Abstract
Health professionals constitute a group that is at a high risk of COVID-19. They have been found to experience difficulties in many issues, one of which is that they face the risk of infecting themselves and others due to interaction with high-risk patients. The present study investigates how demographical and individual factors and work addiction affected work-life balance and mental health needs of health professionals. The data of the present study were collected in the first wave of pandemic. The hypothesized structural equation model was rejected based on the fit indices. The second analysis of modified model was significant and indicated that whether health professionals live alone or with others such as family members had direct effects on work addiction, indirect effects on work-life balance, and needs for mental health. In addition, gender and working hours had direct effects on work-life balance. The highest effect on work-life balance was caused by work addiction. Moreover, work addiction had a moderate effect on mental health needs. As a result, the current study showed that work-life balance, work addiction, and the need for mental health were affected during the COVID-19 pandemic.
Keywords: Work-life balance, Work addiction, Health professionals, COVID-19, Coronavirus
Health professionals constitute a group that is at a high risk of COVID-19 in Turkey and worldwide (Cetintepe & Ilhan, 2020). In the COVID-19 pandemic, just as in the SARS epidemic, health professionals have been found to experience difficulty in dealing with many issues (Brooks et al.,; 2020; Wu et al., 2013), one of which is that they face the risk of infecting themselves and others by contact with high-risk patients (Chen et al., 2020). In spite of developing naturally, epidemics such as COVID-19 cause health workers to face the obligation of maintaining patient care despite the risk of transmission (Baki & Piyal, 2020). In addition, health professionals also had difficulties such as the experience of being stigmatized as a result of having to provide care services for the patients with COVID-19and having to work under difficult conditions due to strict safety measures, long working hours, fear of getting sick and dying, helplessness and despair caused by the deaths of the patients they cared for, and cancellation of their annual leave (Bao et al., 2020; Wang et al., 2020a; Xiang et al., 2020).
It is a known fact that health professionals have similar problems in their personal and work life during the COVID-19 pandemic and have to deal with both the stress and psychological consequences of the pandemic (Babore et al., 2020; Trumello et al., 2020). Some of the biggest problems of health professionals are the risk of transmitting the virus to their family members and the hardships of taking care of their children due to the closure of nurseries (Chen et al., 2020). Amid the COVID-19 pandemic, women (Lai et al., 2019; Tang et al., 2016), young people (Wu et al., 2013), those with less work experience, and health professionals with children have psychologically been affected more, the reasons for which have been stated as being exposed to long-term quarantine, fear of infecting their families, having an infected family member, and fear of death (Serrano-Ripoll et al., 2020). Since many health professionals are afraid of infecting family members, they have used alternative accommodation options and thus remained separate from their family members and have been unable to fulfill their parental roles in order not to infect those they usually take care of in their families (Dai et al., 2020). However, the balance between professional sacrifice and the fear for themselves and their loved ones has been observed to deteriorate (Ho et al., 2020).
Work-life balance is defined as the relationship between work and off-work life, and the balance in which the demands in a person’s job and personal life are equal (Korkmaz & Erdogan, 2014; Lockwood, 2003). The deterioration in work-life balance leads to important consequences in health professionals’ lives and behaviors. Numerous factors such as irregular working hours, shift working system, role ambiguity, role conflict, lack of occupational safety, excessive or low workload, insufficient wages, and the physical factors arising from the work environment have had negative effects on health professionals during COVID-19 pandemic (Althobaiti et al., 2020; Enli-Tuncay et al., 2020). Nakisci-Kavas and Develi (2020) stated that the COVID-19 pandemic caused serious problems especially for female health professionals disturbing the balance between their family life and work life. In addition, Humphries et al. (2020) found that 73% of a group of health professionals were dissatisfied with their work-life balance, which negatively affected their well-being. In this context, the challenges experienced in different aspects in the COVID-19 pandemic led health professionals to re-question their professions and develop workplace phobia, creating tendencies to quit their jobs (Baki & Piyal, 2020; Malik et al., 2021).
Work-life balance influences the level of work commitment of a professional (Korkmaz & Erdogan, 2014). The concept of work commitment suggests that individuals feel vigorous while doing their work, dedicate themselves to their jobs or get satisfaction from their jobs, and concentrate on their work (Kabar, 2017). In the COVID-19 pandemic, it has been observed that the working environment and conditions are becoming more difficult for health workers in terms of increasing workload, working under pressure, exposure to violence and insults from patients, and meeting the wishes of patients and hospital management (Yüncü & Yılan, 2020). As a consequence of all these problems, health professionals experience physical exhaustion, learned helplessness, health threats, lack of information, fear, anxiety, despondency, loneliness, fatigue, sleep disorders, and psychological problems in the early stage (Bao et al., 2020; Cullen et al., 2020). In addition, in the COVID-19 pandemic health professionals have been unable to handle the physical and emotional burden that arises with increased workload due to long working hours, lack of time, and the increase in the number of infected patients; therefore, their levels of burnout and intentions to leave work are high (Araslar, 2021; Prakash & Pabalkar, 2020). Based on these reasons, the COVID-19 pandemic negatively affected the commitment of health workers to work and work-life balance.
While the total number of cases and mortality is regularly monitored and reported, what is known about the changes in the workplace and life of health professionals during the COVID-19 pandemic is very limited (Schwartz et al., 2020). This study aims to be descriptive in order to determine the balance between the work commitment and life of health professionals during the COVID-19 pandemic.
The Present Study
The present study was conducted with health professionals during COVID-19 pandemic in Turkey. Health professionals have been under risk all over the world since they are in direct contact with patients. Many health professionals got sick and lost their life. The increasing number of patients extended working hours and shifts and increased the workload. In the meantime, health professionals began to fear to transmit the virus to the people they live with, their families and loved ones. When we look at the whole picture and the effect the virus has on societies, we hypothesized that life balance and mental health were affected as well. Taking all these into account, the purpose of the present study was to investigate how demographical and individual factors and work addiction affected work-life balance and mental health needs of health professionals during COVID-19 pandemic. We hypothesized that independent variables of gender, dependents, experience, the people they live with (PTLW), and working hours would have an impact both on work-life balance and work addiction. There are studies (see Aziz & Cunnigham, 2008; Fagan, et al., 2012; Holly & Mohnen, 2012; Smith, 2011) showing the relationship between these variables, which supported our hypothesis. For example, Aziz and Cunnigham (2008) found that work-life imbalance was positively correlated with work addiction. In addition, they stated that working hours was a significant predictor of work-life balance. In the working paper published by International Labour Office (Fagan et al., 2012), long hours of work may have been a trigger for work addiction, and this had an effect on work-life balance. Furthermore, long hours of work were a significant predictor of work-life conflict. The German Institute for Economic Research (Holly & Mohnen, 2012) had similar results in terms of negative impact of long hours of work on work-life balance. We also hypothesized that the changing work-life balance and work addiction would have an impact on participants’ mental health needs. In the literature, studies (Balkin et al., 2018; Jones et al., 2006) showed that work-life balance and work addiction affected mental health. Based on the hypothesized model and the purpose of the study, we investigated answers for the following research questions:
What are the direct and indirect effects of demographic variables (gender, dependents, experience, whom they live with, and working hours) on the work-life balance, work addiction, and need for mental health?
What are the direct and indirect effects of work addiction on the work-life balance and need for mental health?
Are there differences among health professional’s working area (nurse, midwife, paramedic, technician and officials, and doctor) in terms of work addiction and work-life balance scores?
Method
Participants and Procedures
After the study was approved by the relevant institution’s ethics board, the instrument package was collected using Google Forms platform. The participation link was sent through personal connections, WhatsApp groups, social media (Instagram, Facebook, and Twitter), and personal emails. The participation was voluntary, and filling the online form took approximately 10 min. The data were collected in the first wave of the pandemic between April 12 and 25, 2020.
An a priori power analysis using G*Power 3.0.10 (Faul et al., 2009) was used to calculate the minimum sample size needed for this study. Using F tests family and a minimum level of power of 0.95, a medium effect size as f2 = 0.15, and a 0.05 alpha level, the estimated target sample size for this study was reported to be 129. A total of 343 health professionals attended the study from different institutions (e.g., state and private hospitals, family clinics). Three participants who did not respond more than 20% of the items were removed from the data sheet. Four participants were excluded from the study since they did not meet the criteria (were students in the nursing program and not working). Hence, the final analysis included 336 participants.
There were more women (n = 289, 86%) than men (n = 47, 14%) in the study. The mean age of participants was 31.56 years (SD = 8.50; range, 20–59 years). Participants reported their level of education as high school (n = 42, 12.5%), community college (n = 52, 15.5%), undergraduate (n = 207, 61.6%), and graduate (n = 35, 10.4%). Responses to the field of profession were as follows: nurse 37.5% (n = 126); midwife 36.6% (n = 123); technician 10% (n = 34); official 6% (n = 20); paramedic 4.1% (n = 14); medical doctor 3.3% (n = 11); pharmacist 1.5% (n = 5); and dentist 1% (n = 3). The mean of experience was 9.28 years (SD = 8.55; range, 1–40 years). Participants’ average weekly working hours was 42.94 h (SD = 12.36; range, 5–72 h). Responses to the marital status query were as follows: married, 52% (n = 175); single, 46% (n = 154); and separated or widowed, 2% (n = 7). Participants’ responses to the question of whom they live with were as follows: parents or family, %78 (n = 262); alone, 18.2% (n = 61); and friends, %3.8 (n = 13). We asked the participants whether they need psychological help or not. 25.6% of the participants (n = 85) reported they needed psychological help, 44.3% (n = 149) reported they did not, and 30.1% (n = 101) reported that they were not sure.
Measures
Work Addiction
Work Addiction Risk Test (WART) Turkish form (Apaydın, 2011) was used to collect data. The original version of the instrument was developed by Robinson (1999) to measure work addiction with 25 items. After the WART was translated and adapted to Turkish, the form demonstrated a different structure than the original version. The 22 items are categorized into four subscales based on the exploratory and confirmatory factor analysis. The subscales evaluate compulsive tendencies (CT; 8 items), control (7 items), impaired communication/self-absorption (IC; 5 items), and self-worth (2 items).
The WART uses a four-point Likert-type response format with values ranging from 1 (never) to 4 (always). Higher scores mean a high level of work addiction. The measure includes items such as “I prefer to do most things myself, rather than ask for help” and “I stay busy and keep many irons in the fire.” Robinson (1999) reported that WART had a strong internal consistency of the total score, α = 0.88. Apaydın (2011) did not report a reliability score for the WART. For the current study, Cronbach’s alpha of total score was 0.86 and for the compulsive tendencies subscale was 0.78, 0.77 for the control, 0.54 for the impaired communication/self-absorption, and 0.28 for the self-worth. Hence, the self-worth subscale was excluded from the analysis since the alpha score was very low.
Work addiction was represented as a latent variable in the study and estimated by the ordered factor indicators. Hence, a second-order factor analysis was conducted to confirm construct validity. The results indicated that the WLB had an acceptable fit: χ2 (145) = 313.09, p < 0.001; CFI = 0.89; TLI = 0.87; SRMR = 0.054; and RMSEA = 0.058 [90% CI = 0.050–0.067].
Work-Life Balance
The 20-item Work-Life Balance (WLB) was used to measure health professionals’ WLB. Apaydın (2011) developed and validated the instrument in Turkish. This 20-item measure consists of four subscales: (a) work-life harmony (WLH; 6 items), (b) neglecting life (NL; 6 items), (c) making time for personal activities (MTPA; 4 items), and (d) over-commitment to work (OCW; 4 items).
The WLB measure uses a five-point response format with values ranging from 1 (strongly disagree) to 5 (strongly agree). The instrument includes items such as “I can balance my work and personal life” and “I keep working non-stop on weekends.” Higher scores reflect a high level of WLB. Apaydın (2011) reported a total of 0.91 Cronbach’s alpha coefficient for the total scores of reliability meaning a strong point of consistency. The reliability of subscale scores were 0.88 (work-life harmony), 0.81 (neglecting life), 0.77 (making time for personal activities), and 0.79 (over-commitment to work). For the current study, Cronbach’s alpha of total score was 0.91, and for the subscales were 0.83, 0.84, 0.66, and 0.74, respectively.
Work-life balance was represented as a latent variable in the study and estimated by the ordered factor indicators. Hence, a second-order factor analysis was conducted to confirm construct validity. The results indicated that the WLB had an acceptable fit: χ2 (162) = 442.77, p < 0.001; CFI = 0.90; TLI = 0.88; SRMR = 0.064; and RMSEA = 0.072 [90% CI = 0.064–0.080].
Data Analysis
We screened the data for entry errors and missing values before conducting the analysis. Descriptive statistics, structural equation model (SEM), and MANOVA were conducted to answer the research questions. Before proceeding with analyses, we evaluated model assumptions including independence, multivariate normality, linearity, and homogeneity of variance–covariance matrices. The assumption of normality was met based on the Shapiro–Wilk test (W > 0.01) and box plots. To assess the assumptions of linearity, standardized residual plots were inspected. Box’s M was inspected to assess the assumption of homogeneity of covariances and met (11.81, p = 0.49).
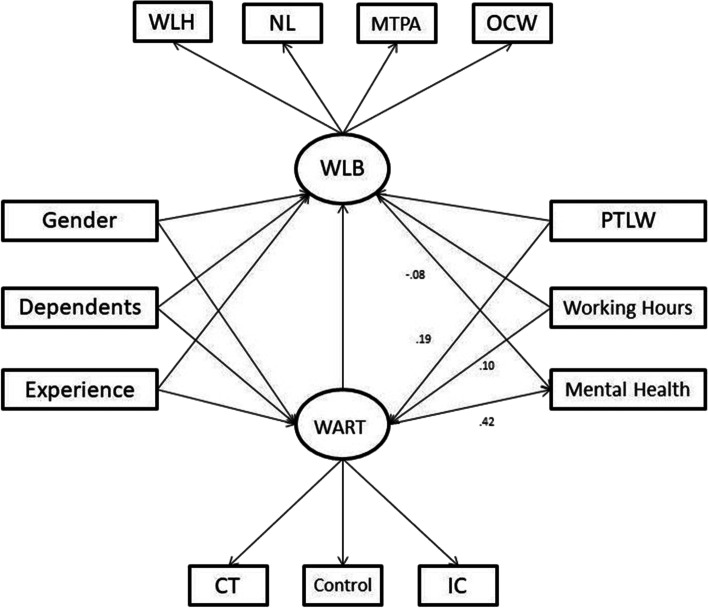
SEM procedures based on the existing literature and the analysis of covariance structures were used to identify and test the hypothesized model (Fig. 1) comprising the latent variables of work addiction and work-life balance, and observed variables of gender, dependents, experience, working hours, mental health need, and PTLW. The observed variables of “gender (0 = women, 1 = men),” “dependents (0 = none, 1 = children, other family members),” and “PTLW (0 = alone, 1 = parents, own family, friends)” were converted into the dummy variables with 0/1 coding. In addition, we treated these variables as continues independent variables.
Fig. 1.
Hypothesized structural model depicting the relations between gender; dependents; experience; WLB, work-life balance; WART, work addiction; PTLW, people they live with; working hours; and mental health need. WLH, work-life harmony; NL, neglecting life; MTPA, making time for personal activities; OCW, over-commitment to work; CT, compulsive tendencies; IC, impaired communication/self-absorption
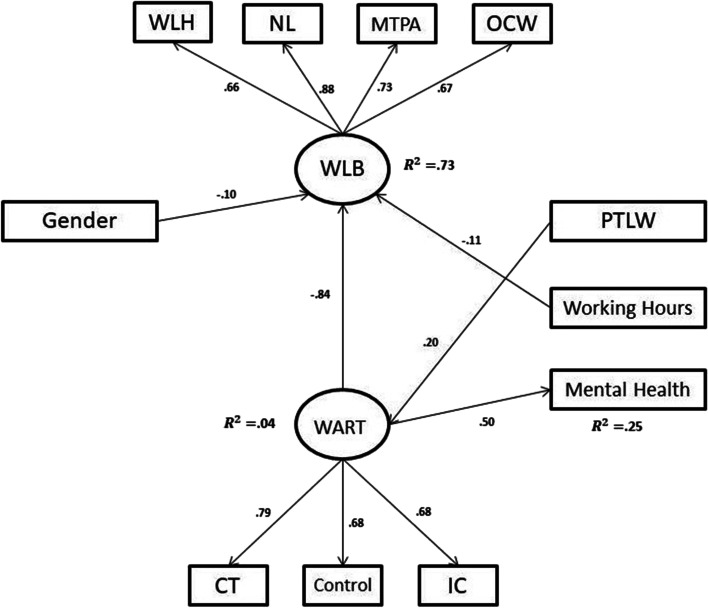
Analyses were conducted in SPSS 24.0 and AMOS 22.0. The model fit was evaluated using goodness-of-fit indices of chi-square (χ2), the ratio of chi-square to its degrees of freedom (χ2/df), the comparative fit index (CFI), the parsimonious normed comparative fit index (PCFI), the root mean square error of approximation (RMSEA), and the standardized root mean residual (SRMR). The WLB was an exogenous variable and had hypothesized effects from work addiction and other five observed variables. The work addiction was also an exogenous variable and had effects from other five observed variables. Finally, the mental health need variable was an endogenous variable and had direct effects from WLB and work addiction and indirect effects from other five observed variables. Based on the results of statistical analysis, variables which had insignificant paths were removed from the model. The new modified model was called selected structural model (Fig. 2).
Fig. 2.
Selected structural model depicting the relations between gender; WLB, work-life balance; WART, work addiction; PTLW, people they live with; working hours; and mental health need
Results
The descriptive statistics and correlations between variables were presented in Table 1. As expected, the highest and the most significant relationship was between work addiction and WLB (r = − 0.63, p < 0.01). The lowest relationship was between number of dependents and work addiction (r = − 0.63, p < 0.01). The hypothesized model was tested, and the fit indices indicated that the model was not acceptable: χ2(58) = 220.48, p < 0.001, χ2/df = 3.80; CFI = 0.87; PCFI = 0.64; RMSEA = 0.09 [90% CI = 0.078–0.104]; and SRMR = 0.060. First, we inspected regression weights for possible modifications. We found that the regression weights from experience, gender, working hours, and dependents to work addiction were not significant (p > 0.05). In addition the regression weights from PTLW and dependents to WLB and from WLB to mental health were not significant (p > 0.05). Hence, the insignificant paths were removed from the model, and we re-ran the analysis. The results indicated that the second model had a mediocre fit: χ2(51) = 162.96, p < 0.001, χ2/df = 3.19; CFI = 0.91; PCFI = 0.70; RMSEA = 0.08 [90% CI = 0.067–0.095]; and SRMR = 0.052. The model estimates were inspected for a third modification. We found that the regression weight from experience to WLB was not significant (p > 0.05). Therefore, the experience variable was removed from the model, and we re-ran the analysis. The fit indices of the final SEM were χ2(41) = 119.95, p < 0.001, χ2/df = 2.92; CFI = 0.93; PCFI = 0.70; RMSEA = 0.07 [90% CI = 0.060–0.090]; and SRMR = 0.045 indicating an acceptable model fit. All the regression weights were significant, so the third model was final and selected model (Fig. 2).
Table 1.
Means, standard deviations, reliability coefficients, and bivariate correlations for scores among variables
| Variable | Work Addiction | Work-life Balance |
|---|---|---|
| 1.Relationship | .01 | .05 |
| 2.Dependents | .13** | − .04 |
| 3.Experience | .05 | .03 |
| 4.Working hours | .10 | − .21* |
| 5.PTLW | .18* | − .14** |
| 6.Mental health need | .40* | − .04 |
| 7.Work addiction | - | − .63* |
| M | 2.36 | 3.33 |
| SD | .41 | .70 |
| α | .86 | .91 |
PTLW people they live with
*p < .01
**p < .05
Results of Direct Effects
Gender, working hours, work addiction, and PTLW had direct effects on mental health and WLB in the final model. Participants’ gender had a significant direct effect on WLB. The total of this direct effect was − 0.10. This means that male health professionals’ WLB was affected negatively from their gender. The second finding was the direct effect of working hours on WLB (. − 11). This finding showed that as the duration of the working hours increased, the work-life balance decreased. In the selected model, PTLW had a direct effect on work addiction (0.20). As the number of people living with the participants increased, their work addiction also increased. Finally, we found that work addiction had a direct effect on mental health (0.50). This result showed that as participants’ work addiction increased, their mental health needs increased as well. Based on R2, PTLW explained 4% of the total variance in work addiction, and PTLW and work addiction explained 25% of the total variance in mental health need.
Another variable affected WLB was work addiction. Compared to other variables, work addiction had the highest direct and total effect on WLB (. − 84). As the work addiction of the participants increased, there was a serious decrease in their work-life balance. Based on the squared multiple correlation value (R2), gender, work addiction, working hours, and PTLW explained 73% of the total variance in WLB of health professionals.
Results of Indirect Effects
Indirect effects represent mediation effects in SEM. Work addiction was a mediator between demographic variables and work-life balance and mental health needs. The demographic variable of PTLW had indirect effects on mental health and WLB in the final model. PTLW had indirect effect on WLB (β = − 0.17, p < 0.01) and mental health (β = 0.10, p < 0.01) through work addiction. In other words, when the number of people living with the participants increased, there was a decrease in their WLB and an increase in need help for mental health through work addiction.
Differences Based on the Professional Field
A one-way MANOVA was conducted to determine the differences among health professional’s working area (nurse, midwife, paramedic, technician and officials, and doctor) in terms of work addiction and work-life balance scores. Before we conducted the analysis, some of the groups were combined since they included few participants. We combined doctors, pharmacists, and dentists under the group of doctor; and we combined technicians and officials under the group of technician. The assumption of homogeneity of covariances (Box’s M = 11.81, p = 0.490) was met. The analysis indicated that there were not significant differences among health professionals based on the two dependent variables, Wilks’ λ = 0.973, F(8, 660) = 1.154, p = 0.32.
Discussion
Health professionals have always been at the frontline in the fight against the COVID-19 crisis and actively involved in providing care to COVID-19 patients while managing this crisis (Lai et al., 2019). Thus, there is an increasing necessity for personal and professional interventions that can strengthen the personal well-beings and resources of the health professionals aimed at protecting them from the negative psychological effects of COVID-19 in their work and life spaces (Kalaitzaki & Tamiolaki, 2020). The psychological empowerment of health professionals indirectly guarantees a physically and spiritually healthier workforce, leading to quality healthcare services (Republic of Turkey Ministry of Health, 2020). In this context, this study was carried out amid the COVID-19 pandemic to determine the work-life balance and work addiction levels of health professionals and to examine their needs for psychological help.
Our study found that gender was a variable that directly affected work-life balance. The work-life balance of male health professionals was poorer than women. In the literature, there were similar results to our research results, which indicated that women felt more job satisfaction than men with a better work-life balance (Asadullah & Fernández, 2008; Glasgow & Sang, 2016). The results of this study were similar to those in the literature. We believe that this finding may result from women’s problem-solving skills, empathy skills, and their ability to express their feelings comfortably. However, some studies in the literature (Bhui et al., 2016; Doble & Supriya, 2010) reported that women experience imbalances in working life, and emphasized the importance of ensuring a supportive working environment. In influenza pandemic, Aoyagi et al. (2015) stated that male workers and those who trust their personal skills had a higher willingness to work. In this context, we can assume that the provision of nursery services and appropriate break times provided for health professionals during the pandemic increased the work-life balance of women.
Working hours directly affected the work-life balance. As the working hours of health professionals increased, work-life balance decreased. Sahu and colleagues (2020) reported that in a study conducted with orthopedists, approximately 60% of health professionals stated that their work-life balance was upside down in the COVID-19 pandemic. The lack of balance between the two living spaces triggers stress, creates a conflict between work and family, and affects work and family life quality and individual well-being negatively (Carıkcı & Celikkol, 2009; Efeoglu & Ozgen, 2007). In addition to strenuous working hours, health professionals were faced with solving daily critical problems such as shortcomings in the medical institution, insufficient personal protection measures, fear of getting infected, and risk of spreading the virus (Lai et al., 2019). It was, therefore, believed that the busy working hours and the inability to provide the mental well-being and physical equipment required by the health professionals during such hours negatively affected the work-life balance of health professionals. It was believed that this increase in health professionals’ working hours during the pandemic negatively affected their family life, their roles, and responsibilities in the family.
The people with whom the health professionals live together directly affected the work addiction in our study. Health professionals who were in close contact with COVID-19 and Ebola virus patients were vulnerable to infection and faced the risk of spreading the virus both among their colleagues and family members (Lehmann et al., 2015; Lu et al., 2020). In other words, the fact that health professionals live with others increased work addiction. This study found that work addiction directly affected the need for health professionals to seek psychological help. As work addiction increased, the need for health professionals to seek psychological help increased. Some studies with health professionals concluded that married people experience more psychological distress, while those with children experience more work stress (Chew et al., 2020; Mo et al., 2020). In addition, in a study conducted amid influenza pandemic, having children was found to reduce the willingness to work (Aoyagi et al., 2015). It was considered to be related to the fear of carrying/transmitting the virus, as well as to the fact that the married people cannot spend time with the people they live with due to difficult working conditions. According to another result in our study, the variable of the person with whom the health professionals live also accounts for 4% of the work addiction. In other words, 4% of health professionals present higher work addiction as they live with someone else. In fact, what was expected was that health professionals living with someone should feel more comfortable because their social support resources would be high and their need for psychological help would be low. However, it was thought that health professionals became more committed to their jobs because they were afraid of spreading COVID-19 to the family members they live with, and their need for seeking psychological help increased due to difficult working conditions.
Work addiction is basically a concept related to the positive attitude of individuals towards work and the action of working. Individuals with this attitude feel energetic and happy while working and are proud of their work (Ateşoğlu, 2018). In the hypothesized model, work-life balance and work addiction did not seem to be affected by the experience level of the health professionals and the presence of family members they have to take care of (dependents). Similarly, Baki and Piyal (2020) found that health professionals could accept the increased risk of infection due to their work; however, health professionals were concerned about transmission in family. In addition, health professionals stated that COVID-19 increased burnout levels as well as negative effects on family life (Yüncü & Yılan, 2020).
In addition, gender, working hours, and the people that they live together did not seem to affect the work-life balance in the model. Work-life balance did not affect the need for psychological help either. However, health professionals experience many problems due to stressful work life, difficulties in providing patients with healthcare, and setbacks in the health system (Gillespie et al., 2007; McCann et al., 2013). Work environments of health institutions cannot be considered among the institutions where the quality of work life is at the desired level, and it is more difficult to provide quality conditions in such institutions compared to other lines of work (Blazer et al., 2008). In light of this information, the hypothesized model was re-analyzed, and some statistical significance was found.
The factors of work addiction and the person they live with also account for 25% of the health professionals’ need for psychological help. Psychological problems such as anxiety, stress, depression, posttraumatic stress disorder, and reduced social functionality were known to increase during the pandemic (Chew et al., 2020; Qiu et al., 2020; Wang et al., 2020b). Anxiety especially became an important problem in healthcare professionals (Huang et al., 2020). Some reports have emphasized the seriousness of the psychological problems of health professionals, focusing on the urgency of providing psychological care (Kang et al., 2018; Xiang et al., 2020). Babore et al. (2020) found that social support was a significant protective factor of stress for healthcare professionals during the COVID-19 pandemic. It is also increasingly recognized that a number of personal assets and resources (e.g., communication, social support, coping strategies) are positively associated with psychological resilience or posttraumatic growth (Palacio et al., 2019). Recognizing and strengthening psychological needs should be a priority for health professionals (Kalaitzaki & Tamiolaki, 2020). According to another result of this study, work addiction had a direct effect on work-life balance at a high rate of 84%. As the work addiction of health professionals increased, the work-life balance decreased. We believe that this relationship may be related to the lack of a definitive method to prevent contamination on returning home and being unable to find time to communicate with their family members in different ways (such as online, face-to-face communication, telephone conversations) due to heavy working conditions. Given the indirect effects of the model, the people they live with affected the need for seeking psychological help and work-life balance. Health professionals living together with someone had a reduced work-life balance. Here, the mediating variable was determined as work addiction. Health professionals living with someone trigger work addiction, leading to disrupted work-life balance. Likewise, living with someone increases the need of the health professional to seek psychological help. Our research results were in conformity with the results of the study by Niuniu et al. (2020) and Lee et al. (2005) stating nurses who had elderly individuals in their families or had children presented high concerns about their family members.
This study included 5 different groups of health professionals as doctors (MD, dentists and pharmacists), nurses, midwives, paramedics, and technicians (technicians and hospital clerks). No statistically significant difference was found among health professional groups in terms of work addiction and work-life balance, being an indication that health professionals’ life balances and work commitments did not differ during the pandemic. In other words, healthcare professionals were affected similarly by this process. The identification of COVID-19 in the saliva of infected patients revealed that dentists are also at risk (Soysal et al., 2020). Pharmacists continued to serve in the pandemic process as the health professionals that are most easily accessible to the public (Visacri et al., 2021). However, it was known that the people with the highest risk of getting infected by the COVID-19 are those who are in contact with patients or those who care for them (Ministry of Health, 2017). It was stated that nurses, who are primarily responsible of patient care, continue to work with positive emotions gradually although they felt intense negative emotions in the early stage of the pandemic (Niuniu et al., 2020). Another study concluded that doctors and nurses, full-time employees, those with high perceived personal security level, those with high knowledge of pandemic risk and clinical knowledge, those with professional role-specific knowledge, and those who received influenza pandemic intervention training were found more willing to work (Aoyagi et al., 2015). In another study on arthroplasty surgeons, who are also a group of health professionals, the professionals were said to have been negatively affected by the COVID-19 pandemic in regard to career development (Culp & Frisch, 2020).
In our study, we concluded that work-life balance can be explained by variables such as gender, work addiction, working hours, and the people with whom health professionals live during the pandemic. There were different results in the literature regarding work-life balance and gender factor. Hämmig and Bauer (2009) stated in their research that work-life balance affected mental health for both genders, in addition to suggesting that three out of five men had difficulty in maintaining work-life balance (Meenakshi et al., 2013). In addition, the presence of opportunities with which women can maintain their family order along with career support may have been effective in maintaining their work-life balance in business today (Fujimoto et al., 2013). In our study, we assume that there may be some mental concerns among the reasons of over-addiction and low work-life balance of individuals living with others. The fear of harming their loved ones may be among the first of these spiritual concerns. Such fear leads to the worst possible work environment for health professionals. In the literature, Trumello et al. (2020) reported that stress, burnout, secondary trauma, anxiety, and depression scores were higher among health professionals who worked with COVID-19 patients in areas with higher rates of contagion in Italy.
In our study, working time, which is another factor that explains the work-life balance, stands out as an important issue. There were a large number of scientific studies in the literature supporting the increased risk of developing depression, burnout syndrome, and myocardial infarction when health professionals are exposed to such working hours (Aronsson et al., 2017; Theorell et al., 2015). Health professionals work overtime, and their work schedules and year leave schemes often change. It was, therefore, believed that adjusting the working conditions and working hours may provide a solution for the maintenance and protection of both the physical and psychological well-being of health professionals. For all these reasons, we think that our study will make an important contribution to the literature in the pandemic as it is the first study to examine the work-life balance and extent of work addiction of health professionals in terms of many variables in addition to trying to create a model.
Implications and Limitations
As in Turkey, the selfless efforts of health professionals have been effective in the fight against the COVID-19 pandemic all over the world. Considering that the current study was carried out in the first wave of the pandemic, it is understood that there may be many factors that affect the mental health needs of health workers and their work-life balance. Based on the results of the present study, there are implications for hospital administrations, policymakers and mental health professionals.
When the results are carefully examined, sharing a home with family or friends was a positive factor for their mental health; however, it was a negative factor for health professionals’ work-life balance. It is understood that reasonable working hours are needed for health professionals to spend enough time with their families and loved ones. On the other hand, they need social relationships that can strengthen their mental health and communicate in non-risky environments. At this point, open group therapies for health workers can be organized in hospitals where they can participate voluntarily. Nearly 20,000 health professionals were employed in Turkey through additional appointments during the pandemic period. However, this number is not enough considering the current shortage of healthcare professionals. The number of jobs should be increased in order to have experienced staff and health professionals who have established work-life balance in the future considering that there may be future health disasters. As a matter of fact, health professionals were given emergency visas and work permits by some countries for employment. Finally, mental health professionals can diversify ways to provide services to healthcare professionals by turning to online services and increasing the number of materials available for remote and self-services. The efforts carried out at this point are promising but not sufficient.
As in previous studies, the current study had its own limitations. First, this study had a cross-sectional design meaning the study was conducted on a specific time. Thus, demographic variables such as working hours, the people that health professionals live together, and dependents may affect work-life balance and work addiction differently in some other time. Another limitation was related to the low reliability scores of the self-worth and impaired communication/self-absorption subscales of work addiction and making time for personal activity subscale of work-life balance measures. We had to exclude the two-item self-worth subscale from the analysis. As a result, the psychometric characteristics of work addiction measure differed from its original form. However, the three-factor model was acceptable based on the CFA results. The last limitation was the unbalanced numbers of genders. The majority of participants were women (84%) in the study. This may have caused the study results to be more influenced by women’s views and to reflect women’s life balance more. Studies where the gender distribution is equal or close are needed in the future.
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Althobaiti, S., Alharthi, S., & AlZahrani, A. M. (2020). Medical systems’ quality evaluated by perceptions of nursing care: Facing COVID-19 pandemic. International Journal for Quality Research, 14(3), 895–912. 10.24874/IJQR14.03-16.
- Aoyagi Y, Beck CR, Dingwall R, Nguyen-Van-Tam JS. Healthcare workers’ willingness to work during an influenza pandemic: A systematic review and meta-analysis. Influenza and Other Respiratory Viruses. 2015;9(3):120–130. doi: 10.1111/irv.12310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apaydın, Ç. (2011). Relationship between workaholism levels of faculty members and work-life balance and work-famıly lıfe balance. (Unpublished Doctoral Dissertation), Ankara University, Educational Administration and Policy Department, Ankara.
- Araslar, A. (2021). The effect of workload and work-life balance on the intention to leave. (Unpublishing Master Thesis). Bursa Uludag University, Social Sciences Institute, Bursa.
- Aronsson, G., Theorell, T., Grape, T., Hammarström, A., Hogstedt, C., Marteinsdottir I., …, & Hall, C. (2017). A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health, 17(264), 1-1310.1186/s12889-017-4153-7 [DOI] [PMC free article] [PubMed]
- Asadullah, N. M. & Fernández, R. M. (2008). Work-life balance practices and the gender gap in job satisfaction in the UK: Evidence from matched employer-employee data. IZA Discussion Paper, 3582. Bonn, Germany: Institute for the Study of Labor (IZA).
- Ateşoğlu, L. (2018). The work commitment of public and private sector employees according to some demographic variables. III. International Al- Farabi Social Sciences Congress (104–111), Ankara.
- Aziz S, Cunningham J. Workaholism, work stress, work-life imbalance: Exploring gender’s role. Gender in Management: An International Journal. 2008;23:553–566. doi: 10.1108/17542410810912681. [DOI] [Google Scholar]
- Babore, A., Lombardi, L., Viceconti, M. L., Pignataro, S., Marino, V., Crudele, M., …, & Trumello, C. (2020). Psychological effects of the COVID-2019 pandemic: Perceived stress and coping strategies among healthcare professionals. Psychiatry Research, 293, 1–6.10.1016/j.psychres.2020.113366 [DOI] [PMC free article] [PubMed]
- Baki S, Piyal B. Work-family conflict as regard to healthcare workers in extraordinary situations such as COVID-19 pandemic. Health and Public; 2020. pp. 119–123. [Google Scholar]
- Balkin RS, Reiner SM, Hendricks L, Washington A, McNeary S, Juhnke GA, Hunter Q. Life balance and work addiction among African Americans. The Career Development Quarterly. 2018;66(1):77–84. doi: 10.1002/cdq.12123. [DOI] [Google Scholar]
- Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet. 2020;395(10224):37–38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhui K, Dinos S, Galant-Miecznikowska M, de Jongh B, Stansfeld S. Perceptions of work stress causes and effective interventions in employees working in public, private and non-governmental organisations: A qualitative study. Bjpsych Bulletin. 2016;40(6):318–325. doi: 10.1192/pb.bp.115.050823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazer FN, Konca GE, Ugur S, Ucak H, Erdemir F, Cıtak E. Working conditions of nurses in Turkey. Turkish Nurses Association Publications; 2008. [Google Scholar]
- Brooks, S., Webster, R., Smith, L., Woodland, L., Wessely, S., …, & Gideon, N. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395, 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed]
- Carıkcı İ, Celikkol O. The effects of work – family conflict on organizational commitment and intention to leave. Journal of Süleyman Demirel University Institute of Social Sciences. 2009;9(9):153–170. [Google Scholar]
- Cetintepe, P. A & Ilhan, N. M. (2020). Risk reduction in healthcare workers in the COVID-19 outbreak. Journal of Biotechnology and Strategic Health Research, 1, 20–54. 10.34084/bshr.712539.
- Chen, Q., Liang, M., Li, Y., Guo, J., Fei, D., Wang, L., …, & Zhang, Z. (2020). Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry, 7, e15-e16. 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed]
- Chew, N., Lee, G., Tan, B., Jing, M., Goh, Y., Ngiam, N., …, & Sharma, V. K. (2020). A multinational, multicenter study on the psychological outcome sand associated physical symptoms amongst health care workers during COVID-19 outbreak. Brain, Behavior, and Immunity, 21, 1–7. 0889–1591(20)30523–7. [DOI] [PMC free article] [PubMed]
- Cullen, W., Gulati, G,. & Kelly, B. D. (2020). Mental health in the Covid-19 pandemic. QJM: An International Journal of Medicine, 113(5), 311–312. 10.1093/qjmed/hcaa110. [DOI] [PMC free article] [PubMed]
- Culp MB, Frisch BN. COVID-19 Impact on young arthroplasty surgeons. The Journal of Arthroplasty. 2020;35(7):42–44. doi: 10.1016/j.arth.2020.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai, Y., Hu, G., Xiong, H., Qiu, H., & Yuan, X. (2020). Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. medRxiv, 2, 624–646. 10.1101/2020.03.03.20030874.
- Doble N, Supriya MV. Gender differences in the perception of work-life balance. Management. 2010;5(4):331–342. [Google Scholar]
- Efeoglu İE, Ozgen H. Effects of work-family life conflict on job stress, job satisfaction and organizational commitment: A research in the pharmaceutical sector. CU Journal of Social Sciences Institute. 2007;16(2):237–254. [Google Scholar]
- Enli-Tuncay F, Koyuncu E, Ozel S. A review of protective and risk factors affecting psychosocial health of healthcare workers in pandemics. Ankara Med J. 2020;20(2):488–501. doi: 10.5505/amj.2020.02418. [DOI] [Google Scholar]
- Fagan, C., Lyonette, C., Smith, M., & Saldaña-Tejeda, A. (2012). The influence of working time arrangements on work-life integration or ‘balance’: A review of the international evidence. ILO Working Paper (Pub. No. 994705033402676). https://ideas.repec.org/p/ilo/ilowps/994705033402676.html
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods. 2009;41:1149–1160. doi: 10.3758/brm.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Fujimoto Y, Azmat F, Hartel C. Gender perceptions of work-life balance: Management implications for full-time employees in Australia. Australian Journal of Management. 2013;38(1):147–170. doi: 10.1177/0312896212449828. [DOI] [Google Scholar]
- Gillespie BM, Chaboyer W, Wallis M, Grimbeek P. Resilience in the operating room: Developing and testing of a resilience model. Journal of Advanced Nursing. 2007;59:427–438. doi: 10.1111/j.1365-2648.2007.04340.x. [DOI] [PubMed] [Google Scholar]
- Glasgow S, Sang K. Gender and work-life balance. In: Arshed N, McFarlane J, Macintosh R, editors. Enterprise and its business environment. Good fellow Publishers; 2016. pp. 135–150. [Google Scholar]
- Hämmig O, Bauer GF. Work-life imbalance and mental health among male and female employees in Switzerland. International Journal of Public Health. 2009;54:88–95. doi: 10.1007/s00038-009-8031-7. [DOI] [PubMed] [Google Scholar]
- Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Annals of the Academy of Medicine, Singapore. 2020;49(3):155–160. doi: 10.47102/annals-acadmedsg.202043. [DOI] [PubMed] [Google Scholar]
- Holly, S. & Mohnen, A. (2012). Impact of working hours on work-life balance (Report No. 465). Deutsches Institut für Wirtschaftsforschung (DIW). https://www.econstor.eu/bitstream/10419/62340/1/722921012.pdf
- Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., …, & Cao, B. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet, 395, 497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed]
- Humphries, N., McDermott, A. M., Creese, J., Matthews, A., Conway, E., & Byrne, J. P. (2020). Hospital doctors in Ireland and the struggle for work–life balance. European Journal of Public Health, 30(Supplement_4), iv32-iv35. 10.1093/eurpub/ckaa130 [DOI] [PMC free article] [PubMed]
- Jones F, Kinman G, Payne N. Work stress and health behaviors: A work-life balance issue. In: Jones F, Burke R, Westman M, editors. Work-life balance: A psychological perspective. Taylor and Francis; 2006. pp. 185–215. [Google Scholar]
- Kabar, M. (2017). The relationship between high school teachers' job commitment levels and emotional intelligence levels. (Unpublished Master’s Thesis), Istanbul Sabahattin Zaim University, Institute of Health Sciences, Istanbul.
- Kalaitzaki AE, Tamiolaki A. The healthcare professionals amidst COVID-19 pandemic: A perspective of resilience and posttraumatic growth. Asian Journal of Psychiatry. 2020;52:102172. doi: 10.1016/j.ajp.2020.102172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang HS, Son YD, Chae SM, Corte C. Working experiences of nurses during the Middle East respiratory syndrome outbreak. International Journal of Nursing. 2018;24(e12664):1–8. doi: 10.1111/ijn.12664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakisci-Kavas B, Develi A. Çalışma yaşamındaki sorunlar bağlamında COVID-19 pandemisinin kadin sağlık çalışanları üzerindeki etkisi. International Anatolian Journal of Social Sciences. 2020;4(2):84–112. [Google Scholar]
- Korkmaz O, Erdogan E. The effect of work-life balance on employee satisfaction and organizational commitment. Ege Academic Review. 2014;14(4):541–557. [Google Scholar]
- Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., …, & Hu, S. (2019). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease. JAMA Network Open, 20(3), 1-1210.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed]
- Lee SH, Juang YY, Su YJ, Lee H, Lin Y, Chao C. Facing SARS: Psychological impacts on SARS team nurses and psychiatric services in a Taiwan general hospital. General Hospital Psychiatry. 2005;27:352–358. doi: 10.1016/j.genhosppsych.2005.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann M, Bruenahl CA, Löwe B, Addo MM, Schmiedel S, Lohse AW, Schramm C. Ebola and psychological stress of health care professionals. Emerging Infectious Diseases. 2015;2:913–914. doi: 10.3201/eid2105.141988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H, Stratton CW, Tang Y. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. Journal of Medication Virol. 2020;92(4):401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockwood, R. N. (2003). Work/life balance challenges and solutions. SHRM Research Quarterly. Retrieved from https://deepcbds.com/wp- ontent/uploads/2020/02/Work_Life_Balance_Challenges_and_Solutio.pdf
- Malik S, Ullah I, Irfan M, Kwasi-Ahorsu D, Lin C, Pakpour AH, Griffiths MD, Rehman I, Minhas R. Fear of COVID-19 and workplace phobia among Pakistani doctors: A survey study. BMC Public Health. 2021;21(833):1–9. doi: 10.1186/s12889-021-10873-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mccann CM, Beddoe E, Mccormick K, Huggard P, Kedge S, Adamson C, Huggard J. Resilience in the health professions: A review of recent literature. International Journal of Wellbeing. 2013;3:60–81. doi: 10.5502/ijw.v3i1.4. [DOI] [Google Scholar]
- Meenakshi P, Subrahmanyam V, Ravichandran K. The importance of work-life-balance. Journal of Business and Management. 2013;14(3):31–35. doi: 10.9790/487X-1433135. [DOI] [Google Scholar]
- Ministry of Health. (2017). Annual Health, Labour and Welfare Report. http://www.gender.go.jp/english_contents/pr_act/pub/pamphlet/women-and-men13/pdf/2-6.pdf
- Mo, Y., Deng, L., Zhang, L., Lang, Q., Liao, C., Wang, N., …, & Huang, H. (2020). Work stress among Chinese nurses to support Wuhan for fighting against the COVID-19 epidemic. Journal of Nursing Management, 00, 1–8. 10.1111/JONM.13014 [DOI] [PMC free article] [PubMed]
- Niuniu, S., Luoqun, W., Suling, S., Dandan, J., Runluo, S., Lili, M., … & Hongyun, W. (2020). A qualitative study on the psychological experience of caregivers of COVID-19 patients. American Journal of Infection Control, 48, 592−598. 10.1016/j.ajic.2020.03.018 [DOI] [PMC free article] [PubMed]
- Palacio GC, Krikorian A, Gómez-Romero MJ, Limonero JT. Resilience in caregivers: A systematic review. American Journal of Hospice & Palliative Medicine. 2019;37(8):648–658. doi: 10.1177/1049909119893977. [DOI] [PubMed] [Google Scholar]
- Prakash S, Pabalkar V. Occupational stress among Indian doctors during COVID-19. European Journal of Molecular & Clinical Medicine. 2020;7(9):1862–1880. [Google Scholar]
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implication sand policy recommendations. General Psychiatry. 2020;33(2):1–3. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Republic of Turkey Ministry of Health. (2020). Evaluation of healthcare professionals with COVID-19 theme. http://www.tkdcd.org/public/uploads/files/COVID19_TemasiOlanSaglikCalisanlarininDegerlendirilmesi_25032020.pdf
- Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA, Pastor-Moreno G, Castro A, Ruiz-Pérez I, Zamanillo Campos R, Gonçalves-Bradley DC. Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. Journal of Affective Disorders. 2020;277:347–357. doi: 10.1016/j.jad.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson RE. The Work Addiction Risk Test: Development of a tentative measure of workaholism. Perceptual and Motor Skills. 1999;88:199–210. doi: 10.2466/pms.1999.88.1.199. [DOI] [PubMed] [Google Scholar]
- Sahu D, Agrawal T, Rathod V, Bagaria V. Impact of COVID 19 lockdown on orthopedic surgeons in India: A survey. Journal of Clinical Orthopedics and Trauma. 2020;11:283–290. doi: 10.1016/j.jcot.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J, King CC, Yen MY. Protecting health care workers during the COVID-19 coronavirus outbreak -Lessons from Taiwan’s SARS response. Clinical Infectious Diseases. 2020;71(15):858–860. doi: 10.1093/cid/ciaa255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, A.L. (2011). Gender and workaholism: A study of New Zealand academics. (Unpublished Master Thesis), Victoria University, Master of Commerce and Administration, Wellington.
- Soysal F, Isler SC, Peker I, Akca G, Ozmeric N, Unsal B. The impact of COVID-19 pandemic on dentistry practices. Journal of Klinik. 2020;33(1):5–14. doi: 10.5152/kd.2020.22. [DOI] [Google Scholar]
- Tang L, Pan L, Yuan L, Zha L. Prevalence and related factors of post-traumatic stress disorder among medical staff members exposed to H7N9 patients. International Journal of Nursing Sciences. 2016;4(1):63–67. doi: 10.1016/j.ijnss.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theorell, T., Hammarström, A., Aronsson, G., Träskman, L. B., Grape, T., Hogstedt, C., …, & Hall, C. (2015). A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health, 15(1), 1–14. 10.1186/s12889-015-1954-4 [DOI] [PMC free article] [PubMed]
- Trumello, C., Bramanti, S. M., Ballarotto, G., Candelori, C., Cerniglia, L., Cimino, S., …, & Babore, A. (2020). Psychological adjustment of healthcare workers in Italy during the covid-19 pandemic: Differences in stress, anxiety, depression, burnout, secondary trauma, and compassion satisfaction between frontline and non-frontline professionals. International Journal of Environmental Research and Public Health, 17(22), 8358. 10.3390/ijerph17228358 [DOI] [PMC free article] [PubMed]
- Visacri MB, Figueiredo IV, Lima TM. Role of pharmacist during the COVID-19 pandemic: A scoping review. Research in Social & Administrative Pharmacy: RSAP. 2021;17(1):1799–1806. doi: 10.1016/j.sapharm.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., …, & Ho, C. (2020a). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity, 87, 40-48. 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the ınitial stage of the 2019 coronavirus disease (COVID-19) International Journal of Environmental Research and Public Health. 2020;17(5):1–25. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, P., Fang, Y, Guan, Z., Fan, B., Kong, J., Yao, Z., …, & Hoven, C. W. (2013). The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry, 54, 302–311. 10.1177/070674370905400504 [DOI] [PMC free article] [PubMed]
- Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, Chee H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yüncü V, Yılan Y. Investigating the impacts of COVID-19 pandemic on healthcare staff: A case study. Igdir University Journal of Social Sciences. 2020;2:373–401. [Google Scholar]