Abstract
Smoking is the most well-established cause of chronic airflow obstruction (CAO) but particulate air pollution and poverty have also been implicated. We regressed sex-specific prevalence of CAO from 41 Burden of Obstructive Lung Disease study sites against smoking prevalence from the same study, the gross national income per capita and the local annual mean level of ambient particulate matter (PM2.5) using negative binomial regression. The prevalence of CAO was not independently associated with PM2.5 but was strongly associated with smoking and was also associated with poverty. Strengthening tobacco control and improved understanding of the link between CAO and poverty should be prioritised.
Keywords: COPD epidemiology
Introduction
The most important cause of chronic airflow obstruction (CAO) is tobacco smoking. The Global Burden of Disease programme has suggested that air pollution is second only to smoking in determining loss of disability-adjusted life-years due to chronic respiratory disease.1 Evidence for this was obtained by applying the risk of disease associated with air pollution exposure, as estimated from various studies, to the known distribution of fine particulate matter (PM2.5) across the world.
In this analysis, we investigated the ecological association (ie, using aggregated data)2 between the prevalence of CAO, as estimated from a large multisite study, and levels of ambient PM2.5.
Methods
The prevalence of CAO and the prevalence of smoking were estimated for 41 sites of the Burden of Obstructive Lung Disease (BOLD) study (online supplemental file for details).3 The level of poverty of each site was estimated from the gross national income (GNI) per capita at the time of the survey, using data from the World Bank.4 Annual mean PM2.5 levels (all composition, and dust and sea-salt removed (DSSR)) for each site coordinates and a 10 km radius buffer (site as centre) were obtained from a public dataset.5 6
thoraxjnl-2020-216223supp001.pdf (119.6KB, pdf)
The unit of our analysis was the site, and the analysis was stratified by sex (online supplemental file for details).
Results
The prevalence of CAO across sites ranged from 3.5% to 23.2% in men, and from 2% to 19.4% in women (table 1). As expected, the prevalence of CAO was substantially lower among never smokers (online supplemental table S1).
Table 1.
Survey date, prevalence of chronic airflow obstruction (CAO) and smoking in men and women, gross national income (GNI) per capita and annual mean PM2.5 levels for the 41 sites of the Burden of Obstructive Lung Disease study
| Site | Mid-date of survey | CAO in men (%) |
CAO in women (%) |
Ever smoking prevalence in men (%) |
Ever smoking prevalence in women (%) |
GNI per capita, PPP (current international $) |
PM2.5 (all composition) (μg/m3) |
PM2.5 (all composition) 10 km radius buffer (μg/m3) |
PM2.5 (dust and sea-salt removed) (μg/m3) | PM2.5 (dust and sea-salt removed) 10 km radius buffer (μg/m3) |
| Albania (Tirana) | 17/02/2013 | 12.8 | 4.2 | 63.0 | 11.4 | 10 750 | 25 | 16.7 | 15 | 10.0 |
| Algeria (Annaba) | 28/06/2012 | 9.3 | 4.5 | 76.5 | 0.7 | 13 230 | 21 | 14.5 | 8 | 5.5 |
| Australia (Sydney) | 30/07/2006 | 7.9 | 13.8 | 60.8 | 47.5 | 32 970 | 7 | 6.6 | 4 | 4.0 |
| Austria (Salzburg) | 11/01/2005 | 12.8 | 19.4 | 64.4 | 44.3 | 34 940 | 23 | 18.1 | 20 | 16.0 |
| Benin (Sèmè-Kpodji) | 06/03/2014 | 6.6 | 8.1 | 4.6 | 0 | 2100 | 28 | 24.8 | 13 | 11.7 |
| Cameroon (Limbe) | 11/02/2015 | 6.3 | 4.3 | 35.9 | 2.9 | 3390 | 41 | 37.0 | 20 | 18.0 |
| Canada (Vancouver) | 30/12/2003 | 12.8 | 12.0 | 66.0 | 50.3 | 31 540 | 5 | 5.9 | 4 | 5.2 |
| China (Guangzhou) | 26/11/2002 | 9.9 | 6.3 | 81.4 | 6.3 | 3520 | 40 | 38.7 | 39 | 37.2 |
| England (London) | 27/02/2007 | 16.1 | 15.8 | 71.8 | 57.1 | 35 240 | 15 | 15.3 | 13 | 13.2 |
| Estonia (Tartu) | 25/02/2009 | 8.7 | 5.2 | 63.8 | 31.5 | 19 880 | 12 | 10.7 | 11 | 9.4 |
| Germany (Hannover) | 16/07/2005 | 10.0 | 7.8 | 73.1 | 50 | 32 350 | 20 | 20.0 | 18 | 18.2 |
| Iceland (Reykjavik) | 28/04/2005 | 8.9 | 13.3 | 70.7 | 61.3 | 35 470 | 4 | 4.1 | 1 | 1.4 |
| India (Kashmir) | 11/03/2011 | 17.3 | 15.4 | 76.4 | 28.8 | 4580 | 33 | 33.6 | 26 | 26.7 |
| India (Mumbai) | 13/05/2007 | 6.2 | 7.9 | 15.6 | 0 | 3610 | 39 | 40.3 | 34 | 34.6 |
| India (Mysore) | 08/04/2012 | 11.2 | 5.5 | 22.1 | 1.4 | 4850 | 22 | 22.1 | 19 | 19.9 |
| India (Pune) | 24/09/2009 | 5.8 | 6.7 | 20.9 | 0.3 | 4000 | 45 | 44.9 | 40 | 39.3 |
| Jamaica | 01/03/2015 | 10.3 | 7.5 | 64.2 | 18.5 | 8280 | 8 | 6.5 | 3 | 2.3 |
| Kyrgyzstan (Chui) | 04/07/2013 | 13.9 | 7.9 | 77.9 | 7.5 | 3050 | 19 | 18.5 | 9 | 8.9 |
| Kyrgyzstan (Naryn) | 02/07/2013 | 11.0 | 4.7 | 60.4 | 2.4 | 3050 | 24 | 23.5 | 7 | 7.0 |
| Malawi (Blantyre) | 24/10/2013 | 6.9 | 9.1 | 30.6 | 2.5 | 1120 | 11 | 11.1 | 11 | 10.5 |
| Malawi (Chikwawa) | 15/04/2015 | 18.0 | 9.4 | 48.6 | 11.3 | 1190 | 16 | 15.5 | 15 | 14.5 |
| Malaysia (Penang) | 15/08/2013 | 4.4 | 3.4 | 49.7 | 0 | 23 470 | 33 | 22.8 | 30 | 20.8 |
| Morocco (Fes) | 17/10/2010 | 11.9 | 7.5 | 59.3 | 1.0 | 6240 | 24 | 19.1 | 6 | 5.0 |
| Netherlands (Maastricht) | 30/06/2008 | 19.0 | 17.2 | 73.7 | 60.3 | 45 110 | 14 | 14.1 | 13 | 12.6 |
| Nigeria (Ile-Ife) | 10/09/2011 | 7.5 | 6.7 | 23.4 | 3.7 | 4920 | 30 | 34.3 | 15 | 17.1 |
| Norway (Bergen) | 13/08/2005 | 14.8 | 10.2 | 71.0 | 57.8 | 48 300 | 7 | 6.7 | 4 | 4.4 |
| Pakistan (Karachi) | 18/01/2015 | 14.6 | 6.5 | 48.6 | 8.0 | 5050 | 68 | 67.9 | 17 | 17.0 |
| Philippines (Manila) | 25/12/2005 | 13.0 | 5.2 | 83.9 | 31.1 | 5050 | 28 | 27.6 | 21 | 20.6 |
| Philippines (Nampicuan-Talugtug) | 21/08/2007 | 16.3 | 12.3 | 77.0 | 30.1 | 5710 | 13 | 12.6 | 10 | 10.2 |
| Poland (Krakow) | 10/05/2005 | 15.0 | 12.3 | 79.4 | 43.8 | 13 650 | 37 | 35.8 | 34 | 33.5 |
| Portugal (Lisbon) | 26/08/2008 | 13.9 | 9.5 | 61.6 | 22.1 | 25 590 | 14 | 10.9 | 8 | 6.5 |
| Saudi Arabia (Riyadh) | 06/10/2012 | 3.5 | 2.8 | 48.3 | 2.2 | 51 250 | 64 | 64.1 | 13 | 13.0 |
| South Africa (Uitsig-Ravensmead) | 05/04/2005 | 23.8 | 16.2 | 84.4 | 57.9 | 9610 | 8 | 7.5 | 5 | 4.5 |
| Sri Lanka | 28/09/2013 | 11.7 | 3.9 | 48.9 | 0.2 | 10 370 | 15 | 14.2 | 10 | 9.3 |
| Sudan (Gezeira) | 25/04/2016 | 5.6 | 6.0 | 47.8 | 1.4 | 4260 | 40 | 40.2 | 5 | 5.0 |
| Sudan (Khartoum) | 25/03/2013 | 10.4 | 10.0 | 38.4 | 2.9 | 2690 | 39 | 38.4 | 6 | 5.7 |
| Sweden (Uppsala) | 20/03/2007 | 10.2 | 8.3 | 68.5 | 52.7 | 41 850 | 8 | 6.7 | 7 | 5.7 |
| Trinidad & Tobago | 23/06/2015 | 6.6 | 6.7 | 51.3 | 12.0 | 33 280 | 7 | 7.1 | 1 | 1.0 |
| Tunisia (Sousse) | 01/11/2010 | 8.4 | 2.0 | 79.9 | 9.1 | 9750 | 20 | 17.3 | 6 | 5.3 |
| Turkey (Adana | 30/12/2003 | 19.8 | 9.1 | 81.0 | 30.5 | 9430 | 32 | 27.7 | 17 | 14.8 |
| USA (Lexington, KY) | 13/02/2006 | 13.6 | 16.2 | 78.6 | 54.3 | 47 160 | 11 | 9.9 | 10 | 9.7 |
PM2.5, particulate matter <2.5 µm aerodynamic diameter; PPP, Purchasing power parity.
The prevalence of smoking varied from 4.6% to 84.4% in men and from 0% to 61.3% in women. The levels of all composition PM2.5 ranged from 4 µg/m3 in Reykjavik (Iceland) to 68 µg/m3 in Karachi (Pakistan). The GNI varied from $1120 in Malawi to $51 250 in Saudi Arabia (table 1).
Lower PM2.5 levels were weakly correlated with a higher prevalence of CAO, in both sexes (figure 1A). Among never smokers (figure 1B) and when using DSSR PM2.5, there was no correlation (figure 1C).
Figure 1.
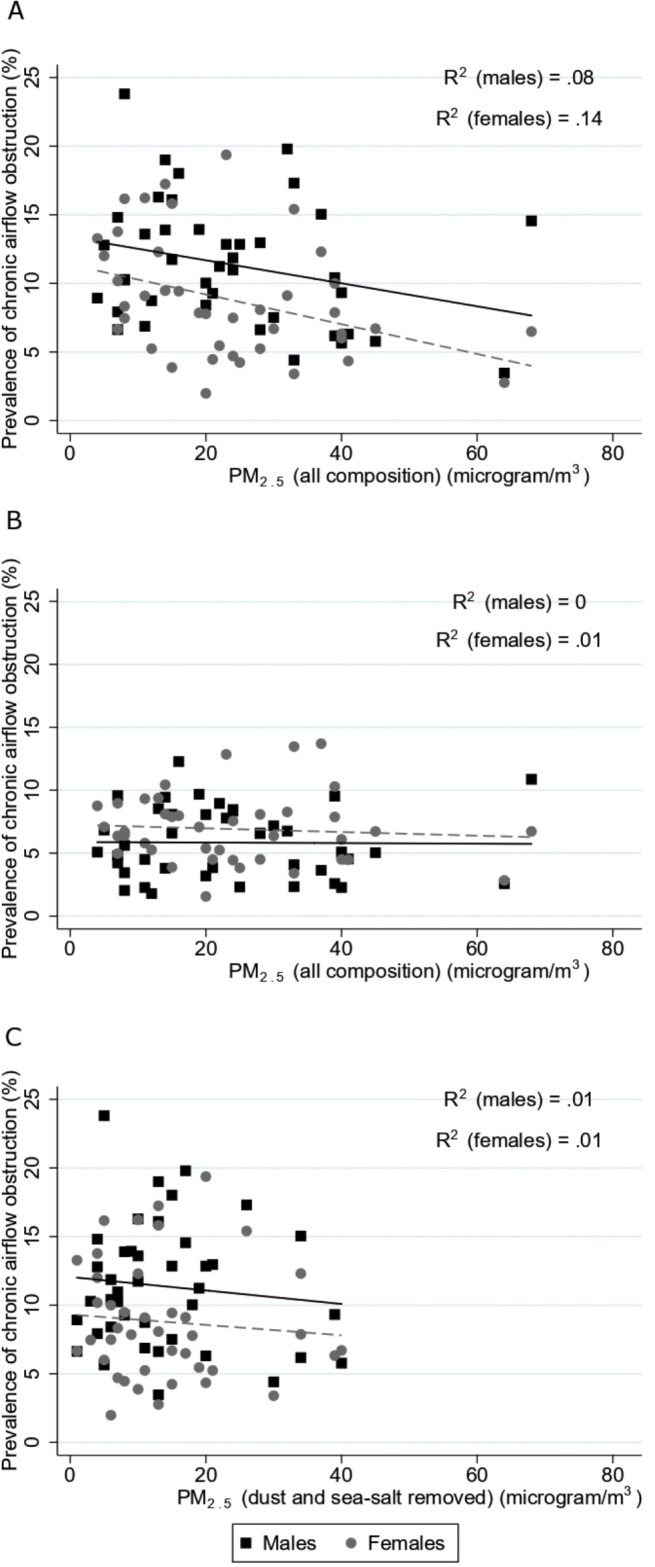
Relation between prevalence of chronic airflow obstruction and annual mean levels of (a) PM2.5 (all composition, μg/m3) for the whole sample, (B) PM2.5 (all composition, μg/m3) for never smokers and (C) PM2.5 (dust and sea-salt removed, μg/m3) for the whole sample.
In both sexes, the prevalence of CAO was strongly positively associated with smoking and negatively associated with GNI. There was no association of prevalence of CAO with levels of PM2.5 (all composition) (table 2). The sensitivity analyses using all composition PM2.5 for a 10 km radius buffer and using DSSR PM2.5 showed no substantive difference from the main analysis (online supplemental tables S2–S4).
Table 2.
Ecological negative binomial regression of chronic airflow obstruction against log(GNI), smoking and log(PM2.5), by sex
| Variable | men | women | ||||
| Rate ratio | 95% CI | P value | Rate ratio | 95% CI | P value | |
| Smoking | 4.17 | 2.40 to 7.26 | <0.001 | 11.3 | 5.64 to 22.6 | <0.001 |
| Log(GNI) | 0.90 | 0.81 to 0.99 | 0.04 | 0.83 | 0.73 to 0.94 | 0.003 |
| Log(PM2.5) | 0.92 | 0.78 to 1.07 | 0.28 | 1.05 | 0.89 to 1.25 | 0.55 |
GNI, gross national income; PM2.5, particulate matter <2.5µm aerodynamic diameter.
Discussion
We were unable to show evidence of an ecological association between the prevalence of CAO and annual mean levels of PM2.5, although we have shown clear independent associations with the prevalence of smoking and GNI.
Our findings suggest that PM2.5 is unlikely to have a substantial effect on the prevalence of CAO. We have previously shown that indoor burning of solid fuels, another source of PM2.5, is also unlikely to be substantially associated with CAO,7 a conclusion supported by the findings of three large Chinese studies.8–10 Our findings are compatible with the large European ESCAPE project, which showed little evidence of an effect of any pollutant on the FEV1/FVC or its change over time.11
This analysis has several strengths. The aggregate data on prevalence of CAO and smoking were taken directly from the BOLD study. Spirometry was post-bronchodilator, and its quality was assured with a strong training programme and regular review of all spirograms in a quality control centre.
All ecological analyses have potential weaknesses. One is the temptation to ascribe the associations observed at the site level to similar associations at an individual level. In this instance, there is independent analysis showing the association of CAO with smoking12 and poverty13 at the individual level within the BOLD study.
Ecological analyses are also prone to confounding. There are strong ecological associations between the prevalence of smoking, GNI and PM2.5. The poorer countries have fewer smokers, less CAO and greater pollution levels. This probably explains the negative association of CAO with PM2.5 in the population as a whole, which was not seen for never smokers (figure 1B), or with DSSR PM2.5, or in the regression analysis adjusted for smoking prevalence and GNI.
Ecological analyses can be misleading if the average exposure in a site does not represent the exposure of those with the disease.14 Although there may be differences in pollution exposure within each site, these are likely to be small compared with the larger variation between sites, which ranged from 4 µg/m3 in Reykjavik (Iceland) to 68 µg/m3 in Karachi (Pakistan). It is unlikely that anyone living in Karachi will have exposure to ambient PM2.5 lower than any of those living in Reykjavik. The wide variation in income across sites is probably less well represented by GNI. Using the same estimate of GNI for rural and urban areas is likely to lead to more substantial errors than the approximations made for PM2.5. Nevertheless, we have found an association between poverty and CAO both at the ecological and individual levels in the BOLD study,13 and it is likely that the imprecision introduced here by using GNI to represent the site income has reduced the strength of association with CAO.
These results do not imply that air pollution is not harmful to lung growth in utero and during childhood, lung health or general health, and we clearly do not address in this study the potential of PM2.5 to cause other pathologies or to trigger acute exacerbations of disease. We cannot exclude the possibility that the toxicology of PM2.5 varies geographically, that a component of PM2.5 causes CAO but it is not always present, or that there is another pollutant that is highly correlated with PM2.5 in some sites that causes CAO. Several researchers have suggested that the properties15 or sources16 of particles may also be important in determining their effects.
This ecological study shows that, after adjustment for smoking and GNI, ambient PM2.5 is unlikely to explain a substantial amount of the prevalence of CAO, while the ecological association of smoking with CAO is strong and the association of poverty with CAO indicates that this is also likely to play an important role in its origins.
Acknowledgments
The authors thank the participants and field workers of this study for their time and cooperation, and the BOLD (Burden of Obstructive Lung Disease) Coordinating Centre members for their technical and scientific support.
Footnotes
Twitter: @andrefsamaral, @Marks1Guy
Collaborators: The BOLD (Burden of Obstructive Lung Disease) Collaborative Research Group members
Albania: Hasan Hafizi (PI), Anila Aliko, Donika Bardhi, Holta Tafa, Natasha Thanasi, Arian Mezini, Alma Teferici, Dafina Todri, Jolanda Nikolla, and Rezarta Kazasi (Tirana University Hospital Shefqet Ndroqi, Albania); Algeria: Hamid Hacene Cherkaski (PI), Amira Bengrait, Tabarek Haddad, Ibtissem Zgaoula, Maamar Ghit, Abdelhamid Roubhia, Soumaya Boudra, Feryal Atoui, Randa Yakoubi, Rachid Benali, Abdelghani Bencheikh, and Nadia Ait-Khaled (Faculté de Médecine Annaba, Service de Epidémiologie et Médecine Préventive, El Hadjar, Algeria); Australia: Christine Jenkins (PI), Guy Marks (PI), Tessa Bird, Paola Espinel, Kate Hardaker, Brett Toelle (Woolcock Institute of Medical Research, Sidney, Australia); Austria: Michael Studnicka (PI), Torkil Dawes, Bernd Lamprecht, and Lea Schirhofer (Department of Pulmonary Medicine, Paracelsus Medical University, Salzburg, Austria); Bangladesh: Akramul Islam (PI), Syed Masud Ahmed (Co-PI), Shayla Islam, Qazi Shafayetul Islam, Mesbah-Ul-Haque, Tridib Roy Chowdhury, Sukantha Kumar Chatterjee, Dulal Mia, Shyamal Chandra Das, Mizanur Rahman, Nazrul Islam, Shahaz Uddin, Nurul Islam, Luiza Khatun, Monira Parvin, Abdul Awal Khan, and Maidul Islam (James P. Grant School of Public Health, BRAC [Building Resources Across Communities] University, Institute of Global Health, Dhaka, Bangladesh); Benin: Herve Lawin (PI), Arsene Kpangon, Karl Kpossou, Gildas Agodokpessi, Paul Ayelo, Benjamin Fayomi (Unit of Teaching and Research in Occupational and Environmental Health, University of Abomey Calavi, Cotonou, Benin); Cameroon: Bertrand Mbatchou (PI), Atongno Humphrey Ashu (Douala General Hospital, Douala, Cameroon); Canada: Wan C. Tan (PI) and Christine Lo (Center for Heart Lung Innovation, University of British Columbia, Vancouver, BC, Canada); China: NanShan Zhong (Principal Investigator [PI]), Shengming Liu, Jiachun Lu, Pixin Ran, Dali Wang, Jingping Zheng, and Yumin Zhou (Guangzhou Institute of Respiratory Diseases, Guangzhou Medical College, Guangzhou, China); Estonia: Rain Jõgi (PI), Hendrik Laja, Katrin Ulst, Vappu Zobel, and Toomas-Julius Lill (Lung Clinic, Tartu University Hospital, Tartu, Estonia); Gabon: Ayola Akim Adegnika (PI) (Centre de Recherches Medicale de Lambarene, Lambarene, Gabon); Germany: Tobias Welte (PI), Isabelle Bodemann, Henning Geldmacher, and Alexandra Schweda-Linow (Hannover Medical School, Hannover, Germany); Iceland: Thorarinn Gislason (PI), Bryndis Benedikdtsdottir, Kristin Jörundsdottir, Lovisa Gudmundsdottir, Sigrun Gudmundsdottir, and Gunnar Gundmundsson, (Department of Allergy, Respiratory Medicine, and Sleep, Landspitali University Hospital, Reykjavik, Iceland); India: Mahesh Rao (PI) (JSS Medical College, Mysuru, India); Parvaiz A Koul (PI), Sajjad Malik, Nissar A Hakim, and Umar Hafiz Khan (Sher-i-Kashmir Institute of Medical Sciences, Srinagar, J&K, India); Rohini Chowgule (PI), Vasant Shetye, Jonelle Raphael, Rosel Almeda, Mahesh Tawde, Rafiq Tadvi, Sunil Katkar, Milind Kadam, Rupesh Dhanawade, and Umesh Ghurup (Indian Institute of Environmental Medicine, Mumbai, India); Sanjay Juvekar (PI), Siddhi Hirve, Somnath Sambhudas, Bharat Chaidhary, Meera Tambe, Savita Pingale, Arati Umap, Archana Umap, Nitin Shelar, Sampada Devchakke, Sharda Chaudhary, Suvarna Bondre, Savita Walke, Ashleshsa Gawhane, Anil Sapkal, Rupali Argade, and Vijay Gaikwad (Vadu Health and Demographic Surveillance System, King Edward Memorial Hospital Research Centre Pune, Pune India); Sundeep Salvi (PI), Bill Brashier, Jyoti Londhe, and Sapna Madas (Chest Research Foundation, Pune India); Jamaica: Althea Aquart-Stewart (PI), Akosua Francia Aikman (University of the West Indies, Kingston, Jamaica); Kyrgyzstan: Talant M. Sooronbaev (PI), Bermet M. Estebesova, Meerim Akmatalieva, Saadat Usenbaeva, Jypara Kydyrova, Eliza Bostonova, Ulan Sheraliev, Nuridin Marajapov, Nurgul Toktogulova, Berik Emilov, Toktogul Azilova, Gulnara Beishekeeva, Nasyikat Dononbaeva, and AijamalTabyshova (Pulmunology and Allergology Department, National Centre of Cardiology and Internal Medicine, Bishkek, Kyrgyzstan); Malawi: Kevin Mortimer (PI), Wezzie Nyapigoti, Ernest Mwangoka, Mayamiko Kambwili, Martha Chipeta, Gloria Banda, Suzgo Mkandawire, and Justice Banda (the Malawi Liverpool Wellcome Trust, Blantyre, Malawi); Malaysia: Li-Cher Loh (PI), Abdul Rashid, and Siti Sholehah (RCSI & UCD Malaysia Campus, Penang, Malaysia); Morocco: Mohamed C Benjelloun (PI), Chakib Nejjari, Mohamed Elbiaze, and Karima El Rhazi (Laboratoire d’épidémiologie, Recherche Clinique et Santé Communautaire, Fès, Morocco); Netherlands: E.F.M. Wouters and Lowie Vanfleteren (Maastricht University Medical Center, Maastricht, the Netherlands); Nigeria: Daniel Obaseki (PI), Gregory Erhabor, Olayemi Awopeju, and Olufemi Adewole (Obafemi Awolowo University, Ile-Ife, Nigeria); Norway: Amund Gulsvik (PI), Tina Endresen, and Lene Svendsen (Department of Thoracic Medicine, Institute of Medicine, University of Bergen, Bergen, Norway); Pakistan: Asaad A. Nafees (PI) Muhammad Irfan, Zafar Fatmi, Aysha Zahidie, Natasha Shaukat and Meesha Iqbal (Aga Khan University, Karachi, Pakistan); Philippines: Luisito F. Idolor (PI), Teresita S. de Guia, Norberto A. Francisco, Camilo C. Roa, Fernando G. Ayuyao, Cecil Z. Tady, Daniel T. Tan, Sylvia Banal-Yang, Vincent M. Balanag, Jr., Maria Teresita N. Reyes, and Renato. B. Dantes (Lung Centre of the Philippines, Philippine General Hospital, Nampicuan and Talugtug, the Philippines); Renato B. Dantes (PI), Lourdes Amarillo, Lakan U. Berratio, Lenora C. Fernandez, Norberto A. Francisco, Gerard S. Garcia, Teresita S. de Guia, Luisito F. Idolor, Sullian S. Naval, Thessa Reyes, Camilo C. Roa, Jr., Ma. Flordeliza Sanchez, and Leander P. Simpao (Philippine College of Chest Physicians, Manila, the Philippines); Poland: Ewa Nizankowska Mogilnicka (PI), Jakub Frey, Rafal Harat, Filip Mejza, Pawel Nastalek, Andrzej Pajak, Wojciech Skucha, Andrzej Szczeklik, and Magda Twardowska, (Division of Pulmonary Diseases, Department of Medicine, Jagiellonian University School of Medicine, Krakow, Poland); Portugal: Cristina Bárbara (PI), Fátima Rodrigues, Hermínia Dias, João Cardoso, João Almeida, Maria João Matos, Paula Simão, Moutinho Santos, and Reis Ferreira (the Portuguese Society of Pneumology, Lisbon, Portugal); Saudi Arabia: M. Al Ghobain (PI), H. Alorainy (PI), E. El-Hamad, M. Al Hajjaj, A. Hashi, R. Dela, R. Fanuncio, E. Doloriel, I. Marciano, and L. Safia (Saudi Thoracic Society, Riyadh, Saudi Arabia); South Africa: Eric Bateman (PI), Anamika Jithoo (PI), Desiree Adams, Edward Barnes, Jasper Freeman, Anton Hayes, Sipho Hlengwa, Christine Johannisen, Mariana Koopman, Innocentia Louw, Ina Ludick, Alta Olckers, Johanna Ryck, and Janita Storbeck, (University of Cape Town Lung Institute, Cape Town, South Africa); Sri Lanka: Kirthi Gunasekera (PI), Rajitha Wickremasinghe (Medical Research Institute, Central Chest Clinic, Colombo, Sri Lanka); Sudan: Asma Elsony (PI), Hana A. Elsadig, Nada Bakery Osman, Bandar Salah Noory, Monjda Awad Mohamed, Hasab Alrasoul Akasha Ahmed Osman, Namarig Moham ed Elhassan, Abdel Mu‘is El Zain, Marwa Mohamed Mohamaden, Suhaiba Khalifa, Mahmoud Elhadi, Mohand Hassan, and Dalia Abdelmonam (the Epidemiological Laboratory, Khartoum, Sudan); Sweden: Christer Janson (PI), Inga Sif Olafsdottir, Katarina Nisser, Ulrike Spetz Nyström, Gunilla Hägg, and Gun-Marie Lund (Department of Medical Sciences: Respiratory Medicine and Allergology, Uppsala University, Uppsala, Sweden); Trinidad and Tobago: Terence Seemungal (PI), Fallon Lutchmansingh, Liane Conyette (University of the West Indies, St. Augustine, Trinidad and Tobago); Tunisia: Imed Harrabi (PI), Myriam Denguezli, Zouhair Tabka, Hager Daldoul, Zaki Boukheroufa, Firas Chouikha, and Wahbi Belhaj Khalifa (University Hospital Farhat Hached, Faculté de Médecine, Sousse, Tunisia); Turkey: Ali Kocabaş (PI), Attila Hancioglu, Ismail Hanta, Sedat Kuleci, Ahmet Sinan Turkyilmaz, Sema Umut, and Turgay Unalan (Department of Chest Diseases, Cukurova University School of Medicine, Adana, Turkey); United Kingdom: Peter GJ Burney (PI), Anamika Jithoo, Louisa Gnatiuc, Hadia Azar, Jaymini Patel, Caron Amor, James Potts, Michael Tumilty, and Fiona McLean, Risha Dudhaiya (National Heart and Lung Institute, Imperial College London, London, UK); United States of America: A Sonia Buist (PI),(Oregon University of Health Sciences, Portland, OR) Mary Ann McBurnie, William M Vollmer, Suzanne Gillespie (Kaiser Permanente Center for Health Research, Portland, OR); Sean Sullivan (University of Washington, Seattle, WA); Todd A Lee, Kevin B Weiss, (Northwestern University, Chicago, IL); Robert L Jensen, Robert Crapo (Latter Day Saints Hospital, Salt Lake City, Utah); Paul Enright (University of Arizona, Tucson, AZ); David M. Mannino (PI), John Cain, Rebecca Copeland, Dana Hazen, and Jennifer Methvin, (University of Kentucky, Lexington, KY).
Contributors: AFSA, CM and PGJB analysed the data. AFSA and PGJB drafted the manuscript. AFSA, PGJB, JP, CM, FM, DM, TARS, MPA, LCL, CJ, SJ, MD, IH, EFMW, HC, KM, RJ, EDB, EF, MAG, WT, DO, AES, MS, AAS, PK, HL, AAN, OA, GE, TG, TW, AG, RN, LG, AK, GM, TS, BMN, CB and ASB discussed the results, read and approved the final manuscript.
Funding: Supported by Wellcome Trust grant 085790/Z/08/Z for the BOLD (Burden of Obstructive Lung Disease) Study. The initial BOLD programprogramme was funded in part by unrestricted educational grants to the Operations CenterCentre in Portland, Oregon from Altana, Aventis, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Merck, Novartis, Pfizer, Schering-Plough, Sepracor, and the University of Kentucky (Lexington, KY). A full list of local funders can be found at https://www.boldstudy.org.
Competing interests: RN reports grants and personal fees from Boehringer Ingelheim, AstraZeneca and Novartis outside the submitted work. EDB reports personal fees from Novartis, AstraZeneca, Orion, Menarirni, Boehringer Ingelheim and ALK outside the submitted work. KM reports grants from GlaxoSmithKline during the conduct of the study. TW reports grants from Boehringer Ingelheim and Pfizer during the conduct of the study. FM reports fees from Medycyba Praktyczna, Sandoz and Chiesi outside the submitted work. DM reports salary and shares from GlaxoSmithKline outside the submitted work. IH reports grants from Boehringer Ingelheim during the conduct of the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
The BOLD (Burden of Obstructive Lung Disease) Collaborative Research Group members:
Hasan Hafizi, Anila Aliko, Donika Bardhi, Holta Tafa, Natasha Thanasi, Arian Mezini, Alma Teferici, Dafina Todri, Jolanda Nikolla, Rezarta Kazasi, Hamid Hacene Cherkaski, Amira Bengrait, Tabarek Haddad, Ibtissem Zgaoula, Maamar Ghit, Abdelhamid Roubhia, Soumaya Boudra, Feryal Atoui, Randa Yakoubi, Rachid Benali, Abdelghani Bencheikh, Nadia Ait-Khaled, Guy Marks, Tessa Bird, Paola Espinel, Kate Hardaker, Brett Toelle, Michael Studnicka, Torkil Dawes, Bernd Lamprecht, Lea Schirhofer, Akramul Islam, Syed Masud Ahmed, Shayla Islam, Qazi Shafayetul Islam, Mesbah Ul-Haque, Tridib Roy Chowdhury, Sukantha Kumar Chatterjee, Dulal Mia, Shyamal Chandra Das, Mizanur Rahman, Nazrul Islam, Shahaz Uddin, Nurul Islam, Luiza Khatun, Monira Parvin, Abdul Awal Khan, Maidul Islam, Herve Lawin, Arsene Kpangon, Karl Kpossou, Gildas Agodokpessi, Paul Ayelo, Benjamin Fayomi, Bertrand Mbatchou, Atongno Humphrey Ashu, Wan C Tan, Christine Lo, NanShan Zhong, Shengming Liu, Jiachun Lu, Pixin Ran, Dali Wang, Jingping Zheng, Yumin Zhou, Rain Jõgi, Hendrik Laja, Katrin Ulst, Vappu Zobel, Toomas-Julius Lill, Ayola Akim Adegnika, Tobias Welte, Isabelle Bodemann, Henning Geldmacher, Alexandra Schweda-Linow, Thorarinn Gislason, Bryndis Benedikdtsdottir, Kristin Jörundsdottir, Lovisa Gudmundsdottir, Sigrun Gudmundsdottir, Gunnar Gundmundsson, Mahesh Rao, Parvaiz A Koul, Sajjad Malik, Nissar A Hakim, Umar Hafiz Khan, Rohini Chowgule, Vasant Shetye, Jonelle Raphael, Rosel Almeda, Mahesh Tawde, Rafiq Tadvi, Sunil Katkar, Milind Kadam, Rupesh Dhanawade, Umesh Ghurup, Sanjay Juvekar, Siddhi Hirve, Somnath Sambhudas, Bharat Chaidhary, Meera Tambe, Savita Pingale, Arati Umap, Archana Umap, Nitin Shelar, Sampada Devchakke, Sharda Chaudhary, Suvarna Bondre, Savita Walke, Ashleshsa Gawhane, Anil Sapkal, Rupali Argade, Vijay Gaikwad, Sundeep Salvi, Bill Brashier, Jyoti Londhe, Sapna Madas, Althea Aquart-Stewart, Akosua Francia Aikman, Talant M Sooronbaev, Bermet M Estebesova, Meerim Akmatalieva, Saadat Usenbaeva, Jypara Kydyrova, Eliza Bostonova, Ulan Sheraliev, Nuridin Marajapov, Nurgul Toktogulova, Berik Emilov, Toktogul Azilova, Gulnara Beishekeeva, Nasyikat Dononbaeva, Aijamal Tabyshova, Kevin Mortimer, Wezzie Nyapigoti, Ernest Mwangoka, Mayamiko Kambwili, Martha Chipeta, Gloria Banda, Suzgo Mkandawire, Justice Banda, Li-Cher Loh, Abdul Rashid, Siti Sholehah, Mohamed C Benjelloun, Chakib Nejjari, Mohamed Elbiaze, Karima El Rhazi, E.F.M Wouters, Lowie Vanfleteren, Daniel Obaseki, Gregory Erhabor, Olayemi Awopeju, Olufemi Adewole, Amund Gulsvik, Tina Endresen, Lene Svendsen, Asaad A Nafees, Muhammad Irfan, Zafar Fatmi, Aysha Zahidie, Natasha Shaukat, Meesha Iqbal, Luisito F Idolor, Teresita S de Guia, Norberto A Francisco, Camilo C Roa, Fernando G Ayuyao, Cecil Z Tady, Daniel T Tan, Sylvia Banal-Yang, Vincent M Balanag, Renato B Dantes, Lourdes Amarillo, Lakan U Berratio, Lenora C Fernandez, Norberto A Francisco, Gerard S Garcia, Teresita S de Guia, Luisito F Idolor, Sullian S. Naval, Thessa Reyes, Camilo C Roa, Ma Flordeliza Sanchez, Leander P Simpao, Ewa Nizankowska Mogilnicka, Jakub Frey, Rafal Harat, Filip Mejza, Pawel Nastalek, Andrzej Pajak, Wojciech Skucha, Andrzej Szczeklik, Magda Twardowska, Cristina Bárbara, Fátima Rodrigues, Hermínia Dias, João Cardoso, João Almeida, Maria João Matos, Paula Simão, Moutinho Santos, Reis Ferreira, M Al Ghobain, H Alorainy, E El-Hamad, M. Al Hajjaj, A Hashi, R Dela, R Fanuncio, E Doloriel, I Marciano, L. Safia, Eric Bateman, Anamika Jithoo, Desiree Adams, Edward Barnes, Jasper Freeman, Anton Hayes, Sipho Hlengwa, Christine Johannisen, Mariana Koopman, Innocentia Louw, Ina Ludick, Alta Olckers, Johanna Ryck, Janita Storbeck, Kirthi Gunasekera, Rajitha Wickremasinghe, Asma Elsony, Hana A Elsadig, Nada Bakery Osman, Bandar Salah Noory, Monjda Awad Mohamed, Suhaiba Khalifa, Mahmoud Elhadi, Mohand Hassan, Dalia Abdelmonam, Christer Janson, Inga Sif Olafsdottir, Katarina Nisser, Ulrike Spetz Nyström, Gunilla Hägg, Gun-Marie Lund, Terence Seemungal, Fallon Lutchmansingh, Liane Conyette, Imed Harrabi, Myriam Denguezli, Zouhair Tabka, Hager Daldoul, Zaki Boukheroufa, Firas Chouikha, Wahbi Belhaj Khalifa, Ali Kocabaş, Attila Hancioglu, Ismail Hanta, Sedat Kuleci, Ahmet Sinan Turkyilmaz, Sema Umut, Turgay Unalan, Peter GJ Burney, Anamika Jithoo, Louisa Gnatiuc, Hadia Azar, Jaymini Patel, Caron Amor, James Potts, Michael Tumilty, Fiona McLean, Risha Dudhaiya, A Sonia Buist, Mary Ann McBurnie, William M Vollmer, Suzanne Gillespie, Sean Sullivan, Todd A Lee, Kevin B Weiss, Robert L Jensen, Robert Crapo, Paul Enright, David M Mannino, John Cain, Rebecca Copeland, Dana Hazen, and Jennifer Methvin
Ethics statements
Patient consent for publication
Not required.
References
- 1. GBD 2015 Chronic Respiratory Disease Collaborators . Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet Respir Med 2017;5:691–706. 10.1016/S2213-2600(17)30293-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Morgenstern H. Ecologic studies in epidemiology: concepts, principles, and methods. Annu Rev Public Health 1995;16:61–81. 10.1146/annurev.pu.16.050195.000425 [DOI] [PubMed] [Google Scholar]
- 3. Buist AS, Vollmer WM, Sullivan SD, et al. The burden of obstructive lung disease initiative (BOLD): rationale and design. COPD 2005;2:277–83. 10.1081/COPD-57610 [DOI] [PubMed] [Google Scholar]
- 4. World Bank . Gni per capita, ppp (current international $). Available: https://databank.worldbank.org/indicator/NY.GNP.PCAP.CD/1ff4a498/Popular-Indicators [Accessed 19 Oct 2019].
- 5. Atmospheric Composition Analysis Group . Surface PM2.5. Available: http://fizz.phys.dal.ca/~atmos/martin/?page_id=140 [Accessed 18 Feb 2020].
- 6. van Donkelaar A, Martin RV, Brauer M, et al. Global estimates of fine particulate matter using a combined Geophysical-Statistical method with information from satellites, models, and monitors. Environ Sci Technol 2016;50:3762–72. 10.1021/acs.est.5b05833 [DOI] [PubMed] [Google Scholar]
- 7. Amaral AFS, Patel J, Kato BS, et al. Airflow obstruction and use of solid fuels for cooking or heating: BOLD results. Am J Respir Crit Care Med 2018;197:595–610. 10.1164/rccm.201701-0205OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smith M, Li L, Augustyn M, et al. Prevalence and correlates of airflow obstruction in ∼317,000 never-smokers in China. Eur Respir J 2014;44:66–77. 10.1183/09031936.00152413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fang L, Gao P, Bao H, et al. Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med 2018;6:421–30. 10.1016/S2213-2600(18)30103-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet 2018;391:1706–17. 10.1016/S0140-6736(18)30841-9 [DOI] [PubMed] [Google Scholar]
- 11. Schikowski T, Adam M, Marcon A, et al. Association of ambient air pollution with the prevalence and incidence of COPD. Eur Respir J 2014;44:614–26. 10.1183/09031936.00132213 [DOI] [PubMed] [Google Scholar]
- 12. Buist AS, McBurnie MA, Vollmer WM, et al. International variation in the prevalence of COPD (the BOLD study): a population-based prevalence study. Lancet 2007;370:741–50. 10.1016/S0140-6736(07)61377-4 [DOI] [PubMed] [Google Scholar]
- 13. Townend J, Minelli C, Mortimer K, et al. The association between chronic airflow obstruction and poverty in 12 sites of the multinational BOLD study. Eur Respir J 2017;49:1601880. 10.1183/13993003.01880-2016 [DOI] [PubMed] [Google Scholar]
- 14. Greenland S, Morgenstern H. Ecological bias, confounding, and effect modification. Int J Epidemiol 1989;18:269–74. 10.1093/ije/18.1.269 [DOI] [PubMed] [Google Scholar]
- 15. Künzli N, Mudway IS, Götschi T, et al. Comparison of oxidative properties, light absorbance, total and elemental mass concentration of ambient PM2.5 collected at 20 European sites. Environ Health Perspect 2006;114:684–90. 10.1289/ehp.8584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Muala A, Rankin G, Sehlstedt M, et al. Acute exposure to wood smoke from incomplete combustion--indications of cytotoxicity. Part Fibre Toxicol 2015;12:33. 10.1186/s12989-015-0111-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
thoraxjnl-2020-216223supp001.pdf (119.6KB, pdf)


