Abstract
Background
The interval between inpatient hospitalization for symptomatic coronary artery disease (CAD) and post-discharge office consultation is a vulnerable period for adverse events.
Methods
Content was customized on a smartphone app-based platform for hospitalized patients receiving percutaneous coronary intervention (PCI) which included education, tracking, reminders and live health coaches. We conducted a single-arm open-label pilot study of the app at two academic medical centers in a single health system, with subjects enrolled 02/2018–05/2019 and 1:3 propensity-matched historical controls from 01/2015–12/2017. To evaluate feasibility and efficacy, we assessed 30-day hospital readmission (primary), outpatient cardiovascular follow-up, and cardiac rehabilitation (CR) enrollment as recorded in the health system. Outcomes were assessed by Cox Proportional Hazards model.
Findings
118 of 324 eligible (36·4%) 21–85 year-old patients who underwent PCI for symptomatic CAD who owned a smartphone or tablet enrolled. Mean age was 62.5 (9·7) years, 87 (73·7%) were male, 40 of 118 (33·9%) had type 2 diabetes mellitus, 68 (57·6%) enrolled underwent PCI for MI and 59 (50·0%) had previously known CAD; demographics were similar among matched historical controls. No significant difference existed in all-cause readmission within 30 days (8·5% app vs 9·6% control, ARR -1.1% absolute difference, 95% CI -7·1–4·8, p = 0·699) or 90 days (16·1% app vs 19·5% control, p = 0.394). Rates of both 90-day CR enrollment (HR 1·99, 95% CI 1·30–3·06) and 1-month cardiovascular follow up (HR 1·83, 95% CI 1·43–2·34) were greater with the app. Weekly engagement at 30- and 90-days, as measured by percentage of weeks with at least one day of completion of tasks, was mean (SD) 73·5% (33·9%) and 63·5% (40·3%). Spearman correlation analyses indicated similar engagement across age, sex, and cardiovascular risk factors.
Interpretations
A post-PCI smartphone app with live health coaches yielded similarly high engagement across demographics and safely increased attendance in cardiac rehabilitation. Larger prospective randomized controlled trials are necessary to test whether this app improves cardiovascular outcomes following PCI.
Funding
National Institutes of Health, Boston Scientific.
Clinical trial registration
NCT03416920 (https://clinicaltrials.gov/ct2/show/NCT03416920).
Keywords: Digital health, Smartphone, Apps, Outcomes
Research in context.
Evidence before this study
Although mobile health platforms have been proposed as novel health care strategies, evidence to indicate feasibility and safety in transitional care is limited. Smartphone apps with third-party health coaches to improve the inpatient to outpatient care transition for cardiovascular disease within existing clinical workflows have not been well described. Whether such apps can bridge high risk care gaps and improve adoption of guideline-supported therapies is unclear.
Added value of this study
This study reports the results of a pilot study utilizing a smartphone app with live health coaching provided at hospital discharge in 118 patients post-percutaneous coronary intervention. The app delivers customized education content, allows medication and step tracking, and provides personalized feedback from non-clinician live health coaches. This study shows that an app improves hospital discharge with a high degree of engagement and improved transition to outpatient care and therapies, such as increased cardiac rehabilitation enrollment, compared with historical controls. There was no evidence of excess cardiovascular risk with use of the app, as measured by short-term readmissions.
Implications of all the available evidence
Patients are willing to engage both with an app targeting cardiovascular disease as well as third-party health coaches with resultant improved outpatient care transition linked to improved long-term outcomes. Engagement was similar across demographics and socioeconomic indices. With recent digital health infrastructure expansion, similar smartphone apps may be feasible tools to optimize long-term risk reduction after hospital discharge.
Alt-text: Unlabelled box
1. Introduction
Myocardial infarction (MI) is a leading cause of morbidity and mortality in the United States and worldwide[1,2]. Acute management of MI comprises pharmacological and revascularization strategies to reduce recurrent ischemic events, including cardiovascular death [3,4]. Secondary prevention measures include adherence to guideline-based pharmacologic strategies, management of cardiovascular risk factors, diet and lifestyle counseling, and participation in cardiac rehabilitation. Both patient- and treatment-specific factors are associated with short-term adverse events.
Cardiac rehabilitation (CR) has been demonstrated to reduce both mortality rates and hospital admissions after coronary artery disease (CAD) events, such as MI, by providing a comprehensive secondary prevention framework in randomized controlled trials [5], [6], [7]. Despite the known benefits, barriers to CR remain, and are highlighted by low referral, enrollment and completion rates [8,9]. Non-commercial insurance status, non-white race, older age, female gender, distance to facility, medical comorbidities, and geographic socioeconomic factors are correlated with lower CR utilization rates [10,11]. Among level I guideline recommendations, CR consistently attains the lowest adherence rates [12].
Mobile health platforms have been previously proposed as novel care strategies with recent rapid adoption to minimize SARS-CoV-2 transmission [13,14]. Smartphone and internet-based programs may safely deliver elements of CR [15], [16], [17], [18]. Virtual strategies may improve access to care and facilitate lifestyle modification [19]. Smartphone applications (apps) concurrent with CR may improve CR adherence [20,21]. Randomized controlled trials to evaluate the potential synergy of digital health platforms with traditional CR are underway[22], [23], [24]. The Million Hearts Cardiac Rehabilitation Collaborative aims to improve CR enrollment itself, but whether engagement earlier through digital health strategies may support this goal is not presently known [25].
Here, we customized an app to address the inpatient-outpatient transition post-percutaneous coronary intervention (PCI) to improve enrollment of CR. Our goals were to assess feasibility of smartphone application deployment during inpatient hospitalization and evaluate efficacy of the app in improving CR enrollment as well as short-term safety of engagement with third-party health coaches compared to matched historical controls.
2. Methods
2.1. Study participants
The present study is an open-label, single-arm, multi-center clinical trial with stratified enrollment and matched historical controls (NCT03416920). The study protocol was approved by the Massachusetts General Brigham Institutional Review Board (#2017P002582).
Between 02/2018 and 05/2019, patients were identified via electronic health records on the day after PCI for either non-MI symptomatic CAD or acute MI at study sites (Massachusetts General Hospital [MGH] and Brigham and Women's Hospital [BWH]) within the Mass General Brigham (MGB, formerly Partners) healthcare system. Enrollment for symptomatic CAD, in the absence of MI, was capped at 50 participants per prespecified protocol. English-speaking patients aged 21–70 years who owned a smartphone or tablet and had a longitudinal MGB primary care provider were considered for inclusion. Inclusion criteria were later liberalized to include patients aged up to 85 years and without MGB primary care providers due to patient interest. Patients with recent (within 1 month) use of illicit substances or alcohol abuse, in-hospital acute MI, known pregnancy, dementia or cognitive delay or incarceration were excluded.
Historical controls were ascertained by query of a centralized clinical data repository to identify a historical patient population who met study eligibility criteria, except smartphone or tablet possession information was not available, who underwent PCI from 01/01/2015 through 12/31/2017 at the two study sites. Historical controls were then identified in a 1:3 manner via propensity matching [26] (nearest neighbor method, MatchIt Package v2·0·2, RStudio) on key demographic criteria including age, sex, state of residence (Massachusetts [MA]/non-MA), PCI Type (MI/symptomatic CAD), diabetes mellitus type 2 (DM2), MGB primary care provider (yes/no), insurance type (commercial/Medicaid/Medicare/other) and PCI site (MGH/BWH). Identified controls were then validated for all demographics by physician manual chart review; 11 identified controls were removed due to validation failure. Balance diagnostics were verified using standardized mean difference (cobalt package, v4·2·2, RStudio) [27].
2.2. Digital health platform
Content on a digital health platform from a Massachusetts-based health care technology company (Wellframe, Boston, MA) was customized for hospitalized patients receiving percutaneous coronary intervention [28]. The mobile health platform consisted of a patient-facing mobile app, a clinical dashboard and a suite of clinical programs with configurable rules (Supplementary Figure 1). The patient mobile app featured a personalized adaptive daily health checklist that included reminders to engage in health behaviors and a series of personalized, interactive surveys, articles and encouragement (Supplementary Text). The patient mobile app was compatible with both smartphones and tablets.
2.3. Trial procedures
Enrolled participants in the intervention arm provided written and verbal consent, and the app was installed on their personal smartphone and (if requested) tablet within 48 h of hospital discharge (Supplementary Text). Patients had active accounts on the study app for 90 days, after which each participant was contacted once by a member of the study staff. During this phone call, staff asked a series of standardized questions to determine clinical outcomes.
Manual chart review by study physicians was conducted for all participants in both the interventional and historical control arms to harmonize outcome adjudication between both groups. In both groups, planned or unplanned hospitalization within an MGB hospital with documentation of date within 30- or 90-days was used for readmission rates. Emergency department (ED) or urgent care (UC) visit with subsequent hospitalization was counted as a single readmission. Admission or presentation with documentation of a chief complaint consistent with cardiac etiology (i.e. CAD, heart failure, arrhythmia), admission requiring cardiac consultation or admission to a cardiology ward unit was coded as a cardiovascular (CV) hospitalization.
2.4. Trial outcomes
We primarily assessed the safety of the app, as assessed by 30-day all-cause hospital readmission, and secondarily 90-day all-cause hospital readmission. We also secondarily assessed enrollment in CR at an MGB site within 90 days and follow up with an MGB cardiologist within 1 month of hospitalization (to harmonize outcome ascertainment between the intervention group and the historical control group). We evaluated feasibility metrics including conversion rate, or the study enrollment rate among the total number of eligible patients. Among the participants in the intervention group, we evaluated various engagement metrics (Supplementary Table 1).
2.5. Statistical analyses
Differences in baseline characteristics between study groups were first assessed by Fisher's exact tests or two-sample t-tests (if variables were continuous). Clinical outcome risks, including 30- and 90-day all cause and CV readmission, 90-day CR enrollment, and 1-month outpatient cardiology follow-up were estimated between study groups by Cox proportional hazards models. Models were adjusted for age, sex, hypertension, hyperlipidemia, known coronary artery disease, peripheral artery disease, DM2 and smoking. Baseline was set at date of PCI, and if the aforementioned events did not occur, last follow-up was established at date of death or last follow-up within 90 days (data were right censored at 90 days if events did not occur). The proportional hazards assumption was evaluated by examining Schoenfeld residuals and was met.
Spearman correlation analysis was used to correlate engagement metrics with age, sex, reason for PCI (MI, non-MI symptomatic CAD) or known cardiovascular risk factors (smoking, hypertension, hyperlipidemia, DM2, peripheral arterial disease and known CAD). Mean daily engagement was then dichotomized into top 25th percentile and bottom 75th percentile. Multivariate ANOVA was used to correlate quartiles of engagement with 90-day CR enrollment, 90-day all cause readmission and 1-month outpatient follow up.
Statistical significance was assigned at two-sided alpha=0·05. Analyses were performed in RStudio (v1·2·5001, RStudio Inc, Boston MA; R version 3·6·1, R Foundation, Vienna, Austria). Confirmation of normality for parametric statistical tests and techniques was performed (psych package, v2·1·3, RStudio).
2.6. Sample size estimation
Initial sample size and power calculations in the trial protocol were performed based on target enrollment of 150 subjects and 1:4 matched historical controls (Supplementary Table 2). Sample size calculations were subsequently revised to 1:3 matched historical controls in the statistical analysis plan to ensure adequate balance across all matching criteria while maintaining a relatively contemporary historical time period
2.7. Ethics statement
This protocol (2017P002582) was reviewed and approved by the Mass General Brigham Human Research Committee Institutional Review Board (IRB). During the review, the IRB specifically considered the risks and anticipated benefits, if any, to subjects, the selection of subjects, the procedures for obtaining and documenting informed consent, the safety of subjects and the privacy of subjects and confidentiality of data. Informed consent was obtained from all participants enrolled in the clinical trial prior to app onboarding via electronic signature (Adobe eSign). Informed consent was waived by the IRB for historical controls.
2.8. Role of funding source
This study was supported by an investigator-initiated grant from Boston Scientific. The sponsor had no role in the design of this study, and did not have a role in the execution, analyses, interpretation of the data, writing of the report or decision to submit results for publication; however, company representatives were permitted to review and comment on the manuscript prior to submission.
3. Results
3.1. Baseline characteristics
1994 patients were screened at time of PCI at two study sites. 1026 patients were not eligible primarily due to elective PCI after cap attained (370), advanced age (209), or medical complexity deemed not suitable for study by the treating team (208) (Supplementary Figure 3). The mean age of those excluded for advanced age was 86.8 years old (standard deviation 3.6 years). The median age of the same group was 87 years (IQR 5 years). Of the 968 remaining patients who were eligible, 650 were unable to be approached by research staff to be enrolled prior to discharge largely due to logistical timing issues. Other barriers to enrollment included lack of smartphone password leading to delay in app download often leading to failed enrollment (51). Of 324 eligible patients approached, 118 (36·4%) were enrolled in the study. All 118 participants utilized the smartphone-based application. 68 of 118 (57·6%) underwent PCI for MI, and 29 of 118 (24·6%) were for ST elevation MI. Mean (standard deviation [SD]) age was 62.5 (9·7) years, 87 (73·7%) were male, 40 (33·9%) had DM2, and 59 (50·0%) had previously known CAD. Demographics were similar between enrolled participants and historical controls (Table 1). Adjusted standard mean differences for covariates were < 0·25 (Supplementary Figure 4).
Table 1.
Baseline characteristics of all subjects. Demographics across both historical controls and participants enrolled in the study app were similar. Fisher's exact testing was used to evaluate differences across groups (†Two-sample t-testing was used for continuous variables). (SD = Standard Deviation, Min = Minimum, Max = Maximum, MI = PCI for Acute Myocardial Infarction, Elective = PCI for Symptomatic Coronary Artery Disease without Acute Myocardial Infarction, MGH = Massachusetts General Hospital, BWH = Brigham and Women's Hospital, MA = Massachusetts).
| Historical Control Group (n = 343) | Intervention Group (n = 118) | p-value (Fisher's exact test) | |
|---|---|---|---|
| Age, years | |||
| Mean (SD) | 63.4 (10.3) | 62.5 (9.72) | 0.396† |
| Median [Min, Max] | 64.0 [35.0, 84.0] | 63.5 [38.0, 80.0] | |
| Sex | |||
| Male | 247 (72.0%) | 87 (73.7%) | 0.811 |
| Female | 96 (28.0%) | 31 (26.3%) | |
| PCI Type | |||
| MI | 217 (63.3%) | 68 (57.6%) | 0.322 |
| Elective | 126 (36.7%) | 50 (42.4%) | |
| Site | |||
| MGH | 267 (77.8%) | 93 (78.8%) | 0.898 |
| BWH | 76 (22.2%) | 25 (21.2%) | |
| Ethnicity | |||
| White | 273 (79.6%) | 102 (86.4%) | 0.649 |
| Black | 14 (4.1%) | 3 (2.5%) | |
| Hispanic | 11 (3.2%) | 1 (0.8%) | |
| Asian | 10 (2.9%) | 3 (2.5%) | |
| Other | 19 (5.5%) | 6 (5.1%) | |
| Unknown | 16 (4.7%) | 3 (2.5%) | |
| Insurance Type | |||
| Commercial | 204 (59.5%) | 72 (61.0%) | 0.995 |
| Medicaid | 24 (7.0%) | 8 (6.8%) | |
| Medicare | 110 (32.1%) | 37 (31.4%) | |
| Other | 5 (1.5%) | 1 (0.8%) | |
| State | |||
| MA | 279 (81.3%) | 99 (83.9%) | 0.581 |
| Non-MA | 64 (18.7%) | 19 (16.1%) | |
| MGB Primary Care Provider | |||
| Yes | 160 (46.6%) | 54 (45.8%) | 0.915 |
| No | 183 (53.4%) | 64 (54.2%) | |
| Diabetes Mellitus Type 2 | |||
| Yes | 128 (37.3%) | 40 (33.9%) | 0.579 |
| No | 215 (62.7%) | 78 (66.1%) | |
| Hypertension | |||
| Yes | 244 (71.1%) | 81 (68.6%) | 0.640 |
| No | 99 (28.9%) | 37 (31.4%) | |
| Hyperlipidemia | |||
| Yes | 266 (77.6%) | 88 (74.6%) | 0.528 |
| No | 77 (22.4%) | 30 (25.4%) | |
| Peripheral Arterial Disease | |||
| Yes | 31 (9.0%) | 7 (5.9%) | 0.337 |
| No | 312 (91.0%) | 111 (94.1%) | |
| Known Coronary Artery Disease | |||
| Yes | 156 (45.5%) | 59 (50.0%) | 0.649 |
| No | 187 (54.5%) | 59 (50.0%) | |
3.2. Study app engagement
Engagement with the app, as defined by completion of at least one task either daily or weekly, fell in a parabolic distribution (Supplementary Figure 5). Patients set up a mean (SD) of 3·45 (6·23) medication reminders per day. Patients sent a median [IQR] of 1 [9] message and the clinical care team sent a median [IQR] of 12 (11) messages per participant. The number of messages sent by health coaches was highly correlated with the number of messages sent by individual participants (Spearman r2=0·82, p<2·2 × 10−16, Supplementary Figure 6). Spearman correlation analyses revealed no significant associations between number of messages per participant and age, sex or known cardiovascular risk factors or PCI indication.
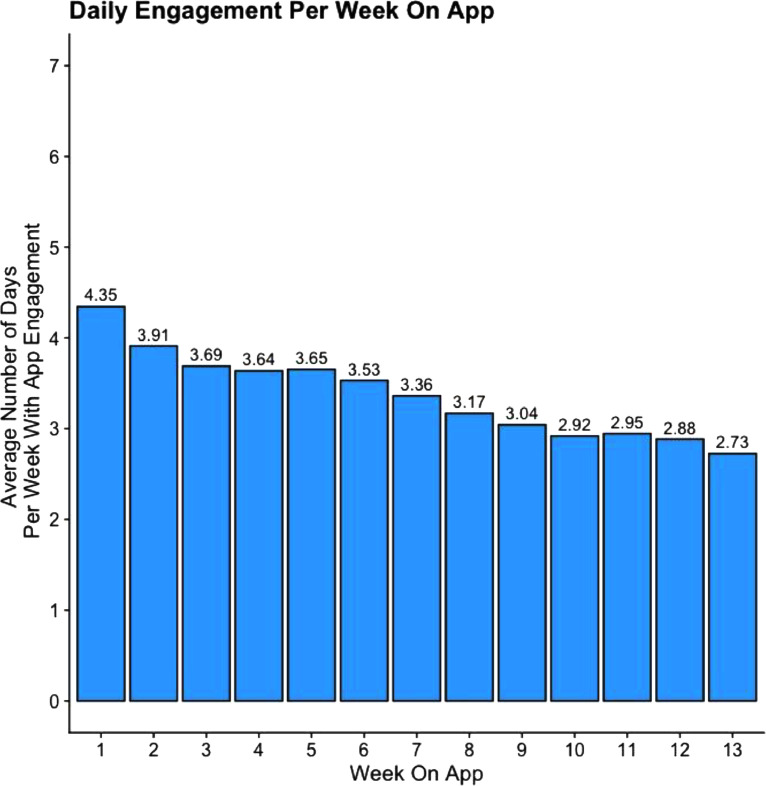
Engagement rates were durable across 30- and 90-day periods (Table 2). At 30- and 90-days, 68 (57·6%) and 63 (53·5%) participants respectively opened at least 50% of the articles suggested by the app. At 30- and 90-days, 55 (46·6%) and 49 (41·5%) participants respectively completed at least 50% of the surveys sent via the app. At 30- and 90-days, 62 (52·5%) and 65 (55·1%) participants respectively reported in the app completing their physical activity goal at least 50% of the time. At 30- and 90-days, 73 (61·9%) and 69 (58·5%) participants had completed at least one task on 50% or more of the days using app. At 30- and 90-days, 95 (80·5%) and 79 (66·9%) participants had completed at least one task on 50% or more of the weeks using app. Participant engagement peaked in the first week with participants logging in an average 4.35 days and tapered down to logging in 2.73 days per week by the last week of the study period (Fig. 1). Spearman correlation analyses revealed no significant correlations between engagement metrics and age, sex or known cardiovascular risk factors (Supplementary Figure 7). 43 out of 45 (95·6%) patients who responded to the in-app end of study survey felt that the application improved their control over their health (Supplementary Table 3). 39 out of 75 (52·0%) patients who answered the end of study phone call were still using the app at 90 days and 38 (50·7%) said they would continue using the app if they could.
Table 2.
Engagement with app. Engagement metrics were similar between the 0–30 and 0–90 day study time periods, suggesting stable usage of the app amongst users who were engaged early (within 30 days).
| ENGAGEMENT METRIC | TIME PERIOD | COMPLETION RATE # (%) |
||
|---|---|---|---|---|
| >25% | >50% | >75% | ||
| Content Completion (Percentage of articles opened) | 0–30 Days | 84 (71.2%) | 68 (57.6%) | 52 (44.1%) |
| 0–90 Days | 78 (66.1%) | 63 (53.4%) | 41 (34.7%) | |
| Medication Adherence (Percentage of medication reminder tasks completed) | 0–30 Days | 40 (81.6%)* | 39 (79.6%)* | 33 (67.3%)* |
| 0–90 Days | 42 (85.7%)* | 40 (81.6%)* | 29 (59.2%)* | |
| Survey Completion (Percentage of survey tasks completed) | 0–30 Days | 65 (55.1%) | 55 (46.6%) | 42 (35.6%) |
| 0–90 Days | 62 (52.5%) | 49 (41.5%) | 32 (27.1%) | |
| Physical Activity Completion (Percentage of self-reported days physical activity goal was met) | 0–30 Days | 74 (62.7%) | 62 (52.5%) | 51 (43.2%) |
| 0–90 Days | 73 (61.9%) | 65 (55.1%) | 51 (43.2%) | |
| Daily Engagement (Percentage of days with completion of at least one task) | 0–30 Days | 73 (61.9%) | 64 (54.2%) | 54 (45.8%) |
| 0–90 Days | 69 (58.5%) | 56 (47.5%) | 43 (36.4%) | |
| Weekly Engagement (Percentage of weeks with at least one day of completion of one task) | 0–30 Days | 95 (80.5%) | 78 (66.1%) | 70 (59.3%) |
| 0–90 Days | 79 (66.9%) | 70 (59.3%) | 63 (53.4%) | |
*Medication adherence percentage calculated from 49 participants who set up reminders.
Fig. 1.
Weekly app engagement. Patients’ interaction with the app decreased gradually over time but the overall rate was stable amongst patients who engaged early (within first 30 days). Engagement peaked at 4.35 days in the first week and gradually decreased to 2.73 days by the last week of the study period. (Engagement = a day with completion of at least one task; Week = 7-day period starting from enrollment).
3.3. Study intervention outcomes
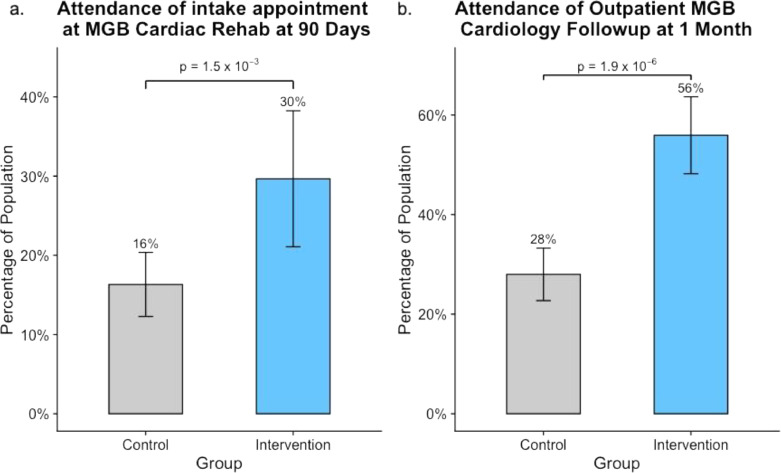
There was an increased rate in 90-day enrollment in CR at an MGB site (29·7% vs 16·3%, p = 1·5 × 10−3) (Fig. 2a) for the intervention group versus historical controls. Among those who enrolled in CR, we observed that 21/35 (60·0%) in the intervention group and 23/56 (41·1%) in the historical control group completed CR (p = 0·09). We observed consistent relationships within both sites (Supplementary Figure 8). Among those who enrolled in CR, demographics were largely similar between the intervention and historical control groups (Supplementary Table 4).
Fig. 2.
A smartphone app and longitudinal cardiovascular care. (a) Two-fold increase in attendance of cardiac rehabilitation intake and (b) two-fold increase in 1-month outpatient cardiovascular follow up in the intervention group. Error bars represent confidence intervals. (MGB = Mass General Brigham).
For the intervention arm, phone follow-up was also performed and successful for 75 (63·5%) participants. Of those in the intervention group who were successfully contacted by phone, 46 (61·3%) enrolled in CR at any site within 90 days. In this group, 22 (29·3%) specifically participated in CR at an MGB site.
66 (55·9%) participants in the intervention group attended 1-month outpatient MGB cardiology follow-up compared to 96 (28·0%) among historical controls (p = 1·9 × 10−8) (Fig. 2b). For those who attended a 1-month outpatient MGB cardiology follow-up, the mean number of days from PCI date to first outpatient MGB cardiology follow-up was mean (SD) 18·1 (7·43) in the intervention group and 19·1 (7·61) in the historical control group (p = 0·39). Of those in the intervention group who were successfully contacted by phone, 73 of 75 (97·3%) followed up with a cardiologist at any site. In this group, 58 (77·3%) followed up at an MGB cardiology site.
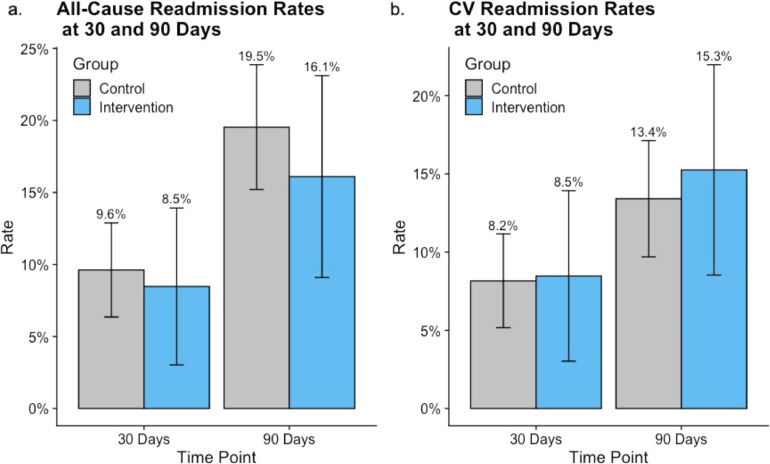
We observed no significant difference in all-cause readmission rates within 30 or 90 days at an MGB hospital between the historical control and intervention groups (33 [9·6%] vs 10 [8·5%], p = 0·699; 67 [19·5%] vs 19 [16·1%], p = 0·394) (Fig. 3a). All 30-day readmissions were noted to be unplanned; 1 of 67 (1·5%) and 1 of 19 (5·2%) 90-day readmissions were planned in the historical control and intervention groups respectively. We also observed no significant difference in 30- or 90-day cardiovascular-related readmission rates between the historical control and intervention groups (28 [8·2%] vs 10 [8·5%], p = 0·930; 46 [13·4%] vs 18 [15·3%], p = 0·191 respectively) (Fig. 3b). In the intervention arm, daily engagement rate did not predict 90-day all cause readmission (p = 0·289), 90-day CR enrollment (p = 0·969) nor 1-month outpatient cardiology follow-up (p = 0·803) at MGB facilities (Supplementary Figure 9).
Fig. 3.
Use of a smartphone app and readmission rates post-PCI. No significant difference in (a) all-cause readmissions or (b) cardiovascular readmission to MGB facilities at either 30- or 90-days post-PCI. Error bars represent confidence interval.
4. Discussion
The present smartphone app including third-party health coaches helped bridge a care gap shortly after hospital discharge for PCI and facilitated participation in CR. 1 in 3 individuals approached accepted the app and 52% of individuals surveyed were still using the app daily at 90 days. For every 8 individuals who used the app, 1 additional individual enrolled in CR compared to historical controls. Importantly, use of an app with third-party health coaches did not lead to excess short-term readmissions in the studied population.
Our results permit several conclusions regarding smartphone application use for cardiovascular disease applications and generate new hypotheses regarding the prevention of cardiovascular disease using digital health strategies. First, onboarding patients for digital health care solutions during inpatient hospitalization is feasible. Prior digital health initiatives have largely targeted patients in the ambulatory setting or at time of enrollment at CR with the aim of promoting preventive activities and promoting long-term maintenance [22]. However, the weeks to months between hospital discharge and outpatient CR or cardiovascular follow-up after the index event represents a missed opportunity [29]. Our study indicates an opportunity to initiate comprehensive cardiovascular disease prevention earlier and facilitate CR enrollment [9,23]. Use of EHR-integrated digital health tools to engage patients and clinicians in discharge planning tasks has been shown to be feasible, acceptable and valuable [30]. Therefore, creating standardized clinical workflows to incorporate onboarding with patient-facing digital health tools at time of discharge may enhance usability of patient discharge paperwork and potentially clinical outcomes. The largest barrier to enrollment in this study was logistical issues related to rapid patient discharge which may potentially be mitigated by incorporation of combined telemedicine and in person recruitment protocols in future.
Second, our study shows that patients are willing to engage both with an app targeting cardiovascular disease as well as third-party health coaches. Previous digital health interventions involving automated one-way texting/messaging and structured questionnaires have had mixed success in promoting durable lifestyle changes [31]. Although behavioral modification studies and patient opinions have suggested that personalized virtual feedback is felt to be the most effective means for enacting change, very few studies have been able to create individualized interventions as they require human guidance [17,32,33]. The use of physicians or physician extenders in the role of virtual health coaches within prior studies of digital health interventions in cardiology has allowed for personalization at the cost of limited scalability [34]. Our study is novel in its utilization of third-party health coaches external to the health system to support patient engagement with minimal burden to clinical staff. Engagement with our framework was markedly greater compared to population-based preventive cardiovascular interventions to-date using apps. In a study of nearly 50,000 individuals in the community, surveys and study procedures over 7 days were only completed by 3–10% of participants [35,36]. Apps aligned with the healthcare teams that provide passive and active engagement designed for patients with cardiovascular disease may provide more durable effects.
Third, patient engagement with digital health tools may not be predicted by traditional cardiovascular risk factors including comorbidities. There was notably no difference in engagement with the app by age despite preconceived notions of technologic proficiency in older patients. There are some reports of older adults (age >65 years) reporting difficulty with digital health technology but an increasing body of evidence suggests that thoughtful application of technology may be well received in this population [37], [38], [39], [40]. Further study is needed to determine whether newer mobile technologies can be adopted into populations previously not represented, such as the elderly and medically complex, who have historic disparities in CR enrollment [11,17].
Fourth, despite the resource-rich environment of the app, there was still increased patient engagement with healthcare teams as measured by outpatient follow-up rate and increased adherence to guideline-supported care plans, such as CR enrollment, compared with historic controls. There was no evidence of excess cardiovascular risk, as measured by short-term readmissions, suggesting that participants did not use the app as a surrogate for care. Whether this ‘bridging’ strategy may optimize long-term risk reduction through facilitating CR enrollment, cardiovascular follow-up, patient education, and motivational coaching requires longer term study in randomized controlled trials.
While our study has several strengths, it also has many limitations. First, the participants in this study may not be fully representative of all patients with CAD. Eligibility of participants required both smartphone ownership and app usage which may have added selection and response bias to these results. Additionally, the 118 participants who opted to enroll may not be reflective of the entire eligible population as participants who opt to enroll in this novel study may be more engaged in health maintenance compared to those who declined. However, since no significant difference was observed in readmission rates, selection bias may not have been a major factor in our study. Enrollment rates at present were similar to other comparable studies but selection bias cannot be definitively excluded without the use of randomized control trials [41], [42], [43]. Second, reliance on historical controls with propensity matching may lead to imbalance of unavailable phenotypes or systematic healthcare changes. We focused on relatively short duration, contemporary time periods at two sites, and matched used several clinical features related to health-related behaviors to mitigate this risk [10]. Persistently low rates of readmission for the two groups indicate the lack of major new systematic endeavors in addressing readmission rates between the two periods. Additionally, there were no other formal systemic endeavors targeting CR enrollment rates within the healthcare system studied. Third, use of historical controls permitted us to only ascertain clinical events from the electronic health record and thus, from within our health system. Power is maximized since the studied health system is the largest in New England, but this may have led to reduced absolute rates observed. If similar trends were observed outside of the healthcare system, then greater absolute risk differences may be truly present with the current data thus biasing our results to the null. Fourth, given the small sample size and short-term follow up, we cannot exclude the possibility of reduced power in the assessment of clinical cardiovascular outcomes. Finally, we must also acknowledge the potential for smartphone-based technology to worsen current inequities in healthcare (the “digital divide”) [44,45].
In conclusion, a post-PCI smartphone app, with live health coaches, deployed upon discharge yields similarly high engagement across demographics. Compared to historical controls, use of the app did not reduce short-term hospital readmission but was associated with two-fold higher attendance in CR. These results are limited by potentially reduced power, single arm open-label design, potential selection bias in eligibility and enrollment, and the use of historical controls for comparison. Prospective randomized controlled trials are necessary to test whether this digital health platform improves cardiovascular outcomes following PCI.
Contributors
All co-authors had access to the data. P.N., P.F., and K.P. had full access to all the data in the study and verify the integrity of the data. K.P. conducted all data analysis and drafted the first draft of the manuscript with edits from P.N. P.N and K.P. take responsibility for the accuracy of the data analysis. All co-authors reviewed and approved the final manuscript prior to submission.
Declaration of Competing Interest
The study was supported by an investigator-initiated grant to P.N. from Boston Scientific. The sponsor had no role in the design of this study, and did not have a role in the execution, analyses, interpretation of the data, or decision to submit results for publication; however, company representatives were permitted to review and comment on the manuscript prior to submission. P.N. also reports investigator-initiated grants from Apple, Amgen, AstraZeneca, and Novartis; he is a scientific advisor to Apple, Genentech, Novartis, AstraZeneca, Forsite Labs and Blackstone Life Sciences, and he reports spousal employment and equity in Vertex. S.W. reports grants from Amgen, Arena, AstraZeneca, Bristol Myers Squibb, Daiichi Sankyo, Eisai, Eli Lilly, Janssen, Merck and Sanofi-Aventis and consulting fees from ARENA, AstraZeneca, Aegerion, Allergan, Angelmed, Boehringer-Ingelheim, Boston Clinical Research Institute, Bristol Myers Squibb, Daiichi Sankyo, Eisai, Eli Lilly, Icon Clinical, Janssen, Lexicon, Merck, Servier, St Jude Medical, and Xoma. S.W. also reports personal membership in the TIMI Study Group which receives institutional research grant support through Brigham and Women's Hospital as well as spousal employment in Merck.
Acknowledgments
K.P. is supported by a grant from the National Heart, Lung, and Blood Institute (5-T32HL007208-43). P.N. is supported by grants from the National Heart, Lung, and Blood Institute (R01HL142711, R01HL148565, R01HL148050) and a Hassenfeld Award from Massachusetts General Hospital. The present study was primarily supported by an investigator-initiated grant to P.N. from Boston Scientific and a grant from the National Heart, Lung, and Blood Institute (5-T32HL007208-43) supporting K.P.
Data sharing statement
A data dictionary defining types of data collected during this study will be made available to others in supplementary text with publication. Individual level participant data will not be made available to others due to privacy concerns. Study protocol and statistical analysis plan will be made available to any academic researchers who request it from corresponding author.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.ebiom.2021.103593.
Appendix. Supplementary materials
References
- 1.Lozano R., Naghavi M., Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.S. Virani Salim, Alvaro Alonso, Aparicio Hugo J. Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 3.O'Gara Patrick T., Kushner Frederick G., Ascheim Deborah D. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary. Circulation. 2013;127(4):529–555. doi: 10.1161/CIR.0b013e3182742c84. [DOI] [PubMed] [Google Scholar]
- 4.Amsterdam E.A., Wenger N.K., Brindis R.G. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;130(25) doi: 10.1161/CIR.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 5.Heran B.S., Chen J.M., Ebrahim S. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011;(7) doi: 10.1002/14651858.CD001800.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawler P.R., Filion K.B., Eisenberg M.J. Efficacy of exercise-based cardiac rehabilitation post–myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am Heart J. 2011;162(4):571–584. doi: 10.1016/j.ahj.2011.07.017. e2. [DOI] [PubMed] [Google Scholar]
- 7.Anderson L., Oldridge N., Thompson D.R. Exercise-based cardiac rehabilitation for coronary heart disease: cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67(1):1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 8.Johnson N., Fisher J., Nagle A., Inder K., Wiggers J. Factors associated with referral to outpatient cardiac rehabilitation services. J Cardpulm Rehabil. 2004;24(3):165–170. doi: 10.1097/00008483-200405000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Aragam K.G., Dai D., Neely M.L. Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol. 2015;65(19):2079–2088. doi: 10.1016/j.jacc.2015.02.063. [DOI] [PubMed] [Google Scholar]
- 10.Sukul D., Seth M., Barnes G.D. Cardiac Rehabilitation use after percutaneous coronary intervention. J Am Coll Cardiol. 2019;73(24):3148–3152. doi: 10.1016/j.jacc.2019.03.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sérvio T.C., Britto R.R., de Melo Ghisi G.L. Barriers to cardiac rehabilitation delivery in a low-resource setting from the perspective of healthcare administrators, rehabilitation providers, and cardiac patients. BMC Health Serv Res. 2019;19 doi: 10.1186/s12913-019-4463-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dahhan A., Maddox W.R., Sharma G.K. The gaps in cardiac rehabilitation referral: the elephant in the room. J Am Coll Cardiol. 2015;66(22):2574. doi: 10.1016/j.jacc.2015.06.1359. [DOI] [PubMed] [Google Scholar]
- 13.Scherrenberg M., Wilhelm M., Hansen D. The future is now: a call for action for cardiac tele-rehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2020 doi: 10.1177/2047487320939671. Published online July 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keesara S., Jonas A., Schulman K. Covid-19 and Health Care's Digital Revolution. N Engl J Med. 2020;382(23):e82. doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- 15.Aspry K., Wu W.-.C., Salmoirago-Blotcher E. Cardiac rehabilitation in patients with established atherosclerotic vascular disease: new directions in the era of value-based healthcare. Curr Atheroscler Rep. 2016;18(2):10. doi: 10.1007/s11883-016-0561-x. [DOI] [PubMed] [Google Scholar]
- 16.Dalal H.M., Zawada A., Jolly K., Moxham T., Taylor R.S. Home based versus centre based cardiac rehabilitation: cochrane systematic review and meta-analysis. BMJ. 2010:340. doi: 10.1136/bmj.b5631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frederix I., Caiani E.G., Dendale P. ESC e-cardiology working group position paper: overcoming challenges in digital health implementation in cardiovascular medicine. Eur J Prev Cardiol. 2019;26(11):1166–1177. doi: 10.1177/2047487319832394. [DOI] [PubMed] [Google Scholar]
- 18.Schmid J.-.P. Telehealth during COVID-19 pandemic: will the future last? Eur J Prev Cardiol. 2020:zwaa016. doi: 10.1093/eurjpc/zwaa016. Published online September 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton S.J., Mills B., Birch E.M., Thompson S.C. Smartphones in the secondary prevention of cardiovascular disease: a systematic review. BMC Cardiovasc Disord. 2018;18(1):25. doi: 10.1186/s12872-018-0764-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu L., Li F., Zhou C., Li J., Hong C., Tong Q. The effect of mobile applications for improving adherence in cardiac rehabilitation: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2019;19 doi: 10.1186/s12872-019-1149-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su J.J., Yu D.S.F., Paguio J.T. Effect of eHealth cardiac rehabilitation on health outcomes of coronary heart disease patients: a systematic review and meta-analysis. J Adv Nurs. 2020;76(3):754–772. doi: 10.1111/jan.14272. [DOI] [PubMed] [Google Scholar]
- 22.Lunde P., Bye A., Bergland A., Nilsson B.B. Effects of individualized follow-up with a smartphone-application after cardiac rehabilitation: protocol of a randomized controlled trial. BMC Sports Sci Med Rehabil. 2019;11 doi: 10.1186/s13102-019-0148-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yudi M.B., Clark D.J., Tsang D. SMARTphone-based, early cardiac REHABilitation in patients with acute coronary syndromes [SMART-REHAB Trial]: a randomized controlled trial protocol. BMC Cardiovasc Disord. 2016;16(1) doi: 10.1186/s12872-016-0356-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gonzalez M., Sjölin I., Bäck M. Effect of a lifestyle-focused electronic patient support application for improving risk factor management, self-rated health, and prognosis in post-myocardial infarction patients: study protocol for a multi-center randomized controlled trial. Trials. 2019;20 doi: 10.1186/s13063-018-3118-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pirruccello James P., Traynor Kathleen, Aragam Krishna G. “Road Map” to Improving enrollment in cardiac rehabilitation: identifying barriers and evaluating alternatives. J Am Heart Assoc. 2017;6(10) doi: 10.1161/JAHA.117.007468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ho D.E., Imai K., King G., Stuart E.A. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Polit Anal. 2007;15(3):199–236. doi: 10.1093/pan/mpl013. [DOI] [Google Scholar]
- 27.Zhang Z., Kim H.J., Lonjon G., Zhu Y. Balance diagnostics after propensity score matching. Ann Transl Med. 2019;7(1) doi: 10.21037/atm.2018.12.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Forman D.E., LaFond K., Panch T., Allsup K., Manning K., Sattelmair J. Utility and efficacy of a smartphone application to enhance the learning and behavior goals of traditional cardiac rehabilitation: a feasibility study. J Cardiopulm Rehabil Prev. 2014;34(5):327–334. doi: 10.1097/HCR.0000000000000058. [DOI] [PubMed] [Google Scholar]
- 29.Varnfield M., Karunanithi M., Lee C.-.K. Smartphone-based home care model improved use of cardiac rehabilitation in postmyocardial infarction patients: results from a randomized controlled trial. Heart. 2014;100(22):1770–1779. doi: 10.1136/heartjnl-2014-305783. [DOI] [PubMed] [Google Scholar]
- 30.Fuller T.E., Pong D.D., Piniella N. Interactive digital health tools to engage patients and caregivers in discharge preparation: implementation study. J Med Internet Res. 2020;22(4) doi: 10.2196/15573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williamson C., Kelly P., Niven A., Graham Baker P, Mutrie N. Get the message? A scoping review of physical activity messaging. Int J Behav Nutr Phys Act. 2020;17 doi: 10.1186/s12966-020-00954-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salvi D., Ottaviano M., Muuraiskangas S. An m-Health system for education and motivation in cardiac rehabilitation: the experience of HeartCycle guided exercise. J Telemed Telecare. 2018;24(4):303–316. doi: 10.1177/1357633X17697501. [DOI] [PubMed] [Google Scholar]
- 33.DeSmet A., De Bourdeaudhuij I., Chastin S., Crombez G., Maddison R., Cardon G. Adults’ preferences for behavior change techniques and engagement features in a mobile app to promote 24-hour movement behaviors: cross-sectional survey study. JMIR MHealth UHealth. 2019;7(12):e15707. doi: 10.2196/15707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harzand A., Witbrodt B., Davis-Watts M.L. Feasibility of a smartphone-enabled cardiac rehabilitation program in male veterans with previous clinical evidence of coronary heart disease. Am J Cardiol. 2018;122(9):1471–1476. doi: 10.1016/j.amjcard.2018.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McConnell M.V., Shcherbina A., Pavlovic A. Feasibility of Obtaining Measures of Lifestyle From a Smartphone App: the MyHeart Counts Cardiovascular Health Study. JAMA Cardiol. 2017;2(1):67–76. doi: 10.1001/jamacardio.2016.4395. [DOI] [PubMed] [Google Scholar]
- 36.Shcherbina A., Hershman S.G., Lazzeroni L. The effect of digital physical activity interventions on daily step count: a randomized controlled crossover sub-study of the MyHeart counts cardiovascular health study. Lancet Digit Health. 2019;1(7):e344–e352. doi: 10.1016/S2589-7500(19)30129-3. [DOI] [PubMed] [Google Scholar]
- 37.Bostrom J., Sweeney G., Whiteson J., Dodson J.A. Mobile health and cardiac rehabilitation in older adults. Clin Cardiol. 2019;43(2):118–126. doi: 10.1002/clc.23306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kumar K.R., Pina I.L. Cardiac rehabilitation in older adults: new options. Clin Cardiol. 2019;43(2):163–170. doi: 10.1002/clc.23296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jaana M., Paré G. Comparison of Mobile Health Technology Use for Self-Tracking Between Older Adults and the General Adult Population in Canada: cross-Sectional Survey. JMIR MHealth UHealth. 2020;8(11):e24718. doi: 10.2196/24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Richard E., Moll van Charante E.P., Hoevenaar-Blom M.P. Healthy ageing through internet counselling in the elderly (HATICE): a multinational, randomised controlled trial. Lancet Digit Health. 2019;1(8):e424–e434. doi: 10.1016/S2589-7500(19)30153-0. [DOI] [PubMed] [Google Scholar]
- 41.Chow C.K., Redfern J., Hillis G.S. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA. 2015;314(12):1255–1263. doi: 10.1001/jama.2015.10945. [DOI] [PubMed] [Google Scholar]
- 42.Quinn C.C., Shardell M.D., Terrin M.L., Barr E.A., Ballew S.H., Gruber-Baldini A.L. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34(9):1934–42. doi:10.2337/dc11-0366 [DOI] [PMC free article] [PubMed]
- 43.Gremaud Allene L., Carr Lucas J., Simmering Jacob E. Gamifying accelerometer use increases physical activity levels of sedentary office workers. J Am Heart Assoc. 2018;7(13) doi: 10.1161/JAHA.117.007735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Eberly L.A., Khatana S.A.M., Nathan A.S. Telemedicine outpatient cardiovascular care during the COVID-19 pandemic: bridging or opening the digital divide? Circulation. 2020;142(5):510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Narla A., Paruchuri K., Natarajan P. Digital health for primary prevention of cardiovascular disease: promise to practice. Cardiovasc Digit Health J. 2020;1(2):59–61. doi: 10.1016/j.cvdhj.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.