Abstract
Background
In this study, we examined the relationship between low levels of physical activity, high consumption of sugar-sweetened beverages and low consumption of whole grain bread and experiencing insomnia in adolescence and psychological distress in young adults.
Methods
This prospective study was based on information retrieved from the Trøndelag Health Study (HUNT) in Norway and included adolescents (age 13–19) participating in Young-HUNT3 (2006–2008) and in HUNT4 (2017–2019) 11 years later (age 23–31). The study sample consisted of 2,230 participants (1,287 females and 943 males). The exposure variables collected in adolescence included self-reported physical activity, consumption of sugar-sweetened beverages and whole grain bread and insomnia, and psychological distress in young adulthood was used as an outcome variable. The relationship between lifestyle behaviours in adolescence and psychological distress in young adulthood was examined using multivariable logistic regression, adjusted for gender, age and psychological distress in adolescence and educational level in young adulthood.
Results
An increased odds of psychological distress was shown among young adults who reported low levels of physical activity (OR: 1.44, 95 % CI: 1.10–2.89), high consumption of sugar-sweetened beverages (OR: 1.49, 95 % CI: 1.12–1.98), low consumption of whole grain bread (OR: 1.35, 95 % CI: 1.04–1.77) and insomnia (OR: 1.69, 95 % CI: 1.23–2.33) in adolescence. In terms of absolute differences, unhealthy lifestyle behaviours increased the risk of psychological distress in young adulthood between 3.18 (95 % CI: 0.29–6.07) (low whole grain bread consumption) and 6.01 (95 % CI: 1.95–10.07) (insomnia) percentage points.
Conclusions
Low levels of physical activity, high consumption of sugar-sweetened beverages and low consumption of whole grain bread and insomnia during adolescence were associated with psychological distress in young adulthood.
Keywords: Lifestyle behaviours, Physical activity, Sugar-sweetened beverages, Whole grain bread, Insomnia, Psychological distress, Prospective data, The HUNT study
Background
The prevalence of mental disorders has been associated with increased rates of mortality [1] and disability-adjusted life years [2]. Common mental disorders, such as depressive disorders and anxiety disorders, are highly prevalent among young adults in their 20 s, and those suffering from a mental disorder in their 20 s have an increased risk of experiencing a mental disorder later in life [3]. The first onset of mental health disorders appears to start in childhood or adolescence and may persist throughout life [4]. Thus, from a public health perspective, it is crucial to identify any modifiable factors preceding the development of mental health problems in adulthood.
Healthy lifestyle behaviours have been associated with improved psychological well-being, lower psychological distress and fewer mental health difficulties [5, 6], and the importance of focusing on lifestyle factors in the prevention and treatment of mental illness have been highlighted in a recent meta-review [7]. Moreover, a recent population-based prospective study among Canadian children and adolescents confirmed that adherence to lifestyle recommendations developed to promote physical health in children and prevent chronic diseases later in life also had short-term benefits for mental health and may reduce the future burden of mental illness [8]. A study among French adults also showed that increasing the number of healthy lifestyle behaviours was associated with a lower risk of depressive symptoms [9]. However, most previous studies examining the association between lifestyle behaviours and psychological distress have been cross-sectional, and few studies have examined the longitudinal relationship between adolescence and young adulthood.
Lifestyle behaviours include a broad range of behaviours, and to identify the potentially potent areas for preventing psychological distress, it may be useful to focus on the everyday lifestyle practices and choices that most adolescents face, such as physical activity, dietary patterns and sleep. The results from a longitudinal study and meta-analysis of prospective studies indicated that physical activity may have a preventive effect on the development of depression [10, 11]. Another prospective cohort study reported that low levels of physical activity in adolescents were associated with poor mental health in early adulthood among females but not for males [12]. On the other hand, the results from other prospective studies did not find longitudinal associations between physical activity and the symptoms of depression and anxiety [13, 14], while other prospective studies reported an inverse association between sport participation and symptoms of depression and anxiety [15, 16]. The inconsistency in these findings calls for further longitudinal studies.
Evidence has also confirmed the importance of the relationship between dietary patterns or quality and mental health early in the lifespan [17]. Several prospective studies and a recent meta-analysis concluded that the consumption of soft drinks is a major risk factor for developing depression among adults [18–21], and similar findings were shown among Norwegian adolescents [22]. Another longitudinal study showed that reducing adolescents’ intake of soft drinks resulted in reduced aggressive behaviour but no changes in depressive symptoms [23]. No significant association between sugar-sweetened beverage consumption and depression risk was found in a prospective cohort study (10-year follow-up) among Spanish students, but the results indicated that the consumption of sugar and overall low carbohydrate quality was associated with an increased risk of depression [21]. A recent review has also reported that diets rich in omega-3-polyunsaturated fatty acids and dietary fibre may reduce the risk of developing the symptoms of depression and anxiety [24]. A cross-sectional study among adults revealed an inverse association between the consumption of whole grains and depression scores [25]. To the best of our knowledge, it remains unknown what the unique preventive potential of dietary fibre and soft drink consumption during adolescence might be for reducing the risk of psychological distress later in young adulthood.
In addition, several studies have indicated that total sleep time and sleep quality in adolescence seem to predict psychological distress [26, 27], depression and anxiety [28–30] and that sleep problems frequently co-occur with anxiety and depression [26]. Moreover, a recent longitudinal study among youth showed that adherence to sleep recommendations was the most consistent predictor of depressive symptoms [31]. However, a recent cross-sectional study among 60 adolescents found no significant relationship between sleep duration and psychological distress [27]. Because of inconclusive findings, a recent study emphasised the importance of future research examining the relationship between sleep habits in adolescence and anxiety and depression later in life [26].
Both low socioeconomic status (SES) and mental health difficulties in childhood have also been associated with poor lifestyle beahviour [32, 33], as well as mental health problems [33–35]; therefore, mental health difficulties in adolescence and SES should be taken into account when examining the relationship between different lifestyle behaviours and mental health.
The evidence for which lifestyle behaviours in adolescence should be addressed when aiming to prevent the onset of psychological distress is currently limited and inconsistent. To the best of our knowledge, few studies have assessed the relative influence of multiple modifiable lifestyle behaviours in adolescence on psychological distress in young adulthood. Thus, the purpose of the current study was to examine the relationship between low levels of physical activity, high consumption of sugar-sweetened beverages and low consumption of whole grain bread and insomnia in adolescence and psychological distress in young adulthood.
Methods
The present prospective study was a part of the Trøndelag Health Study (HUNT). Data collection for the first measurements, which covered the adolescent part, was conducted in 2006–2008 (Young-HUNT3), whereas the second wave of the HUNT study, which covered the adult part, was conducted in 2017–2019 (HUNT4). All adolescents aged 13–19 years living in the county of Trøndelag in Norway were invited to participate in the Young-HUNT3 study by completing a self-reported questionnaire during school hours. In 2017–2019, 11 years later, the same population (now aged 23–31) were invited to participate in a fourth wave of the adult part of the HUNT study (HUNT4) and completed this survey by filling out a comprehensive health-related questionnaire at home. Participation was voluntary, and the respondents were informed that they could withdraw from the studies at any time. The HUNT study is a collaboration between the HUNT Research Centre (Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology NTNU), Trøndelag County Council, Central Norway Regional Health Authority and the Norwegian Institute of Public Health.
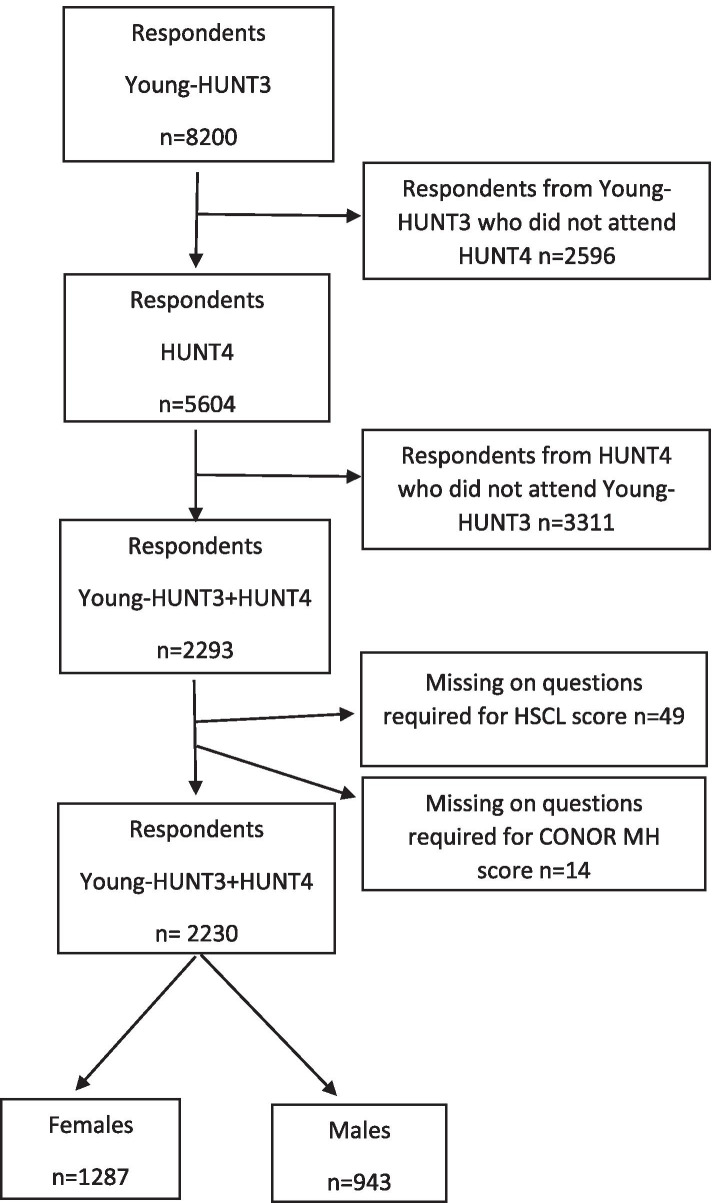
In the Young-HUNT3 study, 8,200 respondents agreed to participate (78.4 % of all invited) and in HUNT4, 56,078 respondents agreed to participate (54 % of all invited). In the present study, those participating in both Young-HUNT3 and HUNT4 were included, resulting in a total of 2,293 respondents (1,320 females and 973 males). Finally, after excluding those with missing information on any HSCL-5 items or CONOR MH items, the current study comprised 2,230 respondents(1,287 females and 943 males). The flowchart in Fig. 1 shows the population in 2004–2006 and 2017–2019.
Fig. 1.
Flowchart for the study population: Norwegian HUNT studies, Young-HUNT3 in 2006–2008 and HUNT4 in 2017–2019
Measures
Outcome variable—young adult psychological distress
In HUNT4, psychological distress was assessed by the Conor Mental Health Index (CONOR-MHI). This measurement consists of seven items reflecting the various aspects of psychological distress. The CONOR-MHI is a modified version of the General Health Questionnaire [36] and Hopkin’s Symptoms Checklist [37]. The respondents were asked if during the last two weeks they had felt ‘nervous and unsettled’, ‘troubled by anxiety’, ‘secure and calm’, ‘irritable’, ‘happy and optimistic’, ‘sad/depressed’ or ‘lonely’. Each question had four answer categories, ranging from ‘No’ (1) to ‘Very’ (4). The average CONOR-MHI score was calculated by dividing the total score by seven (number of items). Missing values were replaced with the sample mean value for each item. Records with two or more missing items were, however, excluded (see Fig. 1). In the present study, a cut-off point of ≥2.15 was used to determine psychological distress, which is considered a valid cut-off value for the prediction of psychological distress [38].
Exposure variables—lifestyle behaviours in adolescence
The respondents were asked the following: ‘Outside of school hours, how many hours do you usually exercise in your free time so much that you get out of breath or sweat?’ The response options were as follows: ‘Never’, ‘Approximately 30 min a week ‘Approximately 1–1 ½ hours a week’, ‘Approximately 2–3 hours a week’, ‘Approximately 4–6 hours a week’ or ‘7 hours and more per week’. A high level of physical activity was defined as ‘Four hours or more per week’ (reference category), and ‘Less than 4 hours’ was defined as a low level of physical activity.
The consumption of sugar-sweetened beverages was measured by the following: ‘How often do you drink the items listed below?’ The response alternatives were ‘Seldom/never’, ‘1–6 glasses a week’, ‘1 glass a day’, ‘2–3 glasses a day’ and ‘4 or more glasses a day’. Consumption of whole grain bread was measured by the following question: ‘How often do you eat the items listed below?’ The response alternatives were ‘Several times a day’, ‘Once a day’, ‘Every week but not every day’, ‘Less than once a week’ and ‘Never’. Consumption was dichotomised into ‘Daily consumption and more’ (reference category for whole grain) and ‘Less than daily consumption’ (reference category for sugar-sweetened soft drinks).
Classification of insomnia was based on two questions, as follows: ‘Have you had problems falling asleep during the last month?’ and ‘During the last month, did you ever wake up too early, not being able to fall asleep again?’ The following response options were given: ‘Almost every night’, ‘Often’, ‘Occasionally’ and ‘Never’. The respondents were classified with insomnia if they answered ‘Often’ or ‘Almost every night’ on at least one of the questions and with no insomnia if they answered ‘Less than often’ (reference category) for both questions, which is in accordance with former research [39, 40].
Control variables
Age of the adolescents
The age of the respondents in YoungHUNT3 varied between 12.8 and 20.9 years and was dichotomised as ≤ 16 years and >16 years (reference category).
Highest education as young adults
Education was assessed by the following question (HUNT4): ‘What is your highest level of education?’ and divided into four categories: ‘Primary school’, ‘High school’, ‘College ≤4 years’ and ‘College >4 years’. Educational level as young adults was dichotomised into ‘No higher education’, including primary school and high school) and ‘Higher education’, including college ≤4 years and college >4 years (reference category).
Psychological distress in adolescence
In the YongHUNT3, psychological distress was assessed by the Hopkins Symptom Checklist-5 (HSCL-5), a five-item shortened version of the HSCL-25. HSCL-25 is a widely applied screening tool designed to measure the symptoms of depression and anxiety [41]. The HSCL-5 has been shown as a reliable and valid short form of the HSCL-25 and has been recommended as a screening instrument for symptoms of depression and anxiety [42, 43]. The respondents were asked if during the last 14 days they had been affected by the following: ‘constantly afraid and anxious; felt tense or uneasy; felt hopeless about the future; felt dejected or sad; worried too much about various things’. The five questions had four response alternatives, ranging from ‘Not bothered’ (1) to ‘Very much bothered’ (4). The responses were summarised across all items, and the mean score was used as a measure of psychological distress. In the present study, a cut-off point at >2.0 was used to determine psychological distress, which is considered a valid cut-off value for the prediction of psychological distress in adolescents [43]. We excluded the respondents with missing values on at least one of the HSCL-5 items (Fig. 1).
Analyses
Analyses were carried out using SPSS 25.0 and STATA 16.0 for Windows. Baseline characteristics and lifestyle behaviours stratified by gender were presented as proportions with a 95 % confidence interval (CI) in each stratum.
Binominal logistic regression analyses were used to explore the association between low levels of physical activity, high consumption of sugar-sweetened beverages and low consumption of whole grain bread and experiencing insomnia during adolescent and psychological distress in young adults. All four models were adjusted for gender, age, psychological distress in adolescence and highest education in young adulthood. The associations were presented as odds ratios (OR) with a 95 % CI. Furthermore, logistic regression models were used to estimate the absolute risk differences at the follow-up 11 years later with the covariates as their mean. A risk difference describes how a 1-unit change in an independent variable (e.g., physical activity or not) alters the absolute risk of a current outcome (psychological distress). The risk difference focuses on the absolute effect of the risk factor (e.g., low level of physical activity) on the excess risk of disease (e.g., psychological distress) in those who have a risk factor compared with those who do not. From a public health point of view, this information might be more informative than a relative estimate like the OR, which examines the strength of an association.
An interaction analysis was used to examine the influence of gender on the strength of the relationship between physical activity and psychological distress. The possible interaction effects were examined using LR tests (likelihood ratio test) by contrasting models with and without interaction terms. The main effect model included physical activity, gender age, psychological distress and highest education as the independent variables and was tested against models, here also including interactions between physical activity by gender. A parallel interaction analysis was carried out for sugar-sweetened beverages, whole grain bread and insomnia. The incremental change in the log likelihood between the main effect models and the four models, including interactions, was not significant. Thus, the fit was not improved with the other interaction models. Therefore, only the main effect model has been presented in the results.
Results
Table 1 presents the differences in psychological distress between males and females in young adulthood with unhealthy lifestyle behaviours during adolescence and background characteristics.
Table 1.
Psychological distress in young adulthood among males and females with unhealthy lifestyle behaviors during adolescence and background charactertics
| Variables | Males (n = 943) | Females (n = 1287) |
|---|---|---|
| High level of psychological distress (n = 90 ) % (95% CI) |
High level of psychological distress (n = 182) % (95% CI) | |
| Young-HUNT3 2006-2008 | ||
| Lifestylehabits | ||
| Physical activity | ||
| < 4 hours per week after school | 10.2 (7.3-13.0) | 17.7 (14.9-20.6) |
| Sugar-sweetened beverages | ||
| Daily consumption | 11.3 (8.1-14.4) | 19.2 (14.4-23.9) |
| Whole grain bread | ||
| Less than daily consumption | 12.4 (8.7-16.2) | 17.5 (13.9-21.0) |
| Sleeping | ||
| Insomnia | 8.0 (6.1-10.0) | 12.4 (10.3-14.4) |
| Psychological distress (HSCL-5) | ||
| High level (>2.0) | 22.0 (11.5-32.6) | 25.2 (19.7-30.7) |
| Age | ||
| ≤ 16 | 12.2 (9.5-15.0) | 15.3 (12.6-17.9) |
| HUNT4 2017-2019 | ||
| Education level as young adults | ||
| No higher education | 11.2 (8.7-13.7) | 18.1 (14.8-21.5) |
The dependent variable consistent of two categories coded as low level of psychological distress (CONOR MHI < 2.15) in young adults (HUNT4 2017-2019) and high level of psychological distress (CONOR MHI ≥2.15)
The results in Table 1 show that among adolescents with a low level of physical activity, high consumption of sugar-sweetened beverages, low consumption of wholegrain bread and insomnia, a higher proportion of females than males reported a high level of psychological distress in young adulthood (17.7 % vs. 10.2 %, 19.2 % vs. 11.3 %, 17.5 % vs. 12.4 % and 12.4 % vs. 8.0 %, respectively). Similarly, among adolescents with high level of psychological distress, a higher proportion of females than males reported a high level of psychological distress in young adulthood (25.2 % vs. 22.0 %, respectively). Further, among young adults with a low level of higher education, a higher proportion of females than males reported psychological distress (18.1 % vs. 11.2 %, respectively).
In Table 2, the regression analysis for each lifestyle behaviour in adolescence shows the OR and risk differences of psychological distress in adulthood.
Table 2.
Odds ratio and absolute risk differencesa of psychological distress in adulthood in relation to lifestyle behaviours in adolescence
| Crude modela | Adjusted modela | Crude model | Adjusted model | |
|---|---|---|---|---|
| Variables | OR | OR | Risk differencesa | Risk differences |
| Physical activity | ||||
| ≥ 4 hours per week after school | 1 (ref) | 1 (ref) | ||
| < 4 hours per week after school | 1.63 (1.25–2.11) | 1.44 (1.10–1.89) | 5.09 (2.41–7.77) | 3.68 (0.95–6.42) |
| Sugar-sweetened beverages | ||||
| Less than daily consumption | 1 (ref) | 1 (ref) | ||
| Daily consumption | 1.34 (1.03–1.75) | 1.49 (1.12–1.98) | 3.25 (0.16–6.35) | 4.30 (1.07–7.52) |
| Whole grain bread | ||||
| Daily consumption | 1 (ref) | 1 (ref) | ||
| Less than daily consumption | 1.57 (1.21–2.04) | 1.35 (1.04–1.77) | 5.00 (1.98–8.02) | 3.18 (0.29–6.07) |
| Insomnia | ||||
| No insomnia | 1 (ref) | 1 (ref) | ||
| Insomnia | 2.30 (1.72–3.08) | 1.69 (1.23–2.33) | 10.62 (6.25–14.99) | 6.01 (1.95–10.07) |
Crude: Bivariate analysis. OR: odds ratio; 95% CI. Adjusted; Adjusted for gender, age, psychological distress in adolescence and highest education as young adults from the main effects model. aEstimated risk differences (percentage points, with 95% CI) for psychological distress for each lifestyle behavior with the covariates as their mean
A higher odds of psychological distress was observed among those with a low level of physical activity (OR: 1.44, 95 % CI: 1.10–1.89), high consumption of sugar-sweetened beverages (OR: 1.49, 95 % CI: 1.12–1.98), low consumption of whole grain bread (OR: 1.35, 95 % CI: 1.04–1.77) and insomnia (OR: 1.69, 95 % CI: 1.23–2.33) compared with those with more healthy physical activity, dietary and sleeping behaviours. In terms of absolute differences, unhealthy lifestyle habits increased the risk of psychological distress in young adulthood between 3.18 (95 % CI: 0.29–6.07) (less whole grain bread) and 6.01 (95 % CI: 1.95–10.07) (insomnia) percentage points.
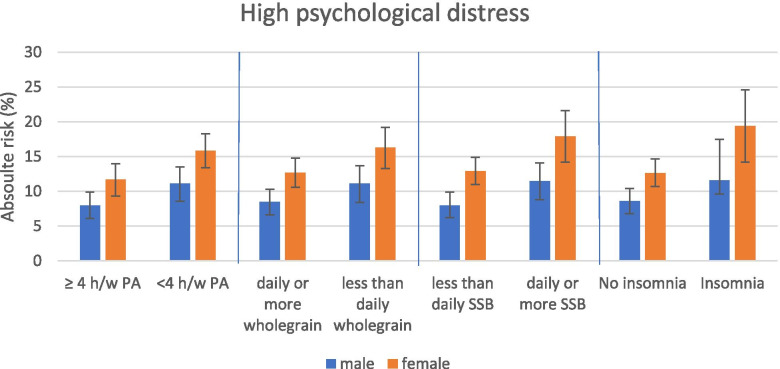
The increase in the risk differences of psychological distress according to the different lifestyle behaviours and genders are shown in Fig. 2. For both genders, the risk differences for the development of psychological distress in young adulthood was statistically significant for all examined lifestyle behaviours.
Fig. 2.
Estimated 11-year risk of psychological distress among young adults according to lifestyle behaviours in adolescence and gender. SSB: sugar-sweetened beverages
Discussion
Our main findings indicate that unhealthy lifestyle behaviours, including low levels of physical activity, high consumption of sugar-sweetened beverages, low consumption of whole grain bread and insomnia in adolescence, increase the risk of psychological distress in young adulthood by 3 to 6 % points. Our results may not be directly comparable to the results from previous studies because of differences in population, study design and measures of lifestyle behaviours and psychological distress. However, some similarities and differences can be seen. A prospective study among adolescents found that adherence to lifestyle recommendations for physical activity, sedentary behaviour, diet and sleep had short-term benefits for mental health problems [8].
In general, women reported more psychological distress in young adulthood than men. Additionally, for all examined lifestyle behaviours, we observed an additive effect of unhealthy lifestyle for both genders. A low level of physical activity in adolescence is associated with an increased risk of psychological distress in young adulthood. The results from another study showed that a low level of physical activity in adolescence (14 and 15 years of age) was associated with poor mental health seven years later in females but not males [12]. Another study among Dutch adolescents did not find evidence indicating that physical activity may have protective effects on depressive symptoms, regardless of gender [44]. The inconsistency in these findings may be because of variations in the follow-up period and differences in age at the follow-up.
The current study showed that the high consumption of sugar-sweetened soft drinks in adolescence was associated with more psychological distress for both genders in adulthood. This is in line with prospective studies showing that the high consumption of sugar-sweetened beverages is related to mental health problems in adolescence [45] and depressive symptoms in adulthood [19, 21, 46]. However, the present study revealed that on average, women with daily or high consumption of sugar-sweetened beverages have a 5.0 % points higher risk of psychological distress in young adulthood than men. A study among children and adolescents did not find longitudinal effects of soft drink consumption on mental health problems but revealed that the prevalence of mental health problems predicted soft drink consumption over an average of six years [47]. Additionally, higher exposure to added sugars and poor quality of carbohydrates (measured by an overall carbohydrate quality index) were associated with a higher risk of depression in a prospective cohort study; however, no significant association between the consumption of sugar-sweetened beverages and depression risk was found [21]. High consumption of soft drinks has been suggested as a dysfunctional method of emotion-focused coping with mental health problems [47]. A possible biological mechanism for the association between sugar-sweetened beverages and psychological distress might be related to the chronic systemic inflammation induced by sugar [48, 49]. The mechanisms by which a proinflammatory diet could increase the risk of psychological distress may be through proinflammatory nutrients activating the innate immune system, which can lead to low-grade inflammation and mental health disorders [50].
The present study also showed that the high consumption of whole grain bread in adolescence was associated with decreased risk of psychological distress in young adulthood for both genders. To the best of our knowledge, few longitudinal studies have examined the relationship between whole grain bread consumption in adolescence and psychological distress in adulthood. In the Young-HUNT cohort, low whole grain bread consumption in adolescence was associated with a high risk of psychological distress 11 years later. A longitudinal study among adults found that the high consumption of nonrefined grain was significantly related to lower depression and anxiety [51]. Also, for whole grain bread consumption, we observed an additive effect of gender and unhealthy behaviour. The gender-stratified analyses in the present study also revealed that females with low consumption of whole grain bread had a 3.6 % points higher risk for psychological distress than men. Similarly, another prospective study among women found that the consumption of whole grain foods was inversely associated with depression in women [52]. Whole grain bread is an important source of nutrients, together contributing with other whole grain products to approximately 50 % of the fibre intake in the Norwegian population [53]. A recent meta-analysis found that increased intake of dietary fibre was associated with a lower risk of depression in adults [54]. Similarly, a cross-sectional study among Spanish children showed an association between the increased intake of fibre and lower levels of depressive symptoms [55]. The mechanism linking psychological distress to dietary fibre is unclear, but a recent review suggested that dietary fibre lowers inflammation by modifying both the permeability of the gut and pH level, and a reduction in inflammatory compounds may alter neurotransmitter concentration to reduce depressive symptoms [56]. Additionally, whole grain bread contains fatty acids, which have been linked to an increased risk of depressive symptoms, but they also contain zink, folic acid and B6, which may be inversely associated with depression have been shown to have a protective effect against and mental health symptoms in different populations [57, 58].
Finally, the present study revealed an association between insomnia and a higher prevalence of psychological distress for both genders, which is in line with previous studies [27, 29]. Moreover, one study by F. Orchard, et al. [26] confirmed that sleep quality and total sleep time at age 15 predicted anxiety and depression symptoms (and diagnoses) at ages 17, 21 and 24. Prospective studies and a review of prospective studies have also shown that not getting an adequate amount of sleep was associated with symptoms of depression, DSM-IV major depression [28, 31, 59] and anxiety symptoms [30]. Sleep problems frequently co-occur with anxiety and depression and are common in adolescents [26]. A prospective study examining the association between sleep deprivation and symptoms of depression and major depression found reciprocal effects for major depression and sleep deprivation but not for depressive symptoms [59]. Short sleep duration and insomnia seem to be not simply symptoms of physical or mental illness, but also more predictive of chronic mental health symptoms [60]. Gender differences were also identified in the present study: females with insomnia problems had a 6.7 % points higher risk for psychological distress than men with insomnia problems. Studies examining the mechanisms linking sleep and psychological distress are scarce. A review by Blake et al. [61] concluded that biological, psychological and social mechanisms underlie insomnia and internalising symptoms (anxiety and depression) in adolescence.
Strengths and limitations
A strength of the current study is the longitudinal design, which is based on a large, representative population of Norwegian adolescents. The long follow-up period (11 years) made it possible to prospectively examine the association between physical activity, consumption of whole grain bread and sugar-sweetened beverages and insomnia in adolescence and psychological distress in young adulthood. This is a strength compared with previous studies, which have generally been restricted to the adolescent or adult period and have short follow-up periods.
Furthermore, the analyses were adjusted for well-known confounders such as gender, age, psychological distress in adolescence and a higher educational level in adulthood. However, we cannot exclude the possible residual confounders attributable to unknown or unmeasured factors; for example, when assessing the longitudinal associations of diet and beverage consumption during a week in adolescence, diet may also be a confounder. The measures are based solely on self-reports, which can be prone to recall bias, especially concerning items measuring lifestyle behaviours. For example, participants tend to over-report physical activity in self-report measures when compared with objectively measured activity [62]. There is the potential for selection bias because the participants must have attended both HUNTH3 and HUNT4 to be included. Previous analyses have shown that those not participating in HUNT studies have lower education and worse health [63]. A comparison of educational level between the subpopulation included in our study with the total HUNT4 population revealed a further selection of individuals with higher educational levels (50 % vs., 39 %, respectively) [64]. Information on physical activity, consumption of whole grain bread and sugar-sweetened beverages and insomnia was not updated throughout the follow-up period. Additionally, the interpretation of whole grain bread by the participants may not always be correct because of the use of malt and sirup (‘colouring’) to provide more moisture and increase the shelf life of the bread. A brown bread can be defined by the participants as ‘whole grain bread’, but in reality, it may not be.
Conclusions
Insomnia at ages 13–19 seems to predict psychological distress 11 years later. The same patterns were observed for low physical activity, low consumption of whole grain bread and high consumption of sugar-sweetened beverages. On average, the risk of psychological distress is increased for both genders in the case of unhealthy behaviour. This knowledge is important to develop generic prevention approaches to reduce mental health problems and strengthen mental health in adolescence and in adults.
Acknowledgements
The Trøndelag Health Study is a collaboration between the HUNT Research Centre (Faculty of Medicine and Health Sciences, Norwegian University of Technology NTNU), Trøndelag County Council, Central Norway Regional Health Authority and the Norwegian Institute of Public Health. We are also grateful to all the participating adolescents. Additionally, thank you Curt Hagquist for your input regarding the presentation of the results.
Abbreviations
- HSCL-5
Hopkins Symptoms Checklist-5
- CONOR-MHI
Conor mental health index
- OR
Odds ratio
- HUNT
Trøndelag Health Study
- CI
Confidence interval
- SES
Socioeconomic status
- SSB
Sugar-sweetened beverages
Authors' contributions
THS developed the project. All the authors participated in the study’s design and provided a critical review and editing of the manuscript. ALK and THS drafted the manuscript. ALK conducted the statistical analysis and data interpretation. KR participated in the statistical analysis. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Availability of data and materials
The HUNT Research Centre has permission from the Norwegian Data Inspectorate to store and handle these data. To protect the participants’ privacy, the HUNT Research Centre aimed to limit storage of data outside the HUNT databank and cannot deposit data in open repositories. The HUNT databank has precise information on all data exported to different projects and can reproduce these on request. There are no restrictions regarding data export given approval of applications to HUNT Research Centre. For more information, see http://www.ntnu.edu/hunt/data.
Declarations
Ethics approval and consent to participate
The HUNT studies were approved by the Data Inspectorate of Norway and by the Regional Committee for Medical Research Ethics (reference 101672), and all information from the HUNT was treated according to the guidelines of the Data Inspectorate. Participation was based on informed consent from participants aged 16 years or older. In accordance with Norwegian law, the parents of those younger than 16 years consented on behalf of their child.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334–41. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. 2019;21:10. doi: 10.1007/s11920-019-0997-0. [DOI] [PubMed] [Google Scholar]
- 3.Gustavson K, Knudsen AK, Nesvåg R, Knudsen GP, Vollset SE, Reichborn-Kjennerud T. Prevalence and stability of mental disorders among young adults: Findings from a longitudinal study. BMC Psychiatry. 2018;18:65. doi: 10.1186/s12888-018-1647-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorders: A review of recent literature. Current Opinion in Psychiatry. 2007;20:359. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Velten J, Bieda A, Scholten S, Wannemüller A, Margraf J. Lifestyle choices and mental health: A longitudinal survey with german and chinese students. BMC Public Health. 2018;18:632. doi: 10.1186/s12889-018-5526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Velten J, Lavallee KL, Scholten S, Meyer AH, Zhang X-C, Schneider S, et al. Lifestyle choices and mental health: A representative population survey. BMC Psychology. 2014;2:58. doi: 10.1186/s40359-014-0055-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Firth J, et al. A meta-review of ‘lifestyle psychiatry’: The role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry. 2020;19:360–80. doi: 10.1002/wps.20773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loewen OK, Maximova K, Ekwaru JP, Faught EL, Asbridge M, Ohinmaa A, et al. Lifestyle behavior and mental health in early adolescence. Pediatrics. 2019;143:e20183307. doi: 10.1542/peds.2018-3307. [DOI] [PubMed] [Google Scholar]
- 9.Adjibade M, Lemogne C, Julia C, Hercberg S, Galan P, Assmann KE, et al. Prospective association between combined healthy lifestyles and risk of depressive symptoms in the French nutrinet-santé cohort. J Affect Disord. 2018;238:554–62. doi: 10.1016/j.jad.2018.05.038. [DOI] [PubMed] [Google Scholar]
- 10.McPhie ML, Rawana JS. The effect of physical activity on depression in adolescence and emerging adulthood: A growth-curve analysis. J Adolesc. 2015;40:83–92. doi: 10.1016/j.adolescence.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 11.Schuch FB, et al. Physical activity and incident depression: A meta-analysis of prospective cohort studies. Am J Psychiatry. 2018;175:631–48. doi: 10.1176/appi.ajp.2018.17111194. [DOI] [PubMed] [Google Scholar]
- 12.Poulsen PH, Biering K, Andersen JH. The association between leisure time physical activity in adolescence and poor mental health in early adulthood: A prospective cohort study. BMC Public Health. 2016;16:3. doi: 10.1186/s12889-015-2658-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Toseeb U, Brage S, Corder K, Dunn VJ, Jones PB, Owens M, et al. Exercise and depressive symptoms in adolescents: A longitudinal cohort study. JAMA Pediatrics 2014;168:1093-1100. doi:10.1001/jamapediatrics. 2014.1794. [DOI] [PubMed]
- 14.Gunnell KE, Flament MF, Buchholz A, Henderson KA, Obeid N, Schubert N, et al. Examining the bidirectional relationship between physical activity, screen time, and symptoms of anxiety and depression over time during adolescence. Prev Med. 2016;88:147–52. doi: 10.1016/j.ypmed.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 15.Jewett R, Sabiston CM, Brunet J, O’Loughlin EK, Scarapicchia T, O’Loughlin J. School sport participation during adolescence and mental health in early adulthood. J Adolesc Health. 2014;55:640–4. doi: 10.1016/j.jadohealth.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 16.Ashdown-Franks G, Sabiston CM, Solomon-Krakus S, O’Loughlin JL. Sport participation in high school and anxiety symptoms in young adulthood. Ment Health Phys Act. 2017;12:19–24. doi: 10.1016/j.mhpa.2016.12.001. [DOI] [Google Scholar]
- 17.O’Neil A, Quirk SE, Housden S, Brennan SL, Williams LJ, Pasco JA, et al. Relationship between diet and mental health in children and adolescents: A systematic review. Am J Public Health. 2014;104:e31–42. doi: 10.2105/AJPH.2014.302110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hu D, Cheng L, Jiang W. Sugar-sweetened beverages consumption and the risk of depression: A meta-analysis of observational studies. J Affect Disord. 2019;245:348–55. doi: 10.1016/j.jad.2018.11.015. [DOI] [PubMed] [Google Scholar]
- 19.Kang D, Kim Y, Je Y. Non-alcoholic beverage consumption and risk of depression: Epidemiological evidence from observational studies. Eur J Clin Nutr. 2018;72:1506–16. doi: 10.1038/s41430-018-0121-2. [DOI] [PubMed] [Google Scholar]
- 20.Guo X, Park Y, Freedman ND, Sinha R, Hollenbeck AR, Blair A, et al. Sweetened beverages, coffee, and tea and depression risk among older us adults. PLoS One. 2014;9:e94715. doi: 10.1371/journal.pone.0094715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sanchez-Villegas A, Zazpe I, Santiago S, Perez-Cornago A, Martinez-Gonzalez MA, Lahortiga-Ramos F. Added sugars and sugar-sweetened beverage consumption, dietary carbohydrate index and depression risk in the seguimiento universidad de navarra (sun) project. Br J Nutr. 2018;119:211–21. doi: 10.1017/S0007114517003361. [DOI] [PubMed] [Google Scholar]
- 22.Lien L, Lien N, Heyerdahl S, Thoresen M, Bjertness E. Consumption of soft drinks and hyperactivity, mental distress, and conduct problems among adolescents in oslo, norway. Am J Public Health. 2006;96:1815–20. doi: 10.2105/AJPH.2004.059477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mrug S, Jones LC, Elliott MN, Tortolero SR, Peskin MF, Schuster MA. Soft drink consumption and mental health in adolescents: A longitudinal examination. J Adolesc Health. 2020 doi: 10.1016/j.jadohealth.2020.05.034. [DOI] [PubMed] [Google Scholar]
- 24.Taylor AM, Holscher HD. A review of dietary and microbial connections to depression, anxiety, and stress. Nutr Neurosci. 2020;23:237–50. doi: 10.1080/1028415X.2018.1493808. [DOI] [PubMed] [Google Scholar]
- 25.Kim WK, Shin D, Song WO. Are dietary patterns associated with depression in U.S. adults? J Med Food. 2016;19:1074–84. doi: 10.1089/jmf.2016.0043. [DOI] [PubMed] [Google Scholar]
- 26.Orchard F, Gregory AM, Gradisar M, Reynolds S. Self-reported sleep patterns and quality amongst adolescents: Cross‐sectional and prospective associations with anxiety and depression. J Child Psychol Psychiatry. 2020;61:1126–37. doi: 10.1111/jcpp.13288. [DOI] [PubMed] [Google Scholar]
- 27.Jamieson D, Beaudequin DA, McLoughlin LT, Parker MJ, Lagopoulos J, Hermens DF. Associations between sleep quality and psychological distress in early adolescence. J Child Adolesc Ment Health. 2020;32:77–86. doi: 10.2989/17280583.2020.1811288. [DOI] [PubMed] [Google Scholar]
- 28.Cairns KE, Yap MBH, Pilkington PD, Jorm AF. Risk and protective factors for depression that adolescents can modify: A systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2014;169:61–75. doi: 10.1016/j.jad.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 29.Hertenstein E, et al. Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Med Rev. 2019;43:96–105. doi: 10.1016/j.smrv.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 30.Narmandakh A, Roest AM, de Jonge P, Oldehinkel AJ. The bidirectional association between sleep problems and anxiety symptoms in adolescents: A trails report. Sleep Med. 2020;67:39–46. doi: 10.1016/j.sleep.2019.10.018. [DOI] [PubMed] [Google Scholar]
- 31.Patte KA, Faulkner G, Qian W, Duncan M, Leatherdale ST. Are one-year changes in adherence to the 24-hour movement guidelines associated with depressive symptoms among youth? BMC Public Health. 2020;20:1–12. doi: 10.1186/s12889-020-08887-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fontes AS, Pallottini AC, Vieira DAdS, Fontanelli MdM, Marchioni DM, Cesar CLG, Alves MCGP, Goldbaum M, Fisberg RM. Demographic, socioeconomic and lifestyle factors associated with sugar-sweetened beverage intake: A population-based study. Revista Brasileira de Epidemiologia. 2020;23:e200003. doi: 10.1590/1980-549720200003. [DOI] [PubMed] [Google Scholar]
- 33.Debbia F, Rodríguez-Muñoz PM, Carmona-Torres JM, Hidalgo-Lopezosa P, Cobo-Cuenca AI, López-Soto PJ, et al. Association between physical activity, food consumption and depressive symptoms among young adults in spain: Findings of a national survey. Issues Ment Health Nurs. 2020;41:59–65. doi: 10.1080/01612840.2019.1672223. [DOI] [PubMed] [Google Scholar]
- 34.Veldman K, Reijneveld SA, Ortiz JA, Verhulst FC, Bültmann U. Mental health trajectories from childhood to young adulthood affect the educational and employment status of young adults: Results from the trails study. J Epidemiol Community Health. 2015;69:588–93. doi: 10.1136/jech-2014-204421. [DOI] [PubMed] [Google Scholar]
- 35.Mulraney M, Coghill D, Bishop C, Mehmed Y, Sciberras E, Sawyer M, et al. A systematic review of the persistence of childhood mental health problems into adulthood. Neurosci Biobehav Rev. 2021;129:182–205. doi: 10.1016/j.neubiorev.2021.07.030. [DOI] [PubMed] [Google Scholar]
- 36.Goldberg DP. The detection of psychiatric illness by questionnaire: A technique for the identification and assessment of non-psychotic illness. Oxford University Press; 1972.
- 37.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behav Sci. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 38.Søgaard AJ, Bjelland I, Tell GS, Røysamb E. A comparison of the conor mental health index to the HSCL-10 and HADS. Nor Epidemiol. 2003;13:279–84. [Google Scholar]
- 39.Neckelmann D, Mykletun A, Dahl AA. Chronic insomnia as a risk factor for developing anxiety and depression. Sleep. 2007;30:873–80. doi: 10.1093/sleep/30.7.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Strandheim A, Bjerkeset O, Gunnell D, Bjørnelv S, Holmen TL, Bentzen N. Risk factors for suicidal thoughts in adolescence-a prospective cohort study: The young-hunt study. BMJ Open. 2014;4. [DOI] [PMC free article] [PubMed]
- 41.Hesbacher PT, Rickels K, Morris R, Newman H, Rosenfeld H. Psychiatric illness in family practice. J Clin Psychiatry. 1980;41:6–10. [PubMed] [Google Scholar]
- 42.Schmalbach B, Zenger M, Tibubos AN, Kliem S, Petrowski K, Brähler E. Psychometric properties of two brief versions of the hopkins symptom checklist: HSCl-5 and HSCL-10. Assessment. 2019:1073191119860910. [DOI] [PubMed]
- 43.Strand B, Dalgard O, Tambs K, Rognerud M. Measuring the mental health status of the norwegian population: A comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (sf-36) Nord J Psychiatry. 2003;57:113–8. doi: 10.1080/08039480310000932. [DOI] [PubMed] [Google Scholar]
- 44.Stavrakakis N, Roest A, Verhulst F, Ormel J, De Jonge P, Oldehinkel A. Physical activity and onset of depression in adolescents: A prospective study in the general population cohort trails. J Psychiatr Res. 2013;47:1304–8. doi: 10.1016/j.jpsychires.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 45.Lien L, Sagatun Å, Heyerdahl S, Søgaard AJ, Bjertness E. Is the relationship between smoking and mental health influenced by other unhealthy lifestyle factors? Results from a 3-year follow-up study among adolescents in oslo, norway. J Adolesc Health. 2009;45:609–17. doi: 10.1016/j.jadohealth.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 46.Knüppel A, Shipley MJ, Llewellyn CH, Brunner EJ. Sugar intake from sweet food and beverages, common mental disorder and depression: Prospective findings from the whitehall ii study. Sci Rep. 2017;7:1–10. doi: 10.1038/s41598-017-05649-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kadel P, Schneider S, Mata J. Soft drink consumption and mental health problems: Longitudinal relations in children and adolescents. Soc Sci Med 2020:113123. [DOI] [PubMed]
- 48.Geng M, Jiang L, Wu X, Ding P, Liu W, Liu M, et al. Sugar-sweetened beverages consumption are associated with behavioral problems among preschoolers: A population based cross-sectional study in china. J Affect Disord. 2020;265:519–25. doi: 10.1016/j.jad.2020.01.076. [DOI] [PubMed] [Google Scholar]
- 49.Tolkien K, Bradburn S, Murgatroyd C. An anti-inflammatory diet as a potential intervention for depressive disorders: a systematic review and meta-analysis. Clin Nutr. 2019;38:2045–52. doi: 10.1016/j.clnu.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 50.Bosma-den Boer MM, van Wetten M-L, Pruimboom L. Chronic inflammatory diseases are stimulated by current lifestyle: How diet, stress levels and medication prevent our body from recovering. Nutr Metab (Lond) 2012;9:1–14. doi: 10.1186/1743-7075-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gibson-Smith D, Bot M, Brouwer IA, Visser M, Giltay EJ, Penninx B. Association of food groups with depression and anxiety disorders. Eur J Nutr. 2020;59:767–78. doi: 10.1007/s00394-019-01943-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gangwisch JE, Hale L, Garcia L, Malaspina D, Opler MG, Payne ME, et al. High glycemic index diet as a risk factor for depression: Analyses from the women’s health initiative. Am J Clin Nutr. 2015;102:454–63. doi: 10.3945/ajcn.114.103846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Helsedirektoratet.Utviklingen i norsk kosthold. 2020 https://www.helsedirektoratet.no/rapporter/utviklingen-i-norsk-kosthold.
- 54.Fatahi S, et al. Association of dietary fiber and depression symptom: A systematic review and meta-analysis of observational studies. Complement Ther Med. 2020:102621. [DOI] [PubMed]
- 55.Rubio-López N, Morales-Suárez-Varela M, Pico Y, Livianos-Aldana L, Llopis-González A. Nutrient intake and depression symptoms in spanish children: The aniva study. Int J Environ Res Public Health. 2016;13:352. doi: 10.3390/ijerph13030352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Swann OG, Kilpatrick M, Breslin M, Oddy WH. Dietary fiber and its associations with depression and inflammation. Nutr Rev. 2019;78:394–411. doi: 10.1093/nutrit/nuz072. [DOI] [PubMed] [Google Scholar]
- 57.Ljungberg T, Bondza E, Lethin C. Evidence of the importance of dietary habits regarding depressive symptoms and depression. Int J Environ Res Public Health. 2020;17:1616. doi: 10.3390/ijerph17051616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xu Y, Zeng L, Zou K, Shan S, Wang X, Xiong J, Zhao L, Zhang L, Cheng G. Role of dietary factors in the prevention and treatment for depression: An umbrella review of meta-analyses of prospective studies. Translational psychiatry. 2021;11:1–13. doi: 10.1038/s41398-020-01158-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Roberts RE, Duong HT. The prospective association between sleep deprivation and depression among adolescents. Sleep. 2014;37:239–44. doi: 10.5665/sleep.3388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Biddle DJ, Hermens DF, Lallukka T, Aji M, Glozier N. Insomnia symptoms and short sleep duration predict trajectory of mental health symptoms. Sleep Med. 2019;54:53–61. doi: 10.1016/j.sleep.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 61.Blake MJ, Trinder JA, Allen NB. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: Implications for behavioral sleep interventions. Clin Psychol Rev. 2018;63:25–40. doi: 10.1016/j.cpr.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 62.Steene-Johannessen J, Anderssen SA, Van der Ploeg HP, Hendriksen IJ, Donnelly AE, Brage S, et al. Are self-report measures able to define individuals as physically active or inactive? Med Sci Sports Exerc. 2015;48:235–44. doi: 10.1249/MSS.0000000000000760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Langhammer A, Krokstad S, Romundstad P, Heggland J, Holmen J. The HUNT study: Participation is associated with survival and depends on socioeconomic status, diseases and symptoms. BMC Med Res Methodol. 2012;12:143. doi: 10.1186/1471-2288-12-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.NTNU HUNT forskningssenter. Hunt databank. 2021 https://hunt-db.medisin.ntnu.no/hunt-db/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The HUNT Research Centre has permission from the Norwegian Data Inspectorate to store and handle these data. To protect the participants’ privacy, the HUNT Research Centre aimed to limit storage of data outside the HUNT databank and cannot deposit data in open repositories. The HUNT databank has precise information on all data exported to different projects and can reproduce these on request. There are no restrictions regarding data export given approval of applications to HUNT Research Centre. For more information, see http://www.ntnu.edu/hunt/data.