Abstract
Introduction: Since breast imaging requires very close contact with patients, a protocol is needed to perform safe daily screening activities during the COVID-19 pandemic. Materials and methods: Patients were triaged and separated into three different clinical scenarios by performing a telephone questionnaire before each diagnostic exam or a nasopharyngeal swab before every recovery. Specific procedures for each scenario are described. Results: From July to October 2020, 994 exams were performed. A total of 16 cancers and 7 suspected COVID-19 patients were identified. No medical were was infected. Conclusion: This protocol is an example of the practical use of guidelines applied to a breast unit to assist specialists in preventing COVID-19 infection and optimizing resources for breast cancer diagnosis.
Keywords: : breast neoplasms, clinical practice patterns, COVID-19, pandemics, screening
Lay abstract
On March 11th, 2020, the WHO officially declared the COVID-19 infection pandemic. Since breast cancer represents the most frequent cancer in women of all ages, and breast imaging examinations require very close contact with patients, a protocol was designed to optimize the management of patients and healthcare workers, performing strict COVID-19 screening and avoiding any impairment of survival of patients with breast cancer. Patients were separated into three different clinical scenarios (non-COVID-19 patients, suspected COVID-19 patients and confirmed COVID-19 patients) by performing a telephone questionnaire before each diagnostic exam or a nasopharyngeal swab before every recovery. Specific procedures for each scenario are described. Confirmed or suspected patients are rescheduled if not urgent. From July to October 2020, 994 exams were performed. A total of 16 cancers and 7 suspected COVID-19 patients were identified. No medical staff were infected. This study demonstrates efficacy in terms of continuity in the provision of an essential level of care in a breast cancer screening and ambulatory setting, providing an example of the practical use of guidelines applied to a breast unit, to assist specialists in preventing COVID-19 infection and optimizing resources for breast cancer diagnosis.
On January 30th, 2020, the WHO officially declared the coronavirus disease 2019 (COVID-19; SARS-CoV-2) epidemic as a public health emergency, and, on March 11th, officially defined the rapid universal spread of infection as a pandemic [1,2]. On June 30th, WHO data reported 17,106,007 confirmed cases worldwide since the start of the outbreak and 668,910 deaths. On the same date, in Italy, 247,158 cases had been confirmed, including 35,132 deaths reported to the WHO [2,3]. The predominant virus transmission mechanism is by droplet contact. Other mechanisms of infection include contact with infected surfaces touched by people who, without correct hands disinfection, then touch their own mouth, nose or eyes [1]. The risk of being infected also depends on physical proximity [4]. People are often infectious 2–3 days before they exhibit symptoms, so the proportion of presymptomatic transmission ranges from 48% to 62% [5]. Spread from asymptomatic carriers is estimated at 25% [6]. Thus, solely screening for symptoms does not provide protection for all people [6].
There is no chance of physical distancing when performing breast imaging, such as mammography or ultrasound (US), or breast intervention procedures, such as US-guided fine-needle agoaspiration cytology (US-FNAC), US-guided core needle biopsy (US-CNB) and vacuum-assisted breast biopsy (VABB), so that a radiologist or a radiographer works within 20–30 cm of the patient's face. During the outbreak, breast screening activities were interrupted, as resources were routed to COVID-19 care; accordingly, only cancer emergency-related situations remained ongoing. More recently, from July 1st, screening activities have resumed. Nevertheless, as strategies to prevent the spread of the infection are mandatory, based upon our experience at the Breast Unit of the Caserta Local Health Authority, focusing on patients undergoing their first diagnostic exam at the Department of Diagnostic Senology, District 12, subsequently sent to the Department of Breast Surgery, A. Guerriero Hospital, a protocol was developed to optimize the management of patients and medical staff, performing strict COVID-19 screening and avoiding any impairment of the survival of patients with breast cancer. The aim of this study is to present this protocol, which was focused on patient management and schedules. International guidelines were followed for the protection of patients and staff.
Materials & methods
Literature and guidelines have identified four phases of SARS-CoV-2 infection, depending on the country's COVID-19 status [7]:
Phase 1 – semiurgent setting: severe disease with no community spread. Hospital resources (ICU beds, ventilator capacity and medical supplies) are ample. Operational changes are focused on resource rationalization and preparedness.
Phase 2 – urgent setting: severe disease with contained community spread. Large but controlled number of COVID-19-infected patients with no overload of hospital resources. Operational changes are focused on the progressive reduction of case numbers.
Phase 3 – lockdown: severe disease with uncontained community spread (spike of cases) even with containment procedures in place. Hospital resources are stressed but sufficient, with significant redirection to COVID-19 care.
Phase 4 – uncontrolled pandemic: severe disease with uncontrolled spread. Resources are exhausted even if fully directed to COVID-19 care.
According to the above classification, following a period of lockdown and a gradual easing of containment measures, on June 15th, Italy went back to a phase 1, semiurgent setting, so that screening activities resumed on July 1st. The SIRM Italian College of Breast Radiologists [8] promoted guidelines to protect both patients and healthcare workers (HCWs; including radiologists, radiographers, nurses and reception staff) against infection or disease spread during breast imaging procedures. In an effort to optimize human and technological resources, and based upon a clinical practice point of view, three kinds of scenarios can be identified:
Non-COVID-19 patient = first scenario.
Suspected COVID-19 patient = second scenario.
Confirmed COVID-19 patient = third scenario.
A non-COVID-19 patient is defined using a reverse transcriptase-polymerase chain reaction (RT-PCR) test, with a negative result. Since laboratory tests are not still validated for screening purposes, and considering the high number of asymptomatic or paucisymptomatic cases, HCWs must treat all patients as if they were infected [9]. Nevertheless, since the most common symptoms of the disease are fever, coughing and shortness of breath, a SARS-CoV-2 infection telephone questionnaire was created (Figure 1) to identify both positive and clinically suspected COVID-19 patients who must be postponed and rescheduled after two weeks from the first asymptomatic day. The first asymptomatic day was established by a complete health evaluation made by the general practitioner doctor (GP). The above statements followed the recommendations of national legislation ISS COVID-19 n. 1/2020 and its revisions, properly adapted to our local requirements [10].
Figure 1. SARS-CoV-2 infection telephone questionnaire.
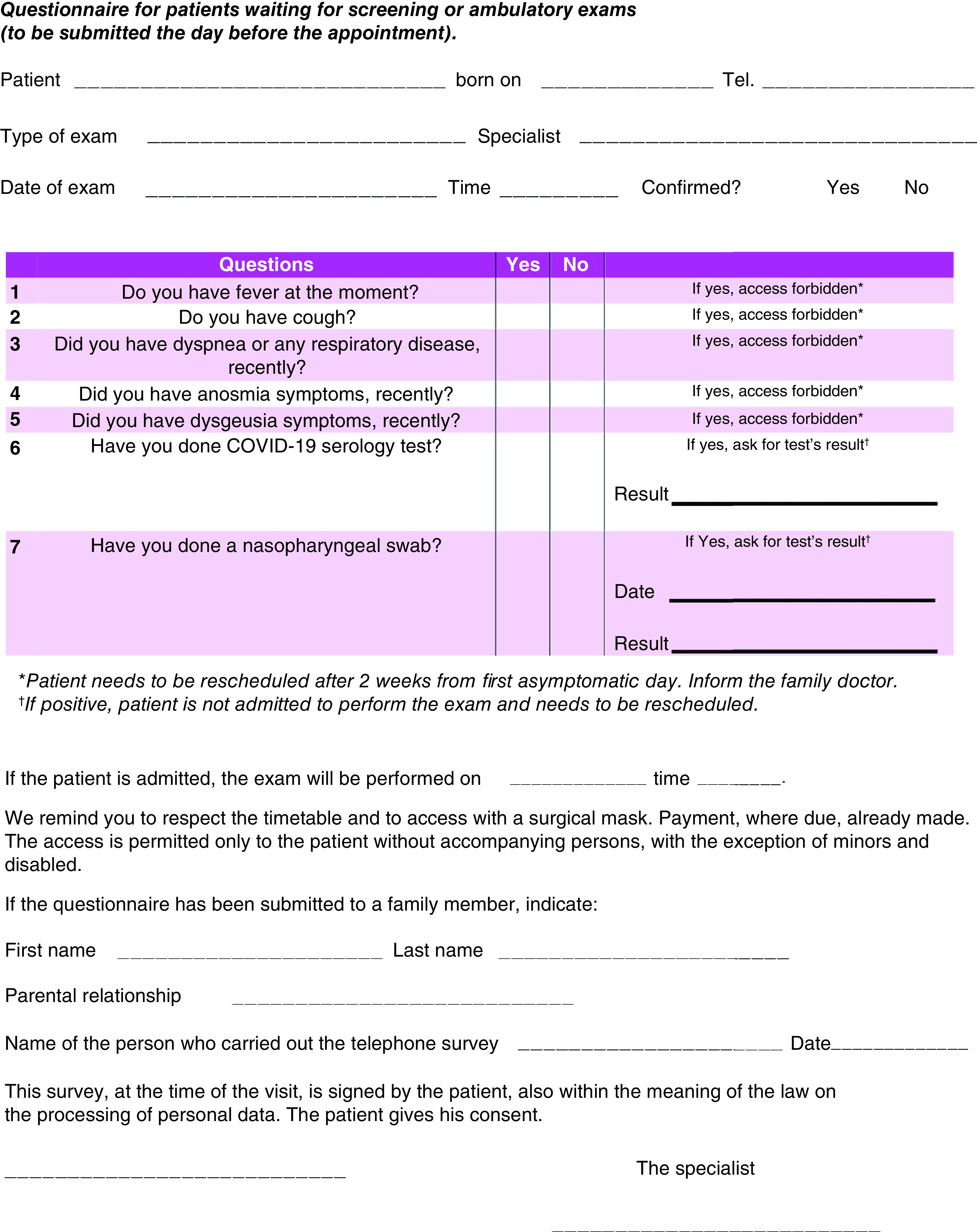
If any answer is positive, the patient will not be admitted to the radiological exam and rescheduled after a complete health evaluation is made by his/her general practitioner doctor.
For patients admitted to procedures, hand sanitization and body temperature checks are performed before entering the department; then, the medical and paramedical staff must follow specific procedures according to the identified clinical scenario. The time-lapse between the exams is 20 min, taking into account patient accommodation, exam time, accurate machine and room disinfection, and air ventilation (at least 10 min are needed).
At the Department of Diagnostic Senology, both screening and ambulatory outpatients are routinely welcome. The first group includes women aged 50–69 or >40 years with a high risk for breast cancer (familiarity, genetics, breast density), collected through the Sani.ARP web portal [11] who present for mammography as the first-level exam. Ultrasound represents a second-level exam, usually to clarify mammography or digital breast tomosynthesis (DBT) findings. US can outperform mammography, particularly regarding younger patients with dense breasts.
The second group includes women of all ages who need a breast imaging exam (mammography or US) for symptoms, oncologic follow-up or extra-screening periodic evaluation. According to our Diagnostic-Therapeutic Care Pathway (DTCP) [12], a DBT in double projection (medio-lateral-oblique and cranio-caudal) with synthetic 2D view reconstructions is performed. Screening exams are validated in double-blind reading by two radiologists; ambulatory exams are validated in single reading by a dedicated radiologist.
Examinations that are more complex are scheduled on a single day, always following full specific safety procedures. In particular, a whole daily session per week is dedicated to breast interventional radiology, including FNAC, CNB and VABB. US-guided interventional procedures (FNAC and CNB) are routinely performed with lower costs than VABB. Furthermore, since these procedures have a similar risk to performing US examinations as standalone, only patients who underwent these exams were triaged. Patients recruited to undergo a VABB procedure, instead, received an RT-PCR test at the department two days before the exam. If negative, she/he would be admitted to perform the biopsy and discharged on the same day the procedure was completed. If the patient should undergo breast surgery, a second RT-PCR test was performed at recovery, and the patient is discharged as soon as she/he is clinically stable, usually two days after surgery. To follow-up, a dedicated well-trained breast care nurse or radiographer (the case manager) called the patient at home, on the first and third day after discharge to verify her/his clinical status.
Methods at the department of diagnostic senology
According to the recommendations of national legislation ISS COVID-19 n. 1/2020 [10] and WHO recommendations released on February 2020 [2], properly adapted to our local requirements and as shown in Figure 2, all patients were subjected to a telephone triage the day before the radiologic exam by a dedicated breast radiographer. The pool of questions, shown in Figure 1, is asked again before the exam is performed, and finally evaluated by the radiologist. Body temperature measurement is performed for each patient before entering the hospital. Each appointment is scheduled every 20 min, to allow the exam execution (DBT plus 2D synthetic reconstructions), time for additional imaging (including magnification views or spot views) and time for equipment disinfection and air ventilation (at least 10 min). No more than two patients are allowed in the waiting room at the same time. No accompanying caregiver is allowed to stay, except for people with mental or physical disabilities requiring assistance. Two different doors are designated for entrance and for exit, respectively; the patient will not pass from through the same corridor twice and will not encounter the following patient. To avoid infection by SARS-CoV-2 for all medical and paramedical staff and for patients, additional procedures must be adopted, depending on different clinical scenarios:
First scenario – non-COVID-19 patient: while waiting for a radiological procedure, all patients wear surgical masks and keep distance from other people (1 m). No other people, included accompanying people, are allowed to stay in the waiting room. The healthcare staff should wear surgical masks, avoids direct contact with the patient's oral and respiratory secretions, wear goggles or face shields and wear gloves and wash hands before wearing gloves and after removing them. A surgical cap and shoe covers are recommended. The ultrasound probe should be covered with a dedicated cap and disinfected after every procedure [9,13,14]. After each radiological procedure, the room and the radiological equipment must be cleaned and disinfected with chloro-derivate solutions and the room should be open for appropriate ventilation (>25 cycles/h) [9,15,16].
Second scenario – suspected COVID-19 patient (infection under investigation, patient waiting for swab results): taking into account the highly contagious nature of SARS-CoV-2, these patients are not permitted to undergo breast imaging examinations until a negative result on the RT-PCR test is obtained, unless the needed exam is urgent (breast emergencies and urgent cancer included, locally advanced breast cancer with bleeding/hemorrhage or ulceration, mastitis, abscesses or trauma) [17,18]. As in the first scenario, the patient wears a surgical mask and follows the rules for social distancing in the waiting room. Radiological staff should wear an N95/FFP2 mask, goggles or face shield, gloves and cap. Ultrasound and mammographic machines must be covered by a plastic sheet and disinfected after the procedure with chloro-derivate solutions and the room should be open for correct air ventilation (>25 cycles/h) [9,16].
Third scenario – confirmed COVID-19 patient: taking into account the highly contagious nature of SARS-CoV-2, breast imaging examinations or breast surgery should be postponed and rescheduled after two weeks from the first asymptomatic day unless it is urgent (Figure 2) [17,18]. In this case, the patient wears a surgical mask and stays isolated from other people. Radiological staff wears FFP3 masks, eye protection, impermeable full-length long-sleeved gown, gloves and cap. HCWs must pay maximal attention to dressing and undressing procedures, as suggested by Spallanzani Hospital [19]. Ultrasound and mammographic machines must be covered by a plastic sheet and disinfected after the procedure with chloro-derivate solutions and the room should be open for correct air ventilation (>25 cycles/h) [9,13,16].
Figure 2. Flowchart outlining prehospitalization, inhospital and posthospital procedures.
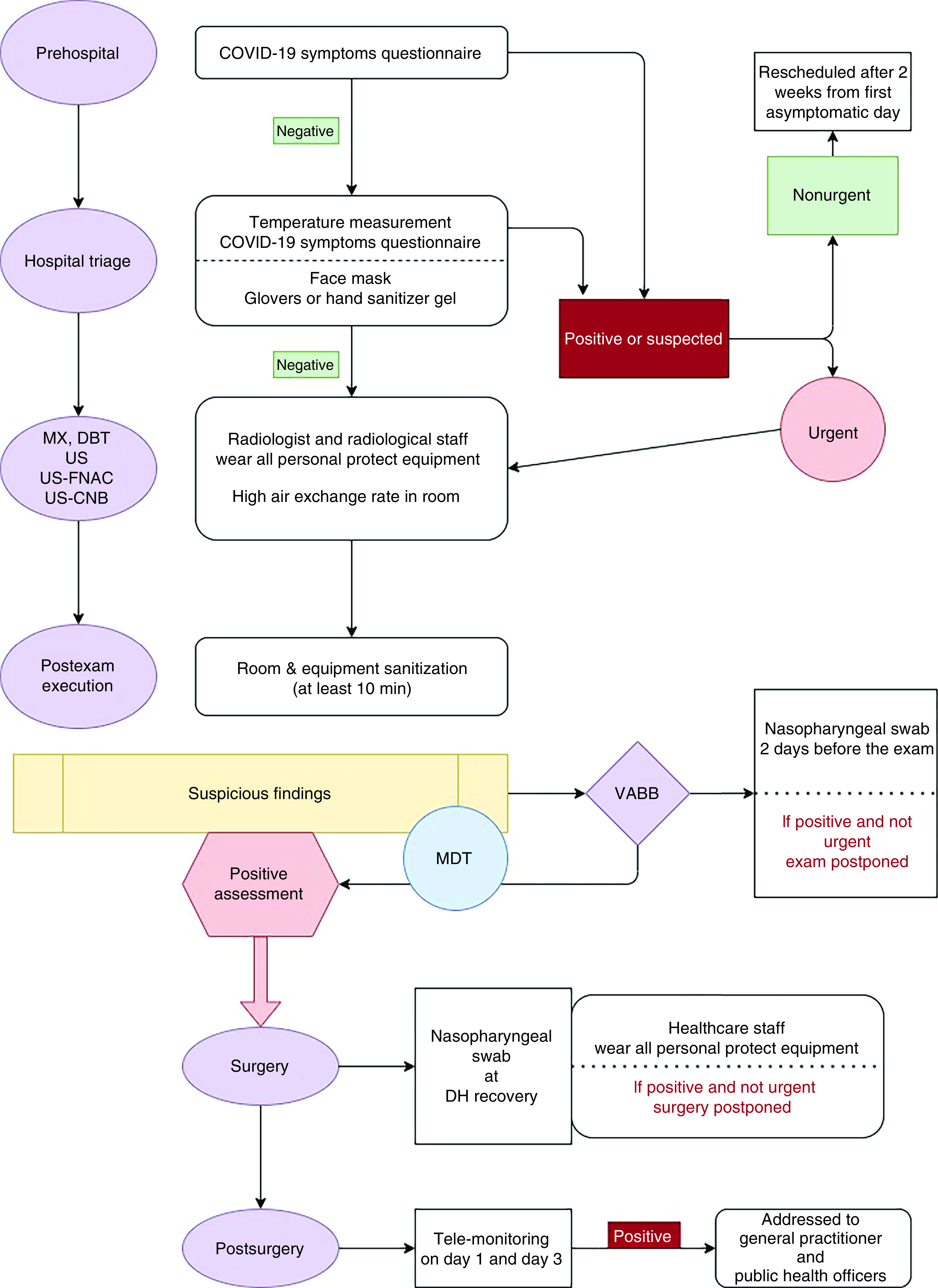
CNB: Core-needle biopsy; DBT: Digital breast tomosynthesis; FNAC: Fine-needle agoaspiration cytology; MDT: Multidisciplinary team meeting; MX: Mammography; US: Ultrasound; VABB: Vacuum-assisted breast biopsy.
Methods at the department of breast surgery
All patients who received doubtful or positive assessments deserving of surgery at the Department of Diagnostic Senology, District 12, Caserta, were referred to our Department of Breast Surgery located at the Anastasia Guerriero Hospital of Marcianise (Caserta). Benign findings requiring surgery were delayed. In the case of a positive assessment, patients with confirmed breast cancer are discussed at the multidisciplinary team meeting (MDT) virtually attended by a breast radiologist, breast surgeon, oncologist and pathologist to avoid face-to-face contact.
All the necessary precautions must be taken before, during and after surgery and during patient transfer [20]. All the HCWs involved must be periodically trained about COVID-19 symptoms and prevention methods. Before the operation, all resources (devices, HCWs, intensive care beds) should be recorded to predetermine availability. This makes it possible to reserve stretchers, operating rooms and elevators for COVID-19-infected patients who need surgery. In the operating rooms, only the minimum number of HCWs should be admitted. They must wear all the necessary personal protective equipment, such as N95/FFP2 masks, sterile surgical gowns, disposable sterile gloves and caps, goggles or protective visors. Alcohol-based hand antiseptic is provided. Surgical staff wears FFP3 masks, eye protection, impermeable full-length long-sleeved gowns, gloves and caps. HCWs must pay maximal attention to dressing and undressing procedures, as suggested by Spallanzani Hospital [19].
Postoperative care
To minimize the risk of readmission, patients were discharged as soon as they were clinically stable, usually one to three days after surgery. Postdischarge visits were reduced to the minimum required. If a patient developed COVID-19 related symptoms, a breast-care nurse or a trained radiographer, both identified as case managers, informed public health officers and family doctors to follow up on the infection's clinical course. They must also monitor all the established pathways after hospital discharge.
Results
Following this organization model and according to the DTCP [11], from July 1st to October 31st, 2020, at the Department of Diagnostic Senology, District 12, Caserta, 994 exams were performed. In particular, 534 DBTs were performed as first-level screening evaluation, 126 DBTs as ambulatory exams, and 67 monolateral DBTs as oncologic follow-up or as second-level examinations. A total of 213 US examinations were also performed, including 121 ambulatory patients and 92 second-level screening exams (Table 1).
Table 1. Exams performed at the Department of Diagnostic Senology.
| Exam | n | Type of exam/results |
|---|---|---|
| Digital breast tomosynthesis | 727 | 534 as screening test |
| 126 as ambulatory exams | ||
| 67 monolateral as follow-up | ||
| Ultrasound | 213 | 121 as ambulatory exams |
| 94 as second-level screening test | ||
| Fine-needle agoaspiration citology | 28 | C1: 1 |
| C2: 15 | ||
| C3: 2 | ||
| C4: 2 | ||
| C5: 8 | ||
| Core needle biopsy | 9 | B2: 1 |
| B3: 1 | ||
| B5: 7 | ||
| Tomobiopsy (vacuum-assisted breast biopsy with tomosynthesis) | 17† | B2: 10 |
| B3: 3 | ||
| B5: 4 |
1 VABB was delayed and rescheduled after the end of the considered period.
In cases of suspicious findings at DBT or US, classified according to BI-RADS score [21], from B3 to B5, 28 FNAC, 9 CNB and 17 VABB procedures were performed (Table 1). One C1 was identified at FNAC that resulted in B2 at CNB; 15 C2, one of these also received VABB for a concurrent lesion, resulting in B2; two C3 resulted in B5 at CNB; two C4 resulted in B3 and B5, respectively, at CNB; and eight C5, 4 of these received CNB resulting in B5. Sixteen patients directly received VABB; of these, nine resulted in B2, three resulted in B3 and four resulted in B5. Sixteen breast cancers (BCs), 7 in women aged 50–69 years (screening range), 4 in women aged <50 years, 4 in women aged >70 years and one in a man aged 43 years old were identified (Table 2). Of these, 11 patients underwent surgery at the Department of Breast Surgery (two nipple-sparing mastectomy and 9 quadrantectomy), one patient started neoadjuvant chemotherapy and four patients were managed at other regional institutions.
Table 2. Pathological examinations with treatments for each diagnosis.
| Age | Sex | FNAC | CNB | VABB | Diagnosis | Therapy |
|---|---|---|---|---|---|---|
| 43 | M | C4 | B3 | DCIS | Nipple-sparing mastectomy | |
| 28 | F | C2 | Fibroadenoma | |||
| 30 | F | C2 | Fibroadenoma | |||
| 42 | F | B2 | Fibrosis | |||
| 44 | F | B5 | DCIS | QUAD | ||
| 46 | F | C2 | Cyst | |||
| 46 | F | B5 | DCIS | Unknown† | ||
| 47 | F | C1 | B2 | FBD | ||
| 48 | F | C2 | Cyst | |||
| 48 | F | B5 | Diffuse DCIS | Nipple-sparing mastectomy | ||
| 49 | F | C4 | B5 | Invasive ductal carcinoma with LCIS | QUAD | |
| 49 | F | B3 | Sclerosing adenosis with columnar cell hyperplasia | |||
| 50 | F | B2 | UDH | |||
| 50 | F | C2 | Fibroadenoma | |||
| 50 | F | C5 | Invasive ductal carcinoma | QUAD | ||
| 50 | F | C2 | Cyst | |||
| 50 | F | C2 | FBD | |||
| 52 | F | B2 | Sclerosing adenosis | |||
| 52 | F | C2 | Fibroadenoma | |||
| 52 | F | C5 | Invasive ductal carcinoma | QUAD | ||
| 54 | F | B5 | DCIS | QUAD | ||
| 54 | F | C2 | Fibroadenoma | |||
| 54 | F | C2 | B2 | Sclerosing adenosis | ||
| 54 | F | C5 | Invasive ductal carcinoma | Unknown† | ||
| 55 | F | C2 | Seroma | |||
| 55 | F | C5 | B5 | Invasive ductal carcinoma | Neoadjuvant chemotherapy | |
| 56 | F | B2 | UDH | |||
| 57 | F | C2 | Fibroadenoma | |||
| 59 | F | C3 | B5 | Invasive ductal carcinoma | QUAD | |
| 60 | F | C2 | Fibroadenoma | |||
| 61 | F | C2 | Fibroadenoma | |||
| 61 | F | C2 | Atypical fibroadenoma | |||
| 62 | F | B2 | Apocrine metaplasia | |||
| 63 | F | B2 | Sclerosing adenosis | |||
| 63 | F | C3 | B5 | Invasive ductal carcinoma | QUAD | |
| 64 | F | B4 | Apocrine metaplasia | |||
| 67 | F | B3 | UDH + ADH | |||
| 68 | F | B2 | UDH | |||
| 69 | F | B3 | ADH | |||
| 71 | F | C5 | B5 | Multifocal ductal carcinoma | QUAD | |
| 74 | F | C5 | B5 | Invasive ductal carcinoma | Unknown† | |
| 77 | F | B2 | UDH | |||
| 77 | F | C5 | B5 | Invasive ductal carcinoma | QUAD | |
| 84 | F | C5 | Bilateral ductal carcinoma | Unknown† |
Patient received surgery elsewhere.
ADH: Atypical ductal hyperplasia; CNB: Core needle biopsy; F: Female; DCIS: Ductal carcinoma in situ; FBD: Fibrocystic breast disease; FNAC: Fine-needle agoaspiration cytology; LCIS: Lobular carcinoma in situ; M: Male; QUAD: Quadrantectomy; UDH: Usual ductal hyperplasia; VABB: Vacuum-assisted breast biopsy.
During the same period, at the Department of Breast Surgery, 54 surgical treatments were performed. Of these, 40 were performed for breast cancer patients (74.1%). Five women were identified as suspected COVID-19 patients and rescheduled. Two women, who received DBT, showed suspected SARS-CoV-2 infection symptoms two days after the exam; case managers informed their family doctors and they performed a RT-PCR test, with negative and positive results, respectively. For the patient affected, VABB was delayed and rescheduled beyond the period considered in this paper (at November, sclerosing adenosis, B2). Finally, no one from the medical staff was infected during this period.
Discussion & conclusion
Due to the COVID-19 emergency, breast cancer units across Italy suffered a significant reduction in their clinical activity. Hospital resources were redistributed from elective and semielective procedures to COVID-19 patients in critical conditions [22], with a subsequent scarcity that could delay diagnostic evaluations and treatment for patients with BC. BC is the most frequent cancer in women of all ages, with more than 5000 early breast cancer (defined as carcinoma in situ or infiltrating cancer less than 1 cm) diagnoses every year [23]. The Italian national screening program improved the prognosis of patients with BC, reaching a survival rate of 87% at 5 years with a significant reduction of about 30% of tumors in advanced stages [24]. This reduction represents a relevant resource for our health system because it results in a lower use of adjuvant therapies, shorter surgery times, earlier return to work and a significant improvement in quality of life. The estimated doubling time of breast cancer ranges between 45 and 260 days [25]: this growth rate variability does not allow for the precise estimation of the impact on patients who could not undergo breast cancer imaging tests during the COVID-19 outbreak. The literature investigating the association between delay and prognosis in patients with BC has yielded conflicting results [26], but a short delay (e.g., 6–12 weeks) should not affect the overall outcome [8]. However, the periodic interruption of BC screening activities, following the spread of SARS-CoV-2 infection in the population, could have a considerable effect on the female population.
A recent study that compared the breast unit activity in the first half of 2020 to the same period in 2019 reported an increased number of referrals either for diagnostic exams in suspected BC patients (estimated around 28%) or for patients who received their first treatment for a BC diagnosis (estimated around 16%) [27]. Vanni et al. [28] estimated that 50% of the 11,000 cases will be identified with a delay of only 6 months, associated with a cancer stage progression. They report that 8125 BC diagnoses could be missed due to a screening interruption of three months [28]. This delayed diagnosis has several consequences, such as more invasive breast surgery or neoadjuvant or adjuvant therapy with a worse patient outcome and an increase in healthcare costs. Jacob L et al. [29] showed a significant reduction in new cancer diagnoses in Germany between March and May of 2020 compared with 2019. This trend was similar both in general and specialized practices and in almost all sex and age groups [29]. A study from a secondary care hospital in Italy revealed that the incidence of BC diagnoses decreased by 26% in 2020 [30] in comparison with 2018–2019, while Kaufman et al. showed a decrease of 51.8% in the United States [31].
In our experience, from July to October 2019, of a total of 1827 DBTs performed, 46 BC cases (2.5%) were identified. In particular, 36 BC were identified from 1736 screening exams (50–69 years) and 10 BC were identified from 88 ambulatory exams (four women aged 45–49 years and six >69 years). Referring to 2020, in the same time interval, of a total of 660 DBTs performed, 16 BC (2.4%) were identified. In particular, 7 BC were identified from 534 screening exams and 9 BC were identified form 126 ambulatory exams (five in women aged 45–49 years and four >69 years). A statistically significant difference (p < 0.01) was found in the data recorded among the two categories of patients (screening and ambulatory) in comparison with 2019 and 2020, such that the reduction of new diagnoses in the screening range reflect a massive decrease in the number of mammographies performed among 50–69 year-old asymptomatic women, in contrast with the increase in examinations for women in the other age ranges.
The reduction in the number of new BC diagnoses during the pandemic might also be caused by the patients' fear of contracting SARS-CoV-2 infection. In fact, women with a suspected breast lesion and those with diagnosed BC frequently refused surgery because of the risk of developing symptoms of COVID-19 [32], probably due to the belief that hospitals are infectious reservoirs [29]. The decreasing rate of healthcare utilization for nonurgent pathologies combined with the rapid overload of the healthcare system, due to the high number of patients infected with COVID-19, supported this trend [29] such that nonurgent care services were delayed or suspended. According to this scenario, triaging both patients' clinical status and urgent clinical cases, and awake and fast surgery are mandatory to optimize the allocation of the limited resources during higher peaks, increasing the number of treated patients and reducing hospitalizations as well as the risk of cross-infection [33].
It is also useful to underline that the spreading of COVID-19 infection can not only affect patients' decision-making process but may have also a psychological impact on HCWs. Ng et al. [34] found a high level of perceived risk, anxiety and fears in HCWs with a prevalence of anxiety (22.5%) and burnout (43.5%), but these values had not increased from pre-COVID-19 rates. Conversely, in Italy, Rossi et al. [35] found a high level of post-traumatic stress symptoms (49.4%), depression (24.7%), anxiety (19.8%), insomnia (8.3%), and high perceived stress (21.9%), especially in young women and frontline HCWs, while no difference was found in low-risk environments [33]. More investigations are needed since different perceptions of risk could be significantly influenced by effective public health interventions and the different number of confirmed patients with COVID-19 infection among countries (more in Italy and the United States than in China). Moreover, the Italian outbreak emerged mainly in the northern region, presenting a relevant difference in terms of cases and fatality rates across the country [33].
The management of patients and healthcare staff described here is an example of the practical use of national and international guidelines as applied to a Breast Cancer DTCP. The protocol may assist specialists in preventing COVID-19 infection and in optimizing resources for breast cancer diagnosis, especially in Southern Italy, where a low rate of improvement in prognosis has been recorded (84%), mostly related to a minor adherence rate to the organized screening program and a lack of knowledge about the importance of early diagnosis [10].
This study demonstrated efficacy in terms of continuity in the provision of an essential level of care in breast cancer screening and ambulatory settings. Since patients with cancer are forced to choose between seeking treatment and increasing the risk of contracting COVID-19, or postponing therapy and minimizing the risk of contracting the infection, more accessible information for the general population could be useful to clarify that the risk of contamination is relatively low when all effective protective measures are respected [36]. In our experience, this proposed model has resulted in a contraction of the waiting lists by a few weeks with a low rate of advanced breast cancer. The absence of medical and paramedical staff SARS-CoV-2 infection also shows the effectiveness of the infection prevention procedures adopted. Conscientiousness regarding how to improve safety at work, for both patients and clinicians, especially in such an extraordinary condition as a pandemic, is just as important as knowing the biological aspects of pathology. Since the SARS-CoV-2 outbreak seems far from over, this protocol may assist specialists and HCWs in preventing infection during this period, and in future similar conditions.
Summary points.
To prevent infection for both patients and healthcare workers during breast imaging procedures, patients were triaged using a telephone questionnaire and separated into three different clinical scenarios (non-COVID-19 patients, suspected COVID-19 patients, confirmed COVID-19 patients). Specific procedures were developed for each scenario.
To prevent the spread of the infection, suspected or confirmed COVID-19 patients were postponed if not urgent, and rescheduled two weeks after first asymptomatic day.
From July to October 2019, 16 breast cancers were identified in 7 in women aged 50–69 years (screening range) and 9 in the other age ranges; 11 patients underwent conservative treatments.
From July to October 2020, 46 breast cancers were identified in 36 in women aged 50–69 years (screening range) and 10 in the other age ranges.
Comparing 2019 and 2020, a statistically significant difference in the number of new breast cancer diagnoses was not found. However, the reduction of new diagnoses in the screening range in comparison with a substantially equal number of diagnoses among ambulatory patients reflects the massive decrease in the number of breast cancer screening mammographies performed, in contrast with the increase in examinations for symptomatic women in the other age ranges.
A different level of perception of risk, anxiety, fears and other mental health disorders have been recorded among patients and HCWs, both in Italy and in other countries. More investigations are needed since this aspect of the pandemic could be significantly influenced by effective public health interventions and the differential outbreaks in the Italian regions and among other countries.
This study demonstrates efficacy in terms of continuity in the provision of an essential level of care, and the absence of medical and paramedical staff SARS-CoV-2 infection is additional proof of the effectiveness of the infection prevention procedures adopted.
Since the COVID-19 outbreak seems far from over, this protocol may assist specialists and health workers in preventing infection during this period and in future similar conditions.
Author contributions
D Tari: study planning, data curation, investigation, writing original draft, review and editing. F Palermo, A Santarsiere and CD Morelli: data curation, investigation, review and editing. F Pinto: formal analysis, supervision, review and editing. All the authors approved the final version to be published.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Ethical conduct of research
Ethics approval not required, considering the retrospective nature of the study. Written informed consent has been obtained from the patient(s) to publish this paper before any radiological exam either mammography or US and before any interventional procedure.
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.Lake MA. What we know so far: COVID-19 current clinical knowledge and research. Clin. Med. 20(2), 124–127 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus Disease (COVID-19)pandemic. Geneva, Switzerland: (2020). www.who.int/emergencies/diseases/novel-coronavirus-2019 [Google Scholar]
- 3.Salute M della Ministero della Salute (2020). www.salute.gov.it/portale/home.html
- 4.Lu M. The front line: visualizing the occupations with the highest COVID-19 risk. Visual Capitalist (2020). www.visualcapitalist.com/the-front-line-visualizing-the-occupations-with-the-highest-covid-19-risk/ [Google Scholar]
- 5.He X, Lau EHY, Wu P et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 26(5), 672–675 (2020). [DOI] [PubMed] [Google Scholar]
- 6.Kimball A, Hatfield KM, Arons M et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility – King County, Washington, March 2020. MMWR Morb. Mortal. Wkly Rep. 69(13), 377–381 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ng CWQ, Tseng M, Lim JSJ, Chan CW. Maintaining breast cancer care in the face of COVID-19. Br. J. Surg. 107(10), 1245–1249 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Detailed indications for breast cancer care management according to the different phases of the COVID-19 pandemic.
- 8.Pediconi F, Galati F, Bernardi D et al. Breast imaging and cancer diagnosis during the COVID-19 pandemic: recommendations from the Italian College of Breast Radiologists by SIRM. Radiol. Med. 125(10), 926–930 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Provides useful guidelines to prevent infection among patients and healthcare workers.
- 9.Too CW, Wen DW, Patel A et al. Interventional radiology procedures for COVID-19 patients: how we do it. Cardiovasc. Intervent. Radiol. 43(6), 827–836 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Detailed information about how to perform interventional procedures for COVID-19 patients, useful also for breast cancer care.
- 10.Salute M della. Nuovo Coronavirus (2020). www.salute.gov.it/nuovocoronavirus?gclid=EAIaIQobChMIz_rmnZPP6gIVgrTtCh0M6wYPEAAYASAAEgKY0fD_BwE
- 11.Tari DU, Ambrosio C, Ignozzi M, Di Cerbo A. Nuovo programma di screening per il carcinoma della mammella dell'ASL Caserta: procedure diagnostiche e risultati preliminari per l'anno 2015 monitorati attraverso il portale Sani.ARP. Rass. Med. XXXII(1), 7–18 (2016). [Google Scholar]
- 12.ASL Caserta. Revisione dei GOM integrati A.O.U. “L. Vanvitelli” - A.O.R.N. “Sant” Anna e San Sebastiano di Caserta - ASL Caserta ai sensi del DCA 98 del 20.09.2016 e s.m.i. - Delibera ASL/CE n. 765 del 19.06.2020.
- 13.Checklist for preparing your IR service for COVID-19 (2020). www.cirse.org/wpcontent/uploads/2020/04/cirse_APSCVIR_Checklist_COVID19_prod.pdf
- 14.Modalità di Comportamento per L'effettuazione di un Esame Ecografico in Questo Momento Pandemico Su (2020). www.sirm.org/wpcontent/uploads/2020/03/Modalita%CC%80-di-comportamento-per-l%E2%80%99effettuazione-diun-esame-ecografico-.pdf.pdf
- 15.Jin Y-H, Cai L, Cheng Z-S et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil. Med. Res. 7(1), 4 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Rapid advice and guidelines suitable for frontline healthcare personnel.
- 16.Coccolini F, Perrone G, Chiarugi M et al. Surgery in COVID-19 patients: operational directives. World J. Emerg. Surg. 15(1), 25 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahoney MC, Ingram AD. “Breast emergencies: types, imaging features, and management”. Am. J. Roentgenol. 202, W390–W399 (2014). [DOI] [PubMed] [Google Scholar]
- 18.Tryfonidis K, Senkus E, Cardoso M et al. Management of locally advanced breast cancer—perspectives and future directions. Nat. Rev. Clin. Oncol. 12, 147–162 (2015). [DOI] [PubMed] [Google Scholar]
- 19.Pianura E, Stefano FD, Cristofaro M et al. COVID-19: a review of the literature and the experience of INMI Lazzaro Spallanzani two months after the epidemic outbreak. J. Radiol. Rev. 7(3), 196–207 (2020). [Google Scholar]
- 20.Citgez B, Yigit B, Capkinoglu E, Yetkin GS. Management of breast cancer during the COVID-19 pandemic. Med. Bull. Sisli Etfal Hosp. 54(2), 132–135 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]; • A significant review that explains some changes in the approach to breast cancer during the COVID-19 pandemic.
- 21.D'Orsi CJ, Sickles EA, Mendelson EB et al. ACR BI-RADS Atlas 5th Edition, Breast Imaging Reporting and Data System. American College of Radiology, VA, USA: (2013). [Google Scholar]
- 22.Rosenbaum L. Facing Covid-19 in Italy – ethics, logistics, and therapeutics on the epidemic's front line. N. Engl. J. Med. 382, 1873–1875 (2020). [DOI] [PubMed] [Google Scholar]
- 23.I 5 Tumori Più Frequenti in Italia Nel 2019 (2020). www.salute.gov.it/imgs/C_17_notizie_3897_4_file.pdf
- 24.Buonomo OC, Materazzo M, Pellicciaro M, Caspi J, Piccione E, Vanni G. Tor Vergata University-Hospital in the beginning of COVID-19-era: experience and recommendation for breast cancer patients. In Vivo 34(Suppl. 3), 1661–1665 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Provides useful recommendations to prevent infections in breast cancer patients starting from general aspects to specific indications about treatments.
- 25.Bleicher RJ. Timing and delays in breast cancer evaluation and treatment. Ann. Surg. Oncol. 25(10), 2829–2838 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caplan L. Delay in breast cancer: implications for stage at diagnosis and survival. Front. Public Health 2, 87 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gathani T, Clayton G, MacInnes E, Horgan K. The COVID-19 pandemic and impact on breast cancer diagnoses: what happened in England in the first half of 2020. Br. J. Cancer 124, 710–712 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vanni G, Pellicciaro M, Materazzo M et al. Lockdown of breast cancer screening for COVID-19: possible scenario. In Vivo 34, 3047–3053 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jacob L, Loosen SH, Kalder M, Luedde T, Roderburg C, Kostev K. Impact of the COVID-19 pandemic on cancer diagnoses in general and specialized practices in Germany. Cancers 13, 408 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Vincentiis L, Carr RA, Mariani MP, Ferrara G. Cancer diagnostic rates during the 2020 “lockdown”, due to COVID-19 pandemic, compared with the 2018–2019: an audit study from cellular pathology. J. Clin. Pathol. 74, 187–189 (2021). [DOI] [PubMed] [Google Scholar]
- 31.Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Net. Open 3(8), e2017267 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vanni G, Materazzo M, Pellicciaro M et al. Breast cancer and COVID-19: the effect of fear on patients' decision-making process. In Vivo 34(Suppl. 3), 1651–1659 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vanni G, Materazzo M, Santori F, Pellicciaro M et al. The effect of coronavirus (COVID-19) on breast cancer teamwork: a multicentric survey. In Vivo 34(Suppl. 3), 1685–1694 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ng KYY, Zhou S, Tan SH et al. Understanding the psychological impact of COVID-19 pandemic on patients with cancer, their caregivers, and health care workers in Singapore. JCO Glob. Oncol. 6, 1494–1509 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rossi R, Socci V, Pacitti F et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Net. Open 3(5), e2010185 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Szmuda T, Ozdemir C, Ali S et al. Readability of online patient education material for the novel coronavirus disease (COVID-19): a cross-sectional health literacy study. Public Health 185, 21–25 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]


