Abstract
Objective: Female sex hormones have a pro-inflammatory effect, which may help to minimize inflammation. Estrogen's immunoregulatory properties play a significant role in the bi-directional neuroendocrine-immune activity in females. As a result, sex hormones can play a role in men's high mortality rate from coronavirus-2019 (COVID-19). It is aimed to clarify the role of 17-estradiol (E2) in the battle against COVID-19.
Materials and methods: Until April 2021, a study on PubMed was performed. COVID-19, 17-estradiol (E2), immunoregulatory properties, pregnancy, menopausal symptoms, hormonal therapy, ER/ expression on immune cells, and mortality were some of the concepts used in the search.
Results: Regulation of pro-inflammatory immune processes against COVID-19 appears to be associated with increased immune function (pro-inflammatory), anti-inflammatory regulation, and antiviral defense. Women with a severe coronavirus infection had higher serum IgG antibody levels than men, and their IgG production was faster in the early stages of infection. 17-estradiol (E2) levels of blood will increase by 100-fold during pregnancy. COVID-19 in pregnant women had a 15-fold lower mortality rate than other women. While menopause replacement therapy (MRT) for pre/post-menopausal women and its effectiveness in reducing COVID-19 infection is debatable.
Conclusion: MRT may be considered as a viable treatment option for pre/post-menopause women with coronavirus, referring to the fact that sex hormones reduce inflammatory responses and modulate ACE2 expression. The task's difficulty and achieving the desired outcome seem to be challenging.
Key Words: Estradiol, Estrogen Receptor Alpha, Coronavirus, Hormone Replacement Therapy
Introduction
Profiles of steroidal hormones: Sex hormones that have a pro-inflammatory effect may reduce the inflammatory response. In both men and women, glucocorticoids, dehydroepiandrosterone (DHEA), and androgens are ineffectively lower in patients than in healthy people. For example, androgens have an anti-inflammatory effect, while estrogens have a pro-inflammatory effect. An enhanced immune response to infections must be stimulated during the growth of the reproductive system to protect its health. The expression of the estrogen receptors on the lymphocytes, macrophages, and dendritic cells (DC) shows that sex hormones can be a significant regulator in immune responses. Sex hormones influence both the immune and reproductive systems. Immune responses to diseases and vaccines are stronger in women than in men. Females, on the other hand, have a higher incidence of autoimmune diseases. Interestingly, during pregnancy, the same immune response shifts to accommodate the alien fetus and avoid rejection. The mother of the seahorse produces the eggs, but the father carries them, cultivates them during gestation, and gives birth to them. The immune response of the male seahorse changes during the parental stage, according to studies (1, 2).
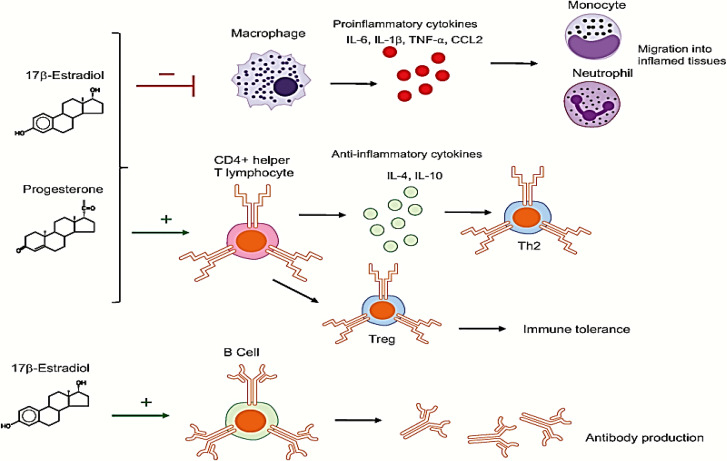
Estradiol and progesterone are important modulators of inflammatory and behavioral processes. These steroid hormones have peripheral and neurological effects, as well as anti-inflammatory effects, by reshaping immune cells and stimulating antibody production through genomic effects on nuclear hormone receptors (3, 4) (Figure 1).
Figure 1.
Steroid hormones and reshaping of immune cells
17β-estradiol (E2) in the high physiological concentration inhibits the pro-inflammatory cytokines by macrophages for production: interleukin 6 (IL-6), interleukin 1β (IL-1β), and tumor necrosis factor α (TNF-α), and chemokine CCL2, therefore blocking migration of neutrophils and monocytes into inflamed regions.
Progesterone (P4) suppresses pro-inflammatory cytokines production by macrophages and dendritic cells: interleukin 1β (IL-1β) and interleukin 12 (IL-12).
E2 or P4 in high concentration stimulate anti-inflammatory cytokines: CD4+ T-helper cell, interleukin 4, and interleukin 10 productions, and favor Th2-type anti-inflammatory responses. E2 and P4 also enhance the expansion of regulatory T cells (Treg), therefore promoting immune tolerance.
E2 stimulates B cells for production of antibody (1).
Estrogens receptors expression on the immune cells: All immune cells express estrogen receptors (ERs), which act as transcriptional regulators for cellular function. CD4+ T lymphocytes, for example, express ERɑ messenger RNA at a higher level than ER, while B cells express ERβ at a higher level than ERɑ messenger RNA in human peripheral blood mononuclear cells. Both ERs have low expression in CD8+ T cells and monocytes in the peripheral blood (4). These results indicate that higher estrogen/progesterone levels and higher receptor expression during pregnancy promote fetal growth and prevent it from being excreted by the mother. Despite the difficulty of pregnancy immunology, the immune system must be able to protect the mother.
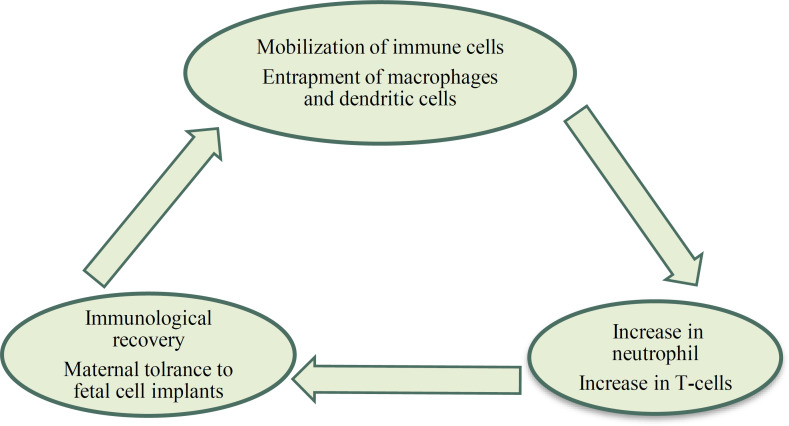
Maternal Immune changes: During pregnancy, the maternal immune system undergoes the most significant changes in order to protect the mother and her fetus from infections while avoiding harmful immune responses against her fetus. Some portions of the immune system are strengthened while others are suppressed during pregnancy. Although there is little evidence to validate common suppression of the maternal immune system during pregnancy, it should be noted that many molecules/cells of the maternal immune system have an essential role in the development of the placenta and the fetus. The pro-inflammatory/anti-inflammatory processes must be balanced, and the T helper 1/T helper 2 immune cells must change during pregnancy (5). The pattern of pregnancy immune tolerance is a balance of both innate/adaptive immune systems that can protect the fetus from infection while not interfering with the mother's health. Pregnancy is thus not only a chronic disease that does not inhibit the immune system, but it is also a special condition that modulates the immune system (6). Finally, the fetus is completely grown and ready for birth during the last immunological period of pregnancy, which is achieved by re-inflammation. With the influx of immune cells into the myometrium during the labor stage, an inflammatory process occurs once more. The uterus contracts, the baby is expelled, and the placenta ruptures in this pro-inflammatory area. It can be either a pro-inflammatory/anti-inflammatory condition, depending on the stage of pregnancy (7-9) (Figure 2).
Figure 2.
Maternal immunity changes during pregnancy
Pinna et al. announced in March 2020 that the initial positive test for COVID-19 in asymptomatic pregnant women increased immediately after delivery, indicating that the incidence of coronavirus infection increased hospitalization in the intensive care unit. They reported that Mortality in pregnant women is 15 times lower than in other women against COVID-19 (1). We must agree that pregnancy immunology clashes with the maternal immune system's complexity during pregnancy. More understanding of this relationship will aid in the provision of appropriate care for patients experiencing pregnancy difficulties, as well as the development of public policies to assist pregnant women during pandemics.
Coronavirus: In the last two decades, after severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), COVID-19 (Corona-virus-disease-2019) as coronavirus disease is the third respiratory infection that was firstly defined in Asia (10, 11). The first report of COVID-19 was in December 2019 in Wuhan, China. Coronavirus of Wuhan 2020 belongs to the Beta coronavirus (12). The Coronaviridae family is the causative agent of respiratory, intestinal, hepatic, and neurological diseases in humans and animals. Coronaviruses are the largest group of positive- sense RNA viruses with a wide range of natural hosts. The first coronavirus in 1937 was isolated from chicken embryos (13). Coronaviruses have been widely distributed and have been found as human pathogen since the 1960s. These zoological viruses are common between animals and humans. The name coronavirus is due to the presence of a structure with a crown on its surface (like the sun) under an electron microscope. Coronavirus is a member of the orthocoranavirinae sub-family with four types that was differentiated by their protein classification: Alpha, Beta, Gamma and Delta coronaviruses (14).
1- Feature of the female reproductive system response to the coronavirus: Epidemiological findings from the SARS epidemic and the COVID-19 pandemic show a general feature of increased disease severity and mortality in men compared to women (3). In contrast, female patients had more active T cells than male patients during SARS-CoV-2 infection. Women with severe coronavirus infection have a higher concentration of serum IgG antibody compared with men, and the IgG generation in the primary phases of infection is stronger in females than in males. Significantly, a weak T cell response was negatively associated with patients' age and was linked with worse disease severity in men than women (4). Immune mechanisms indicate a more severe virus infection response in post-menopausal women (Immuno-senescence). Therefore, estrogens and progesterone can play a protective role against direct antiviral activity in women.
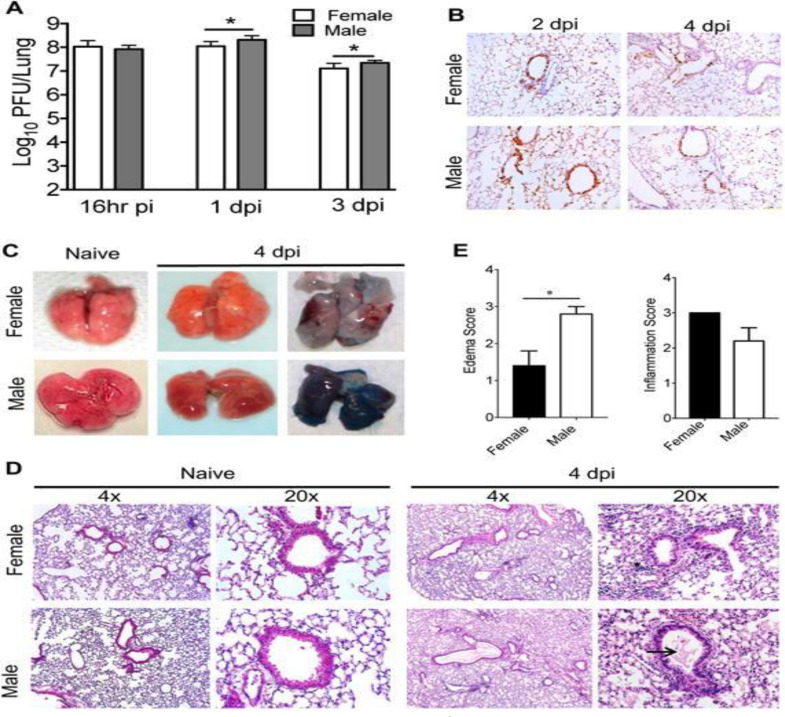
2- Female Sex hormones & immune-protective feature against Coronavirus: Estrogens display potent immune-modulating functions in influenza infection, which can lead to a more suitable innate immune response in the lungs. While this modulation processes have been associated with decreased pro-inflammatory cytokine/chemokine responses prior to clinical disease (15-17). Further, SARS-CoV-2 and SARS-CoV both produce deadly pneumonia with the same apparent female protection. In 2017, Channappanavar and colleagues reported that SARS-CoV infection modeling in mice associated with increased susceptibility to SARS-CoV in male mice compared to female mice. In comparison to male mice, female mice had lower virus titers and lower infiltration with inflammatory immune cells (monocytes, macrophages, and neutrophils) for producing fewer inflammatory cytokines such as IL-6, IL-1, and TNF-, as well as fewer chemokines (CCL2). Pulmonary injury was lower in female mice with lower mortality (20%) compared to male mice (80%) with improved vascular leakage, and alveolar edema. Their findings about ovariectomized mice or female mice were treated by 17β-estradiol (E2) inhibitor showed augmented mortality. As a result, they hypothesized that E2 signaling plays a crucial protective role in mice infected with SARS-CoV and that this sex distribution is similar to that seen in patients with COVID-19 (18) (Figure 3).
Figure 3.
Virus titer and lung pathology in mice infected with MA15
Dpi: day of primary infection
Male and female 9-month-old mice (n=4-5 mice per group) were infected with 5000 PFU MA15 and lungs for titer (A), staining of viral antigen in the lungs at different times post infection (B), gross pathology and vascular leakage in the lungs of naive male and female mice infected with MA15 (C), and its histology (D) with inflammation and edema scores were determined at day 4 post infection (E). Statistical significance was determined as described in Materials and Methods. *P<0.05 (18).
3- E2 receptors: ER-2 genome & virus: In human nasal epithelial cell culture, Pretez and et al., looked at this basal-sex disparity (hNEC). They exposed endogenous E2, raloxifene, and bisphenol A to hNEC cultures from adult male and female donors. E2 binds to the estrogen receptor (ER-ɑ), which is essential for the human reproductive system's physiological hemostasis. To see whether these results were sex-linked, cell cultures were infected with the seasonal influenza-A virus. In cell culture based on the ER-2 genome, E2 reduced viral titers, and the genomic ER antagonist ICI 182,780 was able to reverse E2's antiviral effects. The results of these study showed that treating of hNECs with E2 had no effect on secretion of interferon/chemokine, but considerably reduced cell metabolic processes in human respiratory epithelial cells were infected with influenza-A virus. Beta-estrogen receptors (ER-β) were responsible for the substantial reduction in influenza-A virus replication (19).
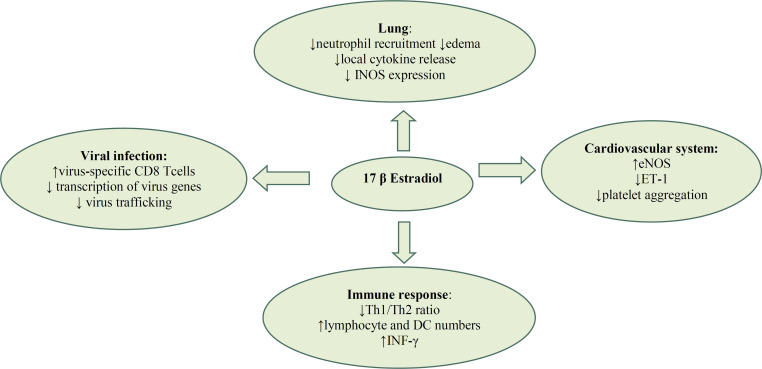
The genomic and non-genomic actions of estrogen can activate nuclear estrogen receptor alpha (ER-α), ER-β and membrane G- protein- coupled estrogen receptor (GPER1). These signaling pathways are linked to anabolic defensive effects in the lungs (20), cardiovascular system (21) and immune system (22). Stelzig et al. in 2020 reported that E2 can modulate the level of ACE2 gene expression (23). In 2021, Lemes et al showed that E2 can be a possible therapeutic target for promoting cell defense against SARSCoV2 in an experimental study on VERO E6 cells with 17estradiol (24). Acute lung injury in mice models shows that female mice have better immune protection than male mice (25), which can be enhanced by estrogen replacement in ovariectomized mice (26). E2 molecule decreases the permeability of the pulmonary arteries and edema associated with pulmonary vasoconstriction by increasing levels of prostacyclin and nitric oxide (NO) (27, 28) (Figure 4).
Figure 4.
Effects of 17β-estradiol in different compartments/systems
Estrogen has been shown to influence virus replication and maturation, but no evidence has been given for SARS-CoV-2. Estrogen is well known to be involved in inflammatory responses to pathogens and infections, and ERs have been associated with virus gene transcription suppression. For example in hepatocytes infection by the hepatitis B virus (HBV), the interaction between ER-α and virus gene expression done by hepatocyte nuclear factor 4α (HNF)-4α with binding to HBV enhancer I. The interaction between the hepatitis C model and 17-estradiol (in vitro) was able to interrupt the virus life cycle, and Fulvestrant (anti-estrogen) was able to block this effect (29). Estradiol's modulatory function in systemic and pulmonary inflammatory responses has been confirmed by numerous studies.
Fast actions through coupling with membrane receptors can help maintain pulmonary microvascular flow in stressful conditions like hypoxia, which could be an adjunct therapy for patients with COVID-19 (28).
4- Hormone replacement therapy (HRT): Estrogen replacement: The first study of the Women's Health Initiative (WHI) findings for hormone therapy trials was almost ten years ago. Early results from the WHI in 2002 gave the impression that HRT could increase the risk of breast cancer, heart disease, and stroke in women by a small amount. Experiments on a variety of animal models have shown that estrogen replacement in ovariectomized animals has a largely neuroprotective effect, and thus can lower the risk of Alzheimer's disease (30).
5- Hormone replacement therapy (HRT): is it a risk or a benefit? Menopause is a hormonal and natural process that all women go through and it is impossible to go through without experiencing any side effects, so women can expect it. While estrogen replacement therapy or estrogen + progesterone may help with menopause symptoms, it may also increase the risk of certain diseases. By interfering with feedback and feedforward mechanisms, MHT (menopausal hormone therapy) can disrupt hormonal homeostasis in women. Various phenotypic and metabolic changes occur during the menopausal process, influencing body weight, adipose tissue distribution, and energy consumption, as well as insulin secretion and sensitivity.
When taken together, these factors can increase the risk of type 2 diabetes in women (T2DM) (31). Estrogen may relieve symptomatic menopause, lower chronic disease rates, and increase health-related quality of life for women who are candidates for MHT. MHT has fewer complications, particularly for women in the early stages of menopause (32). Early MHT perimenopause intervention is advised to preserve energy metabolic homeostasis and improve average life expectancy. Numerous studies have shown that menopausal obesity is the product of a complex network of neural and endocrine and metabolic pathways in which ovarian hormone plays an important role. During the menopausal process, the increased risk of weight gain, central accumulation of body fat and energy metabolism disorders leads to increased CVD and overall mortality in women (33). It's debatable whether MHT has detrimental or beneficial effects on the cardiovascular (CV) system. As a result, the impact of MHT on body mass, body fat redistribution, and insulin resistance contribute to protective cardio metabolic effects. In comparison to men, women develop atherosclerosis and clinical cardiovascular diseases (CVD) at a later age, particularly in the post-menopausal period (34). A systematic review and meta-analysis of randomized controlled trials (RCTs) and observational studies to assess the connection between menopausal hormone therapy and cardiovascular disease in 2020 by Kim et al showed that before beginning therapy in post-menopausal women, the underlying condition and the timing of initiation should be carefully considered (35). MacLennan and et al. reported that early HT initiation from around menopause may be helpful for certain cognitive domains, whereas late HT initiation may be detrimental. The timing of HT initiation appears to be crucial. A sample size of 2,500 women will be needed to completely test these hypotheses and further investigate these patterns by route and form of HT regimen in this population (36). Despite these, there is still debate about the CVD risks and benefits of MHT. As a result, the importance of additional research evaluating the following variables has been emphasized: estrogen dosage, route of delivery, timing after menopause, length of use, other hormone effects, pre-existing pathology, and age has been emphasized (35).
Discussion
Individual age and gender are strong predictors of coronavirus in 2019 (COVID-19), do such factors indicate preferential treatment options? This study focuses on the gender differences in estradiol function and its immune-protective role in women against coronavirus infection. Studies on severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) showed that men have a tendency to develop more severe infections than women. The X chromosome is recognized which contains the largest number of immune-related genes of the whole human genome. Numerous studies have been performed on the X chromosome to understand the role of its genes in the development and attack of autoimmunity (37), but paradoxically, increased immune function in women is associated with the possibility of improving inflammatory processes and autoimmune diseases. The incidence rate of autoimmune diseases is 8-9 times higher in women compared to men (38). Estrogen receptors (ERα/β) are expressed in most immune cells. This expression confirms the prominent role of ERs on innate/adaptive immune function responses. For example, the important influence of estrogen and its receptors on B cell, dendritic cell functions are well recognized in lupus. In lupus this immune-protective effect of ERα is multifactorial, or in arthritis models, ERα agonists act to facilitate the immune-protective effect. Therefore, ERα modulating function can be a significant target for autoimmunity therapeutic (39). E2 influences the expression of human angiotensin-converting enzyme 2 (ACE2) protein (as the host cell receptor), which can have a significant role in coronavirus uptake (40).
In women, regulation of pro-inflammatory immune processes against COVID-19 appears to be associated with increased anti-inflammatory regulation, and antiviral defense (41).
Anti-inflammatory regulation (inflammatory machinery): This effect on the innate immune system induces reduction of the secretion of inflammatory cytokines by monocytes and macrophages, delay on the neutrophil apoptosis, and increasing the expression of neutrophil annexin 1 without increasing activation of them (42, 43). Experimental findings show that leukocyte function, macrophage phagocytosis, and an increase in anti-inflammatory T lymphocytes are more efficient and quick in women compared to men (44). Population of the dendritic cell is signaled by E2 through the ER-α (45). The intracellular ERs activation can able shorten the lipopolysaccharide-induced (LPS) pro-inflammatory phase by triggering the resolution of inflammation in RAW264.7 (intrinsic/extrinsic programs). This activity can regulate the SOCS3 and STAT3 signaling pathways which associate with E2 facilitation for the progress of the inflammatory procedure to the IL10-dependent “acquired deactivation” phenotype. This process is able to respond to tissue remodeling and the repair of homeostatic circumstances (46). This theory that E2 has a significant role in protection against chronic inflammatory diseases is impressed by the menstrual cycle and pregnancy. The occurrence of disorders is accompanied by powerful components of the inflammatory process. As a side effect of menopause, metabolic diseases (osteoporosis, atherosclerosis, diabetes), and arthritis are symptoms of ovarian function loss (47). Fertile female mammals are less vulnerable to these diseases than male mammals (48). Estrogens are effective in treating metabolic dysfunction and vascular disease by modulating inflammatory processes. Although the connection between the two fields is still unclear, estrogens' anti-inflammatory properties on metabolism regulation have been suggested (49). Estrogen has anti-inflammatory effects on the vascular system through a variety of mechanisms, including direct antioxidant effects, nitric oxide (NO) development, suppression of the renin-angiotensin system and cytokines, and inhibition of vasoconstriction (50). Therefore, the complexity of the E2 performance is enormous. Maciuszek et al. in 2020 showed that E2 decreased LPS-stimulated expression of intermediated genes in pro-inflammatory/anti-inflammatory processes in-vitro, but did not alter ERs gene expression. Their in-vivo study showed that E2-treated induced upregulation of gene expression of pro-inflammatory/anti-inflammatory mediators (51).
Antiviral defense: Influenza infection model in mice showed a larger morbidity and mortality in female mice than males. It is associated with higher induction of pro-inflammatory cytokines and chemokines (TNFα, IFNγ, IL-6 and CCL2) in females. Administration of high doses of estradiol in this modeling of mice could defend female mice against injuring extreme inflammatory responses in the lung by the recruitment of neutrophils. In the lung, the ER-α response was able to increase TNFα and IFNγ production through virus-specific CD8 + T cells (52). Production of the type I Interferon (IFNs) of CD8 + T cells has a control role in the maintenance of immune homeostasis. The ability of plasmacytoid dendritic cells (pDCs) to produce IFN1 is faster and more abundant than others. The prominent role of IFN-1 in pDC-related diseases is important. Deficiency of IFN-1 production can severely increase some allergic reactions and the risk of viral infections, and its high production can cause autoimmune reactions (53). In women, the protective-immune function of E2 is directly related to the ovarian cycle. When E2 levels are higher, for example in pregnancy, this cycle is affected by an increase in the T cell population (54). The pattern of Th1/Th2 cytokine is widely known for allergies, infection, and autoimmunity diseases. Pregnancy appears to be accompanied by a Th2 pattern. The synthesis of type-1 cytokines (IFN- and IL-2) and type-2 cytokines (IL-10) did not differ between ovarian cycle phases. The output of the type-2 cytokine IL-4, on the other hand, was significantly higher in the luteal phase of the ovarian cycle than in the follicular phase. The immune response is moved toward a Th2-type response during the luteal phase of the ovarian cycle, as evidenced by increased IL-4 development during this phase of the cycle. Increased levels of progesterone and 17-E2 in the luteal phase of the ovarian cycle may play a role in the immune response's shift to a type-2 response, according to these findings, therefore, the Th2 pattern tends to be associated with pregnancy (55).
MRT in post-menopausal women with COVID-19: cannot be considered as an appropriate treatment. According to research, the timing of hormone therapy (HT) activation seems to be very important. Early onset HT initiation may be beneficial, while delayed onset HT initiation may be harmful. While MRT is recommended for pre/post-menopausal women, its effectiveness in reducing COVID-19 infection is debatable. Menopause is an independent risk factor for COVID-19. E2 is negatively correlated with COVID-19’s severity probably due to their regulation of cytokines related to immunity and inflammation. Female's health and post-menopausal have significantly higher IL-6 responses to acute stress (56). A substantial number of patients also had signs of acute stress disorder, but these were often mild to moderate. The results of Parker and et al.'s study in 2021 showed a total of 58 subjects were enrolled which at the start of the study, 36% of the participants had elevated anxiety symptoms and 29% had elevated depression symptoms. After two weeks of follow-up 9% had raised anxiety symptoms, 20% had raised depression symptoms, and 25% had mild-to-moderate acute stress disorder symptoms. Discharge to home was not linked to a reduction in psychological symptoms (57).
Conclusion
If inflammatory responses are maintained over time, they can have clinical consequences for the development and maintenance of inflammatory-related diseases that are common in older women. Therefore, High levels of interleukin-6 in menopausal women can more rapidly lead patients with coronavirus into the cytokine storm which is characterized by immune dysregulation and hyper inflammation. MRT intervention for post-menopausal women with coronavirus infection, in acute or persistent traumatic distress, should focus on evidence-based trauma strategies to address the unique challenges of COVID-19.
Acknowledgments
Authors have no conflict of interests.
Notes:
Citation: Zafari Zangeneh F, Sarmast Shoushtari M. Estradiol and COVID-19: Does 17-Estradiol Have an Immune-Protective Function in Women Against Coronavirus? J Family Reprod Health 2021; 15(3): 150-9.
References
- 1.Pinna G. Sex and COVID-19: A Protective Role for Reproductive Steroids. Trends Endocrinol Metab. 2021;32:3–6. doi: 10.1016/j.tem.2020.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schmidt M, Naumann H, Weidler C, Schellenberg M, Anders S, Straub RH. Inflammation and sex hormone metabolism. Ann N Y Acad Sci. 2006;1069:236–46. doi: 10.1196/annals.1351.021. [DOI] [PubMed] [Google Scholar]
- 3.Viveiros A, Rasmuson J, Vu J, Mulvagh SL, Yip CYY, Norris CM, et al. Sex differences in COVID-19: candidate pathways, genetics of ACE2, and sex hormones. Am J Physiol Heart Circ Physiol. 2021;320:H296–H304. doi: 10.1152/ajpheart.00755.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mauvais-Jarvis F, Klein SL, Levin ER. Estradiol, Progesterone, Immunomodulation, and COVID-19 Outcomes. Endocrinology. 2020;161:bqaa127. doi: 10.1210/endocr/bqaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morelli SS, Mandal M, Goldsmith LT, Kashani BN, Ponzio NM. The maternal immune system during pregnancy and its influence on fetal development. Research and Reports in Biology. 2015;6:171–89. [Google Scholar]
- 6.Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014;370:2211–8. doi: 10.1056/NEJMra1213566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mor G, Cardenas I, Abrahams V, Guller S. Inflammation and pregnancy: the role of the immune system at the implantation site. Ann N Y Acad Sci. 2011;1221:80–7. doi: 10.1111/j.1749-6632.2010.05938.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mor G, Cardenas I. The Immune System in Pregnancy: A Unique Complexity. Am J Reprod Immunol. 2010;63:425–33. doi: 10.1111/j.1600-0897.2010.00836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buddola V. Recent Developments in Applied Microbiology and Biochemistry. 1st Edition. 2018. pp. 13–20. [Google Scholar]
- 10.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beaudette ER, Hudson CB. Cultivation of the virus of infectious bronchitis. J Am Vet Med Assoc. 1937;90:51–8. [Google Scholar]
- 12.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17:181–92. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robinson DP, Lorenzo ME, Jian W, Klein SL. Elevated 17β-estradiol protects females from influenza A virus pathogenesis by suppressing inflammatory responses. PloS Pathog. 2011;7:e1002149. doi: 10.1371/journal.ppat.1002149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robinson DP, Hall OJ, Nilles TL, Bream JH, Klein SL. 17β-estradiol protects females against influenza by recruiting neutrophils and increasing virus-specific CD8 T cell responses in the lungs. J Virol. 2014;88:4711–20. doi: 10.1128/JVI.02081-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vermillion MS, Ursin RL, Attreed SE, Klein SL. Estriol reduces pulmonary immune cell recruitment and inflammation to protect female mice from severe influenza. Endocrinology. 2018;159:3306–20. doi: 10.1210/en.2018-00486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mauvais-Jarvis F, Klein SL, Levin ER. Estradiol, Progesterone, Immunomodulation, and COVID-19 Outcomes. Endocrinology. 2020;161:bqaa127. doi: 10.1210/endocr/bqaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Phiel KL, Henderson RA, Adelman SJ, Elloso MM. Differential estrogen receptor gene expression in human peripheral blood mononuclear cell populations. Immunol Lett. 2005;97:107–13. doi: 10.1016/j.imlet.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 18.Channappanavar R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, Perlman S. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol. 2017;198:4046–53. doi: 10.4049/jimmunol.1601896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peretz J, Pekosz A, Lane AP, Klein SL. Estrogenic compounds reduce influenza A virus replication in primary human nasal epithelial cells derived from female, but not male, donors. Am J Physiol Lung Cell Mol Physiol. 2016;310:L415–25. doi: 10.1152/ajplung.00398.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tofovic SP, Jackson EK. Estradiol metabolism: Crossroads in pulmonary arterial hypertension. Int J Mol Sci. 2019;21:116. doi: 10.3390/ijms21010116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ. 2017;8:33. doi: 10.1186/s13293-017-0152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Di Florio DN, Sin J, Coronado MJ, Atwal PS, Fairweather D. Sex differences in inflammation, redox biology, mitochondria and autoimmunity. Redox Biol. 2020;31:101482. doi: 10.1016/j.redox.2020.101482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stelzig KE, Canepa‐Escaro F, Schiliro M, Berdnikovs S, Prakash YS, Chiarella SE. Estrogen regulates the expression of SARS‐CoV‐2 receptor ACE2 in differentiated airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2020;318:L1280–1. doi: 10.1152/ajplung.00153.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lemes RMR, Costa AJ, Bartolomeo CS, Bassani TB, Nishino MS, Pereira GJDS, et al. 17β‐estradiol reduces SARS‐CoV‐2 infection in vitro. Physiol Rep. 2021;9:e14707. doi: 10.14814/phy2.14707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carey MA, Card JW, Voltz JW, Germolec DR, Korach KS, Zeldin DC. The impact of sex and sex hormones on lung physiology and disease: lessons from animal studies. Am J Physiol Lung Cell Mol Physiol. 2007;293:L272–8. doi: 10.1152/ajplung.00174.2007. [DOI] [PubMed] [Google Scholar]
- 26.Speyer CL, Rancilio NJ, McClintock SD, Crawford JD, Gao H, Sarma JV, et al. Regulatory effects of estrogen on acute lung inflammation in mice. Am J Physiol Cell Physiol. 2005;288:C881–90. doi: 10.1152/ajpcell.00467.2004. [DOI] [PubMed] [Google Scholar]
- 27.Lahm T, Albrecht M, Fisher AJ, Selej M, Patel NG, Brown JA, et al. 17β-Estradiol attenuates hypoxic pulmonary hypertension via estrogen receptor-mediated effects. Am J Respir Crit Care Med. 2012;185:965–80. doi: 10.1164/rccm.201107-1293OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Breithaupt-Faloppa AC, Correia CJ, Prado CM, Stilhano RS, Ureshino RP, Moreira LFP. 17β-Estradiol, a potential ally to alleviate SARS-CoV-2 infection. Clinics (Sao Paulo) 2020;75:e1980. doi: 10.6061/clinics/2020/e1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Magri A, Barbaglia MN, Foglia CZ, Boccato E, Burlone ME, Cole S, et al. 17,β-estradiol inhibits hepatitis C virus mainly by interference with the release phase of its life cycle. Liver Int. 2017;37:669–77. doi: 10.1111/liv.13303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zandi PP, Carlson MC, Plassman BL, Welsh-Bohmer KA, Mayer LS, Steffens DC, et al. Hormone replacement therapy and incidence of Alzheimer disease in older women: The Cache County Study. JAMA. 2002;288:2123–9. doi: 10.1001/jama.288.17.2123. [DOI] [PubMed] [Google Scholar]
- 31.Paschou SA, Papanas N. Type 2 Diabetes Mellitus and Menopausal Hormone Therapy: An Update. Diabetes Ther. 2019;10:2313–20. doi: 10.1007/s13300-019-00695-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Temkin SM, Mallen A, Bellavance E, Rubinsak L, Wenham RM. The role of menopausal hormone therapy in women with or at risk of ovarian and breast cancers: Misconceptions and current directions. Cancer. 2019;125:499–514. doi: 10.1002/cncr.31911. [DOI] [PubMed] [Google Scholar]
- 33.Zhu J, Yi M, Xing L, Yu Zh, Guo X, Chen X, et al. Ovarian Hormonal Change-Related Energy Metabolism and Obesity in Menopausal Women. Hormone Therapy and Replacement in Cancer and Aging-related Diseases. 2019. [Google Scholar]
- 34.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2019 Update: A Report from the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 35.Kim JE, Chang JH, Jeong MJ, Choi J, Park J, Baek C, et al. A systematic review and meta-analysis of effects of menopausal hormone therapy on cardiovascular diseases. Sci Rep. 2020;10:20631. doi: 10.1038/s41598-020-77534-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.MacLennan AH, Henderson VW, Pain BJ, Mathias J, Ramsay EN, Ryan P, et al. Hormone therapy, timing of initiation, and cognition in women aged older than 60 years: the REMEMBER pilot study. Menopause. 2006;13:28–36. doi: 10.1097/01.gme.0000191204.38664.61. [DOI] [PubMed] [Google Scholar]
- 37.Bianchia I, Lieo A, Gershwinc ME, Invernizzi P. The X chromosome and immune associated genes. J Autoimmun. 2012;38:J187–92. doi: 10.1016/j.jaut.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 38.Kovats S. Estrogen receptors regulate innate immune cells and signaling pathways. Cell Immunol. 2015;294:63–9. doi: 10.1016/j.cellimm.2015.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leitman DC, Paruthiyil S, Vivar OI, Saunier EF, Herber CB, Cohen I, et al. Regulation of specific target genes and biological responses by estrogen receptor subtype agonists. Curr Opin Pharmacol. 2010;10:629–36. doi: 10.1016/j.coph.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoffmann M, Kleine-Weber H, Schroeder S, Kruger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–80. doi: 10.1016/j.cell.2020.02.052. e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ueda K, Karas RH. Emerging evidence of the importance of rapid, non-nuclear estrogen receptor signaling in the cardiovascular system. Steroids. 2013;78:589–96. doi: 10.1016/j.steroids.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 42.Molloy EJ, O’Neill AJ, Grantham JJ, Sheridan-Pereira M, Fitzpatrick JM, Webb DW, et al. Sex-specific alterations in neutrophil apoptosis: The role of estradiol and progesterone. Blood. 2003;102:2653–9. doi: 10.1182/blood-2003-02-0649. [DOI] [PubMed] [Google Scholar]
- 43.Nadkarni S, Cooper D, Brancaleone V, Bena S, Perretti M. Activation of the annexin A1 pathway underlies the protective effects exerted by estrogen in polymorphonuclear leukocytes. Arterioscler Thromb Vasc Bio. 2011;31:2749–59. doi: 10.1161/ATVBAHA.111.235176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scotland RS, Stables MJ, Madalli S, Watson P, Gilroy DW. Sex differences in resident immune cell phenotype underlie more efficient acute inflammatory responses in female mice. Blood. 2011;118:5918–27. doi: 10.1182/blood-2011-03-340281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kovats S. Estrogen receptors regulate an inflammatory pathway of dendritic cell differentiation: mechanisms and implications for immunity. Horm Behav. 2012;62:254–62. doi: 10.1016/j.yhbeh.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Villa A, Rizzi N, Vegeto E, Ciana P, Maggi A. Estrogen accelerates the resolution of inflammation in macrophagic cells. Scientific Reports. 2015;5:15224. doi: 10.1038/srep15224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gubbels Bupp MR. Sex, the ageing immune system and chronic disease. Cell Immunol. 2015;294:102–10. doi: 10.1016/j.cellimm.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 48.Olsen NJ, Kovacs WJ. Gonadal steroids and immunity. Endocr Rev. 1996;17:369–84. doi: 10.1210/edrv-17-4-369. [DOI] [PubMed] [Google Scholar]
- 49.Monteiro R, Teixeira D, CalhauC Estrogen Signaling in Metabolic Inflammation. Mediators Inflamm. 2014;2014:615917. doi: 10.1155/2014/615917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chakrabarti S, Lekontseva O, Davidge ST. Estrogen is a Modulator of Vascular Inflammation. IUBMB Life. 2008;60:376–82. doi: 10.1002/iub.48. [DOI] [PubMed] [Google Scholar]
- 51.Maciuszek M, Pijanowski l, Pekala-Safinska A, Kemenade BML, Chadzinska M. 17β-Estradiol affects the innate immune response in common carp. Fish Physiol Biochem. 2020;46:1775–94. doi: 10.1007/s10695-020-00827-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Robinson DP, Lorenzo ME, Jian W, Klein SL. Elevated 17beta-estradiol protects females from influenza A virus pathogenesis by suppressing inflammatory responses. PLoS Pathog. 2011;7:e1002149. doi: 10.1371/journal.ppat.1002149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bencze D, Fekete T, Pázmándi K. Type I Interferon production of plasmacytoid dendritic cells under control. Int J Mol Sci. 2021;22:4190. doi: 10.3390/ijms22084190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Arruvito L, Sanz M, Banham AH, Fainboim L. Expansion of CD4+CD25+ and FOXP3+ regulatory T cells during the follicular phase of the menstrual cycle: implications for human reproduction. J Immunol. 2007;178:2572–8. doi: 10.4049/jimmunol.178.4.2572. [DOI] [PubMed] [Google Scholar]
- 55.Faas M, Bouman A, Moesa H, Heineman MJ, de Leij L, Schuiling G. The immune response during the luteal phase of the ovarian cycle: A Th2-type response? Fertil Steril. 2000;74:1008–13. doi: 10.1016/s0015-0282(00)01553-3. [DOI] [PubMed] [Google Scholar]
- 56.Parker C, Shalev D, Hsu I, Shenoy A, Cheung S, Nash S, et al. Depression, Anxiety, and Acute Stress Disorder Among Patients Hospitalized with COVID-19: A Prospective Cohort Study. J Acad Consult Liaison Psychiatry. 2021;62:211–19. doi: 10.1016/j.psym.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Endrighi R, Hamer M, Steptoe A. Post-menopausal Women Exhibit Greater Interleukin-6 Responses to Mental Stress Than Older Men. Ann Behav Med. 2016;50:564–71. doi: 10.1007/s12160-016-9783-y. [DOI] [PMC free article] [PubMed] [Google Scholar]