Abstract
In response to the need of more rigorous data on medical cannabis and chronic pain, we conducted a 3-month prospective study incorporating ecological momentary assessment (EMA) to examine the effects of medical cannabis on pain, anxiety/depression, sleep, and quality of life. Data were collected from 46 adults (Mean age=55.7±11.9, 52.2% male) newly initiating medical cannabis treatment for chronic pain. Participants completed a baseline survey, EMA for approximately 1 week pre- and up to 3 weeks post-medical cannabis treatment, and a 3-month follow-up survey. The self-reported EMA data (2535 random and 705 daily assessments) indicated significant reductions in momentary pain intensity (b = -16.5, p < .001, 16.5 points reduction on 0-100 visual analog) and anxiety (b = -0.89, p < .05), and significant increase in daily sleep duration (b = 0.34, p < .01) and sleep quality (b = 0.32, p <.001) after participants initiated medical cannabis for a few weeks. At 3 months, self-reported survey data showed significantly lower levels of worst pain (t = -2.38, p < .05), pain interference (t = -3.82, p < .05), and depression (t = -3.43, p < .01), as well as increased sleep duration (t = 3.95, p < .001), sleep quality (t = -3.04, p < .01), and quality of life (t = 4.48, p < .001) compared to baseline. In our sample of primarily middle-aged and older adults with chronic pain, medical cannabis was associated with reduced pain intensity/inference, lower anxiety/depression, and improved sleep and quality of life.
Keywords: pain, anxiety, depression, medical cannabis, ecological momentary assessment
Despite the inconsistent findings on its effectiveness, medical cannabis is increasingly accessible in the United States (U.S.) and other countries, with chronic pain as the most commonly cited condition for use (Cooke et al., 2019). The 36 million adults 45 years and older in the U.S. living with chronic pain (Dahlhamer et al., 2018) represent a fast-growing segment of cannabis users. A recent analysis of the National Survey on Drug Use and Health data showed a 10% annual increase of past year cannabis use for 50-64 years old and a 15% annual increase for 65 and older between 2002 and 2014 (Salas-Wright et al., 2017). This increasing trend in cannabis use among middle aged and older adults may reflect the trend of individuals seeking medical cannabis as an alternative pain treatment to more conventional options (Boehnke et al., 2019).
Current Evidence Regarding Cannabis's Efficacy on Chronic Pain
Current research evidence of cannabis's efficacy on chronic pain is relatively restricted to clinical trials of FDA-approved products (e.g., nabiximols) or low potency smoking cannabis (National Academies of Sciences, 2017). The studies have been primarily short-term (2-6 weeks) and often relied on retrospective self-reported outcomes from surveys (Deshpande et al., 2015). Several recent meta-analyses reached inconsistent conclusions: while some showed significant effects of cannabis on chronic pain (Whiting et al., 2015), others showed no such effect (Stockings et al., 2018). Similarly, some research showed that medical cannabis has significant “opioid-sparing” effect, while others found no such effect (Dyer, 2019; Segura et al., 2019; Shah et al., 2019; Wen & Hockenberry, 2018). The potential of medical cannabis as an alternative treatment for chronic pain needs to be carefully examined by weighing potential risks against benefits, based on quality scientific data (Lev-Ran et al., 2013; Volkow et al., 2014).
Importance of Investigating Real-World Medical Cannabis Use
With increased accessibility of medical cannabis, there is an urgent need to investigate the real-world medical cannabis products, which usually have a higher concentration of tetrahydrocannabinol (THC) and/or cannabidiol (CBD) compared to recreational cannabis (i.e., cannabis that is not obtained from a licensed dispensary) and a greater diversity in administration modes (e.g., vape, capsule, tincture, cream). Currently there are no guidelines for clinicians to discuss the risk and benefits of cannabis use in chronic pain management, including side effects (Cooke et al., 2019). With the increasing prevalence of medical cannabis use as an alternative pain treatment, it would be a missed opportunity if data on efficacy and side effects associated with diverse medical cannabis products (e.g., vape vs. concentrate) are not investigated (Vyas et al., 2018).
Ecological Momentary Assessment (EMA) as a Tool for Medical Cannabis Research
One of the significant barriers to medical cannabis research is the product diversity in administration mode, chemical composition, and lack of standard dosing. Smartphone-based ecological momentary assessment (EMA) provides an ideal tool for capturing detailed self-reported data about product information, patterns of use, symptom relief, and side effects in patients’ daily lives with high ecological validity and lower recall bias/errors (Shiffman et al., 2008). Some prior research has used EMA to examine cannabis use and its consequences, but the majority focused on adolescents or young adults specific to recreational use (Emery et al., 2020). Studies characterizing medical cannabis use in patients’ daily lives and tracking real-time outcomes (i.e., measured in the moment via EMA) such as pain intensity, anxiety/depressive symptoms, and sleep duration/quality can address a significant gap in current understanding. To the best of our knowledge, there has not been any research tracking health outcomes using EMA among individuals initiating medical cannabis treatment over time.
Medical Cannabis in Florida
Florida has become the fastest growing medical cannabis market in the U.S. As of December 2020, approximately 447,400 persons hold an active medical cannabis card in Florida (Florida Department of Health, 2020). Patients first go to a medical cannabis doctor for certification if they have one of the qualifying conditions for medical cannabis use. The doctor will write a recommendation (not prescription) specifying the upper limit of THC and CBD content (in mgs) that the patient can purchase in a defined period (first refill is 70 days, then every 210 days) and the recommended administration mode/s. Then, the patient can go to the dispensaries to purchase whatever product as long as it is within the recommended dosage limit. Each product is labeled with the minimum concentration of THC and/or CBD (in ratio, percentage, or milligrams) with a total amount of cannabinoids in milligrams. During the first few weeks, patients often experiment with different products, administration modes, and doses as they seek to find options that work well for their condition/s while minimizing potential side effects. Therefore, EMA also allows for the unique opportunity to capture the dynamic process of self-titrating medical cannabis use during this period and the associated health benefits and side effects, whereas a follow up after several months could provide evidence on medical cannabis’ effects after the self-titration is complete.
Purpose of the Current Study
The main purposes of the study were: 1) to examine the real-time health outcomes before and after initiating medical cannabis treatment (i.e., real-time pain intensity, anxiety/depressive symptoms, and sleep) in adults with chronic pain using a smartphone-based EMA, and 2) to examine effects of medical cannabis on pain, anxiety/depression, sleep, and quality of life at 3 months after initiation of medical cannabis treatment using survey questionnaires. This study is considered an initial step toward a larger prospective cohort study that assesses real-time and long-term (12-month) outcomes among older adults with chronic pain initiating medical cannabis vs. a control group who will not initiate medical cannabis.
METHODS
Participants
Patients were eligible if they were 18 years or older, were seeking but had not yet initiated medical cannabis treatment, had a smartphone, and indicated that chronic pain was their primary reason for medical cannabis use. Participants were excluded if they had terminal diseases (e.g., cancer) or a condition known to cause cognitive impairment (e.g., Parkinson's disease). The study protocol was approved by the University of Florida Institutional Review Board, and all participants provided written consent prior to participation.
Procedures
This study included a baseline survey, an up to 4-week period of EMA, and a 3-month follow-up survey. Participants were compensated up to $210 for the EMA portion of the study, and $25 for each survey. Data reported in this paper were collected between April 2019 and September 2020.
Recruitment
Participants were recruited from four medical cannabis clinics in North-Central Florida. When new patients with chronic pain came in to seek medical cannabis treatment, doctors or clinical staff would briefly introduce the study and refer interested patients to research staff who were either present in the clinic or available by phone to complete a screening. After the physician assessment and submission of the medical cannabis card application for the patients, it took at least one week before the participants’ medical cannabis card was approved by the state. Participants would not be able to obtain medical cannabis products before their application was approved. The waiting period provided an ideal opportunity for the baseline assessments including the survey and baseline EMA. Eligible participants were scheduled for an in-person baseline assessment at the medical cannabis clinic or a university research space. Due to the COVID-19 pandemic, participants recruited after March 2020 completed their baseline assessment remotely via Zoom video-conferencing or over the phone with informed consent and survey links sent to them prior to the appointment.
Sample Characteristics
Our sample included 46 participants (52.2% male, 47.8% female) with an average age of 55.7 (SD = 11.9). Complete demographic information is summarized in Table 1. The majority of the participants were non-Hispanic white, which was consistent with the demographics of medical cannabis patients in Florida (Brown et al., 2020). Most participants reported having some college education or higher, and were married or living with a long-term partner. More than half of the sample were not employed (either disabled or retired), and their income levels spanned across a wide range with relatively even distribution across four categories (i.e., under $20K, $20K-40K, $40-60K, and over $60K). The baseline pain intensity in the past 24 hours measured by Brief Pain Inventory (Cleeland & Ryan, 1994) was 8.2 (SD = 1.5) at its worst, 6.1 (SD = 1.9) on average, and 4.4 (SD = 2.0) at its least, indicating this sample suffered from moderate to severe pain. The majority (91.3%) of participants reported having used cannabis in their lifetime and 33.3% reported current non-dispensary cannabis use in the past 30 days.
Table 1.
Sample Characteristics of the Study Population (N = 46)
| Variable | Value |
|---|---|
| Age in years | |
| Mean ± SD | 55.7±11.9 |
| Hispanic | |
| Yes | 3 (6.5%) |
| No | 43 (93.5%) |
| Race | |
| White | 21(87.5%) |
| Black/African American | 3 (12.5%) |
| Gender | |
| Male | 24 (52.2%) |
| Female | 22 (47.8%) |
| Education | |
| High school graduate or GED | 8 (17.4%) |
| Some college or technical/trade school | 19 (41.3%) |
| College or higher | 19 (41.3%) |
| Marital status | |
| Married/living with a long-term partner | 27 (58.7%) |
| Divorced/separated | 13 (26.3%) |
| Widowed | 2 (4.3%) |
| Never married and not living with a long-term partner | 4 (8.7%) |
| Employment status | |
| Yes, employed for wages | 14 (30.4%) |
| Yes, self-employed | 4 (8.7%) |
| No | 28 (60.9%) |
| Income | |
| 0-$20,000 | 12 (26.1%) |
| $20,001-$40,000 | 11 (23.9%) |
| $40,001-$60,000 | 9 (19.6%) |
| More than $60,000 | 8 (17.4%) |
| Don’t know/don’t want to answer | 6 (13.0%) |
| Cannabis use prior to starting medical cannabis | |
| Used in past 30 days | 14 (33.3%) |
| Not used in past 30 days, but within 12 months | 8 (19.1%) |
| Not used for more than 12 months | 20 (47.6%) |
Survey Questionnaire: Baseline and Follow-Up
After consenting and before receiving their medical cannabis card, participants completed a baseline survey (either paper-and-pencil or online) which included questions such as demographics (e.g., age, gender, ethnicity/race, education, marital status, employment status, and income); history of and current cannabis use (other than medical cannabis); and health outcomes such as pain intensity and pain interference, depression, anxiety, sleep, and overall health-related quality of life (detailed below). At approximately 3 months after their baseline survey, participants completed a follow-up survey. The follow-up survey included the same health-related questions as the baseline survey in order to evaluate possible changes in health outcomes over 3 months (e.g., pain, sleep, quality of life).
Demographics.
Age was reported in years. Gender was categorized into male, female, transgender, or other. Ethnicity/race was assessed with two questions—one asking about whether they were Hispanic/Latino, the other asking about which race group they consider themselves belonging to (i.e., White, Black/African American, Native American, Asian, Multiracial, and Other). Education was categorized into elementary school or below, some high school, high school graduate or GED, some college or technical/trade school, college or trade school graduate, and graduate school or higher. Marital status was categorized into married/living with a long-term partner, divorced/separated, widowed, and never married. Employment was categorized into yes or no, with additional information regarding the non-employment status (i.e., student, retired, disabled, unable to work, or other). Income level was categorized into 0-$20,000, $20,001-$40,000, $40,001-$60,000, $60,001-$80,000, $80,001-$100,000, and more than $100,000. For all questions, participants were also provided the option “Don’t know/don’t want to answer”.
History of and current cannabis use.
Participants were asked to report whether they had ever used cannabis in their lifetime, if so, when was their first use (age). If they reported yes, participants were also asked how long it has been since they last used cannabis that is not medical cannabis. Answering options included “within the past 30 days”, “more than 30 days but within the past 12 months”, and “more than 12 months ago”.
Pain intensity.
The Brief Pain Inventory (BPI; Cleeland & Ryan, 1994) is a widely used measurement tool for assessing clinical pain, which allows participants to rate the severity of their pain using numerical levels. Participants were first asked to report whether they had any pain that was “more than minor everyday kind of pain” in the past four weeks. If yes, they were further asked to report whether they had more than minor pain in the past 24 hours. If the answer was still yes, they used a scale from 0 to 10 to rate their pain intensity “at its worst”, “on average”, “at its least” in the past 24 hours, and “right now”, with higher scores indicating higher pain intensity. Individual score ratings (especially pain at its worst) were used to represent participants’ pain intensity levels based on the BPI user guide (Cleeland, 2009).
Pain interference.
The PROMIS Short Form v1.0-Pain Interference 4a (adult version) (Amtmann et al., 2010) was used to measure pain interference at baseline and follow up. This measure is a four-item scale assessing to what extent pain has interfered with participants’ daily lives (e.g., household chores, social activities) in the past seven days, on a five-point Likert scale ranging from 1-“not at all” to 5-“very much”. The mean score of the four items was calculated with a higher score indicating more pain interference. The Cronbach's alpha for this scale in the current study was .93, indicating excellent internal reliability.
Depression.
The Patient Health Questionnaire (PHQ-8) was used to measure depressive symptoms (Kroenke et al., 2001). The PHQ is a widely used measure for assessing the severity of depressive symptoms in both clinical and research settings (Kroenke et al., 2009). Participants were asked to rate their depressive symptoms over the past two weeks on a four-point scale from 0-“not at all” to 3-“nearly every day”. A total score of the eight items was calculated to represent the overall severity of depressive symptoms, with a higher score indicating more severe depression. The Cronbach's alpha for this scale in the current study was .88.
Anxiety.
The 7-item scale for generalized anxiety disorder (GAD-7) was used for measuring generalized anxiety (Spitzer et al., 2006). The GAD-7 is also a widely used measure that has been applied in both clinical and research settings (Löwe et al., 2008). Participants were asked to rate their anxiety symptoms on a four-point scale from 0-“not at all” to 3-“nearly every day” in the past two weeks. A total score was calculated to represent the overall anxiety severity, with a higher score indicating higher level of anxiety. The Cronbach's alpha for this scale in the current study was .93.
Sleep quality.
We adapted three questions from the widely used Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989) to assess sleep quality. These included how long (in minutes) it has taken for the participant to fall asleep each night, how many hours of actual sleep they usually got, and how they would rate their sleep quality from 0 “very bad” to 3 “very good”, in the past 30 days.
Health-related quality of life.
The Short-Form Health Survey (SF-8; Ware et al., 2001) was used to measure overall health-related quality of life. SF-8 is one of the most extensively validated and widely used measure for patient-reported quality of life worldwide (Tomás et al., 2018). Participants were asked to answer eight questions on general health, physical functioning, role limitations due to physical health problems, bodily pain, energy level, social functioning, mental health, and role limitations due to emotional problems during the past four weeks. The mean score of the eight items was calculated to indicate the overall health-related quality of life. The Cronbach's alpha for this scale in the current study was .83.
EMA
Participants completed approximately one week of baseline EMA before they initiated medical cannabis treatment and three weeks of EMA after they started the treatment. After completion of the survey, research staff instructed the participants to download the mEMA app (ilumivu Inc.), which is a commercial EMA app compatible with both iOS and Android systems, onto their smartphone and taught them how to use the app. The app allows researchers to program the schedule (e.g., randomized or at a specific time) for the assessments and automatically sends a push notification when it is time for the assessment on the participant's smartphone. Each participant received one daily assessment and 3-4 random assessments per day for approximately three weeks. They were given 60 minutes to complete the daily assessments and 30 minutes for the random assessments. Participants received the daily assessment every day at 10am and the schedule for the random assessments was set up using the randomization function when we created the EMA survey on the ilumivu platform. We used four hours as the approximate interval between random prompts during participants’ awake hours (between 8am and 10pm unless participants requested other timeframe), which automatically generates 3-4 time points for the random assessments in the system. The daily prompts included 10 questions asking about participants’ health in the past 24 hours, including sleep duration (in hours), sleep quality (from 1-“very poor” to 5-“very good”), and whether they used any other medication (e.g., opioid, sleeping pills). The random prompts included 18 questions on real-time feelings and symptoms, such as their real-time pain intensity level (i.e., 0-100 visual analog), anxiety and depressive symptoms using the respective subscale from the Brief Symptoms Inventory (Derogatis & Melisaratos, 1983) on a five-point Likert scale from 1-“not at all” to 5-“extremely”. After they started using medical cannabis, the daily and random prompts also included some additional questions (five for daily and six for random prompts, respectively) on medical cannabis use and outcomes (e.g., product composition, dosage, administration mode, and side effects).
Since this study was an initial step toward a larger project, we adjusted our EMA procedures over time to make it more suitable for the specific population. We intended to capture at least one-week baseline data before participants initiated medical cannabis use and track their outcomes for at least two weeks after they started using medical cannabis. Therefore, the original plan was to have three weeks of EMA assessments in total. We also originally planned for only one daily prompt and three random prompts per day (n = 84 in total for three weeks). To encourage participants to be more adherent to the EMA procedure, the incentives were set to be $105 if participants completed at least 60% of all the prompts (n = 50), and another $105 if they completed at least 80% of all the prompts (n = 67). If they didn’t complete at least 60%, the incentives were prorated based on how many they completed. However, many of our participants encountered technological difficulties with the EMA app where they either didn’t receive some prompts, or their responses were partially recorded. Some of these difficulties were due to device or app issues, whereas others may have been attributable to participants not being technologically savvy. To account for these issues, we increased the frequency of random prompts from three to four times per day and allowed participants to extend their EMA period if they desired to continue until they completed the 60% or 80% of the total prompts. This flexibility allowed us to collect more data points to capture the changes in symptoms, which was the main goal of this pilot study, but also resulted in a wider range of days of EMA completed by participants.
Statistical Analysis
Descriptive analyses (mean, standard deviation, frequency and percentage, etc.) were conducted on selected variables (i.e., demographics, history of and current cannabis use, pain level and interference) at baseline to describe the sample characteristics. Cronbach's alpha was calculated for established scales (described in the Measures) to test the internal consistency of each scale.
For EMA data, to assess whether real-time health outcomes changed after participants started using medical cannabis, we used linear mixed effects models to estimate the changes in pain intensity, anxiety, depressive symptoms, sleep duration, and sleep quality during the pre- and post-medical cannabis periods (Bolger & Laurenceau, 2013). Missing data were minimal (< 5%) because participants need to provide an answer to each question before they could advance to the next question. Missing data on questions only occurred when the survey was terminated in the middle due to technical difficulties (e.g., app crashed, internet connection issue). The analyses were based on available data points for each outcome without any imputation because there were sufficient data points for each outcome. Pairwise deletion was the default when there was missingness in any variable included in the models. For each outcome of interest, we built three mixed effects models progressively to identify the model that best fit the data. Pre- and post-medical cannabis changes in outcomes were contrasted by including a dichotomous variable in the model to indicate whether the datapoint was pre- or post-cannabis treatment (0 vs. 1). For example, we first built a mixed effects model with only a random intercept, which allows each participant's baseline value to vary freely when examining whether pain level changed before and after participants started using medical cannabis. Then we added a random slope in the model to allow the rate of change in pain intensity to also vary freely. Finally, we added potential covariates such as gender, race, and age to control for these variables in the model. At each step of adding a new parameter in the model, we compared model fitness to the previous model using an ANOVA test and AIC/BIC values, with a significant ANOVA test and smaller AIC/BIC values indicating better fit. Results from the model with the best fitness were presented for each outcome variable.
For survey data, we used paired t-tests to examine changes in pain intensity, anxiety/depression, sleep quality, and health-related quality of life by comparing 3-month follow-up and baseline survey results.
Type I error was set at p < 0.05 for all statistical analyses. Data cleaning and descriptive analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC). The linear mixed effects model analyses were conducted using the lme4 package (Bates et al., 2015) with the open source software R Version 3.6.2 (R Core Team, 2019).
RESULTS
Real-Time Outcomes Pre- and Post-Medical Cannabis Treatment during the EMA Period
EMA Completion Rates
Thirty-nine of the 46 participants completed the EMA portion (one older participant found the mEMA app difficult and was unable to learn how to use it; two discontinued with the EMA portion due to busy work schedules; four withdrew from the study after they completed the baseline survey). In the final analysis, we also excluded two participants who completed less than seven days of EMA which was unlikely to be sufficient data for capturing the changes pre- and post-medical cannabis treatment. These two participants were in the EMA period for between two and four weeks, but had many glitches while using the EMA app, so they only completed very few assessments. As a result, 37 participants’ EMA data were included in the final analysis (2514 random and 705 daily assessments). The compliance rate was 80.8% and 90.3% for daily and random prompts respectively (based on 21 daily prompts, 63 random prompts as required). The range of random and daily assessments completed by each participant was 12-112 and 8-41 respectively.
Nature and Composition of Medical Cannabis Products and Side Effects
A wide range of products were used by participants with many using at least two during their treatment (e.g., sublingual drop plus vaping). Sublingual/oral and vaping were the two most commonly used administration modes, reported in 554 (37.9%) and 544 (37.2%) out of 1461 random assessments after participants started medical cannabis. The composition of medical cannabis products used by the participants ranged from 100% CBD to 100% THC with various THC:CBD ratios in between (e.g., 1:1, 20:1, 60:1). The most commonly reported side effects included balance problems and dizziness, reported in 250 (17.1%) and 160 (10.9%) out of 1461 random assessments, respectively, after the initiation of medical cannabis treatment.
Changes in EMA Measured Real-Time Health Outcomes
Mixed effects models for each outcome contrasting pre- and post-treatment EMA data with random intercept and random slope had the best model fitness and showed significant reduction in real-time pain intensity level (b = -16.5, p< .001, meaning that there was a 16.5 point reduction on the 0-100 visual analog), anxiety (b = -0.89, p< .05, meaning that there was a 0.89-point decrease of anxiety on the five-point Likert scale), longer sleep duration (b = 0.34, p< .01, meaning that there was a 0.34 hour increase in sleep), and better sleep quality (b = 0.32, p<.001, meaning that there was a 0.32 point increase of sleep quality on the five-point Likert scale), after participants started using medical cannabis. However, there was no significant improvement in real-time depressive symptoms (b = -0.17, p= .06). Gender, age, and race were not significantly associated with changes in the outcomes in any of the mixed effects models, and the models including these covariates did not have significantly better model fitness than the ones without these variables. Thus, the results reported above were based on models without these covariates.
Figure 1 presents the pain intensity trajectories of the 37 participants over the course of their EMA period. The overall group trajectory showed an initial steep reduction in pain intensity after participants started medical cannabis treatment, and then the reduction became smaller in magnitude where the pain intensity level fluctuated to some extent but remained relatively stable.
Figure 1.
Pain Intensity Trajectory of 37 Adults Pre- and Post-Medical Cannabis Treatment
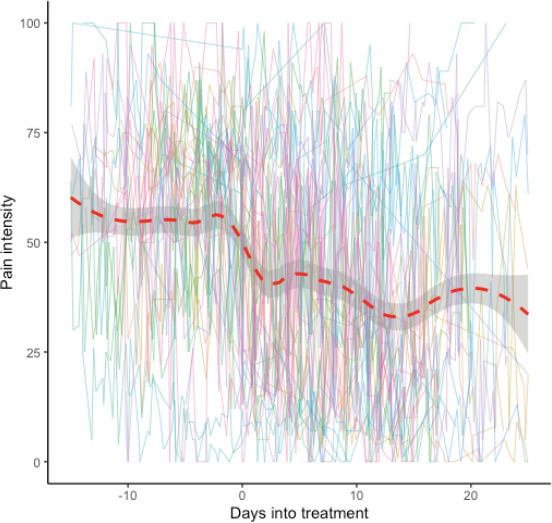
Note. The individual lines represent the real-time pain intensity ratings for each participant over time. The red dash line represents the overall trend of the 38 participants. Data from all participants were aligned so that Day 0 was the first day of starting medical cannabis for each participant. The time axis therefore indicates how many days before (negative numbers) or after (positive numbers) medical cannabis treatment. The overall trend curve was constructed using LOWESS with bandwidth of 0.3 (Cleveland, 1979). The overall trend curve was constructed data up to 15 days before and 20 days after Day 0, given that this was the period where the majority of participants had available data.
Changes in Health Outcomes Measured by Survey at Baseline and 3 Months
A total of 42 participants (91.3% retention rate) out of the original 46 participants completed the 3-month follow-up survey. Five (11.9%) out of the 42 participants reported discontinuation of medical cannabis use at three months. Results reported in the sections below were based on all 42 participants who completed the follow-up survey. In Table 2, main outcomes at baseline and three months are presented, with an additional column to show the results for only those who were still using medical cannabis at three months (n = 37), which were not significantly different from the results based on all 42 participants (“intention to treat”).
Table 2.
Main Outcomes Based on Survey Data at Baseline and 3-Month Follow Up, Mean (SD)
| Measures with respective score range or measuring unit | Baseline (N = 46) | 3 months (N = 42) | 3 months: MC subgroup1 (N = 37) |
|---|---|---|---|
| Pain | |||
| No more than minor pain (%)* | 13.0% | 33.3% | 35.1% |
| At its worst (0-10)* | 8.15(1.51) | 7.25(2.25) | 7.46(2.13) |
| At its least (0-10) | 4.37(1.98) | 3.64(2.18) | 3.87(2.19) |
| On average (0-10)* | 6.05(1.91) | 5.21(2.35) | 5.46(2.26) |
| Pain interference (1-5)* | 3.64(1.09) | 2.90(1.11) | 2.96(1.16) |
| Anxiety (1-21) | 6.50(6.10) | 4.69(5.64) | 4.54(5.73) |
| Depression (1-24)* | |||
| Sleep | 8.50(6.10) | 5.67(5.42) | 5.46(5.44) |
| Time to fall asleep (minutes) | 65.7(54.9) | 50.8(45.8) | 47.0(46.8) |
| Hours of sleep (hours)*** | 5.31(1.83) | 6.17(1.79) | 6.36(1.72) |
| Sleep quality (1-5)** | 1.17(0.93) | 1.64(0.85) | 1.73(0.84) |
| Quality of life (1-5)*** | 2.72(0.68) | 3.27(0.78) | 3.23(0.77) |
Note. 1MC subgroup refers to those who were still using medical cannabis at 3-month follow up.
p < .05,
p < .01,
p < .001.
Pain Intensity and Pain Interference
At baseline, six (13.0%) out of the 46 participants reported that they had no more than minor everyday kind of pain in the past 24 hours, whereas 40 of them reported moderate to severe pain based on their BPI score as described in the sample characteristics. At the 3-month follow up, 14 (33.3%) out of the 42 participants who completed the follow up survey reported no more than minor pain in the past 24 hours. The proportion of participants who reported no more than minor pain at follow-up was significantly higher than baseline (χ2 = 6.59, df = 1, p < .05). For those who reported more than minor pain in the past 24 hours at baseline and follow-up, their worst pain (mean difference = -0.92, t = -2.38, df = 24, p < .05) and average pain (mean difference = -0.84, t = -2.31, df = 24, p < .05) were both significantly reduced compared to baseline average and worst intensity scores. Pain interference was also significantly reduced compared to baseline (mean difference = -0.75, t = -3.82, df = 41, p < .05).
Anxiety, Depression, Sleep Quality, and Quality of Life
At 3-month follow up, participants did not show significant reduction in anxiety measured by GAD-7 compared to the baseline (mean difference = -1.12, t= -1.51, df= 41, p= .14), but they showed significant improvement in their depressive symptoms compared to baseline (mean difference = -2.31, t= -3.43, df= 41, p< .01). With regard to sleep, participants reported no difference in how long it took them to fall asleep (mean difference = -8.33, t= -1.05, df= 40, p= .30), but they reported significant increases in actual sleep time (mean difference = 0.83, t= 3.95, df= 41, p< .001) and sleep quality (mean difference = 0.43, t= 3.04, df= 41, p< .01). Participants also reported significantly better overall health-related quality of life at three months than baseline (mean difference = 0.52 on a five-point Likert scale, t= 4.48, df= 41, p< .001).
DISCUSSION
The purpose of the study was to prospectively track health outcomes among individuals who newly initiated medical cannabis for chronic pain via both survey questionnaire and smartphone-based EMA. With the rapid increase of population using medical cannabis as an alternative to traditional pain treatment, high quality scientific evidence is urgently needed to inform patients, physicians, and policy makers. In this study, we investigated the real-time effects of medical cannabis using smartphone-based EMA, which allows for the capture of changes in daily symptoms (e.g., pain, anxiety, depression, and sleep) over several weeks. We also conducted a baseline and follow-up survey which allowed for examination of effects of medical cannabis on pain and related health outcomes at three months after participants started using medical cannabis. The discussion below is organized by outcome domains. We also included some discussion on applying EMA in medical cannabis research, as we believe that EMA could be a potentially valuable tool for future research on medical cannabis use and its health/side effects.
Medical Cannabis's Effects on Pain in Real-Time and 3 Months
Recent meta-analyses have reached inconsistent conclusions on whether cannabis is effective in treating chronic pain (Fisher et al., 2021; National Academies of Sciences, 2017; Stockings et al., 2018; Whiting et al., 2015). For example, the National Academies of Sciences, Engineering, and Medicine (2017) report found substantial evidence to support the effectiveness of cannabis for chronic pain, whereas the International Association for the Study of Pain (2021) position statement based on their two-year comprehensive review concluded that they do not endorse general use of cannabis or cannabinoids for pain relief due to the lack of high-quality clinical evidence (Fisher et al., 2021). In this study, there was a significant reduction in patient reported momentary pain level after they started medical cannabis treatment compared to baseline pain level in the EMA assessments. The magnitude of reduction was 16.5 points out of a 0- to 100-point visual analog. As illustrated in Figure 1, the baseline real-time pain intensity score for the group was around 60 before initiating medical cannabis treatment, with a 16.5 point reduction representing 27.5% reduction, which is considered clinically significant improvement (Salaffi et al., 2004). This was significantly larger than the pooled change in pain intensity generated from the meta-analysis in Stockings et al.'s (2018) paper, which was 3 mm reduction on a 100 mm visual analogue scale. There could be several possible explanations for this discrepancy. Most of the studies reviewed by Stockings et al. (2018) used either lower potency smoking cannabis (i.e., flower) or FDA-approved products (e.g., Nabiximols, Dronabinol). This study examined the effects of real-world cannabis products sold at various Florida dispensaries, which have a higher potency (% of THC) and greater diversity of chemical components (e.g., THC:CBD ratio). The differences in cannabis products may have resulted in the different efficacy for pain reduction. Also, prior studies mostly relied on retrospective self-report of pain as the outcome. EMA may provide more accurate pain ratings as it captures real-time pain ratings in patients’ daily lives (May et al., 2018). Also, there were significant individual differences in the pain trajectory as shown in Figure 1. Although our analysis did not show significant differences in the comparison of real-time outcomes before and after medical cannabis treatment by gender, age, and race, future research with larger samples is needed to investigate interpersonal factors (e.g., age, gender, health status) that may impact outcomes from medical cannabis use.
Our results also showed sustained improvement after medical cannabis treatment on pain and related outcomes over three months with a high follow-up rate (>90%). There was a significant increase in the proportion of participants reporting no more than minor pain in the past 24 hours at 3-month follow up compared to the baseline (33% vs. 13%). Moreover, for those who reported more than minor pain, their worst and average pain intensity was significantly lower than their baseline ratings. In addition to pain intensity, there was also significant reduction in pain interference. Participants reported significantly less impact of pain on their daily activities and functioning (i.e., pain interference), which is an important aspect in evaluating pain treatment (Dworkin et al., 2005).
Medical Cannabis's Effect on Anxiety/Depression, Sleep and Quality of Life Outcomes in Real-Time and 3 Months
Anxiety, depression, and insomnia are common comorbidities associated with chronic pain (Wilson et al., 2002). Successful pain management strategies should also evaluate patients’ physical and emotional functioning as core measures (Turk et al., 2003). Our study showed significant reductions in participants’ real-time anxiety after they started medical cannabis, and significant reduction in depressive symptoms over 3 months. These findings are inconsistent with the conclusion from Stockings et al's (2018) meta-analysis that cannabis had no significant impacts on physical or emotional functioning in individuals with chronic pain. Stockings et al. also concluded that there was low-quality evidence whether cannabis improved sleep among individuals with chronic pain. However, our study indicated significant improvement in sleep including a longer duration of sleep and better sleep quality both in daily EMA assessments and at the 3-month follow up, which is consistent with a recent prospective study based on observational data from new medical cannabis patients with chronic pain (Gruber et al., 2021). Again, there are several potential explanations for the discrepancy as noted above. Psychological factors such as expectancy or placebo effect could also play a role (Kaptchuk, 2002). Future research may consider using EMA in a larger sample or adding objective measures (e.g., polysomnography for sleep) to further validate our findings. Additionally, there are numerous causes and conditions that contribute to experiencing chronic pain. Individuals living with chronic pain represent a highly heterogeneous group. Medical cannabis research moving forward will need to pay more attention to the type of chronic pain being treated (e.g., neuropathic, musculoskeletal, cancer).
Participants also reported lower levels of depressive symptoms at three months, despite that medical cannabis did not show significant effect on improving real-time depressive symptoms. The result is plausible because improved sleep, reduced pain, and less anxiety over time can help improve mood and thus reduce depression. This is in line with prior research that shows improvement in anxiety often precedes the improvement in depression in people having co-occurrence of these two mental health issues (Bomyea et al., 2015). Our results also showed that sleep duration and self-reported sleep quality at three months were significantly improved, which is consistent with the results based on real-time data collected in the EMA. This finding suggests that the effect of medical cannabis on sleep in first few weeks during the EMA period persisted over three months. Finally, participants reported significant better overall health-related quality of life at three months compared to baseline, which is an important clinical outcome when evaluating chronic pain treatment (Dworkin et al., 2005).
Using EMA for Medical Cannabis Study
There is an increasingly wide application of smartphone-based EMA in various research areas including chronic pain and monitoring clinical interventions. We leveraged this tool to investigate medical cannabis use and real-time assessment of health and side effects in individuals with chronic pain (May et al., 2018). Our findings suggest that even with the older adult population, an EMA procedure combining one daily and 3-4 random prompts throughout the day is feasible and highly acceptable. It should be noted that 7 of the 46 participants didn’t complete the EMA procedure either due to challenges in using the app or their busy work schedule (these tended to be younger participants who were employed). Among those who completed the EMA procedure, their compliance rate for the daily and random prompts, based on how many assessments they were required to complete, was 80.8% and 90.3% respectively. This finding is consistent with prior studies that shows relatively high compliance rates of EMA procedures in older adult population (Cain et al., 2009).
Participants reported their medical cannabis use in great detail, including several important aspects of their use such as administration mode and dosage, which is critical to advance the research on cannabis's potential medicinal effects (Volkow & Weiss, 2020). Our results indicated that sublingual/oral and vaping were the most commonly used administration modes, reported in 37-38% of the post-medical cannabis treatment EMA sessions. Although participants reported the estimated dosage of their medical cannabis use, it was difficult to accurately measure and standardize the dose. As the EMA data showed, participants used a wide range of medical cannabis products, which made it challenging to convert their use to a common metric across different products (e.g., using the mgs of THC and mgs of CBD as a standard measure), especially for vaping and smoking. More education on the dosing of medical cannabis for patients to be able to record their doses in mgs of THC or CBD may help address this challenge in future research.
Strengths, Limitations, and Future Directions
This study took an initial step toward capturing real-time and longer-term effects of medical cannabis on individuals with chronic pain. One strength of the study was the inclusion of both pre- and post-medical cannabis use periods where pain level, mental health symptoms, and sleep quality can be compared. Another strength was the use of a smartphone-based EMA allowed us to examine the fluctuations in daily symptoms with a large number of data points during the first few weeks after medical cannabis initiation. Additionally, we had a high follow-up rate (over 90%), which helps to reduce the potential bias due to drop out. Despite these strengths, our sample size was relatively small and predominantly white. Future research with larger and diverse (e.g., oversampling of under-represented racial/ethnic groups) samples with a longer follow-up period (e.g., one year) is needed to further confirm the findings from this study. Also, despite the advantage of collecting data in real-time using EMA, our results were still based on self-report, which could be subject to biases resulted from social desirability or expectancy. Future studies could add objective measures for various health outcomes, such as incorporating biological measures (e.g., inflammatory biomarkers) or wearable sensors (e.g., monitors for sleep and/or physical functioning) to better evaluate the impact of medical cannabis on individuals with chronic pain. Finally, despite the current obstacles, randomized clinical trials of medical cannabis products may be a valuable next step to produce more rigorous evidence on medical cannabis and chronic pain.
Conclusions
In this middle aged and older adult sample with chronic pain, our findings provided preliminary evidence to support significant effects of medical cannabis on real-time pain intensity, anxiety, and sleep measured by EMA. We also found effects of medical cannabis on pain intensity, pain interference, depression, sleep quality, and overall health-related quality of life at 3 months after medical cannabis treatment.
Funding and Acknowledgements:
This project is supported by the University of Florida Center for Research to Investigate Substance use and Pain (UF-CRISP) and part of the University of Florida's “Creating the Healthiest Generation” Moonshot Initiative, which is supported by the UF Office of the Provost, UF Office of Research, UF Health, UF College of Medicine, and the UF Clinical and Translational Science Institute.
The REDCap service is funded by NCATS grant UL1 TR000064.
We would like to thank all the clinics (Releafe Now, CannaMD, and Florida Marijuana Doctor) who helped with the study recruitment. We especially appreciate the recruitment support from Drs. John (Jack) Crump and Justin Davis, Ms. Debbie Mendez-Vigo, and Ms. Jessica Walters. We are grateful to all the individuals who participated in our research.
REFERENCES
- Amtmann, D., Cook, K. F., Jensen, M. P., Chen, W. H., Choi, S., Revicki, D., Cella, D., Rothrock, N., Keefe, F., Callahan, L., & Lai, J. S. (2010). Development of a PROMIS item bank to measure pain interference. Pain, 150(1), 173–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates, D., Mächler, M., Bolker, B., & Walker, S. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48. [Google Scholar]
- Boehnke, K. F., Scott, J. R., Litinas, E., Sisley, S., Williams, D. A., & Clauw, D. J. (2019). Pills to pot: Observational analyses of cannabis substitution among medical cannabis users with chronic pain. The Journal of Pain, 20(7), 830–841. [DOI] [PubMed] [Google Scholar]
- Bolger, N., & Laurenceau, J.-P. (2013). Intensive Longitudinal Methods: An Introduction to Diary and Experience Sampling Research. Guilford Publications. [Google Scholar]
- Bomyea, J., Lang, A., Craske, M. G., Chavira, D. A., Sherbourne, C. D., Rose, R. D., Golinelli, D., Campbell-Sills, L., Welch, S. S., Sullivan, G., Bystritsky, A., Roy-Byrne, P., & Stein, M. B. (2015). Course of symptom change during anxiety treatment: Reductions in anxiety and depression in patients completing the Coordinated Anxiety Learning and Management program. Psychiatry Research, 229(1-2), 133–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, J. D., Costales, B., van Boemmel-Wegmann, S., Goodin, A. J., Segal, R., & Winterstein, A. G. (2020). Characteristics of older adults who were early adopters of medical cannabis in the Florida Medical Marijuana Use Registry. Journal of Clinical Medicine, 9(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. [DOI] [PubMed] [Google Scholar]
- Cain, A. E., Depp, C. A., & Jeste, D. V. (2009). Ecological momentary assessment in aging research: a critical review. Journal of Psychiatric Research, 43(11), 987–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleeland, C. S., & Ryan, K. M. (1994). Pain assessment: global use of the Brief Pain Inventory. Annals of the Academy of Medicine Singapore (23), 2. [PubMed] [Google Scholar]
- Cleeland, C. S. (2009). The Brief Pain Inventory User Guide. Retrieved July 7, 2021, from https://www.mdanderson.org/education-and-research/departments-programs-and-labs/departments-and-divisions/symptom-research/symptom-assessment-tools/BPI̲UserGuide.pdf [Google Scholar]
- Cleveland, W. S. (1979). Robust locally weighted regression and smoothing scatterplots. Journal of the American Statistical Association, 74(368), 829–836. [Google Scholar]
- Cooke, A. C., Knight, K. R., & Miaskowski, C. (2019). Patients' and clinicians' perspectives of co-use of cannabis and opioids for chronic non-cancer pain management in primary care. The International Journal on Drug Policy, 63, 23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlhamer, J., Lucas, J., Zelaya, C., Nahin, R., Mackey, S., DeBar, L., Kerns, R., Von Korff, M., Porter, L., & Helmick, C. (2018). Prevalence of chronic pain and high-impact chronic pain among adults - United States, 2016. MMWR.Morbidity and Mortality Weekly Report, 67(36), 1001–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis, L. R., & Melisaratos, N. (1983). The Brief Symptom Inventory: an introductory report. Psychological Medicine, 13(3), 595–605. [PubMed] [Google Scholar]
- Deshpande, A., Mailis-Gagnon, A., Zoheiry, N., & Lakha, S. F. (2015). Efficacy and adverse effects of medical marijuana for chronic noncancer pain: Systematic review of randomized controlled trials. Canadian Family Physician Medecin de Famille Canadien, 61(8), E372–E381. [PMC free article] [PubMed] [Google Scholar]
- Dworkin, R. H., Turk, D. C., Farrar, J. T., Haythornthwaite, J. A., Jensen, M. P., Katz, N. P., Kerns, R. D., Stucki, G., Allen, R. R., Bellamy, N., Carr, D. B., Chandler, J., Cowan, P., Dionne, R., Galer, B. S., Hertz, S., Jadad, A. R., Kramer, L. D., Manning, D. C., Martin, S., McCormick, C. G., McDermott, M. P., McGrath, P., Quessy, S., Rappaport, B. A., Robbins, W., Robinson, J. P., Rothman, M., Royal, M. A., Simon, L., Stauffer, J. W., Stein, W., Tollett, J., Wernicke, J., Witter, J., & IMMPACT. (2005). Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain, 113(1-2), 9–19. [DOI] [PubMed] [Google Scholar]
- Dyer, O. (2019). Access to medical marijuana does not reduce opioid overdoses in US, study finds. BMJ (Clinical research ed.), 365, l4188. [DOI] [PubMed] [Google Scholar]
- Emery, N. N., Carpenter, R. W., Treloar Padovano, H., & Miranda, R. (2020). Why don't they stop? Understanding unplanned marijuana use among adolescents and young adults. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 34(5), 579–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher, E., Moore, R. A., Fogarty, A. E., Finn, D. P., Finnerup, N. B., Gilron, I., Haroutounian, S., Krane, E., Rice, A. S. C., Rowbotham, M., Wallace, M., & Eccleston, C. (2021). Cannabinoids, cannabis, and cannabis-based medicine for pain management: a systematic review of randomised controlled trials. Pain, 162(Suppl 1), S45–S66. [DOI] [PubMed] [Google Scholar]
- Florida Department of Health. (2020). Office of Medical Marijuana Use (OMMU) weekly updates. https://knowthefactsmmj.com/about/weekly-updates/ [Google Scholar]
- Gruber, S. A., Smith, R. T., Dahlgren, M. K., Lambros, A. M., & Sagar, K. A. (2021). No pain, all gain? Interim analyses from a longitudinal, observational study examining the impact of medical cannabis treatment on chronic pain and related symptoms. Experimental and Clinical Psychopharmacology, 29(2), 147–156. [DOI] [PubMed] [Google Scholar]
- IASP Presidential Task Force on Cannabis and Cannabinoid Analgesia (2021). International Association for the Study of Pain Presidential Task Force on cannabis and cannabinoid analgesia position statement. Pain, 162(Suppl 1), S1–S2. [DOI] [PubMed] [Google Scholar]
- Kaptchuk, T. J. (2002). The placebo effect in alternative medicine: can the performance of a healing ritual have clinical significance? Annals of Internal Medicine, 136(11), 817–825. [DOI] [PubMed] [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B., Berry, J. T., & Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1-3), 163–173. [DOI] [PubMed] [Google Scholar]
- Lev-Ran, S., Roerecke, M., Le Foll, B., George, T., McKenzie, K., & Rehm, J. (2013). The Association between cannabis use and depression: A systematic review and meta-analysis of longitudinal studies. European Psychiatry, 28(S1), 1–1. [DOI] [PubMed] [Google Scholar]
- Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Herzberg, P. Y. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. [DOI] [PubMed] [Google Scholar]
- May, M., Junghaenel, D. U., Ono, M., Stone, A. A., & Schneider, S. (2018). Ecological momentary assessment methodology in chronic pain research: A systematic review. The Journal of Pain, 19(7), 699–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2017). In The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- R Development Core Team (2019). R: A Language and Environment for Statistical [Google Scholar]
- Computing. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Salaffi, F., Stancati, A., Silvestri, C. A., Ciapetti, A., & Grassi, W. (2004). Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. European Journal of Pain (London, England), 8(4), 283–291. [DOI] [PubMed] [Google Scholar]
- Salas-Wright, C. P., Vaughn, M. G., Cummings-Vaughn, L. A., Holzer, K. J., Nelson, E. J., AbiNader, M., & Oh, S. (2017). Trends and correlates of marijuana use among late middle-aged and older adults in the United States, 2002-2014. Drug and Alcohol Dependence, 171, 97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute, Cary, NC. (2013). The SAS system for Windows. Release 9.4. SAS Institute, Cary, NC. [Google Scholar]
- Segura, L. E., Mauro, C. M., Levy, N. S., Khauli, N., Philbin, M. M., Mauro, P. M., & Martins, S. S. (2019). Association of US medical marijuana laws with nonmedical prescription opioid use and prescription opioid use disorder. JAMA Network Open, 2(7), e197216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah, A., Hayes, C. J., Lakkad, M., & Martin, B. C. (2019). Impact of medical marijuana legalization on opioid use, chronic opioid use, and high-risk opioid use. J General Internal Medicine, 34(8), 1419–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman, S., Stone, A. A., & Hufford, M. R. (2008). Ecological momentary assessment. Annual Review of Clinical Psychology, 4, 1–32. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Stockings, E., Campbell, G., Hall, W. D., Nielsen, S., Zagic, D., Rahman, R., Murnion, B., Farrell, M., Weier, M., & Degenhardt, L. (2018). Cannabis and cannabinoids for the treatment of people with chronic noncancer pain conditions: a systematic review and meta-analysis of controlled and observational studies. Pain, 159(10), 1932–1954. [DOI] [PubMed] [Google Scholar]
- Tomás, J. M., Galiana, L., & Fernández, I. (2018). The SF-8 Spanish Version for Health-Related Quality of Life assessment: Psychometric study with IRT and CFA models. The Spanish Journal of Psychology, 21, E1. [DOI] [PubMed] [Google Scholar]
- Turk, D. C., Dworkin, R. H., Allen, R. R., Bellamy, N., Brandenburg, N., Carr, D. B., Cleeland, C., Dionne, R., Farrar, J. T., Galer, B. S., Hewitt, D. J., Jadad, A. R., Katz, N. P., Kramer, L. D., Manning, D. C., McCormick, C. G., McDermott, M. P., McGrath, P., Quessy, S., Rappaport, B. A., Robinson, J. P., Royal, M. A., Simon, L., Stauffer, J. W., Stein, W., Tollett, J., & Witter, J. (2003). Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain, 106(3), 337–345. [DOI] [PubMed] [Google Scholar]
- Volkow, N. D., Baler, R. D., Compton, W. M., & Weiss, S. R. B. (2014). Adverse health effects of marijuana use. New England Journal of Medicine, 370(23), 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow, N. D., & Weiss, S. R. B. (2020). Importance of a standard unit dose for cannabis research. Addiction (Abingdon, England), 115(7), 1219–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyas, M. B., LeBaron, V. T., & Gilson, A. M. (2018). The use of cannabis in response to the opioid crisis: A review of the literature. Nursing Outlook, 66(1), 56–65. [DOI] [PubMed] [Google Scholar]
- Ware, J., Kosinski, M., Dewey, J., & Gandek, B. (2001). How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8 Health Survey. Quality Metric Incorporated. [Google Scholar]
- Wen, H., & Hockenberry, J. M. (2018). Association of Medical and Adult-Use Marijuana Laws With Opioid Prescribing for Medicaid Enrollees. JAMA Internal Medicine, 178(5), 673–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiting, P. F., Wolff, R. F., Deshpande, S., Di Nisio, M., Duffy, S., Hernandez, A. V., Keurentjes, J. C., Lang, S., Misso, K., Ryder, S., Schmidlkofer, S., Westwood, M., & Kleijnen, J. (2015). Cannabinoids for medical use: A systematic review and meta-analysis. JAMA, 313(24), 2456–2473. [DOI] [PubMed] [Google Scholar]
- Wilson, K. G., Eriksson, M. Y., D'Eon, J. L., Mikail, S. F., & Emery, P. C. (2002). Major depression and insomnia in chronic pain. The Clinical Journal of Pain, 18(2), 77–83. [DOI] [PubMed] [Google Scholar]


