Abstract
Background:
Among people receiving residential treatment for a substance use disorder (SUD), premature treatment termination predicts poor post-treatment outcomes. We examined the utility of the alternative model for personality disorders (AMPD) for predicting premature residential SUD treatment termination, including interactions with age and gender.
Methods:
Participants (N = 374) were receiving residential treatment for SUD and enrolled in a clinical trial with two conditions: Skills for Improving Distress Intolerance (SIDI) and Supportive Counseling (NCT01741415). Participants were assessed at intake on AMPD traits using the Personality Inventory for DSM-5 (PID-5) and tracked longitudinally. After establishing gender and age measurement invariance, we used competing risk models to predict treatment completion versus premature termination using interactions of PID-5 scores with age and gender.
Findings:
Disinhibition and Negative Emotionality domains and facets predicted premature treatment termination, particularly among younger, male participants. There were positive effects of SIDI on treatment completion for participants with high levels of domain and facet Negative Emotionality. A small proportion (≈ 12 %) of the PID-5 items showed differential item functioning by age or gender; however, the aggregate impact on test-level total scores was negligible.
Conclusions:
Participants (particularly young men) displaying poor self-control and emotional regulation are at risk for premature termination. These findings, together with minimal aggregate differential item functioning at the scale level, suggest that the PID-5 is a practically useful, construct-valid, non-proprietary measure, aspects of which can be used for screening in residential SUD treatment. Furthermore, among those with high negative emotionality, SIDI may be effective in preventing premature treatment termination.
Keywords: Treatment attrition, Treatment completion, Addiction, Substance use, Personality, Dimensional, Personality disorders, Risk factors
1. Introduction
Substance misuse continues to be a global problem affecting individuals, families, and communities. For example, in the United States, ≈ 20 million people aged 12+ suffer from substance use disorders (SUDs) (Substance Abuse and Mental Health Services Administration [SAMHSA], 2018). Approximately 2.5 million people with an SUD received specialty inpatient treatment in the past year (SAMHSA, 2018). However, 24–54 % of these patients prematurely terminate treatment (SAMHSA, 2018; Stark, 1992). Early treatment termination is one of the strongest predictors of poor outcomes upon community reintegration, including poor health, relapse, and readmission to residential treatment (Brewer et al., 1998; Moos et al., 1995; Stark, 1992; Stevens et al., 2015). Identifying patients vulnerable to premature termination is critical.
1.1. Demographic and personality factors predict early treatment termination
Demographic, personality, and psychopathology variables are all related to treatment completion. In a systematic review, age and gender each predicted premature termination in ≈ 50 % of studies (Brorson et al., 2013; but see Hedges and Olkin, 1980). Moreover, personality traits - particularly neuroticism, aggression, impulsivity, sensation seeking, and hostility are robust and well-established predictors of premature treatment termination (Loree et al., 2015; Patkar et al., 2004; Petry and Bickel, 2000; Stevens et al., 2015, 2014), and substance use treatment outcomes more generally (Basharpoor et al., 2019; Hershberger et al., 2017). Aspects of disinhibition predict premature termination and other addiction treatment outcomes across inpatient and outpatient samples, types of substance use disorder (opiates, alcohol, cocaine, etc.), definitions of disinhibition (e.g., as sensation-seeking or impulsivity), and assessment modality (self-report or behavioral task; Loree et al., 2015, but see Stevens et al., 2014 for opposing findings).
1.2. Demographic moderation of personality–treatment attrition relationships
Personality traits can help to distinguish people who will successfully complete residential addictions treatment from those who will not. However, previous findings are mixed, which may be due to small sample sizes or variation in the relevance of these traits by demographic subgroups. For example, several studies have also shown robust gender differences in neuroticism and aspects of disinhibition, such that women tend to have higher levels of neuroticism and lower levels of disinhibition compared to men (South et al., 2018, 2017; Suzuki et al., 2019). In terms of treatment retention specifically, some studies have also found the impacts of maladaptive personality traits (e.g., hostility) on treatment attrition to be stronger for women than men (Petry and Bickel, 2000; Siqueland et al., 2002). However, most studies examining the intersection of personality and treatment attrition have used samples that were heavily, if not entirely, male (Kravitz et al., 1999; Samuel et al., 2011). Given this overrepresentation of men, relatively small sample sizes, and discrepancies in the literature, there is a clear need for large-scale investigations that examine whether gender moderates the relationship between personality characteristics on treatment outcomes (Brorson et al., 2013; Samuel et al., 2011).
In addition to gender, age may similarly moderate personality–treatment attrition relationships. Both theoretical models and empirical research suggest that some maladaptive personality traits and associated behaviors (e.g., sensation-seeking, impulsivity) are elevated in young adults (Steinberg et al., 2008), but then may ‘burn out’ over time, whereas other (e.g., emotional distress, anger) remain relatively stable (Argyriou et al., 2020; Engels et al., 2003; Paris, 2003; Stepp and Pilkonis, 2008; Ullrich and Coid, 2009; Zanarini et al., 2007). Accordingly, the predictive value of some traits as risk factors for early treatment termination may vary with age. For example, elevated levels of high-activity traits like impulsivity and sensation-seeking may signal attrition propensity in relatively young people, but these traits’ predictive validity may be lower among older populations where both trait levels and attrition base rates are lower. To this end, understanding the moderating effects of demographics on personality is a clinically relevant question for treatment selection and triage. If personality characteristics predict attrition and do so particularly well in a demographic subgroup, it may be more cost-effective and practical to administer trait-focused interventions in this subgroup. It may also be useful to “frontload” (i.e., administer treatment sessions over a shorter period) psychological treatments (Storch et al., 2007) for this subgroup, given the increased risk of treatment dropout.
1.3. Measurement invariance
A crucial step before examining demographic characteristics as moderators of trait–outcome relationships is to establish that the measure functions equivalently across groups. If the relationship between observed scale scores and the underlying latent trait differs across groups—that is, the scale demonstrates measurement non-invariance—this can produce spurious interaction effects (Borsboom, 2006; Embretson, 1996). To date, however, examining measurement invariance of clinical traits across demographic groups has not been common practice. Consequently, relatively few studies have examined measurement invariance of pathological personality traits across demographic factors (Argyriou et al., 2020; Suzuki et al., 2019; Van den Broeck et al., 2013). Differential functioning could produce spurious trait by demographic interactions in estimating treatment prognosis, efficacy, or effectiveness; such effects would need to be incorporated into scoring and interpretation.
1.4. Current study
The current study estimated the predictive power of major personality factors (i.e., Negative Emotionality, Detachment, Disinhibition, Antagonism, and Psychoticism) and the 25 associated facets for premature treatment termination from a residential addiction treatment facility. We used the Personality Inventory for DSM-5 (Krueger et al., 2012), a non-proprietary measure that was built to index the alternative model for personality disorders (AMPD), which in turn bridges the continuum between normal and pathological traits. Based on previous research, we hypothesized that traits related to disinhibition, antagonism, and neuroticism would best predict premature treatment termination. Evidence that baseline PID-5 scores predict premature termination would support the longitudinal predictive validity of the AMPD for a critical clinical care outcome.
We also examined interactions of AMPD traits with age and gender to examine if AMPD traits better predict treatment attrition for some subgroups than others. We predicted that PID-5 facets and domains would better predict treatment attrition for younger, rather than older people. Given the mixed literature, we had no directional predictions for gender. Identifying whether trait–attrition relationships differ across age and gender groups can enhance the clinical utility of attrition prediction models by tailoring attrition risk assessments to each patient’s characteristics. To avoid spurious interactions, we first fit measurement invariance models, then estimated participant’s trait factor scores while accounting for any differential item functioning.
2. Method
2.1. Participants
Participants were 374 patients (241 men, 133 women; 295 non-Latino White, 61 Black, 18 other racial/ethnic groups, mean age = 34.51 [SD = 10.78]) who were receiving residential treatment for SUD and enrolled in a clinical trial with two conditions: Skills for Improving Distress Intolerance (SIDI) and Supportive Counseling (SC). Comparison of these two conditions on the primary outcomes of post-treatment and follow-up changes in distress tolerance and substance use is the focus of another report (Bornovalova et al., under review). Study participants were recruited between April 2013 and October 2017. 309 (82.6 %) were court-mandated to treatment. Educational level was evenly distributed: 100 (26.7 %) participants had less than a high school diploma, 142 (38.0 %) had a high school diploma or GED equivalent, and 132 (35.3 %) had some college education or higher. To avoid effects of possible substance withdrawal symptoms, all baseline assessments occurred within 7–14 days of admission. Inclusion criteria included: age 18–65, ability to give informed consent, and ability to understand English1,2. The protocol was approved by the University of South Florida institutional review board (Pro00009634).
2.2. Setting
The residential addiction treatment facility serves as an alternative to county jails for substance users but accepts voluntary admissions as well. Treatment involves a mix of strategies adopted from Alcoholics and Narcotics Anonymous and group sessions focused on psychoeducation and relapse prevention. All participants complete detoxification (if needed) prior to entering this treatment facility. Complete abstinence from drugs and alcohol (except for caffeine and nicotine) is required upon entry and throughout the program. Regular drug testing is provided and any drug or alcohol use results in immediate dismissal. All patients are required to stay in the residential treatment for a minimum of 30 days. Beyond the 30-day checkpoint, most participants are encouraged to stay longer at the facility to stabilize psychosocially and enhance abstinence outcomes. A patient was considered to have successfully completed treatment when they met criteria for a less restrictive environment, including obtaining stable housing and income/benefits. This process generally took 3–6 months.
2.3. Measures
2.3.1. Treatment completion
The site liaison obtained treatment completion information through continuous contact with the residential treatment site throughout the study period. Of the 374 participants, 116 (31.7 %) terminated treatment prematurely (departing before meeting transition criteria). Reasons for premature termination included rule breaking (e.g., possessing contraband, destruction of property, sexual relations with other patients), arrest or transfer to jail/prison, transfer to a higher-level treatment facility (e.g., for non-suicidal self-injury), and/or unwillingness to participate in the treatment plan. Of the remaining participants, 240 (64.2 %) ended treatment successfully. The remaining 18 participants were censored. Of these, 10 (2.7 %) ended treatment prematurely for medical reasons (e.g., unmanageable diabetes, cancer), 2 (0.5 %) had missing data on their discharge status (successful/unsuccessful), and 6 (1.6 %) continued in treatment for longer than 185 days, generally due to being treated for more severe psychotic disorders; to avoid overfitting to these unusual cases, these participants were treated as censored at 185 days.
2.3.2. Alternative model for personality disorders traits
The AMPD includes 25 pathological personality traits nested within 5 higher-order superfactors (Negative Affectivity, Detachment, Antagonism, Disinhibition, Psychoticism). It is a conceptual descendent of the influential Five-Factor (Big Five) model of personality (Goldberg, 1990; John et al., 2008; McCrae and Costa, 1997). AMPD traits were assessed using the 220-item Personality Inventory for DSM-5 (PID-5; Krueger et al., 2012), scored using the updated procedures (American Psychiatric Association, 2014). AMPD traits, as measured by the Personality Inventory for DSM-5 (PID-5; Krueger et al., 2012), correlate with normal-range Big Five traits (Al-Dajani et al., 2016) and with traditional personality disorder diagnoses in clinical and non-clinical settings (Few et al., 2013; Miller et al., 2015). In other analysis of the AMPD in this sample (Wiernik et al., 2020), we examined the longitudinal invariance, treatment changes, and predictors of relapse/recidivism of the PID-5 traits. Table 1 reports reliabilities for each scale.
Table 1.
Baseline Characteristics of Participants Completing vs Terminating Treatment.
|
|
Complete Treatment |
Terminate Treatment |
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| α | ω | Mean or Prop. | SD | Mean or Prop. | SD | d/Diff | 95%CI | ||
| Demographics | |||||||||
| Days in treatment | ― | ― | 135.35 | 48.94 | 78.48 | 50.56 | −56.87 | −67.87 | −45.87 |
| Age (years) | ― | ― | 35.74 | 11.00 | 32.26 | 9.83 | −3.47 | −5.84 | −1.11 |
| Prop. male | ― | ― | 0.62 | ― | 0.68 | ― | 0.06 | −0.04 | 0.17 |
| Prop. white | ― | ― | 0.83 | ― | 0.74 | ― | −0.09 | −0.18 | 0.00 |
| Prop. completed high school | ― | ― | 0.77 | ― | 0.66 | ― | −0.11 | −0.21 | −0.01 |
| Prop. court mandate | ― | ― | 0.82 | ― | 0.87 | ― | 0.05 | −0.04 | 0.13 |
| Prop. active condition (SIDI) | ― | ― | 0.51 | ― | 0.53 | ― | 0.02 | −0.10 | 0.14 |
| PID-5 Traits | |||||||||
| Negative Affectivity | 0.93 | 0.93 | −.06 | 1.00 | .11 | 1.02 | .16 | −.06 | 0.39 |
| Emotional Lability | 0.87 | 0.87 | −.07 | 1.00 | .09 | 1.02 | .16 | −.07 | 0.38 |
| Anxiousness | 0.89 | 0.90 | .04 | 1.00 | .10 | 1.00 | .14 | −.08 | 0.36 |
| Separation Insecurity | 0.88 | 0.89 | −.07 | 0.99 | .12 | 1.04 | .18 | −.04 | 0.41 |
| Submissiveness | 0.77 | 0.77 | −.04 | 0.99 | −.09 | 1.02 | −.12 | −.34 | 0.10 |
| Hostility | 0.89 | 0.89 | −.11 | 0.97 | .21 | 1.04 | .32 | .09 | 0.54 |
| Perseveration | 0.86 | 0.86 | −.07 | 0.99 | .13 | 1.02 | .20 | −.02 | 0.42 |
| Detachment | 0.91 | 0.92 | −.05 | 1.01 | .07 | 1.00 | .12 | −.10 | 0.34 |
| Anhedonia | 0.82 | 0.82 | −.05 | 0.99 | .08 | 1.04 | .13 | −.09 | 0.35 |
| Depressivity | 0.92 | 0.92 | −.04 | 1.01 | .05 | 1.02 | .09 | −.14 | 0.31 |
| Intimacy Avoidance | 0.79 | 0.80 | −.02 | 1.01 | −.01 | 1.01 | .01 | −.21 | 0.23 |
| Restricted Affectivity | 0.74 | 0.74 | −.09 | 0.94 | .11 | 1.09 | .19 | −.03 | 0.42 |
| Suspiciousness | 0.65 | 0.68 | −.04 | 1.02 | .06 | 0.97 | .10 | −.13 | 0.32 |
| Withdrawal | 0.89 | 0.89 | −.05 | 1.00 | .06 | 1.01 | .11 | −.11 | 0.33 |
| Antagonism | 0.91 | 0.92 | −.05 | 0.98 | .12 | 1.05 | .18 | −.05 | 0.40 |
| Attention Seeking | 0.88 | 0.89 | −.05 | 1.01 | .11 | 0.98 | .16 | −.07 | 0.38 |
| Grandiosity | 0.75 | 0.75 | −.08 | 0.96 | .13 | 1.05 | .22 | −.01 | 0.44 |
| Callousness | 0.89 | 0.90 | −.13 | 0.89 | .24 | 1.14 | .38 | .15 | 0.60 |
| Deceitfulness | 0.87 | 0.88 | −.05 | 0.99 | .10 | 1.02 | .15 | −.08 | 0.37 |
| Manipulativeness | 0.86 | 0.86 | −.04 | 0.96 | .14 | 1.09 | .18 | −.04 | 0.40 |
| Disinhibition | 0.91 | 0.91 | −.10 | 1.01 | .18 | 0.96 | .28 | .05 | 0.50 |
| Distractibility | 0.90 | 0.90 | −.08 | 1.02 | .13 | 0.99 | .21 | −.01 | 0.43 |
| Impulsivity | 0.83 | 0.84 | −.08 | 0.99 | .17 | 0.98 | .25 | .02 | 0.47 |
| Irresponsibility | 0.74 | 0.74 | −.08 | 1 | .13 | 1.01 | .22 | −.01 | 0.44 |
| Rigid Perfectionism | 0.89 | 0.89 | −.06 | 0.98 | .09 | 1.05 | .15 | −.07 | 0.37 |
| Risk Taking | 0.88 | 0.88 | −.09 | 1 | .21 | 0.99 | .31 | .08 | 0.53 |
| Psychoticism | 0.96 | 0.96 | −.04 | 1.04 | .02 | 0.91 | .06 | −.17 | 0.28 |
| Eccentricity | 0.95 | 0.95 | −.07 | 1.02 | .10 | 0.96 | .17 | −.05 | 0.40 |
| Perceptual Dysregulation | 0.88 | 0.88 | −.04 | 1.04 | .00 | 0.89 | .04 | −.18 | 0.26 |
| Unusual Beliefs | 0.86 | 0.87 | −.02 | 1.01 | .01 | 0.97 | .02 | −.20 | 0.25 |
Note: Tx = treatment, prop. = proportion, SD = standard deviation, Diff. = difference, d = Cohen’s d, 95 % CI = 95 % asymmetric confidence interval. Domain names are italicized. PID-5 values are for estimated factor scores accounting for any differential item functioning; comparisons for PID-5 sum scores are available in Table S1.
2.4. Analyses
2.4.1. Survival analyses
We predicted treatment completion using competing risks proportional hazard models (Therneau and Grambsch, 2000) using the survival package (Therneau, 2020, version 3.2 3) in R (R Core Team, 2020, version 4.0.2)3. In these models, participants are all initially in an “in treatment” state. The model predicts each patient’s probability of transitioning from this state to either the “treatment completed” or “treatment terminated” states at each day of treatment. A positive β coefficient (hazard ratio [HR] > 1.0) for “treatment completed” indicates that a person higher on the predictor is more likely to successfully complete treatment and do so faster. A positive β coefficient (HR > 1.0) for “treatment terminated” indicates that a person higher on that predictor is more likely to prematurely terminate treatment and do so faster.
A competing risks model is important when modeling treatment termination. A traditional survival analysis assumes non-informative censoring—participants who are censored are equally likely to experience the event (premature termination) as those who are not. When predicting premature termination, many people successfully complete treatment. This is a distinct endpoint; they are not merely “yet to terminate.”
We first fit a simple competing risks model with no covariates to examine overall treatment completion and termination trends. Next, we fit models adding age, gender, one PID-5 trait score, and trait × age and trait × gender terms.4 In all models, we used men as the reference gender group (men = 0, women = 1), centered age at 18, and standardized PID-5 traits as z-scores. We estimated PID-5 scores using full information maximum likelihood (FIML) from the final measurement models accounting for any DIF (see Measurement Invariance in supplemental materials). Finally, in our exploratory analyses, we added condition and the interaction of condition with PID-5 traits to the model already containing age and gender.
We note that the 25 facets tested are nested in 5 domains due to theoretical and empirical intercorrelation. Hence, multiple tests conducted in the present study are highly correlated and represent an examination of the robustness of results. Consistent with statistical recommendations (Vasilopoulos et al., 2016), we report empirical unadjusted p-values and confidence intervals; our interpretations consider the number of tests conducted among correlated outcomes.
To interpret results, we regarded a trait coefficient of as a clinically-relevant moderate effect size (Anvari and Lakens, 2019; Wiernik et al., 2017). An effect of this magnitude corresponds, for example, to an increased termination risk for age-18 men from 44 % with mean-level scores (z = 0) to 71 % with highly-elevated scores (z = +2), as well a decrease in time-to-termination among terminating patients from 75 days (z = 0) to only 53 days (z = +2). For effect size comparisons across age or gender groups, we regarded a difference of as clinically meaningful. Such a difference reflects a change from moderate-to-strong to weak-to-negligible predictive utility.
3. Results
Descriptive statistics for variables among participants completing versus terminating treatment are shown in Tables 1 and S1. Table S2 shows correlations among all variables. As a group, participants who prematurely terminated treatment were similar in age, gender, race/ethnicity, education, court mandate status, and treatment condition in the clinical trial. Participants who terminated treatment scored somewhat to moderately higher (d ≥ .30) on Hostility, Callousness, and Risk Taking; differences on other scales were smaller (cf. Gignac and Szodorai, 2016, estimated quartiles of the empirical effect size distribution in individual differences research as d ≈ .20, .40, .60).
3.1. Measurement invariance
Tables S3 and S4 show measurement invariance results and estimated latent trait mean differences across gender and age. A small proportion of indicators showed DIF. DIF effects were small to moderate (| ESSDi | <.50) and intuitive. Combined DIF effects on test-level total scores were minimal (ESSDt ranged .092 to .084). See the supplement for details.
3.2. Survival analyses
Fig. 1 shows a Kaplan–Meier curve for the simple survival model with no covariates. Participants completing treatment did so after a median of 155 days (IQR = 94, 182). Participants who terminated treatment prematurely did so after a median of 72 days (IQR = 37, 118).
Fig. 1.
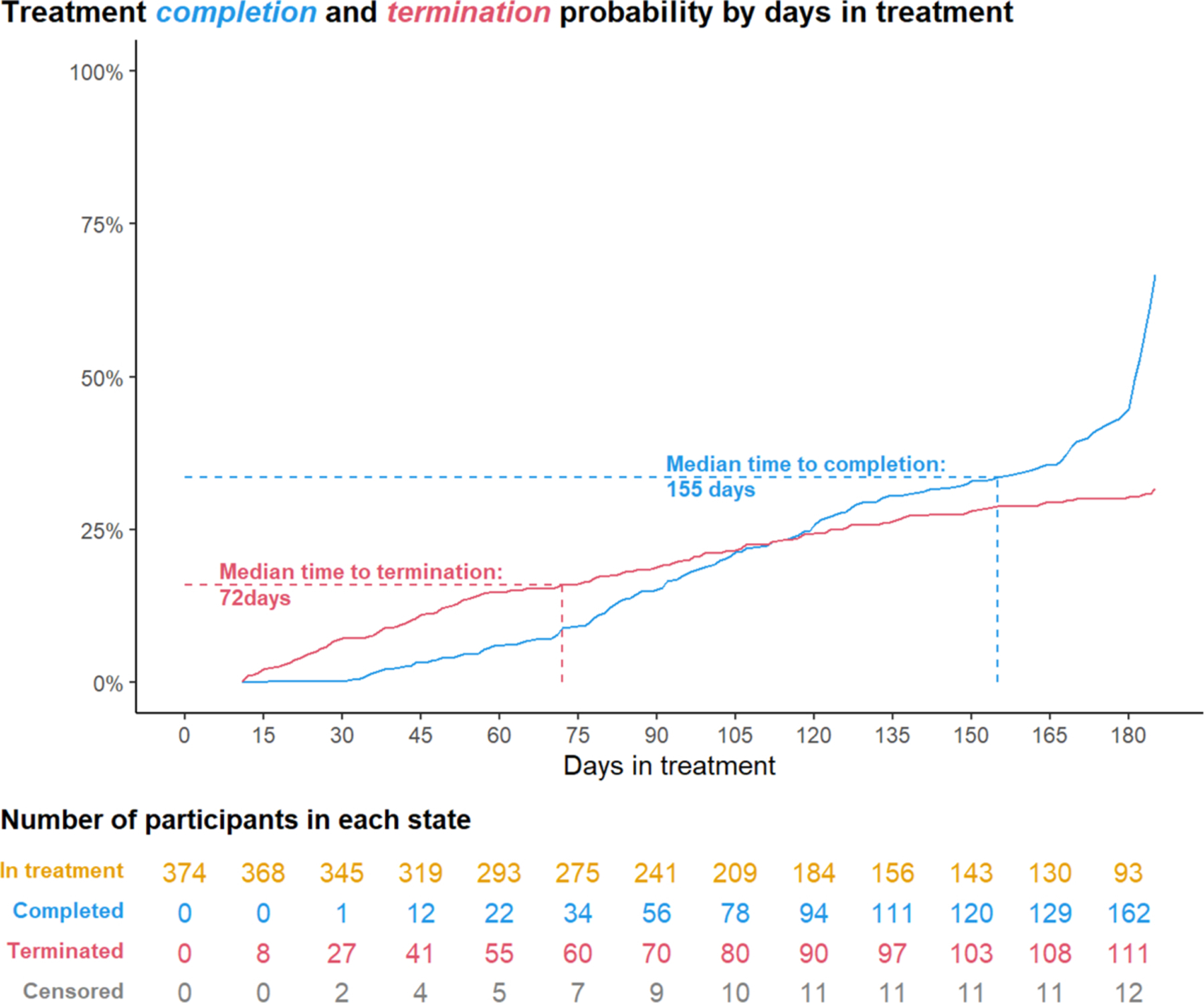
Participants who successfully completed treatment did so after a median of 155 days (IQR = 94, 182).
Participants who prematurely terminated treatment did so after a median of 72 days (IQR = 37, 118).
3.2.1. Gender consistent effects
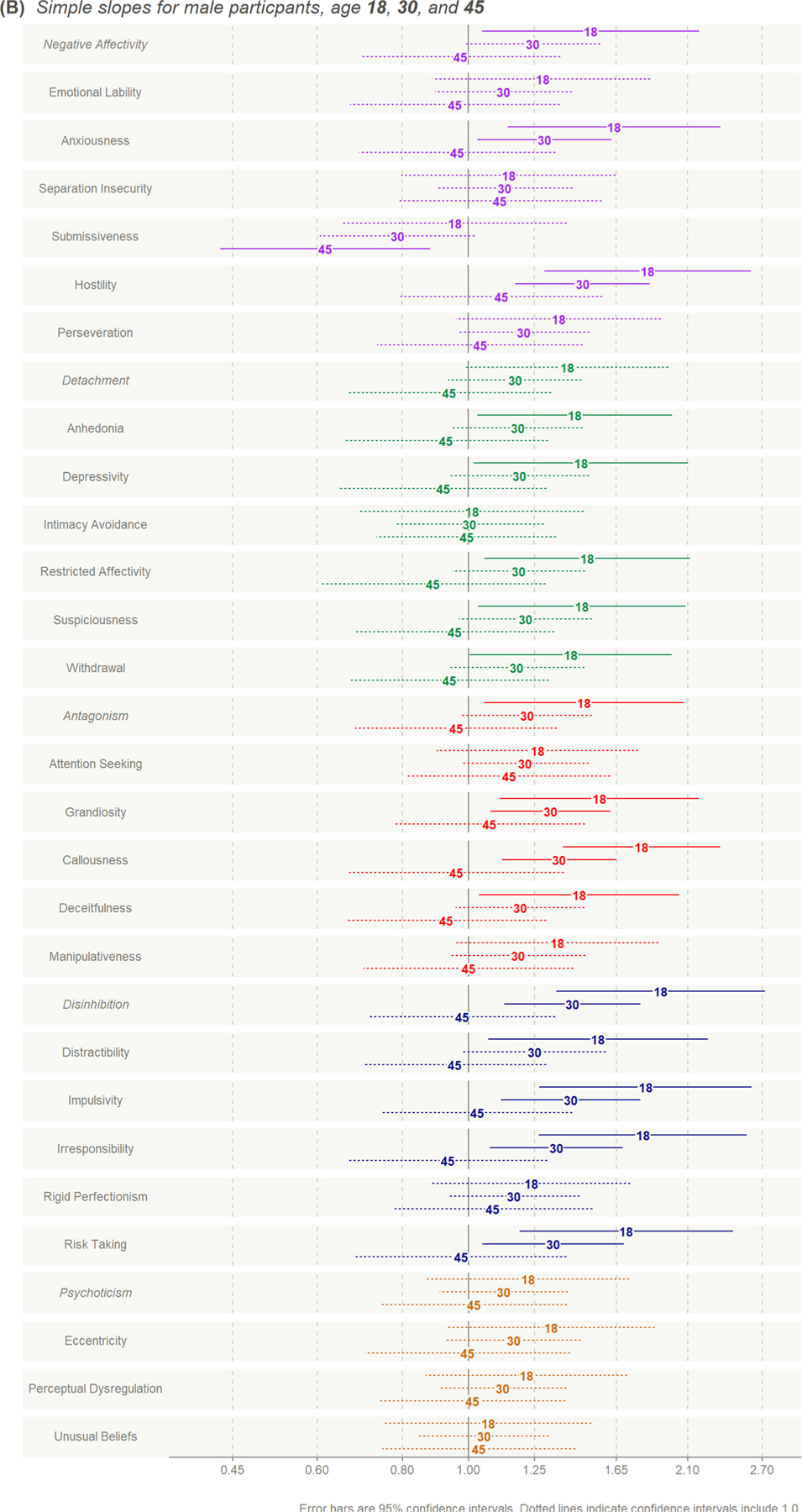
Fig. 2A shows forest plots of hazard ratios for each PID-5 scale for men and women, age-18. Table S5 gives full model coefficients. Table S6 gives estimated simple slopes for PID-5 traits for men age-18, women age-18, men age-30, and men age-455. Fig. 3A shows predicted treatment termination survival curves for men and women, age-18, for PID-5 traits that showed moderate to large effects on termination (β ≥ .40, HR 1.49 for at least one group), which were consistent in magnitude across gender. These curves show the predicted probability that an age-18 person who is (1) male or female with (2) a trait z-score of ‒2, ‒1, 0, 1, or 2, will prematurely terminate by a given day in treatment.
Fig. 2.
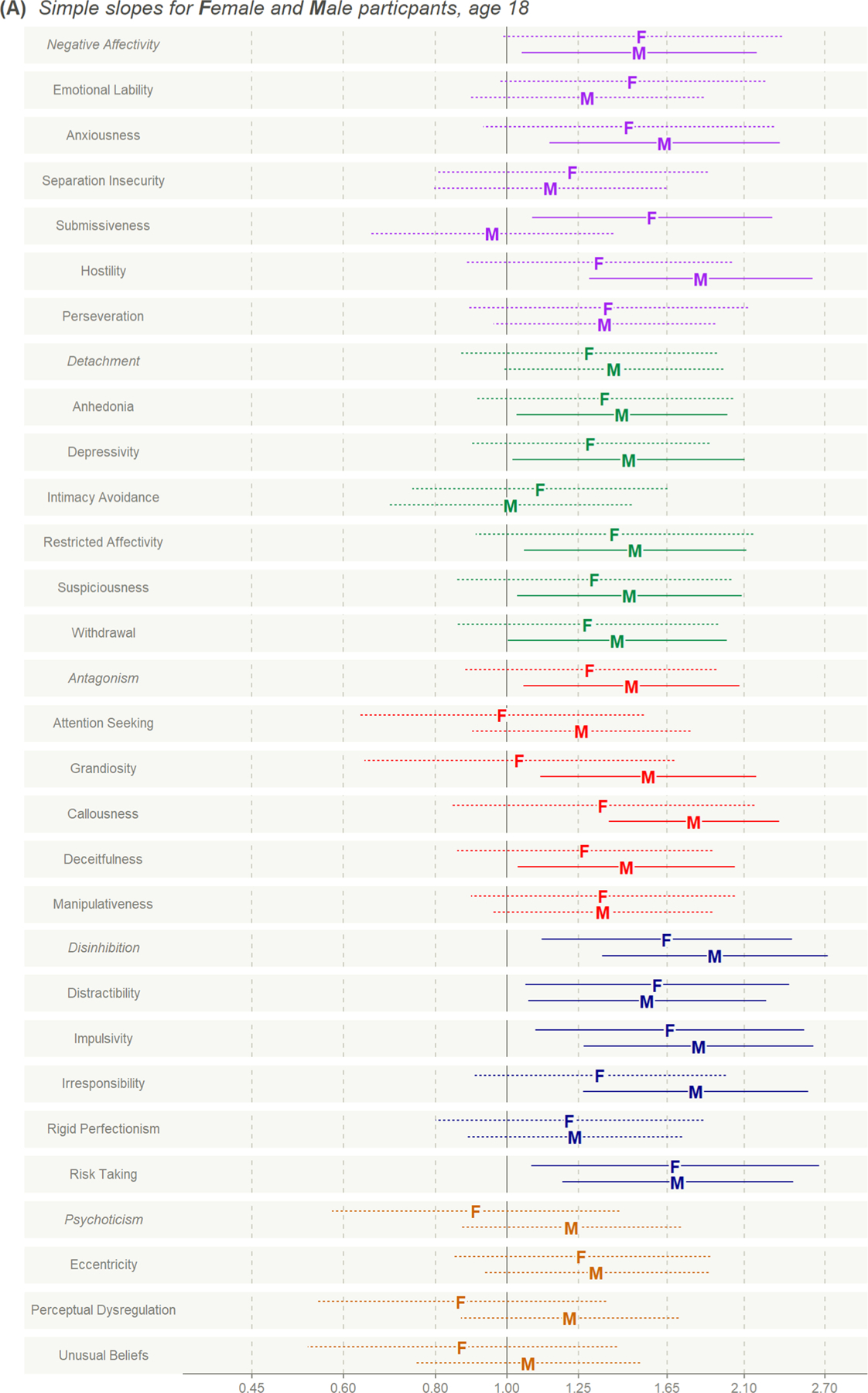
Hazard ratios for PID-5 z-scores predicting premature treatment termination.
Fig. 3.
Trait interactions with gender.
Predicted termination probability by number of days in treatment and PID-5 trait z-score.</p/>Overall, 46 % of age-18 men with mean-level Disinhibition scores (z = 0), but 85 % of age-18 men with highly-elevated Disinhibition (z = +2), are expected to prematurely terminate.
By 61 days, 21 % of age-18 men with mean-level Disinhibition scores (z = 0), but 57 % of age-18 men with highly-elevated Disinhibition (z = +2), are expected to prematurely terminate.
Among age-18 men who terminate treatment, median expected time to termination is 76 days (IQR = 37, 118) when Disinhibition z = 0, but 43 days (IQR = 24, 81) when Disinhibition z = +2.
The trait with the largest effect on treatment termination was Disinhibition (for men age-18, β = .65, HR = 1.92, 95 % CI 1.35, 2.73). This hazard ratio estimates how much more likely a participant is to terminate treatment on a specific day if they are 1 SD higher on the trait ( z = +1). Hazard ratios are most easily interpreted using treatment termination curves. Fig. 3A shows that 46 % of age-18 men with mean-level Disinhibition scores (z = 0) are expected to prematurely terminate, compared with 85 % of age-18 men with highly-elevated Disinhibition (z = +2). Among age-18 men who terminate treatment, median expected time to termination is 76 days when Disinhibition z = 0, but 43 days when Disinhibition z = +2. In addition to Disinhibition, domain Negative Affectivity and facets Distractibility, Impulsivity, Risk Taking, Anxiousness, and Restricted Affectivity each showed moderate to large relationships with treatment termination and termination time that were consistent across genders. For these traits, trait effects on termination were estimated to be similar in size or only slightly smaller for women compared to men. Effects for other traits were smaller.6
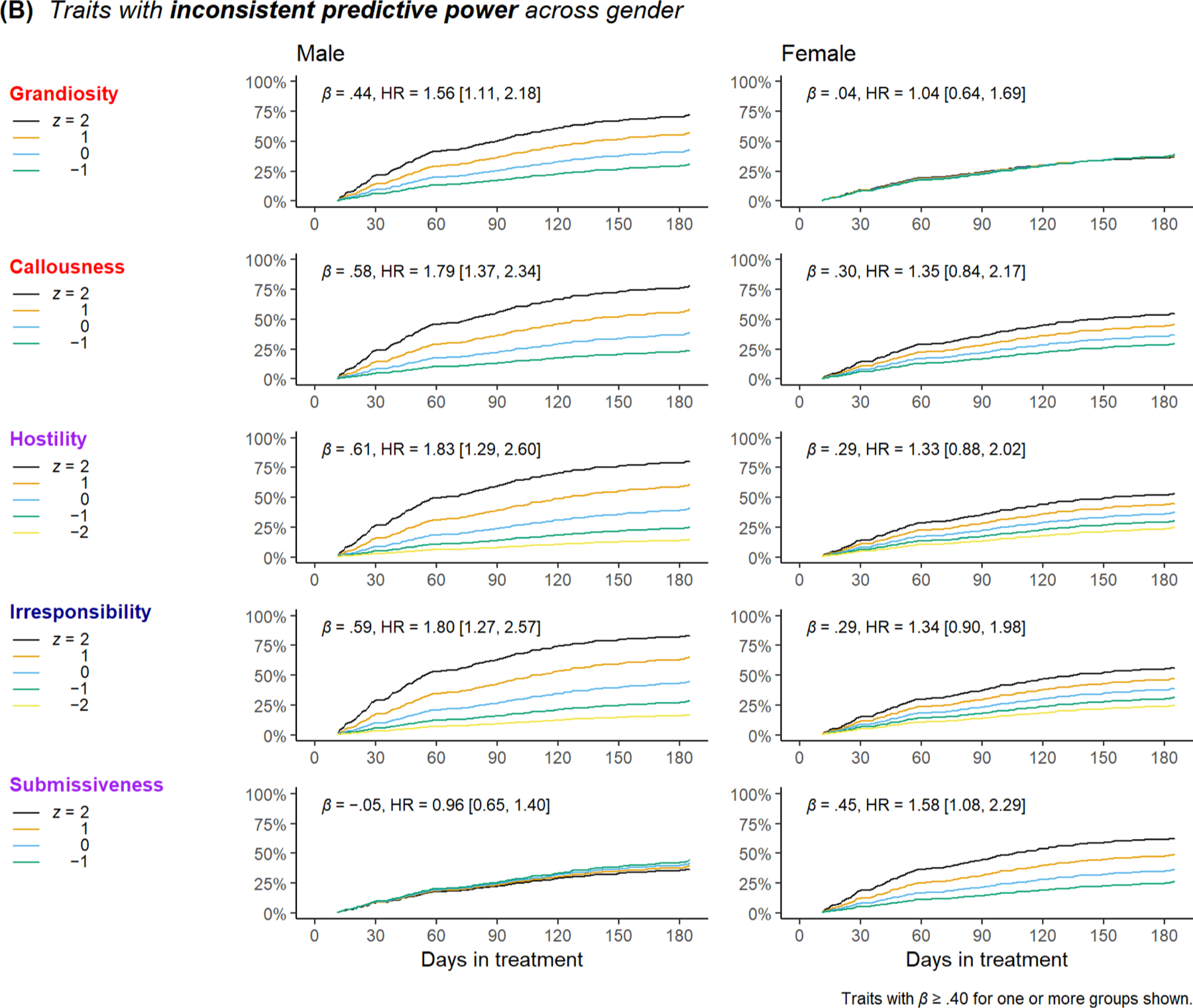
3.2.2. Gender inconsistent effects
Fig. 3B shows treatment termination curves for men and women, age-18, for PID-5 traits whose relationships with premature treatment termination differed substantially across genders ( β > .20 with a simple slope ≥ .40 for one group). Grandiosity was moderately positively related to treatment termination among men (β = .44, HR = 1.56, 95 % CI 1.11, 2.18), but not among women (β = .04, HR = 1.04, 95 % CI 0.64, 1.69). Conversely, Submissiveness was moderately positively related to termination among women (β = .45, HR = 1.58, 95 % CI 1.08, 2.29) but not among men (β = .05, HR = 0.96, 95% CI 0.65, 1.40). Callousness, Hostility, and Irresponsibility related to termination more strongly among men (β ≈ .60, HR ≈ 1.80, 95% CI ≈ 1.80, 2.50) than women (β ≈ .30, HR ≈ 1.35, 95% CI ≈ 0.85, 2.05).
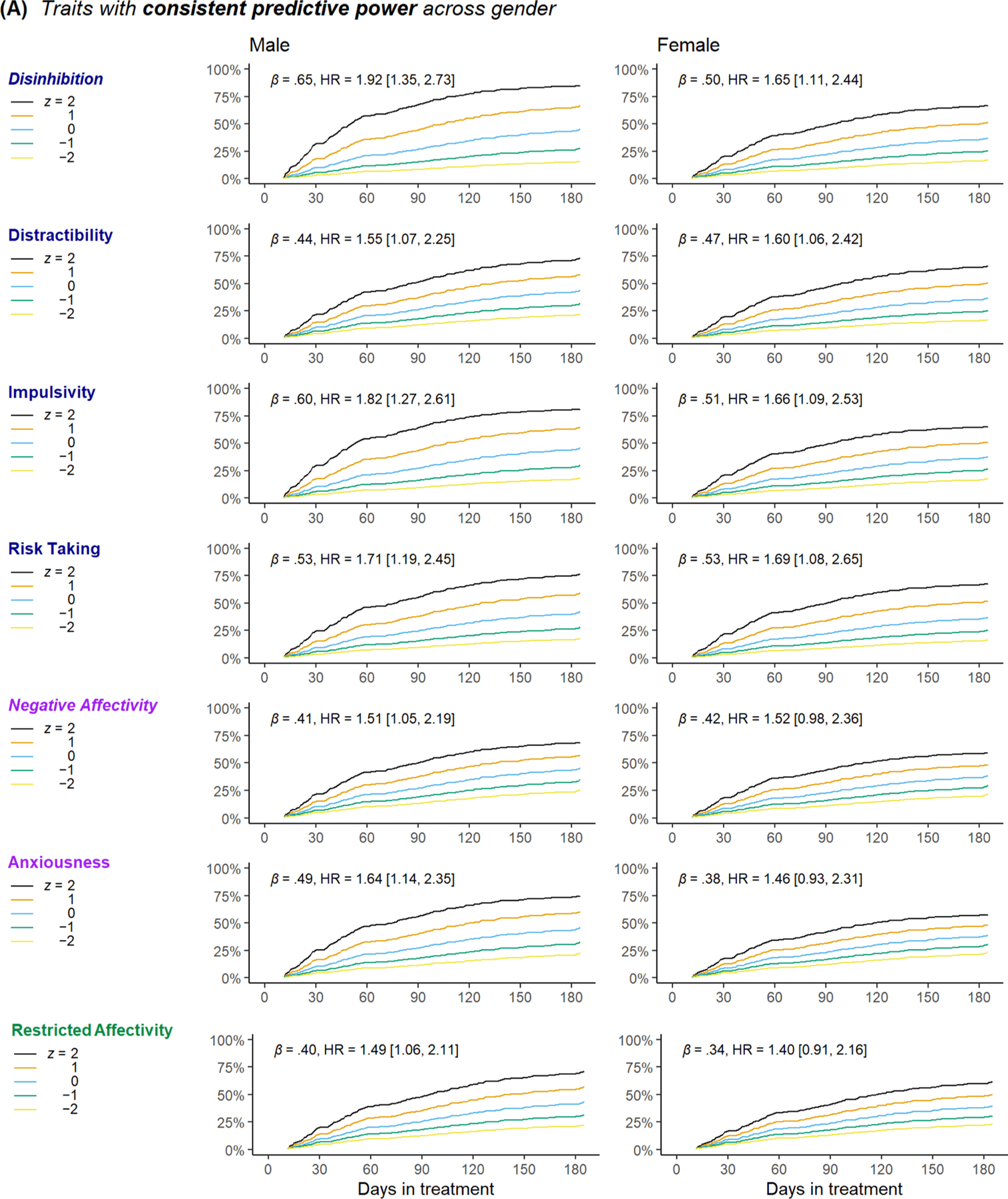
3.2.3. Age × trait interactions
In general, older participants were less likely to prematurely terminate (across models, , , mean 95 % CI bounds 0.66, 0.98), regardless of their standings on PID-5 traits. Fig. 2B shows a forest plot of hazard ratios for men aged 18, 30 and 45 for all PID-5 traits. Age had a general attenuating effect on PID-5–termination relationships (see Fig. 4A). For example, whereas Disinhibition strongly predicted faster treatment termination among age-18 men (β = .65, HR 1.92, 95 % CI 1.35, 2.73), this relationship was predicted to be much smaller among age-30 men (β = .35, HR = 1.42, 95 % CI 1.13, 1.79) and absent entirely among age-45 men (β = .02, HR = 0.98, 95 % CI 0.71, 1.34). Most other traits showed similar attenuation with age. The sole exception to this pattern was Submissiveness, which appeared to become more negatively related to termination among older participants—older participants who were higher on Submissiveness were predicted to be less likely to terminate early (for age-45 men, β = .48, HR = 0.62, 95 % CI 0.43, 0.88).
Fig. 4.
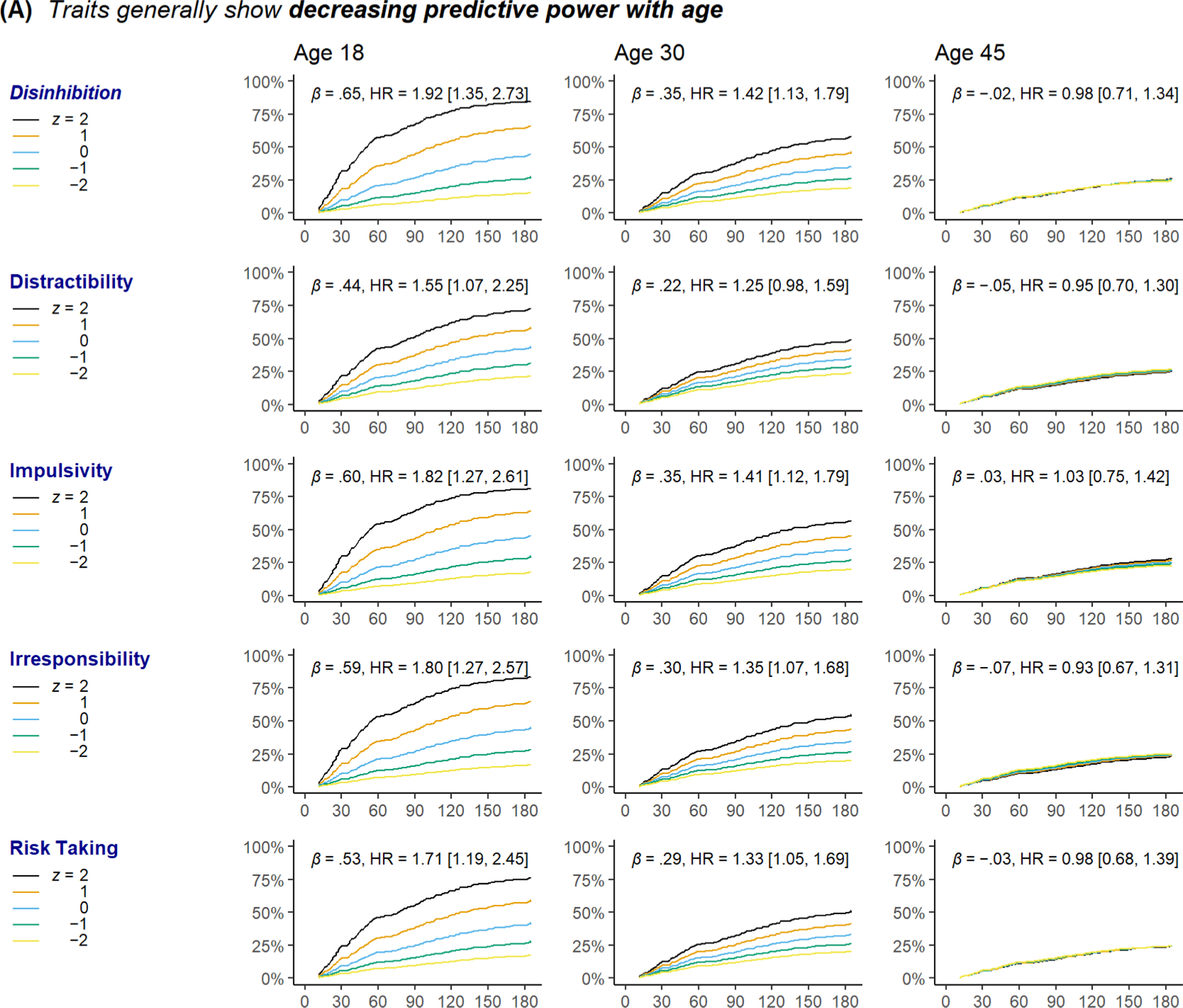
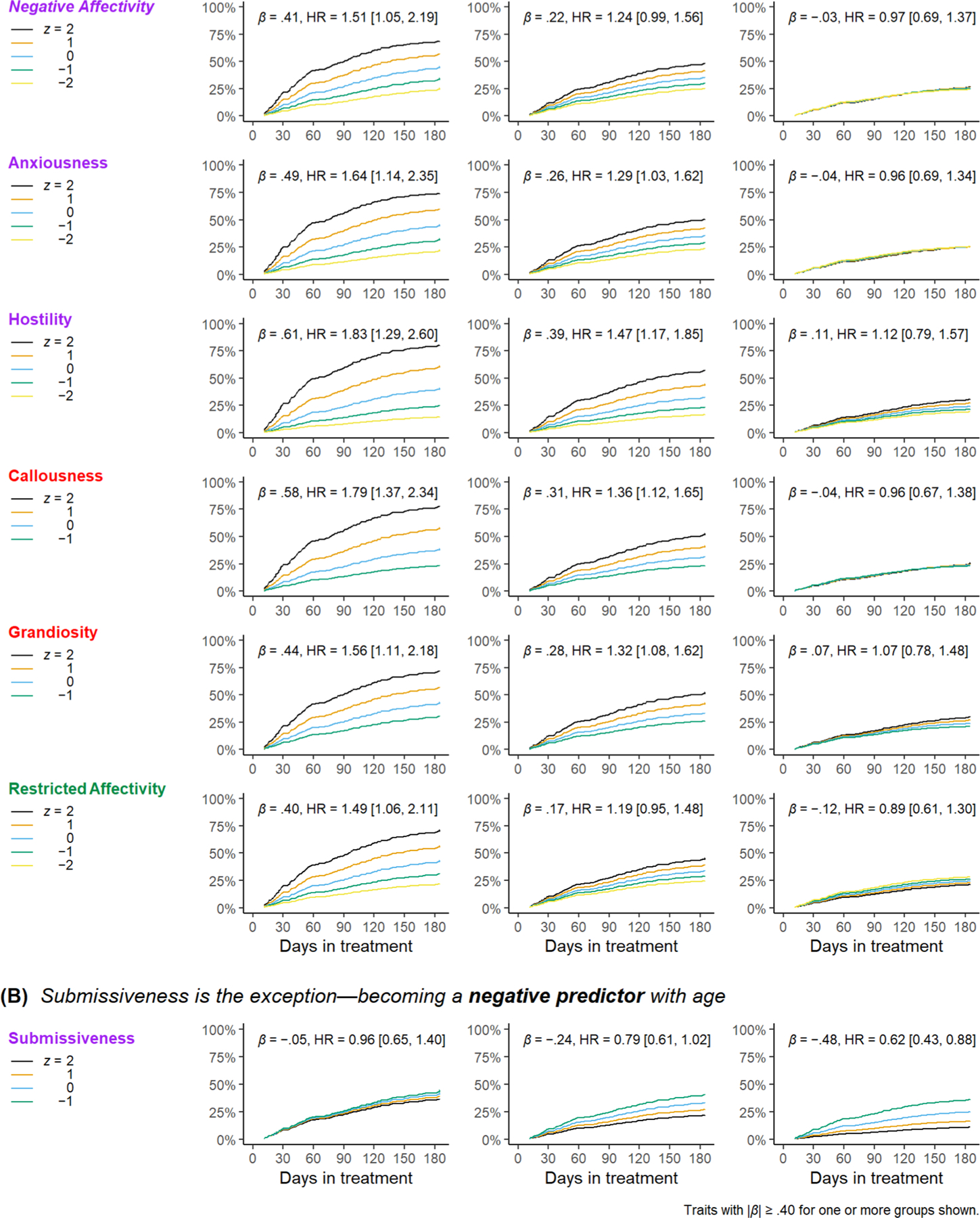
Trait interactions with age.
Predicted termination probability by number of days in treatment and PID-5 trait z-score.
3.2.4. Exploratory analyses
Because data were drawn from a randomized clinical trial, we also estimated models including trial condition and condition × trait interaction terms using the smaller subsample eligible for the trial. Results are shown in Table S7. The pattern of results for main effects and interactions in these models were similar to models not controlling for trial condition. No main effects of treatment condition were apparent, but the active Skills for Improving Distress Intolerance (SIDI) treatment had small positive interactions with Negative Affectivity, Emotional Lability, Anxiousness, and Distractibility for predicting treatment completion ( β ≈ .28, 95 % CI ± .25), relative to a Supportive Counseling condition. Thus, SIDI appeared to help participants with very elevated levels of traits related to emotional volatility, anxiety, and inattention to more quickly successfully complete treatment7.
4. Discussion
We investigated the utility of the DSM-5 alternative model of personality disorders (AMPD) as measured by the PID-5 to predict premature termination of residential addictions treatment. Notably, we examined whether these relationships varied across gender and age groups. To prevent detection of spurious interactions due to differential test functioning, we first examined measurement invariance of the PID-5 scales across gender and age and estimated survival models using scores free of differential functioning. Several notable findings emerged.
4.1. Prediction of premature treatment termination: personality pathology is a risk factor among younger male patients
Consistent with previous literature (Patkar et al., 2004; Petry and Bickel, 2000; Stevens et al., 2014), a host of traits primarily relating to disinhibition and negative emotionality predicted being more likely to prematurely terminate and to do so quicker. Such findings have both research and practice implications. For research, behavioral disinhibition and negative emotionality have long been implicated in both borderline and antisocial personality disorders—two personality disorders that predict treatment termination historically (Brorson et al., 2013). Accordingly, the current results support the construct validity of the AMPD and highlight the utility of dimensional approaches to measuring personality pathology. It should be noted, however, that our findings are not deterministic; that is, even at high levels of risk, not all patients will terminate treatment, and even if terminating, not necessarily doomed to life-persistent use (Kelly et al., 2017). More importantly, identification of risk factors highlights opportunities for clinical intervention. Specifically, our results suggest that community addiction clinicians should be trained in trait-targeted intervention techniques for patients with elevated emotion dysregulation, antagonism, and disinhibition (Roberts et al., 2017). Such approaches may include single-session motivational interviewing (Carroll et al., 2006), positive reinforcement-based treatments (Caldwell et al., 2007, 2006), and treatments aimed at enhancing emotion regulation and impulse control (Bornovalova et al., 2012; Conrod et al., 2010; Stasiewicz et al., 2013). Previous research suggests that a brief, lifestyle intervention for impulsivity effectively increased the likelihood of treatment completion (Thylstrup and Hesse, 2016). More broadly, our results indicate that the PID-5 - especially the disinhibition scales - can be used as a screening tool in community addictions treatment centers, as well as to explore broader mechanisms in addictions treatment outcomes (Díaz-Batanero et al., 2019; Wiernik et al., 2020)8.
Gender moderated several other traits’ relationships with treatment termination time. Several PID-5 traits that are often considered more male-typical (Grandiosity, Callousness, Hostility, Irresponsibility) were strongly related with rapid treatment termination among men, but only weakly or not at all (e.g., Grandiosity) among women. Conversely, a PID-5 trait often considered more female-typical (Submissiveness) was associated with treatment termination and termination time among women, but not men. Notably, PID-5 trait relationships with treatment termination were consistently attenuated by age. For age-45 participants, nearly all PID-5 relationships with treatment termination were null (a negative relationship with Submissiveness being the sole exception). Overall, it appears that maladaptive personality is a risk factor for premature treatment termination primarily among young patients, especially young men.
Finally, there were several interactions of trait and condition. Among patients with high levels of emotional volatility, anxiety, and inattention, participants receiving the distress intolerance skills training (SIDI) were more likely to complete treatment and to do so more quickly. These effects are consistent with SIDI’s theoretical framework, which integrates exposure therapy, dialectical behavior therapy, and acceptance and commitment therapy components. Such treatments have been shown to be beneficial among those with high anxiety and poor emotion regulation (Linehan et al., 2006; Vøllestad et al., 2012). As SIDI is a brief treatment specifically developed for use in residential addiction centers, embedding it in ongoing programs may enhance some positive treatment outcomes.
4.2. Measurement invariance: personality psychopathology assessments function well across age and gender groups
Although ≈12 % of items showed some evidence for differential item functioning by age and gender, the sizes of these effects were consistently small, and scale-level differential test functioning was negligible. These results are consistent with the few other studies that have examined PID-5 measurement invariance (Suzuki et al., 2019; Van den Broeck et al., 2013) and bode well for clinical use of unadjusted PID-5 scale scores to assess and monitor personality pathology across age and gender groups. Computerized scoring algorithms incorporating the small differences in item parameters across groups may be useful to minimize any potential differential test functioning effects.
4.3. Limitations and future directions
We identified several limitations that should be addressed in future research. First, due to limited power, we could not test for potential 3-way interactions (age × gender × trait) in the survival analyses or age gender interactions in the measurement invariance analyses, particularly as such effects are likely to be small in magnitude. Second, socioeconomic and ethnic/cultural differences may have some impact of findings, which should be investigated in future research. Finally, future work is needed to examine whether AMPD traits predict other substance-related treatment outcomes, such as time to relapse or time to incarceration.
4.4. Conclusion
This study is one of few to document the longitudinal criterion-related validity of a measure designed around the AMPD. It is also the first study to examine invariance of the PID-5 using a continuous age indicator and to provide effect size estimates for differential functioning across gender and age. Most importantly, it is only the third study to apply the PID-5 in a residential addiction treatment context and examine clinical utility to inform substance use treatment. Unlike other personality pathology inventories (e.g., Minnesota Multiphasic Personality Inventory), the PID-5 is non-proprietary and freely available. This makes it a valuable tool to provide accessible, open source, and valid clinical screening.
Supplementary Material
Acknowledgments
Role of funding source
The work was supported by DA032582National Institute on Drug Abuse (NIDA).
Footnotes
Submission declaration
The results in this article have never been presented, published, or shared on social networks.
Declaration of Competing Interest
The authors report no declarations of interest.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.drugalcdep.2021.109011.
To be eligible for the clinical trial, participants had to give informed consent, be between the ages of 18 and 65, evidence a DSM-IV substance dependence, receive at least one treatment session in the randomized clinical trial, and plan to reside within the 6-county (within ≈ 2.5-hour drive) catchment area of the residential treatment site for at least six months after completion of the residential treatment. Of the initial sample, 354 participants were eligible for the clinical trial. Detailed description of recruitment, consent, and RCT conditions as well as the CONSORT diagram and treatment manuals are available at https://osf.io/kysdt/ (DOI 10.17605/OSF.IO/QMXBV).
Further characterizations of the sample including psychopathology rates, diagnostic reliability, and differences between completers and noncompleters in the same are presented in the supplemental materials (https://osf.io/htc2v/).
Code for all models as well as an HTML document with all main and supplementary analyses are available at https://osf.io/htc2v/.
We investigated education and cannabis use, which showed > 10% difference between completers and terminators, as potential covariates in the survival models; both negligibly changed estimates of age, gender, trait, or interaction effects, and likelihood ratio tests indicated that these terms can be dropped without a loss in model fit.
We chose the age markers roughly based on the developmental literature: 18 was the lowest eligible age, and generally can be thought of as late adolescence or emerging adulthood; 30 can be thought of as mid-adulthood, and 45 was chosen as the upper marker as several studies have noted that personality disorders and maladaptive personality start ‘burning out’ (declining) around this age.
Whereas several PID-5 traits predicted premature termination and time to termination, PID-5 trait relationships with treatment completion and time to completion were generally negligible. An exception was Suspiciousness, which was somewhat positively related to both treatment completion (for men age-18, β = .39, HR = 1.48, 95% CI 1.13, 1.93) and termination (for men age-18, β = .38, HR = 1.47, 95% CI 1.03, 2.08) among age-18 men and women. Among age-18 women, Attention Seeking (β = .42, HR = 1.52, 95% CI 1.09, 2.11) and Separation Insecurity (β = .37, HR = 1.45, 95% CI 1.06, 1.98) were also somewhat to moderately positively related to completion.
We also examined whether PID-5 traits predicted dropout before 30 days in treatment (Nevents = 26 pre-30 day terminations; Table S8). PID-5 trait differences between this very-early termination group and others showed a similar pattern as comparisons of overall treatment completion versus termination groups, with generally larger effect sizes.
In a separate study, the median time to complete the disinhibition scales was 2 minutes and the maximum time was 4 minutes (Stephan Dilchert, personal communication, June 14, 2021).
References
- Al-Dajani N, Gralnick TM, Bagby RM, 2016. A psychometric review of the Personality Inventory for DSM–5 (PID–5): current status and future directions. J. Pers. Assess 98, 62–81.. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 2014. The Personality Inventory for DSM-5 (PID-5)—Adult Scoring Guidelines [WWW Document]. URL. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM5_The-Personality-Inventory-For-DSM-5-Full-Version-Adult.pdf.
- Anvari F, Lakens D, 2019. Using Anchor-Based Methods to Determine the Smallest Effect Size of Interest
- Argyriou E, Um M, Wu W, Cyders MA, 2020. Measurement invariance of the UPPS-P impulsive behavior scale across age and sex across the adult life span. Assessment 27, 432–453. [DOI] [PubMed] [Google Scholar]
- Basharpoor S, Heidari F, Narimani M, 2019. Personality deviance, distress tolerance, and readiness to change in treatment-seeking substance users. J. Subst. Use 25, 1–6. [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Hunt ED, Lejuez CW, 2012. Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug Alcohol Depend 122, 70–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, 2006. When does measurement invariance matter? Med. Care 44, S176–S181. [DOI] [PubMed] [Google Scholar]
- Brewer DD, Catalano RF, Haggerty K, Gainey RR, Fleming CB, 1998. A meta-analysis of predictors of continued drug use during and after treatment for opiate addiction. Addiction 93, 73–92. [PubMed] [Google Scholar]
- Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F, 2013. Drop-out from addiction treatment: a systematic review of risk factors. Clin. Psychol. Rev 33, 1010–1024. [DOI] [PubMed] [Google Scholar]
- Caldwell MF, Skeem J, Salekin R, Van Rybroek G, 2006. Treatment response of adolescent offenders with psychopathy features: a 2-year follow-up. Crim. Justice Behav 33, 571–596. [Google Scholar]
- Caldwell MF, McCormick DJ, Umstead D, Van Rybroek GJ, 2007. Evidence of treatment progress and therapeutic outcomes among adolescents with psychopathic features. Crim. Justice Behav 34, 573–587. [Google Scholar]
- Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, Kunkel LE, Mikulich-Gilbertson SK, Morgenstern J, Obert JL, Polcin D, Snead N, Woody GE, 2006. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: a multisite effectiveness study. Drug Alcohol Depend 81, 301–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrod PJ, Castellanos-Ryan N, Strang J, 2010. Brief, personality-targeted coping skills interventions and survival as a non–drug user over a 2-year period during adolescence. Arch. Gen. Psychiatry 67, 85–93. [DOI] [PubMed] [Google Scholar]
- Díaz-Batanero C, Ramírez-López J, Domínguez-Salas S, Fernández-Calderón F, Lozano ÓM, 2019. Personality Inventory for DSM-5–Short Form (PID-5-SF): reliability, factorial structure, and relationship with functional impairment in dual diagnosis patients. Assessment 26, 853–866. [DOI] [PubMed] [Google Scholar]
- Embretson SE, 1996. Item response theory models and spurious interaction effects in factorial ANOVA designs. Appl. Psychol. Meas 20, 201–212. [Google Scholar]
- Engels GI, Duijsens IJ, Haringsma R, van Putten CM, 2003. Personality disorders in the elderly compared to four younger age groups: a cross-sectional study of community residents and mental health patients. J. Pers. Disord 17, 447–459. [DOI] [PubMed] [Google Scholar]
- Few LR, Miller JD, Rothbaum AO, Meller S, Maples J, Terry DP, Collins B, MacKillop J, 2013. Examination of the Section III DSM-5 diagnostic system for personality disorders in an outpatient clinical sample. J. Abnorm. Psychol 122, 1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gignac GE, Szodorai ET, 2016. Effect size guidelines for individual differences researchers. Pers. Individ. Dif 102, 74–78. [Google Scholar]
- Goldberg LR, 1990. An alternative” description of personality”: the big-five factor structure. J. Pers. Soc. Psychol 59, 1216. [DOI] [PubMed] [Google Scholar]
- Hedges LV, Olkin I, 1980. Vote-counting methods in research synthesis. PB 88, 359–369. [Google Scholar]
- Hershberger AR, Um M, Cyders MA, 2017. The relationship between the UPPS-P impulsive personality traits and substance use psychotherapy outcomes: a meta-analysis. Drug Alcohol Depend 178, 408–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John OP, Naumann LP, Soto CJ, 2008. Paradigm shift to the integrative Big Five trait taxonomy: history, measurement, and conceptual issues. Handbook of Personality: Theory and Research, 3rd ed. The Guilford Press, New York, NY, US, pp. 114–158. [Google Scholar]
- Kelly JF, Bergman BG, Hoeppner BB, Vilsaint C, White WL, 2017. Prevalence and pathways of recovery from drug and alcohol problems in the United States population: implications for practice, research, and policy. Drug Alcohol Depend 181, 162–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kravitz HM, Fawcett J, McGuire M, Kravitz GS, Whitney M, 1999. Treatment attrition among alcohol-dependent men: is it related to novelty seeking personality traits? J. Clin. Psychopharmacol 19, 51–56. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Derringer J, Markon KE, Watson D, Skodol AE, 2012. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychol. Med 42, 1879–1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Korslund KE, Tutek DA, Reynolds SK, Lindenboim N, 2006. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch. Gen. Psychiatry 63, 757–766. [DOI] [PubMed] [Google Scholar]
- Loree AM, Lundahl LH, Ledgerwood DM, 2015. Impulsivity as a predictor of treatment outcome in substance use disorders: review and synthesis. Drug Alcohol Rev 34, 119–134. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT Jr, 1997. Personality trait structure as a human universal. Am. Psychol 52, 509. [DOI] [PubMed] [Google Scholar]
- Miller JD, Few LR, Lynam DR, MacKillop J, 2015. Pathological personality traits can capture DSM–IV personality disorder types. Personal. Disord. Theory Res. Treat 6, 32–40. [DOI] [PubMed] [Google Scholar]
- Moos RH, Pettit B, Gruber V, 1995. Longer episodes of community residential care reduce substance abuse patients’ readmission rates. J. Stud. Alcohol 56, 433–443. [DOI] [PubMed] [Google Scholar]
- Paris J, 2003. Personality disorders over time: precursors, course and outcome. J. Pers. Disord 17, 479–488. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Murray HW, Mannelli P, Gottheil E, Weinstein SP, Vergare MJ, 2004. Pre-treatment measures of impulsivity, aggression and sensation seeking are associated with treatment outcome for African-American cocaine-dependent patients. J. Addict. Dis 23, 109–122. [DOI] [PubMed] [Google Scholar]
- Petry NM, Bickel WK, 2000. Gender differences in hostility of opioid-dependent outpatients: role in early treatment termination. Drug Alcohol Depend 58, 27–33. [DOI] [PubMed] [Google Scholar]
- R Core Team, 2020. R: a Language and Environment for Statistical Computing R Foundation for Statistical Computing, Vienna, Austria. [Google Scholar]
- Roberts BW, Luo J, Briley DA, Chow PI, Su R, Hill PL, 2017. A systematic review of personality trait change through intervention. Psychol. Bull 143, 117. [DOI] [PubMed] [Google Scholar]
- SAMHSA, 2018. Key Substance Use and Mental Health Indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18–5068), NSDUH Series Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Samuel DB, LaPaglia DM, Maccarelli LM, Moore BA, Ball SA, 2011. Personality disorders and retention in a therapeutic community for substance dependence. Am. J. Addict 20, 555–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siqueland L, Crits-Christoph P, Gallop R, Barber JP, Griffin ML, Thase ME, Daley D, Frank A, Gastfriend DR, Blaine J, 2002. Retention in psychosocial treatment of cocaine dependence: predictors and impact on outcome. Am. J. Addict 11, 24–40. [DOI] [PubMed] [Google Scholar]
- South SC, Krueger RF, Knudsen GP, Ystrom E, Czajkowski N, Aggen SH, Neale MC, Gillespie NA, Kendler KS, Reichborn-Kjennerud T, 2017. A population based twin study of DSM–5 maladaptive personality domains. Personal. Disord. Theory Res. Treat 8, 366–375. [DOI] [PubMed] [Google Scholar]
- South SC, Jarnecke AM, Vize CE, 2018. Sex differences in the Big Five model personality traits: a behavior genetics exploration. J. Res. Pers 74, 158–165. [Google Scholar]
- Stark MJ, 1992. Dropping out of substance abuse treatment: a clinically oriented review. Clin. Psychol. Rev 12, 93–116. [Google Scholar]
- Stasiewicz PR, Bradizza CM, Schlauch RC, Coffey SF, Gulliver SB, Gudleski GD, Bole CW, 2013. Affect regulation training (ART) for alcohol use disorders: development of a novel intervention for negative affect drinkers. J. Subst. Abuse Treat 45, 433–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, Albert D, Cauffman E, Banich M, Graham S, Woolard J, 2008. Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: evidence for a dual systems model. Dev. Psychol 44, 1764–1778. [DOI] [PubMed] [Google Scholar]
- Stepp SD, Pilkonis PA, 2008. Age-related differences in individual DSM criteria for borderline personality disorder. J. Pers. Disord 22, 427–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens L, Verdejo-García A, Goudriaan AE, Roeyers H, Dom G, Vanderplasschen W, 2014. Impulsivity as a vulnerability factor for poor addiction treatment outcomes: a review of neurocognitive findings among individuals with substance use disorders. J. Subst. Abuse Treat 47, 58–72. [DOI] [PubMed] [Google Scholar]
- Stevens L, Goudriaan AE, Verdejo-Garcia A, Dom G, Roeyers H, Vanderplasschen W, 2015. Impulsive choice predicts short-term relapse in substance-dependent individuals attending an in-patient detoxification programme. Psychol. Med 45, 2083–2093. [DOI] [PubMed] [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ, Mann G, Duke D, Munson M, Adkins J,Grabill KM, Murphy TK, Goodman WK, 2007. Family-based cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: comparison of intensive and weekly approaches. J. Am. Acad. Child Adolesc. Psychiatry 46, 469–478. [DOI] [PubMed] [Google Scholar]
- Suzuki T, South SC, Samuel DB, Wright AG, Yalch MM, Hopwood CJ, Thomas KM, 2019. Measurement invariance of the DSM–5 Section III pathological personality trait model across sex. Personal. Disord. Theory Res. Treat 10, 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Therneau TM, 2020. Survival: a Package for Survival Analysis in R
- Therneau TM, Grambsch PM, 2000. Modeling Survival Data: Extending the Cox Model, Statistics for Biology and Health Springer, New York. [Google Scholar]
- Thylstrup B, Hesse M, 2016. Impulsive lifestyle counseling to prevent dropout from treatment for substance use disorders in people with antisocial personality disorder: a randomized study. Addict. Behav 57, 48–54. [DOI] [PubMed] [Google Scholar]
- Ullrich S, Coid J, 2009. The age distribution of self-reported personality disorder traits in a household population. J. Pers. Disord 23, 187–200. [DOI] [PubMed] [Google Scholar]
- Van den Broeck J, Bastiaansen L, Rossi G, Dierckx E, De Clercq B, 2013. Age-neutrality of the trait facets proposed for personality disorders in DSM-5: a DIFAS analysis of the PID-5. J. Psychopathol. Behav. Assess 35, 487–494. [Google Scholar]
- Vasilopoulos T, Morey TE, Dhatariya K, Rice MJ, 2016. Limitations of significance testing in clinical research: a review of multiple comparison corrections and effect size calculations with correlated measures. Anesth. Analg 122, 825–830. [DOI] [PubMed] [Google Scholar]
- Vøllestad J, Nielsen MB, Nielsen GH, 2012. Mindfulness-and acceptance-based interventions for anxiety disorders: a systematic review and meta-analysis. Br. J. Clin. Psychol 51, 239–260. [DOI] [PubMed] [Google Scholar]
- Wiernik BM, Kostal JW, Wilmot MP, Dilchert S, Ones DS, 2017. Empirical benchmarks for interpreting effect size variability in meta-analysis. IOP 10, 472–479. [Google Scholar]
- Wiernik BM, Rappaport L, Volgenau K, Stark S, Fatimah H, Neale M, Bornovalova M, 2020. Criterion-Related Validity and Longitudinal Functioning of the DSM-5 Alternative Model Pathological Personality Traits in a Clinical Sample
- Zanarini MC, Frankenburg FR, Reich DB, Silk KR, Hudson JI, McSweeney LB, 2007. The subsyndromal phenomenology of borderline personality disorder: a 10-year follow-up study. Am. J. Psychiatry 164, 929–935. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


