Abstract
Self-stigma is associated with poor clinical and functional outcomes in Serious Mental Illness (SMI). There has been no review of self-stigma frequency and correlates in different cultural and geographic areas and SMI. The objectives of the present study were: (1) to review the frequency, correlates, and consequences of self-stigma in individuals with SMI; (2) to compare self-stigma in different geographical areas and to review its potential association with cultural factors; (3) to evaluate the strengths and limitations of the current body of evidence to guide future research. A systematic electronic database search (PubMed, Web of Science, PsycINFO, Scopus, and Ovid SP Cumulative Index to Nursing and Allied Health Literature [CINAHL]) following PRISMA guidelines, was conducted on the frequency, correlates, and consequences of self-stigma in SMI. Out of 272 articles, 80 (29.4%) reported on the frequency of self-stigma (n = 25 458), 241 (88.6%) on cross-sectional correlates of self-stigma and 41 (15.0%) on the longitudinal correlates and consequences of self-stigma. On average, 31.3% of SMI patients reported high self-stigma. The highest frequency was in South-East Asia (39.7%) and the Middle East (39%). Sociodemographic and illness-related predictors yielded mixed results. Perceived and experienced stigma—including from mental health providers—predicted self-stigma, which supports the need to develop anti-stigma campaigns and recovery-oriented practices. Increased transition to psychosis and poor clinical and functional outcomes are both associated with self-stigma. Psychiatric rehabilitation and recovery-oriented early interventions could reduce self-stigma and should be better integrated into public policy.
Keywords: self-stigma, serious mental illness, prevalence, correlates, psychiatric rehabilitation
Introduction
For a long time, research on stigma in psychiatric disorders focused on public stigma, or the endorsement of negative beliefs and discriminating attitudes towards individuals by the general population. Over the last two decades, attention has shifted towards the effects of stigma on individuals with Serious Mental Illness (SMI). According to Link and Phelan,1 stigma involves “elements of labeling, stereotyping, separation, status loss, and discrimination” that “co-occur in a power situation that allows the components of stigma to unfold.” The effects of stigma on individuals include perceived, experienced, anticipated, and self-stigma. Perceived stigma is defined as one’s beliefs about the attitudes of the general public towards people with SMI.2 Experienced stigma refers to people with SMI’s experience of discrimination.3 Anticipated stigma—or the expectation that a person will be discriminated against because of their SMI—can occur even if the person has no previous experience of discrimination and contributes to social withdrawal and self-stigma.3 Self-stigma—or internalized stigma—describes the transformation process wherein a person’s previous social identity (defined by social roles such as son, brother, sister, friend, employee, or potential partner) is progressively replaced by a devalued and stigmatized view of oneself, known as “illness identity.” 4 Self-stigma occurs when a person moves beyond mere awareness of public stigma and actually agrees with it and applies it to themself.2 Stigma resistance is defined as a person’s ability to deflect or challenge stigmatizing beliefs.5,6
There is a growing body of evidence—including meta-analyses—on the effects of self-stigma on people with SMI.7–12 In a meta-analysis of 127 articles, Livingston and Boyd7 reported that most studies were conducted in Europe or North America (77.5%), and that schizophrenia was the most common diagnosis (54.3%). Self-stigma is frequent in Europe (41.7% of 1229 participants with schizophrenia and 21.7% of 1182 participants with mood disorders9,10) and North America (36.1% of 144 people with SMI13). Less is known about self-stigma in other geographic areas. The level of self-stigma might vary according to cultural factors (eg, causal attributions of mental illness14) and sociopolitical ideology.15 According to Yang,14 stigma affects “what matters most” in a local social world, by threatening one’s capacity to meet social expectations (eg, the ability to engage in key life activities such as work or marriage14,16) and the whole family’s moral standing and socioeconomic status. Self-stigma might be more common in non-Western countries than in Western countries but this remains unproven.
Compared with those with nonpsychotic disorders, people at risk of psychosis face higher levels of public stigma that can lead to self-stigma.17,18 People with BPD are prone to self-criticism and feelings of shame that can make them more vulnerable to self-stigma.19 They face high levels of stigma, not only from the general public but also from mental health professionals.20 Gerlinger8 reported in a systematic review on stigma in schizophrenia the lack of studies comparing stigma at different stages of illness. It is still unclear whether self-stigma is greater in cases of prolonged psychosis compared with early psychosis, at-risk stages, or other SMI diagnoses.
To date, there have been no literature reviews comparing self-stigma frequency and correlates in different geographical and cultural areas (Europe, North America, South America, Middle East, South Asia, South-East Asia, and Oceania). Similarly, to our knowledge, no literature review has been conducted comparing internalized stigma in at-risk stages, schizophrenia, BD, MDD, BPD, and anxiety disorders. Self-stigma was negatively associated with self-esteem, self-efficacy, quality of life (QoL), and clinical and functional outcomes.7 However, it is difficult to disentangle the specific effects of self-stigma, as measures of perceived or experienced stigma are often used to assess the correlates of self-stigma (43.9% of the 127 studies7). Most studies were cross-sectional (86.7% of 127 studies7). The longitudinal effects of self-stigma remain largely unknown. Several interventions (combinations of psychoeducation and cognitive restructuring in most cases, making empowered decisions about disclosure in others) have been designed to reduce self-stigma and its impact on patients’ outcomes.21 Psychiatric rehabilitation brings together a wide range of recovery-oriented interventions.22 Psychiatric rehabilitation could indirectly reduce self-stigma (eg, through improved psychiatric symptoms, self-esteem, cognitive, social, and vocational functioning) although this remains to be investigated. However, the use of psychiatric rehabilitation services also carries the risk of increased labeling and self-stigma.23,24
In summary, three reviews have been conducted on self-stigma since 2010, in schizophrenia8 and BD.11,12 One meta-analysis investigated the correlates of stigma resistance in SMI.6 To our knowledge, there has been no review of self-stigma frequency and correlates in different cultural and geographic areas and for different SMI conditions; nor any specific reviews of self-stigma, excluding explicitly perceived or experienced stigma. The effects of nonspecific recovery-oriented practices on self-stigma remain unknown. Based on the literature, we would expect to find a higher frequency of self-stigma in Eastern countries compared with Western countries. We made the hypotheses that cultural factors would influence self-stigma and that self-stigma would be associated with poor recovery-related outcomes. The present review has three objectives: (1) to review the frequency, correlates, and consequences of self-stigma in individuals with SMI; (2) to compare self-stigma in different geographical areas and to review its potential association with cultural factors; (3) to evaluate the strengths and limitations of the current body of evidence to guide future research.
Methods
A stepwise systematic literature review (PRISMA guidelines)25 was conducted by searching PubMed, Medline, Web of Science, PsycINFO, the Scopus citation index, and Ovid SP Cumulative Index to Nursing and Allied Health Literature (CINAHL) for published, peer-reviewed articles using the following keywords: “schizophrenia” / “bipolar disorder” / “borderline personality disorder” / “major depression” / “depression” / “anxiety disorder” / “serious mental illness” AND “stigma” / “self-stigma” / “internalized stigma”/ “internalised stigma.” No time restriction was set. Only published articles in English or French were included in the review. The reference list of three meta-analyses6,7,26 and three literature reviews8,11,12 on stigma and schizophrenia or BD were screened for additional relevant articles. To be included in this review articles had to meet all of the following criteria: (1) report explicitly on self-stigma (ie, articles on public stigma or using measures of perceived or experienced stigma were excluded); (2) concern a diagnosis of schizophrenia, bipolar disorder, borderline personality disorder, major depression or anxiety disorders; (3) provide quantitative data on the prevalence, correlates, or consequences of internalized stigma or stigma resistance. The first author applied the eligibility criteria and screened the records to select the included studies. The last author reviewed each decision. Disputed items were solved through discussion and by reading the article in detail to reach a final decision. For each study, we extracted the following information: general information (author, year of publication, country, design, population considered, setting, total number of participants, mean age, or age range), outcome measure (scale/items used to measure self-stigma, reliability), the main findings, and variables relating to quality assessment (see supplementary table 2 for the detailed characteristics of the included studies). Quality assessment was performed using the Systematic Appraisal of Quality in Observational Research (SAQOR) tool. This tool comprises six domains (sample, control/comparison group, exposure/outcome measurements, follow-up, confounders, and reporting of data27) and has been adapted for cross-cultural psychiatric epidemiology studies.28 An overall quality score (high, moderate, or low) was determined based on adequacy in the six domains. Means and percentages were weighted for the number of cases per study to obtain prevalence data. Derived weighted means by geographical area and pooled standard deviations were calculated. One-way ANOVA was conducted from these summary data and post hoc pairwise test comparisons were computed using the Tukey–Kramer method. Weighted scores were calculated using proportions of rating scale scores. The frequency of self-stigma is often measured using the Internalized Stigma of Mental Illness Scale.29 A score above the midpoint indicates a moderate to high level of self-stigma.9,29 This choice was made for practical reasons (ie, facilitating comparisons between the studies) as there is no valid cutoff for measuring self-stigma. Stigma resistance is often measured using the ISMI stigma resistance subscale, which shows variable internal consistency (0.56 in Firmin et al meta-analysis6). Only the studies reporting internal consistency of above 0.50 were considered when extracting the correlates of stigma resistance. The study protocol was registered on the PROSPERO database on July 4, 2019 (ID 141282).
Results
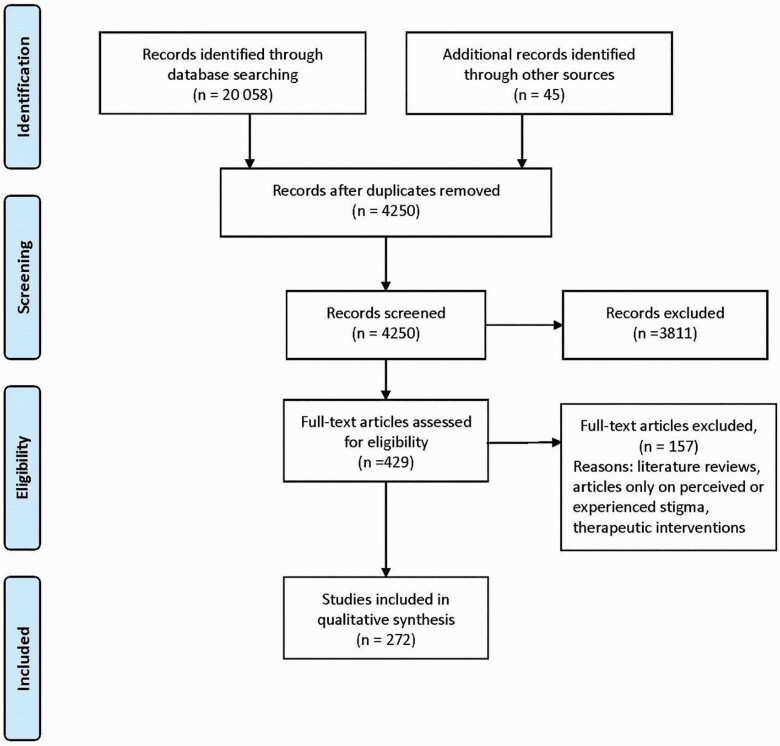
Our search on July 5, 2019 found 3215 articles on PubMed and 11 472 on Web of Science. It was completed by searching PsycINFO, the Scopus citation index, and Ovid SP CINAHL on March 25, 2020 then updated on April 16, 2020. The search was completed on August 22, 2020 using the additional terms “psychosis,” “depression,” “internalized stigma,” and “internalised stigma.” This resulted in 5371 supplementary articles. After manually removing all duplicates, there were 4250 remaining references. Based on their titles and abstracts, 3811 articles were excluded for lack of relevance. Most of these articles focused on public stigma, perceived or experienced stigma, or self-stigma in other discriminated populations. Our search strategy yielded 429 full-text articles. After conducting a full-text analysis of all these articles and excluding those which did not meet the inclusion criteria, we ended up with 272 relevant articles (figure 1). See supplementary table 5 for the list of the excluded studies.
Fig. 1.
Review process (Prisma flow diagram)
The 272 articles included were characterized by the heterogeneity of the samples, methods, scales, and reported outcomes. Most were published after 2010 (244 studies; 89.7%) and used cross-sectional designs (231 studies; 84.9%) with only 41 studies (15.1%) reporting longitudinal outcomes. A total of 89 (95 studies (34.9%) were conducted in Europe, 76 (27.9%) in North America, 44 in South-East Asia (16.2%), 24 (8.8%) in the Middle East, 13 (4.8%) in Africa, 10 in South Asia (3.7%), 4 in South America (1.5%), 4 in Oceania (1.5%), and 2 studies (0.7%) compared internalized stigma in different geographical areas (see supplementary table 1 for the geographical distribution of the included studies).30,31 Most studies included outpatients (211 studies, 77.6%). A total of 30 studies (11.3%) were conducted in a psychiatric rehabilitation context, 5 studies (1.8%) in consumer-operated service programs or advocacy groups and 6 studies (2.2%) in prison settings.
A total of 114 studies (41.9%) concerned schizophrenia, 14 (5.1%) BD, 13 (4.8%) MDD, and 13 (4.8%) at-risk stages or first episode psychosis, 2 (0.7%) anxiety disorders and 1 obsessive-compulsive disorder (0.4%). A total of 115 studies (42.3%) looked at SMI. There were large variations in the definition of SMI. Twenty-five studies (9.6%) defined SMI as schizophrenia, BD, or MDD. Fifty-four studies (20%) used a broad definition of SMI and included participants with anxiety disorders (AD, n = 25), obsessive-compulsive disorder (n = 11), and personality disorders (13 studies). Twelve studies (4.6%) investigated self-stigma in schizophrenia and BD (n = 6), schizophrenia and MDD (n = 1), mood disorders (n = 2), schizophrenia and AD (n = 1), AD and MDD (n = 1), and BPD and social phobia (n = 1). Twenty-four studies (8.1%) did not specify the different forms of SMI. Most studies included young (18–34 years old; 50 studies [18.4%]) or middle-aged participants (35–50 years old; 185 studies [68%]). See supplementary table 6 for the characteristics of studies that included people less than 18 years old. One hundred and ninety-two studies (70.6%) used the Internalized Stigma of Mental Illness29 scale to measure internalized stigma and 33 studies (12.1%) the Self-Stigma of Mental Illness Scale32 (SSMI). Forty-seven studies (17.3%) measured self-stigma with other scales. Most of the instruments used to measure self-stigma in non-Western countries were adaptations of scales designed in Europe or North America (n = 74; 80%). The quality ratings of the included studies obtained using SAQOR27 ranged from high to moderate (respectively, 57.7% and 42.3%). The results are shown in table 1.
Table 1.
Research Characteristics of the 272 Studies Included in the Review
| Characteristic | All studies (n = 272) % |
|---|---|
| Publication date | |
| Pre 2011 | 28 (10.3%) |
| 2011 or later | 244 (89.7%) |
| Study design | |
| Cross-sectional | 231 (84.9%) |
| Longitudinal | 41 (15.1%) |
| Region of study | |
| North America | 76 (27.9%) |
| Europa | 95 (34.9%) |
| South Asia | 10 (3.7%) |
| South East Asia | 44 (16.2%) |
| Middle East | 24 (8.8%) |
| South America | 4 (1.5%) |
| Africa | 13 (4.8%) |
| Australia | 4 (1.5%) |
| Others | 2 (0.7%) |
| Study sites | |
| Single site | 270 (99.3%) |
| Multiple countries/sites | 2 (0.7%) |
| Diagnosis | |
| Severe mental illness | 115 (42.3%) |
| Bipolar disorder | 14 (5.1%) |
| Obsessive-compulsive disorder | 1 (0.4%) |
| Major depressive disorder | 13 (4.8%) |
| Anxiety disorder | 2 (0.7%) |
| Schizophrenia | 114 (41.9%) |
| At risk stages/first episode psychosis | 13 (4.8%) |
| Mean age | |
| <18 years old | 3 (1.1%) |
| 18–34 years old | 50 (18.4%) |
| 35–50 years old | 185 (68%) |
| >50 years old | 13 (4.8%) |
| Mixed | 21 (7.7%) |
| % articles including people <18 | |
| Yes | 24 (8.8%) |
| No | 248 (91.2%) |
| Internalized stigma measures | |
| Internalized Stigma of Mental Illness (ISMI) | 192 (70.6%) |
| Self-Stigma of Mental Illness Scale (SSMIS) | 33 (12.1%) |
| Others | 47 (17.3%) |
| Patient status | |
| Inpatient | 28 (10.3%) |
| Outpatient | 211 (77.6%) |
| Mixed | 32 (11.8%) |
| Not reported | 1 (0.3%) |
| Psychiatric rehabilitation | |
| Yes | 47 (17.3%) |
| No | 225 (82.7%) |
| Quality rating | |
| High | 157 (57.7%) |
| Moderate | 115 (42.3%) |
Frequency of Self-stigma
Eighty articles (29.4%) reported data on self-stigma extent in SMI, or on the proportion of individuals with moderate to high self-stigma, or on both outcomes. Thirty-three studies were conducted in Europe, 20 studies in North America, 17 in South-East Asia, 9 in Africa, 12 in Middle East, 6 in South Asia, 1 in South America, 1 in Australia, and 1 in Austria and Japan. Nine studies compared the frequency of self-stigma in different countries,9,10,30,33,34 cities,35 or settings.13,36,37 The samples were mostly composed of individuals with schizophrenia (31 studies; 43.4%) or SMI (33 studies; 40.5%). The results are shown in table 2. Forty-seven articles reported on the proportion of moderate to high self-stigma (ISMI >2.5 or above the midpoint on other scales) in a total of 15 871 participants (7500 SMI, 5518 schizophrenia, 1582 BD, 1188 MDD, 64 BPD, 19 AD). Eighty-five articles documented self-stigma extent (ISMI mean total score and standard deviation) in 25 458 participants (11 028 with SMI, 9661 with schizophrenia, 2083 with BD, 2154 with MDD, 377 with AD, 155 with BPD).
Table 2.
Frequency of Internalized Stigma
| Area | Study | Country | N | Mean IS total score | SD | n | High IS (%) | ||
|---|---|---|---|---|---|---|---|---|---|
| Europe | SMI | Evans-Lacko51 | Multi-site | 1835 | 2.2 | 0.5 | - | - | |
| Grambal169 | Czech Republic | 184 | 2.19 | 0.5 | - | - | |||
| Rusch58 | Switzerland | 186 | 1.9 | 0.6 | - | - | |||
| Xu57 | Switzerland | 141 | 1.91 | 0.61 | - | - | |||
| Kamaradova170 | Czech Republic | 332 | 2.10 | 0.5 | - | - | |||
| Bradstreet45 | UK | 272 | 2.2 | 0.49 | - | - | |||
| Krajewski33 | Multi-site | 786 | 2.29 (1.96–2.71) | 0.5 | 786 | 33% (15.2%–57.4%) | |||
| Dubreucq93 | France | 738 | 2.20 | 0.51 | 738 | 31.2% | |||
| Oexle96 | Switzerland | 222 | 2.10 | 0.55 | - | - | |||
| Rusch107 | Switzerland | 116 | 2.15 | 0.54 | - | - | |||
| Szczesniak171 | Poland | 114 | 2.23 | 0.5 | - | - | |||
| Weighted total | 4926 | 2.18 | 0.26 | 1524 | 32% | ||||
| Schizophrenia | Brohan9 | Multi-site | 1129 | 2.40 (2.0–2.97) | 0.56 | 1129 | 41.7% | ||
| Vidovic126 | Croatia | 149 | 2.13 | 0.93 | 149 | 22.8% | |||
| Sibitz172 | Austria | 157 | 2.09 | 0.67 | - | - | |||
| Galderisi173 | Italia | 921 | 2.1 | 0.5 | - | - | |||
| Rossi174 | Italia | 910 | 2.2 | 0.44 | - | - | |||
| Aukst-Margetic81 | Croatia | 117 | 2.13 | 0.44 | - | - | |||
| Hofer30 | Austria | 52 | 2.01 | 0.51 | - | - | |||
| Bouvet175 | France | 62 | 2.23 | 0.46 | - | - | |||
| Vrbova176 | Czech Republic | 197 | 2.18 | 0.46 | - | - | |||
| Surmann177 | Germany | 80 | 2.12 | 0.47 | - | - | |||
| Dubreucq93 | France | 466 | 2.18 | 0.51 | 466 | 29.8% | |||
| Holubova178 | Czech Republic | 103 | 2.20 | 0.47 | - | - | |||
| Szczesniak171 | Poland | 51 | 2.19 | 0.5 | - | - | |||
| Uhlmann179 | Germany | 23 | 2.0 | 0.5 | - | - | |||
| Vrbova176 | Czech Republic | 197 | 2.18 | 0.47 | - | - | |||
| Switaj83 | Poland | 110 | 2.39 | 0.53 | - | - | |||
| Weighted total | 4724 | 2.21 | 0.27 | 1744 | 36.9% | ||||
| Bipolar disorders/MDD | Brohan10 | Multi-site | 577 | 1.94 BD | 1.97 | 0.87 | 1182 | 21.7% | |
| 603 | 2.11 MDD | ||||||||
| Bipolar disorders | Post180 | Austria | 60 | 1.9 BD | 0.57 | - | - | ||
| Dubreucq93 | France | 117 | 2.2 | 0.53 | 117 | 29.9% | |||
| Quenneville181 | Switzerland | 69 | 2.27 | 0.5 | - | - | |||
| Szczesniak171 | Poland | 19 | 2.39 | 0.5 | - | - | |||
| MDD | Lanfredi182 | Multi-site | 516 | 2.2 | 0.5 | - | - | ||
| Dubreucq93 | France | 27 | 2.29 | 0.56 | 27 | 40.7% | |||
| Holubova178 | Czech Republic | 80 | 1.96 | 0.42 | - | - | |||
| Prasko95 | Czech Republic | 72 | 2.36 | 0.49 | - | - | |||
| Szczesniak171 | Poland | 42 | 2.46 | 0.6 | - | - | |||
| Weighted total | BD MDD |
842 | 2.01 | 0.60 | 1326 | 22.7% | |||
| 1340 | 2.16 | 0.47 | |||||||
| Anxiety disorders | Ociskova183 | Czech Republic | 109 | 2.24 | 0.49 | - | - | ||
| Grambal169 | Czech Republic | 37 | 1.98 | 0.54 | |||||
| Dubreucq93 | France | 19 | 2.35 | 0.56 | 19 | 42.1% | |||
| OCD | Moritz184 | Germany | 50 | 1.99 | 0.48 | - | - | ||
| Weighted total | - | 215 | 2.14 | - | 19 | 42.1% | |||
| BPD | Grambal169 | Czech Republic | 35 | 2.45 | 0.50 | - | - | ||
| Dubreucq93 | France | 64 | 2.36 | 0.47 | 64 | 43.8% | |||
| Quenneville181 | Switzerland | 39 | 2.56 | 0.66 | - | - | |||
| Personality disorder | Kamaradova170 | Czech Republic | 17 | 2.37 | 0.58 | - | - | ||
| Weighted total | - | 155 | 2.43 | - | 64 | 43.8% | |||
| North America | SMI | Livingston36 | Canada | 91 | 2.13 | 0.38 | 91 | 10% | |
| Livingston37 | Canada | 71 | 2.10 | 0.35 | 71 | 9% | |||
| Livingston43 | Canada | 94 | 2.22 | 0.49 | 94 | 23.4% | |||
| West13 | USA | 144 | 1.72 | 0.57 | 144 | 36.1% (31%–41%) | |||
| Ritscher-Boyd112 | USA | - | - | - | 82 | 28% | |||
| Ritscher-Boyd185 | USA | 149 | 2.19 | 0.52 | 149 | 24.8% | |||
| Drapalski186 | USA | 100 | 2.3 | 0.4 | 100 | 35% | |||
| Harris38 | USA | 235 | 2.31 | 0.47 | 235 | 37% | |||
| Chronister187 | USA | 101 | 2.2 | 0.45 | 101 | 25% | |||
| Kira188 | USA | 330 | 2.16 | 0.72 | 330 | 40.1% | |||
| Tomar189 | USA | 108 | 2.31 | 0.5 | 108 | 40.7% | |||
| Pearl105 | USA | 319 | 2.11 | 0.53 | - | - | |||
| Jahn190 | USA | 516 | 2.25 | 0.49 | - | - | |||
| Villotti191 | USA | 170 | 1.95 | 0.47 | - | - | |||
| Weighted total | - | 2428 | 2.16 | 1505 | 31.4% | ||||
| Schizophrenia | Firmin192 | USA | - | - | - | 111 | 36.5% (25%–45%) | ||
| O’Connor133 | USA | - | - | - | 353 | 50% | |||
| Link193 | USA | - | - | - | 65 | 26.2% | |||
| Lysaker101 | USA | 70 | 2.36 | 0.54 | |||||
| Weighted total | - | 70 | 2.36 | 0.29 | 529 | 44.2% | |||
| Bipolar disorders | Howland42 | USA | 115 | 2.22 | 0.48 | 115 | 26% | ||
| Bassirnia194 | USA | 112 | 1.94 | 0.47 | - | - | |||
| Weighted total | 227 | 2.08 | 0.22 | ||||||
| South America | Schizophrenia | Caqueo-Uritzar34 | Multi-site | 253 | 2.3 | 0.54 | 253 | 38.6% (28.6%–48.7%) | |
| Weighted total | 253 | 2.3 | 0.29 | ||||||
| Australia | Schizophrenia | Hill195 | Australia | 60 | 2.56 | 0.49 | - | - | |
| Weighted total | 60 | 2.56 | 0.24 | ||||||
| South Asia | SMI | Grover196 | India | 1,403 | 2.29 | 0.47 | 1403 | 29.4% | |
| Maharjan197 | Nepal | - | - | - | 180 | 52% | |||
| Weighted total | - | 1403 | 2.29 | 0.22 | 1583 | 28.6% | |||
| Schizophrenia | Grover196 | India | 707 | 2.37 | 0.51 | 707 | 37.9% | ||
| Singh198 | India | 100 | 2.3 | 0.40 | 100 | 29% | |||
| Pal199 | India | 32 | 2.74 | 0.40 | - | - | |||
| Weighted total | - | 839 | 2.37 | 0.24 | 807 | 36.8% | |||
| Bipolar disorders | Grover196 | India | 344 | 2.23 | 0.38 | 344 | 20.6% | ||
| Pal199 | India | 59 | 2.25 | 0.38 | - | - | |||
| Grover200 | India | 185 | 2.33 | 0.43 | 185 | 28% | |||
| Weighted total | - | 588 | 2.26 | 0.15 | 529 | 23.2% | |||
| MDD | Grover196 | India | 352 | 2.19 | 0.45 | 352 | 21% | ||
| Sahoo201 | India | 107 | 2.39 | 0.57 | 107 | 40.1% | |||
| Weighted total | - | 459 | 2.23 | 0.23 | 459 | 25.5% | |||
| Anxiety disorders | Pal199 | India | 30 | 1.97 | 0.37 | - | - | ||
| South-East Asia | SMI | Picco202 | Singapore | 280 | 2.37 | 0.54 | 280 | 43.6% | |
| Ho97 | China | 136 | 2.3 | 0.6 | 136 | 36.8% | |||
| Young35 | China | 474 | 2.42 (2.34–2.50) | 0.52 | 474 | 43.5% (38.3%–49.5%) | |||
| Kim39 | South Korea | 160 | 2.06 | 0.36 | 160 | 8.1% | |||
| Kao40 | Taiwan | 251 | 2.26 | 0.51 | 251 | 50% | |||
| Weighted total | - | 1301 | 2.32 | 0.26 | 1301 | 39.7% | |||
| Schizophrenia | Lv138 | China | 95 | 2.17 | 0.38 | 95 | 20% | ||
| Hsiao61 | Taiwan | 111 | 2.33 | 0.53 | 111 | 27% | |||
| Lien76 | Taiwan | 170 | 2.36 | 0.52 | 170 | 39.4% | |||
| Kao40 | Taiwan | 151 | 2.42 | 0.44 | 151 | 51% | |||
| Li139 | China | 384 | 2.30 | 0.39 | - | - | |||
| Hofer30 | Japan | 60 | 2.16 | 0.42 | - | - | |||
| Ran127 | China | 232 | 2.46 | 0.28 | - | - | |||
| Mak67 | China | 162 | 2.34 | 0.61 | - | - | |||
| Shin88 | South Korea | 70 | 2.11 | 0.53 | - | - | |||
| Pribadi203 | Indonesia | 300 | 2.5 | 0.94 | 300 | 34% | |||
| Picco202 | Singapore | 74 | 2.41 | 0.52 | |||||
| Kim204 | South Korea | 123 | 2.15 | 0.50 | - | - | |||
| Lu205 | China | 92 | 2.11 | 0.45 | - | - | |||
| Park206 | South Korea | 321 | 2.51 | 0.65 | - | - | |||
| Weighted total | - | 2345 | 2.36 | 0.32 | 827 | 32.4% | |||
| Bipolar disorder | Ran127 | China | 39 | 2.36 | 0.30 | - | - | ||
| Weighted total | 2.36 | 0.09 | |||||||
| MDD | Picco202 | Singapore | 74 | 2.44 | 0.55 | - | - | ||
| Woon207 | Malaysia | 99 | 2.0 | 0.6 | 99 | 23.2% | |||
| Ran127 | China | 182 | 2.43 | 0.28 | - | - | |||
| Weighed total | 355 | 2.31 | 0.20 | 99 | 23.2% | ||||
| Anxiety Disorders OCD |
Picco202 | Singapore | 71 | 2.23 | 0.56 | - | - | ||
| Picco202 | Singapore | 61 | 2.41 | 0.49 | - | - | |||
| Weighted total | - | 132 | 2.31 | ||||||
| Middle East | SMI | Ghanean208 | Iran | - | - | - | 138 | 39% | |
| Tanriverdi209 | Turkey | 217 | 2.59 | 0.33 | - | - | |||
| Hasson-Ohayon210 | Israel | 107 | 2.28 | 0.49 | - | - | |||
| Korkmaz211 | Turkey | 224 | 2.53 | 0.48 | - | - | |||
| Weighted total | 548 | 2.50 | 0.18 | ||||||
| Schizophrenia | Sarisoy41 | Turkey | 109 | 2.17 | 0.51 | 109 | 29.4% | ||
| Çapar212 | Turkey | 250 | 2.76 | 0.37 | - | - | |||
| Olçun213 | Turkey | 76 | 2.51 | 0.55 | - | - | |||
| Yilmaz214 | Turkey | 63 | 2.63 | 0.49 | - | - | |||
| Yildirim94 | Turkey | 200 | 2.74 | 0.46 | - | - | |||
| Tanriverdi209 | Turkey | 46 | 2.54 | 0.25 | |||||
| Weighted total | - | 744 | 2.61 | 0.32 | 109 | 29.4% | |||
| Bipolar disorders | Sarisoy41 | Turkey | 118 | 2.10 | 0.46 | 118 | 18.5% | ||
| Cerit215 | Turkey | 80 | 2.12 | 0.39 | - | - | |||
| Sadighi216 | Iran | 126 | 1.90 | 0.87 | 126 | 27.6% | |||
| Tanriverdi209 | Turkey | 63 | 2.52 | 0.32 | - | - | |||
| Weighted total | - | 387 | 2.10 | 0.35 | 244 | 19.2% | |||
| Africa | SMI | Adewuya217 | Nigeria | - | - | - | 340 | 21.6% | |
| Girma53 | Ethiopia | 422 | 2.32 | 0.30 | 422 | 25.1% | |||
| Ibrahim55 | Nigeria | - | - | - | 370 | 22.5% | |||
| Asrat218 | Ethiopia | - | - | - | 317 | 32.1% | |||
| Weighted total | 422 | 2.32 | 0.09 | 1449 | 25.1% | ||||
| Schizophrenia | Mosanya125 | Nigeria | 256 | 1.94 | 0.68 | 256 | 18.8% | ||
| Fadipe219 | Nigeria | 370 | 2.09 | 0.43 | 370 | 16.5% | |||
| Assefa220 | Ethiopia | - | - | - | 212 | 46.7% | |||
| Bifftu124 | Ethiopia | - | - | - | 411 | 48.6% | |||
| Weighted total | - | 626 | 2.03 | 0.29 | 1249 | 32.6% | |||
Note: MDD, Major Depressive Disorder; OCD, Obsessive Compulsive Disorder; BPD, Borderline Personality Disorder; SMI, Severe Mental Illness. Mean Internalized Stigma refers to ISMI mean total score. High Internalized Stigma refers to the proportion of patients with ISMI > 2.5 or above the midpoint on other scales. Bold faces represents the total sample and the weighted means and proportions.
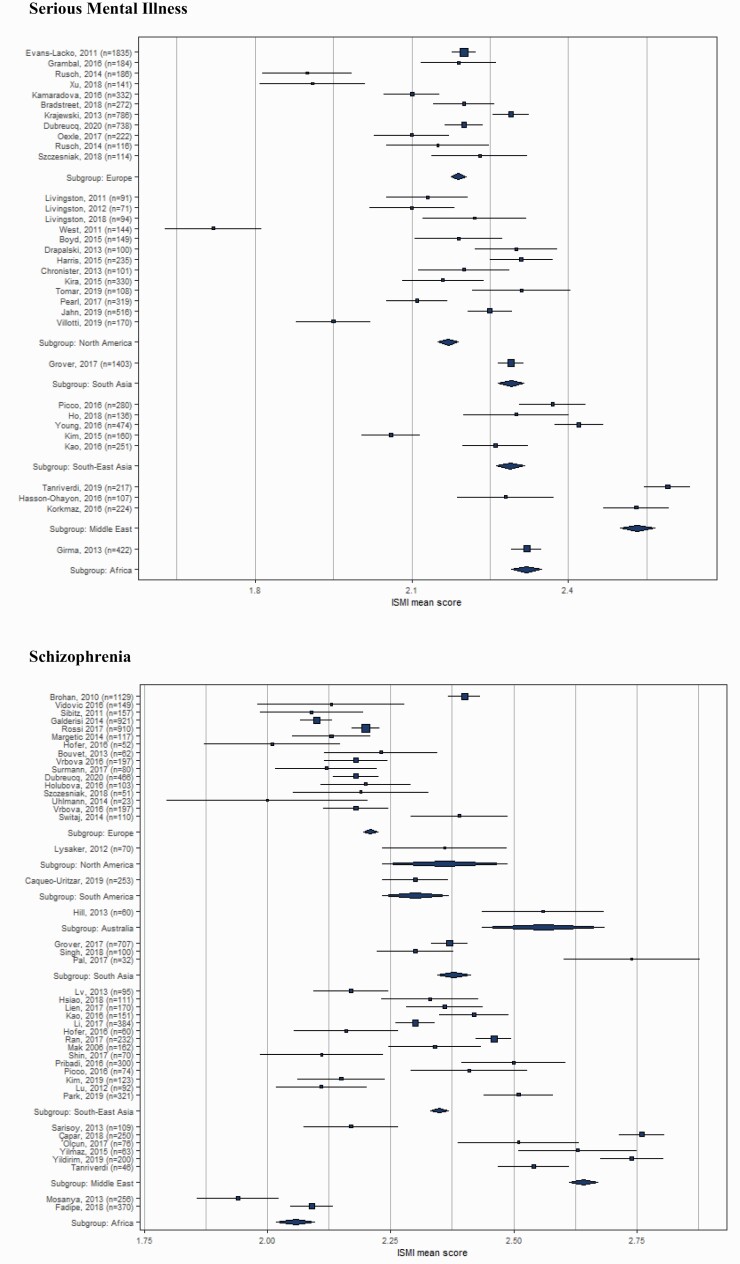
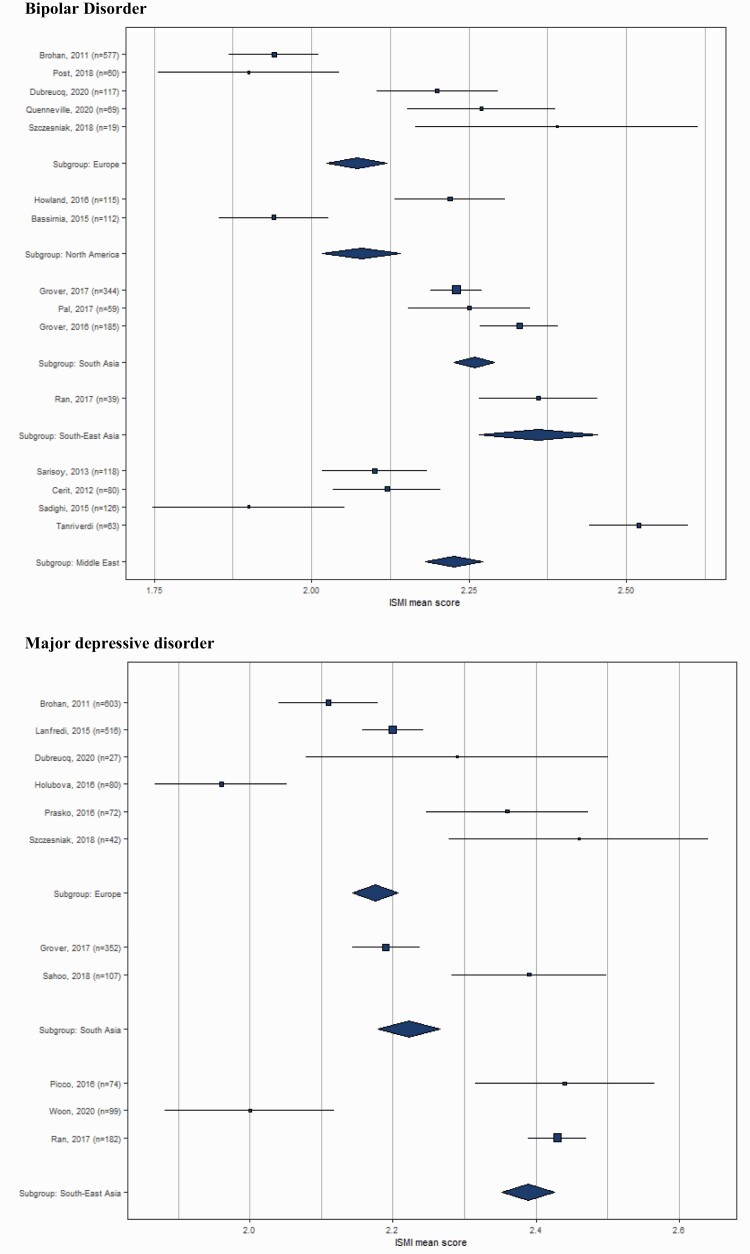
About one-third of people with SMI (31.3%) reported elevated self-stigma. The highest frequency was found in schizophrenia (35.8%). Higher frequency was found in South-East Asia and the Middle East for SMI, and in North America, Europe, and Africa for schizophrenia. Significant between-group differences in mean self-stigma scores were found between Europe and South Asia or South-East Asia for participants with SMI (P < 0.001; weighted mean difference = 0.150 and 0.140), schizophrenia (P < 0.001; 0.159 and 0.143), bipolar disorder (P < 0.001; 0.253 and 0.35), and MDD (P < 0.001; 0.148 and 0.07). Compared with Europe, self-stigma was higher in the Middle East and Africa for SMI (P < 0.001; 0.322 and 0.140) and in the Middle East and South America for schizophrenia (P < 0.001; 0.401 and 0.08). Box plots on the differences by geographical area are provided on table 3. Self-stigma did not differ between South-East Asia and Africa for SMI, South Asia and South-East Asia for schizophrenia, and North America and the Middle East for bipolar disorder. The results are shown in supplementary table S4. There were significant country-related differences in the proportion of people with SMI who reported high self-stigma in Europe (from 15.2% in Sweden9 to 57% in Croatia33), North America (from 9% in Canada37 to 37% in USA38) and in South-East Asia (from 8.1% in South Korea39 to 50% in Taiwan40). Setting-related differences were also found.13,35 Similar variations were found for schizophrenia, BD (18.5% Turkey,41 in remitted BD; 26% USA,42 in non-adherent BD), MDD, obsessive-compulsive disorder and anxiety disorders.
Table 3.
Between-groups Differences by Geographical Area
Means and percentages were weighted for the number of cases per study to obtain prevalence data. Derived weighted means by geographical area and pooled standard deviations were calculated. One-way ANOVA was conducted from these summary data and Post hoc pairwise test comparisons were computed with Tukey–Kramer method. Plots shows the ISMI mean score for each studies and each area with 95% confidence interval.
Cross-sectional Correlates of Self-stigma
Two hundred and forty-one studies (88.6%) reported on cross-sectional internalized stigma correlates. The most common diagnosis was schizophrenia (n = 106; 44%), followed by BD (n = 11; 4.6%) and at-risk states or early psychosis (n = 9; 3.7%). Ninety studies (37.3%) concerned SMI. The results are shown in table 4. See supplementary table 3 for the detailed list of correlates/consequences.
Table 4.
Cross-sectional Correlates and Consequences of Self-stigma
| A | B | C | D | E | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of studies (n = 272) | Non-significant relationship (P > 0.05) | Significant relationship (P < 0.05) | Positive relationship (P < 0.05) | Negative relationship (P < 0.05) | ||||||
| Variables | n | % | n | % | n | % | n | % | n | % |
| Sociodemographic | ||||||||||
| Gender (1) | 62 | 22.8 | 50 | 80.7 | 12 | 19.3 | 3 | 25.0 | 9 | 75.0 |
| Age | 68 | 25.0 | 49 | 72.1 | 19 | 27.9 | 12 | 63.2 | 7 | 36.8 |
| Education | 60 | 22.1 | 37 | 61.7 | 23 | 38.3 | 10 | 43 | 13 | 57 |
| Employment(2) | 37 | 13.6 | 16 | 43.2 | 21 | 56.8 | 2 | 9.5 | 19 | 90.5 |
| Marital status(3) | 40 | 14.7 | 28 | 70 | 12 | 30 | 3 | 25.0 | 9 | 75.0 |
| Income | 16 | 5.9 | 5 | 31.2 | 11 | 68.8 | 0 | 0 | 11 | 100 |
| Source of income (4) | 11 | 4.0 | 6 | 54.5 | 5 | 45.5 | 3 | 60 | 2 | 40 |
| Immigrant status | 1 | 0.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| History of incarceration/homelessness | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Experience of victimization | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Parenting status (5) | 2 | 0.7 | 1 | 50 | 1 | 50 | 1 | 100 | 0 | 0 |
| Internalizing personality traits | 6 | 2.2 | 0 | 0 | 6 | 100 | 6 | 100 | 0 | 0 |
| Self-compassion/mindfulness | 2 | 0.7 | 1 | 50 | 1 | 50 | 0 | 0 | 1 | 100 |
| Locality (urban/rural) (6) | 7 | 2.6 | 4 | 57.1 | 3 | 42.9 | 1 | 33.3 | 2 | 66.7 |
| Illness-related | ||||||||||
| Severity of psychiatric symptoms | 65 | 23 | 10 | 15.4 | 55 | 84.6 | 55 | 100 | 0 | 0 |
| Higher distress from sub-threshold psychotic symptoms/psychiatric symptoms | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Age of onset | 26 | 9.6 | 19 | 73.0 | 7 | 27.0 | 0 | 0 | 7 | 100 |
| Illness duration | 32 | 11.8 | 22 | 68.7 | 10 | 31.3 | 7 | 70.0 | 3 | 30.0 |
| Stage of illness | 1 | 0.4 | 1 | 100 | 0 | 0 | - | - | - | - |
| Diagnosis(7) | 38 | 14.0 | 20 | 52.6 | 18 | 47.4 | NA | - | NA | - |
| Insight | 32 | 11.8 | 0 | 0 | 32 | 100 | 32 | 100 | 0 | 0 |
| Parental insight | 1 | 0.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Subjective clinical severity | 3 | 1.1 | 0 | 0 | 3 | 100 | 3 | 100 | 0 | 0 |
| Perceived cognitive dysfunction | 4 | 1.5 | 0 | 0 | 4 | 100 | 4 | 100 | 0 | 0 |
| Hospitalizations | 38 | 14.0 | 23 | 60.5 | 15 | 39.5 | 14 | 93.3 | 1 | 6.7 |
| Treatment setting (8) | 6 | 2.2 | 3 | 50 | 3 | 50 | 1 | 33.3 | 2 | 66.7 |
| Involuntary hospitalizations (IH) | 3 | 1.1 | 1 | 33.3 | 2 | 66.7 | 2 | 100 | 0 | 0 |
| Negative emotional reactions to IH | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Forensic patient status | 3 | 1.1 | 2 | 66.7 | 1 | 33.3 | 1 | 100 | 0 | 0 |
| Compulsory community treatment | 1 | 0.4 | 1 | 100 | 0 | 0 | - | - | - | - |
| History of suicide attempt | 6 | 2.2 | 1 | 16.7 | 5 | 83.3 | 5 | 100 | 0 | 100 |
| Social anxiety | 3 | 1.1 | 0 | 0 | 3 | 100 | 3 | 100 | 0 | 0 |
| Comorbid post-traumatic stress disorder | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Comorbid personality disorder | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Cormorbid substance use disorder | 3 | 1.1 | 1 | 33.3 | 2 | 66.7 | 2 | 100 | 0 | 0 |
| Drug extra-pyramidal side-effects | 4 | 1.5 | 0 | 0 | 4 | 100 | 4 | 100 | 0 | 0 |
| Cognitive functioning | 6 | 2.2 | 1 | 16.7 | 5 | 83.3 | 0 | 0 | 5 | 100 |
| Social cognition | 4 | 1.5 | 1 | 25 | 3 | 75 | 0 | 0 | 3 | 100 |
| Metacognitive abilities | 7 | 2.6 | 0 | 0 | 7 | 100 | 0 | 0 | 7 | 100 |
| Dysfunctional attitudes | 1 | 0.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Use of negative coping strategies | 8 | 2.9 | 0 | 0 | 8 | 100 | 8 | 100 | 0 | 0 |
| Environment-related | ||||||||||
| Country level of public stigma | 6 | 2.2 | 0 | 0 | 6 | 100 | 6 | 100 | 0 | 0 |
| Perceived stigma | 18 | 6.6 | 0 | 0 | 18 | 100 | 18 | 100 | 0 | 0 |
| Self-labelling | 3 | 1.1 | 0 | 0 | 3 | 100 | 3 | 100 | 0 | 0 |
| Stigma stress | 4 | 1.5 | 0 | 0 | 4 | 100 | 4 | 100 | 0 | 0 |
| Group value | 3 | 1.1 | 0 | 0 | 3 | 100 | 0 | 0 | 3 | 100 |
| Perceived legitimacy | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Social network | 11 | 4.0 | 0 | 0 | 11 | 100 | 0 | 0 | 11 | 100 |
| Sense of belonging | 2 | 0.7 | 0 | 0 | 2 | 100 | 0 | 0 | 2 | 100 |
| Perceived social support | 21 | 8.4 | 0 | 0 | 21 | 100 | 0 | 0 | 21 | 100 |
| Loneliness | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Family sense of coherence | 1 | 0.4 | 0 | 0 | 1 | 100 | 0 | 0 | 1 | 100 |
| Experienced and anticipated stigma | 13 | 4.8 | 0 | 0 | 13 | 100 | 13 | 100 | 0 | 0 |
| Expressed emotion in families | 1 | 0.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Associative stigma in MHP | 1 | 0.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Cultural factors | ||||||||||
| Attributing mental illness to supernatural causes | 3 | 1.1 | 0 | 0 | 3 | 100 | 3 | 100 | 0 | 0 |
| History of traditional treatment | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Loss of face in Eastern countries | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Psychosocial | ||||||||||
| Self-efficacy | 13 | 4.8 | 0 | 0 | 13 | 100 | 0 | 0 | 13 | 100 |
| Empowerment | 11 | 4.0 | 0 | 0 | 11 | 100 | 0 | 0 | 11 | 100 |
| Self-esteem | 44 | 16.2 | 0 | 0 | 44 | 100 | 0 | 0 | 44 | 100 |
| Hope | 19 | 7.0 | 0 | 0 | 19 | 100 | 0 | 0 | 19 | 100 |
| Depression | 41 | 15.1 | 0 | 0 | 41 | 100 | 41 | 100 | 0 | 0 |
| Suicide risk | 15 | 5.5 | 1 | 6.7 | 14 | 93.3 | 14 | 100 | 0 | 0 |
| Help-seeking/Therapeutic alliance | 5 | 1.8 | 0 | 0 | 5 | 100 | 0 | 0 | 5 | 100 |
| Treatment adherence | 15 | 5.5 | 0 | 0 | 15 | 100 | 0 | 0 | 15 | 100 |
| Subjective social status | 1 | 0.4 | 0 | 0 | 1 | 100 | 0 | 0 | 1 | 100 |
| Psychosocial function | 27 | 9.9 | 0 | 0 | 27 | 100 | 0 | 0 | 27 | 100 |
| Activity | 1 | 0.4 | 0 | 0 | 1 | 100 | 0 | 0 | 1 | 100 |
| Self-reported physical health | 2 | 0.7 | 0 | 0 | 2 | 100 | 0 | 0 | 2 | 100 |
| Capacity for intimacy/satisfaction in intimate relationships | 4 | 1.5 | 0 | 0 | 4 | 100 | 0 | 0 | 4 | 100 |
| Self-reported parenting experiences | 1 | 0.4 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 100 |
| Quality of life | 41 | 15.1 | 0 | 0 | 41 | 100 | 0 | 0 | 41 | 100 |
| Wellbeing | 9 | 3.3 | 0 | 0 | 9 | 100 | 0 | 0 | 9 | 100 |
| Satisfaction with life | 8 | 2.9 | 0 | 0 | 8 | 100 | 0 | 0 | 8 | 100 |
| “why try effect” | 2 | 0.7 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Coming out (CO)/CO assertiveness | 1 | 0.4 | 1 | 100 | 0 | 0 | - | - | - | - |
| Benefits from being out | 1 | 0.4 | 0 | 0 | 1 | 100 | 0 | 0 | 1 | 100 |
| Stigma resistance | 11 | 4.0 | 0 | 0 | 11 | 100 | 0 | 0 | 11 | 100 |
| Resilience | 7 | 2.6 | 0 | 0 | 7 | 100 | 0 | 0 | 7 | 100 |
| Personal recovery | 22 | 8.1 | 0 | 0 | 22 | 100 | 0 | 0 | 22 | 100 |
1)Columns D + E; 1 = Men.
2) Columns D + E; 1 = Employed.
3) Columns D + E; 1 = Married.
4) Columns D + E; 1 = Income earner.
5) Columns D + E; 1 = Mothers.
6) Columns D + E; 1 = Urban.
7) Columns D+ E; not applicable (heterogeneity of the samples).
8) Columns D + E; 1= Inpatients.
Table 4 presents the relationships between sociodemographic, illness-related, environment-related, cultural and psychosocial variables with self-stigma (includes 272 studies).
Few sociodemographic characteristics correlated significantly with self-stigma. Immigrant status, history of incarceration or homelessness,36,43 parenting status (mothers > fathers44), shame proneness, and avoidant or self-defeating personality traits (n = 6 studies) were associated with higher self-stigma. The results were contrasted for all other sociodemographic variables (age, gender, education level, employment, marital status, income, and source of income). Other personal characteristics (attachment style, self-compassion) were not associated with self-stigma.45,46 Residual psychiatric symptomatology, positive and negative symptoms for schizophrenia, and depressive symptoms for BD were associated with higher self-stigma in most studies (84.6% significance; n = 65). Social anxiety (n = 3) and distress from sub-threshold psychotic symptoms47 were positively correlated with self-stigma. Self-stigma was equally severe in participants with ultra-high risk and established psychosis.48 Internalized shame about mental illness and fear accuracy in an emotion recognition task were negatively associated in people at risk of psychosis.49 Stigma stress, identified as a predictor of self-stigma in several studies (n = 4), was positively associated with transition to psychosis.50 Comorbid post-traumatic stress disorder (n = 2) and an increased number of drug side effects (n = 4) were positively associated with self-stigma.
Public stigma51 and other dimensions of stigma were associated with self-stigma (perceived stigma, n = 18 studies; perceived stigma from mental health providers,52n = 1; experienced stigma, n = 9; anticipated stigma, n = 3). Cultural factors such as attributing mental illness to supernatural causes,53–55 a history of traditional treatment,53,55 and loss of face in Eastern countries35,56 were associated with self-stigma. Concerns about losing face (or the fear of losing face because of being diagnosed with SMI) mediated the relationship between perceived stigma and self-stigma.56 Stigma stress (n = 4) and negative emotional reactions to involuntary psychiatric admission57,58 were significant correlates of self-stigma, in contrast with compulsory community treatment,37 forensic status,36 and the number of involuntary admissions.57–59 In-group value (ie, how people with SMI see their own group,60 social networks and support (n = 11; n = 21), membership of an advocacy group, and family support protected against self-stigma.61,62 Family expressed emotion and associative stigma in mental health professionals were associated with higher self-stigma.63,64 Self-stigma mediated the effects of family expressed emotion and in-group value on psychosocial function and personal recovery.64,65
Insight into illness (n = 32 studies), parental insight,66 self-perception of clinical severity (n = 3), perceived cognitive dysfunction (n = 4), and attributions of personal responsibility67 were associated with higher self-stigma. Impairments in cognitive and metacognitive function (n = 5; n = 7), dysfunctional attitudes68 and avoidant coping strategies (n = 8) were associated with higher self-stigma. Conversely preserved cognitive abilities,69–71 empowerment, self-efficacy, self-agency, and stigma resistance protected against self-stigma.9,10,62,72 Mixed results were found for other illness-related correlates (age of onset, psychiatric diagnosis, illness duration, history of suicide attempts, inpatient status, past psychiatric admission, and number of hospitalizations).
In general, self-stigma was positively associated with depressive symptoms (n = 41) and suicidal ideation (n = 14) and negatively correlated with hope (n = 19), help seeking (n = 5), and treatment adherence (n = 15). Single studies found negative associations with therapeutic alliance73 and shared decision making.74 Insight into illness,70,75–80 avoidant personality traits,81 and coping strategies,82 loneliness,83 and resilience84 moderated the relationship with depression and self-esteem mediated the effects of self-stigma on hope.85 Self-stigma mediated the effects of perceived cognitive dysfunction and experienced stigma on suicidality86,87 and QoL.88 Self-stigma was negatively associated with QoL (n = 41), self-esteem (n = 44), self-efficacy (n = 13), well-being (n = 9), life satisfaction (n = 8), empowerment (n = 11), resilience (n = 7), stigma resistance (n = 11), and personal recovery (n = 22). Self-stigma positively correlated with the “why try effect” 89 and later stages of self-stigma with a higher impact on hope, self-esteem, psychosocial function, and personal recovery.89,90 Participants in the late stages of self-stigma reported more reasons for not disclosing their psychiatric diagnosis, in contrast with those in the early stages who reported greater benefits from being “out”.91
Self-stigma was negatively associated with global functioning (n = 27). Higher demoralization and decreased resilience mediated the relationship between self-stigma and psychosocial function.75,92 Self-stigma was negatively associated with relational satisfaction.41,93 Self-stigma positively correlated with sense of loneliness,83,94 fear of intimate relationships,41 and self-stigma on parenting abilities for mothers living without their children.44
Self-stigma and Longitudinal Outcomes
Forty-one studies reported longitudinal outcomes associated with internalized stigma. These studies mainly included participants with SMI (n = 15; 36.6%), schizophrenia (n = 16; 39%) or at-risk stages/early psychosis (n = 5; 12.2%). Twelve studies included young participants (<18, n = 1; 18–35, n = 11) and three individuals over 50 years old (10.7%). Fifteen were conducted in psychiatric rehabilitation settings (36.5%). The duration of follow-up ranged from 6 weeks95 to 2 years.96 The results are shown in table 5.
Table 5.
Longitudinal Correlates and Consequences of Self-stigma
| A. | B. | C. | D. | E. | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of studies (n = 41) | Non-significant relationship (P > 0.05) | Significant relationship (P < 0.05) | Positive relationship (P < 0.05) | Negative relationship (P < 0.05) | ||||||
| Variables | n | % | n | % | n | % | n | % | n | % |
| Correlates of increased self-stigma at follow-up | ||||||||||
| Female sex | 5 | 12.2 | 4 | 80 | 1 | 20 | 1 | 100 | 0 | 0 |
| Hospitalizations | 1 | 2.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Duration of untreated psychosis | 1 | 2.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Baseline psychiatric symptoms | 5 | 12.2 | 0 | 0 | 5 | 100 | 5 | 100 | 0 | 0 |
| Shame, self-contempt about IH and stigma stress | 2 | 4.9 | 0 | 0 | 2 | 100 | 2 | 100 | 0 | 0 |
| Negative coping strategies | 1 | 2.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Correlates of reduced self-stigma at follow-up | ||||||||||
| Attending to recovery-oriented daycare/vocational rehabilitation/COSP | 5 | 12.2 | 0 | 0 | 5 | 100 | 5 | 100 | 0 | 0 |
| Work without experienced discrimination | 1 | 2.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Receiving no disability benefits during PR | 1 | 2.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Longitudinal consequences of self-stigma | ||||||||||
| Psychiatric symptoms | 5 | 12.2 | 0 | 0 | 5 | 100 | 5 | 100 | 0 | 0 |
| Social anxiety | 1 | 2.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Depression | 6 | 14.6 | 0 | 0 | 6 | 100 | 6 | 100 | 0 | 0 |
| Suicide risk | 4 | 9.8 | 0 | 0 | 4 | 100 | 4 | 100 | 0 | 0 |
| Risk of hospitalizations | 1 | 2.4 | 0 | 0 | 1 | 100 | 1 | 100 | 0 | 0 |
| Self-esteem | 3 | 7.3 | 0 | 0 | 3 | 100 | 0 | 0 | 3 | 100 |
| Treatment adherence | 3 | 7.3 | 0 | 0 | 3 | 100 | 0 | 0 | 3 | 100 |
| Psychosocial function | 9 | 21.9 | 0 | 0 | 9 | 100 | 0 | 0 | 9 | 100 |
| Quality of Life | 3 | 7.3 | 0 | 0 | 3 | 100 | 0 | 0 | 3 | 100 |
| Life satisfaction | 1 | 2.4 | 0 | 0 | 1 | 100 | 0 | 0 | 1 | 100 |
| Personal recovery | 2 | 4.9 | 0 | 0 | 2 | 100 | 0 | 0 | 2 | 100 |
Note: COSP, consumer-operated service program; IH, involuntary hospitalization; PR, Psychiatric rehabilitation.
Table 5 presents the longitudinal relationships between sociodemographic, illness-related, environment-related, and psychosocial variables with self-stigma (includes 41 studies).
Fifteen studies reported on the baseline factors influencing the level of self-stigma at follow-up. Residual psychiatric symptoms,97–100 negative emotional reactions to involuntary hospitalization,57,99 and emotional distress98,101 were the most significant baseline factors associated with self-stigma at follow-up. Duration of untreated psychosis97 and baseline coping strategies102 were associated with higher self-stigma in single studies. Mixed results were found for self-stigma stability over time with no specific intervention.86,102–104 Attending psychiatric rehabilitation was associated with significant reductions in self-stigma extent (from a mean total ISMI score of 2.31 on admission to 1.96 at discharge; 38 2.36–2.20; 101 2.11–1.96; 105 2.1–2.04; 106 1.80–1.50 in participants having worked in the past year without being discriminated against107) and in the proportion of participants with high self-stigma (ISMI > 2.5 from 37% to 13.7%; 38 reduction in ISMI levels at follow up > 25% in 38% of the participants with mean self-stigma > 2103). Not receiving disability benefits during psychiatric rehabilitation was associated with a greater reduction in self-stigma.38 Attending consumer-operated service programs was associated with self-stigma reduction.108
Twenty-eight studies reported on the longitudinal consequences of self-stigma. Self-stigma at baseline was associated with increased positive symptoms,109 emotional discomfort,100 social anxiety,110 depression,111,112 suicidal ideation,96,113 and an increased risk of psychiatric hospitalization114 at follow-up. Participants with high self-stigma reported reduced self-esteem,112 decreased life satisfaction,115 lower personal recovery,116 less use of adaptive coping strategies,102 and lower treatment adherence117 at follow-up. Baseline self-stigma was associated with poorer social and vocational functioning109,118 at follow-up, and less benefits from vocational rehabilitation.119 A change in self-stigma during follow-up predicted depression. Increases in self-stigma were associated with more depressive symptoms109 and higher suicidality.99,120 Decreases in self-stigma were associated with less depression.104,105 Increased self-stigma was associated with more negative attitudes towards psychiatric medication,120,121 poorer social function,122 reduced self-esteem,99 and lower personal recovery.116 Reduced self-stigma was associated with decreased subjective clinical severity,105 higher self-esteem,101 and improved global functioning.105 Baseline self-stigma was not associated with QoL at follow-up.37 Decreased self-stigma during follow-up was, however, associated with improvements in QoL105 during psychiatric rehabilitation.
Self-stigma and Stigma Resistance
Thirty-one studies (11.9%) reported data on stigma resistance frequency in SMI. The results are shown in table 6. Stigma resistance was higher in mood disorders (59.7%10) than in schizophrenia (53.1%; n = 5). Stigma resistance in schizophrenia varied within Europe (from 49.2%9 to 63%123 and Africa (from 49.4% in Ethiopia124 to 72.7% in Nigeria125). Stigma resistance was negatively correlated with self-stigma in Austria,30,123 Croatia,126 Nigeria,125 and South Africa.62 In some countries, self-stigma and stigma resistance were both high (USA,42 Turkey, Ethiopia,124 India, Bolivia,34 Peru,34 Chile,34 and China127) and in Canada these were both low.36,37 Metacognitive abilities,128–130 social network,123,131 social power,132 self-compassion,131 psychological flexibility,131 fear of negative evaluation,128 perceived stigma,60,114 negative symptoms,130 and coping strategies129,133 were associated with high stigma resistance.
Table 6.
Prevalence of Stigma Resistance
| Area | Study | Country | n | Mean SR | SD | n | High SR (%) | |
|---|---|---|---|---|---|---|---|---|
| Europe | SMI | Grambal169 | Czech Republic | 184 | 2.52 | 0.57 | - | - |
| Dubreucq93 | France | 738 | 2.54 | 0.51 | 693 | 54.1 | ||
| Weighted total | 922 | 2.53 | ||||||
| Schizophrenia | Brohan9 | Multi-site | 1129 | 2.47 (2.29–2.7) | 0.51 | 1129 | 49.2% | |
| Vidovic126 | Croatia | 149 | 2.37 | 0.99 | 149 | 54% | ||
| Sibitz123 | Austria | 157 | 2.73 | 0.76 | 157 | 63.3% | ||
| Hofer30 | Austria | 52 | 2.94 | 0.53 | - | - | ||
| Bouvet175 | France | 62 | 2.46 | 0.55 | - | - | ||
| Vrbova176 | Czech Republic | 197 | 2.56 | 0.48 | - | - | ||
| Surmann177 | Germany | 80 | 2.35 | 0.58 | - | - | ||
| Dubreucq93 | France | 466 | 2.56 | 0.51 | 466 | 55.4% | ||
| Weighted total | - | 2292 | 2.51 | 1435 | 51.2% | |||
| Bipolar Disorders/MDD | Brohan10 | Multi-site | 1182 | 2.81 | 0.98 | 1182 | 59.7% | |
| Dubreucq93 | France | 117 BD | 2.52 | 0.53 | 117 | 52.1% | ||
| 27 MDD | 2.58 | 0.53 | 27 | 59.3% | ||||
| Weighted total | 1326 | 2.77 | 1326 | 59.02% | ||||
| Anxiety disorders | Grambal169 | Czech Republic | 37 | 2.30 | 0.56 | - | - | |
| Dubreucq93 | France | 19 | 2.44 | 0.68 | 19 | 36.8% | ||
| Borderline Personality Disorder | Grambal169 | Czech Republic | 35 | 2.27 | 0.57 | - | - | |
| Dubreucq93 | France | 64 | 2.52 | 0.48 | 64 | 51.6% | ||
| North America | SMI | Livingston37 | Canada | 71 | 2.07 | 0.38 | - | - |
| Livingston43 | Canada | 94 | 2.10 | 0.50 | 94 | 15.9% | ||
| Ritsher-Boyd112 | USA | - | - | - | 82 | 29% | ||
| Weighted total | - | 165 | 2.08 | 176 | 22% | |||
| Bipolar Disorders | Howland42 | USA | 115 | 3.06 | 0.46 | - | - | |
| South America | Schizophrenia | Caqueo-Uritzar34 | Multi-site | 253 | 2.4 | 0.61 | - | – |
| South Asia | Schizophrenia | Singh198 | India | 100 | 2.3 | 0.70 | 100 | 45% |
| Pal199 | India | 32 | 2.84 | 0.50 | - | |||
| Weighted total | - | 132 | 2.43 | 100 | 45% | |||
| Bipolar Disorders | Pal199 | India | 59 | 2.43 | 0.42 | - | - | |
| Grover200 | India | 185 | 2.21 | 0.51 | - | - | ||
| Weighted total | - | 244 | 2.26 | - | - | |||
| South-East Asia | SMI | Ran127 | China | 453 | 2.49 | 0.42 | - | - |
| Lau221 | Singapore | 280 | 2.87 | 0.47 | 280 | 82.9% | ||
| Weighted total | 733 | 2.63 | ||||||
| Schizophrenia | Li139 | China | 384 | 2.28 | 0.45 | - | - | |
| Hofer30 | Japan | 60 | 2.35 | 0.46 | - | - | ||
| Ran127 | China | 232 | 2.50 | 0.36 | - | - | ||
| Weighted total | - | 676 | 2.36 | - | - | |||
| Middle East | SMI | Ghanean208 | Iran | 138 | 2.46 | 0.39 | - | - |
| Schizophrenia | Sarisoy41 | Turkey | 109 | 2.56 | 0.62 | - | - | |
| Çapar212 | Turkey | 250 | 2.41 | 0.35 | - | - | ||
| Olçun213 | Turkey | 76 | 2.60 | 0.60 | - | - | ||
| Karakas222 | Turkey | 60 | 2.62 | 0.63 | - | - | ||
| Yilmaz214 | Turkey | 63 | 2.66 | 0.43 | - | - | ||
| Weighted total score | - | 558 | 2.51 | - | - | |||
| Bipolar Disorders | Sarisoy41 | Turkey | 118 | 2.38 | 0.54 | - | - | |
| Sadighi216 | Iran | 126 | 2.76 | 0.98 | 126 | 57.49% | ||
| Weighted total score | 246 | 2.55 | ||||||
| Africa | SMI | Girma53 | Ethiopia | 422 | 2.41 | 0.40 | - | - |
| Sorsdahl62 | South Africa | 142 | 2.90 | - | - | - | ||
| Weighted total | - | 564 | 2.53 | - | - | |||
| Schizophrenia | Mosanya125 | Nigeria | 256 | 2.79 | 0.53 | 256 | 72.7% | |
| Bifftu124 | Ethiopia | 411 | 2.52 | - | 411 | 49.4% | ||
| Weighted total | 667 | 2.62 | 667 | 58.34% | ||||
Note: MDD, Major Depressive Disorder; SMI, Severe Mental Illness. Mean stigma resistance refers to ISMI stigma resistance subscale mean score. High stigma resistance refers to the proportion of patients with ISMI stigma resistance subscale > 2.5. Bold faces represents the total sample and the weighted means and proportions.
Discussion
Research on self-stigma in SMI has considerably progressed over the past decade (244 articles since 2010 and 28 studies published prior to this).7 Self-stigma was present in all geographical areas with higher frequency in South-East Asia and the Middle East for SMI (>39%). Self-stigma in SMI was higher in the Middle East, South Asia, South-East Asia, and Africa than in Europe or North America. Schizophrenia was associated with high self-stigma in all geographical areas (32.6%–44.2%). Self-stigma in schizophrenia was higher in the Middle East, South-East Asia, South Asia, and South America than in Europe. Self-stigma differed according to the geographical area in mood disorders (higher self-stigma in South Asia and South-East Asia in comparison with Europe, North America, or the Middle East). Variations in patterns of stigma according to the cultural area might explain these differences. The greater public stigma relating to SMI in Eastern countries compared with Western countries could explain the higher levels of self-stigma in South Asia and South-East Asia.134 Other potential factors contributing to higher self-stigma include feelings of shame about not meeting the social expectations of “what matters most” in one’s social group,14,16 moral or supernatural causal attributions of mental illness, and social concerns about the spillover effects disclosing mental illness might have on the social and economic status of family members.53,55,134 The frequency of self-stigma is consistently high across the world. This concurs with several cross-national studies on perceived, experienced, or anticipated stigma.3,135–137 Lower rates of experienced stigma, but similar levels of self-stigma for people with schizophrenia were reported in China and India compared with Western countries.16,138,139 Cultural factors (eg, concerns about disclosure spillover on family members) leading to higher self-stigma and social withdrawal might explain these variations.14,16,138,139 Most of the instruments used for assessing self-stigma in non-Western countries were adapted from scales developed in Europe or North America and did not include culture-specific items. These scales might not reflect all the culture-specific forms of stigma.55,140 Anti-stigma campaigns and self-stigma reduction interventions should take into consideration cultural factors (eg, cost/benefits of strategic disclosure in a given cultural context35,54,141).
Cultural and socio-ideological factors might account for the large country-related variations that were found within geographical areas. Higher public stigma was found in Eastern/Southern Europe compared with Western Europe.142–144 Compared with Western Europe or Canada, higher levels of self-reported sociopolitical conservatism were found in Eastern Europe and the USA.145,146 Gonzales147 and De Luca148 found that self-reported political conservatism and right-wing authoritarianism were associated with increased public stigma. Cultural factors (eg, the endorsement of traditional cultural values, higher in China than in Taiwan or South Korea149) might contribute to the differences observed between Guangzhou and Hong Kong35 or between Taiwan and South Korea.39,40 These variations could be related to sample characteristics (eg, higher reliance on family support in Guangzhou compared with Hong Kong; 35 higher proportion of patients with BD in Korea than in Taiwan39,40).
Sociodemographic and illness-related correlates yielded mixed results in line with previous reviews.7,8 Self-stigma was high in BPD but this is based on a small number of studies with small sample sizes. Self-stigma was equally severe in the at-risk stages as in psychosis.111 Further research is needed to confirm this result. Self-stigma was closely associated with perceived and experienced stigma. These concepts are distinct and should be better differentiated between, as stereotype awareness and self-labeling do not necessarily imply stereotype agreement, self-application, and increased self-stigma.91,150 Self-support groups and recovery-oriented services promoting positive group identification60,106 should be further developed to prevent or reduce self-stigma. Reducing self-stigma implies targeting the explicitly negative views about the self that relate to being diagnosed with SMI. Making an empowered decision about disclosing an SMI diagnosis might be effective for adolescents or people in the early stages of self-stigma.91,151 People in the late stages of self-stigma may need to take part in group interventions combining psychoeducation and cognitive restructuring.21,57 Interventions should be proposed to each individual according to his/her personal needs and level of self-stigma.
The association between self-stigma with treatment setting varies (50% significance). Two studies reported higher self-stigma in outpatients compared with inpatients152,153 and one the opposite.83 Loneliness, low social support, perceived stigma, experienced stigma, and anticipated stigma might contribute to higher self-stigma in outpatients.152,153 Participating in community activities, good social support, and attending psychiatric rehabilitation services or consumer-operated service programs protect against self-stigma.9,62,105,108 Stigma stress, negative emotional reactions to involuntary hospitalization, and the use of avoidant coping strategies after discharge contribute to higher self-stigma.57,58,102 Improved inpatient care (ie, the implementation of recovery-oriented practices and interventions targeting stigma stress, therapeutic alliance and coping strategies) might result in better patient outcomes after discharge, although this remains to be investigated.
The development of recovery-oriented practices in mental health facilities should be encouraged as it could reduce perceived stigma, stigma stress,57–59 and negative emotional reactions to involuntary admissions.57–59 Peer-supported self-management interventions, Joint Crisis Plans, “No Force First” policies, and selective disclosure programs could improve self-stigma through reduced stigma stress and perceived coercion.151,154–156 Recovery-oriented training programs for mental health professionals improve personal recovery in people with SMI.157 They may also improve mental health professionals’ job satisfaction, burnout, and associative stigma of mental illness.15,63 Their effectiveness in reducing self-stigma in patients should be investigated.
Given the potential relationships with stigma stress,50 duration of untreated psychosis,97 distress from sub-threshold psychotic symptoms,47 and transition to psychosis,50 the effects of recovery-oriented early interventions on self-stigma and its consequences should be further investigated. Strategic disclosure programs result in people making empowered decisions about whether to disclose a diagnosis of SMI or not. They result in improved stigma stress and self-stigma in adolescents with SMI151 and should be integrated into recovery-oriented early intervention services.
As expected,7,8 self-stigma was negatively associated with recovery-related outcomes and positively associated with depression and suicidal ideation. Cognitive impairments, dysfunctional attitudes, and avoidant coping strategies were positively associated with self-stigma. Insight into illness was the most significant moderator of internalized stigma. Perceived cognitive dysfunction, perceived and experienced stigma all had indirect effects on clinical and functional outcomes via self-stigma. Baseline self-stigma was associated with poorer recovery-related outcomes and less benefit from vocational rehabilitation at follow-up.8,119 Reduction in self-stigma was associated with improved depression, suicidality, attitudes towards medication, self-esteem, QoL, and social function at follow-up.
Improved treatment (ie, recovery-oriented practices and nonspecific interventions targeting therapeutic alliance, dysfunctional attitudes, self-esteem, or coping strategies) could indirectly reduce self-stigma.158–160 Recovery-oriented psychoeducation improves treatment adherence and reduces the risk of hospitalization.161 Improved therapeutic alliance is associated with better recovery-related outcomes after attending to early interventions services.158 Other interventions such as cognitive behavioral therapy, cognitive remediation, or social skills training might reduce self-stigma through improved symptoms, dysfunctional attitudes, and functioning.22,159,160,162 Given the potential relationship between expressed emotion in the families of people with SMI and self-stigma and recovery-related outcomes,64,65 family psychoeducation could be effective for self-stigma.163 Family psychoeducation should be recovery-oriented and address both public stigma and self-stigma.164–167 The relationship between self-stigma in people with SMI and in their relatives is still unclear and should be further investigated.168
Stigma resistance and self-stigma were negatively associated with each other6 but with different patterns. Self-stigma and stigma resistance are distinct constructs and should be measured using more specific scales.6
Limitations
There are some limitations to this review due to the heterogeneity in the definition of SMI and in the samples, settings, methods, scales, and reported outcomes. Few articles reported longitudinal outcomes with a limited number of studies conducted in psychiatric rehabilitation settings. This review excluded studies where self-stigma was not the main focus, which means that stigma in all its forms (ie, perceived, experienced or anticipated stigma, and self-stigma) could actually have more wide-ranging effects on people with SMI. However, by focusing on self-stigma, this review provides a more accurate understanding of its effects on people with SMI. The heterogeneity of the samples, methods, scales, and reported outcomes in the included articles limited the possibilities for extracting comparable data. The large number of studies included in this review and the range of countries represented is however a considerable strength. The under-reporting of negative or nonsignificant results due to publication bias and the exclusion of unpublished studies from this review might have limited the accuracy of the synthesis. The present systematic review does not include a meta-analysis. This decision was made due to the large number of studies and the heterogeneity of the samples, methods, scales, and reported outcomes. Statistical analyses were used to compare self-stigma frequency in different geographical areas (the second objective of the present study). Future meta-analyses with a more limited focus (eg, on the impact of self-stigma on recovery-related outcomes) could be conducted to explore the present findings in more detail.
Conclusions
In short, self-stigma is a severe problem in all SMI conditions (including the at-risk stages) and all geographical areas and is associated with poor clinical and functional outcomes. Levels of public, perceived, and experienced stigma (including from mental health providers) are significant predictors of self-stigma, pleading for the reinforcement of anti-stigma campaigns and the development of recovery-oriented practices in mental health settings. The respective associations between the duration of untreated psychosis, self-stigma, and transition to psychosis support the development of recovery-oriented early intervention programs. Psychiatric rehabilitation could be an effective means of reducing self-stigma and should therefore be further developed in public policies.
Supplementary Material
Acknowledgments
The authors would like to thank Mrs Kim Barrett for proofreading the manuscript. They are also grateful to the reviewers of a previous version of the manuscript for their helpful comments.
Author contribution: The two authors had full access to the data in the study and take the responsibility for the integrity of the data and the accuracy of the data analysis. Dr Julien Dubreucq drafted the article. Dr Julien Dubreucq and Prof Nicolas Franck carried out the literature review. M. Julien Plasse did the statistical analysis. Prof Nicolas Franck critically revised the article. Both authors were involved in the collection and analysis of the data. Both authors contributed to and approved the final manuscript.
Conflicts of interests: none.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–385. [Google Scholar]
- 2. Corrigan PW, Larson JE, Rüsch N. Self-stigma and the “why try” effect: impact on life goals and evidence-based practices. World Psychiatry. 2009;8(2):75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M; INDIGO Study Group . Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet. 2009;373(9661):408–415. [DOI] [PubMed] [Google Scholar]
- 4. Yanos PT, Roe D, Markus K, Lysaker PH. Pathways between internalized stigma and outcomes related to recovery in schizophrenia spectrum disorders. Psychiatr Serv. 2008;59(12):1437–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thoits PA. Resisting the stigma of mental illness. Soc Psychol Q. 2011;74(1):6–28. [Google Scholar]
- 6. Firmin RL, Luther L, Lysaker PH, Minor KS, Salyers MP. Stigma resistance is positively associated with psychiatric and psychosocial outcomes: a meta-analysis. Schizophr Res. 2016;175(1–3):118–128. [DOI] [PubMed] [Google Scholar]
- 7. Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71(12):2150–2161. [DOI] [PubMed] [Google Scholar]
- 8. Gerlinger G, Hauser M, De Hert M, Lacluyse K, Wampers M, Correll CU. Personal stigma in schizophrenia spectrum disorders: a systematic review of prevalence rates, correlates, impact and interventions. World Psychiatry. 2013;12(2):155–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brohan E, Elgie R, Sartorius N, Thornicroft G; GAMIAN-Europe Study Group . Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN-Europe study. Schizophr Res. 2010;122(1–3):232–238. [DOI] [PubMed] [Google Scholar]
- 10. Brohan E, Gauci D, Sartorius N, Thornicroft G; GAMIAN-Europe Study Group . Self-stigma, empowerment and perceived discrimination among people with bipolar disorder or depression in 13 European countries: the GAMIAN-Europe study. J Affect Disord. 2011;129(1–3):56–63. [DOI] [PubMed] [Google Scholar]
- 11. Ellison N, Mason O, Scior K. Bipolar disorder and stigma: a systematic review of the literature. J Affect Disord. 2013;151(3):805–820. [DOI] [PubMed] [Google Scholar]
- 12. Hawke LD, Parikh SV, Michalak EE. Stigma and bipolar disorder: a review of the literature. J Affect Disord. 2013;150(2):181–191. [DOI] [PubMed] [Google Scholar]
- 13. West ML, Yanos PT, Smith SM, Roe D, Lysaker PH. Prevalence of internalized stigma among persons with severe mental illness. Stigma Res Action. 2011;1(1):3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yang LH, Chen FP, Sia KJ, et al. “What matters most:” a cultural mechanism moderating structural vulnerability and moral experience of mental illness stigma. Soc Sci Med. 2014;103:84–93. [DOI] [PubMed] [Google Scholar]
- 15. Yanos PT, DeLuca JS, Salyers MP, Fischer MW, Song J, Caro J. Cross-sectional and prospective correlates of associative stigma among mental health service providers. Psychiatr Rehabil J. 2020;43(2):85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Koschorke M, Padmavati R, Kumar S, et al. Experiences of stigma and discrimination of people with schizophrenia in India. Soc Sci Med. 2014;123:149–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yang LH, Wonpat-Borja AJ, Opler MG, Corcoran CM. Potential stigma associated with inclusion of the psychosis risk syndrome in the DSM-V: an empirical question. Schizophr Res. 2010;120(1–3):42–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yang LH, Anglin DM, Wonpat-Borja AJ, Opler MG, Greenspoon M, Corcoran CM. Public stigma associated with psychosis risk syndrome in a college population: implications for peer intervention. Psychiatr Serv. 2013;64(3):284–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rüsch N, Hölzer A, Hermann C, et al. Self-stigma in women with borderline personality disorder and women with social phobia. J Nerv Ment Dis. 2006;194(10):766–773. [DOI] [PubMed] [Google Scholar]
- 20. Gunderson JG, Herpertz SC, Skodol AE, Torgersen S, Zanarini MC. Borderline personality disorder. Nat Rev Dis Primers. 2018;4:18029. [DOI] [PubMed] [Google Scholar]
- 21. Yanos PT, Lucksted A, Drapalski AL, Roe D, Lysaker P. Interventions targeting mental health self-stigma: a review and comparison. Psychiatr Rehabil J. 2015;38(2):171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Franck N, Bon L, Dekerle M, et al. Satisfaction and needs in serious mental illness and autism spectrum disorder: the REHABase psychosocial rehabilitation project. Psychiatr Serv. 2019;70(4):316–323. [DOI] [PubMed] [Google Scholar]
- 23. Moritz S, Gawęda Ł, Heinz A, Gallinat J. Four reasons why early detection centers for psychosis should be renamed and their treatment targets reconsidered: we should not catastrophize a future we can neither reliably predict nor change. Psychol Med. 2019;49(13):2134–2140. [DOI] [PubMed] [Google Scholar]
- 24. Yang LH, Lo G, WonPat-Borja AJ, Singla DR, Link BG, Phillips MR. Effects of labeling and interpersonal contact upon attitudes towards schizophrenia: implications for reducing mental illness stigma in urban China. Soc Psychiatry Psychiatr Epidemiol. 2012;47(9):1459–1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wood L, Byrne R, Varese F, Morrison AP. Psychosocial interventions for internalised stigma in people with a schizophrenia-spectrum diagnosis: a systematic narrative synthesis and meta-analysis. Schizophr Res. 2016;176(2–3):291–303. [DOI] [PubMed] [Google Scholar]
- 27. Ross LE, Grigoriadis S, Mamisashvili L, et al. Quality assessment of observational studies in psychiatry: an example from perinatal psychiatric research. Int J Methods Psychiatr Res. 2011;20(4):224–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kohrt BA, Rasmussen A, Kaiser BN, et al. Cultural concepts of distress and psychiatric disorders: literature review and research recommendations for global mental health epidemiology. Int J Epidemiol. 2014;43(2):365–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. 2003;121(1):31–49. [DOI] [PubMed] [Google Scholar]
- 30. Hofer A, Mizuno Y, Frajo-Apor B, et al. Resilience, internalized stigma, self-esteem, and hopelessness among people with schizophrenia: cultural comparison in Austria and Japan. Schizophr Res. 2016;171(1–3):86–91. [DOI] [PubMed] [Google Scholar]
- 31. Mileva VR, Vázquez GH, Milev R. Effects, experiences, and impact of stigma on patients with bipolar disorder. Neuropsychiatr Dis Treat. 2013;9:31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Corrigan P, Watson A, Barr L. The self-stigma of mental illness: implications for self-esteem and self-efficacy. J Soc Clin Psychol. 2006;25:875e884. [Google Scholar]
- 33. Krajewski C, Burazeri G, Brand H. Self-stigma, perceived discrimination and empowerment among people with a mental illness in six countries: Pan European stigma study. Psychiatry Res. 2013;210(3):1136–1146. [DOI] [PubMed] [Google Scholar]
- 34. Caqueo-Urízar A, Boyer L, Urzúa A, Williams DR. Self-stigma in patients with schizophrenia: a multicentric study from three Latin-America countries. Soc Psychiatry Psychiatr Epidemiol. 2019;54(8):905–909. [DOI] [PubMed] [Google Scholar]
- 35. Young DK, Ng PY. The prevalence and predictors of self-stigma of individuals with mental health illness in two Chinese cities. Int J Soc Psychiatry. 2016;62(2):176–185. [DOI] [PubMed] [Google Scholar]
- 36. Livingston JD, Rossiter KR, Verdun-Jones SN. ‘Forensic’ labelling: an empirical assessment of its effects on self-stigma for people with severe mental illness. Psychiatry Res. 2011;188(1):115–122. [DOI] [PubMed] [Google Scholar]
- 37. Livingston J. Self-stigma and quality of life among people with mental illness who receive compulsory community treatment services. J Community Psychol. 2012;40:699–714. [Google Scholar]
- 38. Harris JI, Farchmin L, Stull L, Boyd J, Schumacher M, Drapalski AL. Prediction of changes in self-stigma among veterans participating in partial psychiatric hospitalization: the role of disability status and military cohort. Psychiatr Rehabil J. 2015;38(2):179–185. [DOI] [PubMed] [Google Scholar]
- 39. Kim WJ, Song YJ, Ryu HS, et al. Internalized stigma and its psychosocial correlates in Korean patients with serious mental illness. Psychiatry Res. 2015;225(3):433–439. [DOI] [PubMed] [Google Scholar]
- 40. Kao YC, Lien YJ, Chang HA, Wang SC, Tzeng NS, Loh CH. Evidence for the indirect effects of perceived public stigma on psychosocial outcomes: the mediating role of self-stigma. Psychiatry Res. 2016;240:187–195. [DOI] [PubMed] [Google Scholar]
- 41. Sarısoy G, Kaçar ÖF, Pazvantoğlu O, et al. Internalized stigma and intimate relations in bipolar and schizophrenic patients: a comparative study. Compr Psychiatry. 2013;54(6):665–672. [DOI] [PubMed] [Google Scholar]
- 42. Howland M, Levin J, Blixen C, Tatsuoka C, Sajatovic M. Mixed-methods analysis of internalized stigma correlates in poorly adherent individuals with bipolar disorder. Compr Psychiatry. 2016;70:174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Livingston J, Patel N, Bryson S, et al. Stigma associated with mental illness among Asian men in Vancouver, Canada. Int J Soc Psychiatry. 2018;64(7):679–689. [DOI] [PubMed] [Google Scholar]
- 44. Lacey M, Paolini S, Hanlon MC, Melville J, Galletly C, Campbell LE. Parents with serious mental illness: differences in internalised and externalised mental illness stigma and gender stigma between mothers and fathers. Psychiatry Res. 2015;225(3):723–733. [DOI] [PubMed] [Google Scholar]
- 45. Bradstreet S, Dodd A, Jones S. Internalised stigma in mental health: an investigation of the role of attachment style. Psychiatry Res. 2018;270:1001–1009. [DOI] [PubMed] [Google Scholar]
- 46. Døssing M, Nilsson KK, Svejstrup SR, Sørensen VV, Straarup KN, Hansen TB. Low self-compassion in patients with bipolar disorder. Compr Psychiatry. 2015;60:53–58. [DOI] [PubMed] [Google Scholar]
- 47. Denenny D, Thompson E, Pitts SC, Dixon LB, Schiffman J. Subthreshold psychotic symptom distress, self-stigma, and peer social support among college students with mental health concerns. Psychiatr Rehabil J. 2015;38(2):164–170. [DOI] [PubMed] [Google Scholar]
- 48. Pyle M, Morrison AP. Internalised stereotypes across ultra-high risk of psychosis and psychosis populations. Psychosis. 2017;9:1–9. [Google Scholar]
- 49. Larsen EM, Herrera S, Bilgrami ZR, et al. Self-stigma related feelings of shame and facial fear recognition in individuals at clinical high risk for psychosis: a brief report. Schizophr Res. 2019;208:483–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rüsch N, Heekeren K, Theodoridou A, et al. Stigma as a stressor and transition to schizophrenia after one year among young people at risk of psychosis. Schizophr Res. 2015;166(1–3):43–48. [DOI] [PubMed] [Google Scholar]
- 51. Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychol Med. 2012;42(8):1741–1752. [DOI] [PubMed] [Google Scholar]
- 52. Wang K, Link BG, Corrigan PW, Davidson L, Flanagan E. Perceived provider stigma as a predictor of mental health service users’ internalized stigma and disempowerment. Psychiatry Res. 2018;259:526–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Girma E, Tesfaye M, Froeschl G, Möller-Leimkühler AM, Dehning S, Müller N. Facility based cross-sectional study of self-stigma among people with mental illness: towards patient empowerment approach. Int J Ment Health Syst. 2013;7(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Makanjuola V, Esan Y, Oladeji B, et al. Explanatory model of psychosis: impact on perception of self-stigma by patients in three sub-Saharan African cities. Soc Psychiatry Psychiatr Epidemiol. 2016;51(12):1645–1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ibrahim AW, Mukhtar YM, Sadique PK, et al. A facility-based assessment of internalized stigma among patients with severe mental illnesses in Maiduguri, North-Eastern Nigeria. Int Neuropsychiatr Dis J. 2016;6(1):1–11. [Google Scholar]
- 56. Chen ES, Chang WC, Hui CL, Chan SK, Lee EH, Chen EY. Self-stigma and affiliate stigma in first-episode psychosis patients and their caregivers. Soc Psychiatry Psychiatr Epidemiol. 2016;51(9):1225–1231. [DOI] [PubMed] [Google Scholar]
- 57. Xu Z, Lay B, Oexle N, Drack T, et al. Involuntary psychiatric hospitalization, stigma stress and recovery: a 2-year study. Epidemiol Psychiatr Sci. 2018a;31:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Rüsch N, Müller M, Lay B, et al. Emotional reactions to involuntary psychiatric hospitalization and stigma-related stress among people with mental illness. Eur Arch Psychiatry Clin Neurosci. 2014;264(1):35–43. [DOI] [PubMed] [Google Scholar]
- 59. Chang CC, Wu TH, Chen CY, Lin CY. Comparing self-stigma between people with different mental disorders in Taiwan. J Nerv Ment Dis. 2016;204(7):547–553. [DOI] [PubMed] [Google Scholar]
- 60. Rüsch N, Corrigan PW, Wassel A, et al. Ingroup perception and responses to stigma among persons with mental illness. Acta Psychiatr Scand. 2009;120(4):320–328. [DOI] [PubMed] [Google Scholar]
- 61. Hsiao CY, Lu HL, Tsai YF. Effect of family sense of coherence on internalized stigma and health-related quality of life among individuals with schizophrenia. Int J Ment Health Nurs. 2018;27(1):138–146. [DOI] [PubMed] [Google Scholar]
- 62. Sorsdahl KR, Kakuma R, Wilson Z, Stein DJ. The internalized stigma experienced by members of a mental health advocacy group in South Africa. Int J Soc Psychiatry. 2012;58(1):55–61. [DOI] [PubMed] [Google Scholar]
- 63. Verhaeghe M, Bracke P. Associative stigma among mental health professionals: implications for professional and service user well-being. J Health Soc Behav. 2012;53(1):17–32. [DOI] [PubMed] [Google Scholar]
- 64. Chan KKS, Lam CB. The impact of familial expressed emotion on clinical and personal recovery among patients with psychiatric disorders: the mediating roles of self-stigma content and process. Am J Orthopsychiatry. 2018;88(6):626–635. [DOI] [PubMed] [Google Scholar]
- 65. Chan RCH, Mak WWS, Lam MYY. Self-stigma and empowerment as mediating mechanisms between ingroup perceptions and recovery among people with mental illness. Stigma and Health. 2018a;3(3):283–293. [Google Scholar]
- 66. Gaziel M, Hasson-Ohayon I, Morag-Yaffe M, Schapir L, Zalsman G, Shoval G. Insight and satisfaction with life among adolescents with mental disorders: assessing associations with self-stigma and parental insight. Eur Psychiatry. 2015;30(2):329–333. [DOI] [PubMed] [Google Scholar]
- 67. Mak WW, Wu CF. Cognitive insight and causal attribution in the development of self-stigma among individuals with schizophrenia. Psychiatr Serv. 2006;57(12):1800–1802. [DOI] [PubMed] [Google Scholar]
- 68. Park SG, Bennett ME, Couture SM, Blanchard JJ. Internalized stigma in schizophrenia: relations with dysfunctional attitudes, symptoms, and quality of life. Psychiatry Res. 2013;205(1–2):43–47. [DOI] [PubMed] [Google Scholar]
- 69. West ML, Mulay AL, DeLuca JS, et al. Forensic psychiatric experiences, stigma, and self-concept: a mixed-methods study. J Forens Psychiatry Psychol. 2018;29:574–596. [Google Scholar]
- 70. Lysaker PH, Vohs J, Hasson-Ohayon I, Kukla M, Wierwille J, Dimaggio G. Depression and insight in schizophrenia: comparisons of levels of deficits in social cognition and metacognition and internalized stigma across three profiles. Schizophr Res. 2013;148(1–3):18–23. [DOI] [PubMed] [Google Scholar]
- 71. Chan RCH, Mak WWS. Common sense model of mental illness: understanding the impact of cognitive and emotional representations of mental illness on recovery through the mediation of self-stigma. Psychiatry Res. 2016;246:16–24. [DOI] [PubMed] [Google Scholar]
- 72. Chiu MY, Davidson L, Lo WT, Yiu MG, Ho WW. Modeling self-agency among people with schizophrenia: empirical evidence for consumer-based recovery. Psychopathology. 2013;46(6):413–420. [DOI] [PubMed] [Google Scholar]
- 73. Kvrgic S, Cavelti M, Beck EM, Rüsch N, Vauth R. Therapeutic alliance in schizophrenia: the role of recovery orientation, self-stigma, and insight. Psychiatry Res. 2013;209(1):15–20. [DOI] [PubMed] [Google Scholar]
- 74. Hamann J, Bühner M, Rüsch N. Self-stigma and consumer participation in shared decision making in mental health services. Psychiatr Serv. 2017;68(8):783–788. [DOI] [PubMed] [Google Scholar]
- 75. Cavelti M, Kvrgic S, Beck EM, Rüsch N, Vauth R. Self-stigma and its relationship with insight, demoralization, and clinical outcome among people with schizophrenia spectrum disorders. Compr Psychiatry. 2012;53(5):468–479. [DOI] [PubMed] [Google Scholar]
- 76. Lien YJ, Chang HA, Kao YC, Tzeng NS, Lu CW, Loh CH. Insight, self-stigma and psychosocial outcomes in Schizophrenia: a structural equation modelling approach. Epidemiol Psychiatr Sci. 2018;27(2):176–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lysaker PH, Roe D, Yanos PT. Toward understanding the insight paradox: internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophr Bull. 2007;33(1):192–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Valiente C, Provencio M, Espinosa R, Duque A, Everts F. Insight in paranoia: the role of experiential avoidance and internalized stigma. Schizophr Res. 2015;164(1–3):214–220. [DOI] [PubMed] [Google Scholar]
- 79. Konsztowicz S, Lepage M. The role of illness engulfment in the association between insight and depressive symptomatology in schizophrenia. J Psychiatr Res. 2019;111:1–7. [DOI] [PubMed] [Google Scholar]
- 80. MacDougall AG, Vandermeer MR, Norman RM. Negative future self as a mediator in the relationship between insight and depression in psychotic disorders. Schizophr Res. 2015;165(1):66–69. [DOI] [PubMed] [Google Scholar]
- 81. Aukst-Margetić B, Jakšić N, Boričević Maršanić V, Jakovljević M. Harm avoidance moderates the relationship between internalized stigma and depressive symptoms in patients with schizophrenia. Psychiatry Res. 2014;219(1):92–94. [DOI] [PubMed] [Google Scholar]
- 82. Espinosa R, Valiente C, Rigabert A, Song H. Recovery style and stigma in psychosis: the healing power of integrating. Cogn Neuropsychiatry. 2016;21(2):146–155. [DOI] [PubMed] [Google Scholar]
- 83. Świtaj P, Grygiel P, Anczewska M, Wciórka J. Loneliness mediates the relationship between internalised stigma and depression among patients with psychotic disorders. Int J Soc Psychiatry. 2014;60(8):733–740. [DOI] [PubMed] [Google Scholar]
- 84. Rossi A, Galderisi S, Rocca P, et al. Personal resources and depression in schizophrenia: the role of self-esteem, resilience and internalized stigma. Psychiatry Res. 2017;256:359–364. [DOI] [PubMed] [Google Scholar]
- 85. Mashiach-Eizenberg M, Hasson-Ohayon I, Yanos PT, Lysaker PH, Roe D. Internalized stigma and quality of life among persons with severe mental illness: the mediating roles of self-esteem and hope. Psychiatry Res. 2013;208(1):15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Stip E, Caron J, Tousignant M, Lecomte Y. Suicidal ideation and schizophrenia: contribution of appraisal, stigmatization, and cognition. Can J Psychiatry. 2017;62(10):726–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Oexle N, Waldmann T, Staiger T, Xu Z, Rüsch N. Mental illness stigma and suicidality: the role of public and individual stigma. Epidemiol Psychiatr Sci. 2018;27(2):169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Shin YJ, Joo YH, Kim JH. Self-perceived cognitive deficits and their relationship with internalized stigma and quality of life in patients with schizophrenia. Neuropsychiatr Dis Treat. 2016;12:1411–1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Corrigan PW, Bink AB, Schmidt A, Jones N, Rüsch N. What is the impact of self-stigma? Loss of self-respect and the “why try” effect. J Ment Health. 2016;25(1):10–15. [DOI] [PubMed] [Google Scholar]
- 90. Cunningham KC, Lucksted A. Social cognition, internalized stigma, and recovery orientation among adults with serious mental illness. Psychiatr Rehabil J. 2017;40(4):409–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Corrigan PW, Michaels PJ, Powell K, et al. Who comes out with their mental illness and how does it help? J Nerv Ment Dis. 2016;204(3):163–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Galderisi S, Rucci P, Kirkpatrick B, et al. Interplay among psychopathologic variables, personal resources, context-related factors, and real-life functioning in individuals with schizophrenia: a network analysis. JAMA Psychiatry. 2018;75(4):396–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Dubreucq J, Plasse J, Gabayet F, et al. Self-stigma in serious mental illness and autism spectrum disorder: results from the REHABase national psychiatric rehabilitation cohort. Eur Psychiatry. 2020;63(1):e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Yildirim T, Kavak Budak F. The relationship between internalized stigma and loneliness in patients with schizophrenia. Perspect Psychiatr Care. 2020;56(1):168–174. doi: 10.1111/ppc.12399. [DOI] [PubMed] [Google Scholar]
- 95. Prasko J, Ociskova M, Grambal A, et al. Personality features, dissociation, self-stigma, hope, and the complex treatment of depressive disorder. Neuropsychiatr Dis Treat. 2016;12:2539–2552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Oexle N, Rüsch N, Viering S, et al. Self-stigma and suicidality: a longitudinal study. Eur Arch Psychiatry Clin Neurosci. 2017;267(4):359–361. [DOI] [PubMed] [Google Scholar]
- 97. Ho RWH, Chang WC, Kwong VWY, et al. Prediction of self-stigma in early psychosis: 3-Year follow-up of the randomized-controlled trial on extended early intervention. Schizophr Res. 2018;195:463–468. [DOI] [PubMed] [Google Scholar]
- 98. Ben-Zeev D, Frounfelker R, Morris SB, Corrigan PW. Predictors of self-stigma in schizophrenia: new insights using mobile technologies. J Dual Diagn. 2012;8(4):305–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Xu Z, Müller M, Lay B, et al. Involuntary hospitalization, stigma stress and suicidality: a longitudinal study. Soc Psychiatry Psychiatr Epidemiol. 2018;53(3):309–312. [DOI] [PubMed] [Google Scholar]
- 100. Lysaker PH, Davis LW, Warman DM, Strasburger A, Beattie N. Stigma, social function and symptoms in schizophrenia and schizoaffective disorder: associations across 6 months. Psychiatry Res. 2007;149(1–3):89–95. [DOI] [PubMed] [Google Scholar]
- 101. Lysaker PH, Roe D, Ringer J, Gilmore EM, Yanos PT. Change in self-stigma among persons with schizophrenia enrolled in rehabilitation: associations with self-esteem and positive and emotional discomfort symptoms. Psychol Serv. 2012;9(3):240–247. [DOI] [PubMed] [Google Scholar]
- 102. Moses T. Coping strategies and self-stigma among adolescents discharged from psychiatric hospitalization: a 6-month follow-up study. Int J Soc Psychiatry. 2015;61(2):188–197. [DOI] [PubMed] [Google Scholar]
- 103. Lysaker PH, Tunze C, Yanos PT, Roe D, Ringer J, Rand K. Relationships between stereotyped beliefs about mental illness, discrimination experiences, and distressed mood over 1 year among persons with schizophrenia enrolled in rehabilitation. Soc Psychiatry Psychiatr Epidemiol. 2012;47(6):849–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Lagger N, Amering M, Sibitz I, Gmeiner A, Schrank B. Stability and mutual prospective relationships of stereotyped beliefs about mental illness, hope and depressive symptoms among people with schizophrenia spectrum disorders. Psychiatry Res. 2018;268:484–489. [DOI] [PubMed] [Google Scholar]
- 105. Pearl RL, Forgeard MJC, Rifkin L, et al. Internalized stigma of mental illness: changes and associations with treatment outcomes. Stigma Health. 2017;2:2–15. [Google Scholar]
- 106. Sibitz I, Provaznikova K, Lipp M, Lakeman R, Amering M. The impact of recovery-oriented day clinic treatment on internalized stigma: preliminary report. Psychiatry Res. 2013;209(3):326–332. [DOI] [PubMed] [Google Scholar]
- 107. Rüsch N, Nordt C, Kawohl W, et al. Work-related discrimination and change in self-stigma among people with mental illness during supported employment. Psychiatr Serv. 2014;65(12):1496–1498. [DOI] [PubMed] [Google Scholar]
- 108. Segal SP, Silverman CJ, Temkin TL. Self-stigma and empowerment in combined-CMHA and consumer-run services: two controlled trials. Psychiatr Serv. 2013;64(10):990–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Cavelti M, Rüsch N, Vauth R. Is living with psychosis demoralizing? Insight, self-stigma, and clinical outcome among people with schizophrenia across 1 year. J Nerv Ment Dis. 2014;202(7):521–529. [DOI] [PubMed] [Google Scholar]
- 110. Lysaker PH, Yanos PT, Outcalt J, Roe D. Association of stigma, self-esteem, and symptoms with concurrent and prospective assessment of social anxiety in schizophrenia. Clin Schizophr Relat Psychoses. 2010;4(1):41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Pyle M, Stewart SL, French P, et al. Internalized stigma, emotional dysfunction and unusual experiences in young people at risk of psychosis. Early Interv Psychiatry. 2015;9(2):133–140. [DOI] [PubMed] [Google Scholar]
- 112. Ritsher JB, Phelan JC. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Res. 2004;129(3):257–265. [DOI] [PubMed] [Google Scholar]
- 113. Rüsch N, Oexle N, Thornicroft G, et al. Self-contempt as a predictor of suicidality: a longitudinal study. J Nerv Ment Dis. 2019;207(12):1056–1057. [DOI] [PubMed] [Google Scholar]
- 114. Rüsch N, Corrigan PW, Wassel A, et al. Self-stigma, group identification, perceived legitimacy of discrimination and mental health service use. Br J Psychiatry. 2009;195(6):551–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Chio FHN, Mak WWS, Chan RCH, et al. Unraveling the insight paradox: one-year longitudinal study on the relationships between insight, self-stigma, and life satisfaction among people with schizophrenia spectrum disorders. Schizophr Res. 2018;197:124–130. doi: S0920-9964(18)30034-30033. [DOI] [PubMed] [Google Scholar]
- 116. Oexle N, Müller M, Kawohl W, et al. Self-stigma as a barrier to recovery: a longitudinal study. Eur Arch Psychiatry Clin Neurosci. 2018;268(2):209–212. [DOI] [PubMed] [Google Scholar]
- 117. Campbell DG, Bonner LM, Bolkan CR, et al. stigma predicts treatment preferences and care engagement among veterans affairs primary care patients with depression. Ann Behav Med. 2016;50(4):533–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Berry C, Greenwood K. Direct and indirect associations between dysfunctional attitudes, self-stigma, hopefulness and social inclusion in young people experiencing psychosis. Schizophr Res. 2018;193:197–203. [DOI] [PubMed] [Google Scholar]
- 119. Yanos PT, Lysaker PH, Roe D. Internalized stigma as a barrier to improvement in vocational functioning among people with schizophrenia-spectrum disorders. Psychiatry Res. 2010;178(1):211–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Xu Z, Mayer B, Müller M, et al. Stigma and suicidal ideation among young people at risk of psychosis after one year. Psychiatry Res. 2016;243:219–224. [DOI] [PubMed] [Google Scholar]
- 121. Xu Z, Müller M, Heekeren K, et al. Self-labelling and stigma as predictors of attitudes towards help-seeking among people at risk of psychosis: 1-year follow-up. Eur Arch Psychiatry Clin Neurosci. 2016;266(1):79–82. [DOI] [PubMed] [Google Scholar]
- 122. Yanos PT, West ML, Gonzales L, Smith SM, Roe D, Lysaker PH. Change in internalized stigma and social functioning among persons diagnosed with severe mental illness. Psychiatry Res. 2012;200(2–3):1032–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Sibitz I, Unger A, Woppmann A, Zidek T, Amering M. Stigma resistance in patients with schizophrenia. Schizophr Bull. 2011;37(2):316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Bifftu BB, Dachew BA, Tiruneh BT. Stigma resistance among people with schizophrenia at Amanuel Mental Specialized Hospital Addis Ababa, Ethiopia: a cross-sectional institution based study. BMC Psychiatry. 2014;14:259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Mosanya TJ, Adelufosi AO, Adebowale OT, Ogunwale A, Adebayo OK. Self-stigma, quality of life and schizophrenia: an outpatient clinic survey in Nigeria. Int J Soc Psychiatry. 2014;60(4):377–386. [DOI] [PubMed] [Google Scholar]
- 126. Vidović D, Brecić P, Vilibić M, Jukić V. Insight and self-stigma in patients with schizophrenia. Acta Clin Croat. 2016;55(1):23–28. [DOI] [PubMed] [Google Scholar]
- 127. Ran MS, Zhang TM, Wong IY, et al. Internalized stigma in people with severe mental illness in rural China. Int J Soc Psychiatry. 2018;64(1):9–16. [DOI] [PubMed] [Google Scholar]
- 128. Firmin RL, Luther L, Salyers MP, Buck KD, Lysaker PH. Greater metacognition and lower fear of negative evaluation: potential factors contributing to improved stigma resistance among individuals diagnosed with schizophrenia. Isr J Psychiatry Relat Sci. 2017;54(1):50–54. [PubMed] [Google Scholar]
- 129. Kao YC, Lien YJ, Chang HA, Tzeng NS, Yeh CB, Loh CH. Stigma resistance in stable schizophrenia: the relative contributions of stereotype endorsement, self-reflection, self-esteem, and coping styles. Can J Psychiatry. 2017;62(10):735–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Nabors LM, Yanos PT, Roe D, et al. Stereotype endorsement, metacognitive capacity, and self-esteem as predictors of stigma resistance in persons with schizophrenia. Compr Psychiatry. 2014;55(4):792–798. [DOI] [PubMed] [Google Scholar]
- 131. Chan KKS, Lee CWL, Mak WWS. Mindfulness model of stigma resistance among individuals with psychiatric disorders. Mindfullness. 2018b;9:1433–1442. [Google Scholar]
- 132. Campellone TR, Caponigro JM, Kring AM. The power to resist: the relationship between power, stigma, and negative symptoms in schizophrenia. Psychiatry Res. 2014;215(2):280–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. O’Connor LK, Yanos PT, Firmin RL. Correlates and moderators of stigma resistance among people with severe mental illness. Psychiatry Res. 2018;270:198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Krendl AC, Pescosolido BA. Countries and cultural differences in the stigma of mental illness: the east–west divide. J Cross-Cult Psychol. 2020;51(2):149–167. [Google Scholar]
- 135. Alonso J, Buron A, Bruffaerts R, et al. Association of perceived stigma and mood and anxiety disorders: results from the World Mental Health Surveys. Acta Psychiatr Scand. 2008;118(4):305–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Rose D, Willis R, Brohan E, et al. Reported stigma and discrimination by people with a diagnosis of schizophrenia. Epidemiol Psychiatr Sci. 2011;20(2):193–204. [DOI] [PubMed] [Google Scholar]
- 137. Üçok A, Karadayı G, Emiroğlu B, Sartorius N. Anticipated discrimination is related to symptom severity, functionality and quality of life in schizophrenia. Psychiatry Res. 2013;209(3):333–339. [DOI] [PubMed] [Google Scholar]
- 138. Lv Y, Wolf A, Wang X. Experienced stigma and self-stigma in Chinese patients with schizophrenia. Gen Hosp Psychiatry. 2013;35(1):83–88. [DOI] [PubMed] [Google Scholar]
- 139. Li J, Guo YB, Huang YG, et al. Stigma and discrimination experienced by people with schizophrenia living in the community in Guangzhou, China. Psychiatry Res. 2017;255:225–231. [DOI] [PubMed] [Google Scholar]
- 140. Yang LH, Thornicroft G, Alvarado R, Vega E, Link BG. Recent advances in cross-cultural measurement in psychiatric epidemiology: utilizing ‘what matters most’ to identify culture-specific aspects of stigma. Int J Epidemiol. 2014;43(2):494–510. [DOI] [PubMed] [Google Scholar]
- 141. Xu Z, Huang F, Kösters M, Rüsch N. Challenging mental health related stigma in China: systematic review and meta-analysis. II. Interventions among people with mental illness. Psychiatry Res. 2017;255:457–464. [DOI] [PubMed] [Google Scholar]
- 142. Special Eurobarometer n°248. Mental Well-being. 2006. https://ec.europa.eu/health/ph_information/documents/ebs_248_en.pdf. Accessed December 26, 2019.
- 143. Special Eurobarometer n°345. Mental Health. 2010. https://ec.europa.eu/commfrontoffice/publicopinion/archives/ebs/ebs_345_en.pdf. Accessed December 26, 2019.
- 144. Pescosolido BA, Medina TR, Martin JK, Long JS. The “backbone” of stigma: identifying the global core of public prejudice associated with mental illness. Am J Public Health. 2013;103(5):853–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Pew Research Center. Eastern and Western Europeans Differ on Importance of Religion, Views of Minorities, and Key Social Issues. 2018. www.pewresearch.org. Accessed September 22, 2019.
- 146. Pew Research Center. European Public Opinion Three Decades After the Fall of Communism. 2019. www.pewresearch.org. Accessed September 22, 2019.
- 147. Gonzales L, Yanos PT, Stefancic A, Alexander MJ, Harney-Delehanty B. The role of neighborhood factors and community stigma in predicting community participation among persons with psychiatric disabilities. Psychiatr Serv. 2018;69(1):76–83. [DOI] [PubMed] [Google Scholar]
- 148. DeLuca JS, Vaccaro J, Seda J, Yanos PT. Political attitudes as predictors of the multiple dimensions of mental health stigma. Int J Soc Psychiatry. 2018;64(5):459–469. [DOI] [PubMed] [Google Scholar]
- 149. Zhang YB, Lin MC, Nonaka A, et al. Harmony, hierarchy and conservatism: a cross-cultural comparison of confucian values in China, Korea, Japan, and Taiwan. Commun Res Rep. 2005;22(2):107–115. [Google Scholar]
- 150. Yang LH, Link BG, Ben-David S, et al. Stigma related to labels and symptoms in individuals at clinical high-risk for psychosis. Schizophr Res. 2015;168(1–2):9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Mulfinger N, Müller S, Böge I, et al. Honest, Open, Proud for adolescents with mental illness: pilot randomized controlled trial. J Child Psychol Psychiatry. 2018;59(6):684–691. [DOI] [PubMed] [Google Scholar]
- 152. James TT, Kutty VR. Assessment of internalized stigma among patients with mental disorders in Thiruvananthapuram district, Kerala, India. Asia Pac J Public Health. 2015;27(4):439–449. [DOI] [PubMed] [Google Scholar]
- 153. Segalovich J, Doron A, Behrbalk P, Kurs R, Romem P. Internalization of stigma and self-esteem as it affects the capacity for intimacy among patients with schizophrenia. Arch Psychiatr Nurs. 2013;27(5):231–234. [DOI] [PubMed] [Google Scholar]
- 154. Johnson S, Lamb D, Marston L, et al. Peer-supported self-management for people discharged from a mental health crisis team: a randomised controlled trial. Lancet. 2018;392(10145):409–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Thornicroft G, Farrelly S, Szmukler G, et al. Clinical outcomes of Joint Crisis Plans to reduce compulsory treatment for people with psychosis: a randomised controlled trial. Lancet. 2013;381(9878):1634–1641. [DOI] [PubMed] [Google Scholar]
- 156. Ashcraft L, Bloss M, Anthony WA. Best practices: the development and implementation of “no force first” as a best practice. Psychiatr Serv. 2012;63(5):415–417. [DOI] [PubMed] [Google Scholar]
- 157. Meadows G, Brophy L, Shawyer F, et al. REFOCUS-PULSAR recovery-oriented practice training in specialist mental health care: a stepped-wedge cluster randomised controlled trial. Lancet Psychiatry. 2019;6(2):103–114. [DOI] [PubMed] [Google Scholar]
- 158. Browne J, Mueser KT, Meyer-Kalos P, Gottlieb JD, Estroff SE, Penn DL. The therapeutic alliance in individual resiliency training for first episode psychosis: relationship with treatment outcomes and therapy participation. J Consult Clin Psychol. 2019;87(8):734–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Green MF, Horan WP, Lee J. Nonsocial and social cognition in schizophrenia: current evidence and future directions. World Psychiatry. 2019;18(2):146–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Granholm E, Harvey PD. Social skills training for negative symptoms of schizophrenia. Schizophr Bull. 2018;44(3):472–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Xia J, Merinder LB, Belgamwar MR. Psychoeducation for schizophrenia. Cochrane Database Syst Rev. 2011;15(6):CD002831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Dubreucq J, Ycart B, Gabayet F, et al. Towards an improved access to psychiatric rehabilitation: availability and effectiveness at 1-year follow-up of psychoeducation, cognitive remediation therapy, cognitive behaviour therapy and social skills training in the FondaMental Advanced Centers of Expertise-Schizophrenia (FACE-SZ) national cohort. Eur Arch Psychiatry Clin Neurosci. 2019;269(5):599–610. [DOI] [PubMed] [Google Scholar]
- 163. Pharoah F, Mari J, Rathbone J, et al. Family intervention for schizophrenia. Cochrane Database Syst Rev. 2010;( 12):CD000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Corrigan PW, Watson AC, Miller FE. Blame, shame, and contamination: the impact of mental illness and drug dependence stigma of family members. J Fam Psychol. 2006;20:239–246. [DOI] [PubMed] [Google Scholar]
- 165. Glynn SM, Cohen AN, Niv N. New challenges in family interventions for schizophrenia. Expert Rev Neurother. 2007;7(1):33–43. [DOI] [PubMed] [Google Scholar]
- 166. Vauth R, Bull N, Schneider G. Emotions- und stigmafokussierte Angehörigenarbeit bei psychotischen Störungen. Göttingen: Hogrefe; 2009. [Google Scholar]
- 167. Hasson-Ohayon I, Pijnenborg GHM, Ben-Pazi A, Taitel S, Goldzweig G. Coping with information style and family burden: possible roles of self-stigma and hope among parents of children in a psychiatric inpatient unit. Eur Psychiatry. 2017;42:8–13. [DOI] [PubMed] [Google Scholar]
- 168. Morris E, Hippman C, Murray G, et al. Self-stigma in relatives of people with mental illness scale: development and validation. Br J Psychiatry. 2018;212(3):169–174. [DOI] [PubMed] [Google Scholar]
- 169. Grambal A, Prasko J, Kamaradova D, et al. Self-stigma in borderline personality disorder—cross-sectional comparison with schizophrenia spectrum disorder, major depressive disorder, and anxiety disorders. Neuropsychiatr Dis Treat. 2016;12:2439–2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Kamaradova D, Latalova K, Prasko J, et al. Connection between self-stigma, adherence to treatment, and discontinuation of medication. Patient Prefer Adherence. 2016;10:1289–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Szcześniak D, Kobyłko A, Wojciechowska I, Kłapciński M, Rymaszewska J. Internalized stigma and its correlates among patients with severe mental illness. Neuropsychiatr Dis Treat. 2018;14:2599–2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Sibitz I, Amering M, Unger A, et al. The impact of the social network, stigma and empowerment on the quality of life in patients with schizophrenia. Eur Psychiatry. 2011;26(1):28–33. [DOI] [PubMed] [Google Scholar]
- 173. Galderisi S, Rossi A, Rocca P, et al. The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry. 2014;13(3):275–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Rossi A, Galderisi S, Rocca P, et al. The relationships of personal resources with symptom severity and psychosocial functioning in persons with schizophrenia: results from the Italian Network for Research on Psychoses study. Eur Arch Psychiatry Clin Neurosci. 2017;267(4):285–294. [DOI] [PubMed] [Google Scholar]
- 175. Bouvet C, Bouchoux A. [Exploring the relationship between internalized stigma, insight and depression for inpatients with schizophrenia]. Encephale. 2015;41(5):435–443. [DOI] [PubMed] [Google Scholar]
- 176. Vrbova K, Prasko J, Holubova M, et al. Self-stigma and schizophrenia: a cross-sectional study. Neuropsychiatr Dis Treat. 2016;12:3011–3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Surmann M, Gruchalla LV, Falke S, et al. The importance of strengthening competence and control beliefs in patients with psychosis to reduce treatment hindering self-stigmatization. Psychiatry Res. 2017;255:314–320. [DOI] [PubMed] [Google Scholar]
- 178. Holubova M, Prasko J, Matousek S, et al. Comparison of self-stigma and quality of life in patients with depressive disorders and schizophrenia spectrum disorders—a cross-sectional study. Neuropsychiatr Dis Treat. 2016;12:3021–3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Uhlmann C, Kaehler J, Harris MS, Unser J, Arolt V, Lencer R. Negative impact of self-stigmatization on attitude toward medication adherence in patients with psychosis. J Psychiatr Pract. 2014;20(5):405–410. [DOI] [PubMed] [Google Scholar]
- 180. Post F, Pardeller S, Frajo-Apor B, et al. Quality of life in stabilized outpatients with bipolar I disorder: associations with resilience, internalized stigma, and residual symptoms. J Affect Disord. 2018;238:399–404. [DOI] [PubMed] [Google Scholar]
- 181. Quenneville AF, Badoud D, Nicastro R, et al. Internalized stigmatization in borderline personality disorder and attention deficit hyperactivity disorder in comparison to bipolar disorder. J Affect Disord. 2020;262:317–322. [DOI] [PubMed] [Google Scholar]
- 182. Lanfredi M, Zoppei S, Ferrari C, et al. Self-stigma as a mediator between social capital and empowerment among people with major depressive disorder in Europe: the ASPEN study. Eur Psychiatry. 2015;30(1):58–64. [DOI] [PubMed] [Google Scholar]
- 183. Ociskova M, Prasko J, Kamaradova D, Grambal A, Sigmundova Z. Individual correlates of self-stigma in patients with anxiety disorders with and without comorbidities. Neuropsychiatr Dis Treat. 2015;11:1767–1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Moritz S, Spirandelli K, Happach I, Lion D, Berna F. Dysfunction by disclosure? Stereotype threat as a source of secondary neurocognitive malperformance in obsessive-compulsive disorder. J Int Neuropsychol Soc. 2018;24(6):584–592. [DOI] [PubMed] [Google Scholar]
- 185. Boyd JE, Juanamarga J, Hashemi P. Stigma of taking psychiatric medications among psychiatric outpatient veterans. Psychiatr Rehabil J. 2015;38(2):132–134. [DOI] [PubMed] [Google Scholar]
- 186. Drapalski AL, Lucksted A, Perrin PB, et al. A model of internalized stigma and its effects on people with mental illness. Psychiatr Serv. 2013;64(3):264–269. [DOI] [PubMed] [Google Scholar]
- 187. Chronister J, Chou CC, Liao HY. The role of stigma coping and social support in mediating the effect of societal stigma on internalized stigma, mental health recovery, and quality of life among people with serious mental illness. J community psychol 2013;41:582–600. [Google Scholar]
- 188. Kira IA, Ramaswamy V, Lewandowski L, Mohanesh J, Abdul-Khalek H. Psychometric assessment of the Arabic version of the Internalized Stigma of Mental Illness (ISMI) measure in a refugee population. Transcult Psychiatry. 2015;52(5):636–658. [DOI] [PubMed] [Google Scholar]
- 189. Tomar N, Brinkley-Rubinstein L, Ghezzi MA, Van Deinse TB, Burgin S, Cuddeback GS. Internalized stigma and its correlates among justice-involved individuals with mental illness. Int J Ment Health. 2019;49(20):1–11. doi: 10.1080/00207411.2019.1703358 [DOI] [Google Scholar]
- 190. Jahn DR, Leith J, Muralidharan A, et al. The influence of experiences of stigma on recovery: mediating roles of internalized stigma, self-esteem, and self-efficacy. Psychiatr Rehabil J. 2020;43(2):97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Villotti P, Corbière M, Dewa CS, et al. A serial mediation model of workplace social support on work productivity: the role of self-stigma and job tenure self-efficacy in people with severe mental disorders. Disabil Rehabil. 2018;40(26):3113–3119. [DOI] [PubMed] [Google Scholar]
- 192. Firmin RL, Lysaker PH, Luther L, et al. Internalized stigma in adults with early phase versus prolonged psychosis. Early Interv Psychiatry. 2019;13(4):745–751. [DOI] [PubMed] [Google Scholar]
- 193. Link BG, Wells J, Phelan JC, Yang L. Understanding the importance of “symbolic interaction stigma”: how expectations about the reactions of others adds to the burden of mental illness stigma. Psychiatr Rehabil J. 2015;38(2):117–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Bassirnia A, Briggs J, Kopeykina I, Mednick A, Yaseen Z, Galynker I. Relationship between personality traits and perceived internalized stigma in bipolar patients and their treatment partners. Psychiatry Res. 2015;230(2):436–440. [DOI] [PubMed] [Google Scholar]
- 195. Hill K, Startup M. The relationship between internalized stigma, negative symptoms and social functioning in schizophrenia: the mediating role of self-efficacy. Psychiatry Res. 2013;206(2–3):151–157. [DOI] [PubMed] [Google Scholar]
- 196. Grover S, Avasthi A, Singh A, et al. Stigma experienced by patients with severe mental disorders: a nationwide multicentric study from India. Psychiatry Res. 2017;257:550–558. [DOI] [PubMed] [Google Scholar]
- 197. Maharjan S, Panthee B. Prevalence of self-stigma and its association with self-esteem among psychiatric patients in a Nepalese teaching hospital: a cross-sectional study. BMC Psychiatry. 2019;19(1):347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Singh A, Mattoo SK, Grover S. Stigma and its correlates in patients with schizophrenia attending a general hospital psychiatric unit. Indian J Psychiatry. 2016;58(3):291–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Pal A, Sharan P, Chadda RK. Internalized stigma and its impact in Indian outpatients with bipolar disorder. Psychiatry Res. 2017;258:158–165. [DOI] [PubMed] [Google Scholar]
- 200. Grover S, Hazari N, Aneja J, Chakrabarti S, Avasthi A. Stigma and its correlates among patients with bipolar disorder: a study from a tertiary care hospital of North India. Psychiatry Res. 2016;244:109–116. [DOI] [PubMed] [Google Scholar]
- 201. Sahoo S, Grover S, Malhotra R, Avasthi A. Internalized stigma experienced by patients with first-episode depression: a study from a tertiary care center. Indian J Soc Psychiatry. 2018;34:21–29. [Google Scholar]
- 202. Picco L, Pang S, Lau YW, et al. Internalized stigma among psychiatric outpatients: associations with quality of life, functioning, hope and self-esteem. Psychiatry Res. 2016;246:500–506. [DOI] [PubMed] [Google Scholar]
- 203. Pribadi T, Lin EC, Chen PS, Lee SK, Fitryasari R, Chen CH. Factors associated with internalized stigma for Indonesian individuals diagnosed with schizophrenia in a community setting. J Psychiatr Ment Health Nurs. 2020;27(5):584–594. [DOI] [PubMed] [Google Scholar]
- 204. Kim EY, Jang MH. The mediating effects of self-esteem and resilience on the relationship between internalized stigma and quality of life in people with schizophrenia. Asian Nurs Res (Korean Soc Nurs Sci). 2019;13(4):257–263. [DOI] [PubMed] [Google Scholar]
- 205. Lu Y, Wang X. Correlation between insight and internalized stigma in patients with schizophrenia. Shanghai Arch Psychiatry. 2012;24(2):91–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Park K, MinHwa L, Seo M. The impact of self-stigma on self-esteem among persons with different mental disorders. Int J Soc Psychiatry. 2019;65(7–8):558–565. [DOI] [PubMed] [Google Scholar]
- 207. Woon LS, Khoo SI, Baharudin A, Midin M. Association between insight and internalized stigma and other clinical factors among patients with depression: a cross-sectional study. Indian J Psychiatry. 2020;62(2):186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Ghanean H, Nojomi M, Jacobsson L. Internalized stigma of mental illness in Tehran, Iran. Stigma Research and Action 2011;1:11–17 [Google Scholar]
- 209. Tanriverdi D, Kaplan V, Bilgin S, et al. The comparison of internalized stigmatization levels of patients with different mental disorders. J Subst Use. 2019;25(3):251–257. doi: 10.1080/14659891.2019.1675790 [DOI] [Google Scholar]
- 210. Hasson-Ohayon I, Mashiach-Eizenberg M, Lysaker PH, Roe D. Self-clarity and different clusters of insight and self-stigma in mental illness. Psychiatry Res. 2016;240:308–313. [DOI] [PubMed] [Google Scholar]
- 211. Korkmaz G, Küçük L. Internalized stigma and perceived family support in acute psychiatric in-patient units. Arch Psychiatr Nurs. 2016;30(1):55–61. [DOI] [PubMed] [Google Scholar]
- 212. Çapar M, Kavak F. Effect of internalized stigma on functional recovery in patients with schizophrenia. Perspect Psychiatr Care. 2019;55(1):103–111. [DOI] [PubMed] [Google Scholar]
- 213. Olçun Z, Şahin Altun Ö. The correlation between schizophrenic patients’ level of internalized stigma and their level of hope. Arch Psychiatr Nurs. 2017;31(4):332–337. [DOI] [PubMed] [Google Scholar]
- 214. Yılmaz E, Okanlı A. The effect of internalized stigma on the adherence to treatment in patients with schizophrenia. Arch Psychiatr Nurs. 2015;29(5):297–301. [DOI] [PubMed] [Google Scholar]
- 215. Cerit C, Filizer A, Tural Ü, Tufan AE. Stigma: a core factor on predicting functionality in bipolar disorder. Compr Psychiatry. 2012;53(5):484–489. [DOI] [PubMed] [Google Scholar]
- 216. Sadighi G, Reza Khodaei M, Fadai F, et al. Self-stigma among people with bipolar-I disorder in Iran. Iran Rehabil J. 2015;13(1):28–32. [Google Scholar]
- 217. Adewuya AO, Owoeye AO, Erinfolami AO, Ola BA. Correlates of self-stigma among outpatients with mental illness in Lagos, Nigeria. Int J Soc Psychiatry. 2011;57(4):418–427. [DOI] [PubMed] [Google Scholar]
- 218. Asrat B, Ayenalem AE, Yimer T. Internalized stigma among patients with mental illness attending psychiatric follow-up at Dilla University Referral Hospital, Southern Ethiopia. Psychiatry J. 2018;2018:1987581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Fadipe B, Adebowale TO, Ogunwale A, et al. Internalized stigma in schizophrenia: a cross-sectional study of prevalence and predictors. Int J Cult Ment Health. 2018;11(1):1–12. doi: 10.1080/17542863.2018.1450431 [DOI] [Google Scholar]
- 220. Assefa D, Shibre T, Asher L, Fekadu A. Internalized stigma among patients with schizophrenia in Ethiopia: a cross-sectional facility-based study. BMC Psychiatry. 2012;12:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Lau YW, Picco L, Pang S, et al. Stigma resistance and its association with internalised stigma and psychosocial outcomes among psychiatric outpatients. Psychiatry Res. 2017;257:72–78. [DOI] [PubMed] [Google Scholar]
- 222. Karakaş SA, Okanlı A, Yılmaz E. The effect of internalized stigma on the self-esteem in patients with schizophrenia. Arch Psychiatr Nurs. 2016;30(6):648–652. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.