Abstract
Objectives
To compare the incidence and severity of invasive pneumococcal diseases (IPDs), pneumococcal pneumonia and all-cause pneumonia during the COVID-19 pandemic period with universal masking and social distancing with that of previous 5 years.
Design
Retrospective observational study on incidence of IPDs, pneumococcal pneumonia and all-cause pneumonia between January 2015–December 2019 and March 2020–March 2021. January–February 2020 was excluded from analysis as it was treated as a transitional period between normal time and pandemic.
Setting
Episode-based data by retrieval of hospitalisation records from the Hospital Authority’s territory-wide electronic medical record database in Hong Kong.
Participants
Hospitalised patients with IPD (n=742), pneumococcal pneumonia (n=2163) and all-cause pneumonia (including COVID-19 pneumonia, n=453 999) aged 18 years or above. Control diagnoses were included to assess confounding from health-seeking behaviours.
Primary and secondary outcomes
Primary outcome is the incidence of diseases between two periods. Secondary outcomes include disease severity surrogated by length of stay and mortality.
Results
Monthly average number of IPD, pneumococcal pneumonia and all-cause pneumonia hospitalisation significantly decreased by 88.9% (95% CI 79.8% to 98.0%, p<0.0005), 72.5% (95% CI 65.9% to 79.1%, p<0.0005) and 17.5% (95% CI 16.8% to 18.2%, p<0.0005), respectively. Changes in trend from January 2015–December 2019 to March 2020–March 2021 were −70% (95% CI −87% to −35%, p=0.0025), –43% (95% CI −59% to −19%, p=0.0014) and −11% (95% CI −13% to −10%, p<0.0005), respectively. Length of stay for IPD and pneumococcal pneumonia episodes were insignificantly different in the two periods. No reductions in hospitalisations for control diagnoses were observed.
Conclusions
Incidence of IPD, pneumococcal pneumonia and all-cause pneumonia decreased during the COVID-19 pandemic. This was observed with universal masking and social distancing. We postulated this is related to reduced transmission of respiratory viruses and bacteria.
Keywords: COVID-19, respiratory infections, thoracic medicine, epidemiology, public health
Strengths and limitations of this study.
A territory-wide study with near 100% practice of universal masking and wide practise of social distancing.
Other factors including temperature and air quality were also included in our analysis.
Disease severity of invasive pneumococcal disease, pneumococcal pneumonia and all-cause pneumonia was compared between the two periods.
Data from private sector (<10%) were not included in our study.
The causal relationship cannot be ascertained from this retrospective study.
Introduction
COVID-19 due to SARS-CoV-2 infections was first reported in late 2019.1 It became a global pandemic and was declared as a public health emergency of international concern on 30 January 2020 by the WHO.2 As of 22 September 2021, more than 229 million people were infected, causing more than 4.7 million deaths globally.
Pneumococcal disease is caused by Streptococcus pneumoniae infection, with at least 100 known serotypes of pneumococci.3 Pneumococcal disease can be roughly divided into non-invasive disease and invasive disease. Non-invasive disease includes sinusitis, acute otitis media and pneumonia. Invasive pneumococcal disease (IPD) is defined as isolation of S. pneumoniae from a normally sterile sites, including blood and cerebrospinal fluid.4 IPD is a notifiable disease in Hong Kong since 9 January 2015. Pneumococcal infection is a major cause of morbidity and mortality worldwide,5 with 1.6 million estimated deaths annually in 2005.6 Incidence of IPD and mortality of pneumococcal pneumonia is higher at extremes of age.7 8
The first pneumococcal conjugated vaccine (PCV), Prevnar 7 (PCV7), was introduced to the USA in 2000 and incorporated in Hong Kong Childhood Immunisation Programme for children under 2 years old since September 2009.9 10 In Hong Kong, PCV7 was replaced by the 10-valent and 13-valent PCVs (PCV10 and PCV13) in 2010 and 2011, respectively.11 12 PCV13 was effective in preventing vaccine-type pneumococcal pneumonia, bacteraemia and non-bacteraemic community-acquired pneumonia.13 Decline in incidences of all-cause pneumonia in children and the elderly was reported after implementation of PCV in childhood vaccination programme.14 15 The 23-valent polysaccharide vaccine (PPSV23) was effective in preventing pneumococcal pneumonia and reducing mortality from pneumococcal pneumonia in nursing home residents.16 In our locality, the elderly aged 65 years and above without high-risk conditions, namely immunodeficiency or chronic cardiac, pulmonary, liver or renal disease, or diabetes mellitus, were recommended to receive either a single dose of PCV13 or a single dose of PPSV23. The number of PPSV23 vaccine recipients aged 65 years or above increased from 35 000 in year 2015/2016 to 81 700 in 2019/2020, with approximately 46% of the population in the age group cumulatively vaccinated in 2020.17 Pneumonia is a common disease causing hospitalisation, accounting for 2.9% of all inpatient discharges and death in Hong Kong.18 It is the second leading cause of death with age-specific death rates increased markedly after age 65 years.17
Whether patients with COVID-19 are more susceptible to pneumococcal superinfection is still under debate. Superinfection of pneumococcal in patients with COVID-19 was reported.19 Yet, low frequency of bacterial coinfection in patients with early COVID-19 was also observed.20 21 There is limited evidence on the incidence and severity of IPD, pneumococcal pneumonia and all-cause pneumonia during COVID-19 pandemic, especially in areas where universal masking and social distancing were widely practised. Since January 2020, universal masking in public area was voluntarily performed by Hong Kong citizens against COVID-19. Cross-sectional telephone self-reported surveys by the Hong Kong Public Opinion Research Institute showed the percentages of those wearing masks were 74.5% on 20–23 January 2020 (n=1008), 97.6% on 5–20 February (n=10 405) and 98.9% on 4–19 March (n=15 739).22 On 23 July 2020, masking was mandatory in public areas upon the introduction of Prevention and Control of Disease (Wearing of Mask) Regulation (Cap. 599I). Social distancing measurements were voluntarily practised by the public and have been implemented by the government since 25 January 2020. These public health interventions were shown to associate with relatively low rate of COVID-19 and early termination of influenza season in Hong Kong.23 Our previous studies suggested universal masking and social distancing were associated with significant reduction in acute exacerbation of chronic obstructive pulmonary disease and asthma in Hong Kong.24 25 In the current study, we hypothesised that the aforementioned COVID-19-related public health interventions and reduction in respiratory virus activities would be associated with reduction in hospitalisation due to pneumococcal infections and pneumonia in general.
Materials and methods
A retrospective study assessing the numbers of IPD, pneumococcal pneumonia and all-cause pneumonia which required hospitalisation during the period of COVID-19 in Hong Kong, comparing with that in the preceding 5 years as a baseline, was conducted. The study period was 1 January 2015–31 March 2021 with exclusion of 1 January 2020–28 February 2020 from analysis, when public health practices such as mask wearing were not yet fully adopted.
Data source
Episode-based data were obtained by retrieval of hospitalisation records from the Hospital Authority’s territory-wide electronic medical record database, Clinical Data Analysis and Reporting System (CDARS), which provides 90% of inpatient hospital care service in Hong Kong.24 25
Diagnosis code of pneumococcal pneumonia (International Classification of Diseases-9 [ICD-9] code 481) was searched on CDARS. IPD is a notifiable disease since January 2015 with monthly number notified cases and age obtained from the Department of Health, Hong Kong Special Administrative Region (HKSAR). Monthly number of influenza virus detection was collected from a territory-wide laboratory surveillance for both inpatients and outpatients in both public and private medical sectors from the Centre for Health Protection (CHP), HKSAR.17
All-cause pneumonia including the following ICD-9 codes for viral, bacterial, tuberculous, fungal and unspecified pneumonia, pneumonia due to inhalation of food or vomitus and lung abscess were obtained from CDARS (ICD-9 codes 003.22, 055.1, 0.1160–1.1166, 112.4, 115, 117.3, 480, 481, 482, 483.1, 483.8, 485, 486, 487, 507.0, 513). Patients with COVID-19-associated pneumonia were included in the all-cause pneumonia dataset. The contribution of COVID-19 within all-cause pneumonia was queried using ICD codes for COVID-19 disease (ICD-9 codes 079.89, 480.8, 519.8). Demographics data (including sex, age), clinical data (including hospitalisation date, length of stay, episode death, date of death) were collected. The results including admission number of various diseases were available in the CHP website and the Hospital Authority Statistics Report.17 26
Inclusion/exclusion criteria
Patients (1) aged 18 years or above, and (2) hospitalised for the listed diseases (pneumococcal pneumonia, IPD and pneumonia) were included in the study.
Children aged 0–17 years old were excluded in this study. Duplicated record of a single patient with different diagnoses in the same hospital admission was removed.
Other diagnoses
The number of hospitalisations for other common medical and surgical conditions including acute kidney injury (AKI) (ICD-9 codes 580, 584), fracture hip (ICD-9 code 820) and peritonitis due to peritoneal dialysis (PD peritonitis) (ICD-9 code 996.68) was collected. These were included to evaluate the possibility of decrease in hospital attendance due to various reasons such as fear of COVID-19 infection in hospital. These diseases were selected as non-communicable diseases and have minimal interactions with environmental factors including mean ambient temperature and air pollution.
Other variables
Monthly mean ambient temperature was obtained from the Hong Kong Observatory.27 Air quality was measured by Air Quality Health Index (AQHI), which is calculated based on the cumulative health risk attributable to a 3-hour moving average concentration of ozone, nitrogen dioxide, sulphur dioxide and particulate matter.28 It was reported in a scale of 1–10 and 10+ and grouped into five health risk categories, namely low (1-3), moderate (4-6), high (7), very high (8-10) and serious (10+) with different precautionary actions advised. People with respiratory illness were advised to minimise their outdoor stay when AQHI was high to serious. The AQHI was reported hourly in 13 stations located in different areas of Hong Kong. The total number of hours with AQHI recorded as high to serious grades was expressed as percentage of the total number of hours collected in a month.
Statistical method
The total number of hospitalisations due to IPD, pneumococcal pneumonia and all-cause pneumonia was collected and analysed. Each disease was further divided into three different age groups, including 18–49 years, 50–64 years, and 65 years or above for analysis.
Analysis was done on the number of hospitalisations between January 2015–December 2019, the period prior to COVID-19 (period 1) and March 2020–March 2021 (period 3), while January–February 2020 (period 2) was treated as a transition period and excluded from the analysis. Wilcoxon rank-sum test was first used to analyse the statistical significance of the number of hospitalisations between period 1 and period 3. Generalised linear models were then applied for statistical inference of various types of responses. Log-linear model was used for studying the effect of the pandemic as intervention under segmented regression framework in terms of the change in trend (ie, an increase or decrease in the level of the segment) between period 1 (pre-intervention segment) and period 3 (post-intervention segment) on the monthly hospitalisation count. Regression coefficients of log-linear model can be interpreted as the effect due to pandemic by log-linear model.29 We assumed temporal dependence can be adjusted by the effect of the pandemic, including masking, social distancing and other behavioural changes, and climate-related variables including temperature and AQHI.
Generalised linear model was used for comparing the mortality rate of individuals between the two time periods.30 Hospitalisation length of stay (LOS) was described in days using median and SD. Statistical inference of the LOS in hospitalisation of individuals was done by Wilcoxon rank-sum test with OR and relative risks and CIs calculated.29
Monthly incidence rate for each disease was calculated using the total population followed by age group stratification (18–49 years, 50–64 years and ≥65 years) and expressed as number per 100 000 person-years. Age-specific population data were obtained from the Census and Statistics Department.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Results
Invasive pneumococcal disease
The total number of notified IPD episodes was 742 in the entire study, with 699 reported in period 1 and 17 reported in period 3. Pneumococcal serotypes for 684 of the 699 episodes in period 1, and 13 of the 17 episodes in period 3 were successfully determined. The proportions attributed to PCV13 serotypes were 66.5% (465 of 699) and 29.4% (5 of 17), respectively, for period 1 and period 3. Serotype 3 was the most common serotype in both periods, accounting for 41.3% (289 of 699) and 17.6% (3 of 17) in total, respectively. From period 1 to period 3, the monthly number of IPDs caused by PCV13 serotypes declined by 95.1% (95% CI 93.4% to 96.4%) while those for non-PCV13 serotypes declined by 83.0% (95% CI 78.8% to 86.5%), and those for PPSV23 serotypes declined by 94.1% (95% CI 92.3% to 95.5%). The small difference between decline in PCV13 and PPSV23 serotypes was mainly attributed to serotype 6A which was included in PCV13 but not in PPVS23.
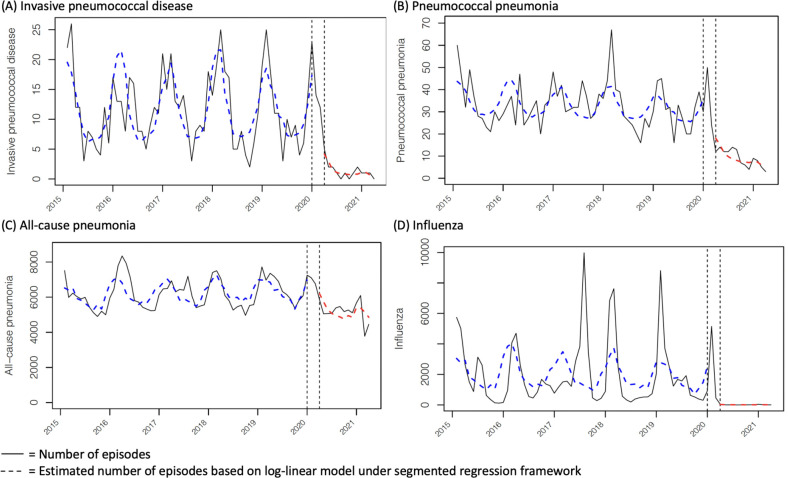
Monthly number of IPDs peaked in January–February each year except in 2016, with the peak in April (figure 1A and online supplemental figure S1). Monthly average number of notified IPD episodes was 11.7±6.2 in period 1, with significant decrease to 1±4.3 in period 3 (p<0.0005). By log-linear model segmented regression, relative risk of IPD in period 3 was 0.85 (95% CI 0.75 to 0.96, p=0.0089) (online supplemental table S1). Further analysis on the relative risk of different age groups showed significant decline in relative risk of IPD in those aged ≥65 years (0.78, 95% CI 0.61 to 0.99, p=0.041). Estimated change in trend in the mean number of cases from period 1 to period 3 was −70% (95% CI −87% to −35%, p=0.0025) (figure 1A, online supplemental table S1).
Figure 1.
Trend analysis of monthly numbers of invasive pneumococcal disease (IPD), pneumococcal pneumonia, all-cause pneumonia and influenza in Hong Kong, January 2015–March 2021. Numbers of IPD were those obtained through mandatory notification. Numbers of pneumococcal pneumonia and all-cause pneumonia were territory-wide hospitalisations by discharge diagnoses. Numbers of influenza viruses were those detected in respiratory specimens in a territory-wide laboratory surveillance. The two vertical lines delineated the time intervals from January 2015 to December 2019 (period 1, prior to COVID-19), January to February 2020 (period 2, excluded form analysis) and March 2020 to March 2021 (period 3, COVID-19 pandemic).
bmjopen-2021-055575supp001.pdf (358KB, pdf)
Incidence rates per 100 000 person-years were 2.2 in period 1 and 0.2 in period 3, with an interval reduction of 88.9% (95% CI 79.8% to 98.0%, p<0.0005). Incidence rate ratio between period 1 and period 3 was 0.11 (95% CI 0.07 to 0.18, p<0.0005) (table 1). IPD is most prevalent in age ≥65 years. The magnitude of reduction in incidence rate was similar across different age groups, ranging from 81.3% to 93.5% (p<0.0005 for all age groups) (table 1).
Table 1.
Incidence and number per 100 000 person-years of pneumococcal pneumonia, invasive pneumococcal disease (IPD) and pneumonia
| Disease* | All ages | 18–49 years | 50–64 years | ≥65 years | ||||
| No of episodes | Incidence rate per 100 000 person-years |
No of episodes | Incidence rate per 100 000 person-years |
No of episodes | Incidence rate per 100 000 person-years |
No of cases | Incidence rate per 100 000 person-years |
|
| IPD | ||||||||
| Period 1 | 699 | 2.2 | 125 | 0.7 | 195 | 2.2 | 379 | 6.2 |
| Period 2 | 26 | 2.4 | 5 | 0.9 | 6 | 2.0 | 15 | 6.6 |
| Period 3 | 17 | 0.2 | 3 | 0.08 | 8 | 0.4 | 6 | 0.4 |
| % reduction† | 88.9% (79.8% to 98.0%)*** | 88.6% (66.8% to 110.4%)*** | 81.3% (62.1% to 100.4%)*** | 93.5% (82,2% to 104.8%)*** | ||||
| IRR‡ | 0.11 (0.07 to 0.18)*** | 0.11 (0.04 to 0.36)*** | 0.19 (0.09 to 0.38)*** | 0.07 (0.03 to 0.15)*** | ||||
| Pneumococcal pneumonia | ||||||||
| Period 1 | 1970 | 6.2 | 217 | 1.3 | 435 | 4.9 | 1318 | 21.7 |
| Period 2 | 74 | 6.9 | 11 | 2.0 | 14 | 4.7 | 49 | 32.4 |
| Period 3 | 119 | 1.7 | 8 | 0.2 | 24 | 1.2 | 87 | 5.9 |
| % reduction | 72.5% (65.9% to 79.1%)*** | 82.5% (64.5% to 100.5%)*** | 74.8% (61.0% to 88.6%)*** | 73.0% (65.2% to 80.8%)*** | ||||
| IRR‡ | 0.28 (0.23 to 0.33)*** | 0.18 (0.09 to 0.35)*** | 0.25 (0.17 to 0.38)*** | 0.27 (0.22 to 0.34)*** | ||||
| All-cause pneumonia | ||||||||
| Period 1 | 372 660 | 1169.7 | 19 502 | 115.3 | 38 360 | 432.4 | 314 798 | 5177.1 |
| Period 2 | 13 865 | 1288.2 | 843 | 153.6 | 1448 | 484.6 | 11 574 | 5062.3 |
| Period 3 | 67 474 | 964.5 | 2473 | 69.3 | 6181 | 318.3 | 58 820 | 3958.0 |
| % reduction | 17.5% (16.8% to 18.2%)*** | 39.9% (37.1% to 42.7%)*** | 26.4% (24.3% to 28.5%)*** | 23.5% (22.8% to 24.3%)*** | ||||
| IRR‡ | 0.83 (0.82 to 0.83)*** | 0.60 (0.58 to 0.63)*** | 0.74 (0.72 to 0.76)*** | 0.77 (0.76 to 0.77)*** | ||||
*P<0.05–0.01, **p<0.01–0.005, ***p<0.005.
*Period 1, January 2015–December 2019 (before COVID-19); period 2, January 2020–February 2020 (transition period); period 3, March 2020–March 2021 (post-COVID-19).
†Percentage reduction in period 3 relative to period 1 as the baseline.
‡IRR between period 1 and period 3.
IRR, incidence rate ratio.
The overall median LOS for IPD was 12 (IQR 16) days in period 1 and 12 (IQR 11) days in period 3 (table 2), with statistically insignificant difference (p=0.89). Statistically insignificant variations in LOS of different age groups were observed.
Table 2.
Median length of stay and mortality rate of pneumococcal pneumonia, invasive pneumococcal disease (IPD) and pneumonia in the periods
| Median length of stay; days (IQR) | Mortality rate; % (95% CI) | |||||||
| All ages | 18–49 years | 50–64 years | ≥65 years | All ages | 18–49 years | 50–64 years | ≥65 years | |
| IPD | ||||||||
| Period 1 | 12 (16) | 13 (19) | 13 (17) | 12 (13) | 12.1 (8.8 to 16.1) | 9.1 (3.4 to 18.7) | 8.4 (3.7 to 15.9) | 15.3 (10.3 to 21.4) |
| Period 3 | 12 (11) | 4 (3) | 16 (19) | 12 (6) | 6.3 (1.6 to 30.2) | 0.0 | 0.0 | 14.3 (3.6 to 57.9) |
| Pneumococcal pneumonia | ||||||||
| Period 1 | 9 (14) | 7 (14) | 9 (15)* | 10 (14) | 13.1 (11.7 to 14.8)* | 4.2 (1.9 to 7.7) | 7.5 (5.3 to 10.5)** | 16.3 (13.6 to 18.7) |
| Period 3 | 12 (17) | 7 (13) | 13 (20)* | 12 (16) | 22.7 (15.5 to 31.3)* | 0.0 | 29.2 (12.6 to 51.1)** | 23.0 (14.6 to 33.2) |
| All-cause pneumonia | ||||||||
| Period 1 | 6 (9)*** | 4 (6)*** | 6 (9)** | 6 (10) | 20.5 (20.4 to 20.6)*** | 5.3 (4.9 to 5.6)* | 13.0 (11.4 to 12.0)*** | 22.4 (22.2 to 22.4)*** |
| Period 3 | 6 (10)*** | 4 (8)*** | 6 (10)** | 6 (10) | 24.2 (24.9 to 25.6)*** | 6.8 (5.9 to 7.9)* | 16.1 (5.2 to 17.0)*** | 27.0 (26.6 to 27.3)*** |
*P<0.05–0.01, **p<0.01–0.005, ***p<0.005.
Pneumococcal pneumonia
In the entire study period, there were 2163 episodes of hospitalisation for pneumococcal pneumonia, with 1970 episodes in period 1 and 119 episodes in period 3 (table 1). Monthly number of pneumococcal pneumonia peaked in January–February each year except in 2016, with the peak in April (figure 1B and online supplemental figure S1). The average monthly hospitalisation was 32.8±9.9 episodes in period 1, with significant drop to 9.2±3.9 episodes in period 3 (p<0.0005). By log-linear model segmented regression, relative risk of pneumococcal pneumonia was 0.90 (95% CI 0.86 to 0.95, p<0.005) in period 3. Trend analysis revealed a change of −43% (95% CI −59% to −19%, p=0.0014, figure 1B, online supplemental table S1) from period 1 to period 3. Age group analysis showed similar change in trend for all age groups, with statistical significance in age ≥65 years (−41%, 95% CI −61% to −12%, p=0.010) from period 1 to period 3 (online supplemental table 1 and online supplemental figure 2).
Overall, the incidence rate of hospitalisation for pneumococcal pneumonia decreased significantly by 72.5% (95% CI 65.9% to 79.1%, p<0.0005), from 6.2 per 100 000 person-years in period 1 to 1.7 per 100 000 person-years in period 3. Incidence rate ratio between period 1 and period 3 was 0.28 (95% CI 0.23 to 0.33, p<0.0005) (table 1). Incidence rate per 100 000 person-years showed statistically significant reduction in all age groups, ranging from 73.0% to 82.5%.
Majority of the patients with pneumococcal pneumonia were treated with inpatient care. The total numbers of patients treated as outpatients and discharged from emergency department were 30 in period 1 and 0 in period 3.
The overall median LOS for pneumococcal pneumonia in period 1 and period 3 were 9 (IQR 14) days and 12 (IQR 17) days in all age groups (p=0.051) (table 2). Age group stratification showed insignificant changes in LOS in those aged 18–49 years (p=0.8051) and those aged ≥65 years (p=0.226). Increase in LOS from 9 (IQR 15) days to 13 (IQR 20) days was observed in age group 50–64 years, and was statistically significant (p=0.019). Mortality rates for all ages were 13.1% (95% CI 11.7% to 14.8%) in period 1 and 22.7% (95% CI 15.5% to 31.3%) in period 3 (p=0.0187). Mortality rate was only statistically significant in age group 50–64 years (p=0.0007) but not in age group 18–49 years (p=0.9917) and age group ≥65 years (p=0.246) (table 2).
All-cause pneumonia
In the entire study period, total hospitalisation episodes for all-cause pneumonia was 453 999, of which 372 660 episodes in period 1 and 67 474 episodes in period 3. Among the 67 474 patients in period 3, 331 were diagnosed with COVID-19 and pneumonia. Monthly number of all-cause pneumonia peaked in January–March each year (figure 1C and online supplemental figure S1). Mean monthly number of hospitalisations for all-cause pneumonia declined by 16.4% (95% CI 15.7% to 17.1%, p<0.0005) from 6211±845.0 episodes in period 1 to 5190.3±593.8 episodes in period 3 (p<0.0005) (figure 1C). Estimated change in trend in the mean number of cases in period 3 was −11% (95% CI −13% to −10%, p<0.0005). By log-linear model segmented regression, relative risk of all-cause pneumonia in period 3 compared with period 1 was 0.98 (95% CI 0.98 to 0.99, p<0.0005) (online supplemental table S1).
Overall, the incidence rate per 100 000 person-years was 1169.7 in period 1, with 17.5% (95% CI 16.8% to 18.2%, p<0.0005) reduction in period 3 to 964.5 per 100 000 person-years in period 3. Incidence rate ratio between period 1 and period 3 was 0.83 (95% CI 0.82 to 0.83, p<0.0005) (table 1). The incidence rate decreased in period 3 compared with period 1 in all age groups.
The overall median LOS for all-cause pneumonia episodes were 6 (IQR 9) days in period 1 and 6 (IQR 10) days in period 3 (p<0.005) (table 2). Different age groups showed decrease in LOS but were only statistically significant in age 18–49 years and 50–64 years. The mortality rate increased from 20.5% (95% CI 20.4% to 20.6%) in period 1 to 24.2% (95% CI 24.9% to 25.6%) in period 3 (p<0.005) for all-cause pneumonia. The increase in mortality rate was statistically significant in all age groups (table 2).
For subgroup of aspiration pneumonia, the total number of hospitalisations in the entire study period was 21 183, with 17 990 episodes in period 1 and 2684 episodes in period 3. Mean monthly numbers of aspiration pneumonia were 299.8±31.3 in period 1 and 206.5±30.5 in period 3 (p<0.0005).
COVID-19
In period 3, the total reported case of COVID-19 infection at age 18 years or above was 10 348.15 Among these patients, 331 were diagnosed with pneumonia. Majority of them were in the age group 65 years old or above (n=175), 58 of them were in age group 18–49 years, while 98 patients in age group 50–64 years. None of the patients were diagnosed with coinfection of COVID-19 and pneumococcal pneumonia.
Influenza
The total number of influenza A or B viruses detected from January 2015 to March 2021 in Hong Kong was 123 732. The monthly number of influenza detection decreased drastically by 99.5% (95% CI 99.4% to 99.5%, p<0.0005) from 1966±2179 in period 1 to 10±18 in period 3 (figure 1D and online supplemental figure S1). The monthly average numbers of respiratory specimens tested were 4313±1172 in period 1 and 3203±1868 in period 3.
By log-linear model segmented regression, relative risk of influenza was 0.92 (95% CI 0.88 to 0.95, p<0.0005). Estimated change in trend in the mean number of detection in period 3 was −99.0% (95% CI −99.3% to −98.7%, p<0.0005) of that in period 1 (figure 1D).
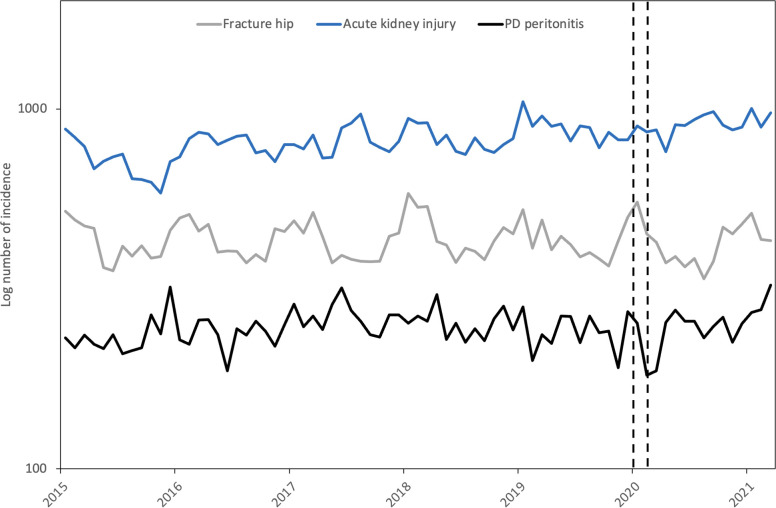
Other diagnosis: AKI, PD peritonitis and fracture hip
The monthly average numbers of hospitalisation episodes for AKI in period 1 and period 3 were 807.8±87.5 and 911.7±62.6, respectively (p<0.0005) (figure 2). The monthly average numbers of hospitalisation episodes for PD peritonitis were 246.7±27.7 in period 1 and 255.9±31.9 in period 3 (p=0.23). The monthly average numbers of hospitalisation episodes for fracture hip were 432.9±53.1 in period 1 and 417.3±51.6 in period 3 (p=0.37).
Figure 2.
Admission numbers of fracture hip, acute kidney injury and PD peritonitis. PD peritonitis, peritonitis due to peritoneal dialysis.
Discussion
Hong Kong is a city with a population of 7.5 million where universal masking and social distancing were widely practised during the COVID-19 pandemic period. This study showed a drastic decrease in numbers of hospitalisation for IPD and pneumococcal pneumonia and a lesser but still very significant decrease in all cause pneumonia after anti-COVID-19 measures in March 2020–March 2021.
During COVID-19 period, decrease in incidence of IPD was observed in Taiwan and Singapore.31 32 The decrease in IPD in Hong Kong was greater in magnitude compared with other countries.33 Our study added new information on the incidence and severity of IPD, pneumococcal pneumonia and all-cause pneumonia in terms of age stratification.
In our patients with COVID-19, there was no pneumococcal coinfection. This may partly be contributed by the infrequent investigation of pneumonia with pneumococcal urinary tests and PCR assays. In an Italian study of 469 patients with COVID-19, 9% was found to be positive for urinary pneumococcal antigen. However, the positive result had no impact on clinical outcome.34 In another study that investigated the respiratory specimens of patients with COVID-19 using PCR assays, 60% were found to be positive for S. pneumoniae but it was unable to distinguish between colonisation and infection.35
Introduction of the current PCVs has been highly successful in reducing the incidence of pneumococcal diseases worldwide.36 37 Vaccine efficacy of PCV13 against vaccine-type IPD in children aged ≤5 years was 86%–96%.38 In adults aged ≥65 years, the vaccine efficacy against vaccine-type IPD was reported as 75% and against vaccine-type community-acquired pneumonia were reported as 45.6% and 72.8%, respectively.13 39 In contrast, PPV23 only has vaccine efficacy of 24% against vaccine-type community-acquired pneumonia in those aged ≥65 years.40 In Hong Kong, a marked reduction in vaccine-type IPD was observed in children few years after implementation of PCV in 2009.10 12 However, the indirect effect on adult IPD was not evident. The annual number of adult IPD hospitalisations remains static in period 1 (figure 1A). Universal masking and social distancing measures in Hong Kong were shown to have an association with decrease in the incidence of SARS-CoV-241 42 and influenza43 during the COVID-19 pandemic. Our study showed 88.9% reduction in incidence of adult IPD. The drastic decrease in incidence of IPD included both vaccine and non-vaccine types and was comparable and greater than the reported figure after introduction of pneumococcal vaccines.13 37 IPD can lead to significant mortality and morbidity.44 Our study showed decrease in incidence and trend of IPD and were statistically significant. The decrease in mortality of IPD during the COVID-19 pandemic was statistically insignificant, which can be contributed by the relative small sample size.
Incidence of all-cause pneumonia showed a much lower magnitude of decrease with the lesser decrease observed in those aged ≥65 years (online supplemental figure S2C). In our study, patients with diagnosis of pneumonia during the hospital stay were included. On review of data, majority of patients with pneumonia in age group 65 years or above had other comorbidities including dementia, diabetes mellitus and malignancy included in the same admission. The prevalence of chronic disease is higher in the elderly. The population of Hong Kong has been seeing an ageing trend and the population of 65 years old or above was 1 114 600 in 2015, and increased to 1 371 800 in 2020. The incidence of chronic disease, for example, malignancy increased by 38.1% from 2008 to 2018.17 Patients with chronic diseases are at higher risk of acquiring infection including pneumonia. Moreover, chronic disease can be the cause leading to hospital admission with subsequent development of hospital-acquired pneumonia.
Pneumococcal pneumonia and IPD are debilitating diseases which have been shown to require long length of hospital stay and high hospital cost.45 46 The LOS in pneumococcal pneumonia was slightly increased from 17.7 to 19.5 days but was statistically insignificant. Looking into different age groups, only patients aged 50–64 years old showed statistically significant increase in LOS, while patients in age group 18–49 years old and 65 years old or above showed slight decrease. The severity of pneumococcal pneumonia was comparable in the two periods.
Health-seeking behaviour was also evaluated in our study. Admissions of non-communicable diseases revealed either statistically insignificant decrease in hospital attendance or statistically significant increase in hospital attendance. The incidence of AKI increased in our study from 807.8±87.5 in period 1 to 911.7±62.6 in period 3. Drug-induced AKI is an important cause in Asia.47 Possible explanation can be due to the health-seeking behaviour of patients with intake of over-the-counter medication for mild diseases prior to seeking help from the hospital. Yet, the exact cause of increase in incidence of AKI should be investigated. Our study covered more than 1-year time for COVID-19 pandemic with a relatively stable number of hospital attendances. Hence, the decrease in incidence of pneumococcal pneumonia, IPD and all-cause pneumonia cannot be explained by health-seeking behaviour alone.
Collateral damages were observed during the COVID-19 pandemic,48 49 some of which were contributed by the decrease in general medical services to concentrate healthcare resources for the care of patients with SARS-CoV-2 and the prevention of possible viral spread. However, due to the relatively small number of COVID-19 cases in Hong Kong, provision of acute medical services was minimally disrupted. In our study, the data on admissions for fractures, AKI and PD peritonitis showed no decrease during the COVID-19 pandemic. Hence, the observed decrease in hospital admissions for pneumococcal pneumonia, IPD and all-cause pneumonia should not be artefactual.
Limitations
This is a retrospective observational study and the direct effect of universal masking, social distancing (eg, closure of schools, bars and pubs) and other strategies on pneumococcal pneumonia, IPD and all-cause pneumonia cannot be ascertained. However, our study covered a period of more than 1 year when infection control-related behavioural changes were made throughout, with a consistent observation of decrease in hospitalisation for these diseases seen. Other factors, namely ambient temperature and AQHI, that might have possible effect on the hospitalisation numbers, were also included in our analysis. However, the individual effects of universal masking, social distancing and other strategies cannot be evaluated separately. It is modelled by the effect of the pandemic as a whole in our study.
Our study focused on hospital hospitalisation numbers in the Hospital Authority. For IPD, the incidence was obtained from Central of Health Protection, HKSAR, which included data from both public and private hospitals. The LOS and mortality data of IPD were retrieved from the database in Hospital Authority. Admissions to private hospital or those who received outpatient treatment for pneumococcal pneumonia and all-cause pneumonia were not included in our study. However, Hospital Authority is the largest healthcare provider in Hong Kong which provides 90% of inpatient services in Hong Kong.26 Data from Hospital Authority are representative of the general epidemiology of Hong Kong.
Conclusions
The incidence of pneumococcal pneumonia, IPD and all-cause pneumonia decreased during COVID-19 pandemic compared with the data in previous 5 years. This was observed with widespread practise of universal masking and social distancing. While causality cannot be shown from our data, it is likely that the decrease could be attributed to universal masking and social distancing, which would have reduced the transmission of bacteria and viruses and related bacterial superinfection.
Supplementary Material
Footnotes
Contributors: K-PFC and T-FM were involved in study concept and design; acquisition, analysis and interpretation of data; drafting the work and final approval of the manuscript. MS-MI was involved in critical revision of the manuscript for important intellectual content and final approval of the manuscript. P-LH was involved in study concept and design; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; study supervision and approval of the final version of the manuscript. P-LH is responsible for the overall content as guarantor. The guarantor accepts full responsibility for the finished work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: This work is partly funded by a grant from the Health and Medical Research Fund (reference number CID-HKU1-13), Food and Heatlh Bureau, the Government of Hong Kong Special Administrative Region.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (Reference Number UW-21-325).
References
- 1.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–42. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 2.WHO . World Health organization statement on the second meeting of the International health regulations (2005) emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV. Available: https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) [Accessed 10th May 2021].
- 3.Ganaie F, Saad JS, McGee L, et al. A New Pneumococcal Capsule Type, 10D, is the 100th Serotype and Has a Large cps Fragment from an Oral Streptococcus. mBio 2020;11:e00937–20. 10.1128/mBio.00937-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ludwig E, Bonanni P, Rohde G, et al. The remaining challenges of pneumococcal disease in adults. Eur Respir Rev 2012;21:57–65. 10.1183/09059180.00008911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drijkoningen JJC, Rohde GGU. Pneumococcal infection in adults: burden of disease. Clin Microbiol Infect 2014;20 Suppl 5:45–51. 10.1111/1469-0691.12461 [DOI] [PubMed] [Google Scholar]
- 6.World Health organization pneumococcal disease. Available: https://www.who.int/ith/diseases/pneumococcal/en/; [Accessed 07th June 2021].
- 7.Burgos J, Luján M, Larrosa MN, et al. The problem of early mortality in pneumococcal pneumonia: a study of risk factors. Eur Respir J 2015;46:561–4. 10.1183/09031936.00034415 [DOI] [PubMed] [Google Scholar]
- 8.Chi R-C, Jackson LA, Neuzil KM. Characteristics and outcomes of older adults with community-acquired pneumococcal bacteremia. J Am Geriatr Soc 2006;54:115–20. 10.1111/j.1532-5415.2005.00528.x [DOI] [PubMed] [Google Scholar]
- 9.Ho P-L, Chiu SS, Chow FKH, et al. Pediatric hospitalization for pneumococcal diseases preventable by 7-valent pneumococcal conjugate vaccine in Hong Kong. Vaccine 2007;25:6837–41. 10.1016/j.vaccine.2007.07.039 [DOI] [PubMed] [Google Scholar]
- 10.Ho P-L, Chiu SS, Ang I, et al. Serotypes and antimicrobial susceptibilities of invasive Streptococcus pneumoniae before and after introduction of 7-valent pneumococcal conjugate vaccine, Hong Kong, 1995-2009. Vaccine 2011;29:3270–5. 10.1016/j.vaccine.2011.02.025 [DOI] [PubMed] [Google Scholar]
- 11.Deloria Knoll M, Bennett JC, Garcia Quesada M, et al. Global landscape review of serotype-specific invasive pneumococcal disease surveillance among countries using PCV10/13: the pneumococcal serotype replacement and distribution estimation (PSERENADE) project. Microorganisms 2021;9:742. 10.3390/microorganisms9040742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ho P-L, Law PY-T, Chiu SS. Increase in incidence of invasive pneumococcal disease caused by serotype 3 in children eight years after the introduction of the pneumococcal conjugate vaccine in Hong Kong. Hum Vaccin Immunother 2019;15:455–8. 10.1080/21645515.2018.1526555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonten MJM, Huijts SM, Bolkenbaas M, et al. Polysaccharide conjugate vaccine against pneumococcal pneumonia in adults. N Engl J Med 2015;372:1114–25. 10.1056/NEJMoa1408544 [DOI] [PubMed] [Google Scholar]
- 14.López EL, Glatstein E, Ezcurra GC, et al. Rapid Decrease in Rates of Hospitalization Resulting From Invasive Pneumococcal Disease and Community-Acquired Pneumonia in Children Aged <60 Months After 13-Valent Pneumococcal Conjugate Vaccine Introduction in Argentina. J Pediatric Infect Dis Soc 2018;7:30–5. 10.1093/jpids/piw089 [DOI] [PubMed] [Google Scholar]
- 15.Nieto Guevara J, Daza C, Smith R. Decrease in hospitalizations for pneumonia in children under five years of age in an Indian reservation in Panama after the introduction of the Heptavalent pneumococcal conjugate vaccine (PCV7). Int J Pediatr 2013;2013:514578. 10.1155/2013/514578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maruyama T, Taguchi O, Niederman MS, et al. Efficacy of 23-valent pneumococcal vaccine in preventing pneumonia and improving survival in nursing home residents: double blind, randomised and placebo controlled trial. BMJ 2010;340:c1004. 10.1136/bmj.c1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centre for health protection, department of health, Hong Kong special administrative region. Available: https://www.chp.gov.hk/ [Accessed 05th May 2021].
- 18.Department of health public health information system (PHIS). Available: https://www.healthyhk.gov.hk/phisweb/en/chart_detail/26/ [Accessed 05th May 2021].
- 19.Cucchiari D, Peric s JM, Riera J. Hospital Clínic 4H team. pneumococcal superinfection in COVID-19 patients: a series of 5 cases. Med Clin 2020;155:502–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karami Z, Knoop BT, Dofferhoff ASM, et al. Few bacterial co-infections but frequent empiric antibiotic use in the early phase of hospitalized patients with COVID-19: results from a multicentre retrospective cohort study in the Netherlands. Infect Dis 2021;53:102–10. 10.1080/23744235.2020.1839672 [DOI] [PubMed] [Google Scholar]
- 21.Hughes S, Troise O, Donaldson H, et al. Bacterial and fungal coinfection among hospitalized patients with COVID-19: a retrospective cohort study in a UK secondary-care setting. Clin Microbiol Infect 2020;26:1395–9. 10.1016/j.cmi.2020.06.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Community health module research reports, Hong Kong public opinion research Institute. Available: https://www.pori.hk/research-reports [Accessed 10th April 2021].
- 23.Chan KH, Lee P-W, Chan CY, et al. Monitoring respiratory infections in covid-19 epidemics. BMJ 2020;369:m1628. 10.1136/bmj.m1628 [DOI] [PubMed] [Google Scholar]
- 24.Chan KPF, Ma TF, Kwok WC, et al. Significant reduction in hospital admissions for acute exacerbation of chronic obstructive pulmonary disease in Hong Kong during coronavirus disease 2019 pandemic. Respir Med 2020;171:106085. 10.1016/j.rmed.2020.106085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan K-PF, Kwok W-C, Ma T-F, et al. Territory-Wide study on hospital admissions for asthma exacerbations in the COVID-19 pandemic. Ann Am Thorac Soc 2021;18:1624–33. 10.1513/AnnalsATS.202010-1247OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hospital authority statistical report. Available: https://www3.ha.org.hk/Data/HAStatistics/StatisticalReport [Accessed 12th April 2021].
- 27.Hong Kong Observatory. Available: https://www.hko.gov.hk/en/wxinfo/pastwx/mws/mws.htm [Accessed 18th April 2021].
- 28.Air quality health index monthly summary. Available: https://www.aqhi.gov.hk/en/aqhi/statistics-of-aqhi/aqhi-monthly-summary.html [Accessed 18th April 2021].
- 29.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002;27:299–309. 10.1046/j.1365-2710.2002.00430.x [DOI] [PubMed] [Google Scholar]
- 30.Agresti A. Categorical data analysis. 3rd edn. Wiley, 2012. [Google Scholar]
- 31.Lim RH, Chow A, Ho HJ. Decline in pneumococcal disease incidence in the time of COVID-19 in Singapore. J Infect 2020;81:e19–21. 10.1016/j.jinf.2020.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Juan H-C, Chao C-M, Lai C-C, et al. Decline in invasive pneumococcal disease during COVID-19 pandemic in Taiwan. J Infect 2021;82:282–327. 10.1016/j.jinf.2020.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teng JLL, Fok KMN, Lin KPK, et al. Substantial decline in invasive pneumococcal disease (IPD) during COVID-19 pandemic in Hong Kong. Clin Infect Dis 2021;27:ciab382. 10.1093/cid/ciab382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valsecchi P, Colaneri M, Zuccaro V, et al. Impact of pneumococcal urinary antigen testing in COVID-19 patients: outcomes from the San Matteo COVID-19 registry (SMACORE). J Pers Med 2021;11:762. 10.3390/jpm11080762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhu X, Ge Y, Wu T, et al. Co-Infection with respiratory pathogens among COVID-2019 cases. Virus Res 2020;285:198005. 10.1016/j.virusres.2020.198005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bennett JC, Hetrich MK, Garcia Quesada M, et al. Changes in Invasive Pneumococcal Disease Caused by Streptococcus pneumoniae Serotype 1 Following Introduction of PCV10 and PCV13: Findings from the PSERENADE Project. Microorganisms 2021;9:696. 10.3390/microorganisms9040696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Waight PA, Andrews NJ, Ladhani SN, et al. Effect of the 13-valent pneumococcal conjugate vaccine on invasive pneumococcal disease in England and Wales 4 years after its introduction: an observational cohort study. Lancet Infect Dis 2015;15:535–43. 10.1016/S1473-3099(15)70044-7 [DOI] [PubMed] [Google Scholar]
- 38.Berman-Rosa M, O'Donnell S, Barker M, et al. Efficacy and effectiveness of the PCV-10 and PCV-13 vaccines against invasive pneumococcal disease. Pediatrics 2020;145:e20190377. 10.1542/peds.2019-0377 [DOI] [PubMed] [Google Scholar]
- 39.McLaughlin JM, Jiang Q, Isturiz RE, et al. Effectiveness of 13-Valent pneumococcal conjugate vaccine against hospitalization for community-acquired pneumonia in older us adults: a test-negative design. Clin Infect Dis 2018;67:1498–506. 10.1093/cid/ciy312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lawrence H, Pick H, Baskaran V, et al. Effectiveness of the 23-valent pneumococcal polysaccharide vaccine against vaccine serotype pneumococcal pneumonia in adults: a case-control test-negative design study. PLoS Med 2020;17:e1003326. 10.1371/journal.pmed.1003326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cheng VC-C, Wong S-C, Chuang VW-M, et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect 2020;81:107–14. 10.1016/j.jinf.2020.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chan JF-W, Yuan S, Zhang AJ, et al. Surgical mask partition reduces the risk of noncontact transmission in a golden Syrian hamster model for coronavirus disease 2019 (COVID-19). Clin Infect Dis 2020;71:2139–49. 10.1093/cid/ciaa644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wong S-C, Lam GK-M, AuYeung CH-Y, et al. Absence of nosocomial influenza and respiratory syncytial virus infection in the coronavirus disease 2019 (COVID-19) era: implication of universal masking in hospitals. Infect Control Hosp Epidemiol 2021;42:218–21. 10.1017/ice.2020.425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chan T, Tay MZ, Kyaw WM, et al. Epidemiology, vaccine effectiveness, and risk factors for mortality for pneumococcal disease among hospitalised adults in Singapore: a case-control study. BMC Infect Dis 2020;20:423. 10.1186/s12879-020-05140-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Darbà J, Marsà A. Hospital incidence, in-hospital mortality and medical costs of pneumococcal disease in Spain (2008-2017): a retrospective multicentre study. Curr Med Res Opin 2021;37:523–30. 10.1080/03007995.2021.1876007 [DOI] [PubMed] [Google Scholar]
- 46.Brotons P, Gelabert G, Launes C, et al. Cost of hospitalizing children with invasive pneumococcal pneumonia. Vaccine 2013;31:1117–22. 10.1016/j.vaccine.2012.12.025 [DOI] [PubMed] [Google Scholar]
- 47.Yang L. Acute kidney injury in Asia. Kidney Dis 2016;2:95–102. 10.1159/000441887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bersano A, Kraemer M, Touzé E, et al. Stroke care during the COVID-19 pandemic: experience from three large European countries. Eur J Neurol 2020;27:1794–800. 10.1111/ene.14375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Del Vecchio Blanco G, Calabrese E, Biancone L, et al. The impact of COVID-19 pandemic in the colorectal cancer prevention. Int J Colorectal Dis 2020;35:1951–1. 10.1007/s00384-020-03635-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-055575supp001.pdf (358KB, pdf)
Data Availability Statement
No data are available.