Abstract
Background and Objectives
Staff–resident communication is a critical part of nursing home (NH) care. Reducing elderspeak and increasing person-centered communication has been shown to reduce behavioral symptoms experienced by persons living with dementia. An online version of a successful classroom-based communication-training program that reduced staff elderspeak and resident behavioral symptoms was evaluated. The objective of this study was to establish feasibility and determine the preliminary effects of the online program in preparation for a national pragmatic clinical trial.
Research Design and Methods
Seven NHs were randomized to immediate intervention or wait-list control conditions. The NHs were provided with the web-based training program that staff individually accessed. Primary outcomes were knowledge scores and communication ratings of a video-recorded interaction, using pre- to posttraining comparisons.
Results
Knowledge increased from a mean pretest score of 61.9% (SD = 20.0) to a mean posttest score of 84.6% (SD = 13.5) for the combined group. Knowledge significantly improved between Time 1 and Time 2 for the immediate intervention participants (p < .001), but not for the wait-list control participants (p = .091), and this difference was statistically significant (p < .001). Ability to recognize ineffective, inappropriate, nonperson-centered, and elderspeak communication improved after training (p < .001). The magnitude of improvement in communication recognition was comparable to that of the original classroom format.
Discussion and Implications
The adapted communication intervention was feasible and improved knowledge and communication. Online instruction can improve access to quality education and is an effective means to improve dementia care by overcoming barriers to in-person training.
Clinical Trials Registration Number: NCT03849937
Keywords: Continuing education, Dementia, Elderspeak, Person-centered care, Staff-resident interactions
Background and Objectives
The population of persons living with Alzheimer’s disease and other dementias will expand from 6 to 14 million by 2050, increasing dementia care costs to $1.1 trillion (Alzheimer’s Association, 2020). Of today’s 1.4 million nursing home (NH) residents, 61% have moderate to severe dementia, and up to 90% exhibit behavioral and psychological symptoms of dementia (BPSD) such as physical and verbal aggression, agitation, and wandering (Kales et al., 2015). BPSD increase time to provide care, and NH staff, primarily Certified Nursing Assistants (CNAs), report that BPSD represent the most stressful aspect of their job (Brodaty et al., 2003; Maas & Buckwalter, 2006). It is estimated that BPSD increase costs of dementia care by 25% to 35% (Beeri et al., 2002).
The Communication Predicament of Aging theory establishes the research-supported link between elderspeak (i.e., patronizing/infantilizing communication) and BPSD (Williams et al., 2009). When younger people communicate with older adults, they tend to modify their speech by simplifying, clarifying, and altering the underlying affective quality of messages, based on stereotypes of older adults (Ryan, Hummert, et al., 1995). The resulting implicit message of incompetence begins a negative feedback loop for older persons, who react with depression, withdrawal, and dependency. Elderspeak is especially threatening to self-concept and personhood, critical to the well-being of persons living with dementia (Kitwood, 1997). The need-driven dementia-compromised behavior model recognizes BPSD as the expression of unmet needs of persons living with dementia (Talerico et al., 2002). Communication that staff can modify to prevent BPSD is an essential and constant part of the environment connecting persons living with dementia to others and affirming their self-concept. The Communication Enhancement Model provides a framework for overcoming patronizing communication and subsequent behavioral challenges of persons living with dementia by facilitating an individual assessment of communication accommodation needs (Ryan, Meredith, et al., 1995).
Our theoretically driven Changing Talk (CHAT) educational intervention increases staff awareness of the message elderspeak conveys and guides practice of more effective communication using three 1-hr, in-person training sessions. In our most recent randomized controlled trial testing CHAT, linear mixed modeling determined that the change in elderspeak was predicted by participation in CHAT (p = .028) and baseline elderspeak (p < .001), while resistiveness to care (RTC) in persons living with dementia was predicted by the change in elderspeak (p < .001), baseline RTC (p < .001), communication disability, and comorbid illnesses (Williams, Perkhounkova, et al., 2017). It was demonstrated that CHAT effectively reduced both elderspeak use by care staff and subsequent RTC in residents with dementia.
Despite the success of CHAT in reducing elderspeak and RTC, we found challenges to educating NH staff using an in-person classroom-based approach. Our challenges were consistent with difficulties typical with NH staff education including turnover, absenteeism, heavy workloads, and personal conflicts, which limited participation (Beeber et al., 2010; Low et al., 2015). The classroom format of CHAT limited staff access, participation, and feasibility for widespread dissemination. Creative, efficient approaches are needed to overcome NH staff education barriers (Institute on Medicine, 2009; Silvestre et al., 2015). E-learning provides new opportunities to deliver evidence-based interventions in busy care environments and has shown to provide equivalent outcomes to traditional classroom-based education (Halabisky et al., 2010; Pusa et al., 2019; Soper, 2017). We created online modules of the original CHAT intervention—Changing Talk Online (CHATO)—to overcome these educational barriers to enhance dissemination.
The original CHAT program included high interactivity including group discussions, role playing, and evaluating one’s own communication through an audio-recorded care encounter. To ensure a continued robust educational experience, an instructional designer adapted the CHAT content to CHATO and interactive activities through the web-based platform (Williams, Abd-Hamid, et al., 2017). CHATO contains the same theoretically driven content in an online format that allows independent access for asynchronous learning by busy NH staff. The objective of this pilot trial was to establish feasibility and test preliminary efficacy of the CHATO modules, building on the success of the original CHAT study. In addition, strategies to increase dissemination and translation of skills to practice were identified and tested in preparation for a large-scale national pragmatic clinical trial evaluating CHATO effects on reducing resident BPSD and the use of psychoactive medications that are commonly used to control BPSD. We hypothesized that the online version of the CHAT intervention—CHATO—would effectively increase knowledge of elderspeak and person-centered communication in dementia care.
Research Design and Methods
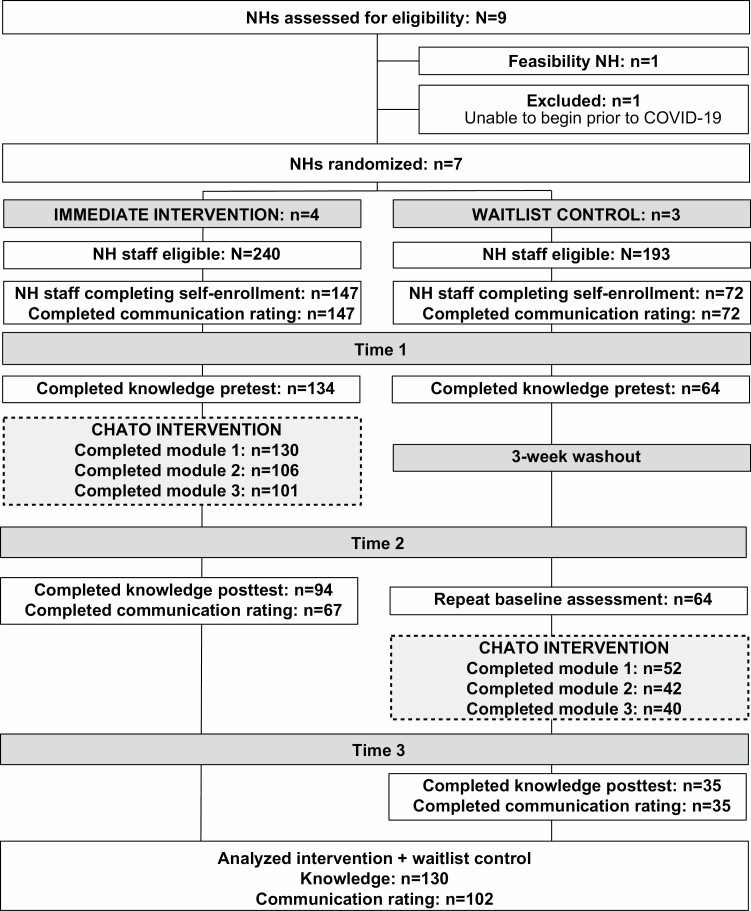
Nine NHs were recruited for the pilot trial (Figure 1). Staff in one NH completed an initial feasibility pilot to identify changes needed to access the online format. Two 13-item knowledge test forms were developed and revised based on psychometric analysis following this feasibility pilot; thus, this initial NH was not included in the current analysis. An additional NH withdrew participation at the start of the coronavirus disease 2019 pandemic.
Figure 1.
Consort diagram for CHATO. Note: CHATO = Changing Talk Online; NH = nursing home.
The staff in the remaining seven NHs were cluster-randomized by NH to the immediate intervention or wait-list control groups. The staff in the immediate intervention NHs completed communication ratings and the knowledge test and then completed the three training modules and posttraining evaluation activities. Using a crossover design, the staff in the wait-list NHs completed communication ratings and the knowledge test and then a different form of the knowledge test after a 3-week waiting period followed by completion of the modules and posttraining evaluation activities. Knowledge test forms were randomly assigned to wait-list control participants at pretest; all participants took different test forms at posttest.
Intervention
The CHAT and CHATO interventions have interchangeable content that is conceptually based on the Communication Predicament of Aging Model and Communication Enhancement Model (Ryan, Hummert, et al., 1995; Ryan, Meredith, et al., 1995). The CHAT and CHATO intervention alerts NH staff to elderspeak and its negative effects, imparts knowledge of taking the older adult’s perspective, and guides self-evaluation and practice of effective communication (Williams et al., 2004). Improved communication, based on individual assessment of resident abilities, supports positive self-concept and meets socialization needs, reducing need-driven dementia-compromised behavior or BPSD.
An instructional designer, subject matter nurse educator, item writer, and media team created the CHATO training using the ADDIE model of instructional design along with game-based learning theory. The adaptation process and theoretical approach to self-directed adult learning is reported elsewhere (Williams, Abd-Hamid, et al., 2017). CHATO is presented in three 1-hr modules similar to the original CHAT intervention (Williams et al., 2004). Session 1 introduces effective versus ineffective communication. Participants identify communication issues in video vignettes. Session 2 focuses on identification and negative effects of elderspeak, using video-recorded examples. Session 3 includes improved communication practices tailored to each resident’s abilities. Participants critique communication in videos and correct transcripts to eliminate elderspeak. CHATO includes a total of 20 video clips of actual care encounters between NH staff and residents and nine interactive exercises. The interactive exercises must be successfully completed to advance through the program, assuring delivery fidelity and dose of the intervention.
The modules were primarily accessed by staff at work during their shifts. The modules were designed for computer access and are not compatible in a smartphone or tablet format. While trialing the platform with the feasibility NH, it was noted that many staff do not have access to a computer outside of work, so the remaining NHs were encouraged to establish a computer workspace at the NH and compensate staff to complete the modules during worktime. Staff in each NH were provided unique login codes to create an individual account. They completed demographic data and then progressed through the modules. The modules did not have to be completed in one sitting. It was possible to stop and come back to the training and resume at the same point of departure.
Using a pragmatic approach, each NH administrator recruited staff to participate in the pilot training. Most administrators reported that staff were not required to take the training as a condition of employment, rather they were encouraged to self-enroll in the modules. Each NH designated a computer for staff to access the modules and time for them to complete the training. An implementation toolkit was provided to each NH which provided strategies and resources to encourage participation in the modules. Continuing education credit was given to the staff following completion of the modules.
Measures
Two equivalent 13-item forms of a scenario-based Changing Talk Scale (CHATS) for knowledge of communication in dementia care were developed targeting 13 objectives. The initial feasibility NH was used to streamline the online module processes and to evaluate the reliability and equivalency of the CHATS forms. Discussion of development and validation of the CHATS will be provided elsewhere. Test score was calculated as the percentage of correct answers.
A communication rating exercise was also completed at the beginning of module 1 and after completing module 3; participants watched the same video of a real NH interaction and rated the staff speaker for effectiveness, appropriateness, person-centeredness, and use of elderspeak communication. One item rating effectiveness was scored on a 5-point Likert scale (0 = ineffective; 4 = effective). One item rating appropriateness also used a 5-point Likert scale (0 = inappropriate; 4 = appropriate). Recognizing elderspeak was evaluated with six items scored yes (1) or no (0) (range = 0 to 6) for recognizing key features of elderspeak communication. Recognizing person-centered communication was evaluated with three items scored for occurrence, yes (1) or no (0) (range = 0 to 3) with lower score indicating appropriate recognition of nonperson-centered (i.e., inappropriate) communication.
Feasibility NH
Prior to commencing the CHATO pilot trial, staff in one NH completed a feasibility pilot to identify changes needed to access the online modules. Based on this feasibility pilot, streamlined strategies for enrolling participants into the platform and strategies for completing the modules during work time were developed. Successful direct care staff enrollment (42%) and completion rates (72%) along with increases in knowledge (p = .024) and communication ratings indicated the platform was ready for the larger pilot trial.
Analyses
SAS software (version 9.4) was used for analysis. Descriptive statistics were calculated for NHs and staff participants. Mean knowledge test scores were calculated at each time point for the immediate intervention and wait-list control groups, excluding participants who did not complete CHATO. Mean changes in test scores between time points were calculated and tested using the paired-samples t test. Mean test score changes were compared between the immediate intervention and wait-listed participants using the independent samples t test. Mean communication ratings before and after the training were calculated for all participants who completed CHATO. Mean changes in ratings were calculated and tested using the Wilcoxon signed-rank test.
Results
Enrollment, Participation, and Completion
Between December 2019 and March 2020, staff from the seven randomized NHs participated in the pilot that was approved by the University Institutional Review Board (IRB). Descriptive information about the NHs and participating staff are provided in Tables 1 and 2.
Table 1.
Nursing Home Characteristics (N = 7)
| Characteristic | Mean (SD) | Range |
|---|---|---|
| Number of beds | 65.1 (28.2) | 31–117 |
| Number of residents | 53.6 (28.8) | 31–102 |
| Long-stay quality star rating (0–5) | 4.3 (0.8) | 3–5 |
| Case mix index | 1.3 (0.2) | 1.1–1.5 |
| Long-stay residents receiving antipsychotic medication | 12.0% (8.1%) | 4.7%–23.6% |
| Long-stay residents receiving antianxiety or hypnotic medication | 18.4% (12.2%) | 5.2%–40.4% |
| Non-Hispanic White residents | 91.1% (10.5%) | 74.2%–100.0% |
| Residents with dementia | 44.4% (21.3%) | 18.6%–71.0% |
| Staff turnover rate | 29.1% (16.3%) | 6.6%–52.0% |
| Average hourly wage | ||
| Certified Nursing Assistant | $12.40 ($1.59) | $10.25–$14.00 |
| Licensed Practical Nurse | $20.29 ($2.20) | $18.00–$23.20 |
| Registered Nurse | $26.88 ($2.90) | $23.00–$30.11 |
Notes: SD = standard deviation. Collected from Nursing Home Compare (2019 Q4) or nursing home administrator.
Table 2.
Direct Care Staff Demographics (N = 219)
| Variable | n (%)a |
|---|---|
| Age | |
| <25 years | 22 (10.0) |
| 25 to 40 years | 77 (35.2) |
| 41 to 54 years | 70 (32.0) |
| 55 years or greater | 49 (22.4) |
| Missing | 1 (0.5) |
| Gender | |
| Male | 15 (6.8) |
| Female | 203 (92.7) |
| Missing | 1 (0.5) |
| Race | |
| American Indian/Alaskan Native | 4 (1.8) |
| White | 175 (79.9) |
| Black or African American | 3 (1.4) |
| Otherb | 0 (0.0) |
| Missing | 37 (16.9) |
| Ethnicity | |
| Not Hispanic or Latino | 153 (69.9) |
| Hispanic or Latino | 0 (0.0) |
| Missing | 66 (30.1) |
| Role | |
| Certified Nursing Assistant | 112 (51.1) |
| Licensed Practical Nurse | 17 (7.8) |
| Registered Nurse | 55 (25.1) |
| Otherc | 20 (9.1) |
| Missing | 15 (6.8) |
| Highest education | |
| High school or less | 54 (24.7) |
| Associate degree or some college | 129 (58.9) |
| Bachelor’s degree or higher | 27 (12.3) |
| Missing | 9 (4.1) |
| Years in health care role | |
| Less than 5 years | 89 (40.6) |
| 5 to <10 years | 43 (19.6) |
| 10 years or greater | 78 (35.6) |
| Missing | 9 (4.1) |
Notes: Sample of 219 are staff who completed enrollment.
aMay not sum to 100.0% due to rounding.
bOther includes Asian and Native Hawaiian or Other Pacific Islander.
cOther includes dietary (n = 8), social work (n = 6), activities (n = 4), housekeeping (n = 3), therapy (n = 1), and transportation (n = 1).
Nursing homes
A convenience sample of seven NHs from four states in midwest and northwest United States were selected from a database of NHs expressing interest in the training. The NHs averaged 65 beds and cared for mostly non-Hispanic White residents (91.1%). Most did not have a special care unit (n = 5) and were not-for-profit facilities (n = 5). The NHs were generally rated as above average with an average 4.3-star Nursing Home Compare quality indicator rating.
NH Staff
We encouraged NHs to include all staff in training with a goal of changing the communication culture in each NH. Across the seven NHs, 650 staff were eligible to take the training. Results are reported only for direct care staff, defined as individuals who have daily communication with residents. Of the 433 eligible direct care staff, 219 (50.6%) assented and self-enrolled in CHATO. Of those enrolled, 141 (64.4%) completed the training. Staff participants were mostly CNAs (51.1%) and nurses (32.9%). They were mostly female (92.7%) with an average age of 42.6 (SD = 13.7) years. Staff had an average of 9.2 (SD = 9.3) years in their current role and 6.9 (SD = 7.8) years at their current NH.
Outcome Findings
Knowledge (CHATS)
Between Time 1 and Time 2 the CHATS scores increased on average by 4.3 points (SD = 20.2, n = 64, p = .091) for the wait-listed participants and by 20.8 points (SD = 22.7, n = 95, p < .001) for the immediate intervention participants (Table 3). The difference between the groups was statistically significant (p < .001). For the wait-listed participants who completed the training between Time 2 and Time 3, the knowledge scores increased by 22.9 points (SD = 19.4, n = 35, p < .001) after the training. Combining all participants in both groups who tested before and after the training resulted in mean increase of 22.7 points (SD = 22.3, n = 130, p < .001).
Table 3.
Knowledge Test (CHATS) Score Changes
| Intervention group | N | Time 1 or 2 Mean (SD) |
Time 2 or 3 Mean (SD) |
Change Mean (SD) |
p |
|---|---|---|---|---|---|
| Waitlist control: Time 1 (pretest 1) to Time 2 (pretest 2) | 64 | 58.7 (20.5) | 63.0 (17.6) | 4.3 (20.2) | .091 |
| Waitlist control crossover: Time 2 (pretest 2) to Time 3 (posttest) | 35 | 64.0 (17.6) | 86.8 (13.8) | 22.9 (19.4) | <.001 |
| Immediate: Time 1 (pretest) to Time 2 (posttest) | 95 | 63.0 (18.8) | 83.8 (13.4) | 20.8 (22.7) | <.001 |
| Immediate + waitlist control crossover: pretest to posttest | 130 | 61.9 (20.0) | 84.6 (13.5) | 22.7 (22.3) | <.001 |
Notes: CHATS = Changing Talk Scale; SD = standard deviation. Knowledge test (CHATS) scoring: 13 items scored incorrect (0) or correct (1). Test score was calculated as the percentage of correct answers. At Time 1 no participant had completed the training. At Time 2 only immediate group participants completed the training. At Time 3 wait-listed control participants completed the training. p Values are for the paired-samples t test.
Communication ratings
An improvement in effective (M = −0.6, SD = 1.5, p < .001) and appropriate communication (M = −0.9, SD = 1.5, p < .001) after training was demonstrated after training for the combined groups (Table 4). Participants also improved in their ratings of person-centered communication (M = −0.2, SD = 0.5, p < .001) and recognizing elderspeak (M = 0.2, SD = 0.4, p < .001) after the training. Compared to results from our original CHAT classroom training, the CHATO training demonstrated a comparable or greater magnitude of change in recognizing critical aspects of communication (Williams et al., 2016).
Table 4.
Communication Ratings Pre and Post CHATO (n = 102)
| Training period | Effective communication | Appropriate communication | Recognizes elderspeak | Recognizes person-centered communication |
|---|---|---|---|---|
| Pretraining—Mean (SD) | 2.7 (1.2) | 3.1 (1.2) | 0.6 (0.2) | 0.5 (0.4) |
| Posttraining—Mean (SD) | 2.1 (1.1) | 2.2 (1.1) | 0.7 (0.3) | 0.3 (0.4) |
| Change (post–pre)—Mean (SD) | -0.6 (1.5) | -0.9 (1.5) | 0.2 (0.4) | -0.2 (0.5) |
| p | <.001 | <.001 | <.001 | <.001 |
Notes: CHATO = Changing Talk Online; SD = standard deviation. Effective rating: mean score for one item scored 1 = ineffective to 5 = effective; lower score indicates improvement. Appropriate rating: mean score for one item scored 1 = inappropriate to 5 = appropriate; lower score indicates improvement. Recognizes elderspeak subscale: mean score for six items scored yes (1) or no (0); higher score indicates improvement. Recognizes person-centered communication subscale: mean score for three items scored yes (1) or no (0); lower score indicates improvement. p Values are for the Wilcoxon signed-rank test.
Discussion and Implications
Results indicate that NH staff will enroll in and complete online education. The training improved their knowledge and recognition of ineffective communication practices demonstrating equivalent or greater improvement compared to the original in-person training. The benefits of online training include the ability to expand educational opportunities by increasing access and allowing a flexible approach that meets the need of individual schedules. Although we were concerned that the online format without peer interactions would not achieve the same degree of learning as the classroom-based program, this did not prove to be the case. An instructional designer led the transition from CHAT to CHATO and included activities with high interactivity such as virtual discussion boards to engage with peers in the online training.
This training in person-centered communication for NH dementia care has been developed stepwise and iteratively through the NIH Stage Model for Behavioral Intervention Development (National Institue of Aging, 2016). Early Stage 1 development of CHAT (Williams, 2006; Williams et al., 2003) led to Stage III testing of CHAT in controlled NH settings to establish efficacy (Williams, Perkhounkova, et al., 2017). After this additional Stage I modification of the original CHAT content to online module format, CHATO is now positioned for effectiveness testing (Stage IV) with NHs to maximize external validity in preparation for future implementation and dissemination research (Stage V) (Onken et al., 2014).
Ongoing research will test the online modules in a larger nationwide trial that will evaluate more distal outcomes including changes in behavioral symptoms and psychoactive medication use among persons living with dementia in the participating NHs (http://nursing.kumc.edu/research/chato.html). The larger sample size will confirm these effects and will evaluate whether differential use of implementation strategies and supports effects outcomes. This national pragmatic trial of 120 nursing will utilize a similar wait-list control design. In addition, costs related to outcomes will be evaluated. A protocol paper for this trial is forthcoming.
The CHATO training and the associated web-based platform was shown to be feasible in this trial. The knowledge gains and communication ratings demonstrated the intervention’s efficacy. A pragmatic approach to recruiting staff within individual NHs was taken in order to prepare for the national trial. Over half of the eligible direct care staff enrolled in the training and nearly two thirds of those staff completed all three modules. Rates of direct care staff participation varied between NHs ranging from 19% to 80% participation from direct care staff. Nurses and nursing assistants had the highest rates of participation and although the training can be taken by any NH staff it is targeted toward nursing care staff as they provide the most direct care. Participation by other ancillary care staff such as speech/music/occupation therapy or dietary varied between NHs. Three of the seven NHs focused exclusively on recruiting nursing care staff and recruited no other ancillary staff. In this pragmatic approach NH leadership used the implementation toolkit to encourage NH staff to self-enroll in the trial. Additional results related to feasibility and implementation including program evaluations, diffusion ratings of the intervention, and a description of the implementation toolkit are forthcoming. Exploration of the consequences of individual facilities choosing their own implementation plan via the toolkit and the effectiveness of these individual plans will be explored in this forthcoming manuscript.
The NHs in this pilot trial were recruited from a subset of NHs that expressed interest in participating in the national trial. NHs were selected on a convenience basis based on their readiness to participate. Five of seven of these NHs are nonprofit, which may have influenced their ability to participate in research that takes place during scheduled shifts and adopt interventions to improve quality based on the known incongruity between for-profit and nonprofit NHs (Comondore et al., 2009). Similarly, this sample of NHs had high ratings for overall quality. The national trial will use a stratified sampling method to ensure diversity across region, star rating, size, and rurality. Closed captioning will be added to the modules prior to the national trial to aid in content comprehension. Depending on the results of the larger trial, future research can focus on adapting the content for more diverse caregivers with less English proficiency.
Direct costs of the intervention were not measured in this pilot trial. Costs would be limited to the salary associated with staff time to complete the training, salary associated with implementation efforts by NH leadership, and technology costs to maintain the educational platform. Module completion time varied for each individual due to the interactive nature of the education with an average of 68.0 min (SD = 27.9 min) per module. A formal cost analysis will be completed in the national trial and compared to the costs associated with the CHAT intervention. It is hypothesized that the CHATO intervention will cost less to implement than CHAT due to the reducing the costs of interventionist time. It was estimated to cost $4.31 for a one percentage point reduction in restiveness to care in residents with dementia from reducing elderspeak in the CHAT trial (Williams, Ayyagari, et al., 2017).
Online training that is accessible, flexible, and effective is critical for reaching staff in NHs where staffing shortages and heavy workloads prohibit attendance in classroom educational programs. This pilot demonstrated that NHs and staff at varied locations and with differing demographic characteristics participated in the training and experienced improved outcomes. The CHATO training led to gains in knowledge by NH staff related to person-centered communication in this pilot study. The larger national trial will evaluate if this knowledge gain will reduce BPSD in NH residents.
Funding
This research was supported by the National Institute on Aging (grant number R61AG061881). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
None declared.
References
- Alzheimer’s Association . (2020). 2020 Alzheimer’s disease facts and figures. https://www.alz.org/media/Documents/alzheimers-facts-and-figures.pdf
- Beeber, A. S., Zimmerman, S., Fletcher, S., Mitchell, C. M., & Gould, E. (2010). Challenges and strategies for implementing and evaluating dementia care staff training in long-term care settings. Alzheimer’s Care Today, 11(1), 17–39. https://www.nursingcenter.com/journalarticle?Article_ID=990089 [Google Scholar]
- Beeri, M. S., Werner, P., Davidson, M., & Noy, S. (2002). The cost of behavioral and psychological symptoms of dementia (BPSD) in community dwelling Alzheimer’s disease patients. International Journal of Geriatric Psychiatry, 17(5), 403–408. doi: 10.1002/gps.490 [DOI] [PubMed] [Google Scholar]
- Brodaty, H., Draper, B., & Low, L. F. (2003). Nursing home staff attitudes towards residents with dementia: Strain and satisfaction with work. Journal of Advanced Nursing, 44(6), 583–590. doi: 10.1046/j.0309-2402.2003.02848.x [DOI] [PubMed] [Google Scholar]
- Comondore, V. R., Devereaux, P. J., Zhou, Q., Stone, S. B., Busse, J. W., Ravindran, N. C., Burns, K. E., Haines, T., Stringer, B., Cook, D. J., Walter, S. D., Sullivan, T., Berwanger, O., Bhandari, M., Banglawala, S., Lavis, J. N., Petrisor, B., Schünemann, H., Walsh, K., … Guyatt, G. H. (2009). Quality of care in for-profit and not-for-profit nursing homes: Systematic review and meta-analysis. BMJ (Clinical Research Ed.), 339, b2732. doi: 10.1136/bmj.b2732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halabisky, B., Humbert, J., Stodel, E. J., MacDonald, C. J., Chambers, L. W., Doucette, S., Dalziel, W. B., & Conklin, J. (2010). e-Learning, knowledge brokering, and nursing: Strengthening collaborative practice in long-term care. Computers, Informatics, Nursing, 28(5), 264–273. doi: 10.1097/NCN.0b013e3181ec28b9 [DOI] [PubMed] [Google Scholar]
- Institute on Medicine . (2009). Redesigning continuing education in the health professions. https://www.nap.edu/catalog/12704/redesigning-continuing-education-in-the-health-professions
- Kales, H. C., Gitlin, L. N., & Lyketsos, C. G. (2015). Assessment and management of behavioral and psychological symptoms of dementia. BMJ (Clinical Research Ed.), 350, h369. doi: 10.1136/bmj.h369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitwood, T. (1997). The experience of dementia. Aging and Mental Health, 7, 15–22. doi: 10.1080/13607869757344 [DOI] [Google Scholar]
- Low, L. F., Fletcher, J., Goodenough, B., Jeon, Y. H., Etherton-Beer, C., MacAndrew, M., & Beattie, E. (2015). A systematic review of interventions to change staff care practices in order to improve resident outcomes in nursing homes. PLoS One, 10(11), e0140711. doi: 10.1371/journal.pone.0140711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas, M. L., & Buckwalter, K. C. (2006). Providing quality care in assisted living facilities: Recommendations for enhanced staffing and staff training. Journal of Gerontological Nursing, 32(11), 14–22. doi: 10.3928/00989134-20061101-04 [DOI] [PubMed] [Google Scholar]
- National Institue of Aging . (2016). Stage model for behavioral intervention development. https://www.nia.nih.gov/research/dbsr/stage-model-behavioral-intervention-development
- Onken, L. S., Carroll, K. M., Shoham, V., Cuthbert, B. N., & Riddle, M. (2014). Reenvisioning clinical science: Unifying the discipline to improve the public health. Clinical Psychological Science, 2(1), 22–34. doi: 10.1177/2167702613497932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pusa, S., Dorell, Å., Erlingsson, C., Antonsson, H., Brännström, M., & Sundin, K. (2019). Nurses’ perceptions about a web-based learning intervention concerning supportive family conversations in home health care. Journal of Clinical Nursing, 28(7–8), 1314–1326. doi: 10.1111/jocn.14745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan, E. B., Hummert, M. L., & Boich, L. H. (1995). Communication predicaments of aging; Patronizing behavior toward older adults. Journal of Language and Social Psychology, 14(1–2), 144–166. doi: 10.1177/0261927x95141008 [DOI] [Google Scholar]
- Ryan, E. B., Meredith, S. D., MacLean, M. J., & Orange, J. B. (1995). Changing the way we talk with elders: Promoting health using the communication enhancement model. International Journal of Aging & Human Development, 41(2), 89–107. doi: 10.2190/FP05-FM8V-0Y9F-53FX [DOI] [PubMed] [Google Scholar]
- Silvestre, J. H., Bowers, B. J., & Gaard, S. (2015). Improving the quality of long-term care. Journal of Nursing Regulation, 6(2), 52–56. doi: 10.1016/S2155-8256(15)30389-6 [DOI] [Google Scholar]
- Soper, T. (2017). Knowledge into learning: Comparing lecture, e-learning and self-study take-home packet instructional methodologies with nurses. Nursing Open, 4(2), 76–83. doi: 10.1002/nop2.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talerico, K. A., Evans, L. K., & Strumpf, N. E. (2002). Mental health correlates of aggression in nursing home residents with dementia. The Gerontologist, 42(2), 169–177. doi: 10.1093/geront/42.2.169 [DOI] [PubMed] [Google Scholar]
- Williams, K. N. (2006). Improving outcomes of nursing home interactions. Research in Nursing & Health, 29(2), 121–133. doi: 10.1002/nur.20117 [DOI] [PubMed] [Google Scholar]
- Williams, K., Abd-Hamid, N. H., & Perkhounkova, Y. (2017). Transitioning communication education to an interactive online module format. Journal of Continuing Education in Nursing, 48(7), 320–328. doi: 10.3928/00220124-20170616-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, K. N., Ayyagari, P., Perkhounkova, Y., Bott, M. J., Herman, R., & Bossen, A. (2017). Costs of a staff communication intervention to reduce dementia behaviors in nursing home care. The Journal of Nursing Home Research Sciences, 3, 22–27. doi: 10.14283/jnhrs.2017.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, K., Bossen, A., Perkhounkova, Y., & Hein, M. (2016). Knowledge to practice: Nursing home staff perceptions and intentions for learned communication skills. Journal of Gerontological Nursing, 42(3), 26–34. doi:10:3928/00989134-20160212-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, K. N., Herman, R., Gajewski, B., & Wilson, K. (2009). Elderspeak communication: Impact on dementia care. American Journal of Alzheimer’s Disease and Other Dementias, 24(1), 11–20. doi: 10.1177/1533317508318472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, K., Kemper, S., & Hummert, M. L. (2003). Improving nursing home communication: An intervention to reduce elderspeak. The Gerontologist, 43(2), 242–247. doi: 10.1093/geront/43.2.242 [DOI] [PubMed] [Google Scholar]
- Williams, K., Kemper, S., & Hummert, M. L. (2004). Enhancing communication with older adults: Overcoming elderspeak. Journal of Gerontological Nursing, 30(10), 17–25. doi: 10.3928/0098-9134-20041001-08 [DOI] [PubMed] [Google Scholar]
- Williams, K. N., Perkhounkova, Y., Herman, R., & Bossen, A. (2017). A communication intervention to reduce resistiveness in dementia care: A cluster randomized controlled trial. The Gerontologist, 57(4), 707–718. doi: 10.1093/geront/gnw047 [DOI] [PMC free article] [PubMed] [Google Scholar]