Abstract
Using fluorescent in situ hybridization (FISH) with rRNA-targeted fluorescently labelled oligonucleotide probes, pathogens were rapidly detected and identified in positive blood culture bottles without cultivation and biotyping. In this study, 115 blood cultures with a positive growth index as determined by a continuous-reading automated blood culture system were examined by both conventional laboratory methods and FISH. For this purpose, oligonucleotide probes that allowed identification of approximately 95% of those pathogens typically associated with bacteremia were produced. The sensitivity and specificity of these probes were 100%. From all 115 blood cultures, microorganisms were grown after 1 day and identification to the family, genus, or species level was achieved after 1 to 3 days while 111 samples (96.5%) were similarly identified by FISH within 2.5 h. Staphylococci were identified in 62 of 62 samples, streptococci and enterococci were identified in 19 of 20 samples, gram-negative rods were identified in 28 of 30 samples, and fungi were identified in two of two samples. Thus, FISH is an appropriate method for identification of pathogens grown in blood cultures from septicemic patients.
The sepsis syndrome is one of the leading causes of death in hospitalized patients (7, 28). The mortality rate of septicemic patients varies between 30 and 70% and depends on several factors, including pathogen and host factors (13, 31, 32). The vast majority (>90%) of cases of bacteremia are caused by a limited number of pathogens, including Staphylococcus spp., Streptococcus spp., Enterococcus spp., Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Candida spp. (30, 35, 36).
Rapid identification of the causative pathogen in septicemia is crucial for several reasons. In light of the identified microorganism, usually grown in blood cultures, (i) appropriate antimicrobial agents can be selected, and thus, unnecessary treatment of typical contaminants can be avoided; (ii) improved susceptibility to antibiotics may be achieved; (iii) the prognosis of the patients with septicemia may be improved; and (iv) expenditures on antimicrobials can be decreased (20, 25, 27, 32, 34).
Standard laboratory detection of bacteremia is usually done by continuous-reading, automated, and computed blood culture systems by monitoring the CO2 production of microorganisms in blood culture bottles (30, 35). If the microcomputer flags bottles as positive, gram stain examination is performed followed by subculture on agars. Thus, species identification can usually be achieved 1 or 2 days after detection of microbial growth by the continuous-monitoring blood culture systems (13).
Methods used for direct identification of microorganisms growing in blood culture bottles include commercial immunologic kits (4, 19) and inoculation of biochemical identification kits (22). However, both antigenic and biochemical variations, as well as the presence of more than one microbial species, such as in polymicrobial infections, may give rise to misinterpretation of data.
Numerous studies have demonstrated the value of molecular techniques, including PCR and hybridization, for amplification and detection of microbial DNA or RNA in order to identify bacteria or fungi in clinical specimens (3, 6, 11, 12, 14, 21, 23, 24, 37). However, PCR techniques are time-consuming and expensive. In situ hybridization with rRNA-targeted fluorescently labelled oligonucleotides has been reported to be a reasonable and rapid method for detection and identification of pathogens (2, 15, 16, 18, 26; K. Trebesius, L. Leitritz, K. Adler, S. Schubert, I. B. Autenrieth, and J. Heeseman, submitted for publication).
The aim of this study was to evaluate the practicability, sensitivity, and specificity of fluorescent in situ hybridization (FISH) for identification of microorganisms grown in blood culture specimens.
MATERIALS AND METHODS
Blood cultures.
Aerobic and anaerobic blood culture bottles (Bactec Plus culture vial aerobic/anaerobic; Becton Dickinson, Heidelberg, Germany) were inoculated with blood from patients with suspected septicemia and placed bottom down into the wells of the data unit of a BACTEC 9240 blood culture system (Becton Dickinson), a continuous-reading, automated, and computed blood culture system that detects the growth of microorganisms by monitoring CO2 production. Incubation was performed according to the manufacturer's recommendations at 35°C. Bottles with a positive growth index were removed from the data units, and an aliquot of the blood culture suspension was taken aseptically with a needle syringe. The aliquot was divided, with one part for gram stain examinations, one part for subculture on agar plates, and one part for FISH. The organisms grown on agar plates were identified by standard laboratory methods (13), including biotyping (e.g., catalase test, slide coagulase test, bile solubility test, cytochrome oxidase test, API 20E strip, API Staph Strip, API Strep Strip, and API 20NE strip [bio Merieux, Nuertingen, Germany]) and serotyping.
Microbial reference strains.
The following microorganisms (bacteria and fungi) were purchased from the American Type Culture Collection (ATCC; Manassas, Va.) or Deutsche Sammlung von Mikroorganismen und Zellkulturen (Braunschweig, Germany) and were used for evaluation of the specificity of oligonucleotide probes: Staphylococcus aureus (ATCC 25923, 25423, 29213, and 33862 and DSM 346), Staphylococcus epidermidis (ATCC 12228 and 14990), Staphylococcus cohnii (ATCC 35662), Staphylococcus haemolyticus (DSM 20264), Staphylococcus sciuri (DSM 20345), Staphylococcus schleiferi (DSM 4807 and 6628), Candida albicans (ATCC 90028 and DSM 1386), Candida glabrata (ATCC 90030), Candida krusei (ATCC 6258), Candida parapsilosis (DSM 70125), Bacteroides fragilis (ATCC 25285 and DSM 1396), Citrobacter freundii (ATCC 6750 and 8090), E. coli (ATCC 25922 and 35218 and DSM 682), P. aeruginosa (ATCC 27853 and 10145), Stenotrophomonas maltophilia (ATCC 13637 and DSM 50170), Enterobacter aerogenes (ATCC 13048), Enterobacter cloacae (ATCC 13047), Klebsiella oxytoca (clinical isolate), K. pneumoniae (DSM 3104), Proteus mirabilis (ATCC 43071), Proteus vulgaris (clinical isolate), Streptococcus pneumoniae (DSM 20566), Enterococcus faecalis (ATCC 29212), Enterococcus faecium (ATCC 29213), Streptococcus agalactiae (DSM 2134), Streptococcus pyogenes (ATCC 19615, DSM 20565, and DSM 2071), Streptococcus mutans (ATCC 35668 and DSM 20662), Streptococcus salivarius (DSM 20560), and Propionibacterium propionicus (DSM 43307).
FISH.
In situ hybridization of bacteria on glass slides was performed as previously described by Amann et al. (1) with the following modifications. Briefly, for each hybridization reaction, 10 to 15 μl per positive blood culture suspension was dropped on a glass slide and air dried. Oligonucleotide probes used for this study were synthesized and 5′ labelled (Metabion, Munich, Germany) with the fluorochrome Cy3 (red signal) or fluorescein isothiocyanate (FITC; green signal). Depending on the result from the Gram stain examination, a selected set of oligonucleotide probes was used for each sample. In addition, universal eubacterial (1) and universal yeast probes were used for hybridization of each sample in order to detect pathogens not included in the described set of species- or genus-specific probes used in this study. A selected number of the above-mentioned control cells (bacteria and fungi) were used for specificity evaluation of each probe as described previously (26). In brief, bacterial control cells were grown in Luria-Bertani broth and harvested while in exponential growth phase. The cells were centrifuged and fixed with paraformaldehyde or ethanol and stored at −20°C as previously described (1).
FISH was essentially performed as described recently (26; Trebesius et al., submitted). Blood culture samples containing gram-negative bacteria or fungi were incubated in ethanol (sequentially in 50, 80, and 100% ethanol for 5 min each). Streptococci were incubated with lysozyme (Sigma, Deisenhofen, Germany) (1 mg/ml for 10 min at 30°C), and staphylococci were incubated with lysozyme (1 mg/ml for 10 min at 30°C) followed by lysostaphin (Sigma) (1 mg/ml for 5 min at 30°C), each dissolved in 10 mM Tris (pH 8.0). Thereafter, the slides were washed and 5 ng of each oligonucleotide was added in 10 μl of hybridization buffer containing 20% formamide (40% for the Streptococcus genus-specific probe).
The species-, group-, or family-specific probes labelled with Cy3 dye were applied simultaneously with probe EUB338-FITC, complementary to a portion of 16S rRNA found in all Bacteria (1). Aliquots of all samples were tested in parallel with the irrelevant control probe NON338-Cy3, complementary to EUB338, in order to control nonspecific binding of the probes (1). Alternatively, the samples were stained with DAPI (4′,6′-diamidino-2-phenylindole), which detects DNA of bacteria, fungi, and host cells as described previously (26; Trebesius et al., submitted). In the case of yeasts, 18S rRNA-targeted probes were generated and a universal probe that is specific for all yeasts was used simultaneously.
Citifluor (Citifluor Ltd., London, United Kingdom) was used as a mounting medium on hybridized slides. Finally, the slides were analyzed with a Leitz DM RBE microscope (Leica Microsystems, Wetzlar, Germany) equipped with a standard filter set. Two different fluorochromes could be detected simultaneously. Microscopy was done blind by two independent investigators.
RESULTS
Prevalence of microorganisms in a total of 7,998 blood cultures.
In order to design a set of oligonucleotide probes that would allow specific identification of approximately 95% of the microorganisms recovered by blood cultures from bacteremic patients, the prevalence of microorganisms isolated by blood culture from patients of a university hospital in Munich in 1996 and 1997 was evaluated. Of a total of 7,998 blood cultures, 1,128 (14.1%) were flagged positive by BACTEC 9240. The microorganisms grown from these samples are shown in Table 1. Comparable results have been reported by others (27, 30, 35, 36).
TABLE 1.
Prevalence of bacteria and fungi in blood cultures from patients at a University Hospital in Munich in 1996 and 1997
| Species | Prevalence (%)a
|
|
|---|---|---|
| 1996b | 1997c | |
| Coagulase-negative staphylococci | 33.7 | 36.3 |
| S. aureus | 14.7 | 13.7 |
| Enterobacteriaceaed | 16.5 | 16.1 |
| E. coli | 9.6 | 10.6 |
| K. pneumoniae | 2.4 | 2.7 |
| P. aeruginosa | 3.2 | 1.4 |
| S. maltophilia | 0.3 | 6.5 |
| C. albicans | 2.8 | 3.5 |
| C. glabrata | 0.8 | 0.4 |
| C. parapsilosis | 0.5 | 0.6 |
| S. pneumoniae | 3.7 | 1.6 |
| Enterococci | 6.0 | 5.3 |
| Group A streptococci (S. pyogenes) | 0.8 | 1.6 |
| Group B streptococci (S. agalactiae) | 0.6 | 1.6 |
| Group C streptococci | 7.8 | 5.5 |
| Total | 91.4 | 94.1 |
The numbers shown are related to positive blood cultures defined as 100%.
Blood cultures without microbial growth, n = 3,878; blood cultures with microbial growth, n = 618.
Blood cultures without microbial growth, n = 2,992; blood cultures with microbial growth, n = 510.
Including the species E. coli and K. pneumoniae.
Evaluation of probe specificity.
According to these data, a set of fluorescently labelled 16S, 18S, or 23S rRNA-targeted oligonucleotide probes that would cover specific identification of approximately 95% of microorganisms was developed (Table 2). A set of bacterial and yeasts reference strains (see Materials and Methods) was used in order to establish the specificities of these probes. Each probe was tested by FISH for specificity, including the respective target strain as well as related microbial species. All probes turned out to be highly specific and hybridized to the respective target species, genus, and family only and not to related bacterial species, genera, or families. The results for yeasts, staphylococci, and gram-negative rods are depicted in Fig. 1.
TABLE 2.
Oligonucleotide used for FISH of blood cultures according to the result obtained by Gram stain examinationa
| Gram stain examination results | Probe | Sequence (5′-3′) | Target | rRNA positionb | Reference |
|---|---|---|---|---|---|
| Gram-positive cocci (clusters) | Sta | TCC TCC ATA TCT CTG CGC | Staphylococcus spp. | 16/697 | Trebesius et al., submitted |
| Sau | GAA GCA AGC TTC TCG TCC G | S. aureus | 16/69 | This workc | |
| Gram-positive cocci (chains and pairs) | Efs | CCC CTT CTG ATG GGC AGG | E. faecalis | 23/129 | 8 |
| Enc | CCC TCT GAT GGG TAG GTT | Enterococcus spp. | 23/131 | 8 | |
| Str | CAC TCT CCC CTT CTG CAC | Streptococcus spp. | 16/665 | Trebesius et al., submitted | |
| Spn | GTG ATG CAA GTG CAC CTT | S. pneumoniae | 16/195 | This work | |
| Spy | TTC CAA AGC GTA CAT TGG TT | S. pyogenes | 16/620 | Trebesius et al., submitted | |
| Saga | GTA AAC ACC AAA CMT CAG CG | S. agalactiae | 16/67 | Trebesius et al., submitted | |
| Gram-negative rods | Psae | TCT CGG CCT TGA AAC CCC | P. aeruginosa | 23/1506 | Trebesius et al., submitted |
| Ent | CCC CCW CTT TGG TCT TGC | Enterobacteriaceaed | 16/186 | This work | |
| Kpn | CCT ACA CAC CAG CGT GCC | K. pneumoniae | 23/1707 | This work | |
| Sma | GTC GTC CAG TAT CCA CTG T | S. maltophilia | 16/633 | M. Hogardt, K. Trebesius, J. Rosenecker, and J. Heesemann, submitted for publication | |
| Yeasts | Caal | GCC AAG GCT TAT ACT CGC T | C. albicans | 18/1249 | This work |
| Cagl | CCG CCA AGC CAC AAG GAC T | C. glabrata | 18/651 | This work | |
| Ckrus | GAT TCT CGG CCC CAT GGG | C. krusei | 18/1433 | This work | |
| Cpara | CCT GGT TCG CCA AAA AGG C | C. parapsilosis | 18/651 | This work | |
| Controls | Eub | GCT GCC TCC CGT AGG AGT | Eubacteria | 16/338 | 1, 2 |
| PF2 | CTC TGG CTT CAC CCT ATT C | All yeasts | 18/618 | This work | |
| NonEub388 | CGA CGG AGG GCA TCC TCA | Nonee | None | 1, 2 |
For FISH, oligonucleotides were labelled with the fluorochrome Cy-3 or FITC.
First number, type of rRNA (16S, 18S, or 23S); second number, target sequence position of first base of each oligonucleotide.
A comparative analysis of almost 10,000 complete or almost-complete 16S, 18S, or 23S rRNA sequences performed with the ARB software was used to develop oligonucleotide probes for FISH (Trebesius et al, submitted).
Except Proteus spp.
Probe NonEub338, complementary to Eub338, was used to detect nonspecific binding of the oligonucleotides to microorganisms.
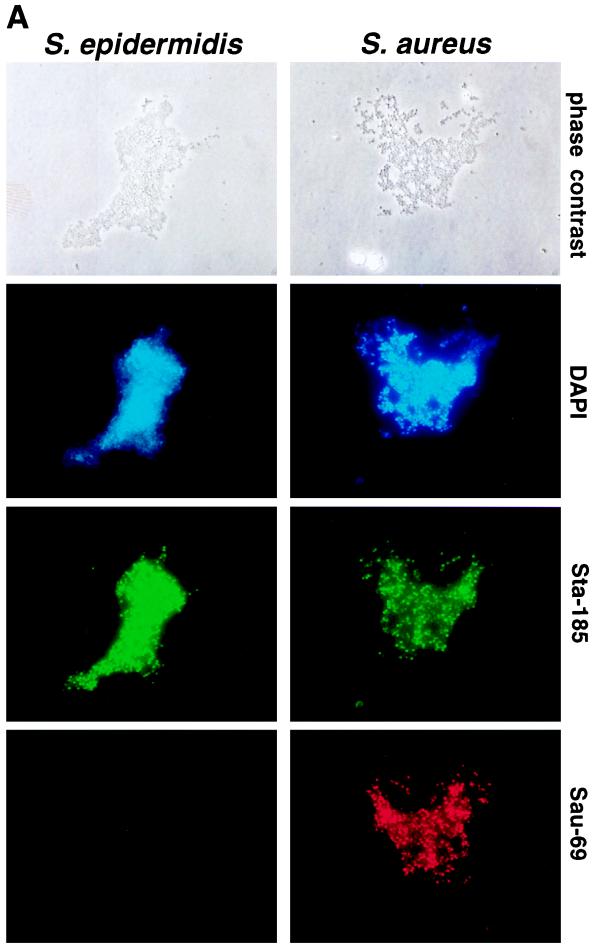
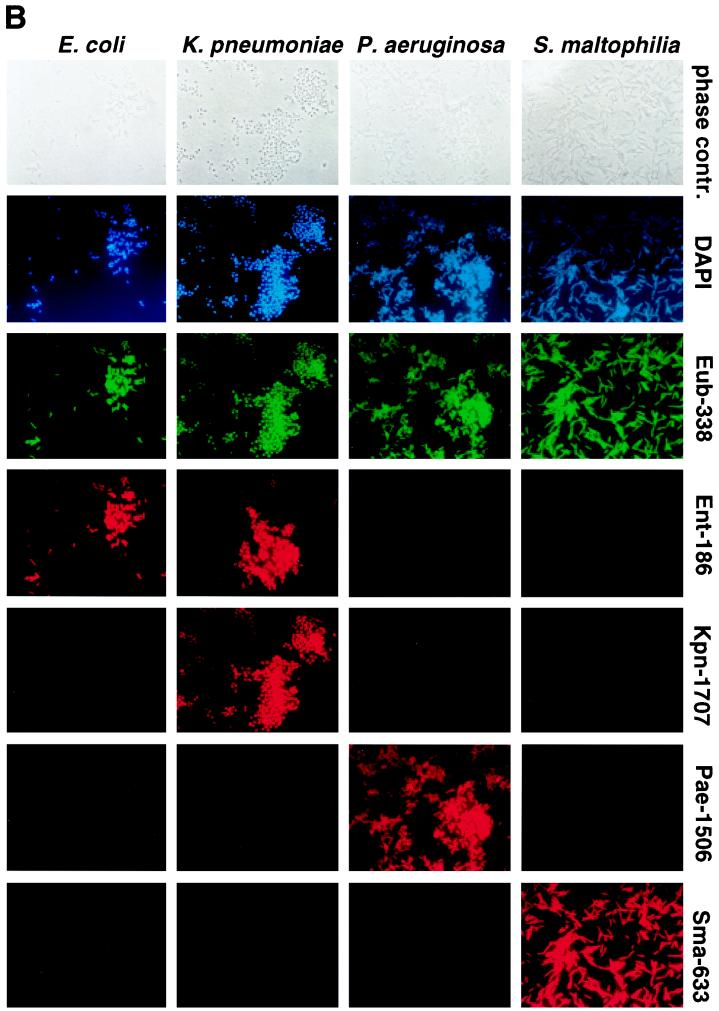
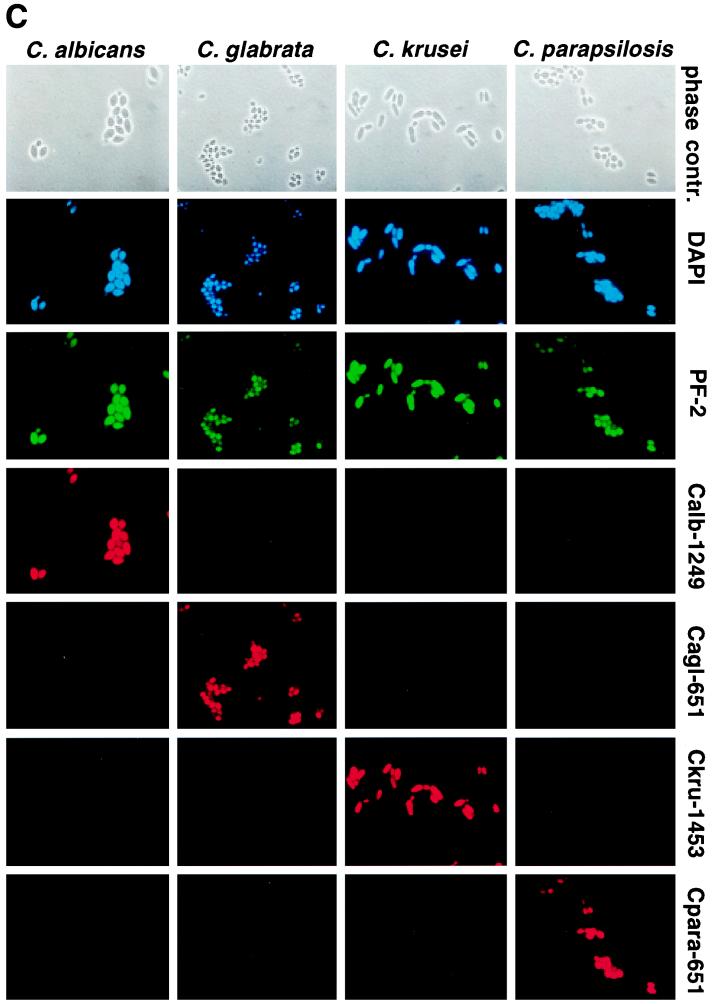
FIG. 1.
Fluorescence microscopy of microorganisms after FISH with various oligonucleotide probes. (A) S. epidermidis (left) and S. aureus (right) were stained with DAPI (blue signal; staining of DNA) following FISH with probes Sta-185-FITC (green signal; specific for all staphylococci) and Sau-69-Cy3 (red signal; specific for S. aureus). (B) E. coli, K. pneumoniae, P. aeruginosa, and S. maltophilia (vertical columns) were stained with DAPI (blue signal; staining of DNA) following FISH with probes Eub-338-FITC (green signal; specific for all Eubacteria) and Ent-186 (specific for all Enterobacteriaceae), Kpn-1707 (specific for K. pneumoniae), Pae-1506 (specific for P. aeruginosa), and Sma-633 (specific for S. maltophilia), each Cy3-labelled (red signal). (C) C. albicans, C. glabrata, C. krusei, and C. parapsilosis (vertical columns) were stained with DAPI (blue signal; staining of DNA) following FISH with probes PF-2-FITC (green signal; specific for all yeasts) and Calb-1249 (specific for C. albicans), Cagl-651 (specific for C. glabrata), Ckru-1453 (specific for C. krusei), and Cpara-651 (specific for C. parapsilosis), each Cy3 labelled (red signal).
By this means, coagulase-positive S. aureus could be segregated from coagulase-negative staphylococci by comparing the hybridization results for probe Sta-185-FITC (specific for all staphylococci) and probe Sau-69-Cy3 (specific for S. aureus) (Fig. 1A). A probe specific for all coagulase-negative staphylococci could not be designed on the basis of conserved 16S rRNA sequences.
In the case of gram-negative bacteria, probes specific for all Enterobacteriaceae, K. pneumoniae, P. aeruginosa, or S. maltophilia were used for FISH and allowed the segregation of P. aeruginosa from, e.g., Enterobacteriaceae (Fig. 1B). A probe specific for E. coli could not be designed on the basis of 16S rRNA sequences.
When yeasts were detected by Gram stain examination, probes specific for C. albicans, C. glabrata, C. krusei, and C. parapsilosis, in addition to universal yeast-specific probe that hybridized to all yeasts, were used for FISH and proved to be highly specific (Fig. 1C). From these data we can conclude that the specificity of FISH with the probes described here was 100%. Furthermore, by using a nonsense oligonucleotide (nonEub388-Cy3), nonspecific binding of the probes to microorganisms was excluded (not shown).
Subsequently, FISH was performed with all blood cultures that revealed a positive growth index of microorganisms as determined by a continuous-reading blood culture system. According to the results obtained by Gram stain examination, a selected set of probes was used for FISH of each sample (Table 2).
Detection and identification of microorganisms in blood cultures by FISH.
Microorganisms (bacteria and fungi) could be detected by FISH in all of the 115 positive blood culture specimens with universal eubacterial and universal yeast probes, which resulted in a sensitivity of 100% compared with conventional Gram stain examination and culture (Table 3). Microscopic sensitivity testing with serially diluted bacterial suspensions revealed a limit of detection by FISH at 103 microorganisms per ml of blood-broth mixture (data not shown).
TABLE 3.
Results of examination of blood cultures with positive growth indices by Gram stain, FISH, and culturea
| Gram stain examination results
|
FISH results
|
Culture results
|
|||
|---|---|---|---|---|---|
| Morphology | n | Oligonucleotide | n | Genus or species | n |
| Gram-positive cocci (clusters) | 62 | Eubacteria | 62 | Eubacteria | 62 |
| Controlb | 0 | ||||
| Staphylococcus spp. | 62 | Staphylococcus spp. | 62 | ||
| Non-S. aureus | 41 | Coagulase-negative Staphylococcic | 41 | ||
| S. aureus | 21 | S. aureus | 21 | ||
| Gram-positive cocci (chains and pairs) | 20 | Eubacteria | 20 | Eubacteria | 20 |
| Control | 0 | ||||
| Streptococcus spp. | 19 | Streptococcus spp. | 19 | ||
| S. pyogenes | 0 | S. pyogenes | 0 | ||
| S. agalactiae | 0 | S. agalactiae | 0 | ||
| Enterococcus spp. | 8 | Enterococcus spp. | 8 | ||
| S. pneumoniae | 7 | S. pneumoniae | 7 | ||
| Viridans group streptococcid | 4 | ||||
| Not identified | 1 | L. lactis | 1 | ||
| Gram-negative rods | 30 | Eubacteria | 30 | Eubacteria | 30 |
| Control | 0 | ||||
| Enterobacteriacea | 23 | Enterobacteriaceae | 23e | ||
| K. pneumoniae | 2 | K. pneumoniae | 2 | ||
| P. aeruginosa | 3 | P. aeruginosa | 3 | ||
| S. maltophilia | 0 | S. maltophilia | 0 | ||
| Not identified | 2 | M. osloensis | 1 | ||
| B. fragilis | 1 | ||||
| Yeasts | 2 | All yeasts | 2 | Yeasts | 2 |
| Control | 0 | ||||
| C. albicans | 2 | C. albicans | 2 | ||
| C. glabrata | 0 | C. glabrata | 0 | ||
| C. parapsilosis | 0 | C. parapsilosis | 0 | ||
| C. krusei | 0 | C. krusei | 0 | ||
| Others | 1 | Eubacteria | 1 | Propionibacterium spp. | 1 |
| Control | 0 | ||||
A total of 115 blood culture specimens were analyzed by FISH. Culture was performed on agar plates, and microorganisms were identified by standard laboratory methods (see Materials and Methods).
A nonsense control oligonucleotide was used (see Materials and Methods).
Coagulase-negative staphylocci included S. epidermidis, S. sciuri, S. haemolyticus, S. schleiferi, and S. cohnii.
Viridans group streptococci were identified by binding of the Streptococcus genus probe detecting all streptococci and simultaneous exclusion of S. pyogenes, S. agalactiae, Enterococcus spp., and S. pneumoniae.
Including E. coli, K. pneumoniae, K. oxytoca, C. freundii, E. aerogenes, and E. cloacae.
In 111 (96.5%) samples, the family, genus, or species of the microorganisms could be identified by FISH with the described set of oligonucleotide probes (Tables 2 and 3). In a total of 62 blood culture specimens, gram-positive cocci in clusters were observed by Gram stain examination. By means of FISH with two probes specific for the genus Staphylococcus and for S. aureus, respectively, segregation of S. aureus versus non-S. aureus bacteria could be achieved in all samples (Table 3) within 2.5 h with a time saving of nearly 1 day compared with conventional laboratory identification (Table 4).
TABLE 4.
Results of FISH of 115 blood culture samples
| Microorganisms | No. of samples | No. identifieda | No. not identified | Time saving (h)b |
|---|---|---|---|---|
| Staphylococci | 62 | 62 | 26.3 ± 13.8 | |
| Streptococci | 20 | 19 | 1c | 46 ± 0.0 |
| Gram-negative rods | 30 | 28 | 2d | 39.8 ± 17.8 |
| Fungi | 2 | 2 | 46 ± 0.0 | |
| Othere | 1 | 1e |
Identification of family, genus, or species.
Time required for species or genus identification by FISH compared to that with culture.
L. lactis.
M. osloensis and Bacteroides spp.
Propionibacterium spp.
In a total of 20 blood culture specimens, gram-positive cocci in pairs or chains were observed by microscopy (Table 3). By means of FISH including probes specific for the genus Streptococcus, for Enterococcus spp., and for the species S. pyogenes, S. agalactiae, and S. pneumoniae, the microorganisms could be identified in 19 of these samples within 2.5 h. One or 2 days later, the findings could be confirmed by culture and conventional biotyping and/or serotyping. However, viridans group streptococci were identified on the genus level only, as an appropriate viridans group-specific 16S rRNA sequence does not exist. Moreover, FISH failed to identify the bacteria in one sample. In this sample standard laboratory methods revealed Lactococcus lactis after 2 days. Nevertheless, a probe specific for L. lactis on the basis of 23S rRNA sequences exists (2) and might be used for examination of blood cultures.
In a total of 30 blood culture specimens, gram-negative rods were observed by microscopy (Table 3). By means of FISH including probes specific for Enterobacteriaceae, K. pneumoniae, P. aeruginosa, and S. maltophilia, respectively, microorganisms could be identified on the species level in five samples (K. pneumoniae, n = 2; P. aeruginosa, n = 3) or on the family level (Enterobacteriaceae) in 23 samples within 2.5 h. In the latter samples, E. coli (n = 17), K. oxytoca (n = 3), Enterobacter spp. (n = 2), and Citrobacter sp. (n = 1) were found by conventional methods after 2 to 3 days. Moreover, by means of FISH, polymicrobial septicemia with, e.g., P. aeruginosa and K. pneumoniae, was rapidly identified. However, in two samples that hybridized to a eubacterial probe (Eub338-FITC) only, suggesting the presence of Eubacteria, Moraxella osloensis and B. fragilis were identified by conventional laboratory methods and sequencing of ribosomal DNA.
In two blood culture specimens, yeasts were identified by Gram stain examination. FISH including probes specific for C. albicans, C. glabrata, C. krusei, or C. parapsilosis revealed the presence of C. albicans within 2.5 h. These results could be confirmed by culture and subsequent biotyping several days later.
In one sample, gram-positive rods were observed and identified as Propionibacterium sp. by conventional techniques after 2 days. Due to the low prevalence of this species in blood cultures, no specific probe had been created and included in this study. Thus, these bacteria were detected by a probe specific for Eubacteria only. Nevertheless, a PCR probe specific for Propionibacterium spp. on the basis of 16S rRNA sequences does exist (9) and might be used for examination of blood cultures.
The data summarized in Table 4 show that 111 of 115 (96.5%) blood culture samples could be rapidly identified by FISH. Thus, a time saving of 1 or 2 days can be achieved in order to establish the microbial family, genus, or species which accounts for a positive blood culture.
DISCUSSION
Septicemia is a life-threatening event which requires rapid appropriate therapy. As the outcome for patients with septicemia depends on factors including the septicemia-causing pathogen, rapid microbiological laboratory diagnosis is desirable (13, 31).
In fact, it is well established that a severe infection may proceed to a systemic inflammatory response syndrome that may culminate in septic shock (17, 29, 31). While in the late phase of these events, immunomodulatory therapy, including anti-inflammatory cytokines or cytokine antagonists as well as coagulation inhibitors and antioxidants, is essential for therapy, appropriate antimicrobial therapy is decisive in the early phase (32). Clearly, rapid identification of the sepsis-causing pathogen is a prerequisite for early appropriate antimicrobial treatment.
As conventional laboratory methods require 1 to 3 days before microorganisms grown in blood cultures can be identified, we wanted to evaluate the practicability, sensitivity, and specificity of FISH for identification of microorganisms from blood cultures. For this purpose, a 16S, 18S, and 23S rRNA-based approach was developed, as 16S, 18S, and 23S rRNA have been extensively used to elucidate the phylogenic relationships of bacteria on the inter- and intragenic levels (2). Moreover, 16S rRNA targets have been used successfully for diagnostic PCR and FISH assays (2, 6, 15, 16, 18, 26; Trebesius et al., submitted).
Testing of the specificities of the various oligonucleotide probes revealed that the probes were highly specific; they hybridized to the desired target strain only and not to related microorganisms. By using a set of oligonucleotides that would theoretically allow identification of ca. 95% of the microorganisms most frequently recovered from blood cultures, we were in fact able to identify 111 of 115 microorganisms grown in blood cultures from septicemic patients on the genus and/or species level within ca. 2.5 h after a blood culture was flagged positive by an automated continuous-reading blood culture system. Thus, depending on the group of microorganisms investigated (bacteria, yeasts, etc.), a time saving of 26 to 46 h was achieved by FISH compared with conventional laboratory methods used for identification. Thus, antimicrobial treatment of these patients could be adjusted 1 or 2 days earlier.
This was particularly important when Gram stain examination revealed gram-positive cocci. In that case, we were able to segregate S. aureus from coagulase-negative staphylococci by FISH. Although coagulase-negative staphylococci are the most prevalent bacteria (ca. 35%) in blood cultures, it is well established that in more than 90% of these cases the bacteria are contaminants from the normal skin flora (25). Therefore, if coagulase-negative staphylococci can be identified immediately, unnecessary or inappropriate antimicrobial therapy can be avoided. On the other hand, the S. aureus-specific probe also hybridized to methicillin-resistant S. aureus (two specimens), which was particularly helpful in the screening of patients with known methicillin-resistant S. aureus infections.
In the case of streptococci, the probes included in this study allowed differentiation between, e.g., S. pneumoniae and enterococci. This allowed treatment with penicillin G or ampcillin plus gentamicin, respectively, to be selected earlier. However, a probe specific for E. faecium, which is often resistant to conventional antibiotics, does not exist. Unfortunately, a probe that would hybridize to all viridans group streptococci could not be designed, as this group is phylogenetically heterogeneous. Therefore, using the set of oligonucleotides described herein, it is not possible to segregate viridans group streptococci from other pathogens with similar morphologies, such as Pediococcus or Leuconostoc, although these species occur only rarely in blood cultures (Table 1) (30, 35).
If gram-negative rods were found by Gram stain examination, we were able to distinguish among P. aeruginosa, S. maltophilia, and Enterobacteriaceae. This is also important, as infections caused by the three types of bacteria should be treated with different antimicrobial agents. E. coli is the most frequent gram-negative bacterium recovered from blood cultures (Table 1) (30, 35, 36). However, there is no probe available that is completely specific for E. coli. The most E. coli-specific probe that we have tested was still reactive with Shigella spp. Although Shigella spp. do not play a significant role, if any at all, in patients with septicemia, we have not included this probe in the present study.
Infections with yeasts, e.g., C. albicans, C. glabrata, or C. krusei, could be recognized by the probes selected. This fact might be important for a differential treatment of fungemia. Thus, it is known that, e.g., C. krusei shows intrinsic resistance against fluconazole (20).
The microorganisms grown in four blood culture specimens containing Propionibacterium spp., M. osloensis, Lactococcus lactis, and Bacteroides spp., respectively, could not be identified on the genus level with the set of oligonucleotide probes used in this study. On the other hand, these bacterial species are rarely recovered from blood culture and do not play important roles in septicemia. Nevertheless, it is possible to include oligonucleotide probes specific for, e.g., Bacteroides spp. for FISH of blood cultures (2).
Recently, the direct identification of intestinal bacteria in blood by means of PCR and Southern hybridization has been demonstrated (11, 12). Although this approach was highly sensitive (detection of 10 to 100 microorganisms per 0.3 ml of blood), it may be associated with several problems, including specificity. Thus, if DNA is detected, it is unclear whether it actually represents live invading microorganisms or simply dead presorbed microorganisms, or microorganisms engulfed in and killed by polymorphonuclear leukocytes. Moreover, the method is time-consuming, expensive, and not appropriate for daily routine work (23). FISH, in contrast, is a rapid, cheap, and reliable method.
Similar to our study, direct identification of bacterial isolates in blood cultures by chemiluminescent DNA probes that detect the rRNAs of certain target organisms has been reported previously (5). However, the method used in the present study is easier and more rapid. Similar to the study referenced above, we feel that the costs of FISH may be justified by what might be saved in unnecessary antimicrobial therapy and possibly a shortened hospital stay. Moreover, reduction of unnecessary antimicrobial treatment not only results in a reduction of expenditures for antimicrobials but also in increased antimicrobial susceptibility of the microorganisms accounting for nosocomial infections (33).
In summary, we have demonstrated that FISH is a rapid and reliable method for direct identification and differentiation of bacteria grown in blood cultures. FISH is rapid, cheap (about $20 per positive blood culture specimen), valid, and appropriate for daily routine work. In our institution, one technician is sufficient for performing all necessary examinations. Because of the simple technical protocol, there are no special equipment or facilities required for performing FISH. Nevertheless, ongoing studies in our institution need to elucidate whether an earlier pathogen identification by FISH actually results in earlier appropriate antimicrobial therapy and in a better clinical outcome for the patients.
ACKNOWLEDGMENTS
We thank Bernadette Grohs and Kristin Adler for expert technical assistance.
REFERENCES
- 1.Amann R I, Krumholz L, Stahl D A. Fluorescent-oligonucleotide probing of whole cells for determinative, phylogenetic, and environmental studies in microbiology. J Bacteriol. 1990;172:762–770. doi: 10.1128/jb.172.2.762-770.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amann R I, Ludwig W, Schleifer K H. Phylogenetic identification and in situ detection of individual microbial cells without cultivation. Microbiol Rev. 1995;59:143–169. doi: 10.1128/mr.59.1.143-169.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brakstad O G, Maeland J A. Direct identification of Staphylococcus aureus in blood cultures by detection of the gene encoding the thermostable nuclease or the gene product. APMIS. 1995;103:209–218. doi: 10.1111/j.1699-0463.1995.tb01097.x. [DOI] [PubMed] [Google Scholar]
- 4.Davis T E, Fuller D D, Aeschleman E C. Rapid, direct identification of Staphylococcus aureus and Streptococcus pneumoniae from blood cultures using commercial immunologic kits and modified conventional tests. Diagn Microbiol Infect Dis. 1992;15:295–300. doi: 10.1016/0732-8893(92)90014-k. [DOI] [PubMed] [Google Scholar]
- 5.Davis T E, Fuller D D. Direct identification of bacterial isolates in blood cultures by using a DNA probe. J Clin Microbiol. 1991;29:2193–2196. doi: 10.1128/jcm.29.10.2193-2196.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Einsele H, Hebart H, Roller G, Löffler J, Rothenhöfer I, Müller C A, Bowden R A, van Burik J A, Engelhard D, Kanz Lothar, Schumacher U. Detection and identification of fungal pathogens in blood by using molecular probes. J Clin Microbiol. 1997;35:1353–1360. doi: 10.1128/jcm.35.6.1353-1360.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fauci A S, Harrison T R. Principles of internal medicine. 14th ed. New York, N.Y: McGraw-Hill; 1998. [Google Scholar]
- 8.Frahm E, Heiber I, Hoffman S, Koob C, Meier H, Ludwig W, Amann R, Schleifer K H, Obst U. Application of 23S rDNA-targeted oligonucleotide probes specific for enterococci to water hygiene control. Syst Appl Microbiol. 1998;21:450–453. doi: 10.1016/S0723-2020(98)80055-6. [DOI] [PubMed] [Google Scholar]
- 9.Greisen K, Loeffelholz M, Purohit A, Leong D. PCR primers and probes for the 16S rRNA gene of most species of pathogenic bacteria, including bacteria found in cerebrospinal fluid. J Clin Microbiol. 1994;32:335–351. doi: 10.1128/jcm.32.2.335-351.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herchline T, Gros S. Improving clinical outcome in bacteremia. J Eval Clin Pract. 1998;4:191–195. doi: 10.1046/j.1365-2753.1998.00003.x. [DOI] [PubMed] [Google Scholar]
- 11.Kane T D, Alexander J W, Johannigman J A. The detection of microbial DNA in the blood: a sensitive method for diagnosing bacteremia and/or bacterial translocation in surgical patients. Ann Surg. 1998;227:1–9. doi: 10.1097/00000658-199801000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kane T D, Johnson S R, Alexander J W, Babcock G F, Ogle C K. Detection of intestinal bacterial translocation using PCR. J Surg Res. 1996;63:59–63. doi: 10.1006/jsre.1996.0223. [DOI] [PubMed] [Google Scholar]
- 13.Koneman E W, Allen S D, Janda W M, Schreckenberger P C, Winn W C. Color atlas and textbook of diagnostic microbiology. 5th ed. Philadelphia, Pa: Lippincott-Raven; 1997. [Google Scholar]
- 14.Kulski J K, Pryce T. Preparation of mycobacterial DNA from blood culture fluids by simple alkali wash and heat lysis method for PCR detection. J Clin Microbiol. 1996;34:1985–1991. doi: 10.1128/jcm.34.8.1985-1991.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lischewski A, Amann R I, Harmsen D, Merkert H, Hacker J, Morschhauser J. Specific detection of Candida albicans and Candida tropicalis by fluorescent in situ hybridization with an 18S rRNA-targeted oligonucleotide probe. Microbiology. 1996;142:2731–2740. doi: 10.1099/13500872-142-10-2731. [DOI] [PubMed] [Google Scholar]
- 16.Lischewski A, Kretschmar M, Hof H, Amann R I, Hacker J, Morschhauser J. Detection and identification of Candida species in experimentally infected tissue and human blood by rRNA-specific fluorescent in situ hybridization. J Clin Microbiol. 1997;35:2943–2948. doi: 10.1128/jcm.35.11.2943-2948.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lynn W A, Cohen J. Adjunctive therapy for septic shock: a review of experimental approaches. Clin Infect Dis. 1995;20:143–158. doi: 10.1093/clinids/20.1.143. [DOI] [PubMed] [Google Scholar]
- 18.Matsuhisa A, Saito Y, Sakamoto Y, Keshi H, Ueyama H, Aikawa Y, Kishi Y, Ohno T. Detection of bacteria in phagocyte-smears from septicemia-suspected blood by in situ hybridization using biotinylated probes. Microbiol Immunol. 1994;38:511–517. doi: 10.1111/j.1348-0421.1994.tb01816.x. [DOI] [PubMed] [Google Scholar]
- 19.Rappaport T, Sawyer K P, Nachamkin I. Evaluation of several commercial biochemical and immunologic methods for rapid identification of gram-positive cocci directly from blood cultures. J Clin Microbiol. 1988;26:1335–1338. doi: 10.1128/jcm.26.7.1335-1338.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rex J H, Pfaller M A, Galgiani J N, Bartlett M S, Espinel-Ingroff A, Ghannoum M A, Lancaster M, Odds F C, Rinaldi M G, Walsh T J, Barry A L. Development of interpretive breakpoints for antifungal susceptibility testing: conceptual framework and analysis of in vitro-in vivo correlation data for fluconazole, itraconazole, and Candida infections. Subcommittee on Antifungal Susceptibility Testing of the National Committee for Clinical Laboratory Standards. Clin Infect Dis. 1997;24:235–247. doi: 10.1093/clinids/24.2.235. [DOI] [PubMed] [Google Scholar]
- 21.Rudolph K M, Parkinson A J, Black C M, Mayer L W. Evaluation of polymerase chain reaction for diagnosis of pneumococcal pneumonia. J Clin Microbiol. 1993;31:2661–2666. doi: 10.1128/jcm.31.10.2661-2666.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schifman R B, Ryan K J. Rapid automated identification of gram-negative bacilli from blood cultures with the AutoMicrobic system. J Clin Microbiol. 1982;15:260–264. doi: 10.1128/jcm.15.2.260-264.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shin J H, Nolte F S, Morrison C J. Rapid identification of Candida species in blood cultures by a clinically useful PCR method. J Clin Microbiol. 1997;35:1454–1459. doi: 10.1128/jcm.35.6.1454-1459.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song J H, Cho H, Park M Y, Na D S, Moon H B, Pai C H. Detection of Salmonella typhi in the blood of patients with typhoid fever by polymerase chain reaction. J Clin Microbiol. 1993;31:1439–1443. doi: 10.1128/jcm.31.6.1439-1443.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Souvenir D, Anderson D E, Palpant S, Mroch H, Askin S, Anderson J, Claridge J, Eiland J, Malone C, Garrison M W, Watson P, Campbell D M. Blood cultures positive for coagulase-negative staphylococci: antisepsis, pseudobacteremia, and therapy of patients. J Clin Microbiol. 1998;36:1923–1926. doi: 10.1128/jcm.36.7.1923-1926.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trebesius K, Harmsen D, Rakin A, Schmelz J, Heesemann J. Development of rRNA-targeted PCR and in situ hybridization with fluorescently labelled oligonucleotides for detection of Yersinia species. J Clin Microbiol. 1998;36:2557–2564. doi: 10.1128/jcm.36.9.2557-2564.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vidal F, Mensa J, Almela M, Martinez J A, Marco F, Casals C, Gatell J M, Soriano E, Jimenez-de-Anta M T. Epidemiology and outcome of Pseudomonas aeruginosa bacteremia, with special emphasis on the influence of antibiotic treatment. Analysis of 189 episodes. Arch Intern Med. 1996;156:2121–2126. [PubMed] [Google Scholar]
- 28.Vincent J L, Bihari D J, Suter P M, Bruining H A, White J, Nicolas-Chanoin M H, Wolff M, Spencer R C, Hemmer M. The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA. 1995;274:639–644. [PubMed] [Google Scholar]
- 29.Warren H S. Strategies for the treatment of sepsis. N Engl J Med. 1997;336:952–953. doi: 10.1056/NEJM199703273361311. [DOI] [PubMed] [Google Scholar]
- 30.Weinstein M P, Mirrett S, Reimer L G, Wilson M L, Smith-Elekes S, Chuard C R, Joho K L, Reller L B. Controlled evaluation of BacT/Alert standard aerobic and FAN aerobic blood culture bottles for detection of bacteremia and fungemia. J Clin Microbiol. 1995;33:978–981. doi: 10.1128/jcm.33.4.978-981.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wenzel R P, Pinsky M R, Ulevitch R J, Young L. Current understanding of sepsis. Clin Infect Dis. 1996;22:407–412. doi: 10.1093/clinids/22.3.407. [DOI] [PubMed] [Google Scholar]
- 32.Wheeler A P, Bernard G R. Treating patients with severe sepsis. N Engl J Med. 1999;340:207–214. doi: 10.1056/NEJM199901213400307. [DOI] [PubMed] [Google Scholar]
- 33.White A C, Atmar R L, Wilson J, Cate T R, Stager C E, Greenberg S B. Effects of requiring prior authorization for selected antimicrobials: expenditures, susceptibilities, and clinical outcomes. Clin Infect Dis. 1997;25:230–239. doi: 10.1086/514545. [DOI] [PubMed] [Google Scholar]
- 34.Wilmore D W. Polymerase chain reaction surveillance of microbial DNA in critically ill patients: exploring another new frontier. Ann Surg. 1998;227:10–11. doi: 10.1097/00000658-199801000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilson M L, Weinstein M P, Mirrett S, Reimer L G, Feldman R J, Chuard C R, Reller L B. Controlled evaluation of BacT/alert standard anaerobic and FAN anaerobic blood culture bottles for the detection of bacteremia and fungemia. J Clin Microbiol. 1995;33:2265–2270. doi: 10.1128/jcm.33.9.2265-2270.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wischnewski N, Kampf G, Gastmeier P, Schlingmann J, Daschner F, Schumacher M, Rüden H. Prevalence of primary bloodstream infections in representative German hospitals and their association with central and peripheral vascular catheters. Zentbl Bakteriol. 1998;287:93–103. doi: 10.1016/s0934-8840(98)80152-7. [DOI] [PubMed] [Google Scholar]
- 37.Zhang Y, Isaacman D J, Wadowsky R M, Rydquist White J, Post J C, Ehrlich G D. Detection of Streptococcus pneumoniae in whole blood by PCR. J Clin Microbiol. 1995;33:596–601. doi: 10.1128/jcm.33.3.596-601.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]