Abstract
Introduction
Tumor staging plays an important role in determining treatment in colorectal cancer. In the recent past, the neutrophil-lymphocyte ratio (NLR) has been used as a predictive marker of inflammation for different types of clinical entities. Our study aims to determine if NLR can predict tumor staging in patients with colorectal cancer.
Materials and methods
We retrospectively analyzed all cases that underwent surgical treatment for colorectal cancer from 2014 to 2020. The NLR, tumor stage, and histology report for all patients were reviewed. Recommended cut-off values for NLR for tumor stage (T), lymph node stage (N), and metastatic stage (M) were determined using receiver operating characteristic (ROC) analysis.
Results
NLR was found to be significantly higher in patients with T3-T4 tumors as compared to T1-T2 tumors (mean: 5.8 vs. 2.6, respectively p < 0.001). The NLR values were higher in cases of N1-N2 groups as compared to N0 groups (mean: 5.7 vs. 3.5, p = 0.07). The NLR was also higher in M1 patients as compared to M0 patients (32.1 vs. 4.5, respectively, p = 0.24) but failed to show a statistical significance.
Conclusion
NLR is a useful predictor of colorectal cancer which can give us some information about the type of tumor we may encounter during surgery.
Keywords: systemic inflammatory response syndrome, cancer metastasis, colorectal neoplasia, neutrophil to lymphocyte ratio (nlr), colorectal cancer
Introduction
Tumour, node, metastasis (TNM) classification plays an important role in predicting the prognosis of various malignancies including colorectal cancer (CRC). There have been other markers such as carbohydrate antigen (CA19-9) and carcinoembryonic antigen (CEA) which have been utilized to assess tumor prognosis and evaluate chances of recurrence [1,2]. Recent studies have indicated that the body hosts immune response to tumor cells which can cause markers of inflammation to get elevated. Inflammatory markers like elevated C-reactive protein (CRP) have shown to be associated with a poor prognosis in cancers [3]. Neutrophil-lymphocyte ratio (NLR) is also an inflammatory status indicator that has been used in assessing prognosis in gastric, breast, and pancreatic cancers [4-6]. In this study, we investigated the predictive ability of preoperative NLR for tumor staging in CRC.
Materials and methods
We retrospectively analyzed the digital records of all patients who were diagnosed with CRC and had undergone hemicolectomy, anterior resection, or abdominoperineal resection for CRC from January 2014 to December 2020 at Father Muller Medical College and Hospital, Mangalore, India. Exclusion criteria included those patients whose records were incomplete, received preoperative chemotherapy, history of recent blood transfusions, immunocompromised patients, patients with hematological disease or chronic inflammatory disease.
Based on the above criteria, among 270 patients who underwent colorectal surgery, 67 patients had to be excluded leaving behind 202 patients for our study. The NLR was calculated by dividing the percentage of neutrophils by lymphocytes from the peripheral WBC count. The patient’s age, sex, NLR, tumor localization, staging, and histological grade were recorded. Patients were staged based on American Joint Committee on Cancer (AJCC) TNM system.
Statistical analysis
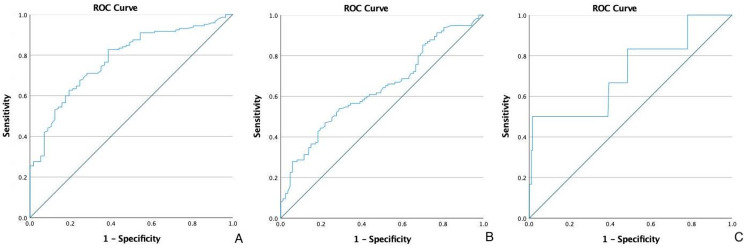
Data were analyzed using IBM SPSS for mac version 25. Data were shown as mean ± SD or median where applicable. The differences between groups were compared by using the student t-test and categorical data were analyzed by the Pearson chi-square test where appropriate. A p-value of less than 0.05 was considered statistically significant. Receiver operating characteristic (ROC) analysis was used to obtain cut-off values to discriminate between various groups. Based on ROC analysis, an NLR cut-off of 2.6 was used to distinguish the early T stage (T1-T2) from the advanced T stage (T3-T4). The area under the ROC curve was 0.779 (95% CI: 0.712-0.846, p < 0.001). An NLR cut-off of 3.3 was used to distinguish N0 from N1-N2 with the area under the ROC curve being 0.639 (95% CI: 0.563-0.715, p < 0.001). For distant metastasis, an NLR of 3.1 was used to distinguish M0 from M1. The area under the ROC curve was 0.720 (95% CI: 0.481-0.959, p = 0.067) (Figure 1).
Figure 1. ROC curve analysis of the neutrophil-to-lymphocyte ratio in patients with colorectal cancer for T stage (A), N stage (B), and M stage (C).
ROC: Receiver operating characteristic.
Results
A total of 202 patients were included in this study. The mean age was 56.2 ± 13.7 years, with age ranging from 25 to 87 years. There were 109 (48.2%) males and 117 (51.8%) females in the study. The most common site for the tumor was in the rectum (39.2%) while the least common site was in the anal canal (2.9%). There were synchronous localization of tumors in two (0.9%) patients (Table 1). In both cases, the tumors were situated in the ascending colon and the transverse colon.
Table 1. Tumor localization of patients with colorectal cancer.
| Tumor localization | n | % |
| Anal canal | 6 | 2.9 |
| Rectum | 79 | 39.2 |
| Left colon | 69 | 34.2 |
| Transverse colon | 11 | 5.4 |
| Right colon | 35 | 17.4 |
| Synchronous tumors | 2 | 0.9 |
| Total | 202 | 100 |
In relation to tumor depth, we found a significantly higher NLR value for T3-T4 tumors as compared to T1-T2 tumors (mean: 5.8 vs. 2.6, p < 0.001). The diagnostic accuracy of NLR at this cut-off was 75.2%. When evaluating NLR based on lymph nodal involvement, the NLR was higher in N1-N2 groups as compared to N0 group (mean: 5.7 vs. 3.5, p = 0.07) but it failed to show any statistical significance. A NLR cut-off of 3.1 was used to distinguish metastatic from non-metastatic disease. The mean NLR was 32.1 for metastatic disease which was higher than non-metastatic disease i.e., 4.5. However, this failed to show any statistical significance (Table 2).
Table 2. Comparing NLR between patient groups with different cancer stages.
Sen: Sensitivity; Spec: Specificity; PPV: Positive predictive value; NPV: Negative predictive value.
| Colorectal Cancer | Mean | SD | Median | p-value | Cut-off value | Sen | Spec | PPV | NPV | Accuracy | |
| Tumor depth | T1-T2 | 2.6 | 1.8 | 2.3 | P < 0.001 | 2.6 | 82.7% | 56.1% | 82.7% | 56.1% | 75.2 |
| T3-T4 | 5.8 | 13.1 | 4.8 | ||||||||
| Lymph node invasion | N0 | 3.5 | 4.9 | 3.3 | P = 0.07 | 3.3 | 64.3% | 48.2% | 62.1% | 50.6% | 57.4 |
| N1-N2 | 5.7 | 14.2 | 4.8 | ||||||||
| Distant organ metastasis | M0 | 4.5 | 9.7 | 3.8 | P = 0.24 | 3.1 | 83.3% | 40.3% | 4.1% | 98.7% | 41.5 |
| M1 | 14.2 | 32.1 | 24.4 | ||||||||
Discussion
CRC is the third most common cause of cancer-related deaths worldwide, with incidence rates higher in the older population [7]. This disease is more commonly diagnosed in men as compared to women [7] but we had more number of women in our study as compared to men. The sigmoid colon is the most common site of cancer in the colon while the rectum is the most common site of cancer in the lower gastrointestinal tract [8]. The most common site of cancer in our study was the rectum (39.2%) followed by the left colon (34.2%). Özgehan G et al. [9] in their study had the majority of tumors arising from the rectum (50.5%) followed by the sigmoid colon (19.4%).
The exact mechanism of elevated NLR and association with various cancers is not clearly understood. The immune system of the body plays an important role in determining the outcome of cancer [10,11]. Neutrophils promote tumor cellular proliferation, invasion as well as vascularization by means of releasing certain factors like chemokines. Hence, an elevated neutrophil count promotes tumor growth and metastasis. Lymphocytes, on the other hand, suppress tumor growth. Lymphocytes are cytotoxic in activity and kill tumor cells as well as produce cytokines that inhibit tumor proliferation and metastasis [12]. In summary, NLR is a reflection of the balance between anticancer immune status and pro-tumor inflammatory status.
In our study, we used NLR at a cut-off of 2.6 to distinguish the early T stage from the advanced T stage with the mean NLR being 2.6 and 5.8, respectively. Özgehan G et al. [9] used a similar cut-off of 2.3 to distinguish early from advanced T stage CRC but the mean NLR was higher for both early and advanced T stage (4.4 and 5.2, respectively). We used a cut-off of 3.3 and 3.1 for N stage and M stage, respectively. Although, the mean NLR was elevated in both cases of lymph nodal spread and tumor metastasis, it failed to show a statistical significance. Özgehan G et al. [9] used a cut-off of 3.2 and 3.4 for N and M stage, respectively and showed that NLR was statistically higher in both cases. They had more number of patients with metastatic disease as compared to study and this may be the reason for statistical significance.
He W et al. [13] studied NLR in metastatic colorectal cancer and found NLR to be significantly elevated. Tang H et al. [14] carried out a systemic review to evaluate NLR's relationship to colorectal liver metastasis. They found NLR to be significantly elevated and also found that an elevated pre-treatment NLR is associated with poor long-term survival. There have been numerous other studies that have utilized NLR to assess prognostic outcome in colorectal cancer. Jeon BH et al. [15] used NLR to assess predictive outcomes in patients with rectal cancer who underwent chemotherapy followed by surgery and found that preoperative elevated NLR was independently associated with decreased five-year disease-free survival. Mazaki J et al. [16] and Dell'Aquila E et al. [17] showed that an elevated NLR is an important prognostic marker in advanced colorectal disease. Due to lack of adequate patient follow-up, we were unable to assess the prognostic relationship between NLR and colorectal cancer in our patients.
Conclusions
NLR is a marker of systemic inflammation and is a valuable predictive indicator of tumor invasion in CRC. An elevated NLR is highly suggestive of local tumor infiltration. NLR has also been shown to be elevated in lymph node spread and distant metastasis. There are numerous investigations available to assess tumor depth but the majority of which are expensive. NLR remains an inexpensive investigation that is easily available to the surgeon's hand. It gives an idea to the surgeon about what they might expect before opening up the abdomen.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Father Muller Institutional Ethics Committee issued approval FMIEC/CCMI 49 612020. Informed consent was waived in view of this being a retrospective study.
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Cancer antigens (CEA and CA 19-9) as markers of advanced stage of colorectal carcinoma. Vukobrat-Bijedic Z, Husic-Selimovic A, Sofic A, Bijedic N, Bjelogrlic I, Gogov B, Mehmedovic A. Med Arch. 2013;67:397–401. doi: 10.5455/medarh.2013.67.397-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Serum p53 antibody as tumor marker for follow-up of colorectal cancer after curative resection. Tang R, Yeh CY, Wang JY, Changchien CR, Chen JS, Hsieh LL. Ann Surg Oncol. 2009;16:2516–2523. doi: 10.1245/s10434-009-0578-2. [DOI] [PubMed] [Google Scholar]
- 3.Preoperative elevation of serum C-reactive protein as an independent prognostic indicator of colorectal carcinoma. Nozoe T, Mori E, Takahashi I, Ezaki T. Surg Today. 2008;38:597–602. doi: 10.1007/s00595-007-3680-8. [DOI] [PubMed] [Google Scholar]
- 4.Preoperative neutrophil-to-lymphocyte ratio (NLR) is associated with reduced disease-free survival following curative resection of pancreatic adenocarcinoma. Garcea G, Ladwa N, Neal CP, Metcalfe MS, Dennison AR, Berry DP. World J Surg. 2011;35:868–872. doi: 10.1007/s00268-011-0984-z. [DOI] [PubMed] [Google Scholar]
- 5.The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M. Oncology. 2007;73:215–220. doi: 10.1159/000127412. [DOI] [PubMed] [Google Scholar]
- 6.Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Ethier JL, Desautels D, Templeton A, Shah PS, Amir E. Breast Cancer Res. 2017;19:2. doi: 10.1186/s13058-016-0794-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bowel cancer statistics. [ Oct; 2021 ];https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer 2021
- 8.Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Chua W, Charles KA, Baracos VE, Clarke SJ. Br J Cancer. 2011;104:1288–1295. doi: 10.1038/bjc.2011.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neutrophil-lymphocyte ratio as a predictive factor for tumor staging in colorectal cancer. Özgehan G, Kahramanca Ş, Kaya İO, et al. Turk J Med Sci. 2014;44:365–368. doi: 10.3906/sag-1305-33. [DOI] [PubMed] [Google Scholar]
- 10.Inflammation and cancer. Coussens LM, Werb Z. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abstracting Keys SEER Training Modules. [ Oct; 2021 ];https://training.seer.cancer.gov/colorectal/abstract-code-stage/keys.html 2021
- 12.Immunity, inflammation, and cancer. Grivennikov SI, Greten FR, Karin M. Cell. 2010;140:883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Initial neutrophil lymphocyte ratio is superior to platelet lymphocyte ratio as an adverse prognostic and predictive factor in metastatic colorectal cancer. He W, Yin C, Guo G, et al. Med Oncol. 2013;30:439. doi: 10.1007/s12032-012-0439-x. [DOI] [PubMed] [Google Scholar]
- 14.Prognostic significance of neutrophil-to-lymphocyte ratio in colorectal liver metastasis: a systematic review and meta-analysis. Tang H, Li B, Zhang A, Lu W, Xiang C, Dong J. PLoS One. 2016;11:0. doi: 10.1371/journal.pone.0159447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neutrophil to lymphocyte ratio: a predictive marker for treatment outcomes in patients with rectal cancer who underwent neoadjuvant chemoradiation followed by surgery. Jeon BH, Shin US, Moon SM, Choi JI, Kim MS, Kim KH, Sung SJ. Ann Coloproctol. 2019;35:100–106. doi: 10.3393/ac.2018.10.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neutrophil-to-lymphocyte ratio is a prognostic factor for colon cancer: a propensity score analysis. Mazaki J, Katsumata K, Kasahara K, et al. BMC Cancer. 2020;20:922. doi: 10.1186/s12885-020-07429-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prognostic and predictive role of neutrophil/lymphocytes ratio in metastatic colorectal cancer: a retrospective analysis of the TRIBE study by GONO. Dell'Aquila E, Cremolini C, Zeppola T, et al. Ann Oncol. 2018;29:924–930. doi: 10.1093/annonc/mdy004. [DOI] [PubMed] [Google Scholar]