Abstract
Background:
Approximately 1,000 out-of-hospital cardiac arrest (OHCA) occur each day in the United States. Although sex differences exist for other cardiovascular conditions such as stroke and acute myocardial infarction, they are less well understood for OHCA. Specifically, the extent to which neurological and survival outcomes after OHCA differ between men and women remains poorly characterized in the U.S.
Methods and Results:
Within the national Cardiac Arrest Registry to Enhance Survival (CARES) registry, we identified 326,138 adults with an OHCA from 2013–2019. Using multivariable logistic regression, we evaluated for sex differences in rates of survival to hospital admission, survival to hospital discharge, and favorable neurological outcome (i.e., without severe neurological disability), adjusted for demographics, cardiac arrest characteristics and bystander interventions. Overall, 117,281 (36%) patients were women. Median age was 62 and 65 years for men and women, respectively. An initial shockable rhythm (25.1% vs 14.7%, standardized difference of 0.26) and an arrest in a public location (22.2% vs. 11.3%; standardized difference of 0.30) were more common in men, but there were no meaningful sex differences in rates of witnessed arrests, bystander cardiopulmonary resuscitation, intra-venous access, or use of mechanical devices for delivering cardiopulmonary resuscitation. Overall, the unadjusted rates of all survival outcomes were similar between men and women: survival to hospital admission (27.0% for men vs. 27.9% for women, standardized difference of −0.02), survival to hospital discharge (10.5% for men vs. 8.6% for women, standardized difference of 0.07), and favorable neurological survival (9.0% for men vs. 6.6% for women, standardized difference of 0.09). After multivariable adjustment, however, men were less likely to survive to hospital admission (adjusted OR= 0.75, 95% CI: 0.73, 0.77), survive to hospital discharge (adjusted OR= 0.83, 95% CI: 0.80, 0.85), or have favorable neurological survival (adjusted OR= 0.88, 95% CI: 0.85, 0.91).
Conclusions:
Compared to women, men with OHCA have more favorable cardiac arrest characteristics but were less likely to survive to hospital admission, survive to discharge, or have favorable neurological survival.
Keywords: Out-of-hospital cardiac arrest, sex differences, survival outcomes, neurological outcomes, epidemiology
INTRODUCTION
Out-of-hospital cardiac arrest (OHCA) is common in the United States, affecting nearly 1000 adults daily.1 Despite two decades of advances in resuscitation interventions, overall rates of survival to hospital discharge after OHCA have remained low at 10.4%, with favorable neurological survival at hospital discharge at 8.4%.1 Although men are known to have a higher OHCA incidence than women2–5, it remains unclear to what extent there may be sex differences in neurological and survival outcomes after OHCA.
Previous studies have assessed for sex differences in OHCA treatment and survival. The results of these studies have been inconsistent, partly due to differences in study design and scope. Some have shown that women have higher rates of survival to hospital discharge than men. 6–9 Other studies have reported that women have lower survival rates to hospital discharge as compared with men. 3,10–12 Furthermore, few studies have evaluated sex differences in rates of favorable neurological survival after OHCA—arguably the most important outcome for patients and their families13. Those that have were outside the United States 11,14,15 and they either had relatively small sample sizes8,11,16–18, or evaluated rates of favorable neurological survival only among those surviving to hospital admission which can be misleading if there are sex differences in survival to hospital admission after OHCA.5,17–19
Accordingly, we leveraged data from the largest U.S.-based registry on OHCA to evaluate for sex differences in rates of favorable neurological survival, as well as rates of survival to hospital admission and to hospital discharge.
METHODS
Data source and Study Population
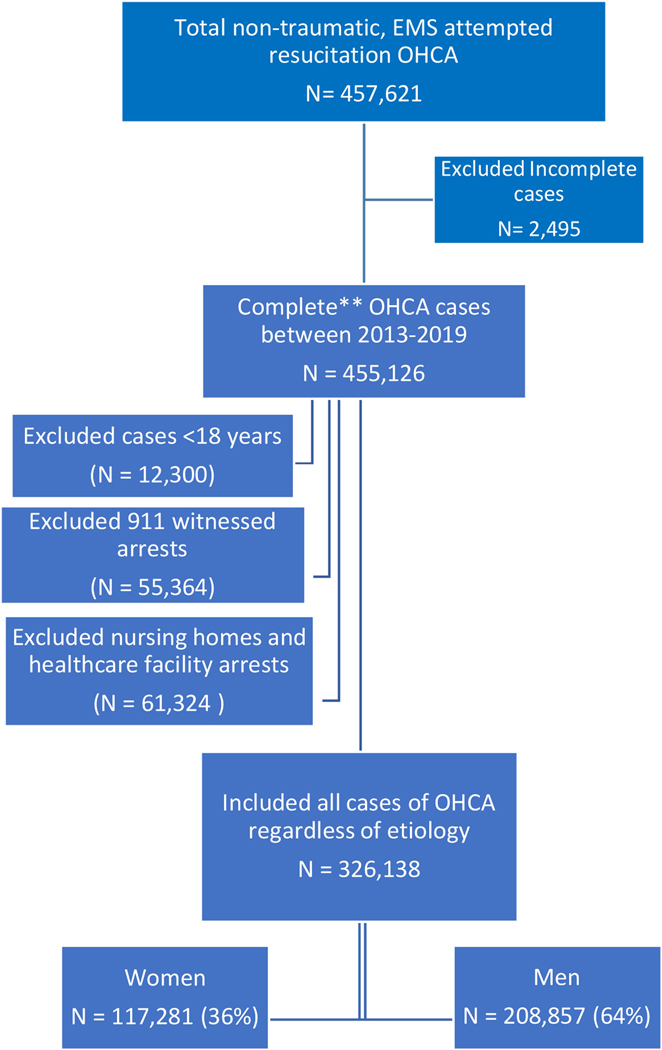
The Cardiac Arrest Registry to Enhance Survival (CARES) registry is the largest, ongoing surveillance registry for OHCA in the United States, encompassing a broad population and thereby providing nationally representative epidemiological estimates. Presently, the catchment area of CARES in the U.S. is approximately 152 million people (or 46% of the U.S. population) across 28 states. For this study, we had a total of 457,621 non-traumatic, EMS attempted resuscitation, OHCA cases registered in CARES from January 1, 2013 to December 31, 2019 (Figure 1). We excluded 2,495 incomplete cases and restricted our final analytical sample to 455,126 cases that had complete record of age, sex, shockable, witnessed arrest, bystander cardiopulmonary resuscitation (CPR), automated external defibrillator (AED), location, year of arrest and survival (survival to hospital admission, survival to hospital discharge and neurological survival). We excluded 12,300 pediatric cases under 18 years of age. As we were interested in OHCAs that were not in healthcare associated settings or had the advantage of a healthcare professional, we also excluded 55,364 cases witnessed by emergency medical service (EMS) providers and 61,324 occurring in nursing homes or healthcare facilities. Our final study cohort was comprised of 326,138 adults with an OHCA regardless of etiology. The study measures and details on the design of the CARES registry and data elements have been described previously.20
Figure 1. Consort Diagram Showing the Final Analytic Sample.
**Completed cases are those that had complete record of age, sex, shockable, witnessed arrest, BCPR, AED, location, year of arrest and survival (survival to hospital admission, survival to hospital discharge and neurological survival).
The categories are excluded in sequence. First, ages<18 were excluded, then all 911 witnessed arrests and then the nursing homes were excluded from the complete data.
Study outcomes
The primary outcome was favorable neurological outcome at hospital discharge, which was defined as survival at discharge with a cerebral performance category (CPC) score of 1 or 2, which denotes survival without severe neurological disability.21 This outcome ensures meaningful survival of OHCA patients, as it connotes sufficient function to remain independent with the activities of daily living.22 We also evaluated as secondary outcomes, survival to hospital admission and survival to hospital discharge. Measuring survival to hospital admission allows us to better understand whether any observed sex differences in the primary outcome may be due to sex differences in the prehospital phase of care.
Statistical analysis
Sample descriptive statistics by sex are presented as medians with interquartile range (IQR) for continuous variables and counts (with percentage distributions) for categorical variables. Due to the large sample size, standardized differences were computed to assess for sex differences in baseline characteristics, with a standardized difference of >0.10 denoting a meaningful difference.23
To evaluate for sex differences in our primary outcome of favorable neurological survival, we constructed a multivariable logistic regression model using generalized estimating equations (GEE) with logit link estimates to account for patient outcomes clustered within EMS agencies. Women were the reference category in all analyses. Besides patient sex, the model controlled for other demographic and cardiac arrest characteristics, including age, race/ethnicity, witnessed arrest status, private vs public location, initial presenting rhythm, if AED shock was applied before EMS arrival, presumed etiology of the cardiac arrest, and whether bystander CPR was administered. We also included calendar year of the cardiac arrest to control for any temporal trends. Additionally, we examined for interactions between sex and all model covariates. Specifically, we performed a sex by age interaction analysis to evaluate sex differences as a function of age, with age stratified by age ˂ 50 and ≥ 50 for all three outcome measures. As a sensitivity analysis, we repeated our analyses to only those patients with a presumed cardiac etiology to their OHCA and for those patients with a witnessed OHCA.
For our secondary outcomes of survival to hospital admission and survival to hospital discharge, we constructed separate multivariable logistic regression models for each of these outcome measures. Furthermore, if there were sex differences in overall survival to discharge, we explored differences in overall survival for two phases of care—survival to hospital admission and, among those who survived to hospital admission, survival to hospital discharge. Evaluating for sex differences in these two phases would allow us to better characterize whether differences in rates of survival to discharge were due to sex differences in prehospital survival or in-hospital survival. All analyses were evaluated at a 2-sided significance level of 0.05 and were performed using SAS version 9.4 (SAS institute, Cary, NC).
Ethics approval: This study was approved by the Institutional Review Board at University of Illinois at Chicago and was determined to be non human subject research.
RESULTS
Among 326,138 adults with OHCA that were included in this study, 208,857 (64%) were men and 117,281 (36%) were women. Table 1 displays the distribution of demographic, cardiac arrest, and clinical characteristics by sex. Men were younger than women, with a median age of 62 and 65, respectively. In our sample, 20.9% (24,494) of women and 21.8% (45,609) of men were less than 50 years of age. Black patients comprised a smaller proportion of men than women. Men were more likely to have certain prehospital factors favoring survival as compared with women, including shockable rhythm (25% vs. 15%; standardized difference, 0.26), AED shock prior to EMS arrival (10% vs. 5%, standardized difference, 0.18), and public location of arrest (22% vs. 11%; standardized difference, 0.30). However, there were no meaningful differences in rates of bystander witnessed arrest (46% vs. 41%) or bystander CPR (40% vs. 38%).
Table 1:
Distribution of Demographic and Clinical Characteristics by Sex in Patients with OHCA
| Characteristic | Total (N= 326,138) n (%) | Men (N= 208,857) n (%) | Women (N= 117,281) n (%) | Standardized Difference |
|---|---|---|---|---|
| Age in years, median (IQR) | 63 (23) | 62 (22) | 65 (25) | 0.126 |
| Race | 0.151 | |||
| Black | 66,141 (20.3%) | 37,808 (18.1%) | 28,333 (24.2%) | 0.149 |
| White | 160,298 (49.2%) | 105,922 (50.7%) | 54,376 (46.4%) | 0.087 |
| Hispanic | 19,520 (6.0%) | 13,002 (6.2%) | 6,518 (5.6%) | 0.028 |
| Other | 9,976 (3.0%) | 6,304 (3.0%) | 3,672 (3.1%) | 0.006 |
| Unknown | 70,203 (21.5%) | 45,821 (21.9%) | 24,382 (20.8%) | 0.028 |
| Initial shockable rhythm | 69,633 (21.4%) | 52,375 (25.1%) | 17,258 (14.7%) | 0.262 |
| Bystander Witnessed | 143,959 (44.1%) | 95,411 (45.6%) | 48,548 (41.4%) | 0.087 |
| Bystander CPR initiated | 127,699 (39.2%) | 83,215 (39.8%) | 44,484 (37.9%) | 0.039 |
| Automated External Defibrillator applied prior to EMS arrival | 96,840 (29.7%) | 64,544 (30.9%) | 32,296 (27.5%) | 0.074 |
| Automated External Defibrillator shock delivered prior to EMS arrival | 27,373 (8.4%) | 21,178 (10.1%) | 6,195 (5.3%) | 0.183 |
| Public location of Arrest | 59,738 (18.3%) | 46,479 (22.2%) | 13,259 (11.3%) | 0.296 |
| Presumed Cardiac Etiology | 277,628 (85.1%) | 179,669 (86.0%) | 97,959 (83.5%) | 0.070 |
| Mechanical CPR Device Used | 75,473 (28.5%) | 49,073 (28.8%) | 26,400 (27.9%) | 0.022 |
| Automated CPR Feedback Device Used | 46,824 (18.3%) | 30,403 (18.5%) | 16,421 (17.9%) | 0.015 |
| Advanced Airway Successfully Placed | 213,197 (79.4%) | 136,821 (79.4%) | 76,376 (79.4%) | 0.002 |
| Impedance threshold device used | 46,906 (18.1%) | 30,193 (18.2%) | 16,713 (18.1%) | 0.003 |
| Were Drugs Administered | 261,279 (92.2%) | 168,049 (92.5%) | 93,230 (91.8%) | 0.025 |
| Vascular Access | 0.130 | |||
| IO (intraosseous catheter) | 135,506 (49.6%) | 83,829 (47.8%) | 51,677 (52.7%) | 0.099 |
| IV (intravenous catheter) | 98,015 (35.8%) | 66,440 (37.9%) | 31,575 (32.2%) | 0.119 |
| IO_IV (intraosseous & intravenous catheter) | 22,456 (8.2%) | 14,637 (8.3%) | 7,819 (8.0%) | 0.013 |
| No_IV(no IV access) | 17,448 (6.4%) | 10,506 (6.0%) | 6,942 (7.1%) | 0.044 |
| 12-Lead electrocardiogram (ECG) placed | 51,074 (19.5%) | 32,532 (19.3%) | 18,542 (19.7%) | 0.010 |
We further explored sex differences in modifiable prehospital care interventions. There were no significant differences in rates of advanced airway placed, impedance threshold device (ITD) used, or 12-lead electrocardiogram (EKG) obtained, CPR feedback device used, mechanical CPR device used, and drugs administered between men and women (Table 1). However, there were statistically significant (p < 0.0001) sex differences in rates of vascular access between men and women with a standardized difference of 0.13 (Table 1), with men having higher likelihood of receiving intravenous lines (38% vs 32%, standardized difference of 0.12) and lower likelihood of intraosseous catheter placement (48% vs 53%, standardized difference of 0.10) compared to women.
Survival Outcomes
Overall, 10,043 (8.6%) women and 21,972 (10.5%) men survived to hospital discharge, and 7,728 (6.6%) women and 18,708 (9.0%) men had favorable neurological outcome, with similar unadjusted rates for both outcomes between men and women (standardized differences of 0.07 and 0.09, respectively) (Table 2). After accounting for baseline differences and within-cluster correlation, compared to women, men had 17% lower odds of surviving to hospital discharge (adjusted OR= 0.83, 95% CI: 0.80–0.85) and 12% lower odds of favorable neurological survival (adjusted OR= 0.88, 95% CI: 0.85–0.91) (Table 2). This difference persisted when the analyses were restricted to OHCA with presumed cardiac etiology cases, which constituted 85.1% of the entire study cohort (for survival to hospital admission adjusted OR 0.76; 95% CI: 0.75–0.78; survival to hospital discharge adjusted OR 0.83; 95% CI: 0.80 – 0.87; for favorable neurological survival adjusted OR 0.88; 95% CI: 0.85–0.92). When the sample was restricted to those with a bystander witnessed arrest, which was 44.1% of the study cohort, for all three outcome measures, the sex difference persisted (survival to hospital admission adjusted OR =0.74 (95% CI 0.72 – 0.76); for survival to hospital discharge adjusted OR = 0.83 (95% CI 0.80 – 0.87); and for favorable neurological survival adjusted OR = 0.88 (95% CI: 0.85 – 0.92).
Table 2:
The Association of Sex for each Survival Outcome in Patients with OHCA.
| Study Outcome, n (%) | Total N=326,138 |
Men N= 208,857 |
Women N=117,281 |
Men vs. Women | |
|---|---|---|---|---|---|
| Crude OR (95% CI) |
Adjusted OR* (95% CI) |
||||
| Survived to Hospital Admission | 89,025 (27.3%) | 56,279 (27.0%) | 32,746 (27.9%) | 0.94 (0.92 – 0.96) | 0.75 (0.73 – 0.77) |
| Survived to Hospital Discharge | 32,015 (9.8%) | 21,972 (10.5%) | 10,043 (8.6%) | 1.22 (1.18 – 1.26) | 0.83 (0.80 – 0.85) |
| Favorable Neurological Survival | 26,436 (8.1%) | 18,708 (9.0%) | 7,728 (6.6%) | 1.33 (1.29 – 1.37) | 0.88 (0.85 – 0.91) |
controlling for centered age, race, year of arrest, witness status, BCPR, shockable rhythm, location, AED shock, cardiac etiology.
To better understand whether sex differences were due to differences in rates of survival to hospital admission or survival to discharge among those survived to hospital admission, we conducted additional analyses for these 2 phases of OHCA resuscitation care. When examining survival to hospital admission, 32,746 (28%) women survived to hospital admission as compared with 56,279 (27%) men (see Table 2). After multivariable adjustment, men had 25% lower odds of surviving to hospital admission (adjusted OR= 0.75, 95% CI: 0.73–0.77). When the logistic regression model was further adjusted for vascular access, it did not attenuate or eliminate the sex difference in survival to hospital admission (data not shown). Of the 89,025 OHCA patients who survived to hospital admission, men and women had no significant differences in survival to hospital discharge (adjusted OR= 0.98, 95% CI: 0.95–1.02) and favorable neurological survival (OR= 1.03, 95% CI: 0.99, 1.07) after accounting for baseline differences and in-hospital treatment with targeted temperature management and coronary angiography.
Interaction Analysis
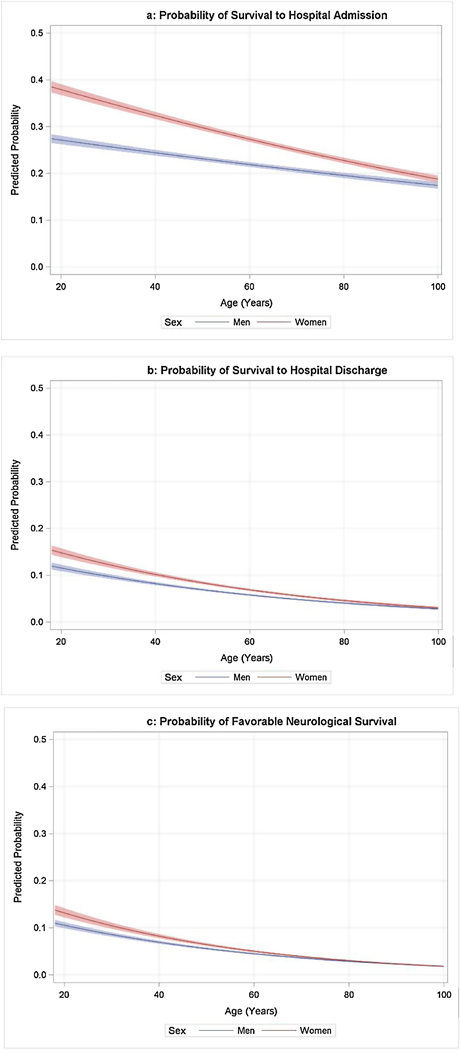
The results of the models assessing interaction between covariates and sex variable, for each of the survival outcomes, are presented in Table 3. There were significant interactions by sex with age, bystander CPR, and cardiac etiology for all three of the survival outcomes. In each stratum of the interaction (e.g., younger vs. older patients), men consistently had lower odds of survival. The sex difference was more pronounced among younger patients (< 50 years of age), those not receiving bystander CPR, and among those classified as without a presumed cardiac arrest etiology. When we plotted the predicted probabilities for men and women across the age spectrum for each outcome measure (Figure 2a-c), men were less likely to survive to hospital discharge than women across the entire age spectrum and less likely to have favorable neurological survival until approximately age 70. There was a more pronounced survival difference in younger patients but the sex difference in survival outcomes remained for older patients, even above 55 years of age (Figure 2a-c).
Table 3.
Interaction Model between Sex and each Covariate by Study Outcomes, adjusted for covariates.
| Survival to Hospital Admission | Survival to Hospital Discharge | Favorable Survival | Neurological | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Stratum | OR (95% CI) | P value for interaction | OR (95% CI) | P value for interaction | OR (95% CI) | P value for interaction |
|
| ||||||
| Age strata | <0.001 | <0.001 | <0.001 | |||
| Among Age <50 | 0.69 (0.66 – 0.72) | 0.76 (0.72 – 0.80) | 0.80 (0.75 – 0.84) | |||
| Among Age ≥50 | 0.79 (0.77– 0.81) | 0.89 (0.86 – 0.92) | 0.95 (0.92 – 0.99) | |||
|
| ||||||
| Race strata | 0.41 | 0.008 | 0.24 | |||
| Among Blacks | 0.76 (0.72 – 0.79) | 0.75 (0.71 – 0.80) | 0.86 (0.81 – 0.92) | |||
| Among Whites | 0.74 (0.72 – 0.76) | 0.84 (0.81 – 0.88) | 0.88 (0.84 – 0.92) | |||
| Among Hispanics | 0.75 (0.68 – 0.84) | 0.78 (0.67 – 0.90) | 0.86 (0.73 – 1.01) | |||
| Among Others | 0.80 (0.71 – 0.90) | 1.00 (0.84 – 1.19) | 1.10 (0.91 – 1.34) | |||
| Among Unknown | 0.76 (0.74 – 0.80) | 0.85 (0.80 – 0.90) | 0.87 (0.82 – 0.92) | |||
|
| ||||||
| AED shock | 0.12 | 0.47 | 0.93 | |||
| Among those w/ AED shock | 0.72 (0.68 – 0.76) | 0.84 (0.79 – 0.90) | 0.88 (0.82 – 0.94) | |||
| Among those w/o AED shock | 0.75 (0.74 – 0.77) | 0.82 (0.79 – 0.85) | 0.88 (0.84 – 0.91) | |||
|
| ||||||
| Shockable rhythm | <0.001 | 0.77 | 0.80 | |||
| Among those w/ shockable | 0.70 (0.68 – 0.73) | 0.82 (0.79 – 0.86) | 0.88 (0.84 – 0.92) | |||
| Among those w/o shockable | 0.76 (0.75 – 0.78) | 0.82 (0.79 – 0.86) | 0.88 (0.84 – 0.92) | |||
|
| ||||||
| Witnessed | 0.003 | 0.22 | 0.29 | |||
| Among witnessed | 0.73 (0.71 – 0.75) | 0.81 (0.77 – 0.85) | 0.86 (0.81 – 0.91) | |||
| Among those w/o Bystander CPR | 0.73 (0.71 – 0.75) | 0.76 (0.73 – 0.80) | 0.82 (0.78 – 0.85) | |||
|
| ||||||
| Bystander CPR | <0.001 | <0.001 | <0.001 | |||
| Among those w/ Bystander CPR | 0.79 (0.76 – 0.81) | 0.90 (0.86 – 0.93) | 0.94 (0.90 – 0.98) | |||
| Among those w/o Bystander CPR | 0.73 (0.71 – 0.75) | 0.76 (0.73 – 0.80) | 0.82 (0.78 – 0.85) | |||
|
| ||||||
| Public location of Arrest | 0.02 | 0.33 | 0.71 | |||
| Among those in public location | 0.71 (0.68 – 0.75) | 0.84 (0.80 – 0.89) | 0.87 (0.82 – 0.92) | |||
| Among those in private location | 0.76 (0.74 – 0.78) | 0.82 (0.79 – 0.85) | 0.88 (0.85 – 0.92) | |||
|
| ||||||
| Cardiac Etiology | <0.001 | <0.001 | <0.001 | |||
| Among those w/ Cardiac Etiology | 0.77 (0.76 – 0.79) | 0.86 (0.83 – 0.89) | 0.91 (0.88 – 0.95) | |||
| Among those w/o Cardiac Etiology | 0.67 (0.64 – 0.70) | 0.72 (0.68 – 0.77) | 0.77 (0.71 – 0.82) | |||
Figures 2a-c.
Predicted Probabilities for Men and Women across the Age Spectrum for each Outcome Measure
DISCUSSION
Using the largest US-based national registry of OHCA, our study found that men were twice as likely to experience OHCA as women and were less likely to survive to hospital discharge and less likely to survive without severe neurological disability. Although men survive at a higher rate than women and have more favorable cardiac arrest prognostic characteristics than women, when adjusted for potential confounders, the odds of survival for OHCA were lower for men than women. Lower overall survival rates in men were driven by lower rates of survival to hospital admission, as rates of survival to discharge among those who survived to hospital admission were similar between men and women. Collectively, our findings provide important insights into the sex differences in OHCA survival.
To date, our study is the largest in the world to evaluate for neurological outcome differences of OHCA by sex. There have been some studies which have evaluated sex differences in survival to hospital discharge after OHCA. The majority have been smaller in sample size and have reported conflicting results, with some showing that men have lower rates of survival to discharge than women6–8 while others have not.3,10,11,24 Our study extends the findings of prior studies by evaluating both survival to hospital discharge and favorable neurological survival from the time of cardiac arrest, as well as evaluating which phase of resuscitation care accounted for observed sex differences. We found that sex differences in survival were driven primarily by lower rates of prehospital survival among men, as there were no sex differences in overall survival and favorable neurological survival between men and women who survived to hospital admission. We did find some differences in prehospital care, such as vascular access differences between men and women, but sex differences in rates of survival to hospital admission persisted after adjusting for these measured process factors. Thus, sex differences in survival rates to hospital admission is either due to unmeasured illness severity between men and women, other unmeasured prehospital treatment differences, or variability in inherent sex-specific injury responses.
Prior studies have not routinely reported sex differences in favorable neurological survival. Although a handful of smaller studies in the U.S. have reported on sex differences in favorable neurological discharge, these have typically evaluated for sex differences from the time of hospital admission or in those with return of spontaneous circulation. 5,17,19 Prior study findings may be misleading if men are less likely to survive to hospital admission, as was demonstrated in this study. Our study was demographically representative of the U.S. and found that men were less likely to have favorable neurological survival than women when measured from the time of initial OHCA, and this difference was driven by lower rates of survival to hospital admission. Several large Asian studies have found no sex differences in rates of neurological survival between men and women11,14,15. The results from these population-based studies may be difficult to translate to the United States, as differences in pre-hospital care protocols and comorbidities between men and women by region may account for these differing results.
Previously, Johnson and colleagues had proposed that sex differences in rates of survival to discharge after OHCA may be restricted only to patients under 55 years of age with no differences in survival among those older than 55.9 As a result, several theories have been proposed as to why women may have higher rates of survival than men after OHCA, including the potential benefits of estrogen 8,25–27 and a genetic protective loci on the X chromosome. 28 Others have proposed that physiologic differences exist between the sexes 29 and potentially higher quality CPR occur in women due to smaller chest cavities. 30 Our analysis found men to have a lower likelihood of survival to hospital admission, survival to hospital discharge, and favorable neurological survival, regardless of age strata. Our findings using the same CARES registry as Johnson et al. suggests that the prior study was likely less representative for the population over 55 years of age. In our study sample, which was more than 10 times the size of the earlier study, we found no meaningful interaction between age and sex for the outcome of survival to hospital discharge. In addition, when age was removed from the logistic regression models, the odds ratios for all the outcome measures did not change significantly.
Overall, our study indicates that men have lower rates of favorable neurological survival than women. The sex differences in OHCA functional neurological survival found in our analysis provides an epidemiological basis to further investigate the pathophysiological pathways associated with sex, and ultimately better inform resuscitation care to improve survival outcomes for both men and women.
Our study should be interpreted in the context of the following limitations. Detailed information on comorbidities and illness severity, as well as socioeconomic status, was not available and could explain observed sex differences for our survival outcomes.31,32 Our study was restricted to the outcomes of survival to hospital admission, survival to hospital discharge, and favorable neurological discharge. We were unable to assess whether sex differences persisted after hospital discharge as CARES does not routinely collect information on survivors of OHCA. Also, CARES does not collect many variables on hospital interventions. As such, we did not have information on intensive care unit interventions, rates of withdrawal of life support treatment and do not resuscitate orders for men and women. However, as survival did not differ between men and women for the subset of patients who survived to hospital admission, these variables would be unlikely to affect our findings from the time of OHCA.
The strength of this study lies in the large sample size and the representation of the United States population. Our database represents an ethnically diverse population across the spectrum of settings from urban to rural. In contrast to prior registry studies, which have been limited by scope and sample sizes, our study did not restrict analyses to only those patients who survived to hospital admission, which would have yielded different results.
Conclusion:
In a large US-based national registry of OHCA, we found that men were less likely to survive to hospital discharge or have favorable neurological outcome across the age spectrum after adjusting for covariates. Lower overall survival rates for OHCA in men were driven by lower rates of survival to hospital admission.
Acknowledgments
The authors would like to thank biostatistics graduate students Ruizhe Chen and Shanta Ghosh for their hours of data cleaning, analysis, and help with formatting tables. We would like to thank Michael Sayre for his critical review and feedback. We would also we would like to thank Rabab Al-Araji for her continued guidance, review of the manuscript, and coordination with CARES. Lastly, we would like to extend our gratitude to the leadership of the Building Interdisciplinary Research Careers in Women Health (BIRCWH) Scholars program, Pauline Maki and Irina Buhimschi, for their support of this study and their unwavering commitment in developing early career investigators through grant support (R01HD084628) from the NIH/NICHD.
Sources of Funding:
The Cardiac Arrest Registry to Enhance Survival registry receives funding from the American Red Cross and the American Heart Association. Dr. Kotini-Shah was supported by an internal career development award by the University of Illinois at Chicago (UIC) College of Medicine and the UIC Building Interdisciplinary Research Careers in Women Health (BIRCWH) Program K12 HD101373 funded by NICHD and NIAAA. Drs. Chan, Del Rios, and Vanden Hoek receive funding from NIH and other sources for their research, but none are relevant to this observational study.
Footnotes
Conflict of Interest Disclosures:
None of the authors have any conflict of interests that were reported.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation. 2019;139(10). [DOI] [PubMed] [Google Scholar]
- 2.Vukmir RB. Prehospital Cardiac Arrest and the Adverse Effect of Male Gender, but Not Age, on Outcome. Journal of Women’s Health. 2003;12(7):667–673. [DOI] [PubMed] [Google Scholar]
- 3.Morrison LJ, Schmicker RH, Weisfeldt ML, et al. Effect of gender on outcome of out of hospital cardiac arrest in the Resuscitation Outcomes Consortium. Resuscitation. 2016;100:76–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasan OF, Al Suwaidi J, Omer AA, Ghadban W, Alkilani H, Gehani AJCMRO. The influence of female gender on cardiac arrest outcomes: a systematic review of the literature. 2014;30. [DOI] [PubMed] [Google Scholar]
- 5.Bosson N, Kaji AH, Fang A, et al. Sex Differences in Survival From Out-of-Hospital Cardiac Arrest in the Era of Regionalized Systems and Advanced Post-Resuscitation Care. J Am Heart Assoc. 2016;5(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teodorescu C, Reinier K, Uy-Evanado A, et al. Survival advantage from ventricular fibrillation and pulseless electrical activity in women compared to men: the Oregon Sudden Unexpected Death Study. Journal of Interventional Cardiac Electrophysiology. 2012;34(3):219–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herlitz J, Engdahl J, Svensson L, Young M, Ängquist K-A, Holmberg S. Is female sex associated with increased survival after out-of-hospital cardiac arrest? Resuscitation. 2004;60(2):197–203. [DOI] [PubMed] [Google Scholar]
- 8.Kitamura T, Iwami T, Nichol G, et al. Reduction in incidence and fatality of out-of-hospital cardiac arrest in females of the reproductive age. Eur Heart J. 2010;31(11):1365–1372. [DOI] [PubMed] [Google Scholar]
- 9.Johnson MA, Haukoos JS, Larabee TM, et al. Females of childbearing age have a survival benefit after out-of-hospital cardiac arrest. Resuscitation. 2013;84(5):639–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahn KO, Shin SD, Hwang SS. Sex disparity in resuscitation efforts and outcomes in out-of-hospital cardiac arrest. Am J Emerg Med. 2012;30(9):1810–1816. [DOI] [PubMed] [Google Scholar]
- 11.Ng YY, Wah W, Liu N, et al. Associations between gender and cardiac arrest outcomes in Pan-Asian out-of-hospital cardiac arrest patients. Resuscitation. 2016;102:116–121. [DOI] [PubMed] [Google Scholar]
- 12.Bray JE, Stub D, Bernard S, Smith K. Exploring gender differences and the “oestrogen effect” in an Australian out-of-hospital cardiac arrest population. Resuscitation. 2013;84(7):957–963. [DOI] [PubMed] [Google Scholar]
- 13.Haywood K, Whitehead L, Nadkarni VM, et al. COSCA (Core Outcome Set for Cardiac Arrest) in Adults: An Advisory Statement From the International Liaison Committee on Resuscitation. Circulation. 2018;137(22):e783–e801. [DOI] [PubMed] [Google Scholar]
- 14.Goto Y, Funada A, Maeda T, Okada H, Goto Y. Sex-specific differences in survival after out-of-hospital cardiac arrest: a nationwide, population-based observational study. Critical Care. 2019;23(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akahane M, Ogawa T, Koike S, et al. The effects of sex on out-of-hospital cardiac arrest outcomes. Am J Med. 2011;124(4):325–333. [DOI] [PubMed] [Google Scholar]
- 16.Winther-Jensen M, Kjaergaard J, Wanscher M, et al. No difference in mortality between men and women after out-of-hospital cardiac arrest. Resuscitation. 2015;96:78–84. [DOI] [PubMed] [Google Scholar]
- 17.Bougouin W, Dumas F, Marijon E, et al. Gender differences in early invasive strategy after cardiac arrest: Insights from the PROCAT registry. Resuscitation. 2017;114:7–13. [DOI] [PubMed] [Google Scholar]
- 18.Karlsson V, Dankiewicz J, Nielsen N, et al. Association of gender to outcome after out-of-hospital cardiac arrest – a report from the International Cardiac Arrest Registry. Critical Care. 2015;19(1):182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Winther-Jensen M, Hassager C, Kjaergaard J, et al. Women have a worse prognosis and undergo fewer coronary angiographies after out-of-hospital cardiac arrest than men. European Heart Journal: Acute Cardiovascular Care. 2017:204887261769636. [DOI] [PubMed] [Google Scholar]
- 20.McNally B, Stokes A, Crouch A, Kellermann AL, Group CS. CARES: Cardiac Arrest Registry to Enhance Survival. Annals of emergency medicine. 2009;54(5):674–683 e672. [DOI] [PubMed] [Google Scholar]
- 21.Stiell IG, Nesbitt LP, Nichol G, et al. Comparison of the Cerebral Performance Category score and the Health Utilities Index for survivors of cardiac arrest. Ann Emerg Med. 2009;53(2):241–248. [DOI] [PubMed] [Google Scholar]
- 22.Phelps R, Dumas F, Maynard C, Silver J, Rea T. Cerebral Performance Category and long-term prognosis following out-of-hospital cardiac arrest. Crit Care Med. 2013;41(5):1252–1257. [DOI] [PubMed] [Google Scholar]
- 23.Austin PC. Using the Standardized Difference to Compare the Prevalence of a Binary Variable Between Two Groups in Observational Research. Communications in Statistics - Simulation and Computation. 2009;38(6):1228–1234. [Google Scholar]
- 24.Blewer AL, McGovern SK, Schmicker RH, et al. Gender Disparities Among Adult Recipients of Bystander Cardiopulmonary Resuscitation in the Public. Circulation: Cardiovascular Quality and Outcomes. 2018;11(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mendelsohn ME, Karas RH. The Protective Effects of Estrogen on the Cardiovascular System. New England Journal of Medicine. 1999;340(23):1801–1811. [DOI] [PubMed] [Google Scholar]
- 26.Ouyang P, Michos ED, Karas RH. Hormone Replacement Therapy and the Cardiovascular System. Journal of the American College of Cardiology. 2006;47(9):1741–1753. [DOI] [PubMed] [Google Scholar]
- 27.Noppens RR, Kofler J, Grafe MR, Hurn PD, Traystman RJ. Estradiol after Cardiac Arrest and Cardiopulmonary Resuscitation is Neuroprotective and Mediated through Estrogen Receptor-β. Journal of Cerebral Blood Flow & Metabolism. 2009;29(2):277–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arking DE, Reinier K, Post W, et al. Genome-Wide Association Study Identifies GPC5 as a Novel Genetic Locus Protective against Sudden Cardiac Arrest. PLOS ONE 2010;5(3):e9879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Airaksinen KEJ, Ikäheimo MJ, Linnaluoto M, Tahvanainen KUO, Huikuri HV. Gender Difference in Autonomic and Hemodynamic Reactions to Abrupt Coronary Occlusion. Journal of the American College of Cardiology. 1998;31(2):301–306. [DOI] [PubMed] [Google Scholar]
- 30.Tomlinson AE, Nysaether J, Kramer-Johansen J, Steen PA, Dorph E. Compression force–depth relationship during out-of-hospital cardiopulmonary resuscitation. Resuscitation. 2007;72(3):364–370. [DOI] [PubMed] [Google Scholar]
- 31.Reinier K, Stecker EC, Vickers C, Gunson K, Jui J, Chugh SS. Incidence of sudden cardiac arrest is higher in areas of low socioeconomic status: A prospective two year study in a large United States community. Resuscitation. 2006;70(2):186–192. [DOI] [PubMed] [Google Scholar]
- 32.Reinier K, Thomas E, Andrusiek DL, et al. Socioeconomic status and incidence of sudden cardiac arrest. Canadian Medical Association Journal. 2011;183(15):1705–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]