Abstract
Background
Prone positioning in non-intubated spontaneously breathing patients is becoming widely applied in practice alongside noninvasive respiratory support. This systematic review and meta-analysis evaluates the effect, timing, and populations that might benefit from awake proning regarding oxygenation, mortality, and tracheal intubation compared with supine position in hypoxaemic acute respiratory failure.
Methods
We conducted a systematic literature search of PubMed/MEDLINE, Cochrane Library, Embase, CINAHL, and BMJ Best Practice until August 2021 (International Prospective Register of Systematic Reviews [PROSPERO] registration: CRD42021250322). Studies included comprise least-wise 20 adult patients with hypoxaemic respiratory failure secondary to acute respiratory distress syndrome or coronavirus disease (COVID-19). Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed, and study quality was assessed using the Newcastle–Ottawa Scale and the Cochrane risk-of-bias tool.
Results
Fourteen studies fulfilled the selection criteria and 2352 patients were included; of those patients, 99% (n=2332/2352) had COVID-19. Amongst 1041 (44%) patients who were placed in the prone position, 1021 were SARS-CoV-2 positive. The meta-analysis revealed significant improvement in the PaO2/FiO2 ratio (mean difference –23.10; 95% confidence interval [CI]: –34.80 to 11.39; P=0.0001; I2=26%) after prone positioning. In patients with COVID-19, lower mortality was found in the group placed in the prone position (150/771 prone vs 391/1457 supine; odds ratio [OR] 0.51; 95% CI: 0.32–0.80; P=0.003; I2=48%), but the tracheal intubation rate was unchanged (284/824 prone vs 616/1271 supine; OR 0.72; 95% CI: 0.43–1.22; P=0.220; I2=75%). Overall proning was tolerated for a median of 4 h (inter-quartile range: 2–16).
Conclusions
Prone positioning can improve oxygenation amongst non-intubated patients with acute hypoxaemic respiratory failure when applied for at least 4 h over repeated daily episodes. Awake proning appears safe, but the effect on tracheal intubation rate and survival remains uncertain.
Keywords: ARDS, awake prone position, COVID-19, hypoxaemic respiratory failure, noninvasive respiratory support, SARS-CoV-2, tracheal intubation
Editor's key points.
-
•
Prone positioning in non-intubated, spontaneously breathing patients is widely applied alongside noninvasive respiratory support. Its effectiveness in improving oxygenation and reducing intubation rate and mortality, and its tolerability, timing, and optimal duration are unclear.
-
•
Awake prone positioning appears to be a safe and tolerable intervention for non-intubated patients with hypoxaemic respiratory failure attributable to acute respiratory distress syndrome or COVID-19.
-
•
Potential benefits include improved oxygenation and mortality rate, but no significant effects on incidence of intubation or critical care admission were found.
-
•
Future research should explore the optimal frequency, duration, and appropriate population for application of awake prone positioning with noninvasive respiratory support. Large, well-designed trials are needed to explore the subject more rigorously and to confirm clinical effectiveness.
Prone positioning is an established evidence-based practice for mechanically ventilated patients with moderate-to-severe acute respiratory distress syndrome (ARDS),1 but it is a novel intervention in spontaneously breathing patients. Physiologically, prone positioning may promote lung recruitment of the posterior dorsal regions because of reversal of atelectasis.2 Proning may also generate a more homogeneous ventilation reducing lung strain attributable to changes in pleural pressure and pleural space distribution,3 and therefore favouring ventilation/perfusion (V/Q) matching4 and reducing shunting.5
Awake prone positioning in hypoxaemic acute respiratory failure (ARF) can be a feasible and safe intervention6 , 7 alongside noninvasive ventilation (NIV) and high-flow oxygen. Despite its anecdotal and theoretical benefit in improving oxygenation, it has not been widely applied in practice until the SARS-CoV-2 pandemic. The unprecedented surge of patients requiring critical care support generated significant pressure on ICU capacity. Clinicians needed to balance local resources with the rapid demand, and awake prone positioning was initially a pragmatic approach with the goal to improve oxygenation, prevent intubation, and potentially reduce the need for ICU admission.8 , 9
The natural progression and the pathophysiological changes of ARDS and COVID-19 respiratory failure affect critically ill patients with different degrees of severity, and 42–58% will require intubation and invasive mechanical ventilation.10 , 11 Invasive mechanical ventilation may lead to additional risks, such as ventilation-associated pneumonia and ventilation-induced lung injury, and its associated mortality rate may reach 27–45%.11 , 12
Several observational studies support the use of awake prone positioning to improve oxygenation for spontaneously breathing patients affected by respiratory failure.13, 14, 15, 16, 17, 18 Its effectiveness in reducing intubation rate and mortality remains unclear,19, 20, 21, 22, 23 and also its tolerability,24 , 25 timing, and optimal duration.26 A general potential concern is that APP may worsen self-inflicted lung injury and delay intubation and mechanical ventilation.19 , 27 It remains unclear if there is a specific window for awake prone positioning to improve oxygenation (in terms of both time and levels of hypoxia), or if there exist subgroups of responders and non-responders.
This review and meta-analysis aims to further evaluate the hypothesis that awake prone positioning in spontaneously breathing patients with ARF is associated with improvement in oxygenation and rate of tracheal intubation and mortality. We also investigated potential risks and limitations associated with awake prone positioning. This work will inform future studies and allow evaluation of potentially effective interventions for improving the management of spontaneously breathing patients with ARF.
Methods
This study was registered on the International Prospective Register of Systematic Reviews (PROSPERO) of the National Institute for Health Research (NIHR), and it is published under registration ID CRD42021250322.
Search strategy
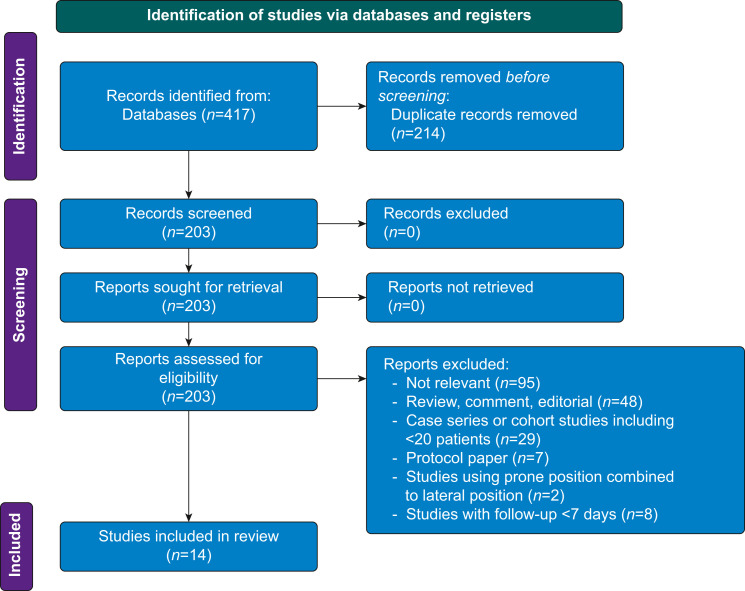
Two reviewers (BF and AP) independently identified all potentially relevant studies published from January 2010 to August 2021. The search strategy involved a combination of keywords as follows: (i) awake prone positioning, (ii) acute respiratory distress or ARDS or hypoxaemic respiratory failure, or (iii) coronavirus 2019 or COVID-19 or SARS-CoV-2. The search ran through electronic databases, including PubMed/MEDLINE, Cochrane Central Register of Controlled Trials, Embase, CINAHL, BMJ Best Practice, WHO SARS-CoV-2 Research Database, National Institute for Health and Care Excellence (NICE), and Cambridge University Press Coronavirus Free Access Collection. The references were identified against our inclusion criteria and duplicates removed, as shown in Figure 1 . There were no language restrictions. Titles and abstracts were reviewed independently in duplicate (BF and AP) for selection of full-text review. Both reviewers also independently reviewed the full text of relevant studies and decided on eligibility. Disagreements were resolved through discussion or by consensus with a third reviewer (ZP). The references retrieved were saved into a customised Excel (Microsoft 365®, Microsoft Corp., Redmond, WA, USA) spreadsheet. This report follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines.28
Fig 1.
Search strategy flow diagram.
Study inclusion criteria
We selected all design studies, including at least 20 participants. Studies were not selected on methodological quality. Eligible studies included adult patients (age ≥18 yr old) with acute hypoxaemic respiratory failure attributable to ARDS or COVID-19 who received PP alongside with any oxygen delivery device, including simple oxygen therapy, high-flow nasal oxygen, CPAP, and NIV. We included patients of any gender admitted to any ward or to ICU.
We excluded studies (i) that applied prone position in intubated patients, (ii) that involved the application of prone positioning combined or mixed to lateral positioning, and (iii) with a follow-up shorter than 7 days.
Data extraction and study quality
Data extraction was undertaken independently and in duplicate (BF and AP) to avoid bias. Data abstracted were stored into a customised Excel database, including study design, patient characteristics, intervention, and outcomes.
Observational studies were assessed for evidence of bias using the Newcastle–Ottawa Scale (NOS),29 and RCTs were assessed with the Cochrane risk-of-bias tool. The GRADE (Grading of Recommendations Assessment), Development and Evaluation guidelines were used for rating the quality of evidence.30
Outcomes
We analysed the following outcomes based on consensus. The primary outcome considered was the change in oxygenation pre and post PP reported as Pao2/FiO2 (P/F) ratio or SpO2/FiO2 (S/F) ratio. The secondary outcomes included the rate of tracheal intubation, mortality, ICU admission, limitations, and adverse events (such as line displacement and pressure sores).
Subgroup analysis
A subgroup analysis was planned based on P/F ratio (P/F ratio <150 mm Hg vs P/F ratio >150 mm Hg) and length of prone positioning (PP <4 h vs PP >4 h).
Study analysis
Where P/F ratio was not available, S/F ratio was transformed into P/F ratio following the validated standard formula.31
We reported dichotomous outcomes using risk ratio and continuous outcomes using mean difference (MD). If mean and standard deviation were not available, data were assessed in the median/inter-quartile range (IQR) and transformed into standard MD format for further comparison.32 The inverse variance method was used to pool the MDs to yield an overall effect size with 95% confidence intervals (CIs).
For each analysis, studies were weighted using the inverse variance method, and data were pooled using a random effects meta-analyses model accounting for the incidence.33 We assessed clinical heterogeneity amongst studies qualitatively, and statistical heterogeneity using the χ2 test and I 2 statistical measure.32 , 34 P-value equal to 0.05 or less was considered to be statistically significant. We assessed publication bias by visually examining funnel plots of treatment effect vs study precision. All statistical data analyses were performed using the statistical software package Review Manager 5.4 (RevMan 5.4.1) from Cochrane Collaboration (Oxford, UK).
Results
A total of 417 studies were identified by the search strategy, and after removal of duplicates 14 studies met the inclusion criteria, as shown in Figure 1. The study characteristics are summarised in Table 1 . All studies were recent and published between 2020 and 2021, comprising patients with moderate-to-severe respiratory failure secondary to ARDS or COVID-19. In all, 2352 patients were included, of those 99% (n=2332/2352) had COVID-19. Amongst 1041 (44%) undergoing awake prone positioning, 1021 were SARS-CoV-2 positive.
Table 1.
Baseline characteristics of included studies. APP, awake prone positioning; ARDS, acute respiratory distress syndrome; BNP, brain natriuretic peptide; CI, confidence interval; COPD, chronic obstructive pulmonary disease; ED, emergency department; HFNO, high-flow nasal oxygen; IQR, inter-quartile range; NC, nasal cannula; NIV, noninvasive ventilation; NRM, non-rebreathing mask; NYHA, New York Heart Association; PC, prospective cohort; P/F, Pao2/FiO2 ratio; PP, prone position; RC, retrospective cohort; RR, risk ratio; sd, standard deviation.
| Authors | Design and country | N | Inclusion criteria | Exclusion criteria | Setting | Oxygen delivery mode | Protocol | Duration of APP session | Follow-up | Oxygenation pre- vs post-APP | Intubation rate, n (%) | Mortality, n (%) | Limitations |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coppo and colleagues13 (2020) | PC Italy Single centre |
56 47 prone 9 supine |
SARS-CoV-2 and hypoxaemia | Not collaborative, altered mental status, NYHA <II, increased BNP, COPD on home, NIV or O2, impending intubation |
ED Ward ICU |
Helmet, CPAP, reservoir mask, Venturi mask |
Assisted prone position encouraged for 3 h, to repeat up to 8 h day−1 | Median 3 h (3–4) up to seven sessions | Hospital discharge | P/F ratio: 163 mm Hg (sd 57) in supine position vs P/F ratio 179 mm Hg (sd 84) 1 h after resupination; P=0.290 | 18/47 (38%) for prone 5/9 (56%) for supine |
5/56 (9%) | 9% discomfort 4% worsening oxygenation 2% coughing |
| Ding and colleagues7 (2020) | PC China Multicentre |
20 prone | ARDS (viral pneumonia) P/F <200 and on NIV |
Requiring intubation | ICU | HFNO and NIV | >30 min, twice daily for 3 days | 2.4 [1.5] h for those not intubated 1.6 [0.5] h for those intubated |
Not reported | Not reported | 9/20 (45%) | 1/20 (5%) | 10% intolerance |
| Dubosh and colleagues16 (2021) | PC USA Single centre |
22 prone | SARS-CoV-2 Hypoxaemia |
Requiring intubation, altered conscious level, spinal instability, vomiting, confusion, inability to cooperate with staying in a prone position | ED | NC, face mask | As tolerated | Median: 2 h (IQR 1–3) | Hospital discharge | Not reported | 7/22 (32%) | 2/22 (9%) | 9/22 (41%) ICU admission |
| Elharrar and colleagues9 (2020) | PC France Single centre |
24 prone | SARS-CoV-2 Hypoxaemia |
Requiring intubation, altered consciousness | Ward | NC, face mask, HFNO | A single episode with no goal duration | 17% <1 h 21%: 1–3 h 63% >3 h |
10 days | No difference; P=0.530 | 5/24 (20.8%) | Not reported | 10/24 (42%) back pain |
| Ferrando and colleagues20 (2020) | PC Spain Multicentre |
199 55 prone 144 supine |
SARS-CoV-2 Hypoxaemia |
Not reported | ICU | HFNO | Prone position was only considered if the duration was >16 h day−1 regardless of the number of sessions | Unclear | 28 days | Not reported | 22/55 (40%) for prone 60/144 (42%) for supine |
(RR 1.04 [95% CI: 0.40–2.72]; P=0.92) | Trend in delay intubation |
| Padrao and colleagues 51 (2020) | RC Brazil Single centre |
166 57 prone 109 supine |
SARS-CoV-2 Hypoxaemia |
Need for intubation, haemodynamic instability, recent abdominal surgery, acute hypercapnic respiratory failure, unstable fractures, pregnancy, clinician judgement | ED Ward ICU | NC, face mask, HFNO, NIV | As tolerated | Unclear 29/57 (58%) >4 h |
15 days | Spo2/Fio2 ratio: 196 mm Hg [128, 254] supine vs 224 mm Hg [159, 307] 4 h after APP; P<0.001 | APP: 33/57 (58%) Control: 53/109 (49%) P=0.39 |
6/57 (11%) for prone 22/109 (20%) for supine P=0.26 |
3.5% accidental removal of peripheral lines |
| Thompson and colleagues15 (2020) | PC USA Single centre |
29 25 prone 4 refused |
SARS-CoV-2 Hypoxaemia |
Altered mental status, inability to turn without help, immediate intubation needed, mild hypoxaemia | HDU | NC, NRM | As tolerated over repeated episodes daily | 4 h (IQR: 1–24) in not intubated 6 h (IQR: 1–24) in intubated |
Up to 49 days or to hospital discharge | Not reported | 12/25 (48%) | 3/25 (12%) | 4/29 (14%) refusal |
| Zang and colleagues18 (2020) | PC China Single centre |
60 23 prone 37 supine |
SARS-CoV-2 Hypoxaemia |
Need for intubation, instability to self-position, basal lung disease, unstable spine, high ICP, severe burns, abdominal surgery, abdominal hypertension, cranial injury, tracheostomy, immune suppression, pregnant, imminent death | ICU | NC, HFNO, NIV | Evaluation of muscle strength and self-positioning Encouraged for 1–2 h per session for three to four times day−1 for 5 days |
9 h (IQR: 8–22) | 90 days | Not reported | APP: 8/23 (35%) Supine: 3/37 (8%) |
10/23 (43%) for prone 28/37 (76%) for supine |
Not reported |
| Ehrmann and colleagues 52 (2021) | RCT Mexico France USA Spain Ireland Canada |
564 prone 557 supine |
SARS-CoV-2 Hypoxaemia |
Unable or refused to provide informed consent, haemodynamic instability, severely obese with BMI >40 kg m−2, pregnant, had a contraindication to awake prone positioning | ICU, HDU ED Ward |
HFNO | As long and as frequently as possible each day | 5 h (IQR: 1.6–8.8) | 28 days | Spo2/Fio2 ratio significantly improved; P-value not reported | APP: 185/564 (33%) Supine: 223/557 (40%) RR: 0.75 (0.62–0.91) |
APP: 117/564 (21%) Supine: 132/557 (24%) RR: 0.87 (0.71–1.07) |
Incidence of skin breakdown, vomiting, and dislodged line was low and similar in both groups |
| Fazzini and colleagues14 (2021) | PC UK Single centre |
46 prone | SARS-CoV-2 Hypoxaemia |
Need for intubation, haemodynamic instability, recent abdominal surgery, acute hypercapnic respiratory failure, facial fractures, spinal instability, unstable fractures, TBI, pregnancy, not collaborative, clinician judgement | Ward | NC, face mask, HFNO, CPAP | Assisted prone position Encouraged as long as tolerated multiple daily sessions |
4 h (IQR: 1–14) | 90 days |
P/F ratio: 115 [43] mm Hg pre-PP vs 148 [70] mm Hg 1–2 h post-PP; P=0.025 Spo2/Fio2 ratio: 141 [37] mm Hg supine vs 188 [49] mm Hg 1–2 h post-PP; P<0.001 |
20/46 (43%) | 14/46 (30%) | 13% anxiety 11% discomfort ICU admission: (APP <1 h: 83%, 10/12 vs APP >1 h: 41%, 14/34; P=0.011) |
| Jouffroy and colleagues (2021) | RC France Multicentre |
379 40 prone 339 supine |
SARS-CoV-2 Hypoxaemia |
Not reported | ICU | Face mask, HFNO, CPAP | 3 h and twice daily when possible | 2.5 days (1.6–3.4) days Total of three sessions |
28 days | P/F (78 [68; 96] vs 63 [53; 77] mm Hg; P=0.004) | 16/44 (40%) HR 0.96; 95% CI: 0.49–1.88 |
23/40 (58%) HR 0.51; 95% CI: 0.16–1.16 |
Not reported |
| Nauka and colleagues22 (2021) | RC USA Multicentre |
41 prone | SARS-CoV-2 Hypoxaemia |
Not reported | Ward ICU |
NC, NRM, HFNO | Not reported | Unclear | Hospital discharge | Spo2/Fio2 ratio: 95 mm Hg (93–133) pre vs 95 mm Hg (92–100) post; P=0.800 | 20/41 (49%) | Not reported | Not reported |
| Rosén and colleagues46 (2021) | RCT Sweden Multi Centre |
75 39 control 36 treatment |
SARS-CoV-2 Hypoxaemia |
Inability to assume PP or semi-prone, immediate need for tracheal intubation, severe haemodynamic instability, previous intubation for COVID-19, pregnancy, terminal illness with less than 1 yr life expectancy, do-not-intubate order, inability to understand oral or written study information | Ward ICU | HFNO or NIV | Control group: APP was not encouraged but prescribed at clinician discretion Treatment group: at least 16 h day−1 Prone or semi prone position allowed Stopped if need for intubation, death, or clinically improved |
Control: 3.4 h (IQR: 1.8–8.4) Treatment: 9.0 h (IQR: 4.4–10.6) |
30 days | Not reported | Control: 13/39 (33%) Treatment: 12/36 (33%) HR: 1.01 (CI: 0.46–2.21); P=0.99 |
Control: 3/39 (8%) Treatment: 6/36 (17%) HR: 2.29 (CI: 0.57–9.14); P=0.30 |
Control: 9/39 (23%) pressure sores in lower back and gluteal region 1/39 (2.6%) cardiac arrest Treatment: 2/36 (6%) pressure sore from HFNO 2/36 (6%) cardiac arrest ICU admission: P=0.580 |
| Tonelli and colleagues17 (2021) | RC Italy Multi Centre |
114 38 prone 76 supine |
SARS-CoV-2 Hypoxaemia |
Not collaborative, altered mental status, NYHA <II, increased BNP, COPD on home, NIV or O2, impending intubation | ICU | HFNO, CPAP, NIV | Assisted prone position Encouraged as long as tolerated aiming for 3 h for one to four sessions a day |
Unclear | 30 days | Not reported | 7/38 (18%) for prone 30/76 (39%) for supine |
5/38 (13%) for prone 17/76 (23%) for supine |
ICU admission: (HR 1.14 [0.96, 1.34]; P=0.183) |
There were five multicentre and six single-centre studies, and one multicentre RCT across Asia, Europe, and North and South America. The NOS found relatively high risk of bias with five studies of good quality, one study of fair quality, and six studies of poor quality (refer to the Supplementary table). The Cochrane risk-of-bias tool reported potential for unclear and high risk of bias with particular loss of precision regarding the blinding of personnel, as seen in the Supplementary materials.
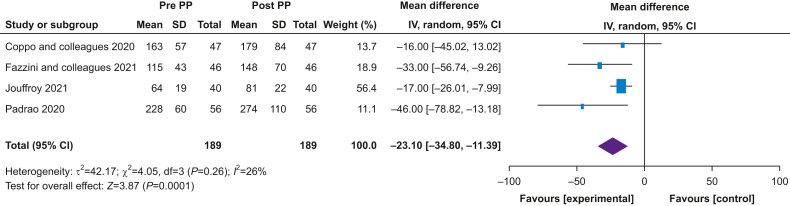
Primary outcome
The MD in Pao2/FiO2 ratio before and after APP was –23.10 (–34.80 to –11.39; P<0.0001; I 2=26%) using outcomes from the five studies that reported this information (see Fig. 2 ). A subgroup analysis was performed for proning duration of >4 or <4 h. There was a difference in Pao2/FiO 2 ratio of –16.91 (–25.25 to –8.31; P<0.0001; l 2=0%) in those placed in prone position <4 h compared with a larger improvement in Pao2/FiO2 ratio of –37.47 (–56.70 to –18.23; P<0.0001; l 2=0%) in those placed in the prone position >4 h. Considering, however, the limited number of studies per subgroup with 87 and 102 patients each, respectively, we were unable to draw substantial conclusions from this analysis.
Fig 2.
Primary outcome: changes in oxygenation. Forest plot demonstrating pooled data of changes in Pao2/FiO2 ratio pre- and post-awake prone positioning using a random effects model. CI, confidence interval; PP, prone position; sd, standard deviation.
Despite all patients included the fitting criteria for moderate-to-severe ARDS (Pao2/FiO2 <200 mm Hg),35 we were unable to evaluate the specific Pao2/FiO2 threshold at which one might benefit most from awake proning, and this remains unclear.
Secondary outcomes
We only included studies with a control group, including patients in supine position only, as qualitative heterogeneity between studies was too large to report a meaningful meta-analysis of outcomes using generic inverse variance. This resulted in a meta-analysis, including studies with patients who only have COVID-19.
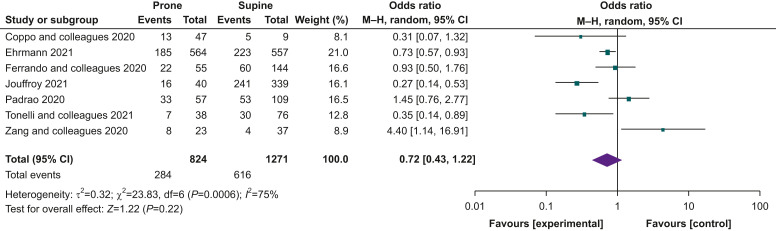
Intubation
The odds ratio (OR) for intubation was 0.72 (95% CI: 0.43–1.22; P=0.220; I 2=75%) for patients who had awake prone positioning compared with supine controls, showing a non-significant benefit and large heterogeneity (see Fig. 3 ). There was a pooled intubation rate of 38.3% for patients with awake prone positioning amongst 12 studies reporting this information. The subgroup analysis of those placed in the prone position >4 h showed an OR for intubation of 1.15 (0.66–1.99; P=0.630; I 2=70%), whereas those placed in the prone position <4 h had an OR of 0.30 (0.18–0.49; P<0.001; I 2=0%). We observed large differences in heterogeneity between these analyses, so we would advise caution in interpreting these results. A small RCT found no difference within 30-day mortality when comparing patients placed in prone position for a median of 3.4 h vs a median of 9 h (cumulative hours per day).
Fig 3.
Secondary outcome: intubation. Forest plot demonstrating pooled data of intubation across studies with comparator group using a random effects model. CI, confidence interval.
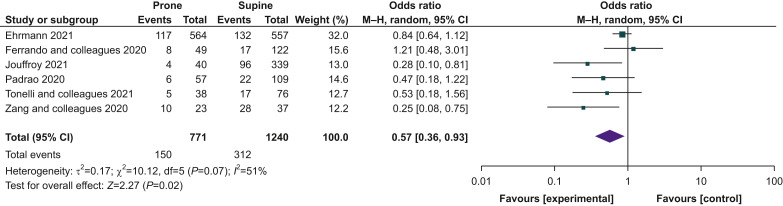
Mortality
Mortality of patients placed in the prone position was reported in 11 studies, with a pooled mortality of 16.8%. The OR for mortality was 0.57 (95% CI: 0.36–0.93; P=0.02; I 2=51%), indicating a statistically significant improvement in prone compared with supine patients (see Fig. 4 ). A subgroup analysis of patients placed in the prone position >4 h revealed an OR for mortality of 0.30 (0.10–0.92; P=0.0001; I 2=86%). Only one study reported mortality rate in patients placed in the prone position <4 h, preventing further subgroup analysis. The small RCT reported no difference was seen in patients placed in the prone position for a cumulative median of 3.4 h compared with those placed in the prone position for 9 h (HR 2.29 [0.57; 9.14]; P=0.300).
Fig 4.
Secondary outcome: mortality. Forest plot demonstrating pooled data of mortality across studies with comparator group using a random effects model. CI, confidence interval.
ICU admission
Only four studies reported incidence of critical care admission, and this was mainly amongst those with no control group. A study observing a selected cohort of patients undertaking awake prone positioning in the emergency department reported 41% (9/22;) incidence of ICU admission. A retrospective cohort study that compared a prone and supine group observed no difference in critical care admission rate (HR 1.14 [0.96, 1.34]; P=0.183). Higher incidence of ICU admission has been noted in patients placed in the prone position for less than 1 h compared with those placed in the prone position for more than 1 h (APP <1 h: 83%, 10/12 vs APP >1 h: 41%, 14/34; P=0.011). A recent RCT found no difference in rate of ICU admission between patients placed in the prone position for a cumulative median of 3.4 h compared with those placed in the prone position for 9 h (P=0.580).
Time and duration of prone positioning
All studies considered different time of enrolment for APP; therefore, stratification based on S/F ratio or P/F ratio was not possible (see Supplementary files). Similarly, authors used various oxygen delivery interface alongside APP, making a subgroup analysis not feasible.
Amongst the studies, the duration of prone positioning varied from less than 1 h up to 16 h day−1. Median duration of APP was 3 h (IQR: 2–16 h), but was not reported in four studies. Awake proning was not tolerated in 15% of patients across six studies reporting this information.
Respiratory changes during and after prone positioning
Only six studies (42%) reported changes in ventilatory frequency (VF) pre- and post-PP. Data are equally divided, with 50% (three of six studies) reporting a statistically significant reduction in VF, or conversely no significant difference was observed after pronation (refer to Supplementary files).
Adverse events
No significant adverse events were reported, but common limitations were back pain (6%), intolerance (5%), anxiety (3%), discomfort (2%), refusal (2%), pressure sores (2%), hypoxaemia (1%), and accidental lines removal (1%). The small RCT reported two cardiac arrests in patients placed in the prone position for a median of 9 h (2/36), and one cardiac arrest in the control group (1/39) placed in the prone position for a median of 3.4 h, but none were attributable to or associated with awake prone positioning.
Discussion
Our systematic review and meta-analysis pooled results from 12 observational studies from international settings, including 1156 non-intubated patients with ARF caused by ARDS or COVID-19 respiratory failure. The primary meta-analysis revealed significant improvement in Pao2/FiO2 ratio and lower mortality, but intubation ratio was unchanged in the prone positioning group.
The specific effects of awake prone positioning in patients with ARF are not yet fully understood. The improvement in oxygenation would suggest that awake prone positioning may follow similar pathophysiological consideration as for intubated patients, irrespective of the nature triggering the underlying lung injury. Several physiological mechanisms may explain the improvement in oxygenation in viral pneumonia (i.e. SARS-CoV-2 or influenza) or ARDS. In prone positioning, the application of a gravitational weight shifts local forces and gradient reopening non-aerated or poorly aerated areas (baby lung concept)2; therefore, lung recruitment of the posterior dependent lung regions is promoted by reversal of atelectasis. When spontaneously breathing patients are placed in prone positioning, a more homogeneous ventilation is promoted by reduced lung stretch and strain with changes in pleural pressure and pleural space distribution throughout lung regions.3 , 36 The improvement in ventilation/perfusion (V/Q) matching may be attributable to better distribution of physical forces (i.e. changes in pleural pressure gradients and gravitational forces and distribution of transpulmonary pressure) and reduced the ‘pendelluft phenomenon’ (i.e. the displacement of gas from a more recruited non-dependent lung region to a less recruited dependent lung region).4 Although lung aeration becomes more homogeneous, shunting can be reduced as the perfusion pattern remains relatively constant.5 These may be the reasons why this short-term intervention would be beneficial and improve patient-centred outcome, such as mortality. The results of this study are consistent with previous systematic reviews supporting that PP in intubated patients with severe ARDS significantly reduced mortality.37 , 38
The value of awake prone positioning39 alongside NIV40 in reducing intubation is questionable, and our results uphold this. Some observational studies have reported decreased VF and excessive work of breathing amongst those awake and placed in the prone position, resulting in a trend towards reduced intubation rate.9 , 14 , 17 , 18 On the contrary, a prospective observational study found no benefit in reducing the risk of intubation, but rather showed a trend for delay.20 A decrease in VF in awake prone positioning may be the result of the decrease in respiratory strain, and this is of clinical importance in avoiding tracheal intubation. We would recommend that future studies report VF as a matter of routine.
In non-intubated patients, a short improvement in oxygenation with awake prone positioning without reducing vigorous spontaneous inspiratory efforts may potentially aggravate lung damage, leading to patient self-inflicted lung injury (P-SILI).41 , 42 P-SILI remains hypothetical, and its clinical implication is yet to be established. This concept has polarised clinicians into different ideological positions, and for some, it is a cause of concern for which advocating for intubation and invasive mechanical ventilation to be ‘performed as soon as possible’ to prevent disease progression.43 , 44 However, no difference has been found in mortality or duration of mechanical ventilation comparing critically ill patients with COVID-19 respiratory failure who were intubated early with those intubated late.45 Therefore, P-SILI should not be a justification for performing intubation, and the harm associated with elective early intubation may outweigh the theoretical benefit.46 Further research should explore the hypothesis if a clear threshold for undertaking intubation and mechanical ventilation exists, and mechanical ventilation should not be the sole solution investigated.
A recent small RCT showed no reduction in intubation or 30-day mortality rate.47 However, the neutral results may be explained by underpowered analysis, awake prone positioning combined with lateral position, and awake prone positioning largely used in the control group. The true impact of intubation and mechanical ventilation on ARDS and COVID-19 respiratory failure is still not entirely understood, and further research is warranted.44 We should be cautious about liberal intubation recommendations, and clinical decisions should be patient specific. Use of intubation and mechanical ventilation are associated with severe complications and increased mortality,48 , 49 and need greater resources, including not only ventilators, but also adequately trained clinicians. In future studies, we recommend reporting the incidence of ventilator-acquired pneumonia and, if numbers permit, analysis by differing oxygen delivery interfaces.
Overall, we found minimal consistency regarding application of awake proning, and there is no clarity about the timing when to start and the optimal duration. Further research is needed to understand when awake prone positioning should be commenced and specifically at what stage (mild vs moderate hypoxia).
Tolerance is a major limitation,47 and it is not feasible aiming for a similar duration of awake prone positioning (>16 h day−1) as per intubated patients.1 The effect of prone positioning may be time dependent and stage dependent (mild vs severe respiratory failure),50 but no difference has been found in intubation or mortality rate comparing awake prone positioning for 3.4 h vs 9 h.47 Ultimately, protocols should target for awake prone positioning more than 1 h, as less has been found to be associated with higher critical care admission and intubation rate.9 , 14
Awake proning appears safe, and a further advantage is that it allows patients to interact with families during hospitalisation, favouring humanisation of care. Patient compliance is key and may be influenced by common factors, such as back pain, intolerance, and anxiety, which make refusal and non-compliance likely. Additional important limiting factors may be obesity (especially central obesity), pregnancy, and most of all the assistance of dedicated healthcare practitioners that can prevent further injuries to the patient. The management of a conscious but rapidly deteriorating patient can be extremely difficult at the ward level; therefore, awake proning requires close input from doctors, nurses, and physiotherapists to ensure it is successful especially during initial sessions. Patients must be aware of the procedure and be cooperative, and clinicians should be mindful of practical considerations, such as optimisation of analgesia, adequate communication, and assistance to improve comfort, adherence, and proper positioning.
Our review is unique as the first to establish a series of important analyses to reflect contemporary application of prone positioning in non-intubated patients with hypoxaemic respiratory failure. The paucity of evidence available consists of the main limitation of this review, as the majority of the studies included are observational in nature. Our review generates the hypothesis if further high-quality evidence is needed. The initial interest surrounding APP was the expectation that this may be a safe and effective strategy able to optimise ventilator shortage during the surge of the SARS-CoV-2 pandemic. Awake prone position may be a potential beneficial and effective intervention, but it may not be significant until applied in the optimal time and duration and to the right population. Awake prone position is a low-cost strategy and practical tool to manage deteriorating patients, but it should be applied by trained practitioners and intubation should not be delayed when clinically indicated. Our findings highlight the importance of identifying a responsive target population and mastering the specifics of the approach and execution of the intervention. These should be the focus of future studies. Larger and well-designed studies (ideally RCTs) are needed to explore the subject more rigorously.
Conclusions
Awake prone positioning may be a promising therapy for non-intubated patients with hypoxaemic respiratory failure attributable to ARDS or COVID-19. Potential benefits include improvement in oxygenation and mortality rate, but there is no significant effect on incidence of intubation or critical care admission. The optimal frequency, duration, and criteria for starting or stopping proning remain unclear. Although no significant adverse events attributable to awake prone positioning were reported, awake prone positioning is not without limitations, and it is associated with intolerance, discomfort, and anxiety.
Authors' contributions
Study design: BF, RP, ZP
Data collection/analysis: BF, AP
Data interpretation: all authors.
Writing of first draft of the paper: BF, AP
Revising of paper for important intellectual content: all authors.
Approval of final version: all authors.
Declaration of interest
RP is an editor of the British Journal of Anaesthesia. The other authors have no conflicts of interest to declare.
Handling editor: Jonathan Hardman
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2021.09.031.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Guérin C., Reignier J., Richard J.C., et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 2.Gattinoni L., Marini J.J., Pesenti A., Quintel M., Mancebo J., Brochard L. The ‘baby lung’ became an adult. Intensive Care Med. 2016;42:663–673. doi: 10.1007/s00134-015-4200-8. [DOI] [PubMed] [Google Scholar]
- 3.Tonelli R., Marchioni A., Tabbì L., et al. Spontaneous breathing and evolving phenotypes of lung damage in patients with COVID-19: review of current evidence and forecast of a new scenario. J Clin Med. 2021;10:975. doi: 10.3390/jcm10050975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Santini A., Mauri T., Dalla Corte F., Spinelli E., Pesenti A. Effects of inspiratory flow on lung stress, pendelluft, and ventilation heterogeneity in ARDS: a physiological study. Crit Care. 2019;23:369. doi: 10.1186/s13054-019-2641-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bamford P., Bentley A., Dean J., Wilson-Baig N. ICS guidance for prone positioning of the conscious COVID patient 2020. https://static1.squarespace.com/static/5e6613a1dc75b87df82b78e1/t/5e99e7f60755047b87934d6e/1587144697447/2020-04-12+Guidance+for+conscious+proning.pdf Available from:
- 6.Scaravilli V., Grasselli G., Castagna L., et al. Prone positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective study. J Crit Care. 2015;30:1390–1394. doi: 10.1016/j.jcrc.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 7.Ding L., Wang L., Ma W., He H. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit Care. 2020;24:28. doi: 10.1186/s13054-020-2738-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sartini C., Tresoldi M., Scarpellini P., et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA. 2020;323:2338. doi: 10.1001/jama.2020.7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elharrar X., Trigui Y., Dols A.-M., et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020;323:2336. doi: 10.1001/jama.2020.8255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frat J.-P., Thille A.W., Mercat A., et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372:2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 11.Confalonieri M., Salton F., Fabiano F. Acute respiratory distress syndrome. Eur Respir Rev. 2017;26:160116. doi: 10.1183/16000617.0116-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walkey A., Summer R., Ho V., Alkana P. Acute respiratory distress syndrome: epidemiology and management approaches. Clin Epidemiol. 2012;4:159–169. doi: 10.2147/CLEP.S28800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coppo A., Bellani G., Winterton D., et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020;8:765–774. doi: 10.1016/S2213-2600(20)30268-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fazzini B., Fowler A.J., Zolfaghari P. Effectiveness of prone position in spontaneously breathing patients with COVID-19: a prospective cohort study. J Intensive Care Soc. 2021 doi: 10.1177/1751143721996542. Advance Access published on February 18. 1751143721996542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thompson A.E., Ranard B.L., Wei Y., Jelic S. Prone positioning in awake, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Intern Med. 2020;180:1537. doi: 10.1001/jamainternmed.2020.3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dubosh N.M., Wong M.L., Grossestreuer A.V., et al. Early, awake proning in emergency department patients with COVID-19. Am J Emerg Med. 2021;46:640–645. doi: 10.1016/j.ajem.2020.11.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tonelli R., Pisani L., Tabbì L., et al. Early awake proning in critical and severe COVID-19 patients undergoing noninvasive respiratory support: a retrospective multicenter cohort study. Pulmonology. 2021 doi: 10.1016/j.pulmoe.2021.03.002. Advance Access published on March 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zang X., Wang Q., Zhou H., Liu S., Xue X. COVID-19 Early Prone Position Study Group. Efficacy of early prone position for COVID-19 patients with severe hypoxia: a single-center prospective cohort study. Intensive Care Med. 2020;46:1927–1929. doi: 10.1007/s00134-020-06182-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Telias I., Katira B.H., Brochard L. Is the prone position helpful during spontaneous breathing in patients with COVID-19? JAMA. 2020;323:2265. doi: 10.1001/jama.2020.8539. [DOI] [PubMed] [Google Scholar]
- 20.Ferrando C., Mellado-Artigas R., Gea A., et al. Awake prone positioning does not reduce the risk of intubation in COVID-19 treated with high-flow nasal oxygen therapy: a multicenter, adjusted cohort study. Crit Care. 2020;24:597. doi: 10.1186/s13054-020-03314-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Padrão E.M.H., Valente F.S., Besen B.A.M.P., et al. Awake prone positioning in COVID-19 hypoxemic respiratory failure: exploratory findings in a single-center retrospective cohort study. Acad Emerg Med. 2020;27:1249–1259. doi: 10.1111/acem.14160. [DOI] [PubMed] [Google Scholar]
- 22.Nauka P.C., Chekuri S., Aboodi M., Hope A.A., Gong M.N., Chen J.-T. A case-control study of prone positioning in awake and nonintubated hospitalized coronavirus disease 2019 patients. Crit Care Explor. 2021;3:e0348. doi: 10.1097/CCE.0000000000000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jones J.R.A., Attard Z., Bellomo R., et al. Repeated proning in non-intubated patients with COVID-19. Respirology. 2021;26:279–280. doi: 10.1111/resp.14008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Retucci M., Aliberti S., Ceruti C., et al. Prone and lateral positioning in spontaneously breathing patients with COVID-19 pneumonia undergoing non-invasive helmet CPAP treatment. Chest. 2020;158:2431–2435. doi: 10.1016/j.chest.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solverson K., Weatherald J., Parhar K.K.S. Tolerability and safety of awake prone positioning COVID-19 patients with severe hypoxemic respiratory failure. Can J Anesth Can Anesth. 2021;68:64–70. doi: 10.1007/s12630-020-01787-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caputo N.D., Strayer R.J., Levitan R. Early self-proning in awake, non-intubated patients in the emergency department: a single ED’s experience during the COVID-19 pandemic. Acad Emerg Med. 2020;27:375–378. doi: 10.1111/acem.13994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sarma A., Calfee C.S. Prone positioning in awake, non intubated patients with COVID-19: necessity is the mother of invention. JAMA Intern Med. 2020;180:1539–1540. doi: 10.1001/jamainternmed.2020.3027. [DOI] [PubMed] [Google Scholar]
- 28.Preferred reporting Items for systematic reviews and meta-analyses. PRISMA 2020-checklist.pdf. http://prisma-statement.org/PRISMAStatement/Checklist Available from:
- 29.Wells G.A., Shea B., O’Connell D., et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Available from:
- 30.Guyatt G.H., Oxman A.D., Vist G.E., et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bilan N., Dastranji A., Ghalehgolab Behbahani A. Comparison of the SpO2/FIO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or acute respiratory distress syndrome. J Cardiovasc Thorac Res. 2015;7:28–31. doi: 10.15171/jcvtr.2014.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hozo S.P., Djulbegovic B., Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mueller M., D’Addario M., Egger M., et al. Methods to systematically review and meta-analyse observational studies: a systematic scoping review of recommendations. BMC Med Res Methodol. 2018;18:44. doi: 10.1186/s12874-018-0495-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.ARDS Definition Task Force. Ranieri V.M., Rubenfeld G.D., et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 36.Tonelli R., Fantini R., Tabbì L., et al. Early inspiratory effort assessment by esophageal manometry predicts noninvasive ventilation outcome in de novo respiratory failure. A pilot study. Am J Respir Crit Care Med. 2020;202:558–567. doi: 10.1164/rccm.201912-2512OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sud S., Friedrich J.O., Taccone P., et al. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med. 2010;36:585–599. doi: 10.1007/s00134-009-1748-1. [DOI] [PubMed] [Google Scholar]
- 38.Munshi L., Del Sorbo L., Adhikari N.K.J., et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14:S280–S288. doi: 10.1513/AnnalsATS.201704-343OT. [DOI] [PubMed] [Google Scholar]
- 39.Weatherald J., Solverson K., Zuege D.J., Loroff N., Fiest K.M., Parhar K.K.S. Awake prone positioning for COVID-19 hypoxemic respiratory failure: a rapid review. J Crit Care. 2021;61:63–70. doi: 10.1016/j.jcrc.2020.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nava S., Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:10. doi: 10.1016/S0140-6736(09)60496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brochard L., Slutsky A., Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195:438–442. doi: 10.1164/rccm.201605-1081CP. [DOI] [PubMed] [Google Scholar]
- 42.Battaglini D., Robba C., Ball L., et al. Noninvasive respiratory support and patient self-inflicted lung injury in COVID-19: a narrative review. Br J Anaesth. 2021;127:353–364. doi: 10.1016/j.bja.2021.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gattinoni L., Coppola S., Cressoni M., Busana M., Rossi S., Chiumello D. COVID-19 does not lead to a “typical” acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201:1299–1300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gattinoni L., Chiumello D., Caironi P., et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46:1099–1102. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Papoutsi E., Giannakoulis V.G., Xourgia E., Routsi C., Kotanidou A., Siempos Effect of timing of intubation on clinical outcomes of critically ill patients with COVID-19: a systematic review and meta-analysis of non-randomized cohort studies. Crit Care. 2021;25:121. doi: 10.1186/s13054-021-03540-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tobin M.J., Laghi F., Jubran A. P-SILI is not justification for intubation of COVID-19 patients. Ann Intensive Care. 2020;10:105. doi: 10.1186/s13613-020-00724-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rosén J., von Oelreich E., Fors D., et al. Awake prone positioning in patients with hypoxemic respiratory failure due to COVID-19: the PROFLO multicenter randomized clinical trial. Crit Care. 2021;25:209. doi: 10.1186/s13054-021-03602-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tobin M.J., Laghi F., Jubran A. Caution about early intubation and mechanical ventilation in COVID-19. Ann Intensive Care. 2020;10:78. doi: 10.1186/s13613-020-00692-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tobin M.J. Basing respiratory management of COVID-19 on physiological principles. Am J Respir Crit Care Med. 2020;201:1319–1320. doi: 10.1164/rccm.202004-1076ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reutershan J., Schmitt A., Dietz K., Unertl K., Fretschner R. Alveolar recruitment during prone position: time matters. Clin Sci. 2006;110:655–663. doi: 10.1042/CS20050337. [DOI] [PubMed] [Google Scholar]
- 51.Padrao E.M.H., Valente F.S., Besen B.A.M.P., et al. Awake prone positioning in COVID-19 hypoxemic respiratory failure: Exploratory findings in a single-center retrospective cohort study. Acad Emerg Med. 2020;27:1249–1259. doi: 10.1111/acem.14160. [DOI] [PubMed] [Google Scholar]
- 52.Ehrmann S., Li J., Ibarra-Estrada M., et al. Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial. Lancet Respir Med. 2021;21:2213–2600. doi: 10.1016/S2213-2600(21)00356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.