Highlights
-
•
In a sample of recurrently depressed women, 12.8% had elevated ADHD symptoms.
-
•
3.4% met ADHD diagnostic criteria; none had a diagnosis from a medical professional.
-
•
ADHD was associated with earlier-onset, more impairing and recurrent depression.
-
•
Recurrently depressed women with ADHD symptoms were more likely to be hospitalised.
-
•
ADHD symptoms were associated with taking non-first-line antidepressant medication.
Keywords: Attention deficit/hyperactivity disorder, ADHD, Depression, Women, Clinical presentation, Clinical management
Abstract
Background
Depression is highly heterogeneous in its clinical presentation. Those with attention deficit/hyperactivity disorder (ADHD) may be at risk of a more chronic and impairing depression compared to those with depression alone according to studies of young people. However, no studies to date have examined ADHD in recurrently depressed adults in mid-life.
Method
In a sample of women in mid-life (n=148) taken from a UK based prospective cohort of adults with a history of recurrent depression, we investigated the prevalence of ADHD and the association of ADHD with clinical features of depression.
Results
12.8% of the recurrently depressed women had elevated ADHD symptoms and 3.4% met DSM-5 diagnostic criteria for ADHD. None of the women reported having a diagnosis of ADHD from a medical professional. ADHD symptoms were associated with earlier age of depression onset, higher depression associated impairment, a greater recurrence of depressive episodes and increased persistence of subthreshold depression symptoms over the study period, higher levels of irritability and increased risk of self-harm or suicide attempt. ADHD symptoms were associated with increased risk of hospitalisation and receiving non-first-line antidepressant medication.
Limitations
ADHD was measured using a questionnaire measure. We focussed on mothers in a longitudinal study of recurrent depression, so the findings may not apply to males or other groups.
Conclusions
Higher ADHD symptoms appear to index a worse clinical presentation for depression. Clinical implications include that in women with early onset, impairing and recurrent depression, the possibility of underlying ADHD masked by depression needs to be considered.
1. Introduction
Depression is a highly heterogeneous disorder that varies in its origins and clinical presentation (Fried and Nesse, 2015; Kendler et al., 1996; Weissman et al., 1986). Studies of children and adolescents have found that individuals with attention deficit/hyperactivity disorder (ADHD), a neurodevelopmental disorder, are at higher risk of early-onset, recurrent depression compared to those without ADHD (Biederman et al., 2008; Riglin et al., 2020). Both epidemiological and clinical studies report associations between early onset depression and neurodevelopmental disorders and traits, especially ADHD (Biederman et al., 2008; Bron et al., 2016; Jaffee et al., 2002; Rice et al., 2019; van Os et al., 1997). One four-year follow-up study of depressed adults and community controls aged 21 to 69 years found increased odds of having probable ADHD in those with longer lasting depressive episodes and in those with a reported age of onset of before 21 years old compared to onset after 21 (Bron et al., 2016). However, the impact of ADHD on different aspects of depression presentation in those with recurrent depression in midlife is not known.
There is evidence to suggest that there is a neurodevelopmental genetic contribution to some forms of depression, including ADHD and schizophrenia genetic risk (Lee et al., 2019; Power et al., 2017; Rice et al., 2019). For instance, one such study of a population sample followed from birth to young adulthood found that an earlier-onset, more chronic class of depression was associated with a higher level of neurodevelopmental traits, including ADHD symptoms, ADHD genetic risk and schizophrenia genetic risk (Rice et al., 2019). Another population-based study found that ADHD genetic risk was increased in those with treatment resistant depression compared to non-treatment resistant depression (Fabbri et al., 2021). Those with depression that is accompanied by ADHD are a clinically important group as they show higher rates of antidepressant treatment resistance, suicide and psychiatric hospitalisation compared to those with depression alone (Biederman et al., 2008, 1996; Chen et al., 2016). ADHD that persists into adulthood is associated with more comorbid mental health problems (Agnew-Blais et al., 2016; Riglin et al., 2016). However, neurodevelopmental disorders that were not identified in childhood can be missed in adults, especially among women (Martin et al., 2018). There is also emerging evidence to suggest that recurrent adult depression may mask underlying neurodevelopmental disorders including ADHD that are missed in clinical practice (McIntosh et al., 2009). However, the rate of ADHD in middle-aged adults with recurrent depression in the community and the impact of ADHD on depression presentation in this group are unknown.
In this UK based longitudinal study spanning 13 years, we aim to investigate ADHD in women with recurrent depression. First, we investigate the prevalence of ADHD in this group. Next, we investigate a number of clinical features of depression potentially associated with ADHD including age of onset, severity, episode recurrence, subthreshold symptom persistence, suicide and self-harm attempts, psychotic affective symptoms and irritability symptoms. Additionally, we investigate the association of ADHD symptoms with aspects of the clinical management of depression, including hospitalisation and use of first-line versus non-first-line antidepressant medication, as an indicator of poor treatment response or a complex clinical presentation.
2. Method
2.1. Sample
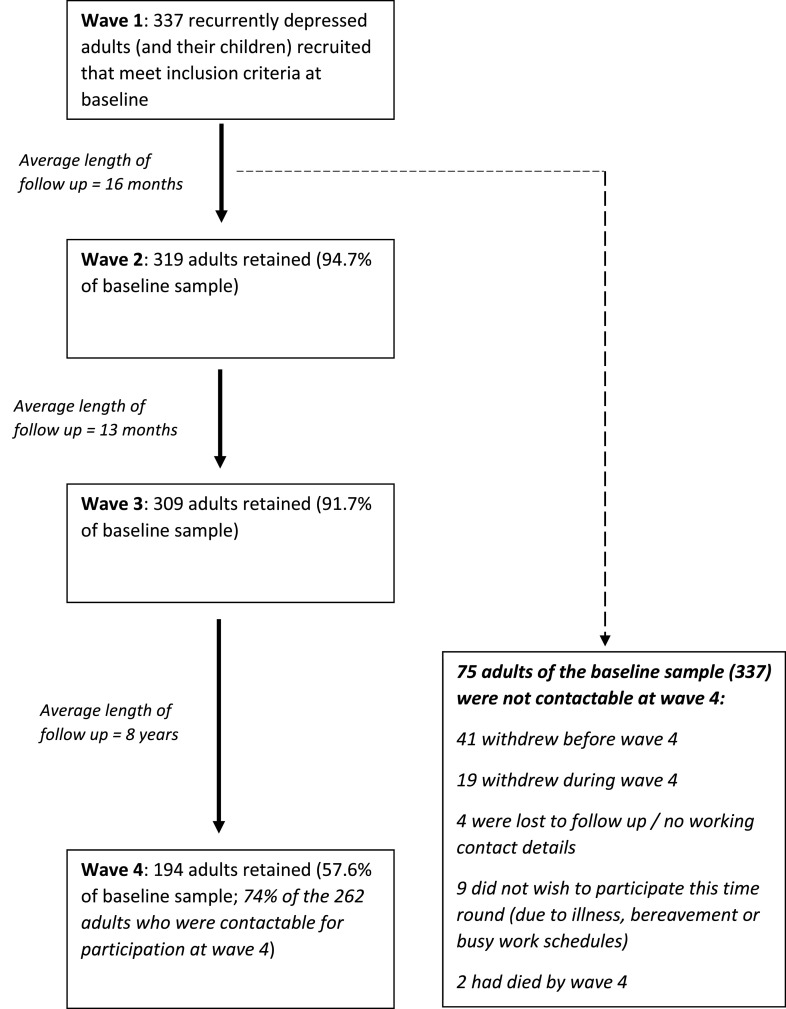
Data came from the Early Prediction of Adolescent Depression (EPAD) study – a prospective longitudinal study of recurrently depressed parents and their offspring based in the UK (Mars et al., 2012). The baseline sample included 337 parents with recurrent unipolar depression (two or more lifetime DSM-IV Major Depressive Disorder (MDD) episodes confirmed at interview) and their offspring. Families were assessed at 4 time points between April 2007 and September 2020 via interview and questionnaire. The average length of follow up was 16 months between the first and second waves, 13 months between the second and third, and 8 years between the third and fourth. The current study focuses primarily on the fourth assessment wave, as adult ADHD data was collected during this wave. The fourth wave was carried out between 2018 and 2020 and 197 families participated. Study design and participation rates are summarised in Fig. 1. Reasons for the lower retention rate between the third and fourth assessment waves include: death of participants, loss to follow-up and withdrawal from the study. Of the 197 participating families at wave 4, 159 mothers had data on their own ADHD symptoms. Of these 159, 148 women (mean age: 53, range: 42 – 67) with complete data on their own ADHD symptoms, clinical features of their depression, irritability and sociodemographic variables formed the primary sample. Analysis of baseline factors associated with drop-out by wave 4 is shown in Supplement 1. Ethical approval was granted by the Multi-Centre Research Ethics Committee for Wales and from the School of Medicine Ethics Committee, Cardiff University. Written informed consent and assent was gained from each of the participants at each wave. More detailed information about recruitment, assessments and sample characteristics at assessment waves 1 to 3 can be found elsewhere (Mars et al., 2015, 2012).
Fig 1.
Study design and participation rates across assessment waves of the EPAD study. The Early Prediction of Adolescent Depression (EPAD) study took place over four assessment waves between April 2007 and September 2020 via interview and questionnaire. Numbers of participants reported are those participating at each wave via questionnaire, interview or both. Only 262 adults were contactable at wave 4. Reasons for this include loss of up to date contact details, withdrawal from the study, death and declining to participate due to ill health, bereavement or other commitments such as work (n=75). Of the 262 contactable participants at wave 4, 68 were unresponsive despite multiple communication attempts.
2.2. Overview of assessment procedure
The sample was recruited mainly from general practice surgeries in South Wales (78%). Additional participants were recruited using a database of individuals who had been identified as having previous unipolar depression, via community mental health teams and advertisements in local media and primary care centres (Mars et al., 2012). The original aim of the study was to conduct a cross-generational study to examine the offspring of parents with recurrent depression, so all participants had biologically related offspring living at home in the age range of 9-17 years at the time of initial recruitment. Recruited adults were screened over the telephone to ensure they met inclusion criteria: suffered from re-current unipolar depression (at least 2 episodes, which were later confirmed using diagnostic interview). Adults were not required to be experiencing a depressive episode at the time of recruitment. Adults who had a lifetime diagnosis of bipolar or psychotic disorder and those who met criteria for DSM-IV mania or hypomania at the time of the interview were excluded.
At each assessment wave (1 through 4), the Schedule for Clinical Assessment (SCAN) (Wing et al., 1990) was used to assess adult DSM-IV MDD based on the symptoms and impairment reported in the preceding month. All cases meeting criteria for diagnosis in addition to subthreshold cases were reviewed by two psychiatrists and diagnoses were made according to clinical consensus. At the baseline assessment, participants were additionally asked to report on their worst ever and second worst ever episodes of depression and associated impairment. They were also asked to retrospectively report on various clinical features of their depression including first age of onset. A life history calendar approach was used for all retrospectively reported information to aid recall (Belli, 1998). At all subsequent assessment waves, participants were asked to report on episodes of depression they had experienced since the previous assessment wave and to report on associated impairment. Participants additionally completed a questionnaire booklet which included questions relating to sociodemographic information, family structure and relationships, and psychiatric symptom measures such as the Beck Depression Inventory (BDI) (Beck et al., 1961).
2.3. Measures
2.3.1. Adult ADHD
Participants completed the Adult ADHD Investigator Symptom Rating Scale (AISRS) (Spencer et al., 2009) via questionnaire at wave 4. The AISRS consists of 18 items based on the DSM-5 (American Psychiatric Association, 2013) symptoms of ADHD. Symptoms were rated on a 4-point scale of “Never/Rarely” (0), “Sometimes” (1), “Often” (2) and “Very often” (3).
Predictor variables were 1) a total ADHD symptom score (possible range: 0-54) and 2) a binary variable of “elevated ADHD symptoms”. Those meeting the AISRS clinical cut point by scoring 24 or higher (Silverstein et al., 2018) were classed as having elevated ADHD symptoms.
Diagnosis: Participants were also asked to complete a further set of questions in the questionnaire if they reported ADHD symptoms: at what age they could recall these symptoms starting in approximate years and to indicate whether the symptoms impacted on functioning in a number of areas of life. For descriptive purposes, participants were classed as meeting DSM-5 criteria for adult ADHD diagnosis if they reported at least 5 current symptoms, an age of onset of these problems prior to 12 years old and associated impairment in home, work or social life (American Psychiatric Association, 2013).
During the interview at assessment wave 4, participants were also asked to report on their recent and current service use and any diagnoses they had received from a medical professional using a questionnaire adapted from the Children's Services Interview (Ford et al., 2007), which was used to establish if any participants had received a clinical diagnosis of ADHD.
2.3.2. Clinical features of depression
2.3.2.1. Age of onset
Participants were asked at baseline interview to report the age of onset (in years) of their first MDD episode. Age of onset was dichotomised so that onset at 25 years old or earlier was classed as early-onset depression based on previous studies (Power et al., 2017).
2.3.2.2. Severity
Impairment associated with depression was measured using the Global Assessment of Functioning (GAF) (American Psychiatric Association, 1994), which was assessed for the worst ever episode reported by the participant at baseline interview and at each subsequent assessment phase for current/recent depression. A binary measure was derived capturing whether participants had ever had a GAF score ≤ 50 during the study period with GAF scores below or equal to 50 indicating serious impairment in work or social life (American Psychiatric Association, 1994).
2.3.2.3. Episode recurrence
A count variable of the recurrence of depressive episodes across the study period was derived. This included a count of the number of assessment points at which participants met clinical criteria for MDD plus the number of times participants reported being depressed since the last assessment wave (possible range=0-7).
2.3.2.4. Subthreshold persistence
In addition to recurrence of depression episodes meeting diagnostic criteria, chronicity of subthreshold symptoms over time is common and impairing (Fergusson et al., 2005; Judd et al., 1998). Thus, as an indicator of persistence of depression symptoms over time, self-report questionnaire measures of depressive symptoms at waves 1 through 4 were used to derive a measure of subthreshold depression persistence. These were the Patient Health Questionnaire (PHQ) (Kroenke et al., 2001) at waves 1 and 4 and the Beck Depression Inventory (BDI) (Beck et al., 1961) at waves 2 and 3 – both valid and reliable measures of depressive symptoms (Beck et al., 1988; Kroenke et al., 2001; Strober et al., 1981). Depressive symptom scores were calculated at each wave. Those falling into the “intermediate” symptoms group (between the “none/mild” and “severe” group: scoring 5-19 on the PHQ or 10-29 on the BDI) were defined at each wave based on the cut points validated for the PHQ and BDI (Beck et al., 1988; Kroenke et al., 2001). A count of the number of times symptoms were of the intermediate level was derived (possible range=0-4).
2.3.2.5. Suicide and self-harm attempt
The SCAN (Wing et al., 1990) was used to assess self-harm or suicide at each wave with the question “Have you thought about harming yourself or even made an attempt at suicide during the last month?”. Participants responses were coded as ‘absent’ (0), ‘intrusive thoughts but no attempt’ (1), ‘injured self but no serious harm resulted’ (2), ‘injured self and serious harm resulted’ (3) or ‘made an attempt at suicide designed to result in death’ (4). A binary variable capturing whether participants had ever reported self-harm or suicide attempts (scored 2 or more) at any of the four assessment waves was derived.
2.3.2.6. Psychotic affective symptoms
A binary variable capturing whether participants had ever endorsed psychotic affective symptoms during the SCAN (Wing et al., 1990) at waves 1 to 4 was derived. Psychotic affective symptoms assessed were delusions of guilt, delusions of catastrophe, hypochondriacal delusions and auditory hallucinations.
2.3.2.7. Irritability
Participants completed the Affective Reactivity Index (ARI) (Stringaris et al., 2012) via questionnaire at wave 4. Though it was developed to assess irritability in children and adolescents, it has been shown to be a reliable and valid measure in adult samples (Stringaris et al., 2012). The ARI consists of 7 items with responses of “Not true” (0), “Somewhat true” (1) or “Certainly true” (2), which are summed to give a total score (possible range=0-14).
2.3.2.8. Hospitalisations
Participants reported the number of times they had ever been hospitalised due to depression at baseline, and the number of times they had been hospitalised since the last assessment wave at waves 2 and 3. At wave 4, participants were not asked explicitly to report the number of hospitalisations, but they were asked to give details of what happened during any depressive episodes experienced since the last wave, which gave an opportunity to disclose hospitalisations. From this information, a binary variable was derived capturing whether participants had ever been hospitalised due to depression.
2.3.2.9. Antidepressant medication
At wave 4, participants reported what medication they were currently taking, including medication for depression. Based upon UK National Institute for Health and Care Excellence (NICE) clinical guidelines for management of adult depression and the British National Formulary (BNF) (Joint Formulary Committee, n.d.; National Institute for Health and Care Excellence (NICE), 2009), a binary variable of no depression treatment or first-line depression treatment (use of an SSRI) versus non-first-line depression medication (use of an antidepressant other than an SSRI, use of two or more antidepressants, or an antidepressant augmented with lithium or an antipsychotic) was derived. The use of non-first-line antidepressant medication might indicate either poor response to standard, first-line antidepressants (SSRIs), or the need to address complexities in a patient's depression presentation (National Institute for Health and Care Excellence (NICE), 2009).
2.3.3. Confounders
All regression analyses presented were adjusted for sociodemographic factors associated with depression that might confound associations (Gilman et al., 2002). The confounders adjusted for were financial status and educational attainment (assessed as having attained qualifications at end of compulsory education, e.g. GCSEs or equivalent qualifications (Yes/No)).
2.4. Analysis
2.4.1. Association between ADHD and clinical features of depression
A series of linear and logistic regression analyses were conducted as appropriate to test the association of ADHD symptoms and clinical features of depression. Continuous ADHD symptoms were standardised (z-scored) so that a one-unit increase was equivalent to one standard deviation increase. All regression analyses were then repeated for ADHD defined as elevated symptoms, entered as a binary variable instead of a continuous variable. This was to test whether the presentation of depression was significantly different for those above the AISRS clinical cut point for ADHD (≥24) compared to those below the cut-point.
2.4.2. Missing data
Regression analyses were repeated with Inverse Probability Weights (IPW) applied to assess possible bias arising from potential non-random missing data. IPW is a reliable approach to handling missing data, particularly in longitudinal cohorts where participants can have missing data for multiple variables (Seaman and White, 2013). Weights were generated using predictors of missingness from the sample (Supplement 2).
3. Results
In the primary sample of recurrently depressed females (n=148), 12.8% (n=19) had elevated ADHD symptoms, indicated by having an AISRS score above the validated clinical cut point (>24), and 3.4% (n=5) met DSM-5 diagnostic criteria for adult ADHD. The lower number of those who met diagnostic criteria was explained by participants not meeting the age of onset criterion specified in the DSM-5 (<12 years). None of the women in the study however, reported having been diagnosed with ADHD by a medical professional or receiving medication for ADHD. Descriptive statistics are shown in Table 1.
Table 1.
Descriptive statistics.
| Variable | Mean (SD) / % (n) | Range |
|---|---|---|
| ADHD symptoms | 11.19 (10.02) | 0 - 50 |
| Age of onset of depression (% onset ≤25 years) | 26.01 (7.98) / 45.3% (67) | 8 - 46 |
| Ever had GAF score ≤ 50 (Severe impairment associated with depression) | 73.0% (108) | Binary: 0=No, 1=Yes |
| Number of MDD episodes during study | 2.42 (1.69) | 0 - 7 |
| Subthreshold depression persistence | 1.97 (1.34) | 0 - 4 |
| Ever hospitalised | 17.6% (26) | Binary: 0=No, 1=Yes |
| Use of non-first-line antidepressants | 20.3% (30) | Binary: 0=No, 1=Yes |
| Ever attempted self-harm or suicide during study | 4.1% (6) | Binary: 0=No, 1=Yes |
| Ever had psychotic affective symptoms during study | 12.8% (19) | Binary: 0=No, 1=Yes |
| Irritability score | 2.65 (2.84) | 0 - 14 |
Descriptive statistics in complete case women (n=148). ADHD attention-deficit/hyperactivity disorder, MDD major depressive disorder, GAF Global Assessment of Functioning, SD standard deviation
3.1. Association between ADHD and clinical features of depression
Standardised ADHD symptoms were associated with an earlier age of depression onset (≤ 25 years) and associated severe impairment (GAF ≤ 50) (Table 2). ADHD symptoms were also associated with MDD episode recurrence over the 13-year period of the study, and persistent subthreshold depressive symptoms over the study period. ADHD symptoms were associated with increased risk of reporting self-harm or suicide attempt during the study period, but were not associated with psychotic affective symptoms. ADHD symptoms were associated with higher irritability symptoms.
Table 2.
Association between adult ADHD symptoms (continuous and dichotomised) and clinical features of depression
| Clinical feature of depression | Association with self-reported adult ADHD symptom score |
Association with dichotomised self-reported adult ADHD symptoms (above clinical cut-point versus below) |
||
|---|---|---|---|---|
| b or OR (95% CI) | p-value | b or OR (95% CI) | p-value | |
| Depression age of onset of 25 or before | OR=1.45 (1.02, 2.05) | 0.040 | OR=2.09 (0.74, 5.88) | 0.163 |
| Ever had GAF score ≤ 50 (Severe impairment associated with depression) | OR=1.73 (1.08, 2.75) | 0.021 | - - | - - - |
| Number of MDD episodes during study | b=0.74 (0.51, 0.98) | <0.001 | b=1.93 (1.17, 2.69) | <0.001 |
| Subthreshold depression persistence | b=0.22 (0.01, 0.43) | 0.044 | b=0.29 (-0.368, 0.948) | 0.385 |
| Ever hospitalised | OR=1.94 (1.29, 2.91) | 0.001 | OR=4.58 (1.58, 13.25) | 0.005 |
| Use of non-first-line antidepressants | OR=2.04 (1.35, 3.09) | 0.001 | OR=5.85 (1.99, 17.23) | 0.001 |
| Ever attempted self-harm or suicide during study | OR=3.46 (1.46, 8.21) | 0.005 | - - - | - - - |
| Ever had psychotic affective symptoms during study | OR=0.89 (0.56, 1.40) | 0.603 | OR=0.92 (0.22, 3.98) | 0.916 |
| Irritability score | b=1.54 (1.18, 1.90) | <0.001 | b=3.55 (2.32, 4.78) | <0.001 |
Results in complete case women are shown (n=148). ADHD symptoms were dichotomised using the clinical cut point of the Adult ADHD Investigator Symptom Rating Scale AISRS (≥24). All participants above the cut point for ADHD had had a GAF score below 50, so the association of dichotomised ADHD and depression impairment could not be tested due to complete separation issues. The association between dichotomised ADHD and suicide or self-harm attempts could not be tested due to small cell sizes. ADHD attention-deficit/hyperactivity disorder, MDD major depressive disorder, GAF Global Assessment of Functioning, b unstandardized beta, CI confidence interval, OR odds ratio
In addition, ADHD symptoms were associated with increased odds of ever being hospitalised and treatment with a non-first-line antidepressant medication, which may be indicative of poor response to first-line antidepressants or a complex clinical presentation. The frequencies of different psychotropic medication types used are reported in Supplement 3, which includes depression medication and other neuropsychiatric medications. Of the primary sample (n=148), 63.5% (n=94) reported taking psychotropic medication and 19.6% (n=29) reported taking more than one psychotropic medication.
The same associations were tested with ADHD as a binary variable: those above the AISRS clinical cut-point for ADHD vs. those below the cut-point. Elevated ADHD symptoms were associated with increased recurrence of depressive episodes, increased irritability symptoms, increased risk of hospitalisation and taking non-first-line depression medication. ADHD symptoms above the clinical cut point were also associated with a 2-fold increase in odds of early onset depression, but this did not reach conventional thresholds for significance. The association of elevated ADHD symptoms with severe impairment could not be tested, as all participants with elevated ADHD symptoms had had a GAF score below or equal to 50, and the association with suicide and self-harm attempts could not be tested due to small cell sizes.
Results remained similar with IPW applied (Supplement 4). However, the association between total ADHD symptoms and subthreshold persistence attenuated after IPW was applied.
4. Discussion
In a prospective, longitudinal study of recurrently depressed women, we investigated the prevalence of ADHD and the effect of comorbid ADHD on the clinical phenotype of depression. In this sample, 12.8% had elevated ADHD symptoms and 3.4% met DSM-5 diagnostic criteria for ADHD. These are higher than estimates reported in general population samples of adults (2.5%) (Simon et al., 2009). None of the participants with ADHD had been clinically diagnosed by a medical professional. ADHD is not typically assessed in adult clinical settings. However, those with high ADHD symptoms were more likely to be taking non-first-line antidepressant medication, which might suggest that these individuals were recognised by clinicians as having a more complex depression presentation or poor response to first-line antidepressants (National Institute for Health and Care Excellence (NICE), 2009). ADHD symptoms were also associated with earlier age of depression onset, higher depression associated impairment, a greater number of depressive episodes over the study assessment period, increased persistence of subthreshold depression symptoms, higher levels of irritability, increased odds of self-harm or suicide and increased odds of hospitalisation.
Our findings suggest that a proportion of women in mid-life with a history of early-onset, recurrent depression that has been severely impairing may have undetected ADHD. Previous studies have shown associations of ADHD in childhood and adolescence with more severe depressive outcomes in young adulthood, such as depression recurrence, suicide and hospitalisation (Biederman et al., 2008; Riglin et al., 2020). There is evidence from a national register-based study that those with ADHD and depression may be at higher risk of antidepressant treatment resistance than those with depression alone (Chen et al., 2016). A four-year follow-up study of depressed adults and controls found that odds of probable ADHD were higher when depression episodes were longer and when participants reported more severe episodes and an age of onset of depression before 21 (Bron et al., 2016). However, no studies to date have examined recurrently depressed adults, or adults in mid-life. Therefore, the present study builds on the existing literature by examining the impact of ADHD on a number of different features of depression presentation in this recurrently depressed group. This is important given the emerging evidence that recurrent adult depression may mask underlying neurodevelopmental disorders such as ADHD that are missed in clinic (McIntosh et al., 2009).
There is much heterogeneity observed in the presentation of depression (Fried and Nesse, 2015; Kendler et al., 1996; Weissman et al., 1986), including in its first age-at-onset and chronicity of illness. Our results suggest that part of this may be accounted for or indexed by comorbid ADHD in some cases. It is possible that some individuals, even if they do not fulfil diagnostic criteria for ADHD, have a more ‘neurodevelopmental type’ of depression characterised by early onset, persistence of symptomatology over time and overlap with neurodevelopmental traits, including ADHD symptoms (Jaffee et al., 2002; Rice et al., 2019; van Os et al., 1997). For instance, one study found that an earlier onset, more chronic class of depressive symptoms from childhood to early adulthood (age 18) was associated with more neurodevelopment traits (ADHD, pragmatic language skills and autistic traits) and ADHD genetic risk scores (Rice et al., 2019). Other studies also suggest that the genetic architecture of earlier onset depression may be more neurodevelopmental in nature and tends to be more strongly associated with neurodevelopmental genetic risk (Musliner et al., 2019; Power et al., 2017; Thapar and Riglin, 2020). The present study is important and novel because it examines women in mid-life with recurrent diagnosed depression from a longitudinal cohort spanning 13 years. It is important to note that those with early onset depression may have symptoms that desist by early adulthood or persist into adulthood (e.g. Jaffee et al., 2002). In the present study of recurrently depressed adults, age of depression onset is measured using retrospective report. This might affect results by capturing a specific, persistent subgroup of those with early onset depression.
Our findings have important clinical implications. They suggest that in women with early onset, recurrent depression in adulthood, the possibility of depression masking underlying ADHD needs to be considered. Effective treatment of ADHD along with depression could improve functioning and associated depression symptoms (Chang et al., 2016). Even for those who do not meet diagnostic criteria for ADHD, higher ADHD symptoms appear to index a worse clinical picture. It is possible that they represent a ‘neurodevelopmental type’ of depression presentation, including earlier age of onset, increased severity and recurrence and more prominent irritability. Therefore, they may require more frequent follow-up or different types of management for depression. It will be important for future studies to examine whether this group might respond to different types of depression treatment to those that are typically used for depression such as cognitive behavioural therapy and SSRI antidepressants.
Limitations of this work include the measurement of ADHD was based on a questionnaire measure completed at one assessment wave. Also, in this study we focussed on women with adolescent children who had participated in a longitudinal study of recurrent depression so the findings may not apply to males or other groups, for example, hospitalised patients. The rate of ADHD observed may be influenced by specific characteristics of the present sample. Rates of ADHD may be higher in this sample because individuals all had recurrent depression. However, given that ADHD is associated with multiple social and educational impairments (Harpin, 2005), those with comorbid ADHD also may be under-represented in this sample. As age of onset was reported retrospectively in this study, results may be affected by recall bias (Drews and Greeland, 1990). In addition, the retrospective data did not allow for reliable differentiation between childhood, adolescent or early adulthood onset depression within the early-onset group, which have been found to behave differently in terms of associations and persistence when age of onset is inferred using prospectively collected data (Rice et al., 2019). Overall comorbidity as opposed to comorbidity with ADHD specifically may have contributed to results. Indeed, we observed high rates of co-occurring anxiety symptoms in the recurrently depressed adults with ADHD symptoms, which is consistent with previous studies that report high rates of comorbidity of ADHD with both anxiety and with depression (Kessler et al., 2006). However, when adjusting our regressions for anxiety symptoms, results remained very similar (Supplement 5), suggesting the impact of ADHD on depression presentation is still observed when accounting for other comorbidity. It is also important to note that although use of non-first-line antidepressant medication can indicate poor response to first-line antidepressants or a complex clinical presentation, there may be other reasons that a non-first-line antidepressant is prescribed, for example, experience of side effects. As is common in longitudinal cohort studies, there was some attrition of the sample over time. Analysis of baseline factors associated with drop-out at wave 4 (Supplement 4), showed that while factors such as lower socioeconomic status and education were associated with attrition, other factors associated with severity of depression and history of depression treatment were not. These included the percentage of the participant's life that they had been unwell since depression onset and previous non-pharmacological treatment for depression (including talking therapies and electroconvulsive therapy). This might suggest that those with more severe depression or a history of depression treatment may be more likely to stay in the current study, which is likely due to the inclusion criteria of the EPAD study, namely that the participant had experienced at least 2 prior episodes of depression. Nevertheless, to account for any potential bias arising from attrition, analyses were adjusted for variables associated with missingness, helping to address potential bias due to missing data (Groenwold et al., 2012). In addition, regression results when inverse probability weights were applied remained similar, suggesting bias due to missingness was minimal (Supplement 3) (Seaman and White, 2013).
To conclude, we found that in a sample of recurrently depressed adults, ADHD was associated with an earlier onset, more impairing and recurrent depression presentation, in addition to increased risk of self-harm, hospitalisation and receiving non-first-line antidepressant medication. Higher ADHD symptoms appear to index a worse clinical presentation for depression. Findings suggest that in women with early onset, recurrent depression, the possibility of underlying ADHD masked by depression needs to be considered. It is also possible that specifically treating ADHD symptoms in women with recurrent depression will improve long-term clinical outcomes.
Funding
The work was supported by the Medical Research Council (MR/R004609/1). The cohort was established with funding from the Jules Thorn Charitable Trust (JTA/06). The work was also supproted by the Wolfson Centre for Young People's Mental Health - established with support from the Wolfson Foundation.
Author contributions
VP and FR conceptualised the study. VP conducted the analysis and drafted the manuscript. DS, JA and RP conducted clinical consensus meetings. AS, BW and JL carried out data collection during the most recent assessment wave. All authors provided critical revision to the manuscript, approved the final version and consented to its publication.
Data availability
The data that support the findings of this study are available on reasonable request from the corresponding author, Victoria Powell. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Declaration of Competing Interest
The authors declare that they have no conflicts of interest.
Acknowledgments
We are very grateful to all the participating families in the Early Prediction of Adolescent Depression study. We thank the GPs and psychiatrists who helped with this study. We thank all of the assistant psychologists and research assistants who carried out data collection. Thank you to Tom Brice for advice on depression medication categories.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.09.010.
Appendix. Supplementary materials
References
- Agnew-Blais J.C., Polanczyk G.V, Danese A., Wertz J., Moffitt T.E., Arseneault L. Evaluation of the persistence, remission, and emergence of attention-deficit/hyperactivity disorder in young adulthood. JAMA Psychiatry. 2016;73:713–720. doi: 10.1001/jamapsychiatry.2016.0465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders (DSM-V).
- American Psychiatric Association . 4th ed. Author; Washington, DC: 1994. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) [Google Scholar]
- Beck A.T., Steer R.A., Garbin M.G. Psychometric properties of the beck depression inventory: twenty-five years of evaluation. Clin. Psychol. Rev. 1988 doi: 10.1016/0272-7358(88)90050-5. [DOI] [Google Scholar]
- Beck A.T., Ward C.H., Mendelson M., Mock J., Erbaugh J. An inventory for measuring depression. Arch. Gen. Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Belli R.F. The structure of autobiographical memory and the event history calendar: potential improvements in the quality of retrospective reports in surveys. Memory. 1998;6:383–406. doi: 10.1080/741942610. [DOI] [PubMed] [Google Scholar]
- Biederman J., Ball S.W., Monuteaux M.C., Mick E., Spencer T.J., McCreary M., Cote M., Faraone S.V. New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. J. Am. Acad. Child Adolesc. Psychiatry. 2008;47:426–434. doi: 10.1097/CHI.0b013e31816429d3. [DOI] [PubMed] [Google Scholar]
- Biederman J., Faraone S., Milberger S., Guite J., Mick E., Chen L., Mennin D., Marrs A., Ouellette C., Moore P., Spencer T., Norman D., Wilens T., Kraus I., Perrin J. A prospective 4-year follow-up study of attention-deficit hyperactivity and related disorders. Arch. Gen. Psychiatry. 1996;53:437–446. doi: 10.1001/archpsyc.1996.01830050073012. [DOI] [PubMed] [Google Scholar]
- Bron T.I., Bijlenga D., Verduijn J., Penninx B.W.J.H., Beekman A.T.F., Kooij J.J.S. Prevalence of ADHD symptoms across clinical stages of major depressive disorder. J. Affect. Disord. 2016;197:29–35. doi: 10.1016/j.jad.2016.02.053. [DOI] [PubMed] [Google Scholar]
- Chang Z., D'Onofrio B.M., Quinn P.D., Lichtenstein P., Larsson H. Medication for attention-deficit/hyperactivity disorder and risk for depression: a nationwide longitudinal cohort study. Biol. Psychiatry. 2016;80:916–922. doi: 10.1016/j.biopsych.2016.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M.-H., Pan T.-L., Hsu J.-W., Huang K.-L., Su T.-P., Li C.-T., Lin W.-C., Tsai S.-J., Chang W.-H., Chen T.-J., Bai Y.-M. Attention-deficit hyperactivity disorder comorbidity and antidepressant resistance among patients with major depression: a nationwide longitudinal study. Eur. Neuropsychopharmacol. 2016;26:1760–1767. doi: 10.1016/j.euroneuro.2016.09.369. [DOI] [PubMed] [Google Scholar]
- Drews C.D., Greeland S. The impact of differential recall on the results of case-control studies. Int. J. Epidemiol. 1990;19:1107–1112. doi: 10.1093/ije/19.4.1107. [DOI] [PubMed] [Google Scholar]
- Fabbri C., Hagenaars S.P., John C., Williams A.T., Shrine N., Moles L., Hanscombe K.B., Serretti A., Shepherd D.J., Free R.C., Wain L.V, Tobin M.D., Lewis C.M. Genetic and clinical characteristics of treatment-resistant depression using primary care records in two UK cohorts. Mol. Psychiatry. 2021 doi: 10.1038/s41380-021-01062-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson D.M., Horwood L.J., Ridder E.M., Beautrais A.L. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch. Gen. Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- Ford T., Hamilton H., Dosani S., Burke L., Goodman R. The children's services interview: validity and reliability. Soc. Psychiatry Psychiatr. Epidemiol. 2007;42:36–49. doi: 10.1007/s00127-006-0092-9. [DOI] [PubMed] [Google Scholar]
- Fried E.I., Nesse R.M. Depression is not a consistent syndrome: an investigation of unique symptom patterns in the STAR*D study. J. Affect. Disord. 2015;172:96–102. doi: 10.1016/j.jad.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman S.E., Kawachi I., Fitzmaurice G.M., Buka S.L. Socioeconomic status in childhood and the lifetime risk of major depression. Int. J. Epidemiol. 2002;31:359–367. doi: 10.1093/intjepid/31.2.359. [DOI] [PubMed] [Google Scholar]
- Groenwold R.H.H., Donders A.R.T., Roes K.C.B., Harrell F.E.J., Moons K.G.M. Dealing with missing outcome data in randomized trials and observational studies. Am. J. Epidemiol. 2012;175:210–217. doi: 10.1093/aje/kwr302. [DOI] [PubMed] [Google Scholar]
- Harpin V.A. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch. Dis. Child. 2005;90:i2–i7. doi: 10.1136/adc.2004.059006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee S.R., Moffitt T.E., Caspi A., Fombonne E., Poulton R., Martin J. Differences in early childhood risk factors for Juvenile-Onset and adult-Onset depression. Arch. Gen. Psychiatry. 2002;59:215–222. doi: 10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- Joint Formulary Committee, n.d. British national formulary [WWW Document]. URL http://www.medicinescomplete.com (accessed 1.26.21).
- Judd L.L., Akiskal H.S., Maser J.D., Zeller P.J., Endicott J., Coryell W., Paulus M.P., Kunovac J.L., Leon A.C., Mueller T.I., Rice J.A., Keller M.B. A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Arch. Gen. Psychiatry. 1998;55:694–700. doi: 10.1001/archpsyc.55.8.694. [DOI] [PubMed] [Google Scholar]
- Kendler K.S., Eaves L.J., Walters E.E., Neale M.C., Heath A.C., Kessler R.C. The identification and validation of distinct depressive syndromes in a population-based sample of female twins. Arch. Gen. Psychiatry. 1996;53:391–399. doi: 10.1001/archpsyc.1996.01830050025004. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Adler L., Barkley R., Biederman J., Conners C.K., Demler O., Faraone S.V, Greenhill L.L., Howes M.J., Secnik K., Spencer T., Ustun T.B., Walters E.E., Zaslavsky A.M. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am. J. Psychiatry. 2006;163:716–723. doi: 10.1176/ajp.2006.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee P.H., Anttila V., Won H. Genomic relationships, novel loci, and pleiotropic mechanisms across eight psychiatric disorders. Cell. 2019;179:1469–1482. doi: 10.1016/j.cell.2019.11.020. e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars B., Collishaw S., Hammerton G., Rice F., Harold G.T., Smith D., Bevan Jones R., Sellers R., Potter R., Craddock N., Thapar A.K., Heron J., Thapar A. Longitudinal symptom course in adults with recurrent depression: impact on impairment and risk of psychopathology in offspring. J. Affect. Disord. 2015;182:32–38. doi: 10.1016/j.jad.2015.04.018. [DOI] [PubMed] [Google Scholar]
- Mars B., Collishaw S., Smith D., Thapar Ajay, Potter R., Sellers R., Harold G.T., Craddock N., Rice F., Thapar Anita. Offspring of parents with recurrent depression: which features of parent depression index risk for offspring psychopathology? J. Affect. Disord. 2012;136:44–53. doi: 10.1016/j.jad.2011.09.002. [DOI] [PubMed] [Google Scholar]
- Martin J., Taylor M.J., Rydell M., Riglin L., Eyre O., Lu Y., Lundstrom S., Larsson H., Thapar A., Lichtenstein P. Sex-specific manifestation of genetic risk for attention deficit hyperactivity disorder in the general population. J. Child Psychol. Psychiatry. 2018;59:908–916. doi: 10.1111/jcpp.12874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntosh D., Kutcher S., Binder C., Levitt A., Fallu A., Rosenbluth M. Adult ADHD and comorbid depression: a consensus-derived diagnostic algorithm for ADHD. Neuropsychiatr. Dis. Treat. 2009;5:137–150. doi: 10.2147/ndt.s4720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musliner K.L., Mortensen P.B., McGrath J.J., Suppli N.P., Hougaard D.M., Bybjerg-Grauholm J., Bækvad-Hansen M., Andreassen O., Pedersen C.B., Pedersen M.G., Mors O., Nordentoft M., Børglum A.D., Werge T., Agerbo E., Consortium, for the B.D.W.G. of the P.G. Association of polygenic liabilities for major depression, bipolar disorder, and schizophrenia with risk for depression in the Danish population. JAMA Psychiatry. 2019;76:516–525. doi: 10.1001/jamapsychiatry.2018.4166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE), 2009. Depression in adults: recognition and management, NICE clinical guideline. doi: 10.1211/CP.2017.20202439. [DOI] [PubMed]
- Power R.A., Tansey K.E., Buttenschøn H.N., Cohen-Woods S., Bigdeli T., Hall L.S., Kutalik Z., Lee S.H., Ripke S., Steinberg S., Teumer A., Viktorin A., Wray N.R., Arolt V., Baune B.T., Boomsma D.I., Børglum A.D., Byrne E.M., Castelao E., Craddock N., Craig I.W., Dannlowski U., Deary I.J., Degenhardt F., Forstner A.J., Gordon S.D., Grabe H.J., Grove J., Hamilton S.P., Hayward C., Heath A.C., Hocking L.J., Homuth G., Hottenga J.J., Kloiber S., Krogh J., Landén M., Lang M., Levinson D.F., Lichtenstein P., Lucae S., MacIntyre D.J., Madden P., Magnusson P.K.E., Martin N.G., McIntosh A.M., Middeldorp C.M., Milaneschi Y., Montgomery G.W., Mors O., Müller-Myhsok B., Nyholt D.R., Oskarsson H., Owen M.J., Padmanabhan S., Penninx B.W.J.H., Pergadia M.L., Porteous D.J., Potash J.B., Preisig M., Rivera M., Shi J., Shyn S.I., Sigurdsson E., Smit J.H., Smith B.H., Stefansson H., Stefansson K., Strohmaier J., Sullivan P.F., Thomson P., Thorgeirsson T.E., Van der Auwera S., Weissman M.M., Breen G., Lewis C.M. Genome-wide association for major depression through age at onset stratification: major depressive disorder working group of the psychiatric genomics consortium. Biol. Psychiatry. 2017;81:325–335. doi: 10.1016/j.biopsych.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice F., Riglin L., Thapar A.K., Heron J., Anney R., O'Donovan M.C., Thapar A. Characterizing developmental trajectories and the role of neuropsychiatric genetic risk variants in early-onset depression. JAMA Psychiatry. 2019;76:306–313. doi: 10.1001/jamapsychiatry.2018.3338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riglin L., Collishaw S., Thapar A.K., Dalsgaard S., Langley K., Smith G.D., Stergiakouli E., Maughan B., O'Donovan M.C., Thapar A. Association of genetic risk variants with attention-deficit/hyperactivity disorder trajectories in the general population. JAMA Psychiatry. 2016;73:1285–1292. doi: 10.1001/jamapsychiatry.2016.2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riglin L., Leppert B., Dardani C., Thapar A.K., Rice F., O’Donovan M.C., Davey Smith G., Stergiakouli E., Tilling K., Thapar A. ADHD and depression: investigating a causal explanation. Psychol. Med. 2020:1–8. doi: 10.1017/S0033291720000665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seaman S.R., White I.R. Review of inverse probability weighting for dealing with missing data. Stat. Methods Med. Res. 2013;22:278–295. doi: 10.1177/0962280210395740. [DOI] [PubMed] [Google Scholar]
- Silverstein M.J., Faraone S.V, Alperin S., Leon T.L., Biederman J., Spencer T.J., Adler L.A. Validation of the expanded versions of the adult ADHD self-report scale v1.1 symptom checklist and the adult ADHD investigator symptom rating scale. J. Atten. Disord. 2018;23:1101–1110. doi: 10.1177/1087054718756198. [DOI] [PubMed] [Google Scholar]
- Simon V., Czobor P., Bálint S., Mészáros Á., Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br. J. Psychiatry. 2009;194:204–211. doi: 10.1192/bjp.bp.107.048827. [DOI] [PubMed] [Google Scholar]
- Spencer T.J., Adler L.A., Qiao M., Saylor K.E., Brown T.E., Holdnack J.A., Schuh K.J., Trzepacz P.T., Kelsey D.K. Validation of the adult ADHD investigator symptom rating scale (AISRS) J. Atten. Disord. 2009;14:57–68. doi: 10.1177/1087054709347435. [DOI] [PubMed] [Google Scholar]
- Stringaris A., Goodman R., Ferdinando S., Razdan V., Muhrer E., Leibenluft E., Brotman M.A. The affective reactivity index: a concise irritability scale for clinical and research settings. J. Child Psychol. Psychiatry. 2012;53:1109–1117. doi: 10.1111/j.1469-7610.2012.02561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strober M., Green J., Carlson G. Utility of the Beck Depression Inventory with psychiatrically hospitalized adolescents. J. Consult. Clin. Psychol. 1981 doi: 10.1037/0022-006X.49.3.482. [DOI] [PubMed] [Google Scholar]
- Thapar A., Riglin L. The importance of a developmental perspective in psychiatry: what do recent genetic-epidemiological findings show? Mol. Psychiatry. 2020;25:1631–1639. doi: 10.1038/s41380-020-0648-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os J., Jones P., Lewis G., Wadsworth M., Murray R. Developmental precursors of affective illness in a general population birth cohort. Arch. Gen. Psychiatry. 1997;54:625–631. doi: 10.1001/archpsyc.1997.01830190049005. [DOI] [PubMed] [Google Scholar]
- Weissman M.M., Merikangas K.R., Priya W., Kidd K.K., Prusoff B.A., Leckman J.F., Pauls D.L. Understanding the clinical heterogeneity of major depression using family data. Arch. Gen. Psychiatry. 1986;43:430–434. doi: 10.1001/archpsyc.1986.01800050028003. [DOI] [PubMed] [Google Scholar]
- Wing J.K., Babor T., Brugha T., Burke J., Cooper J.E., Giel R., Jablenski A., Regier D., Sartorius N. SCAN. Schedules for clinical assessment in neuropsychiatry. Arch. Gen. Psychiatry. 1990;47:589–593. doi: 10.1001/archpsyc.1990.01810180089012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on reasonable request from the corresponding author, Victoria Powell. The data are not publicly available due to their containing information that could compromise the privacy of research participants.