Significance
Zika virus (ZIKV) circulated undetectably for decades until its recent outbreak from 2015 to 2017. Our study demonstrated that a mutation in the ZIKV capsid protein (C-T106A) significantly increased the epidemic potential of ZIKV over its transmission cycle by promoting the efficient assembly of ZIKV virions. Our results offer additional evidence about the evolutionary enhancement of ZIKV infectivity in mammalian hosts and mosquitoes, potentially improving our understanding of the potential relationships between ZIKV evolution and the occasional widespread reemergence in nature.
Keywords: Zika virus, mutation, evolutionary adaptation, mosquito, host
Abstract
Zika virus (ZIKV) caused millions of infections during its rapid and expansive spread from Asia to the Americas from 2015 to 2017. Here, we compared the infectivity of ZIKV mutants with individual stable substitutions which emerged throughout the Asian ZIKV lineage and were responsible for the explosive outbreaks in the Americas. A threonine (T) to alanine (A) mutation at the 106th residue of the ZIKV capsid (C) protein facilitated the transmission by its mosquito vector, as well as infection in both human cells and immunodeficient mice. A mechanistic study showed that the T106A substitution rendered the C a preferred substrate for the NS2B-NS3 protease, thereby facilitating the maturation of structural proteins and the formation of infectious viral particles. Over a complete “mosquito-mouse-mosquito” cycle, the ZIKV C-T106A mutant showed a higher prevalence of mosquito infection than did the preepidemic strain, thus promoting ZIKV dissemination. Our results support the contribution of this evolutionary adaptation to the occasional widespread reemergence of ZIKV in nature.
Zika virus (ZIKV), a mosquito-borne arbovirus belonging to the genus Flavivirus, is transmitted to humans by multiple Aedes mosquito species, such as Aedes aegypti and Aedes albopictus (1–3). This virus circulating between primates and mosquitoes has been in obscurity for decades, causing sporadic human ZIKV infections with no major outbreaks before 2007 (3, 4). Recorded, mild ZIKV outbreaks started in 2007 on the Yap Islands of the Federated States of Micronesia in the western Pacific Ocean, followed by larger epidemics in French Polynesia in the South Pacific (1, 5). Since 2015, ZIKV emerged for the first time in the Americas and rapidly became widespread in 20 countries or territories (6). By 2017, the estimated number of suspected ZIKV infection cases ranged from 223,477 to 1,003,509 (Pan American Health Organization/World Health Organization). Since neurological complications were caused by ZIKV infection, such as Guillain-Barré syndrome in adults and microcephaly in neonates (7, 8), the ZIKV epidemic was declared as an international health emergency by the World Health Organization in 2016.
Moreover, since mosquito-borne viruses efficiently maintain their lifecycle by switching between vertebrate hosts and mosquito vectors, their transmission might be influenced by their capacity of adapting to native hosts. Numerous studies have demonstrated that this evolutionary adaptation often relies on the acquisition of mutations in the viral genome (9, 10). For example, specific amino acid substitutions significantly influenced the preferred vector species involved in the urban transmission of chikungunya virus and promoted its potential of epidemic emergence (10). Given the sudden and overwhelmingly large epidemic from 2015 to 2016, one hypothesis explaining the rapid emergence is that ZIKV acquired some adaptive mutations to enhance its adaptability and infectivity, which resulted in a rapid outbreak in the Americas (11–16). Phylogenetic studies have revealed that ZIKV has evolved into African and Asian clusters (3, 6). The outbreaks in Micronesia, the South Pacific islands, and the Americas were caused by the Asian clade (3). An amino acid substitution from alanine (Ala/A) to valine (Val/V) in nonstructural protein 1 (NS1) of the Asian ZIKV lineage enhanced ZIKV infectivity in A. aegypti by enhancing NS1 antigenemia in infected hosts (12) and in mice by regulating the interferon pathway (13). Other amino acid substitutions in the ZIKV envelope (E) protein or premembrane (prM) protein increased its neurovirulence and caused more severe microcephaly in the mouse fetus (11). Additionally, by comparing the ZIKV genomes of African and Asian lineage, four initial substitutions were found to impair ZIKV fitness in both mosquitoes and mice, while the simultaneous reversion of these four mutations restored fitness (17). Nonetheless, the impact of stable mutations on ZIKV pathogenicity and infectivity in native hosts has yet to be fully elucidated.
Results
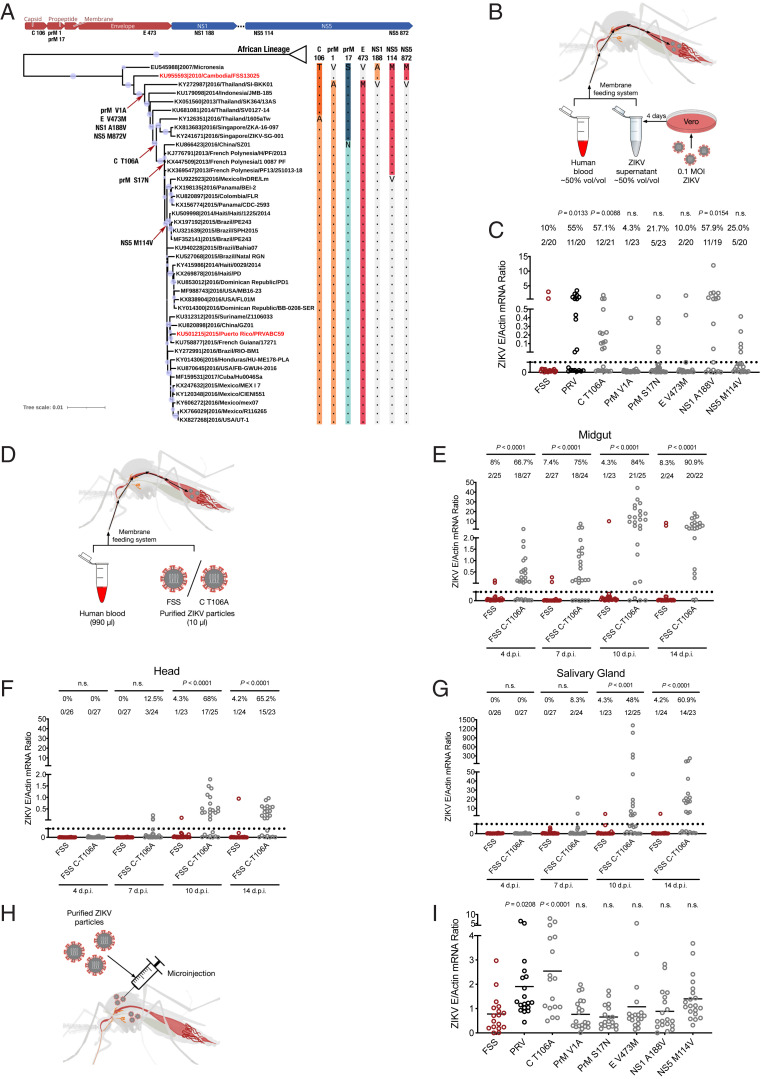
Phylogenetic analysis has revealed seven individual substitutions emerging throughout the genomes of the Asian ZIKV lineage, which have remained stable in the contemporary isolates responsible for the explosive outbreaks in the Americas (14) (Fig. 1A). Since the FSS13025 strain represents the clade corresponding to the preepidemic ZIKV that was prevalent in Southeastern Asia (2007 to 2012) (18), in an infectious clone of this strain, we generated seven ZIKV mutants with those single-residue substitutions, namely FSS-C (capsid) T106A, FSS-prM V1A, FSS-prM S17N, FSS-E V473M, FSS-NS1 A188V, FSS-NS5 (nonstructural protein 5) M114V, and FSS-NS5 M872V. Except for the FSS-NS5 M872V mutant for which the viral titer was reduced, the other mutants replicated well with peak viral titers that are comparable to that of the wild type (SI Appendix, Fig. S1A). They also formed plaques of similar sizes on Vero cells (SI Appendix, Fig. S1B). For comparing the infectivity and prevalence of these ZIKV mutants in A. aegypti mosquitoes, we infected Vero cells with them and collected the culture supernatant 4 d postinfection (dpi) for the following mosquito-feeding experiment. Although the growth curves of these ZIKV mutants were variable, the ZIKV titers in the supernatant were similar at 4 dpi (SI Appendix, Fig. S1C). A mixture containing the supernatant from ZIKV-infected Vero cells (50% volume/volume) and human blood (50% volume/volume) was used to feed A. aegypti via a membrane blood–feeding system (Fig. 1B). The PRVABC59 strain, which represents the clade of epidemic ZIKV in the Americas (2015 to 2016), served as a positive control. Around 8 d postblood meal, ZIKV infectivity was determined by qRT-PCR. Comparing with the parental FSS13025 ZIKV, the ZIKV infection rate and viral loads in the mosquitoes were significantly enhanced by a single substitution of threonine (Thr/T) with Ala at the 106th residue of the C protein (FSS-C T106A) or Ala with Val at the 188th residue of the NS1 protein (FSS-NS1 A188V) (Fig. 1C). In fact, the NS1 A188V substitution has been found to enhance the infectivity of ZIKV in mosquitoes by augmenting NS1 antigenemia in infected mice (12). The high abundance of secreted NS1 in the host blood impaired the mosquito midgut immune barrier, enhancing ZIKV acquisition by a blood meal (19). To exclude any confounding effects caused by secreted NS1, we purified the virions from the supernatant of ZIKV-infected Vero cells. However, comparing the mosquitoes feeding on human whole blood mixed with either the purified FSS-NS1 A188V or its parental FSS13025 virions (990 µL human blood and 10 µL virion), the ZIKV infection rate and viral loads were similar (SI Appendix, Fig. S2 A and B). These data suggest that NS1 A188V does not directly regulate ZIKV infectivity in A. aegypti. Nonetheless, the A. aegypti mosquitoes feeding on purified FSS-C T106A virions (resuspended in human blood) presented a higher infection rate and viral loads than those infected by the parental FSS13025 strain (Fig. 1 D–G). Similar results were noted for the field-derived A. aegypti Danzhou strain (SI Appendix, Fig. S3). These data suggest that the C-T106A mutation directly enhances ZIKV infectivity in mosquitoes. To validate this finding, we next microinjected 50 plaque-forming units (p.f.u.) of purified ZIKV into female A. aegypti mosquitoes intrathoracically (to bypass the gut barrier) (Fig. 1H). The ZIKV burden was determined at 6 dpi by qRT-PCR. The ZIKV FSS-C T106A loads were significantly higher than those of FSS13025 in A. aegypti (Fig. 1I). The viral titer of FSS-C T106A was higher than that of its parental FSS13025 in both the A. albopictus C6/36 and A. aegypti Aag2 cell lines (SI Appendix, Fig. S4). Moreover, in a competition fitness assay, the FSS-C T106A strain was mixed with FSS13025 at a p.f.u. ratio of 1:1 for the initial infection of A. aegypti. At 14 dpi, better fitness of the FSS-C T106A strain over FSS13025 was confirmed by next-generation sequencing (SI Appendix, Fig. S5 B and D). Overall, our data suggest that, in contrast to the NS1 A188V substitution (12), the T106A substitution in the C protein directly facilitates ZIKV infectivity in mosquitoes.
Fig. 1.
The effect of C-T106A substitution on the infectivity and prevalence of A. aegypti mosquitoes. (A) Phylogenetic analysis. Evolutionary mutations among ZIKV strains are indicated at the branch points of the phylogenetic tree. Asian lineage strains FSS13025 and PRVABC59, representing preepidemic and contemporary isolates, are indicated by red labels. The complete open reading frame nucleotide sequences of 47 representative ZIKV strains were aligned and analyzed using the maximum likelihood method with 1,000 bootstrap replicates in the MEGA X program. (B and C) Infectivity of ZIKV mutants in mosquitoes. Vero cells were infected with viruses at a multiplicity of infection (MOI) of 0.1, and the culture supernatant was collected 4 dpi. ZIKV-infected Vero cell supernatants (500 μL) were mixed with fresh human blood (500 μL) for the membrane feeding of A. aegypti. The number at the top of each column represents the infected number/total number. (D–G) Vector competence of A. aegypti to the ZIKV FSS13025 strain or FSS-C T106A mutant. Purified ZIKV virions (10 μL) were mixed with fresh human blood (990 μL) for the membrane feeding of A. aegypti. A final concentration of 1 × 106 p.f.u. ⋅ mL−1 ZIKV was used for mosquito oral infection. The mosquito midguts, heads, and salivary glands were dissected at 4, 7, 10, and 14 d postfeeding. The ZIKV infection (E), dissemination (F), and transmission (G) rates were determined by taking the number of infected midguts (E), heads (F), and salivary glands (G) divided by the total number of engorged mosquitoes. (H and I) The infectivity of ZIKV with single–amino acid mutations in mosquito hemocoel tissues. A. aegypti mosquitoes were infected intrathoracically with 50 p.f.u. of purified ZIKV particles. (C, E–G, and I) Each dot represents a mosquito. P values were determined by the two-sided Fisher’s exact test (C and E–G) or the two-tailed Mann–Whitney U test (I). (C, E–G, and I) P > 0.5 not significant (n.s.). P values were adjusted using the Benjamini–Hochberg procedure (C) or the Dunnett’s test (I) to account for multiple comparisons. (C and I) The P value represents a comparison between the FSS13025 and the other groups. (C, E–G, and I) The limit of detection is illustrated by dotted lines. (C, E–G, and I) Experiments consisted of at least three biological replicates with similar results. FSS and PRV represent the ZIKV FSS13025 and PRVABC59 strains, respectively.
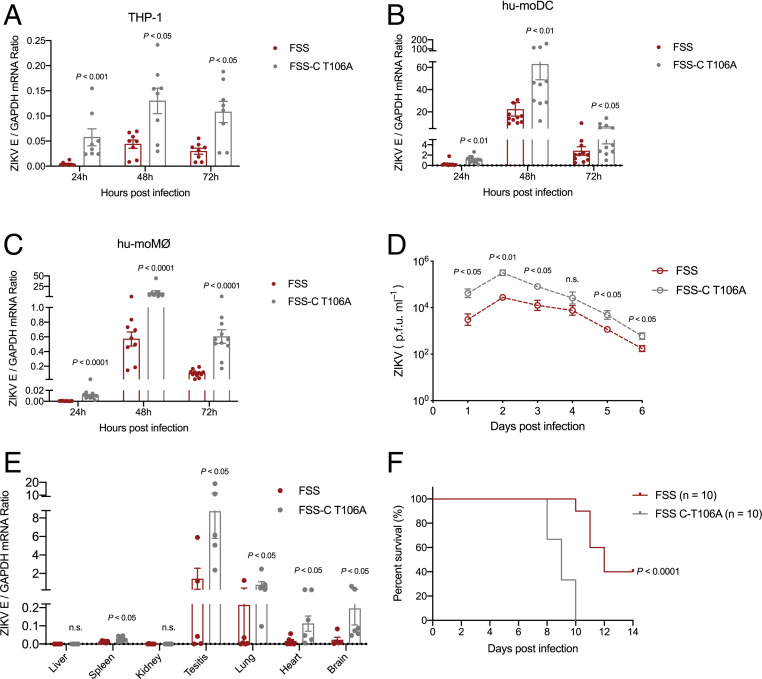
Both humans and mosquitoes are native hosts of the ZIKV transmission lifecycle. Given the role of the C-T106A substitution in mosquitoes, we next investigated this substitution in regulating ZIKV infectivity in mammalian hosts. The FSS-C T106A mutant exhibited much higher infectivity than the FSS13025 strain in multiple human susceptible cells, such as the human monocyte THP-1 cell line (Fig. 2A), human primary monocyte-derived dendritic cells (hu-moDC) (Fig. 2B) and macrophages (hu-moMØ) (Fig. 2C). To address the impact of the C-T106A mutation on ZIKV infectivity and pathogenicity in mammalian hosts, we infected a type I interferon receptor-deficient (ifnar1−/−) 129 mouse (A129 mouse) subcutaneously with 50 p.f.u. of either FSS13025 or FSS-C T106A in one footpad. The A129 mouse is an animal model that is commonly used to study ZIKV infection (20). The FSS-C T106A mutant developed higher viremia than FSS13025 did during the entire course of the infection (Fig. 2D). Consistently, the infection with the FSS-C T106A mutant resulted in a higher viral burden in other mouse tissues (Fig. 2E) and higher mortality (Fig. 2F). In addition, a higher ratio of the FSS-C T106A strain was detected in the mouse viremia by a competition fitness assay (SI Appendix, Fig. S5 B and E). Overall, the C-T106A mutation renders ZIKV more infectious and pathogenic in mammalian hosts.
Fig. 2.
The effect of C-T106A substitution on infectivity in mammalian hosts. (A–C) Replication kinetics of FSS13025 and FSS-C T106A viruses on THP-1 cells (A), hu-moDC (B), and hu-moMØ (C). The cells were infected with 0.1 MOI of the indicated viruses. The infected cells were detected at 24, 48, and 72 h postinfection by qRT-PCR, and the ZIKV quantities were normalized against human GAPDH. (D–F) Comparison of A129 mouse infection by FSS13025 and FSS-C T106A viruses. The 6-wk-old A129 mice were infected with 50 p.f.u. of FSS13025 or FSS-C T106A virus by footpad inoculation. (D) Viraemia detection. The viremia from infected A129 mice (n = 6 per group pooled from three independent biological replicates) was measured over a time course using a plaque assay. (E) Viral loads in mice tissues. At day 7 postinfection, the animals were euthanized, and the viral load in tissues was measured by qRT-PCR. (F) Animal mortality was recorded daily in the animals infected with either the FSS13025 or FSS-C T106A viruses (n = 10 mice per group pooled from three independent biological replicates). (A–E) The data are presented as the means ± SEM. (A–E) The two-tailed Mann–Whitney U test was performed for statistical analysis. (F) The survival rates of the infected mice were plotted using a Kaplan–Meier curve and were statistically analyzed using the log-rank (Mantel–Cox) test. (A–F) P > 0.5 not significant (n.s.). (A–E) Experiments consisted of at least three biological replicates with similar results. FSS represents the ZIKV FSS13025 strain.
The PRVABC59 strain contains C-106A and is more infectious than FSS13025, which contains C-106T (Fig. 1C). We then questioned whether the enhanced infectivity of PRVABC59 was predominantly due to the difference in the C-106 residue. To address this issue, we reversed C-106A to T in PRVABC59, naming this strain “PRV-C A106T.” The ZIKV particles were purified, resuspended in human blood (990 µL human blood and 10 µL virion), and were used to feed A. aegypti via a membrane blood–feeding system (SI Appendix, Fig. S6A). Compared with the PRVABC59 strain, the acquisition of PRV-C A106T resulted in a significant reduction in the ZIKV infection rate and viral loads by A. aegypti (SI Appendix, Fig. S6 B–D). Consistently, the PRV-C A106T mutant presented lower infectivity than the PRVABC59 strain in hu-moDC and hu-moMØ (SI Appendix, Fig. S7), further confirming that the C-106th residue is a key determinant of ZIKV infectivity in its mammalian hosts and mosquito vectors.
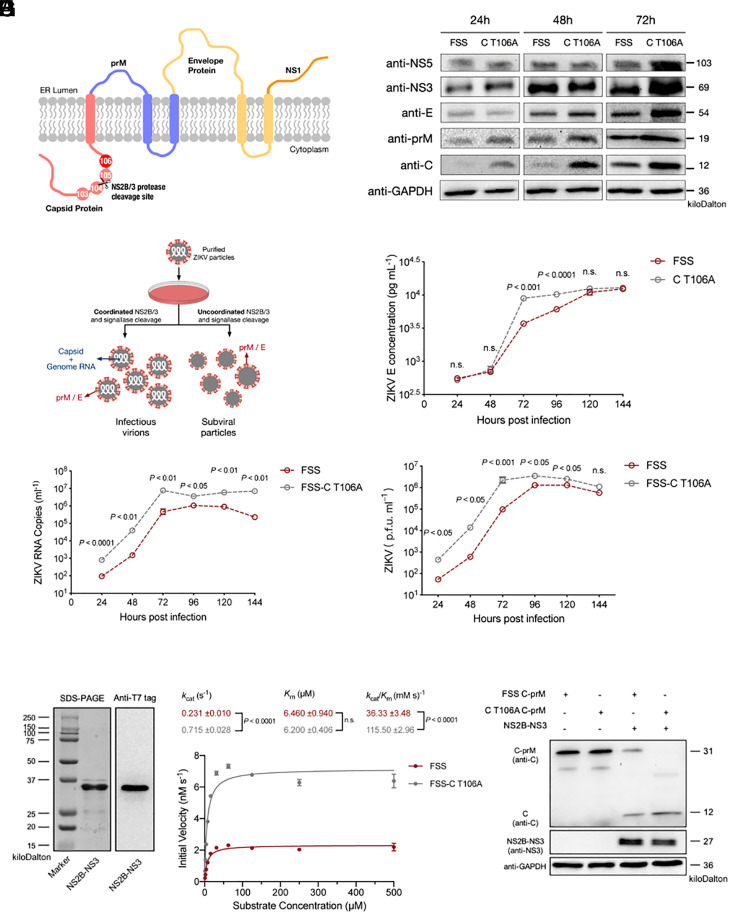
We next aimed to address the mechanism through which the C-T106A substitution promoted ZIKV infection. Common to all flaviviruses, the ZIKV genome encodes a single polyprotein that is cleaved into three structural proteins (C, prM, and E) and seven nonstructural proteins (21). The polyprotein traverses the endoplasmic reticulum (ER) membrane multiple times and is proteolytically processed on the luminal side of the ER membrane by host enzyme signalases and on the cytoplasmic side by a virus-encoded, trypsin-like serine (Ser) protease (NS2B-NS3) (22) (Fig. 3A). In fact, the cleavage of the structural proteins C and prM is a key requirement for flavivirus assembly (22). A motif surrounding the cleavage site located ∼20 amino acids toward the amino terminus of the prM protein plays a significant role in NS2B-NS3–mediated cleavage. Mutants at the basic residues of this motif exhibit severe defects in viral growth in vitro and in vivo (23). Intriguingly, the C-106th position is within this cleavage motif, immediately next to the NS2B-NS3 protease cleavage site (Fig. 3A). We therefore speculated that the C-106th residue is a key determinant of the efficiency of C cleavage by the NS2B-NS3 protease. To test this hypothesis, we collected cell lysates from Vero cells infected with either the FSS13025 or FSS-C T106A strains over a time course. The abundance of multiple ZIKV proteins was assessed by immunoblotting. While the expression levels of E and nonstructural proteins were similar between FSS-C T106A– and FSS13025–infected cells at both 24 and 48 hours post infection (hpi), the C level was significantly higher in FSS-C T106A–infected than in FSS13025-infected cells (Fig. 3B and SI Appendix, Fig. S8 A, B, G, and H). Intriguingly, the C-T106A substitution also slightly enhanced the amount of prM protein (Fig. 3B and SI Appendix, Fig. S8 D and E). Nonetheless, the C, prM, and E protein abundances were all augmented significantly at 72 hpi (Fig. 3B and SI Appendix, Fig. S8 C, F, and I). Similar results were also observed in secreted virions (SI Appendix, Fig. S9). This phenotype could be attributed to the higher infectivity of FSS-C T106A compared to its parental virus. The effective cleavage of a C-prM polyprotein plays a crucial role in nucleocapsid assembly into flaviviral particles, and it acts as a key determinant for the formation of infectious virions (24, 25). Given that the recombinant expression of prM and E proteins generates noninfectious subviral particles (SVPs) without nucleocapsids (26), we presumed that impairing C cleavage might result in SVP generation rather than infectious viral particles (21) (Fig. 3C). Either FSS13025 or FSS-C T106A ZIKV was used to infect Vero cells over a time course. The supernatant of ZIKV-infected cells was collected to assess the generation of virus-encoded proteins, viral genomes, and infectious particles. Within the initial 48 h after infection, there was no difference between the E protein levels in the supernatant of FSS13025 and that of FSS-C T106A–infected Vero cells (Fig. 3D). Nonetheless, higher abundances of ZIKV genomes (Fig. 3E) and infectious ZIKV virions (Fig. 3F) were detected in the supernatant of FSS-C T106A–infected cells. The ratios of E protein to the number of p.f.u. and to the ZIKV genome copy numbers were also calculated, and both were lower in the supernatant of FSS-C T106A–infected cells (SI Appendix, Fig. S10). These data suggest that the C-T106A mutation may result in a more efficient assembly of the nucleocapsid, thereby promoting ZIKV maturation from host cells.
Fig. 3.
The C-T106A substitution promotes ZIKV infection through more efficient C maturation. (A) Schematic representation of ZIKV structural proteins and the viral Ser protease NS2B-NS3 cleavage site on the C protein. (B) Expression of viral proteins in FSS13025- or FSS-C T106A–infected Vero cells. The cells were infected with 0.1 MOI of each virus. At 24, 48, and 72 h postinfection, the infected cells were collected for SDS-PAGE and Western blot analysis. (C) Schematic representation of the ZIKV virion assembly resulting from NS2B-NS3 Ser protease and host signalase cleavage. (D–F) The C-T106A mutation promotes the efficient production of infectious virions. Vero cells were infected with 0.1 MOI of FSS or FSS-C T106A virus. The culture supernatant was collected at the indicated time points postinfection. (D) The concentration of the ZIKV E protein in the collected supernatant was determined by ELISA. (E) The quantity of the ZIKV genome in the collected supernatant was detected by qRT-PCR. (F) The quantity of ZIKV infectious virions in the collected supernatant was detected by the plaque assay. (G and H) The C-T106A substitution promoted NS2B-NS3 Ser protease-mediated cleavage activity. (G) Purification of a recombinant NS2B-NS3 protein with an E. coli expression system. The protein was detected by staining with Coomassie blue in an SDS-PAGE gel and by Western blotting using an anti-T7 tag antibody. (H) The protease activity of recombinant NS2B-NS3 was measured using Abz/Dnp-labeled FSS13025 or FSS-C T106A peptide substrates. The assays were performed in triplicate at 37 °C using a 10-nM enzyme concentration with varying substrate concentrations starting from 500 μM. The Michaelis–Menten kinetics were plotted using a nonlinear regression function. The catalytic rates, the binding affinity of the substrate, and catalytic efficiency are mentioned in the table inset in the graph. (I) Cleavage of C-prM by the NS2B-NS3 protease. The ZIKV NS2B-NS3 protease and ZIKV FSS C-prM proteins with either Thr-106 or Ala-106 substitution were ectopically coexpressed in 293T cells, and the cell lysates were analyzed using Western blotting at 48-h posttransfection. GAPDH expression was used as a loading control. (D–F) The data are presented as the means ± SEM. (D–F) The two-tailed Mann–Whitney U test was performed for statistical analysis. (B, D–G, and I) Experiments consisted of at least three biological replicates with similar results. (H) The data were pooled from four independent biological replicates, and the data are presented as the means ± SD. (H) The P values were determined by the Student’s unpaired t test. (D–F and H) P > 0.5 not significant (n.s.). FSS represents the ZIKV FSS13025 strain.
To process the C-prM peptide, the NS2B-NS3 protease is required to recognize and subsequently mediate cleavages in this peptide. We next assessed whether the C-T106A substitution influenced the enzymatic kinetics between the NS2B-NS3 protease and the C-prM peptide. A ZIKV NS2B-NS3 recombinant protein was expressed and purified using an Escherichia coli expression system (Fig. 3G). The 2-aminobenzoyl/2,4-dinitrophenyl (Abz/Dnp)–labeled 10–amino acid peptides, which contained the NS2B-NS3 cleavage site with either a Thr-106 (Abz-KKRRGTDTSV-Dnp) or an Ala-106 (Abz-KKRRGADTSV-Dnp) substitution, were used in the protease activity assay. Although the affinity values (Km) were 6.460 ± 0.940 μM for Thr-106 peptide and 6.200 ± 0.406 μM for Ala-106 peptide, the catalytic rates were 0.231 ± 0.010 and 0.715 ± 0.028 Abz substrate molecules/s/enzyme molecule, respectively, indicating that the Thr to Ala substitution in the C-106th position resulted in a faster turnover rate and higher catalytic efficiency (Fig. 3H). To address this finding further, we next ectopically coexpressed the ZIKV NS2B-NS3 and ZIKV FSS13025 C-prM proteins with either a Thr-106 or an Ala-106 substitution in 293T cells. The protein with the Ala-106th substitution, but not that with the Thr-106th residue, was completely cleaved by the NS2B-NS3 protease (Fig. 3I). Altogether, these data show that the C-T106A substitution renders the C a preferred substrate of NS2B-NS3, thereby facilitating the maturation of the structural proteins and the formation of infectious viral particles.
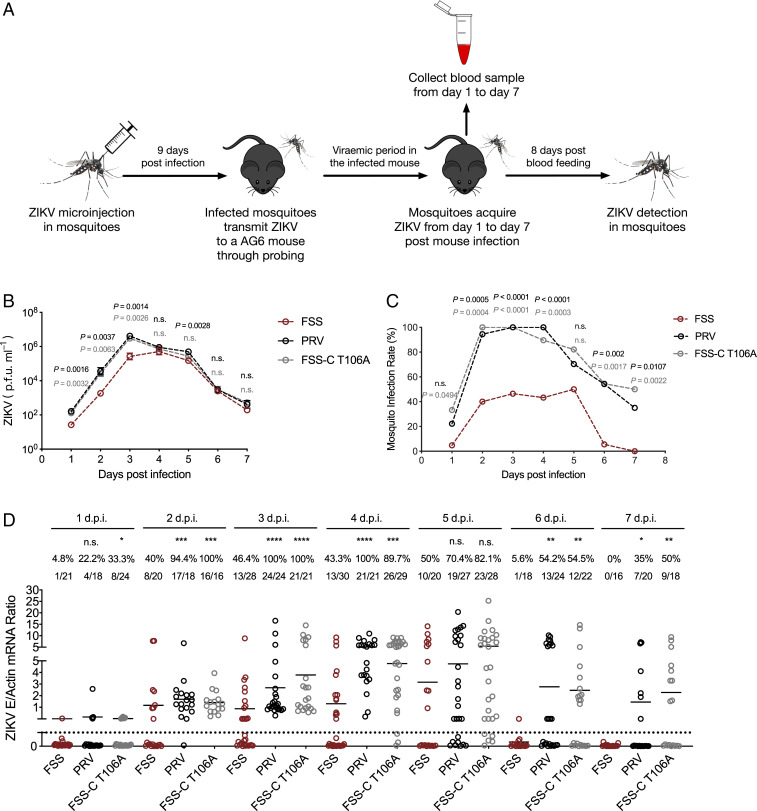
Since the C-T106A substitution robustly enhances ZIKV infectivity in both mosquitoes and mice, we next investigated whether this mutation influenced ZIKV prevalence via a “mosquito–AG6 mice–mosquito” transmission cycle. We intrathoracically microinjected female A. aegypti mosquitoes with an equal titer (50 p.f.u.) of three ZIKV strains, the FSS13025 strain, the FSS-C T106A mutant strain, and the PRVABC59 strain. Around 9 d after viral inoculation, one infected mosquito was allowed to feed on each AG6 mouse (Fig. 4A). Animals that were exposed to infected mosquitoes developed detectable viremia for all three ZIKV strains (Fig. 4B), suggesting that these three ZIKV strains could be efficiently transmitted from infected mosquitoes to mammalian hosts. The infected mice were subsequently subjected to daily probing by naïve A. aegypti from days 1 to 7 postmouse infection. A total of 10 female mosquitoes were fed on one mouse per day. The mouse blood–fed mosquitoes were maintained for an additional 8 d and then euthanized to determine their ZIKV burden by using qRT-PCR (Fig. 4A). Over a transmission cycle, the percentage of mosquitoes infected by the PRVABC59 strain was similar to that infected by the FSS-C T106A strain; however, the FSS-C T106A strain showed a significantly higher prevalence of mosquito infection than did the FSS13025 strain (Fig. 4 C and D). Similarly, better fitness of the FSS-C T106A strain over FSS13025 was observed in a competition fitness assay in the mosquito–AG6 mice–mosquito transmission cycle (SI Appendix, Fig. S5 B and F). The stability of the C-T106A substitution was also confirmed by consecutively passaging the FSS-C T106A infectious, clone-derived virus in Vero cells and C6/36 cells or in these two cell lines alternatively eight times (SI Appendix, Fig. S11). These results indicate that the C-T106A substitution greatly increases the permissiveness of the native hosts to ZIKV, thereby promoting the dissemination of ZIKV through a “host–mosquito” transmission cycle in nature.
Fig. 4.
The C-T106A substitution promotes both ZIKVs during the mosquito-host-mosquito lifecycle. (A) Schematic representation of the study design. (B) Detection of ZIKV viremia by the plaque assay (n = 3 mice per group). (C and D) Comparison of the infection rate (C) and mosquito infectivity (D) of the ZIKV strains (n = 3 mice per group). (D) The number at the top of each column represents the infected number/total number. (D) Each dot represents a mosquito. (B and C) The data are the means ± SEM. The P values were determined by the two-tailed Mann–Whitney U test (B and D) or the two-sided Fisher’s exact test (C). P values were adjusted using the Dunnett’s test (B) or the Benjamini–Hochberg procedure (C and D) to account for multiple comparisons. The black P value represents a comparison between FSS13025 and PRVABC59. The gray P value represents a comparison between FSS13025 and FSS-C T106A. *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001; and n.s., not significant. (D) The limit of detection is illustrated by dotted lines. (B–D) Experiments consisted of at least three biological replicates with similar results. FSS and PRV represent the ZIKV FSS13025 and PRVABC59 strains, respectively.
Discussion
In this study, we demonstrated that the C-T106A mutation was sufficient to promote viral infectivity in both mammalian hosts and mosquito vectors, thereby dramatically increasing the epidemic potential of ZIKV over its transmission cycle. The T106A substitution rendered the C a preferred substrate for the NS2B-NS3 protease, thereby facilitating the maturation of structural proteins and the formation of infectious viral particles. The flaviviral NS2B/NS3 protease is essential for the maturation of virus-encoded protein components. This protease recognizes and cleaves the viral polyprotein at the following junctions: C/prM, NS2A/NS2B, NS2B/NS3, NS3/NS4A, NS4A/2K, and NS4B/NS5. Based on a comprehensive analysis of ZIKV polyprotein sequences from human isolates, researchers identified the preferred amino acids around the Zika NS2B/NS3 protease cleavage site. Of note, arginine (Arg) consistently exists at the first position of the N-terminal side next to the cleavage position (P1) within the cleavage motifs of these ZIKV peptides. The preferred amino acids are Arg/lysine (Lys)/glutamine, and Arg/glycine (Gly) at the P2 and P3 sites, respectively. Concerning the C-terminal side next to the cleavage position (P′), either Gly or Ser acts as the preferred amino acid at the P1′ position (27). Indeed, the T106A substitution occurs at the P2′ position of the ZIKV C-prM cleavage motif. Intriguingly, both Ala and isoleucine are preferred amino acids at P2′ if either Lys or Arg is located at the P1 position, according to the study of ZIKV NS2B/NS3–mediated human protein cleavage (28). Moreover, in a study focused on designing substrates spanning primed positions of ZIKV NS2B/NS3 protease, researchers screened a library of 19 amino acids at P1′, P2′, and P3′ of the substrate. They found that when P1′ or P2′ was occupied by Ala, the substrates were most efficiently hydrolyzed by the ZIKV NS2/NS3 protease (29). Overall, accumulating evidence suggests that the substitution to Ala at the P2′ position of the ZIKV C-prM cleavage motif may result in a more effective cleavage by the ZIKV NS2B/NS3 protease.
Here, we exploited the FSS13025 strain as a representative for preepidemic ZIKV strains. We realized that the selection of this strain might not present the whole landscape of the preepidemic strains. Nonetheless, the ZIKV infection in humans was rarely reported before the first yet mild ZIKV outbreak on the Western Pacific Yap Island in 2007. In total, fewer than 20 sporadic cases of human ZIKV infection were recorded in Africa and Southeastern Asia before 2007 (3). Therefore, a limited number of ZIKV preepidemic strains in the Asian lineage are available in the National Center for Biotechnology Information (NCBI) and other databases. Since the Asian lineage FSS13025 strain was isolated in Cambodia before the ZIKV outbreak, it has been widely used as a representative prepandemic strain (11, 13). An infectious clone of the FSS13025 strain has been well generated, thereby enabling the feasibility of constructing genetic variants based on the FSS13025 strain (30). Our studies showed that two mutations, C-T106A and NS1-A188V, could facilitate ZIKV transmission by promoting its infectivity and prevalence. However, the underlying mechanisms are distinct. Although the NS1-A188V mutation gave ZIKV an advantage in completing its acquisition by conquering the mosquito gut immune barrier (12, 19), this advantage was not observed during intrathoracic infection scenarios. Given that flavivirus NS1 cannot be effectively secreted by infected mosquito cells, it is reasonable to infer that NS1-A188V–mediated NS1 secretion may not be functional in mosquito hemocoel tissues (31). In this study, we found that the C-T106A mutation directly enhanced infectivity and accelerated the dissemination of ZIKV in both mosquitoes and mice, leading to higher transmissibility between vectors and hosts. The C-T106A mutation increased the packaging efficiency of ZIKV, thereby promoting the maturation of ZIKV from host cells and contributing to its rapid dissemination.
The pathogenicity and transmission of certain pathogens result in part from the evolution of the pathogens themselves as well as complicated factors, such as urbanization, globalization, climate change, and the distribution of their reservoir hosts. Nonetheless, the ability of RNA viruses to emerge and cause human diseases is often linked to the viral adaptation to their hosts or vectors. This adaptation can occur readily because of the high-error frequency of viral, RNA-dependent RNA polymerases, followed by the positive Darwinian selection of mutant strains in viral populations within infected hosts or vectors. Our results suggest that polymorphisms at the C-106th position promote the susceptibility of Aedes mosquitoes and mice to ZIKV infection and might play essential roles in the adaptation of ZIKV to mosquito vectors and vertebrate hosts. In addition, other single–amino acid substitutions have been reported in ZIKV to affect its virulence and pathogenesis. Before spreading to the Americas, ZIKV underwent a V473M substitution in the E protein that increased neurovirulence, maternal-to-fetal transmission, and viremia, facilitating urban transmission (14). An NS1-A188V substitution enhanced ZIKV infectivity in mosquitoes by regulating the immune system in mosquito’s midgut (12). A prM-S17N substitution also increased ZIKV infectivity in human and mouse neural progenitor cells, leading to more severe microcephaly and higher-mortality rates in neonatal mice (11). Moreover, another hypothesis claims that, because of four initial mutations that occurred soon after ZIKV reached Asia, ZIKV underwent fitness declines upon its introduction into Asia decades ago (17). Direct simultaneous reversions of these mutations restored ZIKV fitness and resulted in increasing epidemic risk (17). Thus, a better understanding of the mechanisms underlying arbovirus’s reemergence and enhanced transmission is needed, along with the improved surveillance, to facilitate our ability to predict and control newly emerging viral diseases. Here, our results offer additional evidence about the evolutionary enhancement of ZIKV infectivity in mammalian hosts and mosquitoes, which might improve our understanding of the potential relationships between ZIKV evolution and the occasional widespread reemergences in nature.
Materials and Methods
Ethics Statement.
Human blood for mosquito feeding and peripheral blood mononuclear cell (PBMC) isolation were collected from healthy donors who provided written informed consent. The collection of human blood samples was approved by the local ethics committee at Tsinghua University. The blood samples were deidentified prior to use in this study.
Mice, Mosquitoes, Cells, and Viruses.
Both AG6 and A129 mice were donated by the Institute Pasteur of Shanghai at the Chinese Academy of Sciences. The mice were bred and maintained in a specific, pathogen-free animal facility at Tsinghua University. Groups of age- and sex-matched mice, 6 to 8 wk of age, were used for the animal studies. All animal protocols used in this study were approved by the Institutional Animal Care and Use Committee of Tsinghua University and performed in accordance with their guidelines. The laboratory animal facility has been accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International. A. aegypti (Rockefeller and Danzhou strains) were reared in a low-temperature, illuminated incubator (Model 818, Thermo Electron Corporation) at 28 °C and 80% humidity, according to standard-rearing procedures (32). The ZIKV Cambodian strain FSS13025 (KU955593.1) and the mutant viruses were produced from an infectious complementary DNA (cDNA) clone (30). Zika Puerto Rico strain PRVABC59 (KU501215) and PRV-C A106T mutant virus were generated from infectious clone pFLZIKV-PRV (33). The viruses were passaged in Vero cells in virus production-serum free medium (VP-SFM) (11681-020, Gibco). The viruses were titrated using a plaque formation assay (32). Vero cells, 293T cells, and C6/36 cells were maintained in Dulbecco’s Modified Eagle’s Medium (DMEM) (11965-092, Gibco) supplemented with 10% heat-inactivated fetal bovine serum (16000-044, Gibco). THP-1 cells were maintained in Roswell Park Memorial Institute (RPMI) 1640 medium (22400089, Gibco) supplemented with 10% heat-inactivated fetal bovine serum. A. aegypti Aag2 cells were cultured at 28 °C in Schneider’s medium with 10% heat-inactivated fetal bovine serum and 1% antibiotic-antimycotic (15240-062, Invitrogen) for viral infection. The Vero, 293T, C6/36, and THP-1 cell lines were purchased from the American Type Culture Collection (ATCC) (Catalog No. CCL81, CRL-3216, CRL-1660, and TIB-202). All cell lines were authenticated by the ATCC and did not have mycoplasma contamination.
Phylogenetic Analysis of Zika Strains.
To construct a phylogenetic tree, the complete open reading frame nucleotide sequences of 47 representative ZIKV strains were aligned and analyzed with the maximum likelihood method with 1,000 bootstrap replicates using the Molecular Evolutionary Genetics Analysis (MEGA) X program. The ZIKV strains are labeled by GenBank accession number, followed by the year of collection, country, and strain name.
RNA Transcription, Transfection, and Virus Recovery.
The pFLZIKV-FSS13025 and FSS mutant plasmids were amplified in E. coli Top10 (C404010, Invitrogen) and purified using MaxiPrep PLUS (12965, Qiagen). In vitro transcription was performed as described previously (12). In brief, 10 μg plasmid was linearized with the restriction enzyme ClaI, and the mMESSAGE mMACHINE T7 kit (AM1344, Ambion) was used for the in vitro transcription of RNA, according to the kit’s manual. The RNA was precipitated with lithium chloride and quantified by spectrophotometry. It was subsequently transfected into Vero cells seeded in T25 flasks with DMEM and incubated at 37 °C and 5% CO2 using Lipofectamine 3000 reagent (L3000015, Invitrogen). Recombinant viruses in cell culture media were harvested 4 d after transfection, stored in aliquots at −80 °C, and subjected to further investigation.
Membrane Blood Feeding.
Fresh human blood was collected in heparin-coated tubes (367884, BD Vacutainer). Serum and blood cells were separated by centrifugation at 1,000 g for 10 min. The plasma was collected and heat-inactivated at 56 °C for 60 min. The blood cells were washed three times with phosphate-buffered saline (PBS) to remove the heparin. The cells were then resuspended in heat-inactivated plasma. Based on different experimental settings, viral supernatant or purified virions were mixed with the treated blood for mosquito oral feeding via a Hemotek membrane-feeding system (Hemotek Limited). Engorged female mosquitoes were transferred into new containers and maintained under standard conditions. The mosquitoes were subsequently euthanized or dissected at the indicated time points for further analysis.
Purification of Infectious ZIKV Virions.
The purification of flaviviral infectious virions has been described previously (34). In brief, supernatant from ZIKV-infected Vero cells was collected at 4 d after infection. The cell fragments were removed by centrifugation at 1,000 g and 4 °C for 10 min, followed by filtration through a 0.22-µm filter unit (SLGP033RB, Millipore). The supernatant was then carefully transferred into a clean centrifuge tube and centrifuged at 30,000 g and 4 °C for an additional 3 h to pellet the virions. The precipitated virions were washed twice and then solubilized in VP-SFM medium (11681-020, Gibco). Insoluble components were removed using an extra centrifugation step at 12,000 g and 4 °C for 2 min. The virions in the VP-SFM medium were aliquoted and stored at −80 °C.
Intrathoracic Inoculation of ZIKV in Mosquitoes.
Detailed procedures for mosquito microinjection have been described previously (32). In brief, female mosquitoes were anesthetized on a cold tray, and subsequently, a specific titer of ZIKV (50 p.f.u.) was microinjected into the mosquito thoraxes.
Relative Fitness Assays.
FSS strain ZIKV and FSS-C T106A strain ZIKV were mixed at a ratio of 1:1 p.f.u., and the mixture was fed to mosquitos through a membrane-feeding system or inoculated into AG6 mice via footpad injection. Infected mosquitoes were allowed to probe uninfected AG6 mice 14 d postfeeding, and these AG6 mice were exposed to another batch of mosquitoes at the peak of viremia at 4 dpi. Mosquitoes were euthanized 14 d postfeeding. Mouse blood was collected 4 dpi. All mosquito and mouse samples were subjected to next-generation sequencing to compare the ZIKV strain ratio after competition. Total RNA was extracted using the Multisource RNA miniprep kit (AP-MN-MS-RNA-250, Axygen), reverse-transcribed into cDNA using an iScript cDNA synthesis kit (170-8890, Bio-Rad), and amplified using primer sequences shown in SI Appendix, Table S1. All procedures followed the manufacturer’s protocols. Library was constructed with the Rapid DNA Library Prep Kit (HRK-CC200-24, Huaruikang) following the manufacturer’s protocols. Reads were trimmed using Trim Galore! (version 0.6.4_dev) (https://www.bioinformatics.babraham.ac.uk/projects/trim_galore/). The filtered reads were aligned to the reference sequence using Burrow-Wheeler Aligner–mem (version 0.7.17-r1188) software (35). The Genome Analysis Toolkit (GATK) (HaplotypeCaller version 4.1.9.0) (36) was used to call single-nucleotide variants. The frequencies of different residues at positions 101 to 110 in the C protein were analyzed, and sequence logos were generated using the WebLogo 3.0 tool (weblogo.threeplusone.com/) (37).
Human moDC and moMØ Generation.
PBMCs were isolated by Ficoll-Paque density gradient centrifugation (Catalog No. 17144002, GE Healthcare) from healthy donor blood. hu-moDCs and hu-moMØs were generated from PBMCs by adherence to plastic for 2 h at 37 °C in 5% CO2. For moDC generation, monocytes were cultured in RPMI medium 1640 supplemented with 10% heat-inactivated fetal bovine serum, 100 ng/mL granulocyte–macrophage colony-stimulating factor (GM-CSF) (Catalog No. 34–8339-82, eBioscience) and 100 ng/mL IL-4 (Catalog No. 34–8049-82, eBioscience) for 7 d. For macrophage generation, monocytes were cultured in RPMI medium 1640 supplemented with 10% heat-inactivated fetal bovine serum and 100 ng/mL GM-CSF for 7 d.
Expression and Purification of Recombinant Protein.
The genes encoding ZIKV C-prM protein and NS2B-NS3 protein were amplified from infectious clones and cloned into a pcDNA3.1/V5-His/TOPO DNA vector (K4800-01, Invitrogen) and subsequently transfected using X-treme Gene HP DNA transfection reagent (06366236001, Roche) for ectopic expression in 293T cells. The ZIKV NS2B-NS3 gene was cloned into a pET-28a (+) vector (Catalog No. 69864, Millipore) and purified from E. coli. The cloning primers are shown in SI Appendix, Table S1. The ZIKV NS2B-NS3 construct contains the NS2B cofactor region (residues 45 to 96) linked to the NS3 protein (residues 1 to 177) through a G4SG4 linker. Recombinant NS2B-NS3 was induced at 16 °C overnight for the expression in the E. coli BL21 DE3 strain using a 1-mM final concentration of IPTG in soluble form, and it was purified with TALON metal affinity resin (635501, Clontech). The protein was eluted with 300 mM imidazole and subsequently dialyzed in a buffer containing 20 mM Na-Hepes pH 7.5, 150 mM NaCl, 5% glycerol, and 2 mM DTT. The protein concentration was measured using a protein assay dye (500-0006, Bio-Rad), and the protein purity was checked by SDS–polyacrylamide gel electrophoresis (PAGE).
Western Blotting Analysis and Antibodies.
The samples were separated using a 12% SDS-PAGE gel, followed by electrophoretic transfer to polyvinylidene fluoride membranes, which were then blocked and incubated with primary antibodies. The following antibodies were used in the experiments: anti-GAPDH (2118, 1:3,000 dilution); antibodies were obtained from Cell Signaling Technology. Anti-C (GTX133317, 1:2,000 dilution), anti-prM (GTX133305, 1:2,000 dilution), anti-E (GTX133314, 1:2,000 dilution), anti-NS3 (GTX133309, 1:2,000 dilution), and anti-NS5 (GTX133329, 1:2,000 dilution) antibodies were obtained from GeneTex. Anti-T7 tag (11965-092, 1:2,000 dilution) was purchased from Invitrogen. Anti-IgG (H+L chain) (rabbit) pAb-HRP (458, 1:5,000 dilution) and anti-IgG (H+L chain) (mouse) pAb-HRP (330, 1:5,000 dilution) were purchased from the Medical & Biological Laboratory.
ZIKV E Protein Detection by Enzyme-linked Immunosorbent Assay.
The secretion of ZIKV E protein into the Vero cell supernatant was measured using a ZIKV Envelope Protein enzyme-linked immunosorbent assay (ELISA) Kit (KIT40543, SinoBiological). The experiment was performed according to the manual. The samples were diluted to the range of quantification of the kit using the provided sample dilution buffer. Standard samples for the generation of a standard curve were also provided in the kit. The measured amount of ZIKV E protein matched the linearity of this assay. The optical density was measured at 450 nm using an ELISA reader (Varioskan Flash Multimode Reader, Thermo Fisher Scientific).
Mosquito Feeding on Infected Mice.
The female A. aegypti mosquitoes were separated into a netting-covered container and starved for 24 h before engorgement. ZIKV-infected AG6 mice were anesthetized and placed on top of the container. The mosquitoes were allowed to feed on the mice for 30 min in the dark. After being anesthetized on ice, the engorged mosquitoes were transferred to new containers and maintained under standard conditions for an additional 8 d. The mosquitoes were subsequently euthanized for further analysis.
Gene Quantification by qRT-PCR.
Total RNA was isolated from homogenized mosquitoes, cell lysate samples, or homogenized mouse tissue samples using the Multisource RNA miniprep kit (AP-MN-MS-RNA-250, Axygen) and reverse-transcribed into cDNA using an iScript cDNA synthesis kit (170-8890, Bio-Rad). qRT-PCR was performed on the Bio-Rad CFX-96 Touch Real-Time Detection System. The standard curve for ZIKV was generated by amplifying a segment of the ZIKV genome containing the segment for qRT-PCR detection. The PCR products, which contained the T7 promoter sequence on the positive sense strand, were used as DNA templates for in vitro transcription using the MEGAscript T7 Transcription Kit (AM1334, Ambion), according to the manufacturers’ instructions. The number of single-stranded RNA copies (molecules ⋅ microliter−1) was calculated as described previously (34). The absolute quantification of ZIKV RNA in the samples was obtained using a standard curve constructed from the in vitro–transcribed RNA with a linear range from 108 to 101 copies ⋅ μL−1. The primer sequences are shown in SI Appendix, Table S1.
Determination of the Virus Titer by Plaque Assay.
Culture supernatants from infected cells were collected at the indicated time points and centrifuged for 10 min at 1,000 g and 4 °C to separate the supernatant. Blood samples were collected in 0.4% sodium citrate from the tail veins of infected AG6 or A129 mice and centrifuged for 5 min at 6,000 g and 4 °C to isolate the plasma. The presence of infectious viral particles in the supernatant or plasma was determined using a plaque assay (32). The detection limit in the plaque assay is 10 p.f.u. ⋅ mL−1 for infected cell supernatant and 100 p.f.u. ⋅ mL−1 in plasma.
Protease Assays.
Protease activity assays were performed using an FSS13025 peptide substrate, 2-aminobenzoyl-Lys-Lys-Arg-Arg-Gly-Thr-Asp-Thr-Ser-Val-2,4-dinitrophenyl (Abz-KKRRGTDTSV-Dnp) (synthesized by Genescript), or an FSS-C T106A peptide substrate, Abz-KKRRGADTSV-Dnp (synthesized by Genescript). Each substrate had a starting concentration of 500 μM and was serially diluted two times in assay buffer (20 mM Tris·HCl, pH 8.5, 10% glycerol, and 0.01% Triton X-100) and then added to Corning 96-well black plates with 10 nM purified NS2B-NS3 protease diluted in the same buffer. For kinetics measurements, fluorescence readings were measured at 30-s intervals for 10 min using a Varioskan Flash Multimode Reader (Thermo Fisher Scientific) at an excitation wavelength (λex) of 320 nm and an emission wavelength (λem) of 420 nm. The assays were set up in triplicates at 37 °C. To determine the amount of released Abz, a standard Abz curve was plotted with various concentrations of the cleaved Abz-KKRR peptide (synthesized by Genescript). The initial velocities were calculated using the linear regression function in the GraphPad Prism software (GraphPad Software). The data were analyzed and plotted using the Michaelis–Menten equation with GraphPad Prism statistical software (GraphPad Software).
Quantification and Statistical Analysis.
The animals were randomly allocated into different groups. Mosquitoes that died before the measurement were excluded from the analysis. The investigators were not blinded to the allocation during the experiments or to the outcome assessment. No statistical methods were used to predetermine the sample size. Descriptive statistics are provided in the figure legends. The Kruskal–Wallis analysis of variance was conducted to detect any significant variation among replicates. If no significant variation was detected, the results were pooled for further comparison. Given the nature of the experiments and the types of samples, the differences between continuous variables were assessed using a nonparametric Mann–Whitney U test. Differences in mosquito infection rates were analyzed using Fisher’s exact test. The survival rates of the infected mice were statistically analyzed using the log-rank (Mantel–Cox) test. Differences of protein expression in Western blotting were analyzed using the Student’s unpaired t test. For enzymatic assays, the Michaelis–Menten kinetics were plotted using the nonlinear regression function. P values were adjusted using the Dunnett’s test or the Benjamini–Hochberg procedure to account for multiple comparisons. All analyses were performed using GraphPad Prism statistical software (GraphPad Software).
Acknowledgments
We thank the core facilities of the Center for Life Sciences and Center of Biomedical Analysis for technical assistance (Tsinghua University). We thank the Ministry of Education (MOE) Key Laboratory of Bioinformatics and Dr. Xuerui Yang for assistance in next-generation sequencing (Tsinghua University). We thank Dr. Jingjun Qiu for consultation about statistical analysis. This work was funded by grants from the National Key Research and Development Plan of China (2020YFC1200104, 2018YFA0507202, and 2019YFC1200201), the Natural Science Foundation of China (31825001, 81730063, and 81961160737), Tsinghua University Spring Breeze Fund (2020Z99CFG017), the Shenzhen San-Ming Project for prevention and research on vector-borne diseases (SZSM201611064), and the Yunnan Chenggong expert workstation (202005AF150034).
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2113015118/-/DCSupplemental.
Data Availability
All study data are included in the article and/or SI Appendix.
References
- 1.Musso D., Nilles E. J., Cao-Lormeau V.-M., Rapid spread of emerging Zika virus in the Pacific area. Clin. Microbiol. Infect. 20, O595–O596 (2014). [DOI] [PubMed] [Google Scholar]
- 2.Marchette N. J., Garcia R., Rudnick A., Isolation of Zika virus from Aedes aegypti mosquitoes in Malaysia. Am. J. Trop. Med. Hyg. 18, 411–415 (1969). [DOI] [PubMed] [Google Scholar]
- 3.Musso D., Gubler D. J., Zika virus. Clin. Microbiol. Rev. 29, 487–524 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faye O., et al., Molecular evolution of Zika virus during its emergence in the 20th century. Int. J. Infect. Dis. 21, 2–3 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cao-Lormeau V.-M., et al., Zika virus, French polynesia, South Pacific, 2013. Emerg. Infect. Dis. 20, 1085–1086 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Enfissi A., Codrington J., Roosblad J., Kazanji M., Rousset D., Zika virus genome from the Americas. Lancet 387, 227–228 (2016). [DOI] [PubMed] [Google Scholar]
- 7.Oehler E., et al., Zika virus infection complicated by Guillain-Barre syndrome--case report, French Polynesia, December 2013. Euro Surveill. 19, 20720 (2014). [DOI] [PubMed] [Google Scholar]
- 8.Cordeiro M. T., Pena L. J., Brito C. A., Gil L. H., Marques E. T., Positive IgM for Zika virus in the cerebrospinal fluid of 30 neonates with microcephaly in Brazil. Lancet 387, 1811–1812 (2016). [DOI] [PubMed] [Google Scholar]
- 9.Brault A. C., et al., Venezuelan equine encephalitis emergence: Enhanced vector infection from a single amino acid substitution in the envelope glycoprotein. Proc. Natl. Acad. Sci. U.S.A. 101, 11344–11349 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsetsarkin K. A., Vanlandingham D. L., McGee C. E., Higgs S., A single mutation in chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog. 3, e201 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yuan L., et al., A single mutation in the prM protein of Zika virus contributes to fetal microcephaly. Science 358, 933–936 (2017). [DOI] [PubMed] [Google Scholar]
- 12.Liu Y., et al., Evolutionary enhancement of Zika virus infectivity in Aedes aegypti mosquitoes. Nature 545, 482–486 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xia H., et al., An evolutionary NS1 mutation enhances Zika virus evasion of host interferon induction. Nat. Commun. 9, 414 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shan C., et al., A Zika virus envelope mutation preceding the 2015 epidemic enhances virulence and fitness for transmission. Proc. Natl. Acad. Sci. U.S.A. 117, 20190–20197 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pettersson J. H.-O, et al., How did Zika virus emerge in the Pacific Islands and Latin America? MBio 7, e01239-16 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kawai Y., et al., Increased growth ability and pathogenicity of American- and Pacific-subtype Zika virus (ZIKV) strains compared with a Southeast Asian-subtype ZIKV strain. PLoS Negl. Trop. Dis. 13, e0007387 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu J., et al., Role of mutational reversions and fitness restoration in Zika virus spread to the Americas. Nat. Commun. 12, 595 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heang V., et al., Zika virus infection, Cambodia, 2010. Emerg. Infect. Dis. 18, 349–351 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu J., et al., Flavivirus NS1 protein in infected host sera enhances viral acquisition by mosquitoes. Nat. Microbiol. 1, 16087 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rossi S. L., et al., Characterization of a novel murine model to study Zika virus. Am. J. Trop. Med. Hyg. 94, 1362–1369 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murray C. L., Jones C. T., Rice C. M., Architects of assembly: Roles of Flaviviridae non-structural proteins in virion morphogenesis. Nat. Rev. Microbiol. 6, 699–708 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luo D., Vasudevan S. G., Lescar J., The flavivirus NS2B-NS3 protease-helicase as a target for antiviral drug development. Antiviral Res. 118, 148–158 (2015). [DOI] [PubMed] [Google Scholar]
- 23.Amberg S. M., Rice C. M., Mutagenesis of the NS2B-NS3-mediated cleavage site in the flavivirus capsid protein demonstrates a requirement for coordinated processing. J. Virol. 73, 8083–8094 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stocks C. E., Lobigs M., Signal peptidase cleavage at the flavivirus C-prM junction: Dependence on the viral NS2B-3 protease for efficient processing requires determinants in C, the signal peptide, and prM. J. Virol. 72, 2141–2149 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lobigs M., Lee E., Inefficient signalase cleavage promotes efficient nucleocapsid incorporation into budding flavivirus membranes. J. Virol. 78, 178–186 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mukhopadhyay S., Kuhn R. J., Rossmann M. G., A structural perspective of the flavivirus life cycle. Nat. Rev. Microbiol. 3, 13–22 (2005). [DOI] [PubMed] [Google Scholar]
- 27.Voss S., Nitsche C., Inhibitors of the Zika virus protease NS2B-NS3. Bioorg. Med. Chem. Lett. 30, 126965 (2020). [DOI] [PubMed] [Google Scholar]
- 28.Hill M. E., et al., The unique cofactor region of Zika virus NS2B-NS3 protease facilitates cleavage of key host proteins. ACS Chem. Biol. 13, 2398–2405 (2018). [DOI] [PubMed] [Google Scholar]
- 29.Gruba N., et al., One step beyond: Design of substrates spanning primed positions of Zika virus NS2B-NS3 protease. ACS Med. Chem. Lett. 9, 1025–1029 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shan C., et al., An infectious cDNA clone of Zika virus to study viral virulence, mosquito transmission, and antiviral inhibitors. Cell Host Microbe 19, 891–900 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alcon-LePoder S., et al., Secretion of flaviviral non-structural protein NS1: From diagnosis to pathogenesis. Novartis Found. Symp. 277, 233–247,(2006). [DOI] [PubMed] [Google Scholar]
- 32.Liu Y., et al., Transmission-blocking antibodies against mosquito C-type lectins for dengue prevention. PLoS Pathog. 10, e1003931 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang Y., et al., A cDNA clone-launched platform for high-yield production of inactivated Zika vaccine. EBioMedicine 17, 145–156 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Faye O., et al., Quantitative real-time PCR detection of Zika virus and evaluation with field-caught mosquitoes. Virol. J. 10, 311 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li H., Durbin R., Fast and accurate short read alignment with Burrows–Wheeler transform. Bioinformatics 25, 1754–1760 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McKenna A., et al., The genome analysis toolkit: A MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crooks G. E., Hon G., Chandonia J.-M., Brenner S. E., WebLogo: A sequence logo generator. Genome Res. 14, 1188–1190 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All study data are included in the article and/or SI Appendix.