Abstract
Oral traumatic neuromas (TrNs) are relatively rare lesions and they originate from a damaged nerve. They present a diagnostic challenge, due to the complex clinical features that may mimic odontogenic, musculoskeletal, and other neuropathic pain conditions. We describe an interesting and challenging case of painful bilateral intraoral lesions in a 56-year-old South Indian female patient who presented with clinical features consistent with TrN lesions bilaterally, in relation to different branches of the trigeminal nerve. The patient had undergone numerous aggressive dental treatments and interventions over the past three decades, with little or no pain relief. Topical treatment with lidocaine gel utilizing a custom-made neurosensory stent rendered the patient significant and sustained pain relief.
Keywords: Neuropathic pain, neurosensory stent, oral, Tinel's Sign, topical medication, traumatic neuroma, trigeminal nerve
INTRODUCTION
Traumatic neuroma (TrN) is broadly defined as a nonneoplastic condition secondary to trauma (surgical or incidental), characterized histopathologically by the presence of proliferating nerve fibers, inflammatory cells, and fibroblasts in a dense matrix of connective tissue. It is a lesion that results from an attempted repair by a damaged nerve.[1] It has been suggested that, a combination of nerve repair, contraction, and scarring of the wound as part of the healing process, and the accompanying neuronal proliferation contributes to the formation of TrN.[1,2] The prevalence of oral TrN approximately 0.3%, making it a rare entity. The most common sites for a TrN in the head-and-neck region include the inferior alveolar nerve, lingual nerve, and the greater auricular nerve. Consistent with prior publications, this case exemplifies TrN of the terminal branch of V2 and V3 divisions of the trigeminal nerve.[3] However, the occurrence of two anatomically independent lesions in the same patient (left and right sides and differing branches of the trigeminal nerve) is a unique feature of this case that is largely inconsistent with the established TrN literature.
CASE REPORT
Chief complaints
A 56-year-old South Indian female, presented with chief complaints of pain intraorally, on the buccal gingiva in relation to the maxillary left molar (chief complaint 1) and mandibular right molar teeth (chief complaint 2). The pain on the two sites had independent origin and were not temporally related to each other.
History of presenting illness
She revealed that the pain, though slow in onset, had been consistent over the past 28 years. A dull aching pain was initially present only over the upper left molar region which radiated to the eyebrows, temple, and preauricular and postauricular regions on that side. A similar pain started on the lower right molar area 1–2 years later, which radiated to the preauricular and neck region on that side. Both these complaints had started subsequent to minor dental/surgical procedures in the local area of affliction. Chief complaint 1 started following a periodontal curettage in the maxillary left first molar tooth, while chief complaint 2 started following a restoration in mandibular right first molar. In both areas, the patient had continuous background pain of 3–4 intensity that exacerbated while chewing to 7–8 out of 10 on a 0–10 Visual Analog Scale. The background pain was “dull aching” and the exacerbated pain was “pulsating” and “shooting.” For both complaints, the patient underwent various conservative and aggressive dental procedures over the last 30 years in an attempt to obtain pain relief but with no measurable relief of pain. The treatments included, but not limited to, multiple periodontal therapies, restorative treatments, endodontic therapy and eventually extraction of teeth in that region. She was also placed on multiple medications by “specialists,” which included carbamazepine (titrated dose), acetaminophen, gabapentin, nortriptyline, Vitamin B12, and clonazepam. The medications did not render any pain relief over a period of approximately 4 years, even after continued increase/titration of the doses within pharmacologically acceptable levels.
She reported a medical history of Type II diabetes mellitus and dyslipidemia, currently under control with medications. There was no family history of orofacial pain/TMD. Although she stated that she did not sleep well, pain did not wake her up from sleep nor did she get up in the morning with pain. Her psychosocial history revealed that she was under stress now due to the long duration of the problem with no pain relief. She also did not report any habits like bruxism.
Clinical examination
Extraoral, cranial nerve and TMJ examination were within the normal limits. Relevant muscle palpation in the head-and-neck region did not elicit any tender points. Cervical screening also did not reveal any abnormality.
Intraoral examination revealed evidence of multiple dental/restorative procedures performed on the upper left and lower right quadrants. There were no clinically identifiable signs and symptoms of inflammation or a visually discernible lesion. The pain was not reproduced from the hard tissue structures.
Radiographic examination did not reveal any pathology.
Diagnostic tests
Intraoral triggers for the pain were identified. The trigger areas were localized to approximately 3 mm × 3 mm embedded in the buccal oral mucosa in relation to maxillary left first molar and mandibular right second molar teeth [Figure 1]. Positive Tinel's sign (please see discussion below) was elicited in the mandibular right buccal area. The patient's familiar pain was reproduced by firm localized palpation of the trigger areas. Topical anesthetic application with 5% lidocaine gel reduced the pain approximately 20%–30%, and subsequent local anesthetic infiltration peri-lesionally, abolished the chief complaint of pain.
Figure 1.

Localization and marking of the TrN lesions. (a and c) Pressure with cotton bud identifying a 3X3mm area on the mucobuccal fold and gingiva, (b and d) Site of the lesions marked with dye
Differential diagnosis
The differential diagnoses of this type of localized reproducible neuropathic pain include trigeminal neuralgia (TN), painful post traumatic trigeminal neuropathy (PTTN), and trigeminal TrN. The clinical features of reproducibility of pain from percussion/local pressure, rather than by light touch (characteristic of TN); and the fact that there was a lack of refractory period, points the diagnosis in the direction of trigeminal TrN. Conceivably, TrN although not officially classified, has similar features described in the literature with those of PTTN.
Investigations
An magnetic resonance imaging of the brain/brain stem (with and without gadolinium contrast) did not reveal any neurovascular conflict with regard to the left and the right trigeminal nerve or any space-occupying lesions.
Diagnosis
The diagnosis in this case was TrN of the buccal gingiva in relation to maxillary left first molar and mandibular right second molar.
Management
A thermoformed plastic neuropathic stent was fabricated for the topical anesthetic (5% lidocaine) to be retained locally not to exceed 3–4 h per application at the site of the TrN lesion [Figure 2]. The patient was advised and demonstrated the application of the topical anesthetic gel, with instructions to use twice daily. The patient had weekly re-evaluation visits for approximately 2 months. The pain reduced continuously over this period, and at the 3 months re-evaluation visit, the chief complaints related to the TrN locations had completely disappeared. The prognosis of oral TrN is fair to good with these conservative modalities.
Figure 2.
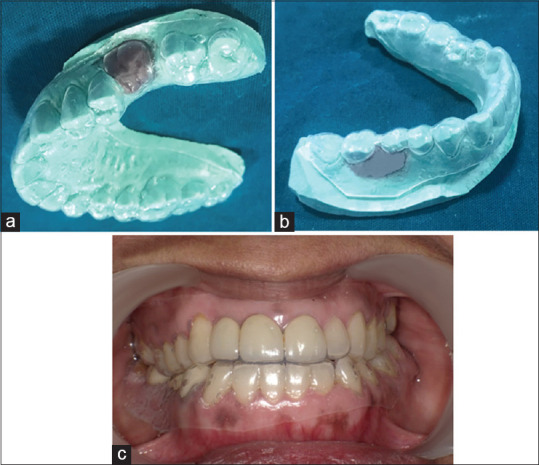
Fabrication of the neurosensory stent. (a and b) Thermoplastic stents with spacer in position, on the maxillary and mandibular casts, (c) The maxillary and mandibular neurosensory stents with topical lidocaine gel seated in the patient's mouth
DISCUSSION
In the head-and-neck region, similar to the other regions of the body, TrN can clinically manifest with a variety of features, often confusing the clinician. Dental procedures have been implicated in the etiology of oral TrN, with extraction of teeth being most common.[4] There are isolated reports of oral TrNs secondary to overextended dental prosthesis.[5] The onset of the symptoms of TrN has been described as starting relatively immediately after the traumatic event, or up to weeks or months after the event.[6] This is consistent with this patient also. The lack of pain relief subsequent to multiple dental treatments, observed in this case, is part of published literature. The spread of the pain in this patient's case goes along with previous scientific publications of pain in the distribution of the affected nerve.[7] The continuous nature of the background pain in this particular case is also in agreement with past literature.[8] The intensity of the background pain of approximately five to six (moderate) on a numerical pain scale of zero to ten is consistent with the literature for oral and extraoral sites of TrN.[9] The seven out of ten pain (severe) for the exacerbated episodes is also consistent with much of the published articles.[9,10] The size of the TrN lesion in this case as elicited clinically is consistent with the literature on oral TrN.[11] Reproduction of patient's familiar pain from the local TrN lesion is one of the clinical methods to confirm the location of the lesion. One of the classic features of TrN appearing in the literature is Tinel's sign, generally described as pain/tingling in the distribution of the nerve, upon percussion of the lesion.[12] However, in the head and neck sites including the intraoral locations, the exact identification of the lesion (especially a small one) can be relatively difficult. In the symptomatic oral TrN cases, the cardinal symptom is pain, both provoked and unprovoked. Sensory changes associated with surgical procedures such as implant placement have been reported.[13] When these changes manifest, the possibility of them being caused by a TrN lesion should be ruled out. The clinical features of TrN reported in the literature are varied and contrasting, and largely depends on the location of the TrN, and the nerve afflicted. Modest reduction in pain on topical anesthetic application and abolishing of the pain on local anesthetic injection are also consistent with existing TrN literature.[14] The overall management of TrN can be subdivided as conservative (medical and adjunct) and surgical. Under medical management, pharmacotherapy seems to be the most preferred method. The medications used for management include tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, calcium channel blockers, and topical anaesthetics.[15,16] Excision of the TrN alone runs the risk of recurrence at the proximal end of the resected nerve, although it offers relatively short-term pain relief.[17,18] In the oral cavity, such a resection could also have the risk of the cut end of the nerve being deeper than the original TrN site, thereby rendering any new TrN formation inaccessible to further therapy. Topical medications employed successfully include local anaesthetic preparations, topical steroids, and neuropathic paste.[19] Lidocaine has been traditionally used successfully in the alleviation of neuropathic pain in general, including TrN pain.[19,20] The use of a custom made acrylic stent or a similar method to deliver the medication locally to the area affected by TrN, is a known practice in intraoral neuropathic pain management.[21,22]
CONCLUSION
TrNs are essentially reparative lesions occurring as a result of trauma, and are not true neoplasms. Although relatively rare, oral TrNs are one of the more prevalent entities in the class of head and neck TrNs. These lesions present a significant diagnostic challenge to the clinician. Occurrence of TrN bilaterally is an extremely rare not reported in the literature. A comprehensive history taking and a thorough clinical examination of the affected tissues are paramount in aiding an appropriate prompt diagnosis. Topical medications such as lidocaine gel can help in achieving measurable pain relief, thereby drastically improving the patient's quality of life. Education of clinicians in general and dental practitioners and pain management specialists in particular is crucial to avoid misdiagnosis and prevent unnecessary, irreversible aggressive treatment and suffering for the patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ulivieri S, Muscas G, Miracco C, Oliveri G, Galluzzi P, Giorgio A. Unusual case of traumatic neuroma of the orbit. Orbit. 2016;35:62–5. doi: 10.3109/01676830.2015.1099703. [DOI] [PubMed] [Google Scholar]
- 2.Foltán R, Klíma K, Spacková J, Sedý J. Mechanism of traumatic neuroma development. Med Hypotheses. 2008;71:572–6. doi: 10.1016/j.mehy.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Eguchi T, Ishida R, Ara H, Hamada Y, Kanai I. A diffuse traumatic neuroma in the palate: A case report. J Med Case Rep. 2016;10:116. doi: 10.1186/s13256-016-0908-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peszkowski MJ, Larsson A. Extraosseous and intraosseous oral traumatic neuromas and their association with tooth extraction. J Oral Maxillofac Surg. 1990;48:963–7. doi: 10.1016/0278-2391(90)90010-y. [DOI] [PubMed] [Google Scholar]
- 5.Lopes MA, Vargas PA, Almeida OP, Takahama A, León JE. Oral traumatic neuroma with mature ganglion cells: A case report and review of the literature. J Oral Maxillofac Pathol. 2009;13:67–9. doi: 10.4103/0973-029X.57672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valverde Guevara YM, Yoshikawa H, Saito I, Maeda T, Seo K. Effect of local application of an antibody against brain-derived neurotrophic factor on neuroma formation after transection of the inferior alveolar nerve in the rat. Neuroreport. 2014;25:1069–74. doi: 10.1097/WNR.0000000000000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chau MN, Jönsson E, Lee KM. Traumatic neuroma following sagittal mandibular osteotomy. Int J Oral Maxillofac Surg. 1989;18:95–8. doi: 10.1016/s0901-5027(89)80139-0. [DOI] [PubMed] [Google Scholar]
- 8.Salemis NS. Traumatic neuroma as a rare cause of intractable neuropathic breast pain following cancer surgery: Management and review of the literature. Intractable Rare Dis Res. 2018;7:185–90. doi: 10.5582/irdr.2018.01041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rasmussen OC. Painful traumatic neuromas in the oral cavity. Oral Surg Oral Med Oral Pathol. 1980;49:191–5. doi: 10.1016/0030-4220(80)90043-2. [DOI] [PubMed] [Google Scholar]
- 10.Sist TC, Jr, Greene GW. Traumatic neuroma of the oral cavity. Report of thirty-one new cases and review of the literature. Oral Surg Oral Med Oral Pathol. 1981;51:394–402. doi: 10.1016/0030-4220(81)90149-3. [DOI] [PubMed] [Google Scholar]
- 11.Jham BC, Costa NL, Batista AC, Mendonça EF. Traumatic neuroma of the mandible: A case report with spontaneous remission. J Clin Exp Dent. 2014;6:e317–20. doi: 10.4317/jced.51659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neumeister MW, Winters JN. Neuroma. Clin Plast Surg. 2020;47:279–83. doi: 10.1016/j.cps.2019.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Padmanabhan H, Kumar AV, Shivashankar K. Incidence of neurosensory disturbance in mandibular implant surgery – A meta-analysis. J Indian Prosthodont Soc. 2020;20:17–26. doi: 10.4103/jips.jips_373_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jain S, Mannan K. The diagnosis and management of Morton's neuroma: A literature review. Foot Ankle Spec. 2013;6:307–17. doi: 10.1177/1938640013493464. [DOI] [PubMed] [Google Scholar]
- 15.Khan J. Neuropathic pain. J Indian Prosthodont Soc. 2016;16:114–5. doi: 10.4103/0972-4052.179317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mendell JR, Sahenk Z. Clinical practice. Painful sensory neuropathy. N Engl J Med. 2003;348:1243–55. doi: 10.1056/NEJMcp022282. [DOI] [PubMed] [Google Scholar]
- 17.Ngamsom S, Nakamura S, Kabasawa Y, Harada H, Tohyama R, Kurabayashi T. Imaging findings of intraosseous traumatic neuroma of the mandible. Oral Radiol. 2018;34:257–61. doi: 10.1007/s11282-017-0286-8. [DOI] [PubMed] [Google Scholar]
- 18.Kang J, Yang P, Zang Q, He X. Traumatic neuroma of the superficial peroneal nerve in a patient: A case report and review of the literature. World J Surg Oncol. 2016;14:242. doi: 10.1186/s12957-016-0990-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sommer C, Cruccu G. Topical treatment of peripheral neuropathic pain: Applying the evidence. J Pain Symptom Manage. 2017;53:614–29. doi: 10.1016/j.jpainsymman.2016.09.015. [DOI] [PubMed] [Google Scholar]
- 20.Derry S, Wiffen PJ, Moore RA, Quinlan J. Topical lidocaine for neuropathic pain in adults. Cochrane Database Syst Rev. 2014;2014:CD010958. doi: 10.1002/14651858.CD010958.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pickering G, Martin E, Tiberghien F, Delorme C, Mick G. Localized neuropathic pain: An expert consensus on local treatments. Drug Des Devel Ther. 2017;11:2709–18. doi: 10.2147/DDDT.S142630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khawaja N, Yilmaz Z, Renton T. Case studies illustrating the management of trigeminal neuropathic pain using topical 5% lidocaine plasters. Br J Pain. 2013;7:107–13. doi: 10.1177/2049463713483459. [DOI] [PMC free article] [PubMed] [Google Scholar]


