Abstract
Objective: This study aimed to explore the application effect of clinical nursing pathway model in elderly patients with hypertension and cerebral infarction. Methods: A total of 106 elderly patients with hypertension and cerebral infarction were recruited and divided into a control group (n=51) and a test group (n=55). Both groups of patients received conventional care, and the test group was given additional care if clinical nursing pathway. The blood pressure indexes, knowledge of stroke, nursing satisfaction, neurological deficit, and activity of daily living (ADL) of the two groups of patients were observed. Results: After nursing care, the scores of Stroke Knowledge Questionnaire (SKQ) and Barthel index (BI) increased in both groups, and they were significantly higher in the test group than in the control group. The scores of systolic blood pressure (SBP), diastolic blood pressure (DBP) and National Institutes of Health Stroke Scale (NIHSS) decreased significantly in both groups after nursing, and they were lower in the test group than the control group. In addition, patients in the test group exhibited higher nursing satisfaction than the control group, as well as higher rates of blood pressure control at discharge, two months, four months and six months after discharge. Conclusion: The application of clinical nursing pathway can improve the disease cognition and quality of life of elderly patients with hypertension and cerebral infarction, and promote their recovery.
Keywords: Clinical nursing pathway, hypertension, cerebral infarction, quality of life
Introduction
The World Health Organization (WHO) has identified hypertension as one of the most important risk factors for morbidity and mortality worldwide, causing approximately 9 million deaths each year [1]. Hypertension, the main risk factor for cerebral infarction, is caused by a sudden decrease or cessation of blood flow in the local blood supply arteries, resulting in ischemia, hypoxia and tissue necrosis in the blood supply area [2]. Most patients with cerebral infarction will suffer from varying degrees of sensory, speech, motor and neurological deficits, which are irreversible in nature [3]. It will not only cause a serious reduction or loss of work capacity, but also bring a huge psychological burden, which seriously affects the quality of daily life [4]. The elderly people with hypertension and cerebral infarction are at a higher risk of disability and death, and the two diseases have become major public health problems endangering the health of the elderly [5]. Clinically, the disease usually requires active symptomatic treatment, but in the course of treatment, high-quality nursing intervention during the treatment is also extremely important [6].
Clinical nursing pathway is a standardized process and a nursing model based on the characteristics of the disease that can improve the patient’s compliance and rehabilitation effect, and the nursing staffs who provide this nursing model can reasonably arrange all nursing work under the standardized treatment and nursing process to avoid blindness [7]. Some previous studies have displayed the application of clinical nursing pathway in clinical work. For example, the team of Yang showed through a meta-analysis that the implementation of clinical nursing pathways in patients undergoing endoscopic thyroidectomy resulted in shortened length of stay, reduced hospital costs, and increased patient satisfaction [8]. According to the team of Zhang, the clinical nursing pathway can improve the overall nursing quality, shorten the hospitalization time, and reduce the occurrence of complications in patients undergoing percutaneous coronary intervention when compared to those receiving traditional nursing model [9]. Besides, it is supported that compared with traditional nursing, fast-track program can significantly shorten the postoperative hospital stay, with notably reduced medical expenses and postoperative complications [10]. Traditional nursing models are getting problems meeting the needs of most patients [11].
The application effect of clinical nursing pathway in elderly patients with hypertension and cerebral infarction is still unclear. In this study, we applied this nursing model to patients and discussed its application effect.
Materials and methods
Clinical data
A total of 106 cases of elderly patients with hypertension and cerebral infarction admitted to Wenling First People’s Hospital from March 2019 to March 2020 were recruited as research objects. This research was carried out with the approval of the Ethics Committee of Wenling First People’s Hospital. All the subjects and their families were informed and signed informed consent forms for the study. Inclusion criteria: patients aged 60 years and above; patients met the diagnostic criteria of hypertension of WHO and World Hypertension League [12], and were diagnosed as cerebral infarction by imaging [13]. Exclusion criteria: patients were complicated with severe dysfunction of heart, kidney or liver, secondary hypertension, malignant tumor, or mental illness.
Nursing methods
One hundred and six elderly patients with hypertension and cerebral infarction were recruited and divided into a control group (n=51) and a test group (n=55). Patients in both groups received conventional care. Things we nursing staff did included informing the attending physician to monitor the patient’s condition, performing medication checks and basic diagnostic and therapeutic aids, and explaining the condition and precautions to patients.
On this basis, patients in the test group were given clinical nursing pathway, and the measures were as follows:
Psychological nursing: we communicated with patients and their families in a gentle tone, evaluated their psychological stress, and asked for information about their cultural background and family support. The actual situation of each patient was assessed to formulate personalized health education to correct his/her bad habits in life, such as smoking and drinking, and to maintain a healthy lifestyle. We organized health knowledge lectures and interviewed patients and their families one by one, so as to encourage them to build up the confidence in correctly facing diseases.
Nutritional nursing: we controlled the diet of patients reasonably, assisted them to cultivate a good eating habit, and kept them from eating irritating food. We made recipes according to patients’ preferences. The diet was mainly high in cellulose and vitamins and low in cholesterol and fat, and the patient was asked to have more meals a day but less food at each, so that the stomach and intestines could fully absorb nutrients. For patients with severe dysphagia, we offered nasal feeding fluids to make sure of a reasonable nutritional supply.
Comfort nursing: we instructed the patients to keep comfortable body position and posture when they were in bed. The buccal mucosa of paralytic patients was cleaned, as well as the food left in the mouth. We helped the patients to turn over regularly, cleaned their skin, changed the sheets frequently, and kept them dry, so as to prevent pressure sores. For patients with indwelling catheter, nursing care of urinary catheter was strengthened, and the urinary catheter was cleaned regularly.
Rehabilitation nursing: patients were asked to do limb function exercises according to their own conditions. We assisted the patients with supplementary exercises until they were able to perform functional limb training on their own. We regularly massaged their muscles, instructed them to relax their shoulders and upper limbs until they felt no pain when passively lifted the joints. Their upper and lower limbs were also passively stretched. Patients were encouraged to sit up as soon as possible and keep their torso upright. After that, their exercises were gradually in transition to standing against the wall and standing balance training. Patients were assisted for walking training, with a cane-affected leg-healthy leg in sequence, and after stabilization, handrail walking could be done, followed by the transition to independent walking.
Continuing nursing: follow-up and exercise guidance were given to patients after their discharge, so that we could evaluate their health knowledge and guide them in self-care. According to the health status of patients, they were encouraged to do exercises such as walking and Tai Chi one hour after meals, and the exercise time was controlled at 30 min/d.
Outcome measures
The clinical data of patients was collected, and their blood pressure indexes were measured, including systolic blood pressure (SBP) and diastolic blood pressure (DBP). They were followed up with WeChat, text message and telephone.
(1) The Stroke Knowledge Questionnaire (SKQ) [14] was applied to evaluate the patients’ knowledge of stroke. There were 8 items in the questionnaire, including daily life, diet, medication, premonition symptoms of stroke, etc. All of them were single choice items, and were divided into “I don’t know” (0 points) and “I know” (1 point). The higher the score, the better the patient’s knowledge of stroke health.
(2) The nursing satisfaction questionnaire [15] was applied to investigate the patients’ nursing satisfaction. The total score was 100, with a questionnaire score below 60 as dissatisfied, a score of 60-89 as satisfied, and a score above 90 as greatly satisfied. Satisfaction = (greatly satisfied + satisfied)/total cases × 100%.
(3) The National Institutes of Health Stroke Scale (NIHSS) [16] was applied to evaluate the neurological deficits of patients, including 11 items such as sensation, limb movement and consciousness level. The higher the score, the more serious the neurological deficit of patients.
(4) Barthel index (BI) [17] was used to evaluate patients’ activity of daily living (ADL), including 10 items such as fasting, walking on flat ground, and going up and down stairs. The higher the score, the better the patient’s ADL.
Statistical methods
SPSS25.0 software (IBM, Armonk, NY, USA) was adopted for statistical analysis. Figures were plotted using GraphPad Prism 7.0 (Beijing Tianyan Rongzhi Software Co., Ltd., China) version of the medical graphics software. The enumeration data was represented by the number of cases and percentage [n (%)], compared by chi-square test. The measurement data was expressed as mean ± standard deviation (Mean ± SD), t-test or paired t-test was adopted. P<0.05 was used as the basis for statistical conclusion.
Results
Clinical data of patients
We collected the clinical data of patients, and the statistical comparison showed no significant difference between the control group and the test group in terms of age, gender and other general clinical data (P>0.05), as shown in Table 1.
Table 1.
Clinical data of the control group and the test group
| Category | Control group (n=51) | Test group (n=55) | t/χ2 value | P value |
|---|---|---|---|---|
| Course of hypertension (year) | 10.72±2.67 | 11.36±2.75 | 1.214 | 0.228 |
| Age (years) | 67.08±3.31 | 68.15±3.57 | 1.597 | 0.113 |
| Gender | 0.239 | 0.625 | ||
| Male | 32 (62.75) | 37 (67.27) | ||
| Female | 19 (37.25) | 18 (32.73) | ||
| Education level | 0.654 | 0.884 | ||
| University | 8 (15.69) | 10 (18.18) | ||
| Senior high school | 17 (33.33) | 18 (32.73) | ||
| Junior high school | 19 (37.25) | 22 (40.00) | ||
| Primary school | 7 (13.73) | 5 (9.09) | ||
| Area of cerebral infarction (cm2) | 5.01±1.25 | 5.13±1.39 | 0.466 | 0.642 |
| Site of cerebral infarction | 1.239 | 0.538 | ||
| Left | 13 (25.49) | 10 (18.18) | ||
| Right | 27 (52.94) | 29 (52.73) | ||
| Bilateral | 11 (21.57) | 16 (29.09) | ||
| Smoking history | 0.044 | 0.834 | ||
| Present | 24 (47.06) | 27 (49.09) | ||
| Absent | 27 (52.94) | 28 (50.91) | ||
| TG (mmol/L) | 1.55±0.53 | 1.53±0.64 | 0.174 | 0.862 |
| TC (mmol/L) | 4.22±0.89 | 4.28±0.91 | 0.343 | 0.732 |
| LDL-C (mmol/L) | 2.85±0.23 | 2.86±0.24 | 0.219 | 0.827 |
| HDL-C (mmol/L) | 1.13±0.42 | 1.15±0.45 | 0.236 | 0.814 |
Patient health knowledge of stroke and neurological score
We applied SKQ to evaluate patients’ knowledge of stroke. There was no significant difference in SKQ score between the two groups before care (P>0.05). After care, however, the SKQ score elevated in both groups (P<0.05), and was higher in the test group than in the control group (P<0.05). In addition, we applied NIHSS to assess the neurological function of patients before and three months after care, and found no significant difference in the score between the two groups before care (P>0.05). After care, both groups of patients had reduced NIHSS scores (P<0.05), and the decrease was more obvious in the test group (P<0.05). More details are shown in Figure 1.
Figure 1.
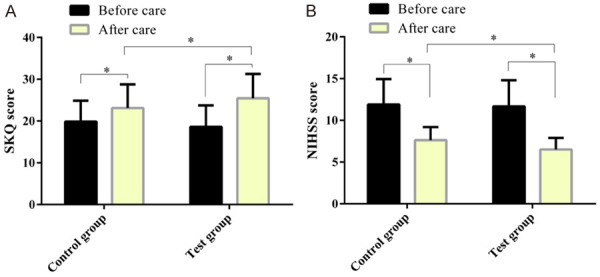
Patient health knowledge of stroke and neurological score. After care, the SKQ score is elevated and the NIHSS score is decreased in both groups. In the test group, the SKQ score is higher, and the NIHSS score shows greater decrease. Note: *P<0.05.
Patient blood pressure
We observed the blood pressure of two groups of patients, and found no remarkable difference in SBP and DBP between the two groups before care (P>0.05). After care, SBP and DBP decreased markedly in both groups (P<0.05), and they were lower in the test group than in the control group (P<0.05), as shown in Figure 2.
Figure 2.
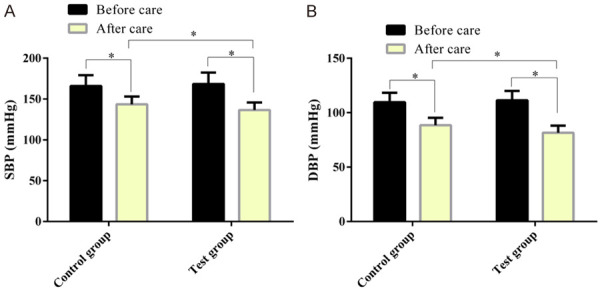
Comparison of blood pressure between two groups of patients. After care, SBP (A) and DBP (B) decrease significantly in both group, and they are lower in the test group than in the control group. Note: *P<0.05.
Patient nursing satisfaction
We applied nursing satisfaction questionnaire to assess patients’ nursing satisfaction. In the control group, 21 patients were greatly satisfied with nursing (41.18%), 20 were satisfied (39.22%), and 10 were dissatisfied (19.61%). In the test group, however, 32 patients were greatly satisfied with nursing (58.18%), 20 were satisfied (36.36%), and 3 were dissatisfied (5.45%). The total satisfaction of the test group was markedly higher than that of the control group (P<0.05). More details are shown in Table 2.
Table 2.
Nursing satisfaction of patients in the two groups
| Type | Control group (n=51) | Test group (n=55) | χ2 value | P value |
|---|---|---|---|---|
| Great satisfied | 21 (41.18) | 32 (58.18) | 4.926 | 0.026 |
| Satisfied | 20 (39.22) | 20 (36.36) | ||
| Dissatisfied | 10 (19.61) | 3 (5.45) | ||
| Satisfaction degree | 80.39 | 94.55 |
Patient ADL
BI was applied for the assessment of ADL of two groups of patients. There was no remarkable difference in BI between the two groups before care (P>0.05). After care, the BI elevated in both groups (P<0.05), and was higher in the test group than in the control group, as shown in Figure 3.
Figure 3.
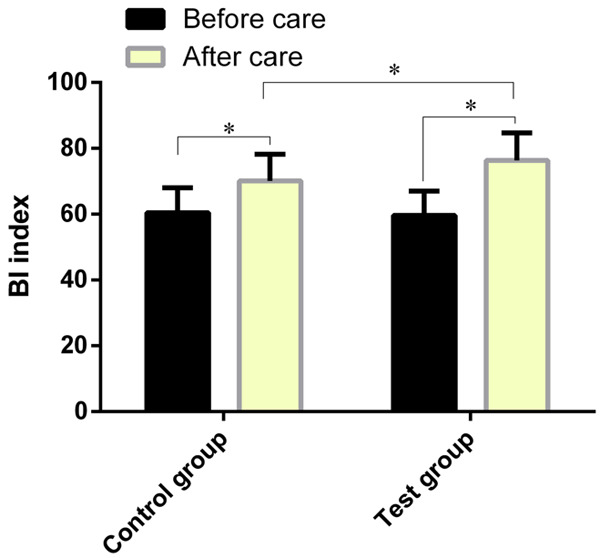
Patient ADL. After care, the BI is elevated in both groups, and the BI is higher in the test group than in the control group. Note: *P<0.05.
Patient blood pressure control rate
We assessed patients’ blood pressure control rate at discharge, and 2 months, 4 months, and 6 months after discharge. The blood pressure control rates of patients in the test group were higher than those in the control group at the four time points above (P<0.05). More details are shown in Table 3.
Table 3.
Blood pressure control rate of two groups of patients at different time points
| Nursing compliance | Control group (n=51) | Test group (n=55) | χ2 value | P value |
|---|---|---|---|---|
| At discharge | 40 (78.43) | 51 (92.73) | 4.452 | 0.035 |
| Two months after discharge | 33 (64.71) | 45 (81.82) | 3.987 | 0.046 |
| Four months after discharge | 30 (58.82) | 48 (87.27) | 11.020 | <0.001 |
| Six months after discharge | 25 (49.02) | 47 (85.45) | 16.120 | <0.001 |
Discussion
Patients with cerebral infarction caused by hypertension usually have severe psychological burden and limb dysfunction, which seriously affects their quality of life [18]. In this study, we implemented clinical nursing pathway model for elderly patients with hypertension and cerebral infarction. We found that this nursing model can improve the blood pressure, nerve function and ADL of patients, and promote their rehabilitation.
Clinical nursing pathway is to implement patient-centered medical service concept to standardize the entire care process according to the clinical pathway form, which can improve the nursing work efficiency, and the nursing items will not be missed [19]. Clinically, it can shorten the length of stay, save the cost of nursing, and promote the therapeutic effect of patients [20]. The team of Naqib indicated that clinical pathway and nursing education program can improve the immediate pain management of anesthetized patients after operation, as well as their rehabilitation quality [21]. The above shows that clinical nursing pathway program has significant benefits for patients’ recovery. In our research, the implementation of clinical nursing pathway can improve patients’ health knowledge of stroke and control the blood pressure. Our follow-up also revealed a good rate of blood pressure control. As we all know, patients with hypertension and cerebral infarction often have negative emotions [22]. The improvement of patients’ health knowledge will help them adjust their behavior and enable them to actively cooperate with treatment. Further research showed that the implementation of clinical nursing pathway could improve the neurological function score and ADL of patients. Similarly, the team of Li applied clinical nursing pathway to patients with acute cerebral hemorrhage, and found notably shortened length of stay, improved clinical efficacy and nursing satisfaction, and reduced adverse reactions during hospitalization [23]. Our research also indicated that clinical nursing pathway improved patients’ nursing satisfaction, suggesting that this model of nursing is well accepted by patients and has good application value. Clinical nursing pathway is a type of standard care process developed through assessing the patient’s symptoms, cognitive status, etc., and the implementation of psychological care for patients can improve their health knowledge and their self-care ability [24]. Nutritional nursing can improve patients’ eating habits, and reasonable intake of food can make patients’ blood pressure under better control [25]. Regular turning, management of the oral cavity, skin and urinary catheter in comfort care can actively prevent complications [26]. Reasonable arrangement of rehabilitation exercise and continuing nursing guidance are beneficial to patients’ neurological function repair and limb rehabilitation, which can help develop good living habits and enhance their ADL [27]. Therefore, the implementation of clinical nursing pathway can promote the rehabilitation of patients with cerebral infarction caused by hypertension. Nevertheless, there are still some shortcomings in our research. The adverse events of patients were not systematically evaluated. In addition, the complications that occurred during nursing were not observed. These limitations need to be further investigated in the future.
This study indicates that the application of clinical nursing pathway can improve the disease cognition and quality of life of elderly patients with hypertension and cerebral infarction, and promote their recovery.
Disclosure of conflict of interest
None.
References
- 1.Kitt J, Fox R, Tucker KL, McManus RJ. New approaches in hypertension management: a review of current and developing technologies and their potential impact on hypertension care. Curr Hypertens Rep. 2019;21:44. doi: 10.1007/s11906-019-0949-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drummond GR, Vinh A, Guzik TJ, Sobey CG. Immune mechanisms of hypertension. Nat Rev Immunol. 2019;19:517–532. doi: 10.1038/s41577-019-0160-5. [DOI] [PubMed] [Google Scholar]
- 3.Sakuta K, Mukai T, Suzuki K, Nishiwaki K, Yaguchi H. Irreversible vasculopathy proceeds rapidly in POEMS syndrome. Intern Med. 2019;58:3573–3575. doi: 10.2169/internalmedicine.3279-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Q, Cao C, Gong L, Zhang Y. Health related quality of life in stroke patients and risk factors associated with patients for return to work. Medicine (Baltimore) 2019;98:e15130. doi: 10.1097/MD.0000000000015130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.He D, Yu Y, Wu S, Tian S, Yu H, Xu S, Chu L. Mixed cerebrovascular disease in an elderly patient with mixed vascular risk factors: a case report. BMC Neurol. 2019;19:26. doi: 10.1186/s12883-019-1248-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tan Q, Zhang M, Wang Y, Zhang M, Wang Y, Xin Q, Wang B, Li Z. Frequency-specific functional connectivity revealed by wavelet-based coherence analysis in elderly subjects with cerebral infarction using NIRS method. Med Phys. 2015;42:5391–5403. doi: 10.1118/1.4928672. [DOI] [PubMed] [Google Scholar]
- 7.Fu S, Han H, Fan C, Jiang Y. Clinical nursing pathway improves the nursing satisfaction in patients with acute cerebral hemorrhage: a randomized controlled trial protocol. Medicine (Baltimore) 2020;99:e22989. doi: 10.1097/MD.0000000000022989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang Y, Hu X, Zhang Q, Cao H, Li J, Wang J, Shao Y, Xin S. Effect of clinical nursing pathway for endoscopic thyroidectomy in Chinese patients: a meta-analysis. Int J Nurs Pract. 2016;22:224–231. doi: 10.1111/ijn.12357. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Z, Bai J, Huang Y, Wang L. Implementation of a clinical nursing pathway for percutaneous coronary intervention: a randomized controlled trial protocol. Medicine (Baltimore) 2020;99:e22866. doi: 10.1097/MD.0000000000022866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen ZX, Liu AH, Cen Y. Fast-track program vs traditional care in surgery for gastric cancer. World J Gastroenterol. 2014;20:578–583. doi: 10.3748/wjg.v20.i2.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanders SL, Bantum EO, Owen JE, Thornton AA, Stanton AL. Supportive care needs in patients with lung cancer. Psychooncology. 2010;19:480–489. doi: 10.1002/pon.1577. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y, Tang T, Tang K. Cooking frequency and hypertension with gender as a modifier. Nutr J. 2019;18:79. doi: 10.1186/s12937-019-0509-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bryan RN, Levy LM, Whitlow WD, Killian JM, Preziosi TJ, Rosario JA. Diagnosis of acute cerebral infarction: comparison of CT and MR imaging. AJNR Am J Neuroradiol. 1991;12:611–620. [PMC free article] [PubMed] [Google Scholar]
- 14.Komolafe MA, Olorunmoteni OE, Fehintola FO. Effect of health education on level of awareness and knowledge of Nigerian in-school adolescents on stroke and its risk factors. J Stroke Cerebrovasc Dis. 2020;29:104757. doi: 10.1016/j.jstrokecerebrovasdis.2020.104757. [DOI] [PubMed] [Google Scholar]
- 15.Karaca A, Durna Z. Patient satisfaction with the quality of nursing care. Nurs Open. 2019;6:535–545. doi: 10.1002/nop2.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao XJ, Li QX, Liu TJ, Wang DL, An YC, Zhang J, Peng YB, Chen RY, Chang LS, Wang Y, Zhang L, Fan HY, Wang XJ, Zheng FX. Predictive values of CSS and NIHSS in the prognosis of patients with acute cerebral infarction: a comparative analysis. Medicine (Baltimore) 2018;97:e12419. doi: 10.1097/MD.0000000000012419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang Y, Chen Y, Chen K, Wei D, Li P, Zeng W, Pei J, Mao H, Jia J, Zhang Z. Increased intrinsic connectivity for structural atrophy and functional maintenance after acute ischaemic stroke. Eur J Neurol. 2019;26:935–942. doi: 10.1111/ene.13913. [DOI] [PubMed] [Google Scholar]
- 18.Chen CH, Hung KS, Chung YC, Yeh ML. Mind-body interactive qigong improves physical and mental aspects of quality of life in inpatients with stroke: a randomized control study. Eur J Cardiovasc Nurs. 2019;18:658–666. doi: 10.1177/1474515119860232. [DOI] [PubMed] [Google Scholar]
- 19.Xu Z, Chen B, Li G, Dai W. The interference in the suicide ideation of patients with malignant tumors by mental clinical nursing pathway. Patient Prefer Adherence. 2014;8:1665–1669. doi: 10.2147/PPA.S74132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwarzbach M, Rossner E, Schattenberg T, Post S, Hohenberger P, Ronellenfitsch U. Effects of a clinical pathway of pulmonary lobectomy and bilobectomy on quality and cost of care. Langenbecks Arch Surg. 2010;395:1139–1146. doi: 10.1007/s00423-010-0600-y. [DOI] [PubMed] [Google Scholar]
- 21.Naqib D, Purvin M, Prasad R, Hanna IM, Dimitri S, Llufrio A, Hanna MN. Quality improvement initiative to improve postoperative pain with a clinical pathway and nursing education program. Pain Manag Nurs. 2018;19:447–455. doi: 10.1016/j.pmn.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 22.Donkor ES, Owolabi MO, Bampoh PO, Amoo PK, Aspelund T, Gudnason V. Profile and health-related quality of life of Ghanaian stroke survivors. Clin Interv Aging. 2014;9:1701–1708. doi: 10.2147/CIA.S62371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li W, Gao J, Wei S, Wang D. Application values of clinical nursing pathway in patients with acute cerebral hemorrhage. Exp Ther Med. 2016;11:490–494. doi: 10.3892/etm.2015.2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hwang B, Moser DK, Dracup K. Knowledge is insufficient for self-care among heart failure patients with psychological distress. Health Psychol. 2014;33:588–596. doi: 10.1037/a0033419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Juraschek SP, Miller ER 3rd, Weaver CM, Appel LJ. Effects of sodium reduction and the DASH diet in relation to baseline blood pressure. J Am Coll Cardiol. 2017;70:2841–2848. doi: 10.1016/j.jacc.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jaul E. Assessment and management of pressure ulcers in the elderly: current strategies. Drugs Aging. 2010;27:311–325. doi: 10.2165/11318340-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 27.Chen L, Han Z, Gu J. Early path nursing on neurological function recovery of cerebral infarction. Transl Neurosci. 2019;10:160–163. doi: 10.1515/tnsci-2019-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]


