Abstract
Background:
As the incidence of overweight continues to increase among children and adolescents in Guatemala, underweight remains a prominent health problem. However, the prevalence of overweight or underweight and associated risk factors has not been investigated among adolescent girls.
Objective:
To determine the prevalence of underweight and overweight/obesity and associated sociodemographic, dietary, and lifestyle factors among adolescent girls in Jutiapa, Guatemala.
Methods:
A cross-sectional study of a subsample of 392 girls aged 12 to 17 years from an agriculture-nutrition trial was conducted. Anthropometric data were obtained using standard methods. Sociodemographic, dietary, and lifestyle data were collected using a structured questionnaire. Multivariable logistic regression was conducted using underweight (body mass index [BMI] for age <5th percentile) and overweight/obesity (BMI for age ≥85th percentile) as outcome variables.
Results:
The prevalence of underweight and overweight/obesity was 9.9% and 15.6%, respectively. Age (15–17 years), high waist circumference, high blood pressure, father being a farmer, large family (>5 persons), hours spent watching TV, and high red meat consumption were significantly associated with underweight. Whereas being in school, high waist circumference, high blood pressure, overweight/obese mother, unemployed father, watching TV for more than 2 hours, having soft drinks at home, and meeting fruit recommendations were significantly associated with overweight/obesity.
Conclusions:
Our findings highlight the importance of concurrently addressing underweight and overweight/obesity among adolescent girls in rural Guatemala. Studies in various parts of the country are needed to confirm the results of the present study and for appropriate strategies to be implemented to reduce both underweight and overweight.
Keywords: adolescents, Guatemala, BMI, overweight, underweight, obesity, associated factors
Introduction
As the prevalence of obesity increases in low- and middle-income countries (LMICs), the double burden of overnutrition and undernutrition has become a challenging public health problem, particularly in countries like Guatemala, where the prevalence of undernutrition in children <5 years remains high.1 According to the 2015 Global School-based Student Health Survey (GSHS), the underweight prevalence among students aged 13 to 17 years slightly decreased from 11.3% to 10.2%. At the same time, that of overweight increased from 27.3% to 29.2% between 2009 and 2015.2 Adolescence is a critical period of development, and being underweight or overweight has been linked with lifelong negative health consequences. Underweight adolescents experience a higher risk of infectious diseases, more reduced cognitive function, psychiatric disorders, and poor perceived health.3,4 For girls of childbearing age, underweight is particularly dangerous and associated with an array of adverse pregnancy outcomes, including maternal mortality, preterm birth, and intrauterine growth retardation.3 Obese children are at increased risk of becoming obese adults5 and consequently at higher risk for cardiovascular disease, diabetes, and other costly chronic comorbidities.6
Few studies have investigated underweight risk factors among adolescents in Guatemala, where research has mainly focused on malnourished infants and toddlers7,8 or school-aged children 5 to 9 years.1 A systematic review of multilevel factors that influence the underweight nutritional status in adolescents of LMICs revealed the complexity of understanding the societal burden of both underweight and overweight status.9 Individual-level factors include age, sex, birth order, religion, ethnicity, education, literacy level, employment status, and marital status. At the household level, parental education and occupation, household size and composition, mother’s knowledge of nutrition, and family income/resources were also associated with undernutrition. Determinants at the community/environmental level, such as residence, sanitation, school type, and seasonality, were also identified as essential factors. Daily lifestyle habits like physical activity and diet are also known to be associated with underweight status.3 However, very little is known about the intersectionality of factors that influence nutritional status in Central and Latin America among young girls of reproductive age.
Although the prevalence of overweight/obesity among female adolescents has reached epidemic proportions (from 28.4%. to 34.6%) in Guatemala, few studies have explored why.10–12 The increasing overweight/obese population in the country has been attributed to severe food insecurity, physical activity, and obesogenic environments.13,14 According to the 2015 GSHS, 13.6% of surveyed students went hungry because there was not enough food in their home during the past 30 days.2 About 32.9% ate food from a fast-food restaurant 2 days or more during the past 7 days. Sixty percent of female students usually drank carbonated soft drinks 1 or more times per day during the past 30 days. Only 34.7% went to physical education class 3 days or more weekly in the school year, while 25.6% spent 3 or more hours per day doing sitting activities compared to 20.9% among boys. A small percentage of girls (8.7%) were physically active for at least 60 min/d during the past 7 days as compared to 12.7% of boys.2 Several studies identified context-based factors affecting adolescent nutrition status in LMICs, such as parents’ nutrition status or junk food consumption, but this information is lacking in Guatemala.15–17
Despite the increasing recognition of the health challenges in Guatemala’s adolescent populations, there is limited evidence to guide decision-making and resource allocation for interventions, especially at the rural level. Population-based cross-sectional surveys, such as the GSHS, have been used worldwide to evaluate the prevalence of adolescent health needs and behaviors in a country or cross-country comparisons.18–20 However, country-level estimates may be less helpful in informing the local, community-based interventions common in rural, resource-limited settings. Thus, administering available surveys at the local level offers a solution for providing rapid, local estimates of health burdens in at-risk populations. Further, underweight or overweight prevention is vital during adolescence, which is a critical developmental period that strongly influences future health and economic success. For this reason, we targeted the understudied rural female adolescents living in hard-to-reach villages in Guatemala.1,10 The objectives of this study were to determine the prevalence of underweight and overweight/obesity and the associated sociodemographic, lifestyle, and dietary risk factors in a population of high-risk female adolescents in rural Guatemala.
Methods
Study Setting
The study was conducted between June and August 2017 in Jutiapa in Guatemala’s southeastern region (near the border with El Salvador). Most people in the area are identified as Ladinos, having Spanish (96.8%) and Indigenous Mayan cultural (3.2%) ancestry.21 In Jutiapa, one of Guatemala’s rural regions, families rely on subsistence farming. However, agriculture is continuously threatened by extreme weather and climate change such as droughts and floods, which force people to migrate in search of alternative opportunities for income generation.22 Migration toward the United States and Mexico is common, and laborers also migrate to nearby urban centers where food purchase can lead to a more varied diet and higher reliance on “ready-to-eat” and fast foods, compared to rural households.23
Study Design
Although this cross-sectional survey was a new study in terms of objectives and data collection, it was carried out in a subsample obtained from the sample framework of the baseline evaluation of an ongoing 3-year longitudinal cohort study (2016–2019) conducted by the Institute of Nutrition of Central America and Panama in partnership with HarvestPlus (WDC). The parent study involved an agriculture-nutrition intervention aimed to assess the nutrition impact of a high iron bean crop in adolescents in Eastern Guatemala, especially in rural communities of the 3 departments of Jutiapa, Jalapa, and Chiquimula. Although final publication of results of main trial is still in progress, at this stage, only preliminary results have been published at the Micronutrient Forum 5th Global Conference, November 2020.24
A subsample of 511 adolescent girls (12–17 years old) who completed the nutrition baseline survey of the main trial in 2016 were selected based on location, age, nonpregnancy status, and having no prior chronic conditions. In each study household, only 1 adolescent girl was chosen for assessment. If there was more than 1 adolescent in the house, the eldest female sibling was invited to participate, and in case of absence or refusal, the second eldest was chosen. A total of 461 (90%) adolescent girls were successfully contacted and 392 consented to participate in the study. A group of 67 adolescent girls did not meet our inclusion criteria (pregnancy and age). The main reason for nonparticipation was the failure to find individuals despite repeated visits to their household (n = 30) and refusal to participate (n = 20), while 2 adolescent girls with incomplete records were excluded (n = 2). All the girls and parents were informed verbally about the aims and procedures of the study. Furthermore, informed consent of parents/guardians and assent of the children were obtained before enrollment.
Data Collection
A team of 4 research assistants with extensive experience in data collection in maternal and child health conducted site visits in this community-based study. Selected adolescent girls were evaluated in their communities in a central location, either in their schools or at home. Administrative arrangements were made with the schools in the communities where the adolescents live, with the support of the local community development council members, named Cocodes. Specifically, Cocodes helped with the logistics for interviews of the predetermined eligible adolescents. With the school authorities’ support, arrangements were made with the schools to enable participating girls to be released from classes for 30 to 40 minutes to complete the assessments. A private location in the schools was selected for interviews and anthropometric (ie, weight, height, waist circumference) and blood pressure measurements. If the selected girls did not attend school to complete the evaluation, a new appointment was made to meet at their local school or homes to complete the assessment.
A pretested, structured questionnaire (Supplement A: Questionnaire for Adolescent girls) was used to collect information on sociodemographics, lifestyle and health-related behaviors (eg, participation in games, hours spent watching TV, and playing video or computer games using cell phone/computer, perception of participants health and their weight, and that of their parents), dietary habits (eg, frequency of consumption of different types of food, frequency of having breakfast, and consumption of fast foods), and unhealthy foods (frequency of consumption of red meat and junk foods). Sociodemographic characteristics included age (12–14; 15–17) and family size (≤4 persons; >5 persons). Similarly, socioeconomic characteristics included work status of participants (help with family work, work for income, and housekeeping), their education level (no school; elementary level: <7 grade; middle level: 7–9 grades; and high school: 10–12 grades), occupation of both father (unemployed; agricultural worker; and other: labor and public servant) and mother (unemployed; domestic worker; and other: cook and sales), and household food insecurity.
Information on screen time (eg, participation in games, hours spent watching TV, and playing video or computer games using cell phone/computer) was collected using a questionnaire from the Adolescent Sedentary Activity Questionnaire25 and dichotomized for the analysis according to screen time recommendations: <2 h/d (meets recommendation) or ≥2 h/d (does not meet recommendation). The junk food intake measure (JFIM) was based on the consumption of French fries, chips and salty snacks, pastries, candy, and ice cream. These foods are commonly consumed among Guatemala girls.26,27 Each food item was assigned a score of 0 to 5 depending on frequency of food intake (0 being never/rarely and 5 being 2 or more times per day) so that the JFIM ranged from 0 to 25 (0 being no junk food consumed).
Some diet indicators were collected using GSHS 2015 questionnaire such as household food insecurity, frequency of having breakfast, and consumption of fast foods. For household food insecurity, the respondent was asked the frequency of hunger to determine whether the condition happened rarely (low food insecurity = 1 or 2 times a week), sometimes (middle food insecurity = 3 or 4 times a week), or often (severe food insecurity = more than 4 times a week).21 The rest of the diet indicators were collected using a validated short food frequency questionnaire developed for population-based monitoring surveys.22 Respondents reported consumption of fruit, vegetables, fatty meat products, red meat, and beverages including sugar sweetened drinks (ie, soft drink, diet soft drink, fruit juice), and water versus milk. Frequency response categories for food items were (1) never or rarely, (2) 1 to 2 times per week, (3) 3 to 4 times per week, (4) 5 to 6 times per week, (5) 1 time per day, and (6) 2 times per day. These categories were recoded as never = a; sometimes = b + c, and usually = d + e + f. Responses for the drinks categories were 1 cup or less per week, 2 to 4 cups per week, 5 to 6 cups per week, 1 cup per day, and 2 cups per day (1 cup defined as 250 mL). This instrument has been tested in a “culturally and linguistically diverse” group of adolescents in Nepal.28
Weight was measured using a portable electronic scale (TANITA BC 420 SMA) adjusted to the exact lever ratio of the beam with the participant%% wearing light clothes and no shoes. Height was measured using a stadiometer (SECA 225) with the participant’s shoes off, feet together, and head in the horizontal plane. Body mass index (BMI) was calculated as body weight (kg) divided by the square of height (meter).29 Obesity was defined as BMI-for-age greater than or equal to the 95th percentile. Female adolescents with a BMI-for-age greater than or equal to 85th percentile but less than 95th percentile were classified as overweight. Underweight was defined as BMI-for-age less than the 5th percentile, whereas normal weight adolescents were determined to fall between the 5th to 85th percentiles from the International Obesity Task Force classification system.30 Waist circumference was measured at the midline of the iliac crest and lower costal margin. Blood pressure was measured by an electric sphygmomanometer. The width of the cuff was approximately two-thirds of the upper arm’s length. Three readings were taken, 5 minutes apart. For our analysis, the average of the 3 systolic and diastolic blood pressure readings was considered. Elevated blood pressure was defined as systolic blood pressure >130 mm Hg or diastolic blood pressure >80 mm Hg.31
Statistical Analysis
Statistical analysis was performed using STATA version 14.2 software. Descriptive statistics were used to analyze the characteristics of study participants and to describe anthropometric data. Continuous variables were presented as mean values and SD (mean ± SD) and categorical variables as percentages (%). χ2 tests were used to identify differences in proportions of the categories of the exposure by the nutritional status of adolescent girls, while analysis of variance was used for continuous variables.
The primary outcomes of the study were underweight and overweight/obesity. Covariates were demographic and socioeconomic factors (age, education, work status, mother and father occupation, family size, and food insecurity), lifestyle and health-related behaviors (sedentary behaviors and physical health risk factors), dietary habits (dietary pattern—fruits, vegetables, vegetable oil, sugar and salt added, and soft drinks, and family food practices—daily breakfast, fast food, soft drink available at home), and unhealthy foods consumed by the participants. To assess the general structure of the independent variables, we used principal component analysis (PCA) as the data reduction technique as all the measures were discrete.32 Principal component factor method of extraction with varimax rotation was used for all respondents with complete data. Items with loadings greater than 0.6 were used to interpret the factors. If the number of factors produced was more than 1, only the domain with the largest number of items was chosen (Supplement B: Factors loading using PCA). After reducing the number of variables, assumptions of logistic regressions were checked. Multivariable logistic regression analyses were conducted to explore factors associated with underweight and overweight/obesity compared to normal weight girls. Unadjusted OR and adjusted OR (AOR) and 95% CIs were computed for main outcomes, P values of <.05 were considered statistically significant.
Results
Demographic and Socioeconomic Characteristics of Participants
From the total sample of 392 respondents, 54.1% were 15 to 17 years old, 29.6% had no school education, and only 6.4% had high school education. The majority of the adolescents helped with family work like farming (64.5%) and most were involved in household responsibilities such as cooking, cleaning, and childcare (99.7%). About 88% of adolescent girls had low food insecurity.
As described in Table 1, 9.9% of adolescent girls (n = 39) were underweight and 15.6% (n = 61) were overweight/obese. Approximately 36.1% of adolescent girls who do not attend school were overweight or obese; 25.6% were underweight. Forty percent of underweight girls had fathers who were farmers, while 42.3% of overweight/obese girls reported that their fathers were unemployed. Finally, the underweight prevalence was the highest in households with 4 and more persons (97.4%; P = .039).
Table 1.
Demographic and Socioeconomic Characteristics of Adolescent Girls by BMI Status in Rural Communities of Jutiapa, Guatemala.
| Variables | Sample, n(%) | Underweight, (%) | Normal weight, (%) | Overweight/obesity, (%) | P a |
|---|---|---|---|---|---|
| All | 392 (100) | 9.95 | 74.49 | 15.56 | |
| Age, years | .411 | ||||
| 12–14 | 180 (45.92) | 53.85 | 46.23 | 39.34 | |
| 15–17 | 212 (54.08) | 46.15 | 53.77 | 60.66 | |
| Education | .510 | ||||
| No school | 116 (29.59) | 25.64 | 28.77 | 36.07 | |
| Elementary | 115 (29.34) | 33.33 | 29.79 | 24.59 | |
| Middle | 136 (34.69) | 28.21 | 35.62 | 34.43 | |
| High school | 25 (6.38) | 12.82 | 5.82 | 4.92 | |
| Work status | .721 | ||||
| Family work outside homeb | 253 (64.54) | 71.79 | 63.36 | 65.57 | |
| Work for income | 26 (6.63) | 2.56 | 7.53 | 4.92 | |
| Household domestic workb | 392 (99.74) | 100 | 100 | 98.36 | |
| Maternal occupationc,d | .041 | ||||
| Unemployed | 328 (85.19) | 86.84 | 84.72 | 86.44 | |
| Domestic worker | 30(7.79) | 13.16 | 8.33 | 1.69 | |
| Other§ | 27 (7.01) | 0 | 6.94 | 11.86 | |
| Father occupationc,e | .047 | ||||
| Unemployed | 94 (26.70) | 22.86 | 24.15 | 42.31 | |
| Agriculture | 130 (36.93) | 40.00 | 38.49 | 25.00 | |
| Other§ | 128 (36.36) | 37.14 | 38.49 | 25.00 | |
| Family size | .039 | ||||
| ≤4 persons | 42 (10.71) | 2.56 | 10.62 | 16.39 | |
| >5 persons | 350 (89.29) | 97.44 | 89.38 | 83.61 | |
| Household food insecurity | .898 | ||||
| Low | 344 (87.76) | 87.18 | 87.33 | 90.16 | |
| Moderate | 34 (8.67) | 10.26 | 8.56 | 8.2 | |
| Severe | 14 (3.57) | 2.56 | 4.11 | 1.64 |
Abbreviation: BMI, body mass index.
Comparisons between categorical variables and adolescent girls’ BMI (underweight, normal, and overweight/obesity) were performed using χ2 test.
Family work outside the home in farming, business, or agriculture; household domestic work activities included making masa, cleaning, cooking, childcare, washing, and so on.
Other include for mothers cook, sales; and for father laborer, public servants.
n = 385.
n = 352.
Lifestyle and Health-Related Behaviors of Participants
As shown in Table 2, approximately half of the participants (51.0%) played games after school or during the weekends, and 41.8% played games at school. More than 60% watched TV for 2 or more hours per day. Over one-third of participants reported having dinner in front of the TV 3 or more times per week (32.6%) and played video games using a cell phone or a computer 3 or more times per week (33.2%).
Table 2.
Lifestyle and Health-Related Behaviors of Adolescent Girls Aged 12 to 17 Years by BMI Status in Rural Communities of Jutiapa, Guatemala.
| Variables | Sample, n(%) | Underweight, (%) | Normal weight, (%) | Overweight/obesity, (%) | P a |
|---|---|---|---|---|---|
| Health risk behavior | |||||
| Playing games at school | 164 (41.84) | 43.59 | 42.47 | 37.7 | .927 |
| Playing games afterschool or during weekends | 200 (51.02) | 58.97 | 51.03 | 45.9 | .443 |
| Watching TV (≥2 h/d) | 237 (60.46) | 46.15 | 61.99 | 62.3 | .157 |
| Dinner in front of TV (≥3 times/wk) | 128 (32.65) | 28.21 | 31.51 | 40.98 | .294 |
| Using cell/computer (≥2 h/d) | 130 (33.16) | 41.03 | 30.48 | 40.98 | .156 |
| Physical health risk status | |||||
| Perception of own body size | <.001 | ||||
| Normal | 81 (20.66) | 2.56 | 17.81 | 45.90 | |
| Underweight | 286 (72.96) | 97.44 | 79.79 | 24.59 | |
| Overweight/obese | 25 (6.38) | 0 | 2.4 | 29.51 | |
| Mother’s body sizeb | .004 | ||||
| Normal | 105 (27.27) | 47.37 | 25 | 25.42 | |
| Underweight | 60 (15.58) | 10.53 | 18.4 | 5.08 | |
| Overweight/obese | 220 (57.14) | 42.11 | 56.6 | 69.49 | |
| Father’s body sizec | .876 | ||||
| Normal | 97 (27.4) | 31.43 | 27.44 | 24.53 | |
| Underweight | 79 (22.32) | 17.14 | 22.18 | 26.42 | |
| Overweight/obese | 178 (50.28) | 51.43 | 50.38 | 49.06 | |
| Regards self as healthy | 181 (46.17) | 38.46 | 47.26 | 45.9 | .828 |
| Mean ± SD | |||||
| Waist circumference, cm | 68.2 ± 7.3 | 59.9 ± 3.2 | 66.9 ± 4.6 | 79.3 ± 7.9 | <.001 |
| Systolic, mm Hg | 104.6 ± 10.3 | 99.4 ± 11.3 | 103.9 ± 9.6 | 111.2 ± 10.1 | <.001 |
| Diastolic, mm Hg | 66.3 ± 8.8 | 62.5 ± 7.3 | 66.2 ± 7.6 | 69.6 ± 13.1 | <.001 |
| Hypertensiond (%) | 31 (7.91) | 0 | 6.2 | 21.3 | <.001 |
Abbreviation: BMI, Body mass index.
Comparisons between continuous variables and adolescent girls’ BMI (underweight, normal, and overweight/obesity) were performed by analysis of variance while relation with categorical variables was tested using χ2 test.
n = 385.
n = 354.
Hypertension is defined as blood pressure of 130/80 mm Hg or higher.
Regarding physical health risk status, almost half of participants (46.2%) rated themselves as “healthy.” When asked about weight perception, 79.8% of girls with normal weight rated themselves as underweight, whereas 45.9% of overweight/obese girls considered themselves to have a normal weight (P < .001). A significantly high percentage of overweight/obese adolescent girls (69.5%) also had overweight/obese mothers (P = .004). Finally, waist circumference, blood pressure (systolic and diastolic), and the prevalence of hypertension were higher in overweight/obese girls compared to underweight girls (79.3 ± 7.9 cm v. 59.9 ± 3.2 cm; 111.2 ± 10.1 mm Hg vs 99.4 ± 11.3 mm Hg systolic; 69.6 ± 13.1 mm Hg vs 62.5 ± 7.3 mm Hg diastolic, 21.3% vs 0%).
Dietary Habits of Participants
As described in Table 3, 76.0% of participants reported eating breakfast daily and 13.3% consumed 3 or more servings of vegetables per day. In our sample, daily consumption of water of 2 or more cups was 54.6%. Other dietary behaviors included, usually adding 3 or more teaspoons of sugar to drinks (16.8%) and teaspoons of salt to meals (11.5%). Regarding family food practices, 40.8% of participants had soft drinks available at home, and 10.5% reported usually having soft drinks with meals. Vegetable oil was commonly used for cooking home meals (83%). Finally, the prevalence of overweight/obesity was the highest among girls who did not meet daily fruit and vegetable recommendations (2–3 servings per day, 67% and 88%, respectively), ate take out/fast foods (61.5%), and those who usually had a soft drink instead of water/milk (18%).
Table 3.
Dietary Habits of Adolescent Girls Aged 12 to 17 Years by BMI Status (%) From Rural Communities of Jutiapa, Guatemala (N = 392).
| Variables | Sample, n(%) | Underweight, n = 39 | Normal weight, n = 292 | Overweight/obesity, n = 61 | P a |
|---|---|---|---|---|---|
| Eat breakfast daily | 298 (76.02) | 82.05 | 75.34 | 75.41 | .649 |
| Water intake (≥2 cups/d) | 214 (54.59) | 61.54 | 52.4 | 60.66 | .328 |
| Fruit intake | .046 | ||||
| ≥2 servings/d | 180 (45.92) | 56.41 | 47.26 | 32.79 | |
| <2 servings/d | 212 (54.08) | 43.59 | 52.74 | 67.21 | |
| Vegetable intake | .361 | ||||
| ≥3 servings/d | 52 (13.27) | 20.51 | 12.67 | 11.48 | |
| <3servings/d | 340 (86.73) | 79.49 | 87.33 | 88.52 | |
| Eating take out/fast food | .045 | ||||
| Yes | 203 (51.79) | 57.38 | 49.32 | 61.54 | |
| No | 189 (48.21) | 42.62 | 50.68 | 38.46 | |
| Having soft drinkb | 0.034 | ||||
| Never | 146 (37.5) | 30.77 | 37.33 | 42.62 | |
| Sometimes | 207 (52.81) | 58.97 | 54.79 | 39.34 | |
| Usually | 38 (9.69) | 10.26 | 7.88 | 18.03 | |
| Soft drinks with meal | .235 | ||||
| Never | 125 (31.89) | 35.9 | 32.19 | 27.87 | |
| Sometimes | 226 (57.65) | 58.97 | 55.48 | 67.21 | |
| Usually | 41 (10.46) | 5.13 | 12.33 | 4.92 | |
| Soft drinks at home | .462 | ||||
| Never | 232 (59.18) | 56.41 | 60.96 | 52.46 | |
| Sometimes | 134 (34.18) | 38.46 | 33.22 | 36.07 | |
| Usually | 26 (6.63) | 5.13 | 5.82 | 11.48 | |
| Cooking oil | .524 | ||||
| Vegetable oil | 326 (83.38) | 89.74 | 82.82 | 81.97 | |
| Other type | 65 (16.62) | 10.26 | 17.18 | 18.03 | |
| Sugar added to drinks | .480 | ||||
| <3 teaspoons | 326 (83.16) | 69.23 | 84.93 | 83.61 | |
| ≥3 teaspoons | 66 (16.84) | 30.77 | 15.07 | 16.39 | |
| Salt added to meals | .573 | ||||
| Never | 62 (15.82) | 5.13 | 16.1 | 21.31 | |
| Sometimes | 285 (72.7) | 76.92 | 73.29 | 67.21 | |
| Usually | 45 (11.48) | 17.95 | 10.62 | 11.48 |
Abbreviation: BMI, body mass index.
Comparisons between continuous variables between underweight and nonunderweight (normal and overweight) were performed by t test, while relation between categorical variables was tested by χ2 test.
Versus having water or milk.
Unhealthy Foods Consumption of Participants
Table 4 shows that consumption of red meat was significantly associated with BMIs of adolescent girls (P < .001). Underweight was highest among girls who ate red meat 2 or less times a week (91.8%), while overweight/obesity among girls who consumed meat more than 2 times a week was 38.5% of the sample. However, consuming processed meat, French fries, chips, salty snacks, pastries, candy, ice cream, fruit juice, and soft drinks were not significantly associated with BMIs of adolescent girls. Over a quarter of participants reported eating French fries (26.5%), processed meat products (29.8%), ice cream (32.1%), and 43.4% reported eating candy more than 2 times a week. More than half consumed chips and salty snacks (53.8%) and pastries (58.2%) more than twice a week. Regarding beverages, only 13.5% of girls met the fruit juice recommendation while half had more than 1 cup of soft drink per week; 18.3% had high junk food intake.
Table 4.
Unhealthy Foods of Adolescent Girls Aged 12 to 17 Years by BMI Status (%) From rural Communities of Jutiapa, Guatemala (N=392).
| Variables | Sample, n(%) | Underweight, n = 39 | Normal weight, n = 292 | Overweight/obesity, n = 61 | P a |
|---|---|---|---|---|---|
| Red meat | <.001 | ||||
| ≤2 times/wk | 332 (84.69) | 91.8 | 86.3 | 61.54 | |
| >2 times/wk | 60 (15.31) | 8.20 | 13.7 | 38.46 | |
| Processed meat | .473 | ||||
| ≤2 times/wk | 275 (70.15) | 64.1 | 69.86 | 75.41 | |
| >2 times/wk | 117 (29.85) | 35.9 | 30.14 | 24.59 | |
| French fries | .969 | ||||
| ≤2 times/wk | 288 (73.47) | 71.79 | 73.63 | 73.77 | |
| >2 times/wk | 104 (26.53) | 28.21 | 26.37 | 26.23 | |
| Chips and salty snacks | .908 | ||||
| ≤2 times/wk | 181 (46.17) | 48.72 | 45.55 | 47.54 | |
| >2 times/wk | 211 (53.83) | 51.28 | 54.45 | 52.46 | |
| Pastries | .877 | ||||
| ≤2 times/wk | 164 (41.84) | 43.59 | 41.1 | 44.26 | |
| >2 times/wk | 228 (58.16) | 56.41 | 58.9 | 55.74 | |
| Candy | .336 | ||||
| ≤2 times/wk | 222 (56.63) | 46.15 | 57.19 | 60.66 | |
| >2 times/wk | 170 (43.37) | 53.85 | 42.81 | 39.34 | |
| Ice cream | .469 | ||||
| ≤2 times/wk | 266 (67.86) | 61.54 | 69.52 | 63.93 | |
| >2 times/wk | 126 (32.14) | 38.46 | 30.48 | 36.07 | |
| Fruit juice | .356 | ||||
| ≤1 cup/d | 53 (13.52) | 20.51 | 12.33 | 14.75 | |
| >1 cup/d | 339 (86.48) | 79.49 | 87.67 | 85.25 | |
| Soft drink | .443 | ||||
| ≤1 cup/wk | 193 (49.23) | 41.03 | 49.32 | 54.1 | |
| >1cup/wk | 199 (50.77) | 58.97 | 50.68 | 45.9 | |
| Junk food intakeb | .827 | ||||
| Low (score 0–5) | 229 (66.57) | 73.91 | 65.15 | 67.15 | |
| Middle (score 6–8) | 52 (15.12) | 10.87 | 16.29 | 11.76 | |
| High (score 9–25) | 41 (18.31) | 15.22 | 18.56 | 20.59 |
Abbreviation: BMI, body mass index.
Comparisons between categorical variables and adolescent girls’ BMI (underweight, normal, and overweight/obesity) were performed using χ2 test.
Junk food intake measure based on the consumption of fries, chips, pastries, candy, and ice cream, n = 344.
Factors Associated With Underweight and Overweight/Obesity in Adolescent Girls
Several factors were found to be associated with underweight and overweight in the regression analysis, as shown in Tables 5 and 6. Regarding underweight, 15- to 17-year-olds, girls with fathers who were farmers and from large families (>5 persons) were more than twice as likely to be underweight (AOR = 2.61, 95% CI, 1.22–4.64; AOR = 2.63, 95% CI, 1.37–4.96; AOR = 2.57, 95% CI, 1.19–7.31, respectively). However, girls who spent more than 2 hours in front of the TV were less likely to be underweight (AOR = 0.42; 95% CI, 0.16–0.81). Similarly, girls with high waist circumference (≥88 cm), high hypertension, and high consumption of red meat (>2 times a week) were less likely to be underweight (AOR = 0.53, 95% CI, 0.41–0.67; AOR = 0.81, 95% CI, 0.54–0.98; AOR = 0.49, 95% CI, 0.14–0.94, respectively).
Table 5.
Multiple Logistic Regression Analysis of Factors Associated With Underweight in Adolescent Girls From Rural Communities of Jutiapa, Guatemala.a
| Characteristics | OR | 95% CI | AOR | 95% CI |
|---|---|---|---|---|
| Demographic | ||||
| Age, years (15–17 years) | 1.70 | 1.36–3.36b | 2.61 | 1.22–4.64b |
| Education (yes) | 0.80 | 0.38–1.71 | 1.12 | 0.38–3.27 |
| Dad occupation (farmer) | 1.61 | 1.42–2.89b | 2.63 | 1.37–4.96b |
| Family size (>5 persons) | 3.29 | 1.67–7.35c | 2.57 | 1.19–7.31b |
| Lifestyle | ||||
| TV viewing (>2 h/d) | 0.52 | 0.27–1.02 | 0.42 | 0.16–0.81b |
| Dinner in front of TV (>3 times/wk) | 0.79 | 0.38–1.65 | 1.32 | 0.46–3.85 |
| Using cell/computer (≥2 h/d) | 1.46 | 0.74–2.87 | 1.68 | 0.59–4.79 |
| Mom body size (overweight) | 0.82 | 0.35–1.82 | 1.03 | 0.36–2.98 |
| Waist circumference | 0.11 | 0.08–0.16c | 0.53 | 0.41–0.67c |
| High blood pressure (yes) | 0.12 | 0.09–0.17c | 0.81 | 0.54–0.98c |
| Diet | ||||
| Red meat consumption (>2 times/wk) | 0.14 | 0.03–0.61c | 0.49 | 0.14–0.94c |
| Junk food score | 0.84 | 0.36–1.96 | 0.63 | 0.20–1.94 |
| Met fruit recommendations | 1.60 | 0.82–3.11 | 1.36 | 0.51–3.59 |
| Met vegetables recommendations | 1.81 | 0.78–4.19 | 1.28 | 0.40–4.11 |
| Eating take out/fast food | 1.56 | 0.78–3.06 | 1.64 | 0.63–4.24 |
| Soft drinks available in the home | 1.04 | 0.61–1.76 | 0.66 | 0.28–1.55 |
Abbreviation: AOR, adjusted odds ratio.
Hosmer-Lemmeshow goodness-of-fit test of final model: 0.665.
Significance at P value < .05.
Significance at P value < .001.
Table 6.
Multiple Logistic Regression Analysis of Factors Associated With Overweight/obesity in Adolescent Girls From Rural Communities of Jutiapa, Guatemala.a
| Characteristics | OR | 95% CI | AOR | 95% CI |
|---|---|---|---|---|
| Demographic | ||||
| Age, years (15–17 years) | 1.37 | 0.79–2.40 | 0.94 | 0.36–2.50 |
| Education (yes) | 0.82 | 0.35–0.92b | 0.17 | 0.03–0.99b |
| Dad occupation (unemployed) | 2.32 | 1.26–4.28b | 2.38 | 1.18–5.76b |
| Family size (>5 persons) | 0.54 | 0.25–1.18 | 0.53 | 0.15–1.84 |
| Lifestyle | ||||
| TV viewing (>2 h/d) | 1.10 | 0.62–1.92 | 2.62 | 1.39–3.69b |
| Dinner in front of TV (>3 times/wk) | 1.54 | 0.88–2.69 | 0.79 | 0.28–2.24 |
| Using cell/computer (≥2 h/d) | 1.49 | 0.85–2.62 | 1.06 | 0.40–2.78 |
| Mom body size (overweight) | 1.26 | 1.90–2.70b | 1.82 | 1.12–3.80b |
| Waist circumference | 3.27 | 1.43–5.69c | 3.91 | 2.87–9.11c |
| High blood pressure (yes) | 4.71 | 2.17–8.23c | 4.11 | 1.51–8.36b |
| Diet | ||||
| Red meat consumption (>2 times/wk) | 1.45 | 0.17–2.17 | 1.39 | 0.47–3.20 |
| Junk food score | 1.69 | 0.33–2.46 | 1.09 | 0.35–2.82 |
| Met fruit recommendations | 0.52 | 0.29–0.93b | 0.45 | 0.18–0.98b |
| Met vegetables recommendations | 1.42 | 1.80–3.53b | 1.58 | 0.43–5.76 |
| Eating take out/fast food | 1.30 | 0.75–2.27 | 0.98 | 0.40–2.39 |
| Soft drinks available in the home | 1.40 | 0.92–2.13 | 2.36 | 1.69–3.67b |
Abbreviation: AOR, adjusted odds ratio.
Hosmer-Lemmeshow goodness-of-fit test of final model: 0.638.
Significance at P value < .05.
Significance at P value < .001.
As shown in Table 6, the risk of being overweight/obese more than doubled for girls who viewed TV more than 2 h/d and had soft drinks available at home (AOR = 2.62, 95% CI, 1.39–3.69; AOR = 2.36, 95% CI, 1.69–3.67 respectively). Adolescent girls with high waist circumference (AOR = 3.91, 95% CI, 2.87–9.11) and high blood pressure (AOR = 4.11, 95% CI, 1.51–8.36) were 4 times more likely to be overweight/obese. Parental factors, such as having an unemployed father and an overweight/obese mother, also significantly increased the odds of girls being overweight/obese (AOR = 2.38, 95% CI, 1.18–5.76; AOR = 1.82, 95% CI, 1.12–3.80, respectively). However, adolescent girls who went to school and those who met dietary fruit recommendation had lower odds of being overweight/obese (AOR = 0.17, 95% CI, 0.03–0.99; AOR = 0.45, 95% CI, 0.18–0.98, respectively).
Discussion
The prevalence of underweight among rural adolescent girls in our study (10%) is higher than estimates obtained from the 2015 GSHS administered to adolescent females (13–17 years) in Guatemala City.2 Nonetheless, our results are consistent with a study in a rural district of Guatemala, which found that 10.9% of girls aged 5 to 18 years were underweight.33 Like the previous body of literature, we found a high rate of overweight/obesity (16%).14 However, our overweight/obesity rate was lower than previously reported by the 2015 GSHS among urban adolescent girls (31.7%). In a different population of rural adolescent girls in Izabal of northeastern Guatemala, Muros et al1 found higher prevalence of overweight (26.1%) than the national estimate of adolescent girls (24.8%).10 Geographic, economic, seasonal, and behavioral variations of factors across these different settings may account for the difference. Our findings highlight the double burden of overnutrition and undernutrition and the need for intervention in the studied rural community.34 Our results support the growing trend of overweight/obesity in rural areas among adolescent girls in Central and Latin America, with the most current overweight/obesity prevalence ranging from 16.7% to 34.6%.35 According to Torun et al,36 a rural lifestyle is not protective of women’s body weight in Guatemala. Urbanization, “Westernization,” and globalization of food markets drive changes in diet, work, and leisure activities that affect weight gain of individual.
In our study, age (15–17 years), father’s occupation as a farmer, having a large family, waist circumference, and high blood pressure were significantly associated with underweight adolescent girls. Reasons for the high prevalence of underweight among 15 to 17 years old adolescent girls may be related to educational attainment,37–39 food insecurity,33 and fear of being fat.40–42 One study in Southeast Asia reported an increase in the feeling that an underweight body is ideal and of eating disorders among adolescent girls.43 Unfortunately, we do not have data on the girls’ cultural patterns to pursue thinness ideas among our sample. Like our study, Melaku et al44 found that adolescents whose fathers are farmers were more likely to be undernourished than those whose fathers had salaried occupations, and larger families were associated with adolescent undernutrition. The finding on family size is instructive if one considers the low standard of living in Jutiapa and that living in a larger household translates to a higher financial burden and less available food than a small family size.45 In the present study, adolescent girls attending school were less likely to be overweight/obese, suggesting that low educational attainment may increase the risk of obesity either by limiting the ability of the girls to understand and act on health information or that the school environment increases and promotes health and wellness among adolescents. Finally, the negative association found between BMI, blood pressure, and waist circumference agrees with other studies that report that underweight individuals were less likely to have higher blood pressure and waist circumference than those in other BMI categories.46,47
For overweight/obese adolescent girls, high waist circumference, high blood pressure, and unemployed father were positively associated with overweight/obesity, while adolescent girls in school were less likely to be overweight/obese. Consistent with Lambert et al,48 overweight/obese adolescents have higher waist circumference and blood pressure than their non-overweight counterparts. Anthropometric measures are known to predict cardiovascular and metabolic risks in adolescents, suggesting that these measurements should be included in routine health examinations to remind parents of the comorbidity of obesity.49 Our results on girls whose fathers were unemployed were more likely to be obese than employed parents confirm the results of other studies, which showed that fathers’ socioeconomic status (SES) impacts stable household habits, dietary values, and physical activity.50,51 Finally, our findings on adolescent girls attending school confirm the results of a qualitative study among rural Guatemalan adolescent girls that revealed that girls not enrolled in school had fewer physical activity opportunities and were more sedentary.52 These results highlight an urgent need for policy focused on nutrition standards of the school food programs and on creating community-based opportunities for the activity of girls not in school; parent and student nutrition education will be also useful.
This study also indicates that girls of overweight/obese mothers were more likely to be overweight/obese. This finding is consistent with those reported by Naidu et al53 and Çalişir and Karaçam,54 suggesting that overweight/obese adolescent girls are influenced by their environment, including eating patterns of their families and their habitual activities.15 At the same time, it is important to note the considerable tolerance for overweight/obesity by the participating adolescent girls in the municipality of Jutiapa. About 80% of normal weight girls rated themselves as underweight, whereas 45.9% of overweight/obese girls considered themselves to have normal weight. Our finding corroborates a general trend observed in Latin America, where overweight girls severely underestimate their weight status.55–57 These findings suggest that not only are bodyweight norms higher in rural Guatemala than in urban Guatemala,12 but they are also less strict, which can only foster the development of the obesity epidemic.58 A study by Hackman et al59 even highlighted from evidence in Guatemala the need to revise models of weight-related stigma focused on obesity in global contexts. Thus, re-thinking these bodyweight norms will be fundamental to addressing obesity, particularly in the rural environment.
Lifestyle factors such as watching TV for 2 or more hours per day were associated with overweight/obesity. Our findings are consistent with Hong et al,60 who showed that physical activity lowered the risk of obesity. Thus, a family-based approach focusing on diet and physical activity modification and the inclusion of physical exercise in health education in schools should be implemented to help promote healthy weight among adolescent girls. Regarding food and beverage habits, consumption of red meat was associated with underweight, and meeting fruit intake recommendations was negatively associated with overweight/obesity. Appropriate meat consumption provides key micronutrients to optimize growth during childhood and adolescence, as suggested by a study that found lower blood pressure and BMI among children who ate meat daily and more frequently.61 Consistent with our results, Nurwanti et al62 showed that overweight adolescents consumed less fruit than underweight adolescents in rural Indonesia. On the other hand, the consumption of soft drinks at home was positively associated with overweight/obesity. Several studies have also investigated the association of sweetened soft drinks with obesity. However, they obtained inconsistent results,63–65 which may be due to differences in study designs, including definition and classifications of soft drinks (types, amounts consumed, or frequency of consumption) and weight status (BMI or with/without obesity). Decreasing intake of sweetened soft drinks may help weight control for overweight/obese female adolescents.66
To our knowledge, this study is the first to examine sociodemographic, dietary, and lifestyle-associated factors for both underweight and overweight among adolescent girls in rural Guatemala. However, there are some limitations. First, this study was restricted to one geographic region; thus, the results cannot be generalized to all adolescent girls in Guatemala. Second, insufficient physical activity is one of the risk behaviors that can negatively affect adolescents’ health, but we could not use it in our study because of incomplete or missing data. Third, this was a cross-sectional survey, so only associations, and not causations, can be determined. Fourth, although SES strongly influences diet and lifestyle factors, the adolescent participants could not provide this information. However, we collected information on participants’ work status, their education level, occupation of both fathers (unemployed; farmer; public servant; other) and mother (unemployed; domestic worker; cook and sales; other), and household food insecurity. Finally, self-reported questionnaires were used for many measures, including dietary patterns and physical activity behaviors. Thus, bias may be present due to inaccurate self-reporting, misunderstanding of the questionnaire items, or social desirability.67
In conclusion, this study reveals that the prevalence of underweight and overweight/obese was high among adolescent girls in Jutiapa. These conditions were associated with the girls’ sociodemographic characteristics, as well as the lifestyle and dietary habits. These findings demonstrate the need to improve parents’ awareness of the implications of their children’s weight and highlight the need for comprehensive education and promotion of healthy nutrition in rural communities. The plans for weight control among female adolescents may decrease screen time and consumption of soft drinks at home and increase fruit consumption and time for physical activity. Finally, given the paucity of previous data in rural populations in Guatemala, our results represent a starting point for future research. This finding calls for a collaborated study in various parts of the country to validate the current data so that appropriate and beneficial strategies can be planned to reduce underweight and overweight/obesity among adolescent girls in Guatemala.
Supplementary Material
Figure 1.
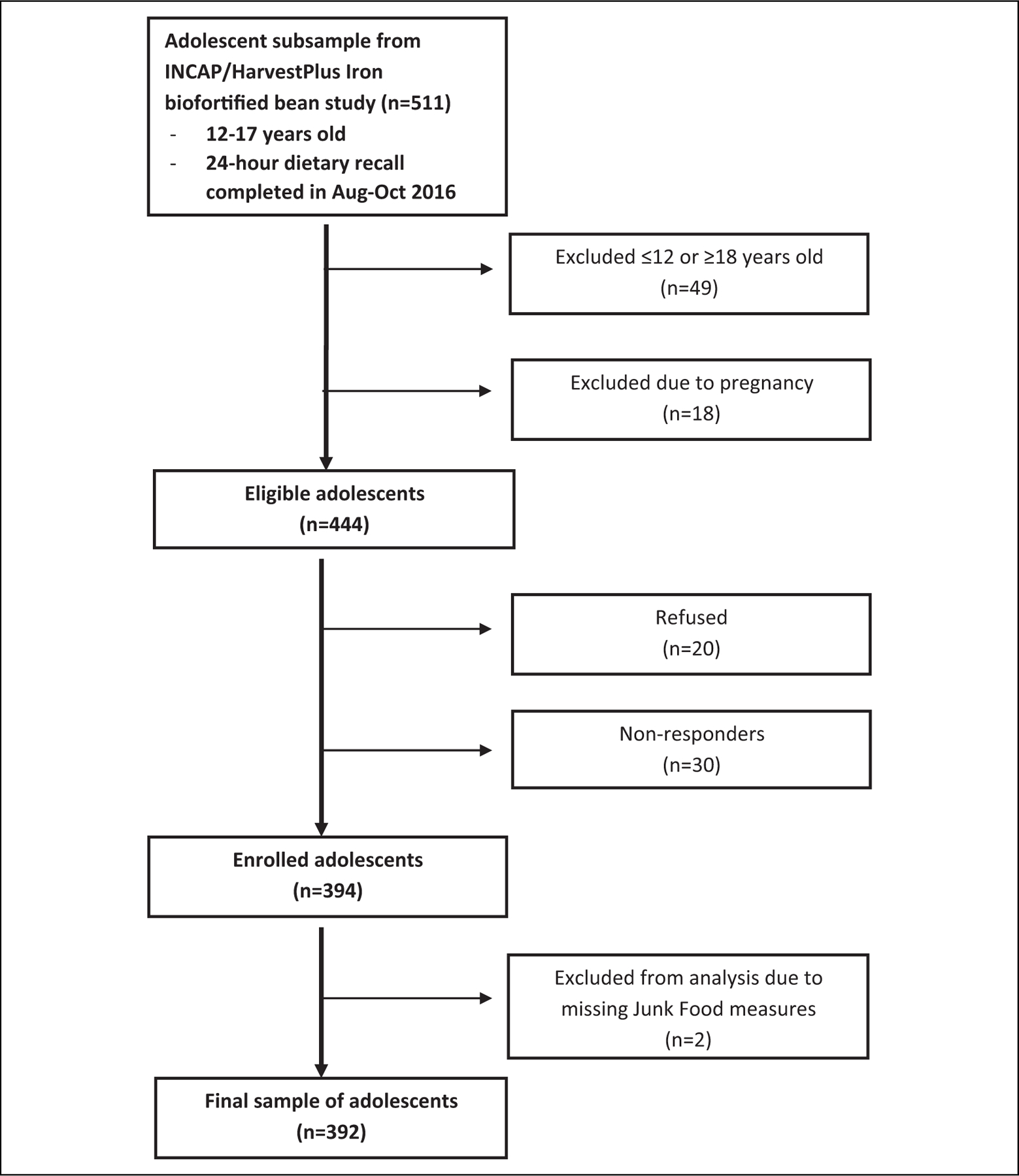
Study flow diagram of female adolescents participating in a cross-sectional survey in rural communities of Jutiapa, Guatemala.
Highlights.
The double burden of overnutrition and undernutrition is an emerging public health concern among adolescent girls in rural areas of Jutiapa, Guatemala.
Low and high BMI were associated with the girls’ sociodemographic characteristics, their lifestyle, and dietary habits, suggesting an urgent need for multicenter studies in various parts of the Guatemala to validate the present results’ generalizability, so that appropriate strategies to reduce both nutrition statuses among adolescent girls can be addressed.
Acknowledgments
The authors thank the adolescent girls who participated in the study. The authors thank the Cocodes in their communities for assisting with study logistics.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Minority Health International Research Training (MHIRT) grant no. T37-MD001448 from the National Institute on Minority Health and Health Disparities, National Institutes of Health, Bethesda, MD, USA, and the Institute for Nutrition of Central America and Panama, Guatemala City, Guatemala.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplementary Materials
Supplemental material for this article is available online.
References
- 1.Muros J, Briones M, Rodriguez G, et al. Double burden of malnutrition in rural and urban Guatemalan schoolchildren. Nutr Hosp. 2016;33(2): 345–350. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO). 2015 Global school-based student health survey (GSHS). Accessed March 24, 2021. https://www.who.int/teams/noncommunicable-diseases/surveillance/data/guatemala
- 3.Ochiai H, Shirasawa T, Nanri H, et al. Lifestyle factors associated with underweight among Japanese adolescents: a cross-sectional study. Arch Public Health. 2017;75(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pu C, Chou YJ. Health ratings for underweight, overweight and obese adolescents: disparities between adolescent’s own report and the parent’s report. Asia Pac J Clin Nutr. 2017;19(2):180–187. [PubMed] [Google Scholar]
- 5.Singh AS, Mulder C, Twisk JWR, Van Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474–488. [DOI] [PubMed] [Google Scholar]
- 6.Günögr NK. Overweight and obesity in children and adolescents. J Clin Res Pediatr Endocrinol. 2014;6(3):129–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagata JM, Gippetti J, Wager S, et al. Prevalence and predictors of malnutrition among Guatemalan children at 2 years of age. PLoS One. 2016;11(11): e0164772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rachmi CN, Agho KE, Li M, Chavez A, Wise PH. Stunting, underweight and overweight in children aged 2.0–4.9 years in Indonesia: prevalence trends and associated risk factors. PLoS One. 2016;11(5): e0154756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madjdian DS, Azupogo F, Osendarp SJ, Bras H, Brouwer ID. Socio-cultural and economic determinants and consequences of adolescent undernutrition and micronutrient deficiencies in LLMICs: a systematic narrative review. Ann N Y Acad Sci. 2018;1416(1), 117–139. [Google Scholar]
- 10.Mazariegos M, Kroker-Lobos MF, Ramírez-Zea M. Socio-economic and ethnic disparities of malnutrition in all its forms in Guatemala. Public Health Nutr. 2019;23(S1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen D, Rivera-Andrade Á , González J, et al. Prevalence of risk factors for noncommunicable diseases in an indigenous community in Santiago Atitlán, Guatemala. Rev Pan Salud Publica. 2017; 41:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Madrigal L, Adams I, Chacon V, Barnoya J. Perceived barriers to achieving a healthy weight: a qualitative study using focus groups at public and private schools in Guatemala City. BMC Public Health. 2017;17(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yates-Doerr E The Weight of Obesity: Hunger and Global Health in Postwar Guatemala. 1st ed. UC Press; 2015. [Google Scholar]
- 14.Johnson RK, Lamb M, Anderson H, et al. The global school-based student health survey as a tool to guide adolescent health interventions in rural Guatemala. BMC Public Health. 2019;19(226): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Syahrul S, Kimura R, Tsuda A, et al. Prevalence of underweight and overweight among school-aged children and its association with children’s sociodemographic and lifestyle in Indonesia. Int J Nur Sci. 2016;3(2):169–177. [Google Scholar]
- 16.de Morais Macieira L, de Andrade J, da Conceicão Santos L. Overweight and obesity and their associated factors among early adolescence school children in urban and rural Portugal. BMC Nutr. 2016;1(3):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borraccino A, Lemma P, Berchialla P, et al. Unhealthy food consumption in adolescence: role of sedentary behaviours and modifiers in 11-, 13- and 15-year-old Italians. Eur J Public Health. 2016;26(4):650–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al Ani MF, Al Subhi LK, Bose S. Consumption of fruits and vegetables among adolescents: a multinational comparison of eleven countries in the eastern Mediterranean region. Br J Nutr. 2016; 116(10):1–8. [DOI] [PubMed] [Google Scholar]
- 19.Beck NI, Arif I, Paumier MF, Jacobsen KH. Adolescent injuries in Argentina, Bolivia, Chile, and Uruguay: results from the 2012–2013 global school-based student health survey (GSHS). Injury. 2016;47(12):2642–2649. [DOI] [PubMed] [Google Scholar]
- 20.Badr HE, Lakha SF, Pennefather P. Differences in physical activity, eating habits and risk of obesity among Kuwaiti adolescent boys and girls: a population-based study. Int J Adolesc Med Health. 2017;31(1). [DOI] [PubMed] [Google Scholar]
- 21.Ministerio de Salud Pública y Asistencia Social (MSPAS) de Guatemala. Encuesta nacional de salud y nutrición materno infantil 2014–2015. 2017. Accessed March 24, 2021. https://www.ine.gob.gt/images/2017/encuestas/ensmi2014_2015.pdf
- 22.Famine Early Warning Systems Network (FEWS Net). National livelihood zone map for Guatemala. 2016. Accessed April 22, 2021. https://fews.net/sites/default/files/documents/reports/Consolidated_GT_LZ_Jan%2031%202017_0.pdf
- 23.Alkerwi A, Crichton GE, Hebert JR. Consumption of ready-made meals and increased risk of obesity: findings from the observation of cardiovascular risk factors in Luxembourg (ORISCAV-LUX) study. Br J Nutr. 2014;113(2):270–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reyes B, Mazariegos M. Efficacy and effectiveness of food system value chain interventions: the impact of biofortified beans – Guatemala effectiveness trial. Micronutrient Forum 5th Global Conference Proceedings. November 8–13, 2020. Bangkok, Thailand. Accessed April 28, 2021. https://www.eventscribe.com/2020/MNF-CONNECTED/agenda.asp?pfp¼On%20Demand [Google Scholar]
- 25.Hardy LL, Booth ML, Okely AD. The reliability of the adolescent sedentary activity questionnaire (ASAQ). Prev Med. 2007;45(1):71–74. [DOI] [PubMed] [Google Scholar]
- 26.Chew A, Moran A, Barnoya J. Food swamps surrounding schools in three areas of Guatemala. Prev Chronic Dis. 2020;17(200029). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li L, Sun N, Zhang L, et al. Fast food consumption among young adolescents aged 12–15 years in 54 low- and middle-income countries. Glob Health Action. 2020;13(1):1795438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karki A, Shrestha A, Subedi N. Prevalence and associated factors of childhood overweight/obesity among primary school children in urban Nepal. BMC Public Health 2019;19(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kuczmarski RJ. CDC growth charts girls body mass index-for-age percentiles 2 to 20 years. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; Update September 9, 2010. Accessed April 20, 2021. https://www.cdc.gov/growthcharts/ [Google Scholar]
- 30.Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ. 2007;335(7612):194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riley M, Hernandez AK, Kuznia AL. High blood pressure in children and adolescents. Am Fam Physician. 2018;98(8):486–494. [PubMed] [Google Scholar]
- 32.Manisera M, van der Kooij AJ, Dusseldorp E. Identifying the component 22 structure of satisfaction scales by nonlinear principal components analysis. Qual Technol Quant Manage. 2010; 7(2):97–115. [Google Scholar]
- 33.Ramirez-Zea M, Kroker-Lobos MF, Close-Fernandez R, Kanter R. The double burden of malnutrition in indigenous and nonindigenous Guatemalan populations. Am J Clin Nutr. 2014; 100(6):1644s–1651s. [DOI] [PubMed] [Google Scholar]
- 34.Jaacks LM, Slining MM, Popkin BM. Recent trends in the prevalence of under- and overweight among adolescent girls in low- and middle-income countries. Pediatr Obes. 2015;10(6):428–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rivera JA, de Cossio TG, Pedraza LS, et al. Childhood and adolescent overweight and obesity in Latin America: a systematic review. Lancet Diabetes Endocrinol. 2014;2(4),321–332. [DOI] [PubMed] [Google Scholar]
- 36.Torun B, Stein AD, Schroeder D, et al. Rural-to-urban migration and cardiovascular disease risk factors in young Guatemalan adults. Int J Epidemiol. 2002;31(1):218–226. [DOI] [PubMed] [Google Scholar]
- 37.Otto N Analysis of the Guatemalan education sector from a human rights-based perspective. 2008. Germany: GTZ. [Google Scholar]
- 38.Pena C Improving Access to Health Care Services Through the Expansion of Coverage Program (PEC): The Case of Guatemala. UNICO Studies Series; 19; 2013. [Google Scholar]
- 39.Guedes D, Almeida F, Neto J, Maia MD, Tolentino TM. Low body weight/thinness overweight and obesity of children and adolescents from a Brazilian region of low economic status. Rev Paul Pediatr. 2013;31(4):437–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patton GC, Selzer R, Coffey C, Carlin JB, Wolfe R. Onset of adolescent eating disorders: population-based cohort study over 3 years. BMJ. 1999;318(7186):765–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prista A, Maia JA, Damasceno A, Beunen G. Anthropometric indicators of nutritional status: implications for fitness, activity, and health in school-age children and adolescents from Maputo, Mozambique. Am J Clin Nutr. 2003;77(4): 952–959. [DOI] [PubMed] [Google Scholar]
- 42.Braveman P A health disparities perspective on obesity research. Prev Chronic Dis. 2009;6(3). [PMC free article] [PubMed] [Google Scholar]
- 43.Pike KM, Dunne PE. The rise of eating disorders in Asia: a review. J Eat Disord. 2015;3(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Melaku YA, Zello GA, Gill TK, Adams RJ, Shi Z. Prevalence and factors associated with stunting and thinness among adolescent students in Northern Ethiopia: a comparison to world health organization standards. Arch Public Health. 2015; 73(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Engle PL, Bentley M, Pelto G. The role of care in nutrition programs: current research and a research agenda. Proc Nutr Soc. 2000;59(1):25–35. [DOI] [PubMed] [Google Scholar]
- 46.Deshmukh PR, Gupta SS, Dongre AR, et al. Relationship of anthropometric indicators with blood pressure levels in rural Wardha. Indian J Med Res. 2006;123(5):657–664. [PubMed] [Google Scholar]
- 47.Momin M, Fan F, Li J, et al. Joint effects of body mass index and waist circumference on the incidence of hypertension in a community-based Chinese population. Obes Facts. 2020;2(2):245–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lambert M, Delvin EE, Levy E, et al. Prevalence of cardiometabolic risk factors by weight status in a population-based sample of Quebec children and adolescents. Can J Cardiol. 2008;24(7):575–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gaya AR, Brand C, Dias AF, et al. Obesity anthropometric indicators associated with cardiometabolic risk in Portuguese children and adolescents. Prev Med Rep. 2017;8:158–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ball K, Mishra G. Whose socioeconomic status influences a woman’s obesity risk; her mother’s, her father’s, or her own? Int J Epidemiol. 2006; 35(1):131–138. [DOI] [PubMed] [Google Scholar]
- 51.El-bayoumy I, Shady I, Lotfy H. Prevalence of obesity among adolescents (10–14 years) in Kuwait. Asia Pac J Public Health. 2009;21(2): 153–159. [DOI] [PubMed] [Google Scholar]
- 52.Kurschner S, Madrigal L, Chacon V, Barnoya J, Rohloff P. Impact of school and work status on diet and physical activity in rural Guatemalan adolescent girls: a qualitative study. Ann N Y Acad Sci. 2020;1468(1):16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Naidu BM, Mahmud SZ, Ambak R, et al. Overweight among primary school-age children in Malaysia. Asia Pac J Clin Nutr. 2013;22(3): 408–415. [DOI] [PubMed] [Google Scholar]
- 54.Calisir H, Karacam Z. The prevalence of overweight and obesity in primary schoolchildren and its correlation with sociodemographic factors in Aydin Turkey. Int J Nurs Pract. 2011;17(2): 166–173. [Google Scholar]
- 55.Edwards NM, Pettingell S, Borowsky IW. Where perception meets reality: self-perception of weight in overweight adolescents. J Pediatr. 2010;125(3): e452–458. [DOI] [PubMed] [Google Scholar]
- 56.Maximova K, McGrath JJ, Barnett T, et al. Do you see what I see? Weight status misperception and exposure to obesity among children and adolescents. Int J Obes. 2008;32(6):1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McArthur LH, Holbert D, Pena M. An exploration of the attitudinal and perceptual dimensions of body image among male and female adolescents from six Latin American cities. Adolescence. 2005;40(160):801. [PubMed] [Google Scholar]
- 58.Cohen E, Boëtsch G, Palstra FP, Pasquet P. Social valorisation of stoutness as a determinant of obesity in the context of nutritional transition in Cameroon: the Bamiléké case. Soc Sci Med. 2013;96:24–32. [DOI] [PubMed] [Google Scholar]
- 59.Hackman J, Maupin J, Brewis AA. Weight-related stigma is a significant psychosocial stressor in developing countries: evidence from Guatemala. Soc Sci Med. 2016;161:55–60. [DOI] [PubMed] [Google Scholar]
- 60.Hong I, Coker-Bolt P, Anderson KR, Lee D, Velozo CA. Relationship between physical activity and overweight and obesity in children: findings from the 2012 national health and nutrition examination survey national youth fitness survey. Am Journal Occup Ther. 2016;70(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim GH, Shin SW, Lee J, et al. Red meat and chicken consumption and its association with high blood pressure and obesity in South Korean children and adolescents: a cross-sectional analysis of KSHES, 2011–2015. Nutr J. 2017;16(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nurwanti E, Hadi H, Chang JS, et al. Rural-Urban differences in dietary behavior and obesity: results of the Riskesdas study in 10–18-year-old Indonesian children and adolescents. Nutrients. 2019; 11(11):2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Berkey CS, Rockett HR, Field AE, Gillman MW, Colditz GA. Sugar added beverages and adolescent weight change. Obes Res. 2004;12(5):778–788. [DOI] [PubMed] [Google Scholar]
- 64.Striegel-Moore RH, Thompson D, Affenito SG, et al. Correlates of beverage intake in adolescent girls: national heart lung and blood institute growth and health study. J Pediatr. 2006;148(2): 183–187. [DOI] [PubMed] [Google Scholar]
- 65.Sun SZ, Empie MW. Lack of findings for the association between obesity risk and usual sugar-sweetened beverage consumption in adults – a primary analysis of database of CSFII–1991, CSFII-1994–1998, NHANESIII, and combined NHANES 1999–2002. Food Chem Toxicol. 2007;45(8):1523–1536. [DOI] [PubMed] [Google Scholar]
- 66.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr. 2006;84(2):274–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Latkin CA, Mai NV, Ha TV, et al. Social desirability response bias and other factors that may influence self-reports of substance use and HIV risk behaviors: a qualitative study of drug users in Vietnam. AIDS Educ Prev. 2016;28(5):417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


