Supplemental Digital Content is available in the text.
Keywords: coronavirus disease 2019, end-of-life, intensive care unit, palliative care, pandemic, patient-centered care
OBJECTIVES:
Patient- and family-centered end-of-life care can be difficult to achieve in light of visitation restrictions and infection-prevention measures. We evaluated how the 3 Wishes Program evolved to allow continued provision of compassionate end-of-life care for critically ill patients during the coronavirus disease 2019 pandemic.
DESIGN:
This is a prospective observational study where data were collected 1 year prior to the coronavirus disease 2019 pandemic and 1 year after (from March 1, 2019, to March 31, 2021). The number of deceased patients whose care involved the 3 Wishes Program, their characteristics, and wishes were compared between prepandemic and pandemic periods.
SETTING:
Six adult ICUs of a two-hospital health system in Los Angeles.
PATIENTS:
Deceased patients whose care involved the 3 Wishes Program.
INTERVENTIONS:
The 3 Wishes Program is a palliative care intervention in which individualized wishes are implemented for dying patients and their families.
MEASUREMENTS AND MAIN RESULTS:
During the study period, the end-of-life care for 523 patients involved the 3 Wishes Program; more patients received the 3 Wishes Program as part of their end-of-life care during the pandemic period than during the prepandemic study period (24.8 vs 17.6 patients/mo; p = 0.044). Patients who died during the pandemic compared with prepandemic were less likely to have family at the bedside and more likely to have postmortem wishes fulfilled for their families. Compared with the 736 wishes implemented during the prepandemic period, the 969 wishes completed during the pandemic were more likely to involve keepsakes. Wishes were most commonly implemented by bedside nurses, although the 3 Wishes Program project manager (not involved in the patient’s clinical care) was more likely to assist remotely during the pandemic (24.8% vs 12.1%; p < 0.001).
CONCLUSIONS:
Bedside innovations, programmatic adaptations, and institutional support made it possible for healthcare workers to continue the 3 Wishes Program and provide compassionate end-of-life care in the ICU during this pandemic.
The coronavirus disease 2019 (COVID-19) pandemic has drastically changed how patients receive medical care and how some patients die. The need for social distancing, personal protective equipment (PPE), and visitation restrictions (1) has resulted in hospitalizations characterized by isolation and separation of patients from their families. Many patients, with or without COVID-19, have died without family at the bedside (2–4). Dignified, patient- and family-centered end-of-life (EOL) care is needed more than ever in ICUs but can be difficult to achieve during a time when strict infection-prevention measures are necessary and resources are stretched thin (5–7). Although the goals of palliative care to relieve suffering by addressing the patients’ and families’ physical, social, psychologic, and spiritual needs (8, 9) remain fundamental, access to a palliative care specialist for EOL care can be limited during periods of high demand (6, 10). As such, the ability of frontline healthcare workers (HCWs) to provide “primary” palliative care becomes essential (6, 10, 11).
The 3 Wishes Program (3WP) is a palliative care intervention in which the clinical team elicits and fulfills final wishes for their dying patients and their families, after having conversations with their families to get to know them as individuals (12). Patients and families are eligible for the 3WP when the treating team determines that the probability of dying is greater than 95% or if there is a decision to withdraw or withhold advanced life support. HCWs ask how they might bring comfort to a dying patient and their family in the final hours or days of life. Wishes may be those of the patient, family, or clinicians, and are often simple, inexpensive, and easily achieved. Studies have shown that these small acts of kindness can ease family grief, enrich interpersonal connections, celebrate legacies, and enhance clinician satisfaction (12–16). Initiated and implemented predominantly by frontline HCWs, the 3WP is a form of primary palliative care that can be implemented without specialist consultation, modified to meet the needs of any group of patients and families (17). Our objective was to evaluate how the 3WP evolved to allow continued compassionate EOL care in several ICUs during the COVID-19 pandemic.
MATERIALS AND METHODS
Study Design and Setting
This prospective observational study was conducted in six adult ICUs (130 total ICU beds) of a two-hospital health system in Los Angeles (Ronald Reagan University of California, Los Angeles [UCLA] Medical Center and UCLA Santa Monica Medical Center). This study was approved by the health system Institutional Review Board (17-001422), reported in accordance with the Standards for Quality Improvement Reporting Excellence 2.0 guideline (18).
For this comparative study, data were collected 1 year prior to the COVID-19 pandemic and 1 year after the start of the pandemic (from March 1, 2019, to March 31, 2021). On March 11, 2020, the World Health Organization declared COVID-19 as a global pandemic (19). By March 31, 2021, there had been 1,158,657 cases of COVID-19 in Los Angeles County, CA (20). During the pandemic, visitation restrictions in this health system depended on community infection rate, ranging from a universal no-visitation policy to a policy allowing two healthy visitors per non-COVID patient, whereas patients with COVID-19 were not allowed any visitors unless they were dying (21). Nonessential personnel were prohibited from visiting the hospital. Patient interactions with spiritual care and social work became virtual only. We documented innovations contributing to 3WP sustainment and expansion in this period.
Method for Health Systemwide 3WP Expansion
The 3WP was initiated at this institution in the Medical ICU of one hospital on December 21, 2017, and sequentially introduced and expanded to other ICUs in the health system (two ICUs were added to the program per year). Prior to expansion to each ICU, the principal investigator (PI) gave a presentation that included the objectives of the program, examples of wishes, and prior research on the influence of the 3WP on families and clinicians.
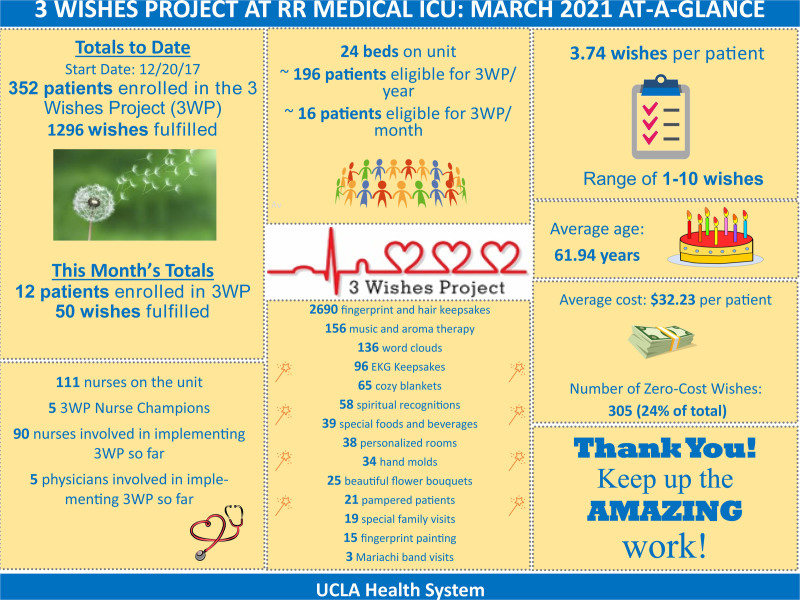
Each unit was then asked to identify at least two nurse champions to serve as “on-the-ground” leaders for the unit. An institutional project manager, who provides administrative support, was available to assist frontline HCWs with wish implementation. The 3WP project manager led training sessions using role-play and training videos (also online) (22) to familiarize unit champions with how to initiate and implement 3WP (23). Unit champions subsequently mentored their colleagues, to share implementation among all unit nurses. Presentations and training sessions were in-person prior to the pandemic, then virtual for units that started providing 3WP after March 2020. Prior to launching in each unit, the project manager supplied the unit with an inventory of commonly used supplies (i.e., fingerprint keepsakes, blankets, frames, and speakers) and 3WP brochures. Supplies and access to the 3WP manager were at no cost to the units and were funded by philanthropic and institutional supports to the 3WP. Unit-specific 3WP enrollments and accomplishments were shared via monthly “At-a-Glance” summary flyers (Fig. 1). Quarterly 3WP meetings were held with unit champions to discuss progress, new ideas, and concerns. Because the 3WP is led by frontline staff, the sharing of personal stories and quantitative data during presentations to the staff, hospital leadership, and other potential supporters was crucial in obtaining support.
Figure 1.
Example of “At-a-Glance” Sheet. These informational sheets are created monthly and individualized for each ICU (this example was for the Ronald Reagan Medical ICU for the month of March 2021). It displays the number of 3 Wishes Program (3WP) patients, wishes achieved, and approximate costs per patient. ECG = electrocardiogram.
The majority of wishes were elicited in-person but those for patients isolated with COVID were over the phone. Wishes were documented and characterized; Characteristics (including Acute Physiology and Chronic Health Evaluation II score, use of life-sustaining treatments, and COVID-19 status) of the dying patients who participated were abstracted from the electronic medical record.
Statistical Analysis
The number of deaths in each ICU per month during the study period was obtained from the institution’s Information Services and Solutions. The monthly number and proportion of deceased patients who received care involving the 3WP was calculated and compared between prepandemic (from March 1, 2019, to March 11, 2020) and pandemic (from March 11, 2020, to March 31, 2021) periods. Characteristics of patients and wishes were expressed in three groups: 3WP patients during the prepandemic period, 3WP patients without COVID-19 during the pandemic, and 3WP patients with COVID-19 during the pandemic. Data are presented using means (standard deviations) or medians (interquartile ranges). Bivariate comparisons between prepandemic and pandemic patient groups were performed using χ2 tests and t test, as appropriate. Analyses were performed using the STATA software, Version 14 (StataCorp, College Station, TX).
RESULTS
Sustainability and Growth During the Pandemic
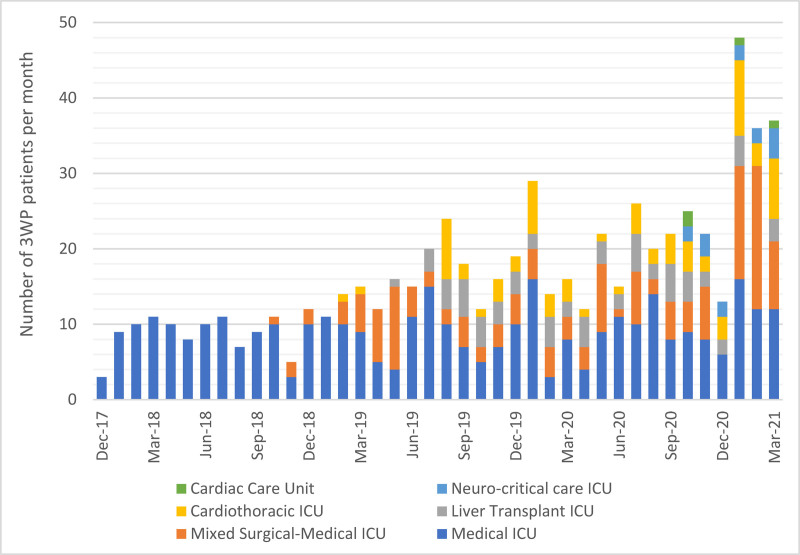
During the 25-month study period, there were 523 patients/families who received the 3WP as part of their EOL care. The number of patients whose EOL incorporated the 3WP increased over time as the 3WP was expanded to all six adult ICUs (medical ICU, neurocritical care unit, cardiac care unit, cardiothoracic ICU, liver transplant ICU, and an academic community hospital mixed-use ICU) by the end of the study period (Fig. 2). The neurocritical care unit and cardiac care unit implemented the program after the pandemic started. There were more patients who received the 3WP as part of their EOL care during the pandemic period than during the prepandemic study period (24.8 vs 17.6 patients per month; p = 0.044), aligned with a significantly higher proportion of patients who had the 3WP incorporated into their care in the pandemic period (47.8% vs 36.2%; p = 0.020).
Figure 2.
3 Wishes Program (3WP) growth over time. Number of patients, by ICU, whose end-of-life care incorporated the 3WP since initiation. The 3WP started in the medical ICU of Ronald Reagan University of California, Los Angeles Medical Center in December 2017 and was sequentially expanded to all six ICUs in the health system.
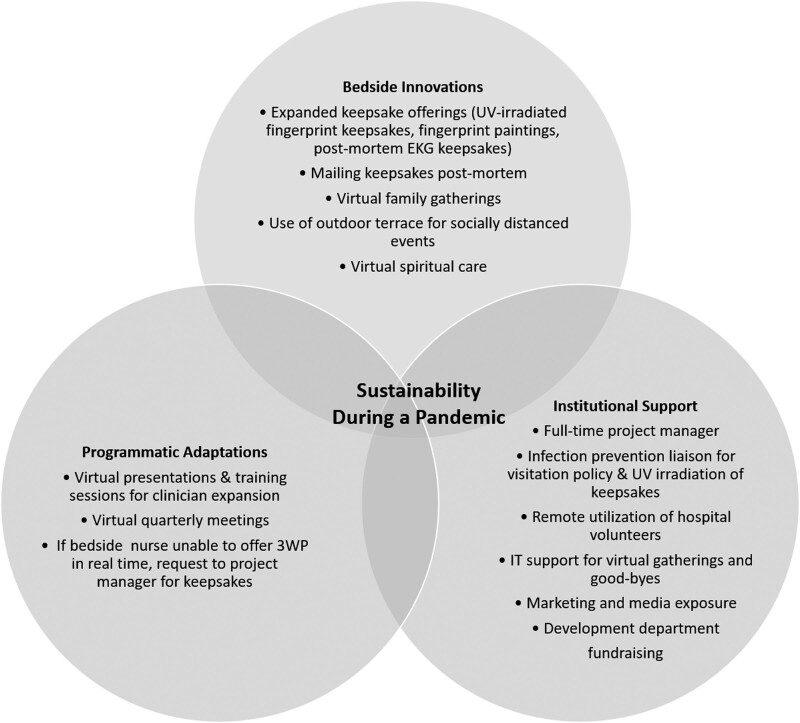
Various bedside innovations, programmatic adaptations, and institutional support enabled the 3WP at this institution to grow despite the restrictions and limitations imposed by the pandemic (Fig. 3). HCWs facilitated virtual spiritual care, social work visits, and family gatherings and farewells via hospital-provided iPads with HIPAA-compliant video-conferencing platforms. With infection prevention and institutional agreement, an EOL visitation policy was created to allow the use of compassionate PPE for one healthy family member to visit a patient dying from COVID-19. For dying patients who did not have COVID-19, an adjacent outdoor terrace was used to host a few small socially distanced gatherings (i.e., a wedding, Mariachi band performance) with departmental approval and following public health policies.
Figure 3.
3 Wishes Program (3WP) sustainability. Bedside innovations, programmatic adaptations, and institutional support allowed the 3WP to be sustained during the pandemic. ECG = electrocardiogram, UV = ultraviolet.
To provide families infection-free fingerprint keepsakes of patients who died of COVID-19, the 3WP team and infection prevention team adapted the hospital’s protocol for Ultraviolet Germicidal Irradiating of N95 masks and created a similar protocol for keepsakes (eSupplement 1, http://links.lww.com/CCX/A816). During the pandemic, HCWs were encouraged to contact the project manager working remotely to assist with the offering of electrocardiogram (ECG) keepsakes to families who were unable to be at the bedside of their dying loved ones, which can be created at any time using remote electronic medical record access. Hospital volunteers (not clinically trained) who were barred from the hospital during the pandemic connected with the 3WP team and developed a creative way to contribute remotely. Three volunteer artists transformed fingerprints obtained by HCWs on blank white paper into one-of-kind personalized commemorative paintings for families (eSupplement 2, http://links.lww.com/CCX/A816). Obtaining family addresses and sending keepsakes via the mail were routine, at no cost to families.
Clinicians from the neurocritical care ICU and the cardiac care unit, who were previously not participating in the 3WP, were recruited via e-mail and trained with video conferencing. The institution’s media, marketing, and development departments helped the program stay visible through local 3WP website development (22), news media releases (24–26), and fundraising events. Quarterly 3WP meetings continued virtually and provided 3WP champions an opportunity to debrief, share creative ideas, and hear updates on patient and family engagement and program achievements.
3WP Patients
Of the 523 patients who received 3WP as part of their EOL care, 215 died during the prepandemic period and 308 died during the pandemic (106 [34.4%] of whom died with COVID-19) (Table 1). In bivariate comparisons with prepandemic patients, patients who died during the pandemic (whether with or without COVID-19) were not different in age, gender, spiritual belief, or length of stay. In bivariate comparisons with prepandemic 3WP patients, 3WP patients with COVID-19 were more likely to have respiratory failure (39.1% vs 84.0%; p < 0.001), require mechanical ventilation (75.4% vs 87.7%; p = 0.01), and die in hospital (98.1% vs 92.1%; p = 0.03). During the pandemic, family or friends were significantly less often at the bedside at the time of death (96.5% of patients during prepandemic period, 53.9% of patients without COVID-19 during the pandemic, and 25.0% of patients with COVID-19; p < 0.001). The 3WP was most commonly initiated by the bedside nurses for patients during the entire study period (75.7% overall). However, the 3WP was more frequently initiated by a 3WP team member (the PI or the project manager) for patients with COVID-19 than patients in the prepandemic period (27.4% vs 14.4%; p < 0.005). The neurocritical care ICU and the cardiac care unit that started during the pandemic cared for 25 patients (one of which had COVID-19); bivariate comparisons did not change when these were excluded.
TABLE 1.
Comparison of Patients Cared for With the 3 Wishes Program Before and During the Pandemic
| Patient Characteristics | Prepandemic | Pandemic | |
|---|---|---|---|
| Patients | Patients Without COVID-19 | Patients With COVID-19 | |
| Date of enrollment | March 1, 2019, to March 10, 2020 | March 10, 2020, to March 31, 2021 | March 10, 2020, to March 31, 2021 |
| Total number of 3WP patients, n | 215 | 202 | 106 |
| Mean age (sd), yr | 61.7 (16.2) | 62.2 (17.1) | 64.3 (16.0) |
| Women, n (%) | 109 (50.9) | 101 (50.0) | 43 (40.6) |
| Race/ethnicity, n (%) | |||
| White | 82 (38.1) | 85 (42.1) | 27 (25.5)a |
| Black | 25 (11.6) | 24 (11.9) | 6 (5.7) |
| Hispanic | 81 (38) | 61 (30) | 61 (57.6)a |
| Asian | 27 (12.6) | 28 (13.9) | 12 (11.3) |
| Other/unknown | 0 (0) | 3 (1.5) | 0 (0) |
| Spiritual belief | |||
| Christian: Catholic/Orthodox | 45 (20.9) | 58 (28.7) | 30 (28.3) |
| Christian: Protestant and other | 84 (39.1) | 64 (31.7) | 45 (42.5) |
| Jewish | 12 (5.6) | 17 (8.4) | 3 (2.8) |
| Muslim/Hindu/Buddhist/Other | 7 (3.8) | 8 (4) | 5 (7.2) |
| No religion indicated | 67 (31.2) | 55 (27.2) | 23 (21.7) |
| Mean Acute Physiology and Chronic Health Evaluation II score (sd) | 30.5 (8.7) | 31.6 (8.5) | 28.4 (9.1)a |
| Diagnostic category at time of ICU admission, n (%) | |||
| Respiratory | 84 (39.1) | 80 (39.6) | 89 (84.0)a |
| Cardiovascular | 61 (28.4) | 60 (29.7) | 11 (10.4)a |
| Sepsis | 34 (15.8) | 30 (14.5) | 4 (3.8)a |
| Gastrointestinal | 18 (8.4) | 16 (7.9) | 0 (0.0)a |
| Neurologic | 11 (5.1) | 14 (6.9) | 2 (1.9) |
| Other | 7 (3.3) | 2 (1.0) | 0 (0.0) |
| Used advanced life support | |||
| Mechanical ventilation, n (%) | 162 (75.4) | 154 (76.2) | 93 (87.7)a |
| Inotropes, n (%) | 162 (75.4) | 154 (76.2) | 93 (87.7)a |
| Hemodialysis, n (%) | 95 (44.2) | 98 (48.5) | 46 (43.9) |
| Length of stay, d, median (interquartile range) | 15 (5–26) | 10.5 (5–22) | 15 (10–25) |
| Died in the hospital, n (%) | 198 (92.1) | 193 (95.5) | 104 (98.1)a |
| Family/friend at bedside at time of death, n (%) | 191 (96.5) | 104 (53.9)a | 26 (25.0)a |
| 3WP Initiated by, n (%) | |||
| Bedside nurse | 163 (75.8) | 161 (79.7) | 72 (67.9) |
| ICU physician | 10 (4.7) | 14 (6.9) | 4 (3.8) |
| 3WP team (not part of clinical care) | 31 (14.4) | 18 (8.9) | 29 (27.4)a |
| Otherb | 9 (4.2) | 9 (4.5) | 1 (0.9) |
| Unknown | 2 (1.0) | 0 (0) | 0 (0) |
3WP = 3 Wishes Program, COVID-19 = coronavirus disease 2019.
ap < 0.05 when compared with patients who participated in the 3 Wishes Program during the prepandemic period.
bOther 3WP initiators included social workers, member of the palliative care team, or the family themselves.
Wish Characteristics
During the study period, there were 736 wishes completed prior to the pandemic and 969 wishes completed during the pandemic, of which 328 (33.8%) wishes were for patients with COVID-19 (Table 2). For all patients, prepandemic or pandemic, with or without COVID-19, keepsakes were the most frequently requested and implemented wishes provided to families. Keepsakes included fingerprint key chains, locks of hair, framed ECG mementos, and personalized fingerprint paintings. During the pandemic, there were significantly higher proportion of keepsakes (compared with other wish categories) (Table 2) provided to families of patients with (52.9% vs 35.5%; p < 0.001) and without COVID-19 (69.5% vs 35.5%; p < 0.001) than the prepandemic period. With only 25% of families at the bedside at the time of death (Table 1) and strict infection control measures, HCW infrequently humanized the environment for patients with COVID-19 compared with those prior to the pandemic (5.4% vs 24.6%; p < 0.001).
TABLE 2.
Comparison of Wish Characteristics Before and During the Pandemic, in patients with and without Coronavirus Disease 2019
| Wish Characteristics | Prepandemic | Pandemic | |
|---|---|---|---|
| Wishes | Wishes for Patients Without COVID-19 | Wishes for Patients With COVID-19 | |
| Total number of wishes | 736 | 571 | 295 |
| Mean number of wishes per patient | 3.4 | 2.8 | 2.8 |
| Wish category, n (%) | |||
| Keepsakes | 260 (35.5) | 302 (52.9)a | 205 (69.5)a |
| Humanizing the environment | 181 (24.6) | 115 (20.1) | 16 (5.4)a |
| Music | 90 (12.2) | 53 (9.3) | 13 (4.4)a |
| Connections | 24 (3.3) | 19 (3.3) | 25 (8.5)a |
| Word clouds | 47 (6.4) | 20 (3.5)a | 10 (3.4)a |
| Rituals and spiritual support | 39 (5.3) | 22 (3.9) | 11 (3.7) |
| Providing food and beverages | 24 (3.3) | 9 (1.6) | 2 (0.7)a |
| Humanizing the patient | 22 (3.0) | 7 (1.2)a | 1 (0.3)a |
| Preparations and final arrangements | 22 (3) | 10 (1.8) | 5 (1.7) |
| Family care | 20 (2.7) | 7 (1.2) | 2 (0.7)a |
| Miscellaneous | 7 (1) | 7 (1.2) | 6 (1.7) |
| Wish implemented by, n (%) | |||
| Bedside ICU nurse | 608 (82.6) | 497 (87.0)a | 210 (71.2)a |
| 3 wishes team (not involved with clinical care) | 89 (12.1) | 54 (9.5) | 73 (24.8)a |
| Family/friend | 43 (5.8) | 18 (3.2)a | 8 (2.7)a |
| Social work/spiritual care | 37 (5.0) | 32 (5.6) | 9 (3.1)a |
| ICU physician | 24 (3.3) | 13 (2.3) | 3 (1.0)a |
| Palliative care team | 6 (0.8) | 2 (0.4) | 0 (0) |
| Timing | |||
| Postmortem | 40 (5.4) | 98 (17.2)a | 134 (45.4)a |
| Cost | |||
| Per patient, mean (sd) | $29.73 (35) | $28.79 (35) | $31.54 (26) |
| Per wish, mean | $8.34 | $8.57 | $10.35a |
| Number of no-cost wishes | 245 (33.3) | 120 (18.7)a | 64 (19.5)a |
COVID-19 = coronavirus disease 2019.
ap < 0.05 when compared with patients who participated in the 3 Wishes Program during the prepandemic period.
Individual wishes were most commonly implemented by the bedside nurses for all patients; however, there was increased utilization of the 3WP project manager or the PI (when not involved in the patient’s clinical care) for wish implementation for patients with COVID-19 (24.8% vs 12.1%; p < 0.001). With visitation restrictions, families and friends were less involved with wish implementation after the pandemic started (3% vs 5.8%; p = 0.005), and wishes were more commonly provided postmortem (26.9% vs 5.4%; p < 0.001). Social workers, spiritual care providers, as well as palliative care consultants were less likely to implement wishes for patients with COVID-19 than for patients during the prepandemic period. The cost of incorporating the 3WP into EOL care per ICU patient was not significantly different during the pandemic; however, slightly fewer wishes were implemented per patient (3.6 wishes vs 3.2 wishes; p = 0.004). In addition, due to the cost of mailing keepsakes postmortem to families, the cost per wish was higher for patients with COVID-19 ($10.35 vs $8.34; p = 0.047).
DISCUSSION
In this evaluation, we show how innovations to compassionate EOL care allowed an existing program to be sustained and actually grow during the pandemic. Because the 3WP was an established program at the institution, the pandemic was a natural experiment in which we observed how the program changed in terms of the patients cared for, HCW engagement, and institutional support. Addressing the need for compassionate EOL care during the pandemic (11, 27–30), this structured evaluation demonstrates with empirical data how an existing EOL care program can be maintained and expanded to meet the needs of dying patients in the ICU—with and without COVID-19.
During the pandemic, the program adapted to align with infection prevention guidelines. As families were routinely disallowed at the bedside, conversations to learn what is meaningful for the patients during their final moments were facilitated via telephone and video conferencing. Wishes that would often involve family participation, such as humanizing the environment, creating word clouds, or providing family care, were less frequently implemented during the pandemic. Keepsakes that have been shown in a multicenter study to be extremely valuable to bereaved families (16) were more frequently provided. During the pandemic, keepsakes were not only treasured mementos but helped to demonstrate to families that the patient was not abandoned by the clinical team during final moments. HCWs were also encouraged to reach out to the 3WP project manager to request the creation and mailing of ECG keepsakes if they could not offer these to families in-person or real time, due to either limited visitation or HCW workload during surges.
Many of these adaptations created during the pandemic will be continued after it ends. Virtual family visits with chaplains and social workers will be offered to ensure their accessibility and sustain connections. We will also pursue volunteer engagement, recognizing unique unrecognized skillsets (i.e., painting). The wider range of keepsakes created during the pandemic will remain available. Regardless of the status of the pandemic, our team meetings will be a hybrid of in-person and online to facilitate broad participation.
Institutional support in sustaining and expanding the 3WP program during the pandemic was key. UV irradiation of fingerprints is possible not only because the health system had a mechanism in place for the UV irradiation of N95 masks but also because the health system acknowledged the value of the 3WP to dying patients and their families (13–17, 31–34). Hospital volunteers, who were no longer allowed to physically come into the hospital, were given the opportunity to assist with the 3WP remotely. Institutional approval was granted for small socially distanced events on the outdoor terrace. Throughout the pandemic, the hospital-funded project manager was essential in creating monthly At-a-Glance flyers, organizing quarterly meetings, and assisting with postmortem wishes, particularly the mailing of keepsakes to families of patients who died during the pandemic. Clinician familiarity with the 3WP, desire to provide compassionate care for families and patients, and increased institutional support together contributed to the increased program activities.
Palliative care has been increasingly recognized as an essential component of comprehensive care in the ICU (35–37), but several challenges prevent optimal integration (38, 39). Systemic approaches to EOL care are recommended, especially during the pandemic, to mitigate the emotional challenges of providing care to dying patients (27, 40–42). At this institution, the 3WP is an organizational approach that is embedded into frontline HCW’s EOL care practice. Although the assistance of a project manager was helpful at this institution, the 3WP remains an example of primary palliative care—that is, palliative care that is readily provided by frontline bedside HCWs, rather than specialized palliative care consultants. Our HCWs were able to recognize and support our dying patients and their families’ social, psychologic, and spiritual needs, which often involved mobilizing additional resources (i.e., facilitating virtual meetings) and accessing supplies to create meaningful keepsakes for families who were unable to visit their loved ones.
Limitations of this study include it being a single-center experience and at an institution where the 3WP is already an established initiative; the “initiation” of such a program during a pandemic may be more challenging. Not all centers will have the administrative support of a project manager. However, we demonstrated that with institutional support, the 3WP can be sustained and expanded even during a pandemic to provide compassionate EOL care. We were unable to abstract and thus evaluate the effect of hospital census and the need for transfers on pandemic EOL care. Because prior studies have demonstrated many positive influences of the 3WP (13–15), we did not evaluate its effect on families during this study period, acknowledging the possibility that the 3WP was particularly valuable due to the tragic circumstances of the pandemic. The ability to provide compassionate care can help alleviate HCWs’ distress and enhance interpersonal connections during these unprecedented times (41, 43, 44) although this was not measured in this study. Although changes noted over time may plausibly reflect program maturation, baseline data allowed comparisons with prepandemic circumstances, which is rare in studies of EOL interventions during the pandemic.
CONCLUSIONS
In this evaluation, we outlined how a primary palliative care program continued and expanded during the COVID-19 pandemic. Visitation limitations and infection-prevention measures resulted in fewer families at the bedside of dying patients, shifting the profile of terminal wishes and changing how wishes were elicited and implemented. Creative adaptations to the 3WP allowed the preservation of humanistic, compassionate EOL care in this large academic institution.
ACKNOWLEDGMENTS
We thank for the privilege of supporting patients and their families during this difficult time. We thank University of California, Los Angeles (UCLA) CEO Johnese Spisso and the UCLA Board of Advisors for their support of the program. We also thank our funders, including the Perlman Family Foundation, the Wirtschafter Family Foundation, VITAS Healthcare, and Cam and Peter Starrett. We also thank Ellen Haddigan and Lauren Davis (UCLA Development) and Simi Singer (UCLA Media) for their endless advocacy for the program.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Supported, in part, by philanthropic donations from the Perlman Family Foundation, the Wirtschafter Family Foundation, VITAS Healthcare, and Cam and Peter Starrett.
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis. 2020; 20:631–633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moore B. Dying during Covid-19. Hastings Cent Rep. 2020; 50:13–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson-Shaw LK, Zar FA. COVID-19, moral conflict, distress, and dying alone. J Bioeth Inq. 2020; 17:777–782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Selman LE, Chamberlain C, Sowden R, et al. Sadness, despair and anger when a patient dies alone from COVID-19: A thematic content analysis of Twitter data from bereaved family members and friends. Palliat Med. 2021; 35:1267–1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chochinov HM, Bolton J, Sareen J. Death, dying, and dignity in the time of the COVID-19 pandemic. J Palliat Med. 2020; 23:1294–1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Radbruch L, Knaul FM, de Lima L, et al. The key role of palliative care in response to the COVID-19 tsunami of suffering. Lancet. 2020; 395:1467–1469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hart JL, Turnbull AE, Oppenheim IM, et al. Family-centered care during the COVID-19 era. J Pain Symptom Manage. 2020; 60:e93–e97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loscalzo MJ. Palliative care: An historical perspective. Hematology Am Soc Hematol Educ Program. 2008; 2008:465. [DOI] [PubMed] [Google Scholar]
- 9.Clark D. From margins to centre: A review of the history of palliative care in cancer. Lancet Oncol. 2007; 8:430–438 [DOI] [PubMed] [Google Scholar]
- 10.Davies A, Hayes J. Palliative care in the context of a pandemic: Similar but different. Clin Med (Lond). 2020; 20:274–277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sese D, Makhoul A, Hoeksema L, et al. The role of palliative care in COVID-19. Cleve Clin J Med. 2020. May 29. [online ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Cook D, Swinton M, Toledo F, et al. Personalizing death in the intensive care unit: The 3 Wishes Project: A mixed-methods study. Ann Intern Med. 2015; 163:271–279 [DOI] [PubMed] [Google Scholar]
- 13.Vanstone M, Neville TH, Clarke FJ, et al. Compassionate end-of-life care: Mixed-methods multisite evaluation of the 3 Wishes Project. Ann Intern Med. 2020; 172:1–11 [DOI] [PubMed] [Google Scholar]
- 14.Neville TH, Agarwal N, Swinton M, et al. Improving end-of-life care in the intensive care unit: Clinicians’ experiences with the 3 Wishes Project. J Palliat Med. 2019; 22:1561–1567 [DOI] [PubMed] [Google Scholar]
- 15.Vanstone M, Sadik M, Smith O, et al. Building organizational compassion among teams delivering end-of-life care in the intensive care unit: The 3 Wishes Project. Palliat Med. 2020; 34:1263–1273 [DOI] [PubMed] [Google Scholar]
- 16.Neville TH, Clarke F, Takaoka A, et al. Keepsakes at the end of life. J Pain Symptom Manage. 2020; 60:941–947 [DOI] [PubMed] [Google Scholar]
- 17.Neville TH. COVID-19: A time for creative compassion. J Palliat Med. 2020; 23:990–991 [DOI] [PubMed] [Google Scholar]
- 18.Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016; 25:986–992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020; 91:157–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.LA County Daily COVID-19 Data. County of Los Angeles, Public Health. Available at: http://dashboard.publichealth.lacounty.gov/covid19_surveillance_dashboard/. Accessed May 16, 2021
- 21.UCLA Health. COVID-19 Visitor Guidelines. Available at: https://www.uclahealth.org/covid-19-visitor-restrictions. Accessed May 16, 2021
- 22.UCLA Health. 3 Wishes Program. Available at: https://www.uclahealth.org/3wishes/videos-resources. Accessed May 16, 2021
- 23.Bear D, Phung P, Karlin D, et al. How to strategically and successfully expand a palliative care initiative hospital-wide. J Pain Sympt Manage. 2020; 59:525–526 [Google Scholar]
- 24.CBS. People making a difference. In: UCLA Health Program Aims to Make Final Moments Easier for Patients and Family — A Wish at a Time. Los Angeles, CBS News, 2020 [Google Scholar]
- 25.Univision News. ‘3 Wishes Project’ aims to meet demands of dying Covid-19 patients. 2020. Available at: https://twitter.com/UnivisionNews/status/1278108554780651522
- 26.Aleccia J. UCLA end-of-life program adapts during pandemic to help dying patients and their families. Los Angeles Times. 2020. Available at: https://www.latimes.com/california/story/2020-06-29/ucla-program-adapts-coronavirus-helps-dying-patients-families. Accessed June 29, 2020
- 27.Selman LE, Chao D, Sowden R, et al. Bereavement support on the frontline of COVID-19: Recommendations for hospital clinicians. J Pain Symptom Manage. 2020; 60:e81–e86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moore KJ, Sampson EL, Kupeli N, et al. Supporting families in end-of-life care and bereavement in the COVID-19 era. Int Psychogeriatr. 2020; 32:1245–1248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fadul N, Elsayem AF, Bruera E. Integration of palliative care into COVID-19 pandemic planning. BMJ Support Palliat Care. 2021; 11:40–44 [DOI] [PubMed] [Google Scholar]
- 30.deLima Thomas J, Leiter RE, Abrahm JL, et al. Development of a palliative care toolkit for the COVID-19 pandemic. J Pain Symptom Manage. 2020; 60:e22–e25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Takaoka A, Honarmand K, Vanstone M, et al. Organ donation at the end of life: Experiences from the 3 Wishes Project. J Intensive Care Med. 2021; 36:404–412 [DOI] [PubMed] [Google Scholar]
- 32.Takaoka A, Vanstone M, Neville TH, et al. Family and clinician experiences of sympathy cards in the 3 Wishes Project. Am J Crit Care. 2020; 29:422–428 [DOI] [PubMed] [Google Scholar]
- 33.Vanstone M, Neville TH, Swinton ME, et al. Expanding the 3 Wishes Project for compassionate end-of-life care: A qualitative evaluation of local adaptations. BMC Palliat Care. 2020; 19:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Swinton M, Vanstone M, Phung P, et al. Hospital leadership perspectives on the value of the 3 Wishes Project: A qualitative descriptive study. BMJ Leader. 2021; 5:1–6. [Google Scholar]
- 35.Aslakson RA, Curtis JR, Nelson JE. The changing role of palliative care in the ICU. Crit Care Med. 2014; 42:2418–2428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cook D, Rocker G. Dying with dignity in the intensive care unit. N Engl J Med. 2014; 370:2506–2514 [DOI] [PubMed] [Google Scholar]
- 37.Lanken PN, Terry PB, Delisser HM, et al. ; ATS End-of-Life Care Task Force. An official American Thoracic Society clinical policy statement: Palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008; 177:912–927 [DOI] [PubMed] [Google Scholar]
- 38.Nelson JE. Identifying and overcoming the barriers to high-quality palliative care in the intensive care unit. Crit Care Med. 2006; 34:S324–S331 [DOI] [PubMed] [Google Scholar]
- 39.Fassier T, Lautrette A, Ciroldi M, et al. Care at the end of life in critically ill patients: The European perspective. Curr Opin Crit Care. 2005; 11:616–623 [DOI] [PubMed] [Google Scholar]
- 40.Morris SE, Moment A, Thomas JD. Caring for bereaved family members during the COVID-19 pandemic: Before and after the death of a patient. J Pain Symptom Manage. 2020; 60:e70–e74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wei E, Segall J, Villanueva Y, et al. Coping with trauma, celebrating life: Reinventing patient and staff support during the COVID-19 pandemic. Health Aff (Millwood). 2020; 39:1597–1600 [DOI] [PubMed] [Google Scholar]
- 42.Onwuteaka-Philipsen BD, Pasman HRW, Korfage IJ, et al. Dying in times of the coronavirus: An online survey among healthcare professionals about end-of-life care for patients dying with and without COVID-19 (the CO-LIVE study). Palliat Med. 2021; 35:830–842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cook DJ, Takaoka A, Hoad N, et al. Clinician perspectives on caring for dying patients during the pandemic: A mixed-methods study. Ann Intern Med. 2021; 174:493–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kentish-Barnes N, Morin L, Cohen-Solal Z, et al. The lived experience of ICU clinicians during the coronavirus disease 2019 outbreak: A qualitative study. Crit Care Med. 2021; 49:e585–e597 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.