Abstract
Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) is associated with specific coagulopathy that frequently occurs during the different phases of coronavirus disease 2019 (COVID-19) and can result in thrombotic complications and/or death. This COVID-19-associated coagulopathy (CAC) exhibits some of the features associated with thrombotic microangiopathy, particularly complement-mediated hemolytic-uremic syndrome. In some cases, due to the anti-phospholipid antibodies, CAC resembles catastrophic anti-phospholipid syndrome. In other patients, it exhibits features of hemophagocytic syndrome. CAC is mainly identified by: increases in fibrinogen, D-dimers, and von Willebrand factor (released from activated endothelial cells), consumption of a disintegrin and metalloproteinase with thrombospondin type 1 motifs, member 13 (ADAMTS13), over activated and dysregulated complement, and elevated plasma cytokine levels. CAC manifests as both major cardiovascular and/or cerebrovascular events and dysfunctional microcirculation, which leads to multiple organ damage. It is not clear whether the mainstay of COVID-19 is complement overactivation, cytokine/chemokine activation, or a combination of these activities. Available data have suggested that non-critically ill hospitalized patients should be administered full-dose heparin. In critically ill, full dose heparin treatment is discouraged due to higher mortality rate. In addition to anti-coagulation, four different host-directed therapeutic pathways have recently emerged that influence CAC: (1) Anti-von Willebrand factor monoclonal antibodies; (2) activated complement C5a inhibitors; (3) recombinant ADAMTS13; and (4) Interleukin (IL)-1 and IL-6 antibodies. Moreover, neutralizing monoclonal antibodies against the virus surface protein have been tested. However, the role of antiplatelet treatment remains unclear for patients with COVID-19.
Keywords: SARS-CoV-2, COVID-19, Coagulopathy, Microangiopathy, Endothelial dysfunction
Introduction
Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) infections, or Coronavirus disease 2019 (COVID-19), is associated with significant morbidity and mortality.1 The fatality rate was 2.3% in a non-selected population and up to 49% among critically ill patients. In 10% of fatal cases, the most important risk factor was a pre-existing cardiovascular disease.1 Additionally, a non-negligible proportion (20–30%) of patients with SARS-CoV-2 infections experience thromboembolic complications.2, 3, 4 Thrombotic or thromboembolic complications related to SARS-CoV-2 infections have been observed in arteries/arterioles, the microcirculation, and the venous system.5 , 6 With more extensive coagulation disorders, the course of the disease is expected to be more severe. The pathogenesis of SARS-CoV-2-induced coagulopathy is not completely understood.
Interestingly, many patients experience an asymptomatic or mild disease course. Additionally, patients that become seriously ill with multiple-organ failure do not always exhibit the generally accepted risk factors. Furthermore, disease severity does not correlate with the viral load.7 To improve COVID-19 management, there is an urgent need to understand the mechanisms that lead to thrombotic events. This review aimed to summarize the known pathophysiologic mechanisms underlying COVID-19-associated coagulopathy and to comment on current and emerging therapeutic options that are relevant at different stages of disease development.
Virus entry
SARS-CoV-2 enters the host via the angiotensin converting enzyme receptor 2 (ACEIIr), which is expressed in many organs (heart, lung, kidney, intestine) and some cells, including endothelial cells and hematopoietic cells, like macrophages. Although the virus most often enters the host pneumocytes,8 there is evidence that the virus can infect endothelial cells directly and cause diffuse endothelial inflammation.6 The recruitment of immune cells, either directly by the virus or immune-mediated, in the presence of locally dysregulated inflammation, can lead to diffuse endothelial activation and dysfunction.6 Activated endothelial cells express different communication glycoproteins and release high numbers of ultra-large von Willebrand factor (vWF) multimers from Weibel-Palade bodies.9
Microcirculation damage
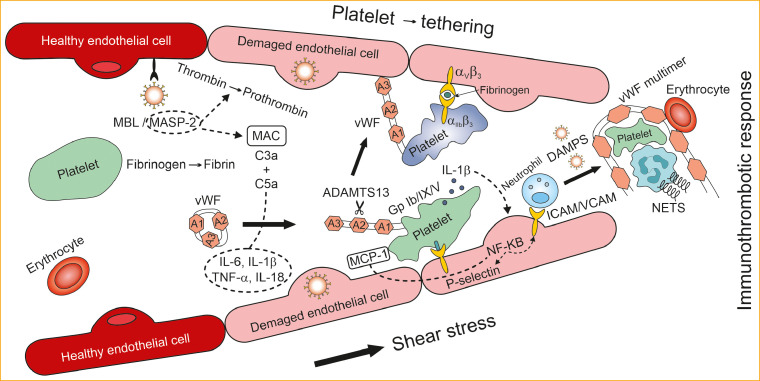
Under normal circumstances, platelets, leukocytes, and erythrocytes flow in intact vessels, together with vWF. However, vWFs do not bind to any blood elements10 , 11; even though platelets express two glycoprotein (GP) receptors capable of binding vWF: the Ib/IX/V complex and αIIbβ3 integrin. Indeed, vWF only interacts with αIIbβ3 integrin after conformational changes occur in activated platelets, and vWF binding to GP Ib/IX/V is probably regulated by non-linear flow in arterioles and capillary beds.12 , 13 Capillary beds and arterioles cause shear stress, which leads to a transitional change in vWF where vWF unfolds from a globular structure and assumes an extended chain structure.13 , 14 In the extended vWF conformation, binding sites are exposed for collagen, GP Ib/IX/V, and a disintegrin and metalloproteinase with thrombospondin type 1 motifs, member 13 (ADAMTS13).13 Long strands of vWF multimers are very effective in attracting and binding platelets. This activity leads to an obstruction in the microcirculation, which results in tissue ischemia and organ injury (Fig. 1 ).
Figure 1.
Pathways leading to immunothrombotic response.
Abbreviations: ADAMTS13: A Disintegrin And Metalloproteinase with a ThromboSpondin type 1 motif, member 13; A1–A3: domains of von Willebrand factor; DAMPS: danger-associated molecular patterns; IL: interleukin; Gp: glycoprotein; TNF: tumor necrosis factor; ICAM: intercellular adhesion molecule; MAC: membrane attack complex; MBL: mannose binding lectin; MASP: MBL associated protease; NF-KB: nuclear factor kappa-light-chain-enhancer of activated B cells; NETs: neutrophile extracellular traps; VCAM: vascular cell adhesion molecule; vWF: von Willebrand factor.
A functional imbalance in vWF multimer sizes can lead to either microcirculation bleeding or thrombosis. Both the size and the platelet-tethering function of vWF multimers are regulated by ADAMTS13, a plasma metalloproteinase.15 In turn, ADAMTS13 activity is not controlled by inhibitors, but by conformational changes in its substrate.15 Endothelium-bound vWF interacts with platelets by binding to GP Ib/IX/V. Then, in an environment with elevated shear forces, this binding results in the aggregation of vWF multimers and platelets. GP Ib/IX/V is connected to the platelet cytoskeleton; consequently, vWF binding influences the platelet shape.16 Nonetheless, the interaction between platelet GP Ib/IX/V and vWF only produces weak intracellular signaling, with limited activation of αIIbβ3 integrin, which orchestrates the platelet conformational change.17 Only activated αIIbβ3 integrin is capable of binding fibronectin, fibrinogen, and vWF, which leads to platelet aggregation and the generation and stabilization of a thrombus in rapid blood flow conditions.18 Thus, it is highly questionable whether prophylactic antiplatelet treatment would be effective in this scenario.
Platelets isolated from patients with COVID-19 exhibited reduced procoagulant properties compared to platelets from healthy volunteers. For example, after dual stimulation with both thrombin and convulxin, COVID-19 platelets showed reduced mitochondrial depolarization and a reduced abundance of phosphatidylserine molecules exposed on the surface.19 Platelets also play important roles in inflammation-induced thrombosis; in particular, they support the generation of thrombin.19 Mouse platelets that could not generate cyclophylin D had reduced procoagulant activity, and thus, they mimicked platelets from patients with COVID-19. After pulmonary microvascular thrombosis was induced, mice deficient in cyclophylin D showed increased mortality compared to mice that expressed wild-type cyclophylin D.19
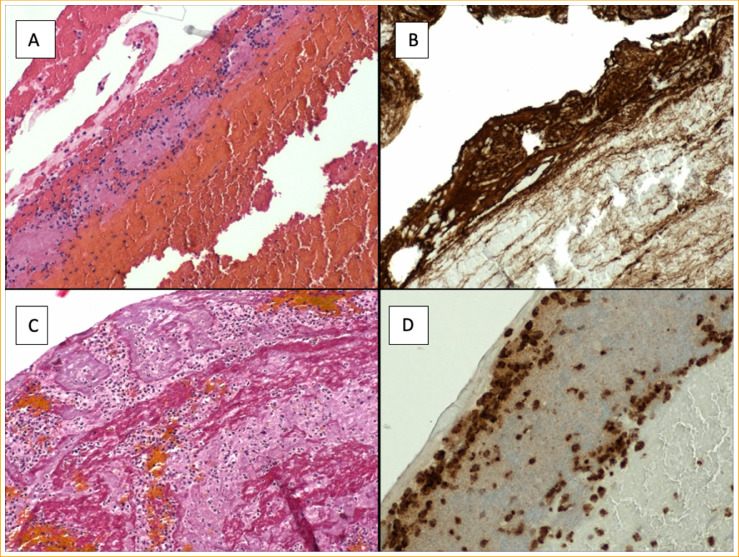
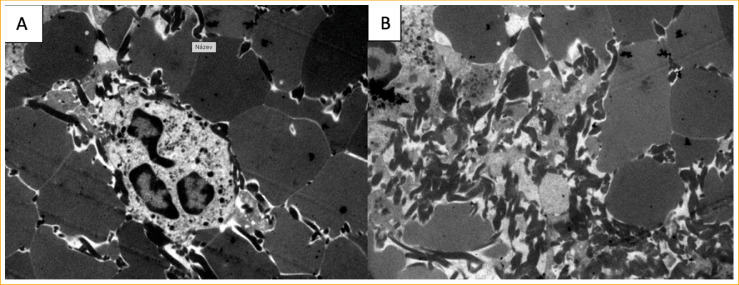
Neutrophil extracellular traps (NETs) and platelets accumulate in the lung microvasculature of patients with COVID-19. NETs are believed to contribute to the development of acute respiratory distress syndrome (ARDS).20 In patients with COVID-19, intravascular pulmonary thrombosis occurs concomitantly with ARDS and mortality.21 Platelets from patients with COVID-19 exhibit hyperreactivity to agonist stimuli and elevated interactions with leukocytes.22 When neutrophils are trapped in vWF multimers in the microcirculation, NETs develop.22 From our own experience with cerebrovascular thrombi, COVID-related thrombi are rich in neutrophile elements, deploy more fibrin strands and vWF is not only on the surface but dispersely in thrombi (for more details see Figure 2, Figure 3 ).
Figure 2.
Thrombus extracted from COVID-19 patient, histopathology (100x, Olympus BX 43). (A) Hematoxylin-eosin staining, thrombus with fibrin deposition and neutrophiles. (B) vWF staining, large deposition of vWf on the thrombus surface. (C) CARSTAIRS staining (fibrin-aimed staining), polymorphonuclears, neutrophiles, monocytes with large fibrin content. (D) CD68 (cluster of differentiation, protein highly expressed by monocyte lineage) staining with neutrophiles on the thrombus surface.
Figure 3.
COVID-19 thrombus electron microscopy - (TEM, Jeol JEM 12 EX). (A) Polyhedrocytes with neutrophile in the center. (B) deposition of large amount of fibrin between neutrophiles, polyhedrocytes at the periphery in detailed view- high magnfication. Polyhedrocytes – deformated erytrocytes (cubic deformation with compression).
The cumulative incidence of SARS-CoV-2 infection in patients with congenital blood disorders (CBD) was 1.73% from a small survey, and the course of the disease was mild.23 We may speculate that a severe hypocoagulation state (i.e., lower vWF/ADAMTS 13 ratio) may protect against COVID-19 associated hypercoagulability state. There is scarce evidence that patients with CBD, affecting 0.1 to 1% of the total population, appear to be less affected by COVID-19 infection.24
Thus, a dysregulation of the platelet coagulation response may increase the susceptibility to thrombotic complications in patients with COVID-19. The dynamic functional changes in platelets, often conflicting, may contribute to an increased susceptibility to thrombotic and/or thrombo-hemorrhagic complications in patients with COVID-19.
The complement theory
Intracellular pathogens, like viruses, must penetrate the mucosa/respiration epithelium and disseminate through the extracellular fluid.25 The humoral part of innate and adaptive immunity responses includes the heat-labile complement system and antigen-specific antibodies, respectively, and both provide a variety of reactions against multiple pathogens. Antibodies attach to virus particles and are carried into the cell with the virus. There, the antibodies act as danger-associated molecular patterns (DAMP) to activate an innate immune reaction, the coagulation cascade, and the release of cytokines/chemokines to stop replication of the virus (Fig. 1).26
Complement comprises of more than 40 proteins, both membrane-bound and soluble. The main function of complement is to opsonize pathogens and induce the innate immunity response, which leads to the elimination of pathogens.27 Generally, complement can be activated through three pathways: (1) the classical (antibody-directed) pathway; (2) the lectin (mannan-binding lectin or ficolin-directed) pathway; and (3) the alternative, spontaneous pathway, which leads to the covalent deposition of C3b on the pathogen surface for macrophage targeting.25 The deposition of C3b on the pathogen surface prevents receptor engagement, acts as an opsonin, and cleaves C5 to C5a and C5b, which is a cofactor for the assembly of the lytic membrane attack complex (MAC).25 , 28 All three complement activation pathways converge to form C3-convertase, which releases C3a and C3b, and subsequently, C3b forms C5-convertase.28 Moreover C3a, C4a, and C5a are potent chemotaxins and anaphylatoxins that induce inflammation and destroy invading pathogens.28
Proteins encoded by SARS-CoV-2 are released into the blood stream after the infected cell dies. These proteins may activate complement, which leads to both small (microangiopathy) and great vessel involvement (pulmonary or systemic embolism). One mechanism might be the interaction between N-protein and mannose-binding lectin-associated serine protease 2, which results in (1) the generation of the terminal complex (i.e., the C5b-9, membrane attack protein) and (2) the release of anaphylatoxins, C3a and C5a, which leads to the production of proinflammatory cytokines, like interleukin (IL)-6, IL-1ß, tumor necrosis factor (TNF)-α, IL-18, and interferon gama.29 In general, recruiting leucocytes and activating platelets and endothelial cells with the potent biological effectors, C3a and C5a, might stimulate an immunothrombotic response in patients with COVID-19. C5a triggers the activation of platelets and the release of prothrombotic factors from platelets. C5a also induces the expression of tissue factor (TF) in monocytes and endothelial cells. Subsequently, TF acts as initiator of coagulation. In addition, C5a suppresses the expression of natural anticoagulant proteins.30 Furthermore, C5a induces the expression of P-selectin (a C3b receptor) and enhances the assembly of C3/C5 convertases on the surface of platelets.31 Moreover, the principal complement-induced procoagulant factors, thrombin and TF, provide feedback, which amplifies complement activation, and thus, escalates the tissue damage process.32 The interplay between the complement and coagulation pathways is bidirectional.28
Cheng et al identified elevated C3 plasma level at admission as an independent risk factor for developing severe COVID-19 infection among younger patients with a median age of 47 years.33 A different group from Wuhan demonstrated lower C3 plasma level and higher D-dimer level as a higher risk factor for in-hospital death.34 These conflicting observations may be associated with different times of blood sampling resulting in the capture of different levels of development of CAC.
Patients with atypical hemolytic-uremic syndrome or paroxysmal nocturnal hemoglobinuria exhibit excess complement activation, due to loss-of-function or gain-of-function gene mutations in several regulatory proteins (e.g., thrombomodulin, factor H, C4bBP, CD46, CD55, CD59).35, 36, 37 This excess complement activation might explain why patients with these conditions display similar reactions to COVID-19. Moreover, the virus surface is known to have procoagulant activity, similar to historic descriptions of herpesviruses.38 , 39 Additionally, the Middle East respiratory syndrome (MERS) was associated with a high incidence of venous thromboembolism.40 Transgenic overexpression of the receptor responsible for virus entry (MERS-CoV) into the cell in mice resulted in progressive pulmonary damage, with diffuse microvascular thrombosis.41 Moreover, intranasal administration of MERS-CoV in mice led to pulmonary tissue damage, with C5b-9 deposition and increases in plasma C5a levels.42 Thus, thrombosis in both small and large vessels is apparently a common characteristic of betacoronaviruses.28 Therefore, the complement system might play a causative role in virus-related organ damage.
The role of anticoagulation treatments
Among patients with COVID-19, one of the most common laboratory findings is an elevation in plasma D-dimer levels.43 Unsurprisingly, older patients and patients with co-morbidities are more likely to die from COVID-19 infections, and both groups have elevated D-dimer levels. In a large cohort of 1099 patients with confirmed COVID-19 infections in China, 46.4% had D-dimers ≥0.5 mg/L, and of those, 60% had a severe case of the illness.44 In a trial by Tang et al., markedly elevated D-dimers were identified as a predictor of mortality in patients with COVID-19.2 Similarly, Huang et al. observed elevated d-dimer levels in patients that required further critical care.45 When plasma D-dimer levels increase in the absence of any severe symptoms, it is a sign of elevated thrombin generation, and thus, D-dimer levels also serve as a marker of the prothrombotic state.43 Of note, the prothrombin time (PT) at admission was rather modestly prolonged in patients that required critical care and in non-survivors. 2
Chronic therapeutic anticoagulation treatment at the time of infection may protect against thrombotic complications and reduce disease severity.46 Indeed, multi-organ failure in patients with sepsis occurred more often in patients that developed a coagulopathy.43 Thus, inhibiting thrombin generation may reduce mortality in patients with COVID-19.47 According to the International Society for Thrombosis and Hemostasis guidelines, prophylactic doses of low-molecular-weight heparin (LMWH) is recommended for all patients that require hospital admission due to a COVID-19 infection, irrespective of disease severity.43 However, the main question to address is whether a therapeutic dose of anticoagulation treatment should be given to all patients or whether it should only be given to pre-specified subgroups; i.e., based on the plasma D-dimer level or the clinical disease severity (severe disease indications: high-flow oxygen treatment, mechanical ventilation, and an inflammatory response). Of note, in a New York retrospective cohort of 2773 patients, 395 had received mechanical ventilation. Among those patients, a full-dose anticoagulation treatment reduced the mortality to 29.1%, compared to 62.7% among those without the treatment.48
Full-dose anticoagulation treatment with heparin reduced the need for organ support and reduced mortality better than the usual prophylactic dose given to hospitalized patients that were moderately ill, based on data from the multiplatform randomized trials (ATTAC, ACTIVE-4a, REMAP-CAP).49 , 50 In contrast, among patients with severe disease that required intensive care unit admission, full-dose anticoagulation treatment with heparin is discouraged due to the higher risk of mortality and bleeding in this subgroup of patients.49 , 50 In addition, full dose enoxaparin or rivaroxaban followed by rivaroxaban to day 30 did not improve clinical outcomes. Moreover, it increased bleeding risk compared with prophylactic anticoagulation in hospitalized patients with elevated D-dimers.51 Different outcomes (for details see Table 1 )48, 49, 50, 51, 52, 53, 54 of prophylactic vs. full dose anticoagulation in patients with COVID-19 may be caused by various disease severity, comorbidities/overall risk profile, co-medication, anticoagulation regimen/type, patient age, male to female ratio and sample size. Given the conflicting results of therapeutic vs. prophylactic anticoagulation treatment in different subgroups of patients with various COVID-19 disease severity, more trials have to be conducted.
Table 1.
Therapeutic v.s. prophylactic anticoagulation treatment in hospitalized COVID-19.
| Study by | Patient count (N) | Age | Male % | Study type | Disease severity | Therapeutic dose AC | Prophylactic dose AC | Mortality rate* |
|---|---|---|---|---|---|---|---|---|
| Paranjpe et al.48 | 2773 | N/A | N/A | Retrospective/obsevational | Various | 28% | N/A | 22.5%† |
| Lawler et al. 49 | 2219 | 59 | 60 | Prospective/randomized | Moderate | 49% | 51% | 19.8 vs.23.6% |
| Goligher EC et al.50 | 1098 | 61 | 70 | Prospective/randomized | Severe | 48% | 52% | 37 vs. 35% |
| Lopes RD et al.51 | 615 | 56 | 60 | Prospective/randomized | Mild/moderate | 50% | 50% | 11 vs.8% |
| Nadkarni et al.52 | 4389 | 65 | 56 | Observational/prospective | Various | 45% | 20% | 29 vs. 22% |
| Ayerbe et al. 53 | 2057 | 67 | 60 | Observational/prospective | Various | 84% | 16% | 14 vs. 18% |
| Lemos et al.54 | 20 | 56 | 85 | Prospective/randomized | Severe (ARDS) | 50% | 50% | 10 vs. 20% |
*mortality rates in therapeutic dose groups vs. usual care† overall mortality
Heparins, including both unfractionated and LMWH, exert non-anticoagulation related effects, by attenuating the inflammatory response, and reducing platelet and neutrophil activation.55 First, heparins block P-selectin, reduce the cross-talk between platelets and neutrophils, and inhibit the release of IL-1ß, E-selection, and ICAM-1.56 Second, heparins have a direct antiviral effect, because they inhibit pathogen adhesion to cell surfaces.57 Specifically, the S1 binding domain of the SARS-CoV-2 virus undergoes a conformational change upon heparin binding.58 In addition, in SARS, the protease, factor Xa, facilitates virus entry into cells, and it is known that heparins inhibit several proteases.55 , 59 Thus, in addition to their anticoagulation effects, heparins may act as both anti-inflammatory and direct anti-viral agents on multiple levels.
The direct thrombin inhibitor, argatroban, was administered to 10 critically ill patients that were treated with extracorporeal membrane oxygenation, due to a COVID-19 infection and an antithrombin deficiency. All 10 patients survived, but 3 had serious bleeding complications.60 Systemic fibrinolysis was not tested in a trial for patients with COVID-19, due to potential harm from bleeding complications. On the other hand, inhaled thrombolytic therapy, which does not increase the risk of bleeding, was previously tested in ARDS and is currently being tested in COVID-related ARDS.61 In ARDS, the group treated with streptokinase inhalation from day 1 to day 8 showed significantly higher PaO2/FIO2 ratios compared to the groups treated with heparin and the standard‐of‐care.62
The role of antiplatelet agents
Activated platelets play a key role in the thromboinflammatory response in patients with COVID-19. They produce a variety of cytokines and chemokines, which recruit neutrophils and enhance NETosis.55 These observations gave rise to the question: can we reduce both major cardiovascular events and microcirculatory damage by administering antiplatelet agents? In an animal model of an influenza virus infection, the combination treatment of eptifibatide (glycoprotein IIb/IIIA blocker), a protease-activated receptor 4 antagonist, and clopidogrel was shown to protect against severe lung injury and death.63 Moreover, acetylsalicylic acid blocked influenza virus propagation and diminished immune activation in patients with HIV infections.64 , 65
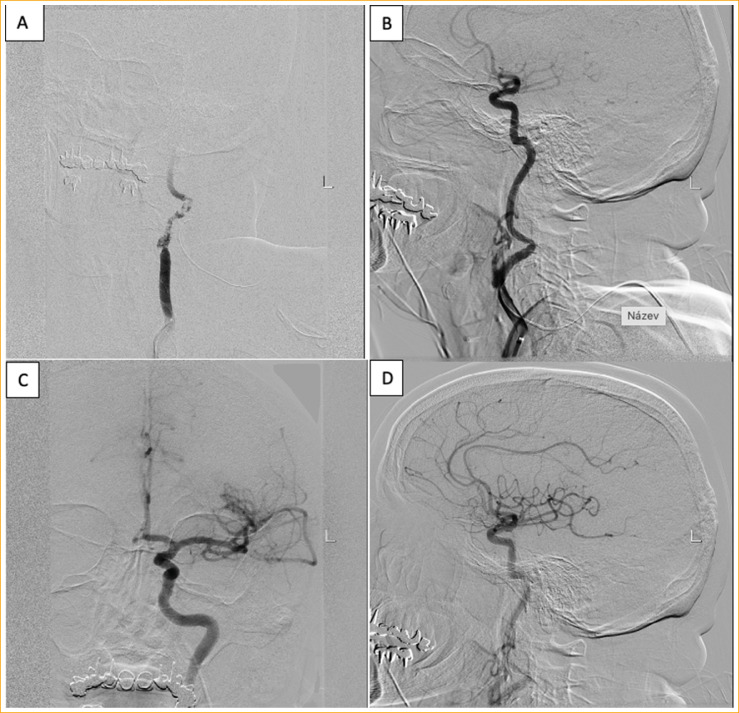
From our anecdotal experience in patient with COVID-19 infection and left internal carotid artery (ICA) occlusion was eptifibatide bolus administration effective in prompt recanalization of ICA (for more details see Fig. 4 ).
Figure 4.
COVID -19 patient with Left Internal carotid artery (ICA) thrombotic occlusion,Epitifibatide recanalization. (A) Thrombosis of the left ICA bulbus origin with no distal intracranial perfusion. (B) Rapid recanalization after IIb/IIIa Eptifibatide bolus administration. (C) Distal intracranial ICA bifurcation recanalization. (D) Anterior cerebral artery (ACA) plus medial cerebral artery (MCA) reperfusion after IIb/IIIa.
In a retrospective cohort that included 152 patients with COVID-19 in Germany, antiplatelet monotherapy (mostly acetylsalicylic acid) showed no benefit.66 The patients treated with antiplatelet agents had more pronounced radiological findings on chest X-rays, but those findings did not translate into a worse clinical outcome. Despite the pathophysiological links and the animal models of similar viral diseases that indicated that antiplatelet treatment could be beneficial against viral infections, to date, no trial has shown that antiplatelet treatment provided clinical improvement in patients with COVID-19. Antiplatelet treatment will be probably more effective in preventing or treatment of arterial occlusions than in microcirculatory damage.
Macrovascular complications of COVID-19
COVID-19 infection poses an increased risk of thromboembolism (TE), resulting in a higher mortality rate. A meta-analysis including 425 studies/8271 patients showed mortality of 23% in patients with TE and 13% in patients without TE.67 Overall deep vein thrombosis rate was 20%, in ICU 28%, pulmonary embolism 13%, in ICU setting 19%.67 For some relevant studies, mostly on well-documented critically ill patients with COVID-19 see Table 2 , the overall mortality ranges from 8.7 to 24%, depending on age and sample size.68, 69, 70, 71, 72, 73 Of note, there are some alarming reports related to spike vaccine-induced thrombosis and thrombocytopenia. Vaccination with ChAdOx1 nCov-19 can result in the rare development of immune thrombotic thrombocytopenia, which clinically mimics autoimmune heparin-induced thrombocytopenia (HIT).74 Similar thrombosis and thrombocytopenia were also observed after Ad26.COV2 vaccine, a recombinant adenovirus serotype 26 vectors encoding the SARS-CoV-2 spike glycoprotein.75 These cases suggest that the occurrence of vaccine-induced immune thrombotic thrombocytopenia could be related to adenoviral vector vaccines. The underlying mechanism appears to be the generation of pathologic antibodies to platelet factor 4 (PF4). Based on the PF4 antibodies and clinical similarity with HIT, platelet transfusion has to be avoided, and the administration of non-heparin anticoagulant and/or intravenous immune globulin should be considered. 76
Table 2.
Macrovascular complications of COVID-19.
| Study by | Patient count (N) | Age | Male % | Study type | Disease severity | PAT | DVT | PE | CVA/MI | MST | OAC (%) | Mortality rate |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gonzales-Fajardo JA et al.68 | 2943 | 65 | 68 | Retrospective | Various | 0.5% | 0.6% | 2% | 0.5% | 0.4% | 42 | 24% |
| Klok et al.69 | 184 | 64 | 76 | Retrospective | Critically ill | 3.7% | 27% | 13.5% | N/A | N/A | 9.2 | 13% |
| Thomas et al.70 | 63 | 70 | 44 | Retrospective | Critically ill | N/A | 1.6% | 7.9% | 3.1% | N/A | 2 | 16% |
| Helms et al. 71 | 150 | 63 | 81 | Retrospective | Critically ill | 8% | N/A | 16.7% | 2.6% | N/A | N/A | 8.7% |
| Tholin et al.72 | 262 | 58 | 58 | Retrospective | Various | N/A | 5% | N/A | N/A | N/A | 19 | N/A |
| Cui et al.73 | 81 | 60 | 46 | Retrospective | Critically ill | 25% | 10% | N/A | N/A | N/A | 10% |
Abbreviations: CV, cerebrovascular accident; DVT, deep vein thrombosis; MI, myocardial infarction; MST, multiple site thrombosis; N/A, not applicable; PAT, peripheral arterial thrombosis; OAC, oral anticoagulation.
New host-directed treatment options
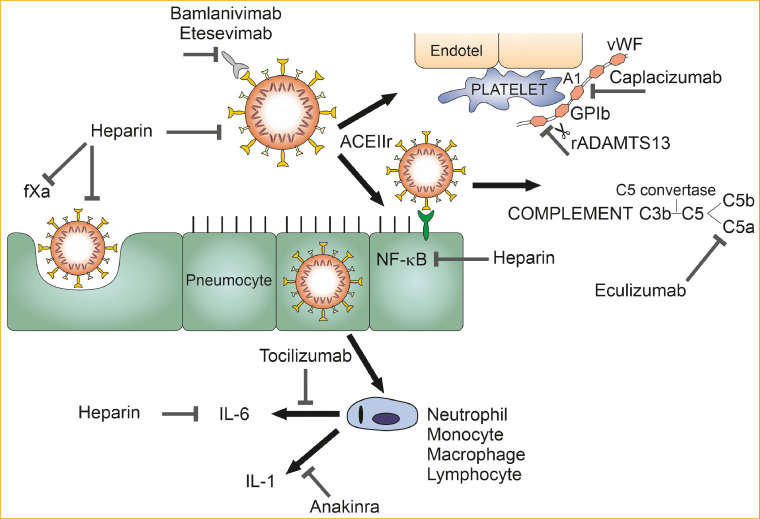
Based on the pathways known to lead to serious illness and complications in patients with COVID-19, four main treatment concepts have emerged (Fig. 5 ): (1) to diminish the cytokine storm by blocking the activities of either the interleukins or complement C5; (2) to prevent or reduce microcirculation damage by blocking the interaction between vWF (A1 domain) and platelets (GP Ib-IX-V); (3) to administer neutralizing monoclonal antibodies to reduce the viral load; and (4) to administer recombinant ADAMTS13.
Figure 5.
Host-directed treatment options. Abbreviations: IL-1: interleukin 1; IL-6: interleukin-6; NF-KB: nuclear factor kappa-light-chain-enhancer of activated B cells; fXa: activated factor X; ACEIIr: angiotensin converting enzyme II receptor; vWf: von Willebrand factor; GPIb: glycoprotein Ib; Endotel: endothelium; rADAMTS13: recombinant A Disintegrin And Metalloproteinase with a ThromboSpondin type 1 motif, member 13.
To date, anti-cytokine monoclonal antibodies that block IL-6 have been the most intensively studied treatments. The efficacy of tocilizumab (TCZ) was studied in a meta-analysis by Aziz et al. They stated that TCZ could potentially reduce mortality and the need for mechanical ventilation in severe COVID-19 cases, compared to the standard-of-care.77 However, in a randomized control trial (RCT) that included 246 patients moderately ill with COVID-19, TCZ did not effectively prevent intubation or death.78
In a retrospective, non-RCT trial, high-dose anakinra, the IL-1 antagonist, was tested in 29 patients with COVID-19 that exhibited moderate to severe ARDS and hyperinflammation. High-dose anakinra was associated with improved respiratory function (72%), delayed or no intubation, and a reduced death rate (10% vs. 44% in the standard-of-care group).79 Moreover, mechanical ventilation-free survival was 72%, compared to 50% in the standard-of-care group.79
In a proof of concept trial, Eculizumab (ECZ), a C5 inhibitor, was tested as an emergency treatment in 80 patients with severe COVID-19, compared to the standard-of-care. Patients that received ECZ showed significantly better survival on day 28 (80% vs. 51.1%) compared to patients that received the standard-of-care. Furthermore, the platelet count and oxygenation were significantly improved with ECZ, compared to the standard-of-care.80
Given the fact that the advanced COVID-19 disease state resembles thrombotic thrombocytopenic purpura/atypical hemolytic uremic syndrome, we propose that caplacizumab should be considered as an experimental treatment option. Caplacizumab is a humanized immunoglobulin that recognizes the vWF A1 domain and inhibits the interaction between vWF and platelet GP1b-IX-V.81 Indeed, breaking vWF-multimer chains might be the solution to COVID-19 microangiopathic thrombosis. However, caution should be taken to avoid bleeding complications, because administration of caplacizumab might lead to platelet-phenotype von Willebrand disease, due to impaired primary hemostasis.
Bamlanivimab and etesevimab are potent anti-spike neutralizing monoclonal antibodies that were isolated from two patients that had recovered from COVID-19 infections.82 In patients with mild to moderate COVID-19 infections, combined bamlanivimab and etesevimab treatment was associated with a significant reduction in the SARS-CoV-2 viral load. 82
Imbalance of vWF/ADAMTS13 is associated with persistence of ultra-long vWF multimers that are highly trombogenic. Incubation of plasma samples from COVID-19 patients with rADAMTS13 reduced abnormally high vWF activity and overall multimer size.83 This ex vivo experiment is by far not a proof of its efficacy in vivo, but this treatment option should be considered in clinical trials.
At present, there are no specific drugs for treating SARS-CoV-2 infections. Over the long term, SARS-CoV-2 infections induce an excessive host immune response, with multiple acute consequences that lead to lung damage and fibrosis. The host-directed therapies described here should be tested further. These approaches may prevent acute and chronic complications and improve the overall outcome in patients with COVID-19. 84
Conclusions
Given the global impact of COVID-19, the associated dysregulated immune response, and the absence of a specific therapy, new host-directed treatment options should be considered. COVID-19 is associated with significant coagulopathy, which leads to both macrovascular and microvascular thrombosis and hyperinflammation. The cornerstones of COVID-19-associated coagulopathy are the excessive generation of thrombin and endothelial/immune dysregulation. Available data have suggested that non-critically ill hospitalized patients should be administered full-dose heparin. In critically ill full dose heparin treatment is discouraged due to higher mortality rate. However, heparin alone might be insufficient for preventing and in particular for treating microvascular damage. It is probably necessary to combine heparin with a host-directed treatment that influences cytokine release, vWf multimers or blocks the complement cascade. The role of antiplatelet therapy in treating COVID-19 remains unclear. Ongoing clinical trials are testing host-directed therapies for treating COVID-19. To date, anakinra, eculizumab, bamlanivimab, and etesevimab were shown to improve clinical outcomes in specific patient populations.
Authors’ contributions
J.P. Conceptualization, Writing - original draft; J.G.: Writing - review & editing. J.M.: Supervision, Writing - review & editing. J.Š. Visualization; V.P. Visualization, Writing - review & editing; T.G. - Writing - review & editing; J.V. Supervision, Writing - review & editing.
Source of funding
Supported by Ministry of Health, Czech Republic; MH CZ - DRO (FNOs/2021).
Declaration of Competing Interest
Authors have no conflict of interest related to this article.
References
- 1.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Tang N., Li D., Wang X., et al. Abnormal coagulation parameterers are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Léonard-Lorant I., Delabranche X., Séverac F., et al. Acute Pulmonary embolism in patients with COVID-19 at CT angiography and relationship to d-dimer levels. Radiology. 2020;296(3):e189–e191. doi: 10.1148/radiol.2020201561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poissy J., Goutay J., Caplan M., et al. Pulmonary embolism in patients with COVID-19:awareness of an increased prevalence. Circulation. 2020;142(2):184–186. doi: 10.1161/CIRCULATIONAHA.120.047430. [DOI] [PubMed] [Google Scholar]
- 5.Levi M., Thachill J., Iba T., et al. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7(6):e438–e440. doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Varga Z., Flammer A.J., Steiger P., et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(2):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joynt G.M., Wu W.K. Understanding COVID-19: what does viral RNA load really mean? Lancet Infect Dis. 2020;20:635–636. doi: 10.1016/S1473-3099(20)30237-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferrario C.M., Jessup J., Chappell M.C., et al. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzymy 2. Circulation. 2005;111(20):2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- 9.Dong J.F., Moake J.L., Nolasco L., et al. ADAMTS-13 rapidly cleaves newly secreted ultralarge von Willebrand factor multimers in the endothelial surface under flowing conditions. Blood. 2002;100(12):4033–4039. doi: 10.1182/blood-2002-05-1401. [DOI] [PubMed] [Google Scholar]
- 10.Giblin JP. Basal secretion of von Willebrand factor from human endothelial cells. Blood. 2008;112(4):957–964. doi: 10.1182/blood-2007-12-130740. [DOI] [PubMed] [Google Scholar]
- 11.Lopes da Silva M, Cutler D. von Willebrand factor multimerization and the polarity of secretory pathways in endothelial cells. Blood. 2016;128(2):277–285. [DOI] [PMC free article] [PubMed]
- 12.Von T.H.M. Willebrand factor and von Willebrand factor-cleaving metalloprotease aktivity in Escherichia coli 0157: H7-associated hemolytic uremic syndrome. Pediatr Res. 2001;49(5):653–659. doi: 10.1203/00006450-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Fowler W.E., Fretto L.J., Hamilton K.K., et al. Substructure of human von Willebrand factor. J Clin Invest. 1985;76(4):1491–1500. doi: 10.1172/JCI112129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siedlecki C.A., Lestini B.J., Kottke-Marchant K.K., et al. Shear dependent changes in the three-dimensional structure of human von Willebrand factor. Blood. 1996;88(8):2939–2950. [PubMed] [Google Scholar]
- 15.Crawley J.T., De Groot R., Xiang Y., et al. Unravelling the scissile bond: how ADAMTS13 recognizes and cleaves von Willebrand factor. Blood. 2011;118(2):3212–3221. doi: 10.1182/blood-2011-02-306597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cemetson KJ. A short history of platelet glycoprotein Ib complex. Thromb Haemost. 2007;98(1):63–68. [PubMed] [Google Scholar]
- 17.Canobio I., Balduinin C., Torti M. Signaling through the platelet glykoprotein Ib-V-IX. Cell Signal. 2004;16(12):1329–1344. doi: 10.1016/j.cellsig.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 18.Goto S., Tamura N., Ishida H., et al. Dependence of platelet thrombus stability on sustained glycoprotein IIb/IIIa activation through adenosine 5‘-diphospate receptor stimulation and cyclic calcium signaling. J Am Coll Cardiol. 2006;47(1):155–162. doi: 10.1016/j.jacc.2005.08.055. [DOI] [PubMed] [Google Scholar]
- 19.Denorme F., Manne B.K., Portier I., et al. COVID-19 patients exhibit reduced procoagulant platelet responses. J Thromb Haemost. 2020;18(11):3067–3073. doi: 10.1111/jth.15107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Middleton E.A., He X.Y., Denorme F., et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136(10):1169–1179. doi: 10.1182/blood.2020007008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lax S.F., Skok K., Zechner P., et al. Pulmonary arterial thrombo- sis in COVID-19 with fatal outcome: results from a prospective, single-center, clinicopathologic case series. Ann Intern Med. 2020;173:350–361. doi: 10.7326/M20-2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manne B.K., Denorme F., Middleton E.A., et al. Platelet gene expression and function in patients with COVID-19. Blood. 2020;136(11):1317–1329. doi: 10.1182/blood.2020007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Álvarez-Roman M.T., Butta Coll N., García barcenilla S., et al. Registry of patients with congenital bleeding disorders and COVID-19 in Madrid. Haemophilia. 2020;26(5):773–778. doi: 10.1111/hae.14089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dorgalaleh A., Dabbagh A., Tabibian S., et al. Patients with congenital bleeding disorders appear to be less severely affected by SRS-CoV-2: is inherited hypocoagulability overcoming acquired hypercoagulability of coronavirus disease 2019 (COVID-19)? Semin Thromb Hemost. 2020;46(7):853–855. doi: 10.1055/s-0040-1713435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tam J.C.H., Bidgood S.R., McEwan W.A., et al. Intracellular sensing of complement C3 activates cell autonomous immunity. Science. 2014;345(6201) doi: 10.1126/science.1256070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McEwan W.A., Tam J.C.H., Watkinson R.E., et al. Intracellular antibody-bound pathogens stimulate immune signaling via the Fc receptor TRIM21. Nat Immunol. 2013;14:327–336. doi: 10.1038/ni.2548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morgan B.P. The complement system: an overview. Methods Mol Biol. 2000;150:1–13. doi: 10.1385/1-59259-056-X:1. [DOI] [PubMed] [Google Scholar]
- 28.Conway E.M., Pryzdial E.L.G. Is the COVID-19 thrombotic catastrophe complement-connected? J Thromb Haemost. 2020;18(11):2812–2822. doi: 10.1111/jth.15050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Calabrese LH. Cytokine storm and the prospects for immunotherapy with COVID-19. Cleve Clin J Med. 2020;87(7):389–393. doi: 10.3949/ccjm.87a.ccc008. [DOI] [PubMed] [Google Scholar]
- 30.Seshan S.V., Franzke C.W., Redecha P., et al. Role of tissue factor in a mouse model of thrombotic mi- croangiopathy induced by antiphospholipid (aPL) antibodies. Blood. 2009;114(8):1675–1683. doi: 10.1182/blood-2009-01-199117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Del Conde I., Cruz M.A., Zhang H., et al. Platelet activation leads to activation and propagation of the com- plement system. J Exp Med. 2005;201(6):871–879. doi: 10.1084/jem.20041497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huber-Lang M., Sarma J.V., Zetoune F.S., et al. Generation of C5a in the absence of C3: a new complement activation pathway. Nat Med. 2006;12(6):682–687. doi: 10.1038/nm1419. [DOI] [PubMed] [Google Scholar]
- 33.Cheng W., Hornung R., Xu K., et al. Complement C3 identified as a unique risk factor for disease severity among young COVID-19 patients in Wuhan, China. Sci Rep. 2021;11(1):7857. doi: 10.1038/s41598-021-82810-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fang S., Wang H., Lu l, et al. Decreased complement C3 level are associated with poor prognosis in patients with COVID-19: a retrospective cohort study. Int Immunopharmacol. 2020;89 doi: 10.1016/j.intimp.2020.107070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang K., Lu Y., Harley K.T., et al. Atypical hemolytic uremic syn- drome: a brief review. Hematol Rep. 2017;9(2):7053. doi: 10.4081/hr.2017.7053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hill A., DeZern A.E., Kinoshita T., et al. Paroxysmal nocturnal haemoglobinuria. Nat Rev Dis Prim. 2017;3:17028. doi: 10.1038/nrdp.2017.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hill A., Kelly R.J., Hillmen P. Thrombosis in paroxysmal nocturnal he- moglobinuria. Blood. 2013;121(25):4985–4996. doi: 10.1182/blood-2012-09-311381. [DOI] [PubMed] [Google Scholar]
- 38.Pryzdial E.L., Sutherland M.R., Ruf W. The procoagulant envelope virus surface: contribution to enhanced infection. Thromb Res. 2014;133(Suppl 1):S15–S17. doi: 10.1016/j.thromres.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sutherland M.R., Raynor C.M., Leenknegt H., et al. Coagulation initiated on herpesviruses. Proc Natl Acad Sci USA. 1997;94(25):13510–13514. doi: 10.1073/pnas.94.25.13510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giannis D., Ziogas I.A., Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li K., Wohlford-Lenane C., Perlman S., et al. Middle East respiratory syndrome coronavirus causes multiple organ damage and lethal disease in mice transgenic for human dipeptidyl peptidase 4. J Infect Dis. 2016;213(5):712–722. doi: 10.1093/infdis/jiv499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gralinski L.E., Sheahan T.P., Morrison T.E., et al. Complement activation contributes to severe acute respiratory syndrome coronavirus pathogenesis. MBio. 2018;9(5) doi: 10.1128/mBio.01753-18. e01753-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thachil J., Tang N., Gando S., et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–1026. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;58:711–712. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lachant D.J., Lachant N.A., Kouides P., et al. Chronic therapeutic anticoagulation is associated with decreased thrombotic complications in SARS-CoV-2 infection. J Thromb Haemost. 2020;18(10):2640–2645. doi: 10.1111/jth.15032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Iba T., Levy J.H., Warkentin T.E., et al. Diagnosis and management of sepsis-induced coagulopathy and disseminated intravascular coagulation. J Thromb Haemost. 2019;17(11):1989–1994. doi: 10.1111/jth.14578. [DOI] [PubMed] [Google Scholar]
- 48.Paranjpe I., Fuster V., Lala A., et al. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76(1):122–124. doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lawler P.R., Goligher E.C., Berger J.S., et al. Therapeutic anticoagulation with heparin in noncritically ill patients with COVID-19. N Eng J Med. 2021;85:790–802. doi: 10.1056/NEJMoa2105911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Goligher E.C., Bradbury C.A., McVerry B.J., et al. Therapeutic anticoagulation with heparin in critically ill patients with covid-19. N Engl J Med. 2021;385:777–789. doi: 10.1056/NEJMoa2103417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lopes R.D., de Barros E., Silva P.G.M., et al. Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated d-dimer concentration (ACTION): an open lable, multicentre, randomized, controlled trial. Lancet. 2021;12(397):2253–2263. doi: 10.1016/S0140-6736(21)01203-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nadkarni G.N., Lala A., Bagiella E., et al. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76:1815–1826. doi: 10.1016/j.jacc.2020.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ayerbe L., Risco C., Ayis S. The association between treatment with heparin and survival in patients with COVID-19. J Thromb Thrombolysis. 2020;50:298–301. doi: 10.1007/s11239-020-02162-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lemos A.C.B., Santo D.A.E., Salvetti M.C., et al. Therapeutic versus prophylactic anticoagulation for severe COVID-19: a randomized phase II clinical trial (HESACOVID) Thromb Res. 2020;196:359–366. doi: 10.1016/j.thromres.2020.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Godino C., Scotti A., Maugeri N., et al. Antithrombotic therapy in patients with COVID-19? Rationale and evidence. Int J Cardiol. 2021;324:261–266. doi: 10.1016/j.ijcard.2020.09.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li X., Zheng Z., Li X., et al. Unfractionated heparin inhibits lipopolysaccharide- induced inflammatory response through blocking p38 MAPK and NF-κB activation on endothelial cell. Cytokine. 2012;(60):114–121. doi: 10.1016/j.cyto.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 57.Esko J.D., Lindahl U. Molecular diversity of heparan sulfate. J Clin Invest. 2001;(108):169–173. doi: 10.1172/JCI13530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mycroft-West CJ, Su D, Elli S, et al. The 2019 coronavirus (SARSCoV-2) surface protein (Spike) S1 receptor binding domain undergoes conformational change upon heparin binding. BioRxiv Preprint April 29, 2020. 10.1101/2020.02.29.971093. [DOI]
- 59.Du L., Kao R.Y., Zhou Y., et al. Cleavage of spike protein of SARS coronavirus by protease factor Xa is associated with viral infectivity. Biochem Biophys Res Commun. 2007;(359):174–179. doi: 10.1016/j.bbrc.2007.05.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Arachchillage D.J., Remmington C., Rosenber A., et al. Anticoagulation with argatroban in patients with acute antithtombin deficiency in severe COVID-19. Br J Haematol. 2020;190(5):e286–e288. doi: 10.1111/bjh.16927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Asakura H., Ogawa H. Perspective on fibrinolytic therapy in COVID-19: the potential of inhalation therapy against suppressed-fibrinolytic-type DIC. J Intensive Care. 2020;18(8):71. doi: 10.1186/s40560-020-00491-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Abdelaal Ahmed Mahmoud A., Mahmoud H.E., Mahran M.A., et al. Streptokinase versus unfractionated heparin nebulization in patients with severe acute respiratory distress syndrome (ARDS): a randomized controlled trial with observational controls. J Cardiothorac Vasc Anesth. 2020;34:436–443. doi: 10.1053/j.jvca.2019.05.035. [DOI] [PubMed] [Google Scholar]
- 63.Le B., Schneider J.G., Boergeling Y., et al. Platelet activation and aggregation promote lung inflammation and influenza virus pathogenesis. Am J Respir Crit Care Med. 2015;191(7):804–819. doi: 10.1164/rccm.201406-1031OC. [DOI] [PubMed] [Google Scholar]
- 64.Mazur I., Wurzer W.J., Ehrhardt C., et al. Acetylsalicylic acid (ASA) blocks influenza virus propagation via its NF-kappaB-inhibiting aktivity. Cell Microbiol. 2007;9(7):1683–1694. doi: 10.1111/j.1462-5822.2007.00902.x. [DOI] [PubMed] [Google Scholar]
- 65.O'Brien M., Montenont E., Hu L., et al. Aspirin attenuates platelet activation and immune activation in HIV-1 infected subjects n Antiretroviral therapy: a pilot study. J Acquir Immune Defic Syndr. 2013;63(3):280–288. doi: 10.1097/QAI.0b013e31828a292c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Banik J., Mezera V., Kohler C., et al. Antiplatelet therapy in patients with COVID-19: a retrospective observational study. Thromb Update. 2021;2:1–9. doi: 10.1016/j.tru.2020.100026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Malas M.B., Naazie I.N., Elsayed N., et al. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: a systematic review and meta-analysis. EclinicalMedicine. 2020;29 doi: 10.1016/j.eclinm.2020.100639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gonazales-Fajardo J.A., Ansuategui M., Romero C., et al. Mortality of COVID-19 patients with vascular thrombotic complications. Med Clin. 2021;156(3):112–117. doi: 10.1016/j.medcle.2020.10.008. (Barc.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Klok F.A., Kruip M., van der Meer N.J.M., et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Thomas W., Varley J., Johnston A., et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at teaching hospital in the United Kingdom. Thromb Res. 2020;191:76–77. doi: 10.1016/j.thromres.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Helms J., Tacquard Ch, Severac F., et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a mlticenter prospective cohort study. Intensive Care Med. 2020;4:1–10. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tholin B., Ghanima W., Einvik G., et al. Incidence of thrombotic complications in hospitalised and non-hospitalised patients after COVID-19 diagnosis. Br J Haematol. 2021;191(3):542–546. doi: 10.1111/bjh.17522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cui S., CHen S., Li X., et al. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;6:10. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Greinacher A., Thiele T., Warkentin T.E., et al. Thrombotic thrombocytopenia after ChAd0x1 nCov-19 vaccination. N Engl J Med. 2021;384(22):2092–2101. doi: 10.1056/NEJMoa2104840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kallam A., Koepsell S.A. Gundabolu. Thrombotic thrombocytopenia after Ad26.COV2.S vaccination. N Engl J Med. 2021;384:1964–1965. doi: 10.1056/NEJMc2105869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Scully M., Singh D., Lown R., et al. Pathologic antiboides to platelet factor 4 after ChAdOx1 nCoV-19 vaccination. N Eng J Med. 2021;384:2202–2211. doi: 10.1056/NEJMoa2105385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Aziz M., Haghbin H., Sitta E.A., et al. Efficacy of tocilizumab I COVID-19: a systematic review and meta-analysis. J Med Virol. 2021;93:1620–1630. doi: 10.1002/jmv.26509. [DOI] [PubMed] [Google Scholar]
- 78.Stone J.H., Frigault M.J., Sterling-Boyd N.J., et al. Efficacy of tocilizumab in patients hospitalized with COVID-19. N Engl J Med. 2020;383(24):2333–2344. doi: 10.1056/NEJMoa2028836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cavalli G., De Luca G., Campochiaro C., et al. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2020;2(6):e325–e331. doi: 10.1016/S2665-9913(20)30127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Annane D., Heming N., Grimaldi-Bensouda L., et al. Eculizumab as an emergency treatment for adult patients with severe COVID-19 in the intensive care unit: a proof of concept study. EclinicalMedicine. 2020;28 doi: 10.1016/j.eclinm.2020.100590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Elverdi T., Eskazan AE. Caplacizumab as an emerging treatment option for aquired thrombotic thrombocytopenic purpura. Drugs Des Dev Ther. 2019;13:1251–1258. doi: 10.2147/DDDT.S134470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gottlieb R.L., Nirula A., Chen P., et al. Effect of bamlanivimab as monotherapy or in ombination with etesevimab on viral lod in patients with mild to moderate COVID-19:a randomized clinical trial. JAMA. 2021;325(7):632–644. doi: 10.1001/jama.2021.0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Turecek P.L., Peck R.C., Rangarajan S., et al. Recombinant ADAMTS13 reduces abnormally up-regulated von Willebrand factor in plasma from patients with severe COVID-19. Thromb Res. 2021;201(18):100–112. doi: 10.1016/j.thromres.2021.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zumla A., Hui Azhar D.I., Memish Z.A., et al. Reducing mortality from 2019-nCoV: host-directed therapies should be an option. Lancet. 2020;(395):e35–e36. doi: 10.1016/S0140-6736(20)30305-6. [DOI] [PMC free article] [PubMed] [Google Scholar]