Abstract
Emotion regulation (ER) is the ability to monitor, evaluate, and modify one’s emotional responses to be appropriate for environmental demands. Poor ER has been considered a transdiagnostic risk factor for a range of internalizing and externalizing disorders and overall decreased well-being in adolescents. A range of evidence-based interventions exist which may improve ER. However, much of the intervention research to date does not include a measure of ER to assess change pre and post treatment, with limited information about the efficacy of these interventions in youth across a range of sample types. There is a clear need for a comprehensive review of the literature examining ER-focused interventions in adolescents with a wide range of presenting disorders. A literature search was originally conducted in January 2020 and an updated search was conducted in February 2021 which elicited 1,245 articles, of which 605 were duplicates and were removed. Abstracts of the remaining 640 articles were screened with 121 articles being reviewed in full. Of note, 16 additional articles were identified through references and other sources during this process and were also included in the full review. Of the 137 articles reviewed in full, 41 studies were ultimately included in the present review. The present paper provides a descriptive review of intervention approaches and findings from community prevention programs, programs for war-affected youth, programs for clinical populations, and programs for incarcerated and delinquent adolescents. The overall pooled effect was significantly different from zero based on the pre/post effects (Hedge’s g = .29, 95% CI [.22, .36]) and the intervention/control effects (Hedge’s g = .19, 95% CI [.06 to .32]). Although neither sex nor age significantly accounted for heterogeneity in effect sizes, there were significant findings for population type (clinical vs. community), with community samples having significantly lower effect sizes on average. Impacts of the different ER measures used and significant methodological variability (e.g., use of control groups, length of intervention) across included studies are discussed. Implications and suggestions for future research are reviewed, specifically, that additional understanding of moderators of effects are needed and that measures used to assess change in ER, both dysregulation and adaptive skill use, may need to more directly align with the intervention’s focus and the strategies taught as part of the intervention.
Keywords: emotion regulation, meta-analysis, adolescent, intervention, review
There has been a proliferation of research over the past 20 years regarding the processes that contribute to successful emotion regulation (ER) and the importance of adaptive ER skills for overall well-being. ER is defined as the ability to monitor, evaluate, and modify one’s emotional responses that appropriately suits environmental demands. A widely used process model of ER (Gross, 1998) describes five types of ER strategies: 1) situation selection, avoiding or approaching a potentially emotionally ladened situation; 2) situation modification, changing aspects of the situation or environment; 3) attentional deployment, influencing perception of the situation or environment; 4) cognitive change, changing cognitive representations; and 5) response modulation, changing emotion-related behaviors. This work has been extended to describe three stages of ER, including 1) identification, which involves distinguishing emotional responses and deciding whether to regulate emotion; 2) selection, which involves choosing which strategies to use; and 3) implementation, which involves applying the appropriate strategy (Gross, 2015). Thus, conceptually, these models of ER lay the groundwork for multi-faceted intervention approaches that can improve adaptive ER strategies and/or reduce maladaptive ER strategies.
Much of the empirical work to date has sought to understand how youth learn these ER strategies (e.g., Kopp, 1989; Kopp & Neufeld, 2003), as well as the short and long-term consequences of deficits in ER during adolescence. Recently, poor ER (either lack of adaptive ER strategies or increased use of maladaptive ER strategies) has been considered as a transdiagnostic risk factor for a range of internalizing and externalizing disorders, academic failure, and overall decreased well-being in adolescents (Aldao et al., 2016; Ehring et al., 2010; Shapero et al., 2016). Additionally, ER has been supported as a mediator between psychopathology and both functional outcomes and comorbid conditions (Bunford et al., 2018; Fogleman et al., 2019; Graziano et al., 2007; Walerius et al., 2018). Further, youth displaying more adaptive ER show improved well-being and more positive outcomes than those who display maladaptive ER (McLaughlin et al., 2011).
Although ER abilities begin to develop during the preschool years and continue into childhood (Zeman et al., 2006), adolescence may be a specific period during which youth use less adaptive and more maladaptive ER strategies compared with both younger and older individuals (Cracco et al., 2017). Adolescents are undergoing a range of developmental changes (i.e., physical development during puberty, increased interpersonal salience of peers and sensitivity to social context, increased expectation and demand for autonomy; Blakemore & Mills, 2014; Steinberg, 2014), and adaptive navigation of this time relies on learning and implementing adaptive ER strategies (and also minimizing the use of maladaptive ER strategies). Adolescents also begin to differentiate their use of ER strategies depending upon socio-emotional context as well as motivation and emotion type (Zeman et al., 2006). Further, research in social neuroscience has largely supported the notion that the brain is particularly sensitive to social context during adolescence (Schriber & Guyer, 2016), indicating that this period may be particularly salient for developing, implementing, and modifying ER strategies that can promote better social adjustment (Chervonsky & Hunt, 2019). Thus, improving adaptive ER abilities during adolescence may be particularly beneficial for helping youth navigate the challenges and opportunities they encounter during this developmental period.
A range of interventions have been developed to improve ER abilities, with ER being shown to be a malleable construct and a potentially salient target for treatment (Gross, 2002). Additionally, improvements in ER have been associated with improvements in psychopathology for a range of disorders (e.g., Wijana et al., 2018; Wolff & Ollendick, 2012). However, much of the research with these intervention methods is with adults or specific clinical populations (e.g., dialectical behavior therapy [DBT] for individuals with borderline personality disorder) and less is understood about their efficacy in community samples and/or adolescents. In this review, we provide a brief synopsis of why ER-focused interventions are needed, particularly during adolescence, a narrative overview of ER focused interventions for adolescents, estimates of effect size for ER focused interventions for improving adolescent ER abilities, and a discussion of the implications for future research.
A Need for ER-Focused Interventions
Although a range of evidence-based interventions exist which may help improve ER skills, most do not explicitly target ER. One exception is the recent Unified Protocol, which has a child and adolescent version (Ehrenreich et al., 2017) and is based in cognitive behavioral therapy (CBT). The Unified Protocol takes a transdiagnostic approach to treating all emotional disorders, in part, by targeting the underlying emotional difficulties and emotional dysregulation (e.g., Ellard et al., 2010). Additionally, although traditional CBT (see Beck & Beck, 2011) or DBT (see Linehan, 1993) interventions may indirectly improve ER by challenging negative cognitions or training competing behaviors, teaching ER skills is not always the primary focus of the treatment nor is it a primary measure used in efficacy or effectiveness evaluation (e.g., Hadley et al., 2017; Smith et al., 2018). In fact, it has been posited that the effectiveness for CBT in treating some disorders, such as anxiety, is limited because it does not target ER, when those are the very skills that need building (Hannesdottir & Ollendick, 2007). In line with this, ER deficits have been found to be a central component of psychopathology in youth (e.g., Compas et al., 2014, 2017) and thus treatments that specifically target improving these skills, regardless of diagnostic status (i.e., Unified Protocol) may be especially relevant for reducing psychological distress and improving overall well-being. This may be due to the fact that some ER strategies work transdiagnostically regardless of the context or diagnosis (e.g., deep breathing), whereas others may be specific to a certain context or population (e.g., distraction).
Limitations of Existing Reviews
Targeting adaptive ER development as a specific intervention component as well as assessing changes in ER pre and post treatment is an important next step to understanding the efficacy of working to improve ER and subsequently reducing psychopathology. ER interventions have been used in a wide range of clinical, non-clinical, and medical populations from childhood through adulthood and in both individual and group formats (e.g., Smyth & Arigo, 2009). These interventions have also been applied to a wide range of psychological disorders and thus may have differing levels of effectiveness depending on the symptoms present. It is possible certain facets of ER (e.g., identification) may be important for some populations or settings, such as school-wide prevention programs where rates of emotion dysregulation are lower, whereas other facets (e.g., selection and implementation of targeted strategies, such as challenging negative thoughts for adolescents with internalizing disorders, but engaging in positive coping behaviors to calm down for adolescents with externalizing disorders) will be most integral for clinical populations who experience high levels of emotion dysregulation. However, the overall effectiveness of interventions for improving ER across heterogenous samples of adolescents has not been investigated.
A recent systematic review of the intervention literature broadly spanning adolescence and adulthood found that ER deficits decreased throughout the course of intervention regardless of the psychopathology present (the review examined depression, anxiety, eating disorders, substance use disorders, and borderline personality disorders), but with large variation in the effect sizes (Cohen’s d = 0.18 to 2.87; Sloan et al., 2017). These results support the possibility that ER may be operating as a transdiagnostic factor, given that findings were consistent regardless of diagnostic status of the participants in the intervention. Notably, only five of the 67 included studies included adolescent samples and thus, the effects were largely relevant to adult samples. Moreover, the Sloan et al. (2017) review focused on clinical populations and did not include prevention programs or community samples, for which ER interventions may have differential effects. Specifically, it is likely that clinical populations and community populations have different baseline levels of dysregulation and adaptive ER skill use; therefore, there may be more or less room to move, so to speak, during and after going through an intervention program. This is an important point of consideration when understanding how well and for whom ER interventions work. Additionally, another recent narrative review focused on 12 ER interventions with an emotion socialization component for young children (ages 0-6; England-Mason & Gonzalez, 2020). Findings indicated that although the included interventions may show promising results for improving parenting behaviors related to ER, there is limited evidence for how these programs improve the child’s ER abilities.
Finally, Moltrecht et al. (2020) reviewed articles and completed a meta-analysis of published studies through April of 2018 using samples of youth aged 6 and 24. The authors limited their search to psychiatric diagnoses with ER difficulties. The authors found moderate improvements in reducing emotion dysregulation (Hedge’s g = −.46) and increasing adaptive ER (Hedge’s g = .36) with large heterogeneity across studies. Importantly, the authors chose to exclude samples with autism, intellectual disability, and specialized medical populations, despite that these populations, specifically autism (Mazefsky et al., 2013) and intellectual disability (McClure et al., 2009) frequently have difficulties with ER. Furthermore, studies with no control group were excluded, which likely excluded many relevant interventions in early stages of development and evaluation. Given the proliferation of interventions to improve ER during the past year (i.e., nearly as many articles were identified in the search for the past year for the present study as were in the search for anytime up until 2020) it is imperative to include work at all stages of development and evaluation. Although Moltrecht et al. (2020) reported non-significant changes in overall effect sizes across different developmental periods, the number of studies in each age subgroup was small. Therefore, the impact of age and development on the efficacy of ER interventions remains an open question.
A more focused examination of adolescents specifically is needed given the salience of this period in both the development of ER strategies (Ahmed et al., 2015; Riediger & Klipker, 2014) as well as the relevance of the adolescent period for the onset and continuation of psychopathology into adulthood (see Holmbeck et al., 2006). Specifically, adolescence involves a confluence of developmental changes that include significant biological and physical changes, increased cognitive capacity, and heightened demands on navigating interpersonal relationships (Casey et al., 2010). Prior work has suggested that adolescence may be a critical time of heightened plasticity to the social environment (Blakemore, 2008; Steinberg, 2005), given that the neural architecture underpinning the cognitive and social processes required for successful ER continues to develop during this period (Casey & Caudle, 2013). Successful peer relationships and psychosocial functioning may be, in part, dependent on employing adaptive ER strategies (Cronin et al., 2018). As such, this may be a salient time to teach adolescents adaptive ways to manage their emotions, possibly having a positive impact on their overall development. Thus, adolescence may represent a critical time for both reducing maladaptive ER as well as for enhancing adaptive ER to promote a healthy transition to adulthood.
This review seeks to address that gap by providing a comprehensive review of the literature examining ER-focused interventions in adolescents with a wide range of presenting disorders and including a meta-analysis of effect sizes. This review and meta-analysis builds off prior work by (1) including studies that examined both clinical and non-clinical samples that implemented ER-specific interventions, (2) systematically describing the interventions, target, and measures included in interventions in addition to providing meta-analytic estimates of effect sizes, and (3) focusing on adolescence specifically to determine the specific effectiveness of these approaches during this developmental period. This synthesis is crucial for understanding the current effectiveness of the rapidly growing ER intervention literature.
Method
Since the focus of the present review is psychosocial interventions for adolescents addressing ER, included studies must have an ER component, consistent with Gross (1998; 2015) process model of ER, taught as part of the intervention, with an adolescent sample whose mean age1 falls within the World Health Organization’s definition of adolescence (i.e., 10-19 years old). Additionally, a measure of ER must have been included at pre- and post-intervention. Much of the research is based upon small pilot studies, which use a wide range of techniques and have varying levels of methodological rigor (e.g., presence of comparison groups and type, length of follow-up periods, type of ER measure). Given the literature focusing on transdiagnostic, ER-based interventions, is still in the early stages, studies were included regardless of these methodological factors. These methodological differences will be accounted for in the meta-analysis and their potential impact on the results will be discussed.
Given the range of study populations and the number and diversity of outcomes examined in this literature, this review specifically focused on whether studies showed improvement in different component processes of ER rather than the overall effect sizes on the psychopathology or behavioral outcomes of interest. This focus was established for several reasons. First, although ER is related to multiple psychopathology outcomes investigated in these studies, the effects are likely not uniform across psychopathology dimensions, complicating interpretation of findings. For example, variations in effect sizes in outcomes could reflect both less change in ER associated with that intervention or could be due to a relatively smaller association between ER and the psychopathology outcome examined in any given study. Second, prior reviews have addressed efficacy for many interventions in targeting specific behaviors, even those related to ER (e.g., self-harm, interpersonal conflict, substance use; Ougrin et al., 2015). As such, the present review examined change in ER measures specifically to maintain its focus on this transdiagnostic process.
Literature Search
A literature search was initially conducted in January 2020 and again prior to resubmission in February 2021; a second search was conducted due to the accelerated rate at which this work has been published and to ensure all recent and relevant studies were eligible for inclusion (see Figure 1 for a flow diagram). The following search combinations were used in PubMed and PsychInfo: "emotion reg*", AND "intervention" OR "treatment" OR “training” OR “therapy” AND “adolescen*” OR “youth” contained in any field. The search elicited 1,245 articles, of which 605 were duplicates and were subsequently removed. Abstracts of the remaining 640 articles were screened for inclusion in the review based on the following criteria: (1) published in English in a peer-reviewed journal, (2) paper reports outcomes from a psychosocial intervention, (3) manuscript authors described their intervention as targeting ER and/or coping skills, and upon review by the first and second author, it fit within a broad conceptualization of ER as defined by the ER process model (Gross, 1998; 2015), (4) a pre and post measure of ER is reported, and (5) target population is adolescents per World Health Organization’s definition (Mage 10 – 19). Exclusion criteria included: qualitative case studies and samples comprised of those with substance use disorders, eating disorders, and mania or psychosis. These clinical populations were excluded for this review, given that individuals with these disorders are frequently treated in a medical milieu/inpatient treatment setting due to comorbid physical health dangers and/or primary use of psychotropic medications. Additionally, these criteria likely excluded some studies and samples whose interventions may have a significant impact on ER (e.g., interventions targeting specific problem behaviors). This work has been extensively reviewed and as such is not the focus of the present review (e.g., Mingebach et al., 2018; Reyno et al., 2006; Sukhodolsky et al., 2004).
Figure 1. PRISMA Flow Diagram of Literature Review.
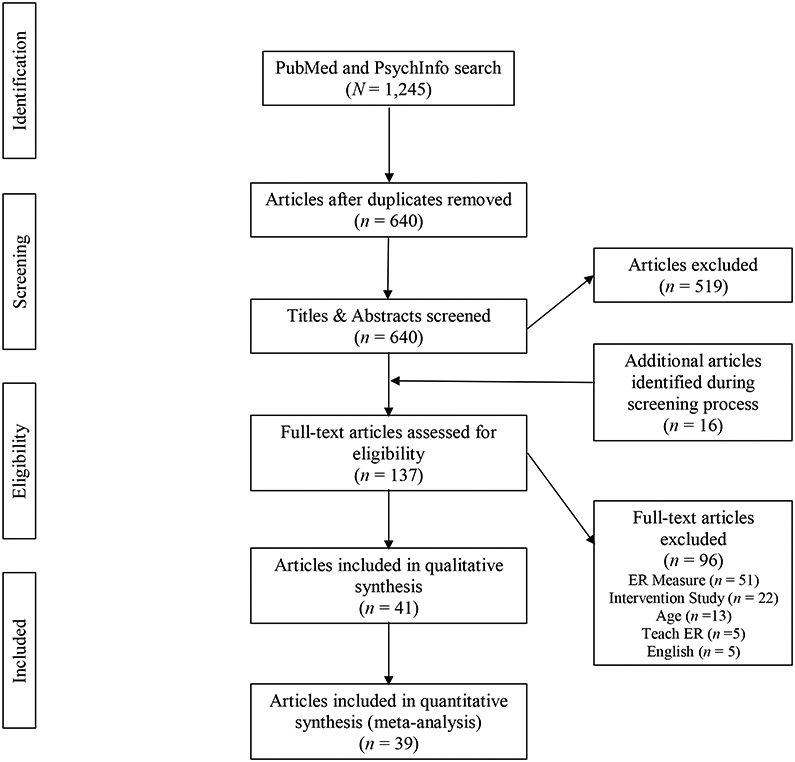
Note. Inclusion criteria were as follows: 1) Published in English in peer-reviewed journal; 2) Empirical study evaluating an intervention; 3) Intervention teaches ER skills; 4) ER measure at pre and post; 5) Mage = 10-19
Of the 640 abstracts screened, 121 articles appeared to pass inclusion criteria and were thus reviewed in full. Of note, 16 additional articles were identified through references and other sources during this process and were also include in the full review. Of the 137 articles reviewed in full, 46 studies met all the inclusion criteria; 4 of these studies met the exclusion criteria and were not included in the review. One additional study was secondary data analysis from the same sample of an already included study; as such, only the primary outcomes paper (published first) was included. This yielded a total of 41 studies meeting all inclusion criteria and no exclusion criteria and being included in the present review. See Table 1 for all included articles and their intervention and sample characteristics; see Figure 1 for the PRISMA diagram.
Table 1.
Study and Sample Characteristics of Included Articles (N = 41)
| Sample Characteristics | Study Characteristics | ||||||
|---|---|---|---|---|---|---|---|
| Author | Intervention | N | Age | % Female | Sample Type | Design | Control group |
| Afshari et al., 2014 | ECBT | 30 | 10.57 | 52.5 | Anxiety | RCT | CBT and no treatment |
| Alampay et al., 2020 | M-BCT | 186 | 11.88 | 58.6 | Low SES Filipino | RCT | Handicrafts |
| Betancourt et al., 2014 | YRI | 436 | 17.90 | 45.6 | War-affected | RCT | Control2 |
| Bjureberg et al., 2017 | ERITA | 17 | 15.31 | 100.0 | NSSI | Pilot | N/A |
| Bjureberg et al., 2018 | ERITA (online) | 25 | 15.70 | 76.0 | NSSI | Pilot | N/A |
| Breaux & Langberg, 2020 | RELAX | 18 | 13.50 | 30.0 | ADHD | Pilot | N/A |
| Broderick & Metz, 2009 | L2B | 137 | 16.9 | 100.0 | Community | Pilot | IAU |
| Claro et al., 2015 | CERTIFY | 28 | 14.20 | 29.0 | School failure risk | Pilot | Usual school supports |
| Conner et al., 2019 | EASE | 20 | 14.94 | 11.8 | ASD | Pilot | N/A |
| Cotter et al., 2020 | L2B | 11 | 14.36 | 73.0 | Obesity | Pilot | N/A |
| Cotton et al., 2016 | M-BCT | 10 | 13.20 | 80.0 | Anxiety | Pilot | N/A |
| Cotton et al., 2020 | M-BCT | 33 | 13.7 | 75.0 | Anxiety w/ BD risk | Pilot | Waitlist |
| Dingle et al., 2016 | Tuned In | 41; 216 | 14.80; 13.60 | 24.0 | At-risk/Mainstream | Pilot | N/A |
| Ford et al., 2012 | TARGET | 59 | 14.70 | 100.0 | Delinquent females | RCT | Enhanced TAU |
| Ford-Paz et al., 2019 | WOW | 960 | N/A1 | 100.0 | Community females | Pilot | N/A |
| Fung et al., 2016 | L2B | 19 | 12.7 | 57.9 | Ethnic minority w/elevated mood symptoms | Pilot | Waitlist |
| Hadley et al., 2020 | HealthTRAC | 38 | 14.71 | 60.0 | Obesity | RCT | Std Behavioral Weight Control |
| Hafeman et al., 2020 | Mindfulness | 17 | 12.1 | 60.0 | At-risk for BD | Pilot | N/A3 |
| Houck et al., 2016 | ERI | 420 | 13.00 | 47.0 | Community | RCT | Health Promotion |
| Johnstone et al., 2020 | ER Program | 295 | 11.04 | 52.5 | Community | RCT | BA and no treatment control |
| Keiley et al., 2007 | MFGI | 73 | 15.60 | 41.1 | Incarcerated | Pilot | N/A |
| Keiley et al., 2015 | MFGI | 115 | 15.70 | 0.0 | Incarcerated males | Pilot | N/A |
| Lam & Seidon, 2020 | L2B | 115 | 12.4 | 34.8 | Lowest academic tier; Hong Kong | RCT | IAU |
| Lau et al., 2020 | L2B | 111 | 15.18 | 73.0 | Elevated depression | RCT | Interpersonal Therapy Skills |
| Lindqvist et al., 2020 | Affect-focused IPDT | 76 | 16.60 | 80.0 | Depression | RCT | Supportive Therapy |
| Metz et al., 2013 | L2B | 216 | 16.5 | 34.1 | Community | Pilot | IAU |
| Newnham et al., 2015 | YRI | 32 | 18.20 | 50.0 | War-affected | Pilot | N/A |
| Punamäki et al., 2014 | TRT | 482 | 11.29 | 49.4 | War-affected | RCT | Waitlist |
| Ramdhonee-Dowlot et al., 2021 | SSL | 100 | 11.75 | 76.0 | Mauritian in RCIs | RCT | Waitlist |
| Riggs Romaine et al., 2018 | JJAM | 57 | 17.45 | 100.0 | Incarcerated females | RCT | TAU |
| Rizzo et al., 2020 | STRONG | 119 | 13.04 | 0.0 | Community males | RCT | Waitlist |
| Santomauro et al., 2016 | CBT with ER | 20 | 15.75 | 40.0 | ASD and Depression | RCT | Waitlist |
| Schoeps et al., 2018 | EEP | 360 | 12.63 | 57.0 | Community | RCT | Usual school supports |
| Schuppert et al., 2009 | ERT | 43 | 16.14 | 88.4 | Borderline traits | Pilot RCT | TAU |
| Schuppert et al., 2012 | ERT | 109 | 15.98 | 96.0 | Borderline traits | RCT | TAU |
| Suveg et al., 2009 | CBT | 37 | 10.47 | 40.5 | Anxiety | Pilot | N/A |
| Thomson et al., 2015 | SAS-OR | 13 | 10.40 | 100.0 | ASD (males) | Pilot | N/A |
| Wijana et al., 2018 | ICT | 49 | 14.60 | 85.7 | NSSI and SI | Pilot | N/A |
| Wolff & Ollendick, 2012 | CBT | 5 | 12.60 | 60.0 | ODD or CD | Pilot | N/A |
| Wolff et al., 2020 | CBT | 30 | 11.55 | 66.0 | Depression and conduct problems | Pilot RCT | N/A4 |
| Yeo et al., 2020 | DBT-A | 51 | 14.73 | 69.3 | Ethnic minority w/ NSSI | Pilot | N/A |
Note. Sample type and study design are as stated in the manuscript; YRI: Youth Readiness Intervention; ERITA: Emotion Regulation Individual Therapy for Adolescents; RELAX: Regulating Emotions Like An eXpert; L2B: Learning to BREATHE; CERTIFY: Cognitive Emotion Regulation Training Intended for Youth; EASE: Emotional Awareness and Skills Enhancement; M-CBT: Mindfulness Cognitive Behavioral Therapy; TARGET: Trauma Affect Regulation: Guide for Education and Therapy; WOW: Working on Womanhood; ERI: Emotion Regulation Intervention; ER: emotion regulation; MFGI: Multiple Family Group Intervention; IPDT: internet based psychodynamic therapy; TRT: Teaching Recovery Techniques; SSL: super skills for life; JJAM: Juvenile Justice Anger Management; STRONG: domestic violence prevention program; EEP: Emotion Education Program; ERT: Emotion Regulation Training; SAS-OR: Secret Agent Society – Operation Regulation; ICT: Intensive Contextual Treatment; NSSI: non suicidal self-injury; ADHD: attention-deficit/hyperactivity disorder; BD: bipolar disorder; RCI: residential care institution; ASD: autism spectrum disorder; SI: suicidal ideation; ODD: oppositional defiance disorder; CD: conduct disorder; RCT: randomized controlled trial; BA: behavioral activation; IAU: instruction as usual; TAU: treatment as usual.
Ford-Paz et al., 2019 reported their participants being in grades 7 through 12;
Betancourt et al., 2014 did not describe their control condition;
Hafeman et al., 2020 compared at-risk youth to a healthy control group that did not participate in the intervention no complete the ER measure at post, as such, only the at-risk group is included here;
Wolff et al., 2020 compared two methods of intervention implementation (decision rule vs. sequential treatment) for the same intervention and did not have an intervention comparison group.
Studies of ER interventions in adolescents included multiple treatment approaches, teaching both specific skills as well as aiming to reduce dysregulation, varied populations of interest, and numerous measures of ER. To facilitate interpretation of findings, we grouped the studies based upon target sample and describe the overall approach and main findings for each study within each of the following sample groups: (1) community and prevention programs or populations, (2) programs for war-affected youth, (3) programs for clinical populations (i.e., externalizing, internalizing, borderline personality, inpatient, and specialized medical/health), and (4) programs for incarcerated or delinquent adolescents.
Pooled Effect Size Analysis
Standardized mean differences were calculated for all measures of ER and included in the narrative review for each study. Pre- and post-intervention means and standard deviations were used to calculate standardized mean differences for all ER measures in line with recommendations by Morris (2008) that minimize bias and enhance precision. Effect sizes were calculated so that improvements in ER (i.e., increases in adaptive ER strategies or ER regulation, declines in maladaptive ER strategies or emotion dysregulation) were always scaled positively, whether calculated from pre- to post-intervention or between intervention and control groups. As such, any negative effect sizes reflect decreases in ER abilities or increases in emotion dysregulation. For studies with follow-up data beyond post-intervention, we included effect sizes in the narrative review, but limited analysis of pooled effect sizes to post-intervention scores only. Further, we elected to convert all mean differences to Hedge’s g due to the variation in sample size and the significant number of pilot studies with relatively smaller samples. Two studies were not included in the effect size analysis due to insufficient data presented in the original manuscript and the inability to contact the authors. As such, a total of 38 studies were included in the effect size analyses, with some papers having multiple effects included due to more than one measure of ER. Effects from the same study were weighted to account for non-independence so that no single study or effect disproportionately accounted for the results (Borenstein et al., 2011). Given the large range in methodological rigor of the included studies, a random effects model was used and pooled effects were examined separately for all studies using pre and post data and again only for those studies with an intervention and control group. Subgroup analyses were also computed to compare adaptive skill use or positive and dysregulation or negative measures of ER. Given reporting pooled effect sizes from pre-post within only one group can yield bias (Cuijpers et al., 2016) a second pooled effect was computed for studies with both an intervention and control group using a pre to post change score. Twenty-one studies with both an intervention and control group were included and again subgroup analyses were completed. To address issues of non-independence of effects given that several studies reported more than one measure of ER, a meta-regression was completed for both pooled effect analyses to determine if the individual studies were accounting for heterogeneity in effect sizes. Lastly, sample characteristics (age, sex, and sample composition) were evaluated as contributors to the heterogeneity among effect sizes. Analyses were run in R version 3.6.2 using the meta package (version 4.11).
ER Interventions for Adolescents
Of the 41 included studies, 17 were randomized controlled trials (RCTs) and 24 were pilot studies (including four effectiveness studies without randomization). Target populations ranged from community samples to prevention programs for at-risk adolescents to clinical populations (e.g., adolescents with borderline personality disorder traits, comorbid conduct problems and depression). The interventions and an overview of their effects on ER are described next, organized by population type to ease organization in description of the interventions and their findings.
Community and Prevention Programs
Thirteen community and prevention programs were identified. Four of nine studies investigated the effects of an ER intervention within school settings broadly (Alampay et al., 2020; Ford-Paz et al., 2012; Johnstone et al., 2020; Schoeps et al., 2018) with five of those eight studies investigating the effects of the specific prevention program, Learning to BREATHE within the school setting (Broderick & Metz, 2009; Fung et al., 2016; Lam & Seidon 2020; Lau et al., 2020; Metz et al., 2013), one study used a mix of at-risk youth and typical youth (Dingle et al., 2016), two studies used at-risk school samples (Claro et al., 2015; Houck et al., 2016), and one study aimed to reduce dating violence for early adolescent males (Rizzo et al., 2020).
The Schoeps et al. (2018) RCT took a preventative approach by providing an emotion education program to 148 seventh and eighth graders (ages 12-15), to help develop the adolescents’ emotional skills, to improve interpersonal relationships, reduce conflicts between peers, and improve coexistence and well-being. The emotion education program took place in 11 sessions administered over 3 months during the school day. Schools were randomly assigned to the intervention (n = 72) or control (n = 76) group. The control group did not participate in the intervention and had access to typical resources provided at the schools. There were no significant differences at post-intervention for perception, expression, or management of emotions (Hedge’s g = −.12, −.07, and −.03, respectively) relative to the control group. At the 6-month follow-up, participants in the emotion education program had significantly better emotional perception (Hedge’s g = .46) and management of emotions (Hedge’s g =.51) relative to the control group with no significant differences in expression (Hedge’s g = .09).
Next, Ford-Paz et al. (2012) examined the feasibility and preliminary outcomes of the Working On Womanhood (WOW) community-developed intervention for ethnic minority girls across multiple schools. WOW aims to serve the social-emotional needs to minority girls with specific modules focused on building emotional intelligence. Skills include learning to label and identify emotions and use coping skills to manage stress. The WOW program is delivered within the school setting using a group intervention format. The current study included 960 girls in grades seven through twelve (age not reported) and did not include a control condition. Results showed a significant decrease in emotion dysregulation at post-intervention, with a small effect size (Hedge’s g = .30).
Several studies investigated the effects of mindfulness or mindfulness-based cognitive therapy (MBCT) programs within the school setting, with three focusing on low-income and marginalized populations. First, Alampay et al. (2020) examined MBCT for Filipino children from “low-resource” schools. Participants were ages 9 to 16, with 87 participants assigned to the intervention group and 99 assigned to an active control. The intervention was in line with standard MBCT and had eight modules including modules related to ER such as increasing awareness and regulating attention, affect, and behavior. The control condition included similar amounts of activity, levels of attention from adults, and peer interaction, with time spent making crafts. Results showed significant improvements in emotion awareness in the intervention group relative to the comparison (Hedge’s g = .41) with no significant differences in non-acceptance of emotions, impulse control, or regulation (Hedge’s g = .27, −.14, and −.11, respectively).
Next, Broderick and Metz (2009) investigated the Learning to BREATHE (L2B) curriculum implemented as part of a typical health class in a private high school. L2B consists of 12 sessions organized around six themes from the BREATHE acronym: Body, Reflection, Emotion, Attention, Tenderness, Habits, and Empowerment, with six modules focusing on topics such as awareness, thoughts, and feelings. The L2B program was developed to use mindfulness to help improve ER skills in adolescents within a group setting. Participants (n = 120) in the intervention group were females in their senior year ages 17 to 19 and those in the control group were juniors (n = 17; ages 16 to 17). The control group did not participate in the intervention. The authors reported significant changes in levels of negative affect (Cohen’s d = .57; means and standard deviations not reported) in the intervention group relative to the control. However, there were no significant changes in emotion dysregulation (Cohen’s d = .28; Hedge’s g could not be calculated as means and standard deviations were not reported and attempts to gain data from authors were unsuccessful). Fung et al. (2016) also examined the L2B intervention in a pilot intervention study of ethnic minority youth. Participants were randomized to either the intervention group (n = 9) or a waitlist control group (n = 10). Relative to the those in the waitlist condition, there were improvements in emotion suppression (Hedge’s g = .57) and decreases in the use of cognitive reappraisal strategies (Hedge’s g = −.98). Using the full sample after all participants had received treatment, there were significant decreases in emotion suppression (Hedge’s g = .68) from pre to post and no significant changes in the use of reappraisal (Hedge’s g = −.26).
Similarly, Lam and Seidon (2020) examined L2B in seventh grade students from Hong Kong public schools in the lowest academic tier. Participants (Mage = 12.4) were randomized to either the L2B intervention (n = 53) or an instruction as usual control (n = 62). There were no significant changes in ER from pre to post relative to the comparison group (Hedge’s g = −.09). Metz et al. (2013) evaluated L2B in a community sample of high schools students. Participants were randomized to either the L2B condition (n = 129; Mage = 16.5) or an instruction as usual condition (n = 87; Mage = 16.4). Results showed significant improvements in ER difficulties, with a small effect size (Hedge’s g = .24). The last study to examine the L2B intervention aimed to evaluate the impact of intervention preference on intervention outcomes for a sample of ethnically diverse youth (Mage = 15.18; Lau et al., 2020). Participants completed either the L2B intervention (n = 62) or an interpersonal therapy adolescent skills training intervention (n = 49). Those in the L2B intervention compared to the interpersonal skills intervention showed larger improvements in the use of cognitive reappraisal strategies (Hedge’s g = .35), with no changes in emotion suppression (Hedge’s g = −.04) at post.
Johnstone et al. (2020) examined the effects of a preventative ER program within five schools in Australia in an RCT. Participants were children (Mage = 11.04) assigned to either the ER intervention (n = 185), behavioral activation control condition (n = 85), or a usual class control condition (n = 25). Both the ER intervention and behavioral activation control condition were delivered over eight sessions of 50 minutes each but differed in their content. The ER intervention was comprised of emotion awareness and understanding, cognitive skills (e.g., challenging unhelpful thoughts), and prevention skills (e.g., promoting adaptive ER), whereas the behavioral activation control condition consisted of identifying avoidance behaviors, understanding worry, and practicing behaviors on a “coping behaviors ladder.” There were significant improvements in the use of cognitive reappraisal strategies between the ER condition and the behavioral activation condition at post (Hedge’s g = .31), but no significant differences in emotion suppression (Hedge’s g = −.01). The findings were reversed comparing the ER condition to the instruction as usual condition with non-significant differences in reappraisal (Hedge’s g = .05) and significant improvements in emotion suppression (Hedge’s g = .49).
Next, Rizzo et al. (2021) aimed to reduce and prevent dating violence among early adolescent males (N = 119; Mage = 13.0) through the Project STRONG intervention. The goal of this intervention is to teach relationship health knowledge, ER, and communication skills. Participants (and a parent) were randomized to either the intervention condition (n = 59) or a waitlist control condition (n = 60). The intervention consisted of six online modules completed across four weeks (1-2 modules per week) in the context of a game in which players must work to restore healthy relationships and reduce violence on an alien planet. ER skills taught were adapted from project TRAC (developed in Houck et al., 2016 described on page 18). There were no significant changes from pre to post on any of the ER measures (Hedge’s g ranged from −.07 to .07).
Dingle, Hodges, and Kunde (2016) included a mix of at-risk youth (n = 41; 76% male) and typical female students (n = 216) to validate the ER intervention Tuned In through an effectiveness trial. Tuned In focuses on improving ER and emotional identification, labelling, and awareness through music. Each session focuses on a different emotion and considers the valence (i.e., positive or negative) and arousal levels (i.e., high or low) associated with that emotion. In the at-risk sample, results showed significant increases in emotional awareness (Hedge’s g = .54), emotion identification (Hedge’s g = .54), and use of healthy emotion management strategies (Hedge’s g = .49) from pre to post-intervention. Similar improvements were also observed in the typically developing female students from pre- to post-intervention in regard to emotional awareness (Hedge’s g = .75), emotion identification (Hedge’s g = .39), and management (Hedge’s g = .57). Additionally, the at-risk youth exhibited a significant decrease in emotional suppression (Hedge’s g = .64), but also a decrease in emotional reappraisal (Hedge’s g = −.52).
The first study using an at-risk school sample aimed to teach cognitive ER strategies through a group intervention (Claro et al., 2015). This sample consisted of 28 adolescents ages 12 to 17 who were at-risk for school failure, who took part in the CERTIFY (Cognitive Emotion Regulation Training Intended for Youth) intervention. Among the participants, 13 adolescents who were not at-risk for school failure and did not take part in the intervention served as a control group. Importantly, their design of selecting a healthier control group with high adaptive skills at baseline may have inflated the effect sizes when comparing across groups. CERTIFY uses a two-pronged approach in that it seeks to both reduce maladaptive cognitive ER while increasing adaptive cognitive ER strategies in adolescents. Each of the eleven sessions work to teach adolescents about cognitive ER, the possible strategies one can use to regulate their emotions, and work towards increasing the likelihood of using the beneficial cognitive ER strategies. For adolescents in CERTIFY, the use of self-reported adaptive cognitive ER skills significantly increased from pre- to post-intervention (Hedge’s g = 1.07) relative to the control; notably, however, this effect size may be inflated, given that the control group exhibited a relatively large decline in adaptive cognitive ER skills over the course of the intervention (Hedge’s g = .40 for just the intervention group pre to post). In contrast, maladaptive cognitive ER skills were not successfully reduced post-treatment for those in the intervention group relative to controls (Hedge’s g = −.61).
Finally, the Houck et al. (2016) study sought to prevent negative outcomes for adolescents at risk for sexual activity and other health risks. The study consisted of 420 seventh graders (ages 12-14) at risk for negative health outcomes due to emotional/behavioral problems or suspected sexual behavior or substance use. Participants were randomly assigned either to an ER intervention or a health promotion intervention. The ER intervention aimed to improve ER skills, to decrease poor decision making that results in unplanned sex, substance use, or physical aggression. The intervention provided psychoeducation on emotions, how emotions and behaviors relate, and recognizing triggers. Additionally, the intervention taught ER strategies for handling decision making including getting away from the trigger, coping skills to release emotional energy in positive ways, and using cognitive reappraisal. Participants in the ER intervention were better able to identify emotion expressions at 6-month follow-up (but not 12-month follow-up) relative to the health risk intervention group, the overall impact of the intervention on ER skills was not significant at either 6-month follow-up (Hedge’s g ranging from −.06 to .08) or 12-month follow-up (Hedge’s g ranging from .00 to .07).
Programs for War-Affected Affected Youth
Three studies investigated the use of an ER intervention on war-affected youth with two RCTs (Punamäki et al., 2014; Betancourt et al., 2014) and one pilot study (Newnham et al., 2015). Punamäki et al. (2014) used the Teaching Recovery Techniques (TRT) intervention which is based in CBT and aims to develop effective coping skills and adaptive ER across two weekly four hour sessions for four weeks. This study included a large sample size (N = 482, Mage = 11.29) of Palestinian adolescents that had been exposed to war. Half the sample was randomized to the intervention condition of group sessions over six weeks, while half was placed in the waitlist control group. Participants in both the TRT intervention and the control group increased in the amount of regulation for feelings of fear, anger, and sadness. However, the TRT group did not significantly outperform the control group on any outcome measure from baseline to post-intervention or 9-month follow-up. Notably, the TRT group’s scores on ER did not improve substantially during the intervention or follow-up (Hedge’s g ranging from −.19 to .02).
The second RCT investigated the Youth Readiness Intervention (YRI) in a sample of 436 (Mage = 17.9) adolescents exposed to war-related trauma from Sierra-Leone (Betancourt et al., 2014). The aim of the YRI, developed from CBT and interpersonal therapy, is to teach ER, anger management, and problem-solving skills though 10 group sessions to address emotion dysregulation, risky behaviors, and functional impairments. The sample was randomly assigned to either the YRI condition or a control group which did not receive the intervention. Results showed significant improvements in ER post-intervention for the YRI group relative to the control group (Hedge’s g = .45), but no significant differences between groups by 6-month follow-up were found (Hedge’s g = .03). The pilot study investigating the feasibility of the YRI with war-affected adolescents (N = 32) from Sierra-Leone (Mage = 18.2; Newnham et al., 2015) also found ER to significantly increase from baseline to posttest with a moderate effect size (Hedge’s g = .73). Overall, there appears to be some initial promising results for the use of ER interventions in youth affected by war, though with additional RCTs needed.
Programs for Clinical and Health Populations
Twenty studies examined the effects of an ER intervention within specific clinical and health populations2. Specifically, three used samples with primarily externalizing behaviors (Breaux & Langberg, 2020; Wolff & Ollendick, 2012; Wolff et al., 2020), four with internalizing behaviors (Afshari et al., 2014; Cotton et al., 2016; Lindqvist et al., 2020; Suveg et al., 2009), two with those at risk for bipolar disorder (Cotton et al., 2019; Hafeman et al., 2020), three with autism spectrum disorder (ASD; Conner et al., 2019; Santomauro et al., 2016; Thomson et al., 2015), two with borderline personality disorder/traits (Schuppert et al., 2009, 2012), four aimed at preventing and reducing non-suicidal self-injury (NSSI; Bjureberg et al., 2017, 2018; Wijana et al., 2018; Yeo et al., 2020), and one with youth in residential treatment centers (Ramdhonee-Dowlot et al., 2021). Lastly, two studies examined ER interventions in the context of obesity (Cotter et al., 2020; Hadley et al., 2020).
Externalizing disorders.
Both interventions for adolescents with externalizing behaviors were pilot studies. Breaux and Langberg (2020) examined the RELAX (Regulating Emotions Like An eXpert) intervention in a small (N = 18) sample of adolescents (Mage = 13.5 years) with attention deficit/hyperactivity disorder (ADHD) and their caregivers. RELAX aims to improve ER and decrease family conflict through teaching both the adolescent and the caregiver ER strategies in addition to communication and conflict management skills. RELAX is delivered via 90-minute group sessions for 8 weeks with the first 60 minutes consisting of separate parent and adolescent skills and psychoeducation-based groups and 30 minutes of consisting of the parents and adolescents working together to problem solve and identify skills to use during the following week. Content includes ER and coping strategies, CBT principles, emotion awareness and identification, and sharing emotions in adaptive ways. Results showed large improvements in ER per both adolescent (Hedge’s g = .49) and parent report (Hedge’s g = .68). Adolescent emotion dysregulation as rated by the intervention clinicians also significantly decreased from pre to post (Hedge’s g = 1.78).
The second study using an externalizing sample, specifically adolescents with a primary diagnosis of oppositional defiant disorder or conduct disorder, was a small pilot study including five adolescents (ages 11-14; Wolff & Ollendick, 2012). The intervention delivered was a flexibly implemented CBT consisting of 11 to 16 weekly 60-90-minute sessions, that was developed based on the Treatment for Adolescent Depression Study (March et al., 2003), parent management techniques, and collaborative problem-solving techniques (e.g., Kazdin et al., 1992; Greene, 1998). Affect identification and regulation was one of 10 major components of the intervention. A significant reduction in parent-reported ER difficulties was found post-intervention (Hedge’s g = 1.46) and these reductions were maintained at a 1-month follow-up.
Lastly, Wolff et al. (2020) examined the effects of a transdiagnostic intervention for youth with comorbid conduct problems and depression. Although the aim of the RCT was to evaluate the effects of decision rule, using the transdiagnostic intervention (n = 19; Mage = 12.6), versus sequential treatment, using a combination of CBT and parent management training (PMT; n = 11; Mage = 10.5), both intervention conditions contained ER material and pre- and post-intervention ER measures and will be considered. The transdiagnostic decision rule condition consisted of six core sessions (e.g., emotion coaching, ER, problem solving) plus additional CBT content. The order of the intervention sessions was delivered based upon identified deficits or problem areas, as well as strengths, prior to and throughout the intervention. Participants in the sequential CBT/PMT treatment were randomized to either start with CBT (six sessions) or start with PMT (six sessions) with the remaining sessions being content from either intervention based, decided by the clinician. Participants assigned to the transdiagnostic decision rule-based treatment exhibited significant improvements in ER difficulties (Hedge’s g = .89) and those in the sequential CBT/PMT condition did not show significant changes in ER difficulties at post (Hedge’s g = .11).
Internalizing disorders.
Four studies used samples of youth with primarily internalizing disorders. First, Afshari et al. (2014) completed a small RCT evaluating emotion-focused CBT compared to CBT and a no treatment control with 10 youth in each condition (total N = 30; Mage = 10.57) diagnosed with separation anxiety disorder. While broad CBT skills were used in both CBT interventions, the CBT only condition focused on managing anxiety only whereas the emotion-focused condition included greater use of emotion identification and regulation skills as well as focused on emotions outside of anxiety. Participants took part in 10 1-hour weekly session in the CBT condition and the same in the emotion-focused condition, with two additional parent sessions. Results showed significant improvements at post-intervention in both dysregulation and adaptive skill use (Hedge’s g = .54 and .56, respectively) for the emotion-focused CBT condition relative to the CBT condition and between the emotion-focused CBT condition and no treatment control condition (Hedge’s g = .90 and 1.04 for dysregulation and adaptive ER, respectively). Cotton et al. (2016) completed a pilot study of a mindfulness-based CBT with 10 adolescents (Mage = 13.2) from an anxiety clinic. This intervention was a 12-week group intervention during which participants learned to identify their thoughts, emotions, and body sensations. Parents rated their child’s ER at pre and post. Results showed an improvement in adolescent ER post intervention, with specific decreases in emotional lability (Hedge’s g = .52) and increases in the use of regulation strategies (Hedge’s g = .60).
The next study (Suveg et al., 2009) also utilized young adolescents from an anxiety clinic (N = 37, Mage = 10.47) and implemented a small pilot study of CBT for anxious youth. Participants received either individual or family CBT, depending on the location of services, for 16 one-hour sessions delivered on a weekly basis. Results showed significant improvement in emotional awareness and identification at post (Hedge’s g = .71). There were also some improvements of ER of worry and sadness: emotional suppression decreased for both worry (Hedge’s g= .63) and sadness (Hedge’s g = .58), and worry dysregulation and use of emotional coping both improved (Hedge’s g = .81 and .58, respectively). There were no significant improvements for ER of anger (Hedge’s g ranging from .16 to .24).
The last study using a sample with internalizing disorders investigated the effects of an affect-focused internet-based psychodynamic therapy for youth with major depression (Lindqvist et al., 2020). Participants had to meet criteria for major depression and were randomized to the intervention condition (n = 34) or to a supportive control condition (n = 38). The intervention consisted of eight modules based in the psychodynamic orientation and including ER skills (e.g., mindfulness skills, evaluating long-term and short-term consequences, avoidance and acceptance, communication) with the goal of decreasing emotional avoidance and increasing openness to and acceptance of emotions. The intervention and the supportive control condition were delivered online with weekly contact from their assigned therapist and tracking of symptoms and well-being. There were significant improvements in ER difficulties in the intervention condition relative to the comparison condition (Hedge’s g = .91).
Bipolar disorder.
Two additional studies examined the effects of MBCT for youth at risk for bipolar disorder (e.g., one parent with a bipolar disorder diagnosis). In Cotton et al. (2020) participants were those diagnosed with anxiety and at increased risk for bipolar disorder. Participants were randomized to MBCT (n = 24; Mage = 13.6) or a waitlist control period (n = 19; Mage = 13.8). Results post intervention showed non-significant changes in ER (Hedge’s g = −.14 for lability and −.21 for regulation) relative to the waitlist control. The second study, Hafeman et al. (2020) used an intervention based in MBCT and mindfulness-based stress reduction to examine changes in resting state functional connectivity in youth at risk for bipolar disorder. Youth took part in an 8-week MBCT intervention and completed measures pre- and post- intervention. Results showed significant improvements in the use of cognitive reappraisal strategies (Hedge’s g = .46) and no change in emotion suppression (Hedge’s g = .14) at post.
Autism spectrum disorder (ASD).
Two pilot studies and one RCT investigated how ER interventions work for adolescents diagnosed with ASD. The first study included 20 participants diagnosed with ASD (Mage = 14.94) who piloted the Emotional Awareness and Skills Enhancement Program (Conner et al., 2019). This was a 16-week one-on-one therapy aiming to build ER skills through decreasing problem behaviors, increasing adaptive skills, and using mindfulness techniques. It is considered a transdiagnostic approach and can be delivered flexibly in 45–50-minute sessions each week. There was no control group. Per parent report, there were significant decreases in emotional reactivity at post-intervention.
The second study included 13 males with ASD (Mage = 10.40 years) who took part in the Secret Agent Society, Operation Regulation intervention (SAS-OR; Thomson et al., 2015). SAS-OR was developed from the well-studied Jr. Detective Program (Beaumont & Sofronoff, 2008) with a focus on ER. Content of the 10 hour-long sessions with the adolescent and parent included identifying stressful situations and triggers, building emotional awareness and emotion recognition, and developing alternative adaptive responses. Results showed significant decreases in emotional lability (Hedge’s g = .39) and decreases in total dysregulation for worry, sadness, and anger (Hedge’s g = .55). There was no significant change in ER broadly (Hedges g = −.13).
The third study using a sample with ASD was specifically investigating the effect of a CBT based intervention with a focus on ER within adolescents with ASD and comorbid depression (Santomauro et al., 2016). Twenty adolescents (Mage = 15.75) took part in the intervention with 10 being randomized to the intervention condition and ten placed on a waitlist. The intervention included 3-4 participants in a group with 11 one-hour sessions focused on teaching strategies to manage symptoms of depression (e.g., identify feelings and thoughts, expressing emotions in adaptive ways). All youth (regardless of condition) exhibited significant increase in the use of cognitive reappraisal strategies when examined together at post-intervention (Hedge’s g = .79). There were no significant findings for changes in expressive suppression (Hedge’s g = .12).
Borderline personality traits.
One pilot study and one RCT examined the effectiveness of ER interventions for adolescents with borderline personality disorder traits. In a pilot study, Schuppert et al. (2009) explored the effectiveness of an ER training in addition to treatment as usual for 43 adolescents (ages 14-19) with borderline personality disorder traits compared to only treatment as usual (which may have included medication, therapy, and the use of emergency services). Adolescents were randomly assigned to one of the two conditions. The ER training consisted of 17 weekly 105 min group meetings and two booster sessions at 6- and 12-weeks post-treatment. The ER training sought to provide adaptive coping strategies for affective instability, daily stressors, and psychological vulnerability, and to reduce harmful behaviors (i.e., self-harm, harm to others), by providing psychoeducation on ER, increasing awareness of behavior and emotion patterns, and ER skills (e.g., taking space, challenge negative or distorted assumptions). This study found no significant improvement post-intervention in affect regulation in the intervention group (Hedge’s g = .18) or relative to the control group (Hedge’s g = .03). ER locus of control, however, significantly improved in the intervention group relative to the control group (Hedge’s g = 1.22). In 2012, Schuppert et al. examined the same ER training in a larger RCT (N = 109, ages 14 - 19) and again compared the intervention to treatment as usual. The intervention group experienced significant improvements in affect regulation (Hedge’s g = .54); however, the treatment group did not improve significantly more than the control group (Hedges g = .12).
Non-suicidal self-injury.
In an effort to reduce or prevent NSSI, Bjureberg et al. (2017) conducted an uncontrolled open trial with N = 17 adolescent females (Mage = 15.31) who took part in Emotion Regulation Individual Therapy for Adolescents (ERITA), a 12-week intervention including modules such as increasing emotional awareness, using ER strategies, and how to control impulses. Additionally, parents followed along with the intervention sessions via an online program. Self-reported difficulties regulating emotion was reported weekly throughout treatment and had significantly decreased by post-treatment (Hedge's g = .59) and these improvements were largely maintained by 6-month follow-up (Hedge’s g = 1.34 from pre to 6-month follow-up). Bjureberg et al. (2018) built upon this work with a second pilot study which used a completely online version of ERITA in which 25 adolescents (Mage = 15.7) took part. Not only was this version of ERITA further adapted based upon feedback from participants in the first sample, but Bjureberg et al. (2018) again included three and six-month follow-up periods to examine long-term effects of the online version of ERITA. Through the online version, treatment providers would give feedback on progress and homework assignments via the online platform or phone app and would provide phone guidance as necessary. Emotion dysregulation consistently declined from pre-treatment through to six-month follow-up with significant differences from pre-treatment to post-treatment, post-treatment to 3-month follow-up, and pre-treatment to 6-month follow-up (Hedge’s g = .62, .38, 1.20, respectively).
Wijana et al. (2018) included a sample of 49 adolescents (Mage = 14.60) who have self-harmed or are suicidal. The Intensive Contextual Treatment for Self-harm intervention was piloted which focuses on improving effective ER and includes a plan for maintenance once treatment ends. At post treatment, there was a significant increase in cognitive reappraisal (Hedge’s g = .46) and no significant change in expressive suppression (Hedge’s g = .19). From the post-treatment to 6- and 12-month follow-ups, the improvement in cognitive reappraisal was maintained (as indicated by a non-significant Hedge’s g = −.19 and −.01 for 6 and 12 month, respectively). Lastly, Yeo et al. (2020) examined the effects of DBT for ethnic minority adolescents who engage in self-harm and have poor self-regulation. Participants were 51 youth (Mage = 14.73) who were engaging in outpatient treatment and referred to a DBT outpatient program due to their history of self-harm. Results showed significant effects from pre to post intervention in reducing emotion dysregulation (Hedge’s g = .84).
Residential treatment centers.
Ramdhonee-Dowlot et al. (2021) evaluated the effects of the Super Skills for Life (SSL) program for youth in residential treatment centers in Mauritius using an RCT. Participants (N = 100; Mage = 11.75) all had been identified as having moderate to high levels of emotional or behavioral problems and were assigned to either the intervention condition or a waitlist control. Those assigned to the SSL intervention (n = 50) participated in eight CBT-based sessions using a transdiagnostic approach to treat emotional and behavioral disorders and includes behavioral activation, communication skills, and feedback on their skill use in a group setting. Participants in the SSL condition showed significant decreases in the use of maladaptive cognitive ER strategies, with large effects (Hedge’s g = 1.58), as well as significant increases in the use of adaptive ER strategies (Hedge’s g = .78) relative to the waitlist group.
Obesity.
Cotter et al. (2020) and Hadley et al., (2020) examined the effects of mindfulness-based interventions within individuals with obesity. Cotter et al. (2020) investigated the previously described L2B intervention in a small sample (N = 11) of adolescents (Mage = 14.36). The authors describe the importance of using ER strategies within interventions for these populations given the connections between emotions and eating. There were no significant changes in ER difficulties from pre to post (Hedge’s g = .04). The final study (Hadley et al., 2020) examined the HealthTRAC intervention. HealthTRAC was developed specifically for this population and is a combination of a standard weight management intervention and an ER intervention (the same ER intervention used in Houck et al., 2016). Each session included a weight control component (e.g., physical activity) and an ER component (e.g., recognizing triggers for feelings) for a total of 14 sessions. The sessions were divided into “skill training” for the first half and “skill application” for the second half. Participants randomized to the intervention condition (n = 19; Mage = 14.89) or the control condition (a standard weight management intervention; n = 19, Mage = 14.53). Those assigned to the HealthTRAC condition showed significant improvement on ER strategies specifically taught in the intervention compared to the comparison group (Hedge’s g = .84). Relative to the comparison group, participants also reported significant increases in ER difficulties (Hedge’s g = −.28) and no significant changes in affect regulation (Hedge’s g = −.08). There were also significant changes in parent-reported ER from pre to post, the effect sizes were small when compared to the comparison group (Hedge’s g = −.15 for lability and −.09 for regulation).
Programs for Incarcerated or Delinquent Adolescents
The final four studies investigated ER interventions in the context of incarcerated (Keiley et al., 2007, 2015; Riggs Romaine et al., 2018) or delinquent (Ford et al., 2012) adolescents. First, an effectiveness trial was conducted for the Multiple Family Group Intervention (MFGI) for incarcerated adolescent males (N = 115; Mage = 15.70) who had sexually offended (Keiley et al., 2015). This intervention helps participants manage tense and difficult situations through learning to work through high arousal and respond differently when those types of emotions arise. Parents meet with the adolescent and group leaders to help build positive and supportive relationships. MFGI was originally piloted by Keiley (2007) in a smaller trial of 73 incarcerated adolescents (Mage = 15.6) which showed small but significant improvements in affect regulation from pre to post intervention (all ps < .05; effect sizes and means and standard deviations not reported). The larger effectiveness trial indicated that according to adolescent-, mother-, and father-report MFGI significantly decreased maladaptive ER from pre to post-intervention (Hedge’s g = .16, .36, .04, for adolescent, mother, and father, respectively). Importantly, according to adolescent’s own report maladaptive ER remained decreased through the 1-year follow-up period (Hedge’s g = .38). The third study used a sample of incarcerated girls (N = 57, Mage = 17.45) to determine the effectiveness of the Juvenile Justice Anger Management (JJAM) which aims to build problem solving, coping, and ER skills through 16 group sessions, twice weekly, for 90-minutes (Riggs-Romaine et al., 2012). Participants were randomized to either the JJAM condition (and were allowed to continue their treatment as usual) or a treatment as usual only condition. JJAM did not significantly increase positive cognitive ER (Hedge’s g = .11) nor did it significantly decrease negative cognitive ER (Hedge’s g = .43), although the change in negative cognitive ER was marginally significant.
The final study by Ford et al. (2012) used an adolescent sample of delinquent girls (N = 59; Mage = 14.7) to investigate the effectiveness of the TARGET (Trauma Affect Regulation: Guide for Education and Therapy) intervention. Participants were randomized to either the TARGET condition or an enhanced treatment as usual group which included supportive therapeutic services to help the adolescent identify goals and ways of achieving them. TARGET including 12 weekly individual sessions. Results showed an improvement in ER from pre to post, for the TARGET group relative to the enhanced treatment as usual condition (Hedge’s g = .34).
Results of Pooled Effect Size Analysis
Thirty-nine studies were included in the pooled effect size analysis of pre to post treatment change in ER, given data was unable to be obtained from two studies included in the narrative review (Broderick & Metz, 2009; Keiley, 2007). There were 84 total effects (i.e., measures of ER) included (see Figure 2) with 52 negative or dysregulation measures and 32 positive or adaptive skill measures. As noted earlier, all effects were scaled so that positive effects sizes indicated either an increase in adaptive skills or a decrease in dysregulation whereas a negative effect indicates a decrease in adaptive skills or an increase in dysregulation such that effective interventions would always yield positive effect sizes, regardless of the measures used in the study.
Figure 2a. Forest Plot of Pooled Effect Size Analysis for Pre and Post Effects, Adaptive ER Effects.
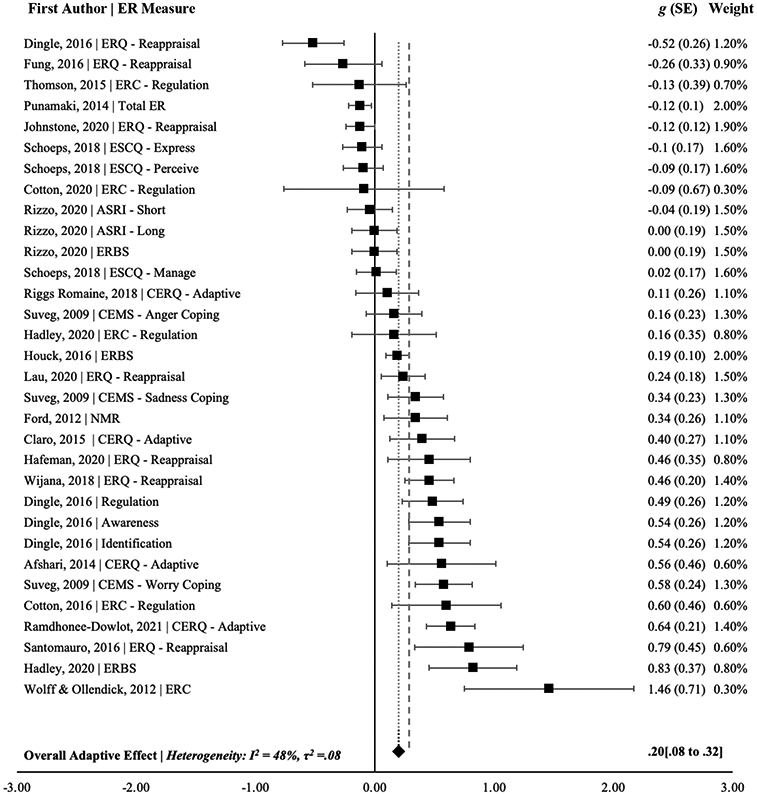
Effect sizes from pre to post treatment ranged from a Hedge’s g of −.19 (Lam & Seidon, 2020) to 1.07 (Ramdhonee-Dowlot et al., 2020) for changes in emotion dysregulation and −.52 (Dingle et al., 2016) to 1.46 (Wolf et al., 2012) for changes in adaptive regulation or skill use. The overall pooled effect from pre to post treatment on ER was significant (Hedge’s g = .29, 95% CI [.22, .36], p < .001) with moderate heterogeneity related to study (I2 = 54%, τ2 =.07) and a prediction interval of Hedge’s g −0.24 to .82. Subgroup analyses showed significant effects regarding reduction in maladaptive or negative ER (Hedge’s g = .35, 95% CI [0.26 to 0.43], p < .05, I2 = 53%, τ2 =.06) and improvement in positive or adaptive ER strategies (Hedge’s g = .20, 95% CI [.08 to 0.32], p<.05, I2 = 48%, τ2 =.08). Given the moderate heterogeneity in effects, a meta-regression was conducted to assess the effects of the individual studies. There was a significant effect of study on the heterogeneity of effect sizes, F(40, 43) = 2.09, p = .009, with 31.25% of the heterogeneity in effect sizes accounted for by study.
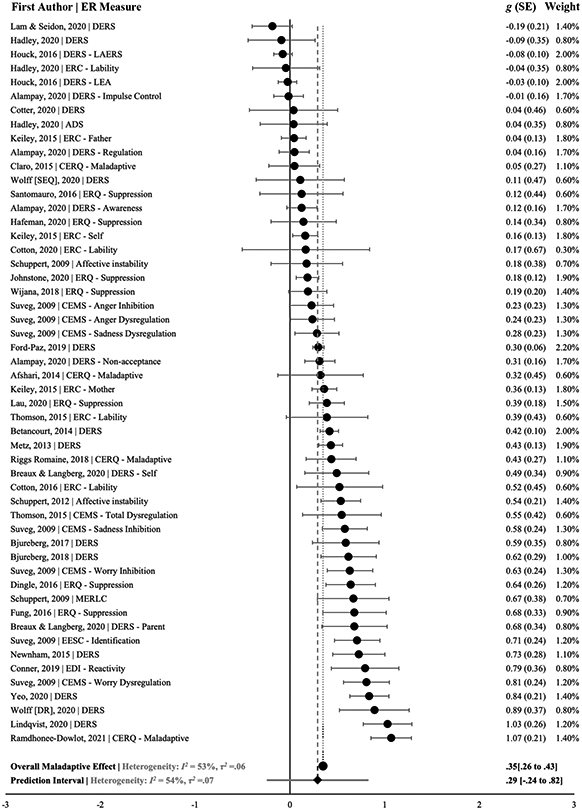
Twenty-two studies with both an intervention and control group were included in the pooled effect size analysis with 49 total measures of ER (see Figure 3). There were 27 effects capturing change in dysregulation and 22 effects capturing change in adaptive regulation. Effect sizes of the intervention relative to the control group ranged from a Hedge’s g of −.61 (Claro et al., 2015) to 1.58 (Ramdhonee-Dowlot et al., 2021) for the dysregulation effects and from −.98 (Fung et al., 2016) to 1.07 (Claro et al., 2015) for the adaptive effects. The overall pooled effect was significantly different from zero (Hedge’s g = .19, 95% CI [.06 to .32]) with a moderate to large amount of heterogeneity related to study (I2 = 69%, τ2 =.17, p<.01) and a prediction interval of Hedge’s g −.61 to 1.00. Subgroup analyses for the dysregulation effects showed an overall small effect of ER interventions ability to decrease dysregulation (Hedge’s g = .22, 95% CI [.03 to .41], I2 = 74%, τ2 =.18, p<.01). By contrast, ER interventions did not show a significant effect relative to control groups in improving adaptive ER skills (Hedge’s g = .16, 95% CI [−.02 to .33], I2 = 56%, τ2 =.13, p<.01). There was no significant effect of study on the heterogeneity of effect sizes, F(23, 25) = 1.35, p = .233, with 12.41% of the variability being accounted for by study.
Figure 3. Forest Plot of Pooled Effect Size Analysis for Studies with an Intervention and Control Group for Both the Dysregulation and Adaptive ER Effects.
Lastly, given the heterogeneity in effects found above, several additional meta-regressions were examined assessing the effects of age, given the wide age range in the present sample (Mage = 10-19), sex, given the ranges of proportions of males to females, and sample types, dichotomized to be community vs. clinical. Meta-regressions were completed on the intervention effects for both the pre-post studies and those with a control and intervention groups. For the pre-post studies, there was no significant effect of age3 (F(1, 80) = 1.31, p = .254), with 0.05% of the heterogeneity in effect sizes accounted for by age. Similarly, for studies with an intervention and control group, no significant proportion (0.00%) of heterogeneity in effects were accounted for by age (F(1, 47) < .01, p = .957). Next, for the pre-post studies, sex was also not significantly associated with the heterogeneity in effect sizes (F(1, 81) = 3.85, p = .053), with 3.05% of the heterogeneity being accounted for by sex. For those studies with an intervention and control group, results were similar and sex was again not associated with heterogeneity in effect sizes with only 3.36% being accounted for (F(1, 47) = 2.84, p = .099).
By contrast, results indicated that effect sizes significantly differed with sample composition (clinical versus community). Studies were designated as clinical samples if they included sampling of individuals based on a specific diagnosis or degree of symptom severity, whereas studies were designated as community if individuals were not sampled based on youth clinical characteristics. Meta-regressions were significant when examining the effects of sample composition for all included studies with pre and post effects, [F(1, 82) = 20.73, p < .001 using clinical populations as the reference group]. Community samples showed significantly lower effect sizes on average (by .29 Hedge’s g units, p < .001) compared to clinical populations. Overall, 18.3% of the heterogeneity in pre and post effect sizes was accounted for by sample composition. Similarly, sample composition also significantly predicted heterogeneity in effect sizes for intervention effects with control groups [F(1, 47) = 5.68, p = .021]. Again, community samples had significantly lower effect sizes, on average (by .29 Hedge’s g units, p = .021) than clinical samples. Overall, 8.3% of the heterogeneity in effects in those intervention studies employing a control group was accounted for by sample composition.
Discussion
Across ER intervention programs for adolescents, there are a wide variety of implementation modalities (individual, group, and school-wide), variability in the rigor of research designs (comparison groups, follow-up periods), and different facets of ER taught and/or measured. Overall review of this literature revealed that interventions to improve ER skills, either by increasing adaptive strategies and/or reducing maladaptive strategies, may be helpful for a range of adolescent populations. Our meta-analytic results indicated a significant overall improvement in ER across all studies from pre to post-intervention (Hedge’s g = .28). These effects appeared to be quite variable (ranging from −0.52 to 1.46), and meta-regression analyses indicated study significantly predicted the heterogeneity in the pooled effect size. However, this is consistent with prior meta-analyses of interventions for internalizing and externalizing behaviors in youth (e.g., Battagliese et al., 2015; Ishikawa et al., 2007; Maughan et al., 2005; Michael et al., 2002). Effects were also larger in pilot and non-controlled studies; however, the overall pooled effect size estimate was still significant (albeit small in magnitude) in studies that included a control group (Hedge’s g = .16). Notably, effect sizes capturing reductions in maladaptive ER were larger in controlled studies relative to those capturing improvements in adaptive ER. Neither age nor sex were significant predictors of the variability in effect sizes, whereas sample composition (clinical versus community) clearly impacted effects, with larger effects observed in clinical relative to community samples.
Several factors are likely contributing to the range in effect sizes, which demonstrated moderate to substantial heterogeneity, as indicated by the I2 values. First, effects observed in non-controlled studies may be overestimating the impact of ER interventions, given that these studies cannot disentangle improvement due to the intervention or a regression to the mean over time. Of the 41 studies reviewed, only 22 studies used a control group and the types of control groups examined varied widely, from wait-list control, treatment as usual, or other related interventions. In some cases, this likely led to an over-estimation of effects such as Claro et al. (2015) using a healthier by design control group (i.e., comparing an at-risk school sample to students not at-risk). Of note, Claro et al. (2015) demonstrated the largest overall effect from pre to post of those studies with intervention and control groups, and it is likely that this effect is inflated due to the study design. In total, 13 of the 22 studies with a control group included an active control condition (e.g., comparison treatment or instruction protocol), which may indicate that interventions with a specific ER component were not resulting in significant improvements over and above other active, evidenced-based interventions or instructional programs. Future work will benefit from using methodologically rigorous comparison groups and working to decompose whether the addition of an ER curriculum incrementally improves the efficacy of an intervention specifically beyond the traditional methods employed.
Second, the types of interventions delivered varied substantially in terms of their focus on ER skills specifically, their duration and dose (e.g., once per week, twice per week, one- or two-hour sessions, total number of sessions), and the populations and contexts in which they were administered (during school, within treatment clinics, group and individual formats). Notably, the largest effect sizes were generally observed in studies measuring a reduction in emotion dysregulation or maladaptive ER strategies among youth with clinical diagnoses. The smallest effect sizes were generally observed for changes in maladaptive ER in studies implementing prevention programs for community youth. Intervention duration and dosage varied substantially among studies producing both small and large effects. Thus, although clinical samples may yield a general pattern of larger effects of ER interventions, it is important to note this may be driven by floor effects (e.g., community populations have less severe ER concerns at baseline and thus less room to improve). Still, future work is needed to determine whether intervention dosage and/or duration impacts improvement both at post-treatment and at follow-up systematically, and whether these effects vary based on diagnoses, age, and or other sample characteristics.
Samples also differed in age and sex composition, as well as which instruments and raters were used to assess ER. Although sex and age were non-significant predictors of study heterogeneity, it will be important moving forward to elucidate for whom and how these interventions are most efficacious. The lack of significant effects of age on the efficacy of ER interventions within adolescent samples may be due to several factors (e.g., insufficient power to detect small moderation effects, age as a poor proxy for developmental effects), including potentially small or absent effects on age and development on intervention efficacy during adolescence. It is important to note that the lack of age moderation should not be equated with a lack of age and developmental effects on the development of ER skills in general. Notably, effects of ER interventions are understudied in older adolescent samples (i.e., late high school, 17-19). This may be an important developmental period during which to teach ER skills given the increases in autonomy and additional social developments (e.g., romantic relationships) that occur in late adolescence.
In addition to age and sex, measurement characteristics should be carefully considered when interpreting these findings. There appears to be misalignment in some studies between intervention targets, which often seek to equip adolescents with adaptive coping and ER strategies and measures of ER used. That is, many of the commonly used, validated measures of ER (e.g., the Difficulties with Emotion Regulation Scale, the Emotion Regulation Checklist) assess negativity/lability or emotion dysregulation; in fact, 62% of the measures in the current review were negative or dysregulation measures, with 19 of the 41 studies only including a dysregulation or maladaptive measure of ER. Other positive or adaptive measures assess only cognitive ER strategies (e.g., emotion suppression, cognitive reappraisal) rather than broadly assessing engagement in positive coping and ER behaviors (e.g., engaging in a positive activity such as exercise or talking to a friend, taking space, and deep breathes to calm down), that are often a focus of these interventions. Although engagement in adaptive or positive ER behaviors likely is correlated with a reduction in emotion dysregulation, this is not typically examined directly in intervention research, with different ER outcomes being viewed as independent outcomes, often with different effects. As such, it will be critical for future intervention research to better align ER measures with specific intervention targets and to disentangle how improvements in certain emotion awareness/ER strategies learned early in the intervention may lead to improvements in more global dysregulation in daily life over time. In this vein, one of the primary reasons a study was excluded from the present review was due to lack of including any ER measure, despite the intervention having a focus on ER (occurred for 51 of the 96 articles excluded during full text review). Further, only five of the 17 ER measures used across included studies were considered to have strong evidence for reliability and validity. Including valid, reliable, and aligned measures will be integral for ER intervention work moving forward. Additionally, utilization of ecological momentary assessment and/or ecological momentary intervention could be useful to see how specific ER strategies in daily life link to negative or dysregulated emotions and behaviors, and how these associations may change over the course of the intervention.
Third, the adolescent subpopulations of focus across the included studies were also variable. Most of the included research was completed with special populations (e.g., youth with ADHD, at risk or incarcerated youth, youth with borderline personality symptoms) with only 12 of the 41 studies using a community sample. Indeed, subgroup analyses showed community samples, on average, exhibited significantly lower effect sizes compared to all other sample types. It will be important to further understand if teaching ER skills is only beneficial to those with a deficit in ER, or if interventions enhancing these skills is useful among typically developing children as well. It’s notable that improvements in ER were documented across a wide range of clinical populations studied including externalizing behaviors (e.g., aggression, oppositionality, ADHD), internalizing behaviors (e.g., depression and anxiety), ASD, borderline personality traits, and war-affected youth. If ER may play a role as a transdiagnostic risk factor or process, these findings might suggest that improving ER via targeted intervention may result in improvement for a variety of youth with different clinical diagnoses. It is likely that teaching the use of adaptive ER strategies would act as a promotive factor (i.e., help all children perform at higher levels) as opposed to only a protective factor (i.e., only help at-risk children succeed). Yet, some work has demonstrated that students at risk (e.g., Lam & Seidon, 2020) did not benefit from the ER intervention L2B, relative to the comparison group, whereas a typically developing community sample showed significant improvements in ER, relative to the comparison, from the same intervention (Metz et al., 2014). Further work is needed to elucidate for whom and how ER interventions may be most effective (e.g., increasing skills use compared to decreasing dysregulation). Additionally, it would be prudent to explore ER interventions for adolescents with depression only, as no study to date has done so, with the Wolff & Ollendick (2012) study including adolescents with comorbid depression and conduct problems, and Santomauro et al. (2016) including adolescents with ASD and depression.
Fourth, findings also suggested that efficacy and effectiveness of interventions may vary depending on whether the strategies taught focus on increasing adaptive ER skills or decreasing maladaptive ER strategies. Notably, these two dimensions, although related, appear to vary quite independently. It may be that some interventions are more efficacious for increasing adaptive ER (e.g., Claro et al., 2015; Wijana et al., 2018; Santomauro et al., 2016) whereas other intervention types are better suited for reducing maladaptive ER strategies (e.g., Bjureberg et al., 2017, 2018; Dingle et al., 2016). Additionally, many of the studies found significant improvement in related emotional constructs (e.g., emotion awareness and identification; Dingle et al., 2016; Houck et al., 2016) but not in measures of ER specifically. Although emotional awareness, naming, recognition, and identification are essential elements of regulation, it is possible that interventions targeting ER have traditionally been focused on building emotional awareness as a first step toward helping youth make changes in their ER strategies. A range of ER strategies (behavioral, cognitive) as well as different facets of ER (identification, awareness, management) should be assessed, particularly those that directly map onto the constructs being taught in the intervention as noted above.
Finally, few studies included follow-ups beyond the post-intervention assessment. Although promising there were significant improvements at post-treatment, studies that did include follow-up periods reported more mixed findings. Indeed, some work found gains to be maintained beyond the intervention period, ranging from one month to one year (e.g., Bjureberg et al., 2017, 2018; Houck et al., 2016; Schoeps et al., 2018; Wolf & Ollendick, 2012). Thus, it is possible that effects of ER interventions continue to increase over time, and it may be that once ER skills are taught, it takes time for these skills to solidify and be used in daily life. This highlights the importance of future ER intervention research doing both short and long-term follow-up visits.
Conclusion and Future Directions
Overall, results provide promise for the ability of ER-focused interventions to improve the adaptive ER skills of adolescents across a range of populations (i.e., clinical, community, and at-risk samples) with the effect of these interventions being stronger for pilot and effectiveness studies, relative to studies with a control group. Future work examining ER interventions needs to continue to employ rigorous research methodologies (e.g., compare to empirically supported treatments, include additional follow-up periods, use a multi-method assessment of change) and to examine their efficacies across a range of adolescent samples. It also remains crucial to refine ER measures used in interventions to ensure reliable and valid measurement of ER change that maps onto the specific skills being taught within the intervention frameworks. Additionally, moderators of treatment effects (e.g., duration, format delivery), as well as mediators associated with changes in ER skills during the intervention (e.g., length of practice, adolescent engagement) need to be examined to best understand for whom and how these intervention are most effective. Given these findings, additional work is needed to determine whether teaching adaptive ER strategies can serve as a promotive factor in normative samples. Understanding for whom teaching ER strategies are beneficial may have important implications for a range of domains from parenting practices to how teachers structure their school classroom environment. Overall, these findings underscore the importance of researchers continuing to explore the utility of ER interventions for additional clinical and community populations, particularly those that will be generalizable to the wider adolescent population in the United States and abroad.
Figure 2b. Forest Plot of Pooled Effect Size Analysis for Pre and Post Effects, Dysregulation and Overall Effects.

Table 2.
Emotion Regulation Measures from Included Articles
| Measure Name | Reporter | Content | Evidence of Validity and Reliability | Study |
|---|---|---|---|---|
| ADS | Self | 6 items; self-reported measure of frequency of difficulties with affect regulation | 1 – minimal evidence of reliability or validity | Hadley et al., 2020 |
| Affective instability | Clinician | Subscale from a structured interview assessing the 9 criteria for borderline personality disorder | 3 – strong evidence of reliability or validity | Schuppert et al., 2009; Schuppert et al., 2012 |
| ASRI | Self; Parent | 27 items; short- and long-term ER abilities | 1 – minimal evidence of reliability or validity | Rizzo et al., 2020 |
| CEMS | Self | 12 Likert items; sadness, anger, and worry regulation | 2 – moderate evidence of reliability or validity | Suveg et al., 2009 |
| CERQ | Self | 36 Likert items; cognitive ER strategies | 3 – strong evidence of reliability or validity | Afshari et al., 2014; Claro et al., 2015; Riggs Romaine et al., 2018; Ramdhonee-Dowlot et al., 2021 |
| CISS | Self; Parent | 48 Likert items; emotion coping | 1 – minimal evidence of reliability or validity | Keiley et al., 2007 |
| DERS | Self; Parent | 36 Likert items1,2 or 16 and 18-item short versions; capacity for emotion regulation | 3 – strong evidence of reliability or validity | Alampay et al., 2020; Betancourt et al., 2014; Bjureberg et al., 2017; Bjureberg et al., 2018; Breaux & Langberg, 2020; Broderick & Metz, 2009; Cotter et al., 2020; Ford-Paz et al., 2019; Hadley et al., 2020; Houck et al., 2016; Lindqvist et al., 2020; Metz et al., 2013; Newnham et al., 2015; Lam & Seidon, 2020; Wolff et al., 2020; Yeo et al., 2020 |
| EDI | Parent | 30 items; ER associated with autism | 2 – moderate evidence of reliability or validity | Conner et al., 2019 |
| EESC | Self | 16 Likert items; deficient emotional expression | 2 – moderate evidence of reliability or validity | Suveg et al., 2009 |
| ERQ | Self | 10 Likert items3; cognitive reappraisal and expressive suppression | 3 – strong evidence of reliability or validity | Dingle et al., 2016; Fung et al., 2016; Hafeman et al., 2020; Johnstone et al., 2020; Lau et al., 2020; Santomauro et al., 2016; Wijana et al., 2018 |
| ERBS | Self | 8 Likert items; assesses ER strategies taught in intervention | 1 – minimal evidence of reliability or validity | Hadley et al., 2020; Houck et al., 2016; Rizzo et al., 2020 |
| ERC | Parent | 24 Likert items; Parental perceptions of child’s management of emotions and lability | 2 – moderate evidence of reliability or validity | Cotton et al., 2016, 2020; Hadley et al., 2020; Keiley et al., 2015; Thomson et al., 2015; Wolff & Ollendick, 2012 |
| ER Questionnaire for Children | Self | 22 vignettes; Level of regulation of fear, anger, and sadness | 1 – minimal evidence of reliability or validity | Punamäki et al., 2014 |
| ESCQ | Self | 45 Likert items; emotional perception, understanding, labeling, expressing, and regulation | 2 – moderate evidence of reliability or validity | Schoeps et al., 2018 |
| MERLC | Self | 6 items; internal locus of control related to emotions subscale | 1 – minimal evidence of reliability or validity | Schuppert et al., 2009 |
| NMR | Self | 30 Likert items; ability to identify, manage, and utilize adaptively a variety of negative emotion states | 3 – strong evidence of reliability or validity | Ford et al., 2012 |
| Weekly Ratings | Clinician; Parent | Weekly ratings of adolescent ER; 3 items on 7-point Likert scale | 1 – minimal evidence of reliability or validity | Breaux & Langberg, 2020 |
Note. Evidence of validity and reliability refers to both validity/reliability studies conducted outside of those included in the present review as well as reliability information (e.g., internal consistency) reported in the included studies, when available. ADS: affect dysregulation scale; ASRI: adolescent self-regulatory inventory; CEMS: Children’s Emotional Management Scales; CERQ: Cognitive Emotion Regulation Questionnaire; CISS: Coping Inventory for Stressful Situations; DERS: Difficulties with Emotion Regulation Scale; EDI: Emotion Dysregulation Inventory; ERC: Emotion Regulation Checklist; NMR: Negative Mood Regulation; MERLC: Multidimensional Emotion Regulation Locus of Control; ERBS: Emotion Regulation Behaviors Scale; ERQ: Emotion Regulation Questionnaire; ESCQ: Emotional Skills and Competencies Questionnaire; EESC: Emotion Expressivity Scale for Children; CEMS: Children’s Emotion Management Scales
the Betancourt et al. 2014 study reported using only 23 items from the DERS and did not report which items or scales were omitted, no validity or reliability information for the reduced item set was presented;
the Alampay et al., 2020 study reported using only four subscales (26 items) of the DERS and reported acceptable internal consistencies;
the Lau et al., 2020 used only the 4-item emotion suppression scale of the ERQ and reported acceptable internal consistencies.
Funding:
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflicts of interest/Competing interests: none.
Studies may still be included if the minimum and maximum ages included in the sample are outside of 10-19 years, if the mean age is within the 10–19-year range.
Of note, despite the focus on clinical populations, only three studies in the present review (Afshari et al., 2014; Dingle et al., 2017; Schuppert et al., 2012) overlap with those included in the recent Moltrecht et al. (2021) meta-analysis of ER interventions.
One study (Ford-Paz et al., 2019) did not report age in their study and was excluded from this analysis.
References
*Indicates a paper reviewed in the present manuscript.
- Ahmed SP, Bittencourt-Hewitt A, & Sebastian CL (2015). Neurocognitive bases of emotion regulation development in adolescence. Developmental Cognitive Neuroscience, 15, 11–25. 10.1016/j.dcn.2015.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alampay LP, Tan LJTG, Tuliao AP, Baranek P, Ofreneo MA, Lopez GD, … & Guintu V. (2020). A pilot randomized controlled trial of a mindfulness program for Filipino children. Mindfulness, 11(2), 303–316. [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical psychology review, 30(2), 217–237. [DOI] [PubMed] [Google Scholar]
- Beck JS, & Beck AT (2011). Cognitive behavior therapy: Basics and beyond. Guilford Publication. [Google Scholar]
- Betancourt TS, McBain R, Newnham EA, Akinsulure-Smith AM, Brennan RT, Weisz JR, & Hansen NB (2014). A behavioral intervention for war-affected youth in Sierra Leone: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(12), 1288–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakemore S-J (2008). The social brain in adolescence. Nature Reviews Neuroscience, 9(4), 267–277. 10.1038/nrn2353 [DOI] [PubMed] [Google Scholar]
- Blakemore S-J, Mills KL (2014). Is adolescence a sensitive period for sociocultural processing? Annual Review of Psychology, 65, 187–207. doi: 10.1146/annurev-psych-010213-115202 [DOI] [PubMed] [Google Scholar]
- Bjureberg J, Sahlin H, Hedman-Lagerlöf E, Gratz KL, Tull MT, Jokinen J, … & Ljótsson B (2018). Extending research on Emotion Regulation Individual Therapy for Adolescents (ERITA) with nonsuicidal self-injury disorder: open pilot trial and mediation analysis of a novel online version. BMC psychiatry, 18(1), 284–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjureberg J, Sahlin H, Hellner C, Hedman-Lagerlöf E, Gratz KL, Bjärehed J, … & Ljótsson B (2017). Emotion regulation individual therapy for adolescents with nonsuicidal self-injury disorder: a feasibility study. BMC psychiatry, 17(1), 411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JP, & Rothstein HR (2011). Introduction to meta-analysis. John Wiley & Sons. [Google Scholar]
- Breaux R & Langberg JM (2020). Development and refinement of the RELAX intervention, an intervention targeting emotion dysregulation and interpersonal conflict in adolescents with ADHD: Results from a pilot study. Evidence-Based Practice in Child & Adolescent Mental Health, 5, 147–163. [Google Scholar]
- Broderick PC, & Metz S (2009). Learning to BREATHE: A pilot trial of a mindfulness curriculum for adolescents. Advances in school mental health promotion, 2(1), 35–46. [Google Scholar]
- Bunford N, Evans SW, & Langberg JM (2018). Emotion dysregulation is associated with social impairment among young adolescents with ADHD. Journal of Attention Disorders, 22(1), 66–82. [DOI] [PubMed] [Google Scholar]
- Casey BJ, & Caudle K (2013). The Teenage Brain: Self Control. Current Directions in Psychological Science, 22(2), 82–87. 10.1177/0963721413480170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Duhoux S, & Cohen MM (2010). Adolescence: What Do Transmission, Transition, and Translation Have to Do with It? Neuron, 67(5), 749–760. 10.1016/j.neuron.2010.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claro A, Boulanger MM, & Shaw SR (2015). Targeting vulnerabilities to risky behavior: An intervention for promoting adaptive emotion regulation in adolescents. Contemporary School Psychology, 19(4), 330–339. [Google Scholar]
- Chervonsky E, & Hunt C (2019). Emotion regulation, mental health, and social wellbeing in a young adolescent sample: A concurrent and longitudinal investigation. Emotion, 19(2), 270. [DOI] [PubMed] [Google Scholar]
- Compas BE, Jaser SS, Bettis AH, Watson KH, Gruhn MA, Dunbar JP, … Thigpen JC (2017). Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychological Bulletin, 143(9), 939–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Jaser SS, Dunbar JP, Watson KH, Bettis AH, Gruhn MA, & Williams EK (2014). Coping and emotion regulation from childhood to early adulthood: Points of convergence and divergence. Australian Journal of Psychology, 66(2), 71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner CM, White SW, Beck KB, Golt J, Smith IC, & Mazefsky CA (2019). Improving emotion regulation ability in autism: The Emotional Awareness and Skills Enhancement (EASE) program. Autism, 23(5), 1273–1287. [DOI] [PubMed] [Google Scholar]
- Cotter EW, Hornack SE, Fotang JP, Pettit E, & Mirza NM (2020). A pilot open-label feasibility trial examining an adjunctive mindfulness intervention for adolescents with obesity. Pilot and Feasibility Studies, 6, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton S, Luberto CM, Sears RW, Strawn JR, Stahl L, Wasson RS, … & Delbello MP (2016). Mindfulness‐based cognitive therapy for youth with anxiety disorders at risk for bipolar disorder: A pilot trial. Early Intervention in Psychiatry, 10(5), 426–434. [DOI] [PubMed] [Google Scholar]
- Cotton S, Kraemer KM, Sears RW, Strawn JR, Wasson RS, McCune N, … & Delbello MP (2020). Mindfulness‐based cognitive therapy for children and adolescents with anxiety disorders at‐risk for bipolar disorder: A psychoeducation waitlist controlled pilot trial. Early intervention in psychiatry, 14(2), 211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cracco E, Goossens L, & Braet C (2017). Emotion regulation across childhood and adolescence: evidence for a maladaptive shift in adolescence. European Child & Adolescent Psychiatry, 26(8), 909–921. [DOI] [PubMed] [Google Scholar]
- Cronin TJ, Pepping CA, & O'Donovan A (2018). Attachment to friends and psychosocial well-being: The role of emotion regulation. Clinical Psychologist, 22(2), 158–167. [Google Scholar]
- Dingle GA, Hodges J, & Kunde A (2016). Tuned In emotion regulation program using music listening: Effectiveness for adolescents in educational settings. Frontiers in Psychology, 7, 859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrenreich-May J, Kennedy SM, Sherman JA, Bilek EL, Buzzella BA, Bennett SM, & Barlow DH (2017). Unified protocols for transdiagnostic treatment of emotional disorders in children and adolescents: Therapist guide. Oxford University Press. [Google Scholar]
- Ehring T, Tuschen-Caffier B, Schnülle J, Fischer S, & Gross JJ (2010). Emotion regulation and vulnerability to depression: spontaneous versus instructed use of emotion suppression and reappraisal. Emotion, 10(4), 563–572. [DOI] [PubMed] [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, & Barlow DH (2010). Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice, 17(1), 88–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford JD, Steinberg KL, Hawke J, Levine J, & Zhang W (2012). Randomized trial comparison of emotion regulation and relational psychotherapies for PTSD with girls involved in delinquency. Journal of Clinical Child & Adolescent Psychology, 41(1), 27–37. [DOI] [PubMed] [Google Scholar]
- Ford-Paz RE, Crown L, Lawton K, Goldenthal H, Day G, Coyne CA, … & Cicchetti C (2019). Working on Womanhood (WOW): A participatory formative evaluation of a community-developed intervention. Evaluation and Program Planning, 72, 237–249. [DOI] [PubMed] [Google Scholar]
- Fung J, Guo S, Jin J, Bear L, & Lau A (2016). A pilot randomized trial evaluating a school-based mindfulness intervention for ethnic minority youth. Mindfulness, 7(4), 819–828. [DOI] [PubMed] [Google Scholar]
- Graziano PA, Reavis RD, Keane SP, & Calkins SD (2007). The role of emotion regulation in children's early academic success. Journal of School Psychology, 45(1), 3–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ (2015). The extended process model of emotion regulation: Elaborations, applications, and future directions. Psychological Inquiry, 26(1), 130–137. [Google Scholar]
- Gross JJ (2002). Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology, 39(3), 281–291. [DOI] [PubMed] [Google Scholar]
- Gross JJ (1998). The emerging field of emotion regulation: An integrative review. Review of general psychology, 2(3), 271–299. [Google Scholar]
- *Hadley W, Houck C, Barker D, Wickham B, Bogner J, & Jelalian E (2020). Preliminary Impact of an Adapted Emotion Regulation Intervention for Adolescents with Overweight and Obesity Attempting to Lose Weight. Journal of Developmental & Behavioral Pediatrics, 41(9), 706–715. [DOI] [PubMed] [Google Scholar]
- *Hafeman DM, Ostroff AN, Feldman J, Hickey MB, Phillips ML, Creswell D, … & Goldstein TR (2020). Mindfulness-based intervention to decrease mood lability in at-risk youth: Preliminary evidence for changes in resting state functional connectivity. Journal of Affective Disorders, 276, 23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannesdottir DK, & Ollendick TH (2007). The role of emotion regulation in the treatment of child anxiety disorders. Clinical Child and Family Psychology Review, 10(3), 275–293. [DOI] [PubMed] [Google Scholar]
- *Houck CD, Barker DH, Hadley W, Brown LK, Lansing A, Almy B, & Hancock E (2016). The 1-year impact of an emotion regulation intervention on early adolescent health risk behaviors. Health Psychology, 35(9), 1036–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Johnstone KM, Middleton T, Kemps E, & Chen J (2020). A pilot investigation of universal school-based prevention programs for anxiety and depression symptomology in children: A randomized controlled trial. Journal of clinical psychology, 76(7), 1193–1216. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Siegel TC, & Bass D (1992). Cognitive problem-solving skills training and parent management training in the treatment of antisocial behavior in children. Journal of Consulting and Clinical Psychology, 60(5), 733–747. [DOI] [PubMed] [Google Scholar]
- *Keiley MK (2007). Multiple-family group intervention for incarcerated adolescents and their families: A pilot project. Journal of Marital and Family Therapy, 33(1), 106–124. [DOI] [PubMed] [Google Scholar]
- *Keiley MK, Zaremba-Morgan A, Datubo-Brown C, Pyle R, & Cox M (2015). Multiple-family group intervention for incarcerated male adolescents who sexually offend and their families: Change in maladaptive emotion regulation predicts adaptive change in adolescent behaviors. Journal of Marital and Family Therapy, 41(3), 324–339. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Sherrill J, George CJ, Pollock M, Tumuluru RV, & Ho V (2006). Contextual emotion-regulation therapy for childhood depression: Description and pilot testing of a new intervention. Journal of the American Academy of Child & Adolescent Psychiatry, 45(8), 892–903. [DOI] [PubMed] [Google Scholar]
- Kopp CB (1989). Regulation of distress and negative emotions: A developmental view. Developmental Psychology, 25(3), 343–354. [Google Scholar]
- Kopp CB, & Neufeld SJ (2003). Emotional development during infancy. In Davidson RJ, Scherer KR, & Goldsmith HH (Eds.), Series in Affective Science. Handbook of affective sciences (pp. 347–374). New York, NY, US: Oxford University Press. [Google Scholar]
- *Lam K, & Seiden D (2020). Effects of a brief mindfulness curriculum on self-reported executive functioning and emotion regulation in Hong Kong adolescents. Mindfulness, 11(3), 627–642. [Google Scholar]
- Lamblin M, Murawski C, Whittle S, & Fornito A (2017). Social connectedness, mental health and the adolescent brain. Neuroscience & Biobehavioral Reviews, 80, 57–68. [DOI] [PubMed] [Google Scholar]
- *Lau AS, Kim JJ, Nguyen DJ, Nguyen HT, Kodish T, & Weiss B (2020). Effects of preference on outcomes of preventive interventions among ethnically diverse adolescents at-risk of depression. Journal of Clinical Child & Adolescent Psychology, 49(6), 820–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Lindqvist K, Mechler J, Carlbring P, Lilliengren P, Falkenström F, Andersson G, … & Philips B (2020). Affect-focused psychodynamic internet-based therapy for adolescent depression: randomized controlled trial. Journal of medical internet research, 22(3), e18047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM (1993). Skills training manual for treating borderline personality disorder. New York, NY: Guilford press. [Google Scholar]
- March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, … Kennard B (2003). Treatment for Adolescents with Depression Study (TADS): Rationale, design, and methods. Journal of the American Academy of Child and Adolescent Psychiatry, 42(5), 531–542. [DOI] [PubMed] [Google Scholar]
- Mazefsky CA, Herrington J, Siegel M, Scarpa A, Maddox BB, Scahill L, & White SW (2013). The role of emotion regulation in autism spectrum disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 52(7), 679–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcclure KS, Halpern J, Wolper PA, & Donahue J (2009). Emotion regulation and intellectual disability. [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Mennin DS, & NolenHoeksema S (2011). Emotion dysregulation and adolescent psychopathology: A prospective study. Behaviour Research and Therapy, 49(9), 544–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Metz SM, Frank JL, Reibel D, Cantrell T, Sanders R, & Broderick PC (2013). The effectiveness of the learning to BREATHE program on adolescent emotion regulation. Research in Human Development, 10(3), 252–272. [Google Scholar]
- Morris SB (2008). Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods, 11, 364–386. [Google Scholar]
- *Newnham EA, McBain RK, Hann K, Akinsulure-Smith AM, Weisz J, Lilienthal GM, … & Betancourt TS (2015). The Youth Readiness Intervention for war-affected youth. Journal of Adolescent Health, 56(6), 606–611. [DOI] [PubMed] [Google Scholar]
- Ougrin D, Tranah T, Stahl D, Moran P, & Asarnow JR (2015). Therapeutic interventions for suicide attempts and self-harm in adolescents: systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 54(2), 97–107. [DOI] [PubMed] [Google Scholar]
- Paus T, Keshavan M, & Giedd JN (2008). Why do many psychiatric disorders emerge during adolescence? Nature Reviews Neuroscience, 9(12), 947–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Punamäki RL, Peltonen K, Diab M, & Qouta SR (2014). Psychosocial interventions and emotion regulation among war-affected children: Randomized control trial effects. Traumatology, 20(4), 241–252. [Google Scholar]
- *Ramdhonee-Dowlot K, Balloo K, & Essau CA (2021). Effectiveness of the Super Skills for Life programme in enhancing the emotional wellbeing of children and adolescents in residential care institutions in a low-and middle-income country: A randomised waitlist-controlled trial. Journal of affective disorders, 278, 327–338. [DOI] [PubMed] [Google Scholar]
- Riediger M, & Klipker K (2014). Emotion regulation in adolescence. In Handbook of emotion regulation, 2nd ed (pp. 187–202). The Guilford Press. [Google Scholar]
- *Riggs Romaine CL, Kemp K, Giallella CL, Goldstein NE, Serico J, & Kelley S (2018). Can we hasten development? Effects of treatment on psychosocial maturity. International Journal of Offender Therapy and Comparative Criminology, 62(9), 2857–2876. [DOI] [PubMed] [Google Scholar]
- *Rizzo CJ, Houck C, Barker D, Collibee C, Hood E, & Bala K (2020). Project STRONG: An online, parent–son intervention for the prevention of dating violence among early adolescent boys. Prevention Science, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Santomauro D, Sheffield J, & Sofronoff K (2016). Depression in adolescents with ASD: A pilot RCT of a group intervention. Journal of Autism and Developmental Disorders, 46(2), 572–588. [DOI] [PubMed] [Google Scholar]
- *Schoeps K, Villanueva L, Prado-Gascó VJ, & Montoya-Castilla I (2018). Development of emotional skills in adolescents to prevent cyberbullying and improve subjective well-being. Frontiers in Psychology, 9, 2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schriber RA, & Guyer AE (2016). Adolescent neurobiological susceptibility to social context. Developmental Cognitive Neuroscience, 19, 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Schuppert HM, Giesen-Bloo J, van Gemert TG, Wiersema HM, Minderaa RB, Emmelkamp PM, & Nauta MH (2009). Effectiveness of an emotion regulation group training for adolescents—A randomized controlled pilot study. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice, 16(6), 467–478. [DOI] [PubMed] [Google Scholar]
- *Schuppert HM, Timmerman ME, Bloo J, van Gemert TG, Wiersema HM, Minderaa RB, … & Nauta MH (2012). Emotion regulation training for adolescents with borderline personality disorder traits: a randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 51(12), 1314–1323. [DOI] [PubMed] [Google Scholar]
- Shapero BG, Abramson LY, & Alloy LB (2016). Emotional reactivity and internalizing symptoms: Moderating role of emotion regulation. Cognitive therapy and research, 40(3), 328–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan E, Hall K, Moulding R, Bryce S, Mildred H, & Staiger PK (2017). Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clinical Psychology Review, 57, 141–163. [DOI] [PubMed] [Google Scholar]
- Smith EN, Romero C, Donovan B, Herter R, Paunesku D, Cohen GL, … & Gross JJ (2018). Emotion theories and adolescent well-being: Results of an online intervention. Emotion, 18(6), 781. [DOI] [PubMed] [Google Scholar]
- Smyth JM, & Arigo D (2009). Recent evidence supports emotion-regulation interventions for improving health in at-risk and clinical populations. Current opinion in psychiatry, 22(2), 205–210. [DOI] [PubMed] [Google Scholar]
- Steinberg L (2014). Age of opportunity: Lessons from the new science of adolescence. New York, NY: Houghton Mifflin Harcourt. [Google Scholar]
- *Suveg C, Sood E, Comer JS, & Kendall PC (2009). Changes in emotion regulation following cognitive-behavioral therapy for anxious youth. Journal of Clinical Child & Adolescent Psychology, 38(3), 390–401. [DOI] [PubMed] [Google Scholar]
- *Thomson K, Riosa PB, & Weiss JA (2015). Brief report of preliminary outcomes of an emotion regulation intervention for children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(11), 3487–3495. [DOI] [PubMed] [Google Scholar]
- Walerius DM, Reyes RA, Rosen PJ, & Factor PI (2018). Functional impairment variability in children with ADHD due to emotional impulsivity. Journal of Attention Disorders, 22(8), 724–737. [DOI] [PubMed] [Google Scholar]
- *Wijana MB, Enebrink P, Liljedahl SI, & Ghaderi A (2018). Preliminary evaluation of an intensive integrated individual and family therapy model for self-harming adolescents. BMC Psychiatry, 18(1), 371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner K, & Gross JJ (2010). Emotion regulation and psychopathology: A conceptual framework. In Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment (pp. 13–37). The Guilford Press. [Google Scholar]
- *Wolff JC, Garcia A, Kelly LM, Frazier EA, Jones RN, & Spirito A (2020). Feasibility of decision rule-based treatment of comorbid youth: A pilot randomized control trial. Behaviour research and therapy, 131, 103625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Wolff JC, & Ollendick TH (2012). Treatment of comorbid conduct problems and depression in youth: A pilot study. Child & Family Behavior Therapy, 34(2), 141–155. [Google Scholar]
- *Yeo AJ, Germán M, Wheeler LA, Camacho K, Hirsch E, & Miller A (2020). Self-harm and self-regulation in urban ethnic minority youth: a pilot application of dialectical behavior therapy for adolescents. Child and adolescent mental health, 25(3), 127–134. [DOI] [PubMed] [Google Scholar]
- Zeman J, Cassano M, Perry-Parrish C, & Stegall S (2006). Emotion regulation in children and adolescents. Journal of Developmental & Behavioral Pediatrics, 27, 155–168. [DOI] [PubMed] [Google Scholar]


