Abstract
Background:
We aimed to identify preoperative psychosocial factors associated with return-to-work (RTW) and the associated cost of productivity loss due to work absenteeism following surgery. Research demonstrates a high economic burden from productivity loss after surgery, but the comparative cost of productivity loss relative to income across different operations has not been examined.
Materials and Methods:
A mixed surgical cohort recruited for a randomized controlled trial were prospectively followed for up to two years following surgery with daily phone assessments to three months, weekly assessments thereafter to six months, then monthly assessments thereafter to determine RTW status, opioid use and pain.
Results:
183 of 207 (88.3%) patients in paid employment prior to surgery, who provided at least one day of follow-up, were included in this analysis. The average cost of productivity loss due to work absenteeism was $13 761 (median $9 064). Patients who underwent total knee replacement incurred the highest income loss. Medical claims filed before surgery were significantly associated with relative income loss (AOR 5.09;95% CI 1.73- 14.96; p<0.01) and delayed postoperative RTW. Elevated preoperative PTSD symptoms were associated with delayed RTW (HR 0.78; 95%CI 0.63-0.96; p-value=0.02) while male gender (HR 1.63; 95%CI 1.11-2.38; p-value=0.01) was associated with faster postoperative RTW.
Conclusion:
Surgery places a high economic burden on individuals due to postoperative productivity loss. Multidisciplinary approaches, such as pathways, that facilitate the operation and recovery may mitigate the economic consequences for patients, employers, and the healthcare system.
Keywords: cost of productivity loss, surgery, return-to-work, total knee arthroplasty, income loss, total joint arthroplasty
1. INTRODUCTION
Employment impacts overall health. Returning to work after surgery across a variety of populations, in different settings, demonstrates improvements in mental health, reduced substance use, enhanced quality of life, and better self-esteem.[1] Return to work (RTW) after a procedure can also reverse the negative effects of unemployment.[1–4] Identifying risk factors for delayed RTW after surgery would characterize patients likely to benefit from early interventions that promote reemployment, and prevent the negative financial and psychosocial impacts of non-RTW.
Several studies have shown the high economic burden of productivity loss following surgery. [5–8] However there remains a lack of literature on the comparative cost of productivity loss relative to income across different operations. Certain orthopedic operations are increasingly performed on younger adults at the peak of their productive capacity.[9, 10] Similarly, breast cancer is more frequently diagnosed among women of working age (age less than 65 years).[11] The impact of surgery on work capacity can have major financial consequences for patients and their families. Understanding the magnitude of productivity loss on income provides an important financial context for quantifying the impact of delayed or non-RTW after surgery.
Estimating productivity loss is also important for resource allocation with respect to prevention and treatment of illness. It provides an indication of the potential social benefits (or cost-savings) if an illness were prevented or treated by alternative modalities. However, certain conditions, such as breast cancer often require surgery and supportive measures to promote RTW are more likely a practical intervention. Several studies have reported on work status following surgery.[5, 6, 8, 12] However, most studies measured productivity loss based on number of days absent without valuating the monetary cost of work absenteeism. [6, 13, 14] Studies that have reported cost burden following surgery were based on small sample size, short follow-up periods, crude assumptions about work absenteeism and limited to one specific operation.[5, 7, 15, 16]
The aim of this secondary analysis was to estimate the cost of productivity loss due to work absenteeism and the impact on income for patients in the 2 years following a variety of operations, and to identify preoperative psychosocial factors associated with time to RTW after surgery.
2. MATERIALS and METHODS
2.1. Data
Data for this secondary analysis was collected as part of a randomized, double-blind, placebo-controlled trial comparing the effect of perioperative gabapentin vs. active placebo on pain resolution and opioid cessation in a mixed surgical cohort of patients undergoing eligible operations (see Table 1 and Supplement ) at a single tertiary academic medical center.[17] Perioperative gabapentin had no effect on postoperative pain resolution but demonstrated a modest effect on accelerating opioid cessation after surgery. Results from the primary analysis have been reported, along with the complete study protocol, and trial methodology.[17] The study protocol and present secondary analysis, was approved by the Stanford University IRB (#16617) and registered at clinicaltrials.gov (NCT01067144). Participants were enrolled between May 25, 2010 and July 25, 2014. All patients provided written, informed consent, and did not receive financial compensation. All work has been reported in line with the CHEERS criteria.
Table 1:
Relative income loss1 by socio-demographic factors
| Relative income loss1 | Less than 10% N (%) | More than 10% N (%) | Crude OR (95%CI) | Adjusted OR (95%CI) 2 |
|---|---|---|---|---|
| Total number of patients, N | 64 | 65 | ||
| Age category | ||||
| 50 years and below | 22 (34.9) | 13 (21.0) | 2.0 (0.9 to 4.5) | |
| Above 50 years | 41 (65.1) | 49 (79.0) | ||
| Gender | ||||
| Male | 35 (54.7) | 25 (38.5) | 1.9 (0.9 to 3.9) | |
| Female | 29 (45.3) | 40 (61.5) | ||
| Marital status | ||||
| Married/living with someone | 48 (75.0) | 50 (78.1) | 1.2 (0.5 to 2.7) | |
| Single3 | 16 (25.0) | 14 (21.9) | ||
| Ethnicity | ||||
| Caucasian | 55 (85.9) | 53 (81.5) | 0.7 (0.3 to 1.8) | |
| Years of schooling, mean (SD) | 16.8 (2.6) | 15.9 (2.8) | 0.8 (−0.1 to 1.7) | |
| Treated with Gabapentin | 35 (54.7) | 27 (41.5) | 0.5 (0.3 to 1.2) | |
| Type of surgery | ||||
| Ambulatory surgery | 16 (25.0) | 4 (6.2) | Reference | Reference |
| Thoracotomy or VATS | 3 (4.7) | 3 (4.6) | 4.0 (0.6 to 27.8) | |
| Total knee replacement | 18 (28.1) | 29 (44.6) | 6.4 (1.9 to 22.3)** | 8.3 (1.7 to 39.8)** |
| Total hip replacement | 14 (21.9) | 22 (33.9) | 6.4 (1.7 to 22.7)** | 13.2 (2.6 to 65.4)** |
| Mastectomy and Lumpectomy | 13 (20.3) | 7 (10.8) | 2.2 (0.5 to 9.0) | |
| Disability claim currently pending | 5 (8.1) | 12 (19.1) | 2.7 (0.8 to 8.1) | |
| Claim filed related to medical problem | 13 (20.3) | 27 (41.5) | 3.4 (1.4 to 7.8)** | 5.1 (1.7 to 14.9)** |
| Return to work- weeks, mean (SD) | 2.3 (1.4) | 12.0 (10.6) | ||
| Ambulatory surgery | 1.1 (0.8) | 26.7 (37.3) | −25 (−43.5 to −7.7)** | |
| Thoracotomy or VATS | 2.3 (1.1) | 11.3 (2.9) | −9.0 (−14.1 to −4.0)** | |
| Total knee replacement | 3.2 (1.4) | 13.1 (7.1) | −9.9 (−13.3 to −6.5)*** | |
| Total hip replacement | 2.3 (1.2) | 9.3 (4.0) | −7.0 (−9.2 to −4.8)*** | |
| Mastectomy | 3.4 (0.9) | 7.6 (1.6) | −4.2 (−6.0 to – 2.4)*** | |
| Lumpectomy | 2.5 (1.2) | 0 | NA | |
| Full-time employment | 54 (84.4) | 51 (78.5) | 1.5 (0.6 to 3.6) |
OR, odds ratio; RTW, return to work; SD, Standard deviation; VATS, video-assisted thoracoscopic surgery
p<0.05,
p<0.01,
p<0.001
Relative income loss is expressed as the cost of productivity loss due to work absenteeism as a percentage of annual income. This is among patients who returned to work following surgery and reported their annual income in the survey.
Adjusted for age, gender, years of education, type of employment (full or part-time), ethnicity, had submitted claim related to medical problem, pain level at non-surgical sites, type of surgery
Single category comprises patients divorced, separated, widowed, or single
Note: The dependent variable is a function of the variable RTW (weeks) and thus it was not included in the multivariate analysis
2.2. Measures
Patients completed presurgical questionnaires assessing demographics, disability and employment status, medical claims filed before surgery (e.g. social security disability insurance, worker’s compensation, other disability insurance), substance use, and pain and opioid use with a modified Brief Pain Inventory (BPI).[17] Past 30-day prescription opioid use was assessed with the question, “How long has it been since you last used opioid medication on a daily basis?” Several author-generated measures were assessed for the risk of pain, delayed recovery and addiction after surgery. (see Supplement). The Opioid Risk Tool (ORT) was administered to screen for opioid-related aberrant behaviors.[18]
Individual annual patient income was assessed with possible responses “Less than $10,000; $10,000- $19,999; $20,000- $29,999; $30,000- $39,999; $40,000- $49,999; $50,000- $59,999; $60,000- $69,999; $70,000- $79,999; $80,000 or more”. Additional assessments included the Marlow-Crowne Social Desirability Scale to assess social desirability bias,[19] Barratt Impulsivity Scale to measure impulsive personality traits,[20] Posttraumatic Stress Disorder Checklist-Civilian Version (PCL-C) to measure post-traumatic stress disorder symptoms,[21] State-Trait Anxiety Inventory to measure current symptoms of anxiety vs. a generalized propensity to be anxious respectively,[22] Beck Depression Inventory-II (BDI-II) to assess the severity of depressive symptoms,[23] and the Euroqol Visual Analog Scale (VAS), which is a vertical visual analogue scale with values between 100 (best imaginable health) and 0 (worst imaginable health), for patients to provide a global assessment of their health.[24]
RTW was assessed via daily calls during the first 90 days to minimize recall bias and determine the exact date of RTW. RTW status was then assessed weekly thereafter from 3 to 6 months, and monthly thereafter from 6 months to 2 years after surgery until patients responded “yes” rather than “no” to the following question: “If you worked before surgery have you returned to work (whether paid or not—any vocational activity)?” Decreasing call frequency accounted for the majority of events anticipated during the first 90 days. Patients were censored for loss to follow-up or competing risks including additional operations (such as breast reconstruction), treatment (receipt of postoperative neoadjuvant chemotherapy), and postoperative complications.
2.3. Cost of productivity loss
We derived the midpoint of each income bracket and treated it as a continuous variable. For patients with an annual income of $80,000 or more, $119,280 was used based on data from the Current Population survey to adjust for the higher median income of the geographic location where participants were enrolled. [25] A similar approach has been used in previous studies.[26, 27] The individual’s annual income was then converted into an average weekly salary by assuming 52 paid work weeks per year. So, a patient with an annual income of $55,000 would have a weekly income of $1057.70. Income loss related to absenteeism was estimated as salary lost as a result of absence from work. The income was inflation-adjusted to 2020 dollars using the annual average Consumer Price Index for All Urban Consumers (CPI-U) provided by the US Department of Labor, Bureau of Labor Statistics.
2.4. Cost of productivity loss relative to income
Relative income loss was expressed as cost of productivity loss as a percentage of patient’s annual income. Relative income loss was grouped into those who incurred < 10% or ≥ 10% income loss due to absenteeism. The 10% cut-off was based on the median percentage loss of income among the patients reported in the present study. The secondary outcome was time to RTW as defined by the first day when a patient answered yes to the RTW question.
2.5. Analysis
Analysis included patients in self-reported paid employment (full or part-time) prior to surgery, who provided at least one follow-up assessment of RTW after surgery. We reported the odd ratios (ORs) for greater than 10% relative income loss. Multivariate analysis was adjusted for age, gender, years of education, type of employment (full or part-time), ethnicity, had submitted claim related to medical problem, pain level at non-surgical sites, and type of surgery.
We conducted a sensitivity analysis of relative income loss using linear regression after imputing missing values to estimate the duration to RTW for patients in paid employment prior to surgery who were right censored (e.g., lost to follow-up, had a second operation, asked to be withdrawn). Predicted values were used to compare outcomes between the primary and combined dataset (consisting of primary and imputed data). Costs are reported in U.S. dollars.
Time to RTW was analyzed using Cox proportional hazards regression. All analyses included surgery type in order to identify patient-specific factors influencing RTW across operations. Variables were first evaluated by univariate analysis of time to RTW . All factors were assessed as candidates for the final multivariable model. SAS version 9.4 (SAS Institute, Cary, N.D.) was used for all analyses. Given that certain operations enrolled primarily female patients (e.g., mastectomy), all significant covariates in the final model were examined for an interaction with gender. Post-hoc, the interaction of age and disability claims filed, or type of surgery were examined.
3. RESULTS
Of 410 patients analyzed in the original trial, 207 patients were in paid employment prior to the surgery. The analysis was confined to 183 (88.4%) patients who provided at least one day of follow-up regarding RTW status. 81.4% (n=149) patients reported postoperative RTW, and 18.6% (n=34) were right-censored. In total 8,259 (97.4%) of 8,476 scheduled RTW assessments were completed during the course of the study, and only 217 (2.6%) were not completed. A majority of patients did RTW after surgery. Among those censored, the median follow-up time was 5.0 (interquartile-IQ range 2.0-8.6) weeks, which was comparable to the median time to RTW reported of 4.7 (IQ range 2.0–8.6) weeks.
Mean age was 53.7 years, and half were male (Supplementary Table 1). Most patients were Caucasian (80.3%), married/living with someone (80.1%), in full-time employment (81.4%) and had an average of 16.2 years of education. Most patients underwent total knee replacement (33.9%), total hip replacement (25.1%), or mastectomy (13.1%) or an ambulatory surgery (hand surgery, carpal tunnel surgery, knee arthroscopy, shoulder arthroscopy; 13.1%). A smaller proportion underwent thoracotomy, video-assisted thoracoscopic surgery (VATS) (7.1%) or lumpectomy (7.7%).
At 76 days post-surgery, 75% of patients had RTW and most were in full-time employment. The mean time to RTW following surgery was 6.8 weeks. Patients who underwent total knee replacement took a median of 47 days (IQ range 28- 87) days to RTW compared to patients undergoing lumpectomy who took a median of 15 (IQ range 7-20) days to RTW.
The average cost of productivity loss due to work absenteeism was $13761 (median $9064 per patient). Lumpectomy was associated with lowest income loss, followed by mastectomy. More than half of the patients incurred ≥ 10% relative income loss with patients who underwent total hip and knee replacement incurring the highest loss (Figure 1).
Figure 1: Boxplot for relative income loss due to absenteeism by surgery type.
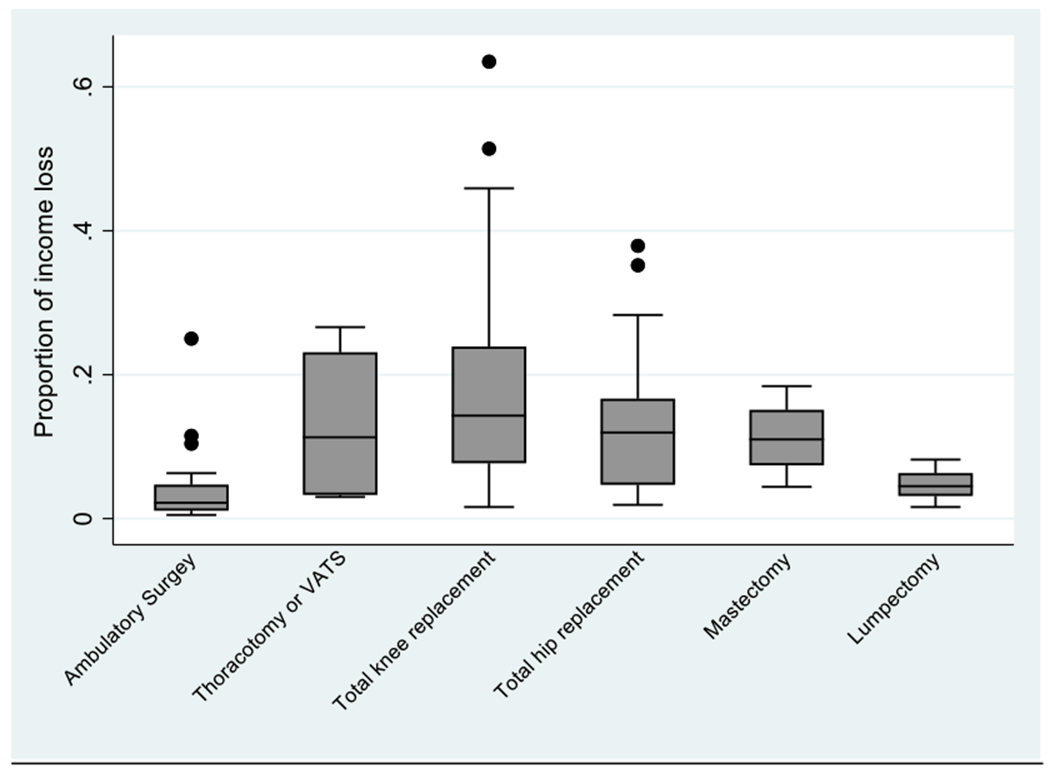
Relative income loss is expressed as the cost of productivity loss due to work absenteeism as a proprotion of annual income. The plots depict the median (line inside the shaded box), the interquartile range (box), values within 1.5 box-lengths from either end of the box (whiskers) and outliers (dots). VAT, video-assisted thoracoscopic surgery.
Medical claims filed before surgery and surgery type were significantly associated with ≥ 10% relative income loss in the multivariate logistic regression model (Table 1). Patients who had filed claims related to medical problems preoperatively were 5.1 times more likely to incur ≥ 10% relative income loss compared to non-claimants. There were no other significant differences between the two groups (see Supplementary Table 2). No significant difference in the results were found when the analysis was restricted to non-claimants (Supplementary Table 3). Type of surgery remained significantly associated with ≥ 10% relative income loss.
3.1. Sensitivity Analysis
After imputing missing values of right-censored patients, the overall mean income loss following surgery for the combined data (primary data and the imputed data) was $13 941 compared to $13 761 for the primary data (Supplementary Table 4).
3.2. Preoperative Factors of RTW
A number of preoperative factors were significantly associated with delayed RTW in univariate Cox regression (Table 2). In the final multivariable model (Table 3), every 3-point increase in the ORT score was associated with a 29% reduction in the rate of RTW (p-value=0.0004). Every 8-point increase in the PCL-C Score was associated with a 22% reduction in the rate of RTW (p-value=0.02). Any medical claim filed before surgery was significantly associated with delayed RTW (p-value=<0.0001). Also, undergoing total knee or hip replacement was associated with greater delayed in RTW compared to ambulatory operations (p<0.0001), In contrast, male gender (HR 1.63;95%CI 1.11-2.38; p-value=0.0008) significantly increased the rate of RTW. There was no significant interaction of these preoperative factors with gender, age, type of operation or disability claim filed.
Table 2.
Determinants of Time to RTW: Univariate Analysis
| Characteristic | Hazard Ratio | Hazard Ratio 95% Confidence Interval | p-value |
|---|---|---|---|
| Baseline pain other than surgical site (0-10)1 | 0.82 | (0.66-1.00) | 0.05 |
| Male Gender | 1.43 | (1.04-1.98) | 0.03 |
| Type of Surgery | 0.02 | ||
| Other (hand surgery, knee arthroscopy, etc.)- Reference |
0.0005 | ||
| Thoracotomy or VATS | 0.52 | (0.24-1.14) | |
| Total knee replacement | 0.34 | (0.21-0.57) | |
| Total hip replacement | 0.48 | (0.28-0.82) | |
| Mastectomy | 0.39 | (0.20-0.75) | |
| Lumpectomy | 0.95 | (0.45-2.04) | |
| Years of school completed starting with 1st grade2 | 1.34 | (1.06-1.70) | 0.02 |
| Claims filed related to medical problem | <0.0001 | ||
| None-Reference | |||
| Social Security Disability Insurance | 0.28 | (0.15-0.52) | |
| Workers’ compensation | 0.45 | (0.20-1.03) | |
| Personal injury (unrelated to work) | 0.84 | (0.31-2.29) | |
| Other disability insurance | 0.38 | (0.22-0.66) | |
| VA Service connection | 0.28 | (0.04-2.01) | |
| Pending Disability Claim | 0.51 | (0.31-0.83) | 0.007 |
| Opioid Risk Tool Score3 | 0.85 | (0.72-1.00) | 0.05 |
| PTSD Checklist-Civilian Version (PCL-C) Score4 | 0.82 | (0.68-0.98) | 0.03 |
RTW, return to work; VATS, video-assisted thoracoscopic surgery
Hazard ratio represents an increase of 3 points on the Numeric Rating Scale of Pain.
Hazard ratio represents an increase in 4 years of school completed.
Hazard ratio represents an increase in 3 points on the Opioid Risk Tool Score.
Hazard ratio represents an increase in 8 points on the PCL-C Score
Table 3.
Determinants of RTW: Multivariable Analysis
| Characteristic | Hazard Ratio | Hazard Ratio 95% Confidence Interval | p-value |
|---|---|---|---|
| Opioid Risk Tool Score1 | 0.71 | (0.59-0.86) | 0.0004 |
| PTSD Checklist-Civilian Version (PCL-C) Score2 | 0.78 | (0.63-0.96) | 0.02 |
| Male Gender | 1.63 | (1.11-2.38) | 0.01 |
| Claims filed related to medical problem | <0.0001 | ||
| None-Reference | |||
| Social Security Disability Insurance | 0.26 | (0.13-0.50) | |
| Workers’ compensation | 0.26 | (0.10-0.68) | |
| Personal injury (unrelated to work) | 0.70 | (0.25-1.95) | |
| Other disability insurance | 0.32 | (0.18-0.58) | |
| VA Service connection | 0.15 | (0.02-1.12) | |
| Type of Surgery | <0.0001 | ||
| Other (hand surgery, knee arthroscopy, etc.) -Reference |
|||
| Thoracotomy or VATS | 0.64 | (0.28-1.47) | |
| Total knee replacement | 0.36 | (0.21-0.61) | |
| Total hip replacement | 0.34 | (0.19-0.60) | |
| Mastectomy | 0.60 | (0.28-1.31) | |
| Lumpectomy | 1.84 | (0.79-4.29) |
RTW, return to work
Hazard ratio represents an increase in 3 points on the Opioid Risk Tool Score.
Hazard ratio represents an increase in 8 points on the PCL-C Score.
4. DISCUSSION
To our knowledge, this is the first study to identify preoperative psychosocial factors associated with postoperative RTW in patients undergoing a range of operations and the associated cost of productivity loss due to work absenteeism. The majority of patients employed before surgery had returned to work 10.9 weeks post-surgery. Medical claims filed before surgery (e.g., social security disability insurance, worker’s compensation, other disability insurance) and surgery type were significantly associated with a relative income loss. Similarly, medical claims filed before surgery and patients undergoing total hip or knee replacement operations demonstrated a reduced rate of RTW. Elevated preoperative post-traumatic stress disorder (PTSD) symptoms and ORT scores were also associated with a reduced rate of RTW.
Much research examining RTW after cancer diagnosis has focused on women with breast cancer.[28] Breast cancer results in the greatest productivity loss among all cancers.[29] Our findings demonstrate that patients undergoing total hip or knee arthroplasty are at even higher risk for delayed RTW emphasizing the relative impact of joint replacement surgery on productivity loss. When examining cancer survivors, financial necessity is cited as a driving factor for RTW.[28] Supplemental income secondary to disability claims may have similarly delayed RTW in our study participants serving as a buffer to income loss. However, the delays in RTW are still likely to result in a relative income loss among patients with pre-existing disability claims. Patients nearing retirement may be more likely to retire rather than RTW, and also may be more likely to pursue disability claims prior to retirement. However, we did not see a significant interaction of delayed RTW risk factors with age, thus decreasing the likelihood of age as a true mediator of these effects. Future work is needed to fully understand the impact of disability claims on surgical recovery, return to work, and productivity loss
Among patients undergoing total hip or knee arthroplasty the rates of RTW are reportedly similar, and patients who took preoperative sick leave due to hip or knee arthritis took a longer time to RTW.[30] Our findings similarly demonstrate comparable reduced rates of return to work when comparing patients who had undergone total hip or knee replacement. In a systematic review spanning 3,073 patients in 14 studies, the most important factors delaying or preventing RTW among patients undergoing total knee arthroplasty were a more physical nature of employment and preoperative absence from work. Given the high reported years of education in our surgical cohort, a higher percentage of patients in our study were likely college-educated, and thus less likely to have highly physical employment facilitating RTW.[31] Our findings amy represent a conservative estimate of productivity loss. Patients taking sick leave for less than 180 days prior to joint replacement surgery had better health profiles and were more likely to RTW after surgery.[30, 32] Thus, preoperative sick leave and claims for medical status may be a proxy for poorer health profiles. Our research simultaneously examined the relative significance of patient-reported psychosocial health status and disability claims and emphasizes the importance of disability insurance in delaying RTW. In patients who had undergone total hip arthroplasty, patients were less likely to RTW if they had disability insurance claims.[33] Future research is needed to determine whether disability insurance serves to buffer the income loss associated with postoperative recovery or ultimately results in productivity loss over time by delaying RTW.
Males were more likely to RTW after surgery in our study, and this may relate to cultural expectations, societal pressure, [28] or higher preoperative earnings[34] Overall, 73.5% (n=50) of men compared to 49.4%(n=44) of women in our study reported an annual income in the highest income bracket. Among patients undergoing total hip or knee arthroplasty, male sex is a significant independent predictor or faster RTW.[35] Overall, research is sparse regarding factors affecting productivity loss after total knee or hip arthroplasty,[36] and focused research to determine specific predictors of productivity loss in this group of surgical patients is warranted.
Previously, no associations have been reported between preoperative psychological distress and RTW after total joint replacement.[37] By simultaneously considering PTSD, anxiety, and depressive symptoms, we found PTSD symptoms to be a significant predictor of delayed RTW. As neither education nor age were associated with RTW in our cohort, mood may better predict the rate of RTW after surgery. From a clinical perspective, mood symptoms present a modifiable patient-specific risk factor to promote RTW after surgery.
Among patients treated for moderate-to-severe injuries, social dysfunction after trauma was significantly associated with PTSD, functional limitations, and delayed RTW.[38] In a national cohort of surgical inpatients hospitalized for trauma, PTSD symptoms, assessed by the PCL-C, was significantly associated with impairments across functional outcomes including not returning to work, impaired activities of daily living, and worse physical and mental health status.[39] In contrast to the development of PTSD symptoms after trauma, our findings highlight the importance of pre-existing PTSD symptoms prior to surgical injury. We found that preoperative PTSD symptoms assessed by the PCL-C were significantly associated with delayed RTW in non-trauma surgical patients. Thus, interventions to decrease PTSD symptoms prior to and during the perioperative phases of care may promote postoperative RTW. Implementing preoperative PTSD treatments, such as eye movement desensitization and reprocessing, or trauma-focused cognitive behavioral therapy, may promote RTW and improve health outcomes.[40]
The ORT was developed as a screening instrument for the risk of opioid-related aberrant behaviors, but validation of the tool has not been successful.[41] The ORT assesses family history of substance use and history of preadolescent sexual abuse. Specific childhood adversities including physical and sexual abuse, neglect, and parent psychopathology are associated with increased odds of PTSD.[42] Therefore, elevated ORT scores may identify patients with prior childhood adversities making them prone to develop PTSD symptoms. Future research to measure longitudinal changes of mood in response to surgery are needed to delineate the importance of PTSD symptoms in delaying RTW and increasing productivity loss.
Disease related factors including comorbidities and pain have been reported to impede RTW.[43] We did not find an association of preoperative pain intensity with RTW. Patients with elevated preoperative pain and certain medical comorbidities were excluded from the trial, which may have accounted for differences in findings. Prior research has similarly reported a lack of association between preoperative physical activity levels and time to RTW after total joint arthroplasty.[44]
In addition to lost productivity, surgery places a large financial burden on healthcare system. More than 640 000 total knee procedures are performed in the US each year resulting in a total annual cost of about $10.2bn.[45] Multidisciplinary approaches that prevent or delay the need for surgery or reduce the invasiveness of the surgery required may reduce direct and indirect costs. For example, injury prevention, weight management and early conservative management for hip and knee arthritis has delayed the need for surgery.[46] Early screening for breast cancer may reduce the need for a mastectomy while smoking cessation programs may reduce the risk of lung cancer and need for thoracotomy. These strategies for disease prevention and delayed progression, may ultimately minimize productivity loss.
4.1. Limitations
Our findings relied on self-report which could be subject to bias and measurement error. The study did not assess barriers or facilitators to RTW. However, patients were censored for competing risks. Thus, indirectly accounting for RTW barriers. Censored patients were not included in the primary relative income loss analysis. However, we found similar results in the sensitivity and RTW survival analyses, accounting for each censored patient’s postoperative course until the time of the competing risk. As such, significant risk factors identified in the multivariable analysis may be relevant to patients experiencing postoperative complications or additional operations.
The study assumed patients returned to the same work status as reported prior to surgery. However, previous studies have found that patients who had undergone joint replacement surgery were more likely to work less hours post-surgery while other studies have found that patients were able to return to the same work status (or increase their work hours) as the surgery restored optimal function to the joint.[47] In addition, our analysis did not account for job-specific benefits that would allow for delayed RTW while preserving income. Our analysis did not account for “paid time off’ or “medical leave”, and our results may have over-estimated productivity loss. However, patients may have previously consumed sick leave or other types of leave which were no longer available after the operation. This may particularly apply to patients with chronic conditions such as knee or hip osteoarthritis leading to total joint replacement surgery. Further, work-specific disability insurance would allow for delayed RTW with preservation of some income. However, we were not able to differentiate whether pre-existing disability claims were operation specific. If pre-existing disability claims were a supplement to job-related income, patients would still experience some degree of productivity loss albeit less exaggerated. Future research is needed to examine productivity loss after surgery accounting for these protective factors.
5. CONCLUSIONS
In conclusion, medical claims filed before surgery, undergoing total joint arthroplasty, and elevated preoperative PTSD symptoms were significantly associated with relative income loss and delayed RTW after surgery, while male gender promoted postoperative RTW.
Supplementary Material
Highlights.
Postoperative return to work (RTW) improves mental health and quality of life.
We compared the cost of productivity loss relative to income across operations.
The average cost of productivity loss due to work absenteeism was $13,761.
Total knee replacement incurred the highest income loss across operations.
Preoperative medical claims and PTSD symptoms were associated with delayed RTW.
Acknowledgements:
The authors gratefully acknowledge the assistance of all who made this project possible including the patients who dedicated their time.
Funding:
This study was supported by the National Institutes of Health (NIH) National Institute on Drug Abuse (grant numbers K23DA025152, R01DA045027), the Stanford Department of Anesthesiology, Perioperative, and Pain Medicine, and the NIH National Center for Translational Science (grant number KL2TR003143).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CRediT author statement
Jennifer M. Hah: Conceptualization, Methodology, Validation, Formal Analysis, Investigation, Writing-Original Draft
Evelyn Lee: Methodology, Formal Analysis, Writing-Original Draft
Rupendra Shrestha: Methodology, Formal Analysis, Writing-Review &Editing
Luke Pirrotta: Writing-Review & Editing
James Huddleston: Investigation, Writing-Review & Editing
Stuart Goodman: Investigation, Writing – Review & Editing
Derek F. Amanatullah: Investigation, Writing – Review & Editing
Frederick M. Dirbas: Investigation, Writing – Review & Editing
Ian R. Carroll: Investigation, Writing – Review & Editing, Funding Acquisition
Deborah Schofield: Conceptualization, Methodology, Writing – Review & Editing
Disclosures: The authors report no conflict of interest.
Data statement: The authors have no ethical permission to share data.
The data are considered personally identifiable, although all personal identifiers were been removed before data-cleaning and analyses. Therefore, the database cannot be shared publicly. Yet, the data can be made available to researchers upon reasonable request, in the condition of clearance by the responsible ethics committee.
Provenance and peer review, not commissioned, externally peer reviewed.
Contributor Information
Jennifer M. Hah, Division of Pain Medicine, Department of Anesthesiology, Perioperative, and Pain Medicine, Stanford University, Stanford, CA, USA.
Evelyn Lee, Centre for Economic Impacts of Genomic Medicine, Macquarie University, Sydney, NSW, Australia.
Rupendra Shrestha, Centre for Economic Impacts of Genomic Medicine, Macquarie University, Sydney, NSW, Australia.
Luke Pirrotta, Stanford Systems Neuroscience and Pain Lab, Stanford University, Stanford, CA, USA.
James Huddleston, Department of Orthopaedic Surgery, Stanford University, Stanford, CA, USA.
Stuart Goodman, Department of Orthopaedic Surgery and (by courtesy) Bioengineering, Stanford University, Stanford, CA, USA.
Derek F. Amanatullah, Department of Orthopaedic Surgery, Stanford University, Stanford, CA, USA.
Frederick M. Dirbas, Department of General Surgery, Stanford University, Stanford, CA, USA.
Ian R. Carroll, Division of Pain Medicine, Department of Anesthesiology, Perioperative, and Pain Medicine, Stanford University, Stanford, CA, USA.
Deborah Schofield, Centre for Economic Impacts of Genomic Medicine, Macquarie University, Sydney, NSW, Australia.
References
- 1.Drummond M, Methods for the economic evaluation of health care programmes. Fourth edition, ed. Oxford medical publications. 2015, Oxford, United Kingdom ; New York, NY, USA: Oxford University Press. xiii, 445 pages. [Google Scholar]
- 2.Broemer L, et al. , Exploratory study of functional and psychological factors associated with employment status in patients with head and neck cancer. Head Neck, 2021. 43(4): p. 1229–1241. [DOI] [PubMed] [Google Scholar]
- 3.Rashid H, et al. , Returning to work in lung cancer survivors-a multi-center cross-sectional study in Germany. Support Care Cancer, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strube P, et al. , Influence of Anxiety and Depression, Self-Rated Return-to-Work Problems, and Unemployment on the Outcome of Outpatient Rehabilitation After Shoulder Arthroscopy. Am J Phys Med Rehabil, 2019. 98(12): p. 1118–1124. [DOI] [PubMed] [Google Scholar]
- 5.Fayssoux R, et al. , Indirect costs associated with surgery for low back pain—a secondary analysis of clinical trial data. Population health management, 2010. 13(1): p. 9–13. [DOI] [PubMed] [Google Scholar]
- 6.Clayton M and Verow P, A retrospective study of return to work following surgery. Occupational medicine, 2007. 57(7): p. 525–531. [DOI] [PubMed] [Google Scholar]
- 7.Sigurdsson E, et al. , Early discharge and home intervention reduces unit costs after total hip replacement: results of a cost analysis in a randomized study. International journal of health care finance and economics, 2008. 8(3): p. 181–192. [DOI] [PubMed] [Google Scholar]
- 8.Kamdar BB, et al. , Return to work and lost earnings after acute respiratory distress syndrome: a 5-year prospective, longitudinal study of long-term survivors. Thorax, 2018. 73(2): p. 125–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernstein J and Derman P, Dramatic increase in total knee replacement utilization rates cannot be fully explained by a disproportionate increase among younger patients. Orthopedics, 2014. 37(7): p. e656–e659. [DOI] [PubMed] [Google Scholar]
- 10.Ackerman IN, et al. , Hip and knee osteoarthritis affects younger people, too. journal of orthopaedic & sports physical therapy, 2017. 47(2): p. 67–79. [DOI] [PubMed] [Google Scholar]
- 11.Ekenga CC, et al. , Early-stage breast cancer and employment participation after 2 years of follow-up: A comparison with age-matched controls. Cancer, 2018. 124(9): p. 2026–2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hylkema TH, et al. , Activity impairment and work productivity loss after total knee arthroplasty: a prospective study. The Journal of arthroplasty, 2019. 34(11): p. 2637–2645. [DOI] [PubMed] [Google Scholar]
- 13.Tilbury C, et al. , Return to work after total hip and knee arthroplasty: a systematic review. Rheumatology, 2014. 53(3): p. 512–525. [DOI] [PubMed] [Google Scholar]
- 14.Leichtenberg C, et al. , Determinants of return to work 12 months after total hip and knee arthroplasty. The Annals of The Royal College of Surgeons of England, 2016. 98(6): p. 387– 395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koenig L, et al. , How does accounting for worker productivity affect the measured cost-effectiveness of lumbar discectomy? Clinical Orthopaedics and Related Research®, 2014. 472(4): p. 1069–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hollingworth W, et al. , Costs and cost-effectiveness of spinal cord stimulation (SCS)for failed back surgery syndrome: an observational study in a workers’ compensation population. Spine, 2011. 36(24): p. 2076–2083. [DOI] [PubMed] [Google Scholar]
- 17.Hah J, et al. , Effect of Perioperative Gabapentin on Postoperative Pain Resolution and Opioid Cessation in a Mixed Surgical Cohort: A Randomized Clinical Trial. JAMA Surg, 2018. 153(4): p. 303–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Webster LR and Webster RM, Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the Opioid Risk Tool. Pain Med, 2005. 6(6): p. 432–42. [DOI] [PubMed] [Google Scholar]
- 19.Crowne DP and Marlowe D, A new scale of social desirability independent of psychopathology. J Consult Psychol, 1960. 24: p. 349–54. [DOI] [PubMed] [Google Scholar]
- 20.Patton JH, Stanford MS, and Barratt ES, Factor structure of the Barratt impulsiveness scale. J Clin Psychol, 1995. 51(6): p. 768–74. [DOI] [PubMed] [Google Scholar]
- 21.Ruggiero KJ, et al. , Psychometric properties of the PTSD Checklist-Civilian Version. J Trauma Stress, 2003. 16(5): p. 495–502. [DOI] [PubMed] [Google Scholar]
- 22.Spielberger CD, State-trait anxiety inventory : a comprehensive bibliography. 2nd ed. 1989, Palo Alto, CA (577 College Ave., Palo Alto 94306): Consulting Psychologists Press. 115 p. [Google Scholar]
- 23.Beck AT, et al. , Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess, 1996. 67(3): p. 588–97. [DOI] [PubMed] [Google Scholar]
- 24.EuroQol G, EuroQol--a new facility for the measurement of health-related quality of life. Health Policy, 1990. 16(3): p. 199–208. [DOI] [PubMed] [Google Scholar]
- 25.Flood S, et al. , Integrated public use microdata series, current population survey: Version 6.0 [dataset]. Minneapolis, MN: IPUMS. 2018. [Google Scholar]
- 26.Dowd JB, Palermo TM, and Aiello AE, Family poverty is associated with cytomegalovirus antibody titers in US Children. Health Psychology, 2012. 31(1): p. 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hagerty MR, Social comparisons of income in one’s community: Evidence from national surveys of income and happiness. Journal of Personality and social Psychology, 2000. 78(4): p. 764. [DOI] [PubMed] [Google Scholar]
- 28.Butow P, et al. , Return to work after a cancer diagnosis: a meta-review of reviews and a meta-synthesis of recent qualitative studies. J Cancer Surviv, 2019. [DOI] [PubMed] [Google Scholar]
- 29.Park JH, et al. , Breast Cancer Epidemiology of the Working-Age Female Population Reveals Significant Implications for the South Korean Economy. J Breast Cancer, 2018. 21(1): p. 91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kleim BD, et al. , Understanding the patient-reported factors determining time taken to return to work after hip and knee arthroplasty. Knee Surg Sports Traumatol Arthrosc, 2015. 23(12): p. 3646–52. [DOI] [PubMed] [Google Scholar]
- 31.Drobniewski M, et al. , The return to professional activity patients treated surgically due to advanced gonarthrosis. Int J Occup Med Environ Health, 2021. [DOI] [PubMed] [Google Scholar]
- 32.Malviya A, et al. , Factors influencing return to work after hip and knee replacement. Occup Med (Lond), 2014. 64(6): p. 402–9. [DOI] [PubMed] [Google Scholar]
- 33.Bohm ER, The effect of total hip arthroplasty on employment. J Arthroplasty, 2010. 25(1): p. 15–8. [DOI] [PubMed] [Google Scholar]
- 34.Mandel H and Semyonov M, Gender pay gap and employment sector: Sources of earnings disparities in the United States, 1970–2010. Demography, 2014. 51(5): p. 1597–1618. [DOI] [PubMed] [Google Scholar]
- 35.Rondon AJ, et al. , Return to Work After Total Joint Arthroplasty: A Predictive Model. Orthopedics, 2020. 43(5): p. e415–e420. [DOI] [PubMed] [Google Scholar]
- 36.Kuijer PP, et al. , Beneficial and limiting factors affecting return to work after total knee and hip arthroplasty: a systematic review. J Occup Rehabil, 2009. 19(4): p. 375–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lankinen P, et al. , Are patient-related pre-operative factors influencing return to work after total knee arthroplasty. Knee, 2019. 26(4): p. 853–860. [DOI] [PubMed] [Google Scholar]
- 38.Herrera-Escobar JP, et al. , Long-term social dysfunction after trauma: What is the prevalence, risk factors, and associated outcomes? Surgery, 2019. 166(3): p. 392–397. [DOI] [PubMed] [Google Scholar]
- 39.Zatzick D, et al. , A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg, 2008. 248(3): p. 429–37. [DOI] [PubMed] [Google Scholar]
- 40.Mavranezouli I, et al. , Psychological treatments for post-traumatic stress disorder in adults: a network meta-analysis. Psychol Med, 2020. 50(4): p. 542–555. [DOI] [PubMed] [Google Scholar]
- 41.Clark MR, Hurley RW, and Adams MCB, Re-assessing the Validity of the Opioid Risk Tool in a Tertiary Academic Pain Management Center Population. Pain Med, 2018. 19(7): p. 1382–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McLaughlin KA, et al. , Childhood adversities and post-traumatic stress disorder: evidence for stress sensitisation in the World Mental Health Surveys. Br J Psychiatry, 2017. 211(5): p. 280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cocchiara RA, et al. , Returning to work after breast cancer: A systematic review of reviews. Work, 2018. 61(3): p. 463–476. [DOI] [PubMed] [Google Scholar]
- 44.Boersma AR, et al. , No association between preoperative physical activity level and time to return to work in patients after total hip or knee arthroplasty: A prospective cohort study. PLoS One, 2019. 14(9): p. e0221932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ferket BS, et al. , Impact of total knee replacement practice: cost effectiveness analysis of data from the Osteoarthritis Initiative. bmj, 2017. 356: p. j1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Allen KD, Golightly YM, and White DK, Gaps in appropriate use of treatment strategies in osteoarthritis. Best Practice & Research Clinical Rheumatology, 2017. 31(5): p. 746–759. [DOI] [PubMed] [Google Scholar]
- 47.Tilbury C, et al. , Return to work after total hip and knee arthroplasty: results from a clinical study. Rheumatology international, 2015. 35(12): p. 2059–2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carroll I, et al. , A pilot cohort study of the determinants of longitudinal opioid use after surgery. Anesth Analg, 2012. 115(3): p. 694–702. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


