Abstract
Internet- and mobile-based interventions (IMIs) are being developed for a wide range of psychological disorders and they showed their effectiveness in multiple studies. Specific phobia (SP) is one of the most common anxiety disorders, and research about IMIs for their treatment has also been conducted in recent years. The aim of this paper was to conduct a systematic review and preliminary meta-analysis exploring IMIs for the treatment of SP. A comprehensive search conducted in five different databases identified 9 studies (4 pre-post studies, 5 randomized controlled trials) with 7 Internet-based interventions and 2 mobile-based interventions. Results showed that exposure was the main component of all interventions, and that animal phobia was the most common subtype. Samples included children, adolescents, and adults. A preliminary meta-analysis of the included studies showed that participants receiving IMIs experienced a significant reduction of SP symptoms from pre- to post-treatment (g = 1.15). This systematic review found that there is already some evidence in the literature supporting the potential benefits of IMIs for SP. However, the number of studies included is small and more research should be carried out in the field.
Keywords: Specific phobia, Internet-based treatments, Mobile-based treatments, Systematic review, Meta-analysis
Highlights
-
•
Internet- and mobile-based interventions have been developed for Specific Phobia.
-
•
Nine studies were included in this systematic review.
-
•
Results showed that exposure was the main component of the interventions.
-
•
Preliminary meta-analyses showed a significant reduction of phobic symptomatology.
-
•
There is promising evidence of the potential benefits of IMIs for SP.
1. Introduction
Specific Phobia (SP) is one of the most common anxiety disorders, with an estimated lifetime prevalence of up to 7% (Eaton et al., 2018). Although it can be considered a less severe problem compared to some other psychological disorders, people suffering from it report severe impairment in different domains of their lives (Wardenaar et al., 2017). It has also been associated with a higher probability of developing another anxiety disorder (Trumpf et al., 2010) and physical problems, such as cardiac, respiratory, or gastrointestinal diseases (Witthauer et al., 2016). Taking all of this into consideration, there is a clear need to offer evidence-based psychological treatments for this problem.
Fortunately, the treatment of choice for SP, exposure therapy, has been well-established for decades (Marks, 1987). Furthermore, its mechanisms and how to improve its effectiveness have been studied and discussed over the years (Böhnlein et al., 2020; Craske et al., 2014; Sewart and Craske, 2019). Traditionally, in vivo exposure was the approach clinicians used to deliver treatment for SP, but as technology advanced, research explored other ways to carry out exposure therapy. This is the case of Virtual Reality Exposure Therapy (VRET), which rapidly became a popular alternative for treating SP because it helped to overcome some of the limitations of in vivo exposure. It also presented some advantages for both the patient and the clinician, such as being able to deliver the treatment in the clinician's office. Many studies have been conducted in this field, and VRET has shown comparable results to in vivo exposure (Botella et al., 2017; Wechsler et al., 2019).
However, despite the evidence supporting exposure-based treatments, there are still barriers to their dissemination (Neudeck and Einsle, 2012). Following the guidelines for new ways to provide treatment to those in need of psychological help (Kazdin and Blase, 2011), the Internet became a new alternative to traditional face-to-face treatments. Internet-based interventions have been created, and their effectiveness has been shown for a wide range of psychological disorders, such as depression (Karyotaki et al., 2017, Karyotaki et al., 2018), PTSD (Kuester et al., 2016; Lewis et al., 2018), or even somatic disorders (Carlbring et al., 2018; van Beugen et al., 2014) among others. Internet interventions for the treatment of anxiety disorders have also been widely studied, showing comparable results to face-to-face treatment and acceptance by patients (Andersson and Titov, 2014; Andrews et al., 2018; Arnberg et al., 2014; Kelson et al., 2019; Olthuis et al., 2016). In the case of SP, a self-help treatment with virtual reality components using the Intranet was used to treat animal phobia and showed promising results (Botella et al., 2008).
In recent years, with the further development of technologies, new options have been suggested to deliver psychological treatments in people's homes. This is the case of mobile-based interventions, which have shown evidence of reducing anxiety symptoms (Firth et al., 2017) and have been found to be well-accepted by patients (Menon et al., 2017). These new options have also made VRET more accessible by developing, for example, affordable head-mounted displays to use with smartphones (Kato and Miyashita, 2015), providing the opportunity to deliver mobile-based treatments using virtual reality in people's homes (Stupar-Rutenfrans et al., 2017). However, there is a lack of research and validation of many mental health apps, with only a limited number being evidence-based interventions (Miralles et al., 2020), and so there is a clear need for further research in this field.
Although still scarce, some research has been carried out in the field of Internet- and mobile-based interventions (IMIs) for SP. The aim of this paper is to conduct the first systematic review exploring IMIs in the field of SP, synthesizing the characteristics of the different interventions and their treatment outcomes.
2. Method
The present study was carried out following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009), was registered in the Open Science Framework (OSF) and was made public with the following ID: osf.io/g5x6y.
2.1. Inclusion and exclusion criteria
Studies were included if they met the following criteria: (1) Participants in the study were children, adolescents, or adults who had a diagnosis of SP or presented high scores on self-report measures for phobia; (2) The intervention was focused on SP, or SP was one of the disorders treated in the study, but specific data for SP were reported; (3) The psychological intervention was delivered through the Internet or mobile phone. The intervention could include virtual reality components; (4) Studies had to contain at least pre- and post-treatment measures of phobic symptomatology (randomized and non-randomized).
Studies where the sample had a diagnosis of social anxiety or agoraphobia and studies with a face-to-face component of the intervention were excluded from this review.
2.2. Information sources and searches
Searches were conducted in PubMed, PsycINFO, Web of Science, SCOPUS, and Cochrane to identify relevant studies published prior to December 2020. There were no exclusion criteria regarding the year of publication of the study or the language in which it was written. Due to the different terminology used in publications, variations of the terms “Internet-based treatment”, “mobile-based treatment”, and “phobia” were included in the search, combined with Boolean operators using “AND” and “OR”. In addition, we included some common terms related to phobia, such as “dental anxiety”, “claustrophobia”, and “acrophobia” because we are aware that they are used in some papers in the field of SP. The complete search strings are included in the Appendix. The references of included studies and similar recent systematic reviews were also inspected to identify additional studies that might have been missing in the search.
2.3. Study selection
After carrying out the searches in the different databases and removing duplicates, two independent researchers (SM and JG) examined the titles and abstracts of the studies to select the records that potentially met the inclusion criteria. Differences in the selected studies and doubts were discussed with a third reviewer (SQ). Full texts of the selected studies that appeared to meet the inclusion criteria and those that were in doubt due to insufficient information in the title or abstract were retrieved and reviewed independently by two researchers to confirm that they were suitable for the current review.
2.4. Study quality assessment
The quality of the studies included in this review was assessed using The Study Quality Assessment Tools from the National Heart Lung and Blood Institute (NHLBI; https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools). This tool was chosen because the present systematic review aimed to explore any type of study that has been published for the treatment of SP using IMIs. The NHLBI includes specific criteria to assess six types of study designs: controlled intervention studies, systematic reviews and meta-analyses, observational cohort and cross-sectional studies, case-control studies, before-after studies with no control group, and case series studies. The studies’ quality can be rated as “good”, “fair”, or “poor” after answering the different questions established depending on the study design. Two reviewers (SM and CT) independently rated the studies included in this paper. Disagreements were discussed with a third reviewer (SQ).
2.5. Data synthesis
Firstly, for all the included studies, data about the study design, sample, characteristics of the intervention, and treatment effects in terms of SP symptom reduction were independently extracted from the publications and narratively synthesized. The data extracted by the researchers were compared and discussed with a third researcher if discrepancies were found.
Also, for all the included studies (randomized and pre-post studies), within-group effect sizes were calculated to estimate symptom reduction from pre- to post-treatment. These effect sizes were computed as Hedges' g, assuming a pre-post correlation of 0.7. Sensitivity analyses using alternative pre-post correlations were conducted. A preliminary meta-analysis was conducted by pooling within-group effect sizes with a random-effects model, using a restricted maximum-likelihood estimator (Viechtbauer, 2005) and the Hartung-Knapp-Sidik-Jonkman (HKSJ) method (IntHout et al., 2014). Heterogeneity was explored with the I2 statistic and its 95% confidence interval. We conducted subgroup analyses based on type of design (randomized vs pre-post studies) with a mixed-effects model. Because the number of studies was too small, we did not conduct additional analyses.
Additionally, for the subset of randomized controlled trials (RCTs), we computed between-group effect sizes as standardized mean differences (Hedges’ g) at post-test. We pooled these effect sizes using the same meta-analytical procedures.
3. Results
3.1. Search results
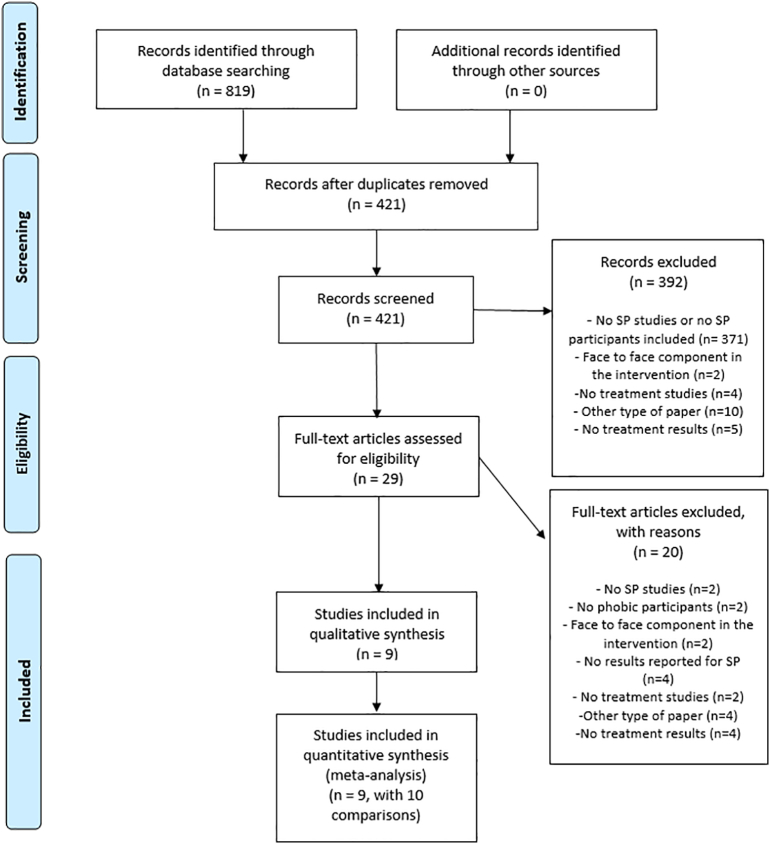
Fig. 1 shows the Flow diagram for the study. Initially, 819 studies were identified upon completion of the search in the different electronic databases. Duplicates were removed, leaving a total of 421 papers that were examined. Finally, 29 full-text papers were retrieved and, after reading them independently and excluding studies that did not meet the inclusion criteria, a total of nine studies were included in the current systematic review.
Fig. 1.
Flow diagram for the systematic review.
3.2. Participants
Table 1 shows selected characteristics of the participants in each study. Overall, participants' mean ages ranged from 9.9 to 41.3 years, with a mean age of 33.58 years across the studies, except for one study (Matthews et al., 2012) where the mean age was not reported. Six studies (66.7%) involved adults suffering from SP, two studies included children or adolescents (22.2%), and one study admitted participants of any age. Almost all the studies had a majority of women participants, and one of them (Matthews et al., 2011) only included female participants in its sample.
Table 1.
Participant and study characteristics.
| Study | Country | Study type | Population | N | Age M (SD) |
Women (%) | Phobia subtype |
|---|---|---|---|---|---|---|---|
| Donker et al. (2019) | The Netherlands | RCT | Adults | Total: 193 IG: 96 CG: 97 |
41.32 (13.67) | 65.83 | Acrophobia |
| Campos et al. (2019) | Spain | RCT | Adults | Total: 69 IG 1: 23 IG 2: 23 CG: 23 |
36.43 (10.23) | 72.47 | Flying Phobia |
| Andersson et al. (2009) | Sweden | RCT | Adults | Total: 27 IG: 13 CG: 14 |
25.6 (4.1) | 84.8 | Spider phobia |
| Shahnavaz et al. (2018) | Sweden | Pre-post | Children and adolescents | Total: 18 IG: 18 |
11 (2) | 61 | Dental phobia |
| Andersson et al. (2013) | Sweden | RCT | Adults | Total: 26 IG: 13 CG: 13 |
27.2 (8.1) | 84.6 | Snake phobia |
| Vigerland et al. (2013) | Sweden | Pre-post | Children | Total: 30 IG: 30 |
9.9 (1.4) | 57 | Specific phobia (various types) |
| Matthews et al. (2011) | Australia | Pre-post | Adults | Total: 17 IG: 17 |
38 (12) | 100 | Spider phobia |
| Matthews et al. (2012) | Australia | Pre-post | All ages | Total: 351 IG 1: 176 IG 2: 124 |
Not referred. | 53 | Spider phobia |
| Arias et al. (2020) | USA | RCT | Adults | Total: 36 IG 1: 18 CG 2: 18 |
26.15 (11.25) | 61.1 | Dental phobia |
RCT: Randomized Controlled Trial; IG: Intervention Group; CG: Control Group.
As for participants’ diagnosis, the studies usually addressed one type of SP, and only one study (Vigerland et al., 2013) accepted participants with different types of fears as long as they met the diagnostic criteria for SP. Related to this, the recruitment method in 66.7% (n = 6) of the papers was a diagnostic interview, whereas the remaining studies recruited participants based on questionnaire scores. The subtypes of SP were animal phobia (spider phobia n = 3; snake phobia n = 1), situational phobia (flying phobia n = 1; dental phobia n = 2), and natural environment phobia (acrophobia n = 1). In the study by Vigerland et al. (2013), which included children with various types of phobias, the sample presented claustrophobia (23%), darkness phobia (40%), acrophobia (13%), animal phobia (47%), and blood injury and injection phobia (10%). Comorbidity with other disorders was only mentioned in three papers (Campos et al., 2019; Shahnavaz et al., 2018; Vigerland et al., 2013), which meant that participants could present other types of phobias, anxiety problems, or psychological problems in general, as long as they were not severe psychological disorders and the principal diagnosis was SP. Sample sizes in the studies ranged from 13 to 351.
3.3. Study design and characteristics
Five of the included studies were RCTs (Andersson et al., 2009, Andersson et al., 2013; Arias and McNeil, 2020; Campos et al., 2019; Donker et al., 2019), and the four remaining studies were pre-post investigations with no control group (Matthews et al., 2011, Matthews et al., 2012; Shahnavaz et al., 2018; Vigerland et al., 2013). Regarding the comparators used in the RCTs, three studies had a waitlist control group, and two studies had another SP treatment. The studies were conducted in five different countries: the Netherlands (n = 1), Spain (n = 1), Australia (n = 2), the USA (n = 1), and Sweden (n = 4). The papers included were published between 2009 and 2020. Detailed study information is shown in Table 1.
3.4. Intervention characteristics
Of the nine studies, seven carried out an Internet-based intervention, and the other two used an app to deliver the treatment through the participant's mobile phone. Table 2 shows the intervention characteristics for each study.
Table 2.
Characteristics of the intervention, outcome measures, attrition, and follow-up data.
| Reference | Format | Intervention program characteristics | Length | Comparator | Outcome measures | Attrition (%) | Follow-up |
|---|---|---|---|---|---|---|---|
| Donker et al. (2019) | App | Six animated modules, 360° videos and a gamified immersive VR environment covering the entire exposure spectrum | 3 weeks | Waitlist | AQ | Post: 41 F-U: 59 |
Exploratory results showed that changes were maintained at 3-month follow-up |
| Campos et al. (2019) | Internet | Six exposure scenarios with real photographs and sounds related to different parts of the flying process | 6 weeks (maximum) | Waitlist | FFQ-II FFS |
Post: 28.26 F-U: 52.2 (3 months) and 71 (1 year) |
Maintenance of changes at 3- and 12-month follow ups with larger effect sizes than those obtained for pre-to-post change |
| Andersson et al. (2009) | Internet | Five text modules with psychoeducational information and images, and videos with instructions to carry out the exposure in real life | 4 weeks | One-session treatment face-to-face | BAT SPQ |
Post: 0 F-U: 7.7 |
Changes maintained at 1-year f-u, with equal results than the ones obtained with the OST condition |
| Shahnavaz et al. (2018) | Internet | Twelve modules of guiding text for parents and children, exposure to dentistry-related video clips and audio files and a package with different dental material sent at their homes for exposure purposes | 12 weeks | NA | PG-BAT (child and parental version) | Post: 11.1 F-U: 16.7 |
Clinical changes in the primary outcome measure were maintained at 1-year f-u |
| Andersson et al. (2013) | Internet | Four text modules with psychoeducational information and images, and videos with instructions to carry out the exposure in real life | 4 weeks | One-session treatment face-to-face | BAT SNAQ |
Post: 0 F-U: 23.1 |
There was an improvement in BAT from post-treatment to 1-year f-u and a maintenance of changes in SNAQ |
| Vigerland et al. (2013) | Internet | Eleven modules for parent and children with psychoeducation about SP and exposure tasks for children to carry out in real life guided by their parents | 6 weeks | NA | CSR | Post: 3 F-U: 0 |
Improvement was maintained at 3-month f-u, with even an additional decrease in the CSR |
| Matthews et al. (2011) | Internet | Six-stage hierarchy of images presented for exposure purposes. Images appeared on screen when participants followed a moving circle with their mouse pointer | 30 days | NA | SUDS FSQ SPQ |
Post: 64.7 | NA |
| Matthews et al. (2012) | Internet | Ten stages of moving or static images presented for exposure purposes. Images appeared on screen when participants followed a moving circle with their mouse pointer | 4 months | NA | FSQ SUDS |
Post: 98.2 | NA |
| Arias and McNeil (2020) | App | Exposure video displaying a preventive dental visit that participants had to watch at least once per day | 7 days | Waitlist | SUDS during BAT | Post: 0 | NA |
AQ: Acrophobia Questionnaire; FFQ-II: Fear of Flying Questionnaire-II; FFS: Fear of Flying Scale; BAT: Behavioral Avoidance Test; SPQ: Spider Phobia Questionnaire; PG-BAT: Picture Guided Behavioral Avoidance Test; SNAQ: Snake Phobia Questionnaire; CSR: Clinician Severity Rating; SUDS: Subjective Units of Distress; FSQ: Fear of Spiders Questionnaire; F-U: Follow-up; NA: Not Applicable.
3.4.1. Internet-based interventions
Exposure was the main treatment component of the seven studies on Internet-based interventions, and all of them except one (Vigerland et al., 2013) included images, videos, or audios of the phobic situation or stimuli in the program. However, only three intervention programs (Campos et al., 2019; Matthews et al., 2011, Matthews et al., 2012) carried out the entire exposure to the phobic object within the program using this media content; that is, participants could do the exposure sessions in the intervention webpage confronting these images or videos. In these studies, after the exposure scenarios were presented, participants were asked to rate their anxiety level in order to continue with the next scenarios. Although most of the other studies also included some kind of media content related to the feared object or situation, the main focus was on encouraging participants to do the exposure exercises in the real world. This is the case of the two Andersson et al., 2009, Andersson et al., 2013 interventions, which included videos to show the participants how to carry out the exposure to spiders or snakes in a real environment; Vigerland et al. (2013), who included written instructions for parents to help their children to establish and work towards the most feared level together in their everyday life; or Shahnavaz et al. (2018), who even sent a practice package of dental tools to participants’ homes so that parents and children could do the exposure tasks together.
Psychoeducation about the problem and other related important information was also included in most of the interventions (Andersson et al., 2009, Andersson et al., 2013; Campos et al., 2019; Shahnavaz et al., 2018). The time required for the interventions ranged from one to four months. It is important to note that the study with the longest time requirement (Matthews et al., 2012) only asked participants to log in at least once before a four-month period had ended, but the intervention did not last the whole time. The most common length was four to six weeks.
Regarding therapist support, all the studies except Matthews et al., 2011, Matthews et al., 2012 included this component. Therapist guidance was delivered by phone or e-mail, depending on the intervention. In four studies (Andersson et al., 2009, Andersson et al., 2013; Shahnavaz et al., 2018; Vigerland et al., 2013), participants had to send the homework exercises to the therapist by email or write them on the web platform, and in two of these studies, the therapist provided feedback about the homework (Shahnavaz et al., 2018; Vigerland et al., 2013). Campos et al. (2019) included two experimental conditions in this line: one condition with therapist support consisting of a brief weekly phone call to encourage participants to continue the intervention or resolve doubts, and a completely self-applied condition where participants did not talk with the therapist until they finished the intervention. It is the only study in this review that presents results for therapist guidance, and the data show that both conditions appeared to have comparable efficacy on the phobic outcome measures.
3.4.2. Mobile-based interventions
Two of the studies included in this review were mobile-based interventions, and the main component was also the exposure technique. Both studies used videos related to the phobic situation that the participant had to watch, but one of them (Donker et al., 2019) included a Virtual Reality approach using 360° videos. This study was also the only one of the two that intended to deliver a traditional intervention over the phone, that is, by including different modules the participant had to complete with psychoeducation and CBT components. The other intervention (Arias and McNeil, 2020) only relied on the participant watching the videos for exposure purposes.
The time required for the interventions ranged from seven days to three weeks. Therapist support was included in both studies, via e-mail, in the form of daily or weekly encouragement.
3.5. Narrative synthesis of treatment outcomes
Outcome measures were different in the included studies, given that they were directed towards different types of SP, but overall the results of the interventions were assessed with specific questionnaires for the subtype of SP being investigated, or with other general assessment tools commonly used for phobic disorders, such as the Behavioral Avoidance Test (BAT), its analogous picture-guided version (PG-BAT), the Subjective Units of Distress Scale (SUDS), or the Clinician Severity Rating (CSR; Silverman and Albano, 1996). The questionnaires that assessed the different types of phobic symptomatology in the studies included in this review were the following: Acrophobia Questionnaire (AQ; Cohen, 1977), Fear of Flying Questionnaire-II (FFQ-II; Bornas et al., 1999), Fear of Flying Scale (FFS; Haug et al., 1987), Spider Phobia Questionnaire (SPQ; Klorman et al., 1974), Fear of Spiders Questionnaire (FSQ; Szymanski and O’Donohue, 1995), and the Snake Phobia Questionnaire (SNAQ; Fredrikson, 1983). Table 2 shows the corresponding assessment tools for each study.
Regarding the effectiveness of the interventions, in the RCTs that used a waitlist as a comparator, the intervention condition showed significant reductions in the phobic symptomatology compared to the control group (Arias and McNeil, 2020; Campos et al., 2019; Donker et al., 2019). In the two RCTs that had an active control condition (Andersson et al., 2009, Andersson et al., 2013), in this case a treatment for specific phobia whose effectiveness had already been established (Öst, 1989), the Internet condition also showed a significant improvement in the phobic symptoms. Four of these studies reported large within-group effect sizes for the IMI condition (Andersson et al., 2009, Andersson et al., 2013; Campos et al., 2019; Donker et al., 2019).
Two of the studies that did not have a control condition also showed significant improvements in the outcome measures, with large within-group effect sizes (Shahnavaz et al., 2018; Vigerland et al., 2013). The remaining two studies without comparators, both by the same author (Matthews et al., 2011, Matthews et al., 2012), showed a decrease on the SUDS over time, but only one study showed significant differences on one of the questionnaires after the intervention (Matthews et al., 2011).
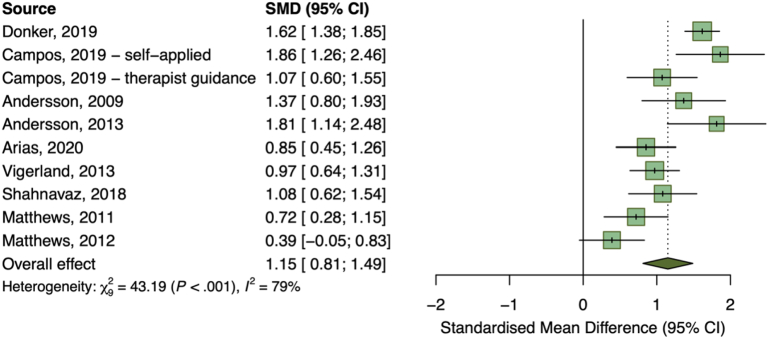
3.6. Preliminary meta-analysis of randomized trials
A preliminary meta-analysis of the nine included studies, with 10 intervention groups, showed that participants receiving IMIs experienced a significant reduction of phobic symptomatology from pre- to post-treatment. The pooled within-group effect size for IMIs was g = 1.15 (95% CI 0.81 to 1.49), with high heterogeneity (I2 = 79%; 95% CI 62 to 89). The forest plot summarizing the results of the meta-analysis is presented in Fig. 2. In sensitivity analyses, the pooled effect size ranged between g = 1.26 (95% CI 0.87 to 1.65) and g = 1.22 (95% CI 0.85 to 1.59), assuming pre-post correlations of 0.25 and 0.5, respectively, and decreased to g = 0.77 (95% CI 0.54 to 1.01) when assuming a correlation of 0.95. Subgroup analyses revealed significant differences based on type of design (Q = 43.19, df = 9, p < 0.0001), with RCTs showing significantly larger within-group effects (g = 1.40; 95% CI 0.98 to 1.83) than pre-post designs (g = 0.80; 95% CI 0.32 to 1.27).
Fig. 2.
Meta-analysis on Internet- and mobile-based interventions for Specific Phobia, based on within-group effect sizes.
For the subgroup of RCTs, between-group effect sizes were computed and pooled separately for those with active and inactive comparators. The three trials (with four intervention groups) that compared IMIs to waitlist control conditions yielded a pooled effect of g = 1.07 (95% CI 0.51 to 1.62). However, no evidence of a significant effect was obtained in two trials comparing IMIs against a face-to-face well-established SP treatment (g = 0.02; 95% CI -1.50 to 1.54).
3.7. Follow-ups
Seven of the nine studies had at least one follow-up, but one of them (Matthews et al., 2012) will not be included in these results because the study presented large drop-out rates and the follow-up was only completed by three participants. Regarding the rest of the studies, three of them carried out a three-month follow up (Campos et al., 2019; Donker et al., 2019; Vigerland et al., 2013) where clinical outcomes for the intervention seemed to be maintained. Four studies had a follow-up after one year (Andersson et al., 2009, Andersson et al., 2013; Campos et al., 2019; Shahnavaz et al., 2018), and they also showed maintenance or improvement on some of the measures. The study by Campos et al. (2019) was the only one that included two follow-ups, at three and 12 months, and they found larger within-group effect sizes than the ones obtained for pre-to-post change.
3.8. Satisfaction and attrition
Four of the studies presented data about patients’ satisfaction with the intervention, and all of them reported a high satisfaction rate (Arias and McNeil, 2020; Donker et al., 2019; Shahnavaz et al., 2018; Vigerland et al., 2013). Although in one of the parent-child interventions (Vigerland et al., 2013) the parent satisfaction was much lower, the results showed that they would still recommend the treatment to a friend.
The attrition rates for the studies ranged from low (0%) to very high (98%), as reported in Table 2. The highest drop-out rate was found in the study by Matthews et al. (2012), where 351 participants were enrolled but only six completed all the intervention stages. However, this study was an exception, and most of the other studies had low or moderate attrition rates at post-treatment. The attrition rates in the follow-ups were higher overall than at post-treatment in the studies that included them, with up to 71% dropping out at the one-year follow-up, as Table 2 shows.
3.9. Study quality assessment
Table 3, Table 4 show the results of the study quality assessment carried out with the NHLBI tool. Two of the categories were used for the studies in this review, specifically, the categories of controlled intervention studies and before-after studies. The RCTs included in this review (Andersson et al., 2009, Andersson et al., 2013; Arias and McNeil, 2020; Campos et al., 2019; Donker et al., 2019) were assessed in the category of controlled intervention studies. Three of them were rated “good”, and the other two were rated “fair”. The reason for rating the two Andersson studies (Andersson et al., 2009, Andersson et al., 2013) “fair” was that they did not include power calculations for the sample size, and they did not conduct intent-to-treat analyses. Apart from that, the only issue with the studies in this category was the moderate drop-out rate in two of the papers (Campos et al., 2019; Donker et al., 2019), but overall, they met the quality criteria.
Table 3.
Quality assessment for controlled studies.
| Donker et al. (2019) | Campos et al. (2019) | Andersson et al. (2009) | Andersson et al. (2013) | Arias and McNeil (2020) | |
|---|---|---|---|---|---|
| 1. Was the study described as randomized, a randomized trial, a randomized clinical trial, or an RCT? | Yes | Yes | Yes | Yes | Yes |
| 2. Was the method of randomization adequate (i.e., use of randomly generated assignment)? | Yes | Yes | Yes | Yes | Yes |
| 3. Was the treatment allocation concealed (so that assignments could not be predicted)? | Yes | Yes | Yes | Yes | Yes |
| 4. Were study participants and providers blinded to treatment group assignment? | No | No | No | No | NR |
| 5. Were the people assessing the outcomes blinded to the participants’ group assignments? | No | No | NR | NR | No |
| 6. Were the groups similar at baseline on important characteristics that could affect outcomes (e.g., demographics, risk factors, co-morbid conditions)? | Yes | Yes | NR | NR | Yes |
| 7. Was the overall drop-out rate from the study at endpoint 20% or lower of the number allocated to treatment? | No | No | Yes | Yes | Yes |
| 8. Was the differential drop-out rate (between treatment groups) at endpoint 15 percentage points or lower? | No | Yes | Yes | Yes | Yes |
| 9. Was there high adherence to the intervention protocols for each treatment group? | Yes | Yes | Yes | Yes | Yes |
| 10. Were other interventions avoided or similar in the groups (e.g., similar background treatments)? | Yes | Yes | Yes | Yes | No |
| 11. Were outcomes assessed using valid and reliable measures, implemented consistently across all study participants? | Yes | Yes | Yes | Yes | Yes |
| 12. Did the authors report that the sample size was sufficiently large to be able to detect a difference in the main outcome between groups with at least 80% power? | Yes | Yes | No | No | Yes |
| 13. Were outcomes reported or subgroups analyzed prespecified (i.e., identified before analyses were conducted)? | Yes | Yes | Yes | Yes | Yes |
| 14. Were all randomized participants analyzed in the group to which they were originally assigned, i.e., did they use an intention-to-treat analysis? | Yes | Yes | No | No | Yes |
| Quality rating | Good | Good | Fair | Fair | Good |
NR: Not Reported.
Table 4.
Quality assessment for before and after studies.
| Shahnavaz et al. (2018) | Vigerland et al. (2013) | Matthews et al. (2011) | Matthews et al. (2012) | |
|---|---|---|---|---|
| 1. Was the study question or objective clearly stated? | Yes | Yes | Yes | Yes |
| 2. Were eligibility/selection criteria for the study population prespecified and clearly described? | Yes | Yes | Yes | No |
| 3. Were the participants in the study representative of those who would be eligible for the test/service/intervention in the general or clinical population of interest? | Yes | Yes | Yes | Yes |
| 4. Were all eligible participants that met the prespecified entry criteria enrolled? | Yes | Yes | NR | No |
| 5. Was the sample size sufficiently large to provide confidence in the findings? | Yes | Yes | Yes | No |
| 6. Was the test/service/intervention clearly described and delivered consistently across the study population? | Yes | Yes | Yes | No |
| 7. Were the outcome measures prespecified, clearly defined, valid, reliable, and assessed consistently across all study participants? | Yes | Yes | Yes | Yes |
| 8. Were the people assessing the outcomes blinded to the participants’ exposures/interventions? | No | No | No | NR |
| 9. Was the loss to follow-up after baseline 20% or less? Were those lost to follow-up accounted for in the analysis? | Yes | Yes | No | No |
| 10. Did the statistical methods examine changes in outcome measures from before to after the intervention? Were statistical tests done that provided p values for the pre-to-post changes? | Yes | Yes | Yes | Yes |
| 11. Were outcome measures of interest taken multiple times before the intervention and multiple times after the intervention (i.e., did they use an interrupted time-series design)? | No | Yes | No | No |
| 12. If the intervention was conducted at a group level (e.g., a whole hospital, a community, etc.) did the statistical analysis take into account the use of individual-level data to determine effects at the group level? | NA | NA | NA | NA |
| Quality rating | Good | Good | Poor | Poor |
NR: Not reported; NA: Not applicable.
In the case of the uncontrolled studies, two of them were rated “good” (Shahnavaz et al., 2018; Vigerland et al., 2013), and the other two were rated “poor” (Matthews et al., 2011, Matthews et al., 2012). In the latter studies, there was no power calculation for the sample size, they had a high or very high drop-out rate, or the inclusion criteria were vague. Therefore, two studies were rated as having a high risk of bias.
The criterion of blinded assessment of the treatment outcomes was not met by any of the studies, but this can be difficult in psychological interventions. However, this was also taken into consideration in the assessment of the quality of the studies.
4. Discussion
The aim of the present study was to summarize the characteristics and treatment outcomes of IMIs for SP in a systematic review. To the best of our knowledge, this is the first review to address this topic.
As previously stated, research in this field has been scarce so far, which was reflected in the number of papers included in this review. Only nine papers met the inclusion criteria, seven Internet-based interventions and two mobile-based interventions. Therefore, the following conclusions should be interpreted with caution. However, despite the small number of studies, the results seem promising. The results of the majority of the studies included in the current review indicate that significant improvements in phobic symptoms can be achieved with IMIs. These promising results are also supported by a preliminary meta-analysis of the nine included studies, where a large effect size for IMIs was observed.
Regarding the characteristics of the samples included, there were more women than men, which coincides with epidemiological studies suggesting that there is a higher prevalence of SP among females (Wardenaar et al., 2017). The most common subtype of SP in the studies was animal phobia; four of the studies included treated this type of phobia, and even in the study that included different subtypes of SP in the sample (Vigerland et al., 2013), animal phobia was the most frequent one. Animal phobia is also the subtype with the highest prevalence in epidemiological studies (Eaton et al., 2018; Wardenaar et al., 2017). Additionally, the different interventions show that it is possible to have IMIs for the treatment of SP in different populations because interventions for children, adolescents, and adults have been developed and used. However, no studies were found for older people, and this could be a field in need of more research because some data show a peak in the incidence of phobias in this age group (Eaton et al., 2018).
Exposure was the main component of all the intervention programs included, which was expected because exposure-based treatments for SP are well known in the literature as the best approach to treat this problem in adults (Wolitzky-Taylor et al., 2008) and children (Ollendick and Davis, 2013). In all the studies, the exposure was delivered from a traditional habituation perspective, that is, by presenting the phobic stimulus and waiting until the anxiety levels decreased, and they did not seem to include more contemporary approaches such as inhibitory learning (Craske et al., 2014). Images, audios, and videos of the phobic stimuli were also an important component of the intervention programs, with five of the studies (Arias and McNeil, 2020; Campos et al., 2019; Donker et al., 2019; Matthews et al., 2011, Matthews et al., 2012) carrying out the exposure inside the program or app with these media resources. Representations of the phobic stimuli, such as pictures, elicit fear reactions in phobic patients. For this reason, therapists also use them in their clinical settings to start exposure therapy or when the feared situation is difficult to access. Thus, IMIs have the potential of delivering interventions for phobias if they have an adequate structure and clear guidelines for patients.
Overall, treatment outcomes for phobic symptomatology were positive in most of the studies, reporting significant pre-to-post treatment changes in participants and, in some cases, large effect sizes. A preliminary meta-analysis of the nine included studies suggested that IMIs contributed to a significant reduction of SP symptoms from pre- to post-treatment, showing large pooled effect size. Particularly large reductions were observed in participants allocated to IMI groups in RCTs, compared to participants taking part in pre-post studies. This could suggest that RCTs might optimize treatment effects, as compared to the effects observed in more naturalistic designs that might be closer to routine care. However, the small number of studies hinders the interpretation of these differences.
Given that RCTs are the gold-standard design to examine treatment effects, we further estimated the efficacy of IMIs by focusing only on between-group effect sizes derived from RCTs. Compared to participants allocated to waiting list control groups, participants receiving IMIs experienced significantly lower SP symptoms at post-treatment. A large pooled effect size was observed for IMIs, although only three RCTs were available in this analysis. On the other hand, no significant effects were observed when comparing IMIs against a face-to-face well-established SP treatment. Nevertheless, only two trials with small sample sizes were included in this comparison, which limits considerably the statistical power that is needed for detecting differences between two effective treatments.
Regarding the maintenance of the clinical changes over time, the studies also reported some promising evidence (Andersson et al., 2009, Andersson et al., 2013; Campos et al., 2019; Donker et al., 2019; Shahnavaz et al., 2018; Vigerland et al., 2013). The only study that did not report significant changes after the intervention on the outcome measures was the one by Matthews et al. (2012). However, this study has the largest drop-out rate (98%), and, therefore, these results are probably biased, given that the study was also rated as having “poor” quality. A possible explanation for this would be that therapeutic support, one of the factors that has been related to better treatment outcomes and higher adherence rates (Domhardt et al., 2019), was not included in the treatment. Furthermore, it was the study that gave participants the most time to complete the treatment, even though the treatment only consisted of 10 stages. Participants in the other interventions included in this review also had flexibility and freedom to access the program, as is common in self-help interventions, but the time span to complete the intervention was significantly shorter, and they also had more specific instructions (i.e. to complete one module each week). This aspect should be taken into consideration when developing future interventions, in order to overcome high drop-out rates.
The study by Campos et al. (2019) explored the role of therapist support and did not find significant differences between the completely self-applied group and the one that received weekly calls. Nevertheless, no conclusions can be drawn because most of the other programs had some type of therapist support, and those that did not (Matthews et al., 2011, Matthews et al., 2012) were rated as having insufficient quality. However, previous research on Internet-based interventions for anxiety also suggests that there are no differences between guided and unguided interventions in terms of treatment outcomes (Olthuis et al., 2016), and that even though guided interventions might be more beneficial, the differences might be smaller than previously thought (Baumeister et al., 2014). As mentioned above, mobile-based interventions are still a relatively new field, and evidence about the role of guidance is still scarce.
Finally, the mean drop-out rate in the studies in this review at post-test was 27.36%, and 29.58% at follow-up, which is lower than the drop-out rate found in IMIs for other emotional disorders such as depression (Josephine et al., 2017). However, the attrition rates varied across the different studies, and so this result must be interpreted with caution. Furthermore, it is also important to note that the follow-up periods were also different in the studies, with some of them including follow-ups after three months and others after one year.
Some limitations of this review should be acknowledged. First, the important heterogeneity in the studies included, in terms of sample size, study design, and outcome measures, makes it difficult to generalize the results. Second, the small number of studies included does not allow us to draw firm conclusions. Specifically, the results of the preliminary meta-analysis should be viewed with caution. Related to this point, the number of mobile-based interventions was very low, with only two studies included, and it was not compensated by the number of Internet-based interventions. Third, this review only included published studies, which can lead to an overestimation of treatment results due to publication bias. Finally, the interpretation of the results is limited to the authors who conducted this systematic review.
5. Conclusions
This systematic review found that interventions for the treatment of SP through IMIs have been developed, and there is already some evidence in the literature supporting the potential benefits of these treatments. However, the number of studies is still small, and firm conclusions cannot be drawn. There is still a need to explore the specific components an IMI for SP should have, use active comparators with larger sample sizes, examine the role of therapeutic guidance and to what degree it is necessary in these interventions, and determine what factors should be considered to improve adherence to these treatments.
Although relatively few studies have been conducted, we aimed to summarize what researchers have found so far, in order to create more interest in this field and guide future research.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This work was supported by Spanish Ministerio de Ciencia, Innovación y Universidades (Programa Estatal I+D+i. RTI2018-100993-B-100), 2018 Research Promotion Plan at Universitat Jaume I (UJI-2018-57), CIBEROBN, an initiative of the ISCIII (ISC III CB06 03/0052), and PhD grant from Generalitat Valenciana (ACIF/2017/191).
Contributor Information
Sonia Mor, Email: smor@uji.es.
Jorge Grimaldos, Email: grimaldo@uji.es.
Cintia Tur, Email: ctur@uji.es.
Clara Miguel, Email: clara.miguelsanz@vu.nl.
Pim Cuijpers, Email: p.cuijpers@vu.nl.
Cristina Botella, Email: botella@uji.es.
Soledad Quero, Email: squero@uji.es.
Appendix A. Search strings used in the systematic review
| Phobia block | Phobi* OR “Phobic Disorders” OR “Specific Phobia” OR “Dental Anxiety” OR “Acrophobia” OR “Claustrophobia” |
| Intervention block | “Internet-based intervention” OR “Internet-based treatment” OR “Internet-delivered treatment” OR “Internet-delivered intervention” OR “online treatment” OR “Mobile App* OR “mhealth” OR “android” OR “iphone” OR “Smartphone” OR “mobile-based” OR “App” OR “Cell phone” OR “Web-based intervention” OR “Web-based treatment” OR “internet intervention” |
| Word combination for search in databases | (“Phobi*” AND “Internet-based intervention”) OR (“Phobi*” AND “Internet-based treatment”) OR (“Phobi*” AND “Internet-delivered treatment”) OR (“Phobi*” AND “Internet-delivered intervention”) OR (“Phobi*” AND “online treatment”) OR (“Phobi*” AND “online intervention”) OR (“Phobi*” AND “mobile app*”) OR (“Phobi*” AND “mhealth”) OR (“Phobi*” AND “android”) OR (“Phobi*” AND “iphone”) OR (“Phobi*” AND “smartphone”) OR (“Phobi*” AND “mobile-based”) OR (“Phobi*” AND “app”) OR (“Phobi*” AND “cell phone”) OR (“Phobi*” AND “web-based intervention”) OR (“Phobi*” AND “web-based treatment”) OR (“Phobi*” AND “Internet intervention”) OR (“Phobi*” AND “Internet treatment”) OR (“phobic disorder” AND “Internet-based intervention”) OR (“phobic disorder” AND “internet-based treatment”) OR (“phobic disorder” AND “internet-delivered treatment”) OR (“phobic disorder” AND “internet-delivered intervention”) OR (“phobic disorder” AND “online treatment”) OR (“phobic disorder” AND “online intervention”) OR (“phobic disorder” AND “mobile app*”) OR (“phobic disorder” AND “mhealth”) OR (“phobic disorder” AND “android”) OR (“phobic disorder” AND “iphone”) OR (“phobic disorder” AND “smartphone”) OR (“phobic disorder” AND “mobile-based”) OR (“phobic disorder” AND “app”) OR (“phobic disorder” AND “cell phone”) OR (“phobic disorder” AND “web-based intervention”) OR (“phobic disorder” AND “web-based treatment”) OR (“phobic disorder” AND “internet intervention”) OR (“phobic disorder” AND “internet treatment”) OR (“Specific phobia” AND “Internet-based intervention”) OR (“Specific phobia” AND “internet-based treatment”) OR (“Specific phobia” AND “internet-delivered treatment”) OR (“Specific phobia” AND “internet-delivered intervention”) OR (“Specific phobia” AND “online treatment”) OR (“Specific phobia” AND “online intervention”) OR (“Specific phobia” AND “mobile app*”) OR (“Specific phobia” AND “mhealth”) OR (“Specific phobia” AND “android”) OR (“Specific phobia” AND “iphone”) OR (“Specific phobia” AND “smartphone”) OR (“Specific phobia” AND “mobile-based”) OR (“Specific phobia” AND “app”) OR (“Specific phobia” AND “cell phone”) OR (“Specific phobia” AND “web-based intervention”) OR (“Specific phobia” AND “web-based treatment”) OR (“Specific phobia” AND “internet Intervention”) OR (“Specific phobia” AND “internet treatment”) OR (“Dental Anxiety” AND “Internet-based intervention”) OR (“Dental Anxiety” AND “internet-based treatment”) OR (“Dental Anxiety” AND “internet-delivered treatment”) OR (“Dental Anxiety” AND “internet-delivered intervention”) OR (“Dental Anxiety” AND “online treatment”) OR (“Dental Anxiety” AND “online intervention”) OR (“Dental Anxiety” AND “mobile app*”) OR (“Dental Anxiety” AND “mhealth”) OR (“Dental Anxiety” AND “android”) OR (“Dental Anxiety” AND “iphone”) OR (“Dental Anxiety” AND “smartphone”) OR (“Dental Anxiety” AND “mobile-based”) OR (“Dental Anxiety” AND “app”) OR (“Dental Anxiety” AND “cell phone”) OR (“Dental Anxiety” AND “web-based intervention”) OR (“Dental Anxiety” AND “web-based treatment”) OR (“Dental Anxiety” AND “Internet Intervention”) OR (“Dental Anxiety” AND “Internet treatment”) OR (“Acrophob*” AND “internet-delivered intervention”) OR (“Acrophob*” AND “online treatment”) OR (“Acrophob*” AND “online intervention”) OR (“Acrophob*” AND “mobile app*”) OR (“Acrophob*” AND “mhealth”) OR (“Acrophob*” AND “android”) OR (“Acrophob*” AND “iphone”) OR (“Acrophob*” AND “smartphone”) OR (“Acrophob*” AND “mobile-based”) OR (“Acrophob*” AND “app”) OR (“Acrophob*” AND “cell phone”) OR (“Acrophob*” AND “web-based intervention”) OR (“Acrophob*” AND “web-based treatment”) OR (“Acrophob*” AND “Internet Intervention”) OR (“Acrophob*” AND “Internet treatment”) OR (“Claustrophob*” AND “Internet-based intervention”) OR (“Claustrophob*” AND “Internet-based treatment”) OR (“Claustrophob*” AND “Internet-delivered treatment”) OR (“Claustrophob*” AND “Internet-delivered intervention”) OR (“Claustrophob*” AND “online treatment”) OR (“Claustrophob*” AND “online intervention”) OR (“Claustrophob*” AND “mobile app*”) OR (“Claustrophob*” AND “mhealth”) OR (“Claustrophob*” AND “android”) OR (“Claustrophob*” AND “iphone”) OR (“Claustrophob*” AND “smartphone”) OR (“Claustrophob*” AND “mobile-based”) OR (“Claustrophob*” AND “app”) OR (“Claustrophob*” AND “cell phone”) OR (“Claustrophob*” AND “web-based intervention”) OR (“Claustrophob*” AND “web-based treatment”) OR (“Claustrophob*” AND “Internet intervention”) OR (“Claustrophob*” AND “Internet treatment”) |
References
- Andersson G., Titov N. Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatry. 2014;13:4–11. doi: 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G., Waara J., Jonsson U., Malmaeus F., Carlbring P., Öst L.G. Internet-based self-help versus one-session exposure in the treatment of spider phobia: a randomized controlled trial. Cogn. Behav. Ther. 2009;38:114–120. doi: 10.1080/16506070902931326. [DOI] [PubMed] [Google Scholar]
- Andersson G., Waara J., Jonsson U., Malmaeus F., Carlbring P., Öst L.G. Internet-based exposure treatment versus one-session exposure treatment of Snake phobia: a randomized controlled trial. Cogn. Behav. Ther. 2013;42:284–291. doi: 10.1080/16506073.2013.844202. [DOI] [PubMed] [Google Scholar]
- Andrews G., Basu A., Cuijpers P., Craske M.G., McEvoy P., English C.L., Newby J.M. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: an updated meta-analysis. Journal of Anxiety Disorders. 2018 doi: 10.1016/j.janxdis.2018.01.001. [DOI] [PubMed] [Google Scholar]
- Arias M.C., McNeil D.W. Smartphone-based exposure treatment for dental phobia: a pilot randomized clinical trial. J. Public Health Dent. 2020;80:23–30. doi: 10.1111/jphd.12340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnberg F.K., Linton S.J., Hultcrantz M., Heintz E., Jonsson U. Internet-delivered psychological treatments for mood and anxiety disorders: a systematic review of their efficacy, safety, and cost-effectiveness. PLoS ONE. 2014 doi: 10.1371/journal.pone.0098118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister H., Reichler L., Munzinger M., Lin J. The impact of guidance on internet-based mental health interventions - a systematic review. Internet Interv. 2014 doi: 10.1016/j.invent.2014.08.003. [DOI] [Google Scholar]
- Böhnlein J., Altegoer L., Muck N.K., Roesmann K., Redlich R., Dannlowski U., Leehr E.J. Factors influencing the success of exposure therapy for specific phobia: a systematic review. Neurosci. Biobehav. Rev. 2020 doi: 10.1016/j.neubiorev.2019.12.009. [DOI] [PubMed] [Google Scholar]
- Bornas F.X., Tortella-Feliu M., de la Banda García, García G., Fullana Rivas M.Á., Llabrés J. 1999. Validación factorial del cuestionario de miedo a volar. Análisis y modificación de conducta. [Google Scholar]
- Botella C., Quero S., Banos R.M., Garcia-Palacios A., Breton-Lopez J., Alcaniz M., Fabregat S. Telepsychology and self-help: the treatment of phobias using the internet. Cyberpsychol. Behav. 2008;11:659–664. doi: 10.1089/cpb.2008.0012. [DOI] [PubMed] [Google Scholar]
- Botella C., Fernández-Álvarez J., Guillén V., García-Palacios A., Baños R. Recent Progress in virtual reality exposure therapy for phobias: a systematic review. Curr Psychiatry Rep. 2017;19 doi: 10.1007/s11920-017-0788-4. [DOI] [PubMed] [Google Scholar]
- Campos D., Bretón-López J., Botella C., Mira A., Castilla D., Mor S., Baños R., Quero S. Efficacy of an internet-based exposure treatment for flying phobia (NO-FEAR Airlines) with and without therapist guidance: a randomized controlled trial. BMC Psychiatry. 2019;19:1–16. doi: 10.1186/s12888-019-2060-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring P., Andersson G., Cuijpers P., Riper H., Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn. Behav. Ther. 2018 doi: 10.1080/16506073.2017.1401115. [DOI] [PubMed] [Google Scholar]
- Cohen D.C. Comparison of self-report and overt-behavioral procedures for assessing acrophobia. Behav. Ther. 1977;8:17–23. doi: 10.1016/S0005-7894(77)80116-0. [DOI] [Google Scholar]
- Craske M.G., Treanor M., Conway C.C., Zbozinek T., Vervliet B. Maximizing exposure therapy: an inhibitory learning approach. Behav. Res. Ther. 2014;58:10–23. doi: 10.1016/j.brat.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domhardt M., Geßlein H., von Rezori R.E., Baumeister H. Internet- and mobile-based interventions for anxiety disorders: a meta-analytic review of intervention components. Depress. Anxiety. 2019 doi: 10.1002/da.22860. [DOI] [PubMed] [Google Scholar]
- Donker T., Cornelisz I., van Klaveren C., van Straten A., Carlbring P., Cuijpers P., van Gelder J.L. Effectiveness of self-guided app-based virtual reality cognitive behavior therapy for acrophobia: a randomized clinical trial. JAMA Psychiatry. 2019;76:682–690. doi: 10.1001/jamapsychiatry.2019.0219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton W.W., Bienvenu O.J., Miloyan B. Specific phobias. Lancet Psychiatry. 2018 doi: 10.1016/S2215-0366(18)30169-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J., Torous J., Nicholas J., Carney R., Rosenbaum S., Sarris J. Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. J. Affect. Disord. 2017 doi: 10.1016/j.jad.2017.04.046. [DOI] [PubMed] [Google Scholar]
- Fredrikson M. Reliability and validity of some specific fear questionnaires. Scand. J. Psychol. 1983;24 doi: 10.1111/j.1467-9450.1983.tb00507.x. [DOI] [PubMed] [Google Scholar]
- Haug T., Berntzen D., Götestam K.G., Brenne L., Johnsen B.H., Hugdahl K. A three-systems analysis of fear of flying: a comparison of a consonant vs a non-consonant treatment method. Behav. Res. Ther. 1987;25 doi: 10.1016/0005-7967(87)90045-3. [DOI] [PubMed] [Google Scholar]
- IntHout J., Ioannidis J.P., Borm G.F. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med. Res. Methodol. 2014;14(1) doi: 10.1186/1471-2288-14-25. 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josephine K., Josefine L., Philipp D., David E., Harald B. Internet- and mobile-based depression interventions for people with diagnosed depression: a systematic review and meta-analysis. J. Affect. Disord. 2017 doi: 10.1016/j.jad.2017.07.021. [DOI] [PubMed] [Google Scholar]
- Karyotaki E., Riper H., Twisk J., Hoogendoorn A., Kleiboer A., Mira A., MacKinnon A., Meyer B., Botella C., Littlewood E., Andersson G., Christensen H., Klein J.P., Schröder J., Bretón-López J., Scheider J., Griffiths K., Farrer L., Huibers M.J.H., Phillips R., Gilbody S., Moritz S., Berger T., Pop V., Spek V., Cuijpers P. Efficacy of self-guided internet-based cognitive behavioral therapy in the treatment of depressive symptoms a meta-analysis of individual participant data. JAMA Psychiatry. 2017;74:351–359. doi: 10.1001/jamapsychiatry.2017.0044. [DOI] [PubMed] [Google Scholar]
- Karyotaki E., Ebert D.D., Donkin L., Riper H., Twisk J., Burger S., Rozental A., Lange A., Williams A.D., Zarski A.C., Geraedts A., van Straten A., Kleiboer A., Meyer B., Ünlü Ince B.B., Buntrock C., Lehr D., Snoek F.J., Andrews G., Andersson G., Choi I., Ruwaard J., Klein J.P., Newby J.M., Schröder J., Laferton J.A.C., van Bastelaar K., Imamura K., Vernmark K., Boß L., Sheeber L.B., Kivi M., Berking M., Titov N., Carlbring P., Johansson R., Kenter R., Perini S., Moritz S., Nobis S., Berger T., Kaldo V., Forsell Y., Lindefors N., Kraepelien M., Björkelund C., Kawakami N., Cuijpers P. Do guided internet-based interventions result in clinically relevant changes for patients with depression? An individual participant data meta-analysis. Clin. Psychol. Rev. 2018 doi: 10.1016/j.cpr.2018.06.007. [DOI] [PubMed] [Google Scholar]
- Kato K., Miyashita H. UIST 2015 - Adjunct Publication of the 28th Annual ACM Symposium on User Interface Software and Technology. Association for Computing Machinery, Inc; 2015. Creating a mobile head-mounted display with proprietary controllers for interactive virtual reality content; pp. 35–36. [DOI] [Google Scholar]
- Kazdin A.E., Blase S.L. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect. Psychol. Sci. 2011;6:21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- Kelson J., Rollin A., Ridout B., Campbell A. Internet-delivered acceptance and commitment therapy for anxiety treatment: systematic review. J. Med. Internet Res. 2019;21 doi: 10.2196/12530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klorman R., Weerts T.C., Hastings J.E., Melamed B.G., Lang P.J. Psychometric description of some specific-fear questionnaires. Behav. Ther. 1974;5 doi: 10.1016/S0005-7894(74)80008-0. [DOI] [Google Scholar]
- Kuester A., Niemeyer H., Knaevelsrud C. Internet-based interventions for posttraumatic stress: a meta-analysis of randomized controlled trials. Clin. Psychol. Rev. 2016 doi: 10.1016/j.cpr.2015.11.004. [DOI] [PubMed] [Google Scholar]
- Lewis C., Roberts N.P., Bethell A., Robertson L., Bisson J.I. Internet-based cognitive and behavioural therapies for posttraumatic stress disorder (PTSD) in adults. Cochrane Database Syst. Rev. 2018 doi: 10.1002/14651858.CD011710.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks I.M. Oxford University Press; 1987. [Google Scholar]
- Matthews A.J., Wong Z.H., Scanlan J.D., Kirkby K.C. Online exposure for spider phobia: continuous versus intermittent exposure. Behav. Chang. 2011;28:143–155. doi: 10.1375/bech.28.3.143. [DOI] [Google Scholar]
- Matthews A.J., Scanlan J.D., Kirkby K.C. Online exposure treatment for spider fear: the effects of moving versus static images on treatment adherence, fear elicitation and habituation. Behav. Chang. 2012;29:15–24. doi: 10.1017/bec.2012.7. [DOI] [Google Scholar]
- Menon V., Rajan T.M., Sarkar S. Psychotherapeutic Applications of Mobile Phone-based Technologies: A Systematic Review of Current Research and Trends. 2017 doi: 10.4103/0253-7176.198956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miralles I., Granell C., Díaz-Sanahuja L., van Woensel W., Bretón-López J., Mira A., Castilla D., Casteleyn S. Smartphone apps for the treatment of mental disorders: systematic review. JMIR mHealth and uHealth. 2020 doi: 10.2196/14897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Altman D., Antes G., Atkins D., Barbour V., Barrowman N., Berlin J.A., Clark J., Clarke M., Cook D., D’Amico R., Deeks J.J., Devereaux P.J., Dickersin K., Egger M., Ernst E., Gøtzsche P.C., Grimshaw J., Guyatt G., Higgins J., Ioannidis J.P.A., Kleijnen J., Lang T., Magrini N., McNamee D., Moja L., Mulrow C., Napoli M., Oxman A., Pham B., Rennie D., Sampson M., Schulz K.F., Shekelle P.G., Tovey D., Tugwell P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neudeck P., Einsle F. Exposure Therapy: Rethinking the Model - Refining the Method. Springer; New York: 2012. Dissemination of exposure therapy in clinical practice: how to handle the barriers? pp. 23–34. [DOI] [Google Scholar]
- Ollendick T.H., Davis T.E. One-session treatment for specific phobias: a review of Öst’s single-session exposure with children and adolescents. Cogn. Behav. Ther. 2013;42:275–283. doi: 10.1080/16506073.2013.773062. [DOI] [PubMed] [Google Scholar]
- Olthuis J.V., Watt M.C., Bailey K., Hayden J.A., Stewart S.H. Therapist-supported internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database Syst. Rev. 2016;3:CD011565. doi: 10.1002/14651858.CD011565.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öst L.G. One-session treatment for specific phobias. Behav. Res. Ther. 1989;27:1–7. doi: 10.1016/0005-7967(89)90113-7. [DOI] [PubMed] [Google Scholar]
- Sewart A.R., Craske M.G. Clinical Handbook of Fear and Anxiety: Maintenance Processes and Treatment Mechanisms. American Psychological Association; 2019. Inhibitory learning; pp. 265–285. [DOI] [Google Scholar]
- Shahnavaz S., Hedman-Lagerlöf E., Hasselblad T., Reuterskiöld L., Kaldo V., Dahllöf G. Internet-based cognitive behavioral therapy for children and adolescents with dental anxiety: open trial. J. Med. Internet Res. 2018;20 doi: 10.2196/jmir.7803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman W.K., Albano A.M. Oxford University Press; 1996. [Google Scholar]
- Stupar-Rutenfrans S., Ketelaars L.E.H., van Gisbergen M.S. Beat the fear of public speaking: mobile 360° video virtual reality exposure training in home environment reduces public speaking anxiety. Cyberpsychol. Behav. Soc. Netw. 2017;20:624–633. doi: 10.1089/cyber.2017.0174. [DOI] [PubMed] [Google Scholar]
- Szymanski J., O’Donohue W. Fear of spiders questionnaire. J. Behav. Ther. Exp. Psychiatry. 1995;26 doi: 10.1016/0005-7916(94)00072-T. [DOI] [PubMed] [Google Scholar]
- Trumpf J., Margraf J., Vriends N., Meyer A.H., Becker E.S. Specific phobia predicts psychopathology in young women. Soc. Psychiatry Psychiatr. Epidemiol. 2010;45:1161–1166. doi: 10.1007/s00127-009-0159-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Beugen S., Ferwerda M., Hoeve D., Rovers M.M., Spillekom-Van Koulil S., van Middendorp H., Evers A.W.M. Internet-based cognitive behavioral therapy for patients with chronic somatic conditions: a meta-analytic review. J. Med. Internet Res. 2014;16 doi: 10.2196/jmir.2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viechtbauer W. Bias and Efficiency of Meta-Analytic Variance Estimators in the Random-Effects Model. J. Educ. Behav. Stat. 2005;30:261–293. doi: 10.3102/10769986030003261. [DOI] [Google Scholar]
- Vigerland S., Thulin U., Ljótsson B., Svirsky L., Öst L.G., Lindefors N., Andersson G., Serlachius E. Internet-delivered CBT for children with specific phobia: a pilot study. Cogn. Behav. Ther. 2013;42:303–314. doi: 10.1080/16506073.2013.844201. [DOI] [PubMed] [Google Scholar]
- Wardenaar K.J., Lim C.C.W., Al-Hamzawi A.O., Alonso J., Andrade L.H., Benjet C., Bunting B., de Girolamo G., Demyttenaere K., Florescu S.E., Gureje O., Hisateru T., Hu C., Huang Y., Karam E., Kiejna A., Lepine J.P., Navarro-Mateu F., Oakley Browne M., Piazza M., Posada-Villa J., ten Have M.L., Torres Y., Xavier M., Zarkov Z., Kessler R.C., Scott K.M., de Jonge P. The cross-national epidemiology of specific phobia in the world mental health surveys. Psychol. Med. 2017;47:1744–1760. doi: 10.1017/S0033291717000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler T.F., Mühlberger A., Kümpers F. Inferiority or even superiority of virtual reality exposure therapy in phobias? - A systematic review and quantitative meta-analysis on randomized controlled trials specifically comparing the efficacy of virtual reality exposure to gold standard in vivo exposure in agoraphobia, specific phobia and social phobia. Front. Psychol. 2019 doi: 10.3389/fpsyg.2019.01758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witthauer C., Ajdacic-Gross V., Meyer A.H., Vollenweider P., Waeber G., Preisig M., Lieb R. Associations of specific phobia and its subtypes with physical diseases: an adult community study. BMC Psychiatry. 2016;16 doi: 10.1186/s12888-016-0863-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitzky-Taylor K.B., Horowitz J.D., Powers M.B., Telch M.J. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin. Psychol. Rev. 2008;28:1021–1037. doi: 10.1016/J.CPR.2008.02.007. [DOI] [PubMed] [Google Scholar]