Abstract
Background
Although falls are common, costly, and often preventable, emergency department (ED)-initiated fall screening and prevention efforts are rare. The Geriatric Emergency Medicine Applied Research Falls core (GEAR-Falls) was created to identify existing research gaps and to prioritize future fall research foci.
Methods
GEAR’s 49 transdisciplinary stakeholders included patients, geriatricians, ED physicians, epidemiologists, health services researchers, and nursing scientists. We derived relevant clinical fall ED questions and summarized the applicable research evidence, adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Scoping Reviews. The highest priority research foci were identified at the GEAR Consensus Conference.
Results
We identified two clinical questions for our review (1) fall prevention interventions (32 studies) and (2) risk stratification and falls care plan (19 studies). For (1) 21/32 (66%) of interventions were a falls risk screening assessment and 15/21 (71%) of these were combined with an exercise program or physical therapy. For (2) eleven fall screening tools were identified, but none were feasible and sufficiently accurate for ED patients. For both questions, the most frequently reported study outcome was recurrent falls, but various process and patient/clinician-centered outcomes were used. Outcome ascertainment relied on self-reported falls in 18/32 (56%) studies for (1) and 9/19 (47%) studies for (2).
Conclusion
Harmonizing definitions, research methods and outcomes is needed for direct comparison of studies. The need to identify ED-appropriate fall risk assessment tools and role of Emergency Medical Services (EMS) personnel persists. Multifactorial interventions, especially involving exercise, are more efficacious in reducing recurrent falls, but more studies are needed to compare appropriate bundle combinations. GEAR prioritizes Five research priorities: (1) EMS role in improving fall-related outcomes, (2) identifying optimal ED fall assessment tools, (3) clarifying patient-prioritized fall interventions and outcomes, (4) standardizing uniform fall ascertainment and measured outcomes, and (5) exploring ideal intervention components.
Keywords: Falls, geriatrics, emergency department, physical therapy, pharmacist, risk assessment, geriatric nurse, multifactorial, alert devices
BACKGROUND
Over 2.8 million older adults (aged 65 years and older) in the United States visit the emergency department (ED) annually after a fall,1 defined as the involuntary and abrupt contact with a ground or lower level.2 Falls in older adults are associated with high injury severity, reduced mobility, functional decline and death,3,4 the rate of deaths from falls among persons aged ≥65 years increased 31% from 2007 to 2016.5 Many patients experience recurrent falls after ED discharge: approximately 10% of older adults experience another fall within 20 days,6 and 2.4% experience another fall-related ED visit within 30 days, which sharply increases to 25% at one year.7 Furthermore, mortality rates for older adults that visit the ED for a fall increase from 2% at seven days to 4.4% at 30 days and significantly increase to 15% at one year following the initial ED visit.8 Although falls are common, costly,9 and recent evidence suggest that falls may be preventable in the ED setting,4,7,10 ED-initiated fall screening and prevention efforts are not widespread,11 perhaps due to the ED environment; limited resources in time and staffing are barriers to implementing impactful change in ED management of falls.12–14
Given the mortality and morbidity associated with falls, there has been interest within emergency medicine to address falls and initiate ED-based fall prevention efforts. The Society for Academic Emergency Medicine (SAEM) Geriatric Emergency Medicine Task Force recognized fall prevention as one of three priority areas over ten years ago.15 SAEM’s Task Force recommended five falls research priorities: (1) identification of patients at high-risk for falls, (2) ED-delivered fall prevention, (3) examining acute care versus rapid response services for injurious falls reduction, (4) determining feasibility of hospital-at-home models for managing high-risk patients with falls, and (5) electronic systems to facilitate care communication between emergency and primary physicians about high-risk individuals.15 Furthermore, the 2010 guidelines for emergency medicine resident core competencies specifically addressed the need for understanding how to recognize fall risk factors and prevent falls.16 In addition, the American College of Emergency Physicians’ Geriatric Emergency Department (GED) Accreditation process cites fall prevention as a potential quality improvement project for accreditation, highlighting falls as a critical topic in the ED care of older adults.17 Finally, the 2013 multi-organizational GED Guidelines recommended initiation of multifactorial fall evaluations for ED patients with falls.18 However, despite these recommendations to prioritize efforts targeting falls, there is a lack of consensus about which ED fall assessment, management tools, and/or interventions are feasible and efficacious in the ED.19 Additionally, a recent large multi-center non-ED study, Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE), failed to reduce fall injuries despite complex individualized interventions and has left clinicians and policymakers skeptical that fall prevention can be adequately achieved.20,21
In response to such gaps in the geriatric emergency medicine literature, we formed the Geriatric Emergency care Applied Research (GEAR) Network, an interdisciplinary group of clinicians, researchers, and patient advocates, to identify and examine clinical questions relevant to five geriatric emergency medicine domains: falls, cognitive impairment, medication safety, elder abuse, and care transitions. These domains were identified based on the recommendations of SAEM and the GED Guidelines, as well as priorities established by GEAR stakeholders. The GEAR-Cognitive Impairment 22 and GEAR-Elder Abuse23 recommendations have already been published. The Geriatric Emergency care Applied Research-Falls (GEAR-Falls) subgroup’s primary objective was to systematically identify, synthesize, and prioritize high-yield research priorities for older adult falls screening and prevention in the ED and pre-hospital setting. A secondary objective was to report ED best practices for fall risk recognition and prevention based on a scoping review of pertinent emergency medicine research.
METHODS
Study Design
Experts from geriatric interest groups, such as the SAEM, the American Geriatrics Society (AGS), and the Gerontological Society of America, with an interest in emergency and aging research were recruited to serve on the GEAR Task Force. Additional researchers were selected based on their publication history in these domains. GEAR-Falls consisted of twelve members: A geriatrician (WH), six emergency physician scientists (UH, CC, SWL, SF, CG, EG), an epidemiologist (EC), a health services researcher (AL), nursing scientists (KS, AM), and a graduate student (NH).
The GEAR-Falls subgroup performed a scoping review adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews reporting guidelines.24 GEAR-Falls held monthly meetings to discuss research priorities and develop clinical questions relevant to falls based on clinical expertise and knowledge of preexisting research.
PICO (Patient-Intervention-Control-Outcome) Questions
GEAR-Falls derived and refined the following PICO questions:
| PICO-1 |
Population: ≥ 60 years old individuals presenting with a fall for ED care. Intervention: Fall prevention interventions (may include multifactorial risk reduction, medication review, exercise training, models of care (hospital-at-home and others) in ED or peri-ED period). We defined peri-ED as care provided during the ED visit or by Emergency Medical Services (EMS) before or after the ED visit. Comparison: Standard of care. Outcome: Quality of ED care metrics, ED operations outcomes (e.g., ED length of stay); patient-centered outcomes (e.g., ED returns for falls, future falls, fear of falling, or functional decline, long-term supports or institutionalization). |
| PICO-2 |
Population: ≥ 60 years old individuals from any pre-ED and ED setting (pre-hospital, paramedic, EMS, ED). Intervention: Risk stratification and falls care plan. Comparison: No risk stratification and no falls care plan. Outcome: ED referral (if from pre-ED settings), quality of ED care metrics (e.g., preventable ED recidivism, 30-day hospitalization rates), ED operations outcomes (e.g., ED length of stay, cost), patient-centered outcomes (e.g., ED returns for falls, future falls, fear of falling, functional decline, long-term supports or institutionalization). |
| PICO-3 |
Population: ≥ 60 years old individuals presenting with a fall for ED care. Intervention: Specific risk factors (such as polypharmacy, frailty etc.). Comparison: None. Outcome: Recurrent falls, fall injury, functional decline, acute care utilization (ED, hospital visit), long-term institutionalization, mortality (Prognosis question). |
GEAR-Falls identified exemplar articles for each PICO question and surveyed 33 investigators from all five GEAR cores to prioritize the PICO questions via teleconference discussions and online voting. PICO questions 1 and 2 were selected as highest priority.
Search Strategy
PICO-1 and PICO-2 and the exemplar articles for both formed the basis of an electronic search strategy devised by a medical librarian (MD) for Ovid Medline 1946-, Embase 1947-, CINAHL 1937-, and Cochrane Central Register of Controlled Trials. All search strategies are listed in Supplement 1.
Study Selection and Data Abstraction
For each PICO question, two authors independently reviewed the titles and abstracts for the search results of PICO-1 and PICO-2 to identify studies that met the inclusion criteria. Inclusion criteria for PICO-1 were fall interventions for adults over age 60 intended to improve quality of care, ED operations, or patient-centered outcomes. Inclusion criteria for PICO-2 were adults over age 60 with a quantitative evaluation of fall risk stratification and a falls care plan.
As PICO-1 had a large number of studies to filter through and adjudicate, PICO-1 studies were divided into three segments using the alphabetical order of the manuscript titles, each segment was reviewed and adjudicated by two independent reviewers (PICO-1 = Segment A: SF, KS; Segment B: CG, AM; Segment C: EC, AL; PICO-2 = WH, EG). Although authors of this manuscript also authored literature that is included in this review, including AL and CC, neither was assigned to review abstracts they had written. After filtering based on study title and abstract was completed, and before starting adjudication, we calculated the unweighted Cohen’s kappa to quantify inter-rater agreement between all reviewers of PICO-1 and the two reviewers of PICO-2. During adjudication, we resolved disagreements on which studies to include or exclude via email or telephone discussions between reviewers. A pre-planned third adjudicator (UH) resolved remaining discrepancies. Final articles were abstracted independently by six investigators (PICO-1 = SF, KS, CG, AM; PICO-2 = WH, EG) and key elements were collected using a predesigned template which included the study setting, inclusion/exclusion criteria, study design, comparator reference standard or control group, and primary/secondary outcomes.
Due to the dearth of literature for both PICO questions, we included conference abstracts, foreign papers with English translation and non-randomized studies. We pre-planned a separate synthesis for abstract results because the data they contain are limited. We excluded studies if they were abstracts of studies that were already included, reported outcomes that did not include our pre-defined PICO outcomes, or were not original research. We included systematic reviews if they pertained to our study objectives and included individual studies we were not already analyzing. Our rationale for inclusion of these studies was that they would enhance our scoping review by adding relevant studies and meta-analyses derived statistical heterogeneity and study quality assessments that we did not conduct.
Synthesis of Best Practices and Building Consensus
Summary tables were presented to all GEAR members at the GEAR consensus conference which occurred in October 2019. GEAR-Falls synthesized current-state knowledge and research gaps and then provided preliminary falls research prioritization rationale. GEAR attendees were then divided into smaller discussion groups to consider the scoping review findings, the preliminary research prioritization questions and debate and further consider research gaps. Discussion groups reconvened, shared their perspectives on research priorities, and streamlined them into common themes. Finally, all GEAR members voted and ranked these research priorities as recommendations for future research. Two non-emergency medicine fall prevention experts subsequently reviewed a statement regarding the impact of the scoping review by GEAR-Falls (see Supplement 5). Two patient advocates (LH, LN) reviewed this scoping review and Consensus Conference Power Point presentations before providing their perspectives via email and teleconference calls (see Supplement 6).
RESULTS
Evidence Synthesis
PICO-1: Fall Prevention Interventions
We completed the search in February 2019. For PICO-1, after removal of duplicates, there were a total of 3,181 unique citations with a focus on interventions for geriatric patients presenting to the ED for a fall. Of the 3,181 studies focusing on interventions, 3,049 were excluded, as they were not ED-based, geriatric, or interventional studies, leaving 32 studies for inclusion in this review (Figure 1). Cohen’s unweighted Kappa coefficient for inter-rater reliability for selecting articles demonstrated fair agreement between reviewers (κ = 0.24, 95% CI: 0.10 – 0.38).25 Discrepancies for initial disagreement included decisions regarding the inclusion of different manuscripts using the same study participants or secondary literature, as well as differing definitions of interventions.
Figure 1.
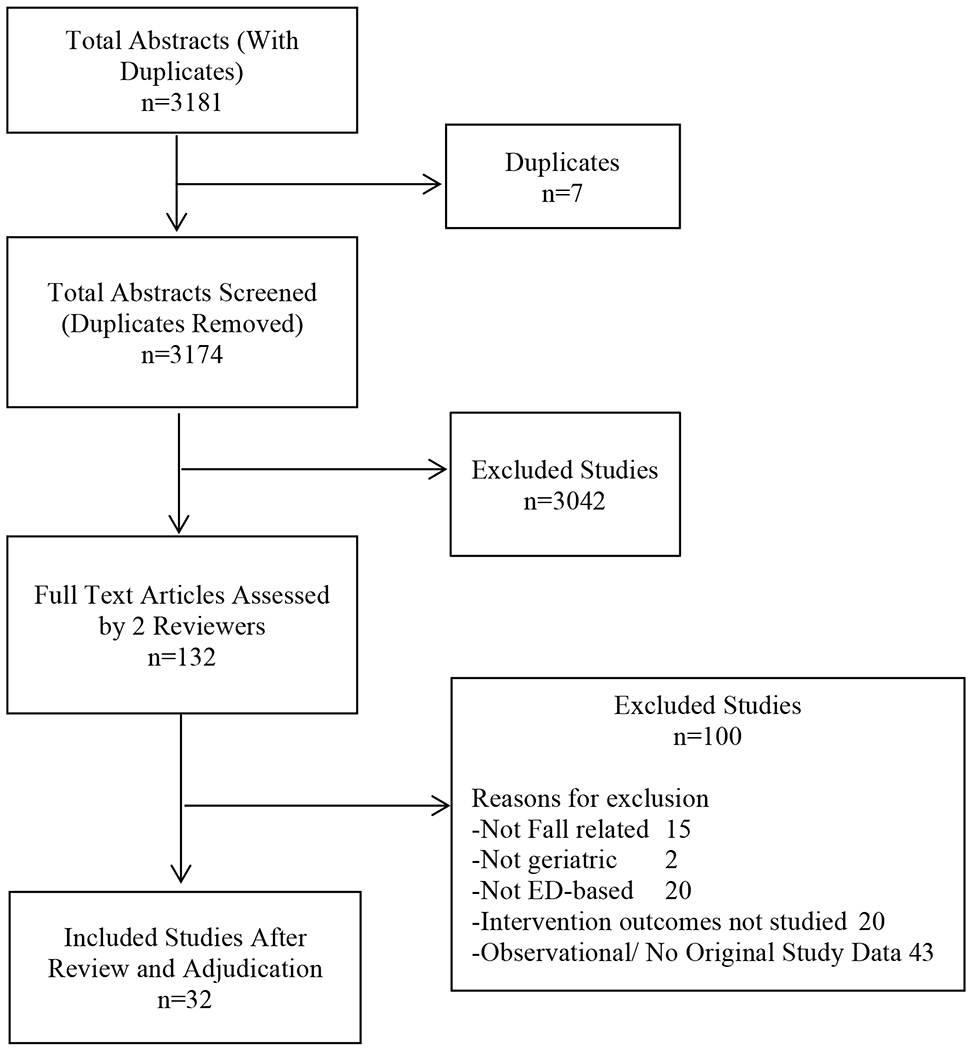
Summary of Scoping Review Quantitative Synthesis for PICO 1
PICO-1 Participant Characteristics
The 32 included studies contained over 500,000 participants from eleven countries worldwide. Studies were published from 1999 to 2019. Mean age of participants ranged from 74.2 to 84.6 years old. All but two studies26,27 included patients presenting to the ED for a fall or fall-related injury. Of the remaining two studies, Harper et al. included patients presenting to the ED with any diagnosis, including falls, provided they were scheduled for discharge,26 and a systematic review by Carpenter et al. encompassed community-dwelling adults with falls, including those who presented to the ED for any reason and had a subsequent fall within 6-months.27 Five studies included ED patients with falls if they sustained at least one fall in the year prior to the ED visit.28–32
PICO-1 Study Characteristics
Of the 32 studies, three were conference abstracts33–35 and three were commentaries on previously published studies.27,30,36 Studies were randomized controlled trials (23),2,26,28,30–33,35–48 prospective observational (2),33,49 retrospective observational (4),7,50–52 and systematic reviews with or without meta-analyses (3).27,34,53
PICO-1 Interventions
Twenty-one of the 32 (66%) interventions consisted of a falls risk assessment – screening for future fall risk2,26,28–30,33,35–38,40–48,54,55 — and 15/21 (71%) were combined with a personalized exercise or physical rehabilitation session led by physical or occupational therapists (home-based or outpatient geriatric settings).2,26,28,30–33,36–38,40,42,43,45,46 Fifteen studies were multifactorial, targeting the assessment and amelioration of individual risk factors for the fall. They included a falls risk assessment, educational guidelines, and referral to a nurse practitioner focused on falls or physical therapists.2,26,27,30–32,36,38,40,42,44,45,47,50,54 Seven interventions were education focused.6,26,32,44,49–51 Two studies included medical alert devices.50,54 Table 1 summarizes the common study, patient, intervention, and outcome characteristics we identified for PICO 1.
Table 1.
Summary of Study, Patient, Intervention, and Outcome Characteristics for PICO 1 and PICO 2
| PICO | 1 | 2 | |
|---|---|---|---|
| Summary |
Population: ≥ 60 years old individuals presenting with a fall for ED care. Intervention: Fall prevention interventions (may include multifactorial risk reduction, medication review, exercise training, models of care (hospital-at-home and others) in ED or peri-ED period). Comparison: Standard of care. Outcome: Quality of ED care metrics, ED operations outcomes (e.g., ED length of stay); patient-centered outcomes (e.g., ED returns for falls, future falls, fear of falling, or functional decline, long-term supports or institutionalization). |
Population: ≥ 60 years old individuals from any pre-ED and ED setting (pre-hospital, paramedic, EMS, ED). Intervention: Risk stratification and falls care plan. Comparison: No risk stratification and no falls care plan. Outcome: ED referral (if from pre-ED settings), quality of ED care metrics, ED operations outcomes (e.g., ED length of stay, cost), patient-centered outcomes (e.g., ED returns for falls, future falls, fear of falling, functional decline, long-term supports or institutionalization). |
|
|
| |||
| Number of Included Studies n | 32 | 17 | |
|
| |||
| Meta-analysis or Systemic Reviews n (%) | 3 (13) | 4 (24) | |
|
| |||
| Randomized Controlled Trials n (%) | 23 (72) | 8 (47) | |
|
| |||
| Interventions / Instruments Validated in the ED (n) |
9 multifactorial interventions, ranging from: Falls risk assessment and physical rehabilitation sessions, Preventive Education (7), Falls risk assessment, educational guidelines, and follow up with nurse practitioner or physical therapist (15), Medical alert devices (2) |
12 Screening Instruments (11 identified): * | |
| CDC STEADI | Paramedic baseline Assessment | ||
| FROP Com | FRIDs using clinical pathways | ||
| Two-Item Screening Tool | EGS | ||
| FIM/FAM | Bedside functional tests | ||
| Timed Up & Go | Clinical pathways only | ||
| SPPB | Unidentified (2 studies), | ||
| Combined with interventions ranging from: | |||
| Education, | Discharge planning, | ||
| ED-based physical therapy | Preventive education | ||
| Follow up calls | At-home visits. | ||
|
| |||
| Total Number of Patients Recruited | 571,071 | At least 17,232 (Samuel 2017, Beales 2016 did not report sample sizes) | |
|
| |||
| Recruitment Period | 1999 - 2019 | 2011 - 2018 | |
|
| |||
| Geographical Locations | 11 Countries | 9 Countries | |
|
| |||
| Mean Age Range | 74.2 – 84.6 | 74.3 - 83.9 | |
|
| |||
| Common Inclusion Criteria (n) | Age 65 and older, Presenting to the ED for a fall or fall related injury, At least one fall in the year prior to the ED visit (5). |
Age 65 and older, Admitted to the ED with a falls-related injury, History of falls within the past year (1), Patient eligible for ED discharge. |
|
|
| |||
| Patient-centered Primary Outcomes (n) | Proportion of participants experiencing recurrent falls (29), Frequency of falls per subject (11), Time to first fall post ED discharge, Change in anxiety from fear of falling, Quality-adjusted life years (QALYs), Functional ability pre-post fall intervention. |
Incidence of recurrent falls (8), Patient participation in fall prevention plans (1), Proportion of positive screens (1), Reduction in falls health care costs (1), Completion of screening (1), Clinical relevance (1), Life-threatening complications (1). |
|
|
| |||
| ED-centered Primary Outcomes | Improvement in documenting a fall related history or exam, 9-month incremental cost-effectiveness ratio (ICER). |
Feasibility of screening. | |
|
| |||
| Secondary Outcomes | Physical disability, Death. |
||
|
| |||
| Follow Up Period Post ED Discharge | 1 – 18 months | 6 – 12 months | |
|
| |||
| Reference Standard (n) | Usual Care | Usual care FROP com with FIM/FAM (1) |
|
|
| |||
| Gold Standard Available | None | None | |
|
| |||
| Risk of Bias in Meta-Analysis / Systematic Review (n) | High (2) | ||
CDC STEADI: Center for Disease Control’s Stop Elderly Accidents, Deaths, and Injuries toolkit; FROP Com: Falls Risk for Older People in the Community; FIM/FAM: Modified Functional Independence Measure/Functional Assessment Measure; TUG: Timed Up & Go; SPPB: Short Physical Performance Battery; FRIDs: Fall Risk Increasing Medications; Emergency Geriatric Screening (EGS).
Interventions varied and were often bundled, not only with fall risk assessments but with other interventions. For example, patient/clinician education was combined with referral to physical therapy.26 This combination of strategies made it difficult to analyze the efficacy of individual intervention components. For example, the PROFET trial showed a statistically significant reduction in subsequent falls for a bundled intervention of medical assessment, occupational therapy assessment, and referral services, but the efficacy of individual components is unknown.2
PICO-1 Study Outcomes
Twenty-one of the 32 studies reported their primary outcome as the proportion of participants experiencing recurrent falls.2,6,7,26–30,32–38,40–42,45,53,55 The duration of follow-up varied greatly, ranging from one month to 18 months post-ED discharge.7,29,50 Two studies did not report a specific timeline.26,27 In addition to number of people with falls per group, eleven studies also reported the frequency of falls per subject as their primary outcome.26–30,33,37,38,40,41,53 Two studies reported on process measures including improvement in documenting a fall related history or exam51 or 9-month incremental cost-effectiveness ratio (ICER).43 Patient-centered outcomes included reduced fear of falling,54 Quality Adjusted Life Years (QALYs),43 and functional ability.46 Secondary outcomes varied greatly with physical disability being the most common,6,26–29,31,34,36–38,40,41 followed by death.26,28,30,39,45
Eighteen studies focused solely or included exercise in their intervention bundles.2,6,7,26–34,36,38,40,42,45,56 In seven studies, physical therapy was associated with reduced risk of falls (7/18 studies, 39%).2,7,29,31,56 Multifactorial interventions in general provided mixed results on reduction in incidence of falls with the majority showing no difference in fall rates or proportion of people with falls in the intervention arm (11/14, 76%).6,26,28,32–34,36,38,40,42,45 However, Close et al. reported 64% reduction in total fall rate,2 as did two additional studies with an exercise component in the intervention (Carpenter et al.27 showed a 22% reduction in fall rate with exercise interventions with two or more components; a randomized controlled trial by Lever et al.30 demonstrated a 36% reduction in fall rate following in-hospital risk assessment and home-based physical or occupational therapy). Almost all studies reported no statistically significant change in time to first fall, fall frequency (except one study37), fall-related hospital admissions (except one study26), or fall-related ED utilization (except one study7).1,2,28,30,32,33,35,36,38,45,48,50,53–55
Interventions were not assessed against one another for comparison. Many studies extended beyond the ED, including follow-up calls and home visits by nurses and physical therapists.1,28,30–33,37,38,41–44,46,53,55 Educational interventions increased participant awareness of fall risks and availability of preventive services, but did not reduce the incidence of falls.1,6,26,32,41 Finally, individual study follow-up was frequently limited by the use of diaries for fall outcome assessment (18/32 studies, 56%), relying solely on self-report or caregiver-report, and thereby risking the underreporting of fall occurrences.26,28–30,32,35,36,38,40–44,46–49,55
PICO-2: Risk Stratification and Falls Care Plan
For PICO-2, we identified 2590 studies, of which 2571 were excluded as they were not ED-based, geriatric, interventional studies, or did not include our desired outcomes (Figure 2), leaving 19 studies for final inclusion (Supplements 2.1 and 2.2). Cohen’s Kappa coefficient for inter-rater reliability showed poor agreement (κ = 0.12, 95% CI: 0.13 – 0.38).25 Reasons for initial disagreement included differing opinions about including systematic reviews, whether screening constituted a “falls care plan”, and whether secondary analyses should be included.
Figure 2.
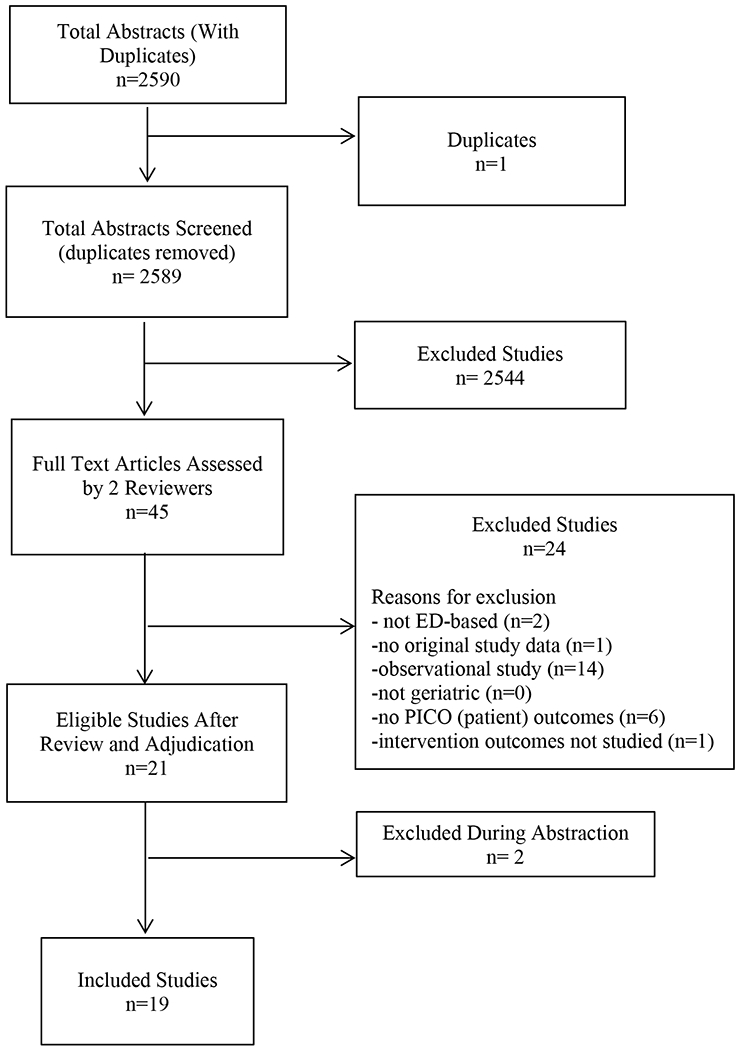
Summary of Scoping Review Quantitative Synthesis for PICO 2
PICO-2 Participant Characteristics
The total number of participants in PICO-2 studies was 17,272 patients. Two studies did not report cohort sizes,57,58 and two other studies used the same cohort of patients.39,59 Studies were published from 2011 to 2018 and originated in nine countries. Mean age ranged between 74.3 and 83.9 years old. Common inclusion criteria were age 65 and older, admitted to the ED with a falls-related injury, or history of falls within the past year,60 and patient eligible for ED discharge. Two studies did not have a recent fall as an inclusion criterion,26,39 and one study did not report the patient characteristics used for inclusion.58 Exclusion criteria varied, the most common was non-English speakers,26,39,55,59,61 and two randomized controlled trials by Mikolaizak excluded cognitively impaired patients.59,61 Five studies specified no exclusion criteria.44,58,60,62,63
PICO-2 Study Characteristics
Seven of the 19 studies that were included were conference abstracts.34,57,58,60,64–66 Seven were randomized controlled trials.26,42,44,59,61,65,67 Eight were prospective studies,39,55,58,60,62–64,66 and four were systematic reviews.34,56,57,68
PICO-2 Risk Stratification Tools
A total of 11 identified screening tools were validated in the ED: Center for Disease Control’s (CDC) Stop Elderly Accidents, Deaths, and Injuries toolkit (CDC STEADI); Falls Risk for Older People in the Community (FROP Com) tool, Two-Item Screening Tool, Modified Functional Independence Measure/Functional Assessment Measure (FIM/FAM), Timed Up & Go (TUG), Short Physical Performance Battery (SPPB), fall risk factors identified by paramedics at baseline assessment, Fall Risk Increasing Medications (FRIDs) identified using clinical pathways, Emergency Geriatric Screening (EGS), various bedside functional tests, and clinical pathways alone. Table 1 summarizes the studies we identified for PICO 2. In addition, we compiled various ED fall screening tools in Supplement 3, including those not studied in our review. We have summarized their administration times, accuracy, and pragmatic features in Supplement 4.
No consensus exists on fall screening tools suitable for ED use. One systematic review of six ED screening tools confirms only one tool had sufficient accuracy to identify ED patients at low risk of future falls, and that instrument did not accurately identify individuals at high-risk for future falls.56 Also, because studies did not directly compare screening tools against each other, ranking them by predictive accuracy and ED applicability is not feasible. Only one study compared the Two-Item Screening Tool (“Are you taking six of more medications?”, “Have you had two or more falls in the past year?”) and the FROP Com screening tool.39 Both tools were shown to have similar predictive characteristics but their predictive characteristics were low (Sensitivity: FROP Com 39% [95% CI 0.27 to 0.51]; Two-Item Screening Tool 48% [95% CI 0.36 to 0.60]; Specificity: FROP Com 70% [95% CI 0.61 to 0.78]; Two-Item Screening Tool 57% [95% CI 0.47 to 0.66]. The need to identify a fall screening tool for the ED remains unmet.
Because most studies (14/19; 74%) combined falls risk screening with an intervention26,42,44,55,58–67 it is unclear if patient-centered outcomes such as rates of recurrent falls, fall-related complications, or healthcare utilization improvements were associated with the screening, intervention, or both. When screening alone was performed, outcomes frequently focused on sensitivity, specificity, or feasibility of screening, rather than patient-centered outcomes. An example is Schoenenberger et al.63 exploring the EGS, which is a five-minute instrument used to screen cognition, falls, mobility, and activities of daily living. Schoenenberger and colleagues developed the screening tool and did not combine it with other interventions. EGS was feasible in 42.5% of ED patients 75 years and older, identifying patients at higher incidence of falls-related diagnoses compared to patients who were not screened (OR 1.80, 95% CI 1.32 – 2.44). However, because the study was aimed at EGS feasibility, patient-centered outcomes such as risk of falls and fall frequency were overlooked. Finally, an added problem with multi-intervention studies was the strength of evidence they presented. Systematic reviews have deemed them low quality due to inadequate sample sizes, high risk of suspected bias, and vague reporting of compliance to interventions.34,68
PICO-2 Falls Care Plan
Ten of 19 studies included highly tailored multifactorial interventions,26,34,42,55,58–61,64,66 which “consist of more than one main category of intervention, but participants receive different combinations of interventions based on an individual assessment to identify potential risk factors for falling”.69 Specific intervention combinations included education, discharge planning, and referrals (e.g. to physical therapy clinics, ophthalmology);55 or physical therapy programs in the ED coupled with follow up calls or at-home visits, and targeted education on preventative strategies.26,42,64
PICO-2 Study Outcomes
Authors most frequently specified fall incidence as the primary outcome.26,39,42,55,59,61,64,65 Other primary outcomes included patient participation in fall prevention plans,60 proportion of positive screens,62 reduction in falls health care costs,44 completion of screening,58 clinical relevance,63 and life-threatening complications.70 Follow-up periods varied from six to twelve months. As in PICO-1, individual studies may have underreported fall occurrence by relying on subjective patient-caregiver recall and personal diaries (8/19 studies, 42%).26,44,55,59,61,64,65,67
Several studies reported improvement in patient-centered outcomes. Incidence of recurrent falls was reduced in three studies, although each study reported the same outcome differently (OR 0.39, 95% CI 0.23 – 0.66;57 IRR 0.53, 95% CI 0.45 – 0.80;61 92% reduction at three months65). Matchar et al. found no difference in fall incidence after implementing a tailored program of physical therapy in a randomized controlled trial, but participants receiving the intervention had fewer injurious falls (OR 0.56, p=0.04) and less decline in physical performance after a fall.42 A multidisciplinary intervention of patients referred to specialists for physiotherapy, occupational therapy, geriatric assessment, and other risk factor targeted assessments, there was no fall reduction in the intention to treat analysis, but the per protocol analysis revealed that patients with high adherence had lower rates of falls (IRR: 0.53 (95% CI: 0.32 – 0.87).59
Process measures related to falls improved in six studies: in a trial of 64 patients who completed the ‘Stepping On’ program, self-awareness related to falls improved in four falls behavioral scales (Cognitive Adaptations, Protective Mobility, Avoidance and Practical Strategies) and two balance measures (Timed Up and Go Test and the 30-second Chair Stand Test).65,61 In a study focused on medication safety in patients with falls, QALYs increased by 0.05 additional QALY.44 A British cluster randomized trial of 4832 patients of referral to community-based falls care service by paramedics vs. usual care revealed no difference in mortality or ED revisits 30 days after discharge, but fewer emergency calls six months after discharge, and higher rates of patient satisfaction in the intervention arm.67 Wahbi et al. found an 11% increase in ED discharge rates, 0.8 day reduction in hospital length of stay, and fewer bed transfers after implementing a multifactorial assessment and referral to geriatric consultations.66 Finally, completion of a fall risk screening tool increased from 10% to 50% after a series of quality improvement initiatives targeted to nurses including training, unannounced audits, and bedside Plan-Do-Study-Act cycles.58
Consensus of Highest-yield ED Research Priorities for Falls
After findings of the data abstraction were presented at the GEAR Consensus Conference in October 2019, the following priority questions were generated by the GEAR Task Force and subsequently ranked as most important to improve falls research. Research priorities were identified in order of decreasing importance as follows:
1 – Pre-hospital assessment, screening and intervention: What role does EMS play in fall assessment, screening, and intervention prior to patient transfer to the ED? Can EMS connect patients to existing resources?
2 – What is the best assessment tool, in terms of feasibility and performance characteristics, to identify fall etiology to inform the design targeted interventions?
3 –What are patient prioritized outcomes (such as maintaining independence, reduce fear of falling, stigma) and interventions?
4 –Determining optimal outcomes: What are the optimal outcomes for ED-based fall studies and how can we best track falls once patients leave the ED?
5 –Intervention components and effectiveness: should fall prevention interventions be tested as a bundle or separate components? What should be in the bundle?
Research questions with the least priority by number of votes included timing of fall risk assessment, patient strata to exclude from routine fall screening, and fall screening in the Ed versus outpatient settings. A plain language summary for the results of our review is included in Supplement 6.
DISCUSSION
In this PRISMA-adherent scoping review and GEAR consensus process we analyzed the gaps between research recommendations made by various scientific societies, such as SAEM and GED, and studies conducted in the ED on the assessment and prevention of falls. We reviewed 51 studies focused on ED falls research and established high-yield research priorities using a consensus-based approach.
Our scoping review uncovered a lag in identifying the proper ED fall risk assessment tools, which in turn precluded from identify high risk fallers in the ED, as per SAEM’s recommendation. Upon closer examination of the literature, the difficulty in reaching consensus on the proper assessment tools, as well as interventions, is due to a deeper gap in standardizing fall research methods, including harmonization of variable definitions, follow up durations and outcome reporting. Areas of agreement during discussions included the need to clearly define “falls”. Before the scoping review was conducted, the workgroup had identified a definition of falls; falls include “slips or trips” that result in landing on the floor or ground or lower level.2 We favored a simple definition of falls that is well accepted, consistent with the World Health Organization definition of falls,71 and conveyed a common conception of what a fall event entails and thus recommend future studies also clearly define falls to allow for comparison across studies. Falls that result from an overwhelming external force (e.g., assault) should be excluded as they are not reflective of an etiology related to aging or functional decline, and therefore require different preventative efforts from those discussed in this review. Variations in the interpretation and meaning of falls across cultures could explain why fall rates differ in studies in similar populations.72 We also recommend that falls should be recorded prospectively, when possible. In order to reduce recall errors and improve fall ascertainment, novel means of determining whether a fall occurred are needed such as wearables with sensors, especially in patients with cognitive impairment.73–76 In addition to improving the accuracy of fall ascertainment, a high priority area of research remains the identification of optimal outcome measures for ED-based fall studies. The Prevention of Falls Network Europe, a consortium of falls experts in Europe, have provided several useful recommendations about desirable fall study outcomes;77 number of falls, number of fallers/non-fallers/frequent fallers, fall rate per person year, and time to first fall. Researchers should consider the following other relevant outcomes: fall injuries (e.g., peripheral fracture rate per person-year), psychological consequences of falling (e.g., by measuring the Falls Efficacy Scale), health-related quality of life (e.g., Short Form 12), and physical activity measures.
The optimal approach to studying ED falls in the context of patient characteristics is not yet defined, although studies shared similar patient phenotypes as evident by their inclusion criteria. Most investigators chose to include older adults with a recent fall rather than include all older adults who presented to ED, indicating that ED-based studies typically focus on secondary prevention. Many of the included studies focused on patients discharged from the ED or those who live in the community rather than in the institutional setting. Reasons for this may vary, including that previous studies have shown that patients with dementia or who live in nursing homes may be less likely to benefit from fall prevention interventions.78 Twelve of the 51 studies excluded patients with dementia, and none included caregivers. However, two newly published studies indicate caregivers are facilitators in ED patients agreeing to fall prevention measures and adherence to recommendations made by fall prevention teams.79,80
Additionally, we detected general consensus regarding the need for a multifactorial intervention. Interventions that focused on providing education alone have limited effect on fall prevention.78 Two large studies focused on discontinuing FRIDs as the sole intervention were also not effective in preventing falls.79,80 Multiple societies such as the US Preventive Services Task Force, AGS, and the CDC recommend multifactorial interventions for the prevention of falls in community-dwelling older adults.81 Most interventions identified in our scoping review favored targeting multiple risk factors that may include medication review, physical therapy targeting functional limitations, and eliminating environmental hazards. These multifactorial interventions have been shown to be most effective in fall prevention because geriatric patients have several risk factors for falls, including lower extremity weakness, poor balance, medication, visual impairment, environmental hazards, and substance use. However, with multifactorial interventions it may be challenging to identify which intervention component is the most efficacious. Determining which component of bundles is most efficacious is therefore a priority area we identified. For example, our study shows that intervention bundles with an exercise component suggest improvements in patient-centered outcomes including recurrent falls, number of injurious falls and post fall performance. It is unclear if the exercise component alone or a specific combination of exercise and additional interventions is responsible for this positive signal. Future studies are encouraged to compare intervention bundles, especially those involving exercise or physiotherapy. A promising approach informed by STEADI may be the recently published GAPcare randomized clinical trial that significantly reduced 6-month fall-related ED visits and all-cause ED visits in older adults presenting with a fall by integrating pharmacist and physical therapist consultation into ED fall evaluations.10,79,80,82,83 Whether these results can be replicated outside of research settings remains to be determined.
A critique of ED-based fall prevention interventions remains that the ED is a chaotic environment that may not be suited to prevention efforts. However, in the case of fall prevention, the ED may be the most suitable place to initiate these efforts because (1) ED patients are at high-risk of future falls and may have the most to gain from fall prevention efforts, and (2) interventions can be delivered while patients await further testing, increasing implementation success. Two large size primary care-based studies that were recently completed illustrate why EDs may be better positioned as fall prevention sites. In the United Kingdom, 9803 older persons from 63 general practices were randomized to control, exercise, or multifactorial fall prevention; but the intervention did not achieve a lower fracture rate; OR 1.20 (95% confidence interval [CI], 0.91 to 1.59).84 In STRIDE, a nurse-administered multifactorial intervention recruited 86 PCP practices with 5,461 participants who were followed for 36 months. There was no reduction in rate of first serious falls injury (hazard ratio, 0.92; 95% confidence interval [CI], 0.80 to 1.06; p=0.25).20 Compared to GAPcare,10 where fall prevention was initiated in the ED, participants in both studies were younger, had fewer prior falls (a major fall risk factor), less cognitive impairment, and relied on less assistive devices for ambulation. Additionally, intervention procedures in these trials were spread out over several weeks, whereas in GAPcare participants received an intervention immediately after a fall event when motivation to change may be high and caregivers are often present. So, while the ED environment may be fast-paced, ED patients may be a high-yield group for intervention and the ED visit may represent a “teachable moment” where intervention uptake may be greater.
Pre-hospital and peri-ED interventions were also identified as a high priority area for future research. Most intervention-screening bundles we included were initiated in the ED but continued after discharge. For instance, interventions often included referral to an ED nurse with specialization in falls who maintained contact with patients after discharge. Given the time pressures ED clinicians face, ED clinicians are likely to benefit from additional professionals to assist with time consuming fall screening or fall prevention interventions such as nurses, physical therapists, pharmacists and geriatricians.14 Engaging these partners in the ED rather than relying on referral to an outpatient clinic alone is important, because several studies reviewed here showed that ED fall patients rarely attended outpatient fall clinics after referral.49,85 The group also identified that EMS personnel could play an important role in assessing fall risk factors and delivering targeted intervention, before or instead of performing these evaluations in the ED. Future falls research should consider the continuum of care in the peri ED period. Many patients with falls are evaluated by paramedics and emergency medical technicians and may not need or desire an ED evaluation. Further exploration of the role EMS plays in fall assessment, screening, and intervention prior to patient transfer to the ED and whether EMS can connect patients to existing resources is necessary.
LIMITATIONS
This scoping review and evidence-based consensus statement has several limitations. Segmenting the filtering and adjudication process for PICO-1 may have introduced agreement bias in our unadjusted Kappa calculations for PICO-1,86 which we did not account for since we did not calculate Kappa values for each of the filtration segments. PICO-2 was not segmented for filtering like PICO-1 alleviating the need to consider agreement bias and Kappa adjustment in PICO-2. Not all stakeholders were present at the consensus conference at the time of voting. However, follow up emails sent out to task force members yielded an overall voter participation prevalence of 100% and enhanced the diversification of opinion and research priorities for GEAR, although international expert opinion and insight are still needed to enhance the depth and generalizability of our findings.
Because this review is not a systematic review, a detailed qualitative and quantitative assessment was out of the scope of this work. Finally, our search strategy may have missed relevant studies or studies that were published after the conclusion of our search, but we made considerable effort to include newer studies in the discussion.
CONCLUSION
In summary, future multidisciplinary falls prevention researchers should quantify the comparable efficacy of competing screening tools for ED settings, where feasibility of assessment tools and interventions tested in other settings may not be directly translatable. Transdisciplinary harmonization of definitions of fall and recurrent fall are needed, in addition to standardized reporting of patient characteristics, follow up periods, fall reporting methods, and priority outcomes measures. Aligning fall-related definitions, methods, and outcomes across healthcare disciplines and settings will catalyze more meaningful comparative assessments of interventions and patient populations. Multifactorial interventions more effectively reduce future falls than single intervention studies, most EDs currently lack the time or resources for even one intervention so untangling the efficacy of individual components is warranted to prioritize resource allocation. While patient or clinician education alone does not reduce falls or fall injuries, the ED presents a unique ‘teaching moment’ for older adults following a fall-related visit. The pre-hospital and ED setting present opportunities to identify previously unrecognized older adults at high risk for falls. Transdisciplinary harmonization of definitions of a fall and recurrent falls are needed, in addition to standardized reporting of patient characteristics, follow up periods, fall reporting methods, and priority outcomes measures. Aligning fall-related definitions, methods, and outcomes across healthcare disciplines and settings will catalyze more meaningful comparative assessments of interventions and patient populations.
Finally, this scoping review and consensus conference discussion process yielded several research priorities for ED fall research, which include examining the role EMS plays in the care of older adults with falls, assessment tools to identify falls etiology, patient prioritized outcomes in addition to optimal outcomes to ED based falls studies and fall intervention components and effectiveness.
Supplementary Material
Acknowledgments:
The authors acknowledge the contributions of Dr. Tom Gill and Dr. Nancy Latham for providing the expert commentary provided in Supplement 5, as well as Libby Hoy for providing the patient summary in Supplement 6.
Financial Support:
1. Building the Geriatric Emergency care Applied Research Network. R21 AG058926. Hwang U (UH).
2. The West Health Institute and the John A. Hartford Foundation in support of the Geriatric Emergency Department Collaborative.
3. CG’s contribution to this manuscript was made possible by the Yale National Clinician Scholars Program and by CTSA Grant Number TL1 TR001864 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Footnotes
Presentations that this work was accepted for, but not presented at due to COVID:
Gettel CJ, Hung WW, Hwang U, et al. Geriatric Emergency care Applied Research (GEAR) network: prioritizing research on falls. Society for Academic Emergency Medicine, Annual Meeting, Denver, CO.
Gettel CJ, Hung WW, Hwang U, et al. Geriatric Emergency care Applied Research (GEAR) network: prioritizing research on falls. Society for Academic Emergency Medicine, New England Regional Meeting, Worcester, MA.
Hammouda N, Hung WW, On behalf of the GEAR Task Force. Geriatric Emergency care Applied Research Network GEAR): Prioritizing Research on Falls. American Geriatric Society Annual Meeting, Long Beach, CA.
Conflict of Interest Disclosure:
NH, CC, WH, AL, SN, SL, CG, AM, EC, SF, KS, SV, EG report no conflicts of interest.
REFERENCES
- 1.Shankar KN LS, Ganz DA. Trends and characteristics of emergency department visits for fall-related injuries in older adults, 2003–2010. West J Emerg Med 2017;18:785–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Close J EM, Hooper R, Glucksman E, Jackson S, Swift C. PRevention Of Falls in the Elderly Trial (PROFET): a randomised controlled trial. The Lancet 1999;353:93–7. [DOI] [PubMed] [Google Scholar]
- 3.Sterling DA OCJ, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma 2001;50:116–9. [DOI] [PubMed] [Google Scholar]
- 4.JA S The STEADI tool kit: a fall prevention resource for health care providers. IHS Prim Care Provid 2013;39:162–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Burns E KR. Deaths from falls among persons aged ≥65 years - United States, 2007-2016. MMWR Morb Mortal Wkly Rep 2018;67:509–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Russell MA HK, Day LM, Blackberry I, et al. A randomized controlled trial of a multifactorial falls prevention intervention for older fallers presenting to emergency departments. J Am Geriatr Soc 2010;58:2265–74. [DOI] [PubMed] [Google Scholar]
- 7.Lesser A IJ, Kent T, Ko KJ. Association between physical therapy in the emergency department and emergency department revisits for older adult fallers: A nationally representative analysis. J Am Geriatr Soc 2018;66:2205–12. [DOI] [PubMed] [Google Scholar]
- 8.Shan WL ZO, Yuchiao C, Kalpana NS. Frequency of ED revisits and death among older adults after a fall. Am J Emerg Med 2015;33:1012–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burns ER SJ, Lee R. The direct costs of fatal and non-fatal falls among older adults - United States. J Safety Res 2016;58:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldberg EM MS, Resnik LJ, Long S, Mellott H, Merchant RC. Can an emergency department-initiated intervention prevent subsequent falls and health care use in older adults? a randomized controlled trial. Ann Emerg Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salter AE KK, Donaldson MG, Davis JC, et al. Community-dwelling seniors who present to the emergency department with a fall do not receive guideline care and their fall risk profile worsens significantly: a 6-month prospective study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 2006;17:672–83. [DOI] [PubMed] [Google Scholar]
- 12.Carpenter CR LA. Falling behind? understanding implementation science in future emergency department management strategies for geriatric fall prevention. Acad Emerg Med 2015;22:478–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davenport K AM, Sri-On J, Liu S. Missed opportunities to diagnose and intervene in modifiable risk factors for older emergency department patients presenting after a fall. Ann Emerg Med 2020;76:730–8. [DOI] [PubMed] [Google Scholar]
- 14.Davenport K CA, Samson M, Sri-On J, Liu SW. Fall prevention knowledge, attitudes, and behaviors: a Survey of emergency providers. West J Emerg Med 2020;21:826–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carpenter CR SM, Hustey FM, Heard K, Gerson LW, Miller DK. High yield research opportunities in geriatric emergency medicine: prehospital care, delirium, adverse drug events, and falls. J Gerontol A Biol Sci Med Sci 2011;66:775–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hogan TM OE, Carpenter CR, Sauvigne K, Irmiter C, Emanuel L, Leipzig RM. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med 2010;17:316–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geriatric emergency department accreditation program. ACEP.org. (Accessed November 10, 2020, at https://www.acep.org/geda/.)
- 18.ACEP. Geriatric emergency department guidelines. Ann Emerg Med 2014;63:e7–25. [DOI] [PubMed] [Google Scholar]
- 19.Carpenter CR CA, Ganz DA, Liu S. Older adult falls in emergency medicine: 2019 update. Clin Geriatr Med 2019;35:205–19. [DOI] [PubMed] [Google Scholar]
- 20.Bhasin S GT, Reuben DB, et al. A randomized trial of a multifactorial strategy to prevent serious fall injuries. N Engl J Med 2020;383:129–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carpenter CR MM. Avoiding therapeutic nihilism from complex geriatric intervention “negative” trials: stride lessons. J Am Geriatr Soc 2020;n/a. [DOI] [PubMed] [Google Scholar]
- 22.Carpenter CR HN, Linton EA, Doering M, Ohuabunwa UK, et al. Delirium prevention, detection, and treatment in emergency medicine settings: a Geriatric Emergency Care Applied Research (GEAR) network scoping review and consensus statement. Acad Emerg Med 2020;n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kayser JM-HN, Rosen TE, Skees S, Doering M, et al. Research priorities for elder abuse screening and intervention: a Geriatric Emergency Care Applied Research (GEAR) network scoping review and consensus statement. J Elder Abuse Negl 2021:1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tricco AC LE, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. [DOI] [PubMed] [Google Scholar]
- 25.Landis JR KG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. [PubMed] [Google Scholar]
- 26.Harper KJ BA, Arendts G, Edwards DG, Petta AC, Celenza A. Controlled clinical trial exploring the impact of a brief intervention for prevention of falls in an emergency department. EMA 2017;29:524–30. [DOI] [PubMed] [Google Scholar]
- 27.CR C Evidence-based emergency medicine/systematic review abstract. Preventing falls in community-dwelling older adults. Ann Emerg Med 2010;55:296–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davison J BJ, Dawson P, Steen IN, Kenny RA. Patients with recurrent falls attending accident & emergency benefit from multifactorial intervention--a randomised controlled trial. Age Ageing 2005;34:162–8. [DOI] [PubMed] [Google Scholar]
- 29.Hwang H-FCS-J, Lee-Hsieh J, Chien D-K, Chen C-Y, Lin M-R. Effects of home-based tai chi and lower extremity training and self-practice on falls and functional outcomes in older fallers from the emergency department-a randomized controlled trial. J Am Geriatr Soc 2016;64:518–25. [DOI] [PubMed] [Google Scholar]
- 30.Lever JA. A multifactorial intervention reduced the mean number of falls but not the proportion who fell in older people with recurrent falls. Evid Based Nurs 2005;8:120-. [DOI] [PubMed] [Google Scholar]
- 31.Liew LK TM, Tan PJ, Mat S, Majid LA, Hill KD, Mazlan M. The modified Otago exercises prevent grip strength deterioration among older fallers in the Malaysian Falls Assessment and Intervention trial (MyFAIT). JGPT 2018. [DOI] [PubMed] [Google Scholar]
- 32.Tan PJ KE, Chinna K, et al. Individually-tailored multifactorial intervention to reduce falls in the Malaysian Falls Assessment and Intervention Trial (MyFAIT): a randomized controlled trial. PloS one 2018;13:e0199219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong EM FC. Preliminary results of a multidisciplinary falls evaluation program for elderly fallers presenting to the emergency department. Ann Emerg Med 2009;54:S81. [Google Scholar]
- 34.Abbas M DSC, Fraser LA. Multifactorial assessment and targeted intervention to prevent recurrent falls in community dwelling elderly individuals presenting to emergency departments: a systematic review and meta-analysis. Endocr Rev 2016;37.26650437 [Google Scholar]
- 35.Cammen TMBD Van Der. Medication prescribing and risk of falls: Results from the Improving Medication Prescribing to reduce Risk of FALLs (IMPROveFALL) study. Eur Geriatr Med 2014;5:S49–S50. [Google Scholar]
- 36.Birks Y A multifactorial intervention after a fall did not prevent falls in elderly patients with cognitive impairment and dementia. Evid Based Nurs 2003;6:114–5. [PubMed] [Google Scholar]
- 37.Chu MM-LFK-K, Lit AC-H, Rainer TH, et al. An occupational therapy fall reduction home visit program for community-dwelling older adults in Hong Kong after an emergency department visit for a fall. J Am Geriatr Soc 2017;65:364–72. [DOI] [PubMed] [Google Scholar]
- 38.de Vries OJ PG, Elders PM, Muller M, Knol DL, et al. Multifactorial intervention to reduce falls in older people at high risk of recurrent falls: a randomized controlled trial. Arch Intern Med 2010;170:1110–7. [DOI] [PubMed] [Google Scholar]
- 39.Harper KJ BA, Arendts G, Edwards DG, Petta AC, Celenza A. Failure of falls risk screening tools to predict outcome: a prospective cohort study. EMJ 2018;35:28–32. [DOI] [PubMed] [Google Scholar]
- 40.Hendriks MC BM, van Haastregt JM, Crebolder HM, Diederiks JM, et al. Lack of effectiveness of a multidisciplinary fall-prevention program in elderly people at risk: a randomized, controlled trial. J Am Geriatr Soc 2008;56:1390–7. [DOI] [PubMed] [Google Scholar]
- 41.Lightbody E WC, Leathley M, Sharma A, Lye M. Evaluation of a nurse-led falls prevention programme versus usual care: a randomized controlled trial. Age Ageing 2002;31:203–10. [DOI] [PubMed] [Google Scholar]
- 42.Matchar DB DP, Lien CT, Ong MH, et al. Randomized controlled trial of screening, risk modification, and physical therapy to prevent falls among the elderly recently discharged from the emergency department to the community: the steps to avoid falls in the elderly study. Arch Phys Med Rehabil 2017;98:1086–96. [DOI] [PubMed] [Google Scholar]
- 43.Matchar DB EK, Duncan PW, Lee M, et al. A cost-effectiveness analysis of a randomized control trial of a tailored, multifactorial program to prevent falls among the community-dwelling elderly. Arch Phys Med Rehabil 2019;100:1–8. [DOI] [PubMed] [Google Scholar]
- 44.Polinder S BN, Mattace-Raso FS, Van der Velde N, et al. Cost-utility of medication withdrawal in older fallers: results from the Improving Medication Prescribing to reduce Risk Of FALL (IMPROveFALL) trial. BMC Geriatr 2016;16:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shaw FE BJ, Richardson DA, Dawson P, Steen NI, McKeith IG, Kenny RA. Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: randomised controlled trial. BMJ (Clinical research ed) 2003;326:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vind AB AH, Pedersen KD, Joergensen T, Schwarz P. Effect of a program of multifactorial fall prevention on health-related quality of life, functional ability, fear of falling and psychological well-being. A randomized controlled trial. Aging Clin Exp Res 2010;22:249–54. [DOI] [PubMed] [Google Scholar]
- 47.Whitehead C WR, Crotty M, Finucane P. Evidence-based clinical practice in falls prevention: a randomised controlled trial of a falls prevention service. Aust Health Rev 2003;26:88–97. [DOI] [PubMed] [Google Scholar]
- 48.Boye ND vdVN, Vries OJ de, et al. Effectiveness of medication withdrawal in older fallers: results from the Improving Medication Prescribing to reduce Risk Of FALLs (IMPROveFALL) trial. Age Ageing 2017;46:142–6. [DOI] [PubMed] [Google Scholar]
- 49.Shankar KN TN, Taylor AA, Breaud AH, Peterson EW, Howland J. Older adult falls prevention behaviors 60 days post-discharge from an urban emergency department after treatment for a fall. Inj Epidemiol 2017;4:18-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ageron FX RC, Perrin-Besson S, Picot F, et al. Effectiveness of a multimodal intervention program for older individuals presenting to the emergency department after a fall in the northern French Alps emergency network. Acad Emerg Med 2016;23:1031–9. [DOI] [PubMed] [Google Scholar]
- 51.Baraff LJ LT, Kader S, Della Penna R. Effect of a practice guideline for emergency department care of falls in elder patients on subsequent falls and hospitalizations for injuries. Acad Emerg Med 1999;6:1224–31. [DOI] [PubMed] [Google Scholar]
- 52.McMahon CG CC, Kenny RA, Bennett K. Inappropriate prescribing in older fallers presenting to an Irish emergency department. Age Ageing 2014;43:44–50. [DOI] [PubMed] [Google Scholar]
- 53.Gates S FJ, Cooke MW, Carter YH, Lamb SE. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: systematic review and meta-analysis. BMJ (Clinical research ed) 2008;336:130–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee JS HM, Carew D, Fisher R, Kiss A, Drummond N. A randomized clinical trial to assess the impact on an emergency response system on anxiety and health care use among older emergency patients after a fall. Acad Emerg Med 2007;14:301–8. [DOI] [PubMed] [Google Scholar]
- 55.Harper KJ BA, Bharat C, Petta AC, Edwards DG, Arendts G, Celenza A. Risk assessment and the impact of point of contact intervention following emergency department presentation with a fall. Phys Occup Ther Geriatr 2017;35:182–94. [Google Scholar]
- 56.Carpenter CR AM, Wildes T, Stark S, Fowler SA, Lo A X. Predicting geriatric falls following an episode of emergency department care: a systematic review. Acad Emerg Med 2014;21:1069–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.LK B “But I’m not a Geriatrician!” incorporating frailty assessment into every encounter in the emergency department. Eur Geriatr Med 2016;7:S96–S7. [Google Scholar]
- 58.Samuel P PJ, Muckle F, Lexchin J, Mehta S, McGovern B, Chartier LB. A comprehensive quality improvement initiative to prevent falls in the emergency department. CJEM 2017;19:S90. [Google Scholar]
- 59.Mikolaizak SA LS, Tiedemann A, Simpson P, et al. A multidisciplinary intervention to prevent subsequent falls and health service use following fall-related paramedic care: a randomised controlled trial. Age Ageing 2017;46:200–7. [DOI] [PubMed] [Google Scholar]
- 60.Greenberg MR JJ, Barraco RD, Moore EC, et al. Emergency Department Stopping Elderly Accidents, Deaths And Injuries (ED STAEDI) program. Ann Emerg Med 2015;66:S1. [DOI] [PubMed] [Google Scholar]
- 61.Mikolaizak SA LS, Tiedemann A, Simpson P, et al. Adherence to a multifactorial fall prevention program following paramedic care: Predictors and impact on falls and health service use. Results from an RCT a priori subgroup analysis. Australas J Aging 2018;37:54–61. [DOI] [PubMed] [Google Scholar]
- 62.Huded J GS, Dresden S, Aldeen AZ, Lindquist L. Identifying fall risks in the emergency department: a missed opportunity. J Am Geriatr Soc 2015;63:S36. [Google Scholar]
- 63.Schoenenberger AW BC, Özgüler O, Moser A, et al. A novel multidimensional geriatric screening tool in the ED: evaluation of feasibility and clinical relevance. Am J Emerg Med 2014;32:623–8. [DOI] [PubMed] [Google Scholar]
- 64.Tan PJ KE, Saedon NI, Chinna K, Tan MP. 105 A randomised controlled study on individually-tailored multifactorial falls intervention in older fallers in Malaysia. Age Ageing 2014;43:i29–i. [Google Scholar]
- 65.Trice SL LK. A60 Innovative partnerships reduce falls: TriHealth, People Working Cooperatively (PWC), CAPS (Certified Aging in Place Specialists) team and Green Township Ohio Emergency Medical Services(EMS). J Am Geriatr Soc 2017;65:S1–S289. [Google Scholar]
- 66.Wahbi O MB, Dumas S, Leyte N, Arendts G. Configuration of a standardized approach to patients >65 years old presenting to emergency department with a fall. EMA 2018;30:19–20. [Google Scholar]
- 67.Snooks HA AR, Chatters R, Dale J, Fothergill RT, et al. Paramedic assessment of older adults after falls, including community care referral pathway: cluster randomized trial. Ann Emerg Med 2017;70:495–505.e28. [DOI] [PubMed] [Google Scholar]
- 68.Zozula A CC, Lipsey K, Stark S. Prehospital emergency services screening and referral to reduce falls in community-dwelling older adults: a systematic review. EMJ 2016;33:345–50. [DOI] [PubMed] [Google Scholar]
- 69.Gillespie LD RM, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Snooks HA CB, Dale J, Foster T, et al. Support and Assessment for Fall Emergency Referrals (SAFER 1): cluster randomised trial of computerised clinical decision support for paramedics. PloS one 2014:e106436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Falls. WHO, 2018. 2021, at https://www.who.int/news-room/fact-sheets/detail/falls.) [Google Scholar]
- 72.Zecevic AA SA, Speechley M, Vandervoort AA. Defining a fall and reasons for falling: comparisons among the views of seniors, health care providers, and the research literature. Gerontologist 2006;46:367–76. [DOI] [PubMed] [Google Scholar]
- 73.Davis JC DL, Khan KM, Bryan S, et al. Cognitive status is a determinant of health resource utilization among individuals with a history of falls: a 12-month prospective cohort study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 2016;27:943–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lipardo DS TW. Falls prevention through Physical And Cognitive Training (falls PACT) in older adults with mild cognitive impairment: a randomized controlled trial protocol. BMC Geriatr 2018;18:193-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Allali G LC, Blumen HM, Callisaya ML, et al. Falls, cognitive impairment, and gait performance: results from the GOOD initiative. JAMDA 2017;18:335–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gonçalves J AJ, Masse FA, Vale FCarvalho, Takahashi AM, Andrade LP. Dual-task as a predictor of falls in older people with mild cognitive impairment and mild Alzheimer’s disease: a prospective cohort study. Braz J Phys Ther 2018;22:417–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lamb SEJ-SE, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the prevention of falls network europe consensus. J Am Geriatr Soc 2005;53:1618–22. [DOI] [PubMed] [Google Scholar]
- 78.Cameron ID DS, Panagoda CE, Murray GR, Hill KD, Cumming RG, Kerse N. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Goldberg EM GC, Hayes K, Shield RR, Guthrie KM. GAPcare: the Geriatric Acute and Post-acute fall prevention intervention for emergency department patients – a qualitative evaluation. OBM Geriatr 2019;3:1-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gettel CJ HK, Shield RR, Guthrie KM, Goldberg EM. Care transition decisions after a fall-related emergency department visit: a qualitative study of patients’ and caregivers’ experiences. Acad Emerg Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Moyer VA obotUSPSTF. Prevention of falls in community-dwelling older adults: U.S. preventive services task force recommendation statement. Ann Int Med 2012;157:197–204. [DOI] [PubMed] [Google Scholar]
- 82.Goldberg EM MS, Ilegbusi A, Resnik L, Strauss DH, Merchant RC. GAPcare: the Geriatric Acute and Post-acute fall prevention intervention in the emergency department: preliminary data. J Am Geriatr Soc 2020;68:198–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Goldberg EM RL, Marks SJ, Merchant RC. GAPcare: the Geriatric Acute and Post-acute fall prevention intervention—a pilot investigation of an emergency department-based fall prevention program for community-dwelling older adults. Pilot Feasibility Stud 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lamb SE BJ, Hossain A, Ji C, et al. Screening and intervention to prevent falls and fractures in older people. N Engl J Med 2020;383:1848–59. [DOI] [PubMed] [Google Scholar]
- 85.Wijck S RC, Tsegai N, Raybould T, Liu S. Unexpected challenges to preventing falls in older adults: a mixed methods study of an emergency department-based falls prevention referral pilot project. Health Educ Care 2019;4. [Google Scholar]
- 86.Byrt T BJ, Carlin JB. Bias, prevalence and kappa. J Clin Epidemiol 1993;46:423–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


