Abstract
Background:
Nitric oxide (NO) is an endogenous substance which has several endocrine functions and may act as neurotransmitter in the brain. High levels of NO may provoke nitrosative stress.
Aim:
It was aimed to examine serum levels of NO in patients with depressive episodes who were treated with electroconvulsive therapy (ECT) in this study.
Methods:
The design was a case–control, follow-up study. Patients with depressive episodes (n = 23) and a healthy control group (n = 21) were enrolled. Three serum samples were obtained from the patient group (before ECT, after first and seventh sessions). NO, nitrite, and nitrate levels were examined.
Statistical Analysis:
Differences between groups were examined with t-test or Mann–Whitney U-test. Longitudinal data were evaluated with Panel Regression Analysis and Kruskal–Wallis Test.
Results:
Serum levels of NO and nitrite decreased significantly after the seventh session of ECT administration compared to the baseline and first session. Nitrate levels did not differ between the assessments.
Conclusions:
Reduction of the serum NO and nitrite levels might be a contributing factor for hypertension during the sessions. These findings are reflect the circulating NO levels. Further studies may dissect NO physiology in the brain in mental disorders and potential external effects.
Keywords: Depressive disorder, electroconvulsive therapy, nitric oxide
INTRODUCTION
Despite the advances in medicine, depressive disorders (DDs) are still the leading cause of disability and depression has high economic burden for individuals or society.[1] Several treatment options have been emerged in the recent years, however many cases with DD remain to be treatment resistant.[2] The electroconvulsive therapy (ECT) is a safe, reliable treatment modality for psychiatric disorders, which remains to be a lifesaving option for the urgent or treatment-resistant cases.[3,4,5,6] On the other hand, the mechanism underlying the therapeutic effects of the ECT still have not been unveiled. Some theories designate changes in gene expression, neuroplasticity, neurotransmitter, and neurotrophins for the mechanism of effect.[7,8] ECT may also be involved with inflammation[9,10] and oxidative stress.[11,12,13] These findings indicate that the ECT provides chemical tranquility. However, the effects of ECT on Nitric Oxide (NO) system could not be clarified yet.
It has been claimed that ECT may stimulate the expression of nitric oxide synthase (NOS) in the brain and increase NO levels.[14,15] Moreover, it is also claimed that anesthetic medication Propofol has the potential to alter NO levels.[16] It has been reported in rat studies that electroconvulsive seizure (ECS) enhanced NO levels,[16] and inhibited NO synthesis (and thereby alleviated cognitive side effects).[17] The NO has several physiological functions, however, the mechanism of action of the NO compound is level dependent, at high levels NO is rapidly converted to reactive nitrogen oxide species (RNOSs).[18] Ischemia, infections, inflammation, and metabolic syndrome may induce the NOS enzyme and thus may increase NO levels and increased activity of NO may cause humoral, endocrine, and immune system changes.[19,20,21,22] Therefore, the interaction between the NO and ECT is complex and difficult to identify.
To the best of our knowledge, this is the first study to assess the effects of ECT on circulating NO levels in patients with depressive episodes. It was aimed to examine serum nitric oxide levels in patients with DD before and after ECT sessions in this study. It has been hypothesized that the ECT alters NO levels and its components.
MATERIALS AND METHODS
Local ethical committee approval was obtained, and all participants provided written informed consent. Patients were invited to participate in the study under observation of an accompanying first-degree relative. Diagnoses were checked with Structured Clinical Interview for the Diagnostic and Statistical Manual-IV by an experienced psychiatrist.[23,24] ECT treatments were planned by independent physicians. Treatment-resistant patients with depression who were planned to be treated with ECT were invited to participate in the study. Patients who did not respond to two different antidepressant therapies from different groups were defined as treatment-resistant depression according to the consensus criteria.[25] Medical and psychiatric history was checked before participation to the study. Nutritional deficiencies, rapid weight reduction, any medical disease (endocrine, cardiac, pulmonary, gastrointestinal, neurologic, etc.,), any psychiatric comorbidities, lifetime history of alcohol or substance use disorder, any systemic infectious diseases in the last month were the exclusion criteria. Healthy volunteers were invited to participate in the study by local advertisements. Consecutive individuals that met the inclusion/exclusion criteria were enrolled. Twenty-three individuals were enrolled in the study group and 21 healthy individuals were recruited to the healthy control group. Seventeen item Hamilton Depression Rating Scale (Ham-D)[26,27] was the clinical evaluation tool for the assessment of disease severity.
Department for the ECT applications was a dedicated unit for ECT which was equipped with life supporting systems (ventilators, respirators, defibrillator, electrocardiogram [ECG]).[28] All ECT procedures were performed in this unit. All patients were controlled with hemogram, biochemistry and hormone tests, X-ray of chest, and magnetic resonance imaging of the cranium before ECT application routinely. Patients were on fast for 12 h prior to ECT sessions. Sessions were performed 3 days a week (Monday, Wednesday, and Friday). ECG, blood pressure, and saturation were routinely observed during the administration. Propofol (1 mg/kg) and succinylcholine (0.5 mg/kg) were administered for the induction of anesthesia. Ventilation support with an airway, ambu mask, and bag was provided before electrical stimulation. Dental arches were shielded with a sponge during the electrical stimulation. The ECT protocol was bilateral and bitemporal, stimulations were fixed, biphasic, and short-pulsed waves. Impedances were lower than 1000 Ohm and the stimulus pulse-width was set to optimal (0.3 ms). Electrical stimulus charges were between 250 and 350 millicoulomb, energy level was set according to age, gender, and history of ECT classically. Seizures were assessed and considered effective if they were more than 20 s. The device was a Thymatron System IV ECT device (Somatics LLC, FL, USA).
After collection of the consents, clinical interviews were performed and clinical assessments were completed. Laboratory test results were recorded. The blood samples were obtained from antecubital veins both from patients and healthy controls. The next day, patients were transferred to the ECT department for the administration of the first ECT session. In 30–45 min following the ECT administration, blood samples were collected from the antecubital veins from each patient. Third blood samples were obtained from the patients 30–45 min after the seventh session. All samples were collected in the morning hours (08:00–12:00), in the patient group the second and third samples were collected 30–45 min after the ECT application. Participants were asked to be on fast for at least 12 h. In the patient group, blood samples were collected prior to ECT administration, after the first session and after the seventh session. The blood samples were left in the room for 30 min for clothing and then centrifuged at 1500 g for 15 min to obtain serums. Serum samples were aliquoted and left in the freezer at − 80°C. Samples were analyzed in the biochemistry laboratory.
Since NO is a very labile molecule, which reacts with molecular oxygen and accumulates in the serum as nitrite and nitrate ions. Nitrite (NO2−) and nitrate (NO3−) are inert end products of NO metabolism. These inorganic anions are unwanted residues in the food chain. Studies have demonstrated that nitrite and nitrate are recycled in blood and tissues for synthesizing NO and other bioactive nitrogen oxides.[29] Thus, they are evaluated as storage pools for NO-like bioactivity, thereby complementing the NO synthase-dependent pathway. Therefore, the stable oxidation end products of NO, nitrite, and nitrate can be readily measured in biological fluids and have been used in vitro and in vivo as indicators of NO production.[30,31] Accordingly, in order to reduce nitrite and nitrate, the sample was treated with Cadmium in glycine solution at 9.7 pH. Then, mixed with fresh reagent and absorbances were evaluated by the spectrophotometer (ultraviolet-1601 Shimadzu, Japan). The results were used to calculate the sample concentrations. Results are presented as mmol/L.
Statistical analyses
All statistical analyses were performed with SPSS software (version 24; IBM incorporation, Armonk, NY, USA). All variables were checked with Shapiro–Wilks’ test for distribution characteristics. Variables with Gaussian distribution were analyzed with parametric tests, whereas variables violating Gaussian distribution were analyzed with nonparametric tests. Variables with Gaussian distribution were reported with means and standard deviations, and variables with Non-Gaussian distribution were reported with medians and quartiles. The Mann–Whitney U-test (education, nitrite, nitrate, and NO levels) or the independent groups t-test (age) were performed for comparisons between two independent groups. Dependent group comparisons were performed with the paired-samples t-test to compare the Ham-D scores before and after the ECT. Comparisons containing three or more groups were performed with Friedman Test for related samples analysis. Post hoc comparisons were performed with Wilcoxon Signed rank test. Longitudinal data analyses were also performed with panel regression analyses. Potential effects of biochemical and demographic variables were checked with repeated measures ANCOVA. The level of NO metabolites was transformed with logarithmic transformation to meet the assumptions of the repeated measures ANCOVA and panel regression analysis. Categorical variables were reported with number and percentage and comparisons were performed with the Chi-square test. Correlation analyses were performed with Spearman's Rank correlation test. All results were two-tailed and the level for statistical significance was set at 0.05.
RESULTS
Comparison between demographic variables is presented in Table 1. Groups differed in age (t = 2.37, P = 0.022) and education (Z = −3.71, P < 0.001) significantly. No difference was observed between the groups in terms of gender (χ2 = 0.09, P = 0.763). Sixteen patients had major DD diagnosis and seven patients had bipolar disorder, depressive episode diagnosis. Patients were hospitalized for 26.00 (21.00–31.25) days. Ham-D scores were significantly lower in the second assessments after the ECT, compared to initial assessments (t = 9.88, P < 0.001). There were no significant difference between the groups in terms of hormone, hemogram, and biochemistry assessments.
Table 1.
Comparison between the groups in terms of demographic variables
| DD (n=23) | HC (n=21) | t/Z/χ2 | P | |
|---|---|---|---|---|
| Age | 43.04±11.69 | 35.43±9.34 | 2.37 | 0.022 |
| Gender (women/men) | 11/12 | 11/10 | 0.09 | 0.763 |
| Education (years) | 5.00 (5.00-11.00) | 15.00 (5.00-17.00) | −3.71 | <0.001 |
| Marital status (m/s) | 7/16 | 14/7 | 5.78 | 0.016 |
| Number of days in the hospital | 26.00 (21.00-31.25) | - | ||
| Diagnosis (MDD/BD) | 16/7 | - | ||
| Number of previous hospitalizations | 3.17±3.19 | - | ||
| Duration of the disorder* | 12.46±11.29 | - | ||
| Number of ECT sessions | 7.14±2.03 | - | ||
| Energy (millicoulomb) | 44.29±12.67 | |||
| EMG seizure duration | 31.61±7.77 | |||
| EEG seizure duration | 47.30±14.05 | |||
| History of previous ECT, n (%) | 7 (30.44) | - | ||
| HAM-D before treatment | 35.70±12.10 | - | ||
| HAM-D after treatment | 9.50 (3.00-19.25) |
*Months. Mann-Whitney U-test, t-test or Chi-square test. DD – Depressive disorder; HC – Healthy control; ECT – Electroconvulsive therapy; MDD – Major depressive disorder; BD – Bipolar disorder; HAM-D – Hamilton Depression Rating Scale; m/s – married/single; EMG – Electromyographic; EEG – Electroencephalogram
Serum nitric oxide levels and its components (nitrite and nitrate) were compared between the groups. Results are presented in Table 2. Accordingly, Nitrite and NO levels did not differ between the groups. However, nitrate levels of the DD group were significantly lower than the HC group (Z = −2.69, P = 0.007). Demographic and biochemical variables were controlled for their potential confounding effects. Neither of the variables had any effect on the metabolites.
Table 2.
Comparison of the nitric oxide, nitrite, and nitrate levels between groups
| DD (n=23) | HC (n=21) | t/Z | P | |
|---|---|---|---|---|
| Nitrite | 2.94±3.08, 2.10 (1.80-3.00) | 2.83±1.49, 2.30 (2.10-3.10) | −1.26 | 0.207 |
| Nitrate | 2.75±0.51, 2.70 (2.50-3.00) | 3.23±0.85, 3.00 (2.80-3.50) | −2.69 | 0.007 |
| NO | 5.70±3.00, 5.20 (4.60-5.80) | 6.07±2.33, 5.30 (4.90-6.75) | −1.09 | 0.274 |
P<0.05 is significant. Mann-Whitney U-test. Mean±SD or medians and IQR are reported. DD – Depressive disorder; HC – Healthy control group; NO – Nitric oxide; SD – Standard deviation; IQR – Interquartile range
Serum levels of NO and its components were compared within the DD group at different time points [Table 3]. Regression results showed that nitrite (adjusted R2 = 0.09, F = 6.70, B = −0.32, t = −2.59, P = 0.012), NO (adjusted R2 = 0.08, F = 6.17, B = −0.31, t = −2.48, P = 0.016) levels differed between the sessions within the patient group in the panel regression analysis. Post hoc comparisons showed that nitrite levels were higher in the base time point (baseline, before ECT) in comparison to the third time point (after seventh session) (Z = −2.60, P = 0.009) [Figure 1]. Furthermore, nitrite (Z = −2.72, P = 0.007) and NO (Z = −2.29, P = 0.022) levels were higher in the second time point (after the first ECT session) in comparison to the third time point (after the seventh ECT session). Correlation analyses within the groups showed that total number of platelet counts were correlated with serum nitrite (Rho = 0.47, P = 0.026) and NO (Rho = 0.52, P = 0.014) levels. No other correlations were detected.
Table 3.
Within group comparison of nitric oxide and metabolites in the depressive disorder group
| Before ECT (n=23) | After first session (n=22) | After seventh session (n=21) | χ 2 | P | |
|---|---|---|---|---|---|
| Nitrite | 2.10 (1.80-3.00), 2.94±3.09 | 2.30 (2.00-3.25), 3.29±2.69 | 1.90 (1.65-2.32), 1.90±0.47 | 7.62 | 0.022 |
| Nitrate | 2.70 (2.503.00), 2.75±0.51 | 2.95 (2.60-3.42), 3.01±0.58 | 2.70 (2.50-3.30), 2.85±0.89 | 1.40 | 0.497 |
| NO | 5.20 (4.60-5.80), 5.70±3.00 | 5.35 (4.87-6.30), 6.31±2.76 | 4.70 (4.03-4.48), 4.73±0.89 | 6.12 | 0.047 |
P<0.05 is significant. Friedman test. Medians and IQR are reported. Post hoc comparisons were performed with Wilcoxon Sign test. NO – Nitric oxide; ECT – Electroconvulsive therapy; IQR – Interquartile range
Figure 1.
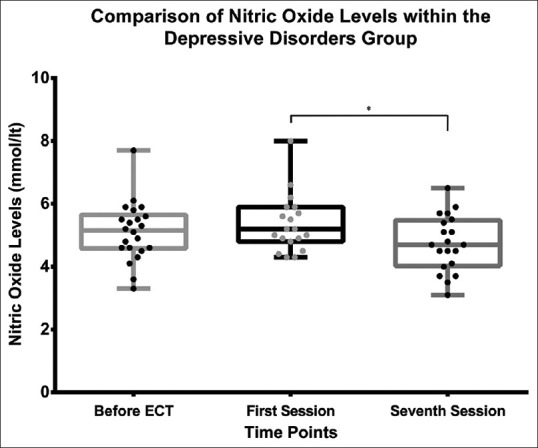
Comparison of nitric oxide (NO) within the patient group showed that NO levels decreased significantly after seventh session in the patient group. *Denotes statistical significance
DISCUSSION
Major findings of this study were nitrate levels of the DD group were significantly lower than the HC group; and within the course of the ECT treatment, nitrite and NO levels were depleted in the DD group following ECT treatment. Statistical analyses showed that nitrite and NO levels were lower after the seventh session of ECT application in comparison to the first and second time points. Furthermore, although the difference could not reach statistical significance, first ECT session slightly increased NO levels. In the brain, NO is involved with endocrine, inflammation, neurotransmission, cellular signaling cascades and altered NO levels may indicate changes in the involved mechanisms. Serum NO levels might be a global assessment of circulating NO cascades, the measurement of NO in serum will only detect the overall pool and not potential clinically relevant compartments.
ECSs have been shown to increase NO levels in rat brain.[32,33] The author's interpretation was that the NOS enzyme becomes activated secondary to the intracellular changes that occurred due to the NMDA receptor hypofunction. It is also suggested that nitrogen groups of the glutamate–glutamine turn-over may interact with NO and reduce its levels by converting it into nitrate groups by the effects of antidepressants.[34] These findings highlight the importance of the NO compound in the central nervous system neurotransmitters. On the contrary, ECS significantly reduced NO levels produced by leukocytes in circulation.[35] In this study, circulatory NO and metabolites have been measured and found to be depleted after the seventh ECT session. Although membranes are highly permeable for the NO molecule, NO in circulation is primarily produced by red blood cells and endothelium in human.[36] Similarly to the results of this study, a recent study reported that a single ECT session decreased the expression of inducible NOS (iNOS) and plasma nitrite levels.[37]
Peripheral nitric oxide levels measurements provided variable results in DDs.[38,39] Furthermore, examinations on polymorphisms of NOS have contributed with mixed findings, although some evidence seems to be present indicating a role of NO in DDs.[38] However, the general trend implies that antidepressant treatment decreases NOS and thereby NO levels and decrease of NO is in parallel with clinical remission.[38,39] For example, circulating NO levels were higher in depressive state of bipolar disorder and decreased following 30 days of treatment in a previous study.[30] As a chemical compound, NO may quickly become metabolized and dissolved, thus assessment of nitric oxide should be administered cautiously. Variable results might be related with several different reasons such as metabolic states, metabolic differences, medications, heterogeneous samples of neuropsychiatric disorders.
The mechanism of the effect of the NO is level dependent, high serum levels of NO may rapidly provoke synthesis of RNOS in the presence of superoxide anion. RNS may cause damage to cell membranes, organelles, proteins and nucleic acids by altering their activity. Furthermore, sulfhydryl groups are prone to nitrosylation and nitrosylation of the thiols cause alterations gene expression, cell growth, apoptotic cascades.[40] Depressive episodes of either bipolar disorder or recurrent DD are characterized by oxidative and nitrosative stress[41] and depletion of NO and related compounds may alleviate the risk of nitrosative stress in patients with depression. In addition to reduction of NO levels, the ECT also reduces immune and inflammatory[9] and oxidative stress[11,12,13] markers. It is therefore possible that production of RNS may also be reduced.
One of the most important function of NO is to reduce the vascular tonus and induce vasodilatation. Likewise, nitrite also provides vasodilatation and increase in oxygen consumption.[29] Systemic tension increases slightly and transiently during ECT and normalizes back within an hour.[42,43] Autonomic response to the sessions may increase the systemic blood pressure during ECT. On the other hand, since ECT reduces levels of NO and nitrite, it is possible to speculate that this effect might be related with the effects of ECT sessions on systemic tension. Likewise, nitrate compounds were successfully used to control systemic hypertension in a patient during ECT previously.[44] Furthermore, nitrite has antioxidant properties[29] and decreased level of nitrite compounds may give rise to production of superoxide radical. Moreover, with exceptions,[45] antidepressant medications may decrease NO levels.[38] Since the patients who participated in the study were treated with various medications simultaneously, reduction of the NO levels may possibly be related with medications. These findings suggest that increased levels of NO may become reversed with either by treatments and/or remission.
Limitations
These results may have influenced by several factors such as heterogeneity of the patient group, medications, and small sample size. Propofol is the most commonly used anesthetic agent[46] and the patients had Propofol during the induction. It inhibits the expression of NO and iNOS isoform[47] and this mechanism may possibly have contributed to the global effect of the ECT on NO levels. Furthermore, nitric oxide is a compound that quickly becomes metabolized, thus should be assessed carefully and results should be viewed cautiously. Anesthesia procedures may also have confounded the results. More assessments, 2 and 6 h after the ECT sessions, may have provided more information about the effects of ECT session on NO levels. On the other hand, major strength of the study is its longitudinal design.
CONCLUSIONS
In this study, NO and nitrite levels were decreased in patients with DD, after the seventh ECT session. It might be speculated that decrease of NO might be related with the transient increase of systemic arterial tension during the ECT since NO and nitrite provide arterial relaxation and vasodilatation and their decrease may enhance arterial tonus and increase blood pressure accordingly. Future studies may investigate the relationship between the level of NO and metabolites with systemic blood pressure. These findings are related with the peripherical serum levels of NO and may not indicate the changes in NO levels in the brain. Further studies may also examine the effects of ECT on NOS enzyme and other metabolic cascades involved with NO. The ECT remains to be a life-saving treatment modality which provides several benefits for the patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Iancu SC, Wong YM, Rhebergen D, van Balkom AJ, Batelaan NM. Long-term disability in major depressive disorder: A 6-year follow-up study. Psychol Med. 2020;50:1644–52. doi: 10.1017/S0033291719001612. [DOI] [PubMed] [Google Scholar]
- 2.Malhi GS, Outhred T, Morris G, Boyce PM, Bryant R, Fitzgerald PB, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders: Bipolar disorder summary. Med J Aust. 2018;208:219–25. doi: 10.5694/mja17.00658. [DOI] [PubMed] [Google Scholar]
- 3.Canbek O, Menges OO, Atagun MI, Kutlar MT, Kurt E. Report on 3 years’ experience in electroconvulsive therapy in Bakirkoy Research and Training Hospital for psychiatric and neurological diseases: 2008-2010. J ECT. 2013;29:51–7. doi: 10.1097/YCT.0b013e318282d126. [DOI] [PubMed] [Google Scholar]
- 4.Canbek O, Yuksel G, Atagun MI, Ipekcıoglu D, Kurt E, Menges OO, et al. Geriatric ECT at a Turkish Teaching Hospital: A 5-year experience. J ECT. 2014;30:e28–9. doi: 10.1097/YCT.0000000000000083. [DOI] [PubMed] [Google Scholar]
- 5.Tørring N, Sanghani SN, Petrides G, Kellner CH, Østergaard SD. The mortality rate of electroconvulsive therapy: A systematic review and pooled analysis. Acta Psychiatr Scand. 2017;135:388–97. doi: 10.1111/acps.12721. [DOI] [PubMed] [Google Scholar]
- 6.Jolly AJ, Singh SM. Does electroconvulsive therapy cause brain damage: An update. Indian J Psychiatry. 2020;62:339–53. doi: 10.4103/psychiatry.IndianJPsychiatry_239_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh A, Kar SK. How electroconvulsive therapy works? Understanding the neurobiological mechanisms. Clin Psychopharmacol Neurosci. 2017;15:210–21. doi: 10.9758/cpn.2017.15.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baldinger P, Lotan A, Frey R, Kasper S, Lerer B, Lanzenberger R. Neurotransmitters and electroconvulsive therapy. J ECT. 2014;30:116–21. doi: 10.1097/YCT.0000000000000138. [DOI] [PubMed] [Google Scholar]
- 9.Yrondi A, Sporer M, Péran P, Schmitt L, Arbus C, Sauvaget A. Electroconvulsive therapy, depression, the immune system and inflammation: A systematic review. Brain Stimul. 2018;11:29–51. doi: 10.1016/j.brs.2017.10.013. [DOI] [PubMed] [Google Scholar]
- 10.Belge JB, van Diermen L, Sabbe B, Parizel P, Morrens M, Coppens V, et al. Inflammation, hippocampal volume, and therapeutic outcome following electroconvulsive therapy in depressive patients: A pilot study. Neuropsychobiology. 2020;79:222–32. doi: 10.1159/000506133. [DOI] [PubMed] [Google Scholar]
- 11.Şenyurt M, Aybek H, Herken H, Kaptanoglu B, Korkmaz A. Evaluation of oxidative status in patients treated with electroconvulsive therapy. Clin Psychopharmacol Neurosci. 2017;15:40–6. doi: 10.9758/cpn.2017.15.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atagun MI, Atay-Canbek O, Balaban OD, Ipekcioglu D, Alpugan B, Yalcin S, et al. Investigating the impact of the ECT on Thiol-Disulphide homeostasis in depressive disorders. Psychiatry Clin Psychopharmacol. 2020;30:136–43. [Google Scholar]
- 13.Kartalci S, Karabulut AB, Ozcan AC, Porgali E, Unal S. Acute and chronic effects of electroconvulsive treatment on oxidative parameters in schizophrenia patients. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1689–94. doi: 10.1016/j.pnpbp.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 14.Rosen Y, Reznik I, Sluvis A, Kaplan D, Mester R. The significance of the nitric oxide in electro-convulsive therapy: A proposed neurophysiological mechanism. Med Hypotheses. 2003;60:424–9. doi: 10.1016/s0306-9877(02)00419-x. [DOI] [PubMed] [Google Scholar]
- 15.Bernstein HG, Heinemann A, Bogerts B. Electro-convulsive therapy, nitric oxide and HPA axis: A closer look at human hypothalamus. Med Hypotheses. 2004;62:158–9. doi: 10.1016/s0306-9877(03)00296-2. [DOI] [PubMed] [Google Scholar]
- 16.Lv F, Shen YW, Peng LH, Li P, Luo J, Wei K, et al. Effects of propofol on expression of hippocampal neuronal nitric oxide synthase and carboxy-terminal PDZ ligand of neuronal nitric oxide synthase in stressed rats undergoing electroconvulsive shock. J ECT. 2013;29:297–302. doi: 10.1097/YCT.0b013e318290fa17. [DOI] [PubMed] [Google Scholar]
- 17.Patil CS, Singh VP, Kulkarni SK. Modulatory effect of sildenafil in diabetes and electroconvulsive shock-induced cognitive dysfunction in rats. Pharmacol Rep. 2006;58:373–80. [PubMed] [Google Scholar]
- 18.Wei T, Chen C, Hou J, Xin W, Mori A. Nitric oxide induces oxidative stress and apoptosis in neuronal cells. Biochim Biophys Acta. 2000;1498:72–9. doi: 10.1016/s0167-4889(00)00078-1. [DOI] [PubMed] [Google Scholar]
- 19.Förstermann U, Sessa WC. Nitric oxide synthases: Regulation and function. Eur Heart J. 2012;33:829. doi: 10.1093/eurheartj/ehr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coleman JW. Nitric oxide in immunity and inflammation. Int Immunopharmacol. 2001;1:1397–406. doi: 10.1016/s1567-5769(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 21.Sharma JN, Al-Omran A, Parvathy SS. Role of nitric oxide in inflammatory diseases. Inflammopharmacology. 2007;15:252–9. doi: 10.1007/s10787-007-0013-x. [DOI] [PubMed] [Google Scholar]
- 22.Wang ZY, Waldeck K, Grundemar L, Håkanson R. Ocular inflammation induced by electroconvulsive treatment: Contribution of nitric oxide and neuropeptides mobilized from C-fibres. Br J Pharmacol. 1997;120:1491–6. doi: 10.1038/sj.bjp.0701083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York, USA: Biometric Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 24.Ázkürkçügil A, Aydemir Á, Yıldız M, Esen Danacı A, Köroğlu E. Reliability and Turkish adaptation of the structured clinical interview for DSM-IV axis I disorders. Med Treatment J. 1999;12:233–6. [Google Scholar]
- 25.Gaynes BN, Lux L, Gartlehner G, Asher G, Forman-Hoffman V, Green J, et al. Defining treatment-resistant depression. Depress Anxiety. 2020;37:134–45. doi: 10.1002/da.22968. [DOI] [PubMed] [Google Scholar]
- 26.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Akdemir AÁ, Dağ İ, Türkçapar HM, İşcan N, Ázbay H. Validity, reliability and clinical use of the Hamilton Depression Rating Scale. Psychiatry Psychol Psychopharmacol. 1996;4:251–8. [Google Scholar]
- 28.Bag S, Canbek O, Atagun IM, Kutlar TM. Early effects of modern electroconvulsive therapy on subjective memory in patients with mania or depression. Indian J Psychiatry. 2016;58:198–203. doi: 10.4103/0019-5545.183782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lundberg JO, Weitzberg E, Gladwin MT. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Discov. 2008;7:156–67. doi: 10.1038/nrd2466. [DOI] [PubMed] [Google Scholar]
- 30.Selek S, Savas HA, Gergerlioglu HS, Bulbul F, Uz E, Yumru M. The course of nitric oxide and superoxide dismutase during treatment of bipolar depressive episode. J Affect Disord. 2008;107:89–94. doi: 10.1016/j.jad.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 31.Savas HA, Gergerlioglu HS, Armutcu F, Herken H, Yilmaz HR, Kocoglu E, et al. Elevated serum nitric oxide and superoxide dismutase in euthymic bipolar patients: Impact of past episodes. World J Biol Psychiatry. 2006;7:51–5. doi: 10.1080/15622970510029993. [DOI] [PubMed] [Google Scholar]
- 32.Jopek R, Kata M, Nowak G. The activity of rat brain nitric oxide synthase following chronic antidepressant treatment. Acta Pol Pharm. 1999;56:307–10. [PubMed] [Google Scholar]
- 33.Nowak G, Kata M, Jopek R, Siedlecki A. Chronic electroconvulsive treatment increases the activity of nitric oxide synthase in the rat brain. Pol J Pharmacol. 1997;49:379–82. [PubMed] [Google Scholar]
- 34.Lozano R, Marín R, Santacruz MJ, Frutos AJ. Blood urea levels associated to antidepressant drug treatment: Role of nitrogen and nitric oxide. Indian J Psychiatry. 2019;61:314–5. doi: 10.4103/psychiatry.IndianJPsychiatry_141_10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roman A, Nalepa I. Effect of repeated administration of paroxetine and electroconvulsive shock on the proliferative response of lymphocytes and the synthesis of nitric oxide by macrophages in rats. J ECT. 2005;21:111–7. doi: 10.1097/01.yct.0000167462.33586.6d. [DOI] [PubMed] [Google Scholar]
- 36.Cortese-Krott MM, Kelm M. Endothelial nitric oxide synthase in red blood cells: Key to a new erythrocrine function? Redox Biol. 2014;2:251–8. doi: 10.1016/j.redox.2013.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bioque M, Mac-Dowell KS, Meseguer A, Macau E, Valero R, Vieta E, et al. Effects of electroconvulsive therapy in the systemic inflammatory balance of patients with severe mental disorder. Psychiatry Clin Neurosci. 2019;73:628–35. doi: 10.1111/pcn.12906. [DOI] [PubMed] [Google Scholar]
- 38.Joca SR, Sartim AG, Roncalho AL, Diniz CF, Wegener G. Nitric oxide signalling and antidepressant action revisited. Cell Tissue Res. 2019;377:45–58. doi: 10.1007/s00441-018-02987-4. [DOI] [PubMed] [Google Scholar]
- 39.Dhir A, Kulkarni SK. Nitric oxide and major depression. Nitric Oxide. 2011;24:125–31. doi: 10.1016/j.niox.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 40.Pérez-Torres I, Manzano-Pech L, Rubio-Ruíz ME, Soto ME, Guarner-Lans V. Nitrosative stress and its association with cardiometabolic disorders. Molecules. 2020;25:2555. doi: 10.3390/molecules25112555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moylan S, Berk M, Dean OM, Samuni Y, Williams LJ, O’Neil A, et al. Oxidative and nitrosative stress in depression: Why so much stress? Neurosc Biobehav Rev. 2014;45:46–62. doi: 10.1016/j.neubiorev.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 42.Takada JY, Solimene MC, da Luz PL, Grupi CJ, Giorgi DM, Rigonatti SP, et al. Assessment of the cardiovascular effects of electroconvulsive therapy in individuals older than 50 years. Braz J Med Biol Res. 2005;38:1349–57. doi: 10.1590/s0100-879x2005000900009. [DOI] [PubMed] [Google Scholar]
- 43.Rumi DO, Solimene MC, Takada JY, Grupi CJ, Giorgi DM, Rigonatti SP, et al. Electrocardiographic and blood pressure alterations during electroconvulsive therapy in young adults. Arq Bras Cardiol. 2002;79:149–60. doi: 10.1590/s0066-782x2002001100007. [DOI] [PubMed] [Google Scholar]
- 44.Ogawa-Okamoto C, Saito S, Nishihara F, Yuki N, Goto F. Blood pressure control with glyceryl trinitrate during electroconvulsive therapy in a patient with cerebral aneurysm. Eur J Anaesthesiol. 2003;20:70–2. doi: 10.1017/s0265021503210139. [DOI] [PubMed] [Google Scholar]
- 45.de Sousa RT, Zanetti MV, Busatto GF, Mouro MG, Zarate CA, Jr, Gattaz WF, et al. Lithium increases nitric oxide levels in subjects with bipolar disorder during depressive episodes. J Psychiatr Res. 2014;55:96–100. doi: 10.1016/j.jpsychires.2014.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Canbek O, Ipekcıoglu D, Menges OO, Atagun MI, Karamustafalıoglu N, Cetinkaya OZ, et al. Comparison of propofol, etomidate, and thiopental in anesthesia for electroconvulsive therapy: A randomized, double-blind clinical trial. J ECT. 2015;31:91–7. doi: 10.1097/YCT.0000000000000190. [DOI] [PubMed] [Google Scholar]
- 47.Yagmurdur H, Ayyildiz A, Karaguzel E, Akgul T, Ustun H, Germiyanoglu C. Propofol reduces nitric oxide-induced apoptosis in testicular ischemia-reperfusion injury by downregulating the expression of inducible nitric oxide synthase. Acta Anaesthesiol Scand. 2008;52:350–7. doi: 10.1111/j.1399-6576.2007.01545.x. [DOI] [PubMed] [Google Scholar]


