Abstract
Objectives
While CT scanning plays a significant role in healthcare, its increasing use has raised concerns about inappropriate use. This study investigated factors driving the changing use of CT among people admitted to tertiary hospitals in Western Australia (WA).
Design and setting
A repeated cross-sectional study of CT use in WA in 2003–2005 and 2013–2015 using linked administrative heath data at the individual patient level.
Participants
A total of 2 375 787 tertiary hospital admissions of people aged 18 years or older.
Main outcome measure
Rate of CT scanning per 1000 hospital admissions.
Methods
A multivariable decomposition model was used to quantify the contribution of changes in patient characteristics and changes in the probability of having a CT over the study period.
Results
The rate of CT scanning increased by 112 CT scans per 1000 admissions over the study period. Changes in the distribution of the observed patient characteristics were accounted for 62.7% of the growth in CT use. However, among unplanned admissions, changes in the distribution of patient characteristics only explained 17% of the growth in CT use, the remainder being explained by changes in the probability of having a CT scan. While the relative probability of having a CT scan generally increased over time across most observed characteristics, it reduced in young adults (−2.8%), people living in the rural/remote areas (−0.8%) and people transferred from secondary hospitals (−0.8%).
Conclusions
Our study highlights potential improvements in practice towards reducing medical radiation exposure in certain high risk population. Since changes in the relative probability of having a CT scan (representing changes in scope) rather than changes in the distribution of the patient characteristics (representing changes in need) explained a major proportion of the growth in CT use, this warrants more in-depth investigations in clinical practices to better inform health policies promoting appropriate use of diagnostic imaging tests.
Keywords: health services administration & management, diagnostic radiology, computed tomography, public health
Strengths and limitations of this study.
This study utilised a large-linked administrative data set over a period of 13 years, allowing the measurement of the contributions of changes in demographic and clinical characteristics to the changing use of CT.
With a rich source of individual level data, this study identified a wide range of demographic and clinical factors driving the use of CT in tertiary hospitals.
Since the decomposition analysis methods only quantified the contribution of observed factors, contribution of any unobserved factors to the change of CT use was summed in the constant coefficient.
Our study was limited to assessing the factors driving the use of CT scanning in tertiary (teaching) hospitals, therefore, caution is needed when generalising the results to other settings.
Introduction
CT is one of the most important technical developments in medicine and is now an essential part of clinical practice.1 2 In Australia, CT accounted for 13% of diagnostic imaging tests with an average of 134 scans per 1000 people in 2017/2018.3 4 It is estimated that diagnostic imaging tests increased the annual effective ionising radiation dose on the Australian population by 50%.5 In acknowledgement of the relatively high radiation burden of diagnostic imaging, Australia introduced diagnostic reference levels in 2011 providing a benchmark to facilitate monitoring and comparison of radiation dose between facilities.6
Despite the advanced technology leading to significant contribution in healthcare, its increasing use has raised a concern about inappropriate use. Approximately one-third of diagnostic imaging tests are estimated to be unnecessary or inappropriate, with the potential to do more harm than good and represent a waste of healthcare resources.7 8 In the case of CT, the potential harm includes exposure to ionising radiation and the associated risk of cancer to population. A previous study found a high rate of inappropriate CT among older patients and those with multimorbidity.9
In response to concerns of inappropriate utilisation of the advanced diagnostic technique, since early 2000, the Royal Australian and New Zealand College of Radiologists have provided the standards of practice for clinical radiology.10 In Western Australia (WA), Diagnostic Imaging Pathways has been deployed to promote appropriate use of imaging.11 12 Most recently, in 2015, NPS MedicineWise launched the Australian ‘Choosing Wisely’ campaigns promoting discussion on reducing low value care,13 changing healthcare provider behaviour and increasing patient knowledge. The overall intention is to improve patient safety and efficiency in health service utilisation.13
While substantial effort is under way to promote appropriate use of imaging tests, current data reporting variation in potentially avoidable diagnostic imaging tests, particularly for CT over the last decade are limited.9 14 15 Recent studies mainly focus on examining the prevalence of low value care,16 the early trend of procedure uptake in hospital settings17 and selected spinal imaging18 following Choosing Wisely campaigns. Therefore, better understanding of changes in the use of CT scanning over the past decade and demographic and clinical factors driving the change in the use of CT are necessary to support monitoring the use of CT scanning and to guide future research and public health interventions. The aim of this study is to use decomposition analysis to examine factors driving changes in CT use between two periods of time in tertiary hospitals in WA: recent (2013–2015) and past (2003–2005).
Methods
We conducted an observational repeated cross-sectional study of CT use in WA in 2003–2005 and 2013–2015 using linked administrative heath data at the individual patient level. Reporting follows the Reporting of studies Conducted using Observational Routinely-collected health Data guidelines.19
Data sources
The data sources included three data sets:
WA Hospital Morbidity Data System (HMDS) (January 2003–May 2016) providing information on diagnosis, date of admission and discharge from all hospitals in WA and basic sociodemographic and clinical characteristics.
WA Emergency Department (ED) presentation data (January 2003–December 2016) providing details of presentation time and date, presentation type, triage code, major diagnostic group and basic sociodemographic characteristics.
WA picture archiving and communication system (PACS) data (January 2003–May 2016) providing documentation on all CT scans conducted in tertiary including date of the scan, and the CT protocols used. All the data sets were linked using probabilistic matching algorithms with a level of data accuracy up to 99.9%.20 21
Details of data linkage process are presented in the website of WA Data Linkage (https://www.datalinkage-wa.org.au/dlb-services/linkage/).
Study population
The study population consisted of all hospital admissions in all four tertiary (teaching) hospitals located centrally in Perth, which accounted for nearly 50% of admissions in public hospitals, in WA between 2003 and 2015 inclusive, for people aged 18 years and older. Non-tertiary admissions (ie, admission from secondary (district general) hospitals) were excluded as CT scans performed in the hospitals are not consistently included in the PACS data set. The study population was then constructed into two study periods; past period (2003–2005) and recent period (2013–2015). To avoid overcounting hospital admissions, for example, where a patient was transferred between hospitals, consecutive tertiary hospital admission records for an individual were aggregated into a single hospital admission where admission or discharge dates were nested or overlapping, or where an admission date was within 1 day of the discharge date. A tertiary hospital admission was counted from the first date of admission in a tertiary hospital–or where applicable–the date of a prior associated tertiary ED presentation so long as it resulted in an admission, to the last discharge date in tertiary hospitals.
Patient and public involvement
This study used linked administrative health data of all tertiary hospital admissions of people aged 18 years or older. The patients were not directly involved in the design or conduct of this study. Our consumer representative (Mr John Stubbs) was involved in the design of the grant application used to fund this research and is a member of the research team providing ongoing input to analysis of the data, interpretation of the results and development of publications. The WA Data Linkage Branch and the data custodians of the WA ED Data Collection and the PACS data provided data for this project.
Outcome measures
The outcome measure of this study was the number of CT scans performed within a tertiary hospital admission. The number of CT scans was counted from the first day admitted to a tertiary hospital/presentation to a tertiary ED until the last date of discharge for that admission. To avoid overcounting the use of CT, multiple CT records with the same day and same anatomic areas were collapsed into one CT event.22
Independent measures
This study measured basic demographic and socioeconomic characteristics including age (18–44, 45–64, 65–74 and 75+ years), sex, indigenous status, residential remoteness classified according to Accessibility Remoteness of Australia Index (ARIA)23 (major cities, inner regional areas, outer regional areas, remote and very remote) and quintiles of the Census-specific Socio-economic Indexes for Areas (SEIFA) index of relative socioeconomic disadvantage24 (least disadvantage, less disadvantage, moderate disadvantage, high disadvantage and highest disadvantage).
Clinical characteristics included major clinical diagnostic groups and the number of morbidities. Major clinical diagnostic groups included mental and behavioural disorders, circulatory system, digestive system, endocrine, nutritional and metabolic diseases, musculoskeletal system, respiratory system, injuries and neoplasms. The conditions were identified in the principal diagnostic field of the hospital morbidity data record using ICD-AM-10 (the International Statistical Classification of Diseases and Related Health Problems, 10th Revision, Australian Modification). Multimorbidity was ascertained using the Multipurpose Australian Comorbidity Scoring system25 using ICD-AM-10 across all diagnostic fields and was classified into 0–1, 2–5 and 6+ comorbidities. In addition, an admission was classified as having had a surgical procedure where the principal procedure field included one of the 20 most common surgical procedure as per ACHI codes (the Australian classification of health intervention).26 Other independent measures included funding source (public or private), admission type (elective or unplanned admission) and admission with/without a transfer from secondary hospitals.
Statistical analysis
Descriptive analysis was conducted to examine the distribution of sociodemographic and clinical characteristics of the study population over two study periods; past period (2003–2005) and recent period (2013–2015) as well as the whole study population (2003–2015). Multivariable decomposition for non-linear response models, an extension of Oaxaca-Blinder decomposition analysis,27 was conducted to decompose the differential rate of CT use between the two study periods into the endowment (distribution of observed patient characteristics) and effect (relative probability of having CT scan) components:
The endowment component quantifies the amount of the difference in the rate of CT use is explained by the changes in the distribution of observed sociodemographic and clinical characteristics between the two study periods.
The effect component describes how much of the difference in the rate of CT scanning is explained by a change in the relative probability of having CT across observed characteristics.
We conducted decomposition analyses for all tertiary admissions and for unplanned tertiary admissions separately using STATA SE V.14.27
Results
Characteristics of tertiary admissions with CT scan by study periods
Of a total of 2 375 787 tertiary hospital admissions over the 12-year period (2003–2015), 303 439 admissions (12.8%) had at least one CT scan. The proportion of admissions incorporating CT increased from 8.9% in the past period (2003–2005) to 16.6% in the recent period (2013–2015) (table 1). Overall, there was a small change in the distribution of both demographic and clinical characteristics among admissions that included CT between the two study periods. For example, the proportion of the patients who had a CT scan and were in the older age group (75+ years) increased from 30.3% to 32.7% and people living in major cities with CT increased from 82.5% to 88.3% between the past and recent period. Similarly within clinical characteristics, multimorbidity (6+ morbidities) accounted for 27.8% of admissions with CT in the past period compared with 28.8% in the recent period. Among major diagnostic groups in the past period, injuries, circulatory system, cancer and digestive system accounted for 15.5%, 15.2%, 11.7% and 10.9% of admissions with CT, compared with 18.8%, 13.1%, 7.9% and 11.2% in recent period. For other characteristics, admission with CT in the recent period had a higher proportion of unplanned admission (90.1% vs 86.8%) and private funding sources (21.0% vs 7.7%) compared with the past period.
Table 1.
Characteristics of the study population by study period and CT scan status
| Study period | All years 2003–2015 (2 375 787) |
|||||||||||
| The past period (2003–2005) (n=519 286) | The recent period (2013–2015) (n=572 642) | |||||||||||
| Without CT scan (n=473 120) |
With CT scan (n=46 166) |
Without CT scan (n=477 462) |
With CT scan (n=95 180) |
Without CT scan (n=2 072 348) |
With CT scan (n=303 439) |
|||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Female | 237 021 | 50.1 | 21 232 | 46.0 | 248 412 | 52.0 | 43 865 | 46.1 | 1 057 280 | 51.0 | 137 988 | 45.5 |
| Age groups | ||||||||||||
| 18–44 years | 134 467 | 28.4 | 10 954 | 23.7 | 145 181 | 30.4 | 20 075 | 21.1 | 621 452 | 30.0 | 67 456 | 22.2 |
| 45–64 years | 144 820 | 30.6 | 12 797 | 27.7 | 150 139 | 31.4 | 27 225 | 28.6 | 651 941 | 31.5 | 87 319 | 28.8 |
| 65–74 years | 91 075 | 19.2 | 8447 | 18.3 | 83 797 | 17.6 | 16 798 | 17.6 | 368 070 | 17.8 | 53 332 | 17.6 |
| 75+ years | 102 758 | 21.7 | 13 968 | 30.3 | 98 345 | 20.6 | 31 082 | 32.7 | 430 885 | 20.8 | 95 332 | 31.4 |
| Indigenous status | 31 708 | 6.7 | 2111 | 4.6 | 32 061 | 6.7 | 4540 | 4.8 | 137 806 | 6.6 | 14 156 | 4.7 |
| SEIFA | ||||||||||||
| Least disadvantage | 129 988 | 27.5 | 12 522 | 27.1 | 130 427 | 27.3 | 27 885 | 29.3 | 595 921 | 28.8 | 90 660 | 29.9 |
| Less disadvantage | 89 310 | 18.9 | 8495 | 18.4 | 87 703 | 18.4 | 17 850 | 18.8 | 364 787 | 17.6 | 53 241 | 17.5 |
| Moderate disadvantage | 91 594 | 19.4 | 9112 | 19.7 | 99 533 | 20.8 | 19 549 | 20.5 | 449 532 | 21.7 | 65 203 | 21.5 |
| High disadvantage | 89 421 | 18.9 | 8923 | 19.3 | 95 607 | 20.0 | 18 104 | 19.0 | 388 311 | 18.7 | 57 090 | 18.8 |
| Highest disadvantage | 70 595 | 14.9 | 6900 | 14.9 | 61 291 | 12.8 | 11 344 | 11.9 | 262 172 | 12.7 | 35 691 | 11.8 |
| Unknown | 2212 | 0.5 | 214 | 0.5 | 2901 | 0.6 | 448 | 0.5 | 11 625 | 0.6 | 1554 | 0.5 |
| ARIA | ||||||||||||
| Major cities | 411 062 | 86.9 | 38 086 | 82.5 | 416 708 | 87.3 | 84 046 | 88.3 | 1 807 380 | 87.2 | 261 292 | 86.1 |
| Inner regional areas | 29 622 | 6.3 | 3663 | 7.9 | 19 675 | 4.1 | 3508 | 3.7 | 108 562 | 5.2 | 15 908 | 5.2 |
| Outer regional areas | 16 251 | 3.4 | 2155 | 4.7 | 19 417 | 4.1 | 3814 | 4.0 | 75 935 | 3.7 | 13 210 | 4.4 |
| Remote | 8968 | 1.9 | 1283 | 2.8 | 10 654 | 2.2 | 1901 | 2.0 | 44 727 | 2.2 | 7336 | 2.4 |
| Very remote | 6205 | 1.3 | 894 | 1.9 | 8167 | 1.7 | 1458 | 1.5 | 28 389 | 1.4 | 4731 | 1.6 |
| Unknown | 1012 | 0.2 | 85 | 0.2 | 2841 | 0.6 | 453 | 0.5 | 7355 | 0.4 | 962 | 0.3 |
|
Number of morbidity (MACSS) (median-IQR) |
2 | 2–3 | 4 | 2–6 | 2 | 2–3 | 4 | 2–6 | 2 | 2–3 | 3 | 2–6 |
| Major clinical conditions | ||||||||||||
| Mental and behaviour disorders | 11 065 | 2.3 | 2015 | 4.4 | 15 514 | 3.2 | 3296 | 3.5 | 61 756 | 3.0 | 11 109 | 3.7 |
| Circulatory system | 35 636 | 7.5 | 7038 | 15.2 | 38 534 | 8.1 | 12 434 | 13.1 | 162 138 | 7.8 | 41 737 | 13.8 |
| Digestive system | 31 437 | 6.6 | 5026 | 10.9 | 38 055 | 8.0 | 10 678 | 11.2 | 150 492 | 7.3 | 32 897 | 10.8 |
| Endocrine | 9160 | 1.9 | 823 | 1.8 | 11 074 | 2.3 | 1381 | 1.5 | 46 268 | 2.2 | 5165 | 1.7 |
| Musculoskeletal system | 21 153 | 4.5 | 1532 | 3.3 | 21 477 | 4.5 | 2819 | 3.0 | 93 520 | 4.5 | 9231 | 3.0 |
| Respiratory system | 15 013 | 3.2 | 2918 | 6.3 | 17 001 | 3.6 | 5241 | 5.5 | 68 859 | 3.3 | 17 149 | 5.7 |
| Injury | 23 483 | 5.0 | 7165 | 15.5 | 31 608 | 6.6 | 17 913 | 18.8 | 126 703 | 6.1 | 53 420 | 17.6 |
| Cancer | 21 608 | 4.6 | 5389 | 11.7 | 22 465 | 4.7 | 7520 | 7.9 | 96 232 | 4.6 | 28 783 | 9.5 |
| Funding sources | ||||||||||||
| Public | 447 927 | 94.7 | 42 612 | 92.3 | 416 248 | 87.2 | 75 202 | 79.0 | 1 894 581 | 91.4 | 258 126 | 85.1 |
| Private | 25 193 | 5.3 | 3554 | 7.7 | 61 214 | 12.8 | 19 978 | 21.0 | 177 767 | 8.6 | 45 313 | 14.9 |
| Unplanned admissions | ||||||||||||
| No | 316 762 | 67.0 | 6089 | 13.2 | 259 764 | 54.4 | 9387 | 9.9 | 1 245 273 | 60.1 | 34 058 | 11.2 |
| Yes | 156 358 | 33.0 | 40 077 | 86.8 | 217 698 | 45.6 | 85 793 | 90.1 | 827 075 | 39.9 | 269 381 | 88.8 |
| Transferred from secondary hospitals | ||||||||||||
| No | 459 539 | 97.1 | 41 742 | 90.4 | 455 496 | 95.4 | 88 480 | 93.0 | 1 990 570 | 96.1 | 277 994 | 91.6 |
| Yes | 13 581 | 2.9 | 4424 | 9.6 | 21 966 | 4.6 | 6700 | 7.0 | 81 778 | 3.9 | 25 445 | 8.4 |
| Surgical procedure | ||||||||||||
| No | 457 900 | 96.8 | 42 803 | 92.7 | 449 708 | 94.2 | 87 721 | 92.2 | 1 975 259 | 95.3 | 280 008 | 92.3 |
| Yes | 15 220 | 3.2 | 3363 | 7.3 | 27 754 | 5.8 | 7459 | 7.8 | 97 089 | 4.7 | 23 431 | 7.7 |
| Morbidity group | ||||||||||||
| 0–1 | 103 369 | 21.85 | 6165 | 13.35 | 116 826 | 24.47 | 13 361 | 14.04 | 514 216 | 24.81 | 46 686 | 15.4 |
| 2–5 | 349 557 | 73.88 | 27 175 | 58.86 | 329 844 | 69.08 | 54 377 | 57.13 | 1 452 109 | 70.07 | 175 377 | 57.8 |
| 6+ | 20 194 | 4.27 | 12 826 | 27.78 | 30 792 | 6.45 | 27 442 | 28.83 | 106 023 | 5.12 | 81 376 | 26.82 |
ARIA, Accessibility Remoteness of Australia Index; SEIFA, Socio-economic Indexes for Areas.
Decomposition results for the use of CT over the two periods
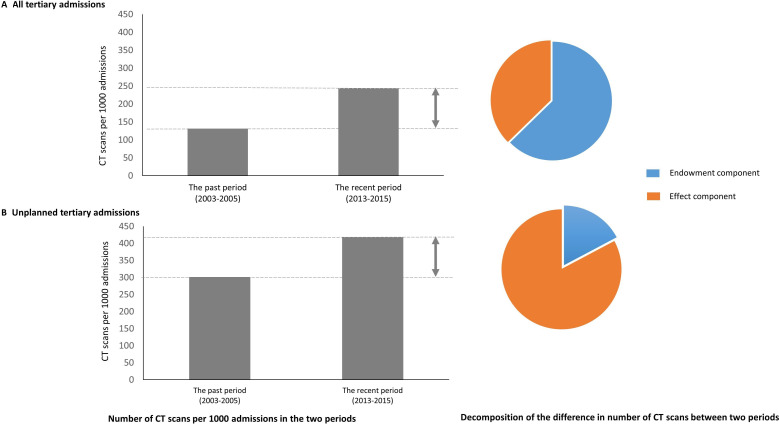
The results of the decomposition analysis of the difference in average number of CT scans between the two periods for all tertiary admissions and unplanned at the aggregated level are presented in figure 1 (detail in online supplemental appendix table 1A, B). The difference in the rate of CT scans between two periods was 112 scans per 1000 admissions (95% CI, 110; 114 per 1000 admissions, p value <0.001) for all tertiary admission and 117 scans per 1000 admissions (95% CI, 112; 120 per 1000 admissions, p value <0.001) for unplanned tertiary admissions. While the change in the number of CT scans per admission across the two analyses was not substantially different, a marked difference in the results of the decomposition analysis was observed. Figure 1 shows that 62.7% of the difference in CT use for all tertiary admission was explained by variation in the distribution of all observed characteristics. The rest of the difference in CT usage was attributable to variation in the relative probability of having CT in observed characteristics and unobserved factors (captured in constant coefficient).
Figure 1.
Decomposition analysis of the difference in average number of CT scans between the two periods. (A) All tertiary admissions. (B) Unplanned tertiary admissions.
bmjopen-2021-052954supp001.pdf (242.9KB, pdf)
In contrast, when the analysis was restricted to unplanned admissions, the variation in the distribution of the observed characteristics explained only 17% of the difference in CT use between two periods, while 82.7% was due to variation in the relative probability of having CT across observed and unobserved factors.
Details of decomposition analysis for all tertiary admissions
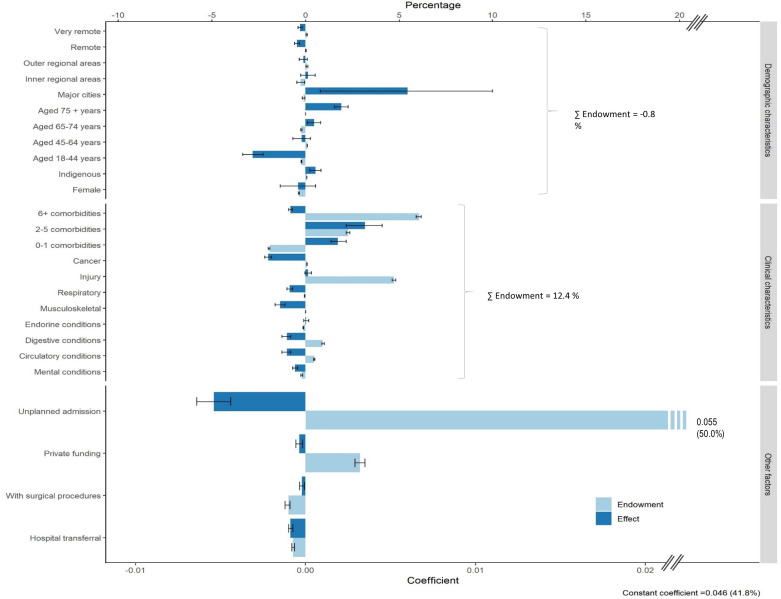
Figure 2 presents decomposition analysis in details of all observed demographic and clinical characteristics. Overall, changes in the distribution of the demographic characteristics including sex, indigenous status, age, SEIFA and ARIA explained only −0.8% of the change in CT use. Change in the distribution of the clinical characteristics including major principal diagnoses and groups of morbidities accounted for 12.4% of the change in CT use. Half of this change (6.1%) was attributable to multimorbidity (six or more morbidities) and 4.7% was due to injuries.
Figure 2.
Details of decomposition analysis of the difference in average number of CT scans between the two periods for all tertiary admissions.
Over the study period changes in the relative probability of having a CT scan over the observed patient characteristics resulted in a 6.8% increase in the rate of CT scanning, while changes in the distribution of the characteristics of the observed patient characteristics reduced the rate of CT scanning by 2.6%. Interestingly, the relative probability of having a CT scan for those with young age was significantly lower than in the past period contributing 2.8% reduction in the number of CT scan between the two periods. In addition, the relative probability of having CT was higher for those identified as living in major cities in the recent period compared with the past period, and lower for people from remote/very remote areas in the recent period compared with the past period. The contribution of each component to the difference in the number of CT’s per admission between the two periods was 5.5% (p value=0.02) and −0.8% (p values <0.001), respectively.
For clinical characteristics, the results indicated a lower relative probability of having a scan during a tertiary admission in the recent period compared with the past period for all the diagnostic groups, with the exception of those admitted for injuries and endocrine disorders. The increase in patients with multimorbidities (2–5 comorbidities) contributed 3.2% to the difference between the two periods.
For other factors, the relative probability of having a CT scan following transfer from a secondary hospital in the recent period was significantly lower than in the past period, contributing 0.8% reduction to the rate of CT scan between the two periods. A lower relative probability of having a CT scan in the recent period compared with the past period for unplanned admission contributed −4.9% to the difference in CT use between the two periods. Unobserved factors captured in the constant coefficient contributed to 41.8% of the variation in CT usage between the two periods.
Details of decomposition analysis for unplanned tertiary admissions
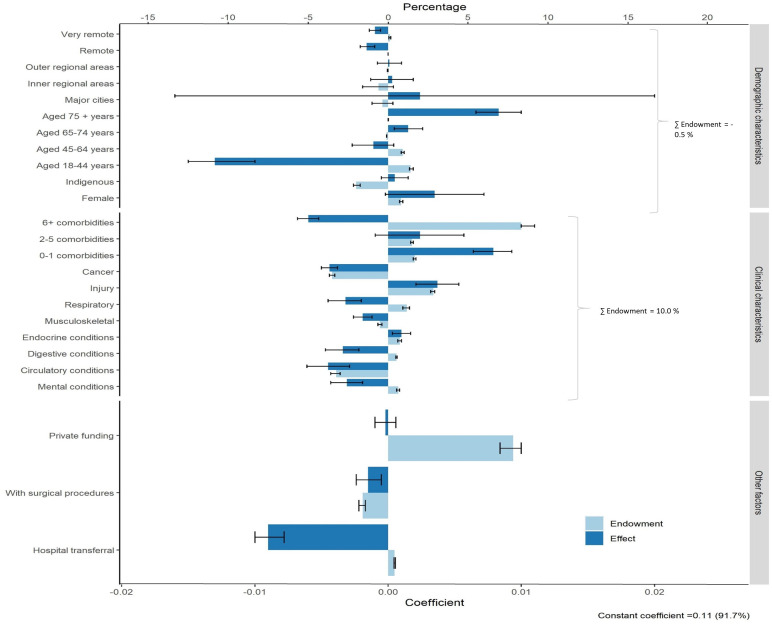
Similar to all tertiary admissions, the results for unplanned admission (figure 3) indicated that a substantial proportion of variation in CT use between the two study periods (10.0%) was attributable to changes in the distribution of the observed clinical characteristics including multimorbidity and major diagnostic groups. However, changes in the distribution of the observed demographic characteristics such as age, sex and accessibility between two periods only explained a total of −0.5% the change in CT use.
Figure 3.
Details of decomposition analysis of the difference in average number of CT scans between the two periods for unplanned tertiary admissions.
For the specific effect component, a similar finding was also observed in unplanned admissions. Specifically, a lower relative probability of having a CT scan for those in the youngest age group (18–44 years) was observed in the recent period compared with the past. Likewise, a lower relative probability of having CT scan in the recent period versus the past period was observed among those admitted for condition such as circulatory, cancer and respiratory; this accounted for −3.8%, −3.7% and −2.7% of the difference in CT use. The relative probability of having a CT scan after transfer from a secondary hospital in the recent period was lower than in the past, contributing −7.5% to the change in the number of CT scans between the two periods.
Discussion
This is the first study to examine the contribution of demographic and clinical characteristics to changes in the rate of CT scanning in tertiary hospitals using multivariable decomposition analysis of linked health administrative data over an extended period of time. We found that nearly two-thirds of the increase in the use of CT was attributable to changes in the distribution of observed characteristics, with changes in proportion of unplanned admissions accounting for the largest component. However, when the analysis was restricted to unplanned admissions, changes in distribution of the observed characteristics only explained about a fifth of the difference in CT usage and the rest was explained by the effect component. In both decomposition analyses, clinical characteristics (12.4% in all admissions and 10% in unplanned admissions) including major diagnostic groups and comorbidities rather than demographic characteristics contributed substantially to explain the variation in CT use between the two periods. Interestingly, our study observed a lower relative probability of having a CT scan in the recent period (2013–2015) compared with the past period (2003–2005) in two subgroups: young adults, which may reflect a movement towards minimising medical radiation exposure in the high risk population, and admissions transferred from secondary hospitals, reflecting either a reduction in inappropriate repeat imaging tests or greater access to CT in non-tertiary hospitals.
A recent study examined factors driving the increasing use of CT scan in Australia with a focus on the use of CT outside of the public hospital setting,28 which accounted for 73% of adult CT scans.29 Although the study also used the decomposition analysis approach, the only endowment component captured in this study was changes in the population age structure; the rest of the difference in CT use was captured in the number of CT scans per capita. The study found that a change in the number of CT scans per capita, interpreted as a ‘scope shift’, rather than changes in the population age structure accounted for a major component in the change of CT use outside hospital settings over the period 1993–2013.28 The previous study used changes in age structure as a marker of changes in need (eg, an ageing population), which had been postulated as the reason for increasing CT scanning rates. The finding that changes in the age structure was responsible for only a small proportion of the rate of CT use suggested that ‘scope shift’ (ie, changes in the practice of CT) was driving the rate of use. Our findings again confirmed that the impact of changing in age structure (ie, increasing proportion of older people) was not a major driver of the use of CT scanning. In addition, by using multivariable decomposition analysis, our study provides a more comprehensive picture of the contribution of various demographic, clinical and other observed factors driving the change in CT use in the hospital setting. This is because our analysis was able to differentiate the influence of changes in the distribution (endowment component) from changes in the relative probability of having CT (effect component) across a large range of observed factors. Our study adds to the literature by showing that it is the change in distribution of comorbidities and clinical conditions which are often highly prevalent in the older population rather than the age of the population itself that contributed the largest component to the growth of CT use. This indicates the need of strengthening public health interventions to promote healthy ageing to reduce the burden on healthcare systems.
Our study found that while many observed factors drive the increase of CT use, the change in the relative probability of having CT scan in the young age group and in those with admissions transferred from secondary hospitals (once the variation in the distribution of these factors was accounted for) reduced the use of CT in the recent period compared with the past period. These finding are encouraging as they confirm a reduction in two groups where there has been concern regarding inappropriate imaging. The results coincide with the goals of education campaigns to raise provider awareness of the risk of ionising radiation, especially among children and young adults.30–32 Since children and young adults are more sensitive and have more years to develop radiation-induced cancer,30 31 radiologists have become more cautious and may have taken care to minimise unnecessary CT scanning.
Despite challenges due to the vast geographical spread of Australia, over the last 15 years, diagnostic imaging services have become more accessible to patients in both major cities and rural areas within a timely and a reasonable distance from their home.31 A report in 2012 shows that more than 90% of Australians can get access to a comprehensive diagnostic imaging facility within a distance of 100 km from their residential areas31 and up to 80% of patients have access to a CT machine within 10 km.31 Between 2003 and 2018, Australia increased the rate of CT equipment per head of population from 40.6 to 67 per million.33 34 The government also provided a diagnostic imaging bulk billing incentive from November 2009 that increased the accessibility to the service through improving patient affordability. In addition, the government endorsed the diagnostic imaging review reform package in 2011 and implemented it between 2011 and 2016, funded through the Medicare Benefits Schedule. One of the package objectives was to ensure accessibility to quality diagnostic imaging services for people in rural and remote areas. In addition, the package also aimed to promote for effective communication between practitioners and imaging service to ensure appropriate imaging.31 The increasing availability and accessibility of diagnostic imaging, in particular to CT scanners, raised concerns of potential overuse of CT scans increasing radiation exposure to patients and contributing additional costs to the healthcare system.15 However, we found that the relative probability of having CT scan in tertiary hospitals for people living in remote and very remote areas in the recent period was less than in the past period. Although the magnitude of the variation was small, it accounts for significantly lower use of CT scan in tertiary hospitals. Likewise, the rate of CT scan among admissions transferred from the secondary hospital in the recent period was also less than in the past period. This would be consistent with government efforts to ensure accessibility of diagnostic imaging service in rural and remote areas as well as improved information transfer between hospitals. Previous studies have highlighted the important role of image sharing technology in improving provider access and avoiding duplication of investigations.35–37 However, a recent study found that repeat CT scanning is relatively common for patients already imaged prior to transfer to a tertiary hospital, although there was a valid clinical reason for repeat scanning in the majority of cases.15 Despite signs of improvement in our study, further detailed exploration is required to establish the proportion of avoidable repeat scans and therefore the potential benefit in terms of reduced radiation exposure and costs.
This study has a number of limitations, largely due to the nature of linked administrative data. This study only decomposed the difference in CT use between the two study periods based on the available observed characteristics available in the administrative data. Thus, the contribution of unobserved factors was not addressed in this study, although they are captured in the constant value. This study only captured the use of CT in tertiary hospitals because we did not have comprehensive data on CT use in non-tertiary settings, limiting our ability to determine whether the lower relative probability of having CT in the recent period in some subgroups was due to changes in practice or increasing accessibility of CT in other healthcare settings. While the linked administrative data can comprehensively capture use of health services over time without loss to follow-up, information about clinical information is limited to relatively high-level diagnostic codes recorded in the HMDS. Therefore, our study cannot provide information about the proportion of scans that were justified.
In conclusion, the use of CT in tertiary hospitals increased between the two study periods in keeping with international trends. This is primarily due to changes in the distribution of unplanned admissions and the clinical characteristics of presenting patients rather than changing demographic characteristics. Among unplanned admissions only, changes in the relative probability of scanning were the major drivers of CT use, with the largest component of this relating to unobserved factors. In both results, clinical characteristics appear to be substantial component driving the growth of CT usage in the tertiary hospital setting, while the role of demographic characteristics was minimal. Our study also highlights a potential improvement in practice towards reducing medial radiation exposure through a decrease CTs in subpopulations such as young adults and in those admitted via transfer admission from other hospitals. While the finding is limited to tertiary settings, the method used in our study can be applied in a broader context to characterise major factors driving the use of CT scanning as well as the use of diagnostic imaging tests. Our study may assist to identify areas worthy of more in-depth investigations to better inform health policy-makers and interventions promoting appropriate use of diagnostic imaging tests.
Supplementary Material
Acknowledgments
We thank the National Health and Medical Research Council, project grant APP1144573 for supporting this work. We would also like to acknowledge the Western Australian Data Linkage Unit and data custodians, as well as the individuals whose data enabled this study. We also acknowledge the contribution of Dr Richard Fox for his work in the conceptualisation and editing of this manuscript, and Mr John Stubbs for his contribution as a consumer representative.
Footnotes
Contributors: NTH is responsible for the overall content as the guarantor. The guarantor acepts full responsibility for the work and/or conduct of the study, ans had access to the data. RM and NTH controlled the decision to publish. RM, MKB, JD, DM, POL, JS, SM and NTH conceived the idea and study design for the manuscript. NTH, RM and SM conducted data analyses and drafted the manuscript. RM, SM, NTH and MB contributed to statistical expertise. RM, MB, JD, DM, POL, JS, SM and NTH contributed in analysis, interpreting the results, drafting and revising critically for important intellectual content of the manuscript. RM, MB, JD, DM, POL and JS secured funding for the study. All authors read and approved the final version of the manuscript for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This work was supported by the National Health and Medical Research Council, project grant APP1144573. The study funders had no role in the study design, conduct, manuscript writing or decision to submit for publication.
Competing interests: The authors have no competing interest to declare. The institutions of RM, NH, DY, MB and DM received grant funding from the National Medical Research Council of Australia for investigator-initiated research. The funding agreement ensured author independence in designing the study, interpreting the data, writing and publishing the report.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data access is limited to only authors who require it for data analysis - the remaining authors do not have access to the data but did have full access to the results of the data analysis. The data that support the findings of this study are available from the relevant data custodians of the study datasets. Restrictions by the data custodians mean that the data are not publicly available or able to be provided by the authors. Researchers wishing to access the datasets used in this study should refer to the WA data linkage application process (https://www.datalinkage-wa.org.au/access-and-application).Data may be obtained from a third party and are not publicly available.Data access is limited to only authors who require it for data analysis - the remaining authors do not have access to the data but did have full access to the results of the data analysis. The data that support the findings of this study are available from the relevant data custodians of the study datasets. Restrictions by the data custodians mean that the data are not publicly available or able to be provided by the authors. Researchers wishing to access the datasets used in this study should refer to the WA data linkage application process (https://www.datalinkage-wa.org.au/access-and-application).
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Human research ethics approval was obtained from Curtin University Human Research Ethics Committee (SMEC-80-10) and the WA Department of Health Human Research Ethics Committee (2011/97) which exempted the study from requiring individual consent.
References
- 1.Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998-2007. JAMA 2010;304:1465–71. 10.1001/jama.2010.1408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pelc NJ. Recent and future directions in CT imaging. Ann Biomed Eng 2014;42:260–8. 10.1007/s10439-014-0974-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Royal Australian and New Zealand College of Radiologist . Radiology at a glance Australia Sydney: the Royal Australian and New Zealand College of radiologist, 2018. https://www.ranzcr.com/college/document-library/radiology-at-a-glance-australia [Google Scholar]
- 4.OECD Data . Computed tomography (CT) exams: OECD data, 2018. Available: https://data.oecd.org/healthcare/computed-tomography-ct-exams.htm
- 5.Australian Radiation Protection and Nuclear Safety Agency . Ionising radiation and health: Australian government, 2015. Available: https://www.arpansa.gov.au/sites/default/files/legacy/pubs/factsheets/IonisingRadiationandHealth.pdf
- 6.Australian Radiation Protection and Nuclear Safety Agency . Current Australian National diagnostic reference levels for multi detector computed tomography: Australian radiation protection and nuclear safety agency, 2018. Available: https://www.arpansa.gov.au/research-and-expertise/surveys/national-diagnostic-reference-level-service/current-australian-drls-update/mdct
- 7.Picano E. Sustainability of medical imaging. BMJ 2004;328:578–80. 10.1136/bmj.328.7439.578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martins R, Raimundo P, Alves P, et al. Appropriateness of radiology test requests by an emergency department: a retrospective study. Acta Med Port 2020;33:7–14. 10.20344/amp.12075 [DOI] [PubMed] [Google Scholar]
- 9.Tung M, Sharma R, Hinson JS, et al. Factors associated with imaging overuse in the emergency department: a systematic review. Am J Emerg Med 2018;36:301–9. 10.1016/j.ajem.2017.10.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Royal Australian and New Zealand College of Radiologists . Quality and standards Sydney: the Royal Australian and New Zealand College of radiologists, 2019. Available: https://www.ranzcr.com/our-work/quality-standards
- 11.DI P. Diagnostic imaging pathways. Government of Western Australia, 2020. [Google Scholar]
- 12.Bairstow PJ, Mendelson R, Dhillon R, et al. Diagnostic imaging pathways: development, dissemination, implementation, and evaluation. Int J Qual Health Care 2006;18:51–7. 10.1093/intqhc/mzi078 [DOI] [PubMed] [Google Scholar]
- 13.Bhatia RS, Levinson W, Shortt S. Measuring the effect of choosing wisely: an integrated framework to assess campaign impact on low-value care. BMJ Quality &amp; Safety 2015;24:523. [DOI] [PubMed] [Google Scholar]
- 14.IK I, Mortele KJ, Prevedello LM, et al. Repeat abdominal imaging examinations in a tertiary care hospital. Am J Med 2012;125:155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blazak P, Hacking C, Presneill J, et al. Early repeat computed tomographic imaging in transferred trauma and neurosurgical patients: incidence, indications and impact. J Med Imaging Radiat Oncol 2018. [DOI] [PubMed] [Google Scholar]
- 16.Colla CH, Morden NE, Sequist TD, et al. Choosing wisely: prevalence and correlates of low-value health care services in the United States. J Gen Intern Med 2015;30:221–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Badgery-Parker T, Pearson S-A, Chalmers K, et al. Low-Value care in Australian public hospitals: prevalence and trends over time. BMJ Qual Saf 2019;28:205–14. 10.1136/bmjqs-2018-008338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hong AS, Ross-Degnan D, Zhang F, et al. Small decline in low-value back imaging associated with the 'choosing wisely' campaign, 2012-14. Health Aff 2017;36:671–9. 10.1377/hlthaff.2016.1263 [DOI] [PubMed] [Google Scholar]
- 19.Benchimol EI, Smeeth L, Guttmann A, et al. The reporting of studies conducted using observational Routinely-collected health data (RECORD) statement. PLoS Med 2015;12:e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holman C D'Arcy J, Bass AJ, Rosman DL, et al. A decade of data linkage in Western Australia: strategic design, applications and benefits of the WA data linkage system. Aust Health Rev 2008;32:766–77. 10.1071/AH080766 [DOI] [PubMed] [Google Scholar]
- 21.Holman CD, Bass AJ, Rouse IL, et al. Population-based linkage of health records in Western Australia: development of a health services research linked database. Aust N Z J Public Health 1999;23:453–9. [DOI] [PubMed] [Google Scholar]
- 22.Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff 2008;27:1491–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.AIHW . Rural, regional and remote health: a guide to remoteness classifications: AIHW, 2004. Available: https://www.aihw.gov.au/reports/rural-remote-australians/guide-to-remoteness-classifications/formats
- 24.Australian Bureau of Statistics . Census of population and housing: socio-economic indexes for areas Canberra. Australian Bureau of Statistics, 2011. [Google Scholar]
- 25.Holman CD, Preen DB, Baynham NJ, et al. A multipurpose comorbidity scoring system performed better than the Charlson index. J Clin Epidemiol 2005;58:1006–14. [DOI] [PubMed] [Google Scholar]
- 26.Australian Institute of Health and Welfare . Admitted patient care 2014–15: Australian hospital statistics. Contract No.: Cat. no. HSE 172. Canberra: AIHW, 2016. [Google Scholar]
- 27.Powers DA, Yoshioka H, Yun M-S. mvdcmp: multivariate decomposition for nonlinear response models. Stata J 2011;11:556–76. 10.1177/1536867X1201100404 [DOI] [Google Scholar]
- 28.Wright CM, Bulsara MK, Norman R, et al. Increase in computed tomography in Australia driven mainly by practice change: a decomposition analysis. Health Policy 2017;121:823–9. 10.1016/j.healthpol.2017.04.010 [DOI] [PubMed] [Google Scholar]
- 29.Gibson DAJ, Moorin RE, CDAJ H. Cohort study of Western Australia computed tomography utilisation patterns and their policy implications. BMC Health Serv Res 2014;14:526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mendelson RM, Bairstow PJ. Inappropriate imaging: why it matters, why it happens, what can be done. J Med Imaging Radiat Oncol 2010;54:173–7. [DOI] [PubMed] [Google Scholar]
- 31.Medical Benefits Reviews Task Group, Diagnostic Imaging Review Team . Review of funding for diagnostic imaging services: final report department of health 2012.
- 32.Mendelson R. Diagnostic imaging pathways Perth: health department of West Australia, 2010. Available: https://www.cancerwa.asn.au/resources/2015-08-19-Richard-Mendelson-presentation.pdf
- 33.Commonwealth of Australia . Availability and accessibility of diagnostic imaging equipment around Australia. Canberra ACT 2600: Parliament House. Contract No.: ISBN 978-1-76010-715-4 2018.
- 34.OECD Data . Computed tomography (CT) scanners: OECD Data, 2018. Available: https://data.oecd.org/healtheqt/computed-tomography-ct-scanners.htm
- 35.van de Wetering R, Batenburg R, Versendaal J, et al. A balanced evaluation perspective: picture archiving and communication system impacts on hospital workflow. J Digit Imaging 2006;19:10–17. 10.1007/s10278-006-0628-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chakera T, Nagree Y, Song S, et al. Bridging the communication gap between public and private radiology services. Med J Aust 2009;191:558–60. 10.5694/j.1326-5377.2009.tb03310.x [DOI] [PubMed] [Google Scholar]
- 37.Vest JR, Jung H-Y, Ostrovsky A, et al. Image sharing technologies and reduction of imaging utilization: a systematic review and meta-analysis. J Am Coll Radiol 2015;12:1371–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-052954supp001.pdf (242.9KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data access is limited to only authors who require it for data analysis - the remaining authors do not have access to the data but did have full access to the results of the data analysis. The data that support the findings of this study are available from the relevant data custodians of the study datasets. Restrictions by the data custodians mean that the data are not publicly available or able to be provided by the authors. Researchers wishing to access the datasets used in this study should refer to the WA data linkage application process (https://www.datalinkage-wa.org.au/access-and-application).Data may be obtained from a third party and are not publicly available.Data access is limited to only authors who require it for data analysis - the remaining authors do not have access to the data but did have full access to the results of the data analysis. The data that support the findings of this study are available from the relevant data custodians of the study datasets. Restrictions by the data custodians mean that the data are not publicly available or able to be provided by the authors. Researchers wishing to access the datasets used in this study should refer to the WA data linkage application process (https://www.datalinkage-wa.org.au/access-and-application).