Abstract
Background:
Breakfast, which is considered as an important meal of the day, is being ignored by an increasing number of people as the pace of modern life accelerates. Although a large number of previous studies have reported the relationship between skipping breakfast and type 2 diabetes mellitus, most of them were cross-sectional studies. It remains unclear how skipping breakfast affects such specific cardio-metabolic diseases as hypertension, strokes and hypercholesterolemia.
Methods:
The protocols and reports of this meta-analysis are based on a meta-analysis of observational studies in epidemiological guidelines (MOOSE). Relevant studies were systematically retrieved from PubMed, Embase, Web of Science and the Cochrane Library, and were restricted to English from the inception to May 10, 2019. All the results were obtained by RRs, and outcomes of interests should include the occurrence of cardiovascular and metabolic diseases.
Results:
Fourteen cohort studies in total were eventually included. Compared with people having breakfast frequency≦3times/week, those with a frequency>3 times/week have reduced the risk of type 2 diabetes mellitus, obesity, Metabolic Syndrome, Low high-density lipoprotein cholesterolemia, Cardiovascular Diseases, cardiovascular Mortality, hypertension and strokes, with (RR = 0.8 [95% CI: 0.7–0.91], P = .142, I2 = 37.6%), (RR = 0.74 [95% CI: 0.59–0.94], P < .001, I2 = 89%), (RR = 0.86 [95% CI:0.75–0.99], P = .512, I2 = 0%), (RR = 0.75 [95% CI:0.61–0.93], P = .643, I2 = 0%), (RR = 0.87 [95% CI:0.81–0.93], P = .479, I2 = 0%), (RR = 0.63 [95% CI:0.51–0.78], P = .396, I2 = 0%), (RR = 0.92 [95% CI:0.86–0.98], P = .419, I2 = 0.7%), and (RR = 0.89 [95% CI:0.79–0.99], P = .238, I2 = 29%), respectively.
Conclusions:
A regular daily breakfast habit benefits the cardio-metabolism to a great extent, reducing the risk of Cardiovascular Diseases, type 2 diabetes mellitus, obesity, hypertension, strokes, Metabolic Syndrome, cardiovascular Mortality, Low high-density lipoprotein cholesterolemia, and Abdominal obesity, while it is not significantly related to hypercholesterolemia and coronary heart disease regardless of gender. Nevertheless, skipping breakfast once a week may greatly reduce the benefits of cardio-metabolism. Therefore, public institutions should promote and encourage citizens to cultivate regular daily breakfast habits.
Keywords: cardiovascular diseases, meta-analysis, metabolic diseases, mortality
1. Introduction
With the acceleration of the pace of modern life, breakfast, which is regarded as an important meal of the day, is being ignored by more and more people, which seemingly as a universal behavior, may have negative effects on your health.[1,2] There are various reasons for skipping breakfast. For office workers, they may not have enough time to eat breakfast. For students, they may lack a good breakfast habit. As for obese patients, they may have a poor appetite or must limit their energy intake. As a matter of fact, regular breakfast habits can keep us energetic in work and study. In addition, eating breakfast can increase satiety, thereby reducing overeating later in the day to restrict weight gain.[3] Recently, several studies have shown that skipping breakfast increases the risk of obesity,[4] hypertension,[5] hypercholesterolemia (HC),[6] type 2 diabetes mellitus (T2DM),[7] metabolic syndrome (MetS),[8] coronary heart disease (CHD),[9] and cardiovascular mortality (CVM).[10] Conversely, can regular breakfast habits reduce cardiovascular and metabolic diseases?
Most of the previous dietary studies have focused on dietary components and combinations,[11–14] such as dietary fat, cereals, and the Mediterranean diet patterns, while few pay attention to the effects of daily eating behavior on cardiovascular diseases (CVD) and metabolic diseases (MetD). Besides, although a large number of previous studies have revealed the relationship between skipping breakfast and diabetes, most of them were cross-sectional ones.[14–17] In this case, it is still unclear how skipping breakfast affects some other specific cardio-metabolic diseases. Therefore, the purpose of this meta-analysis is to systematically investigate the association between regular breakfast habits and cardio-metabolic diseases, and to update the epidemiological evidence so as to better serve public health and health promotion activities.
2. Methods
2.1. Literature search and study selection
The protocols and reports of this meta-analysis rely on a meta-analysis of observational studies in epidemiological guidelines (MOOSE).[18] Relevant studies were systematically retrieved (Zhi-hui and Xu) from PubMed, the Embase database and the Cochrane Library, and were restricted to English from the inception to May 10, 2019. Furthermore, the manual retrieval of the library was carried out. To ensure a comprehensive search, three sets of medical subject headings (MeSH) including “breakfast,” “cardiovascular diseases,” and “metabolic disease” were used. Generally, the Boolean operator “And” is employed between the two sets of keywords, and the “Or” is adopted within each group. Specifically, the first step was to use Boolean operator “Or” to combine the two sets of Mesh (cardiovascular diseases and metabolic diseases) and their corresponding synonyms, and then the Boolean operator “And” was applied to combine the Mesh of breakfast and its related synonyms. Besides, previous meta-analyses and systematic reviews were reviewed for comprehensive inclusion in the study. See Appendix 1 (Supplemental Digital Content) for a detailed search strategy.
According to PICOS criteria, the inclusion criteria for the study were as follows:
-
1.
The study population was the general population, aged > 18 years, with no previous history of metabolic or cardiovascular disease.
-
2.
Regular breakfast eaters as the intervention group.
-
3.
Irregular or non-breakfast eaters as the control or reference group.
-
4.
Outcomes of interests should contain the occurrence of cardiovascular and metabolic diseases.
-
5.
The study type was limited to cohort studies or randomized-controlled trials.
-
6.
Studies were provided with available maximum adjustment odds ratios (ORs), risk ratios (RRs), hazard ratios (HRs), and the corresponding 95% confidence intervals (CIs).
-
7.
Language was limited to English.
Meanwhile, the exclusion criteria were shown below:
-
1.
The study subjects were people who previously had CVD or MetD.
-
2.
The exposure of the studies was non-breakfast frequency, such as specific-ingredients in the food spectrum.
-
3.
Cross-sectional studies, reviews, case reports, conference abstracts, and letters were excluded.
-
4.
The outcomes of studies were non-cardiovascular and non-metabolic diseases.
-
5.
The related ORs, RRs or HRs and the corresponding 95% CIs of studies could not be obtained.
-
6.
The language of studies was non-English.
-
7.
For duplicated publications, the longest follow-up data or the largest number of population would be included for analysis.
2.2. Data extraction and quality assessment
The following data, like the first author, the year of publication, the country, the duration of follow-up, the mean age, females, the sample size, exposure assessment, CVD/MetD assessment, intervention (breakfast frequency), control (breakfast frequency), outcomes, and main findings, were extracted with a unified data list made by two independent reviewers (Li and Liu). Any disagreements and disputes in the process of data extraction shall be resolved through negotiation. Besides, the Newcastle-Ottawa scale (NOS)[19] was adopted to assess the quality of the study, with a total score of 9. To be specific, it is believed that studies with a NOS score over 6 stars are of high quality, while those with a NOS score below 6 stars are considered as low-quality ones.
2.3. Statistical analysis
Our primary outcomes would focus on the risk of cardiovascular and metabolic diseases, as well as specific diseases such as hypertension, type 2 diabetes mellitus, obesity, and strokes. Broadly speaking, the HR was equivalent to the RR, and was thereby directly considered to be the RR.[20] If necessary, use the following formula to convert ORs to RRs and calculate the corresponding 95% CIs. Relative risk=odds ratio/[(1 − P0) + (P0 × odds ratio)], where P0 indicated the incidence of outcomes in the unexposed group.[21] Then, convert the standard error (SE) of the RR with the following formula: SElog(relative risk) = SElog(odds ratio) × log(relative risk)/log(odds ratio).[22] In addition to that, if P0 was rare (P < .05), ignore the differences among various measures of relative risk (e.g., OR, RR, and HR).[23] All the results were shown by RRs. As the reference groups of each study were not identical, the frequency of breakfast was divided into the following five groups: ≤3 times/week, >3 times/week, 4 to 6 times/week, 0 to 6 times/week, and 7 times/week, to ensure homogeneity and effective consolidation of data. This group of one cohort 25 study was 0 to 4, and it was roughly classified as 0 to 3 for the effective combination of data. Besides that, the group with the lowest breakfast frequency was unified into the reference group through the Excel macro file made by Hamling et al[25] based on Greenland and Longnecker's theory.[26] In general, most studies reported specific breakfast frequency, but a few articles did not mention breakfast frequency. We contacted the original authors, and if relevant information was still not available, we would classify “Eats breakfast (yes) or eating breakfast” as 7 times per week and “Eats breakfast (No) or skipping breakfast” as 0 time per week. Besides, if the subject was specifically classified according to gender and age, we would tend to consider it as two studies. Statistical heterogeneity was assessed by using I2 statistics, where 25%, 50%, and 75% of I2 values represented low, medium and high heterogeneity, accordingly.[27] If I2 was ≤50%, the fixed-effect model would be adopted. Otherwise, the random effect-model would be adopted. If the confidence intervals of 95 are on one side of 1, we think there is a significant difference. Meanwhile, Begg's test was performed to evaluate the potential publication bias,[28] and subgroup and sensitivity analysis were used to explore sources of potential heterogeneity. All data analyses were conducted by Stata SE12.0 software.
2.4. Ethical statement
The data analyzed in this study were extracted from previously published studies, and therefore ethical approval was not necessary.
3. Results
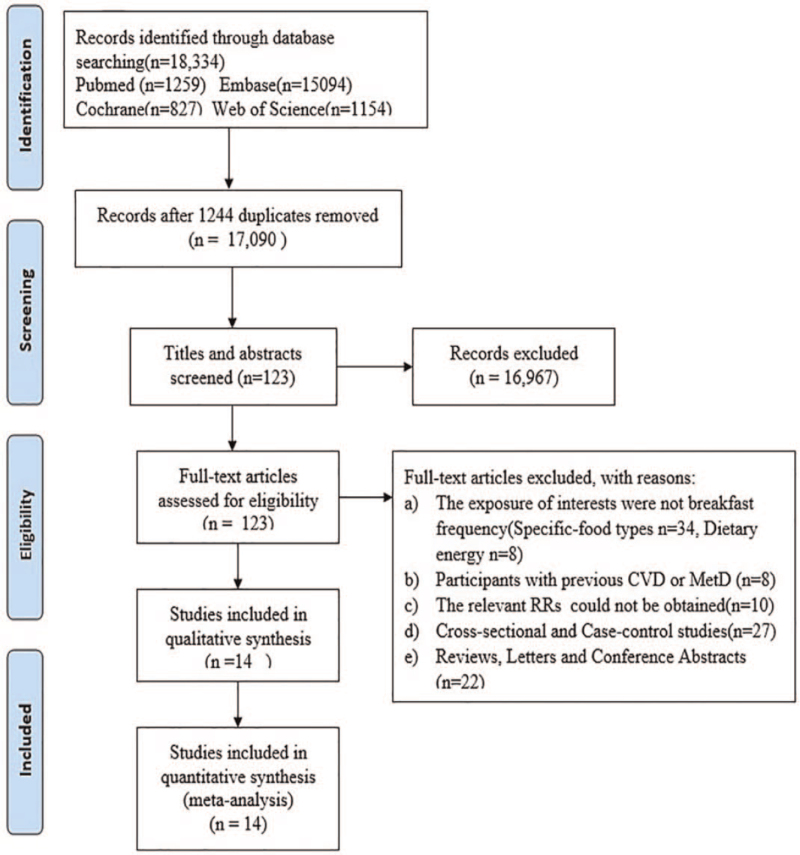
A total of 18,334 studies were identified from the four electronic databases, namely PubMed, Embase, the Cochrane Library, and Web of Science, as shown in Figure 1. No additional studies were added by manual search. Of the 18,334 studies, 17,090 were retained after 1,244 duplicated studies were excluded, and 16,976 unrelated studies were abandoned by screening titles or abstracts. After a detailed review on the full text of 123 studies, 108 studies were eliminated for the following specific reasons:
Figure 1.
The retrieval flow chart.
-
1.
The exposure of interest was not breakfast frequency (specific-food types n = 34, dietary energy n = 8).
-
2.
Participants had a history of CVD or MetD (n = 8).
-
3.
The relevant RRs could not be obtained (n = 10).
-
4.
Cross-sectional and Case–control studies were excluded (n = 27).
-
5.
Reviews, Letters, and Conference Abstracts were excluded (n = 22).
Finally, 14 cohort studies[7,9,24,29–39] were involved, and among them, 6 studies showed the relationship between breakfast frequency and T2DM; 5 studies revealed the risk of obesity; 4 studies reported the risk of hypertension; 3 studies indicated the risk of MetS and abdominal obesity, while 2 pointed out the risk of CVD, strokes, hypercholesterolemia, CVM, Low levels of high-density lipoprotein cholesterol (LHDL-c) and CHD. Table 1 displayed the detailed characteristics of the study. The quality assessment of the included studies was shown in Table 2. All the studies scored over 6 stars were featured with high quality.
Table 1.
Detailed characteristics of the 14 cohort studies included in this meta-analysis.
| Author, year | Country | Follow-up, year | Study design | Sample size, female (%) | Age, year | Exposure assessment | CVD/MetD assessment | Intervention (breakfast frequency) | Control (breakfast frequency) | Outcome | Main findings |
| Jaaskelainen et al[24] 2012 | Finland | 1986–2002 | Cohort study | 6247, 51% | 16 | Q | International Diabetes Federation paediatric definition | 7 | 0∼4 | Obesity | Among 16-year-olds, the five-meal-a-day pattern was robustly associated with reduced risks of overweight /obesity in both genders and abdominal obesity in boys. |
| Hypertension | |||||||||||
| HC | |||||||||||
| A-obesity | |||||||||||
| Sugimori et al[29] 1998 | Japan | 1976–1991 | Cohort study | 2573, 28% | 46.6 | Q | FBS≥ 110 mg/dL or DT | 1∼7 | 0 | T2DM | For females, breakfast skipping is positively associated with incidence of T2DM. |
| Uemura et al[30] 2014 | Japan | 2002–2011 | Cohort study | 4631, 22.3% | 47.6 | Q | FBG≥126 mg/dL, medical record | 1∼2 | 0 | T2DM | Breakfast skipping is positively associated with incidence of T2DM. |
| 3∼5 | |||||||||||
| 6 | |||||||||||
| 7 | |||||||||||
| Byrne et al[31] 2016 | USA | 2003–2012 | Cohort study | 10,248, 68.1% | 41.2 | Q | Concise Health Risk Assessment | 2∼3 | 0–1 | T2DM, | Top priorities for workplace health promotion should include low-fat diet, aerobic exercise, nonsmoking, and adequate sleep. |
| 4∼6 | CVD | ||||||||||
| 7 | Obesity | ||||||||||
| Stroke | |||||||||||
| Hypertension | |||||||||||
| HC | |||||||||||
| Odegaard et al[7] 2013 | USA | 1992–2011 | Cohort study | 3598, 55.7% | 32.0 | Q | BMI ≥ 30 kg/m2 | 4∼6, | 0–3 | T2DM | Daily breakfast intake is strongly associated with reduced risk of a spectrum of metabolic conditions. |
| SBP ≥ 140 mm Hg | 7 | Obesity | |||||||||
| DBP ≥ 90 mm Hg | Hypertension | ||||||||||
| NCEP-ATP III | MetS | ||||||||||
| FBG ≥ 6.99 mmol/L | A-obesity | ||||||||||
| 2 h PG ≥ 11.1 mmol/L | |||||||||||
| Cahill et al[32] 2013 | USA | 1992–2008 | Cohort study | 51,529, 0 | 58.6 | Q | Medical records or autopsy reports | 7 | 0 | CHD | Eating breakfast was associated with significantly lower CHD risk in this cohort of male health professionals. |
| Mekary et al[33] 2013 | USA | 2002–2008 | Cohort study | 121,700, 100% | 67.2 | Q | American Diabetes Association Criteria | 7 | 0–6 | T2DM | Irregular breakfast consumption was associated with a higher T2D risk in women |
| Rong et al[9] 2019 | China | 1988–2011 | Cohort study | 6550, 52% | 53.2 | Household Interview | ICD-9 | 1∼3 | 0 | CVM | Skipping breakfast was associated with a significantly increased risk of mortality from CVD. |
| ICD-10 | 4∼6 | ||||||||||
| 7 | |||||||||||
| Wennberg et al[34] 2014 | Sweden | 1981–2008 | Cohort study | 889, 52.2% | 43 | Q | International Diabetes Federation | 7 | 0 | MetS | Poor breakfast habits in adolescence predicted the metabolic syndrome in adulthood. |
| Hypertension | |||||||||||
| LHDL-c | |||||||||||
| A-obesity | |||||||||||
| Yokoyama et al[35] 2016 | Japan | 1988–2009 | Cohort study | 83,410, 59% | 40–79 | Q | ICD-10 | 7 | 0 | CVM | Our findings showed that skipping breakfast is associated with increasing risk of CVM. |
| ICD-9 | |||||||||||
| Kubota et al[36] 2016 | Japan | 1995–2010 | Cohort study | 82,772, 53.2% | 56.5 | Q | The criteria of the National Survey of Stroke | 7 | 0 | CVD | The frequency of breakfast intake was inversely associated with the risk of stroke |
| Stroke | |||||||||||
| CHD | |||||||||||
| Mekary et al[37] 2012 | USA | 1992–2008 | Cohort study | 29,206, 0% | 58.1 | Q | American Diabetes Association Criteria | 7 | 0 | T2DM | breakfast consumption was inversely associated with T2D risk in men |
| Wijtzes et al[38] 2016 | The Netherlands | 2y | Cohort study | 5913, 50.3% | 6 | Q | International Obesity Task Force | 7 | 0–6 | obesity | Breakfast skipping at age 4 years is associated with a higher percent fat mass at age 6 years |
| Kim et al[39] 2015 | Korea | 2001–2006 | Cohort study | 1228, 100% | 46.9 | Household Interview | NCEP-ATP III | 7 | 0 | MetS | Implications include the need for stronger emphasis on weight control before midlife and experiencing menopause |
A-obesity = Abdominal-obesity, CVD = Cardiovascular Diseases, CVM = cardiovascular Mortality, DBP = diastolic blood pressure, DT = diabetic therapy, FBS = fasting blood sugar, HC = Hypercholesterolemia, ICD = International Statistical Classification of Diseases, LHDL-c = Low HDL cholesterolemia, MetD = Metabolic Diseases, MetS = Metabolic Syndrome, NCEP-ATP III = National Cholesterol Education Program Adult Treatment Panel III criteria, PG = postchallenge glucose, Q = Questionnaire, SBP = systolic blood pressure.
Table 2.
Quality assessment of the 14 included studies.
| Selection | Outcome | |||||||||
| Study (author, year) | Exposed cohort | Nonexposed cohort | Ascertainment of exposure | Outcome of interest | Comparability | Assessment of outcome | Length of followup | Adequacy of follow-up | Total | |
| Jaaskelainen et al (2012) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 | |
| Sugimori et al (1998) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 7 | ||
| Uemura et al (2014) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 | |
| Byrne et al (2016) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 | |
| Odegaard et al (2013) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 7 | ||
| Cahill et al (2013) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 | |
| Mekary et al (2013) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 | |
| Rong et al (2019) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 | |
| Wennberg et al (2014) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 7 | ||
| Yokoyama et al (2016) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 | |
| Kubota et al (2016) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 | |
| Mekary et al (2012) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 | |
| Wijtzes et al (2016) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 | |
| Kim et al (2015) | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | ∗ | 8 |
1 point. Total, total score.
3.1. Meta-analysis
3.1.1. T2DM
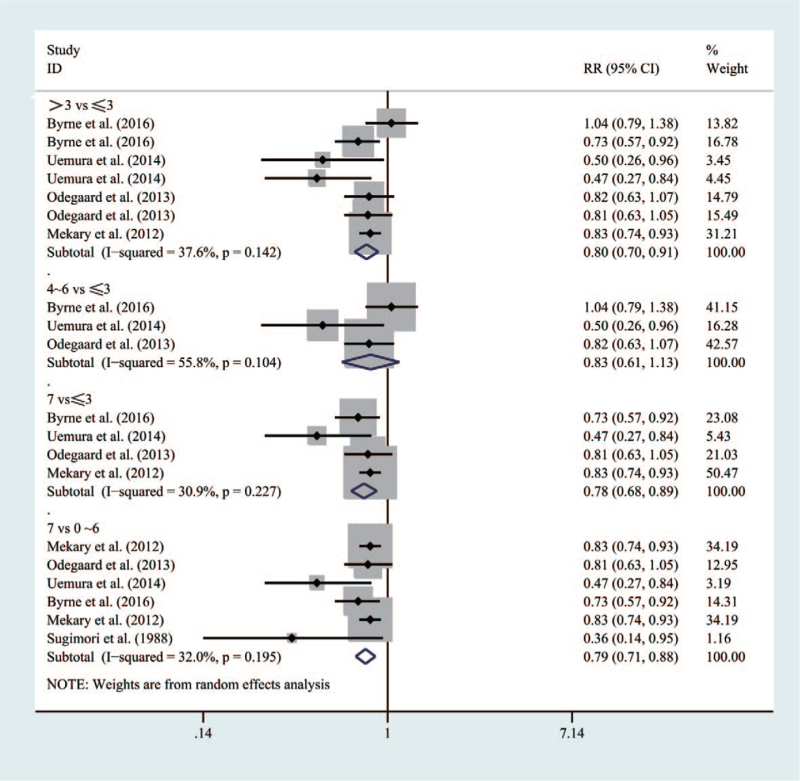
Figure 2 shows that six studies involved 171,956 participants in the current meta-analysis. Compared with people who had a breakfast frequency≤3times/week, those with the frequency>3 times/week and frequency7times/week had a lower risk of T2DM (RR = 0.8 [95% CI: 0.7–0.91], P = .142, I2 = 37.6%) and (RR = 0.78 [95% CI: 0.68–0.89], P = .227, I2 = 30.9%), respectively. Besides, compared with people who had a breakfast frequency0∼6times/week, those with a frequency7times/week would significantly decrease the risk of inducing T2DM (RR = 0.79 [95% CI: 0.71–0.88], P = .195, I2 = 32%). However, risk for T2DM of those with a breakfast frequency4 to 6times/week would not be lower than that of those with a frequency ≤ 3 times/week (RR = 0.83 [95% CI: 0.61–1.13], P = .104, I2 = 55.8%).
Figure 2.
Forest map of the relationship between breakfast frequency and the risk ofT2DM.
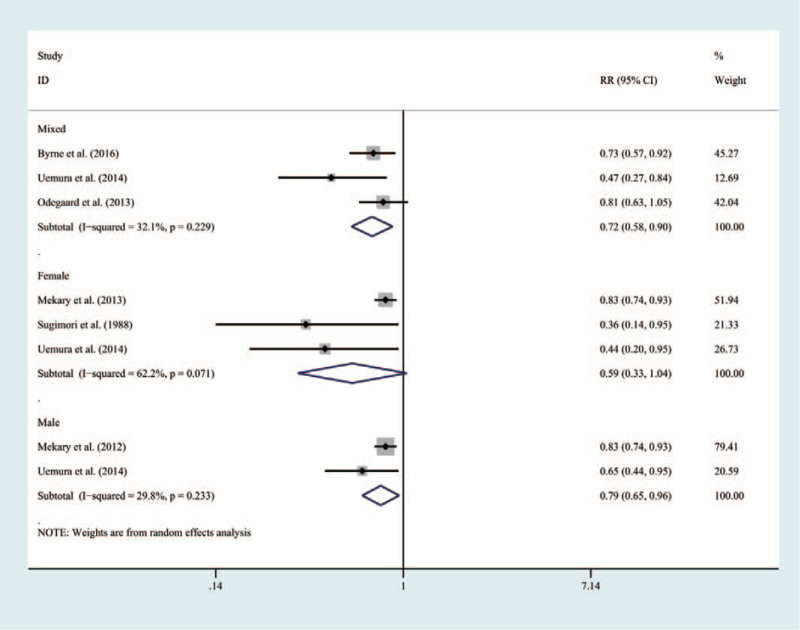
From the perspective of gender, as shown in Figure 3, the mixed population with a breakfast frequency7times/week would have an obvious lower risk for T2DM than those with a frequency≤0∼6times/week (RR = 0.72 [95% CI: 0.58–0.90], P = .229, I2 = 32.9%). Similarly, males with a breakfast frequency 7 times/week could have an obvious lower risk than those with a frequency0∼6times/week (RR = 0.79 [95% CI: 0.65–0.96], P = .233, I2 = 29.8%). However, no significant association was found in females (RR = 0.59 [95% CI: 0.33–1.04], P = .071, I2 = 62.2%).
Figure 3.
Forest map of the relationship between breakfast frequency and the risk of T2DM according to specific gender.
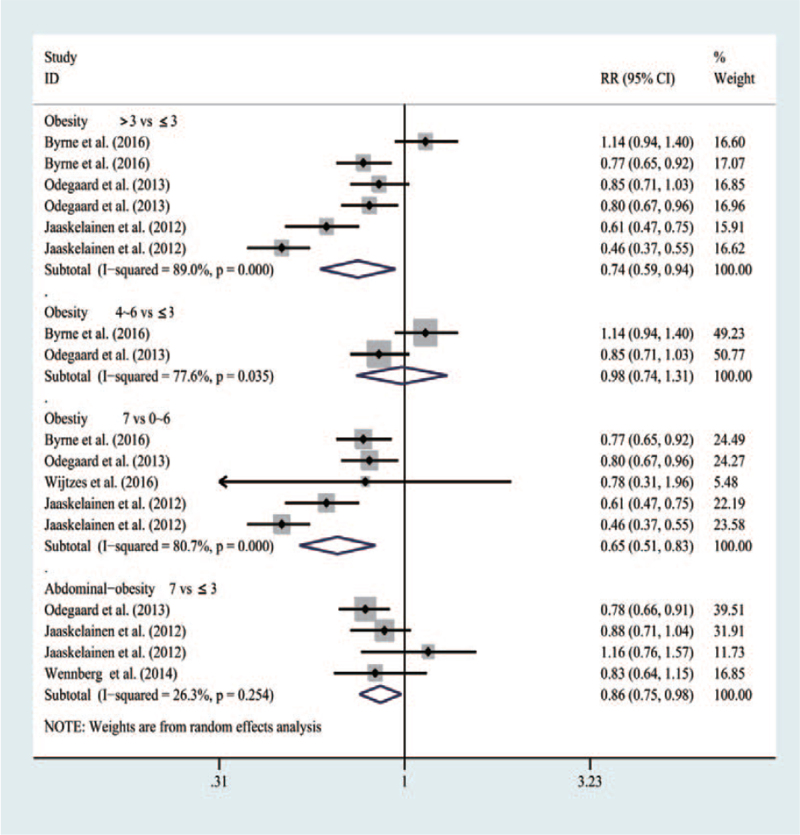
3.1.2. Obesity, abdominal obesity
According to Figure 4, in five studies, 33,494 participants participated in the meta-analysis. Compared with people whose breakfast frequency was≤3times/week, those with a frequency>3 times/week would have a decreasing risk for obesity (RR = 0.74 [95% CI: 0.59–0.94], P < .001, I2 = 89%). Besides, different from people who had a breakfast frequency of 0∼6times/week, those with a frequency7times/week could obviously be featured with a low risk of suffering from obesity (RR = 0.65 [95% CI: 0.51–0.83], P < .001, I2 = 80.7%). Nevertheless, people who had a breakfast frequency4∼6times/week would not have a lower risk of getting obesity than those with a frequency≤3times/week (RR = 0.98 [95% CI: 0.74–1.31], P = .035, I2 = 77.6%).
Figure 4.
Forest map of the relationship between breakfast frequency and the risk of Obesity, Abdominal-obesity.
It should be noted that people who had the breakfast frequency7times/week would have a lower risk of inducing abdominal obesity than those with a frequency≤3times/week (RR = 0.86 [95% CI: 0.75–0.98], P = .254, I2 = 26.3%).
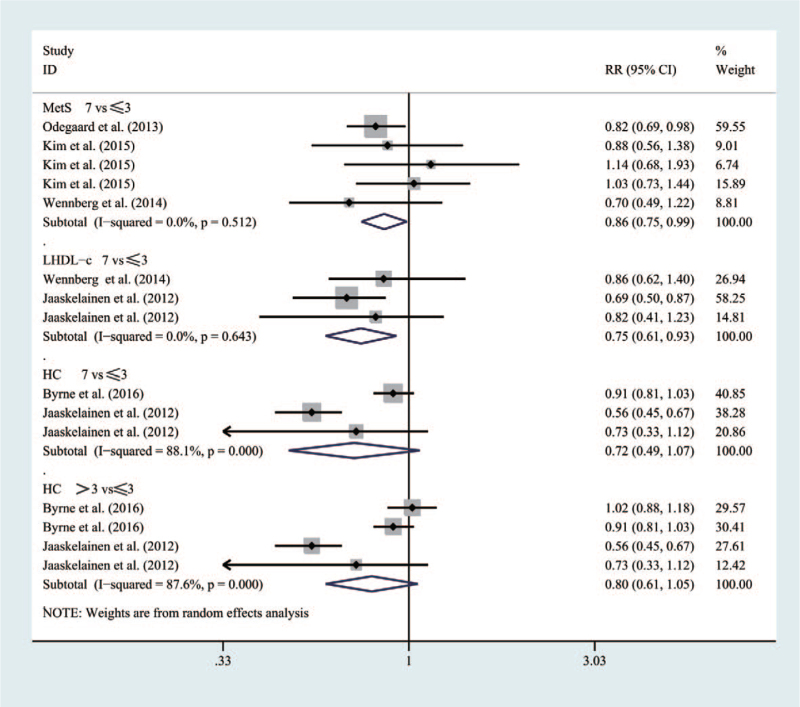
3.1.3. MetS, Low HDL Cholesterolemia (LHDL-c), HC
As shown in Figure 5, five studies included 22,210 participants in the meta-analysis. Compared with people having a breakfast frequency of ≤3times/week, those with a frequency>3 times/week would be featured with the decreasing risk of MetS (RR = 0.86 [95% CI: 0.75–0.99], P = .512, I2 = 0%) and LHDL-c (RR = 0.75 (95% CI: 0.61–0.93], P = .643, I2 = 0%) accordingly.
Figure 5.
Forest map of the relationship between breakfast frequency and the risk of MetS, LHDL-c, HC.
However, for HC, people having a breakfast frequency7times/week would not have a lower risk than those with a frequency≤3times/week (RR = 0.72 [95% CI: 0.49–1.07], P < .001, I2 = 88.1%). Similarly, people with a breakfast frequency>3 times/week could not reduce the risk of getting HC than those with a frequency≤3times/week (RR = 0.80 [95% CI: 0.61–1.05], P < .001, I2 = 87.6%).
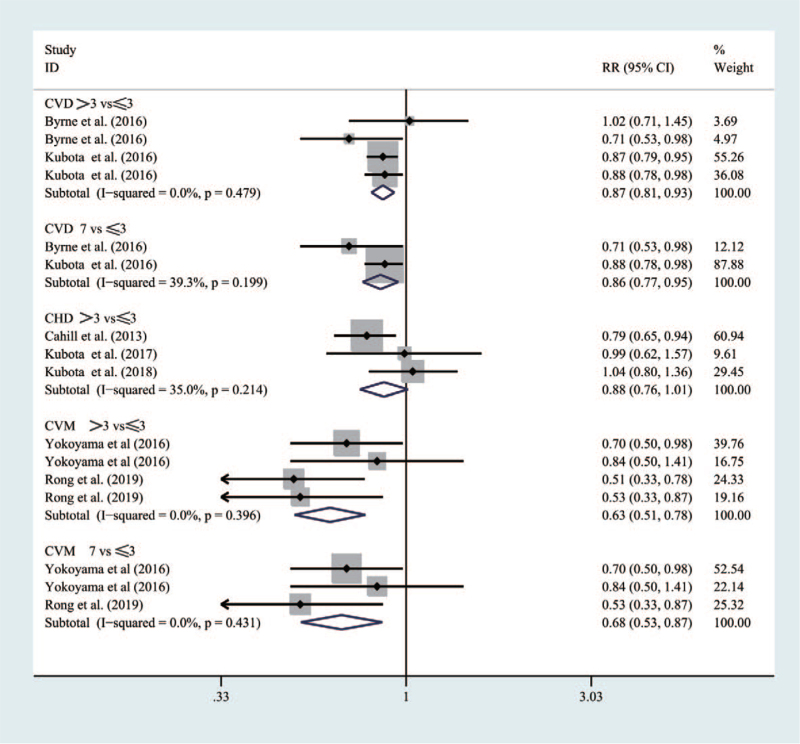
3.1.4. CVD, CHD, and CVM
Figure 6 indicated that five studies were with 160,014 participants in the meta-analysis. Compared with people having a breakfast frequency≤3times/week, those with a frequency>3 times/week would significantly reduce the risk of CVD (RR = 0.87 [95% CI: 0.81–0.93], P = .479, I2 = 0%) and CVM (RR = 0.63 [95% CI: 0.51–0.78], P = .396, I2 = 0%), respectively. Similarly, people with a breakfast frequency7times/week would have an obvious lower risk than those with a frequency≤3times/week for CVD (RR = 0.86 [95% CI: 0.77–0.95], P = .199, I2 = 39.3%) and CVM (RR = 0.68 [0.53–0.87], P = .431, I2 = 0%).
Figure 6.
Forest map of the relationship between breakfast frequency and the risk of CVD, CHD, and CVM.
However, compared with people who had a breakfast frequency≤3times/week, those with a frequency>3 times/week would not have a significant reducing risk for CHD (RR = 0.88 [95% CI: 0.76–1.01], P = .214, I2 = 35%).
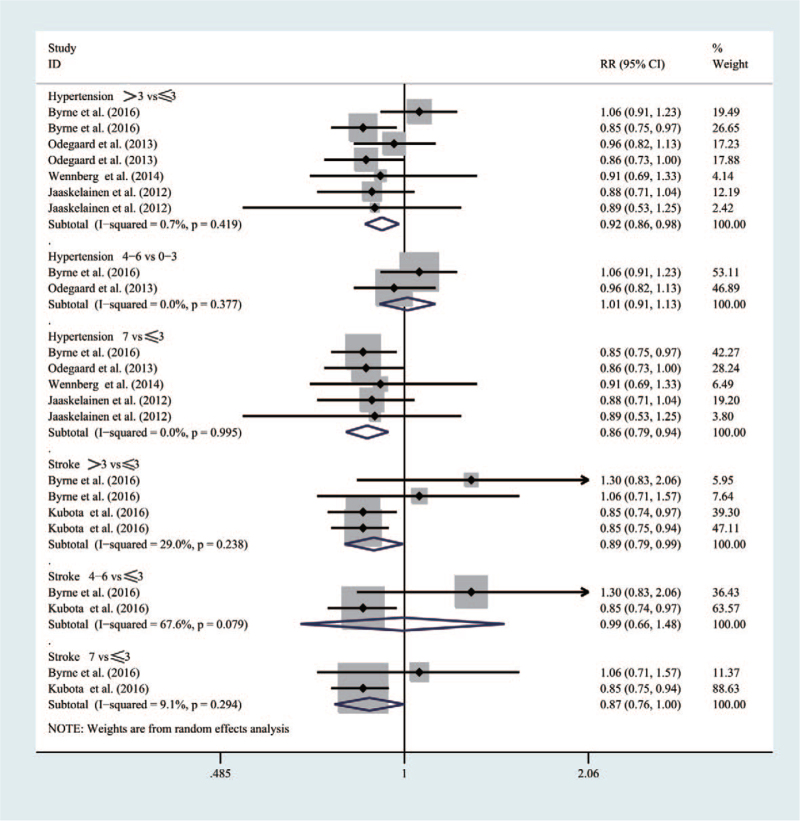
3.1.5. Hypertension, stroke
As shown in Figure 7, considering five studies, 103,754 participants were involved in the meta-analysis. Compared with people who had a breakfast frequency≤3times/week, those with a frequency>3 times/week would have a lower risk of developing hypertension (RR = 0.92 [95% CI: 0.86–0.98], P = .419, I2 = 0.7%) and strokes (RR = 0.89 [95% CI: 0.79–0.99], P = .238, I2 = 29%), respectively. Similarly, people with a breakfast frequency of 7times/week would see an obvious lower risk than those with a frequency of ≤3times/week for hypertension (RR = 0.86 [95% CI: 0.79–0.94], P = .995, I2 = 0%) and strokes (RR = 0.87 [95% CI: 0.76–1.0], P = .294, I2 = 9.9%).
Figure 7.
Forest map of the relationship between breakfast frequency and the risk of Hypertension, Stroke.
However, compared with people who had a breakfast frequency≤3times/week, those with a frequency4∼6times/week could not have a significantly reducing risk of inducing hypertension (RR = 1.01 [95% CI: 0.99–1.13], P = .377, I2 = 0%) and strokes (RR = 0.99 [95% CI: 0.66–1.48], P = .079, I2 = 67.6%).
For T2DM, Figure S1 (Supplemental Digital Content) revealed the funnel plot of the comparison between higher breakfast frequency and lower breakfast frequency. Besides, Begg's test suggested that no significant publication bias was observed (P = .373). According to Figure S2 (Supplemental Digital Content), the sensitivity analysis showed that the pooled results changed slightly after each study was removed one by one.
For strokes, the funnel plot of the comparison between higher breakfast frequency and lower breakfast frequency was displayed in Figure S3 (Supplemental Digital Content). Besides, Begg's test revealed no obvious evidence of a publication bias (P = .929). As shown in Figure S4 (Supplemental Digital Content), from sensitivity analysis, it could be found that after each study was eliminated in sequence, the summary results changed slightly.
As for other specific cardiovascular or metabolic diseases, sensitivity and subgroup analysis could not be conducted due to the limited number of current studies.
4. Discussion
In this meta-analysis, 15 cohort studies were included, with 417,093 participants being involved, and it was indicated that regular breakfast habits (7 times/week) could significantly reduce the occurrence of cardiovascular and metabolic diseases, as well as such specific-diseases as T2DM, obesity, hypertension, strokes, hypercholesterolemia, MetS and abdominal obesity. Moreover, regular breakfast habits (7 times/week) yielded the maximum potential cardio-metabolic benefits, and even skipping breakfast once per week might reduce the benefits for T2DM, obesity, hypertension and strokes to a great extent. However, there was no significant correlation between regular breakfast habits and the occurrence of hypercholesterolemia. Besides, when stratified by gender, no significant correlation can be seen between regular breakfast habits and the risk for T2DM in females.
Breakfast is taken as the most important meal of a day, and irregular breakfast habits were associated with the occurrence of various cardiovascular and metabolic diseases. Several meta-analyses[39–42] have revealed breakfast skipping was closely related to the occurrence of T2DM or obesity. However, most of these studies were cross-sectional, which might weaken the evidence value when being compared with cohort studies. Moreover, few studies have focused on the relationship between breakfast and other specific cardio-metabolic diseases. Diet patterns and physical activity go hand in hand with human health. Recently, Kwok et al[43] have comprehensively investigated the relationship between dietary components and cardiovascular mortality, and then they found many dietary components appear to be beneficial to cardiovascular disease and mortality, including fish, grains, vegetables and nuts, but tinned fruit and processed meat seem to be harmful. Musse et al[44] pointed out that within 30 days after hospital discharge, the association between skipping breakfast concomitant and late-night dinner increased the likelihood of death, reinfarction, and postinfarction angina four to five times. Simultaneously, Cheng et al[45] systematically analyzed the relationship between physical activity and cardiovascular mortality, and it was shown that leisure-time physical activity shows a linearly negative correlation with the risk of cardiovascular mortality. In a sense, the current meta-analyses have enriched previous studies.
In the long process of human evolution, regular eating not only keeps the body at a stable rhythm, but also gradually forms a specific circadian rhythm system and the internal clock, whereas it has been reported that irregular breakfast is a key factor affecting the biological clock.[46,47] Besides, the effects of breakfast frequency on cardio-metabolic diseases might be explained by the following potential mechanisms. First, irregular breakfast is deemed to be a sign of unhealthy eating patterns and lifestyles, which might be a long-term behavior from childhood to adulthood.[48,49] Recently, several studies[50–52] have indicated that irregular breakfast can significantly decrease satiety, thus leading people to eat more at lunch, which will further increase the production of hunger-related hormones that are associated with higher glucose responses and obesity. Secondly, breakfast eating behavior may have a mediating effect on subsequent metabolic outcomes. Studies conducted by Wennberg et al and Nas et al[53,54] have shown that irregular breakfast could result in inflexibility in the metabolic system, thus causing an increase in postprandial hyperglycemia and fat oxidation, while the release rhythm of insulin in the body would not be altered, thus resulting in a low inflammatory state and the impaired blood glucose regulation system. Besides, the study by Myers C et al.[55] showed that the consumption of nutritionally matched fruit smoothie at breakfast did not affect acute dietary intake, yet the effects of consuming fruit smoothie instead of cereal for breakfast on body weight and health biomarkers to be further clarified. Similarly, the study by Rosi A et al[56] showed that food patterns at lunch did not alter after consuming different categories of breakfast, and further work is needed on the effect on the amount of food consumed at lunch.
Thirdly, the study conducted by Uzhova et al[57] suggested that irregular breakfast habits might have an impact on lipid levels, increase atherosclerotic LDL levels, and further cause atherosclerosis that leaded to cardiovascular disease, which was similar to our conclusions. However, no relationship was found between breakfast and hypercholesterolemia in our meta-analysis, which might be related to the current high-energy dietary structure similar to the results of a recent national survey by Jung et al[58] suggesting that lower breakfast frequency was related with metabolic syndrome in men, yet there is no significant association in women. Recently, Yao et al[59] conducted a meta-analysis of the effect of fatty acid composition in breakfast on postprandial lipids, and the results showed that triglyceride after breakfast was not significantly altered regardless of saturated or unsaturated fatty acid composition. However, when a subgroup analysis was performed with 8 h as the cut-off, it was shown that triglyceride levels were decreased until 8 h after the ones having breakfast with saturated acid composition, while triglyceride levels were increased after 8 h after after those having breakfast with unsaturated acid composition. In addition, there may be a cumulative temporal relationship between irregular breakfast behavior and subsequent disease onset, and more research is needed to further explain these complex mechanisms. Fourthly, skipping breakfast can also affect the regulation of hypothalamic-pituitary-adrenal axis on blood pressure, further causing hypertension in the morning.[60,61]
Based on the current meta-analysis, this paper has the following advantages. First, this is the first systematic analysis on specific metabolic diseases, and all related specific diseases were reported in the original study. Secondly, four electronic databases were retrieved, and previous meta-analyses were reviewed to ensure the most comprehensive inclusion of the studies. In addition, all studies mentioned here were cohort ones, which guaranteed the evidence value. Thirdly, the included studies were featured with large sample size and high quality.
Inevitably, the present meta-analysis possesses the following limitations. First, although most studies have adjusted the maximum mixed variable, the influence of residual confounding factors could not be excluded. Secondly, due to the limited number of current studies, sensitivity and subgroup analysis could not be conducted for explaining the high heterogeneity among several studies. Thirdly, in most of the studies, questionnaires were adopted to record the frequency of breakfast. In this case, the influence of subjective factors on the results of the studies could not be ruled out. Finally, as the included studies were mainly limited to Asia, Europe and the Americas, the impact on other regions remains unknown.
5. Conclusions
It can be concluded that daily eating habits would bring the greatest cardio-metabolic benefits, reducing the risk of T2DM, obesity, hypertension, etc, yet not be significantly related to hypercholesterolemia.
Author contributions
ZH Li, LX, and RD have contributed equally to this work.
Zhi-Hui Li had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Acquisition, analysis, or interpretation of data: zhi-hui, li-jie and Wang.
Administrative, technical, or material support: zhi-hui.
Concept and design: zhi-hui, xu, and Wang.
Conceptualization: Zhi-hui Li, lei Xu.
Critical revision of the manuscript for important intellectual content: All authors.
Data curation: Zhi-hui Li, li-jie Li.
Drafting of the manuscript: All authors.
Formal analysis: Zhi-hui Li, lei Xu, rao dai, li-jie Li, haojie wang.
Funding acquisition: rao dai.
Investigation: lei Xu, li-jie Li.
Methodology: Zhi-hui Li, lei Xu, haojie wang.
Obtained funding: None.
Project administration: lei Xu.
Resources: rao dai.
Statistical analysis: Li, liu.
Supervision: rao dai, zhi-hui.
Writing – original draft: Zhi-hui Li.
Writing – review & editing: Zhi-hui Li.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: A-obesity = Abdominal obesity, CVD = Cardiovascular Diseases, CVM = cardiovascular Mortality, DBP = diastolic blood pressure, DT = diabetic therapy, FBS = fasting blood sugar, HC = Hypercholesterolemia, HDL = high-density lipoprotein, ICD = International Statistical Classification of Diseases, MetD = Metabolic Diseases, MetS = Metabolic Syndrome, NCEP-ATP III = National Cholesterol Education Program Adult Treatment Panel III criteria, PG = postchallenge glucose, Q = Questionnaire, SBP = systolic blood pressure.
How to cite this article: Li Zh, Xu L, Dai R, Li Lj, Wang Hj. Effects of regular breakfast habits on metabolic and cardiovascular diseases: A protocol for systematic review and meta-analysis. Medicine 2021;100:44(e27629).
ZHL, LX, and RD have contributed equally to this work.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental digital content is available for this article.
References
- [1].Jackson L. The most important meal of the day: why children skip breakfast and what can be done about it. Pediatric annals 2013;42:e194–7. [DOI] [PubMed] [Google Scholar]
- [2].Barton BA, Eldridge AL, Thompson D, et al. The relationship of breakfast and cereal consumption to nutrient intake and body mass index: the National Heart, Lung, and Blood Institute Growth and Health Study. J Am Diet Assoc 2005;105:1383–9. [DOI] [PubMed] [Google Scholar]
- [3].Kant AK, Graubard BI. 40-year trends in meal and snack eating behaviors of American adults. J Acad Nutr Diet 2015;115:50–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Lee TS, Kim JS, Hwang YJ, et al. Habit of eating breakfast is associated with a lower risk of hypertension. J Lifestyle Med 2016;6:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Smith KJ, Gall SL, McNaughton SA, et al. Skipping breakfast: longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am J Clin Nutr 2010;92:1316–25. [DOI] [PubMed] [Google Scholar]
- [6].Ballon A, Neuenschwander M, Schlesinger S. Breakfast skipping is associated with increased risk of type 2 diabetes among adults: a systematic review and meta-analysis of prospective cohort studies. J Nutr 2018;149:106–13. [DOI] [PubMed] [Google Scholar]
- [7].Odegaard AO, Jacobs DR, Steffen LM, et al. Breakfast frequency and development of metabolic risk. Diabetes Care 2013;36:3100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Cahill LE, Chiuve SE, Mekary RA. Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation 2013;128:337–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Rong S, Snetselaar LG, Xu G, et al. Association of skipping breakfast with cardiovascular and all-cause mortality. J Am Coll Cardiol 2019;73:2025–32. [DOI] [PubMed] [Google Scholar]
- [10].Mohammadi S, Jalaludin MY, Su TT, et al. Dietary and physical activity patterns related to cardio-metabolic health among Malaysian adolescents: a systematic review. BMC Public Health 2019;19:251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kwok CS, Gulati M, Michos ED, et al. Dietary components and risk of cardiovascular disease and all-cause mortality: a review of evidence from meta-analyses. Eur J Prev Cardiol 2019;26:1415–29. [DOI] [PubMed] [Google Scholar]
- [12].Ye EQ, Chacko SA, Chou EL, et al. Greater whole-grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. J Nutr 2012;142:1304–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Martínez-González MÁ, Hershey MS, Zazpe I, et al. Transferability of the Mediterranean diet to non-Mediterranean countries. What is and what is not the Mediterranean diet. Nutrients 2017;9:1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Donin AS, Nightingale CM, Owen CG, et al. Regular breakfast consumption and type 2 diabetes risk markers in 9- to 10-year-old children in the child heart and health study in England (CHASE): a cross-sectional analysis. PLoS Med 2014;11:e1001703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Tin SPP, Ho SY, Mak KH, et al. Lifestyle and socioeconomic correlates of breakfast skipping in Hong Kong primary 4 schoolchildren. Prev Med 2011;52:250–3. [DOI] [PubMed] [Google Scholar]
- [16].Nishiyama M, Muto T, Minakawa T, et al. The combined unhealthy behaviors of breakfast skipping and smoking are associated with the prevalence of diabetes mellitus. Tohoku J Exp Med 2009;218:259–64. [DOI] [PubMed] [Google Scholar]
- [17].Voronova N, Nikitin A, Chistiakov A, et al. Skipping breakfast is correlated with impaired fasting glucose in apparently healthy subjects. Open Med 2012;7:376–82. [Google Scholar]
- [18].Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- [19].Wells GA, Tugwell P, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa, Canada: Ottawa Hospital Research Institute; 2013. 2019. [Google Scholar]
- [20].Spruance SL, Reid JE, Grace M, et al. Hazard ratio in clinical trials. Antimicrob Agents Chemother 2004;48:2787–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zhang J, Kai FY. What's the relative risk?: A method of correcting the odds ratio in cohort studies of common outcomes[J]. JAMA 1998;280:1690–1. [DOI] [PubMed] [Google Scholar]
- [22].Ronksley PE, Brien SE, Turner BJ, et al. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Greenland S. Quantitative methods in the review of epidemiologic literature. Epidemiol Rev 1987;9:01–30. [DOI] [PubMed] [Google Scholar]
- [24].Jääskeläinen A, Schwab U, Kolehmainen M, et al. Associations of meal frequency and breakfast with obesity and metabolic syndrome traits in adolescents of Northern Finland Birth Cohort 1986. Nutr Metab Cardiovasc Dis 2013;23:1002–9. [DOI] [PubMed] [Google Scholar]
- [25].Hamling J, Lee P, Weitkunat R, et al. Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med 2008;27:954–70. [DOI] [PubMed] [Google Scholar]
- [26].Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 1992;135:1301–9. [DOI] [PubMed] [Google Scholar]
- [27].Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;1088–101. [PubMed] [Google Scholar]
- [29].Sugimori H, Miyakawa M, Yoshida K, et al. Health risk assessment for diabetes mellitus based on longitudinal analysis of MHTS database. J Med Syst 1998;22:27–32. [DOI] [PubMed] [Google Scholar]
- [30].Uemura M, Yatsuya H, Hilawe EH, et al. Breakfast skipping is positively associated with incidence of type 2 diabetes mellitus: evidence from the Aichi Workers’ Cohort Study. J Epidemiol 2015;25:351–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Byrne DW, Rolando LA, Aliyu MH, et al. Modifiable healthy lifestyle behaviors: 10-year health outcomes from a health promotion program. Am J Prev Med 2016;51:1027–37. [DOI] [PubMed] [Google Scholar]
- [32].Cahill LE, Chiuve SE, Mekary RA, et al. Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation 2013;128:337–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Mekary RA, Giovannucci E, Cahill L, et al. Eating patterns and type 2 diabetes risk in older women: breakfast consumption and eating frequency. Am J Clin Nutr 2013;98:436–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Wennberg M, Gustafsson PE, Wennberg P, et al. Poor breakfast habits in adolescence predict the metabolic syndrome in adulthood. Pub Health Nutr 2015;18:122–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Yokoyama Y, Onishi K, Hosoda T, et al. Skipping breakfast and risk of mortality from cancer, circulatory diseases and all causes: findings from the Japan Collaborative Cohort Study. Yonago Acta Med 2016;59:55. [PMC free article] [PubMed] [Google Scholar]
- [36].Kubota Y, Iso H, Sawada N, et al. Association of breakfast intake with incident stroke and coronary heart disease: the Japan Public Health Center–Based Study. Stroke 2016;47:477–81. [DOI] [PubMed] [Google Scholar]
- [37].Mekary RA, Giovannucci E, Willett WC, et al. Eating patterns and type 2 diabetes risk in men: breakfast omission, eating frequency, and snacking. Am J Clin Nutr 2012;95:1182–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Wijtzes AI, Jansen W, Bouthoorn SH, et al. Meal-skipping behaviors and body fat in 6-year-old children. J Pediatr 2016;168:118–25.e2. [DOI] [PubMed] [Google Scholar]
- [39].Kim S, Ko Y, Yi G. Role of social determinants and lifestyle on women's metabolic risk during the perimenopausal transition: results from a cohort study. Menopause 2016;23:403–9. [DOI] [PubMed] [Google Scholar]
- [40].Horikawa C, Kodama S, Yachi Y, et al. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med 2011;53:260–7. [DOI] [PubMed] [Google Scholar]
- [41].Bi H, Gan Y, Yang C, et al. Breakfast skipping and the risk of type 2 diabetes: a meta-analysis of observational studies. Pub Health Nutr 2015;18:3013–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Ballon A, Neuenschwander M, Schlesinger S. Breakfast skipping is associated with increased risk of type 2 diabetes among adults: a systematic review and meta-analysis of prospective cohort studies. J Nutr 2019;149:106–13. [DOI] [PubMed] [Google Scholar]
- [43].Kwok CS, Gulati M, Michos ED, et al. Dietary components and risk of cardiovascular disease and all-cause mortality: a review of evidence from meta-analyses [J]. Eur J Prev Cardiol 2019;26:1415–29. [DOI] [PubMed] [Google Scholar]
- [44].Musse GN, Moreira T, Kimura MA, et al. Skipping breakfast concomitant with late-night dinner eating is associated with worse outcomes following ST-segment elevation myocardial infarction. Eur J Prev Cardiol 2020;27:2311–3. [DOI] [PubMed] [Google Scholar]
- [45].Cheng W, Zhang Z, Cheng W, et al. Associations of leisure-time physical activity with cardiovascular mortality: a systematic review and meta-analysis of 44 prospective cohort studies. Eur J Prev Cardiol 2018;25:1864–72. [DOI] [PubMed] [Google Scholar]
- [46].Poggiogalle E, Jamshed H, Peterson CM. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism 2018;84:11–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Wehrens SMT, Christou S, Isherwood C, et al. Meal timing regulates the human circadian system. Curr Biol 2017;27:1768–75.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Park S, Rim SJ, Lee JH. Associations between dietary behaviours and perceived physical and mental health status among Korean adolescents. Nutr Diet 2018;75:488–93. [DOI] [PubMed] [Google Scholar]
- [49].Smith KJ, Breslin MC, McNaughton SA, et al. Skipping breakfast among Australian children and adolescents; findings from the 2011-12 National Nutrition and Physical Activity Survey. Aust N Z J Public Health 2017;41:572–8. [DOI] [PubMed] [Google Scholar]
- [50].Gwin JA, Leidy HJ. A review of the evidence surrounding the effects of breakfast consumption on mechanisms of weight management. Adv Nutr 2018;9:717–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Alwattar AY, Thyfault JP, Leidy HJ. The effect of breakfast type and frequency of consumption on glycemic response in overweight/obese late adolescent girls. Eur J Clin Nutr 2015;69:885–90. [DOI] [PubMed] [Google Scholar]
- [52].Alhussain MH, Macdonald IA, Taylor MA. Irregular meal-pattern effects on energy expenditure, metabolism, and appetite regulation: A randomized controlled trial in healthy normal-weight women. Am J Clin Nutr 2016;104:21–32. [DOI] [PubMed] [Google Scholar]
- [53].Wennberg M, Gustafsson PE, Wennberg P, et al. Poor breakfast habits in adolescence predict the metabolic syndrome in adulthood. Public Health Nutr 2015;18:122–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Nas A, Mirza N, Hägele F, et al. Impact of breakfast skipping compared with dinner skipping on regulation of energy balance and metabolic risk. Am J Clin Nutr 2017;105:1351–61. [DOI] [PubMed] [Google Scholar]
- [55].Myers C, McCartney D, Desbrow B, Khalesi S, Irwin C. Consumption of a smoothie or cereal-based breakfast: impact on thirst, hunger, appetite and subsequent dietary intake. Int J Food Sci Nutr 2021;72:123–33. [DOI] [PubMed] [Google Scholar]
- [56].Rosi A, Mena P, Scazzina F, et al. Food perception at lunchtime does not depend on the nutritional and perceived characteristics of breakfast. Int J Food Sci Nutr 2018;69:628–39. [DOI] [PubMed] [Google Scholar]
- [57].Uzhova I, Fuster V, Fernandez-Ortiz A, et al. The importance of breakfast in atherosclerosis disease: insights from the PESA study. J Am Coll Cardiol 2017;70:1833–42. [DOI] [PubMed] [Google Scholar]
- [58].Jung CH, Lee JS, Ahn HJ, et al. Association of meal frequency with metabolic syndrome in Korean adults: from the Korea National Health and Nutrition Examination Survey (KNHANES). Diabetol Metab Syndr 2017;9:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Yao Y, Pek SX, Toh DWK, Xia X, Kim JE. Effects of fatty acids composition in a breakfast meal on the postprandial lipid responses: a systematic review and meta-analysis of randomised controlled trials. Int J Food Sci Nutr 2020;71:793–803. [DOI] [PubMed] [Google Scholar]
- [60].Lee TS, Kim JS, Hwang YJ, et al. Habit of eating breakfast is associated with a lower risk of hypertension. J Lifestyle Med 2016;6:64–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Witbracht M, Keim NL, Forester S, et al. Female breakfast skippers display a disrupted cortisol rhythm and elevated blood pressure. Physiol Behav 2015;140:215–21. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.