nevertheless, it has implications for future research into risk factors and for prevention programs. For bulimia nervosa, there has been a decline in overall incidence rate over time. The lifetime prevalence rates of anorexia nervosa might be up to 4% among females and 0.3% among males. Regarding bulimia nervosa, up to 3% of females and more than 1% of males suffer from this disorder during their lifetime. While epidemiological studies in the past mainly focused on young females from Western countries, anorexia nervosa and bulimia nervosa are reported worldwide among males and females from all ages. Both eating disorders may carry a five or more times increased mortality risk.
Summary
Anorexia nervosa and bulimia nervosa occur worldwide among females and males of all age groups and are associated with an increased mortality risk.
Keywords: anorexia nervosa, bulimia nervosa, epidemiology, mortality
INTRODUCTION
This review aims to provide an overview of the recently published studies on the epidemiology of anorexia nervosa and bulimia nervosa. It is an update of previous reviews on this subject in this journal [1–3]. For a review of the epidemiology of binge eating disorder, see Keski-Rahkonen in this issue [4].
Box 1.
no caption available
Epidemiological studies provide information about the distribution (who, when and where) of disorders in a defined population and its trends over time. For eating disorders, there are some methodological problems regarding epidemiological research. Eating disorders are relatively rare in the community and help seeking is often avoided or delayed, for example for reasons of denial (particularly in anorexia nervosa) or stigma and shame (particularly in bulimia nervosa). These factors make general population studies on eating disorders costly and ineffective. Several strategies have been used to beat this problem, in particular the use of psychiatric case registers and other medical record-based studies. We must bear in mind that the results of these studies are an underestimation of the occurrence of eating disorders in the community, because not all patients will seek help, will be detected by their general practitioner or be referred to healthcare services. Moreover, different rates over time could be due to different case detection systems and diagnostic criteria, increased awareness leading to earlier detection and referral, and broader availability of treatment facilities, instead of a true increase in occurrence [1,5].
To review the literature, we searched for articles published in English using Medline/PubMed, Embase, PsycINFO and Google Scholar, using several key terms relating to epidemiology, anorexia nervosa and bulimia nervosa. We also checked the reference lists of the articles that we found for any additional articles missed by the database search.
INCIDENCE
Incidence is the number of new cases of a disorder in a population over a specified period of time (usually 1 year). The incidence rate of eating disorders is commonly expressed per 100 000 persons per year (100 000 person-years). The study of newly developed cases of an eating disorder provides clues to unravel its etiology [6]. It is noteworthy that healthcare register-based incidence rates represent the situation at the moment of detection, which is likely to be later than the moment of disorder onset.
Incidence of anorexia nervosa
Martinez-Gonzalez et al.[7▪] conducted a systematic review and meta-analysis of 31 published studies from 1980 to 2019 on the incidence of anorexia nervosa in females, mainly from Western countries. The incidence rates varied widely depending on the methodology, population and diagnostic criteria used. They reported on the incidence rates of only three population-based studies: 120 per 100 000 person-years among Swedish females aged 20–32 years [8], 200 per 100 000 person-years among Spanish females between the age of 12 and 22 years [9] and 270 per 100 000 person-years in Finnish twin females aged 15–19 years [10]. The pooled incidence rate of studies based on outpatient healthcare services (8.8 per 100 000 person-years; 95% confidence interval, CI: 7.8–9.8) was higher than that of hospital admissions (5.0; 95% CI 4.9–5.1) [7▪]. Compared to these all-age rates, the pooled incidence rates were higher for females aged 10–29 years, both in outpatient healthcare services [63.7 per 100 000 person-years (95% CI 61.2–66.1)] and in hospital admissions [8.1 (95% CI 7.6–8.5)] [7▪]. Furthermore, for healthcare register-based studies the incidence rates of anorexia nervosa showed a significant increase over time, especially in outpatient healthcare services. This does not necessarily mean a true increase in the occurrence of anorexia nervosa, as it could represent improved public awareness, detection and treatment rates over time.
Few studies have examined the incidence of anorexia nervosa in the general population; a limitation also encountered in the systematic review by Martinez-Gonzalez et al.[7▪]. The most recent study by Silen et al.[11▪] assessed the incidence rate of anorexia nervosa between the ages of 10 and 20 years according to the Diagnostic and Statistical Manual of Mental Disorders 5th Ed. (DSM-5) criteria in Finnish twins born between 1983 and 1987, yielding an incidence rate of anorexia nervosa of 320 (95% CI 230–440) per 100 000 person-years in the total group, 580 (95% CI 430–810) per 100 000 person-years among females and 30 (95% CI 10–310) per 100 000 person-years among males. These rates are higher than the rates in females described by Martinez-Gonzalez et al.[7▪]. This might be due to the use of the ‘broader’ DSM-5 criteria for anorexia nervosa by Silen et al.[11▪], and to the fact that twins may share genetic and environmental risk factors for anorexia nervosa, leading to a potential overestimation.
Population-based incidence rates are much higher than those derived from primary care and healthcare facilities, reflecting the selection filters on the pathways to (psychiatric) care [5]. Studies in general practices present incidence rates at the earliest stage of detection within the healthcare system. There have been no recent publications on all age groups in primary care since the previous review in this journal [1], that included a Dutch primary care study [12] which examined new cases with anorexia nervosa in a large representative sample of the Dutch population. The overall incidence rate of anorexia nervosa in Dutch females and males of all ages in primary care was fairly constant during three decades: in 1985–1989 it was 7.4 (95% CI 5.6–9.7) per 100 000 person-years, in 1995–1999 7.8 (95% CI 6.0–10.1) and in 2005–2009 6.0 (95% CI 4.3–8.1) [12]. Although no new studies have been published on incidence rates of anorexia nervosa in the total primary care population, Wood et al.[13▪] investigated 11- to 24-year-olds in England and found stable incidence rates between 2004 and 2014 (27.4 per 100 000 person-years; 95% CI 26.0–29.0). Demmler et al.[14] studied the incidence rate of eating disorders (all combined) in general practices in the UK since 2008, and reported a slight decline. The authors ascribe this finding to a decreasing trend in incidence of bulimia nervosa and a stable level of anorexia nervosa incidence, but they did not report rates per eating disorder diagnosis. Another primary care study among 10- to 19-year-olds in the UK reported an increased incidence rate in the age group of 13–16 years for all eating disorders combined, comparing 2018 rates to those in 2003 [15]. It is unclear whether this reflects a true increase in incidence or a shifting in age at detection.
The study of Reas and Ro [16▪], which was included in the meta-analysis by Martinez-Gonzalez et al.[7▪], described recent time trends in the incidence of anorexia nervosa in persons aged 10–49 years, using secondary care data of the Norwegian National Patient Register. The overall incidence rates for males and females combined were stable (differences nonsignificant) from 2010 to 2016, both for narrowly defined anorexia nervosa (18.8–20.4 per 100 000 person-years) and for broadly defined anorexia nervosa (33.2–39.5 per 100 000 person-years). They were also stable per sex for narrowly defined anorexia nervosa: in females 36.3–42.3 per 100 000 person-years, and in males 2.2–4.0 per 100 000 person-years; and for broadly defined anorexia nervosa: in females 63.3–79.1 per 100 000 person-years, and in males 4.4–5.9 per 100 000 person-years. The male to female ratio was found to be 1 : 13 for narrowly defined anorexia nervosa and 1 : 14 for broadly defined anorexia nervosa. This is in accordance with other studies showing considerably lower incidence rates for males, usually by more than a factor of 10, in comparison to females [11▪,12]. The incidence of anorexia nervosa according to DSM-5 criteria in 8- to 17-year-olds was examined in secondary care services in the UK and Ireland [17]. The overall incidence rate was 13.7 (95% CI 12.9–14.5) per 100 000 person-years; in females it was 25.7 (95% CI 24.1–27.3) and in males 2.3 (95% CI 1.8–2.8).
In females, the highest incidence rate of anorexia nervosa is around the age of 15 [11▪,12,17]. Several studies report a remarkable increase in the incidence of anorexia nervosa among girls aged 10–14 years [16▪,17]. Although most research has been performed in young females, some studies report incident anorexia nervosa cases in later life as well [12,16▪]. It is noteworthy that the peri-menopausal period has been suggested as another high-risk period in female life for the onset or recurrence of eating disorders [18,19]. In males, findings regarding the peak period of anorexia nervosa onset are less clear. While some studies have shown comparable [11▪] or a somewhat higher (age 16) peak age of onset [17], others found lower peak ages of 12–13 years [20] in comparison to females.
In summary, recent studies on time trends show fairly stable incidence rates for anorexia nervosa in the last decades [12,16▪], although some healthcare register-based studies suggest an increase in the incidence of anorexia nervosa [7▪], which might be explained by greater public awareness, better detection and the use of broader diagnostic criteria. Incidence rates in males are found to be lower, usually by more than a factor 10, in comparison to females [11▪,16▪]. The rates in males should be interpreted as an underestimation because of underdetection due to a double stigma: the stigma of having a psychiatric disorder, and an additional stigma of suffering from a ‘female-specific’ disorder [21]. Finally, the finding that the incidence of anorexia nervosa is increasing in younger girls (<15 years) has important implications for future research into risk factors [22], the development of prevention programs for younger subjects, and the planning of healthcare services.
Incidence of bulimia nervosa
Few studies have investigated the incidence of bulimia nervosa. In the population cohort study of Finnish twins born in the 1980 s, the incidence rate of DSM-5 bulimia nervosa between 10 and 20 years of age was 100 (95% CI 60–190) per 100 000 person-years overall, and 180 (95% CI 110–340) per 100 000 person-years in females [11▪]. These population-based DSM-5 rates of bulimia nervosa are higher than DSM-IV rates for females aged 10–19 years identified in Dutch primary care (range 20.5–22.0 per 100 000 person-years) [12], partly because of the use of broader DSM-5 criteria in the Finnish study [11▪], but moreover because of the fact that only a small proportion of community ‘cases’ present to (primary) care [3,5]. It is of note that the Finnish study [11▪] investigated the incidence rate between 10 and 20 years of age, which only partly covers the peak age period of 15 to 29 years suggested by other studies [12,16▪].
The Dutch primary care study showed a significant decrease in the all-age incidence rate of bulimia nervosa according to DSM-IV criteria over three decades: in 1985–1989 it was 8.6 (95% CI 6.7–11.0), in 1995–1999 6.1 (95% CI 4.5–8.2) and in 2005–2009 3.2 (95% CI 2.0–4.9) per 100 000 person-years [12]. The English primary care study in 11- to 24-year-olds also showed a significant decline in the incidence rate of bulimia nervosa between 2004 and 2014 (incidence rate ratio: 0.5; 95% CI 0.3–0.7) [13▪]. Also, Demmler et al.[14] explained their all-age finding of a slight decrease in the incidence rate of all eating disorders combined in primary care to a declining trend in incidence of bulimia nervosa.
Findings of the Norwegian National Patient Register study [16▪] support a significant decline in overall incidence rates of bulimia nervosa in secondary care between 2010 and 2016, both in narrowly defined bulimia nervosa [2010: 18.5 per 100 000 person-years (95% CI 16.9–20.2); 2016: 16.1 (95% CI 14.6–17.2)] and in broadly defined bulimia nervosa (2010: 29.4 per 100 000 person-years (95% CI 27.4–31.5); 2016: 26.9 (95% CI 24.9–28.8). A significant decrease in incidence rates was found in all age groups, except for a trend of an increase among girls aged 10–14 years, suggesting a shift to earlier ages of onset or detection. The peak incidence was among females aged 20–29 years. In males, the incidence rates were low and stable over time, ranging between 0.9 and 1.6 for narrowly defined bulimia nervosa, and ranging between 1.7 and 2.5 for broadly defined bulimia nervosa. The male to female ratio was found to be 1 : 24 for narrowly defined bulimia nervosa and 1 : 26 for broadly defined bulimia nervosa. Incident cases of bulimia nervosa also occur in later life [12,16▪].
In conclusion, there is a decline in incidence rates of bulimia nervosa over time. The peak age of incidence ranged between 15 and 29 years. Studies of incidence in males are scarce, but the rates are found to be much lower than in females.
Incidence of anorexia nervosa and bulimia nervosa in non-Western countries
Most epidemiological studies on eating disorders have been conducted in Western countries. Although studies assessing the epidemiology of eating disorders in non-Western countries are still scarce, we will highlight the most recent findings. Two Taiwanese studies [23▪,24] used national health insurance claim data to investigate the epidemiology of eating disorders between 2001 and 2013 in 10- to 49-year-old persons. In comparison to Western countries, the overall anorexia nervosa incidence rate in Taiwan is very low (1.1–1.3 per 100 000 person-years), but stable over time. Regarding bulimia nervosa, the incidence rates in Taiwan among females increased in the years up to 2009 [21.6 (95% CI 17.8–25.4) per 100 000 person-years] and then decreased [16.3 (95% CI 12.8–19.8) per 100 000 person-years] [24], following the trend in changes in incidence of Western countries, although a decade later. The incidence in Taiwan differs from that in Western countries in terms of older age at detection of anorexia nervosa and bulimia nervosa (20–29 years) and an increase in incidence among adults rather than adolescents [23▪,24]. This last finding aligns with findings of increasing numbers of persons in midlife with incident eating disorders in Western countries [19].
A study using data and methodology from the Global Burden of Disease (GBD) Study 2017 [25] reported increasing incidence rates of anorexia nervosa and bulimia nervosa from 1990 to 2017 in China, which is in contrast with the stable (anorexia nervosa) and decreasing (bulimia nervosa) rates in Western countries, but in line with the general trend of an increase in rates in all psychiatric diagnoses in China. Because of methodological issues related to the low prevalence and lack of global coverage of epidemiological studies for eating disorders, GBD calculations on these data must be interpreted with caution [26,27]. In this case [25], study results were difficult to check because 15 of the 39 publications from which data were included had been published in Chinese. From the abstracts of the included studies it would appear that in at least 26 of the 39 publications no formal eating disorder diagnosis had been applied, and that none of the studies addressed incidence. This casts doubts on the validity of the findings.
Prevalence
Prevalence is the proportion of cases in a population present at a certain point or interval in time. The point prevalence is the prevalence at a specific date (point) in time. The 12-month prevalence is the prevalence over an interval of a year. The lifetime prevalence is the proportion of the population that has had the disorder at any moment in life up to the moment of registration. In general, lifetime prevalence rates are higher than point and 12-month prevalence rates, especially when assessed in older populations. Prevalence indicates the demand for care and is therefore useful in the planning of healthcare facilities. Many studies have assessed the prevalence of anorexia nervosa and bulimia nervosa. In this review, we focus on recently published systematic reviews and meta-analyses, supplemented by recently published population-based studies that have not been included in the described reviews and meta-analyses.
Prevalence of anorexia nervosa
Galmiche et al.[28] have performed an extensive systematic review of 94 studies published between 2000 and 2018 that addressed the prevalence of formally diagnosed eating disorders in the general population. They explained the high variability of prevalence rates by the use of different diagnostic instruments [most commonly used: Structured Clinical Interview for DSM (13%), Composite International Diagnostic Interview (12%) and Eating Disorder Examination (11%)], diagnostic criteria [DSM-IV (78%), DSM-5 (14%) and DSM-III-R (4%)] and clinical investigation methods [face-to-face interview (51%), paper-and-pencil questionnaire (27%) or online or by telephone (22%)]. Weighted means were constructed from the prevalence rates and the population size of each study included, but were most likely not stratified for age. No confidence intervals were provided, only minimum-maximum ranges of the prevalence rates. The authors themselves conclude that the small number of studies makes it difficult to estimate weighted mean sex ratios. These limitations hamper the interpretation of some findings that are at odds with previous literature, in particular for point prevalence and 12-month prevalence rates. We therefore reproduce only the ranges of lifetime prevalence rates of anorexia nervosa, which were 0.1% to 3.6% in females and 0% to 0.3% in males.
Another systematic review and meta-analysis by Qian et al.[29] included 33 studies published between 1990 and 2020 on the prevalence of anorexia nervosa in the population. All studies combined, an overall lifetime prevalence rate of 0.2% (95% CI 0.06–0.3) was found. In studies applying DSM-5 criteria (18%; all in Western countries) a higher overall lifetime prevalence rate was found [0.9% (95% CI 0.7–1.1)]. This is in line with previous research showing an increase in anorexia nervosa prevalence rates when applying DSM-5 criteria, in comparison to rates according to DSM-IV criteria [30,31]. Lifetime prevalence rates in males and females (Table 1) were in the lower range of the rates described in the review of Galmiche et al.[28]. This could be explained by a large proportion of studies that had been conducted in Asia (40%) with very large sample sizes and much lower rates compared to Western countries, and the broader period studied (1984–2017) with especially lower prevalence rates before 2000 [29]. That is in contrast to findings described in a previous review in this journal [1] and to the notion that anorexia nervosa rates in Asian countries have been increasing in recent years and that they currently appear to be comparable to, or even higher than, those in Western countries [32–34]. In the review by Qian et al.[29], 6 of the 33 studies included had been published in Chinese and so the results were difficult to evaluate. However, there seems to be a lack of population-based studies using formal diagnostic interviews and applying DSM (-III-R, -IV, or -5) or International Classification of Diseases 10th Ed. (ICD-10) criteria. In Asia ‘non fat-phobic’ presentations of anorexia nervosa are common. In the DSM-5 the possibility of ‘persistent behaviour that interferes with weight gain’, which would apply to nonfat phobic presentations, is added to the DSM-IV B-criterium ‘intense fear of gaining weight or becoming fat’. Thus, the replacement of DSM-IV by DSM-5 criteria for anorexia nervosa will ultimately lead to higher rates among Asian people.
Table 1.
Overview of recently published studies on prevalence rates. Studies are grouped by design and listed in chronological order
| Study | Country | Study time | N | Age | Type of study | Criteria | Prevalence | Anorexia Nervosa | Bulimia Nervosa |
| Systematic review | |||||||||
| Lindvall Dahlgren et al., 2017 [35] | Worldwide | 2012-2017 | 19 studies Range 496–22,397 | 11 and older | Two-stage design studies | DSM-5 | Lifetime | ♀ 1.7–3.6% ♂ 0.1% (1 study) | NR |
| Point | ♀ 0.7–1.2% ♂ 0.1% (1 study) | ♀ 0.6% (2 studies) | |||||||
| Interview-based studies | DSM-5 | Lifetime | ♀ 0.8–1.9% | ♀ 2.6% (1 study) | |||||
| Self-report studies | DSM-5 | Point | ♀ 0.06–1.2% | ♀ 0.5–8.7% | |||||
| Galmiche et al., 2019 [28] | Worldwide | 2000-2018 | 94 studies Range 111–248,558 | 8 and older | Systematic review | DSM-III-R DSM-IV DSM-5 | Lifetime | ♀ 0.1–3.6% ♂ 0–0.3% | ♀ 0.3–4.6% ♂ 0.1–1.3% |
| Qian et al., 2021 [29] | Worldwide | 1984-2017 | 33 studies 315,877 | 15 and older | Systematic review and meta-analysis | DSM-III DSM-III-R DSM-IV DSM-5 ICD-10 | Lifetime | ♀ 0.6% (95% CI 0.3–1.1) ♂ 0.04% (95%CI 0.01–0.1) | ♀ 1.2% (95% CI 0.7–1.9) ♂ 0.4% (95%CI 0.2–0.7) |
| DSM-5 | Lifetime | 0.9% (95%CI 0.7–1.1) | 1.4% (95%CI 0.0–6.3) | ||||||
| DSM-III DSM-III-R DSM-IV DSM-5 ICD-10 | 12-month | ♀ 0.03% (95%CI 0.0–0.06) ♂ 0.01% (95%CI 0.0–0.02) | ♀ 0.3% (95%CI 0.1–0.6) ♂ 0.09% (95%CI 0.02–0.2) | ||||||
| DSM-5 | 12-month | 0.04% (95%CI 0.02–0.06) | 0.1% (1 study) | ||||||
| Two-stage design | |||||||||
| Micali et al., 2017a[36▪▪] | UK | 2009-2012 | 5,658 | Mean: 47.8 (SD 4.5) | Two-stage design | DSM-5 | Lifetime | ♀ 3.6% (95%CI 2.8–4.7) | ♀ 2.2% (95%CI 1.7–2.7) |
| 12-month | ♀ 0.2% (95%CI 0.2–0.5) | ♀ 0.4% (95%CI 0.2–0.7) | |||||||
| Interview-based | |||||||||
| Hay et al., 2017b[37] | Australia | 2014-2015 | 5,737 | 15 and older | Interview-based | DSM-5 | 3-month | 0.4–0.5% | 1.1–1.2% |
| Udo and Grilo, 2018a,b[38▪] | USA | 2012-2013 | 36,306 | 18 and older | Interview-based | DSM-5 | Lifetime | ♀ 1.4% (SE 0.1) ♂ 0.1% (SE 0.04) | ♀ 0.5% (SE 0.06) ♂ 0.08% (SE 0.03) |
| 12-month | ♀ 0.08% (SE 0.03) ♂ 0.01% (SE 0.01) | ♀ 0.2% (SE 0.05) ♂ 0.05% (SE 0.02) | |||||||
| Chen et al., 2019 [39] | Taiwan | 2015-2017 | 4,816 | 7-14 | Interview-based | DSM-5 | Lifetime | 0.2% (95%CI 0.0–0.4) | NR |
| 6-month | 0.2% (95%CI 0.0–0.4) | NR | |||||||
| Mohammadi et al., 2020 [40] | Iran | 2016-2018 | 27,111 | 6-18 | Interview-based | DSM-5 | Lifetime | ♀ 0.1% (95%CI 0.06–0.2) | ♀ 0.1% (95%CI 0.07–0.2) ♂ 0.02% (95%CI 0.01–0.08) |
| Silen et al. 2020 [11▪] | Finland | 2006-2009 | 1,347 | Mean 22.4 (SD 0.7) | Interview-based | DSM-5 | Lifetime | ♀ 6.2% (95%CI 4.6–8.3) ♂ 0.3% (95%CI 0.08–1.3) | ♀ 2.4% (95%CI 1.5–3.9) ♂ 0.2% (95%CI 0.02–1.1) |
| Bagaric et al., 2020b[47▪▪] | Australia | 2017 | 2,977 | Mean 53.9 (SD 19.1) | Interview-based | DSM-5 | Lifetime | NR | ♀ 2.6% (95%CI 2.1–3.2) ♂ 1.2% (95%CI 0.9–1.7) |
| Point | NR | ♀ 0.8% (95%CI 0.5–1.2) ♂ 0.4% (95%CI 0.2–0.7) | |||||||
| Self-report | |||||||||
| Ernst et al., 2017a[41] | Germany | 2009 | 1,654 | Mean: 13.4 (SD 5.8) | Self-report | DSM-5 | Point | 0.3% (95%CI 0.1–0.7) | 0.4% (95%CI 0.2–0.8) |
| Glazer et al., 2019 [42] | USA | 1996-2013 | 9,031 | Mean at baseline: 11.6 (SD 1.6) | Self-report | DSM-5 | Lifetime | ♀ 1.6% | ♀ 2.1% |
| Mitchison et al., 2020 [43] | Australia | 2017 | 5,191 | 11-19 | Self-report | DSM-5 | Point | ♀ 1.3% ♂ 0.0% | ♀ 7.7% ♂ 1.8% |
included in Galmiche et al., 2019.
included in Qian et al., 2021.
CI, confidence interval; NR, not reported; SD, standard deviation; SE, standard error.
In their systematic review, Lindvall Dahlgren, Wisting and Ro [35] focused specifically on the prevalence of DSM-5 defined anorexia nervosa in the general population. Nineteen studies published until 2017 were included. Lifetime prevalence rates for anorexia nervosa in females differed according to the study method; 1.7–3.6% in studies with two-stage design and 0.8–1.9% in interview-based studies. Point prevalence rates in females ranged from 0.06% to 1.2%, predominantly assessed with self-reports.
Since this systematic review [35], several studies [11▪,36▪▪,37,38▪,39–43] have been published that investigated prevalence according to DSM-5 criteria. The prevalence rates reported in these recent studies are shown in Table 1 and are largely in line with those reported in the review. However, the population-based study of Finnish twins born in the 1980 s [11▪], in which the whole sample was diagnostically interviewed, found higher lifetime prevalence rates for anorexia nervosa: 6.2% (95% CI 4.6–8.3) in females and 0.3% (95% CI 0.08–1.3) in males. Suggested explanations for the higher rate found among females were the twin nature of the study, the thorough anorexia nervosa assessment and Finnish socio-cultural characteristics favouring a drive for thinness. Only 55% of the females identified with anorexia nervosa in the study reported that they had been diagnosed in real life by a healthcare professional.
Although epidemiological studies have mainly focused on the traditionally known high-risk group of young females, it has been shown in recent years that anorexia nervosa is prevalent among older persons as well [18,19]. The highest lifetime prevalence rates are found in adults, because of the accumulation of anorexia nervosa first emerging in the peak age period of adolescence [44] combined with incidence later in adulthood. A longitudinal, population-based study among Polish males showed that anorexia nervosa was prevalent in all age groups (10–80+ years) [45]. Although a decrease in point prevalence among females over a 30-year follow-up period was found, with no anorexia nervosa cases by age 50 [46▪], the 12-month prevalence rate in 40- to 50-year-old females was still 0.2% in another study [36▪▪].
Prevalence of bulimia nervosa
The three previously discussed systematic reviews and meta-analyses [28,29,35] also reported prevalence rates for bulimia nervosa. The lifetime prevalence rates for bulimia nervosa ranged from 0.3% to 4.6% in females and from 0.1% to 1.3% in males in the extensive systematic review by Galmiche et al.[28]. As discussed previously, we refrain from reproducing the 12-month and point prevalence rates they report for methodological reasons.
Qian et al.[29] reported an overall lifetime prevalence rate for bulimia nervosa of 0.6% (95% CI 0.3–1.0). This review included a relatively large (40%) proportion of Asian studies. For bulimia nervosa the lifetime prevalence in Western countries was 7.3 times higher than that in Asian countries. The lifetime prevalence rates in females and males (Table 1) were close to the rates described by Galmiche et al.[28]. The pooled overall lifetime prevalence rate rose up to 1.4% (95% CI 0.0–6.3), when using only studies that applied DSM-5 criteria (18%; all in Western countries) [29]. Other studies supported this increase [30,31], which could be explained by the lower required frequency of binge eating and compensatory behaviour in DSM-5 compared to DSM-IV.
Lindvall Dahlgren et al. included only studies that had applied DSM-5 criteria and found few studies on bulimia nervosa, but the authors reported preliminary evidence for an increase in bulimia nervosa prevalence [35]. Two two-stage studies reported a point prevalence rate of 0.6% in females [30,48]. The lifetime prevalence rate was found to be 2.6% among females in one interview-based study [49]. In self-report studies, point prevalence rates ranged from 0.5% to 8.7% in females.
Since these systematic reviews, several studies on the prevalence of DSM-5 defined bulimia nervosa [11▪,36▪▪,37,38▪,40–43,47▪▪] have been published in recent years. Among females, lifetime prevalence rates around 2.3% (range 2.1–2.6%) were consistently found [11▪,36▪▪,42,47▪▪], which gives further support for an increase in bulimia nervosa prevalence since the introduction of DSM-5 criteria. Only one study in a large population-based sample of US adults [38▪] reported a substantially lower lifetime prevalence rate [0.5% (Standard Error 0.06)] in females. Possible explanations for this low rate are the use of lay interviewers rather than clinicians and the use of a questionnaire that has not been validated for eating disorder diagnoses. The combination of these factors could lead to underreporting, especially in the case of bulimia nervosa where stigma and shame around bingeing and purging play an important role.
Few recent studies reported on prevalence in males. The results were in the same order as found in the systematic reviews [28,29], with lifetime prevalence rates ranging between 0.1% and 1.2% [11▪,38▪,47▪▪]. In males like in females [36▪▪,46▪], bulimia nervosa does occur in all age groups up to the age of 80, although the prevalence declines after age 30 [45].
The preliminary evidence for an increase in prevalence of bulimia nervosa in population-based studies is noteworthy in the face of decreasing incidence rates in primary and secondary care. One possible explanation is that people who have a lower frequency of binge eating and compensatory behaviour (meeting DSM-5 but not DSM-IV criteria, i.e. once a week) seek help less often than those who have this behaviour more often, and thus are less often included in care-based studies. Future research is needed to clarify this apparent discrepancy.
Mortality
Mortality could be described as an incidence rate in which the event being measured is death. The crude mortality rate (CMR) is the number of deaths within the study population over a specified period. The standardized mortality ratio (SMR) is the ratio of observed deaths in the study population versus that of expected deaths in the population of origin. For comparison reasons the SMR is preferred, because the CMR is not standardized for age and sex. Mortality is often used as an indicator of the severity of a disorder.
In a previous review in this journal [27], it has been reported that both anorexia nervosa and bulimia nervosa were associated with significantly increased mortality rates. In comparison to age-matched and sex-matched people in the general population, the mortality risk was around two times higher in people followed up after outpatient treatment for anorexia nervosa, or after any treatment for bulimia nervosa. In people followed up after inpatient treatment for anorexia nervosa, the mortality risk was even over five times higher. Since this previous review, a few new studies have been published.
In a landmark meta-analysis of worldwide eating disorder mortality rates by Arcelus et al.[50] the CMR of anorexia nervosa patients was 5.1 deaths per 1000 person-years (95% CI 4.0–6.1). The SMR was 5.9 (95% CI 4.2–8.3), i.e. an almost 6 times increased risk. In a recent study, after 5 years follow-up the SMR of anorexia nervosa inpatients with (complications of) severe malnutrition was found to be as high as 15.9 (95% CI 11.6–21.4) [51]. This study population was probably more severely affected than most of the study populations included in the meta-analysis [50]. For bulimia nervosa, Arcelus et al. reported a CMR of 1.7 per 1000 person-years (95% CI 1.1–2.4) and a SMR of 1.9 (95% CI 1.4–2.6) [50]. Recently, in a large 12-year follow-up study a higher mortality risk was found in females after inpatient treatment for bulimia nervosa compared to similar-age females hospitalized for pregnancy-related events [adjusted hazard ratio 4.7 (95% CI 2.1–10.8)] [52]. This difference could be even larger when compared to the general population. Iwajomo et al. investigated mortality after hospitalization for an eating disorder (anorexia nervosa, bulimia nervosa or eating disorder not otherwise specified) in a Canadian population-based cohort [53▪]. Although results were not presented for each eating disorder separately, the total SMR was five times higher compared to the general population [SMR 5.1 (95% CI 4.8–5.3)]. Rates were higher for males [SMR 7.2 (95% CI 6.6–8.0)] compared to females [SMR 4.6 (95% CI 4.3–4.9)]. This is in line with other recent studies that also found higher mortality rates among males: in people treated for bulimia nervosa in secondary mental healthcare services an overall SMR of 2.5 (95% CI 1.5–4.0) was reported, with significantly higher rates among males compared to females [crude hazard ratio 5.4 (95% CI 1.8–16.5)] [54]. In another study on hospitalization for anorexia nervosa, in-hospital mortality in males was more than twice that for females [odds ratio 2.4 (95% CI 1.5–3.8)] [55]. However, in a study directly comparing males and females from the same hospital, from the same treatment period and for the same follow-up period, no significant differences in SMR were found for anorexia nervosa or for bulimia nervosa [56▪], which might be due to the relatively small sample size of males. The SMRs for each sex-group [57,58] have already been described in the previous review [27]. While there were no significant differences in mortality rates, males with anorexia nervosa or bulimia nervosa did die sooner in comparison to females with anorexia nervosa or bulimia nervosa [56▪].
In summary, recent findings accentuate high mortality rates for anorexia nervosa and bulimia nervosa, with highest rates among those who received inpatient treatment for anorexia nervosa. Although results are still inconclusive, the suggestion that males have a probably higher mortality risk than females underscores the clinical relevance of detecting and treating anorexia nervosa and bulimia nervosa in males.
CONCLUSION
Anorexia nervosa and bulimia nervosa occur among females and males of all age groups worldwide and are associated with an increased mortality risk. The trend of a decreasing peak age at incidence has implications for future research into risk factors, the development of earlier prevention programs and planning of treatment services. Besides the well-known risk group of young females from Western countries, the occurrence of anorexia nervosa and bulimia nervosa in males, older persons and non-Western countries highlights the need for further research in these groups. Moreover, improved awareness will lead to earlier detection and treatment in these groups that suffer from an extra stigma of a ‘young, Western, female-specific’ psychiatric disorder.
Acknowledgements
The authors would like to thank Judith Offringa for her editorial assistance.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Hoek HW. Review of the worldwide epidemiology of eating disorders. Curr Opin Psychiatry 2016; 29:336–339. [DOI] [PubMed] [Google Scholar]
- 2.Smink FR, van Hoeken D, Hoek HW. Epidemiology, course, and outcome of eating disorders. Curr Opin Psychiatry 2013; 26:543–548. [DOI] [PubMed] [Google Scholar]
- 3.Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and other eating disorders. Curr Opin Psychiatry 2006; 19:389–394. [DOI] [PubMed] [Google Scholar]
- 4.Keski-Rahkonen A. Epidemiology of binge eating disorder: prevalence, course, comorbidity, and risk factors. Curr Opin Psychiatry 2021; 34:525–531. [DOI] [PubMed] [Google Scholar]
- 5.Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep 2012; 14:406–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoek HW, van Hoeken D. Review of the prevalence and incidence of eating disorders. Int J Eat Disord 2003; 34:383–396. [DOI] [PubMed] [Google Scholar]
- 7▪.Martinez-Gonzalez L, Fernandez-Villa T, Molina AJ, et al. Incidence of anorexia nervosa in women: a systematic review and meta-analysis. Int J Environ Res Public Health 2020; 17:3824. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study systematically reviews 31 published studies from 1980 to 2019 on the incidence of anorexia nervosa in females, mainly from Western countries. Pooled incidence rates are reported.
- 8.Ghaderi A, Scott B. Prevalence, incidence and prospective risk factors for eating disorders. Acta Psychiatr Scand 2001; 104:122–130. [DOI] [PubMed] [Google Scholar]
- 9.Lahortiga-Ramos F, De Irala-Estevez J, Cano-Prous A, et al. Incidence of eating disorders in Navarra (Spain). Eur Psychiatry 2005; 20:179–185. [DOI] [PubMed] [Google Scholar]
- 10.Keski-Rahkonen A, Hoek HW, Susser ES, et al. Epidemiology and course of anorexia nervosa in the community. Am J Psychiatry 2007; 164:1259–1265. [DOI] [PubMed] [Google Scholar]
- 11▪.Silen Y, Sipila PN, Raevuori A, et al. DSM-5 eating disorders among adolescents and young adults in Finland: A public health concern. Int J Eat Disord 2020; 53:520–531. [DOI] [PubMed] [Google Scholar]; A population-based study that assessed lifetime prevalence and incidence rates of DSM-5 defined eating disorders between the age of 10 and 20 years in Finnish twins born in the 1980 s (N = 1,347) using a semi-structured diagnostic interview.
- 12.Smink FR, van Hoeken D, Donker GA, et al. Three decades of eating disorders in Dutch primary care: decreasing incidence of bulimia nervosa but not of anorexia nervosa. Psychol Med 2016; 46:1189–1196. [DOI] [PubMed] [Google Scholar]
- 13▪.Wood S, Marchant A, Allsopp M, et al. Epidemiology of eating disorders in primary care in children and young people: a clinical practice research datalink study in England. BMJ Open 2019; 9:e026691. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study investigated time trends in the incidence of eating disorders among 11- to 24-year-olds in primary care in England and found stable incidence rates of anorexia nervosa and a significant decline in the incidence rate of bulimia nervosa between 2004 and 2014.
- 14.Demmler JC, Brophy ST, Marchant A, et al. Shining the light on eating disorders, incidence, prognosis and profiling of patients in primary and secondary care: national data linkage study. Br J Psychiatry 2020; 216:105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cybulski L, Ashcroft DM, Carr MJ, et al. Temporal trends in annual incidence rates for psychiatric disorders and self-harm among children and adolescents in the UK. BMC Psychiatry 2021; 21:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16▪.Reas DL, Ro O. Time trends in healthcare-detected incidence of anorexia nervosa and bulimia nervosa in the Norwegian national patient register. Int J Eat Disord 2018; 51:1144–1152. [DOI] [PubMed] [Google Scholar]; A Norwegian register-based study on time trends in the incidene of anorexia nervosa and bulimia nervosa among persons aged 10-49 in secondary care. This study shows stable rates of anorexia nervosa and decreasing rates of bulimia nervosa from 2010 to 2016.
- 17.Petkova H, Simic M, Nicholls D, et al. Incidence of anorexia nervosa in young people in the UK and Ireland: a national surveillance study. BMJ Open 2019; 9:e027339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mangweth-Matzek B, Hoek HW. Epidemiology and treatment of eating disorders in men and women of middle and older age. Curr Opin Psychiatry 2017; 30:446–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samuels KL, Maine MM, Tantillo M. Disordered eating, eating disorders, and body image in midlife and older women. Curr Psychiatry Rep 2019; 21:70. [DOI] [PubMed] [Google Scholar]
- 20.Javaras KN, Runfola CD, Thornton LM, et al. Sex- and age-specific incidence of healthcare-register-recorded eating disorders in the complete Swedish 1979–2001 birth cohort. Int J Eat Disord 2015; 48:1070–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raevuori A, Keski-Rahkonen A, Hoek HW. A review of eating disorders in males. Curr Opin Psychiatry 2014; 27:426–430. [DOI] [PubMed] [Google Scholar]
- 22.van Eeden AE, Oldehinkel AJ, van Hoeken D, Hoek HW. Risk factors in preadolescent boys and girls for the development of eating pathology in young adulthood. Int J Eat Disord 2021; 54:1147–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23▪.Tseng MM, Tu CY, Hsieh SF, Chang CH. Rates and trends in healthcare-detected incidence of anorexia nervosa and bulimia nervosa: a national health insurance claim data study in Taiwan. Int J Eat Disord 2020; 53:331–338. [DOI] [PubMed] [Google Scholar]; This Taiwanese study examined healthcare-detected incidence of anorexia nervosa and bulimia nervosa between 2002 and 2013. The incidence rate of bulimia nervosa among females increased in the years before 2009 and then decreased.
- 24.Tsai MC, Gan ST, Lee CT, et al. National population-based data on the incidence, prevalence, and psychiatric comorbidity of eating disorders in Taiwanese adolescents and young adults. Int J Eat Disord 2018; 51:1277–1284. [DOI] [PubMed] [Google Scholar]
- 25.Wu J, Lin Z, Liu Z, et al. Secular trends in the incidence of eating disorders in China from 1990 to 2017: a joinpoint and age-period-cohort analysis. Psychol Med 2020; 1–11. doi: 10.1017/S0033291720002706. [DOI] [PubMed] [Google Scholar]
- 26.Santomauro DF, Melen S, Mitchison D, et al. The hidden burden of eating disorders: an extension of estimates from the Global Burden of Disease Study. Lancet Psychiatry 2021; 8:320–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry 2020; 33:521–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Galmiche M, Dechelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr 2019; 109:1402–1413. [DOI] [PubMed] [Google Scholar]
- 29.Qian J, Wu Y, Liu F, et al. An update on the prevalence of eating disorders in the general population: a systematic review and meta-analysis. Eat Weight Disord 2021; Published online 8 April 2021. doi: 10.1007/s40519-021-01162-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Machado PP, Goncalves S, Hoek HW. DSM-5 reduces the proportion of EDNOS cases: evidence from community samples. Int J Eat Disord 2013; 46:60–65. [DOI] [PubMed] [Google Scholar]
- 31.Flament MF, Buchholz A, Henderson K, et al. Comparative distribution and validity of DSM-IV and DSM-5 diagnoses of eating disorders in adolescents from the community. Eur Eat Disord Rev 2015; 23:100–110. [DOI] [PubMed] [Google Scholar]
- 32.Kim YR, Nakai Y, Thomas JJ. Introduction to a special issue on eating disorders in Asia. Int J Eat Disord 2021; 54:3–6. [DOI] [PubMed] [Google Scholar]
- 33.Nakai Y, Nin K, Goel NJ. The changing profile of eating disorders and related sociocultural factors in Japan between 1700 and 2020: a systematic scoping review. Int J Eat Disord 2021; 54:40–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu J, Liu J, Li S, et al. Trends in the prevalence and disability-adjusted life years of eating disorders from 1990 to 2017: results from the Global Burden of Disease Study. Epidemiol Psychiatr Sci 2020; 29:e191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lindvall Dahlgren C, Wisting L, Ro O. Feeding and eating disorders in the DSM-5 era: a systematic review of prevalence rates in nonclinical male and female samples. J Eat Disord 2017; 5:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36▪▪.Micali N, Martini MG, Thomas JJ, et al. Lifetime and 12-month prevalence of eating disorders amongst women in mid-life: a population-based study of diagnoses and risk factors. BMC Med 2017; 15:12. [DOI] [PMC free article] [PubMed] [Google Scholar]; This two-stage design study assessed the lifetime and 12-month prevalence of formal eating disorder diagnoses in a population-based sample of females in mid-life in the UK (N = 5,658).
- 37.Hay P, Mitchison D, Collado AEL, et al. Burden and health-related quality of life of eating disorders, including Avoidant/Restrictive Food Intake Disorder (ARFID), in the Australian population. J Eat Disord 2017; 5:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38▪.Udo T, Grilo CM. Prevalence and correlates of DSM-5-defined eating disorders in a nationally representative sample of US adults. Biol Psychiatry 2018; 84:345–354. [DOI] [PMC free article] [PubMed] [Google Scholar]; A very large population-based study of US adults (N = 36,306) on the prevalence of DSM-5 defined eating disorders.
- 39.Chen YL, Chen WJ, Lin KC, et al. Prevalence of DSM-5 mental disorders in a nationally representative sample of children in Taiwan: methodology and main findings. Epidemiol Psychiatr Sci 2019; 29:e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mohammadi MR, Mostafavi SA, Hooshyari Z, et al. Prevalence, correlates and comorbidities of feeding and eating disorders in a nationally representative sample of Iranian children and adolescents. Int J Eat Disord 2020; 53:349–361. [DOI] [PubMed] [Google Scholar]
- 41.Ernst V, Burger A, Hammerle F. Prevalence and severity of eating disorders: a comparison of DSM-IV and DSM-5 among German adolescents. Int J Eat Disord 2017; 50:1255–1263. [DOI] [PubMed] [Google Scholar]
- 42.Glazer KB, Sonneville KR, Micali N, et al. The course of eating disorders involving bingeing and purging among adolescent girls: prevalence, stability, and transitions. J Adolesc Health 2019; 64:165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mitchison D, Mond J, Bussey K, et al. DSM-5 full syndrome, other specified, and unspecified eating disorders in Australian adolescents: prevalence and clinical significance. Psychol Med 2020; 50:981–990. [DOI] [PubMed] [Google Scholar]
- 44.Wonderlich SA, Bulik CM, Schmidt U, et al. Severe and enduring anorexia nervosa: update and observations about the current clinical reality. Int J Eat Disord 2020; 53:1303–1312. [DOI] [PubMed] [Google Scholar]
- 45.Jaworski M, Panczyk M, Sliwczynski A, et al. Eating disorders in males: an 8-year population-based observational study. Am J Mens Health 2019; 13:1557988319860970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46▪.Brown TA, Forney KJ, Klein KM, et al. A 30-year longitudinal study of body weight, dieting, and eating pathology across women and men from late adolescence to later midlife. J. Abnorm Psychol 2020; 129:376–386. [DOI] [PMC free article] [PubMed] [Google Scholar]; A population-based study with a long-term follow-up of 30 years to examine the occurrence of eating disorders and sex differences across the lifespan.
- 47▪▪.Bagaric M, Touyz S, Heriseanu A, et al. Are bulimia nervosa and binge eating disorder increasing? Results of a population-based study of lifetime prevalence and lifetime prevalence by age in South Australia. Eur Eat Disord Rev 2020; 28:260–268. [DOI] [PubMed] [Google Scholar]; This study assessed prevalence rates of bulimia nervosa and binge eating disorder in an Australian general population (N = 2,977) by means of a diagnostic interview. Rates were found to be higher than those reported in previous population-based studies.
- 48.Smink FR, van Hoeken D, Oldehinkel AJ, Hoek HW. Prevalence and severity of DSM-5 eating disorders in a community cohort of adolescents. Int J Eat Disord 2014; 47:610–619. [DOI] [PubMed] [Google Scholar]
- 49.Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J. Abnorm Psychol 2013; 122:445–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry 2011; 68:724–731. [DOI] [PubMed] [Google Scholar]
- 51.Guinhut M, Godart N, Benadjaoud MA, et al. Five-year mortality of severely malnourished patients with chronic anorexia nervosa admitted to a medical unit. Acta Psychiatr Scand 2021; 143:130–140. [DOI] [PubMed] [Google Scholar]
- 52.Tith RM, Paradis G, Potter BJ, et al. Association of bulimia nervosa with long-term risk of cardiovascular disease and mortality among women. JAMA Psychiatry 2020; 77:44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53▪.Iwajomo T, Bondy SJ, de Oliveira C, et al. Excess mortality associated with eating disorders: population-based cohort study. Br J Psychiatry 2020; 1–7. doi: 10.1192/bjp.2020.197. [DOI] [PubMed] [Google Scholar]; Examination of mortality after hospitalization for an eating disorder in a Canadian population-based cohort. Mortality rates were five to seven times higher in patients with an eating disorder in comparison to the general population.
- 54.Himmerich H, Hotopf M, Shetty H, et al. Psychiatric comorbidity as a risk factor for the mortality of people with bulimia nervosa. Soc Psychiatry Psychiatr Epidemiol 2019; 54:813–821. [DOI] [PubMed] [Google Scholar]
- 55.Edakubo S, Fushimi K. Mortality and risk assessment for anorexia nervosa in acute-care hospitals: a nationwide administrative database analysis. BMC Psychiatry 2020; 20:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56▪.Fichter MM, Naab S, Voderholzer U, Quadflieg N. Mortality in males as compared to females treated for an eating disorder: a large prospective controlled study. Eat Weight Disord 2020; 26:1627–1637. [DOI] [PubMed] [Google Scholar]; This large longitudinal study compared mortality rates in males treated in hospital for an eating disorder with those in females. Males with anorexia nervosa or bulimia nervosa died earlier in comparison to females.
- 57.Fichter MM, Quadflieg N. Mortality in eating disorders - results of a large prospective clinical longitudinal study. Int J Eat Disord 2016; 49:391–401. [DOI] [PubMed] [Google Scholar]
- 58.Quadflieg N, Strobel C, Naab S, et al. Mortality in males treated for an eating disorder - a large prospective study. Int J Eat Disord 2019; 52:1365–1369. [DOI] [PubMed] [Google Scholar]