Abstract
Vitamin K2 serves an important role in cardiovascular health through regulation of calcium homeostasis. Its effects on the cardiovascular system are mediated through activation of the anti-calcific protein known as matrix Gla protein. In its inactive form, this protein is associated with various markers of cardiovascular disease including increased arterial stiffness, vascular and valvular calcification, insulin resistance and heart failure indices which ultimately increase cardiovascular mortality. Supplementation of vitamin K2 has been strongly associated with improved cardiovascular outcomes through its modification of systemic calcification and arterial stiffness. Although its direct effects on delaying the progression of vascular and valvular calcification is currently the subject of multiple randomised clinical trials, prior reports suggest potential improved survival among cardiac patients with vitamin K2 supplementation. Strengthened by its affordability and Food and Drug Adminstration (FDA)-proven safety, vitamin K2 supplementation is a viable and promising option to improve cardiovascular outcomes.
Keywords: coronary vessels, atherosclerosis, heart valve diseases, pharmacology, clinical, biomarkers
Key points.
There is an alarmingly high prevalence of vitamin K deficiency and suboptimal recommended intake among the general population in the USA.
A growing body of evidence supports the potential role of vitamin K2 in cardiovascular health.
Vitamin K2 helps regulate the homeostasis of soft tissue calcification through activation of an anti-calcific protein known as matrix Gla protein (MGP).
Studies demonstrate a strong association between vitamin K deficiency, as assessed by plasma inactive MGP, and arterial stiffness, vascular and valvular calcification, heart failure and cardiovascular mortality.
Increased vitamin K2 intake may reduce arterial stiffness, slow progression of vascular and valvular calcification, lower the incidence of diabetes and coronary artery disease, and decrease cardiovascular mortality.
Further efforts are necessary to establish vitamin K2 as a safe, cost-effective, and efficacious supplement for preventing and improving cardiovascular outcomes.
Introduction
Vitamin K is a fat-soluble vitamin that is comprised of multiple similarly structured compounds. Naturally, vitamin K occurs as two vitamers, namely vitamin K1 (phylloquinone) and vitamin K2 (menaquinones; MKs). Vitamin K2 specifically has been highlighted for its long half-life and extrahepatic activity. As such, vitamin K2 plays a pivotal role in the activation of extrahepatic γ-carboxyglutamate (Gla) proteins such as matrix Gla protein (MGP), a small 84-amino acid (14 kDa) protein that is commonly considered the strongest inhibitor of vascular calcification.1 Primarily synthesised by vascular smooth muscle cells (VSMCs), MGP undergoes two forms of post-translational modifications for complete maturation: γ-glutamate carboxylation and serine phosphorylation, the former of which is vitamin-K dependent.2 During states of vitamin K deficiency, MGP remains uncarboxylated and its biological function is impaired.1 There are several forms of MGP depending on the phosphorylation and carboxylation status. The circulating inactive unphosphorylated and uncarboxylated form of MGP (dp-ucMGP) is an established biomarker for vitamin K deficiency.3 4 The use of vitamin K antagonists (VKAs) such as warfarin can induce a deficiency in MGP, which may contribute to the formation and evolution of vascular calcification, an independent predictor of cardiovascular morbidity and mortality.5
In light of expanding preclinical and clinical data on the cardiovascular benefits of vitamin K2, with multiple ongoing clinical trials investigating its role in various outcomes, there is a pressing need to organise our understanding of the pathophysiology, safety, and efficacy of vitamin K2 intake as it relates to markers and outcomes of cardiovascular health. The aim of this comprehensive narrative review, divided into two major sections, is to summarise the literature for scientists and clinicians on: (1) the role of MGP in cardiovascular health, and (2) the cardiovascular benefits of vitamin K2 dietary intake and supplementation. We will first discuss the pathophysiological interplay between vitamin K2 and MGP. By providing an organised framework of the available evidence, we will then elucidate the association of vitamin K deficiency and MGP on the various markers of cardiovascular health. In the second section, this review will outline the clinical impact of dietary and supplemental vitamin K2 intake on these outcomes, citing the data of its use as a novel and practical addition to our arsenal of cardioprotective therapies.
Vitamin K-dependent proteins and cardiovascular health
Role of MGP in cardiovascular health
There is a growing body of evidence supporting the vital role of MGP in cardiovascular disease (CVD).6 This was first demonstrated in MGP knock-out mice who suffered premature death within 6–8 weeks after birth consequent to massive arterial calcification and spontaneous aortic rupture.7 A paradigm shift around vascular calcification has since emerged whereby the previous notion of a passive, degenerative, and irreversible process is presently understood as an actively regulated and tenably preventable or reversible mechanism.1
Figure 1 depicts the mechanism by which vitamin K2 regulates systemic calcification through activation of MGP in VSMCs and chondrocytes. After the transcription and translation of MGP into dp-ucMGP, it undergoes post-translational modification through two distinct processes: (1) kinase-mediated serine phosphorylation,1 and (2) γ‐carboxylation of glutamic acid residues mediated by γ‐carboxylase, which requires vitamin K as a cofactor.2 The latter process is akin to the activation of several other vitamin-K dependent proteins such as coagulation factors. The resultant active form of MGP, an 84‐amino acid (approximately 14 kDa) protein, is thought to protect against soft tissue calcification via several processes. Calcium apatite is the predominant form of calcium crystals that accumulate in blood vessel walls, and it is also commonly found in bone.1 Notably, the process of vascular calcification resembles bone formation as matrix vesicles bud from cells and form a nidus for calcification. In vivo studies have shown that in the absence of activated MGP, VSMCs differentiate into cells with properties of chondrocytes and osteoblasts, producing a matrix that favours calcium crystal deposition.8 MGP regulates calcification directly by inhibiting formation and solubilisation of calcium crystals and through alternative calcification inhibitors such as fetuin-A, as well as indirectly via modulating transcription factors that suppress differentiation of VSMC to an osteoblast-like phenotype.9 10 Moreover, research demonstrates that only the active, carboxylated form of MGP antagonises the action of pro-calcific proteins; for instance, it inhibits bone morphogenic protein-2 (BMP-2), a potent pro-osteoblastic protein heavily expressed in atherosclerotic lesions in states of inflammation and oxidative stress, which induces an osteogenic gene expression profile in VSMC.1 9 11
Figure 1.
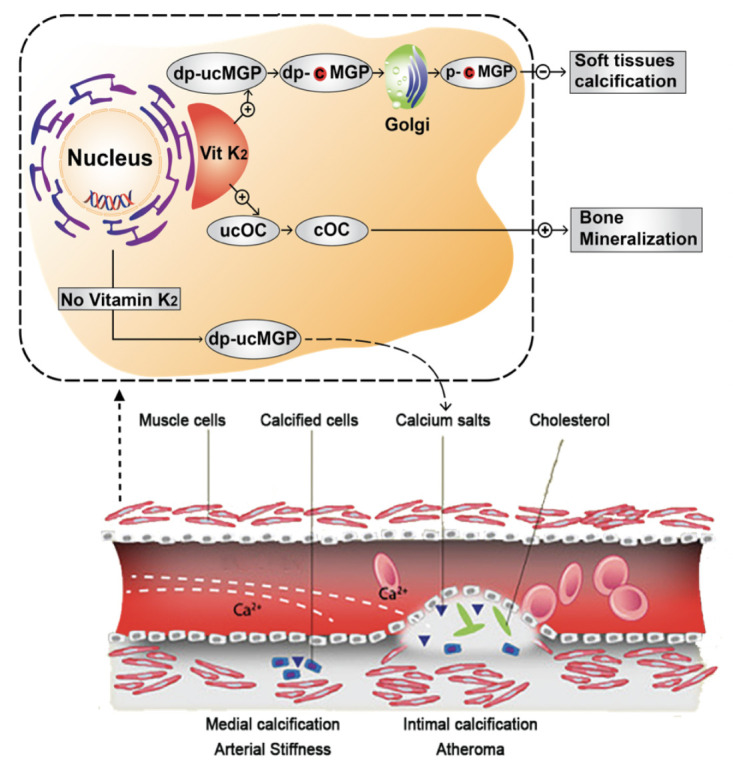
Mechanism of action of vitamin K2. Vitamin K2 is as a cofactor for gamma-carboxylation of dp-ucMGP into dp-cMGP in vascular smooth muscle cells and chondrocytes. dp-cMGP undergoes an additional phosphorylation by a casein kinase in Golgi bodies into p-cMGP, the final active form of MGP that ultimately inhibits soft tissue calcification. Inactive dp-ucMGP is a biomarker of poor vitamin K status in the circulation and is associated with increased deposition of calcium into blood vessels, predisposing to arterial stiffness via medial calcification and atherosclerosis via atheroma calcification. On the other hand, vitamin K-dependent carboxylation activates osteocalcin (OC), also known as bone Gla protein, and the latter not only promotes bone growth but also plays a role in preventing soft tissue calcification through inhibiting calcium and phosphate precipitation.118 dp-uc, dephospho-uncarboxylated; MGP, matrix Gla protein.
Role of other vitamin K-dependent proteins in cardiovascular health
It is important to note that there other vitamin K-dependent proteins implicated in cardiovascular health, including bone Gla protein (or osteocalcin (OC)) and Gas6 (growth arrest-specific 6) protein.12
The role of OC in cardiovascular health is manifested by modulation of vascular calcification through activation of adiponectin, a protein that has been shown to inhibit osteoblastic differentiation of VSMCs.13 Moreover, OC has been shown to reduce arterial stiffness in diabetic rat model.14 These findings have been replicated in human studies, as OC has been shown to be associated with adiponectin in patients with chronic kidney disease (CKD).15 A study by Fusaro et al found lower OC levels in patients with aortic and iliac calcifications as compared with patients without calcifications.16 Moreover, in a prospective study of 774 men aged 51–85 years from the MINOS cohort who had OC measured at baseline and were followed over 10 years with serial measurements of abdominal aortic calcification, higher baseline total OC was associated with a lower abdominal aortic calcification progression rate (OR=0.74 (0.57 to 0.97) per 10 ng/mL variation; p=0.029) and lower 10-year all-cause mortality (HR=0.62 (0.44 to 0.86) per 10 ng/mL variation; p=0.005).17 In light of the above studies, 1 meta-analysis of 46 studies showed no definitive association of OC with vascular calcification; it is important to mention, however, the considerable variability in adjustment for confounders, heterogeneity of the populations and assays used for measurement of serum OC in these studies.
Besides, Gas6 protein is a vitamin K-dependent protein that highly expressed in lungs, hearts and kidneys and has been shown to regulate calcification of VSMCs.18 19 It has also been shown that androgen receptor signalling inhibits vascular calcification through enhanced Gas6 transcription.20 Similar findings have been shown with adiponectin and its effect on vascular calcification through alterations in Gas6 expression.21 Alternatively, Gas6 is also known to protect against endothelial dysfunction and VSMC apoptosis, both of which are mechanisms that mediate vascular calcification.18 22 Moreover, in vitro data revealed that phosphate-induced calcification of VSMC is associated with a downregulation of Gas6 expression.18
Measurement of vitamin K2 levels
In order to investigate the role of vitamin K2 on cardiovascular health, a biomarker reflecting vitamin K status is required. This has been achieved by assessing the status of vitamin K-dependent proteins that require carboxylation, and assays measuring MGP seem to be the most commonly used ones,5 23 24 a measurement that reflects the bioactivity of vitamin K over a span of weeks to months.2 25 The assay that quantifies vitamin K deficiency is that which measures dp-ucMGP.5 With the introduction and growing adoption of automated commercial measurements, most notably through the popular, extensively validated kits by ImmunoDiagnostic Systems (IDS, Boldon, UK), which cost $25 per sample, dp-ucMGP now serves as an accessible and feasible marker for routine laboratory assessment in clinical practice.
The following sections will discuss in detail the relationship of vitamin K status with various markers of cardiovascular health.
Arterial stiffness
Plasma dp-ucMGP has consistently shown an association with measures of central haemodynamics and arterial function including arterial stiffness, a surrogate marker of cardiovascular morbidity and mortality. Specifically, high dp-ucMGP is associated with higher aortic stiffness as assessed by carotid–femoral pulse wave velocity (PWV),26–29 central pressure28 and augmentation index25 in varying patient populations internationally. A recent study by Ikari et al found that after 3 months of replacing warfarin with rivaroxaban, vitamin K deficiency, assessed by inactive forms of prothrombin and OC, was significantly reduced (100% to 2% for inactive prothrombin and 82% to 55% in inactive OC; p<0.05 for both). This was associated with a significant reduction in arterial stiffness via brachial–ankle PWV.30 The role of active MGP seems to extend beyond protection from calcification and is implicated in reduced elastin degradation and collagen formation in the arterial wall, both of which can potentially improve arterial stiffness.31
Coronary and vascular calcification
It is well established that MGP inhibits vascular calcification. This was first reported in human Keutel syndrome, which is characterised by systemic vascular calcification due to loss-of-function mutations in the MGP gene.32 Studies have shown that MGP inhibition of ‘pro-osteoblastic’ transcription factor BMP-2 relies on carboxylation.9 Moreover, warfarin, a VKA, has been shown to accelerate coronary, aortic valvular and mitral annular calcification (MAC).33 34 Genetic studies have also linked polymorphism in the gene encoding MGP with vascular calcification and coronary artery disease (CAD).35 36 The relationship between low vitamin K status and systemic calcification in humans has been described in several studies done on several patient populations. Dalmeijer et al found a greater trend of coronary artery calcification (CAC) in postmenopausal women with higher plasma dp-ucMGP,37 and Liabeuf et al showed a significant association between dp-ucMGP and peripheral arterial calcification score.38 More recently, there are data to suggest that dp-ucMGP may be associated with higher plaque stability; in a study on 100 patients undergoing carotid endarterectomy and histological evaluation of the carotid plaque, elevated dp-ucMGP was associated with less plaque haemorrhage, suggesting more plaque stability.39
Valvular calcification
Aortic stenosis (AS) is commonly described as a degenerative disease characterised by progressive aortic valve calcification with no effective medical therapy to delay its progression available to date. Retrospective work has linked warfarin use to increased aortic and mitral valve calcification in humans,34 and observational data suggest that warfarin is significantly associated with structural and haemodynamic progression of AS.40 Besides, a multicentre observation study on patients with CKD stages 3b–4 and non-valvular atrial fibrillation receiving either warfarin (n=100) or rivaroxaban (n=247) was conducted between 2015 and 2017 to assess their differential impact on valvular calcification measured by echocardiography.41 The study showed that rivaroxaban reduced both mitral and aortic calcification compared with warfarin (p<0.001) irrespective of baseline calcification and confounding factors.
Both MAC and AS are associated with cardiovascular morbidity and mortality as well as with calcium deposition in the aorta and various arterial beds, which may be localised sequelae of a systemic disease of dysregulated calcium metabolism.42 Previously described as passive degeneration, progression of valvular calcification has recently been identified as an active, potentially modifiable process. A cross-sectional study of 839 community patients with stable CAD found a strong association between serum inactive total MGP and MAC in those without diabetes, irrespective of age, renal function, albumin, C reactive protein (CRP) and traditional CVD risk factors. This association persisted after adjusting for calcium, phosphorus and fetuin-A levels.43 Moreover, polymorphism in MGP gene has been implicated in progression of aortic calcification in a randomly selected general population of 296 individuals who participated in the European Vertebral Osteoporosis Study.44
Measuring inactive forms of MGP, reflecting vitamin K deficiency, may ultimately prove useful in identifying individuals at increased risk of cardiac valve disease progression, and by extension, persons at greater risk of heart failure (HF) and CVD events. Elucidating the mechanisms behind valvular calcification may therefore offer novel insights into CVD.
Microvascular function
The benefits of MGP may also extend to microcirculation of various tissues. MGP is abundantly expressed in tissues of the retina,45 kidneys46 and the heart,47 and is postulated to contribute to microvascular integrity of these organs through anti-calcific and anti-stiffness properties. In a community study done on 935 randomly recruited Flemish participants (mean age, 40.9 years; 50.3% women) and followed over a median of 11 years, higher dp-ucMGP was associated with a decrease of retinal arteriolar diameter,48 which is a prognostic marker of cardiovascular outcomes.49
Chronic kidney disease
Markers of vitamin K deficiency have been shown to be associated with indices of adiposity and inflammation as well as diabetes and kidney function.12 50 In one randomised clinical trial, poor vitamin K status as deduced from low plasma levels of carboxylated OC (cOC) was associated with a higher fat mass at different body sites and with waist circumference, while high vitamin K levels as deduced from high cOC levels were inversely associated with high-sensitivity CRP, leptin and insulin.51
Vitamin K deficiency, whether measured through phylloquinone (via uOC assay) or MKs (via dp-ucMGP assays), is very prevalent in patients with CKD with more than 60% having some form of vitamin K deficiency.12 Specifically, functional vitamin K deficiency is also prevalent among haemodialysis and renal transplant recipients52 and may, in part, account for their reduced vitamin K function and increased subsequent risk of vascular calcification.52 53 Despite improvement in vitamin K levels following kidney transplantation, vitamin K deficiency as assessed by dp-ucMGP in kidney transplant patients was associated with significantly increased risk in all-cause mortality (HR=3.10; 95% CI: 1.87 to 5.12) among 518 patients with renal transplant followed over a median follow-up of 9.8 years.54
In regard to renal function, circulating inactive dp-ucMGP was associated with progression to renal dysfunction, as assessed by reduction in glomerular filtration rate (GFR) and presence of microalbuminuria, in a study on 1009 Flemish subjects who were followed for a median of 8.9 years.55 To substantiate these findings, the same investigators studied the histological findings of kidney biopsies from two healthy kidney donors and four patients with renal dysfunction.56 They found that tissues from diseased kidneys but not from healthy kidneys stained positive for calcium deposits and both carboxylated and uncarboxylated MGP, suggesting a potential role of MGP in renal tissue calcification beyond just vascular calcification. Another cross-sectional analyses of 1166 white Flemish and 352 black South Africans supported these findings as higher dp-ucMGP was associated with lower estimated GFR (p≤0.023), and subsequent greater risk of developing more advanced CKD.57
Besides, patients with end-stage renal disease requiring haemodialysis are severely vitamin K deficient as evidenced by higher total MGP.3 One analysis from the VItamin K Italian (VIKI) dialysis study including 387 patients on haemodialysis shows that vitamin K2 deficiency, measured by MK-4 and MK-7 serum levels, is significantly associated with aortic and iliac arterial calcification (OR=2.82 and 1.61, respectively; p<0.05).58 Another study of 842 patients with stable coronary disease in the community setting demonstrated a direct association between GFR and serum levels of inactive, ucMGP after adjusting for confounders.59 Further, MGP has been correlated with serum creatinine in those with HF and CKD.60 61 In a separate study by Kurnatowska et al that investigated 38 non-dialysed Caucasian non-smokers aged 18–70 years with CKD stages 4–5 who were supplemented with vitamin K2, plasma dp-ucMGP was positively associated with proteinuria, serum creatinine, parathyroid hormone (PTH) and fibroblast growth factor 23 (FGF-23), and inversely associated with GFR.61
Cardiac microcirculation
From the perspective of cardiac microcirculation, Paulus and Tschöpe proposed a novel theory surrounding left ventricular (LV) diastolic dysfunction that shifted emphasis from LV afterload to inflammation of the coronary microcirculation,62 ultimately implicating MGP in the disease process. In one study of over 900 Flemish and Swiss patients, dp-ucMGP correlated with diastolic dysfunction as assessed by increased LV filling pressures and higher E/e’ ratio.47 In this study, cardiac biopsies of ischaemic or dilated cardiomyopathy and healthy hearts (n=4 for each) were stained with conformation-specific MGP antibodies. The authors found a higher prevalence of uncarboxylated inactive, dp-ucMGP in the perivascular matrix and interstitium of diseased relative to normal hearts (p≤0.004), concluding that activated MGP is an ubiquitous, locally acting molecule that protects the microcirculation and perivascular matrix from injury caused by calcium deposition by sequestering intracellular calcium, thereby preserving LV diastolic function.
HF measures and mortality
Patients with symptomatic AS frequently develop LV outflow obstruction and LV hypertrophy as a compensatory mechanism to maintain the ejection performance. In light of the dramatic increase in mortality rate after symptom onset, aortic valve replacement is recommended in symptomatic patients with AS.
It is well founded that circulating dp‐ucMGP levels play a role in both systolic and diastolic cardiac function and their associated effects on mortality. In two Norwegian studies, significant associations were found between higher plasma dp-ucMGP and unfavourable echocardiographic measures and mortality among patients with severe AS and chronic heart (HF).60 63 Among 147 patients with symptomatic AS, dp‐ucMGP was significantly higher in diseased patients compared with healthy sex-matched and age-matched controls. Moreover, levels of dp-ucMGP were significantly correlated with neurohormonal (N-terminal pro-brain natriuretic peptide (NT‐proBNP)) and haemodynamic markers (LV ejection fraction and cardiac index) of HF severity in non-warfarin users, and with NT‐proBNP in warfarin users. Importantly, higher dp‐ucMGP concentration correlated with all‐cause mortality (HR ~7) after a mean follow‐up of 23 months,63 suggesting that a dysregulated MGP system may play a role in the development of LV hypertrophy and HF mortality in these patients. Moreover in this study, the risk of mortality was highest in patients who underwent aortic valve replacement. This confers a tenable role for dp‐ucMGP not only in untreated patients with symptomatic AS, but additionally as a pre‐procedural marker for long‐term risk evaluation in patients who undergo aortic valve replacement. The second study found that among 179 patients with chronic systolic and diastolic HF, increased dp-ucMGP was associated with greater disease severity compared with healthy age-matched and sex-matched controls. Elevated dp-ucMGP further correlated with increased CRP, NT-proBNP, systolic (LV ejection fraction) and diastolic dysfunction, and ischaemia as the aetiology for HF.60 After a mean 2.9 years, patients in the highest tertial of dp-ucMGP level had increased all-cause mortality, and dp-ucMGP was markedly higher in those who died due to HF progression.
From a pathophysiological perspective, the MGP system may serve both direct and indirect roles in the cellular processes associated with myocardial remodelling and the development and progression of HF. The absence of myocardial calcification in MGP-deficient mice7 implies possible interplay between MGP and cardiac haemodynamics unrelated to inhibition of calcification. Elevated MGP levels are seen during rapid myocardial response to pressure overload, potentially induced by angiotensin II, suggesting a relationship between neurohormonal maladaptive responses and MGP.64–66 Prior DNA microarray animal and human studies have demonstrated increased mRNA expression of MGP in the LV during acute and chronic pressure overload64 67 and in experimental HF in rats and mice.65 68 Moreover, studies have demonstrated that MGP anchors to the extracellular matrix by binding to vitronectin, which may have modifying effects on members of the transforming growth factor β family that influence cardiac remodelling during HF.69 Most recently, Mustonen et al66 showed that following a myocardial infarction, MGP is rapidly upregulated in response to cardiac overload long before the development of LV hypertrophy and remodelling. While the precise mechanism remains unclear, there is increasing plausibility that plasma dp‐ucMGP and valvular calcification are vital in cardiac dysfunction among patients with AS.
Cardiovascular morbidity and mortality
Accumulating evidence highlights a relationship between a low state of circulating vitamin K, signified by elevated dp-ucMGP, and the development and progression of CVD and mortality.24 Studies from Norway and Czech Republic demonstrate a strong association between higher plasma dp-ucMGP and risk of all-cause mortality.60 63 70 Notably, two Mendelian randomisation studies found that lower genetically predicted dp-ucMGP was causally associated with cardiovascular risk4 and mortality.71
A prospective study over a mean 5.6 years in an elderly population found that high plasma dp-ucMGP concentrations correlated with an increased risk of incident CVD, defined as one or more of coronary heart disease, peripheral arterial disease and CAD, independent of traditional cardiac risk factors and vitamin D status.72 Another investigation showed that elevated dp-ucMGP was associated with an increased hazard of incident CVD (CAD, peripheral artery disease, HF and stroke) after a median follow-up of 11.2 years among 518 patients with type 2 diabetes.73 Additionally, Mayer et al found that among 799 patients with past myocardial infarction, coronary revascularisation, or first ischaemic stroke, increased plasma dp-ucMGP conferred an elevated risk of both all-cause and cardiovascular mortality at 5 years, despite adjusting for potential confounders.70 In a subsequent subcohort analysis of patients with HF within this population, high dp-ucMGP was associated with 5-year all-cause mortality, with the largest HR found among those with elevated BNP (>100 ng/L).74 More recently, the role of dp-ucMGP on cardiovascular outcomes was studied in 894 patients with ischaemic heart disease (at least 6 months after they had myocardial infarction and/or coronary revascularisation); high dp-ucMGP was significantly associated with 2.4 and 3.5 higher risk of 5-year all-cause and cardiovascular mortality, respectively.75
These studies stand in contrast with a prospective case–cohort investigation from the European Prospective Investigation Into Cancer and Nutrition–Netherlands (EPIC-NL) Study which failed to reveal an association between high dp-ucMGP and increased CVD or stroke after a mean 11.5 years.73 Similarly, in the Health ABC Study where plasma vitamin K1 (phylloquinone) and dp-ucMGP were measured in 1061 participants free of CVD (aged 70–79 years) who are followed for over 12 years, the authors did not show an association with either markers of vitamin K and incident CVD; however, in a subset of subjects with treated hypertension, low plasma phylloquinone was associated with higher CVD risk overall (HR= 2.94; 95% CI: 1.41 to 6.13).76 Notwithstanding, a recent meta-analysis aimed in assessing the prospective association between vitamin K2 and CVD and all-cause mortality importantly identified a relationship between elevated plasma dp-ucMGP and all-cause mortality (pooled HR=1.84, 95% CI: 1.48 to 2.28; five studies) and cardiovascular mortality (pooled HR=1.96, 95% CI: 1.47 to 2.61; two studies).6
It remains evident that vitamin K deficiency is strongly associated with several markers of cardiovascular health, and plasma MGP represents a clinically feasible and sensitive tool to assess for such deficiency. Moreover, measuring inactive MGP is a powerful biomarker that can be incorporated in clinical and translational research, particularly for investigating calcification, HF and arterial stiffness. Whether intake of vitamin K2 through supplementation or diet has the potential to reduce the risk of such cardiovascular outcomes will be further discussed in the next sections.
Vitamin K2 and cardiovascular health
The literature surrounding vitamin K2 dates to its discovery in the 1930s and identification of its molecular mechanisms in the 1970s,77 and continues to grow after the recent discovery of the role of active MGP on vitamin K-dependent vascular calcification. Notwithstanding the breadth of research, an organised and succinct understanding of its cardiovascular role remains limited. The following sections provide a comprehensive but concise overview of the evidence related to the cardiovascular benefits of vitamin K2 intake through diet and supplementation.
Dietary intake
Vitamin K is a fat-soluble vitamin found in two forms: (1) phylloquinones (vitamin K1), present in leafy green vegetables and responsible for mediating coagulation, and (2) MKs (vitamin K2), present in fermented food and implicated in systemic calcification.78 Its pattern of bodily distribution appears tissue specific.79 While vitamin K1 concentrates in the liver where it regulates the production of coagulation factors, vitamin K2 is found in extrahepatic tissues such as bones and arteries.79 Long-chain MKs (ie, MK-7) are transported more efficiently to extrahepatic tissues.78 80
Intake of vitamin K2 through diet alone is seemingly inadequate for complete activation of MGP in humans.81 MK-7 is in relatively low abundance in Western diets as it is commonly found in a variety of fermented foods such as natto and, to a much lesser extent, meats and dairy products.78 82 Among a subcohort of 4275 subjects from the Prevention of Renal and Vascular End-stage Disease (PREVEND) Study, 31% had functional vitamin K insufficiency (ie, dp-ucMGP >500 pmol/L).83 Children and those over 40 years of age are mostly vitamin K deficient as measured by dp-ucMGP.84 Human studies have shown that high vitamin K2 intake is associated with reduced coronary artery calcification and CVD risk, and those effects are thought to be mediated by increased activation of MGP.85–87 For example, intake of natto, which is a vitamin K2-rich food common in the Japanese population, has been shown to be associated with lower hazard of CVD mortality (HR=0.75, p trend=0.0004) in a large Japanese cohort study of 13 355 men and 15 724 women, followed over 16 years.88
Oral supplementation
The effective recommended dose of longer chain MKs (MK-7, MK-8 and MK-9) for cardiovascular health benefits is 180–360 µg/day.89 90 Epidemiological evidence suggests that intake of vitamin K1 and K2 reduces cardiovascular and overall mortality.91 A substantial portion of ingested vitamin K1 is converted into K2, which in turn accumulates within the extrahepatic tissues. Studies of vitamin K1 supplementation used markedly higher doses (1–2 mg/day) than vitamin K2, especially MK-7 (180–360 μ/day), most likely due to the predominant extrahepatic activity and vascular tissue specificity of vitamin K2 relative to K1. Both isotypes are potentially comparable in their overall health effects, yet the higher vascular-specific activity of vitamin K2 may make it increasingly appealing as an efficacious option for utilisation in cardiovascular outcomes studies. Supplementing vitamin K2 is also promising in its ability to replete plasma stores of vitamin K2 and ultimately sustain an optimal level for inhibiting calcification. Supplementation has previously been associated with a dose-dependent reduction in circulating dp-ucMGP,82 92 and an ensuing improvement in arterial stiffness among healthy adults and those with end-stage renal disease requiring haemodialysis.26 81 In a supplementary analysis, MK-7 was well tolerated in failing to cause a hypercoagulable state.89 There have been no documented cases of toxicity of vitamin K1, MK-4 or MK-7. Additionally, the WHO has set no upper tolerance level for vitamin K intake.93
Cardiovascular risk factors
The following sections will discuss the influence of vitamin K, specifically focusing on vitamin K2, on various cardiovascular risk factors, including arterial stiffness, endothelial dysfunction, cardiac output, diabetes mellitus, valvular and vascular calcification, and cardiovascular mortality (figure 2). All the published studies in those fields are presented in table 1.
Figure 2.
Role of vitamin K2 on various measures of cardiovascular health. Based on a myriad of preclinical, epidemiological and interventional studies, vitamin K2 has been shown to have strong potential in reducing several surrogate measures of cardiovascular morbidity and mortality, including arterial stiffness, valvular calcification, arterial calcification, cardiac systolic and diastolic functions. In light of such evidence, vitamin K2 has been strongly associated with improved cardiovascular health by improving arterial, endothelial and myocardial function and with potential for improved overall survival.
Table 1.
Role of vitamin K on markers of CVD
| Study | Sample size | Patient population | Study methods | Study findings |
| Arterial stiffness | ||||
| Braam et al94 | 181 | Healthy postmenopausal Caucasians between 50 and 60 years of age Sex: female only Age: 55 |
Design: double-blind RCT Intervention: vitamin D3 (8 µg) +K1 (1 mg) supplementation Follow-up (years): 3 |
Distensibility (+8.8%, p<0.05) Compliance (+8.6%, p<0.05) Pulse pressure (−6.3%, p<0.05) CCA elasticity (−13.2%, p<0.01) |
| Knapen et al90 | 244 | Healthy, postmenopausal subjects aged 55–65 years Sex: female only Age: 60 |
Design: double-blind RCT Intervention: vitamin K2 (MK-7) supplementation (180 µg) Follow-up (years): 3 |
Carotid–femoral PWV Stiffness Index β (p<0.02) |
| Ikari et al96 | 26 | Patients with coronary calcification and at least 1 coronary risk factor Sex: 65% female Age: 69 |
Design: open-label, single arm Intervention: vitamin K2 (MK-4) supplementation (45 mg) Follow-up (years): 1 |
Brachial–ankle PWV by 18% only in patients with vitamin K2 deficiency (p=0.03) |
| Mansour et al27 | 60 | Adult renal transplant recipients with functioning graft for ≥3 months Sex: 43% female Age: 50 |
Design: prospective, single-centre, single-arm trial Intervention: vitamin K2 (MK-7) supplementation (360 µg) Follow-up (weeks): 8 |
Mean carotid–femoral PWV by 14.2% (p<0.001) |
| Vermeer and Hogne95 | 243 | Healthy adults without a history of cardiovascular disease Sex: 54% Age: 61 |
Design: double-blind, placebo-controlled RCT Intervention: vitamin K2 (MK-7) supplementation (180 µg) Follow-up (years): 1 |
Mean carotid–femoral PWV in placebo group (p<0.005) but no significant change in MK-7 group |
| Cardiac output | ||||
| McFarlin et al101 | 26 | Aerobically trained athletes with normal body composition Sex: 31% male Age: 21 |
Design: double-blind RCT Intervention: vitamin K2 supplementation (300 mg for 4 weeks, then 150 mg for 4 weeks) Follow-up (weeks): 8 |
Maximal cardiac output by 12% (p=0.03) |
| Metabolic syndrome | ||||
| Beulens et al102 | 38 094 | Dutch subjects without diabetes aged 20–70 years from the Prospect-EPIC and MORGEN-EPIC cohorts (1993–1997) Sex: 26% male Age: 49 |
Design: prospective, population-based cohort study Intervention: dietary vitamin K1 and K2 intake using FFQ Follow-up (years): 10 |
Risk of incident type 2 diabetes with 10 µg increment increase in dietary vitamin K2 intake (HR=0.93, p=0.04) |
| Choi et al103 | 42 | Healthy young volunteers Sex: Male only Age (median): 29 |
Design: Placebo-controlled trial Intervention: vitamin K2 supplementation (30 mg) Follow-up (weeks): 4 |
Insulin sensitivity index (p=0.01) Disposition index (p<0.01) cOC (p=0.01) |
| Asemi et al119 | 66 | Overweight patients with diabetes with CHD, aged 40–85 years, living in Iran Sex: 47% female Age: 65 |
Design: Double-blind RCT Intervention: vitamin D (5 µg) +K (90 µg)+calcium (500 mg) supplementation Follow-up (weeks): 12 |
Maximum carotid intima media thickness (p=0.02) HOMA-IR (p=0.01) HOMA-B (p=0.01) QUICKI (p=0.01) |
| Knapen et al51 | 214 | Healthy, postmenopausal women Sex: female only Age: 55–65 |
Design: randomised, placebo-controlled trial Intervention: vitamin K2 (MK-7) 180 µg/day or placebo Follow-up (years): 3 |
Only in good responders ( cOC): Total and HMW adiponectin Abdominal fat mass (waist circumference and VAT) |
| Vascular calcification | ||||
| Beulens et al85 | 564 | Healthy Dutch subjects aged 49–70 years not on HRT or contraceptives, sampled (2002–2004) from the PROSPECT-EPIC Study Sex: female only Age: 67 |
Design: population-based, cross-sectional study Intervention: vitamin K1 and K2 (MK-4–MK-10) intake using FFQ Follow-up: |
Coronary calcification with MK intake only (RR=0.80 (0.65 to 0.98), p trend=0.03) |
| Shea et al86 | 388 | Asymptomatic, ambulatory community-dwelling subjects aged 60–80 years Sex: 60% female Age: 68 |
Design: double-blind RCT Intervention: vitamin K1 supplementation (500 µg) Follow-up (years): 3 |
CAC progression in those >85% adherent to supplementation (p=0.03) |
| Fusaro et al58 | 387 | Patients on haemodialysis for ≥1 year Sex: 37% female Age: 64 |
Design: prospective observational study Comparison groups: patients with or without vitamin K1 or vitamin K2 (MK-4, MK-5 or MK-7) deficiency Follow-up (years): 3 |
Risk of abdominal aortic calcification with MK-4 deficiency (OR=2.8, p=0.026) Risk of iliac calcification with MK-7 deficiency (OR=1.6, p=0.042) |
| Kurnatowska et al120 | 42 | Non-smoking, non-dialysed Caucasians with CKD stages 3–5, stable renal function for ≥6 months and CAC ≥10 AU Sex: 48% female Age: 58 |
Design: double-blind RCT Intervention: vitamins K2 (MK-7, 90 µg)+D3 (10 µg) vs D3 (10 µg) Follow-up (months): 9 |
Change in CCA intima-media thickness in vitamin K2 +D group (0.06±0.08 vs 0.14±0.05 mm, p=0.005) Nonsignificant decrease in ΔCAC score in K2 +D group (p=0.7) |
| Ikari et al96 | 26 | Patients with coronary calcification and at least 1 coronary risk factor Sex: 65% female Age: 69 |
Design: open-label, single arm Intervention: vitamin K2 (MK-4) supplementation (45 mg) Follow-up (years): 1 |
CAC score by 14% (p=0.02) |
| Zwakenberg et al110 | 68 | Subjects aged >40 years with CVD, type 2 diabetes, and eGFR >30 Sex: 24% female Age: 69 |
Design: double-blind RCT Intervention: vitamin K2 (MK-7) supplementation (360 µg) Follow-up (months): 6 |
No change in femoral arterial calcification on18F-NaF PET scan (p=0.06) or CT scan (p=0.18) |
| Oikonomaki et al109 | 102 | Adults with ESRD on haemodialysis Sex: not specified Age: 67 |
Design: prospective, randomised, open-label clinical trial Intervention: vitamin K2 supplementation (200 µg) Follow-up (years): 1 |
No change in abdominal aortic calcification via CT-measured Agatston score |
| De Vriese et al108 | 132 | Chronic haemodialysis patients with non-valvular atrial fibrillation and CHA2DS2-VASc score ≥2 Sex: 33% female Age: 80 |
Design: multicentre, prospective, randomised, open-label trial Intervention: VKA vs rivaroxaban vs rivaroxaban +vitamin K2 (2000 µg three times per week) Follow-up (months): 18 |
No differences in change of PWV or coronary artery, thoracic aorta, or cardiac valve calcium scores at follow-up, or all-cause death, stroke or cardiovascular events between groups |
| Bartstra et al111 | 68 | Subjects aged >40 years with CVD, type 2 diabetes, and eGFR >30 Sex: 24% female Age: 69 |
Design: post-hoc analysis of double-blind RCT Intervention: vitamin K2 (MK-7) supplementation (360 µg) Follow-up (months): 6 |
No change in total arterial calcification, assessed by CT scan in several large arterial beds |
| Valvular calcification | ||||
| Geleijnse et al91 | 4807 | Dutch subjects >55 years without prior MI at baseline (1990–1993) Sex: 38% male Age: 67 |
Design: prospective, population-based Intervention: dietary vitamin K1 and K2 using FFQ Follow-up (years): 7 |
Severe aortic calcification in mid and upper tertials of vitamin K2 intake (OR=0.71 and 0.48, respectively; p<0.05) |
| Brandenburg et al107 | 99 | Asymptomatic or mildly symptomatic patients without CKD with aortic valve PFV >2 m/s Sex: 82% male Age: 69 |
Design: prospective, single-centre, open-label RCT Intervention: vitamin K1 supplementation (2 mg) Follow-up (years): 1 |
Progression in aortic valve calcification volume score (10% vs 22%, p=0.04) |
Both ages and follow-up times are presented as mean years, unless otherwise specified, and rounded to the nearest whole number. All RCT study designs are placebo controlled unless otherwise specified. All provided dosages are per daily unless otherwise noted. P values <0.05 denote significance.
AU, Agtston units; CAC, coronary artery calcification; CCA, common carotid artery; CHD, coronary heart disease; CKD, chronic kidney disease; cOC, carboxylated osteocalcin; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate; ESRD, end-stage renal disease; FFQ, Food Frequency Questionnaire; 18F-NaF PET, 18sodium fluoride positron emission tomography; HMW, human molecular weight; HOMA-B, homeostasis model for assessment of B-cell function; HOMA-IR, homeostasis model for assessment of insulin resistance; HRT, hormone replacement therapy; MI, myocardial infarction; MK, menaquinone; N/A, not applicable; PFV, peak flow velocity; PWV, pulse wave velocity; QUICKI, quantitative insulin sensitivity check index; RCT, randomised control trial; RR, relative risk; VAT, estimated visceral adipose tissue area; VKA, vitamin K antagonist.
Arterial stiffness and endothelial dysfunction
Both vitamin K1 and MK-7 reduce arterial stiffness and improve elastic properties of the carotid artery.94 MK-7 supplementation improves arterial stiffness in healthy adults95 postmenopausal women,90 patients with CAD96 and renal transplant recipients,27 as measured by PWV. It is also thought that the protective effects of vitamin K2 on cardiovascular mortality may be related to the vitamin K-dependent regulation of endothelial function.83 Endothelial dysfunction, defined as impaired endothelium-dependent vasodilation, is a significant predictor of adverse cardiovascular outcomes.97 Evidence from a recent study reveals that in genetically driven mice models of high hypercholesterolaemia (ApoE/LDLR−/−), K2-MK-7 improves nitric oxide-dependent endothelial function, assessed by MRI of the flow-mediated dilation, vascular response to acetylcholine administration and endothelial nitric oxide synthase-dependent nitric oxide production.98 Moreover, MGP has been shown in animal models to inhibit osteogenic properties of vascular endothelial cells that is driven by BMP signalling.99
Cardiac output
The role of vitamin K2 in mitochondrial function is mediated by its production of mitochondrial ATP, which has direct implications for contractile muscles (ie, cardiac) that are comprised of abundant mitochondria.100 Intake of vitamin K2 has been associated with increased cardiac output, stroke volume and heart rate, and decreased blood lactate.101 These effects are consistent with the greater maximal cardiovascular performance seen with oral vitamin K2 supplementation.
Metabolic syndrome
Several studies have examined the relationship between vitamin K2 intake and indices of type 2 diabetes mellitus, a major risk factor for CVD. From a large prospective study of 38 094 Dutch individuals (aged 20–70 years), Beulens et al revealed that dietary MK intake (10 µg increment increase) was inversely associated (p=0.04) with incidence of type 2 diabetes.102 In a randomised clinical trial, Choi et al demonstrated that 4 weeks of supplementing 30 mg/day of vitamin K2 (menatetrenone) significantly increased the insulin sensitivity index (p=0.01) and disposition index (p<0.01) compared with placebo in healthy young men.103 The benefits of vitamin K2 extend beyond direct effect on type 2 diabetes as it has been recently shown, in a randomised placebo-controlled trial on 214 postmenopausal healthy women receiving 180 µg/day of vitamin K2 (MK-7) or placebo, to have favourable effect on obesity with reduction in abdominal and visceral fat among those who responded well to MK-7 (manifested through elevated of cOC).51
Vascular and valvular calcification
Anticoagulation-mediated inhibition of vitamin K metabolism has been associated with progression of both vascular and valvular calcification. Animal studies have found increased arterial and soft tissue calcification as a result of inhibition of vitamin K-dependent proteins by VKA.33 80 Long-term VKA use is associated with both coronary and extracoronary vascular calcification in humans.104 105 Sønderskov et al recently demonstrated that among 14 604 participants within the Danish Cardiovascular Screening (DANCAVAS) trial, VKA use was associated with progression of aortic valve calcification, evidenced by a 6% increase in calcification with each year of treatment.106 These results remained consistent after a sensitivity analysis excluding patients with cardiac risk factors on statins showed no progression of calcification in those taking direct oral anticoagulants.
Vitamin K supplementation may delay the progression of aortic valve calcification. In a rat model, warfarin-induced arterial calcification and arterial stiffness, where inactive MGP was highly expressed, appeared to regress with a diet rich in vitamin K.80 The first in-human randomised control trial recently found that among a small cohort of 99 patients with AS, vitamin K1 intake (2 mg daily) decelerated the progression of CT-based aortic valvular calcification compared with placebo (10% vs 22%, respectively; p=0.04).107 It is important to note that 27 patients (12 vitamin K1, 15 placebo) dropped out of the study.
Vitamin K supplementation may also potentially target vascular calcification. Vitamin K2 intake has been inversely correlated with CAC in healthy elderly individuals.91 Further, vitamin K1 slowed the progression of CAC at 3-year follow-up.86 Yet, despite a significant reduction in dp-ucMGP, two recent studies failed to demonstrate a change in aortic calcification scores with vitamin K2 supplementation in those on haemodialysis with or without anticoagulation.108 109 In one double-blind, placebo-controlled trial by Zwakenberg et al, 68 patients with type 2 diabetes mellitus were randomised to receive 360 µg/day of vitamin K2 (MK-7) or placebo for 6 months,110 and there was no significant difference in femoral arterial calcification measured by either 18sodium fluoride positron emission tomography (primary outcome) or CT scan (secondary outcome). A post-hoc analysis of this trial was recently published to investigate the effect of vitamin K2 on CT-based arterial calcification mass, quantified in several large arterial beds, and there was no significant difference between placebo and supplemented groups.111 Both studies were limited by the short duration of follow-up, small sample size, low percentage of severe vitamin K deficiency and high dropout rates. Despite the evident potential of vitamin K2 in modulating vascular and valvular calcification, its definitive role is yet to be fully established.
Cardiovascular morbidity and mortality
Table 2 summarises the studies to date of vitamin K intake and cardiovascular mortality. The first to report on dietary intake of vitamin K2, the prospective Rotterdam study recruited 4807 subjects with dietary data and no history of myocardial infarction between 1990 and 1993, and followed patients until January 2020. The authors stratified groups by quartiles of increasing vitamin K2 intake, and found that the upper tertials of vitamin K2 but not K1 intake was inversely associated with severe aortic calcification (OR=0.48) as well as cardiovascular (relative risk (RR)=0.43) and all-cause (RR=0.74) mortality. These findings persisted after adjusting for traditional risk factors and dietary factors.91 In another prospective cohort study inclusive of women aged 49–70 years without prior CVD who were enrolled between 1993 and 1997 as part of the European Prospect-EPIC cohort (mean follow-up of 8.1±1.6 years), vitamin K2 but not K1 intake was significantly and inversely associated with risk of incident CAD (HR=0.9 per 10 µg/day of vitamin K2 intake).87 These findings were consistent with a prospective Norwegian study that followed 2987 healthy subjects for a median of 11 years and demonstrated an association between vitamin K2 but not K1 and reduced CAD risk (HR=0.52, 95% CI: 0.29 to 0.94, p trend=0.03).112 Moreover, a separate prospective investigation of 40 087 men from the Health Professionals’ Follow-up Study from 1986 to 2000 found a significant trend (RR=0.84, p=0.05) towards a lower incidence of total CAD with increasing intake of food rich in vitamin K1.113
Table 2.
Association of dietary vitamin K intake with coronary disease and cardiovascular mortality
| Study | Sample size | Patient population | Study methods | Study findings |
| Geleijnse et al91 | 4807 | Dutch subjects >55 years without prior MI at baseline (1990–1993) Sex: 38% male Age: 67 |
Design: prospective, population-based Intervention: vitamin K1 and K2 using FFQ Follow-up (years): 7 |
Cardiovascular mortality (RR=0.43 (0.24 to 0.77)) and all-cause mortality (RR=0.74 (0.59 to 0.92)) with K2 but not K1 in upper tertials of energy-adjusted intake |
| Erkkilä et al113 | 40 087 | Healthcare workers aged 40–75 years, free of CVD, stroke and cancer at baseline (1986–2000) Sex: male only Age: 53 |
Design: prospective, population-based Intervention: vitamin K1 using FFQ Follow-up (years): 14 |
Incidence of total CAD (RR=0.84, p trend=0.05) |
| Gast et al87 | 16 057 | Subjects aged 49–70 years free of CVD, recruited from the European Prospect-EPIC cohort (1993–1997) Sex: female only Age: 67 |
Design: prospective, population-based Intervention: vitamin K2 (subtypes MK-7–9) using FFQ Follow-up (years): 8 |
Risk of incident CAD (HR=0.91 (0.85 to 1.00)) |
| Juanola-Falgarona et al114 | 7216 | Community-dwelling adults enrolled in PREDIMED trial, without baseline CVD but with either type 2 diabetes or ≥3 cardiovascular risk factors Sex: 57% female Age: 67 |
Design: prospective, population-based Intervention: dietary vitamin K1 and K2 (subtypes MK-7–9) using FFQ Follow-up (years): 5 |
All-cause mortality with increasing intake of vitamin K1 or K2 (HR=0.57 and HR=0.55, respectively; p<0.05) |
| Cheung et al115 | 3401 | Non-hospitalised participants ≥20 years of age with CKD from the NHANES III Study (1988–1994) Sex: 67% female Age: 62 |
Design: prospective, population-based Intervention: vitamin K1 and K2 using 24-hour dietary recall Follow-up (years): 13 |
All-cause (HR=0.85 (0.72 to 1), p=0.047) and CVD mortality (HR=0.78 (0.64 to 0.95), p=0.016) |
| Zwakenberg et al121 | 33 289 | Dutch subjects aged 20–70 years without baseline CVD, diabetes or cancer recruited from the EPIC-NL cohort (1993–1997) Sex: 26% male Age: 49 |
Design: prospective, population-based Intervention: vitamin K1 and K2 using FFQ Follow-up (years): 17 |
Borderline CHD mortality with higher long chain vitamin K2 intake (HR=0.86 (0.74 to 1.00), p trend=0.06) No association of vitamin K1 or K2 with CVD or all-cause mortality |
| Haugsgjerd et al112 | 2987 | Healthy Norwegian subjects aged 46–49 years without baseline CAD recruited from the Hordaland Health Study (1997–1999) Sex: 57% female Age: 48 |
Design: prospective, population-based Intervention: vitamin K1 and K2 using FFQ Follow-up (years): 11 |
Risk of incident CAD with higher vitamin K2 but not K1 (HR=0.52, p trend=0.03), attenuated by adjusting for dietary confounders (HR=0.58, p trend=0.16) |
Both ages and follow-up times are presented as mean years, or median years in Cheung et al115 and rounded to the nearest whole number. P values <0.05 denote significance.
CAD, coronary artery disease; CHD, coronary heart disease; CKD, chronic kidney disease; CVD, cardiovascular disease; FFQ, Food Frequency Questionnaire; MI, myocardial infarction; MK, menaquinone; NHANES III, National Health and Nutrition Examination Survey; RR, relative risk.
In the prospective PREDIMED (Prevención con Dieta Mediterránea) Study, the authors investigated the impact of dietary vitamin K1 and K2 on all-cause mortality among 7216 participants who were followed for a median of 4.8 years.114 They found a significant and inverse relationship between dietary vitamin K1 intake and risk of all-cause mortality after controlling for potential confounders (HR=0.64, 95% CI: 0.45 to 0.90). On longitudinal assessment, those who increased their intake of vitamin K1 or vitamin K2 had a lower risk of all-cause mortality (HR=0.57 and HR=0.55, respectively) relative to those with reduced or stable intake. These findings are in line with those of patients with CKD who were followed for a median of 13.3 years as part of the National Health and Nutrition Examination Survey III registry (HR=0.78, 95% CI: 0.64 to 95, p=0.016).115 A recent meta-analysis concluded that higher dietary consumption of vitamin K1 and K2 is associated with a lower risk of CAD (pooled HR=0.92, 95% CI: 0.84 to 0.99 and HR=0.70, 95% CI: 0.53 to 0.93, respectively), but has no correlation with all-cause mortality, CVD mortality or stroke.6
Conclusions and future directions
This review covers the rapidly expanding evidence supporting the cardioprotective effects of vitamin K2 intake. Mediated by activated MGP, the benefits of vitamin K2 extend beyond calcification homeostasis and antagonism, and may further include preventing or slowing the progression of arterial stiffness, endothelial dysfunction, diabetes and HF. Moreover, vitamin K2 supplementation appears safe and practical, and its use can be readily investigated in randomised clinical trials. Although the data presented in this review are encouraging, most of the included studies were limited by their non-randomised design, heterogeneity in results, variable dosages and formulations of vitamin K used, small sample sizes, short duration of follow-up and restricted ability to accurately assess vitamin K intake, in turn precluding our ability to infer causality of clinical endpoints. With evidence mounting, the definitive role of vitamin K2 supplementation in delaying progression of vascular and valvular calcification remains the subject of multiple randomised clinical trials.116 117 Nonetheless, the utility of vitamin K2 and MGP in various patient populations such as those with valvular heart disease and cardiomyopathy grows commensurate the data supporting its efficacy in improving cardiac function and decelerating arterial stiffness.
Footnotes
Twitter: @kassisMD
EH and NK contributed equally.
Contributors: EH conceived and designed the study. EH, NK, J-PI and AS collected, analysed and interpreted the data, and performed the literature review. EH, NK and J-PI drafted the manuscript and designed the tables. LJS, TI, SCH, AB and SK revised the manuscript. OA designed the figures. TI, SCH and SK supervised the study. All authors have read and approved the manuscript.
Funding: This study was made possible by a generous gift from Jennifer and Robert McNeil as unrestricted philanthropic support to the Heart and Vascular Institute, Cleveland Clinic.
Disclaimer: The funding source had no role in the design or conduct of the study; collection, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Competing interests: LJS received an institutional grant from NattoPharma.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Proudfoot D, Shanahan CM. Molecular mechanisms mediating vascular calcification: role of matrix Gla protein. Nephrology 2006;11:455–61. 10.1111/j.1440-1797.2006.00660.x [DOI] [PubMed] [Google Scholar]
- 2.Stafford DW. The vitamin K cycle. J Thromb Haemost 2005;3:1873–8. 10.1111/j.1538-7836.2005.01419.x [DOI] [PubMed] [Google Scholar]
- 3.Mizuiri S, Nishizawa Y, Yamashita K, et al. Relationship of matrix Gla protein and vitamin K with vascular calcification in hemodialysis patients. Ren Fail 2019;41:770–7. 10.1080/0886022X.2019.1650065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zwakenberg SR, Burgess S, Sluijs I, et al. Circulating phylloquinone, inactive matrix Gla protein and coronary heart disease risk: a two-sample Mendelian randomization study. Clin Nutr 2020;39:1131–6. 10.1016/j.clnu.2019.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cranenburg ECM, Koos R, Schurgers LJ, et al. Characterisation and potential diagnostic value of circulating matrix Gla protein (MGP) species. Thromb Haemost 2010;104:811–22. 10.1160/TH09-11-0786 [DOI] [PubMed] [Google Scholar]
- 6.Chen H-G, Sheng L-T, Zhang Y-B, et al. Association of vitamin K with cardiovascular events and all-cause mortality: a systematic review and meta-analysis. Eur J Nutr 2019;58:2191–205. 10.1007/s00394-019-01998-3 [DOI] [PubMed] [Google Scholar]
- 7.Luo G, Ducy P, McKee MD, et al. Spontaneous calcification of arteries and cartilage in mice lacking matrix Gla protein. Nature 1997;386:78. 10.1038/386078a0 [DOI] [PubMed] [Google Scholar]
- 8.Murshed M, Schinke T, McKee MD, et al. Extracellular matrix mineralization is regulated locally; different roles of two Gla-containing proteins. J Cell Biol 2004;165:625–30. 10.1083/jcb.200402046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zebboudj AF, Imura M, Boström K. Matrix Gla protein, a regulatory protein for bone morphogenetic protein-2. J Biol Chem 2002;277:4388–94. 10.1074/jbc.M109683200 [DOI] [PubMed] [Google Scholar]
- 10.Price PA, Nguyen TMT, Williamson MK. Biochemical characterization of the serum fetuin-mineral complex. J Biol Chem 2003;278:22153–60. 10.1074/jbc.M300739200 [DOI] [PubMed] [Google Scholar]
- 11.Sweatt A, Sane DC, Hutson SM, et al. Matrix Gla protein (MGP) and bone morphogenetic protein-2 in aortic calcified lesions of aging rats. J Thromb Haemost 2003;1:178–85. 10.1046/j.1538-7836.2003.00023.x [DOI] [PubMed] [Google Scholar]
- 12.Fusaro M, Gallieni M, Porta C, et al. Vitamin K effects in human health: new insights beyond bone and cardiovascular health. J Nephrol 2020;33:239–49. 10.1007/s40620-019-00685-0 [DOI] [PubMed] [Google Scholar]
- 13.Luo X-H, Zhao L-L, Yuan L-Q, et al. Development of arterial calcification in adiponectin-deficient mice: adiponectin regulates arterial calcification. J Bone Miner Res 2009;24:1461–8. 10.1359/jbmr.090227 [DOI] [PubMed] [Google Scholar]
- 14.Huang L, Yang L, Luo L, et al. Osteocalcin improves metabolic profiles, body composition and arterial stiffening in an induced diabetic rat model. Exp Clin Endocrinol Diabetes 2017;125:234–40. 10.1055/s-0042-122138 [DOI] [PubMed] [Google Scholar]
- 15.Bacchetta J, Boutroy S, Guebre-Egziabher F, et al. The relationship between adipokines, osteocalcin and bone quality in chronic kidney disease. Nephrol Dial Transplant 2009;24:3120–5. 10.1093/ndt/gfp262 [DOI] [PubMed] [Google Scholar]
- 16.Fusaro M, Giannini S, Gallieni M, et al. Calcimimetic and vitamin D analog use in hemodialyzed patients is associated with increased levels of vitamin K dependent proteins. Endocrine 2016;51:333–41. 10.1007/s12020-015-0673-z [DOI] [PubMed] [Google Scholar]
- 17.Confavreux CB, Szulc P, Casey R, et al. Higher serum osteocalcin is associated with lower abdominal aortic calcification progression and longer 10-year survival in elderly men of the Minos cohort. J Clin Endocrinol Metab 2013;98:1084–92. 10.1210/jc.2012-3426 [DOI] [PubMed] [Google Scholar]
- 18.Son B-K, Kozaki K, Iijima K, et al. Statins protect human aortic smooth muscle cells from inorganic phosphate-induced calcification by restoring Gas6-Axl survival pathway. Circ Res 2006;98:1024–31. 10.1161/01.RES.0000218859.90970.8d [DOI] [PubMed] [Google Scholar]
- 19.Son B-K, Kozaki K, Iijima K, et al. Gas6/Axl-PI3K/Akt pathway plays a central role in the effect of statins on inorganic phosphate-induced calcification of vascular smooth muscle cells. Eur J Pharmacol 2007;556:1–8. 10.1016/j.ejphar.2006.09.070 [DOI] [PubMed] [Google Scholar]
- 20.Son B-K, Akishita M, Iijima K, et al. Androgen receptor-dependent transactivation of growth arrest-specific gene 6 mediates inhibitory effects of testosterone on vascular calcification. J Biol Chem 2010;285:7537–44. 10.1074/jbc.M109.055087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Son B-K, Akishita M, Iijima K, et al. Adiponectin antagonizes stimulatory effect of tumor necrosis factor-alpha on vascular smooth muscle cell calcification: regulation of growth arrest-specific gene 6-mediated survival pathway by adenosine 5'-monophosphate-activated protein kinase. Endocrinology 2008;149:1646–53. 10.1210/en.2007-1021 [DOI] [PubMed] [Google Scholar]
- 22.Hasanbasic I, Rajotte I, Blostein M. The role of gamma-carboxylation in the anti-apoptotic function of Gas6. J Thromb Haemost 2005;3:2790–7. 10.1111/j.1538-7836.2005.01662.x [DOI] [PubMed] [Google Scholar]
- 23.Braam LA, Dissel P, Gijsbers BL, et al. Assay for human matrix Gla protein in serum: potential applications in the cardiovascular field. Arterioscler Thromb Vasc Biol 2000;20:1257–61. 10.1161/01.atv.20.5.1257 [DOI] [PubMed] [Google Scholar]
- 24.Schurgers LJ, Teunissen KJF, Knapen MHJ, et al. Novel conformation-specific antibodies against matrix gamma-carboxyglutamic acid (Gla) protein: undercarboxylated matrix Gla protein as marker for vascular calcification. Arterioscler Thromb Vasc Biol 2005;25:1629–33. 10.1161/01.ATV.0000173313.46222.43 [DOI] [PubMed] [Google Scholar]
- 25.Hermans MMH, Vermeer C, Kooman JP, et al. Undercarboxylated matrix Gla protein levels are decreased in dialysis patients and related to parameters of calcium-phosphate metabolism and aortic augmentation index. Blood Purif 2007;25:395–401. 10.1159/000108629 [DOI] [PubMed] [Google Scholar]
- 26.Pivin E, Ponte B, Pruijm M, et al. Inactive matrix gla-protein is associated with arterial stiffness in an adult population-based study. Hypertension 2015;66:85–92. 10.1161/HYPERTENSIONAHA.115.05177 [DOI] [PubMed] [Google Scholar]
- 27.Mansour AG, Hariri E, Daaboul Y, et al. Vitamin K2 supplementation and arterial stiffness among renal transplant recipients-a single-arm, single-center clinical trial. J Am Soc Hypertens 2017;11:589-597. 10.1016/j.jash.2017.07.001 [DOI] [PubMed] [Google Scholar]
- 28.Wei F-F, Thijs L, Cauwenberghs N, et al. Central hemodynamics in relation to circulating Desphospho-Uncarboxylated matrix Gla protein: a population study. J Am Heart Assoc 2019;8:e011960. 10.1161/JAHA.119.011960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mansour AG, Ahdab R, Daaboul Y, et al. Vitamin K2 status and arterial stiffness among untreated migraine patients: a case-control study. Headache 2020;60:589–99. 10.1111/head.13715 [DOI] [PubMed] [Google Scholar]
- 30.Ikari Y, Saito F, Kiyooka T, et al. Switching from warfarin to rivaroxaban induces sufficiency of vitamin K and reduction of arterial stiffness in patients with atrial fibrillation. Heart Vessels 2020. [DOI] [PubMed] [Google Scholar]
- 31.Cocciolone AJ, Hawes JZ, Staiculescu MC, et al. Elastin, arterial mechanics, and cardiovascular disease. Am J Physiol Heart Circ Physiol 2018;315:H189–205. 10.1152/ajpheart.00087.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meier M, Weng LP, Alexandrakis E, et al. Tracheobronchial stenosis in Keutel syndrome. Eur Respir J 2001;17:566–9. 10.1183/09031936.01.17305660 [DOI] [PubMed] [Google Scholar]
- 33.Price PA, Faus SA, Williamson MK. Warfarin causes rapid calcification of the elastic lamellae in rat arteries and heart valves. Arterioscler Thromb Vasc Biol 1998;18:1400–7. 10.1161/01.atv.18.9.1400 [DOI] [PubMed] [Google Scholar]
- 34.Lerner RG, Aronow WS, Sekhri A, et al. Warfarin use and the risk of valvular calcification. J Thromb Haemost 2009;7:2023–7. 10.1111/j.1538-7836.2009.03630.x [DOI] [PubMed] [Google Scholar]
- 35.Herrmann SM, Whatling C, Brand E, et al. Polymorphisms of the human matrix Gla protein (MGP) gene, vascular calcification, and myocardial infarction. Arterioscler Thromb Vasc Biol 2000;20:2386–93. 10.1161/01.atv.20.11.2386 [DOI] [PubMed] [Google Scholar]
- 36.Karsli-Ceppioglu S, Yazar S, Keskin Y, et al. Association of Genetic Polymorphisms in the Matrix Gla Protein (MGP) Gene with Coronary Artery Disease and Serum MGP Levels. Balkan J Med Genet 2019;22:43–50. 10.2478/bjmg-2019-0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dalmeijer GW, van der Schouw YT, Vermeer C, et al. Circulating matrix Gla protein is associated with coronary artery calcification and vitamin K status in healthy women. J Nutr Biochem 2013;24:624–8. 10.1016/j.jnutbio.2012.02.012 [DOI] [PubMed] [Google Scholar]
- 38.Liabeuf S, Bourron O, Olivier B, Vemeer C, et al. Vascular calcification in patients with type 2 diabetes: the involvement of matrix Gla protein. Cardiovasc Diabetol 2014;13:85. 10.1186/1475-2840-13-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zwakenberg SR, van der Schouw YT, Vermeer C, et al. Matrix Gla protein, plaque stability, and cardiovascular events in patients with severe atherosclerotic disease. Cardiology 2018;141:32–6. 10.1159/000493006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yamamoto K, Yamamoto H, Takeuchi M, et al. Risk factors for progression of degenerative aortic valve disease in the Japanese- the Japanese aortic stenosis study (JASS) prospective analysis. Circ J 2015;79:CJ-15-0499. 10.1253/circj.CJ-15-0499 [DOI] [PubMed] [Google Scholar]
- 41.Di Lullo L, Tripepi G, Ronco C, et al. Cardiac valve calcification and use of anticoagulants: preliminary observation of a potentially modifiable risk factor. Int J Cardiol 2019;278:243–9. 10.1016/j.ijcard.2018.11.119 [DOI] [PubMed] [Google Scholar]
- 42.Allison MA, Cheung P, Criqui MH, et al. Mitral and aortic annular calcification are highly associated with systemic calcified atherosclerosis. Circulation 2006;113:861–6. 10.1161/CIRCULATIONAHA.105.552844 [DOI] [PubMed] [Google Scholar]
- 43.Parker BD, Schurgers LJ, Vermeer C, et al. The association of uncarboxylated matrix Gla protein with mitral annular calcification differs by diabetes status: the heart and soul study. Atherosclerosis 2010;210:320–5. 10.1016/j.atherosclerosis.2009.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tuñón-Le Poultel D, Cannata-Andía JB, Román-García P, et al. Association of matrix Gla protein gene functional polymorphisms with loss of bone mineral density and progression of aortic calcification. Osteoporos Int 2014;25:1237–46. 10.1007/s00198-013-2577-1 [DOI] [PubMed] [Google Scholar]
- 45.Borrás T, Smith MH, Buie LK. A novel Mgp-Cre knock-in mouse reveals an anticalcification/antistiffness candidate gene in the trabecular meshwork and peripapillary scleral region. Invest Ophthalmol Vis Sci 2015;56:2203–14. 10.1167/iovs.15-16460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fraser JD, Price PA, Lung PP. Lung, heart, and kidney express high levels of mRNA for the vitamin K-dependent matrix Gla protein. Implications for the possible functions of matrix Gla protein and for the tissue distribution of the gamma-carboxylase. J Biol Chem 1988;263:11033–6. [PubMed] [Google Scholar]
- 47.Wei F-F, Trenson S, Monney P, et al. Epidemiological and histological findings implicate matrix Gla protein in diastolic left ventricular dysfunction. PLoS One 2018;13:e0193967. 10.1371/journal.pone.0193967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wei F-F, Huang Q-F, Zhang Z-Y, et al. Inactive matrix Gla protein is a novel circulating biomarker predicting retinal arteriolar narrowing in humans. Sci Rep 2018;8:1–8. 10.1038/s41598-018-33257-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wong TY, Klein R, Nieto FJ, et al. Retinal microvascular abnormalities and 10-year cardiovascular mortality: a population-based case-control study. Ophthalmology 2003;110:933–40. 10.1016/S0161-6420(03)00084-8 [DOI] [PubMed] [Google Scholar]
- 50.Fusaro M, Cianciolo G, Brandi ML, et al. Vitamin K and osteoporosis. Nutrients 2020;12:3625. 10.3390/nu12123625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Knapen MHJ, Jardon KM, Vermeer C. Vitamin K-induced effects on body fat and weight: results from a 3-year vitamin K2 intervention study. Eur J Clin Nutr 2018;72:136–41. 10.1038/ejcn.2017.146 [DOI] [PubMed] [Google Scholar]
- 52.Cranenburg ECM, Schurgers LJ, Uiterwijk HH, et al. Vitamin K intake and status are low in hemodialysis patients. Kidney Int 2012;82:605–10. 10.1038/ki.2012.191 [DOI] [PubMed] [Google Scholar]
- 53.Holden RM, Iliescu E, Morton AR, et al. Vitamin K status of Canadian peritoneal dialysis patients. Perit Dial Int 2008;28:415–8. [PubMed] [Google Scholar]
- 54.Keyzer CA, Vermeer C, Joosten MM, et al. Vitamin K status and mortality after kidney transplantation: a cohort study. Am J Kidney Dis 2015;65:474–83. 10.1053/j.ajkd.2014.09.014 [DOI] [PubMed] [Google Scholar]
- 55.Wei F-F, Trenson S, Thijs L, et al. Desphospho-uncarboxylated matrix Gla protein is a novel circulating biomarker predicting deterioration of renal function in the general population. Nephrol Dial Transplant 2018;33:1122–8. 10.1093/ndt/gfx258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wei F-F, Drummen NEA, Thijs L, et al. Vitamin-K-dependent protection of the renal microvasculature: histopathological studies in normal and diseased kidneys. Pulse 2016;4:85–91. 10.1159/000448008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wei F-F, Drummen NEA, Schutte AE, et al. Vitamin K dependent protection of renal function in multi-ethnic population studies. EBioMedicine 2016;4:162–9. 10.1016/j.ebiom.2016.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fusaro M, Noale M, Viola V, et al. Vascular calcifications, and mortality: vitamin K Italian (VIKI) dialysis study. J Bone Miner Res 2012;27:2271–8. [DOI] [PubMed] [Google Scholar]
- 59.Parker BD, Ix JH, Cranenburg ECM, et al. Association of kidney function and uncarboxylated matrix Gla protein: data from the heart and soul study. Nephrol Dial Transplant 2009;24:2095–101. 10.1093/ndt/gfp024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ueland T, Dahl CP, Gullestad L, et al. Circulating levels of non-phosphorylated undercarboxylated matrix Gla protein are associated with disease severity in patients with chronic heart failure. Clin Sci 2011;121:119–27. 10.1042/CS20100589 [DOI] [PubMed] [Google Scholar]
- 61.Kurnatowska I, Grzelak P, Masajtis-Zagajewska A, et al. Plasma Desphospho-Uncarboxylated matrix Gla protein as a marker of kidney damage and cardiovascular risk in advanced stage of chronic kidney disease. Kidney Blood Press Res 2016;41:231–9. 10.1159/000443426 [DOI] [PubMed] [Google Scholar]
- 62.Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol 2013;62:263–71. 10.1016/j.jacc.2013.02.092 [DOI] [PubMed] [Google Scholar]
- 63.Ueland T, Gullestad L, Dahl CP, et al. Undercarboxylated matrix Gla protein is associated with indices of heart failure and mortality in symptomatic aortic stenosis. J Intern Med 2010;268:483–92. 10.1111/j.1365-2796.2010.02264.x [DOI] [PubMed] [Google Scholar]
- 64.Hwang DM, Dempsey AA, Lee CY, et al. Identification of differentially expressed genes in cardiac hypertrophy by analysis of expressed sequence tags. Genomics 2000;66:1–14. 10.1006/geno.2000.6171 [DOI] [PubMed] [Google Scholar]
- 65.Rysä J, Leskinen H, Ilves M, et al. Distinct upregulation of extracellular matrix genes in transition from hypertrophy to hypertensive heart failure. Hypertension 2005;45:927–33. 10.1161/01.HYP.0000161873.27088.4c [DOI] [PubMed] [Google Scholar]
- 66.Mustonen E, Pohjolainen V, Aro J, et al. Upregulation of cardiac matrix Gla protein expression in response to hypertrophic stimuli. Blood Press 2009;18:286–93. 10.3109/08037050903244643 [DOI] [PubMed] [Google Scholar]
- 67.Mirotsou M, Dzau VJ, Pratt RE, et al. Physiological genomics of cardiac disease: quantitative relationships between gene expression and left ventricular hypertrophy. Physiol Genomics 2006;27:86–94. 10.1152/physiolgenomics.00028.2006 [DOI] [PubMed] [Google Scholar]
- 68.Blaxall BC, Spang R, Rockman HA, et al. Differential myocardial gene expression in the development and rescue of murine heart failure. Physiol Genomics 2003;15:105–14. 10.1152/physiolgenomics.00087.2003 [DOI] [PubMed] [Google Scholar]
- 69.Nishimoto SK, Nishimoto M. Matrix Gla protein C-terminal region binds to vitronectin. co-localization suggests binding occurs during tissue development. Matrix Biol 2005;24:353–61. 10.1016/j.matbio.2005.05.004 [DOI] [PubMed] [Google Scholar]
- 70.Mayer O, Seidlerová J, Bruthans J, et al. Desphospho-uncarboxylated matrix gla-protein is associated with mortality risk in patients with chronic stable vascular disease. Atherosclerosis 2014;235:162–8. 10.1016/j.atherosclerosis.2014.04.027 [DOI] [PubMed] [Google Scholar]
- 71.Liu Y-P, Gu Y-M, Thijs L, et al. Inactive matrix Gla protein is causally related to adverse health outcomes: a Mendelian randomization study in a Flemish population. Hypertension 2015;65:463–70. 10.1161/HYPERTENSIONAHA.114.04494 [DOI] [PubMed] [Google Scholar]
- 72.van den Heuvel EGHM, van Schoor NM, Lips P, et al. Circulating uncarboxylated matrix Gla protein, a marker of vitamin K status, as a risk factor of cardiovascular disease. Maturitas 2014;77:137–41. 10.1016/j.maturitas.2013.10.008 [DOI] [PubMed] [Google Scholar]
- 73.Dalmeijer GW, van der Schouw YT, Magdeleyns EJ, et al. Matrix Gla protein species and risk of cardiovascular events in type 2 diabetic patients. Diabetes Care 2013;36:3766–71. 10.2337/dc13-0065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Seidlerová J, Vaněk J, Vaněk J, et al. The abnormal status of uncarboxylated matrix Gla protein species represents an additional mortality risk in heart failure patients with vascular disease. Int J Cardiol 2016;203:916–22. 10.1016/j.ijcard.2015.10.226 [DOI] [PubMed] [Google Scholar]
- 75.Mayer O, Bruthans J, Seidlerová J, et al. The coincidence of low vitamin K status and high expression of growth differentiation factor 15 may indicate increased mortality risk in stable coronary heart disease patients. Nutr Metab Cardiovasc Dis 2021;31:540-551. 10.1016/j.numecd.2020.09.015 [DOI] [PubMed] [Google Scholar]
- 76.Shea MK, Booth SL, Weiner DE, et al. Circulating vitamin K is inversely associated with incident cardiovascular disease risk among those treated for hypertension in the health, aging, and body composition study (health ABC). J Nutr 2017;147:888–95. 10.3945/jn.117.249375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nelsestuen GL, Zytkovicz TH, Howard JB. The mode of action of vitamin K. identification of gamma-carboxyglutamic acid as a component of prothrombin. J Biol Chem 1974;249:6347–50. [PubMed] [Google Scholar]
- 78.Walther B, Karl JP, Booth SL, et al. Menaquinones, bacteria, and the food supply: the relevance of dairy and fermented food products to vitamin K requirements. Adv Nutr 2013;4:463–73. 10.3945/an.113.003855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Thijssen HH, Drittij-Reijnders MJ. Vitamin K status in human tissues: tissue-specific accumulation of phylloquinone and menaquinone-4. Br J Nutr 1996;75:121. 10.1079/bjn19960115 [DOI] [PubMed] [Google Scholar]
- 80.Schurgers LJ, Spronk HMH, Soute BAM, et al. Regression of warfarin-induced medial elastocalcinosis by high intake of vitamin K in rats. Blood 2007;109:2823–31. 10.1182/blood-2006-07-035345 [DOI] [PubMed] [Google Scholar]
- 81.Westenfeld R, Krueger T, Schlieper G, et al. Effect of vitamin K2 supplementation on functional vitamin K deficiency in hemodialysis patients: a randomized trial. Am J Kidney Dis 2012;59:186–95. 10.1053/j.ajkd.2011.10.041 [DOI] [PubMed] [Google Scholar]
- 82.Caluwé R, Vandecasteele S, Van Vlem B, et al. Vitamin K2 supplementation in haemodialysis patients: a randomized dose-finding study. Nephrol Dial Transplant 2014;29:1385–90. 10.1093/ndt/gft464 [DOI] [PubMed] [Google Scholar]
- 83.Riphagen IJ, Keyzer CA, Drummen NEA, et al. Prevalence and effects of functional vitamin K insufficiency: the PREVEND study. Nutrients 2017;9. 10.3390/nu9121334. [Epub ahead of print: 08 Dec 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Theuwissen E, Magdeleyns EJ, Braam LAJLM, et al. Vitamin K status in healthy volunteers. Food Funct 2014;5:229–34. 10.1039/c3fo60464k [DOI] [PubMed] [Google Scholar]
- 85.Beulens JWJ, Bots ML, Atsma F, et al. Grobbee de and van der Schouw YT. high dietary menaquinone intake is associated with reduced coronary calcification. Atherosclerosis 2009;203:489–93. [DOI] [PubMed] [Google Scholar]
- 86.Shea MK, O'Donnell CJ, Hoffmann U, et al. Vitamin K supplementation and progression of coronary artery calcium in older men and women. Am J Clin Nutr 2009;89:1799–807. 10.3945/ajcn.2008.27338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gast GCM, de Roos NM, Sluijs I, et al. A high menaquinone intake reduces the incidence of coronary heart disease. Nutr Metab Cardiovasc Dis 2009;19:504–10. 10.1016/j.numecd.2008.10.004 [DOI] [PubMed] [Google Scholar]
- 88.Nagata C, Wada K, Tamura T, et al. Dietary soy and natto intake and cardiovascular disease mortality in Japanese adults: the Takayama study. Am J Clin Nutr 2017;105:426–31. 10.3945/ajcn.116.137281 [DOI] [PubMed] [Google Scholar]
- 89.Theuwissen E, Cranenburg EC, Knapen MH, et al. Low-Dose menaquinone-7 supplementation improved extra-hepatic vitamin K status, but had no effect on thrombin generation in healthy subjects. Br J Nutr 2012;108:1652–7. 10.1017/S0007114511007185 [DOI] [PubMed] [Google Scholar]
- 90.Knapen MHJ, Braam LAJLM, Drummen NE, et al. Menaquinone-7 supplementation improves arterial stiffness in healthy postmenopausal women. A double-blind randomised clinical trial. Thromb Haemost 2015;113:1135–44. 10.1160/TH14-08-0675 [DOI] [PubMed] [Google Scholar]
- 91.Geleijnse JM, Vermeer C, Grobbee DE, et al. Dietary intake of menaquinone is associated with a reduced risk of coronary heart disease: the Rotterdam study. J Nutr 2004;134:3100–5. 10.1093/jn/134.11.3100 [DOI] [PubMed] [Google Scholar]
- 92.Dalmeijer GW, van der Schouw YT, Magdeleyns E, et al. The effect of menaquinone-7 supplementation on circulating species of matrix Gla protein. Atherosclerosis 2012;225:397–402. 10.1016/j.atherosclerosis.2012.09.019 [DOI] [PubMed] [Google Scholar]
- 93.Pucaj K, Rasmussen H, Møller M, et al. Safety and toxicological evaluation of a synthetic vitamin K2, menaquinone-7. Toxicol Mech Methods 2011;21:520–32. 10.3109/15376516.2011.568983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Braam LAJLM, Hoeks APG, Brouns F, et al. Beneficial effects of vitamins D and K on the elastic properties of the vessel wall in postmenopausal women: a follow-up study. Thromb Haemost 2004;91:373–80. 10.1160/TH03-07-0423 [DOI] [PubMed] [Google Scholar]
- 95.Vermeer C, Hogne V. Effect of Menaquinone-7 (vitamin K2) on vascular elasticity in healthy subjects: results from a one-year study. Vasc Dis Ther 2020;5:1–4. 10.15761/VDT.1000179 [DOI] [Google Scholar]
- 96.Ikari Y, Torii S, Shioi A, et al. Impact of menaquinone-4 supplementation on coronary artery calcification and arterial stiffness: an open label single arm study. Nutr J 2016;15:53. 10.1186/s12937-016-0175-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Della Rocca DG, Pepine CJ. Endothelium as a predictor of adverse outcomes. Clin Cardiol 2010;33:730. 10.1002/clc.20854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bar A, Kuś K, Manterys A. Vitamin K2-MK-7 improves nitric oxide-dependent endothelial function in ApoE/LDLR−/− mice. Vascul Pharmacol 2019;106581. [DOI] [PubMed] [Google Scholar]
- 99.Chłopicki S, Gryglewski RJ. Angiotensin converting enzyme (ACE) and hydroxymethylglutaryl-CoA (HMG-CoA) reductase inhibitors in the forefront of pharmacology of endothelium. Pharmacol Rep 2005;57 Suppl:86. [PubMed] [Google Scholar]
- 100.Vos M, Esposito G, Edirisinghe JN, et al. Vitamin K2 is a mitochondrial electron carrier that rescues PINK1 deficiency. Science 2012;336:1306–10. 10.1126/science.1218632 [DOI] [PubMed] [Google Scholar]
- 101.McFarlin BK, Henning AL, Venable AS. Oral consumption of vitamin K2 for 8 weeks associated with increased maximal cardiac output during exercise. Altern Ther Health Med 2017;23:26–32. [PubMed] [Google Scholar]
- 102.Beulens JW, Grobbee DE, Sluijs I. Spijkerman am and van der Schouw YT. dietary phylloquinone and menaquinones intakes and risk of type 2 diabetes. Diabetes Care 2010;33:1699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Choi HJ, Yu J, Choi H, et al. Vitamin K2 supplementation improves insulin sensitivity via osteocalcin metabolism: a placebo-controlled trial. Diabetes Care 2011;34:e147. 10.2337/dc11-0551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rennenberg RJMW, van Varik BJ, Schurgers LJ, et al. Chronic coumarin treatment is associated with increased extracoronary arterial calcification in humans. Blood 2010;115:5121–3. 10.1182/blood-2010-01-264598 [DOI] [PubMed] [Google Scholar]
- 105.Weijs B, Blaauw Y, Rennenberg RJMW, et al. Patients using vitamin K antagonists show increased levels of coronary calcification: an observational study in low-risk atrial fibrillation patients. Eur Heart J 2011;32:2555–62. 10.1093/eurheartj/ehr226 [DOI] [PubMed] [Google Scholar]
- 106.Sønderskov PS, Lindholt JS, Hallas J, et al. Association of aortic valve calcification and vitamin K antagonist treatment. Eur Heart J Cardiovasc Imaging 2020;21:718–24. 10.1093/ehjci/jeaa065 [DOI] [PubMed] [Google Scholar]
- 107.Brandenburg VM, Reinartz S, Kaesler N, et al. Slower progress of aortic valve calcification with vitamin K supplementation: results from a prospective interventional proof-of-concept study. Circulation 2017;135:2081–3. 10.1161/CIRCULATIONAHA.116.027011 [DOI] [PubMed] [Google Scholar]
- 108.De Vriese AS, Caluwé R, Pyfferoen L, et al. Multicenter randomized controlled trial of vitamin K antagonist replacement by rivaroxaban with or without vitamin K2 in hemodialysis patients with atrial fibrillation: the Valkyrie study. J Am Soc Nephrol 2020;31:186–96. 10.1681/ASN.2019060579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Oikonomaki T, Papasotiriou M, Ntrinias T, et al. The effect of vitamin K2 supplementation on vascular calcification in haemodialysis patients: a 1-year follow-up randomized trial. Int Urol Nephrol 2019;51:2037–44. 10.1007/s11255-019-02275-2 [DOI] [PubMed] [Google Scholar]
- 110.Zwakenberg SR, de Jong PA, Bartstra JW, et al. The effect of menaquinone-7 supplementation on vascular calcification in patients with diabetes: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr 2019;110:883–90. 10.1093/ajcn/nqz147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bartstra JW, Draaisma F, Zwakenberg SR, et al. Six months vitamin K treatment does not affect systemic arterial calcification or bone mineral density in diabetes mellitus 2. Eur J Nutr 2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Haugsgjerd TR, Egeland GM, Nygård OK, et al. Association of dietary vitamin K and risk of coronary heart disease in middle-age adults: the Hordaland health study cohort. BMJ Open 2020;10:e035953. 10.1136/bmjopen-2019-035953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Erkkilä AT, Booth SL, Hu FB, et al. Phylloquinone intake and risk of cardiovascular diseases in men. Nutr Metab Cardiovasc Dis 2007;17:58–62. 10.1016/j.numecd.2006.03.008 [DOI] [PubMed] [Google Scholar]
- 114.Juanola-Falgarona M, Salas-Salvadó J, Martínez-González Miguel Ángel, et al. Dietary intake of vitamin K is inversely associated with mortality risk. J Nutr 2014;144:743–50. 10.3945/jn.113.187740 [DOI] [PubMed] [Google Scholar]
- 115.Cheung C-L, Sahni S, Cheung BMY, et al. Vitamin K intake and mortality in people with chronic kidney disease from NHANES III. Clin Nutr 2015;34:235–40. 10.1016/j.clnu.2014.03.011 [DOI] [PubMed] [Google Scholar]
- 116.Vossen LM, Schurgers LJ, van Varik BJ, et al. Menaquinone-7 supplementation to reduce vascular calcification in patients with coronary artery disease: rationale and study protocol (VitaK-CAC trial). Nutrients 2015;7:8905–15. 10.3390/nu7115443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lindholt JS, Frandsen NE, Fredgart MH, et al. Effects of menaquinone-7 supplementation in patients with aortic valve calcification: study protocol for a randomised controlled trial. BMJ Open 2018;8:e022019. 10.1136/bmjopen-2018-022019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hauschka PV, Wians FH. Osteocalcin-hydroxyapatite interaction in the extracellular organic matrix of bone. Anat Rec 1989;224:180–8. 10.1002/ar.1092240208 [DOI] [PubMed] [Google Scholar]
- 119.Asemi Z, Raygan F, Bahmani F, et al. The effects of vitamin D, K and calcium co-supplementation on carotid intima-media thickness and metabolic status in overweight type 2 diabetic patients with CHD. Br J Nutr 2016;116:286–93. 10.1017/S0007114516001847 [DOI] [PubMed] [Google Scholar]
- 120.Kurnatowska I, Grzelak P, Masajtis-Zagajewska A, et al. Effect of vitamin K2 on progression of atherosclerosis and vascular calcification in nondialyzed patients with chronic kidney disease stages 3-5. Pol Arch Med Wewn 2015;125:631–40. 10.20452/pamw.3041 [DOI] [PubMed] [Google Scholar]
- 121.Zwakenberg SR, den Braver NR, Engelen AIP, et al. Vitamin K intake and all-cause and cause specific mortality. Clin Nutr 2017;36:1294–300. 10.1016/j.clnu.2016.08.017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study.



