Abstract
Partial meniscectomy or failed meniscus repair can lead to pain, dysfunction, and cartilage degradation due to increased contact forces. Meniscus transplantation can lead to favorable outcomes and cartilage preservation with careful patient selection. Limited data exist on segmental meniscus allograft transplantation, with promising results using synthetic grafts and early animal and biomechanical studies on segmental allograft transplantation, showing similar results to full meniscus allograft transplantation. This article presents a technique for arthroscopic segmental medial meniscus allograft transplant and a brief review of the literature.
Technique Video
Narrative description and video illustration of a 31-year-old female who underwent a right knee medial meniscus segmental transplantation along with revision anterior cruciate ligament reconstruction with Bone Patella Bone autograft.
Introduction
Meniscal tears remain one of the most common orthopaedic injuries. Partial meniscectomy or failed meniscus repair can lead to pain, dysfunction, and cartilage degradation due to increased contact forces in both short- and long-term studies.1, 2, 3, 4 Load distribution through resistance of axial force through the horizontal hoop structure is a key function of intact menisci with transmission of 50% compartment load medially and 70% laterally in extension, increasing to 85% and 90%, respectively, in flexion.5 Specifically, segmental meniscus resection can increase peak local contact stresses by up to 110% and loss of 20% of meniscal tissue can lead to up to 350% increase in joint contact forces in flexion.6, 7, 8 Additionally, the focal area of cartilage immediately adjacent to prior resection can be specifically affected.9
Several studies have shown that meniscus repair can prevent cartilage degradation; however, if this fails or the meniscal tissue is no longer viable, meniscus transplantation is an option that can lead to favorable long-term outcomes and cartilage preservation in the correct patient setting with between 75 and 85% return to sport rates.10, 11, 12, 13, 14, 15 While total meniscal allograft transplantation can be a good option for complete meniscal deficiency, this may remove an excessive amount of viable autogenous meniscus if there is only a segmental deficiency. Treatment of a focal segmental meniscus deficiency with segmental meniscus transplantation to preserve the native anterior and posterior meniscus roots is currently being explored as an alternative technique to preserve native meniscus tissue and normal joint function. We present a technique for arthroscopic medial meniscus segmental transplant using a combination of several fixation techniques.
Surgical Technique
A narrated video with demonstration of the surgical technique for arthroscopic segmental transplantation, as described below, may be reviewed (Video 1).
Preoperative Evaluation
Indications for meniscus transplantation include complete or near-complete meniscus deficiency, age <50, pain limiting desired activities, and minimal cartilage degradation (Outerbridge grade II or better).16 Additionally, patients should have realistic postsurgical activity expectations and be willing to comply with the rehabilitation protocol.7 In this case, a full-thickness segmental meniscus deficiency is functionally similar to a complete meniscus deficiency.17 Contraindications include limb malalignment, skeletal immaturity, knee instability, and obesity (body mass index >35). If a patient presents as a candidate for meniscus transplantation, limb alignment, focal chondral defects, and instability should be addressed at the time of meniscus transplant or in a staged fashion prior to transplantation if these diagnoses exist in conjunction with meniscus deficiency.
Graft Selection
Meniscal allograft is obtained from a certified tissue bank and is sized matched using the patient’s height, weight, and preoperative weight-bearing radiographs to establish standard measurement ratios for the graft.18,19 Additionally, a CT scan can be obtained, which has been shown to increase accuracy compared to radiographs alone.20 MRI can be useful to assess concomitant pathology, but it has not been shown to be more accurate than radiographs using updated measurement techniques.21 Since a central segment of the graft will be used, the presence of tibia bone blocks is not necessary but, if present, can be removed during graft preparation. The meniscus is thawed and prepared while the arthroscopic portion of the procedure is being performed.
Patient Positioning and Visualization
The patient is positioned supine with a well-padded tourniquet on the operative thigh. The leg can either be secured in a well leg holder or can be flexed while supine to allow access to the medial knee. After prepping/draping and surgical time out, the leg is exsanguinated, and the tourniquet inflated. If concomitant anterior cruciate ligament reconstruction with autograft is being performed, the graft is harvested prior to arthroscopy. Medial and lateral arthroscopic portals are established. Diagnostic arthroscopy is then performed, and notch debridement and preparation are conducted (in the setting of concomitant ACL reconstruction).
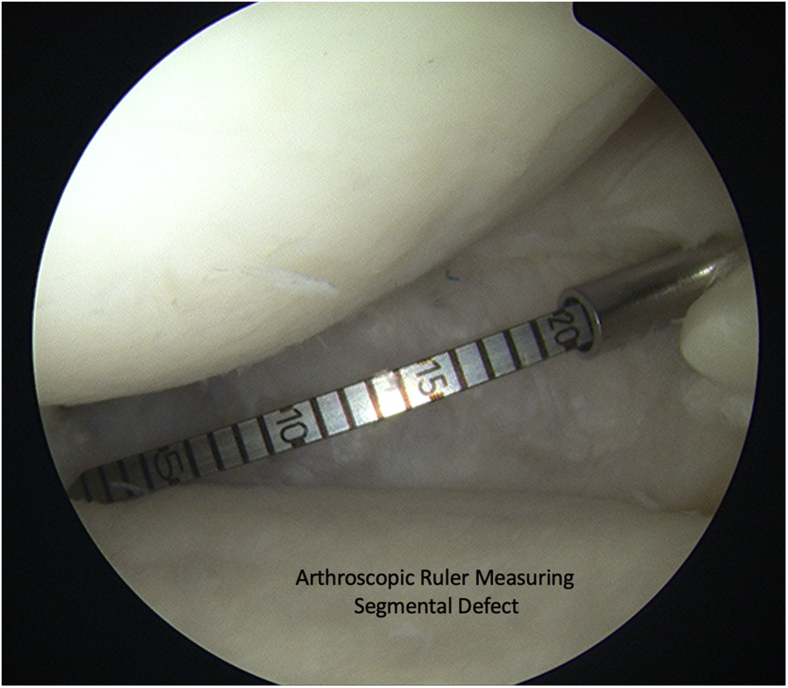
The deficient medial meniscus is then prepared by removing devitalized tissue and any remnant sutures from previous repair attempts with a basket biter or arthroscopic shaver (Fig 1). Once deficient and devitalized meniscal tissue has been debrided back to native capsule, a rasp is used to establish a fresh bleeding bed at the capsular interface and at the free edges of the remaining native posterior and anterior meniscal segments. If visualization is limited and the knee is tight, the medial collateral ligament can be percutaneously trephinated with an 18-gauge spinal needle while applying a valgus load.22 The capsule can also be trephinated with an 18-gauge spinal needle to encourage neovascularization. Once the recipient site has been prepared, the segmental defect is measured with an arthroscopic ruler (Arthrex, Naples, FL) for size matching to the graft (Fig 2).
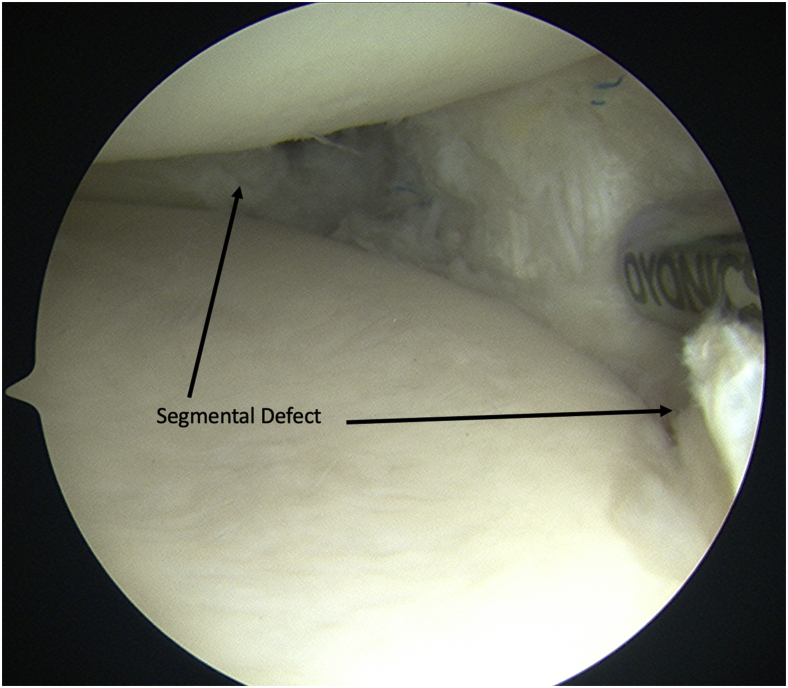
Fig 1.
Viewing from the anterolateral portal of the right knee, the deficient medial meniscus is prepared by removing devitalized tissue and any remnant sutures from previous repair attempts with a basket biter to define the margins of the tear and an arthroscopic shaver. Arrows show the margins of the segmental deficiency.
Fig 2.
The segmental defect is measured with an arthroscopic ruler for size matching to the graft.
Medial Joint Line Approach
The midpoint of the meniscal defect is then marked with a probe, and the medial skin indentation point is marked with a skin marker along the medial joint line. A 4-cm longitudinal incision is made in line with the mark centered 1/3rd superior and 2/3rd inferior to the joint line. Full-thickness skin flaps are elevated, and the sartorius fascia is identified, incised, and elevated along the anterior margin to protect the infrapatellar branch of the saphenous nerve. The posterior medial capsule is then palpated bluntly, ensuring the medial head of the gastrocnemius is posterior. If there are any retained suture knots or all-inside implants, these are removed. A curved retractor can then be placed in this interval for later suture retrieval.
Graft Sizing and Preparation
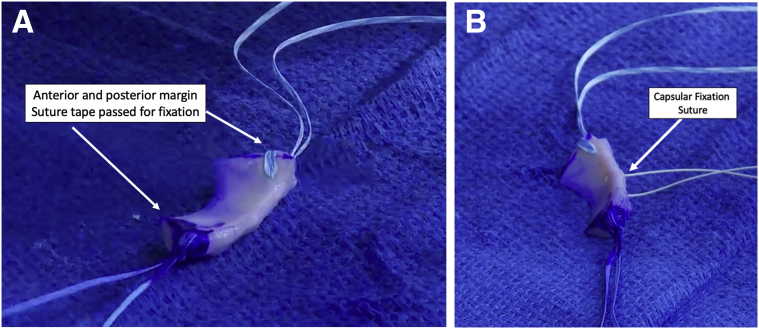
The meniscal tissue is separated from any bone block that may come with it. The fresh meniscus allograft is then marked to correspond to the region of the segmental defect to the same length as previously measured on arthroscopic examination. The segment of graft is sharply cut with vertical anterior and posterior edges to match the segmental defect (Fig 3). Meniscal suture tapes are passed in a luggage tag fashion on the anterior and posterior edges of the graft for later securing into bone tunnels (Fig 4A). A no. 0 Vicryl is passed in a vertical mattress fashion at the midpoint of the graft for repair to the capsule (Fig 4B). The distance between the suture tape tails is again measured as final measurement for location of the tibia bone tunnels, which will anchor the anterior and posterior edges of the segmental transplant.
Fig. 3.
The allograft meniscus is prepared on the back table by cutting vertical anterior and posterior margins to match the size of the segmental defect.
Fig 4.
(A) Meniscal suture tapes are passed in a luggage tag fashion on the anterior and posterior edges of the graft for later securing into bone tunnels. (B) No. 0 Vicryl vertical mattress suture is passed at the midpoint of the graft for repair to the capsule (arrow).
Meniscus Transplant
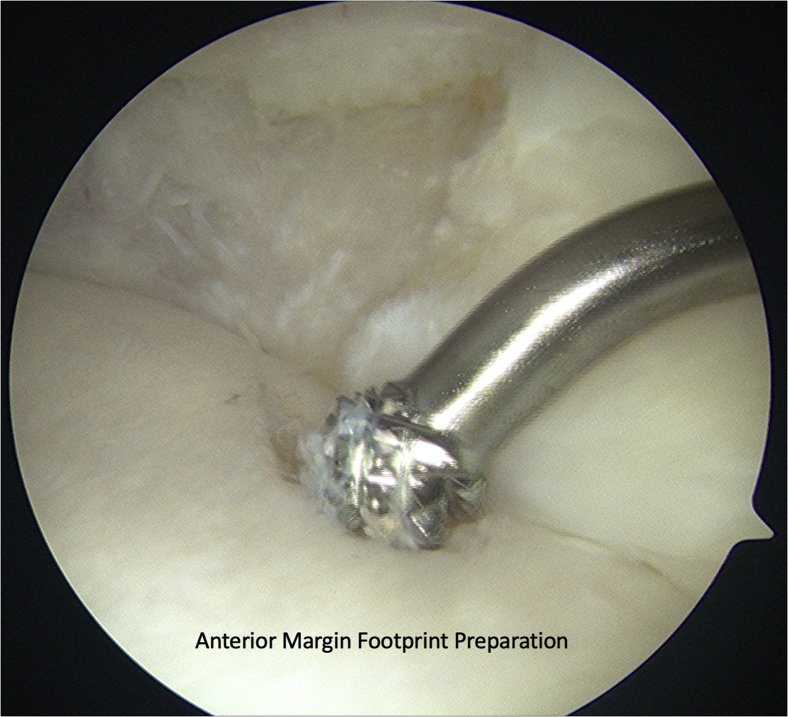
A PassPort cannula (Arthrex, Naples, FL) is placed into the medial portal for graft and instrument passage, and the arthroscope is reinserted into the lateral portal. The previous distance measured between the two suture tapes is marked with a radiofrequency wand onto the tibial cartilage. These sites are prepared using a ring curette and rasp to create a bleeding bone surface (Fig 5). A meniscus root repair guide (Smith & Nephew, Memphis, TN), which uses a cannulated drill bit that can be left in place for subsequent suture passage, is then used to drill both a posterior and anterior tunnel for securing the graft (Fig 6). In this case, the posterior tunnel was drilled at 55° and the anterior tunnel at 65° to prevent tunnel convergence. If an ACL reconstruction is also being performed, care must be taken to avoid the planned distal aperture of the tibial tunnel.
Fig 5.
The anterior and posterior chondral margins of the graft are prepared using a ring curette and rasp (shown in figure) to create a bleeding bone surface.
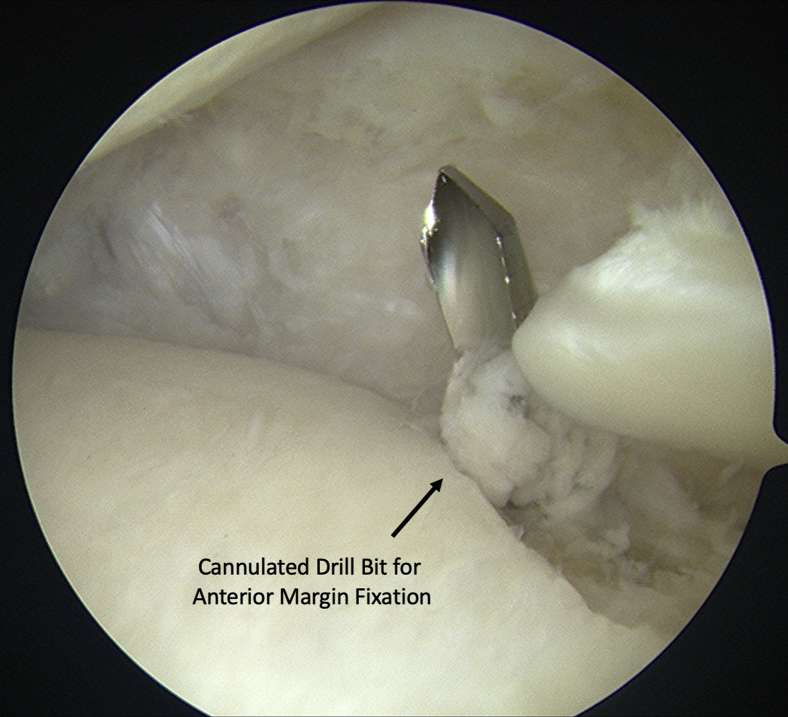
Fig 6.
A cannulated meniscus root tunnel guide, which uses a cannulated drill bit that can be left in place for subsequent suture passage, is used to drill both a posterior and anterior tunnel for securing the graft. Anterior tunnel is shown.
Monofilament sutures are passed retrograde into the cannulated drill bits and retrieved through the medial PassPort cannula (Fig 7). The posterior suture tape is passed into the posterior passing suture, and the meniscus graft is drawn into the medial knee compartment. Once in the knee, a soft tissue grasper can be used to manipulate the graft into place. The anterior suture tape is then passed through the anterior tunnel. Once the graft is in position, tension is placed on the anterior and posterior sutures, and they are secured over a cortical button (Smith & Nephew, Memphis, TN) on the anterior medial tibia. The central vertical mattress Vicryl suture is retrieved in an outside-in fashion through the posteromedial incision and passed through the capsule using either an 18-gauge spinal needle with a passing suture or a bird-beak suture retriever through two separate poke holes. This suture is then tied to the capsule using multiple racking half-hitch knots to secure the central portion of the graft.
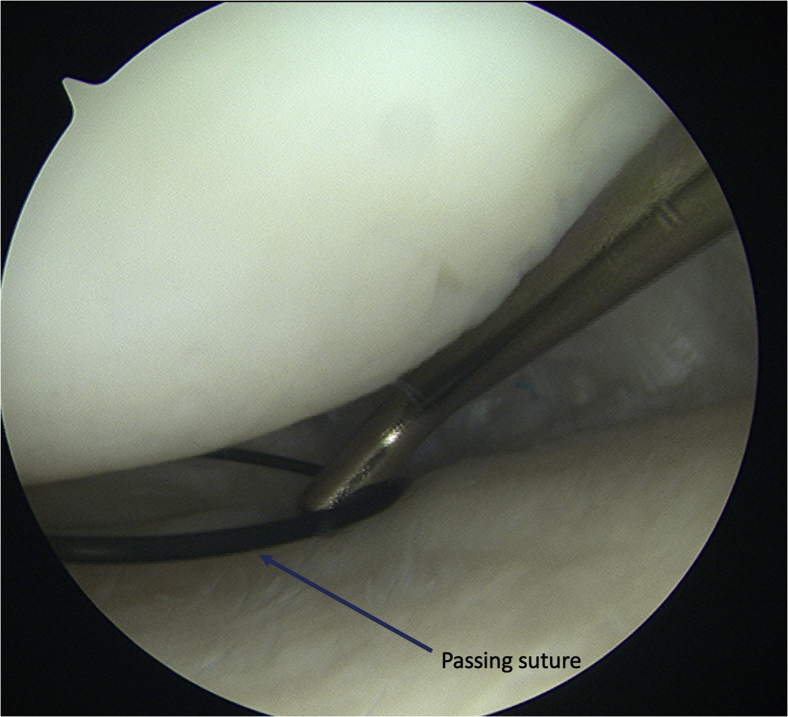
Fig 7.
Monofilament sutures (arrow) are passed retrograde into the cannulated drill bits and retrieved through a medial PassPort cannula.
Multiple vertical mattress sutures (2-0 high strength) are then placed both superiorly and inferiorly to the graft to secure it to the capsule, spaced 5 mm apart using a SharpShooter (Stryker, Kalamazoo, MI) inside-out suture passing device (Fig 8). The sutures are individually retrieved through the prior posterior medial capsular exposure and tied to the capsule with multiple half-hitch knots. Once the segmental meniscal allograft has been secured at the periphery to the capsule, the remaining radial fixation of the posterior and anterior graft to native tissue interface was secured using side-to-side horizontal mattress sutures (Fig 9). This is accomplished using the Ceterix (Smith & Nephew, Memphis, TN) all-inside suture passing device with 2-0 high-strength sutures and tied using a knot pusher using alternating half hitches (Fig 10). The knee is taken through a range of motion, and the final transplant is examined with arthroscopic probe to confirm stability. Pearls and pitfalls of the procedure are outlined in Table 1.
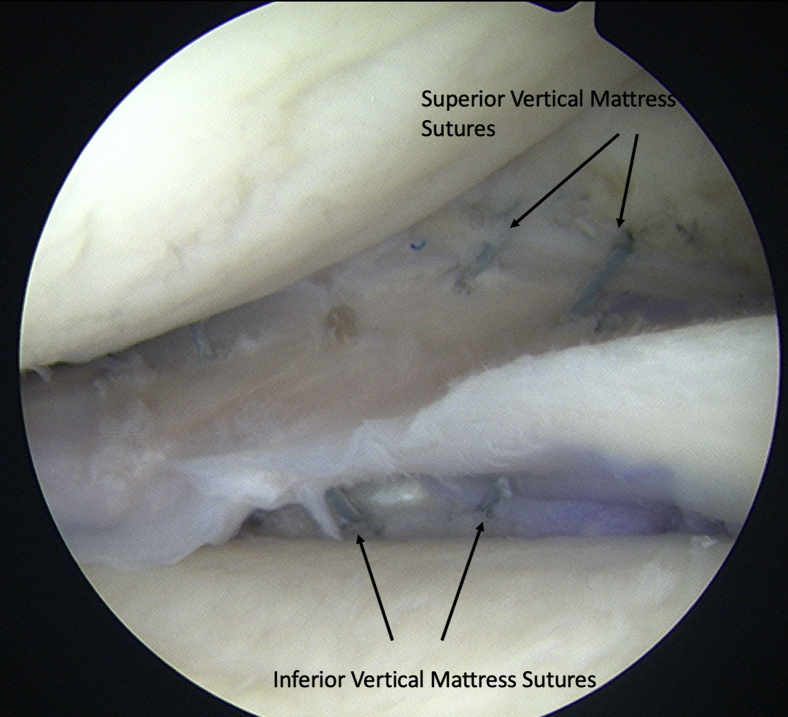
Fig 8.
Multiple 2-0 high-strength vertical mattress sutures (arrows) are then placed both superiorly and inferiorly to the graft to secure it to the capsule, spaced 5 mm apart using a SharpShooter inside-out suture passing device. The sutures are retrieved through a posterior medial approach and tied to the capsule.
Fig 9.
Once the segmental meniscal allograft has been secured at the periphery to the capsule, the remaining radial fixation of the posterior and anterior graft to native meniscus tissue interface is performed using side-to-side horizontal mattress sutures and tied using a knot pusher. Posterior segment fixation is shown.
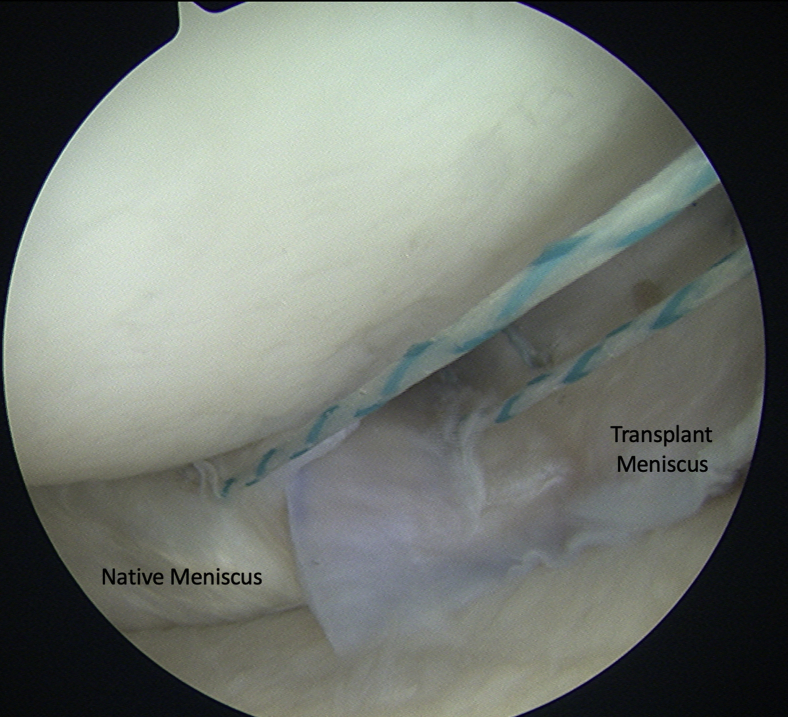
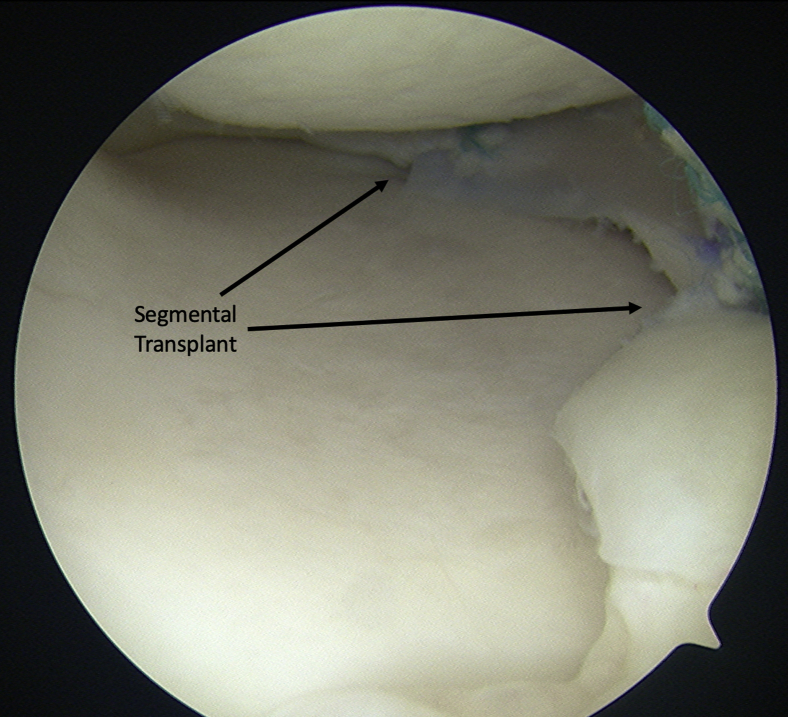
Fig 10.
Final segmental meniscus transplant viewed from the anterior lateral portal. Arrows indicate the anterior and posterior margins of the segmental transplant.
Table 1.
Pearls and Pitfalls of Arthroscopic Segmental Meniscus Allograft Transplant
| Pearls | Pitfalls |
|---|---|
| Obtain adequate exposure to the medial compartment by trephinating or pie crusting the MCL. This may also promote neovascularization of the residual meniscal rim. | Identify and retract infrapatellar branch of saphenous nerve during medial capsule approach to avoid a painful neuroma. |
| Use arthroscopic ruler after native meniscus debridement and preparation to adequately size segmental graft. | Ensure tibia tunnels are drilled away from planned trajectory of ACL graft tunnel, if applicable. |
| Pass anterior and posterior graft bone tunnel fixation sutures through graft during graft preparation to facilitate graft passage into the knee and ease of anchoring into tibial tunnels. | Fixation and healing failure if patient not able to comply with the rehabilitation protocol and restrictions. |
| Use of a low profile all-inside suture passage device allows for radial component repair using intra-articular knots. | Failure to identify and address concomitant ligamentous instability, or malalignment. |
If an ACL reconstruction is also performed, the tibia tunnel can be drilled, and graft fixation can be performed. The medial wound is closed in layered fashion along with the portals. Sterile dressings are applied, and the patient is placed into a T-scope premier locking hinged-range of motion brace (Breg, Carlsbad, CA).
Rehabilitation
Postoperatively, the patient is non-weight bearing for 6 weeks. Range of motion is limited 0-90° for the first 2 weeks, and then advanced, as tolerated. The early restrictions are in place to protect the suture fixation until well incorporated. Physical therapy is initiated immediately postoperatively for quad sets, ROM therapy, and soft tissue modalities. Full unrestricted activity is at 6-9 months postoperatively, pending a strength assessment noting operative extremity strength to be >90% of the contralateral extremity. Release to full activity is also dictated by concomitant procedures.
Discussion
Several surgical technique articles have been published describing various techniques for medial and lateral meniscus allograft transplantation.23, 24, 25, 26, 27 While one other technique for segmental meniscus transplantation has been recently described,28 this technique differs in that it employs a transtibial tunnel technique, which is familiar to most surgeons who perform meniscal root repairs and can be performed arthroscopically. The indications for segmental meniscus transplantation are narrow, as the posterior and anterior meniscus roots must be intact with a large portion of both posterior and anterior meniscus tissue preserved to allow for adequate fixation. This technique combines several previously well-described fixation methods to include soft tissue bone tunnel fixation, radial repair, and inside-out techniques to achieve robust and anatomic fixation to optimize biologic incorporation.
Several studies show favorable long-term survivorship for complete meniscal allograft transplantation of 73.5% at 10 years, 60.3% at 15 years, and 56.2% at 20 years.13,29 Although no clinical outcomes studies have been published for segmental meniscus allograft transplantation, Nyland et al. showed in a porcine biomechanical study that segmental meniscus transplantation restores focal contact forces to similar values to the native meniscus state.30 Strauss et al. looked at collagen healing in sheep at both 39 and 90 days after segmental meniscus transplantation and found that although not completely healed at 90 days, there was progressive collagen healing at the 90-day time frame at the peripheral, posterior, and anterior interfaces.31 The study was limited by low test subject numbers and short-term follow up.
Segmental meniscal deficiency treatment has also been described using either biological or synthetic meniscus scaffolds to promote fibrocartilaginous tissue regeneration and include either bovine Achilles tendon with enriched collagen fibers or synthetic polyurethane material that is slowly biodegradable.32 Much like the results for meniscus allograft transplantation, sample sizes are small; however, long-term clinical outcomes scores show significant improvement over partial meniscectomy alone with proper patient selection.13,29,32
The technique of segmental meniscus allograft transplantation has the potential benefits of restoring native contact forces within the knee, while preserving native meniscal tissue to potentially enhance biologic healing. Additionally, it is reproducible combining well-described fixation techniques and may be technically more reproducible than a complete meniscus allograft transplant. Short- and long-term outcomes with meniscal allograft transplantation have been favorable with proper patient selection and may be similar with segmental transplantation, but further clinical studies are needed.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: M.T.P. receives personal fees from Arthrex, Joint Research Foundation (JRF), SLACK Inc., and Arthrosurface; and is an editorial or governing board member for Arthroscopy, Knee, Orthopedics, and SLACK, as well as a board or committee member for AANA, AAOS, AOSSM, ASES, ISAKOS, the San Diego Shoulder Institute, and the Society of Military Orthopaedic Surgeons. A.F.V. receives personal fees from Arthrex, Smith & Nephew, and Vericel; and is a board or committee member for AOSSM and VJSM. J.A.G. receives support from Bioventus, Mitek, and Smith & Nephew; and is a board or committee member for ASES and AANA; and owns stock or options in Nice Recovery Systems. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Narrative description and video illustration of a 31-year-old female who underwent a right knee medial meniscus segmental transplantation along with revision anterior cruciate ligament reconstruction with Bone Patella Bone autograft.
References
- 1.Chahla J., Cinque M.E., Godin J.A., et al. Meniscectomy and resultant articular cartilage lesions of the knee among prospective National Football League players: An imaging and performance analysis. Am J Sports Med. 2018;46:200–207. doi: 10.1177/0363546517737991. [DOI] [PubMed] [Google Scholar]
- 2.Eichinger M., Schocke M., Hoser C., Fink C., Mayr R., Rosenberger R.E. Changes in articular cartilage following arthroscopic partial medial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 2016;24:1440–1447. doi: 10.1007/s00167-015-3542-7. [DOI] [PubMed] [Google Scholar]
- 3.Schimmer R.C., Brulhart K.B., Duff C., Glinz W. Arthroscopic partial meniscectomy: A 12-year follow-up and two-step evaluation of the long-term course. Arthroscopy. 1998;14:136–142. doi: 10.1016/s0749-8063(98)70031-3. [DOI] [PubMed] [Google Scholar]
- 4.Shelbourne K.D., Dickens J.F. Digital radiographic evaluation of medial joint space narrowing after partial meniscectomy of bucket-handle medial meniscus tears in anterior cruciate ligament-intact knees. Am J Sports Med. 2006;34:1648–1655. doi: 10.1177/0363546506288019. [DOI] [PubMed] [Google Scholar]
- 5.McDermott I.D., Amis A.A. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88:1549–1556. doi: 10.1302/0301-620X.88B12.18140. [DOI] [PubMed] [Google Scholar]
- 6.Baratz M.E., Fu F.H., Mengato R. Meniscal tears: The effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14:270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 7.Frank R.M., Cole B.J. Meniscus transplantation. Curr Rev Musculoskelet Med. 2015;8:443–450. doi: 10.1007/s12178-015-9309-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walker P.S., Erkman M.J. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975:184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
- 9.Souza R.B., Wu S.J., Morse L.J., Subburaj K., Allen C.R., Feeley B.T. Cartilage MRI relaxation times after arthroscopic partial medial meniscectomy reveal localized degeneration. Knee Surg Sports Traumatol Arthrosc. 2015;23:188–197. doi: 10.1007/s00167-014-2997-2. [DOI] [PubMed] [Google Scholar]
- 10.Chalmers P.N., Karas V., Sherman S.L., Cole B.J. Return to high-level sport after meniscal allograft transplantation. Arthroscopy. 2013;29:539–544. doi: 10.1016/j.arthro.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 11.Cole B.J., Dennis M.G., Lee S.J., et al. Prospective evaluation of allograft meniscus transplantation: a minimum 2-year follow-up. Am J Sports Med. 2006;34:919–927. doi: 10.1177/0363546505284235. [DOI] [PubMed] [Google Scholar]
- 12.Drobnic M., Ercin E., Gamelas J., et al. Treatment options for the symptomatic post-meniscectomy knee. Knee Surg Sports Traumatol Arthrosc. 2019;27:1817–1824. doi: 10.1007/s00167-019-05424-3. [DOI] [PubMed] [Google Scholar]
- 13.Novaretti J.V., Patel N.K., Lian J., et al. Long-term survival analysis and outcomes of meniscal allograft transplantation with minimum 10-year follow-up: A systematic review. Arthroscopy. 2019;35:659–667. doi: 10.1016/j.arthro.2018.08.031. [DOI] [PubMed] [Google Scholar]
- 14.Samitier G., Alentorn-Geli E., Taylor D.C., et al. Meniscal allograft transplantation. Part 2: Systematic review of transplant timing, outcomes, return to competition, associated procedures, and prevention of osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2015;23:323–333. doi: 10.1007/s00167-014-3344-3. [DOI] [PubMed] [Google Scholar]
- 15.Smith N.A., Parkinson B., Hutchinson C.E., Costa M.L., Spalding T. Is meniscal allograft transplantation chondroprotective? A systematic review of radiological outcomes. Knee Surg Sports Traumatol Arthrosc. 2016;24:2923–2935. doi: 10.1007/s00167-015-3573-0. [DOI] [PubMed] [Google Scholar]
- 16.Gilat R., Cole B.J. Meniscal allograft transplantation: Indications, techniques, outcomes. Arthroscopy. 2020;36:938–939. doi: 10.1016/j.arthro.2020.01.025. [DOI] [PubMed] [Google Scholar]
- 17.Lee S.J., Aadalen K.J., Malaviya P., et al. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006;34:1334–1344. doi: 10.1177/0363546506286786. [DOI] [PubMed] [Google Scholar]
- 18.Pollard M.E., Kang Q., Berg E.E. Radiographic sizing for meniscal transplantation. Arthroscopy. 1995;11:684–687. doi: 10.1016/0749-8063(95)90110-8. [DOI] [PubMed] [Google Scholar]
- 19.Yoon J.R., Kim T.S., Lim H.C., Lim H.T., Yang J.H. Is radiographic measurement of bony landmarks reliable for lateral meniscal sizing? Am J Sports Med. 2011;39:582–589. doi: 10.1177/0363546510390444. [DOI] [PubMed] [Google Scholar]
- 20.McConkey M., Lyon C., Bennett D.L., et al. Radiographic sizing for meniscal transplantation using 3-D CT reconstruction. J Knee Surg. 2012;25:221–225. doi: 10.1055/s-0031-1292651. [DOI] [PubMed] [Google Scholar]
- 21.Ambra L.F., Kaleka C.C., Debieux P., et al. Radiographic methods are as accurate as magnetic resonance imaging for graft sizing before lateral meniscal transplantation. Am J Sports Med. 2020;48:3534–3540. doi: 10.1177/0363546520963095. [DOI] [PubMed] [Google Scholar]
- 22.Moran T.E., Demers A.J., Shank K.M., Awowale J.T., Miller M.D. Percutaneous medial collateral ligament release improves medial compartment access during knee arthroscopy. Arthrosc Sports Med Rehabil. 2021;3:e105–e114. doi: 10.1016/j.asmr.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chahla J., Olivetto J., Dean C.S., Serra Cruz R., LaPrade R.F. Lateral meniscal allograft transplantation: The bone trough technique. Arthrosc Tech. 2016;5:e371–377. doi: 10.1016/j.eats.2016.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dean C.S., Olivetto J., Chahla J., Serra Cruz R., LaPrade R.F. Medial meniscal allograft transplantation: The bone plug technique. Arthrosc Tech. 2016;5:e329–335. doi: 10.1016/j.eats.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DeFrance M., Ford E., McMillan S. Arthroscopic medial meniscal transplant using multiple fixation techniques. Arthrosc Tech. 2019;8:e1025–e1029. doi: 10.1016/j.eats.2019.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spalding T., Parkinson B., Smith N.A., Verdonk P. Arthroscopic meniscal allograft transplantation with soft-tissue fixation through bone tunnels. Arthrosc Tech. 2015;4:e559–563. doi: 10.1016/j.eats.2015.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woodmass J.M., Johnson N.R., Levy B.A., Stuart M.J., Krych A.J. Lateral meniscus allograft transplantation: The bone plug technique. Arthrosc Tech. 2017;6:e1215–e1220. doi: 10.1016/j.eats.2017.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Seiter M.N., Haber D.B., Ruzbarsky J.J., Arner J.W., Peebles A.M., Provencher M.T. Segmental meniscus allograft transplantation. Arthrosc Tech. 2021;10:e697–e703. doi: 10.1016/j.eats.2020.10.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carter T.R., Brown M.J. Meniscal allograft survivorship and outcomes 20 years after implantation. Arthroscopy. 2020;36:2268–2274. doi: 10.1016/j.arthro.2020.04.029. [DOI] [PubMed] [Google Scholar]
- 30.Nyland J., Campbell K., Kalloub A., Strauss E.J., Kuban K., Caborn D.N.M. Medial meniscus grafting restores normal tibiofemoral contact pressures. Arch Orthop Trauma Surg. 2018;138:361–367. doi: 10.1007/s00402-017-2849-x. [DOI] [PubMed] [Google Scholar]
- 31.Strauss E., Caborn D.N.M., Nyland J., Horng S., Chagnon M., Wilke D. Tissue healing following segmental meniscal allograft transplantation: a pilot study. Knee Surg Sports Traumatol Arthrosc. 2019;27:1931–1938. doi: 10.1007/s00167-019-05355-z. [DOI] [PubMed] [Google Scholar]
- 32.de Caro F., Perdisa F., Dhollander A., Verdonk R., Verdonk P. Meniscus scaffolds for partial meniscus defects. Clin Sports Med. 2020;39:83–92. doi: 10.1016/j.csm.2019.08.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Narrative description and video illustration of a 31-year-old female who underwent a right knee medial meniscus segmental transplantation along with revision anterior cruciate ligament reconstruction with Bone Patella Bone autograft.
Narrative description and video illustration of a 31-year-old female who underwent a right knee medial meniscus segmental transplantation along with revision anterior cruciate ligament reconstruction with Bone Patella Bone autograft.