Abstract
Objective:
The aim of this study was to examine the occurrence of a variety of symptoms, their frequency, bother, burden, and interference in the lives of women in the late reproductive stage (LRS) and compare their experiences to that of women in the menopausal transition (MT) stage.
Methods:
Women ages 35 to 55 years responded to an 82-question online survey offered by Women Living Better. Participants reported current menstrual patterns, recent changes and symptom frequency, bother, and interference. Women's cycles were classified as LRS or MT using Stages of Reproductive Aging Workshop +10 criteria.
Results:
Of 2,406 respondents, 946 met criteria for LRS and 583 for MT. Participants included 30% from outside the United States, 31% from diverse racial/ethnic groups, and 18% reported having difficulty paying for basics. A similar proportion of women in the LRS and MT+ groups reported each of the symptoms: there was a less than 10% difference for 54 of the 61 symptoms. Of mean bother ratings for all symptoms, only hot flashes differed significantly between the LRS and MT groups. LRS women experienced similar levels of symptom-related interference with personal relationships and daily living to those in the MT stage but did not anticipate these symptoms occurring until they were 50 years old.
Conclusions:
Women in the LRS experience symptoms strikingly similar to those often associated with the MT. Women do not expect these changes until the age of 50 years or later and are surprised by such symptoms before cycle irregularity. Research about the epidemiology and management of LRS symptoms, anticipatory guidance for women, and education for clinicians who care for them warrant increased attention.
Keywords: Late reproductive stage, Menopausal transition, Menopause symptoms, Menstrual irregularity, Ovarian aging, Perimenopause symptoms
The transition from her reproductive years to menopause has a unique script for each woman and for many it is a confusing and sometimes difficult journey. Efforts to characterize the physiologic changes and symptoms associated with this transition have increased in recent decades. The creation and revision of the Stages of Reproductive Aging Workshop (STRAW) framework has been an attempt to define and characterize distinct stages on the path to menopause to define and standardize the process for researchers, clinicians, and the women who live it.1,2 Currently it is unclear when women begin to experience symptoms associated with this transition.
Both the healthcare and lay communities have long associated the beginning of the menopausal transition (MT) with clear changes in the menstrual cycle. In 2001 and 2011, STRAW defined entry into the MT as consecutive menstrual cycles that vary by more than 7 days. The late reproductive stage (LRS) immediately precedes the MT in the STRAW framework and is associated with subtle changes to menstrual flow and cycle length.2 A recent scoping review of research about the LRS revealed little attention to women's experiences during this stage.3 Since 2001, when the STRAW criteria were published, only nine studies focused explicitly on the LRS. Results of these studies suggest that women reported symptoms typically associated with the MT such as sleep disruption, hot flashes, breast pain, vaginal dryness,4 urinary incontinence and nocturia,5,6 memory7 and mood changes,4,8 and pain4 before their periods changed significantly.
Since 2018 women have been contributing data about symptoms experienced before the onset of cycle irregularity to Women Living Better (WLB), an evidence-based online resource about the MT (https://womenlivingbetter.org). This prompted us to embark on further study of the LRS. To investigate women's experience during the LRS and the MT we surveyed a convenience sample of midlife women about their experiences with a broad list of symptoms. The aims of this study were to (1) identify symptoms women reported during the LRS, including their frequency, bother, and symptom burden; (2) compare the symptom experiences between women in the LRS and MT stages; (3) describe the level of interference women associate with symptoms during the LRS and MT; and (4) examine women's expectations of when they would experience symptoms possibly related to the MT.
METHODS
Sampling strategy
Women aged 35 to 55 were invited to complete an 82-question online survey (the WLB Survey) hosted on Survey Monkey and offered in English and Spanish. A link to the survey was distributed in the WLB email newsletter and then through email among networks of women. Links were also posted on the social media channels of WLB and other midlife women's groups. One invitation read “Women, 35 to 55, by sharing your experiences anonymously, you can help create a clearer understanding of this woefully under-researched time in women's lives” (WLB Website). Another read: “Together we can create a clearer understanding of the 10 to 15 years leading up to our final menstrual period. These years are currently poorly understood and can be difficult for many women. Our research aims to change that! The survey is anonymous and takes an average of 16 minutes. Please share your experience.” The survey was open from March 3, 2020 to August 3, 2020.
Survey contents
In the first part of the five-part survey we invited women to describe their current menstrual pattern, report changes they perceived, and share whether and how they tracked their cycles. The second part queried about symptoms sometimes associated with the MT as well as their frequency and degree of bother. In the third part, participants were asked to indicate how much their symptoms interfered with their lives. They also identified their most bothersome symptom and whether they had consulted a healthcare provider about it. Participants were invited to comment on their healthcare experience. The fourth part asked about their overall health, satisfaction with the mix of activities in their lives, and levels of stress. In addition, they were asked to share what activities they did for self-care and to manage stress. The final section included demographic characteristics.
The Office for Human Subjects Division at the University of Washington deemed the WLB Survey as exempt from further human subjects’ review. Women were advised that their responses might be used as part of aggregated information to share with women broadly to let them know what their contemporaries are experiencing and allow them to feel less alone. The findings could be shared with women's health scientific researchers to help enhance their understanding of this life phase and with healthcare providers who care for midlife women. Continuance with the survey was interpreted as confirmation that participants were comfortable with these potential uses of their anonymous data. Women were further reminded: “to keep this survey entirely anonymous, please do not include your name, email or any other identifying information anywhere on the survey.”
Inclusion and exclusion criteria
Women were included in the analyses reported here if they met criteria for the LRS or MT using STRAW+10 criteria. Criteria for the LRS and MT stages are described in detail in the Measures section.
Women were excluded from these analyses, if they were using therapies that could affect their menstrual cycles, including hormone-containing agents such as oral contraceptives, hormonal IUDs, a vaginal contraceptive ring, estrogen, or progestogens in any form. Also, women were excluded if they had procedures or conditions that could affect menstrual bleeding, including endometrial ablation or hysterectomy. Exclusion criteria also included potentially confounding factors such as having been pregnant or lactated in the past 3 months; losing or gaining 20% of body weight; or experiencing a major life event, such as death of a close family member.
Measures
In this article we present women's responses to the English version of the survey. Data were also collected in a separate Spanish language survey.
Demographic data
Demographic data included country in which participants were living; highest level of education completed; working for pay full or part time; difficulty paying for basic goods; race/ethnicity; being in a committed relationship and its duration; number of births; and whether women had responsibility for children or other dependents on a daily basis. These data are included in Table 1.
TABLE 1.
Demographic and health-related characteristics of women eligible for staging reproductive aging
| Characteristic | ||
| Age | Mean | Standard deviation |
| 47.4 | 4.3 | |
| Country of residence (n = 1,294) | Number | Percentage |
| USA | 907 | 70% |
| Canada | 180 | 14% |
| United Kingdom | 122 | 9% |
| Mexico | 12 | 1% |
| Australia | 14 | 1% |
| New Zealand | 5 | 0.4% |
| Education level (n = 1,294) | ||
| High school or less | 75 | 6% |
| Some college | 178 | 14% |
| College degree earned | 445 | 34% |
| Some graduate school | 86 | 7% |
| Graduate degree earned | 510 | 39% |
| Work (n = 1,292) | ||
| Working full time for pay | 824 | 64% |
| Working part time for pay | 298 | 23% |
| Do not get paid for work | 170 | 13% |
| Hard to pay for basics (n = 1,294) | ||
| Very hard | 38 | 3% |
| Somewhat hard | 197 | 15% |
| Not hard | 1,059 | 82% |
| Race/ethnicity (n = 1,319) multiple options selected | ||
| Asian | 31 | 2% |
| Black/African American | 42 | 3% |
| White | 1,121 | 69% |
| Hispanic/Latinx | 87 | 5% |
| American Indian/Alaska Native | 10 | 1% |
| Hawaiian/Pacific Islander | 1 | <1% |
| Prefer not to answer | 27 | 2% |
| Committed relationship (n = 1,294) | ||
| Yes | 1,095 | 85% |
| <10 years | 188 | 17% |
| 10 + years | 904 | 83% |
| Number of births (n = 1,093) | ||
| 0 | 214 | 20% |
| 1 | 198 | 18% |
| 2 | 433 | 40% |
| 3+ | 248 | 23% |
| Responsibility for children/other dependents daily (n = 1,296) | 868 | 67% |
Stages of reproductive aging
The LRS (STRAW LRS -3a) and MT were approximated using criteria derived from the STRAW+10 framework.2 Women's menstrual cycles were classified as meeting LRS criteria if they reported having three or more menses in the past 3 months. Women's cycles were then classified as the STRAW LRS -3a stage if they also reported experiencing changes in their cycle length (shorter, longer) or in the amount of flow (increased, decreased) or the number of days of flow (more, fewer) using the questions developed by Mitchell et al.9 Participants who reported three or more menses in the past 3 months with no change in cycle length, amount of flow or number of days of flow could meet STRAW LRS -3b criteria but were excluded from our analysis because of difficulty differentiating between STRAW LRS -3b and -4 and their small numbers (n = 22). Therefore, the analyses reported here focus on women in STRAW LRS stage-3a, labelled as LRS.
Women who reported menstruating less frequently than monthly during the past 3 months (<3 periods in 3 months) approximated the criteria for the MT (STRAW-1 or -2). Because some of these women may have recently entered early postmenopause (PM) we use the designation MT+ to allow for this possibility. Distribution of menstrual cycle characteristics for women whose cycles approximated LRS and MT+ are given in Table 2.
TABLE 2.
Menstrual cycle characteristics for all participants and by late reproductive stage and menopausal transition+ (N = 1,298)
| Menstrual cycle characteristics | All N (%) (n = 1,298) | Late reproductive stage (n = 946) | Menopausal transition+ (n = 352) | Test statistics |
| Cycle length | n = 1,254 | n = 933 | n = 321 | |
| <20 days | 39 (3%) | 31 (3%) | 8 (2%) | |
| 21-24 days | 160 (13%) | 141 (15%) | 19 (6%) | |
| 25-28 days | 491 (39%) | 442 (47%) | 49 (15%) | |
| 29-31 days | 219 (17%) | 182 (20%) | 37 (12%) | |
| 32-35 days | 63 (5%) | 36 (4%) | 27 (8%) | |
| 36+ days | 94 (7%) | 8 (<1%) | 86 (27%) | |
| Varies by >4 days | 153 (12%) | 76 (8%) | 77 (24%) | |
| Do not know | 33 (3%) | 16 (2%) | 17 (5%) | |
| Changes in cycle length | n = 1,298 | n = 946 | n = 352 | Chi Sq = 208, 4 df, P < 0.001 |
| No changes | 247 (19%) | 221 (23%) | 26 (7%) | |
| Yes, getting shorter | 435 (34%) | 381 (40%) | 54 (15%) | |
| Yes, getting longer | 176 (14%) | 69 (7%) | 107 (30%) | |
| Yes, inconsistent | 374 (29%) | 237 (25%) | 137 (39%) | |
| Other | 66 (5%) | 38 (4%) | 28 (8%) | |
| Changes in menstrual flow | n = 1,298 | n = 946 | n = 352 | Chi Sq = 23.0, 7 df, P < 0.002 |
| No changes | 55 (4%) | 42 (4%) | 13 (4%) | |
| Much heavier | 365 (28%) | 264 (28%) | 101 (29%) | |
| Slightly heavier | 119 (9%) | 98 (10%) | 21 (6%) | |
| Slightly lighter | 150 (12%) | 118 (13%) | 32 (9%) | |
| Much lighter | 162 (13%) | 102 (11%) | 60 (17%) | |
| Some heavier and some lighter | 381 (29%) | 278 (29%) | 103 (29%) | |
| Unsure | 24 (2%) | 20 (2%) | 4 (1%) | |
| Changes in menstrual flow days | n = 1,298 | n = 946 | n = 352 | Chi Sq = 15.8, 4 df, P < 0.003 |
| Fewer days of bleeding | 530 (41%) | 395 (42%) | 135 (38%) | |
| More days of bleeding | 352 (27%) | 251 (27%) | 101 (29%) | |
| No change | 259 (20%) | 191 (20%) | 68 (19%) | |
| Unsure | 92 (7%) | 74 (8%) | 18 (5%) | |
| Days of menstrual flow | n = 1,298 | n = 944 | n = 352 | Chi Sq = 37.6, 7 df, P = 0.000 |
| 1 | 6 (3%) | 1 (<1%) | 5 (1%) | |
| 2 | 28 (2%) | 16 (2%) | 12 (3%) | |
| 3 | 132 (10%) | 98 (10%) | 34 (10%) | |
| 4 | 263 (20%) | 207 (22%) | 56 (16%) | |
| 5 | 349 (27%) | 269 (29%) | 80 (23%) | |
| 6 | 224 (17%) | 166 (18%) | 58 (17%) | |
| 7 or more | 241 (19%) | 159 (17%) | 82 (23%) | |
| Menstrual cramps | ||||
| Menstrual cramps worse | 33823% | 26028% | 7616% | Chi sq = 26, 1 df, P < 0.001 |
| Menstrual cramps returned | 21915% | 17218% | 449% | Chi sq = 22, 1 df, P < 0.001 |
| Abdominal cramps like menstrual, not premenstrual | 35124% | 22123% | 12526% | NS |
| Periods less predictable | 611 (47%) | 360 (38%) | 251 (71%) | |
Symptoms
Identifying which symptoms women experienced as well as the bother and burden associated with them during the LRS was the primary focus of this study. We compared our findings of women in the LRS to those in the MT+.
The symptoms included in the WLB survey were drawn from a review of several symptom scales used in studies of community-based populations: Melbourne Women's Midlife Health Project,10 Seattle Midlife Women's Health Study (SMWHS),11,12 Penn Ovarian Aging Study (POAS),13,14 MS-FLASH Trials,15,16 and from women's submissions to the WLB site. Our questionnaire differed from those previously published in three ways. First, we used detailed descriptors of women's experiences. For example, instead of “awakening in the middle of the night” we differentiated “awakening in the middle of the night and remaining awake for an hour or more” from “awakening in the middle of the night and getting back to sleep easily.” Second, all symptoms in our survey used the personal pronoun “I” or “My” and were written as sentences. Finally, we asked women to “please keep in mind that we are interested in learning about symptoms that are new or more common for you than in the past (ie, symptoms that have begun since your mid-30s).”
The symptoms section of the survey was divided into 11 categories. As we noted to respondents, groupings did not suggest a relationship between symptoms but were created for ease of survey completion. A full listing of the symptom statements can be found in Appendix 1 (see Appendix, Supplemental Digital Content 1, which lists all symptom statements by category). An overview of categories, the number of symptoms in each, and some illustrative examples are given below.
Sleep disruption (five items total): I wake in the middle of the night, and I am awake for an hour or more; I wake in the middle of the night and feel panicked, anxious, and/or worried.
Vasomotor symptoms and palpitations (three items total): I have hot flashes (eg, sudden feelings of warmth, I generally heat up more than I used to), I have heart palpitations (eg, racing heart).
Mood changes (ten items total): I feel easily overwhelmed, less able to cope than I used to be, I have low feelings (eg. sad, blue, depressed, down, blah), I experience sudden anger (eg, raging feelings, fly off the handle), I feel like I cannot calm down on the inside (eg, jumpy, startle easily, sensitive fight, or flight response).
Headache and sore breasts (three items total): I have more frequent tension headaches (pressure or tightening feeling, on both sides), I have more frequent migraine headaches (throbbing pain, made worse with exertion, tends to be on one side).
Brain fog and dizziness (six items total): I am more forgetful (ie, cannot remember names or where I have put things); I have more difficulty making decisions (eg, fuzzy thinking, confusion); I feel dizzy and have vertigo (I feel like I am on a boat); I feel lightheaded (I feel like I might pass out).
Symptoms were also included from the following categories: Dryness, itchiness, and acne (four items total), hair changes (four items total), digestive issues (six items total), pain/fatigue (seven items total), painful sex and libido (six items total), and vaginal and urinary changes (seven items total).
First, women were asked to indicate whether they had experienced any of the listed symptoms during the past 3 months (yes/no), and if so, how frequently they experienced each symptom among four options: (1) once or twice a month, (2) four to six times per month, (3) a few times per week, and (4) daily/almost daily. Women then rated the degree of bother associated with their symptoms using a seven-point scale ranging from not at all bothered (0) to extremely bothered (6).
Symptom burden
The concept of symptom burden has been incorporated in studies of symptoms and symptom management strategies for a variety of conditions such as cancer and other chronic illnesses.17 The product of frequency and severity has been incorporated as an outcome in clinical trials.18 We calculated symptom burden as the product of the frequency and bother rating of each symptom. Burden scores could range from 0 to 24, with more frequently experienced and most bothersome symptoms scoring highest.
Symptom interference
Symptom interference has been defined as the degree to which symptoms interfere with aspects of daily living such as work, social activities, leisure activities, and relationships with others.19 We assessed symptom interference by asking women to consider all of the symptoms they reported, and then indicate how much these symptoms interfered with their daily activities and with their family and other relationships. They rated interference from not at all (0) to a great deal (4).
Expectations about timing of changes
Finally, women indicated at what age they assumed they would begin to experience changes on the path to menopause (35-39, 40-44, 45-49, or 50+). Research related to the timing of developmental events suggests that “on time” versus “off time experiences” influence outcomes and “off time experiences” can provoke psychological distress and affect quality of life.20,21
Analysis
Data were analyzed using SPSS19. Power calculations indicated that with 80% power and 99% confidence, we would be able to detect a difference of 5%, for example, 10% versus 15%, between two groups with an N approximating 1,000. Descriptive statistics including frequencies for demographic characteristics of the sample as well as symptoms and related measures were reviewed before hypothesis testing. Women with LRS and MT+ cycles were compared with respect to the number reporting each symptom, the frequency, and bother associated with each symptom. Associations of symptoms with LRS and MT+ group membership were assessed using Chi square tests. Differences between LRS and MT+ groups were analyzed using the Mann-Whitney U test for ordinal ratings of frequency of experience (z values reported) and t tests to assess the statistical significance of differences in bother scores, burden, and interference ratings between the LRS and MT+ groups. Bonferroni correction of P values was used for analyses of tests related to symptoms shown in Tables 3 to 5 (P < 0.001 identified as P/N tests), where 0.05/60 = <0.001.
TABLE 3.
Sleep disruption, vasomotor symptoms and heart palpitations, mood changes, headache and sore breasts, brain fog and dizziness: number reporting (n, %), frequency, bother and burden for women reporting symptoms by late reproductive stage (LRS) and menopausal transition+ groups (N = 1,436)
| Symptom (total N reporting) | Number reporting symptom (n = 1,436) | LRS number reporting (n = 945) | MT+ number reportinga (n = 491) | LRS frequency (modal category) | MT+ frequency (modal category)b | LRS bother rating M (SD) | MT+ bother ratingc M (SD) | LRS burden score M (SD) | MT+ burden scored M (SD) |
| Sleep disruption | |||||||||
| Hard time falling asleep | 42029% | 25727% | 16333% | Few X/wk | Daily/almost daily | 3.5 (1.7) | 3.7 (1.7) | 10.6 (6.8) | 12.1 (7.3) |
| Wake middle of night, back to sleep easily | 43630% | 28430% | 15231% | Few X/wk | Daily/almost dailye | 2.0 (1.6) | 2.2 (1.8) | 6.4 (5.8) | 7.7 (6.5) |
| Wake middle of night, awake >1 h | 62743% | 39642% | 23147% | Few X/wk | Few X/wke | 4.1 (1.6) | 4.3 (1.5) | 10.9 (6.2) | 12.7 (6.9)e |
| Wake middle of night, panic, anxious worried | 35725% | 22624% | 13127% | 1-2 X/mo | Few X/wk | 4.1 (1.6) | 4.1 (1.6) | 9.2 (6.1) | 9.9 (5.9) |
| Wake up very early in the morning | 36125% | 22023% | 14129% | Daily/almost daily | Daily/almost daily | 2.4 (1.7) | 2.5 (1.9) | 7.4 (6.1) | 8.4 (7.0) |
| Vasomotor symptoms and heart palpitations | |||||||||
| Hot flashes | 55739% | 27829% | 27957%f | 4-6 X/mo | Daily/almost dailye | 3.1 (1.6) | 3.7 (1.7)e | 7.6 (6.1) | 12.3 (7.6)e |
| Night/cold sweats | 62844% | 37740% | 25151%f | 4-6 X/mo | Daily/almost dailyf | 3.4 (1.8) | 3.7 (1.7) | 8.3 (6.5) | 11.2 (7.6)e |
| Heart palpitations | 42330% | 27027% | 15331% | 4-6 X/mo | Few X/wke | 3.6 (1.6) | 3.6 (1.8) | 8.0 (5.9) | 9.8 (7.1) |
| Mood changes | |||||||||
| Irritable (eg, short tempered, grumpy, impatient with others) | 80256% | 53757% | 26554% | 4-6 X/mo | Few X/wke | 4.0 (1.5) | 3.8 (1.5) | 10.0 (6.3) | 11.3 (6.6) |
| Feelings of anxiety (eg, more nervous) | 71350% | 45348% | 26053% | Few X/wk | Few X/wke | 4.2 (1.5) | 4.1 (1.5) | 11.8 (6.9) | 12.5 (6.6) |
| Easily overwhelmed, less able to cope | 60542% | 38341% | 22245% | Few X/wk | Few X/wkf | 4.2 (1.5) | 4.3 (1.5) | 11.8 (6.8) | 13.4 (7.0)f |
| Worry more | 44231% | 27930% | 16333% | Few X/wk | Few X/wk | 4.1 (1.5) | 3.4 (1.6) | 13.1 (6.5) | 13.4 (6.8) |
| Low feelings (eg, sad, blue, depressed, down, blah) | 59041% | 36038% | 23047%f | 4-6 X/mo | Few X/wk | 4.2 (1.6) | 4.1 (1.5) | 10.6 (6.8) | 11.3 (7.0) |
| Mood changes suddenly (mood swings) | 40628% | 26728% | 13928% | 4-6X/mo | Few X/wke | 4.3 (1.5) | 4.0 (1.6) | 10.7 (6.2) | 11.5 (6.8) |
| Experiencing panic attacks, feeling panicky | 25418% | 15717% | 9720% | 1-2X/mo | Few X/wk | 2.8 (1.1) | 2.7 (1.1) | 10.5 (6.7) | 10.8 (6.9) |
| Experience sudden anger, raging feelings, fly off the handle | 41329% | 27729% | 13628% | 1-2X/mo | Few X/wke | 1.0 (2.9) | 1.0 (2.6) | 10.1 (6.3) | 11.2 (6.6)e |
| Tearfulness, crying spells | 45932% | 29932% | 16033% | 1-2 X/mo | 4-6 X/moe | 3.5 (1.7) | 3.6 (1.7) | 7.7 (6.0) | 9.1 (6.7) |
| Feel like I can’t calm down on the inside, jumpy startle easily | 37226% | 23225% | 14029% | 4-6X/mo | Few X/wk | 4.4 (1.6) | 4.2 (1.6) | 11.2 (6.5) | 11.7 (7.0) |
| Headaches and sore breasts | |||||||||
| Tension headaches | 51036% | 34136% | 16934% | 4-6 X/mo | 4-6 X/mo | 3.4 (1.5) | 3.5 (1.5) | 7.3 (5.4) | 8.1 (5.6) |
| Migraine headaches | 26619% | 17819% | 8818% | 1-2X/mo | 1-2X/mo | 4.7 (1.4) | 4.4 (1.6) | 8.1 (5.0) | 8.1 (4.7) |
| Sore breasts | 65546% | 49052% | 16534%e | 1-2X/mo | 1-2X/mo | 2.7 (1.6) | 2.7 (1.7) | 4.5 (4.0) | 5.2 (5.3) |
| Brain fog and dizziness | |||||||||
| More forgetful | 90463% | 59660% | 33568%f | Few X/wk | Daily/almost dailye | 3.9 (1.6) | 4.2 (1.6) | 11.3 (6.6) | 13.4 (7.2)e |
| Have a harder time concentrating | 77854% | 49052% | 28859% | Few X/wk | Daily/almost dailye | 4.1 (1.5) | 4.4 (1.4) | 12.8 (6.7) | 14.8 (6.9)e |
| More difficulty making decisions, fuzzy thinking, confusion | 50535% | 31033% | 19540% | Few X/wk | Daily/almost dailye | 4.1 (1.5) | 4.5 (1.4) | 11.8 (6.5) | 14.5 (7.2)e |
| Feel dizzy | 31222% | 20221% | 11022% | 1-2X/mo | Few X/wke | 3.6 (1.7) | 3.9 (1.7) | 7.7 (5.9) | 9.8 (6.4) |
| Have vertigo (feel like I am on a boat) | 20414% | 12313% | 8117% | 1-2X/mo | 1-2X/mo | 3.9 (1.7) | 4.4 (1.6) | 7.2 (5.7) | 9.4 (6.5) |
| Feel lightheaded, like I might pass out | 28220% | 18319% | 9920% | 1-2X/mo | Few X/wk | 3.8 (1.7) | 4.1 (1.6) | 7.4 (5.3) | 9.8 (6.4)f |
LRS, late reproductive stage; MT, menopausal transition.
Chi square.
Mann-Whitney U.
t test.
t test.
P < 0.001.
P < 0.005.
TABLE 5.
Dryness, itchiness and acne, hair changes, digestive issues and pain and fatigue symptoms: number reporting (n, %), frequency, bother and burden for women reporting symptoms by late reproductive stage and menopausal transition+ groups (N = 1,436)
| Symptom (total N reporting) | Number reporting symptom (n = 1,436) | LRS number reporting (n = 945) | MT number reportinga (n = 491) | LRS frequency (modal category) | MT frequencyb (modal category) | LRS bother M (SD) | MT botherc M (SD) | LRS burden score M (SD) | MT burden scored M (SD) |
| Dryness, itchiness and acne | |||||||||
| Skin drier than past | 69548% | 42945% | 266e54% | Daily/almost daily | Daily/almost dailyf | 3.1 (1.7) | 3.1 (1.7) | 10.5 (7.0) | 11.4 (6.8) |
| Skin itchier | 51936% | 31834% | 20141% | Daily/almost daily | Daily/almost daily | 3.5 (1.5) | 3.4 (1.6) | 11.0 (6.3) | 10.9 (6.6) |
| More breakouts | 34624% | 23525% | 11123% | 4.0 (1.7) | 3.8 (1.9) | 9.6 (7.3) | 9.0 (7.4) | ||
| Eyes drier | 57240% | 35137% | 22145%e | Daily/almost daily | Daily/almost daily | 3.4 (1.7) | 3.6 (1.8) | 11.3 (7.1) | 12.6 (7.6) |
| Hair changes | |||||||||
| Hair drier | 48734% | 30132% | 18638% | NA | NA | NA | NA | NA | NA |
| Hair thinner | 47733% | 31834% | 15932% | NA | NA | NA | NA | NA | NA |
| Hair falling out | 35625% | 22123% | 13528% | NA | NA | NA | NA | NA | NA |
| New facial hairs | 58240% | 37440% | 20842% | NA | NA | NA | NA | NA | NA |
| Digestive issues | |||||||||
| Bloating | 50535% | 32434% | 18137% | Few X/wk | Few X/wke | 4.0 (1.5) | 3.9 (1.7) | 10.6 (6.7) | 11.4 (7.0) |
| Heartburn | 28820% | 19020% | 9820% | 4-6X/mo | 4-6X/mo | 3.7 (1.6) | 3.6 (1.5) | 9.0 (6.6) | 9.2 (6.4) |
| Nausea | 18013% | 10311% | 7716% | 4-6X/mo | 4-6X/mo | 4.0 (1.6) | 3.6 (1.5) | 8.7 (6,3) | 9.4 (6.1) |
| Constipation | 23116% | 14315% | 8818% | 4-6X/mo | 4-6X/mo | 4.0 (1.4) | 3.8 (1.6) | 9.2 (5.9) | 10.1 (6.6) |
| Diarrhea | 17212% | 12313% | 4910% | Few X/wk | Few X/wk | 3.8 (1.7) | 3.9 (1.6) | 10.0 (7.1) | 10.2 (6.9) |
| Abdominal pain, heaviness, tightness | 31822% | 20221% | 11624% | 4-6X/mo | 4-6X/mo | 4.0 (1.5) | 3.9 (1.5) | 9.6 (6.4) | 10.2 (6.5) |
| Pain and fatigue | |||||||||
| Joint/muscle pain | 51336% | 30733% | 20642%f | Daily/almost daily | Daily/almost dailye | 3.9 (1.6) | 4.2 (1.4) | 12.2 (7.2) | 14.1e (7.1) |
| Back pain | 30721% | 20021% | 10722% | Daily/almost daily | Daily/almost daily | 3.9 (1.6) | 4.0 (1.4) | 10.8 (7.4) | 12.0 (7.0) |
| Leg pain | 22416% | 13114% | 9319% | Daily/almost daily | Daily/almost daily | 4.2 (1.5) | 4.2 (1.5) | 12.5 (7.3) | 12.9 (7.4) |
| Neck pain | 19714% | 12713% | 7014% | Daily/almost daily | Daily/almost daily | 4.3 (1.5) | 4.1 (1.5) | 12.9 (7.1) | 13.6 (7.4) |
| Shoulder pain | 21215% | 14115% | 7115% | Daily/almost daily | Daily/almost daily | 4.1 (1.5) | 4.0 (1.5) | 12.0 (7.2) | 12.9 (7.4) |
| Joint/muscle stiffness | 42029% | 23925% | 18137%f | Daily/almost daily | Daily/almost daily | 3.9 (1.5) | 4.2 (1.5) | 12.4 (6.9) | 14.3 (7.3) |
| Fatigue, tiredness, sluggishness | 74552% | 47350% | 27255% | Daily/almost daily | Daily/almost dailyf | 4.4 (1.5) | 4.6 (1.4) | 14.0 (7.2) | 15.8f (6.8) |
LRS, late reproductive stage; MT, menopausal transition; NA, not asked.
Chi square.
Mann-Whitney U.
t test.
t test.
P < 0.005.
P < 0.001.
RESULTS
Participants
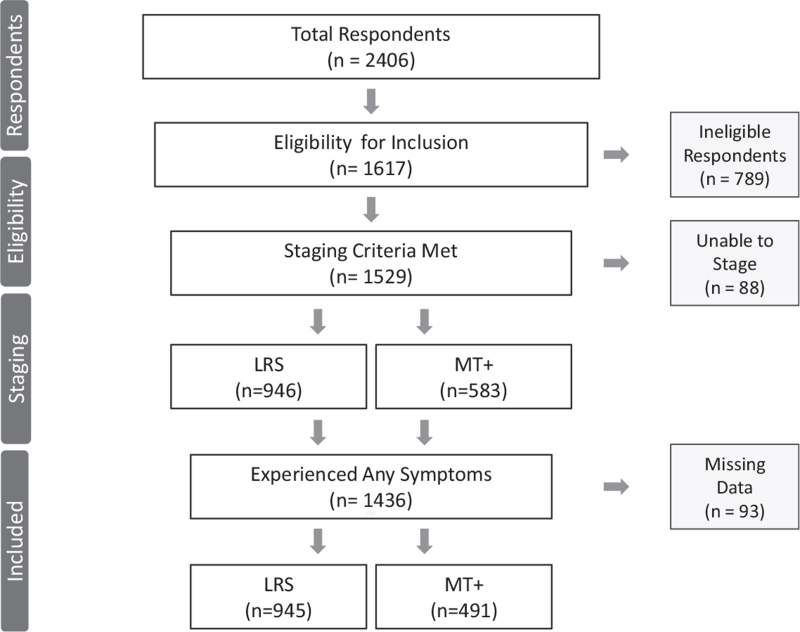
A total of 2,406 women began responding to the English language survey. Of these, 1,617 women met inclusion criteria making them eligible for staging to approximate the LRS and MT+ and 789 were excluded from further analyses (see Fig. 1). Of the 1,617 who met criteria for inclusion, 1,529 met staging criteria for LRS (n = 946) or MT+ (n = 583) and 88 women did not provide adequate data to support staging. Of the 1,529 women asked whether they had experienced symptoms from the categories listed above, 93 did not respond. Of the remaining 1,436 women, 945 were in the LRS and 491 were in the MT+ group.
FIG. 1.
Flow diagram for derivation of study sample included in analyses. LRS, late reproductive stage; MT+, menopausal transition and beyond.
As seen in Table 1, participants who were eligible for inclusion had attained an overall mean age of 47.4 (SD = 4.3) years and lived predominantly in the USA (70%) and Canada (14%). Women identified 37 countries in which they resided. Participants were well-educated, with 34% having completed college, and 39% having earned a graduate degree. A majority worked for pay full time (64%) or part-time (23%) and 13% did not get paid for their work. When asked how difficult it was paying for basics (food, shelter), only 3% indicated it was very difficult, but 15% indicated that it was somewhat difficult. Most participants identified as White (n = 1,121), and smaller numbers identified as Hispanic/Latinx (n = 87), Black/African American (n = 42), American Indian/Alaska Native (n = 10), or Hawaiian/Pacific Islander (n = 1).
A majority of women indicated they were in a committed relationship (85%) with the duration of the relationship of 10 or more years (83%). A majority reported having given birth (80%), with 18% once, 40% twice, and 23% three or more times. A majority had responsibility for caring for children or other dependents on a daily basis (67%).
Women rated their health from poor to excellent, with 41% as good, 36% as very good, and 12% as excellent. Only 11% rated their health as fair or poor. When women were asked whether they experienced “just not feeling like themselves” during this phase of life, 64% indicated they felt this way half of the time or more.
Women also indicated their alcohol intake for a week: 38% reported none, 29% one to two drinks, 15% three to four drinks, 11% five to six drinks, and 7% as seven or more drinks per week. Only 5% reported they currently smoked, 25% were past smokers, and 70% were never smokers.
Menstrual cycle characteristics and stages of reproductive aging
When comparing women with LRS and MT+ cycles, those in the LRS group were significantly (P < 0.001) younger (mean age 46.1, SD = 4.0 years) than the MT+ group (M = 49.8, SD = 3.9 years). A majority of women tracked their menstrual cycles, with 87% overall doing so. The most common methods were using an app on a phone (51%) or a note in a calendar (37%). Rates of tracking did not differ significantly for women in the LRS and MT+ groups. However, a significantly (P < 0.01) larger percentage of women in the LRS versus the MT+ group used an app on their phones to track their cycles (54% vs 44%), whereas fewer LRS women tracked in a calendar (34% and 45%, respectively) than their MT+ counterparts.
Characteristics of the menstrual cycles experienced by women meeting LRS or MT+ criteria are included in Table 2. As expected, these characteristics differed between the LRS and MT+ stages. Women in the LRS group were most likely to report having cycles ranging from 25 to 28 days (n = 442, 47%) or 29 to 31 days (n = 182, 20%), whereas those in the MT+ group were most likely to report having cycles longer than 35 days (n = 86, 27%) and indicated that their cycles did not fit in other categories because they varied by more than 4 days (n = 77, 24%). Women in the LRS group were most likely to report shortening of their cycles (n = 381, 40%), whereas those in the MT+ group were most likely to report inconsistently shorter and longer cycles (n = 137, 39%) and longer cycles (n = 107, 30%) (P < 0.001). As anticipated, women in the LRS group were more likely to report no change in cycle length (23%) than the MT+ group (7%).
Women also reported changes in their menstrual flow. Those in the LRS group were most likely to report having some heavier and some lighter menses (n = 278, 29%) or much heavier flow (n = 264, 28%). Although these flow characteristics were similar in the MT+ group (some heavier and some lighter menses n = 103, 29% and much heavier flow n = 101, 29% respectively) the MT+ group was more likely to report much lighter cycles than the LRS group (P < 0.002).
When asked about changes in the number of bleeding days, women in the LRS group were most likely to report fewer days of bleeding (n = 395, 42%) or more days of bleeding (n = 251, 27%). Although these reports were similar to those in the MT+ group (n = 135, 38% and 101, 29%, respectively), women in the LRS group overall were more likely to report fewer days of bleeding or to be unsure of changes (P < 0.003). The most frequently reported number of days of menstrual flow for the LRS group was 5 days (n = 269, 29%), whereas those in the MT+ group were most likely to report either 5 or 7 or more days of bleeding (n = 80, 23%, n = 82, 23%, respectively) (P < 0.001). In addition, the LRS group reported significantly greater experience of cramps becoming worse (28% vs 16% for LRS and MT+ groups respectively, P < 0.001) and return of menstrual cramps (18% vs 9%, P < 0.001). Less predictability of periods was more common in the MT+ versus the LRS group (71% vs 38%).
Sleep disruption, vasomotor symptoms, heart palpitations, mood changes, headache, sore breasts, and brain fog and dizziness
Approximately 40% or more of all participants (both LRS and MT+ groups) reported the following symptoms: waking up in the middle of the night and remaining awake for an hour or more (n = 627, 43%), having hot flashes (n = 557, 39%); having night sweats or cold sweats (n = 628, 44%); feeling irritable (n = 802, 56%); feeling anxious (n = 713, 50%); feeling easily overwhelmed, less able to cope (n = 605, 42%); feeling low, sad, or blue (n = 590, 41%); having sore breasts (n = 655, 46%); being more forgetful (n = 904, 63%); and having a hard time concentrating (n = 778, 54%) (see Table 3, data column 1).
The proportion of women with LRS and MT+ cycles reporting each of the symptoms is given in Table 3 (columns 2-3). The sleep symptom reported by the largest proportion of women in both the LRS and MT+ groups was awakening in the middle of the night and remaining awake more than 1 hour (42% and 47%, respectively). The vasomotor symptom reported by the largest proportion of women in the LRS group was night sweats/cold sweats (40%) and for the MT+ group was hot flashes (57%). The mood symptom reported by the largest proportion of both the LRS and MT+ group was feeling irritable (57%, 54% respectively) and the most commonly reported cognitive (brain fog) symptom was being more forgetful for both the LRS and MT+ groups (60% and 68%, respectively).
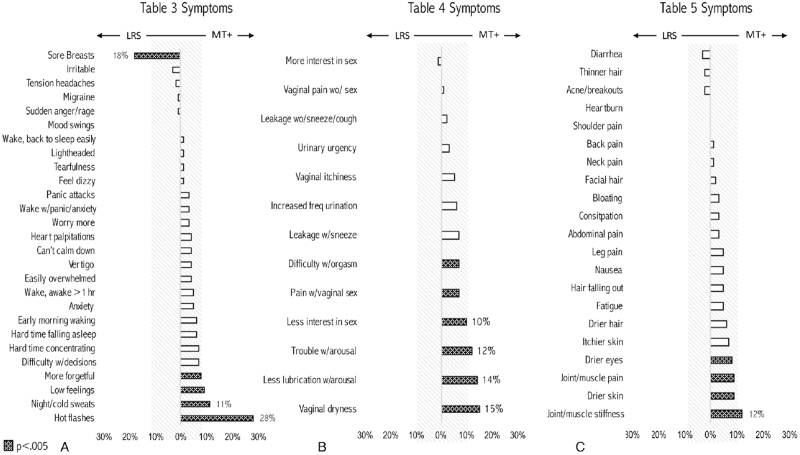
The only symptom reported by a significantly greater proportion of the LRS compared to the MT+ group was sore breasts (52% for LRS and 34% for MT+, P < 0.001). There were only four symptoms that a significantly greater proportion of the MT+ group reported: hot flashes and night sweats (P < 0.001 for both), low feelings (P < 0.001), and forgetfulness (P < 0.002). Figure 2A illustrates the difference in proportions of women in LRS and MT+ experiencing each symptom.
FIG. 2.
Difference in percentage reporting symptoms: LRS vs MT+. (A) Table 3 symptoms. (B) Table 4 symptoms. (C) Table 5 symptoms. Dark cross hatching indicates P < 0.005, open boxes indicate NS; light cross hatching demarcates a 10% difference. LRS, late reproductive stage; MT+, menopausal transition and beyond; NS, not significant.
Women rated the frequency with which they experienced symptoms as once or twice a month, four to six times per month, a few times per week, or daily/almost daily. Table 3 includes the modal (most often selected) frequency category for each of the symptoms for the LRS and MT+ groups. Of the sleep symptoms, participants in both LRS and MT+ groups who reported that they awakened very early in the morning did so daily or almost daily. Women in the LRS group reported their most frequent sleep symptoms occurred a few times per week, including: having a hard time falling asleep, waking in the middle of the night and going back to sleep easily, and waking in the middle of the night and being awake for more than an hour. Women in the MT+ group reported their most frequent sleep symptoms occurred daily or almost daily, including: having a hard time falling asleep, waking up and getting back to sleep easily, and awakening early in the morning daily or almost daily. Both waking in the middle of the night and getting back to sleep easily and waking in the middle of the night and remaining awake for an hour or more occurred significantly more frequently among the MT+ group than the LRS group (P < 0.001 for each).
Vasomotor symptoms and heart palpitation frequency differed between the groups, with the LRS group reporting hot flashes, night/cold sweats, and heart palpitations each four to six times per month and the MT+ group reporting hot flashes and cold/night sweats occurring daily or almost daily and heart palpitations a few times per week. All three symptoms were significantly more frequent among the MT+ group than the LRS group (P < 0.001).
Frequency of mood symptoms also varied between the LRS and MT+ groups. The LRS group reported feeling anxious, easily overwhelmed, and worrying more than a few times per week. The MT+ group reported feeling irritable, anxious, easily overwhelmed, worrying more, having low feelings, sudden mood changes, panic attacks or panicky feelings, sudden anger, and feeling as if they could not calm down a few times per week. The MT+ group reported significantly more frequent experiences of feeling irritable (P < 0.001), anxious (P < 0.002), easily overwhelmed P < 0.003), sudden mood changes (P < 0.003), sudden anger (P < 0.002), and tearfulness/crying spells than the LRS group (P < 0.001).
Of the brain fog and dizziness symptoms, the LRS group most often reported being forgetful, having a harder time concentrating and difficulty making decisions, with these symptoms occurring a few times per week, whereas women in the MT+ group reported these experiences daily or almost daily. The MT+ group had significantly more frequent experiences of brain fog symptoms, including forgetfulness (P < 0.001), difficulty concentrating (P < 0.001), difficulty making decisions (P < 0.001), and feeling dizzy (P < 0.001) than the LRS. In general, the brain fog symptoms described above occurred with greater frequency among women in the MT+ group.
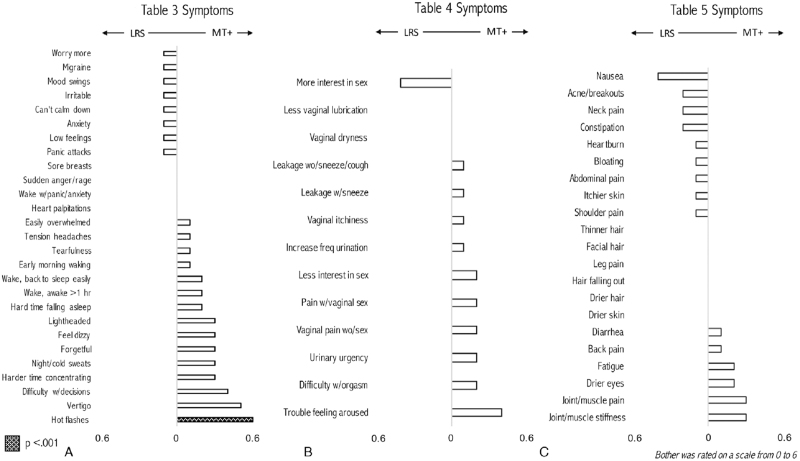
The LRS and MT+ groups rated symptoms differently with respect to those they found most bothersome, but only hot flashes were significantly more bothersome for the MT+ group (P < 0.001). Of the sleep symptoms, the most bothersome symptoms for the LRS group were awakening in the middle of the night and remaining awake for more than an hour and awakening and feeling panicky, anxious, or worried. The MT+ group rated these symptoms similarly. Of the vasomotor and heart palpitations symptoms, women in the LRS group rated heart palpitations as most bothersome, whereas the MT+ group rated hot flashes and night/cold sweats as most bothersome.
Of the mood symptoms, women in the LRS group rated feeling as if they could not calm down as the most bothersome, whereas the MT+ group rated feeling easily overwhelmed as most bothersome. Of the brain fog/dizziness symptoms, women in the LRS group rated having a hard time concentrating and difficulty making decisions/fuzzy thinking/confusion as the most bothersome. Those in the MT+ group rated difficulty making decisions, having a hard time concentrating, and vertigo as their most bothersome symptoms. There were no significant differences in bother scores between the LRS and MT+ groups for the mood or brain fog symptoms or for the headaches and sore breast symptoms. The most bothersome symptom of all 61 symptoms for LRS women was migraine. Figure 3A illustrates differences in mean bother scores for each symptom in Table 3.
FIG. 3.
Difference in mean bother ratings: LRS vs MT+. (A) Table 3 symptoms. (B) Table 4 symptoms. (C) Table 5 symptoms. Dark cross hatching indicates P < 0.001, open boxes indicate NS. Bother was rated on a scale from 0 to 6. LRS, late reproductive stage; MT+, menopausal transition and beyond; NS, not significant.
Women in the LRS and the MT+ groups both rated having a hard time concentrating as the most burdensome symptom. Women in the MT+ group experienced significantly more burden than the LRS group associated with waking in the middle of the night and remaining awake for more than an hour (P < 0.001), hot flashes (P < 0.001), night/cold sweats (P < 0.001), feeling easily overwhelmed (P < 0.005), sudden anger (P < 0.001), being more forgetful (P < 0.001), having a harder time concentrating (P < 0.001), difficulty making decisions (P < 0.001), and feeling light headed (P < 0.002). There were no significant differences in burden scores for the headaches/sore breast symptoms.
Painful sex and libido and vaginal and urinary changes
The painful sex and libido and vaginal and urinary symptoms most commonly (>40%) reported by all women in the LRS and MT+ groups were less interest in sexual activities (n = 799, 56%) and urinary leakage when coughing or sneezing (n = 619, 43%). The proportion of women with LRS and MT+ cycles reporting each symptom is given in Table 4, columns 2 to 3. A significantly larger proportion of women in the MT+ compared to LRS group reported sexual symptoms, including pain with vaginal sex (18% for MT+ vs 11% for LRS), less vaginal lubrication (41% vs 27%), less interest in sexual activity (62% vs 52%), difficulty experiencing orgasm (23% vs 16%), and difficulty with arousal (42% vs 30%) (P < 0.001 for all tests). A small but similar proportion of women in both stages experienced increased interest in sexual activity (8% of the MT+ compared with 9% LRS). Of the vaginal and urinary changes, only vaginal dryness was significantly associated with the MT+ group (31% for MT+ vs 16% for LRS, P < 0.001). Figure 2B illustrates the difference in proportions of women in LRS and MT+ experiencing each symptom.
TABLE 4.
Painful sex and libido and vaginal and urinary changes: number reporting (n, %), frequency, bother and burden for women reporting symptoms by late reproductive stage and menopausal transition+ groups (N = 1,436)
| Symptom (total N reporting) | Number reporting symptom (n = 1,436) | LRS number reporting (n = 945) | MT+ number reportinga (n = 491) | LRS frequency (modal category) | MT+ frequencyb (modal category) | LRS bother M (SD) | MT+ botherc M (SD) | LRS burden score M (SD) | MT+ burden scored M (SD) |
| Painful sex and libido | |||||||||
| Pain with vaginal sex | 197 (14%) | 107 (11%) | 90 (18%)e | Sometimes | Sometimes | 4.4 (1.6) | 4.6 (1.6) | 10.6 (5.2) | 11.2 (4.7) |
| Less vaginal lubrication | 451 (31%) | 252 (27%) | 199 (41%)e | Sometimes | Always | 3.7 (1.6) | 3.7 (2.0) | 9.3 (5.0) | 9.6 (5.9) |
| Less interested in sexual activities | 799 (56%) | 495 (52%) | 304 (62%)e | Always | Always | 3.7 (1.8) | 3.9 (2.0) | 9.3 (5.2) | 10.1 (5.8) |
| More interested in sexual activities | 123 (9%) | 82 (9%) | 41 (8%) | Sometimes | Sometimes | 0.7 (1.3) | 0.3 (0.7) | 1.4 (2.8) | 0.6 (1.6) |
| More difficulty experiencing orgasm | 265 (18%) | 151 (16%) | 114 (23%)e | Sometimes | Always | 4.2 (1.7) | 4.4 (1.9) | 10.3 (5.0) | 11.3 (6.0) |
| More trouble feeling aroused | 489 (34%) | 284 (30%) | 205 (42%)e | Sometimes | Always | 4.0 (1.7) | 4.4 (1.8) | 10.1 (5.1) | 11.5f (5.5) |
| Vaginal and urinary changes | |||||||||
| Vaginal dryness | 308 (21%) | 154 (16%) | 154 (31%)e | Daily | Dailya | 3.7 (1.7) | 3.7 (1.7) | 10.7 (7.3) | 11.9 (7.4) |
| Vaginal itchiness | 239 (17%) | 143 (15%) | 96 (20%) | 1-2X/mo | 4-6X/mo | 3.9 (1.7) | 4.0 (1.6) | 10.0 (7.6) | 10.2 (7.1) |
| Vulvar/vaginal pain without sex | 45 (3%) | 25 (3%) | 20 (4%) | 4-6X/mo | 4-6X/mo | 4.5 (1.6) | 4.7 (1.5) | 11.6 (8.0) | 10.9 (6.4) |
| Urinary leakage sneezing or coughing | 619 (43%) | 384 (41%) | 235 (48%) | 4-6X/mo | Few X/wk, daily | 4.0 (1.7) | 4.1 (1.7) | 11.0 (7.3) | 11.6 (7.5) |
| Urinary leakage at other times | 255 (18%) | 161 (17%) | 94 (19%) | Daily/ almost | Few X/wk | 4.5 (1.7) | 4.6 (1.7) | 12.6 (7.6) | 14.3 (7.3) |
| Increased frequency of urinating | 397 (28%) | 242 (26%) | 155 (32%) | Daily/ almost | Daily/ almost | 3.5 (1.7) | 3.6 (1.8) | 12.1 (7.2) | 12.9 (7.6) |
| Urinary urgency | 258 (18%) | 161 (17%) | 97 (20%) | Daily/ almost | Daily/ almoste | 4.2 (1.6) | 4.4 (1.7) | 12.4 (6.9) | 15.4f (7.8) |
LRS, late reproductive stage; MT, menopausal transition.
Chi square.
Mann-Whitney U.
t test.
t test.
P < 0.001.
P < 0.005.
The frequency of vaginal and urinary symptom experiences was similar for the LRS and MT+ groups. The MT+ group experienced vaginal dryness daily or almost daily (P < 0.005) and urinary urgency daily or almost daily, significantly more frequently than the LRS group (P < 0.001, respectively). There were no significant differences between groups in any other vaginal and urinary symptoms, nor for the painful sex or libido symptoms.
Bother associated with painful sex and libido and vaginal and urinary changes symptoms was greatest for difficulty experiencing sexual arousal (4.4 for MT+ and 4.0 for LRS) and for urinary urgency (4.4 for MT+ and 4.2 for LRS), but these differences were not statistically significant. Vulvar/vaginal pain when not having sex was the most bothersome of all symptoms for MT+ women. Figure 3B illustrates differences in mean bother scores for each symptom in Table 4. The burden associated with vaginal and urinary symptoms was greater for the MT+ versus the LRS group for difficulty with sexual arousal (P < 0.002) and urinary urgency (P < 0.002).
Skin, hair, digestive, pain, and fatigue symptoms
A final set of symptoms was related to skin and hair, digestion, and pain and fatigue (see Table 5). For all participants, the skin symptom reported by the largest proportion of women was drier skin than in the past (n = 695, 48%), with dry skin and dry eyes significantly more likely to be reported by the MT+ than the LRS group (P < 0.002, P < 0.004, respectively). Although both groups rated frequency of skin symptoms as experienced daily or almost daily, skin dryness was significantly more frequent among the MT+ group (P < 0.001). The most bothersome skin symptom was more skin breakouts, but there were no significant group differences in either bother or burden for any of these symptoms.
The digestive symptom reported by the largest proportion of participants was bloating (n = 505, 35%), with no significant associations with the LRS and MT+ groups. Frequency of digestive symptoms was greatest for bloating and diarrhea (few times per week). Bloating was significantly more frequent among the MT+ than the LRS group (P < 0.005). The most bothersome digestive symptoms were bloating, nausea, constipation, and abdominal pain for the LRS group and bloating, diarrhea, and abdominal pain for the MT+ group. There were no significant differences between the LRS and MT+ groups in bother or burden ratings for any of these symptoms.
In the pain and fatigue category, the symptom reported by the largest proportion of participants was fatigue (n = 745, 52% for all; 50% for LRS; and 55% for MT+ groups). A significantly greater proportion of the MT+ group reported joint/muscle pain and joint/muscle stiffness (P < 0.001 for each symptom). Figure 2C illustrates the difference in proportions of women in LRS and MT+ experiencing each symptom. Frequency of pain/fatigue symptoms was daily or almost daily for each symptom, but significantly greater for the MT+ group for joint/muscle pain and fatigue/tiredness (P < 0.002, P < 0.001, respectively). The most bothersome pain/fatigue symptom was fatigue for both LRS and MT+ groups, with no significant group differences in bother ratings. Figure 3C illustrates differences in mean bother scores for each symptom in Table 5. Symptom burden was greatest for fatigue for both LRS and MT+ groups and burden of both fatigue and joint/muscle pain was significantly greater for the MT+ group than the LRS (P < 0.001, P < 0.005, respectively).
Interference with daily living and expectations about age of menopause-related changes
Women indicated the level of interference in daily living activities and in relationships with family and friends with respect to the totality of symptoms they experienced. Women indicated that their symptoms interfered somewhat with both daily activities (46%) and relationships with family and friends (40%). Those in the LRS group reported lower levels of interference with daily living compared to those in the MT+ group (M = 2.1, SD = 1.1 for LRS and M = 2.3, SD = 1.1 for MT) (P < 0.001). The LRS and MT+ endorsed a similar amount of interference related to their symptoms with respect to relationships with family and friends (M = 2.1, SD = 1.1 for LRS; M = 2.2, SD = 1.2 for MT group).
Women's expectations
Finally, we asked women to recall when they were 30 years old at what age they anticipated experiencing menopause-related changes. The most commonly reported age of expected changes was 50 years or older (59%). Twenty-eight percent anticipated changes from 45 to 49 years of age, 9% at 40 to 44 years of age, and 2% at 35 to 39 years of age. The patterns of anticipation were not significantly different between the LRS and MT+ group.
DISCUSSION
Although some women reach menopause easily, others experience a variety of unpleasant or even disruptive symptoms in the preceding years. Characterizing when these symptoms begin is important for providing anticipatory guidance to women, validating their lived experiences, and educating the healthcare providers who care for them: our goal is to contribute to this effort.
A total of 2,406 women responded to the WLB Survey, 1,436 of whom met criteria for the LRS or MT+ stages and rated 61 symptoms with respect to occurrence, frequency, and bother over the previous 3 months. A majority of this well-educated sample was employed for pay, did not have difficulty paying for basics, and described themselves as White. Despite 89% of participants rating their health as good, very good, or excellent, a majority indicated they experienced “not feeling like themselves” in the past 3 months.
The symptom experience of the LRS group is strikingly similar to the MT+ group for most symptoms. For only 8 of 61 symptoms did the LRS and MT+ groups differ by 10% or more in percentage reporting (Fig. 2). Of mean bother ratings, only hot flashes differed significantly between LRS and MT+ (Fig. 3). Overall, the LRS and MT+ groups were more similar than different with respect to symptom ratings across all four metrics—percentage reporting, frequency, bother, and burden.
WLB survey data indicate that women experience considerable symptomatology during the LRS before menstrual irregularity of a week or more, the STRAW criterion delineating the beginning of the MT. Women were asked to report only symptoms that were new or more common than in the past (ie, symptoms that had begun since their mid-30s). Indeed, when we examined the proportion of LRS women in our sample reporting symptoms, we found that more than 40% indicated awakening in the middle of the night and remaining awake for more than an hour, having night or cold sweats, feeling irritable, anxious, easily overwhelmed, being more forgetful, having difficulty concentrating, breast soreness, being less interested in sexual activity, experiencing urinary leakage when coughing or sneezing, dry skin, new facial hair, and fatigue.
Previous research has documented symptoms thought to be associated with menopause during the LRS. The aforementioned scoping review of the LRS found nine studies that identified symptoms including vasomotor, sleep, mood, cognitive, pain, and bladder symptoms.3
Vasomotor symptoms, a hallmark of the MT, have been commonly reported in studies of midlife women. In WLB participants 29% of the LRS group and 57% of the MT+ reported hot flashes and 40% and 51%, respectively reported night/cold sweats. This is similar to the proportion of POAS participants who reported hot flushes (35%) in the premenopausal stage which approximated the LRS. These increased as women entered PM.22,23 SMWHS participants also reported hot flashes during the LRS that increased in severity from the LRS to the MT stages and PM.24
Forgetfulness and difficulty concentrating were rated among the most burdensome and most frequently reported symptoms by WLB participants in both the LRS and MT+ groups. Rochester Investigation of Cognition Across Menopause participants in the LRS performed worse than women in the late MT stage on attention/working memory tasks, but better than women in PM on tests of verbal learning, verbal memory, and motor functioning.7 SMWHS participants reported memory problems (Memory Functioning questionnaire), including forgetfulness, that occurred more frequently during LRS and early MT than the late MT stage.25 Similarly, POAS participants reported difficulty concentrating during the premenopause (analogous to LRS) at a similar rate as women in the early MT.26
As in previous studies, fatigue was commonly reported and the most burdensome symptom in both LRS and MT+ groups in the WLB study. Joint and muscle pain and joint and muscle stiffness were among the most burdensome symptom for both LRS and MT+ women and the proportion reporting both was greater among the MT+ group. SMWHS participants also reported a variety of pain symptoms: back pain increased in severity from the LRS to the MT stages and PM, although joint pain did not change significantly across the MT stages.27 In the POAS cohort, aches were the most prevalent symptom in the premenopause with increases through the late transition stage.23
Sleep disruption has been documented in several studies of midlife women. Approximately 40% of POAS participants in the premenopause reported poor sleep.23,28 Among SMWHS participants only severity of awakening during the middle of the night became more severe with progression through the MT stages.29 The most frequently reported sleep disruption symptom by WLB participants in the LRS was waking in the middle of the night and being awake for more than an hour (42%). While each of the sleep symptoms was more common among the MT+ than the LRS group, none of the differences was statistically significant.
Irritability, anxiety, and feeling overwhelmed were the most reported mood symptoms by WLB participants in the LRS group. The percentage reporting anxiety and feeling overwhelmed was greater for the MT+ versus the LRS group, whereas the percentage reporting irritability was greater for the LRS group. Anxiety, irritability, and mood swings were commonly reported by LRS women in the POAS cohort, but a similar proportion of participants reported these mood symptoms across the MT stages.27 Women in the West Pomerania Study also reported anxiety and mood disorders during the LRS.8 A significantly higher proportion of WLB participants in the MT+ group reported low feelings compared to the LRS group. Depressed mood symptoms were seen in 50% of women in the premenopausal stage and increased to 60% in the late premenopausal stage for POAS participants.30 Similarly, SMWHS participants reported depressed mood symptoms during the LRS which became more severe during the MT stages.31,32
More than 40% of LRS and almost 50% of MT+ women reported urinary leakage with sneezing or coughing. Leakage without sneezing or coughing was the second most bothersome symptom reported by both LRS and MT+ women, and it was the fifth most burdensome symptom for both groups as well. Symptoms of urinary incontinence and nocturia were more commonly reported by women in the LRS than in the MT stages in the University of California, San Francisco Women's Health study.5 Participants in the SMWHS experienced urinary leakage related to coughing or sneezing more frequently during the early MT stage than during the later MT stage and PM.33
There have been several longitudinal studies (eg, POAS, SMWHS, SWAN, Melbourne Women's Midlife Health Project) contributing to understanding symptoms across the MT stages. Only POAS and SMWHS can, however, be used to evaluate the LRS stage as the others did not incorporate the STRAW framework. These studies corroborate that women experience some of the same symptoms during the premenopause (variously defined) as they do during the MT.
Our scoping review3 revealed that much research on late reproductive age women focuses on fertility, including the age-related loss of reproductive potential and success of in vitro fertilization (IVF) in older women. From this body of research, physiologic changes such as diminishing anti-mullerian hormone (AMH), decreased antral follicle count, and rising follicle-stimulating hormone (FSH), as well as considerable individual variation, have been identified in women with regular menstrual cycles,34,35 but investigators have not yet correlated these to symptoms for women during the LRS.
One limitation of our work is that we were not able to collect hormonal data to align with staging or symptoms. Nonetheless, the information available to most clinicians as they encounter women with LRS-related complaints, age, and a menstrual history was included in our survey. We hope that data documenting symptoms often associated with the MT before menstrual cycle irregularity will empower clinicians to validate women's LRS experiences.
Other limitations of this study include the use of an online survey, which restricted participation to those with access to technology. However, the online survey afforded women the ability to respond to questions privately, promoting honest responses. Also, our convenience sample clearly does not represent the general population of midlife women. Our sample is likely biased toward symptomatic women who would be motivated to complete the survey. In addition, the design was cross-sectional, precluding the ability to observe participants’ experiences over time. Finally, the survey was active during the first months of the COVID pandemic during which evidence suggests increased levels of anxiety were widespread.36 Nonetheless, the WLB survey engaged a robust cohort of women who hoped to contribute to an improved understanding of symptoms during the LRS and educate the healthcare providers caring for them.
Another consideration is the effect of age on symptom experiences. Because the stages of reproductive aging occur in the context of general aging, we would expect some symptoms to be correlated with age and others with both age and stages of reproductive aging. We examined the relationship of age to all symptoms, estimating correlations between age and symptoms and partial correlations between stage (LRS and MT+) and each symptom, controlling for age. Burden associated with hot flashes, dryness and itchiness of skin, joint/muscle stiffness, pain with vaginal intercourse and decreased vaginal lubrication, and vaginal dryness were each positively associated with age (P < 0.001) (see Table, Supplemental Digital Content 2, which lists correlations of age and stage controlling for age with symptom burden (Pearson r and partial correlation). Breast soreness and cramps were both negatively associated with age (all P < 0.001). When controlling for age, partial correlations between stage and symptoms were significant for hot flashes, breast soreness, joint/muscle stiffness, pain with vaginal intercourse, decreased lubrication, and vaginal dryness (all P < 0.001).
The LRS and MT+ groups reported similar symptoms in type, frequency, bother and burden, and similar levels of symptom-related interference with relationships and daily living, while they did not anticipate these symptoms would occur until they were older. When these symptoms arise earlier than expected, women are surprised and concerned. In the absence of a 7-day difference between consecutive cycle lengths, healthcare providers may not view these symptom experiences as potentially related to the MT, particularly when women are in their late 30s and early 40s.
Our findings as well as those from previous research suggest that the LRS should be examined in greater detail in future studies. Moreover, clinicians should be alerted to the likelihood that symptoms on the path to menopause may occur during this earlier period of reproductive aging, whereas women's cycles are still regular or when they are noticing only subtle changes to cycle length, days of flow, or amount of flow.
CONCLUSIONS
Many women experience symptoms similar to those reported during the MT before cycle irregularity of a week or more and most do not expect these changes until the age of 50 years or later. Anticipatory guidance for women, education for the clinicians who care for them, as well as ongoing research about the epidemiology, physiology and management of LRS symptoms warrant increased attention. Further enhancement of the STRAW framework will benefit from consideration of recent evidence of women's LRS experience.
Supplementary Material
Supplementary Material
Footnotes
Sources of Funding: None reported.
Financial disclosures/conflicts of interest: None reported.
Supplemental digital content is available for this article.
REFERENCES
- 1.Soules MR, Sherman S, Parrott E, et al. Executive summary: Stages of Reproductive Aging Workshop (STRAW). Fertil Steril 2001; 76:874–878. [DOI] [PubMed] [Google Scholar]
- 2.Harlow SD, Gass M, Hall JE, et al. STRAW + 10 Collaborative Group. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab 2012; 97:1159–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woods NF, Mitchell ES, Coslov ND, Richardson MK. Transitioning to the menopausal transition: a scoping review of research on the late reproductive stage in reproductive aging. Menopause 2021; 28:447–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cray LA, Woods NF, Herting JR, Mitchell ES. Symptom clusters during the late reproductive stage through the early postmenopause: observations from the Seattle Midlife Women's Health Study. Menopause 2012; 19:864–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones HJ, Huang AJ, Subak LL, Brown JS, Lee KA. Bladder symptoms in the early menopausal transition. J Womens Health (Larchmt) 2016; 25:457–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woods NF, Mitchell ES. Consequences of incontinence for women during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women's Health Study. Menopause 2013; 20:915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weber MT, Rubin LH, Maki PM. Cognition in perimenopause: the effect of transition stage. Menopause 2013; 20:511–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jurczak A, Szkup M, Grzywacz A, Safranow K, Grochans E. The analysis of anxiety and mood in healthy late-reproductive-stage women with regard to hormonal and genetic factors. Arch Womens Ment Health 2016; 19:1141–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell ES, Woods NF, Mariella A. Three stages of the menopausal transition from the Seattle Midlife Women's Health Study: toward a more precise definition. Menopause 2000; 7:334–349. [DOI] [PubMed] [Google Scholar]
- 10.Dennerstein L, Dudley E, Hopper J, Guthrie JR, Burger HG. A prospective population-based study of menopausal symptoms. Obstet Gynecol 2000; 96:351–358. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell ES, Woods NF. Symptom experiences of midlife women: observations from the Seattle Midlife Women's Health Study. Maturitas 1996; 25:1–10. [DOI] [PubMed] [Google Scholar]
- 12.Woods NF, Mitchell ES. The Seattle Midlife Women's Health Study: a longitudinal prospective study of women during the menopausal transition and early postmenopause. Womens midlife health 2016; 2:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freeman EW, Sammel MD, Liu L, Martin P. Psychometric properties of a menopausal symptom list. Menopause 2003; 10:258–265. [DOI] [PubMed] [Google Scholar]
- 14.Freeman EW, Sammel MD. Methods in a longitudinal cohort study of late reproductive age women: the Penn Ovarian Aging Study (POAS). Womens Midlife Health 2016; 2:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newton KM, Carpenter JS, Guthrie KA, et al. Methods for the design of vasomotor symptom trials: the Menopausal Strategies: Finding Lasting Answers to Symptoms and Health network. Menopause 2014; 21:45–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woods NF, Hohensee C, Carpenter JS, et al. Symptom clusters among MsFLASH clinical trial participants. Menopause 2016; 23:158–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gapstur RL. Symptom burden: a concept analysis and implication for oncology nurses. Oncology Nursing Forum 2007; 34:673–680. [DOI] [PubMed] [Google Scholar]
- 18.Loprinzi L, Barton DL, Sloan JA, et al. Pilot evaluation of gabapentin for treating hot flashes. Mayo Clin Proc 2002; 77:1159–1163. [DOI] [PubMed] [Google Scholar]
- 19.Carpenter JS. The hot flash related daily interference scale: a tool for assessing the impact of hot flashes on quality of life following breast cancer. J Pain Symptom Manage 2001; 22:979–989. [DOI] [PubMed] [Google Scholar]
- 20.Ruble DN, Brooks-Gunn J. The experience of menarche. Child Dev 1982; 53:1557–1566. [PubMed] [Google Scholar]
- 21.Lennon MC. The psychological consequences of menopause: The importance of timing of a strange life event. J Health Soc Behav 1982; 23:353–366. [PubMed] [Google Scholar]
- 22.Gracia CR, Sammel MD, Freeman EW, et al. Defining menopause status: creation of a new definition to identify the early changes of the menopausal transition. Menopause 2005; 12:128–135. [DOI] [PubMed] [Google Scholar]
- 23.Freeman EW, Sammel MD, Lin H, et al. Symptoms associated with menopausal transition and reproductive hormones in midlife women. Obstet Gynecol 2007; 110:230–240. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell ES, Woods NF. Hot flush severity during the menopausal transition and early postmenopause: beyond hormones. Climacteric 2015; 18:536–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Woods NF, Mitchell ES, Adams C. Memory functioning among midlife women: observations from the Seattle Midlife Women's Health Study. Menopause 2000; 7:257–265. [PubMed] [Google Scholar]
- 26.Mitchell ES, Woods NF. Pain symptoms during the menopausal and early postmenopause: observations from the Seattle Midlife Women's Health Study. Climacteric 2010; 13:467–478. [DOI] [PubMed] [Google Scholar]
- 27.Freeman EW, Sammel MD, Lin H, Gracia CR, Kapoor S. Symptoms in the menopausal transition: hormone and behavioral correlates. Obstet Gynecol 2008; 111:127–136. [DOI] [PubMed] [Google Scholar]
- 28.Hollander LE, Freeman EW, Sammel MD, Berlin JA, Grisso JA, Battistini M. Sleep quality, estradiol levels, and behavioral factors in late reproductive age women. Obstet Gynecol 2001; 98:391–397. [DOI] [PubMed] [Google Scholar]
- 29.Woods NF, Mitchell ES. Sleep symptoms during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women's Health Study. Sleep 2010; 33:539–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freeman EW, Sammel MD, Liu H, Gracia CR, Nelson DB, Hollander BA. Hormones and menopausal status as predictors of depression in women in transition to menopause. Arch Gen Psychiatry 2004; 61:62–70. [DOI] [PubMed] [Google Scholar]
- 31.Mitchell ES, Woods NF. Depressed mood during the menopausal transition: is it reproductive aging or is it life? Womens Midlife Health 2017; 3:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Woods NF, Smith-diJulio K, Percival DB, Tao EY, Mariella A, Mitchell S. Depressed mood during the menopausal transition and early postmenopause: Observations from the Seattle Midlife Women's Health Study. Menopause 2008; 15:223–232. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell ES, Woods NF. Correlates of urinary incontinence during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women's Health Study. Climacteric 2013; 16:653–662. [DOI] [PubMed] [Google Scholar]
- 34.Younis JS, Iskander R, Fauser BCJM, Izhaki I. Does an association exist between menstrual cycle length within the normal range and ovarian reserve biomarkers during the reproductive years? A systematic review and meta-analysis. Hum Reprod Update 2020; 26:904–928. [DOI] [PubMed] [Google Scholar]
- 35.Finkelstein JS, Lee H, Karlamangla A, et al. Antimullerian hormone and impending menopause in late reproductive age: the study of women's health across the nation. J Clin Endocrinol Metab 2020; 105:e1862–e1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fredericksen B, Gomez I, Sagalnicoff A, Ranji U. Coronavirus: a look at gender differences in awareness and actions. The Henry J Kaiser Family Foundation. Available at: https://www.kff.org/womens-health-policy/issue-brief/coronavirus- a-look-at-gender-differences-in awareness-and-actions/. Accessed February 22, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.