Abstract
Hookah smoke is one of the major indoor sources of Volatile Organic Compounds (VOCs), including Benzene, Toluene, Ethylbenzene, and Xylenes (BTEX). The present study aimed to investigate potential exposure to BTEX compounds among primary school children whose parents smoked hookah at home. BTEX concentrations in indoor air were measured in 60 residential buildings of Khesht, southwestern Iran (case = 30 and control = 30). Target compounds were sampled by charcoal tubes, and the samples were then analyzed by GC-FID. Monte Carlo simulation was used to assess the carcinogenic and non-carcinogenic risks of BTX exposure for the children aged 7–13 years. The concentrations of benzene (7.19 ± 3.09 vs. 0.82 ± 0.5 μg/m3), toluene (1.62 ± 0.69 vs. 0.3 ± 0.22 μg/m3), and xylenes (2.9 ± 1.66 vs. 0.31 ± 0.22 μg/m3) were considerably higher in the indoor air of the case houses compared with the control houses (p < 0.05). The Incremental Lifetime Cancer Risk (ILCR) of benzene for non-smoking and smoking houses were estimated 1.8 × 10−6 and 15 × 10−6, respectively, exceeding the recommendations of the World Health Organization (WHO) and the Environmental Protection Agency (EPA) (1 × 10−6). Moreover, Hazard Quotients (HQs) of all BTX compounds were < 1. The indoor benzene concentration was significantly influenced by the floor at which families lived and type of the kitchen. In order to prevent children’s exposure to BTX emitted by hookah, banning indoor smoking is the only way to eliminate these compounds in the indoor air.
Keywords: Indoor air quality, Risk assessment, Hookah smoking, Benzene
Introduction
Indoor air pollution has been one of the rising health concerns, especially in the last decades [1, 2]. Recent studies have reported that the concentrations of some air pollutants were considerably higher indoors than outdoors [3, 4]. In addition, the majority of people were found to spend more time (80–90%) indoors [5, 6]. Therefore, indoor air quality is of paramount importance [7, 8]. Recently, one of the challengeable concerns in indoor air has been the use of tobacco products via water pipe (hookah). Previous studies revealed a strong association between Water pipe Tobacco Smoking (WTS) and numerous diseases, such as low birth weight, respiratory problems, and lung cancer [9–13]. Water pipe tobacco smoking, known as hookah, shisha, and narghile, has globally risen among adults and teenagers, especially in East Mediterranean countries [14, 15]. The important factors contributing to the global spread of hookah smoking have been mentioned to be the increase in the pleasant flavors of tobacco, the wrong belief that hookah is healthier than cigarettes, community acceptance, and lower costs [15–17]. Hookah has been found to have adverse effects on the people exposed to Second-Hand Smoke (SHS) and Third-Hand Smoke (THS) in addition to smokers, which has been reported to cause a wide range of serious health problems [16, 18, 19]. In this context, the World Health Organization (WHO) has reported that half of this population include the children exposed to tobacco smoke in their residence place [20]. Hookah smoke is emitted through the passage of coal-heated air over the tobacco, which produces various contaminants, such as Volatile Organic Compounds (VOCs) [21].
VOCs are one of the most important air pollutants in the atmosphere and indoor environments that evaporate easily at room temperature [22, 23]. Inhalation pathway is the major route of exposure to these contaminants [22, 23]. Among VOCs, Benzene, Toluene, Ethylbenzene, and Xylenes, known as BTEX, are environmentally important. They are emitted into the atmosphere from both natural and artificial sources, such as water pipe tobacco [22, 24]. BTEX compounds in indoor environments can emit from cleaning products, cooking appliances, building materials, furnishing, and domestic fuel. Yet, the combustion of tobacco by various methods, such as cigarette and hookah smoking, has been considered as one of the main sources of the release of these compounds [25–28]. The concentration of benzene emitted from WTS was found to be 271 ± 8 sf per session (up to 6.2 folds higher than the cigarette smoke) [29]. According to previously published papers, exposure to BTEX compounds could have numerous harmful health effects, including weakness, eyes and skin irritation, fatigue, loss of appetite, confusion, cancer, birth defects, and damage to such organs as the liver, kidneys, and the central nervous system [3, 25, 30, 31]. Since benzene can cause anemia and leukemia in humans, it has been known as the most toxic substance among BTEX compounds [32, 33]. Some international organizations, such as the International Agency for Research on Cancer (IARC), have announced benzene and ethylbenzene as carcinogenic (Group 1) and possibly carcinogenic to humans (Group 2B), respectively [4, 34, 35].
Benzene is characterized as a genotoxic carcinogen in humans, and no safe level of exposure can be recommended. The risk of toxicity from inhaled benzene would be the same whether the exposure was indoors or outdoors. According to WHO, there is no reason that the guidelines for indoor air should differ from ambient air guidelines. It is also recommended continuing to use the same unit risk factors [36]. Iran’s Environmental Protection Organization has suggested an annually exposure limit of 5 μg/m3 for benzene in the atmospheric air [37]. German committee on indoor air values established guidelines for indoor concentrations of toluene (guide value I = 0.3 mg/m3 and guide value II = 3 mg/m3) and xylenes (guide value I = 0.1 mg/m3 and guide value II = 0.8 mg/m3) [38].
Up to now, most studies have been done in cafes where people can use water pipes. In Iran, various studies have been conducted on the pollutants emitted from WTS in cafes in Ardabil [27], Bushehr [39], and Tehran [40], and traditional restaurants in Hamadan [41]. However, no attention has been paid to houses where people use water pipes with their families. People prefer to use water pipe at their houses rather than cafes because of its convenience and lower cost [42]. Nonetheless, each session of WTS lasts for averagely one hour. Hence, people at home, especially children, because of their growing lungs and higher breathing rates [43, 44], are exposed to indoor pollutants from hookah smoke. Given the growing concern regarding the increasing use of water pipe in Iran and the lack of sufficient data about BTEX contamination in residential buildings, the present study aimed to evaluate BTEX concentrations and their influencing factors in homes with hookah smoker parents for the first time in southeastern Iran. The primary reason for choosing this area was the high rate of hookah smoking. Another reason was the similarity of house structures, which could largely control the confounders that could affect the results. In addition, pollution from traffic and car exhaust, as the main source of BTEX compounds emissions [45], was very low since the houses were located at a distance of more than 5000 m from the main roads, gas stations, and industries.
Materials and methods
Study area and data collection
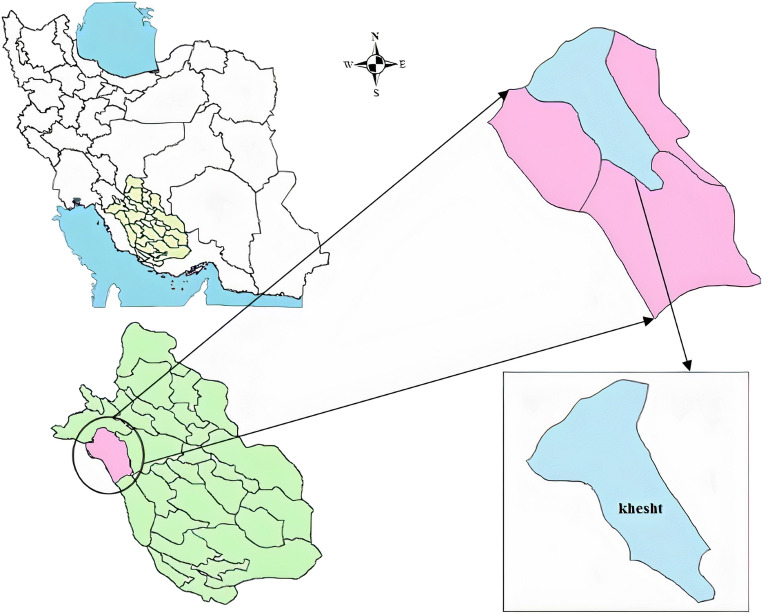
This cross-sectional study was carried out in Khesht, the capital of Khesht District in Kazerun, Fars province, southwest of Iran (29°33′49″N 51°20′13″E) (Fig. 1). The city with 30 km2 in area, is 600 m above the sea level, and has a population of approximately 11 thousand people in 2257 families. The main occupation of the inhabitants of this region is agriculture, especially palm cultivation [4].
Fig. 1.
Location map of the study area
BTEX concentrations in indoor air were investigated in 60 residential buildings in mid-June 2020.Thirty houses in which the parents of primary school children smoked hookah were selected as the case group and thirty houses without hookah smoking were selected as control group. For each house, the background information, including the use of ventilation during cooking, frequency of cooking at home, cooling system, cover of cabinets, type of kitchen, year of construction, floor, and frequency of hookah smoking at home, were recorded in a researcher-made questionnaire. Some of the questions were specific to the case group, including type of tobacco, hookah parents, and number of times a hookah was used during the day. To perform risk assessment, the weight of children was also measured.
Air sampling process
Air samples for BTEX were taken according to the NIOSH Manual of Analytical Method No. 1501 [46]. Sampling was performed by an individual sampler pump (SKC) equipped with a number of adjustable low flow holders at the continuous flow rate of 0.2 l/min for 50 min using charcoal sorbent tubes. After the completion of the sampling period, all samples were immediately transported to the laboratory based on the manufacturing guideline, stored at −20 °C, and analyzed within 72 h [27]. Collecting samples from the BTEX compounds was done between 5 and 8 PM. Sampling was carried out at children’s standing breathing zone (120–150 cm above the ground level).
Sample preparation and analysis
Briefly, BTEX compounds were extracted using 2 ml of carbon disulfide (CS2) from charcoal sorbent. According to this method, vials containing CS2 and charcoal were gently shaken for twenty minutes using an ultrasonic bath. Then, the solvent was transferred into Gas Chromatography (GC) vials and 1 μL of the prepared extraction was taken from the vial for chromatography analysis. Finally, BTEX concentrations were quantified by a GC (Agilent 7890) equipped with a FID detector using a capillary column (30 m, BD-5). Injector and detector temperatures were adjusted at 250 and 300 °C, respectively. Oven temperature was programmed at 40 °C for 10 min, and then reached 230 °C at 10 °C/min [27, 46, 47].
Quality control
The quality control and quality assurance were performed by several approaches, as follows:
The front and back sections of the charcoal tubes were separately analyzed in order to control breakthrough. BTX compounds were detected in the back section of the samples.
Limit of Detection (LOD) and Limit of Quantification (LOQ) were determined by the standard deviation of the target compounds levels per blank sample after six consecutive experiments (Eqs. 1 and 2) [48].
| 1 |
| 2 |
where B was the concentration of the blank sample.
LOD and LOQ for the BTEX compounds have been shown in Table 1. The recovery of the analytical method was tested by injecting 10 μg of the BTEX compounds into the charcoal tubes. Then, they were extracted and analyzed similar to field samples. Averagely, 92% recovery was found for the target compounds. In the present study, ethylbenzene was not detected in any of the samples, thereby replaced with half of the LOD in the statistical analyses.
Table 1.
LOD and LOQ for the BTEX compounds (μg/m3)
| BTEX compounds | LOD | LOQ |
|---|---|---|
| Benzene | 0.02 | 0.05 |
| Toluene | 0.03 | 0.08 |
| Ethylbenzene | 0.04 | 0.12 |
| Xylenes | 0.0 | 0.0 |
Statistical analysis
SPSS (v. 23) and R (v. 3.3.1) were employed in the present study. The normality of the distribution of variables was examined via Kolmogorov-Smirnov test. In addition, Mann-Whitney U test was used to compare the differences between the two independent groups. Spearman’s correlation coefficient was also used to investigate the correlations between the two variables. Furthermore, multivariate linear regression models were carried out using R (v. 3.3.1). Regression models were designed to determine the association between BTX concentrations and independent variables. P values less than 0.05 were considered statistically significant.
Risk assessment
BTEX is one of the most harmful pollutants that has negative impacts on humans exposed to Environmental Tobacco Smoke (ETS), especially children [49]. Although non-carcinogenic effects have been confirmed due to exposure to BTX compounds, benzene has been classified as a carcinogenic compound. In the present study, Incremental Lifetime Cancer Risk (ILCR) and Hazard Quotient (HQ) equations were employed to assess the carcinogenic risk of benzene as well as the non-carcinogenic risks of BTX compounds through the inhalation route, respectively) Eqs. 3 to 7([50]. Finally, ILCR of benzene in the case and control groups was calculated using Monte Carlo simulations (Oracle Crystal Ball software 11.1.2). According to WHO and United States Environmental Protection Agency (USEPA), ILCR ≤1.00 × 10−6 and ILCR >1.00 × 10−6 indicate an acceptable situation and carcinogenic effects, respectively [51]. In addition, HQ > 1 represents a high non-carcinogenic risk, while HQ ≤ 1 indicates an acceptable hazard. The selected parameters used for ILCR of benzene and HQs for BTX have been presented in Table 2.
Table 2.
The exposure variables recommendations for Monte Carlo simulations
| Unit | Value for children (7–13 years old) |
||
|---|---|---|---|
| C | Concentration of the pollutant | mg/m3 | – |
| IRc | Inhalation rate, children | m3/h | 0.65 ± 0.125 [51] |
| EDc | Exposure duration, children | h/d |
14–18 (min-max) (Questionnaires) |
| BWc | Body weight, children | Kg |
21.6–49 (min-max) (Questionnaires) |
| D | Days of exposure per week | D | 7 |
| WK | Weeks of exposure | Week | 50 |
| YE | Years of exposure | Y | 18 |
| YL | Years in lifetime | Y | 70 |
| UR | Unit risk | (mg/kg·d)−1 | Benzene = 0.029 [52] |
| RfD | Reference dose | (mg/kg·d) |
Benzene= 0.01 |
|
Toluene= 2.3 | |||
|
Xylenes= 0.04 |
RfD = RfC (inhalation reference concentration mg/m3) × 15.73 (assumed children (7–13 years old) inhalation rate m3 /d) × 1/BWc (kg); based on RfCs for USEPA, IRIS (benzene = 0.03 mg/m3, toluene = 5 mg/m3, xylenes = 0.1 mg/m3) [27].
| 3 |
| 4 |
| 5 |
| 6 |
| 7 |
where E, EY, and EL represented daily exposure (mg/kg·d), yearly average daily dose received (mg/kg·d), and effective lifetime exposure (mg/kg·d), respectively.
Results and discussion
BTEX concentrations in the indoor air of the case and control houses
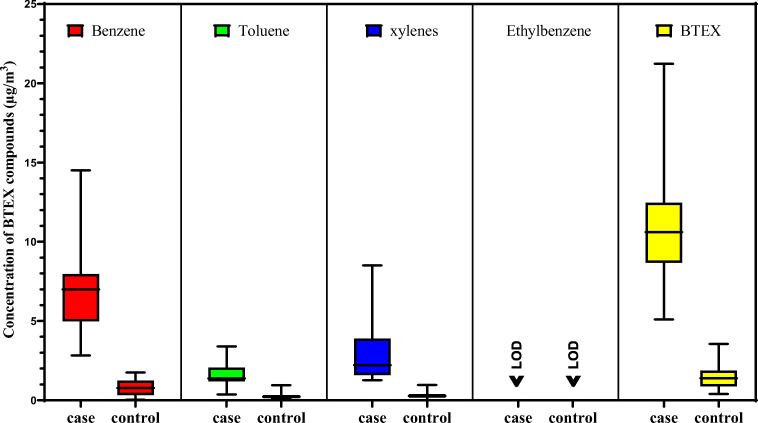
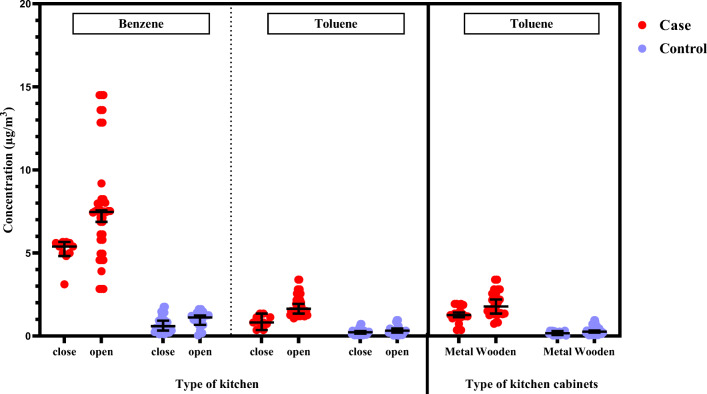
Data on the characteristics of the participants’ houses are presented in Table 3. Moreover, mean and other statistical analyses of BTEX levels in the study groups are presented in Table 4. Accordingly, mean concentrations of benzene, toluene, xylenes, and total BTEX were 8.7, 5.8, 9.4, and 8.2 folds higher in the case group than in the control group. The results revealed a significant difference between the two groups regarding the concentrations of BTX compounds (p < 0.05). The differences in the concentrations of BTX measured in the indoor air of the exposed and non-exposed children’s houses are shown in Fig. 2. The indoor benzene concentration measured in the United States was 5.54–10.5 μg/m3 in the houses exposed to Environmental Tobacco Smoke (ETS) compared with 3.86–7.0 μg/m3 in ETS-free houses [53, 54]. A similar study conducted in Germany reported benzene concentration of 11.0 and 6.5 μg/m3 in ETS and ETS-free houses, respectively [55]. In Italy, these levels were estimated to be 32.2 and 18.9 μg/m3, respectively [56]. Based on ANSES recommended guidelines for houses [47, 57], measured benzene levels in the indoor air of 76.7% of the case houses in the present study were higher than the annual exposure level recommended by IEPO (5 μg/m3). Although benzene concentrations were higher than LE (0.2 μg/m3) and LTE (10 μg/m3) in 100% and 13.3% of the case houses, respectively, they did not exceed the levels of IE (20 μg/m3) and STE (30 μg/m3) in any of the monitored case houses. WHO has suggested no acceptable level for benzene in ambient air, because benzene has been considered a carcinogen chemical substance [49]. Therefore, long-term exposure at any concentration might have adverse effects. Although the average concentration of benzene in the indoor air of the studied case houses was mostly higher than those reported by several studies (Table 5), mean benzene concentration measured in the air of the control houses was lower as compared with other investigations. The higher concentration of benzene in the case houses could be associated with the use of WTS. In fact, benzene was mainly released by burning charcoal from WTS and the mainstream water pipe smoke [29, 58].
Table 3.
Selected characteristics of the participant’s homes
| Exposure type | Exposed group | Control group |
|---|---|---|
| Characteristics | Size (%) | Size (%) |
| Floor of home | ||
| 1st | 22 (73) | 18 (60) |
| 2 ≤ | 8 (27) | 12 (40) |
| Use a ventilator when cooking | ||
| yes | 4 (13) | 13 (43) |
| no | 26 (87) | 17 (57) |
| Number of cooking times during the day | ||
| 3 > | 3 (10) | 1 (3) |
| 3 | 23 (77) | 26 (87) |
| 3 < | 4 (13) | 3 (10) |
| The main cover of kitchen cabinets | ||
| metal | 20 (67) | 16 (53) |
| MDF | 10 (33) | 14 (47) |
| Type of kitchen | ||
| open | 18 (60) | 21 (70) |
| close | 12 (40) | 9 (30) |
| Year of house construction | ||
| 5 > | 2 (7) | 6 (20) |
| 5–10 | 16 (53) | 13 (43) |
| 10 < | 12 (40) | 11 (37) |
| Cooling system | ||
| water cooler | 5 (17) | 10 (33) |
| gas cooler | 25 (83) | 20 (67) |
Table 4.
The summary of BTEX concentrations in the indoor air of the case and control houses (μg/m3)
| Contaminant | Mean ± SD (min-max) |
Median | Geometric (mean ± SD) | P value | |||
|---|---|---|---|---|---|---|---|
| Case | Control | Case | Control | Case | Control | Comparison of cases and controls | |
| Benzene |
7.19 ± 3.09 (2.83–14.5) |
0.82 ± 0.5 (0.06–1.76) |
6.99 | 0.78 | 6.62 ± 1.51 | 0.62 ± 2.39 |
P < 0.05 P = 0.00 |
| Toluene |
1.62 ± 0.69 (0.36–3.39) |
0.3 ± 0.22 (0.1–0.96) |
1.38 | 0.23 | 1.42 ± 1.59 | 0.20 ± 2.52 |
P < 0.05 P = 0.00 |
| Ethylbenzene | ND* | ND | ND | ND | ND | ND | – |
| Xylenes |
2.9 ± 1.66 (1.27–8.5) |
0.31 ± 0.22 (0.01–0.97) |
2.21 | 0.27 | 2.55 ± 1.63 | – |
P < 0.05 P = 0.00 |
| BTEX |
11.74 ± 3.85 (5.13–21.25) |
1.44 ± 0.73 (0.42–3.57) |
10.63 | 1.41 | 11.2 ± 1.37 | 1.22 ± 1.77 |
P < 0.05 P = 0.00 |
*: Not Detected
Fig. 2.
Box plot of the BTX levels in the case and control houses
Table 5.
The concentrations of BTEX compounds in the indoor air in different countries (μg/m3)
| Studies | Benzene | Toluene | Ethylbenzene | Xylenes | Reference |
|---|---|---|---|---|---|
| Cases | 7 | 2 | ND | 3 | Current study |
| Controls | 1 | 0.3 | ND | 0.3 | Current study |
| Seoul, South Korea | 3 | 40 | 8 | 10 | [62] |
| Ardabil, Iran | 15 | 70 | 12 | 48 | [47] |
| Guangzhou | 18 | 173 | – | 99 | [63] |
| Hong Kong | 5 | 52 | 3 | 8 | [64] |
| Japan | 1 | 12 | 4 | 8 | [65] |
| Mexico city | 7 | 76 | 6 | 26 | [66] |
| Spain | 1 | 4 | 0.6 | 0.7 | [67] |
In the current study, the effect of hookah smoking at home on the concentrations of toluene and xylenes was investigated by comparing the differences between the case and control groups. Tobacco smoke has been mentioned as one of the most important sources of xylenes and toluene [59, 60]. Guo et al. also reported a remarkable difference between the smoking and non-smoking homes with respect to the levels of benzene and toluene [61]. However, toluene and xylenes concentrations reported by other studies presented in Table 5 (except for xylenes level reported in Spain) were higher than the results of the current work. Differences in location, characteristics of the houses in terms of distance from the main road, traffic, and green space, differences in the characteristics of the houses in terms of humidity, ventilation, temperature, and outdoor pollution, different activities at homes, and frequency of cooking and cleaning could be the reasons for the discrepancies among the results [46, 47].
In the present study, benzene and toluene had the highest and lowest levels among the studied BTEX compounds in both groups. In addition, Among the BTEX compounds measured in the home air of the two groups, xylenes were the most different. A recent study conducted on indoor air of waterpipe cafés reported that xylenes has the highest concentration among BTEX compounds emitted from hookah smoke [27].
Factors influencing BTX concentrations
The results of multiple regression analysis (β coefficient (p value)) for the association between BTX levels and potentially confounding variables have been documented in Table 6. According to the information in the questionnaires, no painting, reconstruction, or spraying was done in any of the houses in the past 6 months. Additionally, all houses were located more than 5000 m from the main roads and gas stations.
Table 6.
Multivariate linear regression analysis of BTX (μg/m3) with the factors affecting exposure to BTX [β coefficient (p value)]
| Benzene | Toluene | Xylenes | |
|---|---|---|---|
| Type of kitchen | 1.73 (0.01)* | 0.45 (0.03)* | 0.04 (0.62) |
| Cooling system | 0.44 (0.26) | 0.13 (0.1) | 0.56 (0.51) |
| The cover of the cabinets | 0.49 (0.41) | 0.27 (0.004)* | 0.52 (0.46) |
| Year of house construction | 0.57 (0.18) | 0.132 (0.15) | 0.43 (0.47) |
| Number of cooking times during the day | 0.79 (0.33) | 0.04 (0.77) | 0.09 (0.78) |
| Home floor | −1.58 (0.01)* | −0.46 (0.01)* | −1.01 (0.009)* |
| Use of ventilation | 2.45 (0.17) | 0.06 (0.85) | 0.11 (0.89) |
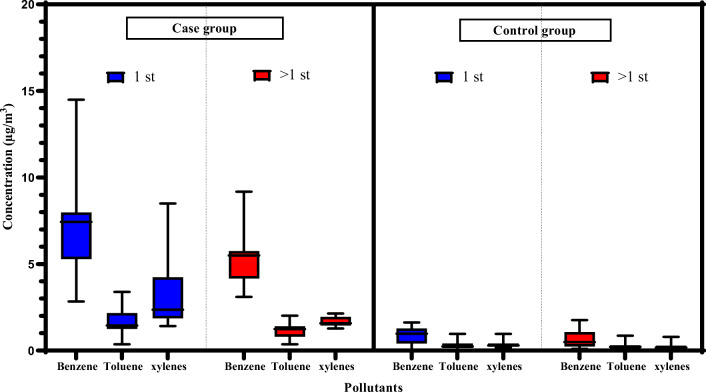
Statistical analysis showed that BTX concentrations were significantly higher in the ambient indoor air of the houses located on the ground floor (case:12.28 ± 3.78 and control:1.59 ± 0.71 μg/m3) compared with those located on the second floor and above (case:8.31 ± 1.96 and control: 1.01 ± 0.62 μg/m3) (Fig. 3). These differences were statistically significant in both groups (p < 0.05). Thus, the floor was found to be a significant predictor of BTX levels in the present work, with the greatest and lowest effects being related to benzene and toluene, respectively (Table 6). Another study conducted in Ardabil, Iran also indicated that BTEX levels were higher on the ground floor compared with other floors [47]. This could be attributed to the proximity of the ground floor to garages and vehicles, as noticeable sources of BTEX [68]. On the other hand, lower levels of BTEX in upper floors could be attributed to the higher air exchange rate [47]. Air velocity increases with altitude and air exchange rates may be higher because of windows and other open corners in upper floors. Therefore, natural ventilation is often more useful and practical than air conditioning systems, because it plays an extremely important role in diluting the concentrations of the indoor air pollutants [69, 70].
Fig. 3.
Comparison of BTX concentrations on the ground floor (1st) and the other floor (1st <) in both case and control groups
According to our findings, the type of kitchen is reported to be associated with raised benzene and toluene levels (Table 6). According to the results, the concentrations of both compounds were significantly higher in buildings with open plan kitchens compared with those with closed kitchens (benzene: 4.71 ± 4.27 vs 2.37 ± 2.05 μg/m3, toluene: 1.13 ± 0.91 vs 0.53 ± 0.39 μg/m3, p < 0.05) (Fig. 4). Among the participants, 35% and 65% reported that they had close and open plan kitchens in their houses. Another study also showed that BTEX levels were higher in open plan kitchens compared with closed kitchens [47]. This might be due to free air diffusion from open plan kitchens to other parts of the house [47]. A previous study showed that cooking habits increased the risk of carcinogenicity in humans by increasing the rate of exposure to potentially hazardous substances released from oil such as benzene [71, 72]. In another study, BTEX levels were reported to be equal in the living room and the kitchen [73], which indicated the impact of the kitchen on other areas of the house, especially the living room (sampling area of the present study).Using household cleaning products such as liquid detergent, to remove foreign matter from surfaces and floors of kitchen can be a potential source of more benzene and toluene emissions from the kitchen [74–79].
Fig. 4.
The concentrations of benzene and toluene in the indoor air of different houses (mean values with 95% CI)
In the present study, toluene level was significantly higher in buildings with wooden/MDF cabinets compared with those with metal cabinets (1.24 ± 1.01 vs 0.71 ± 0.95 μg/m3, Mann-Whitney U test (p < 0.05)) (Fig. 4). Previous studies have also referred to cabinets as a source of VOCs emissions [80]. In addition, the results of other published papers showed that wood-based products, such as panels, wood-based composites, laminated office furniture, laminated flooring, and cabinets, could be a source of VOCs compounds [80]. Since toluene is commonly used in Original Equipment Manufacturer (OEM) product coatings such as those for wood furniture and kitchen cabinets, thus wooden kitchen cabinets have been considered as a potential source of toluene emissions by the Environmental Protection Agency [81].
The relationship between the concentrations of BTX compounds and WTS characteristics
Spearman’s rank correlation coefficient was employed to determine the correlations between BTX compounds. The relationship between benzene-toluene (0.788**), benzene-xylenes (0.785**), and toluene-xylenes (0.785**) were statistically significant. There was no significant relationship between the concentrations of BTX in the indoor air of the case houses and type of tobacco. Although previous studies revealed that the concentrations of BTEX compounds emitted from fruit tobacco were significantly higher compared with traditional tobacco [27], no such relationship was found in the present investigation, which might be due to the high prevalence of traditional tobacco consumption in the study area.
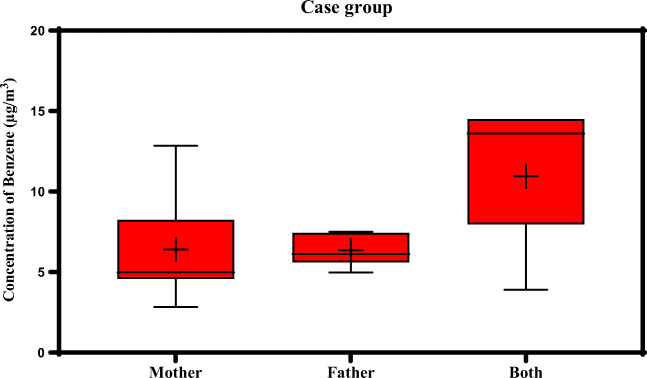
According to the data obtained from the questionnaires, 18%, 44%, and 38% of the children in the case houses had only hookah smoker mothers, only hookah smoker fathers, and both smoker parents, respectively. Although benzene measured in the indoor air of the case houses was not related to the type of tobacco, it was related to the number of hookah users (0.347*) [mothers (6.4 ± 3.05 μg/m3), fathers (6.35 ± 0.91 μg/m3), and both parents (10.95 ± 3.99 μg /m3)] (Fig. 5).
Fig. 5.
The relationship between benzene and number of water pipe users at the case houses
Health risk assessment
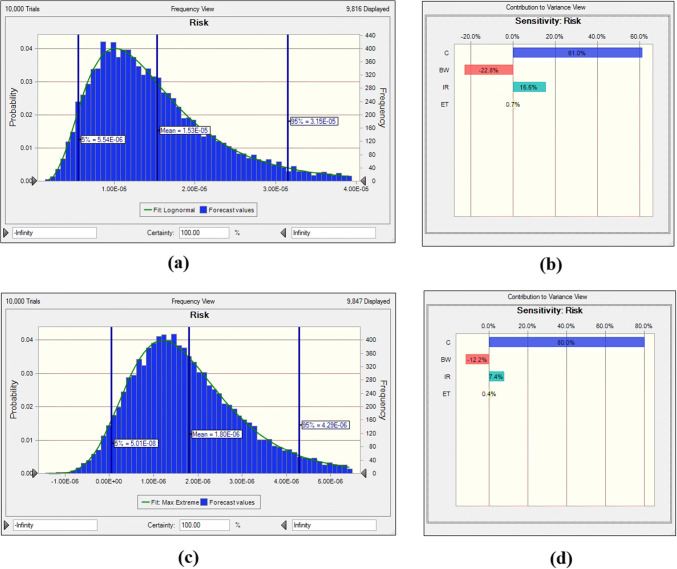
In present study, mean ILCR for benzene in the houses with water pipe smokers was 15 × 10−6 (Fig. 6), which is dramatically higher than the standard limit set by USEPA and WHO (1 × 10−6). This implied a significant risk for children with water pipe using parents [82]. Furthermore, mean ILCR for benzene in the control group was 1.8 × 10−6 (Fig. 6), which is 1.8 times higher than the limits recommended by WHO and USEPA [82]. In several studies performed in cafes in Iran where WTS was not prohibited, the cancer risk obtained for benzene exceeded the acceptable risk value of 1 × 10−6. The amount of ILCR for benzene was 4314 × 10−6 in cafes in Tehran (average concentration of benzene: 4.96 ± 2.96 mg/m3) [27] and 529 × 10−6 in cafes in Hamedan (6.45 ± 0.37 mg/m3) [83], which were much higher than ILCR and average benzene concentration in the present study. This difference could be due to several reasons. First, type of tobacco, since the type of tobacco is a very important factor in the release of BTEX compounds. Concentrations of BTEX compounds emitted from fruit tobacco were significantly higher in comparison with traditional tobacco in cafes of Tehran [27]. In the present study, however, type of tobacco was not associated with BTX emissions in the case group houses. This may be due to lower consumption of fruit tobacco in the case houses (16%). Second, in cafes, several hookahs are used simultaneously during the day. In the houses under the present study, however, most parents smoked hookah only three times a day (66%). Another reason for higher BTEX levels in the indoor air of cafes compared with houses might be the frequent cooking in cafes as well as the vicinity of cafes to main and high traffic streets, which are the sources of BTEX compounds emissions [84]. All the aforementioned items are significant reasons for the high concentrations of BTEX compounds in cafes allowing WTS as compared with the present study. In a recent study, increased cancer risk due to exposure to residential benzene was reported as 1.8 × 10−6 and 80 × 10−6 in dwellings with non-smoking and smoking residents in Hong Kong, respectively [52]. The estimated cancer risk in the case houses in the present study was lower than that reported in other houses with smokers. This might be due to the differences in the parameters used in the risk assessment, including concentrations of the pollutants, duration of exposure, inhalation rate, body weight, and unit risk [47]. Groups at higher risk for BTEX were infants, children, and housewives because they spent most of their time at home, and prolonged exposure to benzene increased the risk of leukemia [49, 85].
Fig. 6.
The carcinogenic risk and sensitivity analysis of benzene in the case (a and b) and control (c and d) groups
The results of HQs of BTX compounds for children aged 7–13 years in the case and control groups are presented in Table 7. Accordingly, HQs of all BTX compounds were < 1 (p < 0.05). By definition, HQ >1 and HQ <1 show potentially dangerous effects, and acceptable non-carcinogenic status following exposure to pollution, respectively [86]. Thus, in the present study, the non-carcinogenic risk of BTX compounds was negligible, and these compounds did not threaten children in terms of non-carcinogenic disorders.
Table 7.
The results of the non-carcinogenic risk assessment of BTX
| Contaminant | Mean ± SD | Minimum | Maximum | |||
|---|---|---|---|---|---|---|
| Cases | Controls | Cases | Controls | Cases | Controls | |
| Benzene | 0.2 ± 0.1 | 0.02 ± 0.01 | 0.07 | 1E-03 | 0.4 | 0.04 |
| Toluene | 1E-04 ± 2E-04 | 3E-05 ± 5E-05 | 4E-05 | 4E-06 | 4E-04 | 1E-04 |
| Xylenes | 0.01 ± 0.02 | 2E-03 ± 3E-03 | 8E-03 | 6E-05 | 0.05 | 6E-03 |
The results of sensitivity analysis for the case and control groups are presented in Fig. 6. The contribution of each parameter to the amount obtained from the ILCR value is also shown as percentage in Fig. 6. The results of sensitivity analysis revealed that the concentration of benzene had the most significant positive effect in the case and control groups, followed by body weight (negative effect) and inhalation rate (positive effect). These results strongly recommend that reductions in the concentration of benzene in indoor air would produce the largest reduction in the ILCR estimates, with considerable benefits to children health by lowering the risk of cancer incidence.
Conclusion
The study findings show that children with hookah smoking parents are exposed to benzene, toluene, and xylenes at their houses. Benzene concentration in the indoor air of the houses with hookah smokers exceeded the safe limits recommended by EPA and Iran environmental protection organization (5 μg/m3). The concentrations of BTX compounds in cases were more than the control group, with the maximum difference estimated for xylenes (p < 0.05). Also, inhalation-ILCR values of benzene for children in the case and control houses were 15 and 1.8 times higher than the standard limit set by USEPA, respectively. This could be considered a potential indoor source of BTX exposure for the children with smoker parents. Although, there was no correlation between concentrations of BTX and type of tobacco in case group, concentration of benzene in indoor air with more hookah smokers were significantly higher than houses with lower smokers. Number of floors of the houses was one of the factors affecting the concentrations of BTX compounds in the present study which declares that natural ventilation such as opening windows during smoking might help to diminish BTX in the indoor air of residential buildings. Open kitchen also played a major role in increasing the emissions of benzene and toluene. In addition, the amount of toluene in the air of the houses with cabinets and doors made of wood (MDF and fiberglass) was higher compared with the houses with metal cabinets and doors.
To the best of our knowledge, although this is the first study to evaluate the risk of BTX compounds in indoor air for children exposed to hookah smoke, this study has limitations to be considered in future studies. It is very important to pay attention to other age groups such as fetuses and prenatal exposure in people. Moreover, other carcinogenic compounds, such as PAHs, aldehydes, and naphthylamines, in the indoor air of houses with hookah smokers are suggested to be measured in future studies. Also, paying attention to the concentrations of BTEX compounds in the outdoor air is another important parameter transferred to indoor environments through ventilation.
Acknowledgements
This article was extracted from the thesis written by Zeynab Tabatabaei, MSc student of Environmental Health engineering. The present work was financially supported by the Vice-chancellor for Research and Technology, Shiraz University of Medical Sciences (proposal No.19458).
Declarations
Conflict of interest
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tsakas MP, Siskos AP, Siskos PA. Indoor air pollutants and the impact on human health. Chem, Emission Cont Radioactive Pollut Indoor Air Qual. 2011:447–84.2011.
- 2.Rostami R, Fazlzadeh M, Babaei-Pouya A, Abazari M, Rastgho L, Ghasemi R, et al. Exposure to BTEX concentration and the related health risk assessment in printing and copying centers. Environmental Science and Pollution Research. 2021:1–12.2021. [DOI] [PubMed]
- 3.Moradi M, Hopke P, Hadei M, Eslami A, Rastkari N, Naghdali Z, et al. Exposure to BTEX in beauty salons: biomonitoring, urinary excretion, clinical symptoms, and health risk assessments. Environ Monit Assess. 2019;191(5):1–10.2019. doi: 10.1007/s10661-019-7455-7. [DOI] [PubMed] [Google Scholar]
- 4.Tabatabaei Z, Baghapour MA, Hoseini M, Shamsedini N. Carcinogenic and non-carcinogenic risk assessment of exposure of housewives to volatile organic compounds (benzene, toluene, ethylbenzene, and xylenes) in the indoor air of houses. J Health Research Commun. 2021;6(4):51–62.2021. [Google Scholar]
- 5.Amoatey P, Omidvarborna H, Baawain MS, Al-Mamun A. Indoor air pollution and exposure assessment of the gulf cooperation council countries: a critical review. Environ Int. 2018;121:491–506.2018. doi: 10.1016/j.envint.2018.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tabatabaei Z, Rafiee A, Abbasi A, Mehdizadeh A, Morovati R, Hoseini M. Investigation of fungal contamination in indoor air and on surfaces of traditional public baths in a historical city. J Environ Health Sci Eng. 2020;18(2):925–32.2020. doi: 10.1007/s40201-020-00516-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernstein JA, Alexis N, Bacchus H, Bernstein IL, Fritz P, Horner E, Li N, Mason S, Nel A, Oullette J, Reijula K, Reponen T, Seltzer J, Smith A, Tarlo SM. The health effects of nonindustrial indoor air pollution. J Allergy Clin Immunol. 2008;121(3):585–91.2008. doi: 10.1016/j.jaci.2007.10.045. [DOI] [PubMed] [Google Scholar]
- 8.Miri M, Alahabadi A, Ehrampoush MH, Ghaffari HR, Sakhvidi MJZ, Eskandari M, Rad A, Lotfi MH, Sheikhha MH. Environmental determinants of polycyclic aromatic hydrocarbons exposure at home, at kindergartens and during a commute. Environ Int. 2018;118:266–73.2018. doi: 10.1016/j.envint.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. 2010;39(3):834–57.2010. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- 10.Naddafi K, Nabizadeh R, Rostami R, Ghaffari HR, Fazlzadeh M. Formaldehyde and acetaldehyde in the indoor air of waterpipe cafés: measuring exposures and assessing health effects. Build Environ. 2019;165:106392.2019. doi: 10.1016/j.buildenv.2019.106392. [DOI] [Google Scholar]
- 11.Rostami R, Zarei A, Saranjam B, Ghaffari HR, Hazrati S, Poureshg Y, Fazlzadeh M. Exposure and risk assessment of PAHs in indoor air of waterpipe cafés in Ardebil, Iran. Build Environ. 2019;155:47–57.2019. [Google Scholar]
- 12.Fazlzadeh M, Rostami R, Hazrati S, Rastgu A. Concentrations of carbon monoxide in indoor and outdoor air of Ghalyun cafes. Atmos Pollut Res. 2015;6(4):550–5.2015. [Google Scholar]
- 13.Rostami R, Kalan ME, Ghaffari HR, Saranjam B, Ward KD, Ghobadi H, et al. Characteristics and health risk assessment of heavy metals in indoor air of waterpipe cafés. Build Environ. 2021;190:107557.2021. [Google Scholar]
- 14.Maziak W, Taleb ZB, Jawad M, Afifi R, Nakkash R, Akl EA, et al. Consensus statement on assessment of waterpipe smoking in epidemiological studies. Tob Control. 2017;26(3):338–43.2017. doi: 10.1136/tobaccocontrol-2016-052958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leavens EL, Driskill LM, Molina N, Eissenberg T, Shihadeh A, Brett EI, Floyd E, Wagener TL. Comparison of a preferred versus non-preferred waterpipe tobacco flavour: subjective experience, smoking behaviour and toxicant exposure. Tob Control. 2018;27(3):319–24.2018. doi: 10.1136/tobaccocontrol-2016-053344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar SR, Davies S, Weitzman M, Sherman S. A review of air quality, biological indicators and health effects of second-hand waterpipe smoke exposure. Tob Control. 2015;24(Suppl 1):i54–i9.2015. doi: 10.1136/tobaccocontrol-2014-052038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Zaatari ZM, Chami HA, Zaatari GS. Health effects associated with waterpipe smoking. Tob Control. 2015;24(Suppl 1):i31–i43.2015. doi: 10.1136/tobaccocontrol-2014-051908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou S, Behrooz L, Weitzman M, Pan G, Vilcassim R, Mirowsky JE, Breysee P, Rule A, Gordon T. Secondhand hookah smoke: an occupational hazard for hookah bar employees. Tob Control. 2017;26(1):40–5.2017. doi: 10.1136/tobaccocontrol-2015-052505. [DOI] [PubMed] [Google Scholar]
- 19.Hoseini M, Yunesian M, Nabizadeh R, Yaghmaeian K, Parmy S, Gharibi H, Faridi S, Hasanvand MS, Ahmadkhaniha R, Rastkari N, Mirzaei N, Naddafi K. Biomonitoring of tobacco smoke exposure and self-reported smoking status among general population of Tehran, Iran. Environ Sci Pollut Res. 2016;23(24):25065–73.2016. doi: 10.1007/s11356-016-7619-8. [DOI] [PubMed] [Google Scholar]
- 20.Weitzman M, Yusufali AH, Bali F, Vilcassim MR, Gandhi S, Peltier R, et al. Effects of hookah smoking on indoor air quality in homes. Tob Control. 2017;26(5):586–91.2017. doi: 10.1136/tobaccocontrol-2016-053165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maziak W, Taleb ZB, Bahelah R, Islam F, Jaber R, Auf R, Salloum RG. The global epidemiology of waterpipe smoking. Tob Control. 2015;24(Suppl 1):i3–i12.2015. doi: 10.1136/tobaccocontrol-2014-051903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davil MF, Naddafi K, Rostami R, Zarei A, Feizizadeh M. A mathematical model for predicting 24-h variations of BTEX concentrations in ambient air of Tehran. Intl J Environ Health Eng. 2013;2(1):4.2013. [Google Scholar]
- 23.Kitwattanavong M, Prueksasit T, Morknoy D, Tunsaringkarn T, Siriwong W. Health risk assessment of petrol station workers in the inner city of Bangkok, Thailand, to the exposure to BTEX and carbonyl compounds by inhalation. Human Ecol Risk Assess Intl J. 2013;19(6):1424–39.2013. [Google Scholar]
- 24.Kim YM, Harrad S, Harrison RM. Concentrations and sources of VOCs in urban domestic and public microenvironments. Environ Sci Technol. 2001;35(6):997–1004.2001. doi: 10.1021/es000192y. [DOI] [PubMed] [Google Scholar]
- 25.El-Hashemy MA, Ali HM. Characterization of BTEX group of VOCs and inhalation risks in indoor microenvironments at small enterprises. Sci Total Environ. 2018;645:974–83.2018. doi: 10.1016/j.scitotenv.2018.07.157. [DOI] [PubMed] [Google Scholar]
- 26.Masekameni MD, Moolla R, Gulumian M, Brouwer D. Risk assessment of benzene, toluene, ethyl benzene, and xylene concentrations from the combustion of coal in a controlled laboratory environment. Int J Environ Res Public Health. 2019;16(1):95.2019. doi: 10.3390/ijerph16010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hazrati S, Rostami R, Fazlzadeh M. BTEX in indoor air of waterpipe cafés: levels and factors influencing their concentrations. Sci Total Environ. 2015;524:347–53.2015. doi: 10.1016/j.scitotenv.2015.04.031. [DOI] [PubMed] [Google Scholar]
- 28.Sakai N, Yamamoto S, Matsui Y, Khan MF, Latif MT, Mohd MA, et al. Characterization and source profiling of volatile organic compounds in indoor air of private residences in Selangor state, Malaysia. Sci Total Environ. 2017;586:1279–86.2017. doi: 10.1016/j.scitotenv.2017.02.139. [DOI] [PubMed] [Google Scholar]
- 29.Schubert J, Müller FD, Schmidt R, Luch A, Schulz TG. Waterpipe smoke: source of toxic and carcinogenic VOCs, phenols and heavy metals? Arch Toxicol. 2015;89(11):2129–39.2015. doi: 10.1007/s00204-014-1372-x. [DOI] [PubMed] [Google Scholar]
- 30.Rafiee A, Delgado-Saborit JM, Sly PD, Amiri H, Hoseini M. Lifestyle and occupational factors affecting exposure to BTEX in municipal solid waste composting facility workers. Sci Total Environ. 2019;656:540–6.2019. doi: 10.1016/j.scitotenv.2018.11.398. [DOI] [PubMed] [Google Scholar]
- 31.Masih A, Lall AS, Taneja A, Singhvi R. Inhalation exposure and related health risks of BTEX in ambient air at different microenvironments of a terai zone in North India. Atmos Environ. 2016;147:55–66.2016. [Google Scholar]
- 32.Smith MT. Advances in understanding benzene health effects and susceptibility. Annu Rev Public Health. 2010;31:133–48.2010. doi: 10.1146/annurev.publhealth.012809.103646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jafari AJ, Faridi S, Momeniha F. Temporal variations of atmospheric benzene and its health effects in Tehran megacity (2010-2013) Environ Sci Pollut Res. 2019;26(17):17214–23.2019. doi: 10.1007/s11356-019-05086-1. [DOI] [PubMed] [Google Scholar]
- 34.Cancer IAfRo. Agents classified by the IARC monographs, vol 1–100. http://monographs iarc fr/ENG/Classification/ClassificationsAlphaOrder pdf. 2010.2010.
- 35.Rafiee A, Delgado-Saborit JM, Gordi E, Quémerais B, Moghadam VK, Lu W, et al. Use of urinary biomarkers to characterize occupational exposure to BTEX in healthcare waste autoclave operators. Sci Total Environ. 2018;631:857–65.2018. doi: 10.1016/j.scitotenv.2018.03.090. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization. Regional Office for E. WHO guidelines for indoor air quality: selected pollutants. Copenhagen: World Health Organization. Regional Office for Europe; 2010 2010.
- 37.Iepo I. Clean Air Standard 2012.2012.
- 38.Fromme H, Debiak M, Sagunski H, Röhl C, Kraft M, Kolossa-Gehring M. The German approach to regulate indoor air contaminants. Int J Hyg Environ Health. 2019;222(3):347–54.2019. doi: 10.1016/j.ijheh.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 39.Heydari G, Ranjbar Vakilabadi D, Kermani M, Rayani M, Poureshgh Y, Behroozi M, Fanaei F, Arfaeinia H. Load characteristics and inhalation risk assessment of benzene series (BTEX) pollutant in indoor air of Ghalyan and/or cigarette cafes compared to smoking-free cafes. Environ Pollut Bioavail. 2020;32(1):26–35.2020. [Google Scholar]
- 40.Masjedi MR, Taghizadeh F, Hamzehali S, Ghaffari S, Fazlzadeh M, Jafari AJ, et al. Air pollutants associated with smoking in indoor/outdoor of waterpipe cafés in Tehran, Iran: concentrations, affecting factors and health risk assessment. Sci Rep. 2019;9(1):1–11.2019. doi: 10.1038/s41598-019-39684-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Samarghandi M, Mehralipour J, Shabanlo A, Rahimpoor R. The evaluation of personal exposure to BTEX compounds in the traditional restaurants in Hamadan in 2013. Avicenna J Clin Med. 2014;21(3):231–9.2014. [Google Scholar]
- 42.Kassem NO, Kassem NO, Liles S, Reilly E, Kas-Petrus F, Posis AIB, et al. Waterpipe device cleaning practices and disposal of waste associated with waterpipe tobacco smoking in homes in the USA. Tob Control. 2020;29(Suppl 2):s123–s30.2020. doi: 10.1136/tobaccocontrol-2019-054959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Buka I, Koranteng S, Osornio-Vargas AR. The effects of air pollution on the health of children. Paediatr Child Health. 2006;11(8):513–6.2006. [PMC free article] [PubMed] [Google Scholar]
- 44.Faridi S, Naddafi K, Kashani H, Nabizadeh R, Alimohammadi M, Momeniha F, et al. Bioaerosol exposure and circulating biomarkers in a panel of elderly subjects and healthy young adults. Sci Total Environ. 2017;593:380–9.2017. doi: 10.1016/j.scitotenv.2017.03.186. [DOI] [PubMed] [Google Scholar]
- 45.Adamović D, Dorić J, Vojinović-Miloradov M. BTEX in the exhaust emissions of motor vehicles. Causes, Impacts and Solutions to Global Warming: Springer; 2013. p. 333–42.
- 46.Dehghani MH, Baghani AN, Fazlzadeh M, Ghaffari HR. Exposure and risk assessment of BTEX in indoor air of gyms in Tehran, Iran. Microchem J. 2019;150:104135.2019. [Google Scholar]
- 47.Hazrati S, Rostami R, Farjaminezhad M, Fazlzadeh M. Preliminary assessment of BTEX concentrations in indoor air of residential buildings and atmospheric ambient air in Ardabil, Iran. Atmos Environ. 2016;132:91–7.2016. [Google Scholar]
- 48.Shrivastava A, Gupta VB. Methods for the determination of limit of detection and limit of quantitation of the analytical methods. Chron Young Sci. 2011;2(1):21.2011. [Google Scholar]
- 49.Organization WH. WHO guidelines for indoor air quality: selected pollutants. 2010.2010. [PubMed]
- 50.Majumdar D, Mukherjeea A, Sen S. BTEX in ambient air of a Metropolitan City. J Environ Prot. 2011;2(01):11.2011. [Google Scholar]
- 51.Baghani AN, Rostami R, Arfaeinia H, Hazrati S, Fazlzadeh M, Delikhoon M. BTEX in indoor air of beauty salons: risk assessment, levels and factors influencing their concentrations. Ecotoxicol Environ Saf. 2018;159:102–8.2018. doi: 10.1016/j.ecoenv.2018.04.044. [DOI] [PubMed] [Google Scholar]
- 52.Gao H, Lee S, Chan L, Li W. Risk assessment of exposure to volatile organic compounds in different indoor environment. Environ Res. 2004;94(1):57–66.2004. doi: 10.1016/s0013-9351(03)00035-5. [DOI] [PubMed] [Google Scholar]
- 53.Heavner DL, Morgan WT, Ogden MW. Determination of volatile organic compounds and ETS apportionment in 49 homes. Environ Int. 1995;21(1):3–21.1995. [Google Scholar]
- 54.Wallace LA. Major sources of benzene exposure. Environ Health Perspect. 1989;82:165–9.1989. doi: 10.1289/ehp.8982165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fromme H. Gesundheitliche Bedeutung der verkehrsbedingten Benzolbelastung der allgemeinen Bevölkerung. Zentralbl Hyg Umweltmed. 1995;196(6):481–94.1995. [PubMed] [Google Scholar]
- 56.Carrer P, Maroni M, Alcini D, Cavallo D, Fustinoni S, Lovato L, et al. Assessment through environmental and biological measurements of total daily exposure to volatile organic compounds of office workers in Milan, Italy. Indoor Air. 2000;10(4):258–68.2000. doi: 10.1034/j.1600-0668.2000.010004258.x. [DOI] [PubMed] [Google Scholar]
- 57.Centre HIAQI. Indoor air quality certification scheme for offices and public places. Government of the Hong Kong Special Administrative Region China; 2003.
- 58.Fowles J, Dybing E. Application of toxicological risk assessment principles to the chemical constituents of cigarette smoke. Tob Control. 2003;12(4):424–30.2003. doi: 10.1136/tc.12.4.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.ATSDR A. Toxicological profile for toluene. USDoHaH Services, editor Atlanta: US Public Health Service 2000:1–357.2000.
- 60.Fay M, Risher J, Wilson JD. Toxicological profile for xylene 2007.2007.
- 61.Guo H, Lee S, Li W, Cao J. Source characterization of BTEX in indoor microenvironments in Hong Kong. Atmos Environ. 2003;37(1):73–82.2003. [Google Scholar]
- 62.Lee JY, Kim K, Ryu SH, Kim CH, Bae G-N. The relative importance of indoor and outdoor sources for determining indoor pollution concentrations in homes in Seoul, South Korea. Asian J Atmos Environ. 2018;12(2):127–38.2018. [Google Scholar]
- 63.Du Z, Mo J, Zhang Y, Xu Q. Benzene, toluene and xylenes in newly renovated homes and associated health risk in Guangzhou, China. Build Environ. 2014;72:75–81.2014. [Google Scholar]
- 64.Lee SC, Li W-M, Ao C-H. Investigation of indoor air quality at residential homes in Hong Kong—case study. Atmos Environ. 2002;36(2):225–37.2002. [Google Scholar]
- 65.Uchiyama S, Tomizawa T, Tokoro A, Aoki M, Hishiki M, Yamada T, Tanaka R, Sakamoto H, Yoshida T, Bekki K, Inaba Y, Nakagome H, Kunugita N. Gaseous chemical compounds in indoor and outdoor air of 602 houses throughout Japan in winter and summer. Environ Res. 2015;137:364–72.2015. doi: 10.1016/j.envres.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 66.Serrano-Trespalacios PI, Ryan L, Spengler JD. Ambient, indoor and personal exposure relationships of volatile organic compounds in Mexico City metropolitan area. J Exposure Sci Environ Epidemiol. 2004;14(1):S118–S32.2004. doi: 10.1038/sj.jea.7500366. [DOI] [PubMed] [Google Scholar]
- 67.Esplugues A, Ballester F, Estarlich M, Llop S, Fuentes-Leonarte V, Mantilla E, Iñiguez C. Indoor and outdoor air concentrations of BTEX and determinants in a cohort of one-year old children in Valencia, Spain. Sci Total Environ. 2010;409(1):63–9.2010. doi: 10.1016/j.scitotenv.2010.09.039. [DOI] [PubMed] [Google Scholar]
- 68.Truc VTQ, Oanh NTK. Roadside BTEX and other gaseous air pollutants in relation to emission sources. Atmos Environ. 2007;41(36):7685–97.2007. [Google Scholar]
- 69.Spengler JD, Chen Q. Indoor air quality factors in designing a healthy building. Annu Rev Energy Environ. 2000;25(1):567–600.2000. [Google Scholar]
- 70.Wong NH, Huang B. Comparative study of the indoor air quality of naturally ventilated and air-conditioned bedrooms of residential buildings in Singapore. Build Environ. 2004;39(9):1115–23.2004. [Google Scholar]
- 71.Chiang T-A, Wu P-F, Wang L-F, Lee H, Lee C-H, Ko Y-C. Mutagenicity and polycyclic aromatic hydrocarbon content of fumes from heated cooking oils produced in Taiwan. Mutation Res/Fundamental Mol Mech Mutagenesis. 1997;381(2):157–61.1997. doi: 10.1016/s0027-5107(97)00163-2. [DOI] [PubMed] [Google Scholar]
- 72.Chiang TA, Wu PF, Ko YC. Prevention of exposure to mutagenic fumes produced by hot cooking oil in Taiwanese kitchens. Environ Mol Mutagen. 1998;31(1):92–6.1998. [PubMed] [Google Scholar]
- 73.Schneider P, Loerinci G, Gebefuegi IL, Heinrich J, Kettrup A, Wichmann H-E. Vertical and horizontal variability of volatile organic compounds in homes in eastern Germany. J Exposure Sci Environ Epidemiol. 1999;9(4):282–92.1999. doi: 10.1038/sj.jea.7500030. [DOI] [PubMed] [Google Scholar]
- 74.Wallace LA, Pellizzari E, Leaderer B, Zelon H, Sheldon L. Emissions of volatile organic compounds from building materials and consumer products. Atmos Environ (1967) 1987;21(2):385–393. [Google Scholar]
- 75.Sack TM, Steele DH, Hammerstrom K, Remmers J. A survey of household products for volatile organic compounds. Atmos Environ Part A. 1992;26(6):1063–70.1992. [Google Scholar]
- 76.Akland G, Whitaker D, Sheldon L. Characterizing the sources of human exposure to proposition 65 substances. Epidemiology. 1998;9(4):S106.1998. [Google Scholar]
- 77.Nazaroff WW, Weschler CJ. Cleaning products and air fresheners: exposure to primary and secondary air pollutants. Atmos Environ. 2004;38(18):2841–65.2004. [Google Scholar]
- 78.Cerón Bretón JG, Cerón Bretón RM, Martínez Morales S, Kahl JD, Guarnaccia C, Lara Severino RDC, et al. Health Risk Assessment of the Levels of BTEX in Ambient Air of One Urban Site Located in Leon, Guanajuato, Mexico during Two Climatic Seasons. Atmosphere. 2020;11(2):165.2020.
- 79.Martins EM, de Sá Borba PF, dos Santos NE, dos Reis PTB, Silveira RS, Corrêa SM. The relationship between solvent use and BTEX concentrations in occupational environments. Environ Monit Assess. 2016;188(11):608.2016. doi: 10.1007/s10661-016-5621-8. [DOI] [PubMed] [Google Scholar]
- 80.Ho DX, Kim K-H, Ryeul Sohn J, Hee Oh Y, Ahn J-W. Emission rates of volatile organic compounds released from newly produced household furniture products using a large-scale chamber testing method. TheScientificWorldJournal. 2011;11(2011):1597–1622. doi: 10.1100/2011/650624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Beauregard D, Branch EI. Locating and estimating air emissions from sources of toluene. US Environ Protect Agency 1993.1993.
- 82.Miri M, Shendi MRA, Ghaffari HR, Aval HE, Ahmadi E, Taban E, et al. Investigation of outdoor BTEX: concentration, variations, sources, spatial distribution, and risk assessment. Chemosphere. 2016;163:601–9.2016. doi: 10.1016/j.chemosphere.2016.07.088. [DOI] [PubMed] [Google Scholar]
- 83.Mehralipour J, Samarghandi MR, Rahimpoor R. Evaluation of exposure to BTEX in hookah smokers and carcinogenic and non-carcinogenic risk assessment. Iranian J Health Safety Environ. 2018;5(4):1128–31.2018. [Google Scholar]
- 84.Buczynska AJ, Krata A, Stranger M, Godoi AFL, Kontozova-Deutsch V, Bencs L, et al. Atmospheric BTEX-concentrations in an area with intensive street traffic. Atmos Environ. 2009;43(2):311–8.2009. [Google Scholar]
- 85.Pyatt D, Hays S. A review of the potential association between childhood leukemia and benzene. Chem Biol Interact. 2010;184(1–2):151–64.2010. doi: 10.1016/j.cbi.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 86.Abbasi F, Pasalari H, Delgado-Saborit JM, Rafiee A, Abbasi A, Hoseini M. Characterization and risk assessment of BTEX in ambient air of a middle Eastern City. Process Saf Environ Prot. 2020;2020.