Abstract
Introduction
Diet and nutrition are leading causes of global morbidity and mortality. Our study aimed to identify and synthesise evidence on the association between food environment characteristics and diet, nutrition and health outcomes in low-income and middle-income countries (LMICs), relevant to urban settings, to support development and implementation of appropriate interventions.
Methods
We conducted a comprehensive search of 9 databases from 1 January 2000 to 16 September 2020 with no language restrictions. We included original peer-reviewed observational studies, intervention studies or natural experiments conducted in at least one urban LMIC setting and reporting a quantitative association between a characteristic of the food environment and a diet, nutrition or health outcome. Study selection was done independently in duplicate. Data extraction and quality appraisal using the National Heart Lung and Blood Institute checklists were completed based on published reports using a prepiloted form on Covidence. Data were synthesised narratively.
Results
74 studies met eligibility criteria. Consistent evidence reported an association between availability characteristics in the neighbourhood food environment and dietary behaviour (14 studies, 10 rated as good quality), while the balance of evidence suggested an association with health or nutrition outcomes (17 of 24 relevant studies). We also found a balance of evidence that accessibility to food in the neighbourhood environment was associated with diet (10 of 11 studies) although evidence of an association with health outcomes was contradictory. Evidence on other neighbourhood food environment characteristics was sparse and mixed. Availability in the school food environment was also found to be associated with relevant outcomes. Studies investigating our other primary outcomes in observational studies of the school food environment were sparse, but most interventional studies were situated in schools. We found very little evidence on how workplace and home food environments are associated with relevant outcomes. This is a substantial evidence gap.
Conclusion
‘Zoning’ or ‘healthy food cart’ interventions to alter food availability may be appropriate in urban LMIC.
PROSPERO registration number
CRD42020207475.
Keywords: health policy, nutrition, public health, nutritional and metabolic disorders, systematic review
Key questions.
What is already known?
There is growing evidence from high-income settings that food environments drive behaviour, nutrition and health outcomes.
We don’t know how, or which aspects of, food environments may be impacting populations in low-income and middle-income countries.
What are the new findings?
This systematic review is the largest known compilation of evidence on the impact of the food environment on health in low-income and middle-income countries, compiling experimental and observational studies to illuminate areas where the evidence is consistent, where it is contradictory, and where it is lacking.
The balance of evidence suggests that availability and accessibility domains of the food environment are associated with diet, nutrition and/or health outcomes, while evidence on the impact of prices, vendor and product properties, marketing and regulation is sparse and mixed.
What do the new findings imply?
Our synthesis can be used to support policy and practice activities to change the availability of healthy and unhealthy food in the neighbourhood environment, particularly in middle-income countries; examples would be zoning laws or healthy food carts.
Affordability and social environment (‘desirability’) interventions appear to be potentially interesting and worthwhile avenues to pursue (little but consistent evidence).
More research is required to understand the impact of workplace and home food environments, vendor and product properties in neighbourhoods and schools, and intervention studies in lower middle-income and low-income countries.
Introduction
Diet and nutrition are among the leading causes of global illness, disability and death; in 2017, 1 in 5 deaths and 255 million disability-adjusted life-years were attributed to dietary risk factors.1 This is largely due to the contribution of dietary risk factors to development of non-communicable diseases (NCDs). The health and economic impacts of NCDs in low-resource settings are disproportionally high2–4; around 80% of NCD deaths occur in low-income and middle-income countries (LMICs).5 Diet also plays a role in wider morbidity and mortality, including from infectious diseases.6 7
The food environment includes ‘physical, economic, policy and sociocultural surroundings, opportunities and conditions’ that are likely to drive dietary behaviour, nutrition and health.8 Systematic reviews of evidence from high-income countries (HICs) have found evidence of associations between availability of specific categories of food outlets and dietary and health outcomes,9–12 as well as evidence suggesting associations between other characteristics of the food environment (eg, affordability, marketing and regulation) and dietary and health outcomes.12 13 These have driven policy-makers to intervene and attempt to regulate the food environment to improve health outcomes.14 15
Globalisation and international trade are homogenising environments and infrastructure worldwide, however, there are still important differences in the food environments, and the way that populations interact with these, between HICs and LMICs.16 For this reason, despite an existing evidence base on the association between the food environment in HICs and diet, nutrition and health outcomes, it is important to also investigate and synthesise evidence from LMICs.
Fifty-five per cent of the world population lives in urban settings, and this figure is projected to rise to 70% by 2050.17 There are differences between urban and rural LMIC settings relating to the food environment, dietary behaviour and health. In urban LMIC, individuals are more likely to buy than grow food for their own consumption and a number of distinct barriers exist which may reduce access to healthy food, such as more expensive fresh food.18 There is evidence that diets, dietary behaviour and related health outcomes may be poorer in urban LMIC settings than in rural LMIC settings. The global burden of disease study noted a marked difference between obesity prevalence in rural and urban populations19 and a more recent review highlights higher prevalence of central obesity in urban residents.20 A systematic review and meta-regression found an association between urbanicity and obesity prevalence in Southeast Asia.21 Further systematic reviews and meta-regression analyses have found that in sub-Saharan Africa, urban residents are more likely to consume salt and less likely to consume vegetables than rural residents.22 23 A 2015 study of 74 Latin American countries found that sales of ultraprocessed products were larger in more urbanised countries.24
Context-specific research is required to understand how the food environment in urban LMIC can support or hinder the diet and health of LMIC populations, to support development of appropriate interventions. LMIC policy-makers need to see evidence that resonates with them to justify taking steps to intervene in the food environment.
Aim
The aim of our study is to identify and synthesise evidence that reports associations between the characteristics of the food environment and diet, health and nutrition outcomes or effects of food environment interventions on these outcomes, in LMICs that are relevant to urban settings.
Methods
A theoretical framework for conceptualising the LMIC food environment
We have adopted Turner et al’s16 conceptual model of the food environment, developed through a series of iterative, international congregations with experts in nutrition and public health. In this conceptual model, the food environment is situated within the broader food system. The model relates four external domains (food availability, prices, vendor and product properties, marketing and regulation) to four personal domains (food accessibility, affordability, convenience and desirability).16 For this review, we are most interested in the external domains of the food environment. However, we also conceive of accessibility (which in Turner’s model includes physical distance to food vendors and individual activity spaces) and affordability (purchasing power) as concepts of interest. This is reflected in our study eligibility criteria and further details are in tables 1 and 2.
Table 1.
Eligibility criteria
| Domain | Inclusion criteria | Exclusion criteria |
| Population/setting | Must feature one or more urban LMIC setting according to the World Bank Data (2020) classification of countries.106 | High-income country settings or high-income country and LMIC settings in which it is impossible to disaggregate the LMIC findings. Exclusively rural settings. |
| Exposure/intervention | One or more of six food environment characteristics defined in table 2 (Availability, Price, Vendor and Product Properties, Marketing and Regulation, Accessibility and/or Affordability). We also collected data on quantitative associations between two further food environment characteristics (Convenience or Desirability) and our outcomes of interest. However, if papers reported associations between these food environment characteristics and our outcomes of interest only, they were excluded. |
Do not include relevant exposures. |
| Outcomes | Must report a quantitative association between a food environment characteristic (as described in exposure/intervention) and: Any health outcome (eg, prevalence of obesity, hypertension, diabetes or any other health outcome) or Diet/ dietary behaviour outcome (eg, foods bought or consumed) or Nutrition outcome (energy intake, macronutrients or micronutrients consumed) |
Do not include relevant outcomes or do not include associations between the exposure/intervention of interest and relevant outcomes. |
| Study design | Quantitative or mixed-methods observational studies (cross-sectional, case–control, longitudinal cohort and mixed-methods studies) or intervention studies (including trials, interrupted time series or other intervention study designs) and natural experiments will be included. | Reviews including systematic reviews Qualitative studies |
| Publication type | Original peer-reviewed published articles | Protocols, full theses, case series and case reports. Conference abstracts. |
LMIC, low-income and middle-income country.
Table 2.
Characterisation of the food environment, adopted from Turner et al16
| Turner concept | External | Internal | ||||||
| Availability | Prices | Vendor and product properties | Marketing and regulation | Accessibility | Affordability | Convenience | Desirability | |
| Turner definition | Presence of food sources or products | Monetary value of food products | Vendor properties (typology, opening hours, services) and product properties (food quality, composition, safety, level of processing, shelf-life, packaging) | Promotional information, branding advertising, sponsorship, labelling, policies | Physical distance, time, space and place, individual activity spaces, daily mobility, mode or transport | Purchasing power | Relative time and effort of preparing, cooking and consuming food product, time allocation | Preferences, acceptability, tastes, desires, attitudes, culture, knowledge and skills |
| Primary outcomes | Secondary outcomes | |||||||
| Examples from the identified literature | Density of food retail outlets of various types. Counts of food retail outlets. Presence of food retail outlets of various types. Availability of specific food items at school or home. |
Monetary value of fruit, vegetables, sugar-sweetened beverages, ultraprocessed food, apples. | Quality of fruit and/or vegetables. Commercial vendor within a school or non-commercialised food environment. |
Billboard advertising of various types. Advertising within food retail locations. Provincial school policies. Individual school policies. School status as a health promoting school. Workplace policy |
Living near a fast-food outlet. Perceived local food availability of various types. Perceptions of ease of access to retail outlets of various types. |
‘I can buy fruit and veg even when they are expensive’ The cost of two servings of fruit and three of vegetables per day relative to household income. |
‘I have time to prepare and eat Fruit and veg’ ‘Fruit and veg are easy to prepare for me’ |
Preferences measured using Likert scales ‘I like it very much’ to ‘I have not tried it’ Culture
|
| No of times this appears | 54 | 4 | 3 | 15 | 22 | 2 | 3 | 11 |
Search strategy and selection criteria
For this systematic review, we conducted a comprehensive search of nine databases: MEDLINE, EMBASE, Global Health, Econlit, Web of Science, Scopus, CINAHL, PsycINFO and Applied Social Sciences Index and Abstracts on 16 September 2020 to identify relevant studies. We did not apply any language restrictions, but restricted the search to studies published since the year 2000. The search strategy was based on those published in Turner et al,25 adapted by two researchers (OO and SW) and an academic librarian. The search terms used in MEDLINE are presented in online supplemental table 1).
bmjgh-2021-006358supp001.pdf (242.5KB, pdf)
After completion of searches, retrieved records were exported to an EndNote library, duplicates were removed and records were then imported and managed using the online platform Covidence. A predefined list of inclusion and exclusion criteria (table 1) was used to sift titles and abstracts in duplicate (SW, IG, HMJ, DM, NA, LA-K and OO), with any study assessed as potentially relevant by either reviewer (or both) retrieved in full for text assessment. Formal eligibility assessment was done in duplicate (SW, IG, AI, HMJ, DM, NA, RI and OO) with disagreements resolved by a third reviewer (OO or SW). Further screening of the reference lists of included studies was also completed by one reviewer (SW).
The protocol for this study was registered online with the PROSPERO database: (CRD42020207475).26
Data analysis
We extracted data into a predetermined and piloted data extraction form on Covidence. We extracted data on study characteristics (citation; study design, duration and timing; setting), participant characteristics, details of the food environment characteristics examined including how these were assessed, details of the health, details of the diet or nutrition outcomes including definition and assessment method and key findings including statistics such as effect sizes as reported.
We conducted quality appraisal using the National Heart Lung and Blood Institute checklists relevant to the study design pertaining to the outcomes of interest (eg, for a mixed-methods study which reported a cross sectional association between a food environment characteristic and a health, diet or nutrition outcome, we would use the checklist for cross sectional studies). Quality was rated good, fair or poor.
Seven studies were abstracted and quality appraised in duplicate, with any variation between extractions resolved by one reviewer (OO). There were no inconsistencies between extractions and so the majority of data extraction and quality appraisal were completed by one reviewer (SW, IG, HMJ, FS, AI or OO) and checked by a second reviewer (SW or OO).
We synthesised identified literature by subdividing the studies into groups first into observational studies and interventional studies. For the synthesis of observational studies, we grouped them based on the food environment characteristics examined, and within these groups, we further subdivided studies into those reporting health, nutrition or diet outcomes respectively. We did not try to standardise the exposures or outcomes of the observational studies. Instead we were most interested in whether an association was reported between the characteristic and an outcome. For the interventional studies we synthesised the findings by comparing the outcomes from studies with elements targeting similar food environment characteristics. We did not apply Grades of Recommendations, Assessment, Development and Evaluation to assess the certainty of the evidence from the identified trials, because of the heterogeneous nature of the complex interventions in these, and the type of recommendations we were seeking to make.
We reported the study according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.27
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report. The corresponding author had full access to all the data in the review and had final responsibility for the decision to submit for publication.
Results
Search results
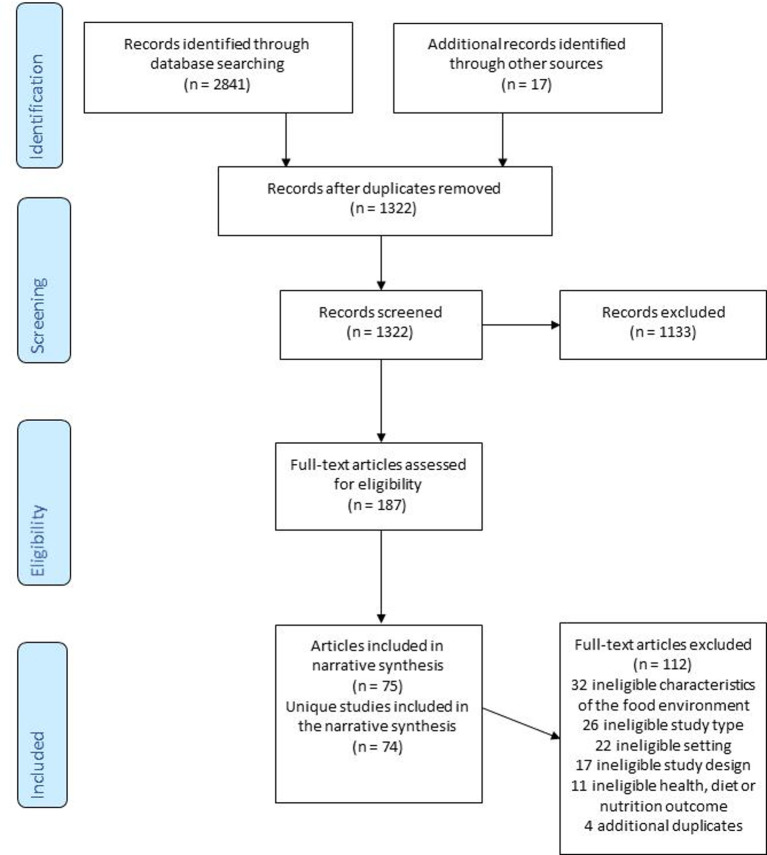
Figure 1 provides the PRISMA diagram and reasons for exclusion. Searches identified 2858 records. Titles and abstracts of 1322 were screened, including 1305 deduplicated records identified through database searching and 17 records identified through reference screening of included studies. We identified 187 articles for full-text review of which 75 articles met eligibility criteria and were included in this systematic review. For a full list of excluded studies, please see online supplemental table 3).
Figure 1.
PRISMA flow diagram. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Description of included studies
Tables 2 and 3 describe the characteristics of the observational and interventional articles included, respectively. Identified studies were published between 2010 and 2020 and included data collected from the year 2000 onwards (although a few studies did not report when data collection occurred). In total 29 countries were represented in the data included in this systematic review, including both higher and lower middle income countries (26 and 20 represented, respectively), as well as low-income countries (three represented: Malawi, Sudan and Syria, all included within multicountry studies).
Table 3.
Characteristics of included observational studies
| Study ID | Study setting | Dates of data collection | Population | Food environment characteristic/s | Outcome |
| Cohort studies | |||||
| Seto, 202071 | Kunming, China, Neighbourhood | Not reported | 12 adults aged 18–31 (mean age 24.6). With average BMI of 21.0. 17% with overweight. | Acc | D |
| Wang, 201234 | China, Neighbourhood | 2004 and 2006 | 185 children aged 6%–18. 51% female. | Av | N |
| Xu, 201335 | 9 provinces, China, Neighbourhood | 2000–2009 | 13 993 male and 15 125 female person-years. Mean age ranged between 44 and 51 over the period 2000–2006. | Av | H |
| Case–control studies | |||||
| Setiyaningsih, 201936 | Surakarta, Indonesia, School | April 2019 | 225 children from 15 schools including 75 with obesity and 150 normal weight. | Av | H |
| Cross-sectional studies | |||||
| Alves, 201976 | Florianopolis, Brazil, Neighbourhood | September 2012–June 2013 | 2484 children aged 7–14 (mean age 10.4). 56.5% female. 66.8% normal weight. | Acc | D |
| Assis, 201950 | Juiz de Fora, Brazil, Neighbourhood | July 2011– December 2021 | 661 children aged 7–14 (median age 11). 51.7% female. | Av | H |
| Azeredo, 201689 | Brazil; School | 2012 | 109104 students majority aged 11%–14. 52.2% female. | Av | D |
| Backes, 201951 | Sao Leopoldo, Brazil, Neighbourhood | 2015 | 1096 women aged 20–69 years. 33.1% with obesity. | Av | H |
| Barrera, 201684 | Cuernavaca and Guadalajara, Mexico, School | October 2012–March 2013 | 725 children aged 9–11 (median age 10). 56.8% female. 24.8% with overweight and 20.7% with obesity. | Av | H |
| Bekker, 201730 | Bloemfontein, South Africa, School | Not reported | 257 students aged 7–14 took part in the quantitative data collection. 61.1% female. | Av | D |
| Camargo, 201962 | Campinas, Brazil, Neighbourhood | July 2014– December 2014 | Residents aged 18+ of two low-income areas. | Av | H |
| Charoenbut, 201829 | Samutprakarn province, Thailand, Workplace | March–June 2011. | 924 workers from 26 industrial factories. 39.1% aged 31%–40. 56.5% female. | Av, M&R, D | D |
| Chor, 201672 | 6 cities, Brazil, Neighbourhood | August 2008– December 2010 | 14749 civil servants at teaching and research institutions aged 35–74 (median age 51 years). 54.4% women. | Acc | D |
| Corrêa, 201852 | Florianopolis, Brazil, Neighbourhood | September 2012–June 2013 | 2195 children aged 7%–14. 47.7% female. The prevalence of overweight/obesity was 29.0% for girls, 37.6% for boys. | Av | H |
| Cunningham-Myrie, 202053 | Jamaica, Neighbourhood | 2008 | 2529 participants in a nationally representative survey, aged 18–74 (Mean age of men=37.0 years, mean age of women=36.7 years). 68.5% female. Mean BMI for women 28.4. Mean BMI for men 24.8. | Av; Acc | H |
| Curioni, 202037 | Rio de Janeiro, Brazil, Neighbourhood | 2012–13 | 2032 civil servants of a university. 46% aged 45–54 years. 60% women. | Av | D |
| da Silva, 201966 | Minas Gerais, Brazil; Neighbourhood | June 2012–July 2016 | 965 women and men aged 20–59 years old (mean age: 34.2). 55.2% female. 13.8% with obesity. | Av | H |
| Dake, 201654 | Accra, Ghana, Neighbourhood | 2011–2013 | 657 participants (mean age 31.5). 54.0% female. 23.29% with overweight, 18.6% with obesity. | Av | H |
| Darfour-Oduro, 202091 | 24 countries: Malawi, Jordan, Egypt, Maldives, Dominica, Grenada, Jamaica, Fiji, Malaysia, Mongolia, Indonesia, Phillippines, Thailand, Benin, Mauritania, Sudan, Algeria, Libya, Morocco, Syrian Arab Republic, Pakistan, Argentina, Honduras, Tonga, School | 2004–2013 | 89843 children aged 13–17. | M&R | D |
| de Freitas, 201960 | Belo Horizonte, Brazil, Neighbourhood | 2013 | 2810 participants, majority aged 30–59 (54.1%). 88.4% female. Mean BMI 27.8. The majority with overweight (62.6%). | Av; V/P; Price; M&R | H |
| Duran, 201538 | Sao Paulo, Brazil, Neighbourhood | 2010–2011 | 1842 adults aged 20–59 (mean age 36.5). 53% female. | Av; Acc; Price | D |
| Fernandes, 201731 | Ghana, School | 2013–2014 | 4258 children aged 5–17 years. 46.9% female. | Av | D |
| Gonçalves, 201987 | Brazil, School | 2013–2014 | 73399 children aged 12–17 years (mean age 14.4 years) from 1247 schools. | Av; V/P | H |
| Goryakin, 201539 | Armenia, Azerbaijan, Belarus, Georgia, Kazakhstan, Kyrgyzstan, Moldova, Russia and Ukraine, Neighbourhood | 2010–2011 | 17998 adults aged 18–95 years. | Av; Acc; M&R | D |
| Guo, 201864 | 12 provinces, China, neighbourhood | 2011–2013 | 1416 children aged 7–17. | Av; M&R | H |
| Guo, 201965 | China, Neighbourhood | 2000–2013 | 4803 children aged 7–17. | Av; M&R | H |
| Hall, 202055 | China, Neighbourhood | November 2016–August 2017 | 1388 women aged 18–67 (median age 41). Mean BMI 24.5% and 64.0% with overweight or obesity. | Av | H |
| Hua, 201463 | Macau, China, Neighbourhood | 2011 | 575 children aged 13–18 from one high school. Mean BMI 21.1. | Av | H |
| Jaime, 201140 | Sao Paulo, Brazil, Neighbourhood | 2003 | 2122 adults aged 18+. | Av | H, D |
| Kelly, 201470 | Thailand, Neighbourhood | 2012 | 1516 students enrolled at an Open University (studying by correspondence and living all over the country). Aged 18–87 (mean age 29). | Av; Acc | H, D, N |
| Kivuyo, 202073 | Punjab, India, Neighbourhood | Not reported | 120 African emigrant students in Pubjab. Age range 18->28 years 64.9% aged 23–27. | Acc; D | D |
| Kroll, 201948 | Khayelitsha, South Africa and Ahodwo, Ghana, Neighbourhood | September–November 2017 | 327 households in Khayelitsha, South Africa and 309 households in Ahodwo, Ghana. | Av | D |
| Leite, 201741 | Santos, Brazil, Neighbourhood | January 2010–June 2011 | 513 children aged under 10. | Av | D |
| Leme, 201793 | Sao Paulo, Brazil, Home | 2014 | 253 adolescent girls aged 14%–18. 70.4% Hy weight, 18.3% overweight and 8.3% obese. | Acc; D | D |
| Li, 201185 | Xi'an City, China, School | May–November 2004 | 1792 children aged 11–17 years (mean age 13.9). 49.8% female. | Av; M&R | H |
| Liu, 201447 | nine provinces, China, Neighbourhood | 2006 | No sample size reported. Aged 18–95 mean age 49.4 for urban and 48.7 for rural participants. 53% female in urban sample, 52% female in the rural sample. | Av; Acc; Conv | D |
| Liu, 202074 | Shenyang, China, Neighbourhood 68 | May 17th–June 23rd 2017 | 3670 children (mean age 10.8) from 26 schools. 49% female. | Acc | H, D |
| Machado, 201782 | Brazil, Neighbourhood | 2008–2009 | 55970 households from a nationally representative survey | Price, Conv | D |
| Matozinhos, 201556 | Belo Horizonte, Brazil, Neighbourhood | 2008–2010 | 5273 adults aged 18–93 (mean age 43.6). 56.5% female. 12.1% with obesity. | Av | H |
| Mendes, 201367 | Belo Horizonte, Brazil, Neighbourhood | 2008–2009 | 3404 adults aged 18+ (mean age 39.7). | Av | H |
| Mendonça, 201942 | Belo Horizonte, Brazil, Neighbourhood | 2013/2014 | 3414 adults aged 20+ (mean age 56.7). 88.1% female. 62.7% with overweight or obesity. | Av; V/P | D |
| Menezes, 201877 | Belo Horizonte, Brazil, Neighbourhood | February 2013–June 2014 | 3414 adults aged 20+ (mean age 56.7). 88.1% female. 62.7% with overweight or obesity. | Acc; Aff; Conv | D |
| Menezes, 201843 | Belo Horizonte, Brazil, Neighbourhood | 2015 | 2944 adults aged 20+ (mean age 56.8). 88.4% female. | Av | D |
| Miller, 201683 | Bangladesh, India, Pakistan, and Zimbabwe, China, Colombia, Iran, Occupied Palestinian Territory, Argentina, Brazil, Chile, Malaysia, Poland, Turkey, South Africa (and three high-income countries: Canada, Sweden, United Arab Emirates, however we extracted data from LMICS only), Neighbourhood | January 1 2003–December 31 2013 | 128112 adults. UMIC median age 51.0, 60% female, mean BMI 28.4. LMIC median age 51.0, 58% female, mean BMI 25.2. LIC median age 47.0, 57% female, mean BMI 23.3 | Aff | D |
| Nogueira, 201844 | Sao Paulo, Brazil, Neighbourhood | February 2015– February 2016 | 521 adolescents aged 12–19 (mean age 15.5). 49.3% female. 70.4% did not have overweight. | Av | D |
| Nogueira, 202057 | Sao Paulo, Brazil, Neighbourhood | Feb 2015–2016 | 504 adolescents aged 12%–19. 48.6% female. 29.6% with overweight or obesity. | Av | H |
| Norbu, 201992 | Pemagatshel District, Bhutan, School | Not reported | 392 children aged 13–17 (mean age 14.5) from six schools. | Unknown | H |
| Ochoa-Meza, 201728 | six cities, Mexico, School and Home | Nor reported | 1434 children aged 10%–12. 49.5% female. | Acc; D | D |
| Oyeyemi, 201279 | Maiduguri, Nigeria, Neighbourhood | August 2010– September 2011 | 1818 adults aged 20–65 (mean 32.2). 39.9% female. 22.8% with overweight and 8.1% with obesity. | Acc | H |
| Opal, 201845 | Delhi, India, Neighbourhood | 2010–2011 | 5364 adults mean ages 43.7–45.6 across three categories of restaurant density. 50% female. | Av | H, D |
| Pessoa, 201546 | Belo Horizonte, Brazil, Neighbourhood | 2008–2010 | 5611 adults aged 18+ (mean age 39.7). 54.8% female. | Av | D |
| Rossi, 201881 | Florianopolis, Brazil, Neighbourhood | September 2012 –June 2013 | 2152 children aged 7%–14. 21.5% had overweight and 12.7% had obesity | Acc | H |
| Trinh, 202061 | Vietnam, Neighbourhood | 2010–2014 | Not reported. | Av | D, N |
| Vedovato, 201575 | Santos City, Brazil, Neighbourhood | January– December 2010 | 538 dyads, children aged 1–10 and mothers 62.1% | Acc | D |
| Velásquez-Meléndez, 201368 | Belo Horizonte, Brazil, Neighbourhood | 2008–2009 | 3425 adults age 18+ (mean age 39.7). 49.9% female. 44% with overweight or obesity. | Av | H |
| Watson, 201369 | Azerbaijan, Armenia, Belarus, Georgia, Kazakhstan, Kyrgyzstan, Moldova, Russia and Ukraine, Neighbourhood | 2010 | 2899 adults. 55.3% female. Male participants mean age 42.0 and mean BMI 25.4. Female participants mean age 43.7 and mean BMI 25.3. | Av; Acc; Price; M&R | H |
| Wertheim-Heck, 201932 | Hanoi, Vietnam, Neighbourhood | 2017–2018 | 400 women of “childbearing age” | Acc | D |
| Widiyanto, 201888 | Java, Indonesia, School | December 2017 | 200 children in junior high school (age not reported). 72% female. 58% with BMI <23 | Av; D | H |
| Wijnhoven, 2014107 | Bulgaria (and other HIC countries—results for Bulgaria extracted for our review), School | September 2007–December 2008 | 179 schools, at least 15 children per school. | Av | H |
| Yazdi Feyzabadi, 201790 | Iran, School | February–March 2015. | 1242 14 year olds. 47.8% female. | Av; M&R; Acc; D | D |
| Zhang, 201249 | China, Neighbourhood | 2006 | 9788 adults. 52.7% female. 23.2% with overweight, 4.9% with obesity. | Av | D |
| Zhang, 201680 | China, Neighbourhood | 2009 and 2011 | 348 children aged 6–17 (mean age 10.9). 49.7% female. | Acc | H |
| Zhang, 202058 | China, Neighbourhood | 2013–2014 | 170872 adults aged 18+. 57.3% female. | Av | H |
| Zheng, 201394 | China, Home | 2008–2009 | 5662 children aged 6%–18. 50.5% female. | Av; D | H |
| Zhou, 201759 | Wuhan, China, Neighbourhood | 2010 | 189 adults aged 35–49. Mean BMI for men 25.5 and mean BMI for women 23.9. | Av | H |
| Zhou, 202086 | Beijing, China, School | May–June in 2016. | 2201 students from 37 schools (mean age 10.2). | Av | H |
| Zuccolotto, 201578 | Brazil, Neighbourhood | May–November 2012 | 282 pregnant women in the second-trimester living in Brazil. Most between 20–29 years. | Acc; D | D |
Acc, Accessibility; Aff, Affordability; Av, Availability; Conv, Convenience; D, Desirability; D, Diet; H, Health; M&R, Marketing and regulation; N, Nutrition; V/P, Vendor or product properties.
Sixty-seven included articles reported 67 unique observational studies, comprised of 6 multicountry studies and 61 focused on one country (table 3). Of those focusing on one country, 28 were based on data from Brazil, 16 from China, two from each of Vietnam, Ghana, Mexico and India. The multi-country studies included two focused on nine countries of the former Union of Soviet Socialist Republics, one examining data from South Africa and Ghana, one study of multiple European countries, from which we extracted data from Bulgaria (the only LMIC included), and two studies of multiple LMICs (one of which also included HICs). Figure 2 shows the countries covered by observational studies included in our review.
Figure 2.
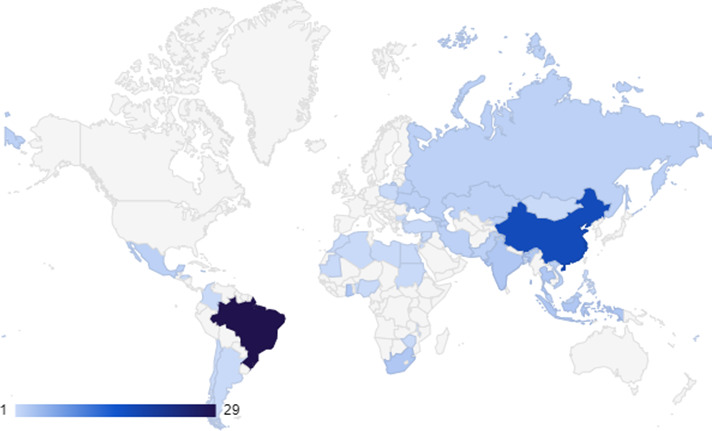
Map to show countries covered by observational studies included in our review.
The observational studies covered the food environment in the home (n=2), school (n=13) and neighbourhood (n=50) setting. With one additional study examining both the home and school environment28 and one further study investigating the food environment in the workplace setting.29 Most used a cross sectional design for investigating the association between the food environment and health, diet or nutrition outcomes (n=63) although these were sometimes nested in a cohort study, or one part of a mixed-methods study.30–32 Three studies used cohort study designs, all from Chinese settings.33–35 One study used a case–control design.36
Study populations included adults and children. Associations were presented between food environment characteristics and diet (n=35), health (n=36) and nutrition (n=3) outcomes, in which three studies examined both diet and health outcomes, one study examined diet and nutrition outcomes and one study examined all three.
The eight interventional articles reported seven unique studies. These include two studies from Iran (one cross-sectional study and one cluster randomised controlled trial (RCT)), one cluster RCT from Brazil, one controlled study from South Africa and one cluster RCT from Thailand (table 4). Additionally, there were two reports of the same cluster RCT carried out in Mexico and a further Mexican cluster RCT. All of these studies are from upper-middle-income countries. All of the included articles report interventions based in schools, except the study in Brazil which evaluates a workplace intervention. Interventions ranged in duration from 4 weeks to ~4 years (in the Iranian cross-sectional study which examined the Iranian Health Promoting Schools programme which was set up in 2011 and the evaluation data collected in 2015). All studies reported the effect of the intervention on dietary outcomes except for one Mexican study which reported health outcomes only.33 The second Mexican study and the Thai study additionally reported health outcomes, and the Iranian cluster RCT and South African study additionally reported nutrition outcomes.
Table 4.
Characteristics of included interventional studies
| Study ID | Study setting (country, setting) | Study design | Dates of data collection | Population (n, description, age) | Food environment characteristic/s | Length of intervention | Outcome |
| Aghdam, 201896 | Tabriz, Iran; School | cRCT | 2015 | 4 control and four intervention schools. 436 children (mean age 9.6). 55.6% female. | Av; M&R; D | 4 weeks | D; N |
| Bandoni, 2011100 | Sao Paulo, Brazil; Workplaces | cRCT | Not reported | 15 intervention and 14 control companies. 1296 and 1214 workers aged 18+ per round of data collection (independent samples). Male majority. | M&R | 6 months | D |
| Bonvecchio-Arenas, 2010; Safdie, 201395 108 | Mexico City, Mexico; School | 3-arm cRCT | 2006–2008 | 8 basic intervention schools, 7 intervention-plus schools and 11 control schools. 830 students (mean age 9.7 years). 50% females. Mean BMI 19.8 and prevalence of overweight/obesity 43%. | Av; M&R; D | 18 months | H, D |
| Chawla, 201799 | Bangkok, Thailand; School | cRCT | Not reported | 2 intervention and two control schools. 452 children aged 10–12 (mean age 9.7 (intervention) 10.0 (control)). 53.5% females. 19.7% overweight or obese in the control group, 16.6% in the intervention group at baseline. | Av; | 6 months | H, D |
| Shamah Levy, 201233 | State of Mexico, Mexico; School | cRCT | 2010–2011 | 30 intervention and 30 control schools. 997 children mainly aged 10–13 (modal age 10). 51.6% females and 49.7% females in intervention and control group respectively. Mean BMI 18.6–18.8. | Av; M&R | 6 months | H |
| Steyn, 201598 | Western Cape, South Africa; School | Controlled study | 2009–2011 | 8 intervention and eight control schools. 998 children (mean age 9.9 in 2009, 12.3 in 2011) | Av; M&R | 3 years | D, N |
| Yazdi-Feyzabadi, 201897 | Kerman, Iran; School | Cross-sectional study | 2015 | 40 schools 1242 children. 47.8% female | M&R | ~4 years | D |
Study design cRCT: food environment characteristics.
Given the heterogeneity in study design, methodology, exposure and outcomes, we have performed a narrative synthesis.
The characteristics of the food environment investigated in the included studies are further described in table 2.
Av, availability; BMI, body mass index; cRCT, cluster randomised controlled trial; D, desirability; M&R, marketing and regulation; N, nutrition; outcome H, health; V/P, vendor or product properties.
Of the included observational studies 42 were rated good, 17 were rated fair and 8 were rated poor (table 5). Further details of our quality appraisal are included in online supplemental table 2. The intervention studies were rated poor (n=3) and fair (n=4) (table 6). Further details on the quality appraisal are presented in online supplemental table 2.
Table 5.
Results of included observational studies
| Setting | Q | Food environment characteristic† | Outcome and significance* | |||||||||
| Av | Price | V/P | M&R | Acc | Aff | Conv | D | Diet | Nutrition | Health | ||
| Neighbourhood | ||||||||||||
| Cohort studies | ||||||||||||
| Wang, 201235 | F | X | Y | |||||||||
| Xu, 201336 | F | X | Y | |||||||||
| Seto, 201934 | F | X | Y | |||||||||
| Cross-sectional studies | ||||||||||||
| Assis, 201940 | G | X | Y | |||||||||
| Backes, 201942 | G | X | Y | |||||||||
| Corrêa, 201846 | G | X | Y | |||||||||
| Curioni, 202048 | G | X | Y | |||||||||
| da Silva49 | G | X | N | |||||||||
| Dake, 201650 | G | X | Y | |||||||||
| Hall, 202058 | G | X | Y | |||||||||
| Jaime, 201160 | G | X | Y | N | ||||||||
| Leite, 201764 | G | X | Y | |||||||||
| Matozinhos, 201570 | G | X | Y | |||||||||
| Mendes, 201371 | G | X | N | |||||||||
| Menezes, 201874 | G | X | Y | |||||||||
| Nogueira, 201876 | G | X | Y | |||||||||
| Nogueira, 202077 | G | X | Y | |||||||||
| Patel, 201880 | G | X | Y | N | ||||||||
| Pessoa, 201581 | G | X | Y | |||||||||
| Velasquez-Melendez, 201385 | G | X | N | |||||||||
| Zhang, 202092 | G | X | Y | |||||||||
| Zhou, 201794 | G | X | Y | |||||||||
| Cunningham-Myrie, 202047 | G | X | X | Y | ||||||||
| Duran, 201553 | G | X | X | X | Y | |||||||
| Goryakin, 201555 | G | X | X | X | Y | |||||||
| Guo, 201856 | G | X | X | O | ||||||||
| Guo, 201957 | G | X | X | O | ||||||||
| Mendonça, 201972 | G | X | X | Y | ||||||||
| Chor, 201645 | G | X | Y | |||||||||
| Liu, 202068 | G | X | Y | N | ||||||||
| Oyeyemi, 201279 | G | X | Y | |||||||||
| Vedovato, 201584 | G | X | Y | |||||||||
| Wertheim-Heck, 201933 | G | X | N | |||||||||
| Kivuyo, 202062 | G | X | X | Y | ||||||||
| Machado, 201769 | G | X | X | Y | ||||||||
| Miller, 201675 | G | X | Y | |||||||||
| Kroll, 201963 | F | X | O | |||||||||
| Trinh, 202083 | F | X | Y | Y | ||||||||
| Zhang, 201290 | F | X | O | |||||||||
| deFreitas, 201952 | F | X | X | X | X | Y | ||||||
| Watson, 201386 | F | X | X | X | X | N | ||||||
| Alves, 201939 | F | X | Y | |||||||||
| Rossi, 201882 | F | X | N | |||||||||
| Menezes, 201873 | F | X | X | X | Y | |||||||
| Zuccolotto, 201596 | F | X | X | Y | ||||||||
| Camargo, 201944 | P | X | Y | |||||||||
| Hua, 201459 | P | X | O | |||||||||
| Kelly, 201461 | P | X | X | N | N | N | ||||||
| Liu, 201467 | P | X | X | X | X | Y | ||||||
| Zhang, 201691 | P | X | Y | |||||||||
| Setting | Q | Food environment characteristic | Outcome | |||||||||
| Av | Price | V/P | M&R | Acc | Aff | Conv | D | Diet | Nutrition | Health | ||
| School | ||||||||||||
| Case–control studies | ||||||||||||
| Setiyaningsih, 201937 | P | X | ||||||||||
| Cross-sectional studies | ||||||||||||
| Azeredo, 201641 | G | X | Y | |||||||||
| Barrera, 201643 | G | X | ||||||||||
| Zhou, 202095 | G | X | ||||||||||
| Wijnhoven, 201488 | G | X | ||||||||||
| Yazdi-Feyzabadi, 201789 | G | X | X | X | Y | |||||||
| Li, 201166 | G | X | X | |||||||||
| Darfour-Oduro, 202051 | G | X | Y | |||||||||
| Ochoa-Meza29 | G | X | Y | |||||||||
| Bekker, 201731 | F | X | Y | |||||||||
| Fernandes, 201732 | F | X | Y | |||||||||
| Goncalves, 201954 | F | X | X | |||||||||
| Widiyanto, 201887 | F | X | ||||||||||
| Norbu, 201978 | P | Unknown | ||||||||||
| Workplace | ||||||||||||
| Cross-sectional studies | ||||||||||||
| Charoenbut, 201830 | G | X | ||||||||||
| Home | ||||||||||||
| Cross-sectional studies | ||||||||||||
| Leme, 201765 | G | |||||||||||
| Ochoa-Meza, 201729 | G | |||||||||||
| Zheng, 201393 | P | X | ||||||||||
*Outcome Y: yes, at least one significant outcome was reported; N: no a significant outcome was not reported; O: other.
†Quality: G: good, F: fair, P: poor.
Table 6.
Results of included interventional studies
| Setting | Q | Food environment characteristic | Modified outcome and significance* | |||||||||
| Av | Price | V/P | M&R | Acc | Aff | Conv | D | Diet | Nutrition | Health | ||
| Schools | ||||||||||||
| Chawla, 201799 | F | X | N | Y | ||||||||
| Bonvecchio-Arenas, 2010108; Safdie, 201395 | F | X | X | X | Y | Y | ||||||
| Shamah Levy, 201233 | F | X | X | Y | ||||||||
| Yazdi-Feyzabadi, 201897 | F | X | N | |||||||||
| Aghdam, 201896 | P | X | X | X | Y | Y | ||||||
| Steyn, 201598 | P | X | X | N | N | |||||||
| Workplace | ||||||||||||
| Bandoni, 2011100 | P | X | Y | |||||||||
Quality: G: good, F: fair, P: poor.
*Outcome Y: yes, a significant outcome was reported; N: no a significant outcome was not reported; O: other.
Acc, accessibility; Aff, affordability; Av, availability; Conv, convenience; D, desirability; M&R, marketing and regulation; V/P, vendor or product properties.
Associations reported in the literature
Fifty observational studies reported associations between neighbourhood food environment characteristics and diet, nutrition or health outcomes. Forty-seven of these were cross-sectional and three were cohort studies.
Neighbourhood availability
Thirty-six of the observational studies (2 cohort studies and 34 cross-sectional studies) examined the association between an availability variable and outcome of interest, of which 26 examined availability alone. The majority of these were investigating the presence, density or number of food retail outlets of various types with their outcomes of interest.
Two cohort studies, both fair-quality, found significant associations between an availability variable and relevant outcome, one with a nutrition outcome,34 and one with a health outcome.35 Of those cross-sectional studies investigating an availability variable, 10 good studies found significant associations between availability and dietary outcomes37–46 as did one poor study.47 Two further fair quality studies reported associations between availability and dietary outcomes although without presenting whether this was statistically significant.48 49
Further, 10 good studies found a significant association between an availability characteristic and a health outcome50–59 as did 2 fair studies60 61 and 1 further poor study.62 Additionally, one poor study reported that prevalence of overweight and mean body mass index (BMI) trended in the same direction as the number of ‘western-style’ restaurants and convenience stores, however, no statistics were presented.63 Two further good studies suggested that availability characteristics were important for childhood obesity prevalence.64 65 In contrast, five good studies did not find an association between availability and health outcomes40 45 66–68 and one additional fair study did not find an association between availability and health outcomes.69 Further, one poor study did not identify an association between availability and health (hypertension or diabetes).70
In summary, identified studies provide good evidence that the food available in the neighbourhood is associated with diet, and the preponderance of evidence suggests that the food available in the neighbourhood is also associated with nutrition and health outcomes.
Neighbourhood accessibility
The next most investigated aspect of the neighbourhood food environment was accessibility included in 18 studies, 1 cohort and 17 cross-sectional. Identified studies provide good evidence that food accessibility is associated with diet, but conflicting evidence of the association between accessibility and health, with no evidence of the association between accessibility and nutrition.
One cohort study of fair quality found an association between accessibility and dietary outcomes.71
Six good cross-sectional studies found accessibility was associated with diet38 39 72–75 as did a further three fair studies76–78 and one poor study.47 However, one further good cross-sectional study found no association between dietary quality and geographical proximity to different formal retail outlets.32
Just two good studies, both cross-sectional, found accessibility was associated with health. A 10 km increase in the distance from a supermarket was associated with a 1.7 kg/m2 higher means BMI (p=0.02) in the middle class in Jamaica53 and participants who did not report commercial places such as shops, stores and markets to be within walking distance of their homes were 49% more likely to be overweight than those who reported proximal facilities in Maiduguri, Nigeria.79 However, one additional poor study found an association between accessibility and health.80 In contrast one good study,74 two fair studies69 81 and one poor study70 found no association between accessibility variables and health outcomes.
Neighbourhood price
Price was examined in four studies all of which were cross-sectional. One good study did not find that price was associated with fruit and vegetable consumption or sugar-sweetened beverage consumption.38 Two further fair studies did not find an association between price and health outcomes. One of these found that fruit and vegetable price or ultraprocessed food price was not associated with overweight60 and the other that the price of apples was not associated with obesity.69 In contrast, one good study found that an 1% increase in the price of ultraprocessed foods acquired at supermarkets would lead to a 0.59% decrease in purchases and this price-elasticity was significant.82
Neighbourhood marketing and regulation
Marketing and regulation characteristics were examined at the neighbourhood level in five cross-sectional studies. One good study found billboard advertising of snacks was negatively related to daily fruit or vegetable consumption for men and women, although the same study found that women’s daily fruit and vegetable consumption was higher in areas with more billboards advertising soft drinks.39 However, two fair studies did not find this translated to an association with health outcomes.60 69 One did not find an association between fruit and vegetable advertising or ultraprocessed food advertising within food retail locations situated in each neighbourhood and overweight.60 The other did not find an association between unhealthy food advertising and obesity. Two good studies found that provincial school policies were important factors for modelling prevalence of childhood obesity.64 65
Neighbourhood vendor and product properties
Two cross-sectional studies examined vendor and product properties at the neighbourhood level. One good study found that the quality of vegetables in commercial establishments was associated with higher consumption of fruit and vegetables,42 while one fair study found that the quality of fruit and vegetables on offer in local food retail outlets was not associated with overweight.60
Neighbourhood affordability
Affordability was examined at the neighbourhood level in two studies both of which found an association with dietary outcomes. One good study found that combined fruit and vegetable intake decreased as the relative cost of two servings of fruits and three servings of vegetables per day increased in communities across 15 LMIC.83 One fair study found that participants perception of affordability (the answer to ‘I can buy FV even when they are expensive’) was associated with fruit and vegetable intake.77
Neighbourhood convenience
Three cross-sectional studies examined convenience characteristics all of which found an association between convenience and dietary outcomes. In one good study, a convenience variable examined the number of food items purchased at supermarkets and found that an increase was associated with an increase in calorie acquisition from ultraprocessed foods and beverages. Responses to ‘I have time to prepare and eat’ and ‘Fruit and vegetables are easy to prepare for me’ were associated with higher fruit and veg consumption in one fair study.77 One poor study found refrigerator ownership is positively correlated with dietary variety.47
Neighbourhood desirability
Two cross-sectional studies examined desirability at the neighbourhood level, one good and one fair, both of which found an association with diet.73 78
School availability
Fourteen observational studies examined an association between a school food environment characteristics and diet, nutrition or health outcome, 1 case–control study and 13 cross-sectional studies.
One poor case–control study36 found that availability was associated with health outcomes. Ten cross-sectional studies examined the association between availability and an outcome of interest. Three good cross-sectional studies84–86 and two fair cross-sectional studies87 88 found an association between an availability characteristic and a health outcome.
One good study found an association between availability and dietary outcomes89 with two additional fair studies that found an association with a dietary outcome.30 31 However, one good study did not find an association between availability (presence of a school canteen) and dietary behaviour (unhealthy snacking).90
School marketing and regulation
The second most common aspect of the school environment studied was marketing and regulation, investigated by three good studies. One found an association between presence of a school fruit and vegetable policy and fruit and vegetable consumption across schools from 24 countries,91 however, another found no association between the schools status as part of the Iranian Health Promoting Schools programme and unhealthy snacking behaviour.90 The third study found no association between school food policy and BMI.85
School vendor and product properties
One fair study examining vendor and product properties was looking specifically at vendor properties, finding that students of schools that offered meals prepared on the premises had lower prevalence of obesity than those who studied where meals were not offered (summarised under availability above). However, where the food was commercialised, obesity prevalence was significantly higher than where there was no commercialisation of foods with a similar association with prevalence of hypertension.87
School accessibility
Two good cross-sectional studies examined accessibility. One found an association with a dietary outcome90 while the other found no association.28
School desirability
Three studies investigated desirability. Two examined associations with diet: One good study found the social norms pressure was associated with unhealthy snacking90 and one good study found an association between ‘preferences’ and vegetable intake. One poor study found peer influence was associated with a health outcome: overweight.88
Other school environment
Finally, there was one poor study of the school food environment in which we were unable to categorise the characteristics investigated as the methodology simply stated that the researchers used 10 questions to collect data on school environment without giving details of the questions.92 This study reported no association between the ‘school environment’ and BMI.
Workplace environment
A single cross-sectional study examined the workplace food environment and dietary outcomes.29 The study found no association between workplace policy (‘Marketing and Regulation’) or the attitude of management (considered part of workplace ‘culture’ and therefore classified as ‘Desirability’) and eating practices across 26 factories. However, they did find an association between workplace nutrition environment (‘Availability’ and ‘Marketing and Regulation’) and individual worker attitude and dietary behaviour suggesting that the more supportive workplace nutrition environment alongside a positive individual attitude to health, the less frequently unhealthy food is consumed.
Home environment
Finally, three cross-sectional studies examined the home food environment. Two good studies found that accessibility and desirability elements were associated with dietary behaviour in adolescents.28 93 One of these additionally found that convenience was associated with dietary behaviour.28 Desirability was also associated with obesity in adolescents in one poor study, as was availability.94
Effects reported in the literature
All of the interventional studies identified were complex interventions with more than one element, sometimes multiple elements altering more than one characteristic of the food environment, and sometimes additional elements which did not target the food environment (eg, educational components). One fair95 and one poor quality study96 evaluating school interventions with elements of availability, marketing and regulation, and desirability found that these improved diet, nutrition and/or health.
Four studies examined school interventions with elements of availability and/or marketing and regulation without desirability elements. One fair97 and one poor-quality study98 found no effect on diet and/or nutrition of these interventions, while similar interventions were found to have an effect on health in one fair quality study,33 and on health but not diet in an additional fair quality study (table 6).99
A study of an intervention which included a marketing and regulation approach, among other elements, in a workplace found that this had a beneficial effect on health (table 6).100
Discussion
This review identified 74 studies including data from 29 countries, investigating the association between food environment characteristics and diet, nutrition and health outcomes in LMICs. All the intervention studies identified were carried out in upper-middle-income countries, observational studies also covered lower-middle and low-income countries (three countries included within multicountry studies). With the great majority of evidence coming from middle-income countries, it is worth considering the extent to which the findings can be generalised to low-income countries. The strongest recommendations from this review arise from the consistent evidence identified (14 studies, 10 of which were rated as good quality) of an association between availability characteristics in the neighbourhood food environment and dietary behaviour, as well as a balance of evidence suggesting an association with health or nutrition outcomes (17 out of 24 relevant studies). This suggests that interventions to increase the availability of healthy food options at the neighbourhood level, or to decrease the availability of unhealthy food are promising and worth investigating. It might be that availability of healthy and unhealthy food options in the neighbourhood is more important in LMIC than in some HIC, as a recent review on this topic focused on the USA and Canada only, included 71 studies and found that associations between food outlet availability and obesity were predominantly null.11 However, they did also find some patterns in the non-null studies suggesting an association between certain food outlets and adult obesity, and more recent studies (including longitudinal studies) support an association between availability and relevant outcomes.101 102 If there is a difference between HIC and LMIC settings, it may be due to differences in socioeconomics factors as well as mobility (due to ownership of motorised vehicles or efficient public transport) which makes it easier to access food outside the neighbourhood local to an individual’s residence in HIC than LMIC. No interventional study examining this element of the neighbourhood food environment relevant to urban LMIC settings was identified by our search. Interventions that have been implemented in HIC include ‘zoning powers’ given to local authorities to enable them to control the food environment through regulating land use—for example, limiting certain food outlets from trading in specific areas. In addition, ‘healthy food carts’ have been used to increase availability to healthy food in deprived urban neighbourhoods with some success.103 Therefore, a key implication for research and policy would be to begin to implement and evaluate similar interventions in LMIC.
We also found a balance of evidence that accessibility to food in the neighbourhood environment was associated with diet (10 out of 11 studies) although there was no evidence of an association with nutrition outcomes and the evidence of an association with health outcomes was contradictory. Again, we did not identify any interventional studies focused on this element of the neighbourhood food environment and would suggest that there is enough evidence that this may be promising and worth further investigation. Interventions are likely to be similar to those addressing availability (eg, ‘zoning’ and ‘healthy food carts’) but could also include increasing accessibility to healthy food outlets, for example, by rerouting public transport links.
Evidence on vendor and product properties, price, and marketing and regulation at the neighbourhood level was sparse and mixed; while evidence on affordability examined at the neighbourhood level was sparse but consistent, two studies both found an association with dietary outcomes. Literature from HIC does support affordability as important for driving dietary and health outcomes, for example, in quantitative studies104 and reported by participants in the qualitative literature.13 Further research is recommended to expand the evidence base on the association between these aspects of the neighbourhood food environment and diet, nutrition and health outcomes.
In keeping with the neighbourhood-level results, 12 observational studies examining availability elements in the school food environment and relevant outcomes found a balance of evidence in favour of an association. Twelve studies consistently identified an association between availability and a health outcome, three out of four studies reported an association between availability and a dietary outcome. The second most common aspect of the school food environment studied was marketing and regulation, investigated by three good studies, but with conflicting findings. Studies investigating our other primary outcomes in observational studies of the school food environment were sparse. We also identified six studies evaluating interventions in the school food environment. All the interventions studied were complex consisting of multiple elements. Two studies that evaluated interventions with elements of availability, marketing and regulation, and desirability found that these improved relevant outcomes whereas four studies investigating similar interventions without desirability elements had mixed results. A systematic review and meta-analysis of school food environment policies identified 91 interventions from the USA, Canada, Europe and New Zealand. This study reported that direct provision of healthy food and drinks (ie, availability interventions) were able to improve some dietary behaviours as were implementation of food, beverage or meal standards (ie, marketing and regulation intervention) although there were mixed findings on health and nutrition outcomes.14 A meta-analysis of six studies investigating multicomponent behavioural and environmental interventions in schools in LMIC suggested an overall effect on change in BMI, whereas meta-analysis of five studies which examined BMI found no observed effect.105 Certainly our findings suggest that further research is needed, but it is also likely that interventions to increase availability of healthy food or to reduce availability of unhealthy food in schools would have a beneficial effect on diets, with the effect on health requiring further investigation.
We found very little evidence from either observational or intervention studies on how workplace food environments and the home food environments are associated with health, diet or nutrition outcomes. This is a substantial evidence gap.
Although we rated many identified studies as ‘good’, the majority of observational studies did take a cross-sectional approach, so due to study design there are inherent weaknesses, even if they were well conducted. Future studies with longitudinal designs, and more controlled intervention studies (including cluster randomised designs) would provide stronger evidence to support future policy decisions.
We used a framework developed through a series of iterative, international congregations with experts in nutrition and public health.16 However, our own research team did not feel that the ‘convenience’ and ‘desirability’ concepts mapped well to our own concept of the food environment. Although we have synthesised evidence on convenience and desirability elements in the papers identified, we did not prioritise papers focused on these elements for inclusion so cannot draw strong conclusions. However, at the neighbourhood level both convenience and desirability characteristics were consistently associated with relevant outcomes in six included observational studies, and in school and home food environments a consistent association was seen between desirability and relevant outcomes. Further, two school food environment interventions with elements of desirability have a beneficial effect on outcomes. This does suggest that it might be worth considering desirability as a future target for intervention, suggesting an important role of the social environment on diet, nutrition and health outcomes in LMIC populations.
The major strength of this study is the rigorous systematic approach to identifying literature, including a search strategy developed with an academic librarian and careful reference screening of all included studies. The chances of reviewing bias are low because we did not limit by language and although we limited by year (to studies published from the year 2000 onwards) the earliest published study we found was published in 2010 so we are unlikely to have missed many earlier studies. The sensitivity of our approach is clear as we have identified more than thrice the number of articles of a recent scoping review on this topic.25 We conducted selection of studies in duplicate by two independent reviewers, with data extraction and quality appraisal conducted by one reviewer and checked by a second, which will have improved the reliability of the data synthesised.
In conclusion, interventions that increase the availability of healthy food and/or decrease the availability of unhealthy food are promising and are likely to have beneficial effects on dietary behaviour and healthy of LMIC populations and there is enough evidence to justify policy and practice implementation on this theme, with evaluation of the outcomes alongside these if possible. More longitudinal and interventional studies are required to inform further recommendations, with affordability and the social environment potentially interesting and worthwhile avenues to pursue.
Acknowledgments
OO, RI and AI are supported by the UK’s National Institute of Health Research (NIHR) Global Health Research Unit on Improving Health in Slums. LA-K is supported by the NIHR Applied Research Centre-West Midlands. DM is supported by a University of Warwick Chancellor’s International Scholarship. The authors wish to acknowledge support from Samantha Johnson, academic librarian at University of Warwick, on developing the search strategy. The authors wish to acknowledge Dr. Yen-Fu Chen, associate professor at University of Warwick, for screening a study in Chinese.
Footnotes
Handling editor: Seye Abimbola
Contributors: OO and SW conceived and designed the study. SW ran the searches. SW, IG, HMJ, DM, NA, LA-K and OO screened titles and abstracts. SW, IG, AI, HMJ, DM, NA, RI and OO screened full texts. SW, IG, HMJ, FS, AI and OO extracted data from and quality appraised included studies. SW and OO checked the data extraction. SW and OO drafted the manuscript. All authors contributed to the final manuscript.
Funding: OO, RI and AI are supported by the NIHR Global Health Research Unit on Improving Health in Slums.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study. This systematic review examines data that is available in the published literature.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Afshin A, Sur PJ, Fay KA, et al. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet 2019;393:1958–72. 10.1016/S0140-6736(19)30041-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaziano TA. Cardiovascular disease in the developing world and its cost-effective management. Circulation 2005;112:3547–53. 10.1161/CIRCULATIONAHA.105.591792 [DOI] [PubMed] [Google Scholar]
- 3.Engelgau M, Rosenhouse S, El-Saharty S, et al. The economic effect of noncommunicable diseases on households and nations: a review of existing evidence. J Health Commun 2011;16 Suppl 2:75–81. 10.1080/10810730.2011.601394 [DOI] [PubMed] [Google Scholar]
- 4.World Health Organisation . Global status report on noncommunicable diseases 2010. Chapter 2: NCDs and development. Geneva: World Health Organisation; 2011: 8. [Google Scholar]
- 5.World Health Organisation . Global status report on noncommunicable diseases 2010. NCDs and development 2011; Chapter 2.
- 6.Calder P, Carr A, Gombart A. Optimal nutritional status for a Well-Functioning immune system is an important factor to protect against viral infections. Nutrients 2020;12:1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maggini S, Pierre A, Calder PC. Immune function and micronutrient requirements change over the life course. Nutrients 2018;10:1531. 10.3390/nu10101531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swinburn B, Sacks G, Vandevijvere S, et al. INFORMAS (international network for food and Obesity/non-communicable diseases research, monitoring and action support): overview and key principles. Obes Rev 2013;14 Suppl 1:1–12. 10.1111/obr.12087 [DOI] [PubMed] [Google Scholar]
- 9.Engler-Stringer R, Le H, Gerrard A, et al. The community and consumer food environment and children's diet: a systematic review. BMC Public Health 2014;14:522. 10.1186/1471-2458-14-522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams J. Scarborough P Fau - Matthews A, Matthews A Fau - Cowburn G, et al. A systematic review of the influence of the retail food environment around schools on obesity-related outcomes. Obes Rev 2014;15:359–74. [DOI] [PubMed] [Google Scholar]
- 11.Cobb LK, Appel LJ, Franco M, et al. The relationship of the local food environment with obesity: a systematic review of methods, study quality, and results. Obesity 2015;23:1331–44. 10.1002/oby.21118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caspi CE, Sorensen G, Subramanian SV, et al. The local food environment and diet: a systematic review. Health Place 2012;18:1172–87. 10.1016/j.healthplace.2012.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pitt E, Gallegos D, Comans T, et al. Exploring the influence of local food environments on food behaviours: a systematic review of qualitative literature. Public Health Nutr 2017;20:2393–405. 10.1017/S1368980017001069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Micha R, Karageorgou D, Bakogianni I, et al. Effectiveness of school food environment policies on children's dietary behaviors: a systematic review and meta-analysis. PLoS One 2018;13:e0194555. 10.1371/journal.pone.0194555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sisnowski J, Street JM, Merlin T. Improving food environments and tackling obesity: a realist systematic review of the policy success of regulatory interventions targeting population nutrition. PLoS One 2017;12:e0182581. 10.1371/journal.pone.0182581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Turner C, Aggarwal A, Walls H. Concepts and critical perspectives for food environment research: a global framework with implications for action in low- and middle-income countries. Glob Food Sec 2018;18:93–101. [Google Scholar]
- 17.United Nations . World urbanization prospects: the 2018 revision: population division of the United nations department of economic and social Affairs (un DESA); 2018: 126.
- 18.Vilar-Compte M, Burrola-Méndez S, Lozano-Marrufo A, et al. Urban poverty and nutrition challenges associated with accessibility to a healthy diet: a global systematic literature review. Int J Equity Health 2021;20:40. 10.1186/s12939-020-01330-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet 2014;384:766–81. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong MCS, Huang J, Wang J, et al. Global, regional and time-trend prevalence of central obesity: a systematic review and meta-analysis of 13.2 million subjects. Eur J Epidemiol 2020;35:673–83. 10.1007/s10654-020-00650-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Angkurawaranon C, Jiraporncharoen W, Chenthanakij B, et al. Urban environments and obesity in Southeast Asia: a systematic review, meta-analysis and meta-regression. PLoS One 2014;9:e113547. 10.1371/journal.pone.0113547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mensah DO, Nunes AR, Bockarie T. Meat, fruit, and vegetable consumption in sub-Saharan Africa: a systematic review and meta-regression analysis. Nutrition Reviews 2020. [DOI] [PubMed] [Google Scholar]
- 23.Oyebode O, Oti S, Chen Y-F, et al. Salt intakes in sub-Saharan Africa: a systematic review and meta-regression. Popul Health Metr 2016;14:1. 10.1186/s12963-015-0068-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pan American Health Organization . Ultra-processed food and drink products in Latin America: sales, sources, nutrient profiles, and policy implications: pan American health organization (PAHO) 2019;72. [Google Scholar]
- 25.Turner C, Kalamatianou S, Drewnowski A, et al. Food environment research in low- and middle-income countries: a systematic scoping review. Adv Nutr 2020;11:387–97. 10.1093/advances/nmz031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Westbury S, Oyebode O. The influence of the urban food environment on diet, nutrition, and health outcomes in low and middle-income countries: a systematic review, 2020. Available: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020207475 [DOI] [PMC free article] [PubMed]
- 27.Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 2021;372:n160. 10.1136/bmj.n160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ochoa-Meza G, Sierra JC, Pérez-Rodrigo C. Factores psicosociales del consumo de verduras en niños escolarizados mexicanos de poblaciones urbanas Y semi-urbanas. Rev Iberoam de Psicol y Salud 2017;8:108–20. [Google Scholar]
- 29.Charoenbut P, Klaewkla J, Srisorrachatr S. Workplace and individual factors influence eating practices of Thai factory workers. Malays J Nut 2018;24:417–26. [Google Scholar]
- 30.Bekker F, Marais M, Koen N. The provision of healthy food in a school tuck shop: does it influence primary-school students' perceptions, attitudes and behaviours towards healthy eating? Public Health Nutr 2017;20:1257–66. 10.1017/S1368980016003487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fernandes M, Folson G, Aurino E, et al. A free lunch or a walk back home? the school food environment and dietary behaviours among children and adolescents in Ghana. Food Secur 2017;9:1073–90. 10.1007/s12571-017-0712-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wertheim-Heck SCO, Raneri JE. A cross-disciplinary mixed-method approach to understand how food retail environment transformations influence food choice and intake among the urban poor: experiences from Vietnam. Appetite 2019;142:N.PAG-N.PAG. 10.1016/j.appet.2019.104370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shamah Levy T, Morales Ruán C, Amaya Castellanos C, et al. Effectiveness of a diet and physical activity promotion strategy on the prevention of obesity in Mexican school children. BMC Public Health 2012;12:152–52. 10.1186/1471-2458-12-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang R, Shi L. Access to food outlets and children's nutritional intake in urban China: a difference-in-difference analysis. Ital J Pediatr 2012;38:30. 10.1186/1824-7288-38-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu H, Short SE, Liu T. Dynamic relations between fast-food restaurant and body weight status: a longitudinal and multilevel analysis of Chinese adults. J Epidemiol Community Health 2013;67:271–9. 10.1136/jech-2012-201157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Setiyaningsih R, Dewi YLR, Adriani RB. Contextual effect of school on the risk obesity among high school students in Surakarta, central Java: a multilevel analysis evidence. J Epidemiology Public Health 2019;4:328–37. [Google Scholar]
- 37.Curioni CC, Boclin KLS, Silveira IH, et al. Neighborhood food environment and consumption of fruit and leafy vegetables: Pro-Saude study, Brazil. Public Health 2020;182:7–12. 10.1016/j.puhe.2020.01.004 [DOI] [PubMed] [Google Scholar]
- 38.Duran AC, de Almeida SL, Latorre MdoRDO, MdRDO L, et al. The role of the local retail food environment in fruit, vegetable and sugar-sweetened beverage consumption in Brazil. Public Health Nutr 2016;19:1093–102. 10.1017/S1368980015001524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goryakin Y, Rocco L, Suhrcke M, et al. Fruit and vegetable consumption in the former Soviet Union: the role of individual- and community-level factors. Public Health Nutr 2015;18:2825–35. 10.1017/S1368980015000105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jaime PC, Duran AC, Sarti FM, et al. Investigating environmental determinants of diet, physical activity, and overweight among adults in Sao Paulo, Brazil. J Urban Health 2011;88:567–81. 10.1007/s11524-010-9537-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leite FHM, de Carvalho Cremm E, de Abreu DSC, et al. Association of neighbourhood food availability with the consumption of processed and ultra-processed food products by children in a city of Brazil: a multilevel analysis. Public Health Nutr 2018;21:189–200. 10.1017/S136898001600361X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mendonça RdeD, Lopes MS, Freitas PP, et al. Monotony in the consumption of fruits and vegetables and food environment characteristics. Rev Saude Publica 2019;53:63. 10.11606/S1518-8787.2019053000705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Menezes MCde, Diez Roux AV, Costa BVdeL, et al. Individual and food environmental factors: association with diet. Public Health Nutr 2018;21:2782–92. 10.1017/S1368980018001623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nogueira L, Fontanelli M, Aguiar B, et al. Access to street markets and consumption of fruits and vegetables by adolescents living in São Paulo, Brazil. Int J Environ Res Public Health 2018;15:517. 10.3390/ijerph15030517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Opal P, Safraj S, Roopa S. Association between full service and fast food restaurant density, dietary intake and overweight/obesity among adults in Delhi, India. BMC Public Health 2018;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pessoa MC, Mendes LL, Gomes CS, et al. Food environment and fruit and vegetable intake in a urban population: a multilevel analysis. BMC Public Health 2015;15:1012. 10.1186/s12889-015-2277-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu J, Shively GE, Binkley JK. Access to variety contributes to dietary diversity in China. Food Policy 2014;49:323–31. [Google Scholar]
- 48.Kroll F, Swart EC, Annan RA. Mapping obesogenic food environments in South Africa and Ghana: correlations and contradictions. Sustainability 2019;11:31. [Google Scholar]
- 49.Zhang X, van der Lans I, Dagevos H. Impacts of fast food and the food retail environment on overweight and obesity in China: a multilevel latent class cluster approach. Public Health Nutr 2012;15:88–96. 10.1017/S1368980011002047 [DOI] [PubMed] [Google Scholar]
- 50.Assis MMde, Leite MA, Carmo ASdo, et al. Food environment, social deprivation and obesity among students from Brazilian public schools. Public Health Nutr 2019;22:1920–7. 10.1017/S136898001800112X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Backes V, Bairros F, Cafruni CB, et al. Food environment, income and obesity: a multilevel analysis of a reality of women in southern Brazil. Cad Saude Publica 2019;35:e00144618. 10.1590/0102-311X00144618 [DOI] [PubMed] [Google Scholar]
- 52.Corrêa E, Rossi CE, das Neves J. Utilization and environmental availability of food outlets and overweight/obesity among schoolchildren in a City in the South of Brazil. J Public Health 2018;40:106–13. [DOI] [PubMed] [Google Scholar]
- 53.Cunningham-Myrie CA, Younger NO, Theall KP, et al. Understanding neighbourhood retail food environmental mechanisms influencing BMI in the Caribbean: a multilevel analysis from the Jamaica health and lifestyle survey: a cross-sectional study. BMJ Open 2020;10:e033839. 10.1136/bmjopen-2019-033839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dake FAA, Thompson AL, Ng SW, et al. The local food environment and body mass index among the urban poor in Accra, Ghana. J Urban Health 2016;93:438–55. 10.1007/s11524-016-0044-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hall BJ, Huang L, Yi G. Fast food restaurant density and weight status: A spatial analysis among Filipina migrant workers in Macao (SAR), People’s Republic of China. Soc Sci Med 2020. [DOI] [PubMed] [Google Scholar]
- 56.Matozinhos FP, Gomes CS, Andrade ACdeS, et al. Neighbourhood environments and obesity among adults: a multilevel analysis of an urban Brazilian context. Prev Med Rep 2015;2:337–41. 10.1016/j.pmedr.2015.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nogueira LR, Fontanelli MdeM, Aguiar BSde, et al. Is the local food environment associated with excess body weight in adolescents in São Paulo, Brazil? Cad Saude Publica 2020;36:e00048619. 10.1590/0102-311x00048619 [DOI] [PubMed] [Google Scholar]
- 58.Zhang X, Zhang M, Zhao ZP. Obesogenic environmental factors of adult obesity in China: a nationally representative cross-sectional study. Environ Res Lett 2020;15:13. [Google Scholar]
- 59.Zhou M, Tan SK, Tao YH. Neighborhood socioeconomics, food environment and land use determinants of public health: isolating the relative importance for essential policy insights. Land Use Policy 2017;68:246–53. [Google Scholar]
- 60.de Freitas PP, de Menezes MC, Lopes ACS. Consumer food environment and overweight. Nutrition 2019;66((de Freitas) University of Minas Gerais, Research Group in Nutrition Interventions of University of Minas Gerais, Belo Horizonte, MG, Brazil(de Menezes) Fiocruz, Research Group in Nutrition Interventions of University of Minas Gerais, Belo Horizonte, MG):108–14.
- 61.Trinh HT, Dhar BD, Simioni M. Supermarkets and household food acquisition patterns in Vietnam in relation to population demographics and socioeconomic strata: insights from public data. Front sustain food syst 2020;4:12. [Google Scholar]
- 62.Camargo DFM, Belon AP, Marín-León L, et al. Comparing food environment and food purchase in areas with low and high prevalence of obesity: data from a mapping, in-store audit, and population-based survey. Cad Saude Publica 2019;35:e00247218. 10.1590/0102-311X00247218 [DOI] [PubMed] [Google Scholar]
- 63.Hua J, Seto E, Li Y, et al. Development and evaluation of a food environment survey in three urban environments of Kunming, China. BMC Public Health 2014;14:235–35. 10.1186/1471-2458-14-235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Guo CL, Zhang B, Wang HJ, et al. A scan of obesogenic environments and a spatial inference of obesity prevalence in Chinese children and adolescents: based on the Chinese health and nutrition survey 2011 data. Biomed Environ Sci 2018;31:729–39. 10.3967/bes2018.098 [DOI] [PubMed] [Google Scholar]
- 65.Guo C, Wang H, Feng G, et al. Spatiotemporal predictions of obesity prevalence in Chinese children and adolescents: based on analyses of obesogenic environmental variability and Bayesian model. Int J Obes 2019;43:1380–90. 10.1038/s41366-018-0301-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Silva FMOda, Novaes TG, Ribeiro AQ, et al. [Environmental factors associated with obesity in the adult population in a medium-sized Brazilian city]. Cad Saude Publica 2019;35:e00119618. 10.1590/0102-311X00119618 [DOI] [PubMed] [Google Scholar]
- 67.Mendes LL, Nogueira H, Padez C, et al. Individual and environmental factors associated for overweight in urban population of Brazil. BMC Public Health 2013;13:988–88. 10.1186/1471-2458-13-988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Velásquez-Meléndez G, Mendes LL, Padez CMP. Built environment and social environment: associations with overweight and obesity in a sample of Brazilian adults. Cadernos de Saúde Pública 2013;29:1988–96. [DOI] [PubMed] [Google Scholar]
- 69.Watson K, Roberts B, Chow C, et al. Micro- and meso-level influences on obesity in the former Soviet Union: a multi-level analysis. Eur J Public Health 2013;23:291–8. 10.1093/eurpub/cks054 [DOI] [PubMed] [Google Scholar]
- 70.Kelly M, Seubsman SA, Banwell C. Thailand’s food retail transition: supermarket and fresh market effects on diet quality and health. Br Food J 2014;116:1180–93. [Google Scholar]
- 71.Seto E, Hua J, Wu L, et al. Models of individual dietary behavior based on smartphone data: the influence of routine, physical activity, emotion, and food environment. PLoS One 2016;11:e0153085. 10.1371/journal.pone.0153085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chor D, Cardoso LO, Nobre AA. Association between perceived neighbourhood characteristics, physical activity and diet quality: results of the Brazilian longitudinal study of adult health (ELSA-Brasil). BMC Public Health 2016;16:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kivuyo Nengilang'et G, Sharma S. Dietary acculturation among African emigrant students in India: determinants and problems. Public Health Nutr 2020;23:2402–9. 10.1017/S1368980019005226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liu Y, Gittelsohn J, Thorne-Lyman AL. Caregiver perceptions of the neighborhood food environment and their relationship with the home food environment and childhood obesity in Northeast China. Appetite 2020;144((Liu, Wen) Institute of Health Science, China Medical University, Shenyang, Liaoning, China(Gittelsohn, Thorne-Lyman, Orta-Aleman) Department of International Health, Center for Human Nutrition, Johns Hopkins Bloomberg School of Public Health, Baltimore):104447. [DOI] [PubMed]
- 75.Vedovato GM, Trude ACB, Kharmats AY, et al. Degree of food processing of household acquisition patterns in a Brazilian urban area is related to food buying preferences and perceived food environment. Appetite 2015;87:296–302. 10.1016/j.appet.2014.12.229 [DOI] [PubMed] [Google Scholar]
- 76.MdA A, Pinho MGM, Correa EN. Parental Perceived Travel Time to and Reported Use of Food Retailers in Association with School Children’s Dietary Patterns. Int J Environ Res Public Health 2019;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Menezes MCde, Diez Roux AV, Souza Lopes AC. Fruit and vegetable intake: influence of perceived food environment and self-efficacy. Appetite 2018;127:249–56. 10.1016/j.appet.2018.05.011 [DOI] [PubMed] [Google Scholar]
- 78.Zuccolotto DCC, Barbieri P, Sartorelli DS. Food environment and family support in relation to fruit and vegetable intake in pregnant women. Archivos Latinoamericanos de Nutrición 2015;65:216–24. [Google Scholar]
- 79.Oyeyemi AL, Adegoke BO, Oyeyemi AY, et al. Environmental factors associated with overweight among adults in Nigeria. Int J Behav Nutr Phys Act 2012;9:32. 10.1186/1479-5868-9-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang J, Xue H, Cheng X, et al. Influence of proximities to food establishments on body mass index among children in China. Asia Pac J Clin Nutr 2016;25:134–41. 10.6133/apjcn.2016.25.1.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rossi CE, Patrícia de Fragas H, Corrêa EN, et al. Association between food, physical activity, and social assistance environments and the body mass index of schoolchildren from different socioeconomic strata. J Public Health 2019;41:e25–34. 10.1093/pubmed/fdy086 [DOI] [PubMed] [Google Scholar]
- 82.Machado PP, Claro RM, Canella DS, et al. Price and convenience: the influence of supermarkets on consumption of ultra-processed foods and beverages in Brazil. Appetite 2017;116:381–8. 10.1016/j.appet.2017.05.027 [DOI] [PubMed] [Google Scholar]
- 83.Miller V, Yusuf S, Chow CK, et al. Availability, affordability, and consumption of fruits and vegetables in 18 countries across income levels: findings from the prospective urban rural epidemiology (pure) study. Lancet Glob Health 2016;4:e695–703. 10.1016/S2214-109X(16)30186-3 [DOI] [PubMed] [Google Scholar]
- 84.Barrera LH, Rothenberg SJ, Barquera S, et al. The toxic food environment around elementary schools and childhood obesity in Mexican cities. Am J Prev Med 2016;51:264–70. 10.1016/j.amepre.2016.02.021 [DOI] [PubMed] [Google Scholar]
- 85.Li M, Dibley MJ, Yan H. School environment factors were associated with BMI among adolescents in Xi'an City, China. BMC Public Health 2011;11:792. 10.1186/1471-2458-11-792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhou S, Cheng Y, Cheng L. Association between convenience stores near schools and obesity among school-aged children in Beijing, China. BMC Public Health 2020;20:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gonçalves VS, Duarte EC, Dutra ES, et al. Characteristics of the school food environment associated with hypertension and obesity in Brazilian adolescents: a multilevel analysis of the study of cardiovascular risks in adolescents (Erica). Public Health Nutr 2019;22:2625–34. 10.1017/S1368980019001010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Widiyanto A, Murti B, Soemanto RB. Multilevel analysis on the Socio-Cultural, lifestyle factors, and school environment on the risk of overweight in adolescents, Karanganyar district, central Java. J Epidemiology Public Health 2018;3:94–104. [Google Scholar]
- 89.Azeredo CM, de Rezende LFM, Canella DS, et al. Food environments in schools and in the immediate vicinity are associated with unhealthy food consumption among Brazilian adolescents. Prev Med 2016;88:73–9. 10.1016/j.ypmed.2016.03.026 [DOI] [PubMed] [Google Scholar]
- 90.Yazdi Feyzabadi V, Keshavarz Mohammadi N, Omidvar N, et al. Factors associated with unhealthy snacks consumption among adolescents in Iran's schools. Int J Health Policy Manag 2017;6:519–28. 10.15171/ijhpm.2017.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Darfour-Oduro SA, Andrade JE, Grigsby-Toussaint DS. Do fruit and vegetable policies, Socio-Environmental factors, and physical activity influence fruit and vegetable intake among adolescents? J Adolesc Health 2020;66:172–80. 10.1016/j.jadohealth.2019.07.016 [DOI] [PubMed] [Google Scholar]
- 92.Norbu W, Wangdi U, Dorji D. Obesity prevalence and contributing factors among adolescents in secondary schools in Pemagatshel district, Bhutan. Int J Adolesc Med Health 2019;31. [DOI] [PubMed] [Google Scholar]
- 93.Leme ACB, Philippi ST. Home food availability, parents'/caregivers' support, and family meals influence on dietary servings of low-income urban adolescent girls from Brazil. Nutrire 2017;42. [Google Scholar]
- 94.Zheng Y, Guo H, Xie X. A population-based study of obesity and its complications in children and adolescents. Int Medical J 2013;20:691–5. [Google Scholar]
- 95.Safdie M, Jennings-Aburto N, Lévesque L, et al. Impact of a school-based intervention program on obesity risk factors in Mexican children. Salud Publica Mex 2013;55 Suppl 3:374–87. 10.21149/spm.v55s3.5138 [DOI] [PubMed] [Google Scholar]
- 96.Aghdam FB, Nadrian H, Sheikhsamani M. School food environment promotion program: applying the socio-ecological approach. Int J Pediatr 2018;6:6878–90. [Google Scholar]
- 97.Yazdi-Feyzabadi V, Omidvar N, Keshavarz Mohammadi N, et al. Is an Iranian health promoting school status associated with improving school food environment and snacking behaviors in adolescents? Health Promot Int 2018;33:1010–21. 10.1093/heapro/dax045 [DOI] [PubMed] [Google Scholar]
- 98.Steyn NP, de Villiers A, Gwebushe N, et al. Did HealthKick, a randomised controlled trial primary school nutrition intervention improve dietary quality of children in low-income settings in South Africa? BMC Public Health 2015;15:1–11. 10.1186/s12889-015-2282-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chawla N, Panza A, Sirikulchayanonta C, et al. Effectiveness of a school-based multicomponent intervention on nutritional status among primary school children in Bangkok, Thailand. J Ayub Med Coll Abbottabad 2017;29:13–20. [PubMed] [Google Scholar]
- 100.Bandoni DH, Sarno F, Jaime PC. Impact of an intervention on the availability and consumption of fruits and vegetables in the workplace. Public Health Nutr 2011;14:975–81. 10.1017/S1368980010003460 [DOI] [PubMed] [Google Scholar]
- 101.Kelman J, Pool LR, Gordon-Larsen P, et al. Associations of unhealthy food environment with the development of coronary artery calcification: the cardia study. J Am Heart Assoc 2019;8:e010586. 10.1161/JAHA.118.010586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bivoltsis A, Trapp G, Knuiman M, et al. The influence of the local food environment on diet following residential relocation: longitudinal results from residential environments (reside). Public Health Nutr 2020;23:2132–44. 10.1017/S1368980019005111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hsiao B-S, Sibeko L, Troy LM. A systematic review of mobile produce markets: facilitators and barriers to use, and associations with reported fruit and vegetable intake. J Acad Nutr Diet 2019;119:76–97. 10.1016/j.jand.2018.02.022 [DOI] [PubMed] [Google Scholar]
- 104.Ferretti F, Mariani M. Sugar-Sweetened beverage affordability and the prevalence of overweight and obesity in a cross section of countries. Global Health 2019;15:30. 10.1186/s12992-019-0474-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Carducci B, Oh C, Keats EC, et al. Effect of food environment interventions on anthropometric outcomes in school-aged children and adolescents in low- and middle-income countries: a systematic review and meta-analysis. Curr Dev Nutr 2020;4:nzaa098. 10.1093/cdn/nzaa098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.The World Bank . Data: world bank country and lending groups, 2020. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [Accessed 14 Sep 2020].
- 107.Wijnhoven TMA, van Raaij JMA, Sjöberg A, et al. WHO European childhood obesity surveillance initiative: school nutrition environment and body mass index in primary schools. Int J Environ Res Public Health 2014;11:11261–85. 10.3390/ijerph111111261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bonvecchio-Arenas A, Theodore FL, Hernández-Cordero S. La escuela como alternativa en La prevención de la obesidad: La experiencia en El sistema escolar mexicano. Revista Española de Nutrición Comunitaria 2010;16:13–16. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-006358supp001.pdf (242.5KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study. This systematic review examines data that is available in the published literature.