Abstract
Objectives:
Although the health consequences of life stress in the general population are well known, how different stressors occurring over the lifetime cause morbidity and mortality in autism is unclear, as are the factors that moderate and mediate these associations. The few studies that have compared autistic and non-autistic individuals have used instruments that yield few stress exposure indices and assess stressors occurring over short time periods.
Method:
To address these issues, we used the Stress and Adversity Inventory to assess lifetime stressor exposure and perceived stressor severity in 127 autistic and 104 non-autistic adults. Moderated mediation analysis examined associations between stressor exposure, physical and mental ill-health with respect to the hypothesised mediating role of stressor perception, and moderation effects of loneliness and social support.
Results:
Autistic adults experienced more lifetime stressors and generally perceived stressors as more severe. Greater perceived stressor severity was related to poorer physical and mental health, and to greater loneliness and lower social support for both groups. An additional post-hoc analysis of the association between diagnostic status and mental ill-health revealed that loneliness mediated the relation between being autistic and having poorer mental health.
Conclusion:
Autistic individuals experienced more lifetime stressors, and their impact on physical and mental health was mediated by perceived stressor severity. Moreover, loneliness and low social support were associated with greater negative impact of lifetime stress exposure on mental health. Interventions that reduce cognitive-perceptual stress appraisals, and that target loneliness and social support, may help reduce stress-related disease in autistic individuals.
Keywords: autism, stress, health, social support, loneliness
A wealth of research has shown that activating and maintaining a multi-level psychological and biological stress response (i.e., stress) to social, psychological, or physical threats (i.e., stressors) has a cumulative cost in allostatic load, the biological “wear and tear” to bodily systems that increases the risk of serious health problems (McEwen, 2005). At the level of the immune system, stress can upregulate inflammatory activity and cause immunosuppression; at the molecular and genomic level, it affects brain plasticity and gene expression, heightening the sensitivity of the stress response. At the psychosocial level, stress can impede executive function, self-regulation and coping, which can cause individuals to engender additional stressors in their lives. Ultimately, stress exposure is known to heighten the risk of psychiatric illness alongside cardiovascular, autoimmune, and neurodegenerative diseases, and to predict early mortality, especially if stressors are interpersonal in nature and occurring early in life (Slavich, 2020).
Despite this general knowledge linking stress and health, the role that stress processes play in the excess mortality associated with autism spectrum conditions (ASC) has received little attention. Data indicate that autistic1 individuals die 16 years earlier (on average) than their non-autistic peers, with particular risks for mortality from suicide (Hirvikoski et al., 2016). The same study found that autistic people with an accompanying intellectual disability had life expectancies up to 30 years shorter than non-autistic people, most notably due to epilepsy-related deaths. Moreover, all autistic people experience more diseases of the nervous, circulatory, and respiratory and digestive systems, as well as high rates of diabetes, epilepsy, gastrointestinal complaints, hypertension, and immune conditions (Cashin et al., 2018; Hirvikoski et al., 2016; Tye et al., 2019).
The causes of morbidity and mortality in ASC are complex and multifaceted, with likely contributions from long-term medication use, barriers to healthcare, and genetic and cellular abnormalities (Tye et al, 2019). However, autistic people are also at higher risk for accumulating greater stressor-driven allostatic load over their lifespans. Indeed, autistic children are more likely to experience family poverty and adverse childhood experiences such as sexual abuse, parental illness, alcoholism, and divorce (Hoover & Kaufman, 2018). Their social difficulties often invoke negative responses from others, which can engender chronic anxiety (Wood & Gadow, 2010). School exclusion, bullying, and alienation are extremely common (Brede et al., 2017; Maïano et al., 2016) and, as adults, autistic people are often socially isolated, naïve, and vulnerable to exploitation, physical, emotional, and sexual victimisation (Griffiths et al., 2019). In addition, autistic adults are more likely to come into contact with the criminal justice system (King & Murphy, 2014), be chronically un- or underemployed (Harmuth et al., 2018), and be socially stigmatised (Botha & Frost, 2018).
Perceiving a stressor as stressful or threatening is an intermediary step preceding the initiation of the stress response (Lebois et al., 2016), and numerous intrapersonal factors influence an individual’s response. In the case of autism, neuropsychological features such as cognitive flexibility can exacerbate the impact of stressors on health (Kerns et al., 2015). Indeed, everyday situations characterized by unpredictability and spontaneity are identified as highly stressful by those with ASC (Goodwin et al., 2007), and perceiving stressors as stressful is highly distressing for this group (Bishop-Fitzpatrick et al., 2017). Appraisal of available resources and coping ability is a crucial determinant of stress perception and, in turn, stressor impact (Lazarus & Folkman, 1984), and it is notable that autistic adults often recognise their coping skills as poor (Hirvikoski & Blomqvist, 2015).
Because interpersonal factors also influence perception of stressors and their impact on health, autistic people are likely disadvantaged due to their characteristic social isolation (Ee et al., 2019). Loneliness is a highly pathogenic factor that exacerbates the perceived severity of life stressors and their physiological impact; the cognitive bias it engenders casts life events in a negative light and further alienates the individual, who may have a greater tendency to resort to maladaptive behaviours and harmful coping styles (Hawkley & Cacioppo, 2010). Whereas loneliness has been robustly associated with heightened morbidity and mortality, social support, in contrast, is known to ameliorate allostatic load in the general population (Uchino et al., 2012). Researchers have differentiated between different types of support (Cohen et al., 1983), such as appraisal support (e.g., having someone to talk through problems with), tangible support (e.g., providing material aid), and belonging support (e.g., spending time with others in companionship and recreational activities). Support may exert a direct effect by reducing the severity with which stressors are perceived, but it can also act as a buffer against the deleterious effects of stressor perception, reducing the activity of physiological pathways that harm health (Cohen & Wills, 1985; Allen et al., in press).
Although much is understood about relationships between stress, stressors, and health in non-autistic people, and about the interplay between interpersonal variables and stressor perception, research has yet to examine potential links between exposure to life stressors and the excess morbidity and mortality of autism. Studies have examined other correlates of stress in autism, such as greater social disability (Bishop-Fitzpatrick et al., 2015, 2017) and lower quality of life (Bishop-Fitzpatrick et al., 2018; Hong et al., 2016). Although these are relevant constructs with respect to mental and physical health, these studies have been subject to criticisms recently levied on stress research in general. Where “stress” has been operationalized using clinical interviews, self- or even other-reports, these methods have yielded crude, single numeric summary scores that fail to consider the different effects of stressors with regards to their timing, duration of exposure, and social-psychological features, or to differentiate the health impact of life stressors themselves from the impact of the way they are perceived (Epel et al., 2018; Slavich, 2019). Furthermore, autism studies commonly conflate ‘stress’ (typically a predictor) with anxiety (the outcome), or with more general terms such as ‘worry’ or ‘psychological distress’. Consequently, no research has linked health outcomes to autistics adults’ actual exposure to, or perceptions of, different life stressors, or highlighted stressors of greatest relevance for their physical and mental health.
In non-autistic populations, researchers have used the Stress and Adversity Inventory for Adults (STRAIN) to investigate how different stressors occurring across the life course are related to cognitive, behavioral, and health outcomes (Slavich & Shields, 2018). The STRAIN is unique in that it assesses both exposure to and perceptions of acute and chronic stressors occurring over the entire lifespan. Classifying stressors based on their timing and duration of exposure, the STRAIN recognises that seemingly similar life stressors may have different effects owing to the specific features of the exposure. Furthermore, in classifying stressors by their specific life domain (e.g., work, marital) as well as their core-social-psychological characteristic (e.g., interpersonal loss, physical danger), the measure acknowledges that seemingly dissimilar stressors (for instance, being bereaved in childhood and divorced as an adult) may share social-psychological characteristics that are meaningful for health (Slavich, 2020). In short, the STRAIN provides a comprehensive overview of cumulative lifetime stress exposure that can be used to study associations between stress and health in high resolution.
The present study was the first to use the STRAIN with autistic adults without intellectual disability. First, we characterised their lifetime stress exposure and stressor perceptions against those of an age-matched, non-autistic (NA) comparison group. Secondly, we examined relations between total lifetime stressor exposure, perceived stressor severity, and physical and mental health outcomes, and then relations between both health outcomes and the specific types of stressors experienced. Thirdly, we investigated loneliness and social support as possible moderators of the association between lifetime stress exposure and health. Based on aforementioned literature, we hypothesized that autistic people would have greater stressor exposure and perceived stressor severity than non-autistic individuals, and that, as previously observed in non-autistic people, stressor severity would mediate the deleterious impacts of stressor exposure on health. Moreover, we hypothesized that whereas loneliness would strengthen the negative effects of the stressors experienced on physical and mental health, social support would buffer these effects. Because autistic people are characteristically lonelier and have poorer social support than non-autistic adults, we expected that the associations between stress on health would be relatively greater for autistic adults.
Method
Participants
Participants were autistic (n = 127; 71% women) and non-autistic adults (n = 104; 61% women). The autistic sample (AU group) was recruited using online advertisements (23%) and by contacting individuals who had previously participated in studies by the first author (77%). The average age of the group was 40.8 years old (SD = 13.9; range: 19–73) and most participants (85.8%) were >18 when diagnosed (Mage of diagnosis = 33.6 years old, SD = 16.5; range: 2–67). They reported the date, institution, and precise diagnosis they received. The age-matched non-autistic (NA) group was 39.6 years old, on average (SD = 13.1; range: 21–76), and was recruited using online advertisements and screened for the absence of ASC, ADHD, and neurological disorders. Drawing on prior work (Bishop-Fitzpatrick et al., 2017), large effect sizes were expected for the comparison of AU and NA participants for lifetime stressor exposure and perceived stressor severity; therefore, only 38 participants per diagnostic group were required to observe group differences at a conservative alpha level of p < .01. In contrast, effect sizes between NA men and women have previously been reported as small (Slavich & Shields, 2018); because statistical comparisons and moderating effects with this factor would likely have been underpowered, we controlled for sex as a covariate in all analyses.
Participant nationalities were British (62% AU, 66% NA), American (12% AU, 5% NA), European (8% AU, 21% NA), Canadian (2% AU, 1% NA), Australian or from New Zealand (4% AU, 2% NA), South American (2% AU, 3% NA), and from the African continent (2% NA participants); the remainder preferred not to say. The diagnostic groups did not differ in male/female ratio, or in the number of individuals qualified to a degree level (57% in both groups) or A-level standard or equivalent (73% and 77% in the AU and NA groups, respectively). This suggests that all participants were likely in the average-to-high IQ range. However, 70% of NA participants reported some form of employment in contrast to 50% of AU participants (χ[1] = 5.651, p =.017). Only 26% of NA participants reported a psychiatric illness as compared to 78% of AU participants (χ(1) = 48.634, p < .001), with anxiety and depression being most common in both groups; additionally, 14% of NA participants were taking psychotropic medication at the time of the study as compared to 47% of AU participants (χ(1) = 26.948, p < .001). Additionally, 9% of AU participants reported comorbid ADD/ADHD, and they were more likely to endorse other kinds of specific learning disability (13% vs. 3% of NA participants: χ(1) = 21.105, p < .001). Relationship status also differed significantly between the groups (χ(5) = 18.380, p = .003), with 51% of AU participants being married, dating, or in a serious relationship, in contrast to 76% of NA participants. Finally, 46% of AU (vs. 22% of NA) participants were single, and of those, 11% (vs. 5%) were never in a relationship. Given this group difference and its potential significance for social support, presence vs. absence of a relationship was used as a covariate in all analyses.
Procedure and Measures
All procedures were approved by the Ethics Committee at Bournemouth University. Participants provided informed consent and completed the scales below (hosted on Qualtrics), and then completed the STRAIN and the two health outcome measures on the dedicated STRAIN server. Scale reliability (α) was judged acceptable for each scale (see Supplementary Materials, 1).
Stress and Adversity Inventory for Adults (STRAIN)
The STRAIN assesses individuals’ lifetime exposure to 55 major stressors that have been associated with psychiatric and physical illness and premature mortality (Slavich & Shields, 2018). For each endorsed stressor, tailored follow-up questions assess that stressor’s frequency, timing, and duration, in addition to the participant’s assessment of the stressor’s severity on a 1–5 scale (see https://www.strainsetup.com). The STRAIN includes stressors from 12 life domains (i.e., housing, education, work, treatment and health, marital and partner relationships, reproduction, adult finances, legal difficulties and involvement in crime [as victim, accused, or perpetrator], other relationships [i.e., friends and family], death of a close other, involvement in life-threatening situations, and possessions [e.g., being robbed]). These stressors can also be categorised by five main social-psychological characteristics: interpersonal loss, physical danger, humiliation, entrapment (e.g., being a caregiver, facing persistent overwhelming job demands), or role change/disruption (e.g., requiring ongoing care as an adult, being forced to move homes). In addition to indexing participants’ extent of exposure to and perceived severity of these stressor types, the STRAIN produces two main indices: total lifetime stressor count and total lifetime perceived stressor severity. The former is created by summing together the reported frequency of each endorsed stressor and the latter by summing together the reported severity for each endorsed stressor. These two main indices have excellent test-retest reliability (ricc = 0.936 and 0.953, respectively). More broadly, the STRAIN has demonstrated strong concurrent and discriminant validity, and predictive and incremental validity across a variety of psychological, cognitive, biological, and clinical outcomes (e.g., Lam et al., 2019; Smith et al., 2020; Stewart et al, 2019).
Outcome Measures: Physical and Mental Health
Participants’ self-reported physical and mental health over the last month were assessed with the Physical Health Questionnaire (PHQ; Schat et al., 2005) and Kessler 6-item Psychological Distress Inventory (K6; Kessler et al., 2002), respectively. These scales have strong psychometric properties including good internal consistency (PHQ: Doi et al., 2018; K6: Prochaska et al., 2012). Higher scores indicate poorer physical and mental health, respectively.
Interpersonal Moderators: Loneliness and Social Support
UCLA Loneliness Scale (Russell, 1996).
Participants rated 20 statements (e.g., “I feel isolated from others”) assessing subjective feelings of loneliness and social alienation. The scale has previously demonstrated strong internal consistency (typical αs = .89 to .94) and psychometric properties (Russell, 1996), with higher scores indicating greater loneliness.
Interpersonal Support Evaluation List 12 (Cohen et al., 1985).
This 12-item scale includes subscales that delineate appraisal support, belonging support, and tangible support as three distinct types of social support. Because it is important to clarify what types of support are most relevant for autistic people (Hedley et al., 2017), we examined the support subscales as independent variables, with higher scores indicating greater perceived availability of social support. The scale has demonstrated good internal consistency (α = .86) and psychometric properties (Merz et al., 2014).
Data Analysis
Characterising lifetime stress exposure in autistic and non-autistic adults
As a preliminary step, we computed descriptive statistics for the STRAIN variables of interest, effect sizes for differences between NA and AU participants, and correlations between these variables (Supplementary Materials, 2). We then compared AU and NA participants’ exposure to stressors occurring in each of the STRAIN’s 12 life domains. In a mixed ANOVA, these different types of stressor were included in a single within-subjects factor (i.e., stressor domain) with 12 levels and a between-subjects factor (i.e., diagnosis) with 2 levels. Because the domain factor violated the assumption of sphericity, Greenhouse-Geisser corrected values are reported throughout. Next, we compared the diagnostic groups on perceived severity of stressors. To ensure that greater perceived stressor severity was not merely the consequence of experiencing more lifetime stressors, we ran 12 between-subjects ANOVAs in which we compared AU and NA groups for perceived severity of stressors in each domain while controlling for stressor exposure in that domain2. Correcting for multiple comparisons resulted in an alpha level for significance of p = .004.
Assessing lifetime stressor exposure and social-psychological stressor types as predictors of health outcomes
Using PROCESS for SPSS (Hayes, 2017) and the two major indices from the STRAIN, we conducted a moderated mediation analysis (Model 59) to examine whether any impact of total lifetime stressor exposure on physical health was mediated by total lifetime perceived stressor severity. As a moderator, we examined effects of diagnosis on each of the pathways in the model. We followed the same moderated mediation pathway to examine relations between exposure to each of the five social-psychological stressor types, the perceived severity of that stressor (as a mediator), and physical health. With 6 analyses for this outcome measure, alpha levels were corrected to p = .008. The same analyses were performed for mental health as the outcome variable.
Investigating loneliness and social support as moderators of relationships between stress and health
Finally, we used PROCESS (model 2) to test the possible moderating influence of our four interpersonal variables, loneliness, appraisal, belonging, and tangible support, on first the relation between total lifetime stressor exposure and total lifetime perceived stressor severity, then the relation between lifetime perceived stressor severity and physical health, and then the relation between lifetime perceived stressor severity and mental health. For these three associations, the four interpersonal variables were examined sequentially as moderators alongside diagnosis, which was held constant to observe interacting moderating effects. As there were four sets of analyses for each of these three relations, alpha levels in each set were corrected to p = .0125. As a preliminary step before this analysis, we computed descriptive statistics for, and correlations between, all variables (see Supplementary Materials 3).
Results
Lifetime stress exposure for autistic versus non-autistic participants
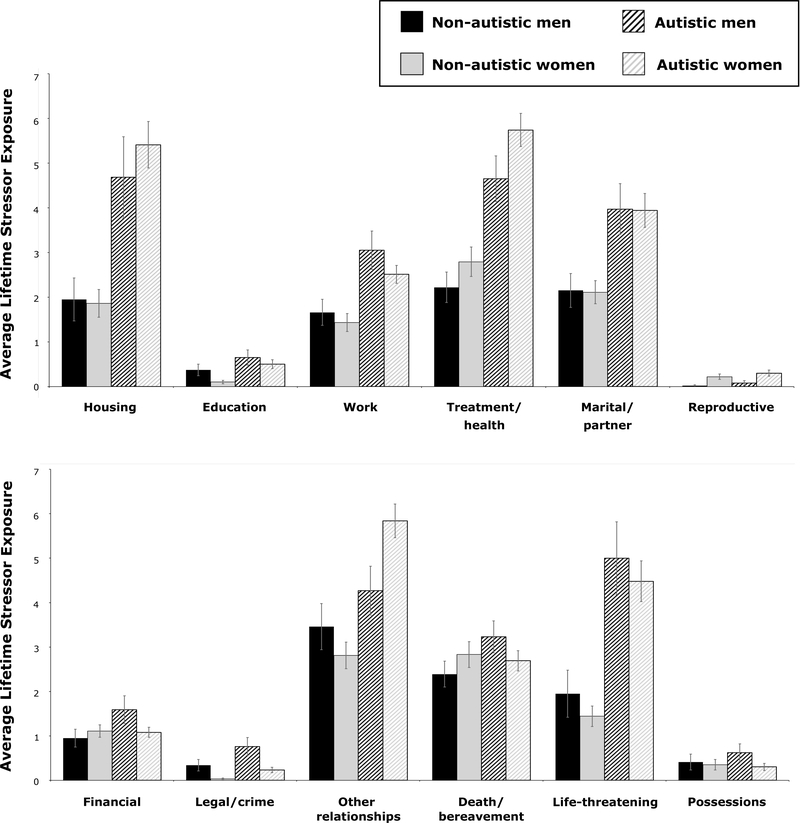
Main effects of stressor domain (F(5.48, 1221.32) = 18.84, p < .001) and diagnosis (F(1, 223) = 58.67, p < .001) revealed that participants reported more stressors for some domains than others, and that AU participants experienced more stressors over the lifespan than their NA counterparts. An interaction of stressor domain and diagnosis (F(5.47, 1214.60) = 15.13, p < .001) showed that the divergence between AU and NA participants was greater for some domains than others, as can be seen in Figure 1. Participants are stratified by sex for descriptive purposes, though sex, as a covariate, did not exert any significant main effect.
Figure 1. Average lifetime stressor exposure across twelve life domains for autistic and non-autistic males and females.
Note. Error bars reflect standard error. Group differences were large for treatment/health and life-threatening stressors (effect sizes: >.8); moderate for housing, work, marital/partner, and other relationship stressors (effect sizes: .5 to .8); small for education, reproductive, and legal/crime stressors (effect sizes: .2 to .5); and negligible for financial, death/bereavement, and possessions stressors (effect sizes: < .2).
When examining total lifetime perceived stressor severity in each domain individually, main effects of diagnosis showed that, regardless of the extent of their exposure to that stressor, AU participants perceived stressors involving work (F(1, 222) = 30.70, p < .001), treatment/health (F(1, 222) = 27.92, p < .001), and friend and familial relationships (F(1, 222) = 9.73, p = .002) as more stressful than did NA individuals. Several other stressor types were perceived as more stressful by AU individuals including stressors involving housing (F(1, 222) = 5.28, p = .022), marital/partner relationships (F(1, 222) = 5.88, p = .016), legal/crime (F(1, 222) = 6.41, p = .012), life-threatening situations (F(1, 222) = 5.15, p = .024), and possessions (F(1, 222) = 4.74, p = .030), but these analyses did not survive correction for multiple comparisons.
Physical health: relations with total lifetime stressor exposure, total lifetime perceived stressor severity, and specific stressor types
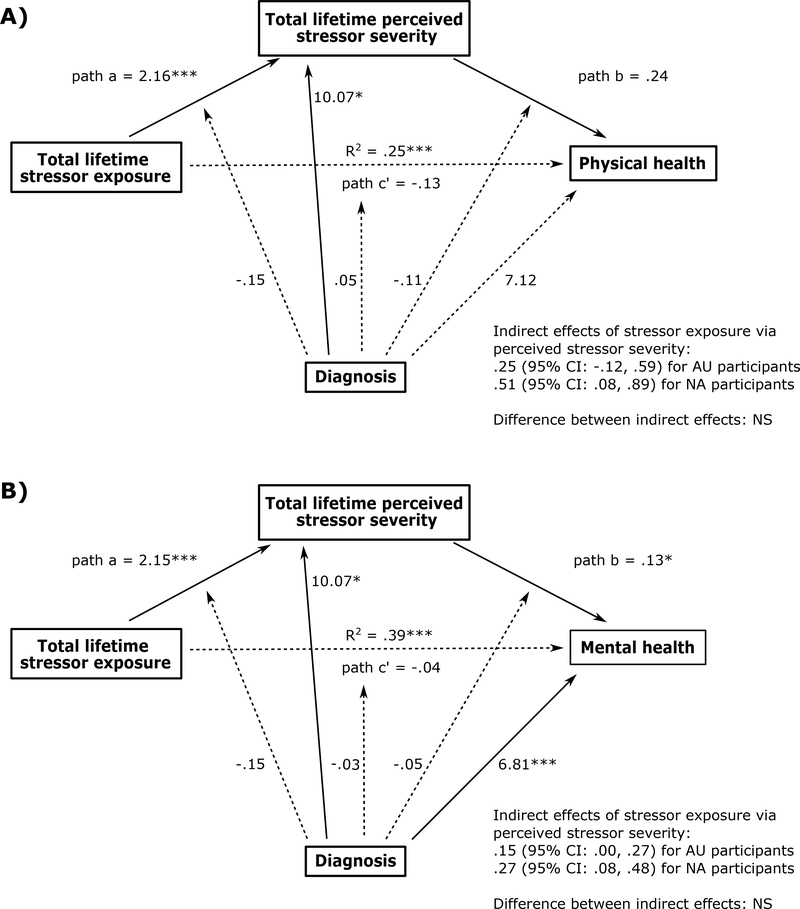
Rather than strengthening the association between lifetime stressor exposure and lifetime perceived stressor severity, diagnostic status was directly related to greater perceived stressor severity (p < .005) and to poorer physical health (p < .05), although the latter association did not survive statistical correction. As hypothesised, the impact of total lifetime stressor exposure on physical health was mediated by perceived stressor severity for NA participants (see Figure 2 Part A and Supplementary Materials 4 for full notations). Although this indirect effect was not significant for AU participants, the magnitude of difference between the groups was non-significant.
Figure 2. Moderated mediation analyses of relations between lifetime stressor exposure and (A) physical health and (B) mental health.
Note. Bold black lines reflect significant associations between predictor variables, mediator and outcome variables, and significant main effects of the moderator on the mediator and outcome variables. In both instances, coefficients are displayed with asterisks representing significance at p < .001 (***) or p < .01 (*). Dotted lines reflect non-significant associations.
When examining the pathways between total lifetime stressor exposure and perceived stressor severity, main effects of diagnosis showed that AU participants perceived physically dangerous stressors, role change/disruption stressors, and humiliation stressors as being more severe than did NA participants (all p < .005). Interestingly, two significant interactions of diagnosis and perceived severity (both p < .0005) showed opposite effects: the relation between actual exposure to role change/disruption stressors and perceived severity of the same was significantly stronger for NA participants (b = 2.14 vs. b = .163 in AU), whereas the opposite was true for entrapment stressors for AU participants (b = 4.50 vs. b = 3.90 in NA).
Physically dangerous stressors were indirectly related to physical health (via perceived stressor severity) for both groups. Interpersonal loss stressors and role change/disruption stressors exerted an indirect effect on physical health for NA but not AU participants; in the case of role change/disruption stressors, 95% confidence intervals (−3.60, −.53) revealed that the magnitude of difference between the diagnostic groups was significant. Finally, humiliation and entrapment stressors did not indirectly affect physical health through perceived severity, and a direct effect of humiliation stressors on health did not survive statistical correction for AU participants (p = .0105).
Mental health: relations with total lifetime stressor exposure, total lifetime perceived stressor severity and specific stressor types
The impact of total lifetime stressor exposure on mental health was fully mediated by perceived stressor severity for both diagnostic groups (see Figure 2 Part B and Supplementary Materials 5). As before, diagnosis did not moderate any pathways but was directly related to poorer mental health in all models. Interpersonal loss stressors indirectly affected mental health for both diagnostic groups. For physically dangerous stressors, a significant interaction between lifetime perceived stressor severity and diagnosis suggested that the association between perceived severity and mental health was relatively stronger for NA (b = .50) than AU (b = .10) participants. Indeed, there was only an indirect effect of physically dangerous stressors on mental health for NA participants, with 95% confidence intervals revealing a marked difference in the strength of this indirect effect between groups (−1.34, −.19). Humiliation stressors, in turn, were not indirectly nor directly related to mental health. The direct effect of entrapment stressors on mental health for AU participants did not survive correction for multiple comparisons (p = .0218); though an indirect effect of these stressors was present for AU but not NA individuals, the difference between groups was not significant. Finally, role change/disruption stressors were indirectly related to mental health for both diagnostic groups, and these stressors also exerted a significant direct effect on mental health for AU participants (p = .006).
Moderating effects of loneliness and social support
On the relation between stressor exposure and perceived stressor severity
Main effects of loneliness and the social support subscales revealed that greater loneliness was related to greater lifetime perceived stressor severity (p < .005), whereas higher appraisal, belonging, and tangible support were associated with lower perceived stressor severity (all p < .01; see Supplementary Materials 6). There were also significant interaction (i.e., moderation) effects for appraisal support and tangible support (both p < .01), where in each case, greater support rendered the association between lifetime stressor exposure and perceived stressor severity stronger (a similar moderating effect of belonging support, at p = .0302, did not survive statistical correction). In addition, combined moderation effects for appraisal support and diagnosis (p = .0024), and tangible support and diagnosis (p = .0076), reflected that this association tended to be weaker for participants with less support, and the participants in these lower tertiles tended to be autistic. Indeed, post-hoc checks revealed that AU participants were disproportionately represented in the lower tertiles for appraisal (χ2(2) = 21.80, p < .001) and tangible support (χ2(2) = 37.74, p < .001).
On the relation between total lifetime perceived stressor severity and physical health
Loneliness, appraisal support, belonging support, and tangible support were not significantly related to physical health, and did not moderate its association with lifetime perceived stressor severity (Supplementary Materials 7). Interestingly, however, the association between lifetime perceived severity and physical health was strongly significant (p = .004) when diagnosis and loneliness were both included as moderators.
On the relationship between total lifetime perceived stressor severity and mental health
Lifetime perceived stressor severity was related to mental health in every model (all p < .01; Supplementary Materials 8). Interestingly, diagnosis (being autistic) was directly associated with poorer mental health when included as a moderator in tandem with each kind of social support (all p < .005). In each of these models, significant moderating effects of diagnosis on the relation between lifetime perceived stressor severity and mental health (all p <.005) reflected that this association was weaker for AU participants. Appraisal, belonging, and tangible support were not significantly associated with mental health, and did not alone moderate its relation with perceived stressor severity. However, they did interact with diagnosis in a combined moderation effect (all p < .01), wherein the relation between lifetime perceived stressor severity and mental health was weakest for participants reporting higher levels of social support, and was even non-significant for AU participants with higher social support. In contrast, when diagnosis and loneliness were modelled as moderators on this association, the effect of diagnosis on mental health and its moderating effect became non-significant, and loneliness exhibited a strong positive association with poorer mental health (p < .001).
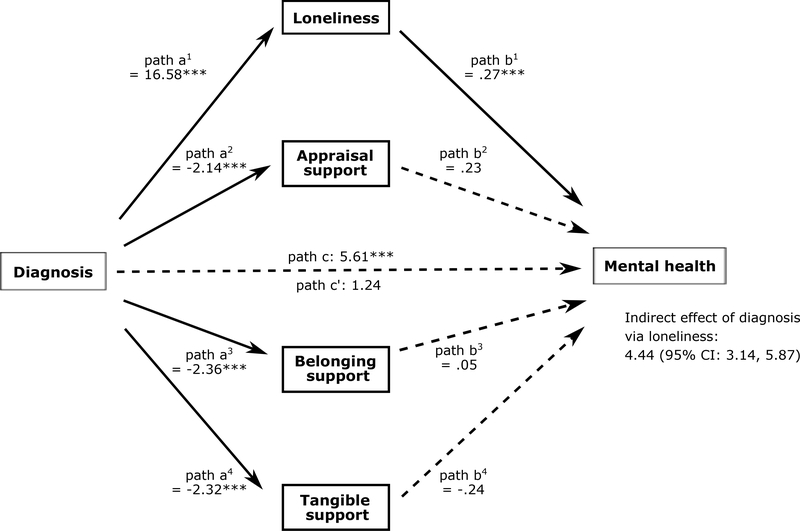
To further examine relations between diagnosis, mental health and interpersonal variables, we conducted a post-hoc mediation analysis (Model 4 in PROCESS) with loneliness, appraisal support, belonging support, and tangible support as parallel mediators in the diagnosis-mental health association (see Figure 3 and Supplementary Materials 9). Diagnosis was significantly associated with each mediator (in each case p <.001), but its total effect on mental health (p < .001) became non-significant when examined as a direct effect. Confidence intervals (3.14, 5.87) showed that diagnosis was only indirectly related to mental health through loneliness.
Figure 3.
Post-hoc mediation analysis, with loneliness, appraisal support, belonging support and tangible support as parallel mediators between diagnosis and mental health.
Discussion
Although stress is a central feature in the lives of autistic individuals, no studies have comprehensively assessed the lifetime stress exposure of autistic people or examined how such stress affects health outcomes in this population. The present data address this first goal by showing that AU participants experienced greater exposure to stressors occurring in all domains across the life course. This finding is consistent with prior research revealing higher rates of childhood bullying and relationship difficulties, victimization, and the ubiquity of unemployment in autistic adults (Griffiths et al., 2019). Differences in lifetime stressor exposure between AU and NA participants were minimal for some stressor types (e.g., bereavement) but moderate for several stressors including housing instability, work, and difficulties in romantic and friend/familial relationships, and large for life-threatening situations and treatment/health-related stressors. Whereas experiences involving traumatic life events and dangerous situations may arise from social vulnerability (Griffiths et al., 2019; Hoover & Kaufman, 2018), those involving treatment and health could reflect the commonality of physical and mental health problems as well as barriers to accessing healthcare and dissatisfaction with services that are commonly experienced by autistic people (Mason et al., 2019), a vicious circle that could itself exacerbate health issues in this vulnerable population.
Although prior research has examined stress exposure and stressor perception in autism (Bishop-Fitzpatrick et al., 2017), the study in question operationalised both constructs with a single general index and neglected to control for the possibility that stressor perception could be inflated by the AU individuals simply experiencing more stressors. The present data disentangled specific stressor types from perceived severity for each type and also controlled for the former to reveal that, even with degree of stressor exposure being held equal, certain stressors were nevertheless perceived as more being stressful by AU participants. The most significant effects in this regard were observed for stressors involving work, treatment/health, and friend/familial relationships. Moreover, our moderated mediation analysis also revealed that AU participants had higher lifetime perceived stressor severity as a whole and, likewise, that they perceived physically dangerous stressors, humiliating stressors, and stressors involving role change/disruption as more being severe than did NA individuals. This finding of heightened perceived stressor severity in autism is consistent with a multitude of intra- and interpersonal factors, which we shall now proceed to discuss. Foremost, however, we consider the significance and implications of these findings in terms of health.
Lifetime stress exposure, mental, and physical health
There is strong scientific consensus that prolonged and repetitive activation of the neuroendocrine stress response incurs a biological cost on numerous bodily systems (McEwen, 2005). Moreover, research has indicated that the manner in which stressors are appraised plays a key role in shaping the subsequent neurobiological stress response (Lazarus & Folkman, 1984). Our first moderated mediation analysis was consistent with this formulation, wherein we found that perceived severity of lifetime stressors mediated the relation between lifetime stressor exposure and poorer mental health for both AU and NA participants. Interestingly, while the same was true for symptoms of physical illnesses for NA participants, lifetime stressor exposure was not directly nor indirectly related to physical health for AU participants via perceived severity. This finding must be treated with caution as the magnitude of the difference between the diagnostic groups was not significant, but it is nonetheless notable insofar as physical health in autism may have a wider range of determinants. For example, autoimmune and gastrointestinal problems that are common in ASC may share aetiological pathways with ASC itself, and health complaints experienced by autistic people likely reflect complex systemic interactions (e.g., between metabolic and immunological pathways) in addition to influences from other risk factors such as anxiety and sleep disturbance (Tye et al., 2019). This causal complexity may be one explanation for why perceived stressor severity could potentially play a less prominent role in shaping the physical health of autistic adults than those in the general population.
In our fine-grained analyses examining how physical health is shaped by stressors involving different social-psychological characteristics, those characterised by interpersonal loss and by role change/disruption were likewise indirectly related to physical health (via perceived stressor severity) for NA but not AU participants. The importance of these social-psychological features of life stressors for health has been documented (e.g., Stewart et al., 2019), with role change/disruption stressors such as caregiving responsibilities, in particular, being extensively linked with physical morbidity (Hawken et al., 2018). A significant diagnostic group difference for role change/disruption stressors revealed that although these stressors were perceived as being more severe by AU participants, the relation between exposure to these stressors and their perceived severity—as well as the relation between the perceived severity of these stressors and physical health—was significantly stronger for NA than autistic individuals. That diagnostic status was directly related to the perceived severity of these stressors but did not interact with lifetime stressor exposure suggests that these stressors were perceived as more severe by AU people regardless of the degree of exposure. This is consistent with the group difference previously observed in the perceived severity of life-threatening situations as a stressor domain. The only stressors that exerted indirect effects on physical health in the AU group were those involving physical danger.
Stressor types that exerted indirect effects on mental health (via lifetime perceived stressor severity) were those involving interpersonal loss and role change/disruption (both diagnostic groups), physical danger (NA participants only), entrapment (AU participants only), and role change/disruption (both diagnostic groups). There were three types of stressors that were directly related to mental health in AU participants, and although the direct effects of humiliation and entrapment on mental health did not survive correction for multiple comparisons, the direct effect of role change/disruption did. That role change/disruption stressors exert a direct effect on mental health aside from their indirect effect via perceived stressor severity is intriguing. One possibility is that these direct effects on mental health may arise from the additional impacts that role change/disruption stressors have on other aspects of an individual’s life, such as their independence, self-worth, and social connectedness. Given the indirect associations we observed between physically dangerous stressors and physical health for both diagnostic groups, it is intriguing that for mental health, a highly significant moderating effect of diagnosis revealed that the perceived severity of these stressors had an effect only for NA individuals. This finding suggests that although these stressors were perceived as being more severe by AU participants and that this perception was associated with physical health, it was not a strong contributor to mental health symptomatology in AU participants. This disconnect between the greater lifetime perceived severity of physically dangerous stressors co-occurring with minimal mental health impact is another avenue for future research and may reflect the importance of other factors for influencing mental health in autism, such as intolerance of uncertainty and sensory sensitivities (South & Rodgers, 2017).
Regarding stressor perception and its health consequences in autism, the present analysis suggests that greater lifetime perceived severity of physically dangerous stressors may degrade physical health, and that greater lifetime perceived severity of interpersonal loss, entrapment, and role change/disruption stressors may degrade mental health. Although the inferred directionality in these associations must be investigated in future research, these findings, along with the observed relation between total perceived stressor severity and mental health, have important clinical implications. Specifically, while every effort should be made to target the societal inequalities and risks that lead to greater stressor exposure in autism, stress perceptions are a modifiable target for reducing stress-related health problems. Relevant interventions may thus include those that address intrapersonal processes that underlie or promote heightened perceptions of stressor severity in autism, including cognitive rigidity, poor emotional awareness, maladaptive coping styles, and reduced self-efficacy (Hirvikoski & Blomqvist, 2015; Kerns et al, 2015). Interventions that enhance reappraisal skills, self-efficacy, and perceived resilience may also help mitigate the negative impact that exaggerated perceived stressor severity has on mental and physical health (Jamieson et al., 2018; Liu et al., 2019). Whether interventions with an interpersonal flavour might also be valuable leads us to consider the impact of interpersonal factors on relations between stressor exposure, perception and health.
Loneliness and social support as moderators of the stress-health link
We investigated whether loneliness and social support moderated stress-health links in this sample given prior research showing that these processes modify the effects of stressor exposure on health in the general public (Cohen & Wills, 1985; Hawkley & Cacioppo, 2010). Loneliness, which itself predicts mental and physical ill health in the general public (Rico-Uribe et al., 2018), has been associated with suicide (Cassidy et al., 2018), self-harm and psychopathology (Hedley et al., 2018) in autism. Indeed, lonely individuals have fewer social buffers to help lessen their negative appraisal of stressors (Cohen & Wills, 1985); they also exhibit a negative cognitive bias that may exacerbate negative appraisals (Hawkley & Cacioppo, 2010). Loneliness also reduces the availability of support to help the individual cope with their perception of the stressor, and increases the likelihood of engaging in maladaptive coping strategies that can exacerbate its health impact.
In the present data, loneliness was directly related to greater lifetime perceived stressor severity and to poorer mental health (a main effect) but did not strengthen (i.e., moderate) associations between lifetime stressor exposure and perceived stressor severity, or between perceived stressor severity and poorer health. Again, this finding suggests a disconnect between actual stressor exposure and perceived stressor severity insofar as people who were highly lonely, which tended to be the case particularly for our AU participants, had greater perceived stressor severity regardless of their degree of actual stressor exposure. When examining the association between perceived stressor severity and mental health, we found that both perceived stressor severity and loneliness contributed unique variance to this outcome, highlighting each as distinct targets for intervention.
Social support has been theorised to exert both main effects and moderating effects on stress and health (Cohen & Wills, 1985): while greater social support may directly predict lower perceived stress and/or better health, it is also proposed to weaken (“buffer”) the relation between stressor exposure and perceived stressor severity, and the relation between perceived stressor severity and health impact. With reference to the former association, we indeed observed main effects where higher levels of appraisal, belonging, and tangible support were related to lower levels of lifetime perceived stressor severity. Moderating effects of appraisal and tangible support were, however, in opposition to the expected buffering effect: in fact, the association between stressor exposure and perceived stressor severity was strongest for AU and NA participants reporting the highest appraisal and tangible support. With reference to the association between perceived stressor severity and health impact, there were no main effects of loneliness or social support on physical health, or moderation effects on the stress-physical health link. For mental health, however, combined moderation effects of appraisal support, belonging support, and tangible support with diagnosis were consistent with our hypotheses: the relation between perceived stressor severity and mental health was weaker at higher levels of social support and even non-significant for autistic people with the highest levels of support.
This latter finding highlights the value of supportive relationships for mental health in autism and points to the importance of having people to talk to (appraisal support), to do things with (belonging support), and to provide material aid (tangible support) for helping maintain wellbeing. However, the unexpected moderating effect of appraisal and tangible support on the relation between lifetime stressor exposure and perceived severity requires further consideration. In part, that relations between stressor exposure and perceived stressor severity were stronger in those with higher levels of appraisal and tangible support likely reflects the aforemention observation that AU participants (more likely to score in the lower tertiles for each type of social support) tended to perceive stressors as more stressful even when they did not experience more of them. Buffering effects are highly sensitive to statistical approach, measurement tools, populations, and needs evoked by the stressor (Cohen & Wills, 1985). It must also be considered that for all participants alike, having more social support might not reduce the likelihood that stressors encountered would be perceived as stressful. There are a multitude of ways that perceived social support can fail to manifest in actual support (Schwarzer & Leppin, 1991). Aside from over- or under-estimations of existing support, there may be discrepancies in individuals’ ability to mobilise support or in the nature of the support mobilised. Some of these scenarios may reflect stress incurred by the social support itself or by the process of accessing it. More broadly, these findings highlight that social relationships are not always beneficial as assumed and that additional research is needed to examine differences between perceived support, actual support, ability to mobilize support, the effects of approach on support received, and the efficacy/cost of accessing support, especially in autism.
Notably, diagnosis was directly related to mental health, as opposed to strengthening its association with perceived stressor severity. In fact, diagnosis made this association more tenuous, which may, again, reflect the importance of additional variables that render the association between stressor perception and mental health less predictable in autism. Correlation coefficients and significance values for the association between diagnosis and mental health changed markedly depending on the second moderator in the model: when diagnosis was modelled in conjunction with loneliness, loneliness explained more of the variance in mental health. Indeed, our post-hoc mediation analysis revealed that being autistic was significantly associated with greater loneliness and lower levels of appraisal, belonging and tangible support. The relationship between autistic status and poorer mental health was mediated by loneliness.
This mediation effect, along with other studies highlighting the role of loneliness in psychopathology in autism (e.g., Cassidy et al, 2018), emphasises the importance of helping autistic people form supportive relationships. Although social support did not weaken the association between stressor exposure and perceived severity, all three types of support were associated with greater perceived stressor severity which, as we previously noted, was related to poorer mental health. Furthermore, each type of support reduced the negative impact of stressor severity on mental health. The gap between perceiving support and benefitting from it, though, suggests the need for interventions that focus on both being aware of and also effectively accessing support.
Strengths, limitations, and future directions
To our knowledge, the present study is the first to comprehensively assess stressors experienced by autistic individuals over the lifespan, to examine associations between stressor exposure and health, and the influence of loneliness and social support on said relations. However, several limitations should also be noted. First, given the cross-sectional nature of this study, conclusions regarding directionality and causality cannot be made. Relatedly, a second limitation is that lifetime stress data were based on self-report, which could be subject to cognitive, memory, and reporting biases (for e.g., if participants in greater distress were inclined to remember more stressful life events). In comparison to other stress assessment tools, the STRAIN has demonstrated greater consistency over time and greater predictive value for independent, investigator-assessed outcomes (Monroe & Slavich, 2020); moreover, it assesses moderate-to-major life stressors which research has shown can be reliably recalled. Nevertheless, to increase confidence in participant recall, future research could pair interview-based assessment tools like the STRAIN with physiological indices of neuroendocrine functioning, which would also afford greater scrutiny of the mechanisms through which stress affects health. Rather than general psychiatric and physical symptomatology, future research should examine the predictive utility of the STRAIN for specific conditions and/or physiological indices of health, ideally within a longitudinal design.
To avoid multicollinearity when examining direct and indirect effects of specific stressors, we examined variables sequentially for physical and then mental health. Although this increased confidence in our statistical approach, future research could consider these associations in a unified model. Although we adjusted for multiple comparisons, false positives are possible and future studies could take a more targeted approach to address these issues.
Stratifying analyses by sex was negated by the disproportionate representation of both NA and AU women. We know, however, that sex is associated with stressor exposure, stressor perception and health outcomes (Slavich & Shields, 2018), so future studies should model effects of this variable and its interactions with diagnostic status. A bimodal distribution of female diagnoses exists where autism is diagnosed in young girls only when they present more stereotyped and obvious presentations, whereas individuals with more subtle difficulties and high cognitive ability are diagnosed much later, or indeed in adulthood (Lehnhardt et al, 2016). Our late-diagnosed sample may be less representative of autistic women diagnosed as children, as late diagnoses are suggestive of stronger verbal IQ, executive function, and camouflage skills (Hull et al., 2020). Given that camouflage is associated with deleterious health outcomes (Cage & Troxell-Whitman, 2019), its interaction with lifetime stress may be important to examine. The generalizability of the present results cannot be extended to autistic cohorts unrepresented here, including individuals with literacy difficulties, without technological access, and those with intellectual disability. In predicting health outcomes, there may be less traditional, autism-specific stressors which should be accounted for and whose impact may vary in accordance with sex and other intrapersonal factors, such as executive function, adaptive abilities, and emotion regulation skills.
Broadly speaking, a comprehensive portrait of the health disparity between autistic and non-autistic individuals requires considering a multitude of interacting variables, from the genome to metabolic function to the social environment in which autistic people live (Botha & Frost, 2018; Tye et al., 2019). Such work should also delineate the contributions of variables that are strongly correlated with stressor exposure, such as socioeconomic status and health behaviours (Cohen et al., 2010), and which may contribute to differences in stress exposure, stress perception, and health in both autistic and non-autistic individuals. Adult socioeconomic status and health behaviours, along with perceptions of stress, are embedded in a trajectory reaching back to childhood and involving neurodevelopment (Nurius et al., 2019). A fuller understanding of adult wellness, illness, and psychopathology in autism, through the lens of stress exposure, should consider such factors and their neurobiological and psychological consequences.
Conclusion
Notwithstanding these limitations, this study is, to our knowledge, the first to comprehensively assess the lifetime stress exposure profiles of autistic individuals and examine factors moderating and mediating relations between lifetime stress exposure and mental and physical health. As hypothesized, we found that autistic adults experience greater exposure to many types of life stressors and perceive these stressors as more severe. The relative importance of perceived stressor severity over actual exposure highlights the potential for targeting stress appraisal to help reduce the negative effects of stress in autistic individuals. Moreover, our findings showing that loneliness and social support influence the negative effects of perceived stressor severity on health suggest the potential importance of targeting these processes to enhance health in autism. Looking forward, future research should continue utilising methodologically and conceptually rigorous instruments for assessing lifetime stress exposure, and further examine the multi-level mechanisms by which life stressors might contribute to elevated morbidity and mortality risk in autism.
Supplementary Material
Acknowledgements
We thank our participants and the owners of the Facebook groups where we advertised our research. We also thank the students who collected some data used here, including Miranda Hart and Imogen Finkle.
Footnotes
Terminology in this field is hotly debated. We employ identity-first language, which is preferred by members of the autistic community who responded to studies on this topic (Bury et al., 2020).
Multicollinearity, checked for each level where stressor exposure was controlled for while comparing perceived stressor severity, never exceeded 4 in VIF or fell below .250 in tolerance for these two types of variable.
References
- Allen KA, Kern ML, Rozek CS, McInereney D, & Slavich GM (in press). Belonging: A review of conceptual issues, an integrative framework, and directions for future research. Australian Journal of Psychology. 10.1080/00049530.2021.1883409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Mazefsky CA, & Eack SM (2018). The combined impact of social support and perceived stress on quality of life in adults with autism spectrum disorder and without intellectual disability. Autism, 22, 703–711. 10.1177/1362361317703090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Mazefsky CA, Minshew NJ, & Eack SM (2015). The relationship between stress and social functioning in adults with autism spectrum disorder and without intellectual disability. Autism Research, 8(2), 164–173. 10.1002/aur.1433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Minshew NJ, Mazefsky CA, & Eack SM (2017). Perception of life as stressful, not biological response to stress, is associated with greater social disability in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47, 1–16. 10.1007/s10803-016-2910-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botha M, & Frost DM (2018). Extending the minority stress model to understand mental health problems experienced by the autistic population. Society and Mental Health, 10, 20–34. 10.1177/2156869318804297 [DOI] [Google Scholar]
- Brede J, Remington A, Kenny L, Warren K, & Pellicano E (2017). Excluded from school: Autistic students’ experiences of school exclusion and subsequent re-integration into school. Autism & Developmental Language Impairments, 2. 10.1177/2396941517737511 [DOI] [Google Scholar]
- Bury S, Jellett R, Spoor J, & Hedley D (2020). “It defines who I am” or “It’s something I have”: what language do [autistic] australian adults [on the autism spectrum] prefer? Journal of Autism & Developmental Disorders, 1–11. 10.1007/s10803-020-04425-3 [DOI] [PubMed] [Google Scholar]
- Cage E, & Troxell-Whitman Z (2019). Understanding the reasons, contexts and costs of camouflaging for autistic adults. Journal of Autism and Developmental Disorders, 49(5), 1899–1911. 10.1007/s10803-018-03878-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cashin A, Buckley T, Trollor JN, & Lennox N (2018). A scoping review of what is known of the physical health of adults with autism spectrum disorder. Journal of Intellectual Disabilities, 22(1), 96–108. 10.1177/1744629516665242 [DOI] [PubMed] [Google Scholar]
- Cassidy S, Bradley L, Shaw R, & Baron-Cohen S (2018). Risk markers for suicidality in autistic adults. Molecular Autism, 9(1), 42. 10.1186/s13229-018-0226-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, Chen E, & Matthews KA (2010). Childhood socioeconomic status and adult health. Annals of the New York Academy of Sciences, 1186(1), 37–55. 10.1111/j.1749-6632.2009.05334.x [DOI] [PubMed] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, & Hoberman HM (1985). Measuring the functional components of social support. In Social Support: Theory, Research and Applications (pp. 73–94). Springer. 10.1007/978-94-009-5115-0_5 [DOI] [Google Scholar]
- Cohen S, & Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- Doi S, Ito M, Takebayashi Y, Muramatsu K, & Horikoshi M (2018). Factorial validity and invariance of the Patient Health Questionnaire (PHQ)-9 among clinical and non-clinical populations. PLoS ONE, 13(7), e0199235. 10.1371/journal.pone.0199235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ee D, Hwang Y. I. (Jane), Reppermund S, Srasuebkul P, Trollor JN, Foley K-R, & Arnold SRC (2019). Loneliness in adults on the autism apectrum. Autism in Adulthood, 1(3), 182–193. 10.1089/aut.2018.0038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epel ES, Crosswell AD, Mayer SE, Prather AA, Slavich GM, Puterman E, & Mendes WB (2018). More than a feeling: A unified view of stress measurement for population science. Frontiers in Neuroendocrinology, 49, 146–169. 10.1016/j.yfrne.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin MS, Groden J, Velicer WF, & Diller A (2007). Brief report: Validating the Stress Survey Schedule for persons with autism and other developmental disabilities. Focus on Autism and Other Developmental Disabilities, 22(3), 183–189. 10.1177/10883576070220030501 [DOI] [Google Scholar]
- Griffiths S, Allison C, Kenny R, Holt R, Smith P, & Baron-Cohen S (2019). The Vulnerability Experiences Quotient (VEQ): A study of vulnerability, mental health and life satisfaction in autistic adults. Autism Research, 12, 1516–1528. 10.1002/aur.2162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmuth E, Silletta E, Bailey A, Adams T, Beck C, & Barbic SP (2018). Barriers and facilitators to employment for adults with autism: A scoping review. Annals of International Occupational Therapy, 1(1), 31–40. 10.3928/24761222-20180212-01 [DOI] [Google Scholar]
- Hawken T, Turner-Cobb J, & Barnett J (2018). Coping and adjustment in caregivers: A systematic review. Health Psychology Open, 5(2), 2055102918810659. 10.1177/2055102918810659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2017). An Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-based Approach (Second Edition). Guilford Press. https://doi.org/978-1-60918-230-4 [Google Scholar]
- Hedley D, Uljarevic M, Wilmot M, Richdale A, & Dissanayake C (2018). Understanding depression and thoughts of self-harm in autism: a potential mechanism involving loneliness. Research in Autism Spectrum Disorders, 46, 1–7. 10.1016/j.rasd.2017.11.003 [DOI] [Google Scholar]
- Hedley D, Uljarević M, Wilmot M, Richdale A, & Dissanayake C (2017). Brief report: Social support, depression and suicidal ideation in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47, 3669–3677. 10.1007/s10803-017-3274-2 [DOI] [PubMed] [Google Scholar]
- Hirvikoski T, & Blomqvist M (2015). High self-perceived stress and poor coping in intellectually able adults with autism spectrum disorder. Autism, 19(6), 752–757. 10.1177/1362361314543530 [DOI] [PubMed] [Google Scholar]
- Hirvikoski T, Mittendorfer-Rutz E, Boman M, Larsson H, Lichtenstein P, & Bölte S (2016). Premature mortality in autism spectrum disorder. British Journal of Psychiatry, 208(3), 232–238. 10.1192/bjp.bp.114.160192 [DOI] [PubMed] [Google Scholar]
- Hong J, Bishop-Fitzpatrick L, Smith LE, Greenberg JS, & Mailick MR (2016). Factors associated with subjective quality of life of adults with autism spectrum disorder: Self-report versus maternal reports. Journal of Autism and Developmental Disorders, 46(4), 1368–1378. 10.1007/s10803-015-2678-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoover DW, & Kaufman J (2018). Adverse childhood experiences in children with autism spectrum disorder. Current Opinion in Psychiatry, 31(2), 128–132. 10.1097/YCO.0000000000000390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull L, Petrides KV, & Mandy W (2020). Cognitive predictors of self-reported camouflaging in autistic adolescents. Autism Research, 14, 523–532. 10.1002/aur.2407 [DOI] [PubMed] [Google Scholar]
- Jamieson JP, Crum AJ, Goyer JP, Marotta ME, & Akinola M (2018). Optimizing stress responses with reappraisal and mindset interventions: an integrated model. Anxiety, Stress and Coping, 31(3), 245–261. 10.1080/10615806.2018.1442615 [DOI] [PubMed] [Google Scholar]
- Kerns CM, Newschaffer CJ, & Berkowitz SJ (2015). Traumatic childhood events and autism spectrum disorder. Journal of Autism and Developmental Disorders, 45, 3475–3486. 10.1007/s10803-015-2392-y [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, Walters EE, & Zaslavsky AM (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32, 959–976. 10.1017/S0033291702006074 [DOI] [PubMed] [Google Scholar]
- King C, & Murphy GH (2014). A systematic review of people with autism spectrum disorder and the Criminal Justice System. Journal of Autism and Developmental Disorders, 44(11), 2717–2733. 10.1007/s10803-014-2046-5 [DOI] [PubMed] [Google Scholar]
- Lam JCW, Shields GS, Trainor BC, Slavich GM, & Yonelinas AP (2019). Greater lifetime stress exposure predicts blunted cortisol but heightened DHEA responses to acute stress. Stress and Health, 35, 15–26. 10.1002/smi.2835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R, & Folkman S (1984). Stress, appraisal and coping. Springer. [Google Scholar]
- Lebois LA, Hertzog C, Slavich GM, Barrett LF, & Barsalou LW (2016). Establishing the situated features associated with perceived stress. Acta Psychologica, 169, 119–132. 10.1016/j.actpsy.2016.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehnhardt FG, Falter CM, Gawronski A, Pfeiffer K, Tepest R, Franklin J, & Vogeley K (2016). Sex-related cognitive profile in autism spectrum disorders diagnosed late in life: implications for the female autistic phenotype. Journal of Autism and Developmental Disorders, 46(1), 139–154. 10.1007/s10803-015-2558-7 [DOI] [PubMed] [Google Scholar]
- Liu JJW, Ein N, Gervasio J, & Vickers K (2019). The efficacy of stress reappraisal interventions on stress responsivity: A meta-analysis and systematic review of existing evidence. PLoS ONE, 14(2). 10.1371/journal.pone.0212854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maïano C, Normand CL, Salvas MC, Moullec G, & Aimé A (2016). Prevalence of school bullying among youth with autism spectrum disorders: a systematic review and meta-analysis. Autism Research, 9(6), 601–615. 10.1002/aur.1568 [DOI] [PubMed] [Google Scholar]
- Mason D, Ingham B, Urbanowicz A, Michael C, Birtles H, Woodbury-Smith M, Brown T, James I, Scarlett C, Nicolaidis C, & Parr JR (2019). A systematic review of what barriers and facilitators prevent and enable physical healthcare services access for autistic adults. Journal of Autism and Developmental Disorders, 49(8), 3387–3400. 10.1007/s10803-019-04049-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS (2005). Stressed or stressed out: What is the difference? Journal of Psychiatry and Neuroscience, 30(5), 315–318. [PMC free article] [PubMed] [Google Scholar]
- Merz EL, Roesch SC, Malcarne VL, Penedo FJ, Llabre MM, Weitzman OB, Navas-Nacher EL, Perreira KM, Gonzalez F, Ponguta LA, Johnson TP, & Gallo LC (2014). Validation of Interpersonal Support Evaluation List-12 (ISEL-12) scores among English- and Spanish-speaking Hispanics/Latinos from the HCHS/SOL Sociocultural Ancillary Study. Psychological Assessment, 26(2), 384–394. 10.1037/a0035248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, & Slavich GM (2020). Major life events: A review of conceptual, definitional, measurement issues, and practices. In Harkness KL & Hayden EP (Eds.), The Oxford handbook of stress and mental health (pp. 7–26). Oxford University Press. 10.1093/oxfordhb/9780190681777.013.1 [DOI] [Google Scholar]
- Nurius PS, Fleming CM, & Brindle E (2019). Life course pathways from adverse childhood experiences to adult physical health: a structural equation model. Journal of Aging and Health, 31(2), 211–230. 10.1177/0898264317726448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JJ, Sung HY, Max W, Shi Y, & Ong M (2012). Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. International Journal of Methods in Psychiatric Research, 21(2), 88–97. 10.1002/mpr.1349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rico-Uribe LA, Caballero FF, Martín-María N, Cabello M, Ayuso-Mateos JL, & Miret M (2018). Association of loneliness with all-cause mortality: A meta-analysis. PLoS ONE, 13(1), e0190033. 10.1371/journal.pone.0190033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. Journal of Personality Assessment, 66(1), 20–40. https://doi.org/14.2327 [DOI] [PubMed] [Google Scholar]
- Schat ACH, Kelloway EK, & Desmarais S (2005). The Physical Health Questionnaire (PHQ): Construct validation of a self-report scale of somatic symptoms. Journal of Occupational Health Psychology, 10, 363–381. 10.1037/1076-8998.10.4.363 [DOI] [PubMed] [Google Scholar]
- Schwarzer R, & Leppin A (1991). Social support and health: A theoretical and empirical overview. Journal of Social and Personal Relationships, 8(1), 99–127. 10.1177/0265407591081005 [DOI] [Google Scholar]
- Shields GS, & Slavich GM (2017). Lifetime stress exposure and health: A review of contemporary assessment methods and biological mechanisms. Social and Personality Psychology Compass, 11, e12335. 10.1111/spc3.12335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM (2019). Stressnology: The primitive (and problematic) study of life stress exposure and pressing need for better measurement. Brain, Behavior, and Immunity, 75, 3–5. 10.1016/j.bbi.2018.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM (2020). Social safety theory: A biologically based evolutionary perspective on life stress, health, and behavior. Annual Review of Clinical Psychology, 16, 265–295. 10.1146/annurev-clinpsy-032816-045159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, & Shields GS (2018). Assessing lifetime stress exposure using the Stress and Adversity Inventory for Adults (Adult STRAIN): An overview and initial validation. Psychosomatic Medicine, 80(1), 17–27. 10.1097/PSY.0000000000000534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T, Johns-Wolfe E, Shields GS, Malat J, Jacquez F, & Slavich GM (2020). Associations between lifetime stress exposure and prenatal health behaviors. Stress and Health, 36, 384–395. 10.1002/smi.2933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- South M, & Rodgers J (2017). Sensory, emotional and cognitive contributions to anxiety in autism spectrum disorders. Frontiers in Human Neuroscience, 11, 20. 10.3389/fnhum.2017.00020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart JG, Shields GS, Esposito EC, Cosby EA, Allen NB, Slavich GM, & Auerbach RP (2019). Life stress and suicide in adolescents. Journal of Abnormal Child Psychology, 47, 1707–1722. 10.1007/s10802-019-00534-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tye C, Runicles AK, Whitehouse AJO, & Alvares GA (2019). Characterizing the interplay between autism spectrum disorder and comorbid medical conditions: An integrative review. Frontiers in Psychiatry, 9, 751. 10.3389/fpsyt.2018.00751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino BN, Bowen K, Carlisle M, & Birmingham W (2012). Psychological pathways linking social support to health outcomes: a visit with the “ghosts” of research past, present, and future. Social Science & Medicine, 74(7), 949–957. 10.1016/j.socscimed.2011.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, & Gadow KD (2010). Exploring the nature and function of anxiety in youth with autism spectrum disorders. Clinical Psychology: Science and Practice, 17, 281–292. 10.1111/j.1468-2850.2010.01220.x [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.