Abstract
Introduction
Health disparities among racial and ethnic and socioeconomic groups are pervasive, and the COVID-19 pandemic has not been an exception. This study explores the key demographic and socioeconomic factors related to racial and ethnic disparities in COVID-19 vaccination coverage.
Methods
Using recent (January 2021–March 2021) data on adults from the U.S. Census Bureau Household Pulse Survey, a regression-based decomposition method was used to estimate how much of the observed racial and ethnic disparities in vaccination coverage could be explained by particular socioeconomic and demographic factors (i.e., age, number of children and adults in household).
Results
Demographics, socioeconomic factors, and experiencing economic hardship during the pandemic each explained a statistically significant portion of vaccination coverage disparities between non-Hispanic White and racial/ethnic minority individuals. The largest disparity was observed among people who identified as Hispanic or Latino, whose vaccination coverage was 8.0 (95% CI=7.1, 8.9) percentage points lower than that of their non-Hispanic White counterparts. Socioeconomic factors explained 4.8 (95% CI=4.3, 5.2) percentage points of this disparity, and economic hardship explained an additional 1.4 (95% CI=1.2, 1.6) percentage points.
Conclusions
This paper identified the key factors related to racial and ethnic disparities in adult vaccination coverage. The variables that explained the largest portions of the disparities were age, education, employment, and income. The study findings can help to inform efforts to increase equitable vaccine access and engage various segments of the population to prevent the further exacerbation of COVID-19 health disparities.
INTRODUCTION
Health inequities observed across racial and ethnic minority groups, such as differences in the rates of chronic disease, arise from differential access to health care and other social determinants of health, which themselves are driven by interpersonal and structural racism.1 , 2 In the U.S., racial and ethnic disparities in healthcare utilization and health outcomes have been well documented,3 , 4 and recent studies have observed racial and ethnic disparities in infections, hospitalizations, mortality, and vaccination coverage during the coronavirus disease 2019 (COVID-19) pandemic.5
In the U.S., SES varies substantially by race, with non-Hispanic Black or African American only (Black), Hispanic or Latino of any race (Hispanic), and non-Hispanic people of other or multiple races (other/multiple) having on average lower levels of household income, educational attainment, and residential stability than non-Hispanic White only (White) and non-Hispanic Asian only (Asian) individuals.6 These differences and their impact on healthcare access may magnify health disparities during the COVID-19 pandemic.7 Numerous studies have documented higher COVID-19 incidence and mortality and lower vaccination coverage for populations with lower SES levels.8, 9, 10, 11 Others have documented disproportionate economic hardship, such as loss of income, loss of health insurance, food insufficiency, and housing instability, among racial/ethnic minority groups during the pandemic.12 , 13 Beyond access to health care, worsened outcomes may have arisen owing to racial and ethnic minority groups’ higher likelihood of living in densely populated areas, living in multigenerational households, having jobs that cannot be performed remotely, using public transit, experiencing language barriers, and having underlying chronic conditions.3 , 4
Cultural differences and historical health policies also lead to differences in attitudes and healthcare-seeking behaviors across racial and ethnic groups. Black and Hispanic people were recently found to have lower levels of knowledge of COVID-19 transmission pathways, symptoms, and mitigation techniques than White people.14 Harmful historical health policies, such as the Tuskegee syphilis study, which left Black men with known syphilis infections untreated, have had longstanding impacts on medical mistrust and mortality among Black Americans.15 , 16 This and other historical abuses, such as forced sterilization policies in the U.S. and Puerto Rico, have resulted in modern-day medical mistrust among disproportionately affected communities.17
This paper quantifies the extent to which disparities in U.S. adult vaccination coverage are explained by racial/ethnic differences in demographics (age, number of children and adults in household), socioeconomic factors (income, education, employment, health insurance status), and economic hardship during the pandemic. The study period, January 2021–March 2021, reflects a period of constrained vaccine supply that may have exacerbated disparities. Although other studies have documented associations between socioeconomic factors, race/ethnicity, and COVID-19 vaccination,11 , 18 this analysis estimates how much of the disparity between racial and ethnic groups is predicted by each factor. This study aims to uncover the key variables associated with vaccination disparities and how they vary across groups. Analyzing the impact of socioeconomic factors and economic hardship during the pandemic identifies factors that may be contributing to the exacerbation of health inequalities. The findings can inform public health strategies to increase COVID-19 vaccination uptake among racial and ethnic minority groups by determining the most important reasons for racial/ethnic disparities in vaccine coverage.
METHODS
Study Population
Study data came from the U.S. Census Bureau Household Pulse Survey (HPS), a collaboration between multiple agencies to collect data on the social and economic impacts of households during the COVID-19 pandemic. Data are collected and released on a biweekly basis and were designed to be representative of the U.S. adult population. Waves 22–27 of the HPS, collected from January 6, 2021 to March 29, 2021, were combined for this analysis. To account for the complex survey design, point estimates were weighted using person-level probability weights, and CIs were calculated using the replicate weights provided in the HPS data. The replicate and probability weights were divided by 6 because 6 waves of the data were pooled.19
Measures
Starting in Wave 22, HPS asked respondents whether they received a COVID-19 vaccine and, among those who had not yet received a vaccine, whether they intended to receive a vaccine (more details are provided in Appendix Table 1, available online). Explanatory variables included demographic factors, socioeconomic factors, and economic hardship during the COVID-19 pandemic. Demographic factors included race/ethnicity, age, number of adults in the household, and number of children in the household. Socioeconomic indicators included household income, education, employment, and whether an individual had any health insurance coverage.
Indicators of economic hardship during the pandemic were included to account for the economic burden that may have temporarily been induced by the pandemic. They allow investigators to test whether those most disproportionately impacted by the economic consequences of the pandemic may also be less likely to receive a vaccination. These indicators included receiving Supplemental Nutrition Assistance Program (SNAP) benefits, receiving unemployment insurance, receiving a stimulus check, lost income during the pandemic, and food sufficiency.
If unvaccinated respondents indicated anything other than definitely intending to get a COVID-19 vaccine, HPS asked a series of questions about reasons why they may choose not to. Respondents could indicate any number of reasons from the following list: concerns about side effects, not knowing whether the vaccine will work, believing that they do not need a vaccine, not liking vaccines, a doctor has not recommended it, they plan to wait and see whether it is safe, thinking that other people need it more right now, concerns about the cost of a COVID-19 vaccine, not trusting COVID-19 vaccines, and not trusting the government.
Statistical Analysis
A variant of a regression-based method known as Oaxaca–Blinder decomposition was used to estimate how much of the disparity in vaccination coverage between racial and ethnic minority and non-Hispanic White respondents was predicted by differences in their underlying characteristics.20 Vaccination coverage was defined as the percentage of respondents who had already received at least 1 dose of a COVID-19 vaccine. Decomposition methods originated in the economics literature to measure wage inequalities,21 , 22 and they have been adopted by health researchers for studying health disparities.23 , 24
At a high level, the decomposition method works by predicting how vaccination coverage between a racial/ethnic group and the White group would change if the levels of the explanatory variables of the minority group were the same as those of the White group. Predicted, or explained, differences were the differences in vaccination coverage one would predict or expect to find on the basis of racial/ethnic differences in factors included in the model. A negative-explained difference means that one would expect vaccination coverage in the racial/ethnic minority group to be lower than that in the White group on the basis of the explanatory factors alone. Differences between the explained and actual disparities indicate how much of the actual disparity cannot be explained by the explanatory factors included in the model. Explained/predicted disparities may be larger in magnitude than the actual disparities; this would indicate that actual disparities are smaller than expected on the basis of the explanatory variables alone and that other factors outside of the model are helping to decrease disparities.
A pooled logistic regression over all racial and ethnic groups was estimated first. The regressions were weighted using the person-level probability weights provided in the HPS data. Decompositions were then calculated between the reference group (White) and each racial and ethnic minority group, for a total of 4 pairwise comparisons. The pooled regression coefficients were used to predict the change in the outcome variable if the comparison group had the same explanatory variable distribution as the reference group. Using the strategy proposed by Yun,25 a detailed decomposition was then calculated to assess how much each individual explanatory variable contributed to the total explained portion. An analogous way to estimate the difference between actual and explained disparities would be to calculate the differences in adjusted prevalence between racial/ethnic groups after estimating the logistic regression. However, this would not provide the detailed decomposition results of interest. All analyses used the replicate weights from the HPS data to account for complex survey design when calculating CIs. Additional details are available in the Appendix (available online).
For ease of presentation and interpretation, results for some similar factors were aggregated. For example, all income levels were summed and presented as 1 income effect. Higher levels of aggregation were also calculated, such as the total of all socioeconomic factors combined. As a sensitivity analysis, the same decomposition analysis on the subsample of respondents aged ≥65 years, who were more likely to be eligible during the study period, was conducted. Furthermore, to better understand the differences between actual and explained disparities, analyses of racial and ethnic differences in vaccination intentions and reasons for not getting a COVID-19 vaccine were conducted.
RESULTS
The estimation sample for the vaccination coverage outcome included 340,046 respondents with nonmissing data collected during January 6, 2021–March 29, 2021. Overall, a weighted 25.1% of these respondents had already received at least 1 dose of a vaccine (Table 1 ). On average, racial and ethnic minority respondents were younger and had larger household sizes than White respondents. Asian and White respondents had higher rates of health insurance coverage, income, and education than Black, Hispanic, and other/multiple respondents. Similarly, White and Asian respondents were less likely to face economic hardship during the pandemic: they had the lowest levels of SNAP benefits and lost income during the pandemic, and they had the highest levels of food sufficiency.
Table 1.
Characteristics of the Study Population by Race and Ethnicity
| Racial/ethnic groupa | Hispanic, | Asian, | Black, | Other/ multiple, | White, | Overall, |
|---|---|---|---|---|---|---|
| %b (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Outcome | ||||||
| Vaccination coverage | 18.87 (18.11, 19.64) |
29.97 (28.91, 31.04) |
21.40 (20.52, 22.28) |
21.72 (20.44, 22.99) |
26.87 (26.55, 27.18) |
25.07 (24.79, 25.35) |
| Demographic variables | ||||||
| Ages 18–34 years | 32.70 (31.75, 33.65) |
29.91 (28.72, 31.09) |
19.98 (19.08, 20.88) |
27.18 (25.87, 28.48) |
21.62 (21.35, 21.89) |
23.74 (23.50, 23.99) |
| Age 35–49 years | 31.69 (30.86, 32.52) |
29.98 (29.12, 30.84) |
32.03 (30.87, 33.18) |
31.49 (29.95, 33.04) |
24.04 (23.88, 24.20) |
26.57 (26.35, 26.80) |
| Ages 50–64 years | 23.69 (22.81, 24.57) |
25.02 (23.94, 26.10) |
31.22 (30.21, 32.23) |
24.86 (23.66, 26.05) |
27.68 (27.47, 27.89) |
27.21 (26.98, 27.43) |
| Ages ≥65 years | 11.92 (11.33, 12.51) |
15.09 (14.31, 15.87) |
16.77 (16.15, 17.38) |
16.47 (15.11, 17.84) |
26.65 (26.46, 26.84) |
22.48 (22.29, 22.66) |
| 1 adultc | 7.24 (6.73, 7.76) |
6.97 (6.39, 7.55) |
15.62 (14.51, 16.72) |
10.73 (9.74, 11.72) |
11.04 (10.72, 11.36) |
10.72 (10.36, 11.08) |
| 2 adultsc | 37.43 (36.22, 38.65) |
41.15 (39.58, 42.72) |
41.10 (40.05, 42.15) |
43.83 (41.86, 45.79) |
55.55 (55.09, 56.01) |
50.21 (49.67, 50.74) |
| ≥3 adultsc | 55.32 (53.88, 56.76) |
51.88 (50.03, 53.73) |
43.28 (41.59, 44.97) |
45.44 (43.06, 47.82) |
33.41 (32.69, 34.12) |
39.07 (38.23, 39.92) |
| 0 childrenc | 50.06 (48.94, 51.18) |
58.57 (56.87, 60.27) |
54.98 (53.89, 56.07) |
56.32 (54.17, 58.48) |
68.27 (67.94, 68.61) |
63.26 (62.89, 63.62) |
| 1 childc | 20.95 (19.90, 21.99) |
20.00 (18.73, 21.27) |
21.26 (20.24, 22.27) |
19.88 (18.24, 21.52) |
15.20 (14.93, 15.46) |
17.09 (16.84, 17.34) |
| 2 childrenc | 16.62 (15.79, 17.45) |
15.37 (14.27, 16.47) |
12.99 (12.26, 13.72) |
13.37 (12.20, 14.54) |
10.84 (10.64, 11.03) |
12.24 (12.01, 12.48) |
| ≥3 childrenc | 12.37 (11.51, 13.24) |
6.06 (5.30, 6.81) |
10.78 (9.82, 11.73) |
10.43 (9.24, 11.61) |
5.69 (5.49, 5.89) |
7.41 (7.20, 7.61) |
| Socioeconomic factors | ||||||
| Health insurance | 80.44 (79.51, 81.37) |
93.47 (92.57, 94.37) |
88.28 (87.36, 89.19) |
87.49 (86.31, 88.67) |
93.48 (93.27, 93.69) |
90.77 (90.51, 91.03) |
| Income <$25,000 | 21.75 (20.71, 22.79) |
10.65 (9.65, 11.65) |
24.27 (23.26, 25.28) |
18.47 (17.17, 19.77) |
11.06 (10.82, 11.29) |
14.26 (14.01, 14.52) |
| Income $25,000–$34,999 | 15.50 (14.49, 16.51) |
8.74 (7.68, 9.80) |
15.21 (14.21, 16.21) |
12.11 (11.01, 13.20) |
9.52 (9.28, 9.76) |
11.05 (10.83, 11.27) |
| Income $35,000–$49,999 | 16.42 (15.51, 17.34) |
10.44 (9.35, 11.52) |
14.68 (13.93, 15.43) |
13.80 (12.43, 15.16) |
11.77 (11.53, 12.02) |
12.78 (12.55, 13.01) |
| Income $50,000–$74,999 | 18.76 (17.86, 19.66) |
14.22 (13.16, 15.29) |
17.66 (16.85, 18.47) |
17.98 (16.73, 19.24) |
18.43 (18.10, 18.76) |
18.18 (17.90, 18.45) |
| Income $75,000–$99,999 | 10.49 (9.84, 11.14) |
12.18 (11.16, 13.21) |
10.09 (9.53, 10.65) |
13.65 (12.30, 14.99) |
14.45 (14.19, 14.70) |
13.26 (13.04, 13.49) |
| Income $100,000–$149,999 | 9.60 (9.10, 10.10) |
17.82 (16.72, 18.93) |
10.55 (9.82, 11.28) |
12.66 (11.73, 13.59) |
17.46 (17.17, 17.74) |
15.42 (15.20, 15.63) |
| Income $150,000–$199,999 | 3.82 (3.52, 4.13) |
10.01 (9.27, 10.75) |
4.21 (3.75, 4.66) |
5.56 (4.91, 6.21) |
8.16 (8.01, 8.32) |
7.11 (6.98, 7.23) |
| Income ≥$200,000 | 3.65 (3.25, 4.05) |
15.94 (14.97, 16.90) |
3.33 (3.05, 3.62) |
5.77 (4.91, 6.63) |
9.15 (8.95, 9.35) |
7.95 (7.79, 8.10) |
| Education: less than high school | 6.84 (6.21, 7.47) |
2.81 (2.03, 3.59) |
1.66 (1.20, 2.12) |
2.69 (1.87, 3.50) |
1.16 (1.01, 1.31) |
2.21 (2.09, 2.32) |
| Education: some high school | 12.95 (12.12, 13.78) |
4.57 (3.59, 5.55) |
6.17 (5.43, 6.91) |
4.14 (3.34, 4.94) |
2.72 (2.55, 2.89) |
4.76 (4.57, 4.94) |
| Education: high school graduate or equivalent | 31.04 (29.90, 32.18) |
13.40 (12.17, 14.62) |
32.37 (30.90, 33.84) |
30.39 (28.63, 32.16) |
28.07 (27.74, 28.40) |
28.30 (28.02, 28.59) |
| Education: some college | 20.50 (19.71, 21.29) |
14.88 (13.89, 15.86) |
22.36 (21.48, 23.24) |
24.12 (22.70, 25.54) |
20.79 (20.55, 21.03) |
20.73 (20.55, 20.91) |
| Education: associate degree | 8.73 (8.19, 9.28) |
7.12 (6.41, 7.84) |
10.32 (9.60, 11.03) |
10.72 (9.89, 11.55) |
10.10 (9.92, 10.28) |
9.79 (9.64, 9.94) |
| Education: bachelor's degree | 12.25 (11.77, 12.73) |
29.19 (28.19, 30.18) |
14.08 (13.46, 14.70) |
16.26 (15.28, 17.24) |
20.81 (20.61, 21.02) |
19.09 (18.92, 19.26) |
| Education: graduate degree | 7.69 (7.30, 8.07) |
28.05 (26.83, 29.27) |
13.04 (12.35, 13.73) |
11.68 (10.96, 12.40) |
16.35 (16.16, 16.54) |
15.12 (14.96, 15.28) |
| Employment: government | 8.37 (7.88, 8.86) |
8.36 (7.68, 9.04) |
12.24 (11.51, 12.97) |
10.61 (9.53, 11.69) |
8.17 (7.99, 8.35) |
8.71 (8.54, 8.89) |
| Employment: private company | 35.89 (34.83, 36.96) |
40.58 (39.19, 41.97) |
29.82 (28.75, 30.88) |
33.33 (32.05, 34.61) |
35.60 (35.21, 35.98) |
35.22 (34.87, 35.57) |
| Employment: nonprofit organization | 4.48 (4.16, 4.80) |
6.72 (6.19, 7.26) |
6.81 (6.24, 7.39) |
5.50 (4.85, 6.15) |
6.31 (6.17, 6.46) |
6.08 (5.94, 6.21) |
| Employment: self-employed | 6.29 (5.80, 6.78) |
6.41 (5.57, 7.25) |
4.13 (3.70, 4.56) |
6.02 (5.27, 6.78) |
6.73 (6.52, 6.94) |
6.36 (6.19, 6.52) |
| Employment: family business | 2.06 (1.66, 2.46) |
1.43 (1.08, 1.77) |
0.91 (0.63, 1.18) |
1.40 (0.90, 1.90) |
1.35 (1.24, 1.46) |
1.42 (1.32, 1.52) |
| Employment: unemployed | 32.68 (31.65, 33.72) |
25.59 (24.13, 27.05) |
29.77 (28.43, 31.10) |
28.18 (26.30, 30.07) |
18.61 (18.28, 18.93) |
22.56 (22.27, 22.85) |
| Employment: sick/disability | 2.30 (1.98, 2.62) |
1.04 (0.74, 1.33) |
3.93 (3.35, 4.51) |
4.63 (3.85, 5.41) |
2.66 (2.52, 2.80) |
2.72 (2.61, 2.84) |
| Employment: retired | 7.93 (7.37, 8.48) |
9.86 (9.08, 10.65) |
12.39 (11.74, 13.05) |
10.32 (9.40, 11.25) |
20.58 (20.32, 20.83) |
16.93 (16.71, 17.15) |
| Economic hardship during the pandemic | ||||||
| Trouble paying household expenses | 32.70 (31.75, 33.65) |
29.91 (28.72, 31.09) |
19.98 (19.08, 20.88) |
27.18 (25.87, 28.48) |
21.62 (21.35, 21.89) |
23.74 (23.50, 23.99) |
| Received SNAP benefits | 17.21 (16.12, 18.30) |
7.83 (6.78, 8.88) |
25.25 (24.29, 26.21) |
17.19 (15.82, 18.57) |
7.62 (7.37, 7.86) |
11.21 (10.97, 11.46) |
| Received unemployment insurance | 19.40 (18.55, 20.26) |
16.67 (15.42, 17.92) |
19.54 (18.34, 20.74) |
17.75 (16.48, 19.03) |
14.11 (13.85, 14.37) |
15.72 (15.44, 16.00) |
| Received a stimulus check | 62.46 (61.43, 63.50) |
54.97 (53.60, 56.33) |
58.57 (57.26, 59.88) |
56.36 (54.63, 58.10) |
52.43 (52.01, 52.84) |
54.83 (54.46, 55.21) |
| Lost income during pandemic | 59.54 (58.58, 60.50) |
44.45 (42.96, 45.94) |
52.76 (51.49, 54.03) |
56.48 (54.65, 58.31) |
41.95 (41.59, 42.31) |
46.35 (46.01, 46.70) |
| Food sufficiency | 82.49 (81.48, 83.50) |
94.61 (93.97, 95.25) |
80.74 (79.80, 81.68) |
83.74 (82.53, 84.96) |
92.95 (92.75, 93.16) |
89.88 (89.63, 90.13) |
Racial and ethnic groups include Hispanic or Latino (Hispanic), non-Hispanic Asian alone (Asian), non-Hispanic Black or African American alone (Black), non-Hispanic persons of other or multiple races (other/multiple), and non-Hispanic White alone (White).
Weighted percentages were calculated using person-level probability weights. CIs were calculated using replicate weights.
Refers to the number of adults or children in the respondent's household.
SNAP, Supplemental Nutrition Assistance Program.
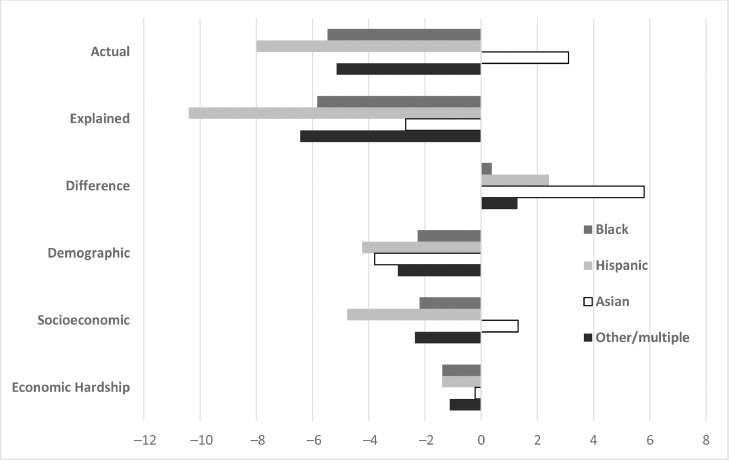
Compared with the White group, all racial and ethnic minority groups except for the Asian group had lower actual levels of vaccination coverage (Table 2 and Figure 1 ). The largest disparity was with the Hispanic group, whose vaccination coverage was 8.0 (95% CI=7.1, 8.9) percentage points lower than that for White respondents.
Table 2.
Vaccination Coverage Decomposition Results
| Racial/ethnic groupa | Black, | Hispanic, | Asian, | Other/multiple, |
|---|---|---|---|---|
| PPb (95% CI) | PP (95% CI) | PP (95% CI) | PP (95% CI) | |
| Actual difference | −5.47 (−6.46, −4.47) | −7.99 (−8.88, −7.10) | 3.11 (1.76, 4.45) | −5.15 (−6.69, −3.60) |
| Explained difference | −5.84 (−6.33, −5.36) | −10.40 (−10.89, −9.91) | −2.69 (−3.23, −2.15) | −6.44 (−7.08, −5.80) |
| Difference between actual and explained | 0.37 (−0.59, 1.34) |
2.41 (1.34, 3.47) |
5.80 (4.52, 7.08) |
1.29 (−0.20, 2.79) |
| Detailed decomposition | ||||
| Demographics | ||||
| Total | −2.26 (−2.52, −2.01) | −4.23 (−4.54, −3.93) | −3.79 (−4.12, −3.46) | −2.97 (−3.41, −2.53) |
| Age | −1.81 (−2.03, −1.58) | −3.57 (−3.83, −3.30) | −3.42 (−3.73, −3.11) | −2.52 (−2.95, −2.08) |
| Household size | −0.46 (−0.58, −0.33) | −0.67 (−0.85, −0.48) | −0.36 (−0.53, −0.20) | −0.45 (−0.59, −0.32) |
| Socioeconomic factors | ||||
| Total | −2.19 (−2.55, −1.84) | −4.77 (−5.20, −4.34) | 1.31 (0.81, 1.81) | −2.35 (−2.76, −1.95) |
| Health insurance | −0.37 (−0.48, −0.26) | −0.94 (−1.15, −0.73) | 0.00 (−0.09, 0.09) | −0.45 (−0.59, −0.32) |
| Income | −0.84 (−1.04, −0.63) | −0.79 (−0.98, −0.59) | 0.26 (0.14, 0.37) | −0.51 (−0.64, −0.37) |
| Education | −0.75 (−0.89, −0.60) | −1.65 (−1.98, −1.32) | 1.64 (1.35, 1.94) | −0.66 (−0.84, −0.49) |
| Employment | −0.24 (−0.44, −0.03) | −1.39 (−1.59, −1.19) | −0.59 (−0.84, −0.34) | −0.73 (−1.03, −0.43) |
| Hardship during pandemic | ||||
| Total | −1.39 (−1.68, −1.09) | −1.40 (−1.64, −1.15) | −0.21 (−0.32, −0.11) | −1.12 (−1.34, −0.89) |
| Trouble paying household expenses | −0.50 (−0.65, −0.35) | −0.53 (−0.70, −0.37) | −0.17 (−0.23, −0.11) | −0.41 (−0.54, −0.28) |
| Received SNAP benefits | −0.28 (−0.50, −0.05) | −0.15 (−0.28, −0.03) | 0.00 (−0.03, 0.02) | −0.16 (−0.29, −0.03) |
| Received unemployment insurance | −0.01 (−0.06, 0.03) | −0.01 (−0.06, 0.03) | −0.01 (−0.04, 0.02) | −0.01 (−0.05, 0.03) |
| Received a stimulus check | −0.11 (−0.15, −0.07) | −0.18 (−0.24, −0.13) | −0.06 (−0.10, −0.02) | −0.08 (−0.12, −0.03) |
| Lost income during pandemic | −0.11 (−0.18, −0.04) | −0.19 (−0.30, −0.08) | −0.03 (−0.06, 0.00) | −0.16 (−0.26, −0.06) |
| Food sufficiency | −0.37 (−0.54, −0.20) | −0.32 (−0.47, −0.17) | 0.06 (0.02, 0.10) | −0.30 (−0.44, −0.16) |
Note: Boldface indicates statistical significance (p<0.05).
Racial and ethnic groups include Hispanic or Latino (Hispanic), non-Hispanic Asian alone (Asian), non-Hispanic Black or African American alone (Black), non-Hispanic persons of other or multiple races (other/multiple), and non-Hispanic White alone (White).
PP difference between racial/ethnic minority group and White group. Weighted percentages were calculated using person-level probability weights. CIs were calculated using replicate weights. Actual differences reflect the weighted difference in the outcome variable between the racial and ethnic minority group and White respondents. Explained differences are the differences predicted on the basis of explanatory variables alone. The detailed decomposition shows how much of the explained disparity is because of each explanatory variable.
PP, percentage point; SNAP, Supplemental Nutrition Assistance Program.
Figure 1.
Racial and ethnic vaccination coverage disparities: actual, explained, and by category.
Note: Non-Hispanic White alone is the comparison group. Explained disparities are the predicted differences on the basis of explanatory variables alone. Racial and ethnic minority groups include Hispanic or Latino (Hispanic), non-Hispanic Asian alone (Asian), non-Hispanic Black or African American alone (Black), non-Hispanic persons of other or multiple races (other/multiple). Actual differences reflect the weighted difference in the outcome variable between White respondents and the racial and ethnic minority group. Explained disparities are the differences predicted on the basis of explanatory variables alone. The detailed decomposition shows how much of the explained disparity is because of each explanatory variable.
Age explained between 1.8 (Black, 95% CI=1.6, 2.0) and 3.6 (Hispanic, 95% CI=3.3, 3.8) percentage points of the disparity across the racial and ethnic minority groups. Socioeconomic factors also explained a large proportion of the disparities for the Black, Hispanic, and other/multiple groups (Table 2). For example, health insurance status, income, education, and employment together explained a 4.8 (95% CI=4.3, 5.2) percentage point disparity for Hispanic respondents. Hardship during the pandemic explained a significant but smaller portion of the disparities. The hardship factors combined explained 1.4 (95% CI=1.1, 1.7) percentage points of the Black disparity and 1.4 (95% CI=1.2, 1.6) percentage points of the Hispanic disparity. Higher proportions having trouble in paying expenses during the pandemic and food insufficiency explained 0.5 (95% CI=0.4, 0.7) and 0.4 (95% CI=0.2, 0.5) percentage point disparities in vaccine coverage, respectively.
Explained disparities or the size of the disparity predicted by the explanatory factors alone were similar in magnitude to actual disparities for the Black and other/multiple groups. Actual disparities were 2.4 (95% CI=1.3, 3.5) and 5.8 (95% CI=4.5, 7.1) percentage points lower than explained disparities for the Hispanic and Asian groups, respectively. When the analysis was restricted to respondents aged ≥65 years, actual disparities decreased in magnitude for all groups except for other/multiple, which increased to 12.5 (95% CI=7.8, 17.2) percentage points (Appendix Table 3, available online). Explained disparities decreased for all groups, and the size of the decrease was similar to the age effect from Table 2.
Data on vaccination intentions and reasons for not getting a vaccine by race were analyzed to describe additional factors related to vaccination outside of the decomposition model (Table 3 and Appendix Figures 1 and 2, available online). Hispanic and Asian respondents had higher levels of endorsing vaccination (vaccinated or definitely will get vaccinated) than their Black and other/multiple counterparts. However, Black and other/multiple respondents had the highest proportion of those who were undecided about getting vaccinated (probably will or probably will not get vaccinated).
Table 3.
Intention to Get a COVID-19 Vaccine and Reasons for Not Getting Vaccinated by Race and Ethnicity
| Racial/ethnic groupa | Hispanic | Asian | Black | Other/ multiple | White | Overall |
|---|---|---|---|---|---|---|
| Sample size,b unweighted n (weighted %c) | ||||||
| Total | 29,343 | 15,361 | 21,505 | 11,638 | 262,217 | 340,064 |
| Vaccinated | 7,799 (18.87) | 5,212 (29.97) | 6,106 (21.40) | 3,384 (21.72) | 90,264 (26.87) | 112,765 (25.07) |
| Definitely will get vaccine | 12,328 (42.72) | 7,499 (49.62) | 6,801 (30.17) | 4,101 (34.45) | 111,717 (41.65) | 142,446 (40.78) |
| Probably will get vaccine | 5,151 (22.42) | 1,942 (15.22) | 4,457 (23.47) | 1,849 (18.98) | 29,463 (14.47) | 42,862 (16.79) |
| Probably not get vaccine | 2,355 (9.16) | 499 (3.40) | 2,630 (14.82) | 1,203 (13.35) | 17,719 (9.39) | 24,406 (9.75) |
| Definitely not get vaccine | 1,710 (6.82) | 209 (1.76) | 1,511 (10.12) | 1,101 (11.47) | 13,054 (7.60) | 17,585 (7.58) |
| Vaccine endorsersd | 20,127 (61.59) | 12,711 (79.59) | 12,907 (51.57) | 201,981 (68.51) | 7,485 (56.16) | 255,211 (65.85) |
| Undecidede | 7,506 (31.58) | 2,441 (18.62) | 7,087 (38.29) | 3,052 (32.33) | 47,182 (23.86) | 67,268 (26.54) |
| Reasons for not getting a COVID-19 vaccine,f weighted % (95% CI) | ||||||
| Concerns about side effects | 51.29 (49.19, 53.39) |
52.78 (49.71, 55.86) |
53.49 (51.65, 55.32) |
55.36 (52.49, 58.22) |
49.86 (49.07, 50.66) |
50.97 (50.41, 51.53) |
| Not knowing whether vaccine will work | 20.35 (18.96, 21.73) |
19.05 (16.16, 21.93) |
20.14 (18.61, 21.67) |
23.61 (21.29, 25.92) |
19.33 (18.81, 19.86) |
19.81 (19.37, 20.24) |
| Believing that they do not need a vaccine | 8.92 (7.88, 9.97) |
8.04 (5.99, 10.08) |
8.14 (7.18, 9.10) |
18.16 (16.10, 20.22) |
17.00 (16.36, 17.65) |
14.14 (13.68, 14.59) |
| Not liking vaccines | 7.57 (6.65, 8.48) |
6.15 (4.22, 8.09) |
9.34 (8.45, 10.23) |
13.34 (10.91, 15.76) |
9.36 (8.89, 9.84) |
9.14 (8.72, 9.56) |
| Doctor has not recommended | 5.70 (4.95, 6.45) |
3.69 (2.57, 4.82) |
7.65 (6.71, 8.59) |
10.03 (8.65, 11.41) |
6.96 (6.55, 7.36) |
6.88 (6.59, 7.18) |
| Plan to wait and see | 48.69 (46.53, 50.86) |
54.10 (51.13, 57.06) |
53.33 (51.56, 55.09) |
48.02 (45.51, 50.54) |
45.78 (45.06, 46.50) |
47.72 (47.07, 48.38) |
| Other people need it more | 29.53 (28.02, 31.03) |
31.39 (28.24, 34.55) |
18.16 (16.78, 19.55) |
29.73 (27.47, 31.99) |
31.92 (31.21, 32.63) |
29.42 (28.94, 29.90) |
| Concerns about cost | 11.11 (9.73, 12.49) |
10.12 (8.28, 11.96) |
6.33 (5.45, 7.21) |
9.93 (8.22, 11.63) |
6.88 (6.45, 7.30) |
7.75 (7.30, 8.21) |
| Not trusting COVID-19 vaccines | 17.48 (16.00, 18.95) |
9.66 (7.88, 11.43) |
24.57 (23.03, 26.11) |
25.15 (22.89, 27.41) |
21.96 (21.35, 22.58) |
21.34 (20.83, 21.84) |
| Not trusting the government | 15.64 (14.35, 16.92) |
6.06 (4.74, 7.39) |
18.03 (16.75, 19.30) |
23.57 (21.75, 25.39) |
20.76 (20.18, 21.33) |
19.17 (18.69, 19.64) |
Racial and ethnic groups include Hispanic or Latino (Hispanic), non-Hispanic Asian alone (Asian), non-Hispanic Black or African American alone (Black), non-Hispanic persons of other or multiple races (other/multiple), and non-Hispanic White alone (White).
Sample sizes are for the pooled logistic regression estimation sample and do not include respondents with missing explanatory variables.
Weighted percentages were calculated using person-level probability weights. CIs were calculated using replicate weights.
The vaccine endorsers sample includes respondents who are vaccinated or say that they definitely will get a COVID-19 vaccine.
The undecided sample includes respondents who said that they probably will or probably will not get a COVID-19 vaccine.
Responses for reasons for not getting a COVID-19 vaccine are restricted to those who say that they probably will, probably will not, or definitely will not get a COVID-19 vaccine.
Among respondents who were not already vaccinated or were definitely planning to get vaccinated, Asian and Hispanic respondents were less likely to report believing that they do not need a vaccine, not trusting COVID-19 vaccines, and not trusting the government when than White respondents (Appendix Figure 2, available online). Black and other/multiple respondents were more likely than White respondents to report concerns about side effects and not trusting COVID-19 vaccines.
DISCUSSION
This analysis highlighted the factors that were key for predicting racial and ethnic disparities in vaccination coverage and intent. The use of a decomposition method allowed the authors to estimate how much of the disparities were associated with underlying differences in explanatory factors. Vaccination coverage was lower for all racial and ethnic minority groups than for the White group, except for the Asian group. Hispanic, Black, and other/multiple respondents had a relatively large proportion of respondents who were undecided (probably will or probably will not get vaccinated), which suggests that there is an opportunity to increase vaccine confidence and uptake in these groups.
Differences in age distributions explained a 3.6 (95% CI=3.3, 3.8) percentage point difference in vaccination coverage between Hispanic and White respondents. If the age distribution was equivalent between these 2 groups, the model would predict reported vaccination coverage among Hispanic respondents to be 3.6 percentage points higher. COVID-19 vaccination eligibility was extended to older populations first, and racial and ethnic minority respondents were younger on average (Table 1). Thus, jurisdictions with younger populations should expect lower levels of vaccination coverage regardless of socioeconomic or discriminatory barriers to access.
Differences in health insurance status, income, education, and employment explained a large portion of the disparity in vaccination coverage between Hispanic and White respondents. Health insurance alone accounted for a 0.9 (95% CI=0.7, 1.2) percentage point disparity. In other words, if Hispanic respondents had 13 percentage points–higher health insurance coverage to match that of White respondents, then the model would predict an additional 1% higher vaccination coverage among Hispanic respondents. Lack of insurance may decrease willingness to get vaccinated because of unfamiliarity with the healthcare system or lack of knowledge that vaccines will be provided at no cost.
Differences between the actual disparities and those explained by the model may indicate that factors outside of the variables included in the model are important drivers of disparities. These differences highlight where knowledge gaps persist, which may be useful to policymakers. Even among those aged ≥65 years, who were more likely to be eligible for the vaccine during the early rollout period, significant unexplained disparities remained for the Asian and other/multiple groups. The analysis of vaccination intentions and reasons for not getting the vaccine helped to fill in this gap and highlighted some of the key factors to focus on when trying to increase vaccine confidence in the population and within specific racial and ethnic groups. For the Black and other/multiple groups, clear and accurate messaging about COVID-19 vaccines from community leaders may increase trust in COVID-19 vaccines and alleviate concerns about side effects, which could increase vaccine confidence.
The findings show that socioeconomic factors remain tightly linked to access to health care, including COVID-19 vaccinations. Hispanic people face substantial socioeconomic barriers and had the lowest vaccination coverage, but they had the second-highest proportion of those who definitely will or probably will get vaccinated. Long-term policies that reduce disparities in underlying socioeconomic factors may help to reduce future healthcare disparities. In the short term, public health efforts that increase vaccine access in areas with low SES levels or address barriers for this population such as time off work and child care may help bridge the gap. The key drivers of disparities identified in this paper can be used to tailor messaging to each racial and ethnic group in a way that corrects vaccination misconceptions. They can also be used to engage healthcare personnel and community leaders to ensure that they are empathetic to and better understand the root causes of common concerns and barriers to vaccination.
Some studies have shown that COVID-19 disparities decrease after controlling for socioeconomic or other factors.26 However, racial and ethnic disparities are interconnected with socioeconomic and cultural factors that have resulted from historical inequities. Documenting that a portion of a disparity can be explained by differences in education or income does not minimize the role of racial or ethnic discrimination in leading to that disparity because historical discrimination has itself contributed to those differences in income and educational distributions.
Limitations
This analysis comes with several limitations. First, the decomposition methodology is descriptive, not causal in nature, and should be interpreted as such. For example, higher levels of both food insufficiency and receiving SNAP benefits significantly explain portions of the Black disparities in vaccine coverage. This is not to say that eliminating SNAP benefits would decrease disparities; rather, receiving SNAP benefits is likely a proxy for economic hardship beyond what is measured in the income variables. Second, the explanatory variables included in the models were limited to those available in the HPS data. Other important explainers might include language spoken, country of origin, computer literacy, political party, transportation mode, and experiences with racism. There may be other modifiable factors that could be more readily impacted by short-term policies to improve vaccination coverage.
The factors in the model are specified as linear and additive, but other specifications may be appropriate. For example, income and household size were included separately, but there may be an important interaction between the 2 factors. As a sensitivity test, the ratio of income to poverty was included in the model, but it had almost no impact on the result. Vaccination status was self-reported and thus subject to recall bias, although the accuracy of the report of COVID-19 vaccination is likely to be at least as high as of influenza vaccination.27 The study period covers January 2021–March 2021, a period when COVID-19 vaccinations were increasing rapidly. Thus, the determinants of vaccination may be changing over time, and the estimates only reflect the average effect over this period when supply was constrained. Finally, nonresponse and missingness in the data reduced the sample size. Although probability weights were used on this subsample, the findings may not be representative of the U.S. adult population.28
CONCLUSIONS
Racial and ethnic minority groups have been disproportionately affected by the health and economic impacts of the COVID-19 pandemic. This paper identified the key factors associated with racial and ethnic disparities in adult vaccination coverage. The findings can help to inform efforts to distribute vaccines equitably and prevent the further exacerbation of COVID-19 health disparities.
Acknowledgments
ACKNOWLEDGMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
No financial disclosures were reported by the authors of this paper.
CRediT AUTHOR STATEMENT
Austin M. Williams: Conceptualization; Data curation; Formal analysis; Methodology; Project administration; Software; Supervision, Visualization; Writing - original draft; Writing - review and editing. Heather B. Clayton: Conceptualization; Supervision; Writing - original draft; Writing - review and editing. James A. Singleton: Conceptualization; Methodology; Supervision; Visualization; Writing - original draft, Writing - review and editing.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2021.10.008.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Media statement from CDC Director Rochelle P Walenksy, MD, MPH, on racism and health. Centers for Disease Control and Prevention. https://www.cdc.gov/media/releases/2021/s0408-racism-health.html. Updated April 8, 2021. Accessed October 19, 2021.
- 2.Racism and health. Centers for Disease Control and Prevention. Office of Minority Health & Health Equity. https://www.cdc.gov/healthequity/racism-disparities/index.html. Updated November 24, 2021. Accessed October 19, 2021.
- 3.Frieden TR, Centers for Disease Control and Prevention (CDC) CDC health disparities and inequalities report - United States, 2013. Foreword. MMWR Suppl. 2013;62(3):1–2. https://www.cdc.gov/mmwr/pdf/other/su6203.pdf [PubMed] [Google Scholar]
- 4.National Academies of Sciences Engineering, and Medicine . The National Academies Press; Washington, DC: 2017. Communities in Action: Pathways to Health Equity. [DOI] [PubMed] [Google Scholar]
- 5.Simmons A, Chappel A, Kolbe AR, Bush L, Sommers BD. Office of the Assistant Secretary for Planning and Evaluation, HHS; Washington, DC: Published March 16, 2021. Health disparities by race and ethnicity during the COVID-19 pandemic: current evidence and policy approaches.https://aspe.hhs.gov/sites/default/files/private/pdf/265206/covid-equity-issue-brief.pdf [Google Scholar]
- 6.Nol RA. U.S. Bureau of Labor Statistics; Washington, DC: Published May 2018. Race, economics, and social status.https://www.bls.gov/spotlight/2018/race-economics-and-social-status/pdf/race-economics-and-social-status.pdf [Google Scholar]
- 7.Kim EJ, Marrast L, Conigliaro J. COVID-19: magnifying the effect of health disparities. J Gen Intern Med. 2020;35(8):2441–2442. doi: 10.1007/s11606-020-05881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karmakar M, Lantz PM, Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the U.S. JAMA Netw Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.36462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karaye IM, Horney JA. The impact of social vulnerability on COVID-19 in the U.S.: an analysis of spatially varying relationships. Am J Prev Med. 2020;59(3):317–325. doi: 10.1016/j.amepre.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hughes MM, Wang A, Grossman MK, et al. County-level COVID-19 vaccination coverage and social vulnerability—United States, December 14, 2020–March 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(12):431–436. doi: 10.15585/mmwr.mm7012e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim D. Associations of race/ethnicity and other demographic and socioeconomic factors with vaccination during the COVID-19 pandemic in the United States. medRxiv. Preprint. Posted online April 14, 2021. https://doi.org/10.1101/2021.02.16.21251769.
- 12.Park J. Who is hardest hit by a pandemic? Racial disparities in COVID-19 hardship in the U.S. Int J Urban Sci. 2021;25(2):149–177. doi: 10.1080/12265934.2021.1877566. [DOI] [Google Scholar]
- 13.Gangopadhyaya A, Karpman M, Aarons J. Urban Institute and The Robert Wood Johnson Foundation; Washington, DC: Published September 2020. As the COVID-19 recession extended into the summer of 2020, more than 3 million adults lost employer-sponsored health insurance coverage and 2 million became uninsured.https://www.urban.org/sites/default/files/publication/102852/as-the-covid-19-recession-extended-into-the-summer-of-2020-more-than-3-million-adults-lost-employer-sponsored-health-insurance-coverage-and-2-million-became-uninsured.pdf [Google Scholar]
- 14.Alsan M, Stantcheva S, Yang D, Cutler D. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among U.S. adults. JAMA Netw Open. 2020;3(6) doi: 10.1001/jamanetworkopen.2020.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alsan M, Wanamaker M. Tuskegee and the health of black men. Q J Econ. 2018;133(1):407–455. doi: 10.1093/qje/qjx029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas SB, Quinn SC. The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the Black community. Am J Public Health. 1991;81(11):1498–1505. doi: 10.2105/ajph.81.11.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jaiswal J, Halkitis PN. Towards a more inclusive and dynamic understanding of medical mistrust informed by science. Behav Med. 2019;45(2):79–85. doi: 10.1080/08964289.2019.1619511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen KH, Srivastav A, Razzaghi H, et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination - United States, September and December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(6):217–222. doi: 10.15585/mmwr.mm7006e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U.S. Census Bureau. Source of the data and accuracy of the estimates for the household pulse survey – phase 3. Suitland-Silver Hill, MD: U.S. Census Bureau. https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/Phase3_Source_and_Accuracy_Week_27.pdf. Published April 2021. Accessed October 19, 2021.
- 20.Jann B. The Blinder–Oaxaca decomposition for linear regression models. Stata J. 2008;8(4):453–479. doi: 10.1177/1536867X0800800401. [DOI] [Google Scholar]
- 21.Oaxaca R. Male–female wage differentials in urban labor markets. Int Econ Rev. 1973;14(3):693–709. doi: 10.2307/2525981. [DOI] [Google Scholar]
- 22.Fortin N, Lemieux T, Firpo S. In: Ashenfelter O, Card D, editors. 4, Part A. Elsevier; Amsterdam, The Netherlands: 2011. Decomposition methods in economics; pp. 1–102. (Handbook of Labor Economics). [DOI] [Google Scholar]
- 23.Thoma ME, Drew LB, Hirai AH, Kim TY, Fenelon A, Shenassa ED. Black–White disparities in preterm birth: geographic, social, and health determinants. Am J Prev Med. 2019;57(5):675–686. doi: 10.1016/j.amepre.2019.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Charasse-Pouélé C, Fournier M. Health disparities between racial groups in South Africa: a decomposition analysis. Soc Sci Med. 2006;62(11):2897–2914. doi: 10.1016/j.socscimed.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 25.Yun MS. Decomposing differences in the first moment. Econ Lett. 2004;82(2):275–280. doi: 10.1016/j.econlet.2003.09.008. [DOI] [Google Scholar]
- 26.Yehia BR, Winegar A, Fogel R, et al. Association of race with mortality among patients hospitalized with coronavirus disease 2019 (COVID-19) at 92 U.S. hospitals. JAMA Netw Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.18039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Irving SA, Donahue JG, Shay DK, Ellis-Coyle TL, Belongia EA. Evaluation of self-reported and registry-based influenza vaccination status in a Wisconsin cohort. Vaccine. 2009;27(47):6546–6549. doi: 10.1016/j.vaccine.2009.08.050. [DOI] [PubMed] [Google Scholar]
- 28.Peterson S, Toribio N, Farber J, Hornick D. U.S. Census Bureau; Suitland-Silver Hill, MD: Published March 24, 2021. Demographic statistical methods division sample design and estimation: nonresponse bias report for the 2020 household pulse.https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/2020_HPS_NR_Bias_Report-final.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.