Summary
The pericapsular nerve group (PENG) block is a novel regional anaesthesia technique that aims to provide hip analgesia with preservation of motor function, although evidence is currently lacking. In this single‐centre, observer‐masked, randomised controlled trial, patients undergoing total hip arthroplasty received pericapsular nerve group block or no block (control group). Primary outcome measure was maximum pain scores (0–10 numeric rating scale) measured in the first 48 h after surgery. Secondary outcomes included postoperative opioid consumption; patient mobilisation assessments; and length of hospital stay. Sixty patients were randomly allocated equally between groups. The maximum pain score of patients receiving the pericapsular nerve group block was significantly lower than in the control group at all time‐points, with a median (IQR [range]) of 2.5 (2.0–3.7 [0–7]) vs. 5.5 (5.0–7.0 [2–8]) at 12 h; 3 (2.0–4.0 [0–7]) vs. 6 (5.0–6.0 [2–8]) at 24 h; and 2.0 (2.0–4.0 [0–5]) vs. 3.0 (2.0–4.7 [0–6]) at 48 h; all p < 0.001. Moreover, the pericapsular nerve group showed a significant reduction in opioid consumption, better range of hip motion and shorter time to ambulation. Although no significant difference in hospital length of stay was detected, our results suggest improved postoperative functional recovery following total hip arthroplasty in patients who received pericapsular nerve group block.
Keywords: anaesthesia, analgesia, arthroplasty, hip surgery, postoperative pain
Introduction
Total hip arthroplasty is one of the most common major orthopaedic procedures to improve patient’s functional status and quality of life [1]. However, despite these advantages, the immediate postoperative period can be associated with severe pain that delays mobilisation and increases hospital stay and risk of thromboembolic events [2].
Regional anaesthesia techniques that have been used to manage postoperative pain include epidural analgesia; lumbar plexus block; parasacral block; fascia iliaca block; and femoral, obturator and sciatic nerve block [3, 4, 5]. However, these techniques may be associated with complications such as epidural hematoma, postoperative headache or prolonged motor block and subsequent delay in hospital discharge [6, 7, 8].
The pericapsular nerve group (PENG) block is an ultrasound‐guided approach, first described by Giron‐Arango et al. for the blockade of the articular branches of the femoral, obturator and accessory obturator nerves that provide sensory innervation to the anterior hip capsule [9, 10]. It has been successfully used as an alternative regional anaesthesia technique for the management of acute pain after hip fracture [11, 12], but its applications are expanding, suggesting a potential role for analgesia after elective hip surgery [13, 14].
To date, there are no published clinical trials that have analysed the impact of this technique in elective hip surgery. We, therefore, conducted a randomised, controlled observer‐masked trial to evaluate the efficacy of the PENG block in improving postoperative analgesia after total hip arthroplasty.
The main outcome was postoperative pain, assessed using a numeric rating scale (NRS) in the first 48 h after total hip arthroplasty. Secondary outcomes included postoperative opioid consumption; patient mobilisation; length of stay; and presence of any adverse effects.
Methods
The study was approved by the Ethics Committee of Campus Bio‐Medico University Hospital in Rome. Enrolment took place from 9 March to 24 December 2020 and was performed at the Day Surgery Department of University Hospital Campus Bio‐Medico of Rome, Italy. Enrolment was offered pre‐operatively to adults undergoing primary hip arthroplasty, aged ≥18 y and ASA physical status 1–3.
Patients were not included in this study if they refused consent; had allergy to local anaesthetics; had infection of the puncture site; weighed <30 kg; were aged <18 y; were assessed as having ASA physical status 4 or more; or who had dementia or cognitive impairment. Eligible patients were randomly allocated into two groups to receive either a PENG block or no block (control group). Randomisation was achieved using computer‐generated lists in blocks of eight with a 1:1 ratio and treatment allocation concealed using consecutively numbered, sealed, opaque envelopes. All patients underwent total hip replacement that was performed by the same surgical team using a posterior approach. Every patient was informed of the sequence of procedures during anaesthesia and surgery, and signed informed consent was obtained before enrolment.
In both groups, patients received mild sedation with intravenous midazolam 0.03 mg.kg‐1. Acetaminophen 1 g, ketorolac 30 mg and dexamethasone 0.1 mg.kg‐1 were given intravenously (i.v.) before surgery as multimodal pre‐emptive analgesia. Spinal anaesthesia was chosen as the main anaesthetic technique. It was performed by injecting 17 mg of ropivacaine 0.5% through a 27G Whitacre needle at the L2–L3 or L3–L4 interspace with the patient in a sitting position.
All patients had wound infiltration of 20 ml ropivacaine 0.375% from the surgeon at the end of the surgical procedure. Infiltration of the surgical wound with local anaesthetic was necessary because PENG block involves only nerve branches supplying pericapsular analgesia. For this reason, we decided to perform wound infiltration in both groups of patients to eliminate any confounding factor linked to patient’s perception of superficial pain.
In the PENG group, the block was performed after spinal anaesthesia and before surgical incision, according to the technique described by Girón‐Arango [9]. A curvilinear probe was used (80‐mm Stimuplex Ultra 360, BBraun, Melsungen, Germany). Puncture was performed in a lateromedial direction until the needle tip reached the plane between the iliopsoas tendon and periosteum and between the anterior inferior iliac spine and iliopubic eminence (Fig. 1). After a negative aspiration test, 20 ml of ropivacaine 0.375% was injected in the plane beneath the iliopsoas muscle. The block was always performed by the same three anaesthetists (GP, FC, RP). Each had almost 5 years of post‐specialisation clinical experience focused on regional anaesthesia, and all had performed almost 20 PENG blocks before patient enrolment started.
Figure 1.
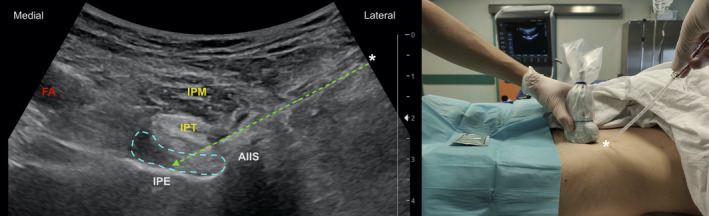
PENG block via a lateromedial approach. Once the needle was placed in the plane between the iliopsoas tendon (IPT) and periosteum and between the anterior inferior iliac spine (AIIS) and iliopubic eminence (IPE), the PENG block was performed by injecting 20 ml of local anaesthetic, the spread of which is visible under the iliopsoas muscle (IPM). Arrow, needle pathway; blue dashed line, local anaesthetic spread; FA, femoral artery. Asterisk, needle entry point.
In both groups, patients received the same postoperative multimodal analgesia, which included ketorolac 60 mg i.v. every 24 h and acetaminophen 1 g i.v. three times per day. Patient‐controlled analgesia (PCA) was given using Zalviso® (AcelRx Pharmaceuticals, Inc., Hayward, CA, USA), a system that releases 15 mcg sublingual sufentanil tablets on demand (lockout period 20 min), the efficacy and safety profile of which has already been demonstrated [15]. All patients were trained in PCA use in the post‐anaesthetic care unit. After the first 10 postoperative hours, patients were asked to ambulate with the help of a walker.
At all postoperative time‐points (12, 24 and 48 h), patients were asked to indicate perceived pain using a 0–10 NRS (0 no pain, 10 worst imaginable pain) the worst pain experienced in the previous 12 h (maximum pain). Total opioid consumption and time to first opioid consumption was derived from the PCA device. The cumulative dose of sublingual sufentanil was converted to milligrams of morphine equivalents for comparison (15 μg sublingual sufentanil = 1.8 mg intravenous morphine) [16].
Motor recovery of the hip joint was assessed at 24 h using range of motion, where active hip flexion (between 0° and 90°) was measured using a protractor. In addition, ‘time to first walk’, defined as the time between the end of surgery and the ability to take at least three steps with the help of the walker, was recorded after the first 10 postoperative hours (at approximately 20:00), and re‐evaluated on the first postoperative day. Length of hospital stay was also recorded. We recorded side‐effects, that is, nausea, vomiting or motor block, defined as inability to flex the hip in the absence of pain. Outcome assessment was performed by the same group of three clinicians (AS, ED, CP), who were blinded to the group allocation.
To calculate sample size, we considered our primary hypothesis, that postoperative analgesia is improved with the PENG block. Although there were no similar clinical trials, we estimated the density of pain scores as mean 2 and SD 1.5, based on published data regarding the use of PENG block for total hip arthroplasty [17, 18]. To simulate power, we used the truncated Gaussian distribution with range 0–10, SD 1.5 and PENG group mean of 2. Under these assumptions and 2‐sided α = 5%, we simulated 10,000 trials with sample size of 30 per group. With an overall sample size of 60 subjects, we estimated 90% power to detect group differences in pain as small as approximately 1. Statistical analysis and graphic presentation were obtained using GraphPad Prism 8 software (GraphPad Software Inc., San Diego, CA, USA).
The parametric distribution of numerical variables was evaluated using the Shapiro–Wilk normality test. Differences between groups were assessed by Student’s t test for continuous parametric variables, while Wilcoxon‐Mann‐Whitney U test was used when appropriate. Categorical variables were compared with Pearson’s χ2 test. A p value <0.05 was considered statistically significant.
Results
Of 62 patients who were assessed for eligibility, two refused to sign informed consent and were therefore not included. The remaining 60 patients were randomly and equally allocated between groups (Fig. 2). No clinically relevant differences were apparent from group characteristics (Table 1). Study outcomes are summarised in Table 2. The maximum NRS pain scores of patients receiving PENG block was lower than the control group at all time‐points, with a median (IQR [range]) of 2.5 (2.0–3.7 [0–7]) vs. 5.5 (5.0–7.0 [2–8]) at 12 h, 3.0 (2.0–4.0 [0–7]) vs. 6.0 (5.0–6.0 [2–8]) at 24 h and 2.0 (2.0–4.0 [0–5]) vs. 3.0 (2.0–4.7 [0–6]) at 48 h, reaching statistical significance (p < 0.001, Fig. 3).
Figure 2.
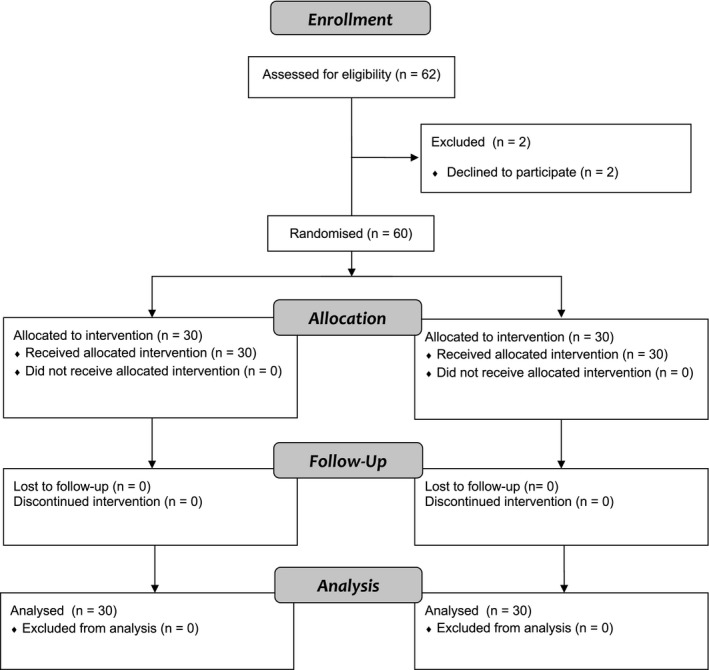
Study flow diagram.
Table 1.
Baseline characteristics. Values are mean (SD) or number.
| PENG | Control | |
|---|---|---|
| n = 30 | n = 30 | |
| Age; y | 66.4 (12.4) | 66.7 (8.6) |
| Sex; m/f | 16/14 | 17/13 |
| BMI; kg.m‐2 | 29.2 (5.2) | 28 (3.9) |
| ASA physical status | ||
| 1 | 3 | 4 |
| 2 | 17 | 15 |
| 3 | 10 | 11 |
| Chronic opiate use | ||
| Yes | 5 | 3 |
| No | 25 | 27 |
| Surgery duration; min | 104 (17) | 107 (22) |
PENG, pericapsular nerve group block.
Table 2.
Study outcomes. Values are median (IQR [range]), number (proportion) or mean (SD).
| PENG | Control | p value | |
|---|---|---|---|
| n = 30 | n = 30 | ||
| Postoperative pain; Maximum NRS | |||
| 0–12 h | 2.5 (2.0–3.7 [0.0–7.0]) | 5.5 (5.0–7.0 [2.0–8.0]) | <0.001 |
| 12–24 h | 3 (2–4 [0–7]) | 6 (5–6 [2–8]) | – |
| 24–48 h | 2 (2–4 [0–5]) | 3.0 (2.0–4.7 [0.0–6.0]) | – |
| Postoperative opioid consumption | |||
| Yes | 20 (77%) | 30 (100%) | 0.001 |
| No | 10 (33%) | 0 | – |
| Time to first opioid; h | 12 (6.7) | 6 (4.9) | 0.001 |
| Total opioid consumption | |||
| Sufentanil tablets; n | 2 (0–2 [0–9]) | 5 (3–6 [2–9]) | <0.001 |
| Intravenous morphine equivalent; mg | 4.0 (4.5) | 8.9 (4.0) | |
| Mobility | |||
| Range of motion; degrees | 62.3 (20.2) | 38.7 (22.4) | <0.001 |
| Time to first walk; h | 22.1 (9.6) | 32.4 (10.6) | <0.001 |
| Length of hospital stay; h | 51.1 (12.6) | 53.3 (13.8) | 0.5 |
| Adverse effects | |||
| Motor block | 0 | 0 | – |
| Nausea/vomiting | 1 (3%) | 3 (10%) | 0.6 |
| Dizziness | 0 | 1 (3%) | >0.9 |
PENG, pericapsular nerve group block; NRS, numeric rating scale.
Figure 3.
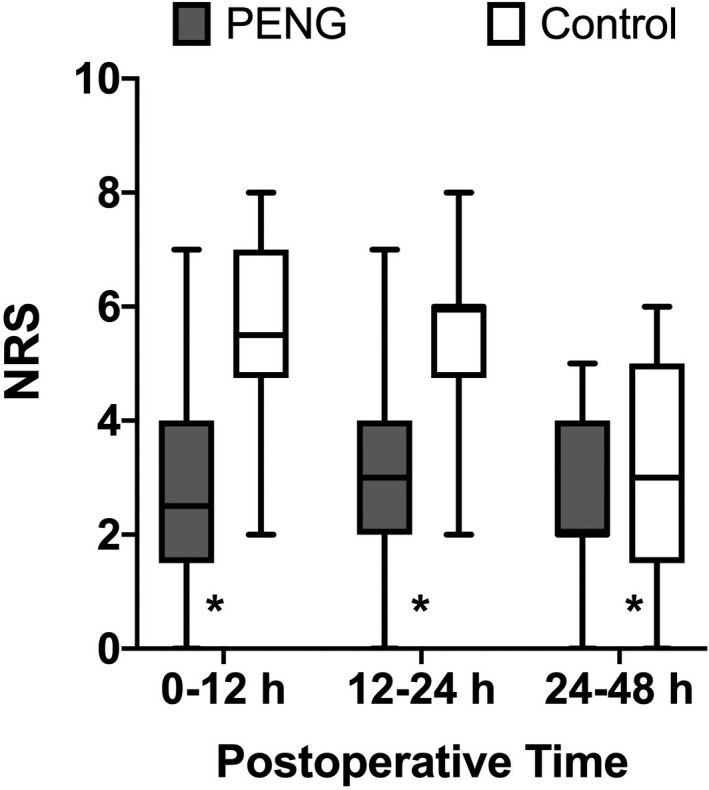
Maximum postoperative (numeric rating scale) pain scores in both study groups reported during three postoperative intervals. Values are median (horizontal bars), IQR (box) and range (whiskers). *denotes statistical significance (p < 0.05); PENG, pericapsular nerve group block.
Every patient in the control group used sufentanil tablets, while 10 patients (33%) in the PENG group did not take any. Total opioid consumption was median (IQR [range]) 2 (0–2 [0–9]) sufentanil tablet administration in the PENG group vs. 5 (3–6 [2–9]) of the control group (p < 0.001, Fig. 4), which is equivalent to 4.0 (4.5) vs. 8.9 (4.0) morphine mg. Mean time to first opioid in the PENG group was 6 h later than the control group.
Figure 4.
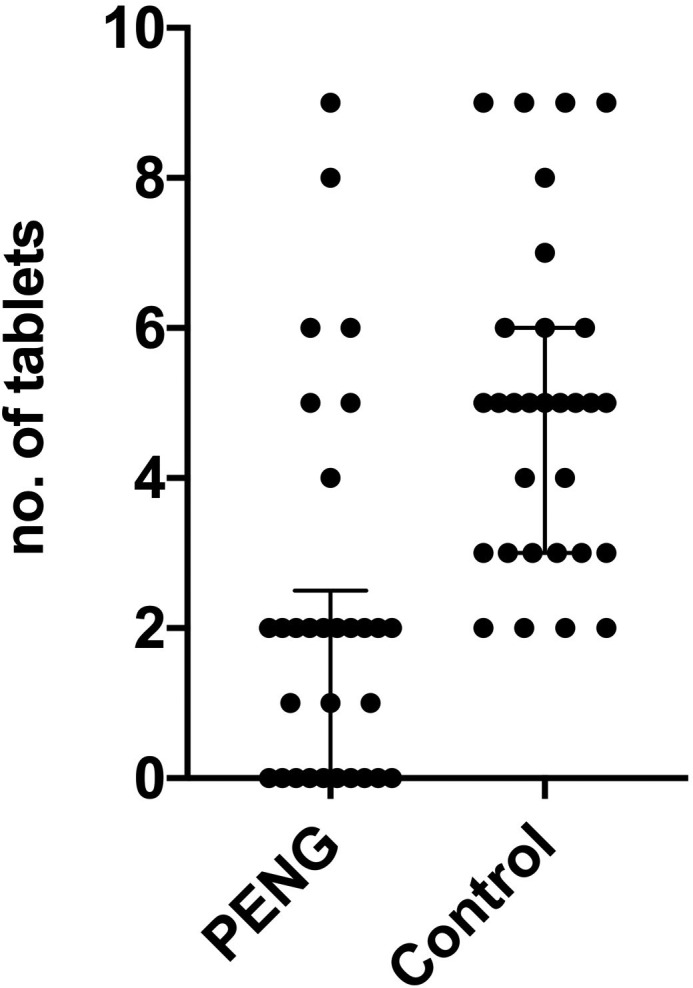
Patient‐controlled administration of sublingual sufentanil among the two groups in the first 48 h after surgery. Dots are the number of sufentanil tablets taken by each patient. PENG, pericapsular nerve group block.
No postoperative motor block was recorded in any group. However, the range of motion and ‘time to first walk’ were significantly better in the PENG group (Table 2).
Although statistically significant, this difference in functional recovery between groups was clinically unimportant, as the two groups were comparable in terms of hospital stay; PENG group 51.1 (12.6) vs. control group 53.3 (13.8) h, p = 0.5. Lastly, there was no difference in the incidence of nausea and vomiting (PENG 3% vs. control 10%), p = 0.6.
Discussion
The PENG block is a new and promising ultrasound‐guided regional anaesthesia technique, aiming to block the branches of femoral nerve, obturator nerve and accessory obturator nerve innervating the anterior hip capsule [10, 19]. Currently, the PENG block has been shown to be effective in reducing pain in different hip‐related procedures, including fracture and hip replacement surgery, although most current evidence is limited to case reports and case series [13, 18, 20, 21, 22].
In this randomised, controlled observer‐masked clinical trial, the PENG block improved postoperative analgesia following total hip replacement, decreasing pain scores and opioid consumption during the first 48 h after surgery. Our findings are consistent with previously published reports. Kukreja et al. [18] reported mild postoperative pain scores in a retrospective case series of patients undergoing hip arthroplasty, while Mysore et al. [17] found that the PENG block was associated with a 2.4 mg reduction in 24‐h hydromorphone consumption among patients receiving local infiltration analgesia following total hip arthroplasty, although average pain scores were comparable. Moreover, PENG block has been successfully used with other techniques to manage total hip arthroplasty analgesia, that is, quadratus lumborum block [14], lumbar erector spinae block [23] and lateral femoral cutaneous nerve block as described by Thallaj [24] The rationale for the addition of the lateral femoral cutaneous nerve block is that PENG block only covers peripheral fibres innervating anterior hip capsule, omitting analgesia for skin incision. However, as described by Nielsen et al., lateral femoral cutaneous nerve block covers only part of the surgical wound in total hip arthroplasty, as most of the surgical incision is innervated by lateral cutaneous branches of the iliohypogastric and subcostal nerves [25]. For this reason, we opted to include wound infiltration with local anaesthetic in both groups to provide analgesia for the surgical incision during the first postoperative hours, and to eliminate any confounding factor linked to a patient’s perception of superficial pain. Since mean ‘time to first opioid’ request in the PENG group was 12 h, it may be considered representative of block duration; this endpoint has never been assessed in previous studies involving the PENG block. Moreover, the better analgesia offered by PENG block resulted in better functional recovery of the hip in the early postoperative period, allowing better range of motion and shortening time to ambulation, although no significant difference in length of stay was detected.
A further aspect is that PENG block involves only sensitive fibres innervating the anterior hip capsule, preserving motor fibres. This consistently favours motor recovery, unlike other techniques such as femoral nerve block, lumbar plexus block and fascia iliaca block, which may affect quadriceps strength. Although pain scores were significantly lower in the PENG group, severe pain was not observed in the control group, suggesting a useful role of wound infiltration combined with multimodal analgesia. However, in the PENG group, 30% of patients did not request opioids, compared with 0% in the control group. Furthermore, PENG block decreased total opioid consumption, reducing the risk of postoperative adverse events such as nausea and dizziness, although this difference between groups was not statistically significant. The lowest difference in pain scores between groups was observed at 48 h, indicating that the PENG block has the best clinical efficacy during the first 24 h postoperatively.
This is the first randomised controlled trial of the use of PENG block for postoperative analgesia following hip replacement. Our results suggest that the PENG block provided optimal postoperative analgesia, fast motor recovery and reduced opioid consumption as recommended by enhanced recovery after surgery protocols [26]. For this reason, PENG block may be a useful regional anaesthesia technique to manage postoperative pain in the context of modern fast‐track hip surgery.
However, this study has some limitations. First, our study included only total hip arthroplasty conducted via the posterior approach, although it is reportedly the most common surgical approach used worldwide [27]. Second, we did not differentiate between static and dynamic postoperative pain; however, range of motion and ‘time to first walk’ are both indirect indices of pain on movement.
The other aspect that should be discussed is that the PENG block provides only anterior hip capsule analgesia. Although the anterior capsule innervation is responsible for the majority of hip‐related pain, it omits the posterior capsule, which is innervated by the nerve to the quadratus femoris and from the superior gluteal nerve, both from the sacral plexus [28]. Therefore, it may be useful for future studies to examine outcomes combining PENG block with sciatic block or local infiltration analgesia techniques to provide complete hip capsule analgesia, as recently suggested by some authors [29, 30].
In conclusion, the PENG block has proved to be an effective opioid sparing analgesic technique, allowing early postoperative mobilisation and worth considering as a valid analgesia option for fast‐track hip surgery protocols.
Acknowledgements
The study was registered on ClinicalTrials.gov (NCT04306133). The authors thank all the investigators of the PENG study group (Appendix 1) for their assistance in realising the study protocol and their efforts in promoting the use of this regional anaesthesia technique. No external funding or competing interests declared.
Appendix 1. PENG study group investigators
Campus Bio‐medico University : F. Gargano, F. Longo, D. Velluti, L. Schiavoni, A. Mattei, G. Nonnis, L. M. Remore, S. Rizzo, L. Paglione, V. Scaduto, T. Coletta, E. Di Giorgio, F. De Rosa, F. La Verde.
Contributor Information
G. Pascarella, Email: g.pascarella@unicampus.it.
collaborators:
F. Gargano, F. Longo, D. Velluti, L. Schiavoni, A. Mattei, G. Nonnis, L. M. Remore, S. Rizzo, L. Paglione, V. Scaduto, T. Coletta, E. Di Giorgio, F. De Rosa, and F. La Verde
References
- 1. Shan L, Shan B, Graham D, Saxena A. Total hip replacement: a systematic review and meta‐analysis on mid‐term quality of life. Osteoarthritis Cartilage 2014; 22: 389–406. [DOI] [PubMed] [Google Scholar]
- 2. Ferrata P, Carta S, Fortina M, Scipio D, Riva A, Di Giacinto S. Painful hip arthroplasty: definition. Clinical Cases in Mineral and Bone Metabolism 2011; 8: 19–22. [PMC free article] [PubMed] [Google Scholar]
- 3. Young AC, Buvanendran A. Pain management for total hip arthroplasty. Journal of Surgical Orthopaedic Advances 2014; 23: 13–21. [DOI] [PubMed] [Google Scholar]
- 4. Tran DQ, Salinas FV, Benzon HT, Neal JM. Lower extremity regional anesthesia: essentials of our current understanding. Regional Anesthesia and Pain Medicine 2019; 44: 143–80. [DOI] [PubMed] [Google Scholar]
- 5. Hogan MV, Grant RE, Lee L Jr. Analgesia for total hip and knee arthroplasty: a review of lumbar plexus, femoral, and sciatic nerve blocks. American Journal of Orthopedics 2009; 38: E129–E133. [PubMed] [Google Scholar]
- 6. Maddali P, Moisi M, Page J, et al. Anatomical complications of epidural anesthesia: a comprehensive review. Clinical Anatomy 2017; 30: 342–6. [DOI] [PubMed] [Google Scholar]
- 7. Liu H, Brown M, Sun LU, et al. Complications and liability related to regional and neuraxial anesthesia. Best Practice and Research: Clinical Anaesthesiology 2019; 33: 487–97. [DOI] [PubMed] [Google Scholar]
- 8. Guay J, Johnson RL, Kopp S. Nerve blocks or no nerve blocks for pain control after elective hip replacement (arthroplasty) surgery in adults. Cochrane Database of Systematic Reviews 2017; 10: Cd011608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Girón‐Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular Nerve Group (PENG) block for hip fracture. Regional Anesthesia and Pain Medicine 2018; 43: 859–63. [DOI] [PubMed] [Google Scholar]
- 10. Del Buono R, Padua E, Pascarella G, et al. Pericapsular Nerve Group (PENG) block: an overview. Minerva Anestesiologica 2021; 87: 458–66. [DOI] [PubMed] [Google Scholar]
- 11. Lin D‐Y, Morrison C, Brown B, et al. Pericapsular nerve group (PENG) block provides improved short‐term analgesia compared with the femoral nerve block in hip fracture surgery: a single‐center double‐blinded randomized comparative trial. Regional Anesthesia and Pain Medicine 2021; 46: 398–403. [DOI] [PubMed] [Google Scholar]
- 12. Del Buono R, Padua E, Pascarella G, Soare CG, Barbara E. Continuous PENG block for hip fracture: a case series. Regional Anesthesia and Pain Medicine 2020; 45: 835–8. [DOI] [PubMed] [Google Scholar]
- 13. Roy R, Agarwal G, Pradhan C, Kuanar D. Total postoperative analgesia for hip surgeries, PENG block with LFCN block. Regional Anesthesia and Pain Medicine 2019; 44: 684. [DOI] [PubMed] [Google Scholar]
- 14. Kukreja P, Schuster B, Northern T, Sipe S, Naranje S, Kalagara H. Pericapsular nerve group (PENG) block in combination with the quadratus lumborum block analgesia for revision total hip arthroplasty: a retrospective case series. Cureus 2020; 12: e12233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fabio C, Giuseppe P, Chiara P, et al. Sufentanil sublingual tablet system (Zalviso®) as an effective analgesic option after thoracic surgery: An observational study. Saudi Journal of Anaesthesia 2019; 13: 222–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Miner JR, Melson TI, Leiman D, et al. Pooled Phase III safety analysis of sufentanil sublingual tablets for short‐term treatment of moderate‐to‐severe acute pain. Pain Management 2019; 9: 259–71. [DOI] [PubMed] [Google Scholar]
- 17. Mysore K, Sancheti SA, Howells SR, Ballah EE, Sutton JL, Uppal V. Postoperative analgesia with pericapsular nerve group (PENG) block for primary total hip arthroplasty: a retrospective study. Canadian Journal of Anesthesia 2020; 67: 1673–4. [DOI] [PubMed] [Google Scholar]
- 18. Kukreja P, Avila A, Northern T, Dangle J, Kolli S, Kalagara H. A Retrospective Case Series of Pericapsular Nerve Group (PENG) block for primary versus revision total hip arthroplasty analgesia. Cureus 2020; 12: e8200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Morrison C, Brown B, Lin DY, Jaarsma R, Kroon H. Analgesia and anesthesia using the pericapsular nerve group block in hip surgery and hip fracture: a scoping review. Regional Anesthesia and Pain Medicine 2021; 46: 169–75. [DOI] [PubMed] [Google Scholar]
- 20. Orozco S, Muñoz D, Jaramillo S, Herrera AM. Pericapsular Nerve Group (PENG) block for perioperative pain control in hip arthroscopy. Journal of Clinical Anesthesia 2020; 59: 3–4. [DOI] [PubMed] [Google Scholar]
- 21. Casas Reza P, Diéguez García P, Gestal Vázquez M, Sampayo Rodríguez L, López ÁS. Pericapsular nerve group block for hip surgery. Minerva Anestesiologica 2020; 86: 463–5. [DOI] [PubMed] [Google Scholar]
- 22. Pagano T, Scarpato F, Chicone G, et al. Analgesic evaluation of ultrasound‐guided Pericapsular Nerve Group (PENG) block for emergency hip surgery in fragile patients: a case series. Arthroplasty 2019; 1: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ince I, Kilicaslan A. Combination of Lumbar Erector Spinae Plane Block (LESP) and Pericapsullar Nerve Group (PENG) block in hip surgery. Journal of Clinical Anesthesia 2020; 61:109672. [DOI] [PubMed] [Google Scholar]
- 24. Thallaj A. Combined PENG and LFCN blocks for postoperative analgesia in hip surgery‐A case report. Saudi Journal of Anaesthesia 2019; 13: 381–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nielsen MV, Nielsen TD, Bendtsen TF, Børglum J. The Shamrock sign: comprehending the trefoil may refine block execution. Minerva Anestesiologica 2018; 84: 1423–5. [DOI] [PubMed] [Google Scholar]
- 26. Rele S, Shadbolt C, Schilling C, Taylor NF, Dowsey MM, Choong PFM. The impact of enhanced recovery after surgery on total joint arthroplasty: protocol for a systematic review and meta‐analysis. Journal of Medical Internet Research Research Protocols 2021; 10: e25581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moretti VM, Post ZD. Surgical approaches for total hip arthroplasty. Indian Journal of Orthopaedics 2017; 51: 368–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Birnbaum K, Prescher A, Hessler S, Heller KD. The sensory innervation of the hip joint–an anatomical study. Surgical and Radiologic Anatomy 1997; 19: 371–5. [DOI] [PubMed] [Google Scholar]
- 29. Öksüz G, Arslan M, Bilal B, Gişi G. A novel indication for pericapsular nerve group (PENG) block: high volume PENG block combination with sciatic block for surgical anesthesia of lower limb. Journal of Clinical Anesthesia 2021; 71: 110218. [DOI] [PubMed] [Google Scholar]
- 30. Del Buono R, Pascarella G, Costa F, Barbara E. Ultrasound‐guided local infiltration analgesia for hip surgery: myth or reality? Minerva Anestesiologica 2019; 85: 1242–3. [DOI] [PubMed] [Google Scholar]


