Abstract
Aim
To determine whether our E-diary can be used to diagnose migraine and provide more reliable migraine-related frequency numbers compared to patients’ self-reported estimates.
Methods
We introduced a self-developed E-diary including automated algorithms differentiating headache and migraine days, indicating whether a patient has migraine. Reliability of the E-diary diagnosis in combination with two previously validated E-questionnaires was compared to a physician’s diagnosis as gold standard in headache patients referred to the Leiden Headache Clinic (n = 596). In a subset of patients with migraine (n = 484), self-estimated migraine-related frequencies were compared to diary-based results.
Results
The first migraine screening approach including an E-headache questionnaire, and the E-diary revealed a sensitivity of 98% and specificity of 17%. In the second approach, an E-migraine questionnaire was added, resulting in a sensitivity of 79% and specificity of 69%. Mean self-estimated monthly migraine days, non-migrainous headache days and days with acute medication use were different from E-diary-based results (absolute mean difference ± standard deviation respectively 4.7 ± 5.0, 6.2 ± 6.6 and 4.3 ± 4.8).
Conclusion
The E-diary including algorithms differentiating headache and migraine days showed usefulness in diagnosing migraine. The use emphasised the need for E-diaries to obtain reliable information, as patients do not reliably recall numbers of migraine days and acute medication intake. Adding E-diaries will be helpful in future headache telemedicine.
Keywords: Telemedicine, electronic diary, data reliability, migraine
Introduction
The gold standard for diagnosing migraine is based on information obtained from a clinical interview and physical and neurological examination. Due to the episodic nature of the disease, most patients experience difficulties in recalling details on frequency and specific characteristics of each individual attack. Daily prospective electronic diaries (E-diaries) may reduce recall bias and increase the reliability of patients’ descriptions of migraine attack characteristics (1). Therefore, E-diaries may have an added value both in clinical practice and for research purposes. In addition, the need for telemedicine was recently emphasised due to the coronavirus outbreak (COVID-19), which made it impossible for certain groups of patients to visit their general practitioner or the hospital. Various telemedicine approaches are already being used in other chronic neurological disorders (2).
There is growing attention for self-monitoring mobile phone E-applications that allow patients with chronic disorders, including migraine, to monitor their own disease-related symptoms or health parameters (3,4). Keeping a headache E-diary may help to discover unrecognised trigger factors, but it can also show that some perceived trigger factors are not as reliable as believed (5). As an example, the need for diary-based information in migraine has emerged from studies showing inaccuracy of self-reported menstrual migraine diagnoses and menstrual cycle lengths (6,7). Although a headache E-diary is not mandatory in clinical practice, its use can be helpful in diagnosing specific headache disorders, such as chronic migraine, menstrual migraine, and medication-overuse headache. In addition, responses to preventive and acute medications could be closely monitored. However, most available daily E-diaries for migraine lack specificity as often only one simple question is asked, such as “Did you suffer from headache today?” or “Did you suffer from migraine today?”, reporting on drug intake but failing to determine whether a reported day was fulfilling the criteria of the International Classification of Headache Disorders third edition (ICHD-3) for migraine (8).
We have developed a time-locked headache E-diary enabling the collection of accurate data for clinical and research purposes based on detailed daily characteristics and an automated algorithm. Additionally, patients with migraine and their physicians receive visual summary reports of registered E-diary data on a daily basis, which provides insight into the course of detailed characteristics over time.
With the current study, we aimed to determine the usefulness of our E-diary in diagnosing migraine in a large group of headache patients referred to the Leiden Headache Clinic of the Leiden University Medical Center by comparing the reliability of the E-diary diagnosis in combination with previously validated E-questionnaires to a physician’s diagnosis as gold standard. In addition, we assessed the added value of E-diaries in the subset of clinically diagnosed patients with migraine, by comparing patients’ self-reported estimates on mean numbers of monthly migraine days, non-migrainous headache days and days with acute medication use to numbers based on E-diaries. Lastly, various criteria on headache duration (e.g. at least 4 h or at least 30 min) are currently used in randomised clinical trials when defining a migraine day, if no migraine-specific acute treatment was taken. We aimed to determine the consequence of using different criteria for headache duration in the definition of migraine days by comparing mean monthly numbers of migraine days based on both time criteria.
Methods
Study population and study flow
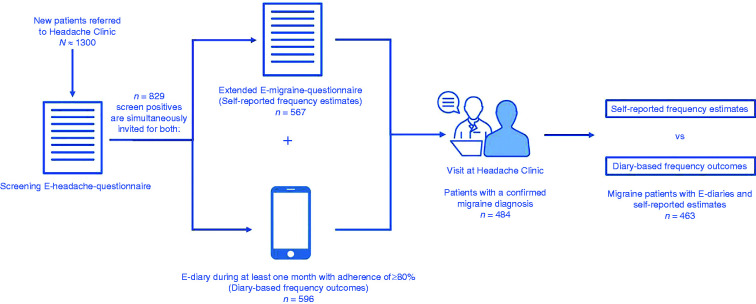
For this study, we identified new patients referred to the Leiden Headache Clinic of the Leiden University Medical Center between October 2018 and May 2020. Study flow is shown in Figure 1. Firstly, headache patients had to fulfill the screening criteria for migraine based on an adapted version of a validated web-based screening E-headache questionnaire (Supplementary information) (9). Using an automated algorithm, screen positives (potential patients with migraine) received an invitation to complete an extended E-migraine questionnaire, after which a validated automated algorithm also determined migraine (subtype) according to ICHD-3 criteria (Supplementary information) (10). Additionally, screen positives were simultaneously asked to complete a daily headache E-diary, starting at least one month prior to their first consultation at the Leiden Headache Clinic. Patients that were screen positive on both migraine and cluster headache were excluded. Only E-diaries registered preceding a first consultation at the Headache Clinic were used for this study. To be eligible for this study, adherence to the E-diary had to be at least 80% of the total registration period. Final diagnosis of patients was made based on the ICHD-3 criteria (8) after a clinical interview and physical and neurological examination by a neurology-resident with consultation of a headache specialist (GMT and/or RF) or by one of the other neurologists with headache expertise at the Leiden Headache Clinic. The study was approved by the medical ethics committee of the Leiden University Medical Center. Since data collection was embedded in clinical practice, patients provided a temporally informed consent at the start of data collection. After their first consultation, they were additionally asked for written informed consent.
Figure 1.
Visual representation of the study flow.
Headache E-diary
The Leiden Headache Center has developed a web-based and time-locked E-diary. Patients received a daily link at 9.00 am by email to access the E-diary covering the previous 24 h (from midnight to midnight), consisting of 6–31 questions depending on a negative/positive reply regarding the presence of headache including its detailed characteristics and associated symptoms (one sided, throbbing, intensity, increasing with physical activities, photophobia/phonophobia, nausea, vomiting), presence of aura symptoms including its characteristics and duration, use of acute (headache-specific) pain medication, (changes in) prophylactic headache medication, presence of menstruation, general wellbeing and pain coping. Completion of the E-diary took approximately 3 min per day. Once a month, up to eight additional questions were asked regarding the type and dose of acute and prophylactic (specific) headache medication used, menstrual cycle regularity and (post)menopausal status. If an E-diary was not completed at 6.00 pm, an alert with the same link was sent by text message as a reminder. No adjustments could be made after completion of an E-diary. When E-diaries were not completed, they were time-locked after 48 h. The E-diary could be filled in by mobile phone (mobile phone E-diary).
An automatic algorithm calculated whether each day was a headache day. A headache day was defined as a day with a headache lasting for at least 1 h and/or for which acute (pain or headache) medication (analgesics or triptans) was used. If a headache was present, the algorithm verified diagnostic criteria for migraine according to the ICHD-3 criteria. Therefore, the registration of migraine days could be used as indication for a migraine diagnosis. The default algorithm in the E-diary calculated migraine days based on a headache duration criterion of at least 4 h if no migraine-specific acute treatment had been taken. Days on which a triptan was used and/or days with aura symptomatology lasting 5–60 min were also interpreted as migraine days (Supplementary information). By definition, each migraine day was also considered a headache day. Headache days not fulfilling the criteria of migraine days were labelled as non-migrainous headache days. Days with aura symptomatology lasting 5–60 min were additionally labelled as aura days. Efficacy of triptans was determined by comparing pre-dose headache intensity to 2 h post-dose headache intensity. Triptan intake was considered effective when a moderate or severe pre-dose headache reduced to mild or no pain 2 h post-dose.
Additionally, migraine days were determined based on a duration criterion of at least 30 min to enable comparison to the 4 h duration criterion.
Results regarding the efficacy of triptans, pain coping and general wellbeing will be presented in future publications.
Eventually, the total number of migraine days, headache days, aura days and days with acute (headache) medication use were calculated for the registered months. These total numbers were reported to physicians by presentation in the electronic patient records together with a visualised summary of registered E-diary data for each day; that is, detailed headache characteristics, associated symptoms, aura symptoms, intake of analgesics, intake of triptans, menstrual bleeding, and change in preventive medication. Once a week, a simplified visualised summary including headache symptoms, intake of acute medication and a general wellbeing score was reported to patients by email.
Mean numbers of monthly migraine days, non-migrainous headache days and days with acute medication use were calculated based on the total number of invited E-diary days. Therefore, missing days were considered headache-free. An E-diary month was set at 28 days.
Self-reported outcomes
Self-reported estimates on mean numbers of monthly migraine days, non-migrainous headache days and days with acute medication use were extracted from the extended E-migraine questionnaire. The corresponding questions asked for estimates per month when looking at the past 3 months. Outcomes were divided by 3 months when patients misunderstood the question and reported estimates > 31 days per month. Thereafter, estimates between 29 and 31 were converted to 28 days, as these outcomes were compared to diary-based results with a maximum of 28 days.
Data analysis and statistics
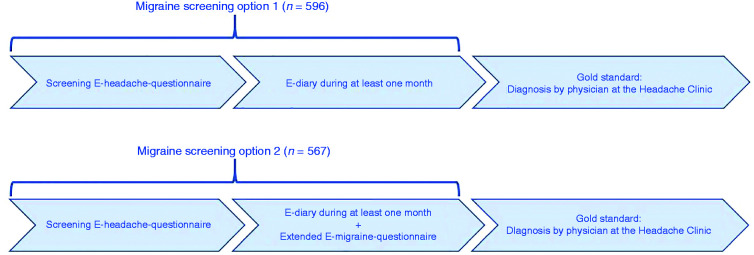
Descriptive statistics were used to present characteristics of the selected headache population. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated as measures of reliability of the two different migraine screening approaches. Firstly, we compared the derived diagnosis based on the combination of the screening E-headache questionnaire and the E-diary to the physicians’ diagnosis as gold standard (Figure 2, option 1). Secondly, we compared the derived diagnosis based on the combination of the screening E-headache questionnaire, the E-diary and the extended E-migraine questionnaire to the physicians’ diagnosis as gold standard (Figure 2, option 2). To fulfill the migraine screening criteria of option 2, both the E-diary and the extended E-migraine questionnaire had to indicate a migraine diagnosis. Similar screening approaches were used to assess the reliability of aura diagnoses.
Figure 2.
Flow chart of the two options for migraine screening approaches.
Mean differences and absolute mean differences were calculated to compare self-reported outcomes and diary-based outcomes (i.e. number of monthly migraine days, non-migrainous headache days, and days with acute medication use). The absolute difference was calculated by absolute (abs) (self-reported value – diary-based value) for each patient as self-reported estimates were both higher and lower compared to diary-based results, nullifying the mean difference. Linear regression models were fitted to investigate the relationship between self-reported outcomes and diary-based outcomes. In addition, Bland-Altman plots were constructed including a linear regression line to evaluate the agreement between self-reported outcomes and diary-based outcomes. No covariates were included because no variables were known or expected to be of influence on self-reported frequency estimates or diary-based frequency results. Lastly, the mean difference in number of monthly migraine days based on two different criteria of headache duration (at least 4 h vs. at least 30 min) was calculated for patients with episodic and chronic migraine. Chronic migraine was defined based on E-diary data by a mean of ≥ 15 headache days per month, from which ≥ 8 days had the features of a migrainous headache and/or triptan intake. Two-sided p-values < 0.05 were considered statistically significant. All analyses were performed in R version 3.6.1 (https://www.r-project.org/).
Results
Participants
Of approximately 1300 new patients who were referred to the Leiden Headache Clinic, a total of 829 screen-positives on the E-headache questionnaire were invited to complete the E-diary, of whom 596 started at least 1 month preceding their first consultation and adhered to the E-diary for a minimum of 80% of the total registration period. Of these 596 patients with appropriate E-diary registrations, 507 patients completed the extended E-migraine questionnaire about the same day as they started to complete E-diaries, 60 patients completed the extended E-migraine questionnaire after the start of E-diary registrations, and 29 did not complete the extended E-migraine questionnaire. At the Headache Clinic, 484 headache patients were diagnosed with migraine by a physician (Figure 1). Only 14 of the screen-negative patients started E-diary registrations after their first consultation, and therefore, appeared to be wrongly screened as non-migraine patient based on the screening E-headache questionnaire. Baseline characteristics of the included population are shown in Table 1. Main diagnoses made by physicians consisted mostly of migraine (81%, of which 39% experienced auras), followed by tension-type headache (8%) and cluster headache (3%). Of the 484 patients with migraine, 154 met the criteria of chronic migraine based on E-diary data. The mean number of completed E-diary days preceding first consultations at the Headache Clinic was 57.8, reflecting a mean E-diary adherence of 96%.
Table 1.
Baseline characteristics of included headache population.
| Headache population (n = 596) | |
|---|---|
| Age, years, mean (SD) | 44.8 (13.6) |
| Female sex, n (%) | 484 (81) |
| Main diagnosis by physician at headache clinic | |
| Migraine, n (%) | 484 (81) |
| Without aura, n (%) | 297 (61) |
| With aura, n (%) | 187 (39) |
| Tension-type headache, n (%) | 45 (8) |
| Cluster headache, n (%) | 20 (3) |
| Chronic daily persistent headache, n (%) | 7 (1) |
| Other headache or no conclusion, n (%) | 40 (7) |
| Number of invited E-diary days, mean (SD) | 60.1 (24.8) |
| Number of completed E-diary days, mean (SD) | 57.8 (23.1) |
Diagnostic aspects
The migraine screening approach consisting of the combination of the screening E-headache questionnaire and our E-diary (Figure 2, option 1) revealed a sensitivity of 98%, specificity of 17%, PPV of 84% and NPV of 68% for migraine (Table 2). The approach including the combination of the screening E-headache questionnaire, the E-diary and the extended E-migraine questionnaire (Figure 2, option 2) resulted in a sensitivity of 79%, specificity of 69%, PPV of 92% and NPV of 43% for migraine (Table 2). Similar screening approaches were used to assess reliability of aura diagnoses. Option 1 resulted in a sensitivity of 60%, specificity of 78%, PPV of 58% and NPV of 80%. Option 2 revealed a sensitivity of 39%, specificity of 98%, PPV of 84% and NPV of 83% (Table 2).
Table 2.
Cross tables regarding the validation of migraine (with and without aura) and aura symptoms separately, based on two screening approaches.
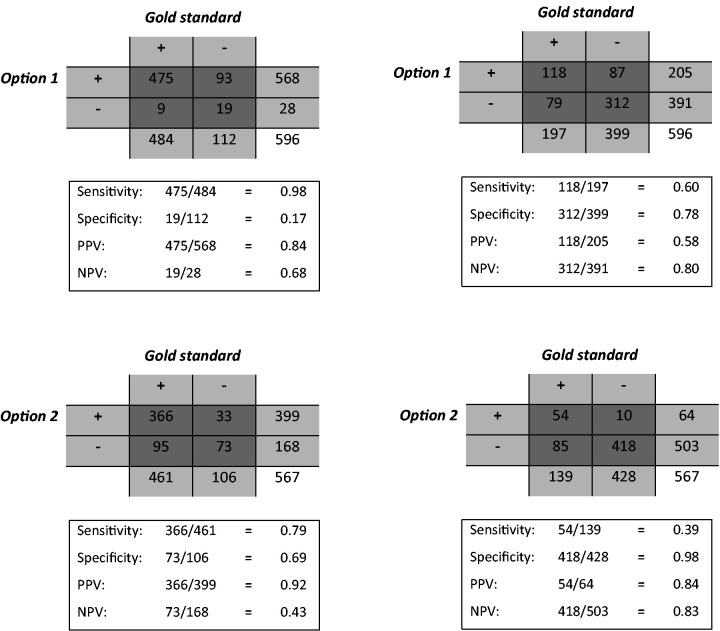
|
Gold standard: Diagnosis by physician at headache clinic. Option 1: Screening E-headache questionnaire + E-diary. Option 2: Screening E-headache questionnaire + E-diary + extended E-migraine questionnaire. PPV: Positive predictive value. NPV: Negative predictive value. For the first approach 596 headache patients were suitable to be included. The number of included patients for the second approach was 567 due to missing extended migraine questionnaires.
Frequency estimates
Crude data on mean self-reported and diary-based outcomes regarding monthly migraine days, non-migrainous headache days and days with acute medication use, including mean differences and absolute mean differences, are shown in Table 3. The absolute mean difference for monthly migraine days was 4.7 ± 5.0, meaning that self-estimated numbers of monthly migraine days were on average 4.7 days lower or higher compared to diary-based numbers. Similarly, self-estimated monthly non-migrainous headache days and days with acute medication use were on average 6.2 days and 4.3 days lower or higher compared to diary-based numbers.
Table 3.
Crude data on self-reported and diary-based outcomes.
| Self-reported | Diary-based | Mean difference | Absolute mean difference | |
|---|---|---|---|---|
| Migraine days/month (mean ± SD) | 9.9 ± 7.0 | 9.0 ± 5.8 | 0.9 ± 6.8 | 4.7 ± 5.0 |
| Non-migrainous headache days/month (mean ± SD) | 9.2 ± 9.3 | 5.2 ± 5.0 | 3.9 ± 8.2 | 6.2 ± 6.6 |
| Days with acute medication use/month (mean ± SD) | 9.4 ± 7.1 | 8.6 ± 5.5 | 0.8 ± 6.4 | 4.3 ± 4.8 |
Absolute difference was calculated by abs(self-reported value – diary-based value) for each patient as self-reported estimates were both higher and lower compared to diary-based outcomes, nullifying the mean difference.
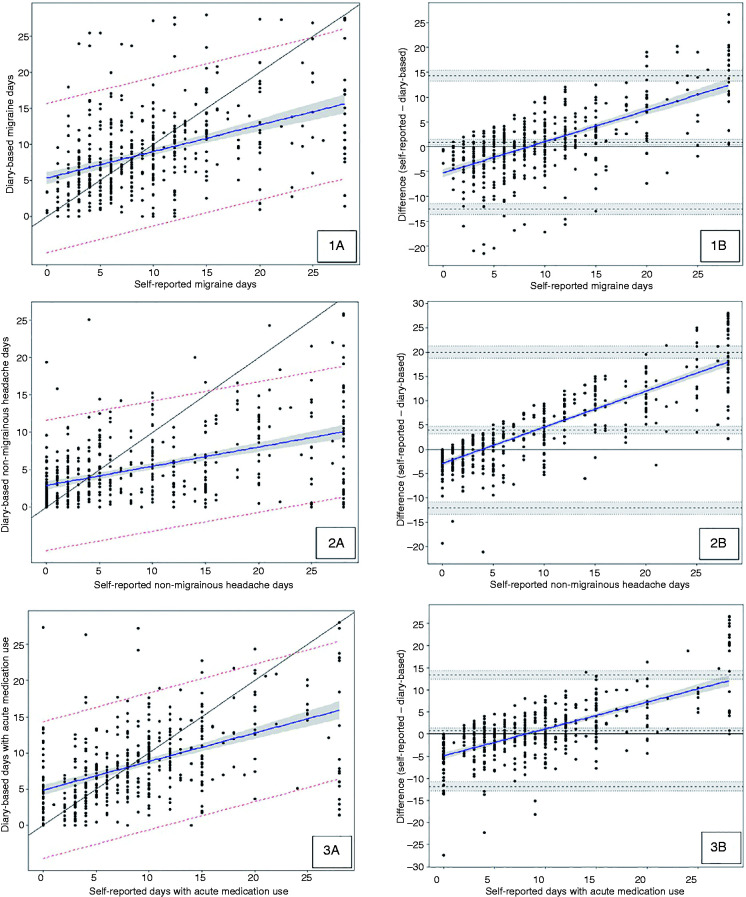
Linear regressions were calculated to assess the correlation between diary-based outcomes and self-reported outcomes. Scatter plots and Bland-Altman plots including linear regression lines for the three outcomes are presented in Figure 3. The majority of data points on the three scatter plots are located far away from the fitted regression lines, resulting in low correlation coefficients, which indicates a weak linear relationship between self-reported and diary-based outcomes. For monthly migraine days, a correlation coefficient of r = 0.44 (95% CI: 0.36–0.51, p < 0.001) was observed, indicating a low positive correlation. Similar results were found for monthly non-migrainous headache days (r = 0.47, 95% CI: 0.40–0.54, p < 0.001) and for monthly days with acute medication use (r = 0.50, 95% CI: 0.43–0.57, p < 0.001). The linear regression models showed wide 95% prediction intervals, implying that a future individual observation is predicted to fall within a large range of values. The three Bland-Altman plots showed wide ranges of agreement within which 95% of the differences between self-reported and diary-based measurements are located, indicating large discrepancy between the outcomes. When comparing linear regression lines to reference lines (x = y) and to equality lines (mean difference = 0), we carefully suggest that numbers of objectively diary-based monthly migraine days and days with acute medication use were underestimated when less than 8 days per month were reported and overestimated when more than 8 days per month were reported. The number of monthly non-migrainous headache days seemed to be overestimated when more than 4 days per month were reported.
Figure 3.
Scatter plots (1A, 2A, 3A) and Bland-Altman plots (1B, 2B, 3B) including regression lines for the comparison of self-reported outcomes and diary-based outcomes, respectively number of monthly migraine days (1), non-migrainous headache days (2) and days with acute medication use (3).
Scatter plots (1A, 2A, 3A): Blue line = linear regression; black line = reference (x = y); interval in grey = 95% confidence interval; interval between red dotted lines = 95% prediction interval. Bland-Altman plots (1B, 2B, 3B): Blue line = linear regression; black line = equality (mean difference = 0); black dotted lines = limits of agreement from −1.96sd to +1.96sd.
Migraine day duration criterion
The number of mean monthly migraine days calculated based on the 30 min criterion on headache duration was 0.5 days higher in patients with episodic migraine (95% CI: 0.3–0.6) and 0.7 days higher in patients with chronic migraine (95% CI: 0.4-0.9) compared to calculations based on the 4 h criterion.
Discussion
In this study we introduced our self-developed time-locked E-diary including an automated algorithm differentiating headache and migraine days based on detailed characteristics according to ICHD-3 criteria. A new era of telemedicine is emerging, in which a diagnosis has already been made prior to a consultation at the Headache Clinic. Making clinical decisions based on information from patients’ memory is not recommended since patients have been shown to unreliably recall migraine-related frequencies. The same high standard as for clinical trials should apply to clinical practice regarding reliability of data, as important decisions are made based on clinical outcome parameters.
We determined the reliability of two migraine screening approaches, including our E-diary, mainly focusing on sensitivity and specificity since these are considered characteristics of the tests and are less affected by the prevalence of the outcome. Both approaches were shown to be useful in screening for migraine. The first approach, consisting of the screening E-headache questionnaire combined with the E-diary is suitable when all true patients with migraine need to be identified and the additional identification of false positives is acceptable. The low specificity may partly be explained by patients who are convinced of having migraine but for whom an official diagnosis has never been made. Since these headache patients probably have more knowledge on symptomatology of migraine, they may be more likely to report these symptoms. The second approach, in which additionally another previously validated extended E-migraine questionnaire is included, appeared to be suitable when only patients with migraine needed to be identified and missing some patients with migraine was not problematic. Therefore, a specific approach could be chosen depending on the aim of the screening. Both screening approaches showed a high specificity in diagnosing auras, indicating that they are able to identify mainly true-positive patients. However, patients with auras could be missed due to lower sensitivity of the screening approaches. This shows that using E-tools for aura diagnoses will likely always remain a challenge and will never completely match up to a direct clinical interview, even though we showed examples of images of visual auras in our E-tools. Our findings apply to headache patients referred to a neurology practice. When the screening approaches are to be implemented in a general practitioner population, PPV may be lower and NPV higher. Although sensitivity and specificity are often considered test characteristics, they may vary in a different mix of patients (spectrum or case-mix bias).
In clinical practice, we would recommend using the second approach as a tool to screen for a migraine diagnosis because this will mainly identify true patients with migraine, which enables physicians to appropriately prepare for consultations. Missing some patients with migraine will not have major consequences since the correct diagnosis still will be made by the physician. When missing some patients with migraine could result in undiagnosed patients, it would be more appropriate to use the first approach, which prevents patients with migraine from missing out on an appropriate migraine treatment. When a migraine diagnosis has already been established by a neurologist or general practitioner, the E-diary may be used for clinical follow-up without completion of additional E-questionnaires. For research purposes, we would recommend to use the second approach to identify patients with migraine who could be included in migraine specific clinical trials. Our E-diary is different from a recently published E-diary study, which evaluated the accuracy of an automated tool for the classification of headache attacks. A substantial level of agreement (kappa 0.74) was found in the classification of 102 attacks as migraine (with or without aura) or tension-type headache by a neurologist with specialisation in headache and the algorithm (11). Their classification tool could not be used for diagnostic screening since only single attacks were classified. Additionally, the classification of auras was based on self-reported aura symptomatology as no characteristics and duration criterion were incorporated in the E-diary.
Most importantly, the need for E-diaries to obtain reliable information was emphasised in our study as patients did not reliably recall migraine-related frequency numbers. Monthly migraine days and days with acute medication use were tended to be underestimated in case of < 8 self-reported migraine days and overestimated in case of high frequency (> 8) self-reported migraine days. Another recently published study using E-diary data from a dietary intervention trial with 182 participants concluded that patients with migraine may underestimate headache frequency based on retrospective estimation (12), whereas our patients mainly overestimated non-migrainous headache days and underestimated migraine days up to 8 self-reported days.
Patients with migraine underestimating their acute medication intake might have major consequences for diagnosing and treating medication-overuse headache. The automatic calculation of monthly total numbers of days with use of analgesics, use of triptans, and use of a combination of both will enable us to perform research on medication-overuse (headache) in the future. Furthermore, with the upcoming new prophylactic treatments it may be that health-care insurance companies will require information on effectiveness to reimburse these prophylactic treatments. Therefore, reliable data are necessary for making the decision on whether to stop or continue medication. Nevertheless, treating physicians should continue to pay attention to the subjective assessment of a patient’s satisfaction during consultation. Information on general wellbeing and coping, as incorporated in our E-diary, could be helpful in shared decision making.
Missing E-diary days were considered headache-free, which is expected to have a negligible influence on numbers of monthly migraine days since mean E-diary adherence was 96% in the selected population. In addition, patients report that they are more likely to register days with headache than days without headache.
We also calculated monthly migraine days based on different duration criteria (30 min vs. 4 h). The similarity between the calculated monthly migraine days can be explained by the intake of triptans because most patients with migraine (n = 341) used triptans and all days with headache for which a triptan was taken were interpreted as migraine days independent of headache duration or other characteristics. However, the seemingly small differences may have scientific relevance as various criteria (e.g. 4 h, 2 h, 30 min) are currently used in outcome measures of randomised clinical trials. In these prophylactic treatment trials, differences in decrease of mean monthly migraine days between active drugs and placebo treatments are approximately between −1 and −4 days/month (13–17). Therefore, researchers should be aware of the consequence of a chosen criterion on headache duration when defining migraine days both in clinical trials and clinical practice when following patients and assess efficacy of therapies.
Our study has some limitations. Physicians were given insight into the registered E-diary data before diagnosing, which may have affected their diagnosis. However, this insight has never stopped them from making different diagnoses based on the interpretation of complete clinical interviews and physical and neurological examinations, and diagnoses were made in consultation with a headache specialist or by headache specialists themselves who were unaware of the E-diagnoses. In patients with a lifetime migraine with aura diagnosis, but with low frequency auras, a diary-based aura diagnosis could have been missed, resulting in an underestimation of the sensitivity of the screening approaches. Lastly, self-reported migraine-related frequency estimates preferably would have been collected at the end of the period with E-diary registrations, since it can be expected that the estimation would have been most accurate at that time point. In addition, the screening E-headache questionnaire asks about mean migraine-related frequency estimates per month when looking at the past 3 months, whereas the mean monthly E-diary estimates were calculated based on an average duration of approximately 2 months. However, in the earlier mentioned dietary intervention trial, concordance between the number of headache days based on an E-diary and retrospective recall questionnaires was assessed on a monthly basis during 4 months, which only showed a mild increase in concordance over time (12). This finding suggests that specifying a limited and more recent period does not significantly affect the degree of recall bias.
The recent experience in using our E-diary showed usefulness in clinical follow-up and evaluation of effectiveness of migraine treatments. Its use has become common practice at the Headache Clinic, to which physicians adjust their treatment strategies. In addition, it enables physicians and patients to prepare for consultations. In patients with migraine, its use may potentially improve understanding of their own disease as they are given insight into the course of symptoms over time. This is also why patients at our Headache Clinic appreciate the E-diary. The E-diary has been implemented in our investigated-initiated clinical trials and real-life-data collection of new treatments and offers opportunities for (ad hoc) research and telemedicine. During the recent COVID-19 outbreak, we were able to assess the effect of Dutch intelligent lockdown measures on migraine-related outcomes (18). More importantly, we were able to start and/or continue consultations with our patients by visualising E-questionnaires and E-diary data in the electronic patient records during video consultation. E-diaries added to E-questionnaires for headache using automated algorithms can thus be helpful in telemedicine. In the future, new research questions and/or clinical outcome measures can easily be implemented since we have developed a flexible E-diary. A new era begins for headache care.
Clinical implications
A new era of telemedicine is emerging, which increases the need for a similar high standard in clinical practice as in clinical trials regarding the reliability of data.
E-diaries need to include detailed headache characteristics to be able to differentiate between headache and migraine days.
The use of E-diaries in clinical practice should be encouraged, since patients with migraine do not reliably recall migraine-related frequencies.
Supplemental Material
Supplemental material, sj-pdf-1-cep-10.1177_03331024211010306 for E-diary use in clinical headache practice: A prospective observational study by Daphne S van Casteren, Iris E Verhagen, Irene de Boer Simone de Vries Lentsch, Rolf Fronczek, Erik W van Zwet, Antoinette MaassenVanDenBrink and Gisela M Terwindt in Cephalalgia
Footnotes
Declaration of conflicting interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: GMT reports consultancy support from Novartis, Lilly, Teva, and independent support from the Dutch Research Council (NWO), and the Dutch Heart & Brain Foundations. AMvdB reports consultancy or industry support from Novartis, Lilly and Teva, and independent support from the Dutch Research Council (NWO) and the Dutch Heart & Brain Foundations. DSvC and IEV report independent support from the Dutch Research Council and the Dutch Brain Foundation. IdB, SdVL, EvZ, and RF declare no conflict of interest.
Ethics or Institutional Review Board Approval: The study was approved by the medical ethics committee of the LUMC.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Irene de Boer https://orcid.org/0000-0002-7261-762X
Supplementary data availability: Data not published within the article will be shared by request from any qualified investigator.
References
- 1.Nappi G, Jensen R, Nappi RE, et al. Diaries and calendars for migraine. A review. Cephalalgia 2006; 26: 905–916. [DOI] [PubMed] [Google Scholar]
- 2.Bloem BR, Dorsey ER, Okun MS. The Coronavirus disease 2019 crisis as catalyst for telemedicine for chronic neurological disorders. JAMA Neurol 2020; 77: 927–928. [DOI] [PubMed] [Google Scholar]
- 3.Huygens MW, Swinkels IC, de Jong JD, et al. Self-monitoring of health data by patients with a chronic disease: Does disease controllability matter? BMC Fam Pract 2017; 18: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beck CA, Beran DB, Biglan KM, et al. National randomized controlled trial of virtual house calls for Parkinson disease. Neurology 2017; 89: 1152–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marmura MJ. Triggers, protectors, and predictors in episodic migraine. Curr Pain Headache Rep 2018; 22: 81. [DOI] [PubMed] [Google Scholar]
- 6.Verhagen IE, van Casteren DS, MaassenVanDenBrink A, et al. Menstrually-related migraine: A comparison between self-reported diagnosis and prospective headache diaries. Cephalalgia 2019; 39: 87–88. [Google Scholar]
- 7.Small CM, Manatunga AK, Marcus M. Validity of self-reported menstrual cycle length. Ann Epidemiol 2007; 17: 163–170. [DOI] [PubMed] [Google Scholar]
- 8.Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018; 38: 1–211. [DOI] [PubMed] [Google Scholar]
- 9.Launer LJ, Terwindt GM, Ferrari MD. The prevalence and characteristics of migraine in a population-based cohort: The GEM study. Neurology 1999; 53: 537–542. [DOI] [PubMed] [Google Scholar]
- 10.van Oosterhout WP, Weller CM, Stam AH, et al. Validation of the web-based LUMINA questionnaire for recruiting large cohorts of migraineurs. Cephalalgia 2011; 31: 1359–1367. [DOI] [PubMed] [Google Scholar]
- 11.Roesch A, Dahlem MA, Neeb L, et al. Validation of an algorithm for automated classification of migraine and tension-type headache attacks in an electronic headache diary. J Headache Pain 2020; 21: 75. doi: 10.1186/s10194-020-01139-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller VE, Faurot KR, Palssson OS, et al. Comparing prospective headache diary and retrospective four-week headache questionnaire over 20 weeks: Secondary data analysis from a randomized controlled trial. Cephalalgia 2020; 40: 1523–1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goadsby PJ, Reuter U, Hallström Y, et al. A controlled trial of erenumab for episodic migraine. N Engl J Med 2017; 377: 2123–2132. [DOI] [PubMed] [Google Scholar]
- 14.Dodick DW, Silberstein SD, Bigal ME, et al. Effect of fremanezumab compared with placebo for prevention of episodic migraine: A randomized clinical trial. JAMA 2018; 319: 1999–2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silberstein SD, Dodick DW, Bigal ME, et al. Fremanezumab for the preventive treatment of chronic migraine. N Engl J Med 2017; 377: 2113–2122. [DOI] [PubMed] [Google Scholar]
- 16.Ferrari MD, Diener HC, Ning X, et al. Fremanezumab versus placebo for migraine prevention in patients with documented failure to up to four migraine preventive medication classes (FOCUS): A randomised, double-blind, placebo-controlled, phase 3b trial. Lancet 2019; 394: 1030–1040. [DOI] [PubMed] [Google Scholar]
- 17.Stauffer VL, Dodick DW, Zhang Q, et al. Evaluation of galcanezumab for the prevention of episodic migraine: The EVOLVE-1 randomized clinical trial. JAMA Neurol 2018; 75: 1080–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Verhagen IE, van Casteren DS, de Vries Lentsch S. et al. Effect of lockdown during COVID-19 on migraine: A longitudinal cohort study. Cephalalgia 2021; 333102420981739. doi: 10.1177/0333102420981739. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-cep-10.1177_03331024211010306 for E-diary use in clinical headache practice: A prospective observational study by Daphne S van Casteren, Iris E Verhagen, Irene de Boer Simone de Vries Lentsch, Rolf Fronczek, Erik W van Zwet, Antoinette MaassenVanDenBrink and Gisela M Terwindt in Cephalalgia