Abstract
Corona pandemic has affected the whole world, and it is a highly researched area in biological sciences. As the current pandemic has affected countries socially and economically, the purpose of this bibliometric analysis is to provide a holistic review of the corona pandemic in the field of social sciences. This study aims to highlight significant, influential aspects, research streams, and themes. We have reviewed 395 journal articles related to coronavirus in the field of social sciences from 2003 to 2020. We have deployed ‘biblioshiny’ a web-interface of the ‘bibliometrix 3.0’ package of R-studio to conduct bibliometric analysis and visualization. In the field of social sciences, we have reported influential aspects of coronavirus literature. We have found that the ‘Morbidity and Mortality Weekly Report’ is the top journal. The core article of coronavirus literature is ‘Guidelines for preventing health-care-associated pneumonia’. The most commonly used word, in titles, abstracts, author’s keywords, and keywords plus, is ‘SARS’. Top affiliation is ‘The University of Hong Kong’. Hong Kong is a leading country based on citations, and the USA is on top based on total publications. We have used a conceptual framework to identify potential research streams and themes in coronavirus literature. Four research streams are found by deploying a co-occurrence network. These research streams are ‘Social and economic effects of epidemic disease’, ‘Infectious disease calamities and control‘, ‘Outbreak of COVID 19,’ and ‘Infectious diseases and the role of international organizations’. Finally, a thematic map is used to provide a holistic understanding by dividing significant themes into basic or transversal, emerging or declining, motor, highly developed, but isolated themes. These themes and subthemes have proposed future directions and critical areas of research.
Keywords: Bibliometric analysis, biblioshiny, conceptual structure, COVID survey, coronavirus, COVID-19, pandemic, r-studio, SARS, social sciences
I. Introduction
Coronavirus infects humans most commonly leads to Upper Respiratory Infection (URI). It is single-stranded RNA viruses that cause various kinds of illnesses in birds and mammals, including humans. Family of coronaviruses is used to be epidemic, but SARS-CoV-2 is declared as the pandemic by WHO. Figure 1 is a clear representation of the spread of COVID-19. The disease spread from a person with the virus to a person through droplets from the mouth and nose [1]. The impact of SARS-CoV-2 causes social and economic damages throughout the world. Figure 1 shows the daily confirm cases in the world by WHO. As of June 23, 2020, there are approximately 8.86 million confirmed cases across the globe and 0.46 million loss of lives. It has a severe social impact. Moreover, coronavirus has affected the social, business, and economic dynamics of the world. As with COVID-19 outbreak throughout the globe, different governmental pandemic mitigation restrictions (PMR) has been imposed. Under these arrangements, maximum social activities are ban in various countries. Non-essential trade within and outside the states has been restricted. Both the infectious disease outbreak and PMR have a significant effect on the development and growth of society economically [2]. It is essential to propose the solution for socio-economic hindrances created from the outbreak of infectious diseases such as Severe Acute Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS), and SARS-CoV 2.
FIGURE 1.
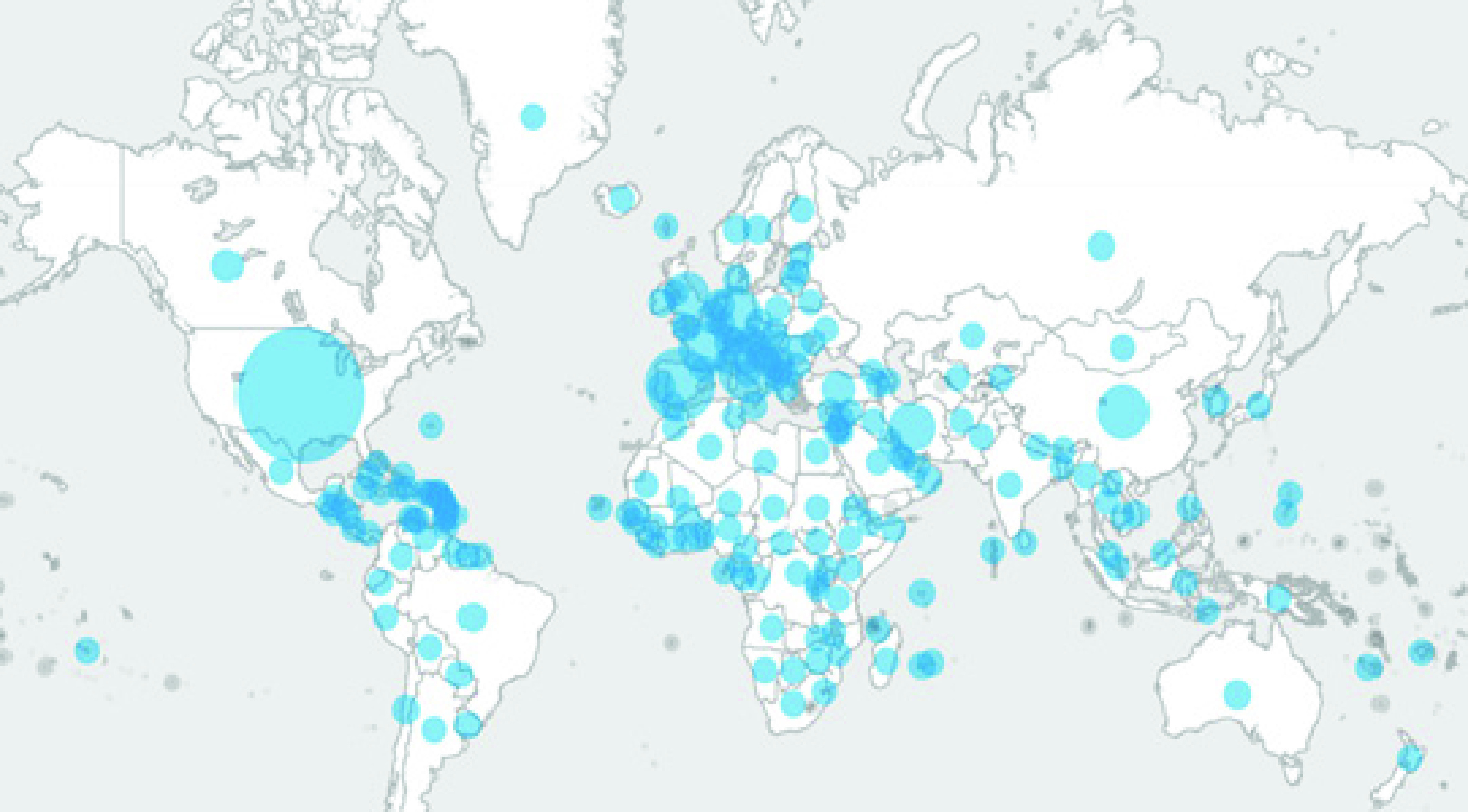
Confirm Cases of COVID-19 in the World [419].
It is imperative to see that there are various epidemic infectious diseases in the past. These viral diseases have put pressure on societies and economies. This study undertakes the past literature of viral infections related to coronavirus in the field of social sciences, economics, and business and performs a bibliometric analysis. The objective of this research is to analyze the literature and identify top countries, authors, affiliations, sources related to infectious viral diseases. Furthermore, this study aims to find research streams and themes by using the literature of coronavirus in the field of social sciences for the period 2003-2020. The themes and research streams may lead the policymakers, scholars, and researchers to the direction for future research and find answers to current problems. Moreover, it is the quantitative approach to provide a systematic study of written publications.
The bibliometric analysis significantly improves the quality of the literature review by introducing a transparent, systematic, and reproducible review process. It provides means for mapping the research fields and influential work without subjective bias that is imperative for holistic aid to the literature process [3]. For bibliometric analysis, this study uses ‘biblioshiny’ the web-based interface of R-package (‘bibliometrix 3.0’).
II. The Procedure of Bibliometric Analysis
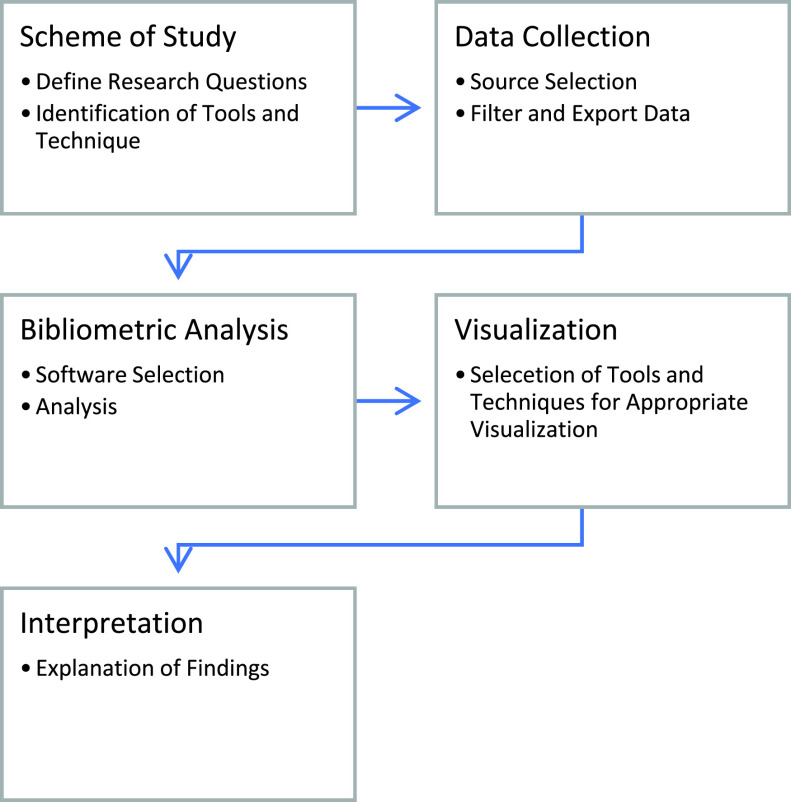
This article proceeds with five steps, known as a bibliometric workflow that is suggested by Zupic and T. Čater [4]. Figure 2 represents the five steps to complete the process of bibliometric analysis of Coronavirus literature.
FIGURE 2.
The Procedure of Bibliometric Analysis.
III. Scheme of Study
The current situation in the world raises many questions that need to be answered. For this research, we consider the following questions to be answered that will help to identify the dynamics of coronavirus literature and provide holistic means for future research in the field where biological sciences links with social sciences. This study addresses the following questions.
-
1.
What are the influential aspects of coronavirus literature in the field of social sciences?
-
2.
Exploring coronavirus literature of social sciences, what are the main trends and key themes?
-
3.
To prepare for the future, what comprehensive lessons can we take from the past literature, and what future agendas can be set?
We answer question 1 with descriptive analysis and find core sources, authors, countries, publications, and affiliation in the coronavirus publications in the field of social sciences. For core sources and core authors, we have used source impact, total citations (TC), and net publications (NP) per year. Moreover, we identify the core sources by using Bradford’s Law. According to Bradford’s Law, sources are divided into three zones. Zone 1 is highly productive and considered as the nuclear zone. Zone 2 is moderately productive, and sources related to zone 3 has low production [5]. We suggest top countries and affiliations based on publication frequency and total citations.
Core areas of study and key themes are imperative for linking various research streams and generating future direction of study. For this purpose, we have adopted some technical tools such as co-occurrence map, thematic map, and thematic evolution. We use keywords plus for analysis because it describes the knowledge structure of the study and helps to identify and link different research areas [6]. The author’s keywords indicate the main issues of the study. Keywords plus are provided by the database that expresses the article contents succinctly. Keywords plus offer more descriptive trends than the author’s assigned keywords [7]. We are deploying ‘biblioshiny’, which is the bibliometric analysis tool provided by the R-program, to identify research streams and themes using keywords of infectious disease literature.
A. Objectives, Tools, and Techniques
The objective of this study is to provide the bibliometric review of the literature of coronavirus in social sciences, which can be used to curb the minus created by the infectious disease in the global social network. Moreover, we aim to provide means to improve our economic and social set up under a globalized network from these pathogens. We have subdivided our objective for better understanding.
The first objective of the study is to find core publications, authors, countries, and institutions. To fulfil this objective, we use ‘biblioshiny’, a web-specific R package (‘bibliometrix 3.0’) for descriptive analysis of documents. Tools from the ‘biblioshiny’ interface for analysis are; Bradford’s Law, global citation, h, g, and m-index. The second objective is the find the key research streams and themes. For this objective, we are using science mapping techniques of conceptual structure and using keywords plus as the input data. After completion of objections 1 and 2, we can provide a comprehensive interpretation and define future research agendas.
IV. Composing of Bibliometric Data
The composition of our bibliometric data has two segments. In the first segment, we select the source from where we can take and analyze articles. For that purpose, we have selected various databases such as Scopus, Web of Science (WOS), Emerald, and google scholar. In the second segment, we have formed the search query for holistic data collection. We have selected the field of social sciences for collection for that purpose, we have applied various filters to our search query and make it match to our objective and optimal results. The final search query is ‘TITLE-ABS-KEY (“coronavirus” OR “corona virus” OR “COVID-19” OR “COVID 19” OR “SARS-CoV 2” OR “betacoronavirus” OR “SARS coronavirus” OR “severe acute respiratory syndrome” OR “MERS-CoV” OR “middle east respiratory syndrome”) AND (LIMIT-TO (SRCTYPE, “j”)) AND (LIMIT-TO (PUBSTAGE, “final”)) AND (LIMIT-TO (DOCTYPE, “ar”)) AND (LIMIT-TO (SUBJAREA, “SOCI”) OR LIMIT-TO (SUBJAREA, “BUSI”) OR LIMIT-TO (SUBJAREA, “ECON”)) AND (EXCLUDE (PUBYEAR, 1999)) AND (LIMIT-TO (LANGUAGE, “English”))’. Approximately all articles are related to a coronavirus search query. The reason for using COVID 19 is to check whether any research hinted towards this keyword in the past. The final search query has able to find 328 articles from social sciences, 27 articles are from economics, econometrics, and finance, and 40 articles are from the field of business, management, and accounting. Business and economics have a significant effect on social wellbeing, which is why we are considering these articles under social sciences. The conceptual framework uses keywords for theme generation, and for efficient analysis, we limit our search query to only journal articles and articles with the English language. The reason for using one comprehensive language to provide efficient bibliometric analysis is that it gives us various tools that compare keywords, articles sources, and affiliations. There are ten articles in other languages, and keyword analysis will perform better in one language. Moreover, we manually analyze the articles, and twelve articles were dropped because they were not according to the objective of this study, our final sample is comprising of 395 articles.
V. Bibliometric Analysis and Visualization
Bibliometric analysis is the application of statistical and mathematical tools to books and media communication [8]. ‘Biblioshiny’ is the tool under the package which is designed for non-coders to provide means for complete scientometric and bibliometric analysis offering numerous options divided into categories of sources, documents, authors, conceptual structure, social structure, and intellectual structure. It allows obtaining multiple results in the shape of tables and graphs, which are not common in other software [9].
Table 1 provides the descriptive characteristics of corona literature that is imperative to understand before moving forward with the analysis. We finalized 395 documents that only journal articles. All these journals use 1699 keywords plus and 873 author keywords. The period we used for corona literature is from 2004 to 2020.
TABLE 1. Descriptive Characteristics of Corona Literature.
| Description | Results |
|---|---|
| Documents | 395 |
| Sources (Journals) | 243 |
| Keywords Plus (ID) | 1699 |
| Author’s Keywords (DE) | 873 |
| Period | 2003 - 2020 |
| Average citations per documents | 16.18 |
| Authors | 1492 |
| Author Appearances | 1671 |
| Authors of single-authored documents | 104 |
| Authors of multi-authored documents | 1388 |
| Single-authored documents | 117 |
| Documents per Author | 0.265 |
| Authors per Document | 3.78 |
| Co-Authors per Documents | 4.23 |
| Collaboration Index | 4.99 |
A total of 1492 authors wrote these documents; among them, only 104 articles are with a single author. There is a high collaboration in corona publications that is shown by the collaboration index. Document per author ratio is 0.264, which means, on average, almost four authors have written one document.
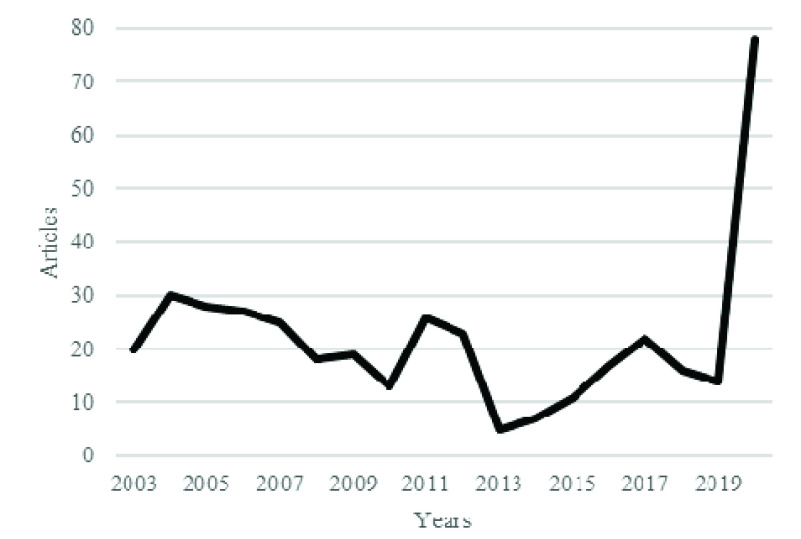
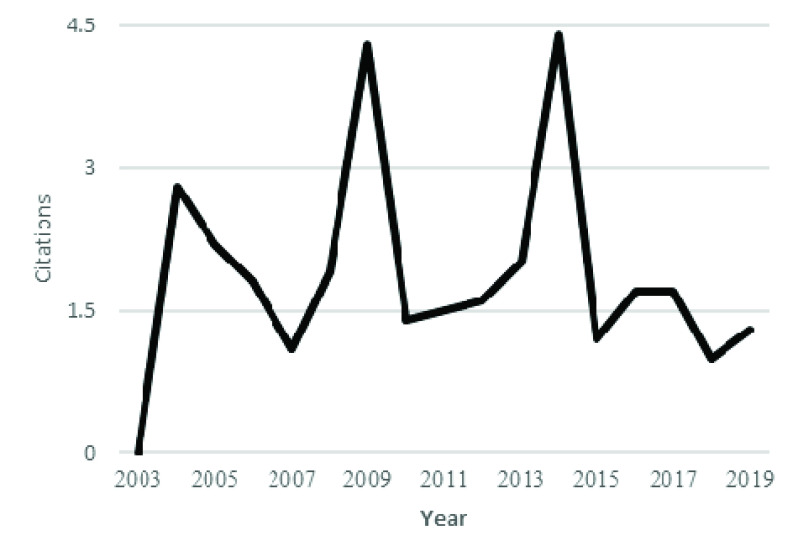
Figure 3 shows the annual production, and figure 4 shows the citation per year for coronavirus publications. There is limited production at the start, but literature production increases with time, especially after the identification of Severe Acute Respiratory Syndrome (SARS) coronavirus in the Guandong province of China. SARS was also an epidemic disease affecting 26 countries and resulted in more than 8000 cases. At that time, implementations of feasible practices for infection control brought the end to this infection [10]. After the control, there was a decrease in both production and citation of coronavirus studies. However, then again, after 2010, there was an increasing trend in the publications and citations of coronavirus studies. There was a significant increase in the annual citation of coronavirus publications from 2013 to 2015. This increase in citation and total production after 2015 is due to the outbreak of MERS.
FIGURE 3.
Annual scientific production.
FIGURE 4.
Average article citation per year.
In addition to the annual production and article citations per year, it is imperative to see the main topics, places, and affiliations of coronavirus publications. Figure 5 presents the three-fold analysis of coronavirus publication with a keyword plus on the left side of the figure, affiliations on the right, and countries of interest in the middle. The figure shows that the USA is working with most of the top affiliations concerning topics related to the outbreak of infectious disease. Furthermore, China, Hong Kong, Canada, and the United Kingdom have significant contributions based on various social science topics of infectious disease. Issues related to SARS are most studied in most of the countries.
FIGURE 5.
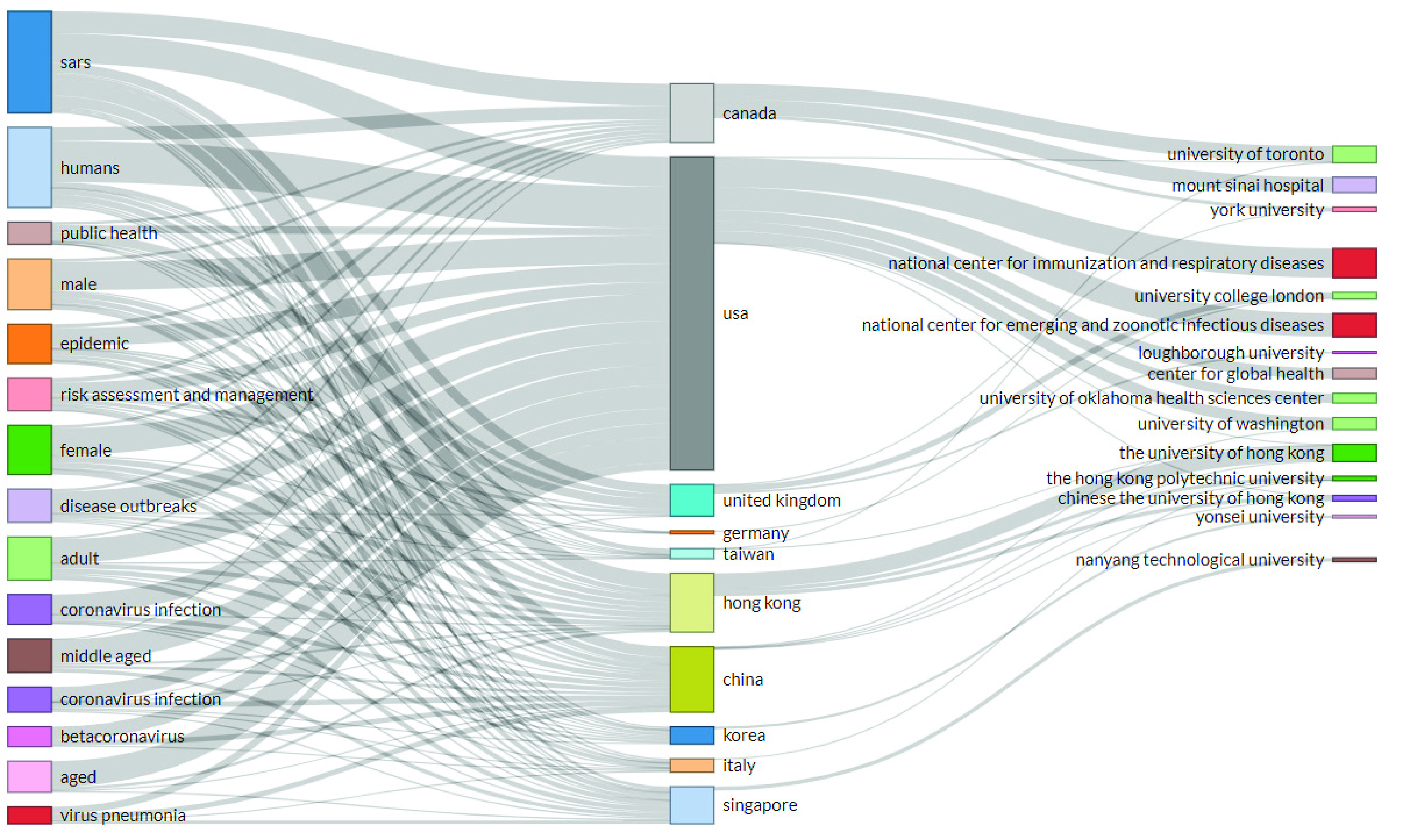
Three-fold analysis of corona literature.
A. Influential Aspects of Coronavirus Literature
1). Core Journals
To find the core journals, involved in publishing coronavirus literature in the field of social sciences, we use source impact and Bradford Law. Table 2 ranks the articles based on h, m, g-index, total citation (TC), and net production (NP) and publication starting year (PY_start). Table 3 represents Bradford law, which divides the journal into three zones. Zones 1 represents core sources for publishing coronavirus articles. This is the nuclear zone representing journals having significant publications. Table 3 reports the journal rankings according to Bradford law. We have found that out of 395 journals, 23 journals comes under core zone 1, the rest of the journals are in zone 2 and zone 3. Top 23 journals are the core publishing sources for corona literature in social sciences.
TABLE 2. Top Ten Journals According to Source Impact.
| Top 10 Journals | h_index | g_index | m_index | TC | NP | PY_start |
|---|---|---|---|---|---|---|
| Morbidity and Mortality Weekly Report | 11 | 18 | 0.647 | 342 | 33 | 2004 |
| Social Science and Medicine | 9 | 9 | 0.529 | 670 | 9 | 2004 |
| Health Security | 4 | 6 | 0.800 | 36 | 8 | 2016 |
| Building and Environment | 7 | 7 | 0.438 | 640 | 7 | 2005 |
| Economic and Political Weekly | 0 | 0 | 0.000 | 0 | 6 | 2020 |
| Fortune | 1 | 1 | 0.056 | 4 | 6 | 2003 |
| Tourism Management | 5 | 6 | 0.333 | 401 | 6 | 2006 |
| Asian Journal of Social Psychology | 4 | 5 | 0.235 | 107 | 5 | 2004 |
| Bioscience Trends | 4 | 5 | 0.333 | 109 | 5 | 2009 |
| International Journal of Hospitality Management | 5 | 5 | 0.278 | 217 | 5 | 2003 |
TABLE 3. Journal Rankings According to Bradford Law.
| Sources | Rank | Freq | cumFreq | Zones |
|---|---|---|---|---|
| Morbidity and Mortality Weekly Report | 1 | 33 | 33 | Zone 1 |
| Social Science and Medicine | 2 | 9 | 42 | Zone 1 |
| Health Security | 3 | 8 | 50 | Zone 1 |
| Building and Environment | 4 | 7 | 57 | Zone 1 |
| Economic and Political Weekly | 5 | 6 | 63 | Zone 1 |
| Fortune | 6 | 6 | 69 | Zone 1 |
| Tourism Management | 7 | 6 | 75 | Zone 1 |
| Asian Journal of Social Psychology | 8 | 5 | 80 | Zone 1 |
| Bioscience Trends | 9 | 5 | 85 | Zone 1 |
| International Journal of Hospitality Management | 10 | 5 | 90 | Zone 1 |
| Asian Journal of Communication | 11 | 4 | 94 | Zone 1 |
| Journal of Contingencies and Crisis Management | 12 | 4 | 98 | Zone 1 |
| Scientometrics | 13 | 4 | 102 | Zone 1 |
| Sustainability (Switzerland) | 14 | 4 | 106 | Zone 1 |
| Asia Pacific Journal of Tourism Research | 15 | 3 | 109 | Zone 1 |
| Australian Journal of International Affairs | 16 | 3 | 112 | Zone 1 |
| Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science | 17 | 3 | 115 | Zone 1 |
| Current Issues in Tourism | 18 | 3 | 118 | Zone 1 |
| Eurasian Geography and Economics | 19 | 3 | 121 | Zone 1 |
| International Journal of Human Resource Management | 20 | 3 | 124 | Zone 1 |
| Journal of Chemical Information and Modelling | 21 | 3 | 127 | Zone 1 |
| Journal of Health Communication | 22 | 3 | 130 | Zone 1 |
| Medical Teacher | 23 | 3 | 133 | Zone 1 |
| Medicine and Law | 24 | 3 | 136 | Zone 2 |
| Safety Science | 25 | 3 | 139 | Zone 2 |
Morbidity and mortality weekly report (MMWR) is a significant platform for publishing coronavirus literature in the field of social sciences. From its recent publications by Ng et al. in [11] stating that during COVID-19 pandemic, test the multipronged surveillance system, in which they provide means to detect coronavirus patients in Singapore. Furthermore, the reporting provided by Burke et al. in [12] and Jernigan in [13], indicated the effect of COVID-19 in the United States and suggested monetary measure to the center of disease control, states, local and public health care to reduce the spread of COVID-19. 70% of symptomatic persons have a travel-related risk of getting coronavirus, 20% having contact with laboratory diagnosed patients. 9% had both risk factors [14].
Published in MMWR, As reported by Foote et al. in [15], the urgency of Isolation and rapid recognition during the infectious disease outbreaks. The study used unannounced mystery patient drills in 49 New York City hospital emergency departments to test protocols and the ability of staff members to manage and identify the infectious patients. The results of the drills indicated that infectious patients were masked and isolated 78% of drills. Moreover, 88% of the time, patients were masked and isolated when travel history was obtained, and 21% when it was not. Median time taken by staff for masking was 1.5 minutes and 8.5 minutes for isolation. The study suggested tool kits for similar drills to enhance the health care system in the United States. The nosocomial outbreak of SARS infectious disease in the health care hospital in Riyadh is also covered by MMWR [16]. It has also published reports regarding found cases and has suggested public guidelines about the Middle-East respiratory syndrome coronavirus (MERS-COV) infection [17]–[19].
Figure 6 shows the growth in the publication by top journals. We use the loess smoothing technique that is the locally weighted smoothing use regression analysis to demonstrate the smooth line with the help of a time plot or scatter plot. Loess smoothing helps to understand treads through time [20]. There has been significant growth in publications by MMWR since 2010. it represents the primary source of coronavirus literature in social sciences. Economic and political weekly have a decreasing trend from 2014 to 2016, then there is a Sharpe increase in the publications from 2016 onwards. Health security has a significant growth for the past three years. Scholars and policymakers should go through these publications during pandemic times because these journals can provide useful information for infectious diseases their socio-economic impact. The rest of the journals has no significant loess smoothing when regress through time.
FIGURE 6.
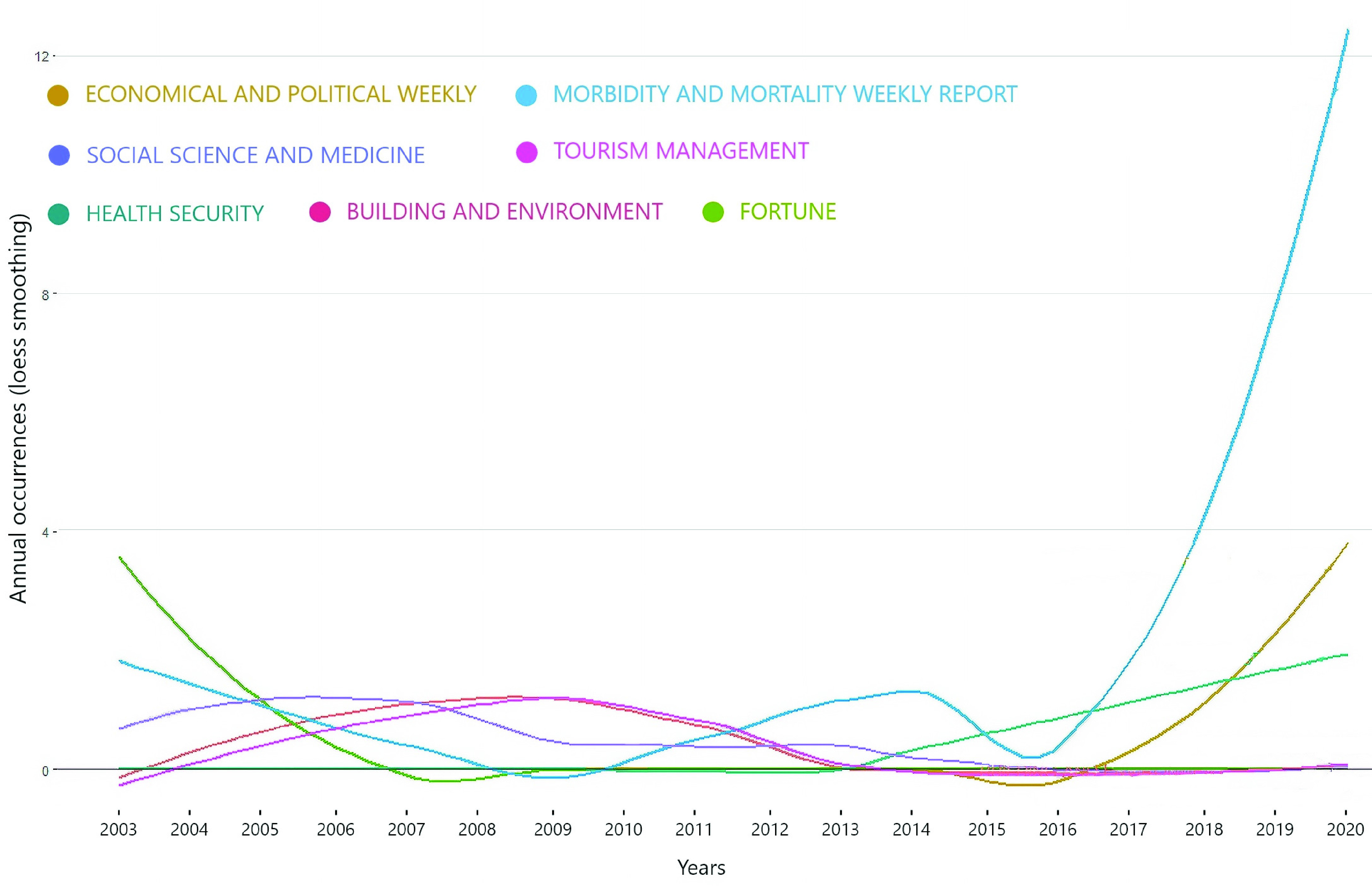
Source Growth.
2). Core Journal Articles
This section highlights the leading articles in coronavirus publications in the field of social sciences. We have listed down the top 10 globally cited articles in table 4.
TABLE 4. Most Globally Cited Article.
| Paper | Total Citations | TC per Year |
|---|---|---|
| Guidelines for preventing health-care-associated pneumonia [21] | 986 | 58.00 |
| Policies and technical guidelines for urban planning of high-density cities - air ventilation assessment (AVA) of Hong Kong [22] | 248 | 20.67 |
| Health care workers’ ability and willingness to report to duty during catastrophic disasters [23] | 241 | 15.06 |
| Responding to global infectious disease outbreaks: Lessons from SARS on the role of risk perception, communication, and management [24] | 201 | 13.40 |
| Perceived travel risks regarding terrorism and disease: The case of Thailand [25] | 148 | 12.33 |
| Distinguishing knowledge-sharing, knowledge-construction, and knowledge-creation discourses [26] | 138 | 11.50 |
| Disease metaphors in new epidemics: The UK media framing of the 2003 SARS epidemic [27] | 119 | 7.44 |
| The impact of crisis events and macroeconomic activity on Taiwan’s international inbound tourism demand [28] | 114 | 9.50 |
| Representations of SARS in the British newspapers [29] | 98 | 5.76 |
| The airborne transmission of infection between flats in high-rise residential buildings: Particle simulation [30] | 95 | 7.31 |
On top of the list, Tablan et al. [21] conducted the study in 2004 regarding guidelines for reducing the incidence of severe acute respiratory infections in health care settings and acute care hospitals. The study from Ng [22] is second on the list of most globally cited articles and can be used for future remedial research regarding coronavirus impacts on the globalized world. They investigated the spread of SARS in 2003 in Hong Kong.
Ng in [22] discussed the implementation and scientific process of air ventilation assessment (AVA) system in urban areas of Hong Kong. Qureshi in [23] reported the surge capacity needs in the situation of catastrophic disasters. He has surveyed surge capacity from health workers and found that 83% were willing to report in the circumstances of mass casualty incidents, but 64% were willing to report in the situation of the SARS outbreak. He also identified that barriers to willingness were fear and concern for family and oneself and tentative health problems.
Smith [24] highlighted the main concerns for the future from the outbreak of SARS in 2006 that we are facing in the 2019 pandemic. He indicated that the epidemic of SARS might assist in dealing with the pandemic situation in the future. He suggested that perception of risk, management, and communication played an essential role in the economic impact of infectious disease. Furthermore, the role of official organizations and media and the establishment of risk priorities for a better system might prevent a future global pandemic. We do not agree with his conclusion that there is low potential for the spread of infectious disease after SARS.
Rittichainuwat and Chakraborty [25] investigated the impact of infectious diseases such as SARS into the hospitality industry of Thailand. Their article comes on fifth highly cited article among 395 articles. They suggested that travelers continue traveling in the time of crises, but they choose less dangerous destinations.
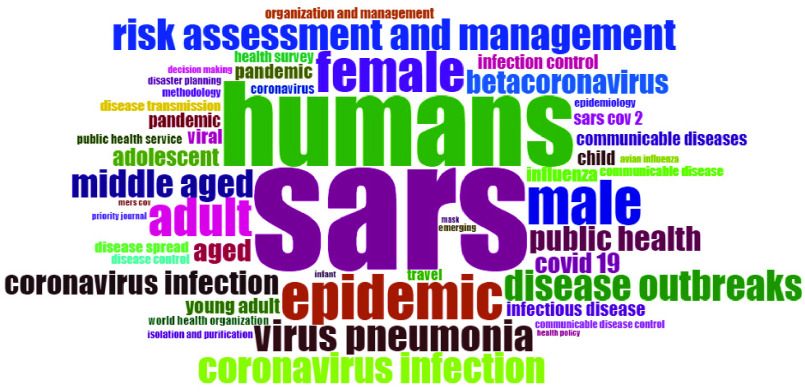
3). Core Words
Table 5 provides the most frequent words used in coronavirus literature in the field of social sciences. The table is divided into four parts of keywords plus, Authors Keywords, Abstract, and Title.
TABLE 5. Most Frequent Words.
| Keyword Plus | Author Keyword | ||
|---|---|---|---|
| Words | Occurrences | Words | Occurrences |
| sars | 228 | sars | 55 |
| humans | 158 | covid 19 | 30 |
| epidemic | 85 | severe acute respiratory syndrome sars | 18 |
| male | 83 | Hong Kong | 17 |
| female | 77 | china | 16 |
| adult | 72 | crisis | 11 |
| virus pneumonia | 60 | pandemic | 11 |
| risk assessment and management | 59 | coronavirus | 9 |
| coronavirus infection | 58 | epidemics | 9 |
| disease outbreaks | 58 | influenza | 9 |
| Abstract | Title | ||
| Words | Occurrences | Words | Occurrences |
| health | 464 | sars | 100 |
| sars | 446 | health | 67 |
| public | 264 | COVID | 51 |
| respiratory | 248 | respiratory | 51 |
| outbreak | 239 | syndrome | 43 |
| disease | 230 | outbreak | 37 |
| syndrome | 221 | public | 35 |
| severe | 211 | crisis | 33 |
| study | 207 | disease | 33 |
| acute | 195 | coronavirus | 29 |
In all parts, SARS is the most common word. Social sciences are related to society, economy, and people, which has been shown in the keywords as well. These keywords are related to infectious diseases, public health, humans. In coronavirus literature, minimal author keywords are used. Keyword plus covers the broad topics, where there are common infectious diseases used as keywords. Additionally, keywords related to Human, male, female, and middle-aged indicate the relationship between coronavirus and society.
There are topics related to disease outbreak and epidemic. Not many researchers used author keywords. Health is the most used word in the abstract, and SARS is the highly used word in the title. Terms used in abstract and title are more generic that are less likely to produce any theme or research stream. Figure 7 shows the word cloud made from keyword plus. Words with high frequency in the literature are more in size. Humans and SARS have the highest frequency in the literature of social sciences. So, these are the biggest of all the words used. Then there is an epidemic, which has a strong history in China and Canada. The literature is about social sciences. That is why much research is done on the social aspects of society. Like many researchers link the infectious disease with humans, gender, age groups animals, etc. There are studies on communicable diseases, disease outbreaks, and viral infections. Some studies link the infectious diseases with travel history, so travel is used as a keyword. Isolation and purification are used in coronavirus literature as a keyword, and it is crucial as well because it helps to strengthen the isolation strategies further and secure the society. Risk assessment and infection control are also used as the keyword in literature, and these studies can be used to elaborate on the solutions for epidemic control further. All these keywords are linked and address many problems that the world is facing today. Use this literature and find a solution that can save the globalized economies from a possible future pandemic.
FIGURE 7.
Word Cloud.
In addition to the word cloud, figure 8 gives us a picture of word growth in literature through time. As shown in the figure, the coronavirus keyword started to grow after 2010. The body of knowledge began to identify the need for this problem to get solved. Beta coronavirus represents coronaviruses one of four genera that infect bets mainly, but the infection can be found in other species like camels, rabbits and humans [31]. Figure 8 uses a loess smoothing technique to analysis the growth of keywords usage overtime. The use of COVID 19 keyword decreases after 2014, but after 2017, there has been a Sharpe increase in the topics related to COVID 19. Throughout the years from 2000 to 2013, SARS dominated the rest of the keywords, but after 2013 there is a decrease in SARS keyword and increase in coronavirus related topics. The growth has been observed in keywords such as coronavirus, pandemic and china.
FIGURE 8.
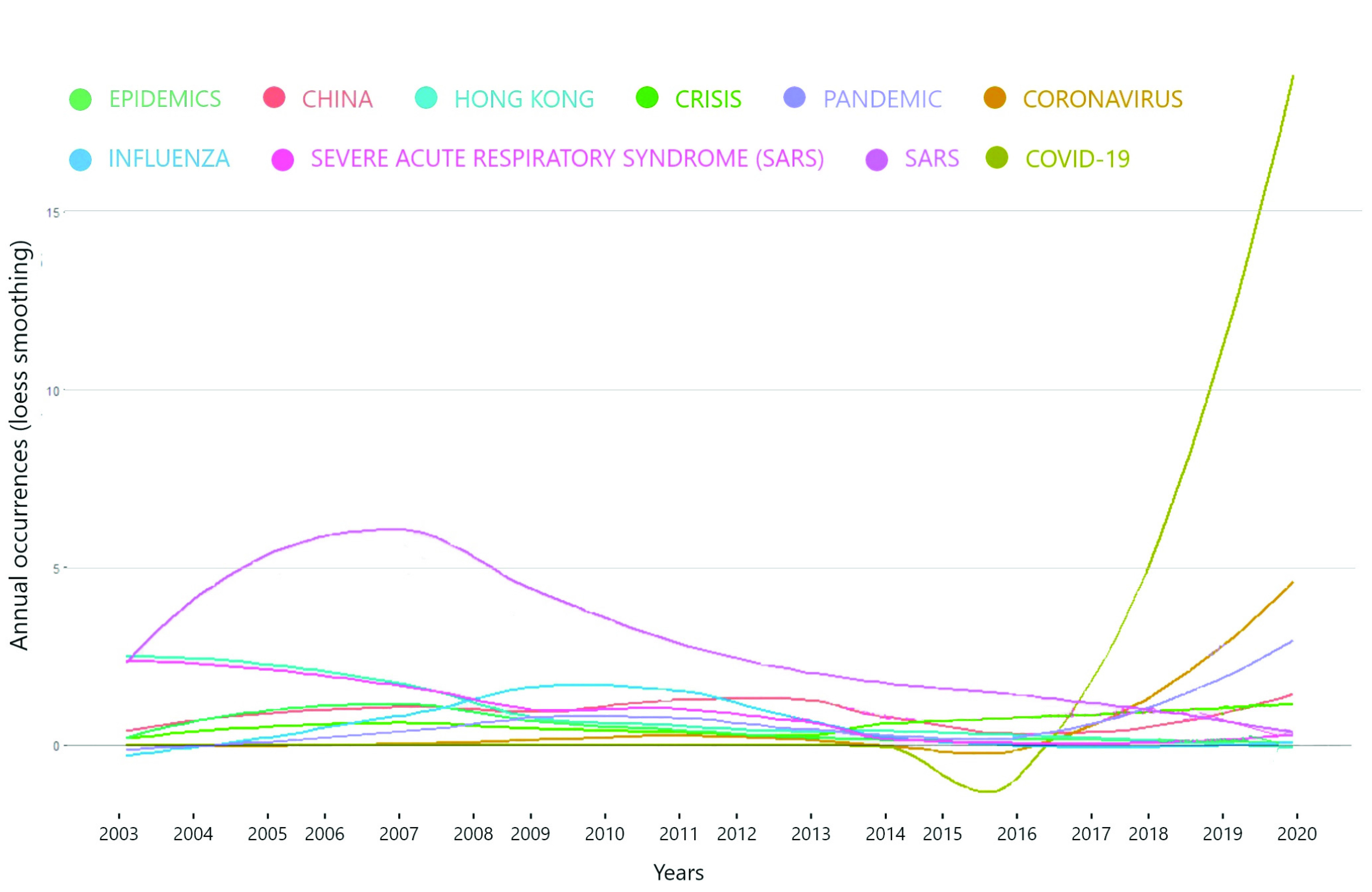
Word Growth Overtime.
4). Main Authors, Affiliation, Institutions and Countries
This section provides information regarding core authors, affiliations, institutions and countries of coronavirus literation in the field of social sciences. There are ten authors having a more significant impact in coronavirus literature, and these authors are listed in table 7. Ranking is on the basis of h-index.
TABLE 6. Top 10 Authors Impact in Corona Pandemic Literature.
| Author | h_index | g_index | m_index | TC | NP | PY_start |
|---|---|---|---|---|---|---|
| Chau | 4 | 4 | 0.235 | 91 | 4 | 2004 |
| Ho | 4 | 4 | 0.235 | 91 | 4 | 2004 |
| Ali | 3 | 4 | 0.188 | 89 | 4 | 2005 |
| Huang | 3 | 4 | 0.273 | 69 | 4 | 2010 |
| Gerber | 3 | 3 | 0.429 | 97 | 3 | 2014 |
| Li | 3 | 3 | 0.176 | 85 | 3 | 2004 |
| Rha | 3 | 3 | 0.375 | 30 | 3 | 2013 |
| Smith | 3 | 3 | 0.200 | 256 | 3 | 2006 |
| Watson | 3 | 3 | 0.429 | 97 | 3 | 2014 |
| Zhang | 3 | 3 | 0.176 | 28 | 3 | 2004 |
TABLE 7. Top Countries in Terms of Publications and Citations.
| Country and Regions | Frequency | Country and Regions | Total Citations |
|---|---|---|---|
| USA | 236 | Hong Kong | 1291 |
| Canada | 79 | USA | 877 |
| China | 75 | UK | 568 |
| UK | 52 | China | 453 |
| Taiwan | 45 | Taiwan | 444 |
| South Korea | 31 | Canada | 379 |
| Singapore | 26 | Thailand | 148 |
| Germany | 18 | Singapore | 98 |
| Italy | 16 | Australia | 97 |
| Australia | 15 | Korea | 65 |
Chau is at number one on the list of authors with the highest impact. Chau, with collaboration with Ho (ranked second), published profoundly impact journal articles. Wong et al. [32] discussed environmental quality and human health. They indicated that despite the absence of the central ventilation system, the nasal discomfort was the primary source of sick building syndrome (SBS). Moreover, they surveyed about indoor environmental quality (IEQ) and concluded that noise rather ventilation was the major IEQ problem. They, in [33], analyzed the impact of crises shock on housing prices using the hedonic price model. They reported a negative impact of SARS on housing prices. Just before this article, they in [34] observed a similar impact on the town planning board (TBT) and housing developers. They concluded that TBT was effected by the shocks created from the outbreak of infectious disease, but developers were not affected by any shocks. They, in [35], investigated the stigmatization created from SARS. They indicated that many residents were affected by stigma in various sorts of being insulted, shunned, and rejected in the domain of work, schooling, services, and interpersonal relationships. According to their respondents, stigmatization decreased but never disappeared after the outbreak.
Ali (Third rank) in [36] discussed the disease outbreak in a political and social context. He suggested that infectious disease outbreaks should be addressed from a global perspective. Ali et al. [37] and Ali and Keil [38] discussed the risk of SARS and its mitigation. He described the political, economic, and social risk factors created from the pandemic and implications of these risk factors in a globalized world. Furthermore, Sanford and Ali [39] discussed various challenges for public health in Toronto after the SARS outbreak.
Huang (ranked four) in his single-authored manuscript [40] described the deteriorated seafood market of china because of the drug residue incidents. He stated the food safety policies and state control over the animal epidemic after the SARS outbreak. He further disclosed through his findings that the state faced hindrance local formers for transforming public rural vets into technology savvy and market-sensitive professionals that can discipline the fish market. His second article discussed the model for individual vulnerability and challenges from the outbreak of an infectious disease such as SARS and H1N1 [41].
Gerber is number fifth on the list of authors, but he has contributed significantly to the field of SARS, MERS, and social sciences. He has started publishing from 2014 with three net publications. He has 97 total citations. Gerber’s first two articles were published in MMWR that studied the first cases of MERS-COV identified in the United States and highlighted the guidelines for health authorities, clinicians, and the public [17], [18].
Li (rank sixth) studies the transmission of viruses and bacteria in [42]. The result of the study suggested that droplets and particles of virus transport short distance during breathing, but it traveled to longer distances during cough. Rha (ranked sixth) in [19] reported SARS as a novel coronavirus in the United States. Further, Rha reported the growth of MERS-CoV infection in the United States and provided guidelines for public health authorities, clinicians, and the general public [17]. Smith is on number eight concerning h and g-index, but he possesses the highest number of citations. Smith, in [24], discussed the risk of a more lethal outbreak than SARS in 2003. He suggested how people perceive the risk of disease outbreak was effected by the role of official organizational policies, research priorities, and the role of media. Smith, in [43], analyzed the economic impact due to the outbreak of infectious diseases. The study suggested that due to pandemic situations, specific steps were taken by states such as school closure and absenteeism from work. The authors suggested that pandemic became the reason for 0.5% to 2.0% GCP loss. In the case of school closure and absenteeism from work, this impact became triple in size.
Table 7 shows two sets of data; the left side represents the countries and regions with many scientific productions over time. On the right side, there are countries with several citations. As the USA is on top with several publications, Canada ranked second, and china ranked 3rd, but in citations, Hong Kong’s total citations are better than the USA. The USA, in the second position, when it comes to citations. The UK published 52 articles on infectious disease in social sciences, but they have 568 citations. Chine comes on forth in terms of citations.
Most relevant affiliations are reported in figure 9. The University of Hong Kong (HKU) comes in the first place. The university has provided a strong basis for research on infectious diseases. It has started the HKU forum on the COVID 19 pandemic and HKU research in COVID 19 for quality publications [44]. University of Toronto (UT) comes on the second list of most relevant affiliations. UT founded in 1827 and became the leading institution of Canada for knowledge creation, discovery, and learning. UT is Canada’s leading research institution [45].
FIGURE 9.
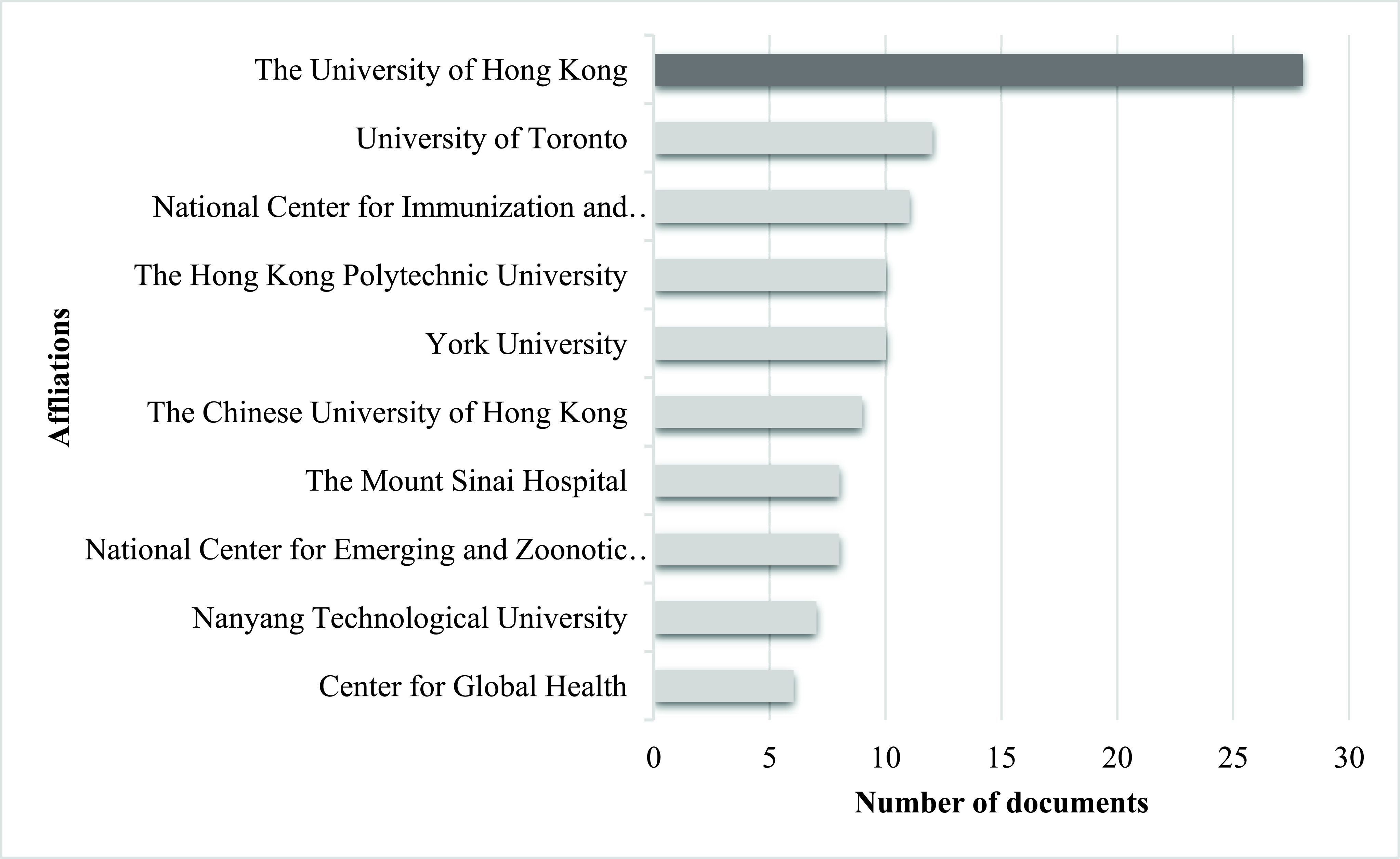
Most Relevant Affiliations.
The national center for immunization and respiratory diseases (NCIRD) at third the list of affiliations. NCIRD is responsible for coordinating, planning, and conducting immunization operations in the United States. It is the part of centers of disease control and prevention. NCIRD provides training, consultation, educational, epidemiological, statistical, and promotional services to state and local health departments in the US [46]. On the fourth position, The Hong Kong Polytechnique University is 80 years old research university. They solve real-world challenges with their diverse interdisciplinary research [47]. Yorks University offers a significant research base. With 95 million in research grants and awards, number 1 in global joint research publications, and 25 research centers, Yorks University comes 5th on the list of impactful affiliations [48]. The Chinese University of Hong Kong comes in sixth place as the impactful affiliations in the publication of infectious disease. It was founded in 1963 with a comprehensive researching university [49]. ‘Another day and another breakthrough’ is the slogan of the research center of Mount Sanai Hospital (ranked seventh). It like a technological and scientific revolution with the mission to create advanced treatments for patients through research laboratories and multi-disciplinary centers [50].
The national center for emerging and zoonotic infectious diseases (NCEZID) is eight on the list of most relevant affiliations. There are seven divisions of NCEZID that work with partners in the United States and all around to world for prevention of illness and deaths from various infectious diseases. Their objective is to protect people from health threats such as foodborne and waterborne illness, and infections spread in hospitals, antibiotic-resistant infections, a deadly disease like Ebola and anthrax, an illness that affects travelers, the disease caused by contact with animals such as SARS, MERS and corona and diseases spread by fleas and mosquitoes [51]. Center of global health (CGH) provides its unique scientific knowledge, technical skills, and research to take global public health actions. Its mission is to improve the safety, security, and health of Americans while restricting mortality and morbidity worldwide [51]. It is the 10th most relevant affiliation for coronavirus publications.
Table 8 presents the data regarding the top 10 corresponding author countries, and the USA is at number one. Corresponding authors from the USA have published 64 articles from which 48 are single country publications (SCP), and 16 are multiple country publications (MCP).
TABLE 8. Corresponding Author’s Country.
| Countries and Regions | Articles | Freq | SCP | MCP | MCPratio |
|---|---|---|---|---|---|
| USA | 64 | 0.24 | 48 | 16 | 0.25 |
| Hong Kong | 44 | 0.17 | 33 | 11 | 0.25 |
| Canada | 27 | 0.10 | 22 | 5 | 0.185 |
| China | 21 | 0.08 | 16 | 5 | 0.238 |
| Taiwan | 19 | 0.07 | 15 | 4 | 0.211 |
| Korea | 14 | 0.05 | 12 | 2 | 0.143 |
| United Kingdom | 14 | 0.05 | 9 | 5 | 0.357 |
| Singapore | 9 | 0.03 | 8 | 1 | 0.111 |
| Italy | 7 | 0.03 | 5 | 2 | 0.286 |
| Australia | 6 | 0.02 | 5 | 1 | 0.167 |
Multiple country publications refer to at least one co-author from a foreign country. Hong Kong is in the second position with correspondence of 44 articles, with 33 SCP and 11 MCP. There are 27 publications in Canada with 22 SCP and 5 MCP. China is the fourth position with the correspondence of 21 research articles for infectious diseases. It has SCP of 16 and MCP if 4. Taiwan comes in the fifth position with 19 corresponding research articles.
The issue of coronavirus is related to global social networks, and for the safety of diverse societies, major collaborations are required on coronavirus literature in the field of social sciences. Table 9 has addressed this issue, but unfortunately, very little collaboration has been observed with countries around the globe. China collaborated with the USA in 3 articles, and the USA collaborated with Korea in 5 publications. The rest of the countries in the table collaborated in 4, 3, and 2 articles only.
TABLE 10. Keywords in Each Cluster.
| Keywords | Clusters | Research Stream |
|---|---|---|
| Public health, uncertainty, unemployment, SARS, epidemic, hotel industry, Asian economy, China, human resource management (HRM), labor market, service sector | Red | Social and economic effects of epidemic disease |
| SARS, crises, resilience, infectious disease, quarantine, tourism, crisis management, tourism demand, globalization, influenza | Blue | Infectious disease calamities and control |
| COVID 19, coronavirus, SARS-CoV 2, pandemic, social media, epidemic | Green | The outbreak of COVID 19 |
| Infectious diseases, global health governance, avian influenza, international health organizations, world health organization | Purple | Infectious diseases and the role of international organizations |
TABLE 11. Themes and Keywords in Thematic Map.
| Cluster Representation | Theme | Keywords in Clusters |
|---|---|---|
| SARS | Basic Theme | SARS, risk assessment and management, public health, infectious disease, disease spread, disease transmission, disease control, world health organization |
| Humans | Basic Theme | Humans, epidemic, disease outbreak, coronavirus infection, male, female, adult, middle age, pandemic, viral |
| Communicable disease | Emerging theme | Communicable disease, organization and management, health survey, methodology, emerging, population surveillance, public health administration |
| Infection control | Motor theme | Infection control, public health service, education, psychological aspect, attitude |
| Avian influenza | Highly developed and Isolated Themes | Avian influenza, health care personal, attitude, acquired immune deficiency syndrome |
| Coronavirus | Highly developed and Isolated Themes | Coronavirus, respiratory disease, viral disease, computer simulation |
TABLE 9. Collaboration Network.
| From | To | Frequency |
|---|---|---|
| China | USA | 9 |
| USA | Korea | 5 |
| UK | Germany | 4 |
| UK | USA | 4 |
| USA | Canada | 4 |
| USA | Taiwan | 4 |
| UK | Hong Kong | 3 |
| USA | Hong Kong | 3 |
| Australia | Korea | 2 |
| China | Hong Kong | 2 |
B. Conceptual Framework
This section helps us to understand various themes using the relationship among words (keyword plus). At first, the study proposes a co-occurrence network that allows us to evaluate multiple topics of coronavirus pandemic in social sciences over time. Then we will put these networks of words on a bi-dimensional matrix called ‘Thematic Map’ to analyze to centrality and density of the network.
1). Co-Occurrence Network
Figure 10 shows the co-occurrence network of keyword plus. The figure is extracted from the ‘biblioshiny’ of R-package (‘bibliometrix’). The co-occurrence network of keywords is showing that coronavirus literature in social sciences can be divided into four streams. Red cluster is the central cluster with high centrality, blue and green clusters are linked together in terms of themes. SARS coronavirus has the highest centrality. Each group divides the coronavirus literature in various research streams.
FIGURE 10.
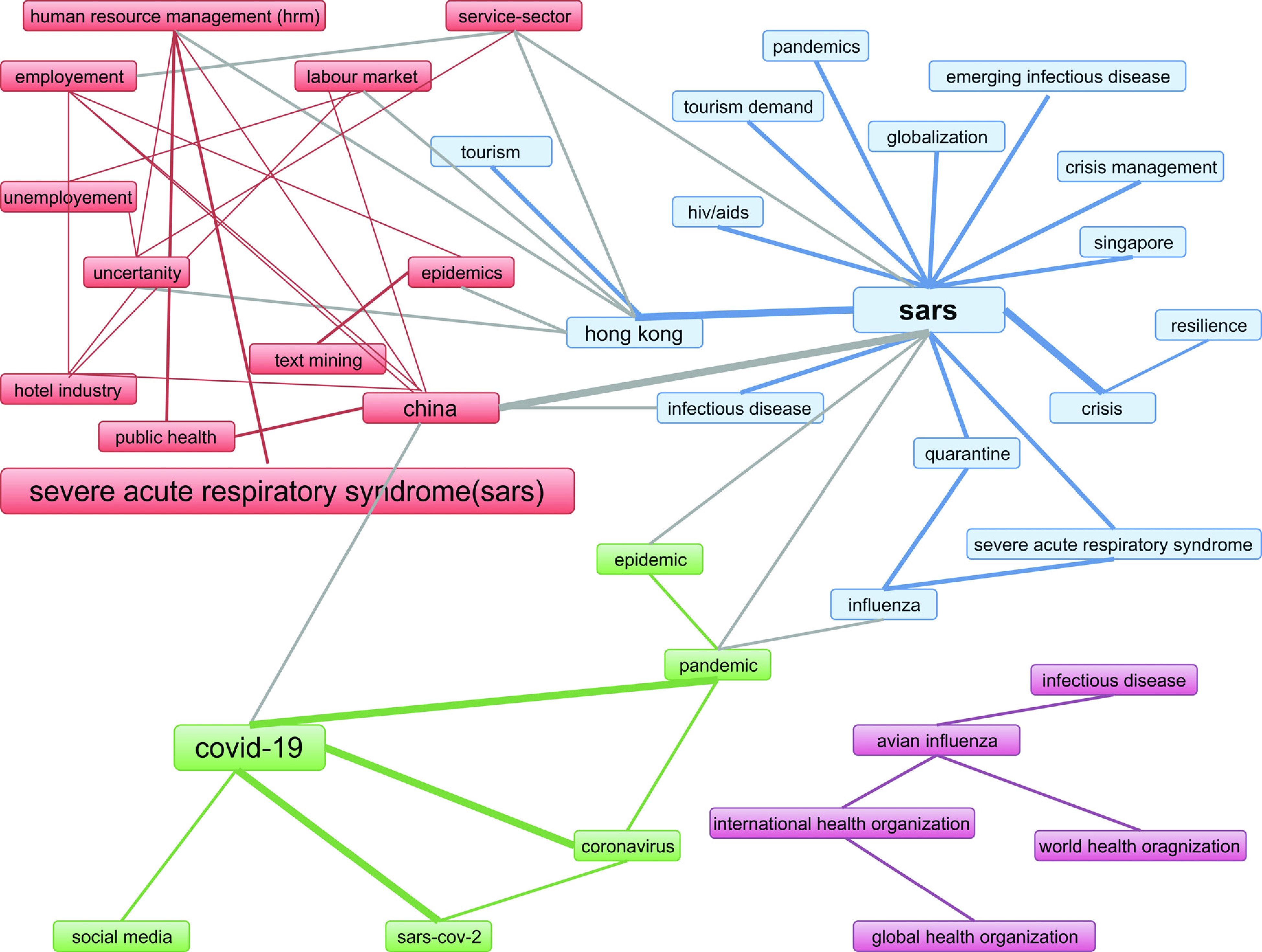
Co-occurrence network.
The red cluster represents the main coronavirus and discusses multiple characteristics of the viral disease. Its epidemic effect on humans and how it outbreaks and communicate from person to person. This research stream is named as ‘social and economic effects of epidemic disease’. The blue cluster represents the research stream of ‘Infectious disease calamities and control’. In this research streams, studies are related to the identification of risk factors from disease outbreaks, health care policy and knowledge about the disease, precautions among people and controlling authorities, preparations to tackle infectious disease, practices, and attitudes of people and government towards contagious disease. The green cluster represents the research stream of the medical solution to contemporary viral disease, i.e., COVID 19. It describes various tests, methodologies, and cures to curb the effect of epidemic disease. It also covers the topics related to the role of social media in communicating and educating the society about novel coronavirus. Purple cluster is the isolated cluster, yet it the important one. It relates to the crucial role of international health organizations in controlling and managing the spread of infectious disease. The purple research stream is titled ‘Infectious disease and the role of international organizations’.
2). Thematic Map
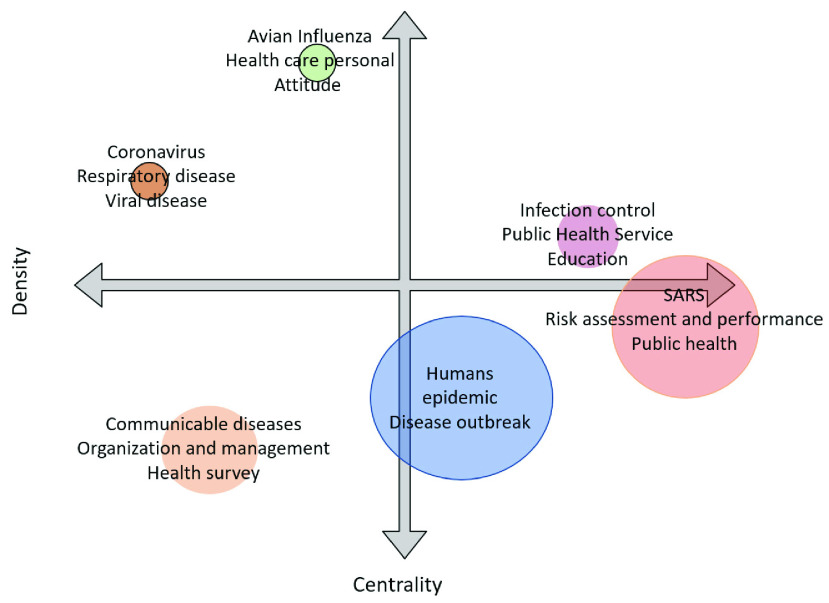
We have detected some research themes now for the superior interpretation of the results. We can categories the identified themes into a strategic diagram to analyze the importance and development of the research theme [52]. Figure 11 represents the thematic map based on density (y-axis) and centrality (x-axis). The centrality measures the importance of the selected theme, and density measures the development of the chosen theme. The graph is divided into four parts. Themes that appear on the lower left part are emerging or declining themes. These are new themes that can emerge to be better or drop from the research area. Themes that come under the lower right part of the thematic map are the basic or transversal themes. These themes represent low density but high centrality. Much research has been done on these themes.
FIGURE 11.
Thematic Map.
The Upper left part represents high density but lower centrality, these themes are highly developed but isolated. The upper right part represents high density and high centrality. The themes in this part are a motor theme, which is developed and essential [53]. The size of the thematic map is to the factors that come under the theme.
Thematic map of figure 11 is constructed based on a full-time span from 2003 to 2020. We have used the top 400 keywords, but items shown in the clusters are set to the minimum frequency of 4 in ‘biblioshiny’ web software. The number of representative labels in each theme is set to 3. This has no link with the literature but represents the subjective judgment of the authors keeping in view the dynamics and best representation of coronavirus literature.
Table 9 is constructed from the clusters shown in figure 11. First cluster is represented by SARS and topics under this cluster are related to risk management and assessment, public health, infectious disease spread and outbreak such as [54]–[60], [24] and [61]. According to the thematic map, these themes come under the basic or transversal themes with high centrality and low density. There is much work in these themes, but it is difficult to find future direction from them because most of the topics are covered. The topics covered in these clusters are related to the Second research theme has some part in emerging themes and many parts in transversal theme. The cluster of the stated theme is represented by humans. Topics related to different characteristics of the virus-host are discussed here. Significant research has been done, and more is required, that is why this theme is converting from emerging to transversal. Research topics under this themes are related to the effect of infectious disease on descriptive of humans such as male, female, adults, old age, middle age, residents, foreigners and travelers such as discussed in [62]–[64], [16], [65], and [66]. This research theme cluster is represented by a communicable disease. It is an emerging theme in coronavirus literature. This theme is indicating the management and organization of communicable diseases with various methodologies [67]–[71] and [72].
Researchers can look this emerging theme from the dimension of communicable disease and public surveillance and role of public health administration [73]–[76], [17] and [18]. Moto themes are highly contributory themes because of high centrality and high density. In coronavirus literature theme with infection control as the representative qualified to be in that part of thematic map. Main dimensions of this theme are public health service, education about infectious disease. Education covers both professional and general public education. Psychological impact of infectious diseases and attitude towards pandemic outbreak. Researchers can understand this theme by going through [77]–[84] and [85].
Themes related to avian influenza is considered as highly developed yet isolated. The density is high, but centrality is low. There is a lot of potential in these themes and researcher can do much impactful work in these themes. Avian influenza is linked with topics related to health care personal, attitude towards pandemic outbreak and acquired immune deficiency syndrome. Theme directions are widely discussed in [86]–[91], [25], [92]–[94] and [95]
The themes represented by coronavirus is also highly developed and isolated. How are these respiratory and viral diseases affecting humans? This theme sees the link between coronavirus, disease outbreak, epidemic, gender and age [96]–[99] and [100]. Finally this theme covers latest computer simulated methods to identify various dynamics of infectious diseases [101]–[103], [42], [104] and [105].
This research stream can be linked with basic themes which are represented by coronavirus and researchers can develop a drug that can be helpful to curb the disease spread. The risk assessment identifies various risk factor involved in the spread of viral diseases. It can be controlled by public feedback. A significant amount of research can be done with public surveys. It can be linked with basic themes and check the risk tolerance, public reactions and preventions with respect to gender, age, and ethnicity. It adds to the body of knowledge and helps in infection control. Infection control is also part of the motor theme. Coronavirus is generated from animals so these themes should be linked with motor and basic themes as well. If research is conducted on emerging themes, then these themes can move to basic or motor themes in future.
3). Thematic Evolution
In addition to the thematic map there is thematic evolution (figure 12), that is showing the historical development of coronavirus literature. Using the keywords plus the thematic evolution depicts the history of themes and how these themes evolved. The thematic evolution is made using ‘biblioshiny’ and with four segments of time. This time segmentation is based on the subjective judgement of the authors keeping in view the better representation of thematic evolution. The first segment is from 1999 to 2010, the second segment is from 2009 to 2015, third is from 2015 to 2019 and last segment is from 2019 to 2020. Themes have evolved with time. As analyzed from 1999 to 2010 the coronavirus literature was about a disease outbreak, epidemic, SARS. From 2011 to 2015 research in SARS got increased and topics related to disease outbreaks evolved into SARS literature. Furthermore, part of epidemic literature evolved into SARS and other parts into effects on humans. Pathogenicity was introduced during the period 2011 to 2015 but evolved into controlled study literature from 2016 to 2019. 3c like protease, was a drug had some success for SARS patients. Studies on the topic were available from 1999 till 2009 but after that it got evolved with other methodologies for protection and disease control.
FIGURE 12.
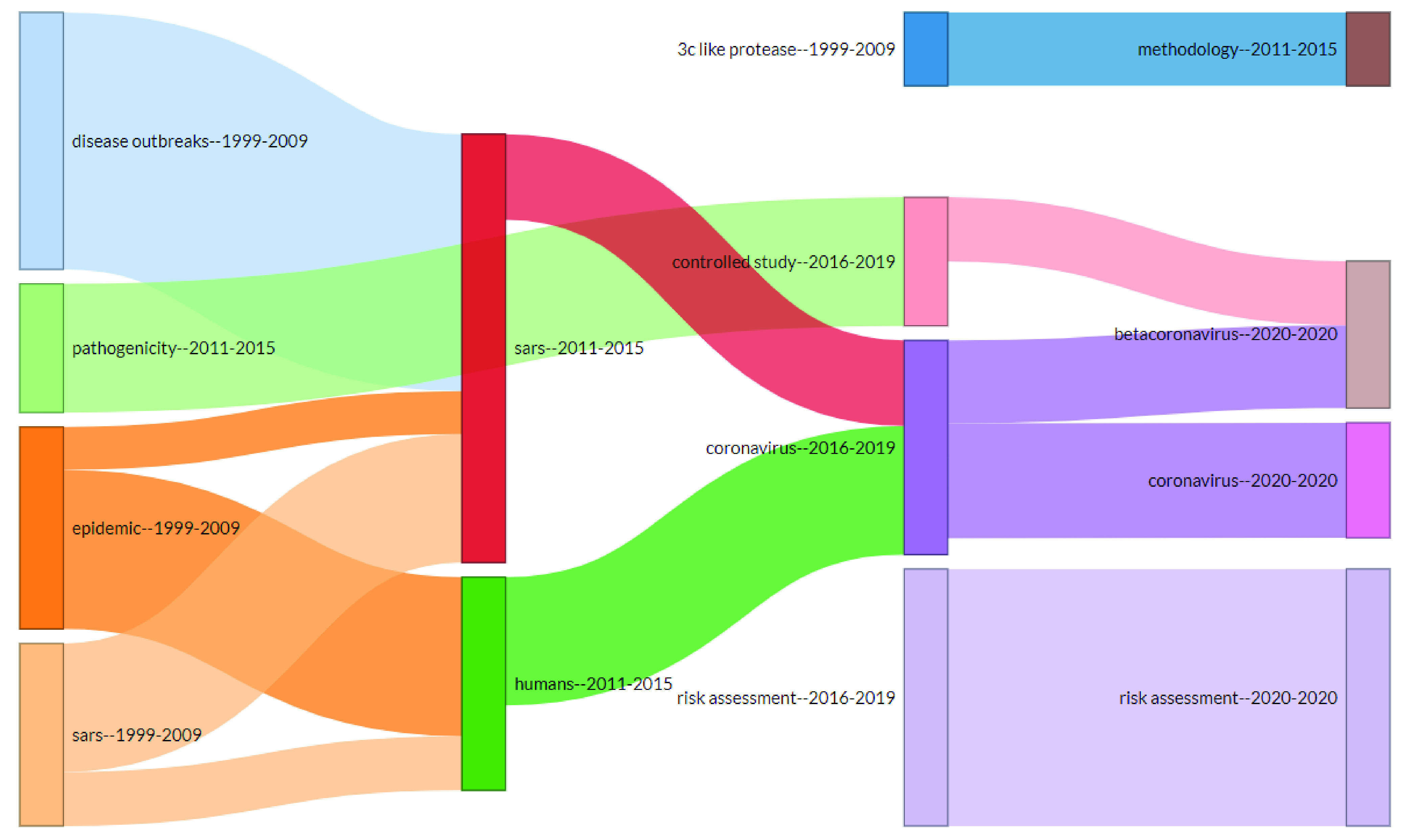
Thematic Evolution.
From 2016 till date topic related to risk assessment are under observation. Part of SARS literature has been used in coronavirus literature and humans’ effect is also studied in coronavirus pandemic literature.
VI. Conclusions
This study has found significant influential aspects of coronavirus literature. These influential aspects provide implication for core future research. The study finds that ‘Morbidity and Mortality Weekly Report’, ‘Social Science and Medicine’ and ‘Health Security’ are top three journals with highest impact in coronavirus literature. There are 23 core journals according to Bradford law. Tablan et al. [21] is the core jounral article with most global citations, who reported the guidelines that are formed to decrease the incidence of pneumonia and other SARS related infections. ‘SARS’ is the word that is most frequently used in titles, author keywords and keywords plus and ‘Health’ in abstract. K.W. Chau and D.C.W. Ho are the authors having the maximum impact according to coronavirus literature. University of Hong Kong is the most relevant affiliation for publishing coronavirus literature. USA has most publications but articles from Hong Kong have most citations. USA is also number one in terms of the corresponding authorship, with correspondence in 64 articles (48 SCP, 16 MCP). Hong Kong and Canada come on second and third. The main collaboration of research is in between the USA and China. The USA also collaborated with Korea, Canada, Taiwan, and Hong Kong.
Conceptual structure from ‘biblioshiny’ R-package has provided key research streams and themes. We have identified four core research streams in coronavirus literature by using co-occurrence network. These research streams are; ‘Social and economic effects of epidemic disease’, ‘Infectious disease calamities and control’, ‘Outbreak of COVID 19’ and ‘Infectious diseases and the role of international organizations’. Combining these research streams will address many issues in the times of pandemic attack.
Furthermore, in conceptual structure, the study has deployed thematic map to put the themes and subthemes on graph and divides them into four parts (dropping or emerging themes, basic themes, highly developed and isolated themes, motor themes). Basic or transversal themes are represented by SARS, risk assessment and management, public health, infectious disease transmission and control and role of world health organization. Moreover, impact of infectious disease on humans and various demographics of humans are also basic themes. Methodologies related to communicable disease and public surveillance; health administrations are emerging themes. Public health services and education for infection control and psychological impact on behaviors and attitudes created by infectious diseases are motor themes. Highly developed but isolated themes of corona literature are topics related to Avian influenza.
A. Future Agendas
As we have reviewed the coronavirus literature thoroughly by looking at various influential aspects and conceptual framework. We can set forth some directions for researchers, doctors, policy makers to investigate the right aspects for answers of alarming issues.
-
1)
Overall limited studies are there on coronavirus outbreak in social sciences. More research is required.
-
2)
Availability of funds for core journals such as the sources found under zone 1 by using Bradford law can create quality future research.
-
3)
Collaboration with core authors, affiliations, and understanding the globally cited articles will create quality future research.
-
4)
According to the influential structure USA and Hong Kong are the coronavirus research hub in social sciences. These two research hubs should collaborate with health and research departments of underdeveloped countries where COVID-19 effects are limited. They should study these countries social habits and vaccine routines. ‘
-
5)
Very limited collaboration among countries has been observed. More collaboration for infectious disease policy and control is required in social sciences fields.
The conceptual framework has cleared some themes for research directions. These directions can be explored by using the following points
-
6)
In the co-occurrence network there are various themes identified with various colors red cluster is the basic cluster relating to public health, uncertainty, epidemic and economy. On the other hand, publications of purple cluster are related to infectious disease and role of international organizations. The link between a red cluster and purple cluster can create strategies for international health organizations to curb the spread of infectious disease and suggest economic development plan under pandemic situations. Similarly, red cluster publications can be linked with blue to identify and study risk factors that are responsible for disease spread. Blue cluster with green can generate studies to identify resilience strategies and crisis management from SARS and MERS related studies and apply them to outbreak of COVID 19.
-
7)
Methodologies and management of Communicable diseases are the emerging theme. Future research is required in this research field.
-
8)
SARS is the old virus in the family of coronaviruses, but the findings related to SARS can be used to identify remedies for novel coronavirus.
-
9)
For theme identification we have used keyword plus. There should be a software that can take essential terms from all sources such as author’s keywords, keywords plus, abstract and title and produce the final form of keywords for the conceptual framework. Studies for such software methodology are required
B. Limitations of the Study
The main limitation of the study is that there is very limited literature available on coronavirus in social science, economics and business field. More research is required to tackle the needs of the economy in a pandemic situation. Furthermore, Due to the limited number of author’s keywords, this study only used keywords plus for development of various themes.
Biographies

Adeel Nasir received the M.Phil. degree in commerce from the University of Central Punjab, and the Ph.D. degree in management sciences from COMSATS University Islamabad, Lahore Campus. He is currently working as an Assistant Professor in tenor track system with the Lahore College for Women University. He has eight years of teaching and research experience. His research interest includes integration of financial practices with computer programing languages, financial markets, management sciences, and bibliometric analysis. He has published 13 research articles that are published in reputable local and international journals. He has presented his research at four international conferences.

Kamran Shaukat received the M.Sc. degree in computer science from Mohammad Ali Jinnah University, Pakistan. He is currently pursuing the Ph.D. degree with The University of Newcastle, Callaghan, NSW, Australia. He is author of many articles in the area of machine learning, databases, and cyber security. He has served the University of the Punjab, Pakistan, for seven years, as a Lecturer. He has served as a Reviewer to many journals, including IEEE Access. He has attended several international conferences, including USA, U.K., Thailand, Turkey, and Pakistan. He received the Gold Medal for his M.Sc. degree.

Ibrahim A. Hameed (Senior Member, IEEE) is currently a Professor and the Deputy Head of Research and Innovation, the Head of the International Master Program in Simulation and Visualization, Faculty of Information Technology and Electrical Engineering, Norwegian University of Science and Technology, Trondheim, Norway, where he has been an Associate Professor with the Department of ICT and Natural Sciences, since 2015.

Suhuai Luo received the bachelor’s and master’s degrees from the Nanjing University of Posts and Telecommunications and the Ph.D. degree from the University of Sydney, all in electrical engineering. His main research interests include image processing, computer vision, machine learning, cyber security, and media data mining. He has lectured and developed curricula for courses in computer science, electrical engineering, and information engineering.

Talha Mahboob Alam received the bachelor’s degree in software engineering from the University of Management and Technology (UMT), Lahore, in 2017, and the master’s degree in computer science from the University of Engineering and Technology (UET), Lahore. He is currently a Researcher. He has several publications in international journals and conferences, including IEEE Access and The Computer Journal. His research interests include data science, data mining, knowledge discovery in databases, bioinformatics, big data, information retrieval, and AI.

Farhat Iqbal received the B.Sc. degree (Hons.) in computer science from the University of the Punjab, Lahore, Pakistan. She has attended many national and international research conferences, including ECTI-CON 2020, Thailand. She has won Full Merit Scholarship, while she was completing her college studies. She has also received merit scholarships during her study at the University of the Punjab. She is currently an Active Researcher. She had published papers in leading conferences and journals. Her current area of research is big data, artificial intelligence, data mining, and cyber security.
Funding Statement
This work was supported by the Norwegian University of Science and Technology, Norway.
Contributor Information
Kamran Shaukat, Email: kamran.shaukat@uon.edu.au.
Ibrahim A. Hameed, Email: ibib@ntnu.no.
References
- [1].WHO. Coronavirus (COVID-19). Accessed: Jun. 23, 2020. [Online]. Available: https://who.sprinklr.com/
- [2].Torsello M. and Winkler M. M., “Coronavirus-infected international business transactions: A preliminary diagnosis,” Eur. J. Risk Regulation, vol. 11, no. , pp. 396–401, 2020, doi: 10.1017/err.2020.30. [DOI] [Google Scholar]
- [3].Ellegaard O. and Wallin J. A., “The bibliometric analysis of scholarly production: How great is the impact?” Scientometrics, vol. 105, no. 3, pp. 1809–1831, Dec. 2015, doi: 10.1007/s11192-015-1645-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Zupic I. and T. Čater, “Bibliometric methods in management and organization,” Organizational Res. Methods, vol. 18, no. 3, pp. 429–472, Jul. 2015, doi: 10.1177/1094428114562629. [DOI] [Google Scholar]
- [5].Wardikar V., “Application of Bradford’s law of scattering to the literature of library & information science: A study of Doctoral theses citations submitted to the universities of Maharashtra, India,” Library Philosophy Pract., vol. 2013, no. 12, p. 44, Dec. 2013. [Google Scholar]
- [6].Li H., An H., Wang Y., Huang J., and Gao X., “Evolutionary features of academic articles co-keyword network and keywords co-occurrence network: Based on two-mode affiliation network,” Phys. A, Stat. Mech. Appl., vol. 450, pp. 657–669, May 2016. [Google Scholar]
- [7].Tripathi M., Kumar S., Sonker S. K., and Babbar P., “Occurrence of author keywords and keywords plus in social sciences and humanities research: A preliminary study,” COLLNET J. Scientometrics Inf. Manage., vol. 12, no. 2, pp. 215–232, Jul. 2018, doi: 10.1080/09737766.2018.1436951. [DOI] [Google Scholar]
- [8].Andrés A., Measuring Academic Research: How to Undertake a Bibliometric Study. Colchester, U.K.: Chandos Publishing, 2009. [Google Scholar]
- [9].Moral-Muñoz J. A., Herrera-Viedma E., Santisteban-Espejo A., and Cobo M. J., “Software tools for conducting bibliometric analysis in science: An up-to-date review,” El Profesional de la Información, vol. 29, no. 1, Jan. 2020, doi: 10.3145/epi.2020.ene.03. [DOI] [Google Scholar]
- [10].WHO |SARS (Severe Acute Respiratory Syndrome). Accessed: Apr. 11, 2020. [Online]. Available: https://www.who.int/ith/diseases/sars/en/
- [11].Ng Y., Li Z., Chua Y. X., Chaw W. L., Zhao Z., Er B., and Pung R., “Evaluation of the effectiveness of surveillance and containment measures for the first 100 patients with COVID-19 in Singapore–January 2–February 29, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 11, pp. 1–5, Mar. 2020, doi: 10.15585/mmwr.mm6911e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Burke R. M., “Active monitoring of persons exposed to patients with confirmed COVID-19—United States, January–February 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 9, pp. 245–246, Mar. 2020, doi: 10.15585/mmwr.mm6909e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Jernigan D. B., “Update: Public health response to the coronavirus disease 2019 outbreak—United States, February 24, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 8, pp. 216–219, Feb. 2020, doi: 10.15585/mmwr.mm6908e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bajema K. L., Oster A. M., and McGovern O. L., “Persons evaluated for 2019 novel coronavirus—United States, January 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 6, pp. 166–170, Feb. 2020, doi: 10.15585/mmwr.mm6906e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Foote M. M. K., Styles T. S., and Quinn C. L., “Assessment of hospital emergency department response to potentially infectious diseases using unannounced mystery patient drills—New York City, 2016,” MMWR. Morbidity Mortality Weekly Rep., vol. 66, no. 36, pp. 945–949, 2017, doi: 10.15585/mmwr.mm6636a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Balkhy H. H., “Notes from the field: Nosocomial outbreak of Middle East respiratory syndrome in a large tertiary care hospital—Riyadh, Saudi Arabia, 2015,” MMWR. Morbidity Mortality Weekly Rep., vol. 65, no. 6, pp. 163–164, Feb. 2016, doi: 10.15585/mmwr.mm6506a5. [DOI] [PubMed] [Google Scholar]
- [17].Rha B., Rudd J., Feikin D., and Watson J., “Update on the epidemiology of Middle East respiratory syndrome coronavirus (MERS-CoV) infection, and guidance for the public, clinicians, and public health authorities—January 2015,” MMWR. Morbidity Mortality Weekly Rep., vol. 64, no. 3, pp. 61–62, 2015. [PMC free article] [PubMed] [Google Scholar]
- [18].Bialek S. R., “First confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection in the United States, updated information on the epidemiology of MERS-CoV infection, and guidance for the public, clinicians, and public health authorities–May 2020,” MMWR. Morbidity Mortality Weekly Rep., no. 19, pp. 431–436, May 2014. [PMC free article] [PubMed]
- [19].Rha B., “Update: Severe respiratory illness associated with a novel coronavirus—Worldwide, 2012-2013,” MMWR. Morbidity Mortality Weekly Rep., vol. 62, no. 10, pp. 194–195, Mar. 2013. [PMC free article] [PubMed] [Google Scholar]
- [20].Royston P., “Lowess smoothing,” Stata Tech. Bull., vol. 1, no. 3, pp. 1–28, 1992. [Google Scholar]
- [21].Tablan O. C., Anderson L. J., Besser R., Bridges C., and Hajjeh R., “Guidelines for preventing health-care-associated pneumonia, 2003 recommendations of the CDC and the healthcare infection control practices advisory committee,” MMWR. Recomm. Rep., vol. 53, no. RR-3, pp. 1–36, 2004. [PubMed] [Google Scholar]
- [22].Ng E., “Policies and technical guidelines for urban planning of high-density cities–air ventilation assessment (AVA) of Hong Kong,” Building Environ., vol. 44, no. 7, pp. 1478–1488, 2009, doi: 10.1016/j.buildenv.2008.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Qureshi K., “Health care Workers’ ability and willingness to report to duty during catastrophic disasters,” J. Urban Health: Bull. New York Acad. Med., vol. 82, no. 3, pp. 378–388, Jul. 2005, doi: 10.1093/jurban/jti086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Smith R. D., “Responding to global infectious disease outbreaks: Lessons from SARS on the role of risk perception, communication and management,” Social Sci. Med., vol. 63, no. 12, pp. 3113–3123, Dec. 2006, doi: 10.1016/j.socscimed.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Rittichainuwat B. N. and Chakraborty G., “Perceived travel risks regarding terrorism and disease: The case of thailand,” Tourism Manage., vol. 30, no. 3, pp. 410–418, Jun. 2009, doi: 10.1016/j.tourman.2008.08.001. [DOI] [Google Scholar]
- [26].van Aalst J., “Distinguishing knowledge-sharing, knowledge-construction, and knowledge-creation discourses,” Int. J. Comput.-Supported Collaborative Learn., vol. 4, no. 3, pp. 259–287, Sep. 2009, doi: 10.1007/s11412-009-9069-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Wallis P. and Nerlich B., “Disease metaphors in new epidemics: The UK media framing of the 2003 SARS epidemic,” Social Sci. Med., vol. 60, no. 11, pp. 2629–2639, Jun. 2005, doi: 10.1016/j.socscimed.2004.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Wang Y.-S., “The impact of crisis events and macroeconomic activity on Taiwan’s international inbound tourism demand,” Tourism Manage., vol. 30, no. 1, pp. 75–82, Feb. 2009, doi: 10.1016/j.tourman.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Washer P., “Representations of SARS in the british newspapers,” Social Sci. Med., vol. 59, no. 12, pp. 2561–2571, Dec. 2004, doi: 10.1016/j.socscimed.2004.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Gao N. P., Niu J. L., Perino M., and Heiselberg P., “The airborne transmission of infection between flats in high-rise residential buildings: Particle simulation,” Building Environ., vol. 44, no. 2, pp. 402–410, Feb. 2009, doi: 10.1016/j.buildenv.2008.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Lau S. K. P., Woo P. C. Y., Yip C. C. Y., Fan R. Y. Y., Huang Y., Wang M., Guo R., Lam C. S. F., Tsang A. K. L., Lai K. K. Y., Chan K.-H., Che X.-Y., Zheng B.-J., and Yuen K.-Y., “Isolation and characterization of a novel betacoronavirus subgroup a coronavirus, rabbit coronavirus HKU14, from domestic rabbits,” J. Virol., vol. 86, no. 10, pp. 5481–5496, May 2012, doi: 10.1128/JVI.06927-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Wong S.-K., Wai-Chung Lai L., Ho D. C.-W., Chau K.-W., Lo-Kuen Lam C., and Hung-Fai Ng C., “Sick building syndrome and perceived indoor environmental quality: A survey of apartment buildings in Hong Kong,” Habitat Int., vol. 33, no. 4, pp. 463–471, Oct. 2009, doi: 10.1016/j.habitatint.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Lai L. W. C., Chau K. W., Ho D. C. W., and Lin V. Y. Y., “Impact of political incidents, financial crises, and severe acute respiratory syndrome on Hong Kong property buyers,” Environ. Planning B: Planning Des., vol. 33, no. 3, pp. 413–433, Jun. 2006, doi: 10.1068/b31125a. [DOI] [Google Scholar]
- [34].Lai L. W. C., Chau K. W., Ho D. C. W., and Lin V. Y. Y., “Impact of political incidents, financial crises, and severe acute respiratory syndrome on Hong Kong regulators and developers,” Environ. Planning B: Planning Des., vol. 33, no. 4, pp. 503–522, Aug. 2006, doi: 10.1068/b31125b. [DOI] [Google Scholar]
- [35].Lee S., Chan L. Y. Y., Chau A. M. Y., Kwok K. P. S., and Kleinman A., “The experience of SARS-related stigma at amoy gardens,” Social Sci. Med., vol. 61, no. 9, pp. 2038–2046, Nov. 2005, doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Salehi R. and Ali S. H., “The social and political context of disease outbreaks: The case of SARS in toronto,” Can. Public Policy, vol. 32, no. 4, pp. 373–385, Dec. 2006, doi: 10.3138/G276-2087-2838-R510. [DOI] [Google Scholar]
- [37].Ali S. H., Keil R., Major C., and van Wagner E., “Pandemics, place, and planning: Learning from SARS,” Plan Canada, vol. 46, no. 3, pp. 34–36, 2006. [Google Scholar]
- [38].Ali S. H. and Keil R., “Global cities and the spread of infectious disease: The case of severe acute respiratory syndrome (SARS) in Toronto, Canada,” Urban Stud., vol. 43, no. 3, pp. 491–509, Mar. 2006, doi: 10.1080/00420980500452458. [DOI] [Google Scholar]
- [39].Sanford S. and Ali S. H., “The new public health hegemony: Response to severe acute respiratory syndrome (SARS) in Toronto,” Social Theory Health, vol. 3, no. 2, pp. 105–125, May 2005, doi: 10.1057/palgrave.sth.8700048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Huang Y., “Neoliberalizing food safety control: Training licensed fish veterinarians to combat aquaculture drug residues in Guangdong,” Mod. China, vol. 42, no. 5, pp. 535–565, Sep. 2016, doi: 10.1177/0097700415605322. [DOI] [Google Scholar]
- [41].Bian L., Huang Y., Mao L., Lim E., Lee G., Yang Y., Cohen M., and Wilson D., “Modeling individual vulnerability to communicable diseases: A framework and design,” Ann. Assoc. Amer. Geographers, vol. 102, no. 5, pp. 1016–1025, Sep. 2012, doi: 10.1080/00045608.2012.674844. [DOI] [Google Scholar]
- [42].Zhao B., Zhang Z., and Li X., “Numerical study of the transport of droplets or particles generated by respiratory system indoors,” Building Environ., vol. 40, no. 8, pp. 1032–1039, Aug. 2005, doi: 10.1016/j.buildenv.2004.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Keogh-Brown M. R., Smith R. D., Edmunds J. W., and Beutels P., “The macroeconomic impact of pandemic influenza: Estimates from models of the United Kingdom, France, Belgium and The Netherlands,” Eur. J. Health Econ., vol. 11, no. 6, pp. 543–554, Dec. 2010, doi: 10.1007/s10198-009-0210-1. [DOI] [PubMed] [Google Scholar]
- [44].Research Highlights–Research–HKU. Accessed: May 24, 2020. [Online]. Available: https://www.hku.hk/research/video/
- [45].About U of T |University of Toronto. Accessed: May 24, 2020. [Online]. Available: https://www.utoronto.ca/about-u-of-t
- [46].Immunization and Respiratory Diseases (NCIRD) Home |CDC. Accessed: Apr. 16, 2020. [Online]. Available: https://www.cdc.gov/ncird/
- [47].About PolyU |The Hong Kong Polytechnic University. Accessed: May 24, 2020. [Online]. Available: https://www.polyu.edu.hk/about-polyu/
- [48].About York University–About York University. Accessed: May 24, 2020. [Online]. Available: https://about.yorku.ca/
- [49].Introducing CUHK |About CUHK |CUHK. Accessed: May 24, 2020. [Online]. Available: https://www.cuhk.edu.hk/english/aboutus/university-intro.html
- [50].Coronavirus COVID-19 Facts & Resources |Mount Sinai–New York. Accessed: May 24, 2020. [Online]. Available: https://www.mountsinai.org/about/covid19
- [51].About the Center for Global Health (CGH)–Centers for Disease Control (CDC). Accessed: Apr. 16, 2020. [Online]. Available: https://www.cdc.gov/globalhealth/resources/reports/annual/2017/about-center-for-global-health.html
- [52].Cobo M. J., López-Herrera A. G., Herrera-Viedma E., and Herrera F., “Science mapping software tools: Review, analysis, and cooperative study among tools,” J. Amer. Soc. Inf. Sci. Technol., vol. 62, no. 7, pp. 1382–1402, Jul. 2011, doi: 10.1002/asi.21525. [DOI] [Google Scholar]
- [53].Biblioshiny–Bibliometrix for no Coders. Accessed: Apr. 16, 2020. [Online]. Available: https://bibliometrix.org/biblioshiny/
- [54].Jang K. and Park N., “The effects of repetitive information communication through multiple channels on prevention behavior during the 2015 MERS outbreak in South Korea,” J. Health Commun., vol. 23, no. 7, pp. 670–678, Jul. 2018, doi: 10.1080/10810730.2018.1501440. [DOI] [PubMed] [Google Scholar]
- [55].Kim I.-H., Feng C.-C., Wang Y.-C., Spitzberg B. H., and Tsou M.-H., “Exploratory spatiotemporal analysis in risk communication during the MERS outbreak in South Korea,” Prof. Geographer, vol. 69, no. 4, pp. 629–643, Oct. 2017, doi: 10.1080/00330124.2017.1288577. [DOI] [Google Scholar]
- [56].Bernard L., Bernard A., Biron A., and Lavoie-Tremblay M., “Exploring Canadians’ and Europeans’ health care professionals’ perception of biological risks, patient safety, and professionals’ safety practices,” Health Care Manager, vol. 36, no. 2, pp. 129–139, 2017, doi: 10.1097/HCM.0000000000000152. [DOI] [PubMed] [Google Scholar]
- [57].Ding H., “Transnational quarantine rhetorics: Public mobilization in SARS and in H1N1 flu,” J. Med. Humanities, vol. 35, no. 2, pp. 191–210, Jun. 2014, doi: 10.1007/s10912-014-9282-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Lai P.-C., Kwong K.-H., and Wong H.-T., “Spatio-temporal and stochastic modelling of severe acute respiratory syndrome,” Geospatial Health, vol. 8, no. 1, pp. 183–192, 2013, doi: 10.4081/gh.2013.65. [DOI] [PubMed] [Google Scholar]
- [59].de Boer J. C., Lok A., van’t Verlaat E., Duivenvoorden H. J., Bakker A. B., and Smit B. J., “Work-related critical incidents in hospital-based health care providers and the risk of post-traumatic stress symptoms, anxiety, and depression: A meta-analysis,” Social Sci. Med., vol. 73, no. 2, pp. 316–326, Jul. 2011, doi: 10.1016/j.socscimed.2011.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Eichelberger L., “SARS and New York’s Chinatown: The politics of risk and blame during an epidemic of fear,” Social Sci. Med., vol. 65, no. 6, pp. 1284–1295, Sep. 2007, doi: 10.1016/j.socscimed.2007.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].McInnes K. and Safian L., “Keeping SARS out: An education program for SARS screeners in one ontario hospital,” J. Nurses Staff Develop. (JNSD), vol. 21, no. 2, pp. 73–78, Mar. 2005, doi: 10.1097/00124645-200503000-00008. [DOI] [PubMed] [Google Scholar]
- [62].Elcin M., Onan A., Odabasi O., Saylam M., Ilhan H., Daylan Kockaya P., Gurcuoglu I., Uckuyu Y., Cengiz D., and Nacar O. A., “Developing a simulation-based training program for the prehospital professionals and students on the management of middle east respiratory syndrome,” Simul. Healthcare: J. Soc. Simul. Healthcare, vol. 11, no. 6, pp. 394–403, Dec. 2016, doi: 10.1097/SIH.0000000000000198. [DOI] [PubMed] [Google Scholar]
- [63].Park H.-J. and Lee B. J., “The role of social work for foreign residents in an epidemic: The MERS crisis in the republic of Korea,” Social Work Public Health, vol. 31, no. 7, pp. 656–664, Nov. 2016, doi: 10.1080/19371918.2016.1160352. [DOI] [PubMed] [Google Scholar]
- [64].Cao W., Zhang X., Xu K., and Wang Y., “Modeling online health information-seeking behavior in China: The roles of source characteristics, reward assessment, and Internet self-efficacy,” Health Commun., vol. 31, no. 9, pp. 1105–1114, Sep. 2016, doi: 10.1080/10410236.2015.1045236. [DOI] [PubMed] [Google Scholar]
- [65].Hoda J., “Identification of information types and sources by the public for promoting awareness of Middle East respiratory syndrome coronavirus in Saudi Arabia,” Health Educ. Res., vol. 31, no. 1, pp. 12–23, Feb. 2016, doi: 10.1093/her/cyv061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Matthews Pillemer F., Blendon R. J., Zaslavsky A. M., and Lee B. Y., “Predicting support for non-pharmaceutical interventions during infectious outbreaks: A four region analysis,” Disasters, vol. 39, no. 1, pp. 125–145, Jan. 2015, doi: 10.1111/disa.12089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Idubor O. I., “Improving detection and response to respiratory events—Kenya, April 2016–April 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 18, pp. 540–544, 2020, doi: 10.15585/mmwr.mm6918a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Wang X., Zhang X., and He J., “Challenges to the system of reserve medical for public health emergencies: Reflections on the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic in China,” Biosci. Trends, vol. 14, no. 1, pp. 3–8, Feb. 2020, doi: 10.5582/bst.2020.01043. [DOI] [PubMed] [Google Scholar]
- [69].Therrien M.-C., Normandin J.-M., and Denis J.-L., “Bridging complexity theory and resilience to develop surge capacity in health systems,” J. Health Org. Manage., vol. 31, no. 1, pp. 96–109, Mar. 2017, doi: 10.1108/JHOM-04-2016-0067. [DOI] [PubMed] [Google Scholar]
- [70].Al Shehri A. M., “A lesson learned from middle east respiratory syndrome (MERS) in saudi arabia,” Med. Teacher, vol. 37, no. 1, pp. S88–S93, Mar. 2015, doi: 10.3109/0142159X.2015.1006610. [DOI] [PubMed] [Google Scholar]
- [71].C. F. D. Control, P. (CDC), D. O. Health, and H. S. (HHS), “Possession, use, and transfer of select agents and toxins; biennial review. Final rule,” Fed. Regist., vol. 77, no. 194, p. 61083, Oct. 2012. [PubMed] [Google Scholar]
- [72].Rubin G. J. and Dickmann P., “How to reduce the impact of ‘low-risk patients’ following a bioterrorist incident: Lessons from SARS, anthrax, and pneumonic plague,” Biosecur. Bioterrorism: Biodefense Strategy, Pract., Sci., vol. 8, no. 1, pp. 37–43, 2010, doi: 10.1089/bsp.2009.0059. [DOI] [PubMed] [Google Scholar]
- [73].Jacobs L. and Potter P. B., “Selective adaptation and human rights to health in China,” Health Hum. Rights, vol. 9, no. 2, pp. 112–134, 2006, doi: 10.2307/4065404. [DOI] [PubMed] [Google Scholar]
- [74].Zapp R., Krajden M., and Lynch T., “SARS: A quality management test of our public health safety net,” Qual. Manage. Health Care, vol. 13, no. 2, pp. 120–129, Mar. 2004, doi: 10.1097/00019514-200404000-00004. [DOI] [PubMed] [Google Scholar]
- [75].Foldy S. L., Barthell E., Silva J., and Biedrzycki P., “SARS Surveillance Project—Internet-enabled multiregion surveillance for rapidly emerging disease,” MMWR. Morbidity Mortality Weekly Rep., vol. 53, Suppl, pp. 215–220, 2004. [PubMed] [Google Scholar]
- [76].Steiner-Sichel L., Greenko J., Heffernan R., Layton M., and Weiss D., “Field investigations of emergency department syndromic surveillance signals—New York City,” MMWR. Morbidity Mortality Weekly Rep., vol. 53, Suppl, pp. 184–189, 2004. [PubMed] [Google Scholar]
- [77].Attenborough F. T., “‘To Rid oneself of the uninvited guest’: Robert Koch, Sergei Winogradsky and competing styles of practice in medical microbiology,” J. Historical Sociol., vol. 25, no. 1, pp. 50–82, 2012, doi: 10.1111/j.1467-6443.2011.01407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Mason K. A., “Mobile migrants, mobile germs: Migration, contagion, and boundary-building in Shenzhen, China after SARS,” Med. Anthropol., vol. 31, no. 2, pp. 113–131, Mar. 2012, doi: 10.1080/01459740.2011.610845. [DOI] [PubMed] [Google Scholar]
- [79].Aiello A., Khayeri M. Y.-E., Raja S., Peladeau N., Romano D., Leszcz M., Maunder R. G., Rose M., Adam M. A., Pain C., Moore A., Savage D., and Schulman R. B., “Resilience training for hospital workers in anticipation of an influenza pandemic,” J. Continuing Edu. Health Professions, vol. 31, no. 1, pp. 15–20, 2011, doi: 10.1002/chp.20096. [DOI] [PubMed] [Google Scholar]
- [80].Beard A., “Forced to shut down,” Harvard Bus. Rev., vol. 89, no. 5, pp. 132–134, 2011. [PubMed] [Google Scholar]
- [81].Cheung C.-K. and Tse J. W.-L., “Institutional trust as a determinant of anxiety during the SARS crisis in Hong Kong,” Social Work Public Health, vol. 23, no. 5, pp. 41–54, Jun. 2008, doi: 10.1080/19371910802053224. [DOI] [PubMed] [Google Scholar]
- [82].Chang K.-H., Gotcher D. F., and Chan M.-Y., “Does social capital matter when medical professionals encounter the SARS crisis in a hospital setting,” Health Care Manage. Rev., vol. 31, no. 1, pp. 26–33, Jan. 2006, doi: 10.1097/00004010-200601000-00005. [DOI] [PubMed] [Google Scholar]
- [83].Tang C. S.-K. and Wong C.-Y., “Psychosocial factors influencing the practice of preventive behaviors against the severe acute respiratory syndrome among older Chinese in Hong Kong,” J. Aging Health, vol. 17, no. 4, pp. 490–506, Aug. 2005, doi: 10.1177/0898264305277966. [DOI] [PubMed] [Google Scholar]
- [84].DiGiovanni C., Conley J., Chiu D., and Zaborski J., “Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak,” Biosecur. Bioterrorism: Biodefense Strategy, Pract., Sci., vol. 2, no. 4, pp. 265–272, 2004, doi: 10.1089/bsp.2004.2.265. [DOI] [PubMed] [Google Scholar]
- [85].Chandler C., “Hong Kong, city of fear,” Fortune, vol. 147, no. 7, p. 55, 2003. [PubMed] [Google Scholar]
- [86].Schaffer A. M. and Burton K. R., “Evaluation of state plans and the livestock emergency response plan (LERP),” Health Secur., vol. 15, no. 6, pp. 611–619, Dec. 2017, doi: 10.1089/hs.2017.0018. [DOI] [PubMed] [Google Scholar]
- [87].Christian K. A., Iuliano A. D., Uyeki T. M., and Mintz E. D., “What we are watching–top global infectious disease threats, 2013-2016: An update from CDC’s global disease detection operations center,” Health Secur., vol. 15, no. 5, pp. 453–462, Sep. 2017, doi: 10.1089/hs.2017.0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Neely A. H. and Nading A. M., “Global health from the outside: The promise of place-based research,” Health Place, vol. 45, pp. 55–63, May 2017, doi: 10.1016/j.healthplace.2017.03.001. [DOI] [PubMed] [Google Scholar]
- [89].Davies S. E., “The international politics of disease reporting: Towards post-Westphalianism?” Int. Politics, vol. 49, no. 5, pp. 591–613, 2012, doi: 10.1057/ip.2012.19. [DOI] [Google Scholar]
- [90].Lim T., Cho J., and Kim B. S., “Predictions and measurements of the stack effect on indoor airborne virus transmission in a high-rise hospital building,” Building Environ., vol. 46, no. 12, pp. 2413–2424, Dec. 2011, doi: 10.1016/j.buildenv.2011.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Lee C.-C. and Chen C.-J., “The reaction of elderly asian tourists to avian influenza and SARS,” Tourism Manage., vol. 32, no. 6, pp. 1421–1422, Dec. 2011, doi: 10.1016/j.tourman.2010.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Gao S., Mioc D., Yi X., Anton F., Oldfield E., and Coleman D. J., “The Canadian geospatial data infrastructure and health mapping,” Cybergeo, vol. 69, no. 9, pp. 245–246, Mar. 2020. [Google Scholar]
- [93].Kuo H.-I., Chen C.-C., Tseng W.-C., Ju L.-F., and Huang B.-W., “Assessing impacts of SARS and avian flu on international tourism demand to Asia,” Tourism Manage., vol. 29, no. 5, pp. 917–928, Oct. 2008, doi: 10.1016/j.tourman.2007.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Blum J., Carstens P., and Talib N., “Government public health policy: Three cautionary tales from Malaysia, South Africa and the United States,” Med. Law, vol. 26, no. 4, pp. 615–642, 2007. [PubMed] [Google Scholar]
- [95].Aginam O., “Globalization of health insecurity: The World Health Organization and the new International Health Regulations,” Med. Law, vol. 25, no. 4, pp. 663–672, 2006. [PubMed] [Google Scholar]
- [96].Jribi S., Ben Ismail H., Doggui D., and Debbabi H., “COVID-19 virus outbreak lockdown: What impacts on household food wastage?” Environ., Develop. Sustainability, vol. 22, no. 5, pp. 3939–3955, Jun. 2020, doi: 10.1007/s10668-020-00740-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Desjardins M. R., Hohl A., and Delmelle E. M., “Rapid surveillance of COVID-19 in the united states using a prospective space-time scan statistic: Detecting and evaluating emerging clusters,” Appl. Geography, vol. 118, May 2020, Art. no.102202, doi: 10.1016/j.apgeog.2020.102202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Baird B. and Millar E., “Abortion at the edges: Politics, practices, performances,” Women’s Stud. Int. Forum, vol. 80, May 2020, Art. no.102372, doi: 10.1016/j.wsif.2020.102372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Evenett S. J., “Sicken thy neighbour: The initial trade policy response to COVID-19,” World Economy, vol. 43, no. 4, pp. 828–839, 2020, doi: 10.1111/twec.12954. [DOI] [Google Scholar]
- [100].Pirouz B., Shaffiee Haghshenas S., Shaffiee Haghshenas S., and Piro P., “Investigating a serious challenge in the sustainable development process: Analysis of confirmed cases of COVID-19 (New type of Coronavirus) through a binary classification using artificial intelligence and regression analysis,” Sustainability, vol. 12, no. 6, p. 2427, Mar. 2020, doi: 10.3390/su12062427. [DOI] [Google Scholar]
- [101].Bifolchi N., Deardon R., and Feng Z., “Spatial approximations of network-based individual level infectious disease models,” Spatial Spatio-Temporal Epidemiol., vol. 6, pp. 59–70, Sep. 2013, doi: 10.1016/j.sste.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Mao C.-K., Ding C. G., and Lee H.-Y., “Post-SARS tourist arrival recovery patterns: An analysis based on a catastrophe theory,” Tourism Manage., vol. 31, no. 6, pp. 855–861, Dec. 2010, doi: 10.1016/j.tourman.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Gao N. and Niu J., “Transient CFD simulation of the respiration process and inter-person exposure assessment,” Building Environ., vol. 41, no. 9, pp. 1214–1222, Sep. 2006, doi: 10.1016/j.buildenv.2005.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Liu Z., Huang C., Fan K., Wei P., Chen H., Liu S., Pei J., Shi L., Li B., Yang K., Liu Y., and Lai L., “Virtual screening of novel noncovalent inhibitors for SARS-CoV 3C-like proteinase,” J. Chem. Inf. Model., vol. 45, no. 1, pp. 10–17, Jan. 2005, doi: 10.1021/ci049809b. [DOI] [PubMed] [Google Scholar]
- [105].Ivanov D., “Predicting the impacts of epidemic outbreaks on global chains: A simulation-based analysis on the coronavirus outbreak (COVID-19/SARS-CoV-2) case,” Transp. Res. E, Logistics Transp. Rev., vol. 136, Apr. 2020, Art. no.101922, doi: 10.1016/j.tre.2020.101922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Drexler M., “Interview with marcelle C. Layton, MD assistant commissioner, bureau of communicable disease new york city department of health and mental hygiene,” Biosecur. Bioterrorism: Biodefense Strategy, Pract., Sci., vol. 2, no. 4, pp. 245–250, Dec. 2004. [DOI] [PubMed] [Google Scholar]
- [107].Schwartz S. J., “Editorial: Studying the effects of the coronavirus pandemic on intercultural relations,” Int. J. Intercultural Relations, vol. 76, p. 52, May 2020, doi: 10.1016/j.ijintrel.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Hui J. M. C. and Tsui M.-S., “Empowerment by hotline: Experiences during the SARS outbreak,” Asia Pacific J. Social Work Develop., vol. 14, no. 1, pp. 65–71, Jun. 2004, doi: 10.1080/21650993.2004.9755943. [DOI] [Google Scholar]
- [109].Henderson J. C., “Managing a health-related crisis: SARS in singapore,” J. Vacation Marketing, vol. 10, no. 1, pp. 67–77, Jan. 2004, doi: 10.1177/135676670301000107. [DOI] [Google Scholar]
- [110].Huang Y. and Smith C. J., “China’s response to pandemics: From inaction to overreaction,” Eurasian Geography Econ., vol. 51, no. 2, pp. 162–183, Mar. 2010, doi: 10.2747/1539-7216.51.2.162. [DOI] [Google Scholar]
- [111].Tam K.-P., Lau I. Y.-M., and Chiu C.-Y., “Biases in the perceived prevalence and motives of severe acute respiratory syndrome prevention behaviors among Chinese high school students in Hong Kong,” Asian J. Social Psychol., vol. 7, no. 1, pp. 67–81, Apr. 2004, doi: 10.1111/j.1467-839X.2004.00135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Lee C. G., “Are tourist arrivals stationary? Evidence from Singapore,” Int. J. Tourism Res., vol. 11, no. 4, pp. 409–414, Jul. 2009, doi: 10.1002/jtr.708. [DOI] [Google Scholar]
- [113].Pai J.-Y., “A study in hospital Noise–A case from taiwan,” Int. J. Occupational Saf. Ergonom., vol. 13, no. 1, pp. 83–90, Jan. 2007, doi: 10.1080/10803548.2007.11076711. [DOI] [PubMed] [Google Scholar]
- [114].Boyd A. D. and Jardine C. G., “Did public risk perspectives of mad cow disease reflect media representations and actual outcomes?” J. Risk Res., vol. 14, no. 5, pp. 615–630, May 2011, doi: 10.1080/13669877.2010.547258. [DOI] [Google Scholar]
- [115].Auter P. J., Douai A., Makady H., and West C., “Circulating health rumors in the ‘Arab World’: A 12-month content analysis of news stories and reader commentary about Middle East Respiratory Syndrome from two Middle Eastern news outlets,” Int. Commun. Gazette, vol. 78, no. 5, pp. 411–431, 2016, doi: 10.1177/1748048516640202. [DOI] [Google Scholar]
- [116].Plog S. C., “Managing tourism crises: An interview with lily shum, former director, the americas, hong kong tourism board,” Cornell Hotel Restaurant Admin. Quart., vol. 46, no. 4, pp. 452–460, Nov. 2005, doi: 10.1177/0010880405281317. [DOI] [Google Scholar]
- [117].Dembek Z. F., Carley K., Siniscalchi A., and Hadler J., “Hospital admissions syndromic surveillance–connecticut, September 2001–November 2003,” MMWR. Morbidity Mortality Weekly Rep., vol. 53, pp. 50–52, Sep. 2004. [PubMed] [Google Scholar]
- [118].Bhuyan R., Lin E. C., and Ricci P. F., “Asian stock markets and the Severe Acute Respiratory Syndrome (SARS) epidemic: Implications for health risk management,” Int. J. Environ. Health, vol. 4, no. 1, pp. 40–56, 2010, doi: 10.1504/IJENVH.2010.033033. [DOI] [Google Scholar]
- [119].Van Wagner E., “The practice of biosecurity in canada: Public health legal preparedness and Toronto’s SARS crisis,” Environ. Planning A: Economy Space, vol. 40, no. 7, pp. 1647–1663, Jul. 2008, doi: 10.1068/a40281. [DOI] [Google Scholar]
- [120].Chien G. C. L. and Law R., “The impact of the Severe Acute Respiratory Syndrome on hotels: A case study of Hong Kong,” Int. J. Hospitality Manage., vol. 22, no. 3, pp. 327–332, 2003, doi: 10.1016/S0278-4319(03)00041-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Tang T. C. and Wong K. N., “Research note: The SARS epidemic and international visitor arrivals to cambodia: Is the impact permanent or transitory?” Tourism Econ., vol. 15, no. 4, pp. 883–890, Dec. 2009, doi: 10.5367/000000009789955206. [DOI] [Google Scholar]
- [122].He W., Wang B., Danish , and Wang Z., “Will regional economic integration influence carbon dioxide marginal abatement costs? Evidence from Chinese panel data,” Energy Econ., vol. 74, pp. 263–274, Aug. 2018, doi: 10.1016/j.eneco.2018.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Liu Y. and Boin A., “Framing a mega-disaster: Political rhetoric and the Wenchuan earthquake,” Saf. Sci., vol. 125, May 2020, Art. no.104621, doi: 10.1016/j.ssci.2020.104621. [DOI] [Google Scholar]
- [124].Füller H., “Pandemic cities: Biopolitical effects of changing infection control in post-SARS Hong Kong,” Geographical J., vol. 182, no. 4, pp. 342–352, Dec. 2016, doi: 10.1111/geoj.12179. [DOI] [Google Scholar]
- [125].Allamani A., “Addiction, risk, and resources,” Substance Use Misuse, vol. 42, nos. 2–3, pp. 421–439, Jan. 2007, doi: 10.1080/10826080601142287. [DOI] [PubMed] [Google Scholar]
- [126].Schwartz J. and Evans R. G., “Causes of effective policy implementation: China’s public health response to SARS,” J. Contemp. China, vol. 16, no. 51, pp. 195–213, May 2007, doi: 10.1080/10670560701194426. [DOI] [Google Scholar]
- [127].Kang M., Kim J. R., and Cha H., “From concerned citizens to activists: A case study of 2015 south korean MERS outbreak and the role of dialogic government communication and citizens’ emotions on public activism,” J. Public Relations Res., vol. 30, nos. 5–6, pp. 202–229, Nov. 2018, doi: 10.1080/1062726X.2018.1536980. [DOI] [Google Scholar]
- [128].Bahri S., “Enhancing quality of data through automated SARS contact tracing method using RFID technology,” Int. J. Netw. Virtual Organisations, vol. 4, no. 2, pp. 145–162, 2007, doi: 10.1504/IJNVO.2007.013540. [DOI] [Google Scholar]
- [129].Centers for Disease Control and Prevention, “SARS update,” Home Healthcare Nurse, vol. 21, no. 7, pp. 441–442, 2003, doi: 10.1097/00004045-200307000-00003. [DOI] [PubMed] [Google Scholar]
- [130].Cooper M., “Japanese tourism and the SARS epidemic of 2003,” J. Travel Tourism Marketing, vol. 19, nos. 2–3, pp. 117–131, Jun. 2005, doi: 10.1300/J073v19n02_10. [DOI] [Google Scholar]
- [131].Gan Y., Liu Y., and Zhang Y., “Flexible coping responses to severe acute respiratory syndrome-related and daily life stressful events,” Asian J. Social Psychol., vol. 7, no. 1, pp. 55–66, Apr. 2004, doi: 10.1111/j.1467-839X.2004.00134.x. [DOI] [Google Scholar]
- [132].Deruelle T., “Bricolage or entrepreneurship? Lessons from the creation of the European centre for disease prevention and control,” Eur. Policy Anal., vol. 2, no. 2, pp. 43–67, 2016, doi: 10.18278/epa.2.2.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [133].Wang Y. and Xi B., “Preparing for future uncertainty: Creating a crisis management team,” Int. J. Hum. Resour. Develop. Manage., vol. 9, no. 1, pp. 81–96, 2009, doi: 10.1504/IJHRDM.2009.021556. [DOI] [Google Scholar]
- [134].Koller D., Nicholas D., Gearing R., and Kalfa O., “Paediatric pandemic planning: Children’s perspectives and recommendations,” Health Social Care Community, vol. 18, no. 4, pp. 369–377, 2010, doi: 10.1111/j.1365-2524.2009.00907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Karan K., Aileen L., and Leng Elaine P. Y., “Emerging victorious against an outbreak: Integrated communication management of SARS in singapore media coverage and impact of the SARS campaign in moving a nation to be socially responsible,” J. Creative Commun., vol. 2, no. 3, pp. 383–403, Nov. 2007, doi: 10.1177/097325860700200307. [DOI] [Google Scholar]
- [136].Min J. C. H., “Forecasting japanese tourism demand in taiwan using an intervention analysis,” Int. J. Culture, Tourism Hospitality Res., vol. 2, no. 3, pp. 197–216, Aug. 2008, doi: 10.1108/17506180810891582. [DOI] [Google Scholar]
- [137].Schwartz J., Evans R. G., and Greenberg S., “Evolution of health provision in pre-SARS China: The changing nature of disease prevention,” China Rev., vol. 7, no. 1, pp. 81–104, 2007. [Google Scholar]
- [138].Hanrieder T. and Kreuder-Sonnen C., “WHO decides on the exception? Securitization and emergency governance in global health,” Secur. Dialogue, vol. 45, no. 4, pp. 331–348, Aug. 2014, doi: 10.1177/0967010614535833. [DOI] [Google Scholar]
- [139].Oh D. C. and Zhou W., “Framing SARS: A case study in toronto of a mainstream newspaper and a chinese ethnic newspaper,” Atlantic J. Commun., vol. 20, no. 5, pp. 261–273, Nov. 2012, doi: 10.1080/15456870.2012.728113. [DOI] [Google Scholar]
- [140].Chen M.-H., “The response of hotel performance to international tourism development and crisis events,” Int. J. Hospitality Manage., vol. 30, no. 1, pp. 200–212, Mar. 2011, doi: 10.1016/j.ijhm.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Lin Y.-C., “Impact of the spread of infectious disease on economic development: A study in risk management,” Int. J. Risk Assessment Manage., vol. 11, nos. 3–4, pp. 209–218, 2009. [Google Scholar]
- [142].Yip P. S. F., Lam K. F., Lau E. H. Y., Chau P.-H., Tsang K. W., and Chao A., “A comparison study of realtime fatality rates: Severe acute respiratory syndrome in Hong Kong, Singapore, Taiwan, Toronto and Beijing, China,” J. Roy. Stat. Soc., A (Statist. Soc.), vol. 168, no. 1, pp. 233–243, Jan. 2005, doi: 10.1111/j.1467-985X.2004.00345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143].Bang J.-I., Park J., Choi A., Jeong J.-W., Kim J., and Sung M., “Evaluation of UR-UVGI system for sterilization effect on microorganism contamination in negative pressure isolation ward,” Sustainability, vol. 10, no. 9, p. 3192, Sep. 2018, doi: 10.3390/su10093192. [DOI] [Google Scholar]
- [144].Chang W. C. and Sivam R.-W., “Constant vigilance: Heritage values and defensive pessimism in coping with severe acute respiratory syndrome in Singapore,” Asian J. Social Psychol., vol. 7, no. 1, pp. 35–53, Apr. 2004, doi: 10.1111/j.1467-839X.2004.00133.x. [DOI] [Google Scholar]
- [145].Caballero-Anthony M., “SARS in Asia: Crisis, vulnerabilities, and regional responses,” Asian Surv., vol. 45, no. 3, pp. 475–495, Jun. 2005, doi: 10.1525/as.2005.45.3.475. [DOI] [Google Scholar]
- [146].Okatch H., Sowicz T. J., Teng H., Pilling L., Harmon M., Brewer C., and Buttenheim A., “Nursing students as epidemiologists: A simulation approach,” Clin. Simul. Nursing, vol. 12, no. 2, pp. 51–61, Feb. 2016, doi: 10.1016/j.ecns.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Wong G., “Has SARS infected the property market? Evidence from Hong Kong,” J. Urban Econ., vol. 63, no. 1, pp. 74–95, Jan. 2008, doi: 10.1016/j.jue.2006.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [148].Wada K., Ohta H., and Aizawa Y., “Correlation of ‘Google Flu Trends’ with Sentinel Surveillance Data for Influenza in 2009 in Japan,” Open Public Health J., vol. 4, pp. 17–20, Oct. 2011, doi: 10.2174/1874944501104010017. [DOI] [Google Scholar]
- [149].Aaltola M., “Contagious insecurity: War, SARS and global air mobility,” Contemp. Politics, vol. 18, no. 1, pp. 53–70, Mar. 2012, doi: 10.1080/13569775.2012.651273. [DOI] [Google Scholar]
- [150].Chan E. H. W., Lam K. S., and Wong W. S., “Evaluation on indoor environment quality of dense urban residential buildings,” J. Facilities Manage., vol. 6, no. 4, pp. 245–265, Sep. 2008, doi: 10.1108/14725960810908127. [DOI] [Google Scholar]
- [151].Wang C.-H. and Kuo N.-W., “Post-occupancy evaluation of negative-pressure isolation rooms: Using the balanced scorecard framework,” J. Architectural Planning Res., vol. 26, no. 1, pp. 1–13, 2009. [Google Scholar]
- [152].Hong T., “Information control in time of crisis: The framing of SARS in China-based newspapers and Internet sources,” Cyberpsychol. Behav., vol. 10, no. 5, pp. 696–699, Oct. 2007, doi: 10.1089/cpb.2007.9968. [DOI] [PubMed] [Google Scholar]
- [153].Asamoa-Baah A., “Can new infectious diseases be stopped? Lessons from SARS and avian influenza: Infectious diseases can emerge and spread with deadly and debilitating effects. But they can be stopped, as experience from SARS shows,” OECD Observer, no. 243, pp. 14–15, 2004.
- [154].Bruno D. M. and Imperato P. J., “A global health elective for US medical students: The 35 year experience of the State University of New York, downstate medical center, school of public health,” J. Community Health, vol. 40, no. 2, pp. 187–198, Apr. 2015, doi: 10.1007/s10900-014-9981-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [155].Mak W. W. S., Mo P. K. H., Cheung R. Y. M., Woo J., Cheung F. M., and Lee D., “Comparative stigma of HIV/AIDS, SARS, and tuberculosis in Hong Kong,” Social Sci. Med., vol. 63, no. 7, pp. 1912–1922, Oct. 2006, doi: 10.1016/j.socscimed.2006.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [156].Nippani S. and Washer K. M., “SARS: A non-event for affected countries’ stock markets?” Appl. Financial Econ., vol. 14, no. 15, pp. 1105–1110, Oct. 2004, doi: 10.1080/0960310042000310579. [DOI] [Google Scholar]
- [157].Law R., To T., and Goh C., “How do Mainland Chinese travelers choose restaurants in Hong Kong?: An exploratory study of individual visit scheme travelers and packaged travelers,” Int. J. Hospitality Manage., vol. 27, no. 3, pp. 346–354, 2008, doi: 10.1016/j.ijhm.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Office of the Federal Register, “Control of communicable diseases. Interim final rule with comment period,” Federal Register, vol. 68, no. 69, pp. 17558–17560, 2003. [PubMed] [Google Scholar]
- [159].Larson B. M. H., Nerlich B., and Wallis P., “Metaphors and biorisks: The war on infectious diseases and invasive species,” Sci. Commun., vol. 26, no. 3, pp. 243–268, Mar. 2005, doi: 10.1177/1075547004273019. [DOI] [Google Scholar]
- [160].Luther C. A. and Zhou X., “Within the boundaries of politics: News framing of sars in China and the united states,” Journalism Mass Commun. Quart., vol. 82, no. 4, pp. 857–872, Dec. 2005, doi: 10.1177/107769900508200407. [DOI] [Google Scholar]
- [161].Stires D., “By the numbers. The bird flu that’s sweeping across Asia,” Fortune, vol. 149, no. 4, p. 34, 2004. [PubMed] [Google Scholar]
- [162].Lee Y. C., “Exploring the roles and nature of science: A case study of severe acute respiratory syndrome,” Int. J. Sci. Edu., vol. 30, no. 4, pp. 515–541, Mar. 2008, doi: 10.1080/09500690701223368. [DOI] [Google Scholar]
- [163].Chandler C., “Road to recovery. Eight months after SARS hit, is Hong Kong finally back?” Fortune, vol. 148, no. 9, p. 54, 2003. [PubMed] [Google Scholar]
- [164].Overby J., Rayburn M., Hammond K., and Wyld D. C., “The China syndrome: The impact of the SARS epidemic in southeast Asia,” Asia Pacific J. Marketing Logistics, vol. 16, no. 1, pp. 69–94, Mar. 2004, doi: 10.1108/13555850410765131. [DOI] [Google Scholar]
- [165].McLafferty S., “Placing pandemics: Geographical dimensions of vulnerability and spread,” Eurasian Geography Econ., vol. 51, no. 2, pp. 143–161, 2010, doi: 10.2747/1539-7216.51.2.143. [DOI] [Google Scholar]
- [166].Goh I. and Tan Y.-Y., “SingaporePharmakon,” Social Identities, vol. 13, no. 3, pp. 393–409, May 2007, doi: 10.1080/13504630701365692. [DOI] [Google Scholar]
- [167].Cheung R. Y.-M. and Au T. K.-F., “Nursing Students’ anxiety and clinical performance,” J. Nursing Edu., vol. 50, no. 5, pp. 286–289, May 2011, doi: 10.3928/01484834-20110131-08. [DOI] [PubMed] [Google Scholar]
- [168].Kostoff R. N., “Literature-related discovery: Potential treatments and preventatives for SARS,” Technological Forecasting Social Change, vol. 78, no. 7, pp. 1164–1173, Sep. 2011, doi: 10.1016/j.techfore.2011.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [169].Xu Z. and Sui D. Z., “Effect of small-world networks on epidemic propagation and intervention,” Geographical Anal., vol. 41, no. 3, pp. 263–282, Jul. 2009, doi: 10.1111/j.1538-4632.2009.00754.x. [DOI] [Google Scholar]
- [170].Chen M.-P., Lee C.-C., Lin Y.-H., and Chen W.-Y., “Did the S.A.R.S. epidemic weaken the integration of asian stock markets? Evidence from smooth time-varying cointegration analysis,” Econ. Res.-Ekonomska Istraživanja, vol. 31, no. 1, pp. 908–926, Jan. 2018, doi: 10.1080/1331677X.2018.1456354. [DOI] [Google Scholar]
- [171].Kaman Lee B., “The HKSAR Government’s PR sense and sensibility: Analysis of its SARS crisis management,” Asian J. Commun., vol. 17, no. 2, pp. 201–214, Jun. 2007, doi: 10.1080/01292980701306621. [DOI] [Google Scholar]
- [172].Cook A. H. and Cohen D. B., “Pandemic disease: A past and future challenge to governance in the united states,” Rev. Policy Res., vol. 25, no. 5, pp. 449–471, Sep. 2008, doi: 10.1111/j.1541-1338.2008.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [173].Zhou Y. R. and Coleman W. D., “Accelerated contagion and response: Understanding the relationships among globalization, time, and disease,” Globalizations, vol. 13, no. 3, pp. 285–299, May 2016, doi: 10.1080/14747731.2015.1056498. [DOI] [Google Scholar]
- [174].Habibi F., “The determinants of inbound tourism to Malaysia: A panel data analysis,” Current Issues Tourism, vol. 20, no. 9, pp. 909–930, Jul. 2017, doi: 10.1080/13683500.2016.1145630. [DOI] [Google Scholar]
- [175].Jia N. and Tsui L., “Epidemic modelling using SARS as a case study,” North Amer. Actuarial J., vol. 9, no. 4, pp. 28–42, Oct. 2005, doi: 10.1080/10920277.2005.10596223. [DOI] [Google Scholar]
- [176].Fong E. and Chang L.-Y., “Community under stress: Trust, reciprocity, and community collective efficacy during SARS outbreak,” J. Community Health, vol. 36, no. 5, pp. 797–810, Oct. 2011, doi: 10.1007/s10900-011-9378-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [177].Ji L.-J., Zhang Z., Usborne E., and Guan Y., “Optimism across cultures: In response to the severe acute respiratory syndrome outbreak,” Asian J. Social Psychol., vol. 7, no. 1, pp. 25–34, Apr. 2004, doi: 10.1111/j.1467-839X.2004.00132.x. [DOI] [Google Scholar]
- [178].Lee P. T. P., “VITLE experience: HKBU library supporting e-learning in a SARS environment,” Library Hi Tech News, vol. 21, no. 1, pp. 19–21, 2004, doi: 10.1108/07419050410526475. [DOI] [Google Scholar]
- [179].Dwyer J. and Tsai D. F.-C., “Developing the duty to treat: HIV, SARS, and the next epidemic,” J. Med. Ethics, vol. 34, no. 1, pp. 7–10, Jan. 2008, doi: 10.1136/jme.2006.018978. [DOI] [PubMed] [Google Scholar]
- [180].Chen M.-H., Jang S. S., and Kim W. G., “The impact of the SARS outbreak on taiwanese hotel stock performance: An event-study approach,” Int. J. Hospitality Manage., vol. 26, no. 1, pp. 200–212, Mar. 2007, doi: 10.1016/j.ijhm.2005.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [181].Schwirian K., “Globalization, plague and the local community: Healthcare capacity, politics, and the microbe war,” Sociol. Focus, vol. 38, no. 3, pp. 151–170, Aug. 2005, doi: 10.1080/00380237.2005.10571262. [DOI] [Google Scholar]
- [182].McKercher B. and Chon K., “The over-reaction to SARS and the collapse of asian tourism,” Ann. Tourism Res., vol. 31, no. 3, pp. 716–719, Jul. 2004, doi: 10.1016/j.annals.2003.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [183].Yoshikawa M. J., “Singapore’s prescription for successful control of transnational emerging infectious diseases,” Southeast Asian Stud., vol. 1, no. 2, pp. 301–331, 2012. [Google Scholar]
- [184].Li H., Yang W., and Chen J. J., “From ‘Cinderella’ to ‘Beloved Princess’: The evolution of early childhood education policy in China,” Int. J. Child Care Educ. Policy, vol. 10, no. 1, p. 2, 2016, doi: 10.1186/s40723-016-0018-2. [DOI] [Google Scholar]
- [185].You M. and Ju Y., “Preferring negative or positive news? A closer examination of journalistic negativity in a health crisis,” Atlantic J. Commun., vol. 26, no. 5, pp. 318–329, Oct. 2018, doi: 10.1080/15456870.2018.1517575. [DOI] [Google Scholar]
- [186].Au A. K. M., Ramasamy B., and Yeung M. C. H., “The effects of SARS on the hong kong tourism industry: An empirical evaluation,” Asia Pacific J. Tourism Res., vol. 10, no. 1, pp. 85–95, Mar. 2005, doi: 10.1080/1094166042000330236. [DOI] [Google Scholar]
- [187].Davies S. E., “Infectious disease outbreak response: Mind the rights gap,” Med. Law Rev., vol. 25, no. 2, pp. 270–292, 2017, doi: 10.1093/medlaw/fwx011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [188].Bybee K., “Medical evacuation of patients with infectious diseases,” J. Petroleum Technol., vol. 63, no. 08, pp. 93–94, Aug. 2011. [Google Scholar]
- [189].Bo Z., “Political succession and elite politics in twenty-first century China: Toward a perspective of ‘Power balancing,”’ Issues Stud., vol. 41, no. 1, pp. 162–189, 2005. [Google Scholar]
- [190].Lynch T. and Dauphinee W., “Quality management case studies in health service emergencies: SARS and wildland-urban interface fires,” Qual. Manage. Health Care, vol. 14, no. 1, pp. 2–17, Jan. 2005, doi: 10.1097/00019514-200501000-00002. [DOI] [PubMed] [Google Scholar]
- [191].Schillmeier M., “Globalizing risks–the cosmo-politics of SARS and its impact on globalizing sociology,” Mobilities, vol. 3, no. 2, pp. 179–199, 2008, doi: 10.1080/17450100802095288. [DOI] [Google Scholar]
- [192].Tan X., “Severe acute respiratory syndrome epidemic and change of people’s health behavior in China,” Health Edu. Res., vol. 19, no. 5, pp. 576–580, May 2004, doi: 10.1093/her/cyg074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [193].McCleary L., Munro M., Jackson L., and Mendelsohn L., “Impact of SARS visiting restrictions on relatives of long-term care residents,” J. Social Work Long-Term Care, vol. 3, nos. 3–4, pp. 3–20, Mar. 2006, doi: 10.1300/J181v03n03_02. [DOI] [Google Scholar]
- [194].Lucchese M. and Pianta M., “The coming coronavirus crisis: What can we learn?” Intereconomics, vol. 55, no. 2, pp. 98–104, Mar. 2020, doi: 10.1007/s10272-020-0878-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [195].Malani A. and Laxminarayan R., “Incentives for reporting infectious disease outbreaks,” J. Hum. Resour., vol. 46, no. 1, pp. 176–202, Jan. 2011, doi: 10.3368/jhr.46.1.176. [DOI] [Google Scholar]
- [196].Qian H., Li Y., Nielsen P. V., and Huang X., “Spatial distribution of infection risk of SARS transmission in a hospital ward,” Building Environ., vol. 44, no. 8, pp. 1651–1658, Aug. 2009, doi: 10.1016/j.buildenv.2008.11.002. [DOI] [Google Scholar]
- [197].Bensimon C. M., Smith M. J., Pisartchik D., Sahni S., and Upshur R. E. G., “The duty to care in an influenza pandemic: A qualitative study of canadian public perspectives,” Social Sci. Med., vol. 75, no. 12, pp. 2425–2430, Dec. 2012, doi: 10.1016/j.socscimed.2012.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [198].Roberts S. L. and Elbe S., “Catching the flu: Syndromic surveillance, algorithmic governmentality and global health security,” Secur. Dialogue, vol. 48, no. 1, pp. 46–62, Feb. 2017, doi: 10.1177/0967010616666443. [DOI] [Google Scholar]
- [199].Chen Y.-C., Kang H.-H., and Yang T.-C., “A study on the impact of SARS on the forecast of visitor arrivals to China,” J. Asia–Pacific Bus., vol. 8, no. 1, pp. 31–50, Mar. 2007, doi: 10.1300/J098v08n01_04. [DOI] [Google Scholar]
- [200].Bensimon C. M., Tracy C. S., Bernstein M., Shaul R. Z., and Upshur R. E. G., “A qualitative study of the duty to care in communicable disease outbreaks,” Social Sci. Med., vol. 65, no. 12, pp. 2566–2575, Dec. 2007, doi: 10.1016/j.socscimed.2007.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [201].Schwartz N. D. and Creswel J., “Flying scared. Seven ways to make air travel safer,” Fortune, vol. 147, no. 8, pp. 72–76, 2003. [PubMed] [Google Scholar]
- [202].Heymann D. L., “Interview with David L. Heymann, MD, representative for polio eradication and former executive director, communicable diseases, World Health Organization. interview by madeline drexler,” Biosecur. Bioterrorism: Biodefense Strategy, Pract., Sci., vol. 1, no. 4, pp. 233–237, 2003. [DOI] [PubMed] [Google Scholar]
- [203].Anderson B. A., “Crisis management in the Australian tourism industry: Preparedness, personnel and postscript,” Tourism Manage., vol. 27, no. 6, pp. 1290–1297, Dec. 2006, doi: 10.1016/j.tourman.2005.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [204].Huarng K.-H., Yu T. H.-K., and Solé Parellada F., “An innovative regime switching model to forecast taiwan tourism demand,” Service Ind. J., vol. 31, no. 10, pp. 1603–1612, Aug. 2011, doi: 10.1080/02642069.2010.485637. [DOI] [Google Scholar]
- [205].Min J. C. H., Kung H.-H., and Chang T., “Testing the structural break of Taiwan inbound tourism markets,” Romanian J. Econ. Forecasting, vol. 22, no. 2, pp. 117–130, 2019. [Google Scholar]
- [206].Wills S. and Forrest P., “Inferior vena cava thrombosis as a cause of haemolysis in a patient on ECMO,” Perfusion, vol. 32, no. 2, pp. 168–170, Mar. 2017, doi: 10.1177/0267659116664023. [DOI] [PubMed] [Google Scholar]
- [207].Bennett S. A., “Flight crew stress and fatigue in low-cost commercial air operations-an appraisal,” Int. J. Risk Assessment Manage., vol. 4, nos. 2–3, pp. 207–231, 2003. [Google Scholar]
- [208].Kraus R., “China IN 2003: From SARS to spaceships,” Asian Surv., vol. 44, no. 1, pp. 147–157, Feb. 2004, doi: 10.1525/as.2004.44.1.147. [DOI] [Google Scholar]
- [209].Lee G. O. M. and Warner M., “Epidemics, labour markets and unemployment: The impact of SARS on human resource management in the Hong Kong service sector,” Int. J. Hum. Resour. Manage., vol. 16, no. 5, pp. 752–771, May 2005, doi: 10.1080/09585190500083202. [DOI] [Google Scholar]
- [210].Chan E., Yim Yiu C., Baldwin A., and Lee G., “Value of buildings with design features for healthy living: A contingent valuation approach,” Facilities, vol. 27, no. 5/6, pp. 229–249, Apr. 2009, doi: 10.1108/02632770910944952. [DOI] [Google Scholar]
- [211].Teo W. L., Lee M., and Lim W.-S., “The relational activation of resilience model: How leadership activates resilience in an organizational crisis,” J. Contingencies Crisis Manage., vol. 25, no. 3, pp. 136–147, Sep. 2017, doi: 10.1111/1468-5973.12179. [DOI] [Google Scholar]
- [212].Caballero-Anthony M., “Health and human security challenges in Asia: New agendas for strengthening regional health governance,” Austral. J. Int. Affairs, vol. 72, no. 6, pp. 602–616, Nov. 2018, doi: 10.1080/10357718.2018.1537356. [DOI] [Google Scholar]
- [213].Setthachotsombut N. and Sua-iam G., “The resilience development for the entrepreneurs tourism sector (RDETS) from the 2019 coronavirus crisis in Thailand,” Afr. J. Hosp. Tourism Leis., vol. 9, no. 2, pp. 1–14, 2020. [Google Scholar]
- [214].Lee-Baggley D., DeLongis A., Voorhoeave P., and Greenglass E., “Coping with the threat of severe acute respiratory syndrome: Role of threat appraisals and coping responses in health behaviors,” Asian J. Social Psychol., vol. 7, no. 1, pp. 9–23, Apr. 2004, doi: 10.1111/j.1467-839X.2004.00131.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [215].Jung E. and Sung H., “The influence of the middle east respiratory syndrome outbreak on online and offline markets for retail sales,” Sustainability, vol. 9, no. 3, p. 411, Mar. 2017, doi: 10.3390/su9030411. [DOI] [Google Scholar]
- [216].Lee G. O. M. and Warner M., “Human resources, labour markets and unemployment: The impact of the SARS epidemic on the service sector in singapore,” Asia Pacific Bus. Rev., vol. 12, no. 4, pp. 507–527, Oct. 2006, doi: 10.1080/13602380600571443. [DOI] [Google Scholar]
- [217].Loveband A., “Nationality matters: SARS and foreign domestic Workers’ rights in taiwan province of China,” Int. Migration, vol. 42, no. 5, pp. 121–145, Dec. 2004. [Google Scholar]
- [218].Lee A. and Cho J., “The impact of city epidemics on rural labor market: The Korean middle east respiratory syndrome case,” Jpn. World Economy, vol. 43, pp. 30–40, Sep. 2017, doi: 10.1016/j.japwor.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [219].Twedell D., “Duty to care,” J. Continuing Edu. Nursing, vol. 40, no. 2, pp. 53–54, Feb. 2009, doi: 10.3928/00220124-20090201-04. [DOI] [PubMed] [Google Scholar]
- [220].Fong V. L., “SARS, a shipwreck, a NATO attack, and September 11, 2001: Global information flows and Chinese responses to tragic news events,” Amer. Ethnologist, vol. 34, no. 3, pp. 521–539, Aug. 2007, doi: 10.1525/ae.2007.34.3.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [221].Bennett D., Chiang C.-F., and Malani A., “Learning during a crisis: The SARS epidemic in taiwan,” J. Develop. Econ., vol. 112, pp. 1–18, Jan. 2015, doi: 10.1016/j.jdeveco.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [222].Olsson E.-K. and Verbeek B., “International organisations and crisis management: Do crises enable or constrain IO autonomy?” J. Int. Relations Develop., vol. 21, no. 2, pp. 275–299, Apr. 2018, doi: 10.1057/s41268-016-0071-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [223].You M., Joo J., Park E., Noh G.-Y., and Ju Y., “Emerging infectious disease content in newspaper editorials: Public health concern or leadership issue?” Sci. Commun., vol. 39, no. 3, pp. 313–337, Jun. 2017, doi: 10.1177/1075547017705392. [DOI] [Google Scholar]
- [224].Shantz J., “Capitalism is making us sick: Behind the SARS crisis in Toronto,” Capital Class, vol. 28, no. 2, pp. 1–7, Jul. 2004, doi: 10.1177/030981680408300101. [DOI] [Google Scholar]
- [225].Samal A. and Jena J., “Assessment of awareness and knowledge towards novel coronavirus (nCoV) amongst University Students in India,” Int. J. Sci. Technol. Res., vol. 9, no. 4, pp. 1142–1148, 2020. [Google Scholar]
- [226].Chan C. K., “Defining health risk by media template: Hong Kong’s news discourse of the Swine Flu pandemic,” Journalism, vol. 17, no. 8, pp. 1018–1036, 2016, doi: 10.1177/1464884915595473. [DOI] [Google Scholar]
- [227].Kim S. S., Chun H., and Lee H., “The effects of SARS on the Korean hotel industry and measures to overcome the crisis: A case study of six Korean five-star hotels,” Asia Pacific J. Tourism Res., vol. 10, no. 4, pp. 369–377, Dec. 2005, doi: 10.1080/10941660500363694. [DOI] [Google Scholar]
- [228].Biao X., “SARS and migrant workers in China: An institutional analysis,” Asian Pacific Migration J., vol. 12, no. 4, pp. 467–500, 2003. [Google Scholar]
- [229].Salleh N. H. M., Othman R., and Ramachandran S., “Malaysia’s tourism demand from selected countries: The ARDL approach to cointegration,” Int. J. Econ. Manage., vol. 1, no. 3, pp. 345–363, 2007. [Google Scholar]
- [230].Suh H. and Kim S.-B., “The macroeconomic determinants of international casino travel: Evidence from South Korea’s top four inbound markets,” Sustainability, vol. 10, no. 2, p. 554, Feb. 2018, doi: 10.3390/su10020554. [DOI] [Google Scholar]
- [231].Ng S. M., Chan T. H. Y., Chan C. L. W., Lee A. M., Yau J. K. Y., Chan C. H. Y., and Lau J., “Group debriefing for people with chronic diseases during the SARS pandemic: Strength-focused and meaning-oriented approach for resilience and transformation (SMART),” Community Mental Health J., vol. 42, no. 1, pp. 53–63, Feb. 2006, doi: 10.1007/s10597-005-9002-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [232].Smith E., Woodd C., Jensen S., and Archer F., “Paramedics and public health emergencies: Is there a’duty to respond’in Australia?: Smith, Burkle Jr, Woodd, Jensen, and Archer examine the concept of’duty to respond’in the Australian SARS context,” Austral. J. Emergency Manage., vol. 25, no. 2, pp. 46–53, 2010. [Google Scholar]
- [233].Davies S. E., “Duty in the time of epidemics: What China and zimbabwe teach us,” Austral. J. Int. Affairs, vol. 66, no. 4, pp. 413–430, Aug. 2012, doi: 10.1080/10357718.2012.692532. [DOI] [Google Scholar]
- [234].Bennett B. and Carney T., “Planning for pandemics: Lessons from the past decade,” J. Bioethical Inquiry, vol. 12, no. 3, pp. 419–428, Sep. 2015, doi: 10.1007/s11673-014-9555-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [235].Chong B. S. and Lee C. H., “Crisis management-dealing with asymmetric information problems,” Thunderbird Int. Bus. Rev., vol. 51, no. 3, pp. 239–248, May 2009, doi: 10.1002/tie.20262. [DOI] [Google Scholar]
- [236].Baehr P., “Social extremity, communities of fate, and the sociology of SARS,” Eur. J. Sociol., vol. 46, no. 2, pp. 179–211, Aug. 2005, doi: 10.1017/S000397560500007X. [DOI] [Google Scholar]
- [237].Wong S. L., Kwan J., Hodson D., and Yung B. H. W., “Turning crisis into opportunity: Nature of science and scientific inquiry as illustrated in the scientific research on severe acute respiratory syndrome,” Sci. Edu., vol. 18, no. 1, pp. 95–118, Jan. 2009, doi: 10.1007/s11191-007-9123-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [238].Tse A. C. B., So S., and Sin L., “Crisis management and recovery: How restaurants in Hong Kong responded to SARS,” Int. J. Hospitality Manage., vol. 25, no. 1, pp. 3–11, Mar. 2006, doi: 10.1016/j.ijhm.2004.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [239].St Louis M., “Global health surveillance,” MMWR. Surveill. Summery, vol. 61, no. 3, pp. 15–19, 2012. [PubMed] [Google Scholar]
- [240].Leavitt J. W. and Leavitt L. A., “After SARS: Fear and its uses,” Dissent, no. FALL, pp. 54–58, 2003.
- [241].Tatem A. J., “Mapping population and pathogen movements,” Int. Health, vol. 6, no. 1, pp. 5–11, Mar. 2014, doi: 10.1093/inthealth/ihu006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [242].Law R., “A perspective on SARS and education in hospitality and tourism,” J. Teach. Travel Tourism, vol. 5, no. 4, pp. 53–59, Jul. 2005, doi: 10.1300/J172v05n04_04. [DOI] [Google Scholar]
- [243].Wen Z., Huimin G., and Kavanaugh R. R., “The impacts of SARS on the consumer behaviour of Chinese domestic tourists,” Current Issues Tourism, vol. 8, no. 1, pp. 22–38, Jan. 2005. [Google Scholar]
- [244].Watkins P., “Survey of the European yarn fairs for autumn/winter 2004/05,” Text. Outlook Int., vol. 2003, no. 107, pp. 93–103, 2003. [Google Scholar]
- [245].Curley M. and Thomas N., “Human security and public health in southeast asia: The SARS outbreak,” Austral. J. Int. Affairs, vol. 58, no. 1, pp. 17–32, Mar. 2004, doi: 10.1080/1035771032000184737. [DOI] [Google Scholar]
- [246].Leung C. S., Ho M. M., Kiss A., Gundlapalli A. V., and Hwang S. W., “Homelessness and the response to emerging infectious disease outbreaks: Lessons from SARS,” J. Urban Health, vol. 85, no. 3, pp. 402–410, May 2008, doi: 10.1007/s11524-008-9270-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [247].Wu C.-C., Lee W.-C., and Lin R. S. J., “Are employees more committed and willing to accept critical assignments during a crisis? A study of organizational commitment, professional commitment and willingness to care during the SARS outbreak in taiwan,” Int. J. Hum. Resour. Manage., vol. 23, no. 13, pp. 2698–2711, Jul. 2012, doi: 10.1080/09585192.2011.637056. [DOI] [Google Scholar]
- [248].Burkom H. S., Murphy S., Coberly J., and Hurt-Mullen K., “Public health monitoring tools for multiple data streams,” MMWR. Morb. Mortal. Wkly. Rep., vol. 54, pp. 55–62, 2005. [PubMed] [Google Scholar]
- [249].Aleman D. M., Wibisono T. G., and Schwartz B., “A nonhomogeneous agent-based simulation approach to modeling the spread of disease in a pandemic outbreak,” Interfaces, vol. 41, no. 3, pp. 301–315, Jun. 2011, doi: 10.1287/inte.1100.0550. [DOI] [Google Scholar]
- [250].Huarng K., Yu T. H.-K., Moutinho L., and Wang Y., “Forecasting tourism demand by fuzzy time series models,” Int. J. Culture, Tourism Hospitality Res., vol. 6, no. 4, pp. 377–388, Oct. 2012, doi: 10.1108/17506181211265095. [DOI] [Google Scholar]
- [251].Tian D. and Zheng T., “Emerging infectious disease: Trends in the literature on SARS and H7N9 influenza,” Scientometrics, vol. 105, no. 1, pp. 485–495, Oct. 2015, doi: 10.1007/s11192-015-1681-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [252].You M. and Ju Y., “Salience of public leaders’ ‘meaning making’ in news coverage of a health crisis,” J. Contingencies Crisis Manage., vol. 27, no. 4, pp. 400–405, 2019, doi: 10.1111/1468-5973.12259. [DOI] [Google Scholar]
- [253].Budd L., Bell M., and Warren A., “Maintaining the sanitary border: Air transport liberalisation and health security practices at UK regional airports,” Trans. Inst. Brit. Geographers, vol. 36, no. 2, pp. 268–279, Apr. 2011, doi: 10.1111/j.1475-5661.2010.00424.x. [DOI] [Google Scholar]
- [254].Major C., “Affect work and infected bodies: Biosecurity in an age of emerging infectious disease,” Environ. Planning A: Economy Space, vol. 40, no. 7, pp. 1633–1646, Jul. 2008, doi: 10.1068/a40289. [DOI] [Google Scholar]
- [255].Davies S. E., “The duty to report disease outbreaks: Of interest or value? Lessons from H5N1,” Contemp. Politics, vol. 17, no. 4, pp. 429–445, Dec. 2011, doi: 10.1080/13569775.2011.619767. [DOI] [Google Scholar]
- [256].Marafa L. M. and Tung F., “Changes in participation in leisure and outdoor recreation activities among Hong Kong people during the SARS outbreak,” World Leisure J., vol. 46, no. 2, pp. 38–47, Jan. 2004, doi: 10.1080/04419057.2004.9674356. [DOI] [Google Scholar]
- [257].Bofinger P., Dullien S., Felbermayr G., Fuest C., and Hüther M., “Economic implications of the corona crisis and economic policy measures [Wirtschaftliche Implikationen der Corona-Krise und wirtschaftspolitische Maßnahmen],” Wirtschaftsdienst, vol. 100, no. 4, pp. 259–265, 2020, doi: 10.1007/s10273-020-2628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [258].Yang S.-U., “Effects of government dialogic competency: The MERS outbreak and implications for public health crises and political legitimacy,” Journalism Mass Commun. Quart., vol. 95, no. 4, pp. 1011–1032, Dec. 2018, doi: 10.1177/1077699017750360. [DOI] [Google Scholar]
- [259].Lee G. O. M. and Warner M., “The impact of SARS on China’s human resources: Implications for the labour market and level of unemployment in the service sector in Beijing, Guangzhou and Shanghai,” Int. J. Hum. Resour. Manage., vol. 17, no. 5, pp. 860–880, May 2006, doi: 10.1080/09585190600640919. [DOI] [Google Scholar]
- [260].Paladini M., “Daily emergency department surveillance system—Bergen County, New Jersey,” MMWR. Morbidity Mortality Weekly Rep., vol. 53, pp. 47–49, Sep. 2004. [PubMed] [Google Scholar]
- [261].Cheng K. M., “Tourism demand in Hong Kong: Income, prices, and visa restrictions,” Current Issues Tourism, vol. 15, no. 3, pp. 167–181, Apr. 2012, doi: 10.1080/13683500.2011.569011. [DOI] [Google Scholar]
- [262].Keil R. and Ali H., “Governing the Sick City: Urban governance in the age of emerging infectious disease,” Antipode, vol. 39, no. 5, pp. 846–873, Dec. 2007, doi: 10.1111/j.1467-8330.2007.00555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [263].Mullin S., “New York City’s communication trials by fire, from West Nile to SARS,” Biosecur. Bioterrorism: Biodefense Strategy, Pract., Sci., vol. 1, no. 4, pp. 267–272, 2003, doi: 10.1089/153871303771861478. [DOI] [PubMed] [Google Scholar]
- [264].Zhang X., Li X., Wan X., Zeng C., Scott C. S., and Schaad D. C., “Attitudes of chinese medical students toward the global minimum essential requirements established by the institute for international medical education,” Teaching Learn. Med., vol. 16, no. 2, pp. 139–144, Apr. 2004, doi: 10.1207/s15328015tlm1602_4. [DOI] [PubMed] [Google Scholar]
- [265].Chakravorty U., Fisher D. K., and Umetsu C., “Environmental effects of intensification of agriculture: Livestock production and regulation,” Environ. Econ. Policy Stud., vol. 8, no. 4, pp. 315–336, Dec. 2007, doi: 10.1007/BF03353963. [DOI] [Google Scholar]
- [266].Chen Y.-D., Brown S. A., Hu P. J.-H., King C.-C., and Chen H., “Managing emerging infectious diseases with information systems: Reconceptualizing outbreak management through the lens of loose coupling,” Inf. Syst. Res., vol. 22, no. 3, pp. 447–468, Sep. 2011, doi: 10.1287/isre.1110.0376. [DOI] [Google Scholar]
- [267].Kahn J., “It’s a small world after all: Ethics and the response to SARS,” Hastings Center Rep., vol. 33, no. 3, p. 6, 2003. [PubMed] [Google Scholar]
- [268].Lin C.-J., “A textual analysis of the coverage of SARS and the image of China–a comparative analysis,” Asian Social Sci., vol. 8, no. 3, pp. 49–62, Feb. 2012, doi: 10.5539/ass.v8n3p49. [DOI] [Google Scholar]
- [269].Gillett J., “Internet Web logs as cultural resistance: A study of the SARS arts project,” J. Commun. Inquiry, vol. 31, no. 1, pp. 28–43, Jan. 2007, doi: 10.1177/0196859906294840. [DOI] [Google Scholar]
- [270].Yang T.-W. and Li E.-C., “Ethical study on the reform and development of medical and health services in China,” Bioethics, vol. 29, no. 6, pp. 406–412, Jul. 2015, doi: 10.1111/bioe.12119. [DOI] [PubMed] [Google Scholar]
- [271].Toohey K., Taylor T., and Lee C.-K., “The FIFA World Cup 2002: The effects of terrorism on sport tourists,” J. Sport Tourism, vol. 8, no. 3, pp. 186–196, 2003, doi: 10.1080/14775080310001690495. [DOI] [Google Scholar]
- [272].Hinsley S., “Planetary health research digest,” Lancet Planet. Health, vol. 4, no. 4, p. e140, 2020, doi: 10.1016/S2542-5196(20)30087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [273].Ratzan S. C., “Making sense of risk,” J. Health Commun., vol. 8, no. 5, pp. 399–400, 2003, doi: 10.1080/713852121. [DOI] [PubMed] [Google Scholar]
- [274].Gearing R. E., Saini M., and McNeill T., “Experiences and implications of social workers practicing in a pediatric hospital environment affected by SARS,” Health Social Work, vol. 32, no. 1, pp. 17–27, Feb. 2007, doi: 10.1093/hsw/32.1.17. [DOI] [PubMed] [Google Scholar]
- [275].Heung Y. Y. J., Wong K. Y. F., Kwong W. Y. E., To S. S. T., and Wong H. C. D., “Severe acute respiratory syndrome outbreak promotes a strong sense of professional identity among nursing students,” Nurse Edu. Today, vol. 25, no. 2, pp. 112–118, Feb. 2005, doi: 10.1016/j.nedt.2004.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [276].Zhang E. and Fleming K., “Examination of characteristics of news media under censorship: A content analysis of selected Chinese newspapers’ SARS coverage,” Asian J. Commun., vol. 15, no. 3, pp. 319–339, 2005, doi: 10.1080/01292980500261639. [DOI] [Google Scholar]
- [277].Jang K. and Baek Y. M., “When information from public health officials is untrustworthy: The use of online news, interpersonal networks, and social media during the MERS outbreak in South Korea,” Health Commun., vol. 34, no. 9, pp. 991–998, Jul. 2019, doi: 10.1080/10410236.2018.1449552. [DOI] [PubMed] [Google Scholar]
- [278].Buus S. and Olsson E.-K., “The SARS crisis: Was anybody responsible?” J. Contingencies Crisis Manage., vol. 14, no. 2, pp. 71–81, Jun. 2006, doi: 10.1111/j.1468-5973.2006.00483.x. [DOI] [Google Scholar]
- [279].Huang Y., Mesak H. I., Hsu M. K., and Qu H., “Dynamic efficiency assessment of the chinese hotel industry,” J. Bus. Res., vol. 65, no. 1, pp. 59–67, Jan. 2012, doi: 10.1016/j.jbusres.2011.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [280].Liu L., He H. F., Dai C. F., Liang L. H., Li T., and Li L. H., “Salmonellosis outbreak among factory workers–Huizhou, Guangdong Province, China, July 2004,” MMWR. Morbidity Mortality Weekly Rep., vol. 55, 1, Suppl 1, pp. 35–38, 2006. [PubMed] [Google Scholar]
- [281].Shi W. and Li K. X., “Impact of unexpected events on inbound tourism demand modeling: Evidence of middle east respiratory syndrome outbreak in South Korea,” Asia Pacific J. Tourism Res., vol. 22, no. 3, pp. 344–356, Mar. 2017, doi: 10.1080/10941665.2016.1250795. [DOI] [Google Scholar]
- [282].Wong S. L., Hodson D., Kwan J., and Yung B. H. W., “Turning crisis into opportunity: Enhancing student’ teachers’ understanding of nature of science and scientific inquiry through a case study of the scientific research in severe acute respiratory syndrome,” Int. J. Sci. Edu., vol. 30, no. 11, pp. 1417–1439, Sep. 2008, doi: 10.1080/09500690701528808. [DOI] [Google Scholar]
- [283].Tai Z. and Sun T., “The rumouring of SARS during the 2003 epidemic in China,” Sociol. Health Illness, vol. 33, no. 5, pp. 677–693, Jul. 2011, doi: 10.1111/j.1467-9566.2011.01329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [284].Wong J. G. W. S., Cheung E. P. T., Cheung V., Cheung C., Chan M. T. Y., Chua S. E., McAlonan G. M., Tsang K. W. T., and Ip M. S. M., “Psychological responses to the SARS outbreak in healthcare students in hong kong,” Med. Teacher, vol. 26, no. 7, pp. 657–659, Nov. 2004, doi: 10.1080/01421590400006572. [DOI] [PubMed] [Google Scholar]
- [285].Harris R., Nadine Wathen C., and Chan D., “Public library responses to a consumer health inquiry in a public health crisis: The SARS experience in Ontario,” Reference User Services Quart., vol. 45, no. 2, pp. 147–154, 2005. [Google Scholar]
- [286].Chui E. and Ko L., “More or less? Welfare provision amidst economic downturn–the Hong Kong experience,” J. Asian Public Policy, vol. 4, no. 1, pp. 4–17, 2011, doi: 10.1080/17516234.2011.574957. [DOI] [Google Scholar]
- [287].Lim S. H. and Sziarto K., “When the illiberal and the neoliberal meet around infectious diseases: An examination of the MERS response in South Korea,” Territory, Politics, Governance, vol. 8, no. 1, pp. 60–76, Jan. 2020, doi: 10.1080/21622671.2019.1700825. [DOI] [Google Scholar]
- [288].Zhan M., “Civet cats, fried grasshoppers, and david Beckham’s pajamas: Unruly bodies after SARS,” Amer. Anthropologist, vol. 107, no. 1, pp. 31–42, Mar. 2005, doi: 10.1525/aa.2005.107.1.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [289].Blum J. D. and Talib N., “Balancing individual rights versus collective good in public health enforcement,” Med. Law, vol. 25, no. 2, pp. 273–281, 2006. [PubMed] [Google Scholar]
- [290].Liu T., Ma J., Su B., Wang H., Wang Q., and Ma X., “A 12-year follow-up study of combined treatment of post-severe acute respiratory syndrome patients with femoral head necrosis,” Therapeutics Clin. Risk Manage., vol. 13, pp. 1449–1454, Apr. 2017, doi: 10.2147/TCRM.S140694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [291].Hung C.-F., “The politics of cyber participation in the PRC: The implications of contingency for the awareness of citizens,” Issues Stud., vol. 42, no. 4, pp. 137–173, 2006. [Google Scholar]
- [292].Chiu W.-T., Huang J.-S., and Ho Y.-S., “Bibliometric analysis of severe acute respiratory syndrome-related research in the beginning stage,” Scientometrics, vol. 61, no. 1, pp. 69–77, 2004, doi: 10.1023/B:SCIE.0000037363.49623.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [293].Tang C. F. and Tan E. C., “The determinants of inbound tourism demand in Malaysia: Another visit with non-stationary panel data approach,” Anatolia, vol. 27, no. 2, pp. 189–200, Apr. 2016, doi: 10.1080/13032917.2015.1084345. [DOI] [Google Scholar]
- [294].Ma S.-Y., “The making and remaking of a Chinese hospital in Hong Kong,” Modern Asian Stud., vol. 45, no. 5, pp. 1313–1336, Sep. 2011, doi: 10.1017/S0026749X10000107. [DOI] [Google Scholar]
- [295].Sofiah S., Hawari K., and Khatun S., “Contextual thermal face detection for fever mass screening,” Adv. Sci. Lett., vol. 23, no. 11, pp. 11330–11334, Nov. 2017, doi: 10.1166/asl.2017.10277. [DOI] [Google Scholar]
- [296].Chandler C., “SARS attacks, China shudders,” Fortune, vol. 147, no. 9, p. 32, 2003. [PubMed] [Google Scholar]
- [297].Whittaker C., Frühauf A., Burthem S. J., Parry R. S., Kotikalapudi M., Liang Y., Barker M. M., Patel P. R., and Kelman I., “A disaster diplomacy perspective of acute public health events,” Disasters, vol. 42, pp. S173–S195, Oct. 2018, doi: 10.1111/disa.12306. [DOI] [PubMed] [Google Scholar]
- [298].Xiao Y., Chen Y., Liu X., Yan Z., Cheng L., and Li M., “Oil flow analysis in the maritime silk road region using AIS data,” ISPRS Int. J. Geo-Inf., vol. 9, no. 4, p. 265, Apr. 2020, doi: 10.3390/ijgi9040265. [DOI] [Google Scholar]
- [299].Overby J., Rayburn M., Wyld D. C., and Hammond K., “Looming cognition for global competition: The approaching avian influenza pandemic,” Asia Pacific J. Marketing Logistics, vol. 17, no. 2, pp. 17–30, Jun. 2005, doi: 10.1108/13555850510672322. [DOI] [Google Scholar]
- [300].Lee S. and Paik J. E., “How partisan newspapers represented a pandemic: The case of the middle east respiratory syndrome in South Korea,” Asian J. Commun., vol. 27, no. 1, pp. 82–96, Jan. 2017, doi: 10.1080/01292986.2016.1235592. [DOI] [Google Scholar]
- [301].Ho D. C. W., Leung H. F., Wong S. K., Cheung A. K. C., Lau S. S. Y., Wong W. S., Lung D. P. Y., and Chau K. W., “Assessing the health and hygiene performance of apartment buildings,” Facilities, vol. 22, no. 3/4, pp. 58–69, Feb. 2004, doi: 10.1108/02632770410527789. [DOI] [Google Scholar]
- [302].Klymchuk S. and Zverkova T., “Using common sense in a mathematical modelling task,” Math. Teach.-Res. J., vol. 7, no. 3, pp. 1–7, 2015. [Google Scholar]
- [303].Pine R. and McKercher B., “The impact of SARS on Hong Kong’s tourism industry,” Int. J. Contemp. Hospitality Manage., vol. 16, no. 2, pp. 139–143, Mar. 2004, doi: 10.1108/09596110410520034. [DOI] [Google Scholar]
- [304].Lee A. Y. L., “Between global and local: The glocalization of online news coverage on the trans-regional crisis of SARS,” Asian J. Commun., vol. 15, no. 3, pp. 255–273, Nov. 2005, doi: 10.1080/01292980500260714. [DOI] [Google Scholar]
- [305].Bennett B., Carney T., and Saint C., “Swine flu, doctors and pandemics: Is there a duty to treat during a pandemic?” J. Law Med., vol. 17, no. 5, pp. 736–747, 2010. [PubMed] [Google Scholar]
- [306].Baehr P., “Susan sontag, battle language and the Hong Kong SARS outbreak of 2003,” Economy Soc., vol. 35, no. 1, pp. 42–64, Feb. 2006, doi: 10.1080/03085140500465840. [DOI] [Google Scholar]
- [307].Ho S. S., Brossard D., and Scheufele D. A., “The polls—trends: Public reactions to global health threats and infectious diseases,” Public Opinion Quart., vol. 71, no. 4, pp. 671–692, 2007, doi: 10.1093/poq/nfm041. [DOI] [Google Scholar]
- [308].Davis D., Ryan D., Sibbald G., Rachlis A., Davies S., Manchul L., and Parikh S., “Severe acute respiratory syndrome and the delivery of continuing medical education: Case study from Toronto,” J. Continuing Edu. Health Professions, vol. 24, no. 2, pp. 76–81, 2004, doi: 10.1002/chp.1340240204. [DOI] [PubMed] [Google Scholar]
- [309].Gao N. P., Niu J. L., Perino M., and Heiselberg P., “The airborne transmission of infection between flats in high-rise residential buildings: Tracer gas simulation,” Building Environ., vol. 43, no. 11, pp. 1805–1817, Nov. 2008, doi: 10.1016/j.buildenv.2007.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [310].Min J. C. H., Lim C., and Kung H.-H., “Intervention analysis of SARS on japanese tourism demand for taiwan,” Qual. Quantity, vol. 45, no. 1, pp. 91–102, Jan. 2011, doi: 10.1007/s11135-010-9338-4. [DOI] [Google Scholar]
- [311].Biswas P. P., “Skewed Urbanisation and the Contagion,” Econ. Political Weekly, vol. 55, no. 16, pp. 13–15, 2020. [Google Scholar]
- [312].Burrer S. L., de Perio M. A., Hughes M. M., and Kuhar D. T., “Characteristics of health care personnel with COVID-19—United States, February 12–April 9, 2020,” Morbidity Mortality Weekly Rep., vol. 69, no. 15, pp. 477–481, 2020, doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [313].Okello P. E., Majwala R. K., Kalani R., and Kwesiga B., “Investigation of a cluster of severe respiratory disease referred from Uganda to Kenya, February 2017,” Health Secur., vol. 18, no. 2, pp. 96–104, 2020, doi: 10.1089/hs.2019.0107. [DOI] [PubMed] [Google Scholar]
- [314].Gold J. A. W., “Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 18, pp. 545–550, 2020, doi: 10.15585/mmwr.mm6918e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [315].Kumar A. and Kumar M., “COVID-19 and the public health system in Bihar,” Econ. Political Weekly., vol. 55, no. 16, pp. 16–19, 2020. [Google Scholar]
- [316].C.-. R. Team C. D. C., “Geographic differences in COVID-19 cases, deaths, and incidence—United States, February 12–April 7, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 15, pp. 465–471, 2020, doi: 10.15585/mmwr.mm6915e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [317].Elaya Perumal U. and Sundararaj R., “Algae: A potential source to prevent and cure the novel coronavirus–A review,” Int. J. Emergency Technol., vol. 11, no. 2, pp. 479–483, 2020. [Google Scholar]
- [318].Ruck Keene A., “Capacity in the time of coronavirus,” Int. J. Law Psychiatry, vol. 70, May 2020, Art. no.101560, doi: 10.1016/j.ijlp.2020.101560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [319].Addo P. C., Jiaming F., Kulbo N. B., and Liangqiang L., “COVID-19: Fear appeal favoring purchase behavior towards personal protective equipment [COVID-19 (New Crown Pneumonia): Fear appeals to promote the purchase of consumer personal protective equipment],” Service Ind. J., vol. 40, nos. 7–8, pp. 471–490, 2020, doi: 10.1080/02642069.2020.1751823. [DOI] [Google Scholar]
- [320].De Vito A. and Gómez J.-P., “Estimating the COVID-19 cash crunch: Global evidence and policy,” J. Accounting Public Policy, vol. 39, no. 2, Mar. 2020, Art. no.106741, doi: 10.1016/j.jaccpubpol.2020.106741. [DOI] [Google Scholar]
- [321].Mahmoud M. A., Al-Zalabani A. H., and Bin Abdulrahman K. A., “Public health education in saudi arabia: Needs and challenges,” Med. Teacher, vol. 38, no. 1, pp. S5–S8, Mar. 2016, doi: 10.3109/0142159X.2016.1142514. [DOI] [PubMed] [Google Scholar]
- [322].Arora A. K. and Srinivasan R., “Impact of pandemic COVID-19 on the teaching–learning process: A study of higher education teachers,” Prabandhan: Indian J. Manage., vol. 13, no. 4, pp. 43–56, 2020, doi: 10.17010/pijom/2020/v13i4/151825. [DOI] [Google Scholar]
- [323].Nicoli F. and Gasparetto A., “Italy in a time of emergency and scarce resources: The need for embedding ethical reflection in social and clinical settings,” J. Clin. Ethics, vol. 31, no. 1, pp. 92–94, 2020. [PubMed] [Google Scholar]
- [324].Dyal J. W., “COVID-19 among workers in meat and poultry processing facilities—19 States, April 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 18, 2020, doi: 10.15585/mmwr.mm6918e3. [DOI] [PubMed] [Google Scholar]
- [325].Squazzoni F., Polhill J. G., Edmonds B., Ahrweiler P., Antosz P., Scholz G., Chappin É., Borit M., Verhagen H., Giardini F., and Gilbert N., “Computational models that matter during a global pandemic outbreak: A call to action,” J. Artif. Societies Social Simul., vol. 23, no. 2, 2020, doi: 10.18564/jasss.4298. [DOI] [Google Scholar]
- [326].Song P. and Karako T., “COVID-19: Real-time dissemination of scientific information to fight a public health emergency of international concern,” Biosci. Trends, vol. 14, no. 1, pp. 1–2, Feb. 2020, doi: 10.5582/BST.2020.01056. [DOI] [PubMed] [Google Scholar]
- [327].La V.-P., Pham T.-H., Ho M.-T., Nguyen M.-H., Nguyen K.-L. P., Vuong T.-T., Nguyen H.-K.-T., Tran T., Khuc Q., Ho M.-T., and Vuong Q.-H., “Policy response, social media and science journalism for the sustainability of the public health system amid the COVID-19 outbreak: The Vietnam lessons,” Sustainability, vol. 12, no. 7, p. 2931, Apr. 2020, doi: 10.3390/su12072931. [DOI] [Google Scholar]
- [328].De Vos J., “The effect of COVID-19 and subsequent social distancing on travel behavior,” Transp. Res. Interdiscipl. Perspect., vol. 5, May 2020, Art. no.100121, doi: 10.1016/j.trip.2020.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [329].Li L., Zhang Q., Wang X., Zhang J., Wang T., Gao T.-L., Duan W., Tsoi K. K.-F., and Wang F.-Y., “Characterizing the propagation of situational information in social media during COVID-19 epidemic: A case study on Weibo,” IEEE Trans. Comput. Social Syst., vol. 7, no. 2, pp. 556–562, Apr. 2020, doi: 10.1109/TCSS.2020.2980007. [DOI] [Google Scholar]
- [330].Knox S., Moghadam S., Patrick K., Phan A., and Choo K.-K. R., “What’s really ‘Happning’? A forensic analysis of Android and iOS Happn dating apps,” Comput. Secur., vol. 94, Jul. 2020, Art. no.101833, doi: 10.1016/j.cose.2020.101833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [331].Kuckertz A., Brändle L., Gaudig A., and Hinderer S., “Startups in times of crisis–A rapid response to the COVID-19 pandemic,” J. Bus. Venturing Insights, vol. 13, Jun. 2020, Art. no. e00169, doi: 10.1016/j.jbvi.2020.e00169. [DOI] [Google Scholar]
- [332].Howarth D. and Verdun A., “Economic and monetary union at twenty: A stocktaking of a tumultuous second decade: Introduction,” J. Eur. Integr., vol. 42, no. 3, pp. 287–293, Apr. 2020, doi: 10.1080/07036337.2020.1730348. [DOI] [Google Scholar]
- [333].Philippidis A., “COVID-19: Top 60 drug treatments in development,” Genetic Eng. Biotechnol. News, vol. 40, no. 4, pp. 10–13, Apr. 2020, doi: 10.1089/gen.40.04.02. [DOI] [Google Scholar]
- [334].Singh Z. D., “COVID-19 should make us re-imagine the world order,” Econ. Political Weekly., vol. 55, no. 13, pp. 10–11, 2020. [Google Scholar]
- [335].Kelly B. D., “Emergency mental health legislation in response to the COVID-19 (Coronavirus) pandemic in Ireland: Urgency, necessity and proportionality,” Int. J. Law Psychiatry, vol. 70, May 2020, Art. no.101564, doi: 10.1016/j.ijlp.2020.101564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [336].Koonin L. M., Pillai S., Kahn E. B., Moulia D., and Patel A., “Strategies to inform allocation of stockpiled ventilators to healthcare facilities during a pandemic,” Health Secur., vol. 18, no. 2, pp. 69–74, Apr. 2020, doi: 10.1089/hs.2020.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [337].Al-Awadhi A. M., Alsaifi K., Al-Awadhi A., and Alhammadi S., “Death and contagious infectious diseases: Impact of the COVID-19 virus on stock market returns,” J. Behav. Exp. Finance, vol. 27, Sep. 2020, Art. no.100326, doi: 10.1016/j.jbef.2020.100326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [338].Ghinai I., Woods S., Ritger K. A., McPherson T. D., and Black S. R., “Community transmission of SARS-CoV-2 at two family gatherings—Chicago, Illinois, February–March 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 15, pp. 446–450, 2020, doi: 10.15585/mmwr.mm6915e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [339].Levkoe C. Z., Knezevic I., Appavoo D., Moraes A., and Scott S., “Serving up food studies online: Teaching about ‘food from somewhere’ from nowhere,” Food, Culture Soc., vol. 23, no. 3, pp. 434–453, 2020, doi: 10.1080/15528014.2020.1754041. [DOI] [Google Scholar]
- [340].Wei W. E., Li Z., Chiew C. J., Yong S. E., Toh M. P., and Lee V. J., “Presymptomatic transmission of SARS-CoV-2—Singapore, January 23–March 16, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 14, pp. 411–415, 2020, doi: 10.15585/mmwr.mm6914e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [341].Kilianski A., O’Rourke A. T., Carlson C. L., Parikh S. M., and Shipman-Amuwo F., “The planning, execution, and evaluation of a mass prophylaxis full-scale exercise in Cook County, IL,” Biosecur. Bioterrorism: Biodefense Strategy, Pract., Sci., vol. 12, no. 2, pp. 106–115, 2014, doi: 10.1089/bsp.2013.0089. [DOI] [PubMed] [Google Scholar]
- [342].Gostin L. O., Friedman E. A., and Wetter S. A., “Responding to covid-19: How to navigate a public health emergency legally and ethically,” Hastings Center Rep., vol. 50, no. 2, pp. 8–12, Mar. 2020, doi: 10.1002/hast.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [343].Usuzaki T., Chiba S., and Shimoyama M., “How can we evaluate an interrelation of symptoms?” Arch. Gerontol. Geriatrics, vol. 89, Jul. 2020, Art. no.104096, doi: 10.1016/j.archger.2020.104096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [344].Seecheran R. and Narayansingh R., “Atrial Arrhythmias in a Patient Presenting With Coronavirus Disease-2019 (COVID-19) Infection,” J. Investigative Med. High Impact Case Rep., vol. 8, p. 2324709620925571, 2020, doi: 10.1177/2324709620925571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [345].Tobolowsky F. A., Gonzales E., and Self J. L., “COVID-19 outbreak among three affiliated homeless service sites—King County, Washington, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 17, pp. 523–526, 2020, doi: 10.15585/mmwr.mm6917e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [346].Heinzerling A., “Characteristics of health care personnel with COVID-19—United States, February 12–April 9, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 15, pp. 472–476, 2020, doi: 10.15585/mmwr.mm6915e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [347].Chang A., “Cleaning and disinfectant chemical exposures and temporal associations with COVID-19—National poison data system, United States, January 1, 2020–March 31, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 16, pp. 496–498, 2020, doi: 10.15585/mmwr.mm6916e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [348].Buendía J. L. and Dovalo A., “State aid versus COVID-19: The commission adopts a temporary framework,” Eur. State Aid Law Qual., vol. 19, no. 1, pp. 3–7, 2020, doi: 10.21552/estal/2020/1/4. [DOI] [Google Scholar]
- [349].Bhardwaj A., “COVID-19 and US–China Tussle,” Econ. Political Weekly, vol. 55, no. 17, pp. 10–12, 2020. [Google Scholar]
- [350].Singh B., “Media in the time of COVID-19,” Econ. Political Weekly, vol. 55, no. 16, pp. 1–6, 2020. [Google Scholar]
- [351].Lasry A., Kidder D., Hast M., Poovey J., and Sunshine G., “Timing of cmmunity mitigation and changes in reported COVID-19 and community mobility—Four US metropolitan areas, February 26–April 1, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 15, pp. 451–457, 2020, doi: 10.15585/mmwr.mm6915e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [352].Mosites E., Parker E. M., and Clarke K. E. N., “Assessment of SARS-CoV-2 infection prevalence in homeless shelters—Four US cities, March 27–April 15, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 17, pp. 521–522, 2020, doi: 10.15585/mmwr.mm6917e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [353].Cioffi A., “Professional autonomy and liability of the resident doctor: Between the hammer and the anvil,” J. Forensic Legal Med., vol. 72, May 2020, Art. no.101965, doi: 10.1016/j.jflm.2020.101965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [354].Goldkind L., LaMendola W., and Taylor-Beswick A., “Tackling COVID-19 is a crucible for privacy,” J. Technol. Hum. Services, vol. 38, no. 2, pp. 89–90, Apr. 2020, doi: 10.1080/15228835.2020.1757559. [DOI] [Google Scholar]
- [355].Bruinen De Bruin Y., Lequarre A.-S., McCourt J., Clevestig P., Pigazzani F., Zare Jeddi M., Colosio C., and Goulart M., “Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic,” Saf. Sci., vol. 128, Aug. 2020, Art. no.104773, doi: 10.1016/j.ssci.2020.104773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [356].Filipe J. A., “Epidemics and Pandemics: Covid-19 and the ‘The Drop of Honey Effect,”’ Int. J. Econ. Bus. Admin., vol. 8, no. 2, pp. 240–249, 2020, doi: 10.35808/ijeba/456. [DOI] [Google Scholar]
- [357].Prashad V., “A socialist cry for civilisational change: COVID-19 and the failure of neo-liberalism,” Econ. Political Weekly, vol. 55, no. 16, pp. 1–8, 2020. [Google Scholar]
- [358].Roxby A. C., Greninger A. L., and Hatfield K. M., “Detection of SARS-CoV-2 among residents and staff members of an independent and assisted living community for older adults—Seattle, Washington, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 14, pp. 416–418, 2020, doi: 10.15585/mmwr.mm6914e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [359].Nagano H., de Oliveira J. A., Barros A. K., and Junior A. D. S. C., “The ‘Heart Kuznets Curve’? Understanding the relations between economic development and cardiac conditions,” World Develop., vol. 132, Aug. 2020, Art. no.104953, doi: 10.1016/j.worlddev.2020.104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [360].Moriarty L. F., “Public health responses to COVID-19 outbreaks on cruise ships—Worldwide, February–March 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 12, pp. 347–352, 2020, doi: 10.15585/mmwr.mm6912e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [361].Kaila R. P. and Prasad A. K. V., “Informational flow on Twitter–Corona virus outbreak–topic modelling approach,” Int. J. Adv. Res. Eng. Technol., vol. 11, no. 3, pp. 128–134, 2020. [Online]. Available: http://www.iaeme.com/IJARET/issues.asp?JType=IJARET&VType=11&IType=3 [Google Scholar]
- [362].Iacus S. M., Natale F., Santamaria C., Spyratos S., and Vespe M., “Estimating and projecting air passenger traffic during the COVID-19 coronavirus outbreak and its socio-economic impact,” Saf. Sci., vol. 129, Sep. 2020, Art. no.104791, doi: 10.1016/j.ssci.2020.104791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [363].Mobaraki K., Salamatbakhsh M., and Ahmadzadeh J., “Standard expected years of life lost as a neglected index for calculating the burden of premature mortality due to middle east respiratory syndrome,” Health Secur., vol. 17, no. 5, pp. 407–409, Oct. 2019, doi: 10.1089/hs.2019.0074. [DOI] [PubMed] [Google Scholar]
- [364].Germain S., “Will COVID-19 mark the end of an egalitarian national health service?” Eur. J. Risk Regulation, vol. 11, no. 2, pp. 358–365, Jun. 2020, doi: 10.1017/err.2020.33. [DOI] [Google Scholar]
- [365].Zemke D. M. V., Neal J., Shoemaker S., and Kirsch K., “Hotel cleanliness: Will guests pay for enhanced disinfection?” Int. J. Contemp. Hospitality Manage., vol. 27, no. 4, pp. 690–710, May 2015, doi: 10.1108/IJCHM-01-2014-0020. [DOI] [Google Scholar]
- [366].Kamel Boulos M. N. and Geraghty E. M., “Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics,” Int. J. Health Geogr., vol. 19, no. 1, pp. 1–12, 2020, doi: 10.1186/s12942-020-00202-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [367].Nikolaou P. and Dimitriou L., “Identification of critical airports for controlling global infectious disease outbreaks: stress-tests focusing in europe,” J. Air Transp. Manage., vol. 85, Jun. 2020, Art. no.101819, doi: 10.1016/j.jairtraman.2020.101819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [368].Riley T., Sully E., Ahmed Z., and Biddlecom A., “Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low-and middle-income countries,” Int. Perspect. Sexual Reproductive Health, vol. 46, pp. 73–76, Apr. 2020, doi: 10.1363/46e9020. [DOI] [PubMed] [Google Scholar]
- [369].Team C. D., “Coronavirus disease 2019 in children—United States, February 12–April 2, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 14, pp. 422–426, 2020, doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [370].Fernandez A. A. and Shaw G. P., “Academic leadership in a time of crisis: The coronavirus and COVID-19,” J. Leadership Stud., vol. 14, no. 1, pp. 39–45, 2020, doi: 10.1002/jls.21684. [DOI] [Google Scholar]
- [371].Nicolaides P., “The corona virus can infect banks too: The applicability of the EU banking and state aid regimes,” Eur. State Aid Law Qual., vol. 19, no. 1, pp. 29–38, 2020, doi: 10.21552/estal/2020/1/7. [DOI] [Google Scholar]
- [372].Leite H., Gruber T., and Hodgkinson I. R., “Flattening the infection curve–understanding the role of telehealth in managing COVID-19,” Leadership Health Services, vol. 33, no. 2, pp. 221–226, 2019, doi: 10.1108/LHS-05-2020-084. [DOI] [Google Scholar]
- [373].Fraioli P., “Malaysia’s political crisis,” Strateg. Comments, vol. 26, no. 2, pp. 7–9, 2020, doi: 10.1080/13567888.2020.1756352. [DOI] [Google Scholar]
- [374].Shen M., “Cohesion in distancing,” AMA J. Ethics, vol. 22, no. 4, pp. E344–E345, 2020, doi: 10.1001/amajethics.2020.344. [DOI] [PubMed] [Google Scholar]
- [375].Schuchat A., “Public health response to the initiation and spread of pandemic COVID-19 in the United States, February 24–April 21, 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 18, pp. 551–556, 2020, doi: 10.15585/mmwr.mm6918e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [376].Niu S., Tian S., Lou J., Kang X., Zhang L., Lian H., and Zhang J., “Clinical characteristics of older patients infected with COVID-19: A descriptive study,” Arch. Gerontol. Geriatrics, vol. 89, Jul. 2020, Art. no.104058, doi: 10.1016/j.archger.2020.104058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [377].Wu Y., Zhu C., Li Y., Guo L., and Wu X., “NetNCSP: Nonoverlapping closed sequential pattern mining,” Knowl.-Based Syst., vol. 196, May 2020, Art. no.105812, doi: 10.1016/j.knosys.2020.105812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [378].Jones-Schenk J., “Hope as a generative force: Lifting our gaze to the future,” J. Continuing Edu. Nursing, vol. 51, no. 5, pp. 203–204, May 2020, doi: 10.3928/00220124-20200415-03. [DOI] [PubMed] [Google Scholar]
- [379].Fraioli P., “Ethiopia’s factional politics,” Strateg. Comments, vol. 26, no. 2, pp. x–xii, 2020, doi: 10.1080/13567888.2020.1762348. [DOI] [Google Scholar]
- [380].Zwald M. L., Lin W., Cooksey G. L. S., and Weiss C., “Rapid sentinel surveillance for COVID-19—Santa Clara County, California, March 2020,” MMWR. Morbidity Mortality Weekly Rep., vol. 69, no. 14, pp. 419–421, 2020, doi: 10.15585/mmwr.mm6914e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [381].Sobieralski J. B., “COVID-19 and airline employment: Insights from historical uncertainty shocks to the industry,” Transp. Res. Interdiscipl. Perspect., vol. 5, May 2020, Art. no.100123, doi: 10.1016/j.trip.2020.100123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [382].Chandler C., “Masks can’t stop this virus,” Fortune, vol. 147, no. 8, p. 42, 2003. [PubMed] [Google Scholar]
- [383].Deurenberg-Yap M., Foo L. L., Low Y. Y., Chan S. P., Vijaya K., and Lee M., “The singaporean response to the SARS outbreak: Knowledge sufficiency versus public trust,” Health Promotion Int., vol. 20, no. 4, pp. 320–326, Dec. 2005, doi: 10.1093/heapro/dai010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [384].Luo W., Su X., Gong S., Qin Y., Liu W., and Li J., “Anti-SARS coronavirus 3C-like protease effects of Rheum palmatum L. extracts,” Biosci. Trends, vol. 3, no. 4, pp. 124–126, 2009. [PubMed] [Google Scholar]
- [385].Ho B. and Tsai T., “The chairman and the coronavirus: Globalization and China’s healthcare system,” Harvard Int. Rev., vol. 25, no. 4, p. 28, 2004. [Google Scholar]
- [386].Banos A. and Lacasa J., “Spatio-temporal exploration of SARS epidemic,” Cybergeo, vol. 2007, no. 1, Nov. 2007, Art. no. 408. [Google Scholar]
- [387].Hazra J., “SARS and it’s implications,” Trans. Inst. Indian Geogr., vol. 26, no. 1, pp. 27–38, 2004. [Google Scholar]
- [388].Ealy J. B. and Kvarta V., “Mentoring an undergraduate research student in the structural and nonstructural properties of drugs,” J. Chem. Educ., vol. 83, no. 12, pp. 1779–1783, 2006. [Google Scholar]
- [389].Aevermann B. D., Pickett B. E., Kumar S., and Klem E. B., “A comprehensive collection of systems biology data characterizing the host response to viral infection,” Sci. Data, vol. 1, no. 1, Oct. 2014, Art. no.140033, doi: 10.1038/sdata.2014.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [390].Li H.-Y., Zhu G.-J., Zhang Y.-Z., Zhang L.-B., Hagan E. A., Martinez S., Chmura A. A., Francisco L., Tai H., Miller M., and Daszak P., “A qualitative study of zoonotic risk factors among rural communities in southern China,” Int. Health, vol. 12, no. 2, pp. 77–85, Mar. 2020, doi: 10.1093/inthealth/ihaa001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [391].Sun Y.-G., Li R., Jiang L., Qiao S., Zhi Y., Chen X.-X., Xie S., Wu J., Li X., Deng R., and Zhang G., “Characterization of the interaction between recombinant porcine aminopeptidase n and spike glycoprotein of porcine epidemic diarrhea virus,” Int. J. Biol. Macromolecules, vol. 117, pp. 704–712, Oct. 2018, doi: 10.1016/j.ijbiomac.2018.05.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [392].Ludolph R., Schulz P. J., and Chen L., “Investigating the effects of mass media exposure on the uptake of preventive measures by Hong Kong residents during the 2015 MERS outbreak: The mediating role of interpersonal communication and the perception of concern,” J. Health Commun., vol. 23, no. 1, pp. 1–8, Jan. 2018, doi: 10.1080/10810730.2017.1388455. [DOI] [PubMed] [Google Scholar]
- [393].Asaad A. M., El-Sokkary R. H., Aedh A. I., Alzamanan M. A. A., and Khalil F. O., “Exploring knowledge and attitude toward middle east respiratory syndrome-coronavirus (MERS-coV) among university health colleges’ students, Saudi Arabia: A cross- sectional study,” Revista Brasileira de Gestao e Desenvolvimento Regional, vol. 15, no. 1, pp. 37–43, 2019, doi: 10.3844/ajidsp.2019.37.43. [DOI] [Google Scholar]
- [394].Contreras G. W., “Getting ready for the next pandemic COVID-19: Why we need to be more prepared and less scared,” J. Emergency Manage., vol. 18, no. 2, pp. 87–89, 2020. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/32181864/ [DOI] [PubMed] [Google Scholar]
- [395].El-Kafrawy S. A., Corman V. M., and Tolah A. M., “Enzootic patterns of Middle East respiratory syndrome coronavirus in imported African and local Arabian dromedary camels: A prospective genomic study,” Lancet Planet. Health, vol. 3, no. 12, pp. e521–e528, Dec. 2019, doi: 10.1016/S2542-5196(19)30243-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [396].Ramshaw R. E., Letourneau I. D., Hong A. Y., Hon J., Morgan J. D., Osborne J. C. P., Shirude S., Van Kerkhove M. D., Hay S. I., and Pigott D. M., “A database of geopositioned middle east respiratory syndrome coronavirus occurrences,” Sci. Data, vol. 6, no. 1, p. 318, Dec. 2019, doi: 10.1038/s41597-019-0330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [397].Wang Z., Chen X., Lu Y., Chen F., and Zhang W., “Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined chinese and western medicine treatment,” Biosci. Trends, vol. 14, no. 1, pp. 64–68, Feb. 2020, doi: 10.5582/bst.2020.01030. [DOI] [PubMed] [Google Scholar]
- [398].Youde J., “MERS and global health governance,” Int. J., Canada’s J. Global Policy Anal., vol. 70, no. 1, pp. 119–136, Mar. 2015, doi: 10.1177/0020702014562594. [DOI] [Google Scholar]
- [399].Lu H., “Drug treatment options for the 2019-new coronavirus (2019-nCoV),” Biosci. Trends, vol. 14, no. 1, pp. 69–71, Feb. 2020, doi: 10.5582/bst.2020.01020. [DOI] [PubMed] [Google Scholar]
- [400].Tian D., Yu Y., Wang Y., and Zheng T., “Comparison of trends in the quantity and variety of science citation index (SCI) literature on human pathogens between China and the united states,” Scientometrics, vol. 93, no. 3, pp. 1019–1027, Dec. 2012, doi: 10.1007/s11192-012-0772-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [401].Attenborough F. T., “Severe acute respiratory syndrome (SARS) and the rhetorical construction of ‘bad’ scientific work,” Public Understand. Sci., vol. 21, no. 2, pp. 211–225, Feb. 2012, doi: 10.1177/0963662510371436. [DOI] [PubMed] [Google Scholar]
- [402].Mukherjee P., Shah F., Desai P., and Avery M., “Inhibitors of SARS-3CLpro: Virtual screening, biological evaluation, and molecular dynamics simulation studies,” J. Chem. Inf. Model., vol. 51, no. 6, pp. 1376–1392, Jun. 2011, doi: 10.1021/ci1004916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [403].Joo H., Maskery B. A., Berro A. D., Rotz L. D., Lee Y.-K., and Brown C. M., “Economic impact of the 2015 MERS outbreak on the republic of Korea’s tourism-related industries,” Health Secur., vol. 17, no. 2, pp. 100–108, Apr. 2019, doi: 10.1089/hs.2018.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [404].Pacios L. F., Tordesillas L., Palacín A., Sánchez-Monge R., Salcedo G., and Díaz-Perales A., “LocaPep: Localization of epitopes on protein surfaces using peptides from phage display libraries,” J. Chem. Inf. Model., vol. 51, no. 6, pp. 1465–1473, Jun. 2011, doi: 10.1021/ci200059c. [DOI] [PubMed] [Google Scholar]
- [405].Wendelboe A. M., Miller J. D. A., and Drevets D., “Tabletop exercise to prepare institutions of higher education for an outbreak of COVID-19,” J. Emergency Manage., vol. 18, no. 2, pp. 1–20, 2020, doi: 10.5055/jem.2020.0464. [DOI] [PubMed] [Google Scholar]
- [406].Rahmatizadeh S., Valizadeh-Haghi S., Kalavani A., and Fakhimi N., “Middle east respiratory syndrome on health information websites: How much credible they are?” Library Philosophy Pract., to be published.
- [407].Attenborough F., “The monad and the nomad: Medical microbiology and the politics and possibilities of the mobile microbe,” Cultural Geographies, vol. 18, no. 1, pp. 91–114, Jan. 2011, doi: 10.1177/1474474010379304. [DOI] [Google Scholar]
- [408].Leshem E., “Severe respiratory illness associated with a novel coronavirus–Saudi Arabia and Qatar, 2012,” Morbidity Mortality Weekly Rep., vol. 67, no. 40, p. 820, Oct. 2012, doi: 10.1001/jama.2012.31393. [DOI] [PubMed] [Google Scholar]
- [409].Kostoff R. N. and Morse S. A., “Structure and infrastructure of infectious agent research literature: SARS,” Scientometrics, vol. 86, no. 1, pp. 195–209, Jan. 2011, doi: 10.1007/s11192-010-0240-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [410].French M. and Monahan T., “Dis-ease surveillance: How might surveillance studies address COVID-19?” Surveill. Soc., vol. 18, no. 1, pp. 1–11, Mar. 2020, doi: 10.24908/ss.v18i1.13985. [DOI] [Google Scholar]
- [411].Deshpande A., Mcmahon B., Daughton A. R., Abeyta E. L., Hodge D., Anderson K., and Pillai S., “Surveillance for emerging diseases with multiplexed Point-of-Care diagnostics,” Health Secur., vol. 14, no. 3, pp. 111–121, Jun. 2016, doi: 10.1089/hs.2016.0005. [DOI] [PubMed] [Google Scholar]
- [412].Choi J.-S. and Kim J.-S., “Factors influencing preventive behavior against middle east respiratory syndrome-coronavirus among nursing students in South Korea,” Nurse Edu. Today, vol. 40, pp. 168–172, May 2016, doi: 10.1016/j.nedt.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [413].Gasta naduy P. A., “Update: severe respiratory illness associated with Middle East respiratory syndrome coronavirus (MERS-CoV)—Worldwide, 2012–2013,” Morbidity Mortality Weekly Rep., vol. 62, no. 23, pp. 480–483, Jun. 2013, doi: 10.1111/ajt.12456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [414].Song J., Song T. M., Seo D.-C., Jin D.-L., and Kim J. S., “Social big data analysis of information spread and perceived infection risk during the 2015 middle east respiratory syndrome outbreak in South Korea,” Cyberpsychol., Behav., Social Netw., vol. 20, no. 1, pp. 22–29, Jan. 2017, doi: 10.1089/cyber.2016.0126. [DOI] [PubMed] [Google Scholar]
- [415].Wang P., Chen K., Zhu S., Wang P., and Zhang H., “Severe air pollution events not avoided by reduced anthropogenic activities during COVID-19 outbreak,” Resour., Conservation Recycling, vol. 158, Jul. 2020, Art. no.104814, doi: 10.1016/j.resconrec.2020.104814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [416].Kim K., Yoon H. Y., and Jung K., “Resilience in risk communication networks: Following the 2015 MERS response in South Korea,” J. Contingencies Crisis Manage., vol. 25, no. 3, pp. 148–159, Sep. 2017, doi: 10.1111/1468-5973.12180. [DOI] [Google Scholar]
- [417].Balajee S. A., Arthur R., and Mounts A. W., “Global health security: Building capacities for early event detection, epidemiologic workforce, and laboratory response,” Health Secur., vol. 14, no. 6, pp. 424–432, Dec. 2016, doi: 10.1089/hs.2015.0062. [DOI] [PubMed] [Google Scholar]
- [418].Shannon G. W. and Willoughby J., “Severe acute respiratory syndrome (SARS) in asia: A medical geographic perspective,” Eurasian Geography Econ., vol. 45, no. 5, pp. 359–381, Jul. 2004, doi: 10.2747/1538-7216.45.5.359. [DOI] [Google Scholar]
- [419].WHO COVID-19 Dashboard. Accessed: Apr. 18, 2020. [Online]. Available: https://covid19.who.int/ [Google Scholar]