Abstract
Cellular senescence represents a distinct cell fate characterized by replicative arrest in response to a host of extrinsic and intrinsic stresses. Senescence provides programming during development and wound healing, while limiting tumorigenesis. However, pathologic accumulation of senescent cells is implicated in a range of diseases and age-associated morbidities across organ systems. Senescent cells produce distinct paracrine and endocrine signals, causing local tissue dysfunction and exerting deleterious systemic effects. Senescent cell removal by apoptosis-inducing “senolytic” agents or therapies that inhibit the senescence-associated secretory phenotype, SASP inhibitors, have demonstrated benefit in both pre-clinical and clinical models of geriatric decline and chronic diseases, suggesting senescent cells represent a pharmacologic target for alleviating effects of fundamental aging processes. However, senescent cell populations are heterogeneous in form, function, tissue distribution, and even differ among species, possibly explaining issues of bench-to-bedside translation in current clinical trials. Here, we review features of senescent cells and strategies for targeting them, including immunologic approaches, as well as key intracellular signaling pathways. Additionally, we survey current senolytic therapies in human trials. Collectively, there is demand for research to develop targeted senotherapeutics that address the needs of the aging and chronically-ill.
Introduction
Chronological age is the preeminent risk factor for the leading causes of morbidity and mortality worldwide1,2. Chronological and biological aging are often correlated3, however, the latter can be accelerated by the co-existence of multiple chronic diseases and geriatric syndromes, which in turn account for inter-individual heterogeneity in terms of risk for development of new diseases, disability, or death4. With these considerations in mind, there is now a growing effort to understand and modulate the root causes of aging to alleviate multimorbidity at a global scale. Cellular senescence has garnered increasing attention as a fundamental driver of chronic conditions and functional decline in late life. Despite its historic discovery in the context of in vitro cell growth arrest following serial passage5, the ramifications of cellular senescence have only recently been appreciated following its implication in a host of age-related and chronic diseases spanning most organ systems. In tandem with our expanding appreciation of senescence in pathology, there is an equally evolving understanding of the role of cellular senescence in basic physiology. This inherent duality in the senescence program alongside our limited understanding has increased research fervor and incited controversies ranging from appropriate laboratory methods for studying senescent cells to their potential role as therapeutic targets.
Here, we survey the current field of cellular senescence research with regards to its inherent heterogeneity in order to address the diverse roles of this cell fate with respect to both physiology and pathology. We first explore the molecular underpinnings of senescence to emphasize how senescent cells are currently defined in light of their underlying diversity. We then explore how this heterogeneity is further compounded by the senescent cell secretome. Finally, we consider the therapeutic implications and approaches for targeting various types of senescent cells as well as the current clinical trials of senolytic drugs.
Cellular Senescence
Despite the controversies surrounding the role of cellular senescence in both health and disease, there is a degree of consensus involving its basic definitions and principles. At its core, cellular senescence represents a cell fate that is characterized by stable proliferative arrest in response to various stressors and, frequently, production of an accompanying secretome termed the “senescence associated secretory phenotype” (SASP). Inducing stressors vary and include replicative stress with associated telomere shortening, activation of DNA damage pathways, epigenetic changes, oxidative stress, mitochondrial dysfunction, radiation, oncogene induction, and mechanical and shear stress, amongst others that have been thoroughly reviewed6. Following stress exposure, cell-cycle checkpoint blockading factors are upregulated that halt replicative progression. Although these cells accumulate damage products, including DNA breaks, and upregulate DNA damage response pathways7,8 in part due to mitochondrial dysfunction and increased reactive oxygen species production9, they do not undergo apoptosis. Instead, they have upregulated pro-survival pathways called senescent cell anti-apoptotic pathways (SCAPs) while key apoptotic mediators are downregulated10-13. In addition to their internal homeostatic perturbations, senescent cells can induce an inflammatory state that provokes both local and systemic inflammation and tissue damage through their SASP14-16.
This cascade of stress, senescence, and subsequent SASP signaling and immune activation is critical for normal development and health. From early development, cells with senescent features are important for body axis patterning, with the associated SASP directing growth of structures such as the limb bud and orchestrating regression of transient features through macrophage-mediated clearance17-19. Furthermore, as senescent cells produce factors that promote tissue remodeling and recruit associated immune components, spatiotemporally regulated senescence is important for mediating the balance between healing and fibrosis in regenerative processes including wound and organ repair20-25. Interestingly, senescent cells can also promote de-differentiation and plasticity of neighboring cells via paracrine mechanisms26,27. Additionally, due to its induction in response to both DNA damage and oncogenic stress, the senescence program may also serve as a tumor suppression mechanism, though its inflammatory properties and DNA damage induction are also associated with increased tumor burden when dysregulated28-30
While there is substantial interest in the beneficial roles of senescent cells, much of cellular senescence research has been aimed at their roles in disease and emphasized their contributions to geriatric decline. This modern wave of attention was promoted by the discoveries that markers of cellular senescence accumulate with aging and accumulation is delayed by interventions that increase healthspan and lifespan31, removal of senescent cells increases healthspan in progeroid mouse models32, and transplantation of a relatively small number of senescent cells into previously healthy animals provokes multisystem dysfunction similar to aged animals33,34. Furthermore, it was found that the correlation of senescent cell accumulation with disease extends to humans35-37, and that senescent cell burden can be safely reduced in a clinical context38. Based on these points, it appears crucial to understand the roles of senescence in morbidity and mortality. To date, deleterious effects of senescent cells have been implicated in a causative or proximal capacity for diseases encompassing most organ systems, including the leading causes of morbidity, death, and healthcare burden such as cardiovascular, pulmonary, neurologic, renal, hepatic, infectious, musculoskeletal, and endocrine diseases29,39-51.
Molecular Basis and Markers of Cellular Senescence
Senescence is a cell fate that is widely regarded as a stress response. Senescence is distinct from other non-proliferative cell fates including quiescence, the latter being reversible with appropriate mitogens, or terminal differentiation, in which cells develop from defined lineages to fulfill specific roles and arrest growth through diverse pathways. In response to internal or external factors such as telomere shortening or ionizing radiation, senescent cell cycle arrest signals primarily converge on the p53/cdkn1a(p21) and/or Retinoblastoma(RB)/cdkn2a(p16) pathways52. Increased levels of the cyclin dependent kinase inhibitors (CDKIs) p21 and p16 can both contribute to G1/S cell cycle blockade, mediated by inhibition of cyclin/cyclin-dependent kinase complex formation and failure to inactivate RB with associated transcriptional repression53. Despite the convergence of senescent growth arrest pathways, there is growing appreciation that different inducing stressors can result in unique senescent subpopulations54. This complexity is further compounded by the fact that currently no single known marker defines senescence with high sensitivity and specificity, though this lack of a gold-standard is not unique to the field. Current practices rely on a combination of phenotypes and sets of markers to suggest cellular senescence. For example, although accumulation of p16 and p21 have been biologically implicated in senescence and are extensively used as molecular markers, various in vitro stressors induce differential expression of these CDKI’s, even within the same cell line55, indicating that neither is fully sufficient or reliable on its own. To complicate this further, the same study also revealed that different cell types can differentially alter their transcriptome in response to the same inducing stressor. Unlike the well-controlled constraints of cell culture models, different stressors can act simultaneously in vivo with both aging and disease. Thus, it is hypothesized that senescent populations are especially diverse in vivo.
Besides p16 and p21, a number of other markers can be used to identify senescent cells, though sensitivity and specificity varies for each (Table 1). Several morphologic features are suggestive of senescence in vitro and can be assessed using approaches such as brightfield microscopy. Compared to their counterparts, senescent cells have increased size and granularity56,57, likely reflecting their altered metabolism and organelle homeostasis. In particular, both mitochondria and lysosomes accumulate in cells exposed to senescence-inducing stressors9,58. Whether causative of, or occurring in response to the stress response, or both, these changes provide an added means for detecting senescent cells. Lysosomal abundance in senescent cells is one of the most commonly used features, as lysosomal senescence-associated beta-galactosidase (SA beta-Gal) activity assays are relatively quick and straightforward to conduct59. However, there are limitations to the specificity of this marker60 and it should be paired with others considered here. Lipofuscins, which are aggregates of lysosomal byproducts, also accumulate within senescent cells and can conveniently be assayed, though such assays have similar limitations to specificity to those of SA beta-Gal assays61. Mitochondrial abundance increases in senescent cells together with altered membrane potential and increased reactive oxygen species (ROS) production, oxidative phosphorylation, and oxygen consumption62. Hence, assays of redox state, mitochondrial function, and mitochondrial biogenesis can be used to enhance senescent cell phenotyping.
Table 1.
Select Features of Senescent Cells
| Morphologic Features | Increased Size [56] |
| Increased Granularity [56, 57] | |
| Cell Cycle Blockade | p21/p53 [52] |
| p16/RB [52] | |
| Mitochondrial Changes | Increased Size/Number [9] |
| Increased ROS [62] | |
| Decreased Membrane Integrity [62] | |
| Lysosomal Changes | Increased Size/Number [58] |
| Increased SA-beta-Gal Activity [59] | |
| Lipofuscin Accumulation [61] | |
| Nuclear Changes | Telomere Shortening [6,52, 63] |
| DNA Damage Response (DDR) (TAF, gamma-H2AX) [8,63] | |
| Lamin B1 loss [65] | |
| Senescence Associated Heterochromatin Foci (SAHF) [66] | |
| Decreased DNA Replication [6] | |
| Additional Selected Features | Cytosolic DNA/cGAS-STING Activation [79, 80, 81] |
| LINE-1 Retrotransposon De-repression [67] | |
| Remodeling of SASP associated super-enhancers [84] | |
| Other Senescence Transcriptional Changes [55, 69, 70] |
Nuclear alterations are prominent features of senescent cells and largely result from activation of the DNA damage response (DDR) pathways that lead to p16 and p21 activation. These pathways also lead to increased phosphorylation and activation of the DDR orchestrator histone, H2AX, which coordinates DNA repair following genotoxic stress and double strand breaks63. This has led to the use of immunohistochemical techniques to label phosphorylated (gamma) H2AX in senescence assays. As this pathway can repair DNA double strand breaks across most of the chromosome, it potentially lacks sensitivity due to its transient nature at most loci. However, double strand breaks are persistent at telomeric loci due to localized inhibition of non-homologous end-joining pathways developed to prevent chromosomal end-to-end fusions64. Due to this, assays for telomere-associated foci of DNA damage (TAFs), assessed by assaying for colocalization of telomeric probes and gamma-H2AX antibodies, which accumulate in cells following senescence inducing stress, are relatively sensitive and specific for detecting senescent cells8. Other nuclear alterations include loss of the nuclear intermediate filament protein and the epigenetic modulator, lamin B165, specific chromatin remodeling patterns termed senescence-associated heterochromatin foci (SAHF)66, and decreased DNA replication, each of which can be assessed using immunofluorescence techniques. Additional genetic and epigenetic markers include de-repression of LINE-1 retrotransposons67 and upregulation of the histone acetyltransferase KAT768.
The cellular senescence research field is currently being propelled by “omic” and bioinformatic approaches that may elicit a better understanding of the senescence landscape and provide new molecular insights with a particular emphasis on heterogeneity. Transcriptomic approaches yield unique perspectives into the dynamics of senescent cells while suggesting novel markers. It was recently revealed that, regardless of the inducing stress and cell type, there appear to be shared profiles of differential gene expression in senescent cells55. This includes a shared downregulation of histone-associated transcripts and upregulation of the lncRNA PURPL which is involved in p53 signal modulation. However, at single cell resolution, transcriptomic analysis reveals that even a single cell faced with identical stressors yields unique senescent subtypes with distinct profiles of differential gene and SASP expression69, calling into question the possibility of ever finding a single “gold standard” senescence marker. Regardless, single cell transcriptomics allow naturally occurring senescent cell populations to be examined by leveraging a multitude of marker transcripts. For example, this technique has been used to show that adipose-derived mesenchymal stem cells accumulate senescence markers with natural aging and altered senescence-associated pathways70. Coupled with epigenomic insight71, proteomic72, and metabolomic73 data, our understanding of the senescent cell fate is growing exponentially and we are on the path to a comprehensive profiling database.
The Senescence-Associated Secretory Phenotype
In addition to the effects mediated by their proliferative arrest, the SASP is a key contributor to the combined physiologic and pathologic roles of senescent cells. The SASP represents a myriad of cytokines, matrix metalloproteinases, microRNAs, chemokines, growth factors, and small molecule metabolites that are both directly secreted or exosomally packaged6,15,74 and are largely under the control of the p53, NF-kB, C-EBP-B, JAK/STAT, and GATA4 transcription factors75-78. Beyond the transcriptional level, there is an evolving understanding that SASP regulation is multi-layered, including contributions from pre-transcriptional signaling cascades such as the cGAS/STING pathway79-81 as well as epigenetic regulation82,83 with particular remodeling noted in the super-enhancer landscape84. Efforts are being made, such as by the SASP atlas, to map and record the resulting senescence secretome and such analyses already indicate the SASP varies with different stressors72. For example, pathogen-related factors, such as lipopolysaccharide or SARS-CoV-2 S1 antigen, can substantially amplify the SASP of existing senescent cells, potentially contributing to the increased risks for cytokine storm and mortality in the elderly and those with chronic diseases that are associated with a high burden of senescent cells due to infections50.
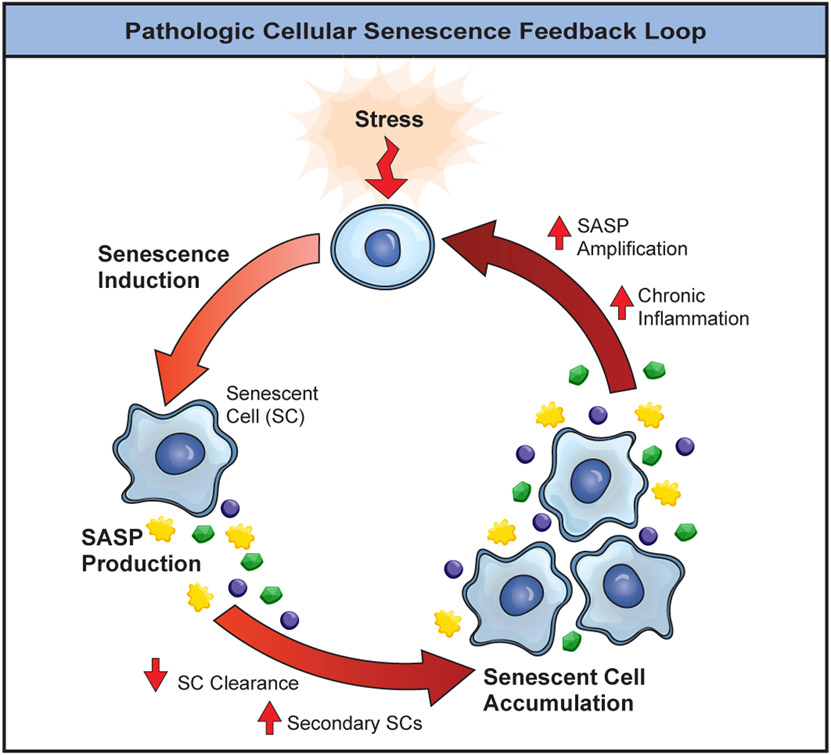
SASP components fulfill many functions, but are classically associated with the chronic inflammatory state of aging85,86. Several SASP components are immunomodulatory87. SASP chemokines such as IL-1, IL-8, and TNF-alpha recruit immune cells including macrophages, neutrophils, and T cells88-90. This allows for senescent and neighboring cells that have accumulated ROS, DNA damage, or oncogenic stress to be destroyed, consistent with the protective role of senescence in tumor prevention. Conversely, these same SASP components (alongside others) when chronically or uncontrollably expressed may perpetuate tumor seeding and invasion through matrix and vascular remodeling. This could explain the apparently contradictory findings implicating senescence in both cancer prevention and progression91-94. Furthermore, the SASP is not only a product of senescent cells, it also induces and reinforces senescence itself through paracrine and autocrine signaling mechanisms34,95,96. In light of this, it is thought that age-associated losses in immune competency in a chronically inflamed milieu may allow senescent cells to evade removal97-99, although this is not fully understood. Additionally, SASP signals confer senescent cells with resistance to immune mediated clearance, for example through upregulation of ligands such as HLA-E, which can inhibit CD8+ T-Cell and Natural Killer cell function100. Regardless of the exact underlying mechanism of immune interplay, senescent cell accumulation can perpetuate a feed-forward cycle of failed clearance coupled with increased SASP signals and resulting secondary senescent cell induction (Figure 1). Of note, though, there is debate over whether cells that are secondarily induced into senescence are similar to those becoming senescent due to a primary stressor, with evidence indicating differences SASP dynamics between primarily- and secondarily-induced senescent cells101. Additionally, senescence and damaging SASP signals are further augmented by aged immune system components. For example, T cells with mitochondrial dysfunction, like those present with aging, cause global increases in senescent cell burden that are associated with increases in frailty and multimorbidity and that appear to be partially mediated by TNF-alpha signaling102. Furthermore, introducing a construct that interferes with DNA repair into hematopoietic progenitors in transgenic mice, so that immune cells prematurely become senescent, causes early development of multiple age-related phenotypes and increases senescent cell burden in multiple tissues in transgenic mice103.
Figure 1. Senescent Cell Accumulation Positive Feedback Loop.
Cellular senescence is induced following exposure to an initial stress. The resulting senescent cells produce a SASP that can potentiate further senescence cell accumulation and impair clearance. In turn, the SASP can be amplified eliciting an environment of chronic inflammation and additional senescence inducing stressors that drive a feed-forward cycle of senescent cell accumulation.
SASP heterogeneity, reflecting the complexity of the underlying senescence program, is further recapitulated in how the SASP impacts the regenerative potential of non-senescent cells. When expressed transiently, NF-kB pathway SASP factors can promote “stemness” and enhance regenerative potential in keratinocyte regeneration models in vivo27. However, interruption of this signal or prolonged exposure to it reduces stemness markers and impairs regenerative capacity27. This highlights the need to consider SASP kinetics and illustrates how chronic senescent cell accumulation and signaling can impair ability to respond to physiologic insults. Opposing roles of the senescent secretome are also evident in the liver. Senescence and associated TGF-beta signaling have been linked with impaired regeneration and biliary fibrosis104, while genetic ablation of senescent cells and ensuing SASP reduction can induce fibrosis in vascular structures105. Although these findings may be artifacts of the underlying model systems used, including continuous elimination of senescent cells, limited specificity of p16 as a senescence marker, and potentially vascular cell populations with associated vascular leakage in the latter study105, there appears to be contextual variability in features of senescence.
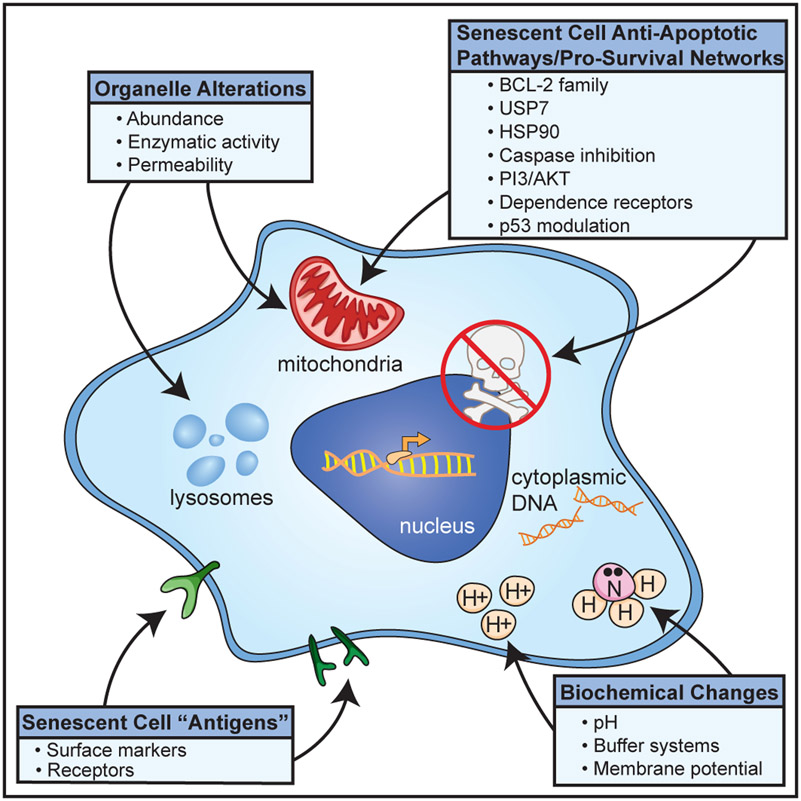
Targeting Senescent Cells
A 2004 report31 of an inverse relation between senescent cell burden and healthspan in mice prompted the initiation of efforts to develop drugs that selectively eliminate senescent cells. The subsequent development of the transgenic INK-ATTAC mouse model32, in which age-related phenotypes were alleviated though selectively removing highly p16-expressing cells from progeroid mice, further supported these efforts. Since senescent cells are highly heterogeneous in both their molecular biology as well as their physiological function, targeted strategies are needed that ideally preserve senescent cells in beneficial contexts while eliminating effects that are detrimental. Broadly, these therapies can be broken down into the major categories of senomorphic and senolytic drugs, though this classification might be somewhat arbitrary as agents with senomorphic effects in one cell type or context may be senolytic in another and vice versa. Senomorphic compounds target pathologic SASP signaling, while senolytics eliminate the underlying senescent cells that release damaging SASP factors. Senomorphics are discussed elsewhere, but in brief senomorphics prevent the production of, antagonize, or neutralize SASP components106,107, and usually require continuous administration. We will instead focus on emerging senolytic strategies that address a root cause of senescence pathology, senescent cells, yielding pleiotropic benefits with intermittent administration. The current senolytic “class” originates from work demonstrating senescent cell clearance with the combination of Dasatinib and Quercetin10 and, subsequently, BCL-2 family inhibitors and others108-112. While the first senolytics were developed using a bioinformatically informed approach aimed at disrupting SCAPs and other pro-survival networks10, the class has expanded to take advantage of additional senescence features and enhance immune-mediated clearance (Figure 2). Broadly, first generation agents act by transiently disabling SCAPs, causing those senescent cells with a tissue-damaging SASP to kill themselves. Importantly, while all senolytic strategies may elicit off-target effects or interfere with beneficial populations, these can often be limited as most therapeutics are amenable to an intermittent “hit-and-run” dosing strategies that do not require daily, or even weekly, administration. This interval dosing strategy is hypothesized to be efficacious given that senescent cells take upwards of 7 days or more (at least in vitro) to accumulate and develop a SASP even when faced with persistent and harsh senescence-inducing stress in vitro67,113, and could potentially take as long to start re-accumulating in vivo.
Figure 2. Senescent Cell Features Targeted by Senolytics.
Select features of senescent cells have been leveraged to specifically reduce their abundance. Broadly, these targets include unique surface markers, SCAP and other survival networks, biochemical adaptations, and changes in organelle characteristics.
Extracellular Targets and Immune-Mediated Clearance
Characterization of senescent cells has revealed unique markers that serve as senescence associated self-antigens. These can be co-opted for immune system-mediated senolytic activity and clearance. A recent study114 took advantage of this using chimeric antigen receptor (CAR) T cells targeted against the urokinase-type plasminogen activator receptor (uPAR) in a mouse model. uPAR is associated with extracellular matrix remodeling that is upregulated at the cell surface of senescent cells during replicative, oncogene-induced, and toxicity-induced senescence. Cytotoxic CAR T cells were able to selectively clear uPAR-expressing senescent cells in vitro and in vivo. CAR T-mediated clearance of senescent cells led to survival and histopathologic benefit in murine models of both carbon tetrachloride- and diet-induced liver fibrosis, suggesting the feasibility and potential of this clearance strategy. However, supratherapeutic CAR T dosing is associated with a proinflammatory cytokine profile, weight loss, and hypothermia, suggesting that careful attention would need to be paid to initial dosing strategies, particularly in geriatric populations where a compromised immune system together with ongoing chronic inflammation may restrict the therapeutic window. Additionally, CAR T approaches in humans involve initial immune system suppression with considerable attendant morbidity and are expensive. Though senolytic CAR T cells appear to be self-limiting114, their expansion and contraction occurs over a period of days, which is a risk in the case of an acute to subacute adverse reaction. Overall, this strategy is highly promising given its preclinical efficacy and senescent cell specificity, but future optimization and testing is necessary before clinical administration.
Co-opted senescence antigens provide an additional strategy for cell clearance through vaccination. Senescent T cell populations accumulate in obese adipose tissue, contributing to inflammation with both local and systemic effects115. These T cell populations bear known senescence associated markers and are characterized by CD4+, CD44high, CD62LLow, PD-1+, and CD153+ expression. Immunization against these cells with a CD153 peptide conjugate promotes senescent T cell clearance from adipose tissue with associated improvements in metabolic function. As with other immune-mediated clearance strategies, vaccination against senescence epitopes will require careful consideration for clinical translation especially in the context of their lasting effects that might be difficult to reverse. As CD 153 is implicated in mycobacterial clearance116, neutralizing antibodies or elimination of positive cells may be contraindicated in those with a history or enhanced susceptibility to mycobacterial infection. Additionally, immunosenescence may limit vaccine response and memory in the geriatric population117.
Modulating SCAPs
Prototypic senolytic drugs were developed to target SCAP networks10. In contrast to a “one drug, one target” approach, SCAP inhibition may interface with several pro-survival signals at once. As a result, these early senolytics typically possess several pharmacologic mechanisms of action that interact synergistically. Prime examples of this are the flavonoid fisetin118 as well as the senolytic combination of the Src kinase inhibitor dasatinib and the flavonoid quercetin (D+Q), which have been utilized and reviewed thoroughly112. In brief, though the precise mechanism of action is unknown (as is the case for most agents), the D+Q combination exerts broad spectrum senolytic activity through interference with several pro-survival networks, including ephrin dependence receptor signaling, PI3K/Akt, and BCL-2 members. The BCL-2 family members (BCL-2, BCL-XL, BCL-W, etc.), which prevent activation of pro-apoptotic mitochondrial signaling cascades, cytochrome C release, and downstream caspase activation are targeted by other senolytics. These compounds, such as Navitoclax (ABT-263), A1331852, and A1155463, display in vitro activity against senescent human lung fibroblasts and umbilical vein endothelial cells10,119 amongst other cell types120. However, in contrast to D+Q, these drugs do not eliminate all senescent populations in vitro, with particular resilience demonstrated by senescent pre-adipocytes that are capable of causing widespread metabolic dysfunction and harm in vivo34. Additionally, the clinical utility of BCL-2 inhibitors as a senolytic is limited by off-target effects on platelets121, neutrophils122, and potentially T-cells123, which can be idiosyncratic (i.e. can occur after a single dose) and might impair hemostasis and further compromise immune function in at-risk populations, though intermittent dosing may help. Additional SCAPs that can be drug targeted include modulation of p53 associated pathways and interruption of the anti-apoptotic transcription factor FOXO412, inhibition of the peptidase USP7124, inhibition of the HSP90 chaperones125, increased apoptotic drive by caspase activation126, and others that are being studied.
Other Approaches
Additional aspects of senescent cells are advantageous for directed senolysis. One such feature is their increased lysosomal enzyme activity. This can be leveraged with the use of prodrugs that are cleaved and activated by the lysosomal enzyme SA beta-Gal or by loading cytotoxic chemicals into galacto-polymer-coated nanoparticles that can be preferentially released into senescent cells127,128. This strategy could suffer from off-target effects in non-senescent cells with high SA beta-Gal activity, such as activated macrophages129. Lysosomal abundance in senescent cells also offers the opportunity for senolysis through increased autophagy. Autophagy is normally involved with the turnover of organelles and other cellular components that are directed to the lysosome for molecular repurposing. Outside of its role as a cellular recycling system, autophagy can lead to activation of cell death pathways when highly activated under persistent stress130. Autophagy is inhibited within senescent cells131, but senescent cells are primed for cell death following an autophagic push. This is demonstrated by autophagy induction and subsequent senolysis with the use of fibrate drugs132, metformin133, mTORC1 inhibitors134, BET inhibition135, and lysosomal acidification with ATM inhibitors136. Beyond organelle targeting, even minor chemical changes can be exploited for preferential senolysis. This is demonstrated by the senolytic activity of cardiac glycosides, which take advantage of changes in membrane potentials and proton concentrations within senescent cells137,138. Furthermore, compensatory responses to these chemical changes in senescent cells may be targeted. For example, senescent cells resist lowered pH produced by lysosomal alterations and other factors by upregulating buffering systems including the glutaminase product ammonia139. Interruption of these buffering systems can induce preferential senescent cell death, and the enzymes that maintain buffer concentrations could be targeted by small molecule drugs.
Clinical Trials of Senolytics
The first clinical study of senolytics published was a pilot, open-label study of 14 patients with idiopathic pulmonary fibrosis140 (IPF; ClinicalTrials.gov identifier [NCT] 02874989). They were administered 9 doses of oral D+Q over 3 weeks. Five days after the final dose, the subjects had improved 6-minute walk distance, walking speed, chair rise ability, and short physical performance battery. This may have been related to the study drug, learning effects, or other factors inherent in open-label study designs. Based on these initial data, a larger, placebo-controlled clinical trial of D+Q for IPF is planned. Interim results were recently reported from a Phase 1, open-label, clinical trial of D+Q in subjects with diabetic kidney disease (DKD; NCT 02848131). By 11 days after the last day of a 3-day oral course of D+Q, 9 subjects with DKD had decreased adipose tissue p16INK4A+ and SA beta-Gal + cells compared to biopsies before D+Q was given38,141. Additionally, 11 days after completing the 3-day senolytic intervention, a composite score of 10 circulating SASP factors was significantly decreased as was activated CD68+ macrophage adipose tissue infiltration and adipose tissue crown-like structures, which are due to fibrosis. In this continuing trial (goal=30 subjects), no serious or severe side effects have emerged so far. Multiple other clinical trials are underway or about to begin (Table 2). These include, among others, trials of D+Q for Alzheimer’s disease (ALSENLITE, NCT 04785300; SToMP-AD, NCT 04685590), the accelerated aging-like state in bone marrow transplant survivors (HTSS; NCT 02652052), the accelerated aging-like state in survivors of childhood cancer (SENSURV; NCT 04733534), and age-related osteoporosis (NCT 04313634) and trials of Fisetin for frailty in older women (AFFIRM; NCT 03430037), diabetic and chronic kidney disease (NCT 03325322), childhood cancer survivors (compared to D+Q in SENSURV), age-related osteoporosis (compared to D+Q in NCT 04313634), osteoarthritis (NCT 04210986), and coronavirus in nursing home, hospitalized, and outpatients (COVID-FIS, NCT 04537299; COVID-FISETIN, NCT 04476953; and COVFIS-HOME, NCT 04771611, respectively). In addition to D+Q and Fisetin, a trial of the Bcl-xL inhibitor UBX1325 for the treatment of diabetic macular edema is currently recruiting (NCT 04537884). A clinical trial of the proposed senolytic compound UBX0101, an inhibitor of the murine double minute 2 (MDM2) negative regulator of p53 for treatment of osteoarthritis (NCT 03513016) was recently halted in phase II following failure to outperform placebo in interim analysis. This is speculated to be due to several factors including that MDM2 inhibitors have senomorphic activity, which could represent their primary mechanism of action and would require continuous administration142. Additionally, UBX0101 required a treatment course of multiple injections in preclinical models143 in contrast to the single injection in the clinical trial. Potential benefits of the UBX0101 arm of the trial may also have been masked due to the clinical benefits of intra-articular saline injection on patient reported outcomes in osteoarthritis144. Until results and data about benefits as well as adverse or off-target events are available from these and other studies, senolytic agents should not be administered outside carefully monitored clinical trials.
Table 2.
New and Ongoing Clinical Trials for Senolytic Therapies.
| Senolytic Therapy |
Indication | Trial |
|---|---|---|
| D+Q | Diabetic Kidney Disease | NCT 02848131 |
| Alzheimer's Disease | ALSENLITE, NCT 04785300 | |
| SToMP-AD, NCT 04685590 | ||
| Accelerated age-like state post Bone Marrow Transplantation | HTSS; NCT 02652052 | |
| Accelerated age-like state in childhood cancer survivors | SENSURV; NCT 04733534 | |
| Age-Related Osteoperosis | NCT 04313634 | |
| Fisetin | Frailty in older women | AFFIRM; NCT 03430037 |
| Diabetic and Chronic Kidney Disease | NCT 03325322 | |
| Accelerated age-like state in childhood cancer survivors | SENSURV; NCT 04733534 | |
| Age-Related Osteoperosis | NCT 04313634 | |
| Osteoarthritis | NCT 04210986 | |
| COVID-19 in Nursing Home Patients | COVID-FIS, NCT 04537299 | |
| COVID-19 in Hospitalized Patients | COVID-FISETIN, NCT 04476953 | |
| COVID-19 in Outpatients | COVFIS-HOME, NCT 04771611 | |
| UBX1325 | Diabetic Macular Edema | NCT 04537884 |
Conclusions and Future Directions
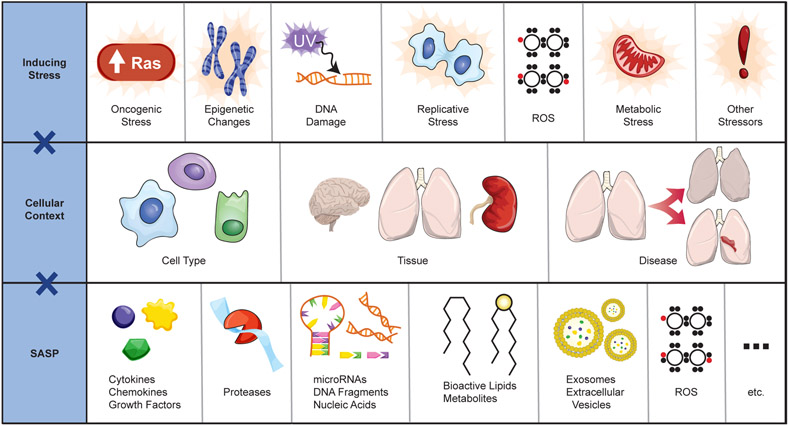
In the last decade there has been exponential growth in cellular senescence research due to its pervasive and widespread implications. Additional field-defining discoveries are certain to follow over the coming years. However, substantial gaps and key questions still remain. Senescent cells exhibit hysteresis, in that their phenotypes are dependent on the context of prior stress. Furthermore, senescent cells are heterogeneous in both form and function. Senescent phenotypes vary by cell type, tissue of origin, tissue of residence, functional impact, and how senescence was induced (Figure 3). This is further complicated by differences between in vitro models and translation from tissue cultures studies to in vivo animal models and ultimately to humans. However, few models exist to study these differences (Table 3). Current animal models such as INK-ATTAC32 or p16-3MR mice25 and other p16-dependent systems105,145-147 are limited because p16Ink4a is not expressed by every senescent cell and non-senescent, frequently abundant cell types, such as activated macrophages, can have high expression of p16Ink4a129. Murine systems using p21 based constructs have been recently developed to address these issues and explore uncharacterized senescent cell populations148. However, it is ultimately unknown if senescent cells in mice are representative of those found in humans. We have begun to address this through transplantation studies34, in which human senescent cells are introduced into murine hosts, but this question remains open. The field is in clear need of novel animal models, senescent cell culture systems, and additional human translational experiments to push forward. Amidst this evolving appreciation of senescent cell heterogeneity, it is likely that there are yet undefined populations and subpopulations of senescent cells that may have distinct phenotypes, possess unique spatiotemporal dynamics, and fulfill distinct physiologic and pathogenic roles in a context-dependent manner. In particular, few studies have been conducted to assess the characteristics of naturally-occurring senescent cells70, which are likely to be the most relevant to aging phenotypes. While there is an abundance of preclinical evidence indicating that senolytics may treat various disease processes or even supplement regenerative therapies149, it is unknown how modulating different senescent cell populations with senotherapeutic strategies will translate into clinical outcomes or whether senolytics differ in efficacy when used preventatively or after a disease process has already begun. Ideally, as our understanding of senescence heterogeneity expands, it will be increasingly possible to use rational design strategies to target and eliminate only the most detrimental senescent cell subpopulations, for example by leveraging single cell differential gene expression profiles across senescent cells. However, these translational questions are challenging to address considering the inherent variations between animal models and humans, which are convoluted by differences in immune function and kinetics of senescent cell accumulation. Collectively, these gaps need to be addressed by the burgeoning cellular senescence field and are likely to evoke interest for the foreseeable future.
Figure 3. Layers of Heterogeneity in Cellular Senescence.
Senescent cells exhibit context dependent phenotypic diversity. Numerous stimuli can induce a stress response sufficient to induce cellular senescence. Furthermore, susceptibility to these stressors and senescent cell characteristics can depend on cell type, tissue, disease state, and other context. The resulting senescent cells display a spectrum of convergent and divergent phenotypes in their secretome and consequent functionality. (ROS, Reactive Oxygen Species).
Table 3.
CDKI Construct Based Models to Study Senescent Cells.
| Model | Construct | Utility | Ref |
|---|---|---|---|
| p16 INK-ATTAC | Transgenic p16 promoter driving drug (AP20187) inducible caspase 8 activation/cell death and GFP | GFP fluorescent tracking and controlled elimination of p16 positive cells via AP20187 administration. | 32 |
| p16-3MR | Transgenic p16 promoter driving trimodality reporter of luciferase, monomeric RFP, and herpes simplex virus 1 thymidine kinase | Bioluminescence assays, RFP fluorescent cell tracking, and controlled elimination of p16 positive cells via ganciclovir administration. | 25 |
| p16-cre | Knock-in of constitutively active Cre, thymidine kinase, and TdTomato to end of endogenous p16 3rd exon | Cre-mediated conditional gene expression (i.e. fluorescent reporter, suicide gene DTA) in cells expressing p16. Of note, this line is crossed with reporter and DTA mouse lines due to reported low p16 expression in vivo and resulting lack of TdTomato expression or ganciclovir sensitivity. | 105 |
| p16-cre | Inducible Cre knock-in at the first exon of the endogenous p16 locus | Cre-mediated conditional gene expression (i.e. fluorescent reporter) in cells expressing p16. | 145 |
| p16-Tdtom+ | Knock-in of TdTomato to first exon of endogenous p16 | Tracking of p16 expressing cells via fluorescent reporter. | 146 |
| p16-Luciferase | Knock-in of firefly luciferase to translational start site of endogenous p16 locus | Bioluminescence assays, and luciferase expression tracking to assess for p16 expression. | 147 |
| p21-Cre | Transgenic p21 promoter driving inducible Cre and GFP | Cre-mediated conditional gene expression (i.e. fluorescent signal tracking via cross with floxed TdTomato reporter line, targeted ablation via DTA) in cells highly expressing p21, following Tamoxifen administration. Tamoxifen independent tracking of p21 expression via GFP. | 148 |
Acknowledgement
The Authors would like to thank Geneva Hargis PhD. for help with drafting figure images and Iman Al-Naggar, PhD. for feedback during the review process. This review was supported in part by Glenn Foundation for Medical Research and AFAR Grant for Junior Faculty (M.X.), the Esperance Fellowship in Personalized Nutrition (N.S.G), The Kenneth and Paula Munson Family Fund for Student Support in Health Sciences Fellowship (N.S.G), Robert and Arlene Kogod (J.L.K.), the Connor Group (J.L.K.), Robert J. and Theresa W. Ryan (J.L.K.), the Noaber Foundation (J.L.K.), Travelers Chair in Geriatrics and Gerontology (G.A.K.), and NIH grants R37AG013925 (J.L.K.), R01AG072301 (J.L.K), P01AG062413 (J.L.K.), R33AG061456 (Translational Geroscience Network; J.L.K., G.A.K.), R21AG063528 (M.X., G.A.K.), R03AG072374 (M.X.), R01AG066679 (M.X.), and R01AG068860 (M.X.).
Footnotes
Conflict of Interest
Patents on senolytic drugs and their uses are held by Mayo Clinic. This research has been reviewed by the Mayo Clinic Conflict of Interest Review Board and was conducted in compliance with Mayo Clinic Conflict of Interest policies.
Data Availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- 1.Miller RA Extending life: scientific prospects and political obstacles. Milbank Q 80, 155–174, doi: 10.1111/1468-0009.00006 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Niccoli T & Partridge L Ageing as a risk factor for disease. Curr Biol 22, R741–752, doi: 10.1016/j.cub.2012.07.024 (2012). [DOI] [PubMed] [Google Scholar]
- 3.Li X et al. Longitudinal trajectories, correlations and mortality associations of nine biological ages across 20-years follow-up. Elife 9, doi: 10.7554/eLife.51507 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferrucci L & Kuchel GA Heterogeneity of Aging: Individual Risk Factors, Mechanisms, Patient Priorities, and Outcomes. J Am Geriatr Soc, doi: 10.1111/jgs.17011 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hayflick L & Moorhead PS The serial cultivation of human diploid cell strains. Exp Cell Res 25, 585–621, doi: 10.1016/0014-4827(61)90192-6 (1961). [DOI] [PubMed] [Google Scholar]
- 6.Gorgoulis V et al. Cellular Senescence: Defining a Path Forward. Cell 179, 813–827, doi: 10.1016/j.cell.2019.10.005 (2019). [DOI] [PubMed] [Google Scholar]
- 7.d'Adda di Fagagna F et al. A DNA damage checkpoint response in telomere-initiated senescence. Nature 426, 194–198, doi: 10.1038/nature02118 (2003). [DOI] [PubMed] [Google Scholar]
- 8.Hewitt G et al. Telomeres are favoured targets of a persistent DNA damage response in ageing and stress-induced senescence. Nat Commun 3, 708, doi: 10.1038/ncomms1708 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Passos JF et al. Mitochondrial dysfunction accounts for the stochastic heterogeneity in telomere-dependent senescence. PLoS Biol 5, e110, doi: 10.1371/journal.pbio.0050110 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu Y et al. The Achilles' heel of senescent cells: from transcriptome to senolytic drugs. Aging Cell 14, 644–658, doi: 10.1111/acel.12344 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kirkland JL & Tchkonia T Cellular Senescence: A Translational Perspective. EBioMedicine 21, 21–28, doi: 10.1016/j.ebiom.2017.04.013 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baar MP et al. Targeted Apoptosis of Senescent Cells Restores Tissue Homeostasis in Response to Chemotoxicity and Aging. Cell 169, 132–147 e116, doi: 10.1016/j.cell.2017.02.031 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marcotte R, Lacelle C & Wang E Senescent fibroblasts resist apoptosis by downregulating caspase-3. Mech Ageing Dev 125, 777–783, doi: 10.1016/j.mad.2004.07.007 (2004). [DOI] [PubMed] [Google Scholar]
- 14.Schnabl B, Purbeck CA, Choi YH, Hagedorn CH & Brenner D Replicative senescence of activated human hepatic stellate cells is accompanied by a pronounced inflammatory but less fibrogenic phenotype. Hepatology 37, 653–664, doi: 10.1053/jhep.2003.50097 (2003). [DOI] [PubMed] [Google Scholar]
- 15.Coppe JP et al. Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS Biol 6, 2853–2868, doi: 10.1371/journal.pbio.0060301 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hari P et al. The innate immune sensor Toll-like receptor 2 controls the senescence-associated secretory phenotype. Sci Adv 5, eaaw0254, doi: 10.1126/sciadv.aaw0254 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Storer M et al. Senescence is a developmental mechanism that contributes to embryonic growth and patterning. Cell 155, 1119–1130, doi: 10.1016/j.cell.2013.10.041 (2013). [DOI] [PubMed] [Google Scholar]
- 18.Davaapil H, Brockes JP & Yun MH Conserved and novel functions of programmed cellular senescence during vertebrate development. Development 144, 106–114, doi: 10.1242/dev.138222 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lorda-Diez CI et al. Apoptosis during embryonic tissue remodeling is accompanied by cell senescence. Aging (Albany NY) 7, 974–985, doi: 10.18632/aging.100844 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Da Silva-Alvarez S et al. Cell senescence contributes to tissue regeneration in zebrafish. Aging Cell 19, e13052, doi: 10.1111/acel.13052 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meyer K, Hodwin B, Ramanujam D, Engelhardt S & Sarikas A Essential Role for Premature Senescence of Myofibroblasts in Myocardial Fibrosis. J Am Coll Cardiol 67, 2018–2028, doi: 10.1016/j.jacc.2016.02.047 (2016). [DOI] [PubMed] [Google Scholar]
- 22.Feng T et al. CCN1-Induced Cellular Senescence Promotes Heart Regeneration. Circulation 139, 2495–2498, doi: 10.1161/CIRCULATIONAHA.119.039530 (2019). [DOI] [PubMed] [Google Scholar]
- 23.Jun JI & Lau LF The matricellular protein CCN1 induces fibroblast senescence and restricts fibrosis in cutaneous wound healing. Nat Cell Biol 12, 676–685, doi: 10.1038/ncb2070 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krizhanovsky V et al. Senescence of activated stellate cells limits liver fibrosis. Cell 134, 657–667, doi: 10.1016/j.cell.2008.06.049 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Demaria M et al. An essential role for senescent cells in optimal wound healing through secretion of PDGF-AA. Dev Cell 31, 722–733, doi: 10.1016/j.devcel.2014.11.012 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mosteiro L et al. Tissue damage and senescence provide critical signals for cellular reprogramming in vivo. Science 354, doi: 10.1126/science.aaf4445 (2016). [DOI] [PubMed] [Google Scholar]
- 27.Ritschka B et al. The senescence-associated secretory phenotype induces cellular plasticity and tissue regeneration. Genes Dev 31, 172–183, doi: 10.1101/gad.290635.116 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schosserer M, Grillari J & Breitenbach M The Dual Role of Cellular Senescence in Developing Tumors and Their Response to Cancer Therapy. Front Oncol 7, 278, doi: 10.3389/fonc.2017.00278 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prieto LI & Baker DJ Cellular Senescence and the Immune System in Cancer. Gerontology 65, 505–512, doi: 10.1159/000500683 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Campisi J Aging, cellular senescence, and cancer. Annu Rev Physiol 75, 685–705, doi: 10.1146/annurev-physiol-030212-183653 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krishnamurthy J et al. Ink4a/Arf expression is a biomarker of aging. J Clin Invest 114, 1299–1307, doi: 10.1172/JCI22475 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baker DJ et al. Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature 479, 232–236, doi: 10.1038/nature10600 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu M et al. Transplanted Senescent Cells Induce an Osteoarthritis-Like Condition in Mice. J Gerontol A Biol Sci Med Sci 72, 780–785, doi: 10.1093/gerona/glw154 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu M et al. Senolytics improve physical function and increase lifespan in old age. Nat Med 24, 1246–1256, doi: 10.1038/s41591-018-0092-9 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Musi N et al. Tau protein aggregation is associated with cellular senescence in the brain. Aging Cell 17, e12840, doi: 10.1111/acel.12840 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Justice JN et al. Cellular Senescence Biomarker p16INK4a+ Cell Burden in Thigh Adipose is Associated With Poor Physical Function in Older Women. J Gerontol A Biol Sci Med Sci 73, 939–945, doi: 10.1093/gerona/glx134 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hickson LJ et al. Diabetic kidney disease alters the transcriptome and function of human adipose-derived mesenchymal stromal cells but maintains immunomodulatory and paracrine activities important for renal repair. Diabetes, doi: 10.2337/db19-1268 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hickson LJ et al. Senolytics decrease senescent cells in humans: Preliminary report from a clinical trial of Dasatinib plus Quercetin in individuals with diabetic kidney disease. EBioMedicine 47, 446–456, doi: 10.1016/j.ebiom.2019.08.069 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martinez-Cue C & Rueda N Cellular Senescence in Neurodegenerative Diseases. Front Cell Neurosci 14, 16, doi: 10.3389/fncel.2020.00016 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shimizu I & Minamino T Cellular senescence in cardiac diseases. J Cardiol 74, 313–319, doi: 10.1016/j.jjcc.2019.05.002 (2019). [DOI] [PubMed] [Google Scholar]
- 41.Hansel C, Jendrossek V & Klein D Cellular Senescence in the Lung: The Central Role of Senescent Epithelial Cells. Int J Mol Sci 21, doi: 10.3390/ijms21093279 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frey N, Venturelli S, Zender L & Bitzer M Cellular senescence in gastrointestinal diseases: from pathogenesis to therapeutics. Nat Rev Gastroenterol Hepatol 15, 81–95, doi: 10.1038/nrgastro.2017.146 (2018). [DOI] [PubMed] [Google Scholar]
- 43.Schmid N et al. Insights into replicative senescence of human testicular peritubular cells. Sci Rep 9, 15052, doi: 10.1038/s41598-019-51380-w (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guo M Cellular senescence and liver disease: Mechanisms and therapeutic strategies. Biomed Pharmacother 96, 1527–1537, doi: 10.1016/j.biopha.2017.11.075 (2017). [DOI] [PubMed] [Google Scholar]
- 45.Baar MP, Perdiguero E, Munoz-Canoves P & de Keizer PL Musculoskeletal senescence: a moving target ready to be eliminated. Curr Opin Pharmacol 40, 147–155, doi: 10.1016/j.coph.2018.05.007 (2018). [DOI] [PubMed] [Google Scholar]
- 46.Farr JN & Khosla S Cellular senescence in bone. Bone 121, 121–133, doi: 10.1016/j.bone.2019.01.015 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Docherty MH, O'Sullivan ED, Bonventre JV & Ferenbach DA Cellular Senescence in the Kidney. J Am Soc Nephrol 30, 726–736, doi: 10.1681/ASN.2018121251 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gruber F, Kremslehner C, Eckhart L & Tschachler E Cell aging and cellular senescence in skin aging - Recent advances in fibroblast and keratinocyte biology. Exp Gerontol 130, 110780, doi: 10.1016/j.exger.2019.110780 (2020). [DOI] [PubMed] [Google Scholar]
- 49.Khosla S, Farr JN, Tchkonia T & Kirkland JL The role of cellular senescence in ageing and endocrine disease. Nat Rev Endocrinol 16, 263–275, doi: 10.1038/s41574-020-0335-y (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Camell CD et al. Senolytics reduce coronavirus-related mortality in old mice. Science, doi: 10.1126/science.abe4832 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhou Y et al. Senolytics alleviate the degenerative disorders of temporomandibular joint in old age. Aging Cell, e13394, doi: 10.1111/acel.13394 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Martinez-Zamudio RI, Robinson L, Roux PF & Bischof O SnapShot: Cellular Senescence Pathways. Cell 170, 816–816 e811, doi: 10.1016/j.cell.2017.07.049 (2017). [DOI] [PubMed] [Google Scholar]
- 53.Giacinti C & Giordano A RB and cell cycle progression. Oncogene 25, 5220–5227, doi: 10.1038/sj.onc.1209615 (2006). [DOI] [PubMed] [Google Scholar]
- 54.Hernandez-Segura A et al. Unmasking Transcriptional Heterogeneity in Senescent Cells. Curr Biol 27, 2652–2660 e2654, doi: 10.1016/j.cub.2017.07.033 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Casella G et al. Transcriptome signature of cellular senescence. Nucleic Acids Res 47, 11476, doi: 10.1093/nar/gkz879 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Biran A et al. Quantitative identification of senescent cells in aging and disease. Aging Cell 16, 661–671, doi: 10.1111/acel.12592 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gosselin K et al. Senescent keratinocytes die by autophagic programmed cell death. Am J Pathol 174, 423–435, doi: 10.2353/ajpath.2009.080332 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Robbins E, Levine EM & Eagle H Morphologic changes accompanying senescence of cultured human diploid cells. J Exp Med 131, 1211–1222, doi: 10.1084/jem.131.6.1211 (1970). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Debacq-Chainiaux F, Erusalimsky JD, Campisi J & Toussaint O Protocols to detect senescence-associated beta-galactosidase (SA-betagal) activity, a biomarker of senescent cells in culture and in vivo. Nat Protoc 4, 1798–1806, doi: 10.1038/nprot.2009.191 (2009). [DOI] [PubMed] [Google Scholar]
- 60.Yang NC & Hu ML The limitations and validities of senescence associated-beta-galactosidase activity as an aging marker for human foreskin fibroblast Hs68 cells. Exp Gerontol 40, 813–819, doi: 10.1016/j.exger.2005.07.011 (2005). [DOI] [PubMed] [Google Scholar]
- 61.Salmonowicz H & Passos JF Detecting senescence: a new method for an old pigment. Aging Cell 16, 432–434, doi: 10.1111/acel.12580 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Summer R et al. Activation of the mTORC1/PGC-1 axis promotes mitochondrial biogenesis and induces cellular senescence in the lung epithelium. Am J Physiol Lung Cell Mol Physiol 316, L1049–L1060, doi: 10.1152/ajplung.00244.2018 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bonner WM et al. GammaH2AX and cancer. Nat Rev Cancer 8, 957–967, doi: 10.1038/nrc2523 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Smogorzewska A, Karlseder J, Holtgreve-Grez H, Jauch A & de Lange T DNA ligase IV-dependent NHEJ of deprotected mammalian telomeres in G1 and G2. Curr Biol 12, 1635–1644, doi: 10.1016/s0960-9822(02)01179-x (2002). [DOI] [PubMed] [Google Scholar]
- 65.Freund A, Laberge RM, Demaria M & Campisi J Lamin B1 loss is a senescence-associated biomarker. Mol Biol Cell 23, 2066–2075, doi: 10.1091/mbc.E11-10-0884 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Aird KM & Zhang R Detection of senescence-associated heterochromatin foci (SAHF). Methods Mol Biol 965, 185–196, doi: 10.1007/978-1-62703-239-1_12 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.De Cecco M et al. L1 drives IFN in senescent cells and promotes age-associated inflammation. Nature 566, 73–78, doi: 10.1038/s41586-018-0784-9 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang W et al. A genome-wide CRISPR-based screen identifies KAT7 as a driver of cellular senescence. Sci Transl Med 13, doi: 10.1126/scitranslmed.abd2655 (2021). [DOI] [PubMed] [Google Scholar]
- 69.Chen W et al. Single-Cell Transcriptome Analysis Reveals Six Subpopulations Reflecting Distinct Cellular Fates in Senescent Mouse Embryonic Fibroblasts. Front Genet 11, 867, doi: 10.3389/fgene.2020.00867 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang B et al. Transplanting cells from old but not young donors causes physical dysfunction in older recipients. Aging Cell 19, e13106, doi: 10.1111/acel.13106 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yang N & Sen P The senescent cell epigenome. Aging (Albany NY) 10, 3590–3609, doi: 10.18632/aging.101617 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Basisty N et al. A proteomic atlas of senescence-associated secretomes for aging biomarker development. PLoS Biol 18, e3000599, doi: 10.1371/journal.pbio.3000599 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fernandez-Rebollo E et al. Senescence-Associated Metabolomic Phenotype in Primary and iPSC-Derived Mesenchymal Stromal Cells. Stem Cell Reports 14, 201–209, doi: 10.1016/j.stemcr.2019.12.012 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Borghesan M et al. Small Extracellular Vesicles Are Key Regulators of Non-cell Autonomous Intercellular Communication in Senescence via the Interferon Protein IFITM3. Cell Rep 27, 3956–3971 e3956, doi: 10.1016/j.celrep.2019.05.095 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kang C et al. The DNA damage response induces inflammation and senescence by inhibiting autophagy of GATA4. Science 349, aaa5612, doi: 10.1126/science.aaa5612 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Salminen A, Kauppinen A & Kaarniranta K Emerging role of NF-kappaB signaling in the induction of senescence-associated secretory phenotype (SASP). Cell Signal 24, 835–845, doi: 10.1016/j.cellsig.2011.12.006 (2012). [DOI] [PubMed] [Google Scholar]
- 77.Huggins CJ et al. C/EBPgamma suppresses senescence and inflammatory gene expression by heterodimerizing with C/EBPbeta. Mol Cell Biol 33, 3242–3258, doi: 10.1128/MCB.01674-12 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Xu M et al. JAK inhibition alleviates the cellular senescence-associated secretory phenotype and frailty in old age. Proc Natl Acad Sci U S A 112, E6301–6310, doi: 10.1073/pnas.1515386112 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yang H, Wang H, Ren J, Chen Q & Chen ZJ cGAS is essential for cellular senescence. Proc Natl Acad Sci U S A 114, E4612–E4620, doi: 10.1073/pnas.1705499114 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Li T & Chen ZJ The cGAS-cGAMP-STING pathway connects DNA damage to inflammation, senescence, and cancer. J Exp Med 215, 1287–1299, doi: 10.1084/jem.20180139 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gluck S et al. Innate immune sensing of cytosolic chromatin fragments through cGAS promotes senescence. Nat Cell Biol 19, 1061–1070, doi: 10.1038/ncb3586 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hayakawa T et al. SIRT1 suppresses the senescence-associated secretory phenotype through epigenetic gene regulation. PLoS One 10, e0116480, doi: 10.1371/journal.pone.0116480 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nacarelli T, Liu P & Zhang R Epigenetic Basis of Cellular Senescence and Its Implications in Aging. Genes (Basel) 8, doi: 10.3390/genes8120343 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tasdemir N et al. BRD4 Connects Enhancer Remodeling to Senescence Immune Surveillance. Cancer Discov 6, 612–629, doi: 10.1158/2159-8290.CD-16-0217 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Franceschi C & Campisi J Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci 69 Suppl 1, S4–9, doi: 10.1093/gerona/glu057 (2014). [DOI] [PubMed] [Google Scholar]
- 86.Stojanovic SD, Fiedler J, Bauersachs J, Thum T & Sedding DG Senescence-induced inflammation: an important player and key therapeutic target in atherosclerosis. Eur Heart J 41, 2983–2996, doi: 10.1093/eurheartj/ehz919 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Munoz-Espin D & Serrano M Cellular senescence: from physiology to pathology. Nat Rev Mol Cell Biol 15, 482–496, doi: 10.1038/nrm3823 (2014). [DOI] [PubMed] [Google Scholar]
- 88.Xue W et al. Senescence and tumour clearance is triggered by p53 restoration in murine liver carcinomas. Nature 445, 656–660, doi: 10.1038/nature05529 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kang TW et al. Senescence surveillance of pre-malignant hepatocytes limits liver cancer development. Nature 479, 547–551, doi: 10.1038/nature10599 (2011). [DOI] [PubMed] [Google Scholar]
- 90.Kale A, Sharma A, Stolzing A, Desprez PY & Campisi J Role of immune cells in the removal of deleterious senescent cells. Immun Ageing 17, 16, doi: 10.1186/s12979-020-00187-9 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kaur A et al. sFRP2 in the aged microenvironment drives melanoma metastasis and therapy resistance. Nature 532, 250–254, doi: 10.1038/nature17392 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Coppe JP, Desprez PY, Krtolica A & Campisi J The senescence-associated secretory phenotype: the dark side of tumor suppression. Annu Rev Pathol 5, 99–118, doi: 10.1146/annurev-pathol-121808-102144 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Waugh DJ & Wilson C The interleukin-8 pathway in cancer. Clin Cancer Res 14, 6735–6741, doi: 10.1158/1078-0432.CCR-07-4843 (2008). [DOI] [PubMed] [Google Scholar]
- 94.Ortiz-Montero P, Londono-Vallejo A & Vernot JP Senescence-associated IL-6 and IL-8 cytokines induce a self- and cross-reinforced senescence/inflammatory milieu strengthening tumorigenic capabilities in the MCF-7 breast cancer cell line. Cell Commun Signal 15, 17, doi: 10.1186/s12964-017-0172-3 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Acosta JC et al. A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nat Cell Biol 15, 978–990, doi: 10.1038/ncb2784 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nelson G et al. A senescent cell bystander effect: senescence-induced senescence. Aging Cell 11, 345–349, doi: 10.1111/j.1474-9726.2012.00795.x (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ovadya Y et al. Impaired immune surveillance accelerates accumulation of senescent cells and aging. Nat Commun 9, 5435, doi: 10.1038/s41467-018-07825-3 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schroth J, Thiemermann C & Henson SM Senescence and the Aging Immune System as Major Drivers of Chronic Kidney Disease. Front Cell Dev Biol 8, 564461, doi: 10.3389/fcell.2020.564461 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Prata L, Ovsyannikova IG, Tchkonia T & Kirkland JL Senescent cell clearance by the immune system: Emerging therapeutic opportunities. Semin Immunol 40, 101275, doi: 10.1016/j.smim.2019.04.003 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pereira BI et al. Senescent cells evade immune clearance via HLA-E-mediated NK and CD8(+) T cell inhibition. Nat Commun 10, 2387, doi: 10.1038/s41467-019-10335-5 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Teo YV et al. Notch Signaling Mediates Secondary Senescence. Cell Rep 27, 997–1007 e1005, doi: 10.1016/j.celrep.2019.03.104 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Desdin-Mico G et al. T cells with dysfunctional mitochondria induce multimorbidity and premature senescence. Science 368, 1371–1376, doi: 10.1126/science.aax0860 (2020). [DOI] [PubMed] [Google Scholar]
- 103.Yousefzadeh MJ et al. An aged immune system drives senescence and ageing of solid organs. Nature 594, 100–105, doi: 10.1038/s41586-021-03547-7 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ferreira-Gonzalez S et al. Paracrine cellular senescence exacerbates biliary injury and impairs regeneration. Nat Commun 9, 1020, doi: 10.1038/s41467-018-03299-5 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Grosse L et al. Defined p16(High) Senescent Cell Types Are Indispensable for Mouse Healthspan. Cell Metab 32, 87–99 e86, doi: 10.1016/j.cmet.2020.05.002 (2020). [DOI] [PubMed] [Google Scholar]
- 106.Tchkonia T, Zhu Y, van Deursen J, Campisi J & Kirkland JL Cellular senescence and the senescent secretory phenotype: therapeutic opportunities. J Clin Invest 123, 966–972, doi: 10.1172/JCI64098 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Xu M, Tchkonia T & Kirkland JL Perspective: Targeting the JAK/STAT pathway to fight age-related dysfunction. Pharmacol Res 111, 152–154, doi: 10.1016/j.phrs.2016.05.015 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhu Y et al. Identification of a novel senolytic agent, navitoclax, targeting the Bcl-2 family of anti-apoptotic factors. Aging Cell 15, 428–435, doi: 10.1111/acel.12445 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yosef R et al. Directed elimination of senescent cells by inhibition of BCL-W and BCL-XL. Nat Commun 7, 11190, doi: 10.1038/ncomms11190 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tchkonia T, Palmer AK & Kirkland JL New Horizons: Novel Approaches to Enhance Healthspan Through Targeting Cellular Senescence and Related Aging Mechanisms. J Clin Endocrinol Metab 106, e1481–e1487, doi: 10.1210/clinem/dgaa728 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Robbins PD et al. Senolytic Drugs: Reducing Senescent Cell Viability to Extend Health Span. Annu Rev Pharmacol Toxicol 61, 779–803, doi: 10.1146/annurev-pharmtox-050120-105018 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kirkland JL & Tchkonia T Senolytic drugs: from discovery to translation. J Intern Med 288, 518–536, doi: 10.1111/joim.13141 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hernandez-Segura A, Brandenburg S & Demaria M Induction and Validation of Cellular Senescence in Primary Human Cells. J Vis Exp, doi: 10.3791/57782 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Amor C et al. Senolytic CAR T cells reverse senescence-associated pathologies. Nature 583, 127–132, doi: 10.1038/s41586-020-2403-9 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yoshida S et al. The CD153 vaccine is a senotherapeutic option for preventing the accumulation of senescent T cells in mice. Nat Commun 11, 2482, doi: 10.1038/s41467-020-16347-w (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sallin MA et al. Host resistance to pulmonary Mycobacterium tuberculosis infection requires CD153 expression. Nat Microbiol 3, 1198–1205, doi: 10.1038/s41564-018-0231-6 (2018). [DOI] [PubMed] [Google Scholar]
- 117.Gustafson CE, Kim C, Weyand CM & Goronzy JJ Influence of immune aging on vaccine responses. J Allergy Clin Immunol 145, 1309–1321, doi: 10.1016/j.jaci.2020.03.017 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Yousefzadeh MJ et al. Fisetin is a senotherapeutic that extends health and lifespan. EBioMedicine 36, 18–28, doi: 10.1016/j.ebiom.2018.09.015 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhu Y et al. New agents that target senescent cells: the flavone, fisetin, and the BCL-XL inhibitors, A1331852 and A1155463. Aging (Albany NY) 9, 955–963, doi: 10.18632/aging.101202 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fan Y, Cheng J, Zeng H & Shao L Senescent Cell Depletion Through Targeting BCL-Family Proteins and Mitochondria. Front Physiol 11, 593630, doi: 10.3389/fphys.2020.593630 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.de Vos S et al. Safety and efficacy of navitoclax, a BCL-2 and BCL-XL inhibitor, in patients with relapsed or refractory lymphoid malignancies: results from a phase 2a study. Leuk Lymphoma 62, 810–818, doi: 10.1080/10428194.2020.1845332 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Roberts AW et al. Targeting BCL2 with Venetoclax in Relapsed Chronic Lymphocytic Leukemia. N Engl J Med 374, 311–322, doi: 10.1056/NEJMoa1513257 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wilson WH et al. Navitoclax, a targeted high-affinity inhibitor of BCL-2, in lymphoid malignancies: a phase 1 dose-escalation study of safety, pharmacokinetics, pharmacodynamics, and antitumour activity. Lancet Oncol 11, 1149–1159, doi: 10.1016/S1470-2045(10)70261-8 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.He Y et al. Inhibition of USP7 activity selectively eliminates senescent cells in part via restoration of p53 activity. Aging Cell 19, e13117, doi: 10.1111/acel.13117 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Fuhrmann-Stroissnigg H et al. Identification of HSP90 inhibitors as a novel class of senolytics. Nat Commun 8, 422, doi: 10.1038/s41467-017-00314-z (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cherif H et al. Curcumin and o-Vanillin Exhibit Evidence of Senolytic Activity in Human IVD Cells In Vitro. J Clin Med 8, doi: 10.3390/jcm8040433 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cai Y et al. Elimination of senescent cells by beta-galactosidase-targeted prodrug attenuates inflammation and restores physical function in aged mice. Cell Res 30, 574–589, doi: 10.1038/s41422-020-0314-9 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Munoz-Espin D et al. A versatile drug delivery system targeting senescent cells. EMBO Mol Med 10, doi: 10.15252/emmm.201809355 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hall BM et al. Aging of mice is associated with p16(Ink4a)- and beta-galactosidase-positive macrophage accumulation that can be induced in young mice by senescent cells. Aging (Albany NY) 8, 1294–1315, doi: 10.18632/aging.100991 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tavassoly I et al. Dynamic Modeling of the Interaction Between Autophagy and Apoptosis in Mammalian Cells. CPT Pharmacometrics Syst Pharmacol 4, 263–272, doi: 10.1002/psp4.29 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Tai H et al. Autophagy impairment with lysosomal and mitochondrial dysfunction is an important characteristic of oxidative stress-induced senescence. Autophagy 13, 99–113, doi: 10.1080/15548627.2016.1247143 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Nogueira-Recalde U et al. Fibrates as drugs with senolytic and autophagic activity for osteoarthritis therapy. EBioMedicine 45, 588–605, doi: 10.1016/j.ebiom.2019.06.049 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bharath LP et al. Metformin Enhances Autophagy and Normalizes Mitochondrial Function to Alleviate Aging-Associated Inflammation. Cell Metab 32, 44–55 e46, doi: 10.1016/j.cmet.2020.04.015 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kucheryavenko O, Nelson G, von Zglinicki T, Korolchuk VI & Carroll B The mTORC1-autophagy pathway is a target for senescent cell elimination. Biogerontology 20, 331–335, doi: 10.1007/s10522-019-09802-9 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wakita M et al. A BET family protein degrader provokes senolysis by targeting NHEJ and autophagy in senescent cells. Nat Commun 11, 1935, doi: 10.1038/s41467-020-15719-6 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kang HT et al. Chemical screening identifies ATM as a target for alleviating senescence. Nat Chem Biol 13, 616–623, doi: 10.1038/nchembio.2342 (2017). [DOI] [PubMed] [Google Scholar]
- 137.Triana-Martinez F et al. Identification and characterization of Cardiac Glycosides as senolytic compounds. Nat Commun 10, 4731, doi: 10.1038/s41467-019-12888-x (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Guerrero A et al. Cardiac glycosides are broad-spectrum senolytics. Nat Metab 1, 1074–1088, doi: 10.1038/s42255-019-0122-z (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Johmura Y et al. Senolysis by glutaminolysis inhibition ameliorates various age-associated disorders. Science 371, 265–270, doi: 10.1126/science.abb5916 (2021). [DOI] [PubMed] [Google Scholar]
- 140.Justice JN et al. Senolytics in idiopathic pulmonary fibrosis: Results from a first-in-human, open-label, pilot study. EBioMedicine 40, 554–563, doi: 10.1016/j.ebiom.2018.12.052 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hickson LJ et al. Corrigendum to 'Senolytics decrease senescent cells in humans: Preliminary report from a clinical trial of Dasatinib plus Quercetin in individuals with diabetic kidney disease' EBioMedicine 47 (2019) 446–456. EBioMedicine 52, 102595, doi: 10.1016/j.ebiom.2019.12.004 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Dolgin E Send in the senolytics. Nat Biotechnol 38, 1371–1377, doi: 10.1038/s41587-020-00750-1 (2020). [DOI] [PubMed] [Google Scholar]
- 143.Jeon OH et al. Local clearance of senescent cells attenuates the development of post-traumatic osteoarthritis and creates a pro-regenerative environment. Nat Med 23, 775–781, doi: 10.1038/nm.4324 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Saltzman BM et al. The Therapeutic Effect of Intra-articular Normal Saline Injections for Knee Osteoarthritis: A Meta-analysis of Evidence Level 1 Studies. Am J Sports Med 45, 2647–2653, doi: 10.1177/0363546516680607 (2017). [DOI] [PubMed] [Google Scholar]
- 145.Omori S et al. Generation of a p16 Reporter Mouse and Its Use to Characterize and Target p16(high) Cells In Vivo. Cell Metab 32, 814–828 e816, doi: 10.1016/j.cmet.2020.09.006 (2020). [DOI] [PubMed] [Google Scholar]
- 146.Liu JY et al. Cells exhibiting strong p16 (INK4a) promoter activation in vivo display features of senescence. Proc Natl Acad Sci U S A 116, 2603–2611, doi: 10.1073/pnas.1818313116 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Burd CE et al. Monitoring tumorigenesis and senescence in vivo with a p16(INK4a)-luciferase model. Cell 152, 340–351, doi: 10.1016/j.cell.2012.12.010 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Wang B et al. An inducible p21-Cre mouse model to monitor and manipulate p21-highly-expressing senescent cells in vivo. Nature Aging, doi: 10.1038/s43587-021-00107-6 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Zhou Y et al. Senolytics improve bone forming potential of bone marrow mesenchymal stem cells from aged mice. NPJ Regen Med 6, 34, doi: 10.1038/s41536-021-00145-z (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.